- Our Program Divisions
- Our Three Academies
- Government Affairs
- Statement on Diversity and Inclusion
- Our Study Process
- Conflict of Interest Policies and Procedures
- Project Comments and Information
- Read Our Expert Reports and Published Proceedings
- Explore PNAS, the Flagship Scientific Journal of NAS
- Access Transportation Research Board Publications
- Coronavirus Disease 2019 (COVID-19)
- Diversity, Equity, and Inclusion
- Economic Recovery
- Fellowships and Grants
- Publications by Division
- Division of Behavioral and Social Sciences and Education
- Division on Earth and Life Studies
- Division on Engineering and Physical Sciences
- Gulf Research Program
- Health and Medicine Division
- Policy and Global Affairs Division
- Transportation Research Board
- National Academy of Sciences
- National Academy of Engineering
- National Academy of Medicine
- Publications by Topic
- Agriculture
- Behavioral and Social Sciences
- Biography and Autobiography
- Biology and Life Sciences
- Computers and Information Technology
- Conflict and Security Issues
- Earth Sciences
- Energy and Energy Conservation
- Engineering and Technology
- Environment and Environmental Studies
- Food and Nutrition
- Health and Medicine
- Industry and Labor
- Math, Chemistry, and Physics
- Policy for Science and Technology
- Space and Aeronautics
- Surveys and Statistics
- Transportation and Infrastructure
- Searchable Collections
- New Releases
VIEW LARGER COVER

Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine
Antimicrobial resistance is a health problem that threatens to undermine almost a century of medical progress. Moreover, it is a global problem that requires action both in the United States and internationally.
Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine discusses ways to improve detection of resistant infections in the United States and abroad, including monitoring environmental reservoirs of resistance. This report sets out a strategy for improving stewardship and preventing infections in humans and animals. The report also discusses the strength of the pipeline for new antimicrobial medicines and steps that could be taken to bring a range of preventive and therapeutic products for humans and animals to the market.
RESOURCES AT A GLANCE
- Report Highlights
- Press Release
- Recommendations
COMMISSIONED PAPERS
- Background Analysis on Progress Toward Meeting Goals and Objectives in the National Action Plan for Combating Antibiotic-Resistant Bacteria (2015-2020)
- Health and Medicine — Health Sciences
- Health and Medicine — Public Health and Prevention
- Health and Medicine — Policy, Reviews and Evaluations
Suggested Citation
National Academies of Sciences, Engineering, and Medicine. 2022. Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine . Washington, DC: The National Academies Press. https://doi.org/10.17226/26350. Import this citation to: Bibtex EndNote Reference Manager
Publication Info
- Paperback: 978-0-309-26945-2
- Ebook: 978-0-309-26952-0
| Chapters | skim | |
|---|---|---|
| i-xxviii | ||
| 1-16 | ||
| 17-28 | ||
| 29-72 | ||
| 73-116 | ||
| 117-164 | ||
| 165-222 | ||
| 223-300 | ||
| 301-320 | ||
| 321-340 | ||
| 341-350 | ||
| 351-352 | ||
| 353-366 |
What is skim?
The Chapter Skim search tool presents what we've algorithmically identified as the most significant single chunk of text within every page in the chapter. You may select key terms to highlight them within pages of each chapter.
Commissioned Papers
Copyright information.
The National Academies Press (NAP) has partnered with Copyright Clearance Center's Marketplace service to offer you a variety of options for reusing NAP content. Through Marketplace, you may request permission to reprint NAP content in another publication, course pack, secure website, or other media. Marketplace allows you to instantly obtain permission, pay related fees, and print a license directly from the NAP website. The complete terms and conditions of your reuse license can be found in the license agreement that will be made available to you during the online order process. To request permission through Marketplace you are required to create an account by filling out a simple online form. The following list describes license reuses offered by the NAP through Marketplace:
- Republish text, tables, figures, or images in print
- Post on a secure Intranet/Extranet website
- Use in a PowerPoint Presentation
- Distribute via CD-ROM
Click here to obtain permission for the above reuses. If you have questions or comments concerning the Marketplace service, please contact:
Marketplace Support International +1.978.646.2600 US Toll Free +1.855.239.3415 E-mail: [email protected] marketplace.copyright.com
To request permission to distribute a PDF, please contact our Customer Service Department at [email protected] .
What is a prepublication?
An uncorrected copy, or prepublication, is an uncorrected proof of the book. We publish prepublications to facilitate timely access to the committee's findings.
What happens when I pre-order?
The final version of this book has not been published yet. You can pre-order a copy of the book and we will send it to you when it becomes available. We will not charge you for the book until it ships. Pricing for a pre-ordered book is estimated and subject to change. All backorders will be released at the final established price. As a courtesy, if the price increases by more than $3.00 we will notify you. If the price decreases, we will simply charge the lower price. Applicable discounts will be extended.
Downloading and Using eBooks from NAP
What is an ebook.
An ebook is one of two file formats that are intended to be used with e-reader devices and apps such as Amazon Kindle or Apple iBooks.
Why is an eBook better than a PDF?
A PDF is a digital representation of the print book, so while it can be loaded into most e-reader programs, it doesn't allow for resizable text or advanced, interactive functionality. The eBook is optimized for e-reader devices and apps, which means that it offers a much better digital reading experience than a PDF, including resizable text and interactive features (when available).
Where do I get eBook files?
eBook files are now available for a large number of reports on the NAP.edu website. If an eBook is available, you'll see the option to purchase it on the book page.
View more FAQ's about Ebooks
Types of Publications
Consensus Study Report: Consensus Study Reports published by the National Academies of Sciences, Engineering, and Medicine document the evidence-based consensus on the study’s statement of task by an authoring committee of experts. Reports typically include findings, conclusions, and recommendations based on information gathered by the committee and the committee’s deliberations. Each report has been subjected to a rigorous and independent peer-review process and it represents the position of the National Academies on the statement of task.

The Cancer Miracle Isn’t a Cure. It’s Prevention.
In the next few years, cancer will become the leading cause of death in the United States. Later in this century, it is likely to be the top cause of death worldwide. The shift marks a dramatic epidemiological transition: the first time in history that cancer will reign as humankind’s number-one killer.
It’s a good news/bad news story. Cancer is primarily a disease of aging, and the dubiously good news is that we are living long enough to experience its ravages. Cancer’s new ranking also reflects public health’s impressive gains against infectious disease, which held the top spot until the last century, and against heart disease, the current number one.
The bad news is that cancer continues to bring pain and sorrow wherever it strikes. Siddhartha Mukherjee titled his magisterial biography of cancer The Emperor of All Maladies , quoting a 19th-century surgeon. He left out the second part of the surgeon’s epithet: “the king of terrors.” Modern targeted treatments and immunotherapy have in some cases led to wondrous cures, and many malignancies are now caught early enough so that their sufferers can live out full lives. But advances in treatment alone will never be enough to fully stem the burden of cancer.
As every public health professional knows, on a population level, the only way to substantially reduce incidence and mortality for any disease is through prevention. And on a broad scale, we have made far less progress preventing cancer than preventing its predecessor scourges. We tamed infections with sanitation and vaccines, abetted by antibiotics. We tamed heart disease through smoking cessation, better medical management of risk factors such as high cholesterol, and improved interventions for a condition that has clear points of intervention and responds more readily to lifestyle changes.
Cancer is a different story. Even today, it continues to occupy our collective imagination as the king of terrors: insidious, capricious, relentless. Anyone who has suffered cancer, or has suffered alongside a loved one with the disease—a considerable portion of the population, given that more than one in three of us will be diagnosed with a malignancy during our lifetime—knows the anguish and helplessness that trail the diagnosis.
In 2015, a study in Science seemed to confirm our primal fear. It argued that only one-third of the variation in cancer risk in tissues is due to environmental assaults or inherited genetic predispositions. The majority of risk, the researchers concluded, was due to “bad luck”—random mutations during normal DNA replication.
And though that study provoked torrents of criticism about whether its conclusions based on tissue studies could be spun up to populations, it’s true that cancer is the price we pay as organisms composed of trillions of cells. Cell division is an imperfect process; like a biological keyboard with a letter missing, it makes mistakes. For that reason, it is unlikely that cancer could ever be eradicated.
The reality of cancer lies somewhere between the public health ideal of perfect prevention and the depressing stochastics of bad luck. Current research suggests that at least half of cancer cases—estimates range from 30 percent to upward of 70 percent—could be prevented by applying what we already know. The other half of cancer cases—including the elusive and often deadly types often caught too late to make a difference, such as ovarian, pancreatic, and brain tumors—could be detected and potentially even prevented far earlier if basic science and promising diagnostic technologies received the sustained government support they need.
Put simply, cancer must be framed not just as a curable disease but equally as a preventable one. “We will always need good treatments,” says Timothy Rebbeck , the Vincent L. Gregory, Jr. Professor of Cancer Prevention at the Harvard T.H. Chan School of Public Health and Dana-Farber Cancer Institute, and director of the School’s Zhu Family Center for Global Cancer Prevention . “But we can’t treat our way out of this problem. In order to make a dent in a public health sense, we must prevent cancer.”
A Grim Tally
In 2019, according to the American Cancer Society, an estimated 1,762,450 people will be diagnosed with cancer in the United States and an estimated 606,880 will die of the disease. Globally, cancer killed an estimated 9.6 million people in 2018—more than malaria, tuberculosis, and HIV combined. In this century, cancer will become not only the leading cause of death worldwide (in 91 nations it already ranks as the first or second cause of death before age 70, according to the World Health Organization) but also the single biggest hurdle to boosting life expectancy in scores of nations.
The reasons for cancer’s ascendancy are complex. Part of the trend is demographic: The human population is both growing and aging each year, meaning more people are vulnerable to the disease, which takes advantage of the waning immune system and the accumulated DNA damage that accompanies aging. But cancer’s chief risk factors are also changing. While smoking is down in the United States, for example, it is up in Africa and the Eastern Mediterranean, as tobacco companies expand into new markets. And while cigarette use is the most important risk factor for cancer worldwide, cancer-causing infections, such as hepatitis and the human papilloma virus (HPV)—both preventable with vaccines—account for up to 25 percent of cancer cases in some low- and middle-income countries.
These shifting sands of causation are also evident in the United States. Over the past 25 years, while cancer deaths have risen in number as the population grows, the cancer death rate has steadily declined. As of 2016, the cancer mortality rate for men and women combined had fallen 27 percent from its peak in 1991. The engine behind this impressive public health feat was the decline in smoking, though early detection and improved treatments also played a role. In 1965, 42 percent of U.S. adults were cigarette smokers; in 2017, just 14 percent. Lung cancer death rates declined in tandem, falling 48 percent from 1990 to 2016 among men and 23 percent from 2002 to 2016 among women.
That public health victory is now in peril. In the next five to 10 years, experts say, the cancer-causing effects of obesity could actually reverse the downward trend ushered in by the decline in smoking. Indeed, obesity could soon become the number-one risk factor for cancer in the United States and eventually around the world. And given obesity’s seeming irreversibility, thwarting cancer’s concomitant rise will be exceedingly difficult. In the U.S., 39.5 percent of adults are now estimated to be obese and an additional 31.8 percent overweight.
Obesity is a well-established risk factor for at least 13 cancers. According to a 2019 report in The Lancet Public Health , excess body weight in the U.S. accounted for up to 60 percent of all endometrial cancers, 36 percent of gallbladder cancers, 33 percent of kidney cancers, 17 percent of pancreatic cancers, and 11 percent of multiple myelomas in 2014.
Increasing obesity among younger people may portend a bigger wave of cancer in the near future, according to the The Lancet Public Health study. In the U.S., the incidence significantly increased for six obesity-related cancers in young adults, with each successively younger generation suffering a higher rate of cancer than the previous generation. These cancer cases serve as sentinels for future disease in older people. In light of rising rates of colorectal cancer among young adults, a trend suggesting environmental factors, the American Cancer Society last year lowered its recommended age for people’s first cancer screening, from 50 to 45.
Calculating the Benefits of Prevention
Two kinds of prevention can substantially reduce cancer deaths. The first, and most important, is primary prevention: averting a malignancy by attacking its causes and promoting the factors that protect against it. Taxes on cigarettes and alcohol, vaccination against cancer-causing pathogens such as HPV and hepatitis B, promoting healthy eating and regular exercise: All are examples of primary prevention. Primary prevention works when social and economic conditions, the built environment, and the public health and medical systems work in concert to support it.
Secondary prevention controls cancer by screening to detect the disease at its earliest stages and, if necessary, intervening early in the course of the disease’s progression. Secondary prevention has helped bring down death rates of breast, cervical, and colorectal cancers, among others.
Long-term epidemiological studies have clarified which cancers are preventable and by how much, if specific risk factors were reduced. A 2016 report in JAMA Oncology by the Harvard Chan School’s Ed Giovannucci , professor of nutrition and epidemiology, and Minyang Song , assistant professor of clinical epidemiology and nutrition, found that 20–40 percent of cancer cases and about half of cancer deaths could potentially be prevented through lifestyle modification, including quitting smoking , avoiding heavy alcohol drinking, maintaining a body mass index of 18.5 to 27.5 , and exercising at moderate intensity for at least 150 minutes or at a vigorous intensity for at least 75 minutes every week. (An additional bonus is that promoting cancer’s protective risk factors could also prevent other common noncommunicable diseases, such as type 2 diabetes, heart disease, dementia, and depression.)
A 2018 study in Science —co-authored by Song, Giovannucci, and Harvard Chan’s Walter Willett , professor of epidemiology and nutrition—made an even more emphatic case for prevention. It noted that for cancers in which most of the driving genetic mutations are caused by the environment—such as lung cancers, melanomas, and cervical cancers—85 to 100 percent of new cases could be eliminated through smoking cessation, avoidance of ultraviolet radiation exposures, and vaccination against HPV, respectively.
“With such further research, we envision that cancer death rates could be reduced by 70 percent around the world, even without the development of any new therapies,” the authors concluded. “Such a reduction, similar to that for heart disease over the past six decades, will only come about if research priorities are changed.” Specifically, the authors argue for more support of molecular, behavioral, and policy research on prevention.
Even individuals at high inherited genetic risk for cancer can benefit from lifestyle change, adds Peter Kraft , professor of epidemiology at the Harvard Chan School. In 2016, Kraft published a paper in JAMA Oncology showing that U.S. women who were in the highest decile of breast cancer risk because of factors they could not alter—mostly genetics but also family history, height, and menstrual and/or reproductive history—actually benefited the most from a healthy lifestyle. In fact, the women who had the highest nonmodifiable risk but also kept their weight down, did not drink or smoke, and did not use menopausal hormone therapy had about the same breast cancer risk as an average woman in the general population.
“Although our day jobs are studying the genetics of cancer, genetics is not destiny, by any means,” says Kraft. “This is something we’ve seen consistently across many cancers—and many diseases generally. Even if you’re high-risk based on your genetics, there’s still plenty that you can do to reduce your risk. In fact, high-risk individuals are the people who seem to reap the biggest benefit from adopting healthy lifestyles.”
Cancer Clues across Two Dimensions
Should anyone still doubt that many cancers are preventable, the inarguable proof is how the disease plays out over time and space. Cancer rates and types can starkly change within a country and starkly vary between countries. These variations are not genetic—a small minority of cancers are directly attributable to known, death-dealing DNA mutations. Rather, they reflect external—and, in principle, modifiable—risk factors.
For example, lung cancer eclipsed all other cancers during most of the 20th century in the United States because per capita cigarette consumption shot up from 54 cigarettes a year in 1900 to 4,345 cigarettes in 1963, then fell to 2,261 in 1998. The initial upward trend was powered by corporate profiteering. The downward slope was powered by the landmark 1964 U.S. Surgeon General’s report on smoking and health, which firmly linked smoking and lung cancer and led to public education, indoor smoking bans, and higher tobacco taxes. Another instance of a breathtaking prevention success within a country took place in the 1980s and 1990s in Taiwan, which saw an 80 percent decline in liver cancer rates in birth cohorts that received hepatitis B vaccination early in life. (The most common causes of liver cancer are infection with the hepatitis B virus in Africa and East Asia, and the hepatitis C virus in the U.S. and Europe.) And Australia recently reported it is on course to completely eliminate cervical cancer in the coming decades through vaccinations.
The spatial dimension of cancer is equally revealing. When racial or ethnic groups migrate from one part of the world to another, their cancer risks quickly take on the local patterns. Between 1975 and 2003, for example, numerous studies looked at cancer incidence in U.S. Caucasians, immigrant groups, and matched controls. Among the populations studied were first- and second-generation Japanese immigrants, Asian American women, Vietnamese Americans, and Hmong refugees from Vietnam, Laos, and Thailand. Drawing on data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program, the studies found that the kinds of cancers that were newly diagnosed among first-generation immigrants in the U.S. were nearly identical to the kinds in their native countries. But over subsequent generations, their cancer patterns became distinctly American. This was especially true for cancers related to hormones, such as breast, prostate, and ovarian cancers, and to cancers attributable to Westernized diets, such as colorectal malignancies.
Understanding Cancer’s Genesis
Given the fact that many cancers can be averted, what would it take to make the dream of prevention a reality?
First, scientists say, we must understand the earliest biological events that give rise to the birth of a cancer cell. While genomic analyses have provided a good molecular description of cancer, researchers still don’t understand how and when cells start to go rogue.
“Cancer initiation is much less well understood than the biology of cancer cells themselves,” says Brendan Manning , professor of genetics and complex diseases at the Harvard Chan School. “Cancer cells are doing things that normal cells do, only in an uncontrolled manner. So, how is cancer initiated? What are the brakes on early cancer? What are the challenges that the cancer cell faces in becoming a cancer cell? How does the cancer cell remove enough of those brakes so that it will become malignant?” Answering those questions will also shed light on the mechanisms by which apparent cancer risk factors, such as aging or obesity or chronic inflammation, trigger uncontrolled cell growth and progression to cancer, says Manning.
Manning’s lab explores how the body’s cells and tissues sense nutrient shifts in their local environment and adapt accordingly. “The cells in our body have the ability to acclimate to changes in nutrient availability, and this is achieved through special lines of communication—referred to as nutrient sensing pathways—that serve to tune cell metabolism to match these changes,” he says. “Understanding these fundamental mechanisms has provided us with key insights into how nutrient sensing becomes corrupted in human cancers, which universally exhibit alterations in cellular metabolism that underlie uncontrolled growth.”
Another biological unknown is the role of the microbiome—the trillions of microbes in and on our bodies—in human cancer. “These living organisms can at times be found right at the site of the cancer,” says Wendy Garrett , professor of immunology and infectious diseases at the Harvard Chan School. “We are beginning to see very provocative associations between the microbiome and cancer, and interesting molecular mechanisms—which are emerging from experiments with cells and in tissue cultures and preclinical mouse models—may explain these associations.”
One intriguing culprit on which Garrett and her colleagues are focusing is Fusobacterium nucleatum , normally a microbial denizen of the mouth. Garrett’s lab and others have shown that the bacterium is abundant in colon tumors. She wants to find out why, whether such bacteria are important early signals for carcinogenesis, and if any interventions—such as changing one’s everyday behaviors and exposures, including diet and tobacco use—map onto the microbiome and could potentially halt the disease process.
The microbiome is proving to be a vast and inviting landscape in cancer biology. In humans, gum disease caused by bacterial infections has been connected to higher risk of pancreatic cancer. In mice, lung tumors appear to alter nearby bacterial populations to help the tumors thrive—and antibiotics appear to shrink the tumors. Experiments in mice have even linked a disrupted gut microbiome to greater risk of invasive breast cancer.
“It’s possible that the cancers for which we currently don’t fully understand risk factors—such as pancreatic and ovarian cancer—might be tied to infections and therefore be preventable,” says Giovannucci. “Forty years ago, we didn’t know what caused stomach cancer. Now we know: the bacterium Helicobacter pylori .” H. pylori is treatable with antibiotics, and stomach cancer rates have dropped considerably as a result.
Prevention via Detection
With many tumors, there is a lag time of 20 years or more between the development of the first cancer cell and the onset of end-stage metastatic disease. Knowing each cancer’s basic biology could lead to a host of new technologies that register early biomarkers of the disease, potentially opening up new ways to head off malignancy before it spreads. That prospect would be transformative for the implacable cancers that don’t cause symptoms until they have reached their late and often incurable stages.
Among these promising biomarkers are proteins that signal early tumors, DNA or RNA, small molecules, circulating tumor cells, immune cells, and other infinitesimal biological entities. Scientists are also fashioning synthetically engineered biomarkers that harness the body’s own biology to spin off early signals of disease. “It’s a matter of screening technology getting refined enough so that you can find two suspicious molecules in four liters of blood which suggest you are at risk for or have already developed cancer,” says Rebbeck.
Sangeeta Bhatia, a biomedical researcher and early-detection pioneer, and the John J. and Dorothy Wilson Professor of Engineering at the Massachusetts Institute of Technology, injects nanoparticles into the bloodstream that respond to cancer-associated enzymes. When the particles find the enzyme for which they are designed, a chemical reaction produces “reporters”: synthetic chemicals eliminated in the urine that can tip off researchers to a nascent malignancy. Her lab is searching for highly specific biomarkers for often-elusive tumors of the ovary and lung and in colon metastasis. Clinical trials for the technology will begin later this year.

“Ultimately, we’d like to be in a place where you could do a urine test on a paper strip for a defined set of cancers,” Bhatia says. Other scientists envision, in the more distant future, continuous monitoring of cancer risk through smart toilets, wearables such as diagnostic imaging bras, and other passive and noninvasive technologies.
In clinical medicine, the value of screening tests is gauged by their sensitivity and specificity. Sensitivity measures a test’s ability to identify people who have the condition that is being tested for; a highly sensitive test will not generate false-negative results. Specificity measures a test’s ability to identify people who do not have the condition that is being tested for; a highly specific test will not generate false-positive results.
All the futuristic approaches described above require knowing that a technology’s molecular quarry is made by a certain kind of cancer cell and only that cancer cell—that is, the screening test must be highly specific. Since many tiny malignancies never go on to become metastatic disease—because the immune system reins in such cells—the ideal biomarker would not only tip off doctors to the presence of a cancer or precancer but also predict whether the suspect cells are aggressive or slow-growing. “[O]ne can imagine a day when healthy individuals are routinely tested for these biomarkers to detect early cancers, along with lipid concentrations to detect early cardiac disease, at periodic visits to their physicians,” the Harvard Chan School scientists wrote in Science in 2018.
Before liquid biopsies, “smart tattoos” that light up in the presence of cancer cells, small ingestibles that monitor the gastrointestinal tract, and other early-detection tests that sample blood, urine, saliva, or the breath can ever become part of the annual physical, they will have to be honed to the point of 99.9 percent accuracy or higher, similar to the accuracy of the early-pregnancy urine tests available at any drugstore. That is, they must be both highly sensitive and highly specific. This high degree of accuracy prevents false negative or false positive results when the test is used in large numbers of people.
Such tests could also help doctors decide whom to monitor more closely for cancer. “Advances in biomarker testing could help us better risk-stratify the population,” says Jane Kim, professor of health decision science at the Harvard Chan School. “The whole point of screening is to pull out the people who are at lowest risk and focus your attention on those at highest risk. Today, with cervical and even colorectal cancer, there is a prevention mechanism: You remove precancerous lesions before they develop into cancer. But with breast cancer, you need early detection, because there are no really strong prevention mechanisms. Risk-stratifying patients would help efficiently identify high-risk patients through prevention and early detection.”
Validating today’s candidate biomarkers will partly depend on long-term cohort studies—such as the Nurses’ Health Study —that have followed healthy volunteers over decades, collected biological material from these volunteers, and tracked the natural course of diseases as the participants aged. To speed the clinical validation of such early diagnostic tests, researchers will first try them out on people at high genetic risk for various cancers, for whom the tests have a higher likelihood of detecting an abnormality and making an impact.
“Combining basic science and cohort studies would also facilitate the discovery and validation of new biomarkers,” says Manning. “If you’re banking molecular information from blood and tissue, and the data changes over time, you can look back retrospectively at thousands of patient outcomes and see if the changes predicted an outcome or might be related to that outcome. Basic science holds the key to determining how that identified biomarker links back to the disease state and whether it is contributing to the disease’s onset—perhaps as a risk factor—or is a consequence of the disease.”
But being able to find an early cancer or predict its progression is not enough. “The key thing is that you have an intervention and that it’s actionable,” says Rebbeck. Such interventions might include surgery, cancer vaccines, anti-inflammatory drugs, a standard chemoprevention treatment, tinkering with the body’s microbiome, or even lifestyle change. “If you detect an early cancer biomarker but cannot act on it, then it may just produce anxiety,” he says. “There is a quote from Sophocles that we sometimes use: ‘Knowledge is but sorrow when wisdom profits not.’”
From Science to Action
Just as crucial will be translating new scientific insights into public health practice—a field known as implementation science. “Public health impact is efficacy times reach,” says Karen Emmons , professor of social and behavioral sciences at the Harvard Chan School. “We often develop interventions without thinking about the end users and what could get in the way of true impact, so shame on us as a field. As a scientific community, we think, rather arrogantly, ‘Well, we’ve shown that colorectal cancer screening is important—why don’t community health centers just make sure that everybody has colorectal cancer screening? It’s clear that vaccines are important—why aren’t all kids getting HPV vaccine?’ But the real question is: How do you structure systems to make those goals possible?”
Today’s cancer prevention and detection efforts regularly fall short in their impact. Although HPV vaccination administered in preadolescence, before a teen becomes sexually active, theoretically prevents some 90 percent of cervical cancers, the U.S. vaccination rate among adolescents is low. In 2017, only 42 percent of girls and 31 percent of boys received the two recommended doses before their 13th birthday. Similarly, in 2015, only 50 percent of women ages 40 years and older reported having a mammogram within the previous year, and only 64 percent within the previous two years.
Even the most well-established intervention against the most formidable cancer threat in the U.S.—lung cancer—is only fitfully used. “For some time after we started doing lung cancer screening for smokers, we didn’t also do smoking cessation with them,” says Emmons. “Even today, we still do it inconsistently. Now how stupid is that?”
Alan Geller , senior lecturer on social and behavioral sciences at the Harvard Chan School, has seen up close how the failure to translate science into action and policy leads to health disparities. “All of my work now is trying to ask the big question of who unnecessarily dies from preventable diseases,” he says. “Smoking rates are at best stabilizing among low-income people in the U.S.—but they’re stabilizing at 30 to 33 percent of the adult population. Among the well-to-do, smoking rates have for years been well below 10 percent. It’s not a racial disparity —it’s an income disparity, because the smoking rate among whites and African Americans is exactly the same. So we should target low-income people. Public health needs to go where high-risk people are.”
Geller adds that with smoking, four strategies could substantially reduce cancer deaths. “First would be to work really hard in the U.S. South, where smoking rates are double those in the North. Second would be working among people with mental health issues, because 41 percent of all smokers have diagnosed mental health conditions. Third would be figuring out how we could intervene with people who have GEDs [general education diplomas, also known as high school equivalency certificates]; 14 million people in the United States have one, and as a group their smoking rates are 40 percent. And fourth would be working with people in public housing—figuring out how their doctors and housing providers can give them access to nicotine replacement therapy, which is extraordinarily inexpensive, and how they can use community health workers and patient navigators. Those are all beautiful, low-cost, public health models for smoking cessation and lung cancer prevention.”
It’s almost a public health truism that when breakthrough medical advances hit the market, they disproportionately benefit people of means and thus widen health disparities. This divide is brutally apparent with cancer. From 2012 to 2016, for example, death rates in the poorest U.S. counties were two times higher for cervical cancer and 40 percent higher for male lung and liver cancers compared with rates in the richest counties. Poverty is also linked with lower rates of routine cancer screening, later stage at diagnosis, and a lower likelihood of receiving the best treatment.
“There are still parts of this nation where the rates of cervical cancer mirror those in developing countries—not developed countries,” notes Susan Curry, distinguished professor of health management and policy and dean emerita of the College of Public Health at the University of Iowa, and immediate past chair of the U.S. Preventive Services Task Force. “Are there barriers to screening within the population eligible to be screened? Are there barriers in terms of the organization and availability of screening? Are there barriers in terms of, you can get screened, but if you don’t have the means to follow up on a positive test or don’t understand what that is, then screening is for naught? We can pinpoint some pretty disturbing disparities. But how much are we investing in the intervention science that we need to close those gaps?”
These divergences are writ larger on the global stage. Earlier this year, The Lancet Global Health published a damningly titled article: “Cervical cancer: lessons learned from neglected tropical diseases.” The malignancy claims 310,000 lives annually around the globe, making it the fourth-most-common cancer killer of women. “[C]ervical cancer is not a disease of the past—it is a disease of the poor,” the authors state. They go on to list the hurdles that cervical cancer—which could virtually be eliminated from the planet with vaccination and screening—shares with neglected tropical diseases: Both accompany poverty; strike populations mostly overlooked by policymakers; are associated with stigma and discrimination; strongly affect female morbidity and mortality; tend to be neglected in clinical research and technological development; and can be controlled, prevented, and conceivably eliminated through currently available solutions that are cheap and effective.
It’s worth noting that in Africa, more people die from cancer than from malaria . And while overall cancer death rates have been rising in Africa—and will double in the next 20 years—malaria death rates are dropping because of concerted efforts to prevent and treat the infection.
A 2009 study in the journal Cancer Epidemiology, Biomarkers & Prevention underscored the fact that the newest and best cancer preventions disproportionately benefit people of means. The study found that the more knowledge, technology, and effective medical interventions there are for a given disease—that is, the more amenable a disease is to early detection and cure—the wider its disparities, because people who have knowledge, income, and useful social relations stand a better chance of surviving. By contrast, with diseases where effective medical interventions are absent or negligible, such as ovarian or pancreatic cancers, social and economic resources are of limited use, and survival differences between the most and least socially advantaged people are minimal.
“When you look at cancers that are preventable, as soon as something comes online to screen or prevent, you start to get pretty sharp disparities by race, ethnicity, and income,” says Emmons. “Colon cancer is a great example. Before sigmoidoscopy and colonoscopy screening came on board, there were actually slightly higher rates of colon cancer in whites than there were in blacks. Literally within three years after these screening tools were introduced, colon cancer rates among whites fell dramatically, but the rates in blacks did not. You see this over and over again.”
Such health inequities represent lives lost to cancer. When Emmons looks at new technologies, she asks: “What is the user perspective? How will the new technology interface with places where lower-income populations get their care? What does the technology mean for population health management, as opposed to managing the health of an individual? If you don’t pay attention to how these technologies are utilized across racial and economic lines, you wind up with persistent disparities that we shouldn’t tolerate.”
The Prevention Mindset
In the 1970s, a New Yorker cartoon depicted two stereotypical (for that era) male scientists standing before a blackboard scrawled with complicated equations. In the middle of these obscure scribbles is the phrase: “THEN A MIRACLE OCCURS….”
So it goes with cancer. “A cure for cancer” is our cultural synonym for a miracle. But as Curry points out, “We’re still waiting for that miracle.” When cancer treatments work, as they increasingly do, they seem indeed miraculous. But often, they come too late. The real miracle would be to prevent cancer from ever striking.
“Prevention is very hard,” Rebbeck concedes. “People want to think about cure. They say we need to cure cancer—and if someone has cancer, you absolutely want to cure it. But what’s not gotten into the public mindset is that we need to prevent cancer so that nobody needs to be cured.”
“For decades, success in cancer control has been ‘just around the corner,’” wrote Tom Frieden, the then-commissioner of the New York City Department of Health and Mental Hygiene, in 2008 in The Oncologist . Frieden, who went on to lead the U.S. Centers for Disease Control and Prevention (CDC), added, “Yet, to wage a true war on cancer, we must expand our approach to give preventive interventions at least as much focus as medical treatment.” Pointedly, he added that such a goal would require correcting the imbalance between “money invested in cancer treatment and money invested in cancer prevention.”
Currently, those two streams of funding are wildly unequal. In fiscal year 2018, the last year for which data is available, only 5.7 percent of the National Cancer Institute (NCI) budget was allotted to cancer prevention and control. Today, even the money for treatment research and other programs may be whittled back. The proposed fiscal year 2020 budget for the NCI is $5.2 billion—nearly $900 million less than the enacted 2019 budget. At the CDC, the proposed budget for cancer prevention and control was trimmed by more than $34 million—a 9 percent cut from last year. Globally, cancer prevention research is allotted an estimated 2 to 9 percent of global cancer research funding.
“The biggest unknown in cancer prevention is how to sustain proven, effective, and lifesaving preventive efforts over the long run,” says Howard Koh , the Harvey V. Fineberg Professor of the Practice of Public Health Leadership at the Harvard Chan School and the Harvard Kennedy School; former assistant secretary for health for the U.S. Department of Health and Human Services; and former commissioner of public health for the Commonwealth of Massachusetts. “Prevention should be integral, not optional. But in government, prevention budgets are always the first items to be cut and the last to be restored.”
Some researchers go so far as to argue that government research funding should be shifted somewhat from treatment to prevention—because solving the front end of the problem will save countless more lives. Others disagree, arguing that cancer will never go away completely and that, even today, we only know how to prevent about half of cancer cases. “You can take the pie and divide it differently or increase the pie,” says Curry. She would like to see more support for front-line public health. “Clearly, we need more dissemination science. There’s a huge gap between what we know and what we do.”
Manning insists that bench science is just as important in prevention. “In most cases, the biggest breakthroughs in biomedical research, including cancer biology, are made using reductionist approaches in which you’re isolating one aspect of the broader biology,” he says. “Stripping a biological problem down to its essence is key. We need to keep funding research that allows us to understand with detail and accuracy the aspects of biology that are important for cancer initiation. But right now, there is an overemphasis at the NIH [National Institutes of Health] and at NCI on supporting research that purports to be directly translatable or is seemingly translatable to treatment for an existing cancer, rather than on understanding how cancer begins.”
Shoe-leather population research and high-tech bench science: Both will be needed to stop cancer’s unabated rise.
Shaping Public Opinion
Desperate entreaties for increased support of cancer prevention are nothing new. In 1929, James Ewing, the director of cancer research at Memorial Hospital in New York City, wrote in Public Health Reports : “It is only within the last few years that cancer has been considered a public health problem. I suppose that the old attitude was due to the fact that cancer is not an infectious disease; also largely because of the popular notion that it is not preventable; and probably also, to a large extent, to the feeling, fairly well grounded, that the disease is incurable.” Ewing hoped for a change in public attitudes. “[C]ancer is a public health problem of the first importance, because many of the forms of cancer are preventable, and if the public were thoroughly informed, a definite reduction in the incidence of cancer might follow.”
Ninety years later, most people still do not grasp that point. Nor do they see that with robust research, the incidence of today’s more elusive and frightening cancers could also fall. In the 2017 American Institute for Cancer Research’s Cancer Risk Awareness Survey, for example, fewer than half of Americans recognized that alcohol, processed meat, high amounts of red meat, low amounts of fruits and vegetables, and not enough physical activity all have clear links to cancer development. And contradicting scientific evidence, they tended to blame cancer on factors they couldn’t control rather than on those they could. Nuclear power ranked eighth as a perceived cause of cancer, for example, and food additives ninth. Obesity—which may soon become the top modifiable risk factor for cancer—ranked 16th.
As Frieden explained in 2008 in The Oncologist , cancer-causing agents “are not primarily trace chemicals found in food, water, or air, but instead are the major constituents of what humans consume voluntarily. These agents are best viewed as toxins, and public policies can substantially reduce our exposure to them.”
A Moon Shot for Prevention
In 1969, the Citizens Committee for the Conquest of Cancer, inspired by the success that year of the Apollo 11 space mission and propelled by the indomitable philanthropist Mary Lasker, conceived of a “moon shot” for cancer. That December, the group ran a full-page ad in The Washington Post and The New York Times : “Mr. Nixon: You can cure cancer.” At the time, a cure was perceived to be imminent.

President Richard Nixon’s grandiloquent response in his 1971 State of the Union address: “The time has come in America when the same kind of concentrated effort that split the atom and took man to the moon should be turned toward conquering this dread disease. Let us make a total national commitment to achieve this goal.”
But the War on Cancer, as the moon shot was called, didn’t reach its goal. Partly, that was because “cure” was an erroneous target. Cancer is not one disease, but more than 200. “We talk about a ‘cure’ for cancer, but no one would ever use the term ‘cure’ for infectious disease—they would talk about a cure for AIDS or TB or malaria,” says the Harvard Chan School’s Giovannucci. “You have to think about these diseases one by one.” More fundamentally, the War on Cancer failed because it spent far too little on cancer prevention and cancer prevention research.
There are many reasons why prevention research is unenticing. Most societies are reactive, not proactive. The final phases of research on treatment are simpler than research on prevention. Curing a patient with advanced disease is more dramatic than preventing disease in a healthy person. And perhaps most conspicuously, treatments earn far higher profits than do new diagnostics or prevention measures.
Yet every great public health success has overcome those entrenched obstacles. “The way I message this to lawmakers is that our well-being is a gift; we can’t take good health for granted, and prevention is a powerful way to protect that gift. When prevention works, you can enjoy the miracle of a perfectly normal, healthy day,” says Koh. “When I interact with lawmakers, I often ask about whether they have experienced the pain of losing a loved one when it could have been prevented. That usually humanizes the conversation and gives it relevance and immediacy.”
A cure for cancer is our culture’s threadbare metaphor for a miracle. But a cancer prevented is even better than a cancer cured. When cancer becomes our leading cause of death—as it soon will—cancer prevention will become our leading cause of life.
Madeline Drexler is editor of Harvard Public Health .
News from the School

Air pollution exposure in infancy may limit economic mobility in adulthood

Reducing health inequities in the Mississippi Delta

Climate change and planetary health concentration launches

Orientation 2024: New students encouraged to engage across differences
The Science History Institute will close at 4pm on Friday, September 27 and reopen at 5pm for Ring the Bell, It’s Lunchtime! An Opening Celebration

Distillations magazine
Aspirin: turn-of-the-century miracle drug.
Aspirin has had a long history as a pain reliever—2,000 years of history. But only in the 1970s did scientists begin to uncover its chemical secrets.
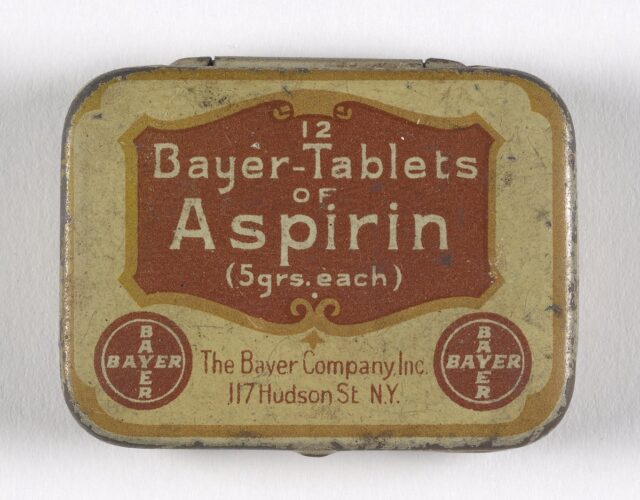
Headache? Fever? Muscle pain? “Take two aspirin and call me in the morning.”
Like most of us, when you experience everyday aches and pains, a bottle of aspirin is probably the first thing you reach for. Yet, while aspirin has been one of the most popular pharmaceutical agents of the past one hundred years, it is actually a synthetic derivative of the natural substance salicylic acid—the associated healing properties of which have been known for millennia.
Salicylic acid is a main component of an herbal extract found in the bark of a number of trees, including the willow tree, and in a number of fruits, grains, and vegetables. As such, salicylic acid—and related salicylates—have long been common components of a normal human diet, functioning as a natural defense against what we consider common ailments today.
The first recorded use of salicylates dates back about 4,000 years to the Sumerians, who noted the pain remedies of the willow tree on early clay tablets. Ancient civilizations in Mesopotamia used the extract from willow trees to treat fever, pain, and inflammation. Both Chinese and Greek civilizations employed willow bark for medical use more than 2,000 years ago, and the Chinese also used poplar bark and willow shoots to treat rheumatic fever, colds, hemorrhages, and goiter. One of the most noteworthy reports of the use of salicylic acid comes from the father of modern medicine, Hippocrates (460–370 BCE). He recommended chewing on willow-tree bark to patients suffering from fever and pain, as well as the use of a tea brewed from willow bark given to women to lessen pain during childbirth. Around 100 CE the Greek physician Dioscorides prescribed willow bark as an anti-inflammatory agent.
Despite this long history, it was not until 1763 that the Reverend Edward Stone of the Royal Society of London conducted one of the first clinical studies on the effects of willow-bark powder by treating patients suffering from ague (a fever thought to be caused by malaria). And approximately 100 years later the Scottish physician Thomas MacLagan studied the effects of willow powder on patients suffering from acute rheumatism, demonstrating that it could relieve fever and joint inflammation.
The chemical investigation of the healing properties of the substance within the willow bark had already begun in earnest, however, during the early 19th century. This investigation was driven in part by Napoleon’s continental blockade on imports, which affected suppliers of Peruvian cinchona-tree bark (another natural source of salicylic acid). In 1828 Johann Büchner, a professor at the University of Munich, isolated a yellow substance from the tannins of willow trees that he named salicin , the Latin word for willow . A pure crystalline form of salicin was isolated in 1829 by Henri Leroux, a French pharmacist, who then used it to treat rheumatism. In the late 1800s large-scale production of salicylic acid for the treatment of pain and fever was initiated by the Heyden Chemical Company in Germany.
The beginning of aspirin as we know it today dates from the same period when Farbenfabriken vorm. Friedrich Bayer and Company, a dye-manufacturing firm in Germany, began to shift its focus from the dye industry to pharmaceutical production. Because the Bayer Company was already well known, it easily developed brand-name recognition as a pharmaceutical maker. The company’s shift to pharmaceutical production coincided serendipitously with a boom in new pharmaceutical agents, making it seem that a new drug was put on the market almost daily.
Just as the medical benefits of salicylic acid had long been known, so too had some of the health issues related to prolonged use of large doses of the drug. Such use often led to gastrointestinal irritation, which could in turn lead to nausea, vomiting, bleeding, and ulcers. In 1895, to counteract such problems, Arthur Eichengrün, the head of chemical research at Bayer, assigned the task of developing a “better” salicylic acid to one of the company’s chemists, Felix Hoffmann. Eventually cited by many as the discoverer of aspirin, Hoffmann approached the task with a personal interest: his father suffered from rheumatism and was taking salicylic acid for it, but he could no longer ingest the drug without vomiting. Hoffmann’s search through the available scientific literature yielded a way to alter salicylic acid chemically through modification of the hydroxyl group on the benzene ring. The key to his discovery, although realized only later, was that this chemical transformation provided a new molecule that the body could absorb without significant gastrointestinal distress. Once ingested, the new molecule was converted back to salicylic acid in the stomach, liver, and blood, thereby providing the desired therapeutic benefits. As such, modern synthetic aspirin can be considered a drug-delivery system for a natural product that has been in medical use for literally thousands of years.
However, this new derivative of salicylic acid did generate some controversy. There was a difference in opinion regarding the potential benefits of acetylsalicylic acid, which would ultimately become a personal dispute as well as a scientific one. Heinrich Dreser, who was responsible for the standardized testing of pharmaceutical agents, disagreed with Eichengrün’s approach to the drug. Eichengrün had distributed Hoffmann’s compound to local physicians, whereas Dreser had no initial interest in supporting the new drug. Ironically, it would be Dreser who published the first article on aspirin, probably because his contract with Bayer provided him royalties for any drug he introduced; Hoffmann and Eichengrün could only gain monetary rewards on patentable compounds. In the article Dreser compared aspirin with other salicylates in an effort to demonstrate that it was more beneficial and less toxic. This work was coupled with human trials whose results were published in 1899 in the journals Die Heilkunde and Therapeutische Monatshefte , showing that aspirin was indeed superior to other known salicylates. On 6 March 1899 the Bayer Company registered the product under the trade name Aspirin and then actively began to distribute the white powder to hospitals and clinics.
According to the theory concerning the origin of the name aspirin, it comes from the combination of acetyl ; the Latin Spiraea , the genus of plants to which meadowsweet belongs and which also contains salicylic aldehyde, a precursor to salicylic acid (in German salicylic acid is Spirsäure ); and -in , which was a common ending for drug names at the time. Although the company name Bayer has long been associated with aspirin, after World War I, Bayer lost the sole right to use the name aspirin . It was acquired in 1919 by Sterling Incorporated for the then unheard-of price of $3 million, along with Bayer’s U.S. drug properties. Eventually Bayer reacquired the trademark from SmithKline Beecham as part of a wider deal, for the price of $1 billion.
The first tablet form of aspirin appeared in 1900, creating an ease of use that quickly expanded the drug’s recognition among professionals. Medical reports highlighted the benefits of aspirin, and its popularity reflected the already significant use of salicylic compounds, coupled with the fact that this new drug was considerably safer and comparably less toxic. In 1915 aspirin became available to the public without a prescription, making it arguably the first modern, synthetic, over-the-counter, mass-market medicine and a household name around the world.
By providing an easy and inexpensive method to alleviate pain, aspirin began to change the experience and expectations of patients and doctors and ultimately the nature of modern medicine itself. Before the mid-1800s Western physicians had considered pain an essential diagnostic tool, something that aspirin alleviated and thus disguised. Doctors would now have to look to other symptoms.
It was not until 1971 that scientists began to understand how aspirin worked in the body as an anti-inflammatory agent—what is now referred to as a nonsteroidal anti-inflammatory drug (NSAID). John Robert Vane, a British pharmacologist, and his graduate student Priscilla Piper performed pioneering work on aspirin, exploring the effects of the drug on isolated lungs from guinea pigs and studying the effects of substances released from the lungs during severe allergic reactions to aspirin. During these studies the scientists identified two uncharacterized substances, one of which turned out to be a prostaglandin—a hormone-like compound involved in causing diverse effects in the body, including vasodilation, vasocontraction, and sending messages of pain and discomfort to the brain. Piper and Vane later discovered that this prostaglandin had an effect similar to a known enzyme responsible for the contraction of nonvascular smooth muscle. Further studies demonstrated that aspirin minimized some effects of vasodilation response, ultimately leading Vane to consider that aspirin was inhibiting the synthesis of prostaglandins. For Vane’s pioneering work he, along with Sune K. Bergström and Bengt I. Samuelsson, received the Nobel Prize in Physiology or Medicine in 1982.
But how does aspirin affect the production of prostaglandins? In 1976 researchers discovered a particular enzyme, cyclooxygenase, or COX, that is responsible for producing a number of biological mediators, including prostaglandins. Aspirin was found to bind selectively and irreversibly to this enzyme, providing the drug’s beneficial properties. This characteristic differs from that of other well-known NSAIDs (e.g., ibuprofen), which are reversible inhibitors. Further research indicated that there was not one COX enzyme, but three, and that each played a different role in the human body. While one COX enzyme is responsible for the synthesis of prostaglandins during inflammatory reactions, a second is involved in producing prostaglandins that help protect the stomach mucosa. Aspirin affects both enzymes, providing analgesic effects as described, but at high doses sometimes results in stomach irritation. In an effort to separate the two effects pharmaceutical companies have worked hard to develop selective COX inhibitors, such as Celebrex, Vioxx, and Mobic, that reduce inflammation without damaging stomach mucosa. However, a number of issues have arisen with these products, most notably with Vioxx, which recent studies have shown to increase the risk for heart attacks.
Aspirin represents one of humankind’s oldest pharmaceutical agents and continues to be a mainstay therapy for a variety of indications. Like all drugs, aspirin can be toxic at high doses (greater than 150 milligrams per kilogram body weight), but the benefits of aspirin clearly outweigh the risks. We might consider aspirin a true “wonder drug,” as it has been shown to be useful in the treatment of a variety of conditions beyond fever and pain, including prevention of coronary artery disease, heart attack, and stroke. Recent studies suggest that aspirin may also limit the rate of growth and the occurrence of certain types of cancer, including prostate, colon, pancreatic, and lung cancer. While new drugs will continue to treat these and other diseases, aspirin will always hold a significant place in the history of pharmaceutical agents.
This article has been excerpted from Molecules That Matter , a compilation of essays published by the Frances Young Tang Teaching Museum and Art Gallery at Skidmore College and by the Chemical Heritage Foundation (now the Science History Institute).
Daniel R. Goldberg is a senior principal scientist in the medicinal chemistry department at Boehringer-Ingelheim Pharmaceuticals in Ridgefield, Connecticut. His main research efforts focus on the discovery of new therapies for autoimmune and cardiovascular diseases.
More from our magazine
We’re Going to Work Miracles
The failed promises of Project Plowshare.

A Tragedy with No End
Why does Garrett Hardin’s pessimistic fable haunt our collective imagination?

That Time Demons Possessed the Telegraph
Solar storms from long ago have become the delight of some scientists—and the dread of others.
Copy the above HTML to republish this content. We have formatted the material to follow our guidelines, which include our credit requirements. Please review our full list of guidelines for more information. By republishing this content, you agree to our republication requirements.
7 incredible medical breakthroughs that changed the world
We know that it is an undisputable fact that research saves lives. Starting new cancer cures is what we do, but the amazing thing about research is that any breakthroughs made can end up benefitting other diseases too, by providing fundamental knowledge about how our organs, tissues and cells work. Just take a look at some of the greatest medical discoveries in history and how they still benefit us today.
Vaccination
The first ever successful vaccine was the smallpox vaccine, introduced in 1796 by Edward Jenner. He observed that milkmaids who had previously caught cowpox seemed to avoid catching smallpox - giving him the idea to stimulate the immune system with a less dangerous or dead part of a germ.
Smallpox was one of the deadliest diseases ever known to mankind, with an estimated 300-500 million people losing their lives to the disease throughout the 19th century. Less than two centuries after the vaccine was introduced, in 1978, a woman named Janet Parker died from smallpox in Birmingham after the virus escaped from a lab. She remains the last person to have died from the disease to date.
Today smallpox remains the only human disease to have been completely eradicated by vaccination – saving countless lives over the years.

Anaesthesia
There is no doubt that surgeries save lives. It’s unlikely to be a surprise to you that the more complex the surgery, the longer the operation takes. But did you know that before anaesthesia, surgeons were hugely limited in how long they could operate for?
Operations considered relatively commonplace today would have been regarded as impossible – either because they would take too long, or because the limited pain relief available at the time, like opium, was insufficient.
The first-ever surgical procedure using anaesthesia was performed in the USA on the 16th of October 1846, in Boston, to remove a tumour from a patient's neck.
Today, surgery is still the main treatment option for most cancer patients and can be curative if the cancer is caught early enough.
Epidemiology
John Snow, a London physician, is widely regarded as the father of epidemiology – the study of the patterns and causes of disease in a population.
Snow set out to prove that cholera, an incredibly common and very deadly disease of the time, wasn’t caused by “bad air” as everyone at the time believed. He was able to find evidence that all of the cases of one particularly bad outbreak of cholera could be linked back to a specific water pump near Bond Street, London, proving the source of cholera to be the contaminated local water supply.
Epidemiology is an important area of research for all diseases, including cancer. By understanding the rate of cancer cases in a population and the common genetic, environmental and lifestyle factors that connect these people, we can better understand the underlying causes of cancer and develop new ways to prevent the disease.

Germ theory
Did you know it took until the 19th century for people to accept that disease is caused by germs? You might have already heard of one of the main players in the field, French chemist Louis Pasteur, who proved that fermentation of wine and souring of milk are caused by living microorganisms.
But have you come across the name Joseph Lister before? A professor of surgery at Glasgow University, Lister was the first to apply germ theory to surgery. In 1865, Lister introduced the antiseptic principle to surgery, revolutionizing the field by providing a way to prevent infection in wounds during and after surgery.
This relatively small change had a dramatic impact, leading to a steep fall in infections and deaths after operations were carried out. Today, surgery is a widespread treatment for many health conditions and without antiseptic principles, even the smallest procedure could be deadly if infection enters the body.
Today, diabetes is a serious but generally well-controlled disease thanks to our understanding of how lifestyle choices can help control symptoms. Advances in treatments, such as insulin injections, also play a big role in fixing some of the molecular problems that are associated with diabetes.
Insulin was first used as a treatment for diabetes in 1922. It was discovered the previous year by scientists at the University of Toronto. Before this discovery was made, Type 1 diabetes (typically diagnosed in young people) couldn’t be successfully treated.
Before insulin, children with type 1 diabetes were expected to live only around 1.5 years after their diagnosis. In adults, only 1 in 5 would be alive 10 years after their diagnosis and those that did live longer suffered from debilitating symptoms caused by diabetes. Today, it’s expected that people with type 1 diabetes will live a normal life.

Gene therapy
For a more recent big breakthrough in the medical field, you don’t need to look any further than gene therapy, which involves introducing genetic material into cells to treat or prevent disease. The very first gene therapy trial was launched in 1990, successfully treating a then four-year-old girl with a rare genetic disease that severely affected her immune system.
Gene therapy is now used by the NHS to treat certain cases of blindness and it holds promise for a wide range of other diseases, including heart disease, haemophilia and cystic fibrosis.
Gene therapy is also on the horizon for cancer, with researchers all over the world investigating how to use gene therapy to kill cancer by boosting the immune system, making other treatments work better and to block molecular processes that allow cancer cells to survive.
3D printing
Finally, something that would have seemed futuristic not too long ago now presents incredible opportunities for the future - 3D printing. The first 3D printer was developed in the 1980s by Chuck Hull to print solid structures for manufacturing. It wasn’t long before the medical world took notice.
Today, 3D printing is already being used to create dental implants and prosthetics, but researchers want to take the technology even further and print whole organs. While there is still a long way to go, scientists have already started to print cells and tissues using a process called 3D bioprinting. This allows scientists to create innovative biomaterials to study in greater detail how the body works.
In the future, we expect to see full 3D printed organs which could be used to test new drugs and even eliminate the need for animal testing.

Incredible breakthroughs like these would never have happened without discovery research, and research cannot happen without Curestarters like you. You can help us start the breakthroughs of tomorrow by donating today.

Donate now & become a Curestarter
Be part of a united effort to stop lives being cut short by cancer.

Share this page
- Share on Facebook
- Share on LinkedIn
- Sign into My Research
- Create My Research Account
- Company Website
- Our Products
- About Dissertations
- Español (España)
- Support Center
Select language
- Bahasa Indonesia
- Português (Brasil)
- Português (Portugal)
Welcome to My Research!
You may have access to the free features available through My Research. You can save searches, save documents, create alerts and more. Please log in through your library or institution to check if you have access.

Translate this article into 20 different languages!
If you log in through your library or institution you might have access to this article in multiple languages.

Get access to 20+ different citations styles
Styles include MLA, APA, Chicago and many more. This feature may be available for free if you log in through your library or institution.

Looking for a PDF of this document?
You may have access to it for free by logging in through your library or institution.

Want to save this document?
You may have access to different export options including Google Drive and Microsoft OneDrive and citation management tools like RefWorks and EasyBib. Try logging in through your library or institution to get access to these tools.

- More like this
- Preview Available
- Scholarly Journal

Conrad Fischer: Routine Miracles: Personal Journeys of Patients and Doctors Discovering the Power of Modern Medicine: Kaplan Publishing, New York, 2009, 336 pp, hard cover, $24.95
No items selected.
Please select one or more items.
Select results items first to use the cite, email, save, and export options
You might have access to the full article...
Try and log in through your institution to see if they have access to the full text.
Content area
J Community Health (2010) 35:106107 DOI 10.1007/s10900-009-9196-y
BOOK REVIEW
Conrad Fischer: Routine Miracles: Personal Journeys of Patients and Doctors Discovering the Power of Modern Medicine
Kaplan Publishing, New York, 2009, 336 pp, hard cover, $24.95
Pascal James Imperato
Published online: 22 October 2009 Springer Science+Business Media, LLC 2009
Routine Miracles is a landmark publication in the history of American medicine. It is so because it draws attention to the powerful but not popularly appreciated discontent of American physicians at a time when doing what was impossible a decade ago has now become routine. If the title appears oxymoronic, it is because what was once considered miraculous in medicine is now indeed routine. Patients who were considered incurable but a short time ago, now have their hearing restored, their heart valves replaced, their vision improved, their cancers cured, and their blocked arteries opened. Dramatic advances in diagnostic imaging and technical innovations with newer drugs have resulted not only in cures, but more importantly in transforming once fatal conditions into benign chronic illnesses that can be easily managed for years.
Never before in the history of mankind have physicians been able to save so many lives, cure so many people, and restore health and happiness to the once hopeless. Despite all these medical breakthroughs, many American doctors are unhappy. Why?
In this volume, Dr. Conrad Fischer, a renowned medical educator and specialist in internal medicine, sets out to explore this professional discontent while simultaneously presenting the perspectives of numerous patients who have triumphed over serious illness thanks...
You have requested "on-the-fly" machine translation of selected content from our databases. This functionality is provided solely for your convenience and is in no way intended to replace human translation. Show full disclaimer
Neither ProQuest nor its licensors make any representations or warranties with respect to the translations. The translations are automatically generated "AS IS" and "AS AVAILABLE" and are not retained in our systems. PROQUEST AND ITS LICENSORS SPECIFICALLY DISCLAIM ANY AND ALL EXPRESS OR IMPLIED WARRANTIES, INCLUDING WITHOUT LIMITATION, ANY WARRANTIES FOR AVAILABILITY, ACCURACY, TIMELINESS, COMPLETENESS, NON-INFRINGMENT, MERCHANTABILITY OR FITNESS FOR A PARTICULAR PURPOSE. Your use of the translations is subject to all use restrictions contained in your Electronic Products License Agreement and by using the translation functionality you agree to forgo any and all claims against ProQuest or its licensors for your use of the translation functionality and any output derived there from. Hide full disclaimer
Suggested sources
- About ProQuest
- Terms of Use
- Privacy Policy
- Cookie Policy
An Initiative of the Program for Bedside Medicine
- See us on youtube
- See us on facebook
- See us on twitter
The miracle of a patient’s recovery
Written by Cassie Myers

Lindsey Freeman before and after her remarkable recovery at Stanford Hospital.

If it was a movie script, you wouldn’t believe it. A 28-year-old woman has a miscarriage while on vacation in Mexico. When she goes to the doctor, a nightmare begins. She ends up spending the next five years in and out of hospitals. At one point, she’s told she’s going to die. She takes chemotherapy, sees a naturopath, sees doctors in her native Ukiah and at Stanford, even goes to Philadelphia and Boston to see experts on the disease. They all agree that nothing can be done.
And then? She gets better. Nobody knows exactly why or how, but she puts on weight. Her skin, once a jaundiced yellow, returns to its normal color. Her doctors’ visits decrease. And as of right now, Lindsey Freeman, 33, is healthy. She lives in Ukiah, where she grew up, with her husband Jordan, daughter Millie, and extended family nearby. She takes Millie to preschool every morning. As she puts it, “I feel like I’ve been given this really strange gift.”
The start of the problem
It all started in March of 2012. On vacation in Mexico, Lindsey Ingram, then 28, suffered a miscarriage. “We didn't really understand why right away,” she explains. “They just knew that I had a hematoma in my uterus.” The doctors discovered a shadow on her lung, and she had surgery to remove a mass.
Ten days before the surgery, Lindsey Ingram married her boyfriend Jordan and became Lindsey Freeman. In December, they were cleared to get pregnant. “I always wanted to be a mom, ” Lindsey explains, “so we jumped on the opportunity.” By the end of December she was pregnant again. The pregnancy seemed normal and healthy up until her due date, when she had to have an emergency C-section and nearly bled out.
Nevertheless, her daughter, Millie Freeman, was born on September 13, 2013. To everyone’s relief Millie, named to honor both Lindsey and Jordan’s grandmothers, was perfectly healthy.
“Knowing later what they ended up finding out, they said that she was actually an absolute miracle,” Lindsey says. “She’s our little miracle child.”

Lindsey with husband Jordan, before and after recovery.

First trips to Stanford
Millie may have been healthy, but Lindsey was not. She was bleeding, a lot, to the point where it became difficult for her to walk. She saw a local hematologist and was in and out of her local hospital, but it was clear that she needed a larger hospital’s resources.
When Millie was eight weeks old, Lindsey went to Stanford. Her first stint there was five and a half weeks. Jordan and Millie moved down with her. “My husband works for my dad, so my dad was just like, ‘Don't even think about coming to work, you need to go be with her and Millie,’” Lindsey says. She was given a private room, where Jordan camped out and Millie played in a playpen.
The Stanford doctors tried everything they could to staunch her bleeding. They tried numerous medications, and eventually one seemed to work. They stopped the bleeding and sent her back home to Ukiah.
But a day after she left the hospital, she started bleeding again. She worked with doctors in Ukiah and Stanford to up the dosage of the medication, but nothing was working. And they still didn’t know the underlying cause. At this point, she explains, “I have zero diagnosis. Their goal was literally just to get me to stop bleeding, and then they would try to figure out what was wrong with me.”
Around this time, Lindsey met Dr. Caroline Berube, a hematologist who became her primary outpatient physician for much of her time at Stanford. Dr. Berube and her colleagues in various departments, including pulmonology, gastroenterology, pediatric hematology, and hospital medicine, desperately tried to stop the bleeding, and—what’s more—to find out what was wrong.
A diagnosis
In February of 2014, Lindsey finally had a diagnosis: KLA, or Kaposiform lymphangiomatosis: a very rare, newly-identified, incurable condition caused by abnormal lymphatic vessels that often cause life-threatening bleeding. It’s usually a pediatric condition-- only a handful of adult cases have ever been reported. Most patients die within three years.
But Lindsey’s team of doctors didn’t give up. They put her on medication and, as she puts it, “For a year and a half I did okay. I wasn't super sick but I didn't really have energy.” She still had blood and iron transfusions, mostly in Ukiah, but she’d also occasionally start bleeding again and wind up back at the hospital.
A turn for the worse
In September of 2015, Lindsey started to turn yellow. She called Jillian Settlemire, RN , a nurse coordinator in Dr. Berube’s office who often calmed Lindsey down and was always a “huge help” during her illness, and explained what was happening. Jillian told Lindsey to come back down to Stanford.
Lindsey calls that “the beginning of this huge kick in the stomach for the next year and a half. I got down to 96 pounds. I was mustard yellow all over: my mouth, my eyes, my fingernails, my skin. And I just kept hearing over and over, ‘We don't know what to do.’” The disease was taking over her liver, and the doctors were working frantically to save her, but she was still sick.
In December of 2015, during one of her stints at Stanford, she and her family were given an apartment near the hospital, so she could come and go with ease. She remembers one particular day, when Dr. Berube came to see her. “I went up there with my dad,” she says “and we just thought we were going over there just for a blood transfusion. But Dr. Berube was really, really worried about me. She looked at my dad and me, and she said, ‘You know, I think it's time you start preparing for the worst if it does happen.’ This was the first time we had heard it. My dad took his glasses and he just chucked them, he was so upset. He punched himself in the face. It was horrible, so horrible. And he walked out. He can't stand crying in front of me -- or anybody -- but he went to the bathroom and he came back and this was the first time that I said, ‘Dad, we have to be strong. We can't think like that. I'm not going anywhere.’ That was the first time we heard it and I thought, Okay, well, this is real now .”
Dr. Berube and Dr. Michael Jeng suggested that she go to the East Coast to see Denise Adams, an expert in the disease, in Boston. Adams suggested that she go to Philadelphia as well. So in March 2016 Lindsey, her husband, her daughter, her parents, and in her in-laws flew to the East Coast to speak to the experts. In both cases, the results were devastating: there was nothing anyone could do. Again she was told that she was going to die.
“That was always what I heard,” Lindsey says. “So I just remember feeling really calm and saying, ‘Okay.’ And I don't know if I was in denial or what, but I always felt like I wasn't gonna die, even though I heard it over and over and over. I just kept thinking, That's not gonna happen . I have to be here for my daughter, you know?”
She saw a naturopath. She kept fighting. As Dr. Berube put it, “This woman would not give up.”

“I really don’t know how I was even alive”
In May of 2016, everything looked even darker. “I don't even know how I could've gotten worse, but I did,” Lindsey says. She was sent back down to Stanford, to see Dr. Berube and her other doctors. A man from Florida, Jack Kelly, happened to be in the area. His daughter had had KLA, too, and had died from it.
Lindsey’s doctors wanted him to visit her. They’d been urging her to start chemotherapy, and hoped talking to him would help persuade her. She agreed to see him. “I was terrified to talk to him just knowing that his daughter had passed away from this disease, “she says, “but he was actually really inspiring. He was really kind.” They talked for a long time, and he told her the chemo was the only chance she had.
“I thought about it, and I was like, I said I would do anything to stay alive for my daughter,” Lindsey says. She agreed to the chemotherapy in June of 2016, doing it about every three weeks until January 2017.
“It just kicked my butt. I was sick, I was throwing up, my liver just wasn't getting any better. I was on all kinds of medication,” she says. And in the meantime, other symptoms were cropping up. She started getting ascites, an accumulation of fluid in the peritoneal cavity that causes abdominal swelling, and had to go regularly to the doctors to get the fluid drained, probably twenty or thirty times overall. And, she adds, “Every time they drained my abdomen or my lung it was blood. It scared every doctor who ever touched me. I really don't even know how I was alive. It was horrible. But I just kept--if I didn't have my daughter, I probably wouldn't have cared so much, but, you know, I had her, I wanted to be there for her.”
Moments of joy
There were moments of joy. If you spend five years in and out of hospitals, you’ll end up spending holidays there, even birthdays, and you’ll grow very close to the staff, doctors and nurses alike. Lindsey remembers one birthday when the Stanford nurses worked especially hard to please her. One nurse “brought me a coffee with my name on it and cookies and then all day long I got flowers and gifts from all these nurses, who were just like so sweet, made my birthday so special. We had dance parties, we were singing and you know, it was great. It was like, well, if I'm gonna be here…”
She remembers another great nurse, Shelly Gray, and says, “Instantly we just loved each other. She came in and she would take Millie for walks. Millie kind of grew up at Stanford. The doctors and the nurses would get to know her as well and so she'd get to know them. Shelly brought Millie this cute little doctor kit, and then we just became friends.”
Lindsey loved Dr. Berube. “She was the sweetest lady. Whether it was good or bad, she just--she was just really heartfelt and really caring.” Another one of her doctors, Errol Ozdalga, “was always so nice and so positive and just upbeat. He was never like that doctor who came in with a sad look on his face. He was always just like smiley and trying to figure out the next thing that we could do.”

Lindsey before and after recovery with nurse, Shelly Gray.
A community of collaborators
During her various visits to Stanford, Lindsey interacted with an enormous amount of people: doctors, nurses, staff, and trainees, who were all part of what Dr. Berube calls the “huge collaboration” of people who worked to save their patient. During her hospitalizations, for example, Lindsey saw dozens of trainees for her daily care, and of course the work took “an emotional toll” on them, too, as Dr. Berube attests. Lindsey’s first hematologist, for example, was Dr. Ameen Salahudeen, and her main GI doctor was Dr. Kirsten Regalia. Both doctors were with her during her first stint at Stanford and became “huge supports” for her throughout the years of her illness.
Even people Lindsey never interacted with personally were involved in her care. “While we were trying to keep her alive,” Dr. Berube explains, “other teams in Stanford research labs were analyzing her biopsy samples and genetics trying to figure out what was wrong with this rare condition.” In the end, Lindsey’s recovery was both unearthly and decidedly earthbound: a surprising result of the work of literally dozens of doctors, nurses, researchers, and staff, all working together to heal one patient.
An inspiration
Even in illness, Lindsey inspired the other people around her. Dr. Berube loved her. “She is this lovely beautiful woman, you know, beautiful inside and out,” she says. “She was very special to us.” She emphasizes Lindsey’s positive attitude and family support, adding that the family’s gratitude for their providers helped not just Lindsey, but the doctors as well. In such a multi-department, interdisciplinary effort, Lindsey’s family’s gratitude helped her providers keep going, even while they coordinated her care through three or four different specialties, as well as on- and off-site clinics.
Jillian Settlemire, Dr. Berube’s nurse coordinator, echoes this praise. She calls Lindsey “probably one of the strongest women I know,” adding that she’s “kind-hearted and optimistic” even through such a “large ordeal.” Taking care of her was a challenge. Jillian and Lindsey were around the same age, and Jillian says, “I would always think about how I would feel if I was her and how scared she must have been.” Ultimately, though, taking care of Lindsey was “a really great experience” for Settlemire. “She’s become one of my favorite patients and I’m happy that I was able to participate in her care,” she concludes.
Lindsey’s hometown of Ukiah is a small community, and they raised $70,000 for her trip to Philadelphia and all the other out-of-pocket expenses (Stanford doctor Kirsten Regalia also contributed).
“My community did not want us to worry about money,” she says. “When I was really bitter at first, somebody told me, ‘You know, you need to have an attitude of gratitude or you're gonna hate this process.’ And it changed my outlook on the whole thing.”
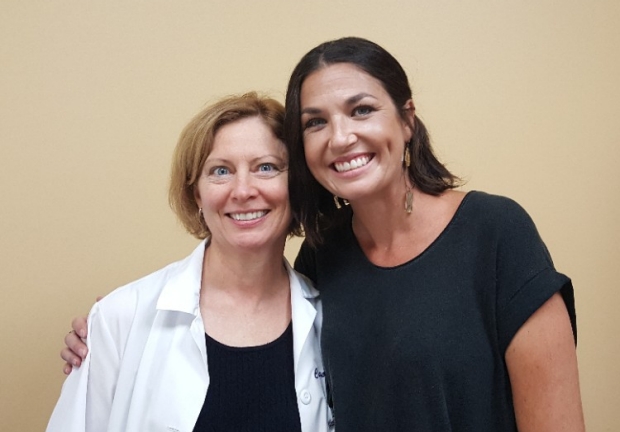
Dr. Caroline Berube with Lindsey
A ray of hope
By November 2016, everything was dire. That Thanksgiving Lindsey was back down at Stanford, and her whole family came down “to say goodbye.” Lindsey thinks it was probably the second or third time they’d done this, but this one seems to stick in her mind. “I was so, so sick,” she says. She was still bleeding, nauseated, jaundiced, and very thin. She’d also gotten a severe infection. “She looked like an end-stage cancer patient,” Berube says.
They tried a few new different treatments. They gave Lindsey IV nutrition, upped the dosage of one of her medications, and Dr. Berube wanted to keep the ascites in Lindsey’s body a little longer to minimize the number of abdominal punctures.
What happened next is still more than a little unexplainable: “Nobody really knows what made me better,” Lindsey says. “Nobody can actually tell me. So we all think it was kind of just like everything combined. And it worked. That's kind of when things just turned around.”

Lindsey’s bleeding subsided. Her ascites stayed away. Dr. Berube wanted her to continue with chemo after she was released from the hospital in early December.
“And all of a sudden, I started putting on weight,” Lindsey says. “I walked past my mirror one day and I was like, ‘there's a little jiggle that I didn't have,’ you know? And I just kind of feel like a miracle was given to me.”
No one rushed to proclaim her healthy. She’d had times, during various stints in the hospital, when things improved briefly and then she “fell off a cliff again.” “It took us a little while to celebrate,” Lindsey says. “We held back. But I also think that once I started putting on weight that we were all a little bit more hopeful.”
Dr. Berube was as surprised as anyone. “Clearly she was dying,” she says. She doesn’t know what fixed Lindsey, but says she thinks it’s “a combination of factors, but I don't know which one was the most important one.” It could’ve been the IV nutrition, or the treatment of the infection, the chemotherapy, or an increased dosage of one of Lindsey’s medications.
“Honestly,” Dr. Berube says, “I've been doing hematology for thirty years. I've never used the word miracle, but I think this was it.”
Lindsey continued to have regular doctor’s visits, but in early 2017 she asked Dr. Berube if she could stop chemotherapy, and Dr. Berube agreed, but reminded her there was no guarantee that they wouldn’t have to start again. But as of this writing, Lindsey hasn’t needed it. Her disease has entered what Dr. Berube calls a “quiet phase” or “a good partial remission.”
Lindsey’s checkups decreased . She still has her blood drawn regularly, but for the first time in five years, she’s been back to normal. She hasn’t been back to the hospital since that Thanksgiving admission in 2016.
“One thing that was really scary for me always was knowing that my daughter was approaching preschool age,” Lindsey says. “I was terrified that I wasn't going to be able to do these normal mom things with her. And now I get to get up in the morning and make her breakfast and get her dressed. Which is all I ever wanted. I just feel like this whole entire thing was this crazy weird bad dream.”
The new normal
So Lindsey’s back in Ukiah, with her family and her daughter. Things are mostly back to normal—she’s woken up from the dream. But she’s carried memories of it with her into waking life.
“I still at least once a week get somebody coming up to me in tears,” Lindsey says. “The other night it happened twice. And now I'm a thousand times more grateful just that I'm healthy.”
The story is bigger than Lindsey, in some ways, but in other ways, it isn’t. “I think it's not only the disease, it's Lindsey's story,” Dr. Berube says. “She's a very special person.”

Subscribe to our mailing list
Related pages, teaching humility at the bedside, what can doctors learn from narrative medicine, interview with dr. eric topol (editor-in-chief of medscape), the internet: the elephant in the examination room.
- Dermatology
- Endocrinology
- Extremities
- Gastroenterology/Hepatology
- Gynecology/Women's Health
- Hematology/oncology
- Ophthalmology
- Perspective
- Rheumatology
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Meta-Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
7 The Miracle of Modern Medicine: The Ethics of Organ Transplantation and Artificial Organs
- Published: June 1998
- Cite Icon Cite
- Permissions Icon Permissions
Medieval Catholic doctors practiced under the heavenly patronage of Saints Cosmos and Damien. According to legend, the two saints were brothers who practiced medicine in fourth-century Syria. Their reputation for skill was enhanced by their generosity in caring for the poor. One day, a certain Vincent, deacon of the local church, came to their clinic. An arrowhead was embedded in his leg, which was rotting away. The holy doctors took one look at the gangrenous limb and told the deacon that their treatments would be futile. He should, they advised, take himself to church and pray for a good death. Vincent followed their advice. While at prayer, he fell asleep (as often happens). Meanwhile, the holy doctors were visited by an angel who told them to go to the church, amputate the leg of a corpse laid out for burial, amputate the sleeping Vincent’s leg, and attach the dead limb to the living man. Vincent awoke with a sound leg, and patient and doctors praised the Lord.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| September 2024 | 2 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Volume 25, Number 1—January 2019
Books and Media
Miracle cure: the creation of antibiotics and the birth of modern medicine.
Cite This Article

- Figure . Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine
Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine ( Figure ) engagingly describes what is arguably the most significant development in the history of medicine: antibiotics. The book chronicles captivating accounts from the conception of the germ theory of disease and the scientific discovery of these life-saving medications to the interplay among the countless contributing idiosyncratic and imperfect individuals and organizations involved, including the pharmaceutical titans. With the contemporary emergence and spread of antibiotic resistance, the book’s message is timely and poignant.
Miracle Cure is relevant for both the science enthusiast and the science novice. Although slightly tangential at times in its background narratives, it intertwines the creation of antibiotics as intricately tied to the evolution of modern medicine and paints both as not just a product of science but as a culmination of economic, political, and social influences. In so doing, it sheds a human light on the discovery and production of antibiotics.
Many medical professionals and nonmedical persons envision the discovery of antibiotics, especially penicillin, as a providential occurrence that revolutionized previously unenlightened medical practices characterized by bloodletting and poisoning. However, Miracle Cure paints them more accurately as products of the iterative process of scientific discovery in an attempt to improve public health and, in some instances, generate personal profit and fame. The lifesaving properties of antibiotics are a secondary theme to the real-life problems overcome, the challenging ethics decisions made, and the delicate scientific egos bruised along the way.
For readers seeking a book that provides insight into the current public health crisis of antibiotic resistance, Miracle Cure does not provide answers or potential solutions, nor was it intended to do so. However, it goes beyond the most apparent impacts antibiotics have had on human health to explore the less publicized effects of antibiotics on regulatory agencies, drug marketing, physician–pharmaceutical industry relationships, research study design, and the practice of medicine.
One of the book’s most important arguments is that antibiotics have forced us to calibrate and recalibrate our idea of medication safety as we transitioned from unregulated mixtures of strychnine, mercury, and arsenic for which the adverse effects were inextricably tied to the morbidity and mortality of underlying disease to tightly regulated, carefully calibrated antibiotics for which safety and efficacy were the norm. Miracle Cure demonstrates that this shift, facilitated by a mix of altruism and greed, caused the “[p]rescription of antibiotic without a specific cause” to reach “disturbing proportions.” The book is a fascinating and important read that translates to a deep understanding of the history of antibiotic development leading up to the current state and its problems.
DOI: 10.3201/eid2501.181184
Original Publication Date: December 04, 2018
Related Links
- More Books and Media Articles
Table of Contents – Volume 25, Number 1—January 2019
| EID Search Options |
|---|
| – Search articles by author and/or keyword. |
| – Search articles by the topic country. |
| – Search articles by article type and issue. |
Please use the form below to submit correspondence to the authors or contact them at the following address:
Keith W. Hamilton, Hospital of the University of Pennsylvania, Ste 110 Silverstein Bldg, 3400 Spruce St, Philadelphia, PA 19104, USA
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Article Citations
Highlight and copy the desired format.
| EID | Hamilton KW. Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine. Emerg Infect Dis. 2019;25(1):196. https://doi.org/10.3201/eid2501.181184 |
|---|---|
| AMA | Hamilton KW. Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine. . 2019;25(1):196. doi:10.3201/eid2501.181184. |
| APA | Hamilton, K. W. (2019). Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine. , (1), 196. https://doi.org/10.3201/eid2501.181184. |
Metric Details
Article views: 2674.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.182(6); 2010 Apr 6

Making a case for medical miracles
Medical Miracles: Doctors, Saints and Healing in the Modern World, Jacalyn Duffin, Oxford University Press; 2008.
A paralyzed woman rose and walked after lying next to the corpse of Saint Diego d’Alcalá in 1555. A three-year-old boy came back to life after a mother’s plea to Saint Andrea Avellino in 1678. A young woman was cured of meningitis following appeals to Saint Vincenza Maria Lopez y Vincuna in 1928.
Do you believe the Roman Catholic Church’s accounts of medical miracles? After examining more than 1400 cases in the canonization files of the Vatican Archives and Library, physician and historian Jacalyn Duffin does, sort of.
Once skeptical, she says she now believes the stories — as a historian. That is, she believes in the honesty and accuracy of the players and people involved in experiencing and verifying the healing events. “These events were miracles for the people involved,” she writes in Medical Miracles: Doctors, Saints and Healing in the Modern World .
On a broader level, what remains constant through time and place are human efforts to delay death. Sick people consult physicians, follow their advice, but also simultaneously seek cures from other possible sources, such as God, states Duffin, the Hannah Chair for the History of Medicine at Queen’s University in Kingston, Ontario.
Focusing on healings from the 16th to the 20th century that led to the canonization of saints by the Catholic Church, this book is about the form and identification of medical miracles, the practice of the attending physicians and the manner in which people sought divine help.
Duffin is less interested in verifying facts — did a medical miracle actually take place? — than in uncovering how the experience and scrutiny of miracle healings changed over four centuries as well as what was constant through the process.
Religion and medicine have never been on opposite sides of the process, Duffin notes, but “religion sits more comfortably with medical science than vice versa.”
Not surprisingly, many important changes occurred. Duffin says the Vatican placed increasing emphasis on medicine and physical healing in investigations of miracles. Over the years, it required greater medical testimony and detailed diagnoses. More doctors became involved in the investigations and more advanced technologies, from the stethoscope to imaging scans, contributed to the church’s demands for greater proof of disease healing.
The types of diseases recorded also changed over time, reflecting shifts in disease prevalence in society and disease classification (nosology) in medical science. For example, the description of diseases such as tuberculosis, smallpox, malaria or simply fevers faded in the records as effective treatments emerged. Evidence of cancer or tumours remained constant, although its descriptor ranged from scirrho, malignant ulcer or tumour to carcinoma and cancer.
One historical constant has been the key role played by doctors in the Vatican’s investigation process. Physicians perform two important steps: They diagnose the condition as hopeless (a medical failure to cure) and they express surprise at the outcome (for which medicine could not take credit). When the Vatican is confident that doctors have exhausted the latest medical therapeutics and eliminated natural causes as an explanation, it can declare a healing miracle.

Another constant is the structure of the healing narrative in the canon record — or the “dramatic arc,” according to Duffin — in which patients recovering from disease moved through “a solid structure of suffering, invocation, healing and thanksgiving.” Patients made similar pleas for divine intervention through prayer, pilgrimages or relics; they shared experiences of dreams or visions at their instant of recovery; they all offered gifts of thanks —prayers, offerings, and so on.
So what prompted this self-professed atheist to become so interested in miraculous healing? Duffin unknowingly contributed to the successful canonization of Marie-Marguerite d’Youville, the first Canadian-born saint. Duffin confirmed severe acute leukemia — with a remission, a relapse and another remission — in a living patient, who attributed her subsequent cure to the intercession of d’Youville. After that, Duffin says, she decided to learn more about miraculous healings, admitting that many of her medical colleagues were baffled by her research interest.
Duffin’s study is good empirical history. She presents ample case narratives involving cancer, blindness, lung conditions and other debilitating diseases.
Based on her exhaustive research, Duffin challenges several historical assumptions, including that the Vatican was averse to the use of new medical therapeutics or technologies as standards of care. At a more mundane level, she explains the miracle record itself — what went into it, the role of doctors, the goal of Vatican leaders and the lives of the people seeking help. Indeed, as Duffin suggests, these records are rich sources for religious, medical and social historians alike.
Regardless of whether you believe in medical miracles, Duffin’s work should inspire further analysis in the convergence of medicine and religion.
Previously published at www.cmaj.ca
The World We Used to Live In: Remembering the Powers of the Medicine Men PDF

| Title | The World We Used to Live In: Remembering the Powers of the Medicine Men |
|---|---|
| Author | |
| Publisher | |
| Category | |
| Released Date | 2016-01-01 |
| Language | English |
| Format | EPUB |
| Pages | 298 |
| Total Downloads | 353 |
| Total Views | 1,421 |
| Rating |
In his final work, the great and beloved Native American scholar Vine Deloria Jr. takes us into the realm of the spiritual and reveals through eyewitness accounts the immense power of medicine men. The World We Used To Live In, a fascinating collection of anecdotes from tribes across the country, explores everything from healing miracles and scared rituals to Navajos who could move the sun. In this compelling work, which draws upon a lifetime of scholarship, Deloria shows us how ancient powers fit into our modern understanding of science and the cosmos, and how future generations may draw strength from the old ways....
Chapter List (14 chapters):
- Chapter 1: The World We Used To Live In
- Chapter 2: Preface
- Chapter 3: Prologue
- Chapter 4: Introduction
- Chapter 5: Chapter One
- Chapter 6: Chapter Two
- Chapter 7: Chapter Three
- Chapter 8: Chapter Four
- Chapter 9: Chapter Five
- Chapter 10: Chapter Six
- Chapter 11: Chapter Seven
- Chapter 12: Chapter Eight
- Chapter 13: Endnotes
- Chapter 14: Bibliography
Rate & write a review
Similar documents.

We the Men of India

The World I Live In

Understanding the Prophetic Times We Live In

The End of Memory: Remembering Rightly in a Violent World

The Way We Were: Remembering Diana

Remembering Tommy: The British Soldier in the First World War

The Way We Live Now
- 1,208 Pages

- 1,209 Pages

Great Men and Women in the History of Medicine

Where We Used to Roam

The World i Live in: Personal Memoirs

We Are the World

Marijuana Medicine: A World Tour of the Healing and Visionary Powers of Cannabis

Dynamic Medicine: The World According to Homeopathy

How to Live in the World and Still Be Happy
Popular uploaders.
- Sandi Wallace
- Susan J Berger
- Sourav Sarkar
- James Francis Keegan III
- Eric Barton
- Nick Flittner
- Alison Lambert
- Susanna Jennicrai
- Mary Brooks
- Corey Turner
- Kathryn Anthony
- Kimberley Bachelot
- Robert M. Ellis
- Michael Monte
- Qazi Fazl Ullah
- Charina Fargesen
- Tamara Heiner
- Ida Annette Minor Ward
- Major James Bliss
- L.F. Peterson
- Melissa Seal
- Terry C. Johnston
- Sophie James
- Philip J. Deloria
- Merck & Co.
- Allen Wright
- Jennifer Houston
Advertisement
Atul Gawande, Being Mortal: Medicine and What Matters in the End
New York: Metropolitan Books, 2014. 304 pp. $26.00. ISBN: 978–0805095159
- Book Review
- Published: 19 August 2016
- Volume 53 , pages 562–566, ( 2016 )
Cite this article

- Alan B. Astrow 1
712 Accesses
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Author information
Authors and affiliations.
Hematology/Medical Oncology, New York Methodist Hospital, 506 6th St., Brooklyn, NY, 11215, USA
Alan B. Astrow
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Alan B. Astrow .
Rights and permissions
Reprints and permissions
About this article
Astrow, A.B. Atul Gawande, Being Mortal: Medicine and What Matters in the End . Soc 53 , 562–566 (2016). https://doi.org/10.1007/s12115-016-0050-4
Download citation
Published : 19 August 2016
Issue Date : October 2016
DOI : https://doi.org/10.1007/s12115-016-0050-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing Home
- Assisted Living
- Assisted Suicide
- Palliative Care Program
- Life Worth Living
- Find a journal
- Publish with us
- Track your research
- Share full article
Advertisement
Supported by
Suddenly, It Looks Like We’re in a Golden Age for Medicine
We may be on the cusp of an era of astonishing innovation — the limits of which aren’t even clear yet.

By David Wallace-Wells
Hype springs eternal in medicine, but lately the horizon of new possibility seems almost blindingly bright. “I’ve been running my research lab for almost 30 years,” says Jennifer Doudna, a biochemist at the University of California, Berkeley. “And I can say that throughout that period of time, I’ve just never experienced what we’re seeing over just the last five years.”
A Nobel laureate, Doudna is known primarily for Crispr, the gene-editing Swiss Army knife that has been called “a word processor” for the human genome and that she herself describes as “a technology that literally enables the rewriting of the code of life.” The work for which Doudna shared the Nobel Prize was published more than a decade ago, in 2012, opening up what seemed like an almost limitless horizon for Crispr-powered therapies and cures. But surveying the recent landscape of scientific breakthroughs, she says the last half-decade has been more remarkable still: “I think we’re at an extraordinary time of accelerating discoveries.”
The pandemic has exhausted many Americans of medicine, and it has become common to process the last few years as a saga of defeat and failure. And yet these brutal years — which brought more than a million American deaths and probably 20 million deaths worldwide, and seemed to return even the hypermodern citadels of the wealthy West to something like the experience of premodern plague — might also represent an unprecedented watershed of medical innovation. Beyond Crispr and Covid vaccines, there are countless potential applications of mRNA tools for other diseases; a new frontier for immunotherapy and next-generation cancer treatment ; a whole new world of weight-loss drugs; new insights and drug-development pathways to chase with the help of machine learning; and vaccines heralded as game-changing for some of the world’s most intractable infectious diseases.
“It’s stunning,” says the immunologist Barney Graham, the former deputy director of the Vaccine Research Center and a central figure in the development of mRNA vaccines, who has lately been writing about a “new era for vaccinology.” “You cannot imagine what you’re going to see over the next 30 years. The pace of advancement is in an exponential phase right now.”
‘World-changing’ innovations
It is sometimes hard to see the silver lining for the cloud, particularly when it’s as dark as the last three years have been. But at the very center of the American Covid experience, amid all the death and suffering and despite the dysfunction that midwifed it into being, sits what would have stood out, in any previous era, as an astonishing biomedical miracle: the coronavirus vaccines. Drug-development timelines in previous history had swallowed whole decades; experts warned not to expect a resolution for years. But the mRNA sequence of the first shot was designed in a weekend, and the finished vaccines arrived within months, an accelerated timeline that saved perhaps several million American lives and tens of millions worldwide — numbers that are probably larger than the cumulative global death toll of the disease.
The miracle of the vaccines wasn’t just about lives saved from Covid. As the first of their kind to be approved by the Food and Drug Administration, they brought with them a very long list of potential future mRNA applications : H.I.V., tuberculosis, Zika, respiratory syncytial virus (R.S.V.), cancers of various and brutal kinds . And the vaccine innovations stretch beyond mRNA: A “world-changing” vaccine for malaria, which kills 600,000 globally each year, is being rolled out in Ghana and Nigeria , and early trials for next-generation dengue vaccines suggest they may reduce symptomatic infection by 80 percent or more.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
Medicine promises people hope. Hope rooted in the discoveries of the past and felt in the therapies of the present. Hope that is inspiring the future. Medicine is riddled with a history of countless breakthroughs that today have become standard of care in many clinical settings. With the first successful vaccine for smallpox by Edward Jenner in ...
Miracle Cure is relevant for both the science enthusiast and the science novice. Although slightly tangential at times in its background narratives, it intertwines the creation of antibiotics as intricately tied to the evolution of modern medicine and paints both as not just a product of science but as a culmination of economic, political, and social influences.
Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine discusses ways to improve detection of resistant infections in the United States and abroad, including monitoring environmental reservoirs of resistance. This report sets out a strategy for improving stewardship and preventing infections in humans and animals.
Clinical miracles can further be subdivided as events against any reasonable prediction and without any explanation—and the marvels present in modern medicine that have an explanation but are wonders that should not be taken for granted. Others may argue that miracles can also be seen in the ordinary and everyday wonders of human life.
He left out the second part of the surgeon's epithet: "the king of terrors." Modern targeted treatments and immunotherapy have in some cases led to wondrous cures, and many malignancies are now caught early enough so that their sufferers can live out full lives. ... In clinical medicine, the value of screening tests is gauged by their ...
Both Chinese and Greek civilizations employed willow bark for medical use more than 2,000 years ago, and the Chinese also used poplar bark and willow shoots to treat rheumatic fever, colds, hemorrhages, and goiter. One of the most noteworthy reports of the use of salicylic acid comes from the father of modern medicine, Hippocrates (460-370 BCE).
Organ transplantation is certainly one of the "miracles" of modern medicine. The impossible dream of replacing a dead or dying vital organ, such as a kidney or a heart, with a living one became a reality on December 23, 1954, when Drs. Joseph Murray and John Merrill of Peter Bent Brigham Hospital transplanted a kidney from one monozygotic twin to another [1].
The thrust, both of clinicians and research, must now turn decisively towards prevention and cure. Also, longevity with well-being is modern medicine's other big challenge. Advances in vaccines for hypertension, diabetes, cancers etc, deserve attention; as also, the role of meditation, yoga, spirituality etc in preventing disease at various ...
This review traces the development of vaccines from ancient times to the present, highlighting major milestones and challenges. It covers the significant impact of vaccines on public health, including the eradication of diseases such as smallpox and the reduction of others such as polio, measles, and influenza. The review provides an in-depth look at the COVID-19 vaccines, which were developed ...
It never ceases to amaze me how quickly humans as a species forget things. Kesiah Winters is a gardener, artist, crafter and rancantour. She lives in Owatonna with her snakes, cats, chickens and ...
Before insulin, children with type 1 diabetes were expected to live only around 1.5 years after their diagnosis. In adults, only 1 in 5 would be alive 10 years after their diagnosis and those that did live longer suffered from debilitating symptoms caused by diabetes. Today, it's expected that people with type 1 diabetes will live a normal life.
Conrad Fischer: Routine Miracles: Personal Journeys of Patients and Doctors Discovering the Power of Modern Medicine. Kaplan Publishing, New York, 2009, 336 pp, hard cover, $24.95. Pascal James Imperato. ... Routine Miracles is a landmark publication in the history of American medicine. It is so because it draws attention to the powerful but ...
Combating Antimicrobial Resistance and Protecting the Miracle of Modern Medicine This new report from the National Academies of Sciences, Engineering, and Medicine, requested by Congress in P.L. 116-94 , the Further Consolidated Appropriations Act, 2020, discusses ways to improve detection of resistant infections in the United States and abroad ...
The miracle of a patient's recovery. Written by Cassie Myers. Lindsey Freeman before and after her remarkable recovery at Stanford Hospital. If it was a movie script, you wouldn't believe it. A 28-year-old woman has a miscarriage while on vacation in Mexico. When she goes to the doctor, a nightmare begins. She ends up spending the next five ...
Abstract. The author uses an autoethnographic account of a close friend's emergency cardiac surgery, and its disastrous outcome, to explore and critique the contemporary search for medical "miracles" and the patchwork and inequitable system of medical reimbursement in the United States. Access Options.
This essay responds to Michael J. Balboni and Tracy A. Balboni's Hostility to Hospitality: Spirituality and Professional Socialization within Medicine (New York: Oxford University Press, 2018). The essay reflects on three themes: structural pluralism, miracles, and empirical research. First, it expands on the Balbonis' proposal of structural pluralism by accentuating the importance of ...
Medieval Catholic doctors practiced under the heavenly patronage of Saints Cosmos and Damien. According to legend, the two saints were brothers who practiced medicine in fourth-century Syria. Their reputation for skill was enhanced by their generosity in caring for the poor. One day, a certain Vincent, deacon of the local church, came to their ...
Miracle Cure: The Creation of Antibiotics and the Birth of Modern Medicine engagingly describes what is arguably the most significant development in the history of medicine: antibiotics.The book chronicles captivating accounts from the conception of the germ theory of disease and the scientific discovery of these life-saving medications to the interplay among the countless contributing ...
Making a case for medical miracles. Medical Miracles: Doctors, Saints and Healing in the Modern World, Jacalyn Duffin, Oxford University Press; 2008. A paralyzed woman rose and walked after lying next to the corpse of Saint Diego d'Alcalá in 1555. A three-year-old boy came back to life after a mother's plea to Saint Andrea Avellino in 1678.
In his final work, the great and beloved Native American scholar Vine Deloria Jr. takes us into the realm of the spiritual and reveals through eyewitness accounts the immense power of medicine men. The World We Used To Live In, a fascinating collection of anecdotes from tribes across the country, explores everything from healing miracles and scared rituals to Navajos who could move the sun.
Being Mortal: Medicine and What Matters in the End. New York: Metropolitan Books, 2014. 304 pp. $26.00. ISBN: 978-0805095159. In the debate over the relative merits of education for STEM (science, technology, engineering, and mathematics) compared with humanistic study, surgeon-author, Atul Gawande, might appear an unlikely champion for the ...
A couple of decades later, it looks like a golden age for new treatments. New trials of breast-cancer drugs have led to survival rates hailed in The Times as "unheard-of," and a new treatment ...