

Ascites Clinical Presentation
- Author: Rahil Shah, MD; Chief Editor: Praveen K Roy, MD, MSc more...
- Sections Ascites
- Pathophysiology
- Epidemiology
- Patient Education
- Physical Examination
- Approach Considerations
- Laboratory Studies
- Imaging Studies
- Medical Care
- Surgical Care
- Long-Term Monitoring
- Medication Summary
- Vasopressin-Related
- Questions & Answers
- Media Gallery
Patients with ascites often state that they have recently noticed an increase in their abdominal girth.
Because most cases of ascites are due to liver disease, patients with ascites should be asked about risk factors for liver disease. These include the following:
Long-term heavy alcohol use
Chronic viral hepatitis or jaundice
Intravenous drug use
Multiple sexual partners
Homosexual activity with a male partner, or heterosexual activity with a bisexual male
Transfusion with blood not tested for hepatitis virus: In the United States, screening of donated blood for hepatitis B virus (HBV) began in 1972; reliable testing of the blood supply for hepatitis C virus (HCV) began in 1992 in developed countries
Living or birth in an area endemic for hepatitis
Patients with alcoholic liver disease who alternate between heavy alcohol consumption and abstention (or light consumption) may experience ascites in a cyclic fashion.
When a patient with a very long history of stable cirrhosis develops ascites, the possibility of superimposed hepatocellular carcinoma ( HCC ) should be considered.
Obesity , hypercholesterolemia , and type 2 diabetes mellitus are recognized causes of nonalcoholic steatohepatitis, which can progress to cirrhosis.
Patients with a history of cancer, especially gastrointestinal cancer, are at risk for malignant ascites. Malignancy-related ascites is frequently painful, whereas cirrhotic ascites is usually painless.
Patients who develop ascites in the setting of established diabetes or nephrotic syndrome may have nephrotic ascites.
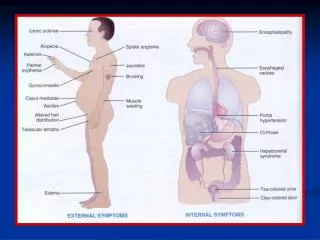
The physical examination in a patient with ascites should focus on the signs of portal hypertension and chronic liver disease. Note the following:
Physical findings suggestive of liver disease include jaundice, palmar erythema, and spider angiomas.
The liver may be difficult to palpate if a large amount of ascites is present, but if palpable, the liver is often found to be enlarged. The puddle sign may be present when as little as 120 mL of fluid is present. When peritoneal fluid exceeds 500 mL, ascites may be demonstrated by the presence of shifting dullness or bulging flanks. A fluid-wave sign is notoriously inaccurate.
Elevated jugular venous pressure may suggest a cardiac origin of ascites. A firm nodule in the umbilicus, the so-called Sister Mary Joseph nodule, is not common but suggests peritoneal carcinomatosis originating from gastric, pancreatic, or hepatic primary malignancy.
A pathologic left-sided supraclavicular node (Virchow node) suggests the presence of upper abdominal malignancy.
Patients with cardiac disease or nephrotic syndrome may have anasarca.
Chiejina M, Kudaravalli P, Samant H. Ascites. StatPearls [Internet] . 2023 Jan. [QxMD MEDLINE Link] . [Full Text] .
Pericleous M, Sarnowski A, Moore A, Fijten R, Zaman M. The clinical management of abdominal ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: a review of current guidelines and recommendations. Eur J Gastroenterol Hepatol . 2016 Mar. 28(3):e10-8. [QxMD MEDLINE Link] .
Weniger M, D'Haese JG, Angele MK, Kleespies A, Werner J, Hartwig W. Treatment options for chylous ascites after major abdominal surgery: a systematic review. Am J Surg . 2016 Jan. 211(1):206-13. [QxMD MEDLINE Link] .
CDC/National Center for Health Statistics. Chronic liver disease and cirrhosis. Centers for Disease Control and Prevention. January 17, 2023. Available at https://www.cdc.gov/nchs/fastats/liver-disease.htm . Accessed: May 30, 2023.
Raza S, Rajak S, Upadhyay A, Tewari A, Sinha RA. Current treatment paradigms and emerging therapies for NAFLD/NASH. Front Biosci (Landmark Ed) . 2021 Jan 1. 26(2):206-37. [QxMD MEDLINE Link] . [Full Text] .
Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol . 2019 Jan. 70(1):151-71. [QxMD MEDLINE Link] .
Fede G, D'Amico G, Arvaniti V, et al. Renal failure and cirrhosis: a systematic review of mortality and prognosis. J Hepatol . 2012 Apr. 56(4):810-8. [QxMD MEDLINE Link] .
Wallerstedt S, Olsson R, Simren M, et al. Abdominal tenderness in ascites patients indicates spontaneous bacterial peritonitis. Eur J Intern Med . 2007 Jan. 18(1):44-7. [QxMD MEDLINE Link] .
Tapper EB, Bonder A, Cardenas A. Preventing and treating acute kidney injury among hospitalized patients with cirrhosis and ascites: a narrative review. Am J Med . 2016 May. 129(5):461-7. [QxMD MEDLINE Link] .
Han CM, Lee CL, Huang KG, et al. Diagnostic laparoscopy in ascites of unknown origin: Chang Gung Memorial Hospital 20-year experience. Chang Gung Med J . 2008 Jul-Aug. 31(4):378-83. [QxMD MEDLINE Link] . [Full Text] .
Wong CL, Holroyd-Leduc J, Thorpe KE, Straus SE. Does this patient have bacterial peritonitis or portal hypertension? How do I perform a paracentesis and analyze the results?. JAMA . 2008 Mar 12. 299(10):1166-78. [QxMD MEDLINE Link] .
[Guideline] Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology . 2021 Aug. 74(2):1014-48. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Aithal GP, Palaniyappan N, China L, et al. Guidelines on the management of ascites in cirrhosis. Gut . 2021 Jan. 70(1):9-29. [QxMD MEDLINE Link] . [Full Text] .
Gallo A, Dedionigi C, Civitelli C, Panzeri A, Corradi C, Squizzato A. Optimal management of cirrhotic ascites: a review for internal medicine physicians. J Transl Int Med . 2020 Dec. 8(4):220-36. [QxMD MEDLINE Link] . [Full Text] .
Gines P, Cardenas A. The management of ascites and hyponatremia in cirrhosis. Semin Liver Dis . 2008 Feb. 28(1):43-58. [QxMD MEDLINE Link] .
Facciorusso A, Amoruso A, Neve V, Antonino M, Prete VD, Barone M. Role of vaptans in the management of hydroelectrolytic imbalance in liver cirrhosis. World J Hepatol . 2014 Nov 27. 6(11):793-9. [QxMD MEDLINE Link] . [Full Text] .
Bellot P, Welker MW, Soriano G, et al. Automated low flow pump system for the treatment of refractory ascites: a multi-center safety and efficacy study. J Hepatol . 2013 May. 58(5):922-7. [QxMD MEDLINE Link] .
Sola-Vera J, Minana J, Ricart E, et al. Randomized trial comparing albumin and saline in the prevention of paracentesis-induced circulatory dysfunction in cirrhotic patients with ascites. Hepatology . 2003 May. 37(5):1147-53. [QxMD MEDLINE Link] . [Full Text] .
[Guideline] Runyon BA, American Association for the Study of Liver Diseases. Management of adult patients with ascites due to cirrhosis: update 2012. National Guideline Clearinghouse. Available at https://guideline.gov/content.aspx?id=45103&search=ascites . Accessed: Nov 6, 2014.
Lata J, Marecek Z, Fejfar T, et al. The efficacy of terlipressin in comparison with albumin in the prevention of circulatory changes after the paracentesis of tense ascites--a randomized multicentric study. Hepatogastroenterology . 2007 Oct-Nov. 54(79):1930-3. [QxMD MEDLINE Link] .
Singh V, Kumar R, Nain CK, Singh B, Sharma AK. Terlipressin versus albumin in paracentesis-induced circulatory dysfunction in cirrhosis: a randomized study. J Gastroenterol Hepatol . 2006 Jan. 21(1 pt 2):303-7. [QxMD MEDLINE Link] .
Mercadante S, Intravaia G, Ferrera P, Villari P, David F. Peritoneal catheter for continuous drainage of ascites in advanced cancer patients. Support Care Cancer . 2008 Aug. 16(8):975-8. [QxMD MEDLINE Link] .
Courtney A, Nemcek AA Jr, Rosenberg S, et al. Prospective evaluation of the PleurX catheter when used to treat recurrent ascites associated with malignancy. J Vasc Interv Radiol . 2008 Dec. 19(12):1723-31. [QxMD MEDLINE Link] .
Sorrentino P, Castaldo G, Tarantino L, et al. Preservation of nutritional-status in patients with refractory ascites due to hepatic cirrhosis who are undergoing repeated paracentesis. J Gastroenterol Hepatol . 2012 Apr. 27(4):813-22. [QxMD MEDLINE Link] .
Guo TT, Yang Y, Song Y, Ren Y, Liu ZX, Cheng G. Effects of midodrine in patients with ascites due to cirrhosis: Systematic review and meta-analysis. J Dig Dis . 2016 Jan. 17(1):11-9. [QxMD MEDLINE Link] .
Seike M, Maetani I, Sakai Y. Treatment of malignant ascites in patients with advanced cancer: peritoneovenous shunt versus paracentesis. J Gastroenterol Hepatol . 2007 Dec. 22(12):2161-6. [QxMD MEDLINE Link] .
Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol . 2017 May. 28(5):1340-1349. [QxMD MEDLINE Link] . [Full Text] .
Liu YB, Chen MK. Epidemiology of liver cirrhosis and associated complications: current knowledge and future directions. World J Gastroenterol . 2022 Nov 7. 28(41):5910-30. [QxMD MEDLINE Link] . [Full Text] .
Tay PWL, Xiao J, Tan DJH, et al. An epidemiological meta-analysis on the worldwide prevalence, resistance, and outcomes of spontaneous bacterial peritonitis in cirrhosis. Front Med (Lausanne) . 2021. 8:693652. [QxMD MEDLINE Link] . [Full Text] .
- Ascites. This computed tomography scan demonstrates free intraperitoneal fluid due to urinary ascites.
- Ascites. Transjugular intrahepatic portosystemic shunt (TIPS).
- Ascites. Massive ascites.

Contributor Information and Disclosures
Rahil Shah, MD Consulting Staff, Lebanon Endoscopy Center Rahil Shah, MD is a member of the following medical societies: American College of Gastroenterology , American Society for Gastrointestinal Endoscopy Disclosure: Received consulting fee from Takeda for speaking and teaching.
Janice M Fields, MD, FACG, FACP Assistant Professor of Internal Medicine, Oakland University William Beaumont School of Medicine; Consulting Staff, Department of Internal Medicine, Section of Gastroenterology, Providence Hospital, St John Macomb-Oakland Hosptial Janice M Fields, MD, FACG, FACP is a member of the following medical societies: American College of Gastroenterology , American College of Physicians-American Society of Internal Medicine , American Gastroenterological Association , American Medical Association , American Society for Gastrointestinal Endoscopy , National Medical Association Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
Praveen K Roy, MD, MSc Clinical Assistant Professor of Medicine, University of New Mexico School of Medicine Praveen K Roy, MD, MSc is a member of the following medical societies: Alaska State Medical Association , American Gastroenterological Association Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Paracentesis
- Fast Five Quiz: How Much Do You Know About Hypothyroidism?
- Chylous Ascites
- Pediatric Surgery for Ascites
- An 18-Year-Old With Nausea and Increased Abdominal Girth
- Fast Five Quiz: What Do You Know About Hyponatremia?

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2002185777-overviewDiseases & Conditions Diseases & Conditions Chylous Ascites
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
A 22-year-old male patient with ascites.
A 22-year-old male patient presented with a 3-day history of abdominal pain, diarrhoea, nausea and vomiting. He reported abdominal distention of a couple of weeks’ duration. He had been hospitalised 7 months earlier, owing to the same symptoms, however, the cause was never clarified. Initial examination showed abdominal distention and blood tests indicated eosinophilia. An abdominal CT scan showed mild ascites and a diffuse thickening of the small intestinal loops, and a cystic formation 3 cm in diameter on the liver. The differential diagnosis included parasite infection and eosinophilic gastroenteritis. Liver MRI revealed a simple biliary cyst. Microbiological tests, stool and blood cultures as well as stool examination for parasites were negative. The diagnostic paracentesis revealed eosinophilic ascites. An endoscopy was performed and histopathology revealed presence of moderate to marked lymphoplasmacytic infiltrate containing eosinophils, compatible with eosinophilic gastroenteritis. The patient responded well to the initiation of corticosteroids.
This case illustrates a rare and heterogeneous condition with a varied presentation. It is characterised by eosinophilia, eosinophilic infiltration of the bowel wall and a wide variety of gastrointestinal symptoms. In fact, eosinophilic gastroenteritis (EG) should be suspected in any patient with gastrointestinal symptoms associated with peripheral eosinophilia. The diagnosis of EG is typically confirmed by endoscopic biopsies and/or eosinophilic ascites (EA). The symptoms are usually chronic and bothersome, with a relapsing course, but they can be successfully controlled with appropriate diagnosis and treatment. The aetiology of this disease remains unknown. It has been associated with food allergy, however, treatment with elimination diets gives poor results, while steroid therapy is effective in 90% of patients. A high index of suspicion is necessary as delays in diagnosis can result in unnecessary suffering.
Case presentation
A 22-year-old Bulgarian man presented with a 3-day history of abdominal pain, diarrhoea, nausea and vomiting. He also reported abdominal distention of a couple of weeks’ duration. He denied having choluria, acholia and haematemesis, as well as fever, night sweats, myalgia and weight loss. He had no history of atopy.
His medical history showed that he had been hospitalised in Bulgaria 7 months earlier, with the same symptoms, associated with ascites, however, the cause of the condition was never clarified despite considerable investigation.
On examination, the patient appeared dehydrated, but he was haemodynamically stable and afebrile. His abdomen was soft, but tender, with some guarding and rebound. No masses or organomegaly were palpated. On percussion, a shifting dullness was observed, which suggested ascites. Normal bowel sounds were present.
Initial investigations showed raised C reactive protein (1.13 mg/dL, reference range 0–0.5 mg/dL) and a white cell count of 13.7×10 9 /L (reference range 4.0–10.0×10 9 /L) at the expense of eosinophilia (3.4×10 9 /L; reference range 0.02–0.5×10 9 /L). An abdominal ultrasound scan showed diffuse thickening of the small intestinal loops, a large peritoneal effusion and a cystic formation of 3 cm in diameter on segment IV of the liver.
Investigations
The patient was hospitalised and laboratory testing showed maintained marked eosinophilia with normal blood count. Renal, hepatic and thyroid function as well as inflammatory markers were normal. Serology for hepatitis viruses and acquired immunodeficiency were negative. Research for parasites and their ova in stool, and coproculture were also negative. Tests for neoplastic markers were negative. An abdominal CT was carried out and the results revealed a cystic formation of 29 mm with a slight parietal enhancement in the IV segment, which was best characterised by liver MRI, which showed that it was a simple biliary cyst. Both imaging studies identified diffuse thickening of the small intestinal loops ( figures 1 and and2) 2 ) associated with multiple mesenteric lymph nodes, but with no criteria of adenopathy. An abdominal diagnostic paracentesis with ultrasound was performed and the patient's condition was found to be an EA with a serum-ascites albumin gradient (SAAG) of 0.8. Cytology identified reactive mesothelial cells and inflammatory cells with a predominance of polymorphonuclear cells with no neoplastic cells. Finally, the patient had an endoscopic study. Total colonoscopy showed no alterations, but the endoscopy identified erosive and erythaematous duodenal mucosa, so biopsies were performed. Histology from duodenal bulb and gastric antrum biopsies showed the presence in the lamina propria of moderate to marked lymphocytic infiltrates containing eosinophils, made evident by Congo Red, which in some areas had scores of 55–60/CGA: high magnification field high magnification field ( figure 3 ).

CT showing diffuse thickening of the small intestinal loops and considerable peritoneal effusion.

MRI showing diffuse thickening of the small intestinal loops.

Duodenal biopsy with lamina propria containing inflammatory infiltrate with eosinophils (Congo Red). These pathological findings are consistent with erosive duodenal mucosa (H&E, ×400).
Differential diagnosis
In this particular case, it was extremely important to first exclude a parasite infection. Cystic lesions of the liver represent a heterogeneous group of disorders. The abdominal ultrasound scan showed a hepatic cyst of 3 cm, which in association with abdominal pain, diarrhoea, nausea, vomiting and eosinophilia, can be indicative of a parasite infection. The ultrasound also showed diffuse thickening of the small intestinal loops and a large peritoneal effusion, which could indicate a complication of a parasite infection. Nevertheless, due to the diversity in clinical presentation of EG differentiation from primary hypereosinophilic syndrome, ascites syndrome, Crohn's disease and malignancies had to be investigated.
Systemic corticosteroids are the mainstay of therapy, and improve symptoms and endoscopic lesions dramatically in the vast majority of patients. So, prednisolone 40 mg/day was initiated.
Outcome and follow-up
Eight days after initiation of prednisolone, the patient had pain remission and normalisation of intestinal transit. He was discharged from hospital and was seen in medical consultation after a month. He remained asymptomatic with no ascites and blood tests showed clear improvement of eosinophilia. Therefore, corticosteroid weaning was started, without relapse to date.
EG is an uncommon disorder, first reported by Kaijser in 1937 as a disease that selectively affects the gastrointestinal tract, and characterised as eosinophil-rich inflammation of the gastrointestinal tract in the absence of known causes for eosinophilia. 1–4
Lesions can appear in the stomach and small intestine. A slight male preponderance has been reported. Although the disease can affect any age group, it mostly afflicts people between 30 and 50 years of age. Most affected individuals have a history of allergies, with some exhibiting eosinophilia and elevated serum IgE levels. 5 In 1970, Klein et al classified the disease according to the anatomic location of eosinophilic infiltration: the mucosal, muscularis and subserosal layers, once they noticed that the EG symptoms often differ depending on the location of eosinophil infiltration. 2 6 7 In fact, when the mucosa is in the primary inflammatory location, stomach ache, diarrhoea and/or weight loss are often noted. If the muscular layer is involved, nausea, vomiting and/or stomach ache may be the symptoms. 1 EA is common when the serosa is involved, and is probably the most unusual and rare presentation of EG. 4 7
In 80% of cases, EG is associated with increased eosinophils in the peripheral blood, and the biopsies of the area involved by the disease often reveal inflammatory cells composed primarily of eosinophils (>20–25/HPF) infiltrating mucous membranes. Several studies suggest a role of various cytokines, such as interleukin 3 and 4, granulocyte macrophage colony-stimulating factor and eotaxin, which are produced by eosinophils. Some studies also advocate that food allergens may play a role in local recruitment of eosinophils. 1 4
Knowledge of the case history, physical examination and paracentesis are essential for the differential diagnosis of EG.
A SAAG value ≥1.1 g/dL suggests with 97% accuracy a diagnosis of ascites secondary to portal hypertension. 8 However, our patient's paracentesis revealed a SAAG value of <1.1 g/dL, which indicates disease of the peritoneum, such as peritoneal carcinomatosis or peritoneal tuberculosis. The abdominal CT scan showed diffuse thickening of the small intestinal loops but without peritoneal implants, and the adenosine deaminase (ADA) level in the ascitic fluid was low, which excluded those diseases. The clinical history and physical examination were not suggestive of pancreatic ascites, intestinal obstruction or infarction, or biliary ascites. Renal function and serum albumin level were normal, so nephrotic syndrome or hypoalbuminaemia was not considered. Research for parasites and their ova in stool and coproculture were negative, rejecting intestinal parasites as the potential cause of the eosinophilia. Given that the paracentesis detected an EA, and a definitive diagnosis of EG requires histological evidence of eosinophilic infiltration, an endoscopic examination was performed. The biopsies of the duodenal bulb and gastric antrum noted moderate to marked lymphocytic infiltrates containing eosinophils. So, after careful investigation, the cause of abdominal pain, diarrhoea, nausea, vomiting and EA in our patient pointed to EG, which was supported further by the biopsy and a rapid clinical response to the steroid therapy. 7 9 10
In summary, EA is a rare presentation of EG and should be considered when diagnosing a young patient with refractory gastrointestinal symptoms, eosinophilia and ascites in the absence of liver disease.
Learning points
- Eosinophilic gastroenteritis (EG) is an uncommon disorder and should be considered in a patient with refractory gastrointestinal symptoms, eosinophilia and ascites.
- EG is a heterogeneous condition with several presentations, so a high index of suspicion is necessary.
- A definitive diagnosis of EG requires histological evidence of eosinophilic infiltration.
- It has been associated with food allergy, however, the treatment with elimination diets gives poor results, while steroid therapy is effective in 90% of patients.
Acknowledgments
The authors thank Dr Augusta Cipriano, anatomic pathologist in Centro Hospitalar e Universitário de Coimbra, EPE, who provided assistance, insight and expertise that greatly assisted the research.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Management of ascites in patients with cirrhosis
Jul 31, 2014
640 likes | 1.03k Views
Management of ascites in patients with cirrhosis. P. Angeli Dept. of Clinical and Experimental Medicine University of Padova. Treviso 4 Giugno 2009. MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS. 1. Compensated cirrhosis. %. 0,75. LT for cirrhosis. Responsive ascites. 0,5.
Share Presentation
- furosemide time
- different sodium intakes
- european liver transplant registry
- gastroenterology
- serum sodium

Presentation Transcript
Management of ascites in patients with cirrhosis P. Angeli Dept. of Clinical and Experimental Medicine University of Padova Treviso 4 Giugno 2009
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS 1 Compensated cirrhosis % 0,75 LT for cirrhosis Responsive ascites 0,5 0,25 Refractory ascites 0 12 24 36 48 60 months G. Fattovich et al. Gastroenterology 1997 ; 112 : 463-472 F. Salerno et al. Am. J. Gastroenterol. 1993 ; 88 : 514-519 European Liver Transplant Registry - 2008 Probability of survival in cirrhotic patients with ascites
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS FUNCTIONAL RENAL ABNORMALITIES IN CIRRHOSIS Abnormality Clinical consequence • Sodium retention • Water retention • Renal vasoconstriction • Ascites and edema • Dilutional hyponatremia • Hepatorenal syndrome
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Circulatory dysfunction in cirrhosis with ascites Portal hypertension/liver failure Increased release of NO, CO and other vasodilators Splanchnic arterial vasodilation Reduction of circulating volume Activation of systemic endogenous vasocontrictors Renal functional abnormalities
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Possible clinical scenario - Complicated ascites • Hyponatremia • Spontaneous bacterial peritonitis • Hepatorenal syndrome - Uncomplicated ascites • Refractory ascites K. Moore et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Treatment of uncomplicated ascites GRADE OF ASCITES TYPE OF TREATMENT • Grade 1 or minimal ascites • Grade 3 or massive ascites • No treatment • Paracentesis, sodium • restriction and diuretics Sodium restriction an diuretics Grade 2 or moderate ascites K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Effects of different sodium intakes on the response to high dose of spironolactone (%) P < 0.05 A. Gauthier, et al. Gut 1986 ; 27 : 705-709.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Effects of different sodium intakes on the response to diuretics M. Bernardi, et al. Liver 1993 ; 13 : 156-162.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Dietary sodium restriction • Dietary sodium intake should be moderately restricted to 90 mmol/day. • There is no indication for a more severe salt restriction. • The use of salt substitutes that contain potassium is contraindicated. • There is no indication for the prophylactic use of salt resctriction in patients who have never had ascites. K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Distal delivery of Na Sites of action of diuretics in the nephron Potassium sparing agents Thiazides Loop diuretics
P < 0.01 Cirrhotics with renal failure P. Angeli, et al. Hepatology. 1998 ; 28 : 937-943. MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Delivery of sodium to the distal tubule (Eq/min) P < 0.01 P. Angeli, et al. Eur. J. Clin. Invest. 1990 ; 20 : 111-117.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Fractional distal sodium reabsorption (%) P < 0.005 P. Angeli, et al. Eur. J. Clin. Invest. 1990 ; 20 : 111-117.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Correlation between aldosteronemia (PA) and hourly urinary sodium excretion (UNa) 10.0 r = 0.78 ; P < 0.001 Healthy subjects 5.0 UNa (mmol/hr) Cirrhotic patients 1.0 0.5 r = 0.94 ; P < 0.001 10 50 100 500 1000 PA M. Bernardi, et al. Gut 1983 ; 24 : 761-766.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Enrolled patients n = 40 Furosemide Spironolactone Responders = 11/20 Non-Responders = 10/20 Responders = 18/20 Non-Responders = 1/20 Responders = 0/1 Responders = 9/10 R.M. Perez-Ayuso, et al. Gastroenterology 1983 ; 84 : 961-968.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Enrolled patients n = 40 Amiloride Potassium canrenoate Responders = 7/20 Non-Responders = 13/20 Responders = 14/20 Non-Responders = 6/20 Responders = 2/6 Responders = 7/13 P. Angeli, et al. Hepatology 1994 ; 19 : 72-79.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Diuretics (1) • The core diuretic should be an aldosterone antagonist and this should be given once per day with food. • The aldosterone antagonist should be given at the initial dose of 100-200 mg/day. The diuretic dosage should be increased stepwise to a maximum of 400 mg/day in case of insufficient response. • Other potassium sparing diuretic (amiloride) are indicated only in those patients with adverse effects due to the aldosterone antagonist. K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Diuretics (2) • In clinical trials a loop diuretic was added (furosemide 20-40 mg/day) once a patient fails to respond to the aldosterone antagonist (sequential diuretic therapy). • The initial dose of furosemide may be increased in a stepwise manner to a maximum of 160 mg/day. K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Patients with spontaneous diuresis n = 6 (12%) Patients that required diuretic therapy = 45 (88%) Responders to spironolactone = 55 (56 %) Responders to spironolactone and furosemide= 18 (40 %) Patients with refractory ascites = 2 (4 %) Enroled patients n = 51 A. Gatta, et al. Hepatology 1991 ; 14 : 231-236.
Normal value MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Delivery of sodium to the distal tubule in sequential diuretic treatment P < 0.01 P < 0.01 (Eq/min) A. Gatta, et al. Hepatology 1991 ; 14 : 231-236.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Open question • Should we go on with sequential diuretic treatment or introduce combined diuretic treatment (aldosterone antagonist and loop diuretic) from the beginning ?
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between spironolactone alone and spironolactone plus furosemide Spironolactone 100-200 mg/day plus furosemide 40-80 mg/day Spironolactone 200-300 mg/day plus furosemide 80-120 mg/day Spironolactone 400 mg/day plus furosemide 120-160 mg/day Spironolactone 100-200 mg/day Spironolactone 200-300 mg/day Spironolactone 400 mg/day 4 days 4 days 4 days 4 days J. Santos, et al. J. Hepatol. 2003 ; 39 : 187-192.
Comparison between spironolactone alone and spironolactone plus furosemide Responders (%) P = N.S. J. Santos, et al. J. Hepatol. 2003 ; 39 : 187-192.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between spironolactone alone and spironolactone plus furosemide Time to obtain response (days) P = N.S. J. Santos, et al. J. Hepatol. 2003 ; 39 : 187-192.
MANAGEMENT OF PATIENTS WITH CIRRHOSIS Comparison between spironolactone alone and spironolactone plus furosemide Excessive response to diuretics (%) P < 0.0025 J. Santos, et al. J. Hepatol. 2003 ; 39 : 187-192.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between sequential versus combined diuretic treatment Potassium canrenoate 200 mg/day plus furosemide 50 mg/day Potassium canrenoate 400 mg/day plus furosemide 100 mg/day Potassium canrenoate 200 mg/day Potassium canrenoate 400 mg/day Potassium canrenoate 400 mg/day plus furosemide 50/day Potassium canrenoate 400 mg/day plus furosemide 100 mg/day 4 days 4 days 4 days 4 days 4 days 4 days Potassium canrenoate 400 mg/day plus furosemide 150 mg/day P. Angeli et al. AASLD 2007
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between sequential versus combined diuretic treatment Responders (%) P = N.S. P. Angeli et al. AASLD 2007
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between sequential versus combined diuretic treatment Adverse effects P. Angeli et al. AASLD 2007
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between sequential versus combined diuretic treatment Time to obtain response (days) P < 0.05 P. Angeli et al. AASLD 2007
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Comparison between sequential versus combined diuretic treatment Time to mobilize ascites (days) P < 0.001 P. Angeli et al. AASLD 2007
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Diuretics (3) • Diuretic dosage should be increased stepwise if there is an insufficient response as defined by a weight loss < 1 Kg in the first week or < 2 Kg every week thereafter until fluid balance is achieved. • The safe upper limit of weight loss is contentious. Most experts agree that the diuretic dosage should be adjusted to achieve a maximum rate of weight loss < 500 gr/day in patients without peripheral edema or < 1 Kg in those with peripheral edema. K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Diuretics (4) • Diuretics are contraindicated or should be stopped in patients with: • Severe hyponatremia (serum sodium < 125 mmol/l) • Progressive renal impairment • Worsening hepatic encephalopathy • Incapacitating muscle cramps • Hypokalemia (serum K < 3.5 mmol/l) stop furosemide • Hyperkalemia (serum K > 6.0 mmol/l) stop aldosterone antagonist. K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Treatment of uncomplicated ascites GRADE OF ASCITES TYPE OF TREATMENT • Grade 1 or minimal ascites • Grade 2 or moderate ascites • No treatment • Sodium resctriction and • diuretics Grade 3 or massive ascites Paracentesis, sodium resctriction and diuretics K. Moore, et al. Hepatology 2003 ; 38 : 258-266.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Therapeutic paracentesis versus diuretics in the treatment of massive ascites: efficacy P < 0.05 % P. Gines, et al. Gastroenterology 1987 ; 93 : 234-141.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Therapeutic paracentesis versus diuretics in the treatment of massive ascites: complications P. Gines, et al. Gastroenterology 1987 ; 93 : 234-141.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Therapeutic paracentesis versus diuretics in the treatment of massive ascites: duration of hospital stay (days) P < 0.001 P. Gines, et al. Gastroenterology 1987 ; 93 : 234-141.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Postparacentesis circulatory dysfunction (PPCD): plasma renin activity (ng/ml/h) * = P < 0.05 * L. Ruiz-Del-Arbol et al. Gastroenterology 1997 ; 113 : 579-586.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Percent decrease in systemic vascular resistance in patients with and without postparacentesis circulatory dysfunction (PPCD) % P < 0.05 with PPCD without PPCD L. Ruiz-Del-Arbol et al. Gastroenterology 1997 ; 113 : 579-586.
P < 0.01 allowing IAP go down after paracentesis MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Percent decrease in systemic vascular resistance in patients with ascites after paracentesis according to intra-abdominal pressure (IAP) keeping IAP constant after paracentesis J. Cabrera et al. Gut 2001 ; 48 : 384-389.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS B 48 h 1 d 1 mo 6 mos Plasma renin activity in patients without and with postparacentesis circulatory dysfunction (PPCD) (ng/ml/h) * = P < 0.0025; ** = P < 0.001 ** ** * B 48 h 1 d 1 mo 6 mos without PPCD with PPCD A. Gines et al. Gastroenterology 1996 ; 11 : 1002-1010.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Probability of survival in patients with and without postparacentesis circulatory dysfunction (PPCD) % without PPCD P = 0.01 with PPCD 2 4 6 8 10 12 14 16 18 months A. Gines et al. Gastroenterology 1996 ; 11 : 1002-1010.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Postparacentesis circulatory dysfunction: plasma renin activity (ng/ml/h) * * = P < 0.001 P. Gines et al. Gastroenterology 1988 ; 94 : 1493-1502.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Prevalence of postparacentesis circulatory dysfunction % P < 0.05 P < 0.025 A. Gines et al. Gastroenterology 1996 ; 11 : 1002-1010.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Liver-related complications frequency for a 100-day period after ascites removal by paracentesis R. Moreau, et al. Liver Int. 2006 ; 26 : 46-54.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Median cost for a 30-day period (Euro) after ascites removal by paracentesis P < 0.05 R. Moreau, et al. Liver Int. 2006 ; 26 : 46-54.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Prevalence of postparacentesis circulatory dysfunction: plasma renin activity (ng/ml/h) P = N.S. R. Moreau et al. Gut 2002 ; 50 : 90-94.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Ascites recurrence after therapeutic paracentesis versus diuretics (%) P < 0.001 G. Fernandez-Esparrach et al. J. Hepatol. 1997 ; 26 : 614-620.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Prevention of spontaneous bacterial peritonitis (SBP) • patients with cirrhosis and upper gastrointestinal hemorrhage • patients with cirrhosis and ascites recovering from an episode of SBP The prevention of SBP is recommended in: A. Rimola, et al. J. Hepatol. 2000 ; 32 : 142-153.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Probability of recurrence of spontaneous bacterial peritonitis (%) P < 0.01 Placebo Norfloxacin 4 8 12 16 20 months P. Gines et al. Hepatology 1990 ; 12 : 716-724.
or • impaired renal function (serum creatinine ≥ 1.2 mg/dl, BUN ≥ 25 mg/dl) or • serum sodium level ≤130 mmol/l MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Primary prevention of spontaneous bacterial peritonitis (SBP) • patients with cirrhosis and low protein ascitic level (15 g/l) and one of the following conditions: • advanced liver failure (CTP ≥ 9 with total serum bilirubin ≥ 3 mg/dl) J. Fernandez et al. Gastroenterology 2007 ; 133 : 818-824.
MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS Probability of development of spontaneous bacterial peritonitis (%) P < 0.001 Placebo Norfloxacin 100 200 300 400 days J. Fernandez et al. Gastroenterology 2007 ; 133 : 818-824.
- More by User
Management of Patients with Renal Disorders
Glomerular Diseases. Acute GlomerulonephritisChronic Glomerulonephritis Nephrotic Syndrome. Glomerulonephritis . Acute Glomerulonephritis. Preceded (10 days) by an infectionAssess for:LesionsSigns of circulatory overloadChange in urine color and amountMild to moderate hypertensionInterventions:Treat cause: antibiotics, corticosteroids, immunosuppressants Restrict sodium, water, potassium, protein Dialysis, plasmapheresisClient education .
1.16k views • 47 slides
Management of Rhinitis in Patients with Asthma
Management of Rhinitis in Patients with Asthma. Michael Schatz, MD, MS Chief, Department of Allergy Kaiser Permanente, San Diego, CA. Some Misconceptions About Rhinitis. Rhinitis is a trivial illness. All rhinitis is allergic. All non-allergic rhinitis is homogeneous .
746 views • 25 slides
Ascites and Renal Failure unresponsive to standard treatment in patients with cirrhosis
Ascites and Renal Failure unresponsive to standard treatment in patients with cirrhosis. Journal Club 23/09/2019. Ilaria Giovo. Refractory ascites. Prognosis. 1). 3). 4). 2). Treatment strategies. Definition. Diagnostic criteria. Diagnostic Criteria. Prognosis. Definition.
682 views • 38 slides
Treatment Selection for HBV-Infected Patients With Decompensated Cirrhosis
Treatment Selection for HBV-Infected Patients With Decompensated Cirrhosis . Robert S. Brown, Jr., MD, MPH Frank Cardile Professor of Medicine Chief, Center for Liver Disease Columbia University College of Physicians & Surgeons NewYork-Presbyterian Hospital New York, New York.
463 views • 23 slides
Ascites in Children
Definition. ? The word ascites is of Greek origin (askos) and means bag or sac.? Ascites describes the condition of pathologic fluid collection within the abdominal cavity. ? Healthy men have little or no intraperitoneal fluid, but women may normally have as much as 20 mL, depending on the phase
665 views • 32 slides
Pathophysiology of Ascites
Volume 350:1646-1654 April 15, 2004 Number 16 Management of Cirrhosis and Ascites Pere Ginès, M.D., Andrés Cárdenas, M.D., Vicente Arroyo, M.D., and Juan Rodés, M.D. Pathophysiology of Ascites
4.31k views • 58 slides

Management of Patients With Adrenal Disorders
Management of Patients With Adrenal Disorders. Dr. Belal M. Hijji, RN, PhD. Learning Outcomes. At the end of this lecture, students will be able to: Identify the composition and functions of the adrenal glands Discuss important aspects of common disorders of the adrenal glands. Introduction.
506 views • 20 slides
Management of patients with multiple trauma
Management of patients with multiple trauma . Prof. M K Alam MS; FRCS. ILO’s. Incidence of trauma Causes and types of trauma Timing and mode of death in trauma patients and its effect on trauma management. Pre-hospital care and triage Hospital care Primary survey and initial management
4.07k views • 112 slides
Ascites in the chronic renal failure patient with cirrhosis
Ascites in the chronic renal failure patient with cirrhosis. Dr.Rajeev Jayadevan MD (Vellore), DNB (Medicine), MRCP(UK), American Board Certification in Medicine American Board Certification in Gastroenterology Senior Consultant Gastroenterologist Sunrise Hospital.
1.04k views • 38 slides
Ascites ≈ most common complication of cirrhosis that leads to hospital admission
Ascites Nader Roushan Assistant Professor Department of internal medicine division of Gastroenterology Tehran University of Medical Sciences 21.10.92. Ascites ≈ most common complication of cirrhosis that leads to hospital admission 85%ascites in US≈ cirrhosis.
1.29k views • 40 slides
MANAGEMENT OF PATIENTS WITH THROMBOCYTOPENIA
MANAGEMENT OF PATIENTS WITH THROMBOCYTOPENIA. ELSHAMI M. ELAMIN, MD CENTRAL CARE CANCER CENTER. ITP DITP HIT TTP ITP during pregnancy. INTROCUCTION. Hemostasis encompasses a series of interrelated and simultaneously occurring events involving: B lood vessels P latelets
1.23k views • 82 slides
Management of Patients With Thyroid Disorders
Management of Patients With Thyroid Disorders. Dr. Belal M. Hijji, RN. PhD May 7 th & 9 th , 2012. Learning Outcomes. At the end of this lecture, students will be able to: Describe the thyroid gland, its functions, and hormones Examine relevant assessment and diagnostic studies.
1.12k views • 38 slides
Approach - Management of ascites in cirrhotic patients Dr . Khaled sheha
Approach - Management of ascites in cirrhotic patients Dr . Khaled sheha. Causes of ascites. Causative disorders Percentage Cirrhosis 85% PHT-related disorder 8% Cardiac disease 3% Peritoneal carcinomatosis 2% Miscellaneous non-PHT disorders 2%.
1.08k views • 38 slides
Pathohysiology of ascites
Pathohysiology of ascites. Waleed Al- hamoudi. Ascites. Ascites is of Greek derivation ("askos") and refers to a bag or sack and describes pathologic fluid accumulation within the peritoneal cavity. Most patients (85%) with ascites have cirrhosis.
725 views • 36 slides
Management of Patients With Musculoskeletal Disorders
Management of Patients With Musculoskeletal Disorders. Acute low Back pain:. Causes: A cut lumbosacral strain, unstable lumbosacral ligaments and weak muscles, osteoarithritis of the spine, spinal stenosis, intervertebral disk problems, and unequal leg length.
881 views • 52 slides
Management of hypertension in patients with diabetes
Management of hypertension in patients with diabetes. Prepared by the CHEP Implementation Task Force in collaboration with. Updated May 2011. The full slide set of the 2011 CHEP Recommendations are available at www.hypertension.ca.
836 views • 50 slides
Management of Infections in Cirrhosis
Fudan University Huashan Hospital Department of Infectious Diseases. Management of Infections in Cirrhosis. Wenhong Zhang, M.D. Department of Infectious Diseases, Huashan Hospital, Fudan University Shanghai, China. Stage of liver cirrhosis. Liver cirrhosis and Infections.
487 views • 31 slides
Portopulmonary hypertension and right heart failure in patients with cirrhosis
Portopulmonary hypertension and right heart failure in patients with cirrhosis. Portopulmonary hypertension and right heart failure in patients with cirrhosis. Antecedentes. Del 5-6% de los px con PortHTN tienen PVR Cirrosis GC y RVP P Vasculatura Pulmonar P. VD PVC
288 views • 12 slides
Problems in management of patients with PAOD
Problems in management of patients with PAOD. K.Roztocil IKEM, Prague 18 Eurochap Congress of the IUA and XIX Congress of the MLAVS, Palermo, October 24-27, 2009. Questions. Current situation in management of patients with PAD Less intensive treatment of risk factors in patients with PAD
579 views • 38 slides
Severity Index for patients with Liver Cirrhosis disease
Severity Index for patients with Liver Cirrhosis disease. Health Decision Analysis 730-001 Yokabid Worku [email protected] 02-19-04. Outline. Liver Cirrhosis and its measures of damage
300 views • 16 slides
Future treatment of patients with HCV cirrhosis
Future treatment of patients with HCV cirrhosis. Marc Bourlière Dept of Hepato -gastroenterology 5 th Paris Hepatitis Conference Saint Joseph Hospital, Marseille Paris, January 30 th 2012. Agenda.
360 views • 35 slides
Management of Patients With Epilepsy
Management of Patients With Epilepsy. Definition. Seizure Single provoked/unprovoked episode Epilepsy Two or more unprovoked seizures. Numbers….Numbers. Unprovoked seizure: Risk in US ~ 1/100 Epilepsy/Recurrent unprovoked seizures 8 th leading cause of morbidity
533 views • 47 slides

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
ASCITES By Dr WAQAR MBBS, MRCP Asst. Professor Maarefa College.
Published by Ervin Boros Modified over 6 years ago
Similar presentations
Presentation on theme: "ASCITES By Dr WAQAR MBBS, MRCP Asst. Professor Maarefa College."— Presentation transcript:

Management of ascites in cirrhosis
HEPATIC FAILURE TITO A. GALLA. HEALTHY LIVER LIVER FUNCTION METABOLISM DETOXIFICATION PROCESS PROTEIN SYNTHESIS MANUFACTURE OF CLOTTING FACTOR.

The EPEC-O Curriculum is produced by the EPEC TM Project with major funding provided by NCI, with supplemental funding provided by the Lance Armstrong.
Body Fluids and Infectious Complications. Body Fluids Intracellular Extracellular Plasma (fluid component of blood) Interstitial fluid (surrounds the.
Gastrointestinal & Hepatic- Biliary Systems Chapter 5 Part II.
Lucy Adkinson. Case history Reminder of different causes Update on recent NICE guidance.
Approach to peritoneal fluid analysis Dr Yasir M Khayyat Assistant Professor,Consultant Gastroenterologist Umm AlQura University.
For final year medical students 2014 Dr Rosalind Pool GPST1
Pleural, Pericardial and Peritoneal Fluids. Pleural, Pericardial and Peritoneal fluids, are fluids contained within closed cavities of the body. The fluid.
This lecture was conducted during the Nephrology Unit Grand Ground by Medical Student under Nephrology Division, Department of Medicine in King Saud University.
Complications of Liver Cirrhosis Ayman Abdo MD, AmBIM, FRCPC.
Pleural Effusion.
NYU Medical Grand Rounds Clinical Vignette Jeffrey Mayne, MD Third Year Resident Internal Medicine 1/17/2012 U NITED S TATES D EPARTMENT OF V ETERANS A.
Nursing Care of Clients with Gallbladder, Liver and Pancreatic Disorders Chapter 27.

Approach - Management of ascites in cirrhotic patients Dr. Khaled sheha.
Cirrhosis. * Definition: Chronic, diffuse, irreversible disorder of the liver characterized by loss of the normal liver architecture and replacement by.
Pleural diseases: Case Studies
Pleural Effusions.

ASCITES IT IS THE CONDITION OF PATHOLOGICAL ACCUMULATION OF FLUID IN ABDOMINAL CAVITY.

CASE PRESENTATION DR NADIA SHAFIQUE. CASE SUMMARY 38 yrs old female GULSHAN diagnosed case of HCV related DCLD (child class C) CTP score 11presented.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.

IMAGES
VIDEO
COMMENTS
Ascites. Case presentation . Epidemiology. Cirrhosis affects 3.6 per 1000 adults in the United States and is responsible for 26,000 deaths per year. Chronic liver disease represents the fourth leading cause of deaths among all races and sexes in the 45- to 54-year-old age group, exceeded only by malignancy, heart disease, and accidents. ...
History. Patients with ascites often state that they have recently noticed an increase in their abdominal girth. Because most cases of ascites are due to liver disease, patients with ascites should be asked about risk factors for liver disease. These include the following: Long-term heavy alcohol use. Chronic viral hepatitis or jaundice.
Ascites Case Presentation.ppt - Free download as PDF File (.pdf), Text File (.txt) or view presentation slides online. Sir, you have missed to mention examination of oral cavity and detailed abdominal examination on palpation. Please include those details. Prajna: Thank you for pointing that out. Let me include those details: ORAL CAVITY: - Lips are pale and dry - Oral mucosa is pale - No ...
The document discusses abdominal distention and ascites. It provides information on causes of abdominal distention including gas, fat, fluid, fetus, feces, and fatal growth. Ascites is defined as pathological accumulation of free fluid in the peritoneal cavity. Causes of ascites include cirrhosis, heart failure, nephritic syndrome, and cancer. A thorough history, physical exam, imaging ...
Download ppt "A RARE CASE OF ASCITES Dr. Siva Krishna DEPARTMENT OF MEDICINE" Similar presentations Presentation of History DR.H.N.SARKERMBBS,FCPS,MACP(USA)MRCP(LONDON) ASSOCIATE PROFESSOR MEDICINE.
Ascites Case Conclusions Presentation: This PowerPoint presentation concludes the ascites modules. The presentation is provided by an instructor and should be given to all of the students after the stations have been completed. Students are shown a brief series of summary slides pertaining to the past activities and original case.
Definition Pathological accumulation of fluid in abdominal cavity >50 ml. Pathophysiology of Ascites From: Robbins Basic Pathology. Causes of Ascites. Rare Causes of Ascites. Imaging • Ultrasound with Dopplers • Easily confirms ascites • May see nodularity of cirrhosis • Evaluate patency of vasculature • No radiation, contrast • CT ...
Presentation Transcript. Pathophysiology of Ascites The chief factor contributing to ascites is splanchnic vasodilatation. Increased hepatic resistance to portal flow due to cirrhosis causes the gradual development of portal hypertension, collateral-vein formation, and shunting of blood to the systemic circulation.
Case presentation. A 22-year-old Bulgarian man presented with a 3-day history of abdominal pain, diarrhoea, nausea and vomiting. He also reported abdominal distention of a couple of weeks' duration. He denied having choluria, acholia and haematemesis, as well as fever, night sweats, myalgia and weight loss. He had no history of atopy.
Ascites..ppt - Free download as Powerpoint Presentation (.ppt), PDF File (.pdf), Text File (.txt) or view presentation slides online. Scribd is the world's largest social reading and publishing site.
THE WHITE ARMY#ComprehensiveClinicalClassClinical case presentation - AscitesPresented by Ms.Prajna Bhushan, 4th Year MBBS, KoIMS, MadikeriMentor : Prof.C.R ...
Management of ascites in patients with cirrhosis P. Angeli Dept. of Clinical and Experimental Medicine University of Padova Treviso 4 Giugno 2009. MANAGEMENT OF ASCITES IN PATIENTS WITH CIRRHOSIS 1 Compensated cirrhosis % 0,75 LT for cirrhosis Responsive ascites 0,5 0,25 Refractory ascites 0 12 24 36 48 60 months G. Fattovich et al. Gastroenterology 1997 ; 112 : 463-472 F. Salerno et al. Am. J ...
Presentation on theme: "ASCITES By Dr WAQAR MBBS, MRCP Asst. Professor Maarefa College."—. Presentation transcript: 4 GRADES OF ASCITES1) Grade 1 : Mild ascites, only detected by ultrasound. Physical exam normal. 2) Grade 2: Moderate ascites, causing moderate abdominal & flank distension 3) Grade 3: Large ascites, causing huge abdominal ...
Ascites ppt - Free download as Powerpoint Presentation (.ppt), PDF File (.pdf), Text File (.txt) or view presentation slides online. This document discusses ascites and spontaneous bacterial peritonitis (SBP) in patients with cirrhosis. It outlines the pathophysiology of ascites development being related to increased resistance to hepatic flow and portal hypertension.
Ascites Presentation - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. This document summarizes ascites, which is fluid in the peritoneal cavity. It describes how ascites is graded based on the amount of fluid visible. It discusses how to assess ascites using physical exam maneuvers and lists the most common causes ...
Case Presentation (M. Fedor and D. Schwartz) The patient is a 58-year-old African American man with past medical history significant for a positive purified protein derivative (PPD) 2 years ago. No treatment was given. He was in his usual state of good health until 6 weeks before admission, when he became aware of breathlessness on mild exertion.