

Clinical Cases
Litfl clinical cases database.
The LITFL Clinical Case Collection includes over 250 Q&A style clinical cases to assist ‘ Just-in-Time Learning ‘ and ‘ Life-Long Learning ‘. Cases are categorized by specialty and can be interrogated by keyword from the Clinical Case searchable database.
Search by keywords; disease process; condition; eponym or clinical features…
| Topic | Title | Keywords |
|---|---|---|
| ECG | ||
| ECG | WCT, ECG, Broad complex, fascicular, RVOT | |
| Toxicology | valproate, valproic acid, hyperammonemia | |
| Toxicology | valproate, valproic acid, hyperammonemia | |
| Toxicology | ||
| Metabolic | priapsim, intracavernosal, cavernosal gas, Ischaemic priapism, stuttering priapism, urology | |
| Metabolic | RTA, strong ion difference, hypocalcaemia | |
| Bone and Joint | DRUJ, dislcoation | |
| ICE | wellens, ECG, cardiac, delay | |
| ICE | SJS, stevens-johnson syndrome, erythema multiforme, rash | |
| ICE | pneumothorax | |
| ICE | ||
| ICE | tibia, fracture, toddler, toddler's fracture | |
| ICE | ECG, EKG, hyperkalaemia, hyperkalemia | |
| ICE | dengue, returned traveler, traveller | |
| ICE | Lisfranc | |
| ICE | mountain, mount everest, alkalaemia, alkalemia | |
| ICE | pancreatitis, alcohol | |
| ICE | segond fracture | |
| ICE | Brugada | |
| ICE | STEMI, hyperacture, myocardial ischemia, anterior | |
| ICE | eryhthema nodosum, panniculitis | |
| ICE | BOS fracture, battle sign, mastoid ecchymosis, bruising | |
| ICE | Galleazi, fracture dislocation | |
| Toxicology | methylene blue, Methaemoglobinemia, methemoglobin | |
| Toxicology | clozapine | |
| Toxicology | Methamphetamine, body stuffing, body packer, body stuffer | |
| Toxicology | TCA, tricyclic, overdose, sodium channel blockade | |
| Toxicology | alprazolam, BZD, benzo, benzodiazepine, benzodiazepines, flumazenil | |
| Toxicology | lithium, neurotoxicity, acute toxicity | |
| Toxicology | baclofen, GABA, Gamma-Hydroxybutyrate, GHB | |
| Toxicology | Carbamazepine, toxidrome, carbamazepine cardiotoxicity, Tegretol, multiple-dose activated charcoal, MDAC | |
| Toxicology | Hepatotoxicity, Acetaminophen, Schiodt score, hepatic encephalopathy, N-acetylcysteine, NAC | |
| Toxicology | beta-blocker, B Blocker, | |
| Toxicology | Cannabinoid Hyperemesis Syndrome, cyclical vomiting, THC, delta-nine-tetrahydrocannabinol | |
| Toxicology | Colchicine | |
| Toxicology | Clonidine | |
| Toxicology | Bath salts | |
| Toxicology | Mephedrone | |
| Toxicology | Bromo-DragonFLY, M-ket, Kmax, Mexxy, Meow-Meow, Mephedrone, Methoxetamine, Naphyrone, NRG-1, Salvia, K2, Spice | |
| Toxicology | ixodes holocyclus, tick, paralysis, | |
| Toxicology | cyanide, carbon monoxide | |
| Toxicology | hypoglycemia | |
| Toxicology | Ciguatera, Scombroid, fugu, puffer fish | |
| Toxicology | ethylene glycol, HAGMA, high anion gap metabolic acidosis, osmolar gap, Fomepizole, alcohol, ethanol | |
| Toxicology | iron toxicity, Desferrioxamine chelation therapy | |
| Toxicology | chloroquine | |
| Toxicology | corrosive agent | |
| Toxicology | Antidote | |
| Toxicology | Oculogyric crisis, OGC, acute dystonia, Acute Dystonic Reaction, butyrophenone, Metoclopramide, haloperidol, prochlorperazine, Benztropine | |
| Toxicology | Tricyclic, Theophylline, Sulfonylureas, Propanolol, Opioids, Dextropropoxyphene, Chloroquine, Calcium channel blockers, Amphetamines, ectasy | |
| Toxicology | verapamil, calcium channel blocker, cardiotoxic, HIET, high-dose insulin euglycemic therapy, | |
| Toxicology | aroma, smell | |
| Toxinology | snake-bite, snake bite, Brown snake, Black, Death adder, Taipan, sea snake, tiger | |
| Toxicology | Anticholinergic syndrome, Malignant hyperthermia, Neuroleptic malignant syndrome, Serotonin toxicity | |
| Toxicology | Serotonin toxicity, Serotonin syndrome, toxidrome | |
| Toxicology | proconvulsive, venlafaxine, tramadol, amphetamines, Bupropion, Otis Campbell | |
| Toxicology | TCA, tricyclic, overdose, sodium channel blockade, Amitriptyline | |
| Toxicology | anticoagulation, warfarin | |
| Toxicology | Mickey Finn, pear, | |
| Toxicology | thyrotoxic storm, Thyroxine, T4 | |
| Toxinology | white-tailed spider, Lampona, L. cylindrata, L. murina | |
| Toxicology | Citalopram, SSRI, | |
| Toxicology | warfarin | |
| Toxicology | warfarin, accidental ingestion, toddler | |
| Toxicology | ||
| Toxinology | Marine, envenoming | |
| Toxinology | Marine, envenoming, penetrating, barb, steve irwin, | |
| Toxinology | Marine, envenoming, Blue-Ringed Octopus, BRO, Hapalochlaena | |
| Toxinology | Jellyfish, marine, Chironex fleckeri, Box Jellyfish | |
| Toxinology | Jellyfish, marine, Jack Barnes, Carukia barnesi, Irukandji Syndrome, Darwin | |
| Toxinology | Jellyfish, marine, Jack Barnes, Carukia barnesi, Irukandji Syndrome | |
| Toxicology | Strychnine, opisthotonus, risus sardonicus | |
| Toxicology | naloxone, Buprenorphine | |
| Toxinology | snake-bite, snake bite, SVDK | |
| Toxinology | Red back spider, redback, envenoming, RBS | |
| Toxinology | Red back spider, redback, envenoming, RBS | |
| Toxicology | ||
| Toxicology | Acetaminophen, N-acetylcysteine, NAC | |
| Pediatric |
| Henoch-Schonlein Purpura, HSP, Henoch-Schönlein |
| Pediatric |
| adrenal insufficiency, glucocorticoid deficiency, NAGMA, endocrine emergency |
| Pediatric |
| Penile Zipper Entrapment, foreskin, release, Zip |
| Pediatric |
| diarrohea, vomiting, hypokalemia, hypokalaemia, dehydration |
| Pediatric |
| infantile colic, TIM CRIES, crying baby |
| Pediatric |
| Pyloric stenosis, projectile vomit, hypertrophic pyloric stenosis, HPS, Rankin |
| Pediatric |
| respiratory distress, wheeze, foreign body, RMB, CXR, right main bronchus |
| Pediatric |
| airway obstruction, stridor, severe croup, harsh cough, heliox, intubation, sevoflurane |
| Pediatric |
| boot-shaped, TOF, coeur en sabot, Tetralogy of Fallot |
| Pediatric |
| Spherocytes, Shistocytes, Polychromasia, reticulocytosis, anemia, anaemia, hemolytic uremic syndrome, HUS |
| Pediatric |
| Reye syndrome, ammonia, metabolic encephalopathy, aspirin |
| Pediatric |
| Ketamine, procedural sedation, pediatric sedation |
| Pediatric |
| Foreign Body, ketamine, laryngospasm, Larson's point, laryngospasm notch |
| EYE |
| ophthalmology, eye trauma, Eyelid laceration, lacrimal punctum |
| EYE |
| ophthalmology, Retrobulbar hemorrhage, haemorrhage, RAPD, lateral canthotomy, DIP-A CONE-G, cantholysis |
| EYE |
| ophthalmology, corneal abrasion, eye trauma, eyelid eversion |
| EYE |
| ophthalmology, commotio retinae, eye trauma, traumatic eye injury |
| EYE |
| ophthalmology, Traumatic iritis, hyphaema, hyphema, |
| EYE |
| ophthalmology, lens dislocation, Anterior dislocation of an intraocular lens |
| EYE |
| ophthalmology, visual loss, loss of vision , blind |
| EYE |
| ophthalmology, Central retinal vein occlusion, CRVO, branch retinal vein occlusion, BRVO |
| EYE |
| ophthalmology, Central retinal artery occlusion, CRAO, cherry red spot, Branch retinal artery occlusion, BRAO |
| EYE |
| ophthalmology, miosis, partial ptosis, anhidrosis, enophthalmos, horner |
| EYE |
| ophthalmology, visual loss, Amaurosis fugax, TIA, transient ischemic attack |
| EYE |
| ophthalmology, Pre-septal cellulitis, preseptal cellulitis, peri-orbital cellulitis, Post-septal cellulitis, post septal cellulitis, orbital cellulitis |
| EYE |
| ophthalmology, AION, giant cell arteritis, GCA, Anterior ischemic optic neuropathy |
| EYE |
| ophthalmology, Herpes simplex keratitis, dendritic ulcer |
| EYE |
| ophthalmology, Conjunctival injection, conjunctivitis, keratoconjunctivitis, Adenovirus, trachoma, bacterial, viral, Parinaud oculoglandular conjunctivitis |
| EYE |
| ophthalmology, Chemical injury, cement, alkali, burn, chemical conjunctivitis, colliquative necrosis, liquefactive |
| EYE |
| ophthalmology, Ultraviolet keratitis, keratopathy, solar keratitis, photokeratitis, welder's flash, arc eye, bake eyes snow blindness. |
| EYE |
| ophthalmology, Parinaud, adie, holmes, tabes dorsalis, neurosyphylis, argyll Robertson, small irregular |
| EYE |
| ophthalmology, anterior Uveitis, HLA-B27, hypopyon |
| EYE |
| ophthalmology, POCUS, ONSD, |
| EYE |
| ophthalmology, Blowout fracture, infraorbital fracture |
| EYE |
| ophthalmology, endophthalmitis, sympathetic ophthalmia, penetrating eye trauma |
| EYE |
| ophthalmology, tobacco dust, Posterior vitreous detachment, vitreous debris, retinal tear, retinal break, Washer Machine Sign, Eales disease |
| EYE |
| ophthalmology, Herpes zoster ophthalmicus, dendriform keratitis, Hutchinson sign |
| EYE |
| ophthalmology, Siedel, FB, rust ring, Corneal foreign body, Seidel test |
| EYE |
| ophthalmology, Papilloedema, Papilledema, pseudopapilloedema |
| EYE |
| ophthalmology, optic disc, optic neuritis, Marcus-Gunn, papillitis, multiple sclerosis, funduscopy, optic atrophy, papilledema |
| EYE |
| ophthalmology, retinal break, POCUS, retinoschisis, Retinal detachment |
| EYE |
| ophthalmology, cupping, glaucoma, optic neuropathy, tonometry, intraocular pressure, open angle, closed angle, gonioplasty, Acute closed-angle glaucoma |
| EYE |
| ophthalmology, Subconjunctival hemorrhage |
| EYE |
| ophthalmology, Meibomitis, blepharitis, entropion, ectropion, canaliculitis, dacryocystitis |
| EYE |
| ophthalmology, blepharospasm, blink, blinking |
| EYE |
| Iritis, keratitis, acute angle-closure glaucoma, scleritis, orbital cellulitis, cavernous sinus thrombosis (CST) |
| EYE |
| ophthalmology, fixed, dilated, pupil, holmes-adie, glass eye |
| ECG |
| Wenckebach, AV block, SA, deliberate mistake, SA block |
| ECG |
| dual chamber AV sequential pacemaker |
| ECG |
| anterior AMI, De Winter T waves, LAD stenosis |
| ECG |
| LMCA Stenosis, ST elevation in aVR, Left Main Coronary Artery |
| ECG |
| LMCA, Left Main Coronary Artery Occlusion, ST elevation in aVR |
| ECG |
| VT, BCT, WCT, Brugada criteria, Verekie |
| ECG |
| severe hypokalaemia, spironalactone, rhabdomyolysis, ECG, u wave, diabetic ketoacidosis |
| ECG |
| pacing, pacemaker, post-op, Mobitz I, Wenckebach, AV block |
| ECG |
| bidirectional ventricular tachycardia, Catecholaminergic Polymorphic Ventricular Tachycardia, CPVT, digoxin toxicity |
| ECG |
| congenital, short QT syndrome, SQTS, AF, Atrial fibrillation |
| ECG |
| RVOT, broad complex tachycardia, BCT, Right Ventricular Outflow Tract Tachycardia, VF, Arrest, Arrhythmogenic Right Ventricular Cardiomyopathy, ARVC |
| ECG |
| NSTEMI, inverted U wave, |
| ECG |
| tricyclic antidepressant, TCA, Doxepin, QRS broadening, cardiotoxic |
| ECG |
| AIVR, Accelerated idioventricular rhythm, Isorhythmic AV dissociation, Sinus arrhythmia, idioventricular |
| ECG |
| LAD, LBBB, High left ventricular voltage, HLVV, WPW, Broad Complex Tachycardia |
| ECG |
| tachy-brady, AVNRT, flutter, polymorphic VT, VF, torsades de pointes, R on T, Cardioversion |
| ECG |
| LBBB, Wellens, ECG, proximal LAD, occlusion, rate-dependent, inferior ischaemia |
| ECG |
| SI QIII TIII, PE, PTE pulmonary embolism, PEA arrest, RBBB, LAD |
| Cardiology |
| HOCM, STE, aVR, LMCA, torsades des pointes. TDP |
| Cardiology |
| aortic arch, right sided, diverticulum of Kommerell |
| Cardiology |
| IABP, CABG, shock, circulatory collapse |
| Cardiology |
| electrical alternans, ECG, pulsus paradoxus |
| Cardiology |
| Intra-aortic Balloon Pump, Waveform, dicrotic notch |
| Cardiology |
| DeBakey, TAA, aortic dissection, CTA |
| Cardiology |
| Tetraology of Fallot, BT shunt, Blalock-Tausig, ToF |
| Cardiology |
| PVP, cement, embolus, Percutaneous Vertebroplasty |
| Cardiology |
| Pulmonary Embolism, PTE, PE, McConnell, thrombolysis, echo |
| Bone and Joint |
| Missed posterior shoulder dislocation |
| Paediatrics |
| rash, neck nodule, Kawasaki |
| Paediatrics |
| rash, fever, scarlet, strawberry, Group A Beta Haemolytic Streptococci (GABHS) |
| Tropical Travel |
| diphtheria, pseudomembrance, grey tonsils, pseudomembrane, tonsillitis, diphtheria, Corynebacterium diphtheriae, gram-positive bacillus |
| Urinalysis |
| purple, urine, indican, indican |
| Urinalysis |
| brown, urine, rhabdomyolysis |
| Urinalysis |
| green, urine, propofol, PRIS |
| Urinalysis |
| green, urine |
| Urinalysis |
| orange, urine |
| Bone and Joint |
| Nail, trauma, hematoma, subungual, haematoma, nail-bed |
| Bone and Joint |
| Extensor tendon, hand injury, extensor digiti minimi, |
| Bone and Joint |
| Thumb, fracture, base, phalanx, metacarpal, Edward Hallaran Bennett, bipartate |
| Paediatrics |
| Food allergy, enterocolitis, |
| Bone and Joint |
| FOOSH, wrist fracture, FOOSH - 'fall onto outstretched hand', Barton fracture, John Rhea Barton |
| Paediatrics |
| pulled elbow, nursemaid, hyperpronation |
| Cardiology |
| Phlegmasia, dolens |
| Cardiology |
| ICC, intercostal, intra-cardiac, iatrogenic |
| Bone and Joint |
| Compartment syndrome, Volkmann, fasciotomy |
| Bone and Joint |
| Ankle, compound, fracture, dislocation, Six Hour Golden Rule, saline, iodine |
| ENT |
| retropharngeal abscess, posterior pharynx, mediastinitis, Lemierre syndrome, Fusobacterium necrophorum |
| ENT |
| enlarged tonsils, pharyngitis, tonsillitis |
| Toxicology | Colgout, colchicine, label, fenofibrate | |
| Tropical Travel | Mary Mallon, Salmonella typhi, typhoid, typhoid mary | |
| Tropical Travel | Dengue Fever, single-stranded RNA virus, Aedes, mosquito, Dengue Shock Syndrome (DSS), Dengue Haemorrhagic Fever (DHF) | |
| Tropical Travel | AIDS, Human immunodeficiency virus, lentivirus, anti-retroviral, | |
| Tropical Travel | tuberculosis | |
| Tropical Travel | Falciparum, Vivax, Ovale, Malariae, Knowlesi, Plasmodium | |
| Tropical Travel | cholera, gram-negative comma-shaped bacillus, rice water stool, John Snow Pump, V. cholerae, vibrio | |
| Tropical Travel | Entamoeba histolytica, protozoan parasite, Amoebic dysentery, Flask Shaped amoebic trophozoite, Bloody stool, | |
| Tropical Travel | shigellosis, Shigella, Enterotoxin, dysentery, | |
| Tropical Travel | Tetanus, Tetanispasmin, Clostridium tetani, lock jaw, Opisthotonus, Autonomic dysfunction, toxoid | |
| Tropical Travel | Rabies Immunoglobulin | |
| Tropical Travel | Koplik, measles, rash, rubeola, Morbilivirus, | |
| Trauma | permissive hypotension, MBA, MVA, widened mediastinum, pleural effusion, ICC | |
| Trauma | knife, penetrating chest wound | |
| Trauma | knife, penetrating chest wound | |
| Trauma | TBSA %, Burns Wound Assessment, Total Body Surface Area | |
| Trauma | Arterial pressure index (API), DPI (Doppler Pressure Index), Arterial Brachial Index or Ankle Brachial Index (ABI) | |
| Trauma | crush injury, degloving, deglove, amputation | |
| Trauma | hip dislocation, Allis reduction, pelvic fracture | |
| Trauma | Pelvis fracture, stabilization, stabilisation, | |
| Trauma | pelvic stabilization, Pelvis fracture, stabilisation, Pre-peritoneal packing | |
| Trauma | massive transfusion protocol, Recombinant Factor VIIa, Thromboelastography (TEG) | |
| Trauma | Critical bleeding, hemorrhagic shock, haemorrhagic shock, lethal triad, acute coagulopathy of trauma | |
| Trauma | penetrating abdominal trauma | |
| Trauma | ||
| Trauma | penetrating chest trauma wound, stab, | |
| Trauma | Right Main Bronchus, RMB, Tracheostomy, Tooth, foreign Body | |
| Trauma | Lobar collapse, aspiration, blood clot | |
| Trauma | ||
| Trauma | Traumatic rupture of the diaphragm with strangulation of viscera | |
| Trauma | eschar, burns, full thickness, | |
| Trauma | supine hypotension syndrome | |
| Trauma | ||
| Trauma | iPhone | |
| Trauma | oleoma, lipogranuloma, | |
| Trauma | oral commissure, lingual artery hemorrhage, | |
| Trauma | polymer fume fever, dielectric heating, super-heating, thermal injury | |
| Trauma | DRE, Digital rectal exam examination trauma | |
| Trauma | Injury Severity score, ISS, golden hour, seatbelt sign | |
| Trauma | primary secondary survey | |
| Trauma | extradural hemorrhage, EDH, Monro-Kellie | |
| Trauma | ||
| Trauma | ||
| Trauma | ||
| Trauma | ||
| Trauma | ||
| Trauma | GU, trauma, penis, penile, urethra, bladder, rupture | |
| Pulmonary | swine flu, pneumomediastinum, CXR | |
| Pulmonary | Thrombocytopenia, antiphospholipid syndrome | |
| Pulmonary | Hermann Boerhaave, Boerhaave syndrome, esophagus rupture, oesophagus | |
| Pulmonary | ||
| Pulmonary | pneumococcal pneumonia, HIV, bronchoscope, anatomy, RMB | |
| Pulmonary | subcutaneous emphysema, FLAAARDS, | |
| Pulmonary | respiratory acidosis, hypercapnoea | |
| Pulmonary | hypersensivity pneumonitis, diffuse alveolar haemorrhage, alveolar infiltrates | |
| Pulmonary | Lung collapse, recruitment maneuver, bronchoscopy | |
| Pulmonary | Vocal cord dysfunction, VCD, paradoxical vocal cord motion, PVCM, posterior chinking | |
| Pulmonary | pneumococcus, Streptococcus pneumoniae, penicillin-resistant | |
| Pulmonary | DOPES, | |
| Pulmonary | asthma | |
| Pulmonary | dyssynchrony, mechanical ventilation, PEEP, Plateau pressure | |
| Pulmonary | pneumomediastinum, tracheostomy, trachy, complication | |
| Pulmonary | PERC rule, D-Dimer, Pulmonary Embolism Rule-out Criteria, HAD CLOTS, | |
| Pulmonary | AMS, acute mountain sickness, high altitude, High-altitude cerebral edema, HACE, HAPE, High-altitude pulmonary edema | |
| Pulmonary | ||
| Resus | Pulseless electrical activity, PEA | |
| Resus | intraosseous access, EZ-IO, | |
| Resus | ||
| Resus | Rocuronium, suxamethonium, succinylcholine, non-depolarising muscle relaxant, sugammadex, safe apnoea time | |
| Resus | FEAST, trial, research, pediatric, fluid resuscitation | |
| Resus | ||
| Resus | ||
| Resus | ||
| Resus | ICC, intercostal | |
| Resus | Mechanical ventilation | |
| Oncology | SVC obstruction | |
| Oncology | Tumour lysis syndrome, Tumor lysis syndrome | |
| Oncology | lung metastases braine mets testicular cancer BEP chemotherapy, Cannonball metastases | |
| Oncology | re-expansion pulmonary oedema edema | |
| Metabolic | abdominal aortic aneurysm, AAA, rupture, CT, rhabdomyolysis, creatine kinase | |
| Metabolic | hypokalemia, hypokalaemia, periodic paralysis, u wave | |
| Metabolic | CATMUDPILES, OGRE, NAGMA, HAGMA, USED CARP, hyperchloraemic metabolic acidosis | |
| Metabolic | anion gap, pyroglutamic acidemia, HAGMA, high-anion gap, high anion, 5-oxoprolinemia, γ-glutamyl cycle, staph aureus, sepsis | |
| Metabolic | HAGMA, high-anion gap, high anion, hypernatraemia, hypernatremia | |
| Metabolic | hypokalaemia, hypokalemia, potassium, systemic bromism, coke, pepsi, coca-cola | |
| Metabolic | CATMUDPILES, renal failure, HAGMA, LTKR | |
| Metabolic | ||
| Metabolic | acute hepatitis, arterial blood gas, fulminant hepatic failure, lactic acidosis, lactic acidosis with hypoglycaemia, metabolic acidosis, metabolic muddle | |
| Metabolic | hyperammonaemia, hyperammonemia | |
| Metabolic | Hyponatraemia, hypertonic saline, ultramarathon, runner, EAH, pontine myelinoysis | |
| Metabolic | Hyponatraemia, hypertonic saline, pontine myelinoysis, Osmolality, desmopressin, SIADH, syndrome of inappropriate anti-diuretic hormone secretion | |
| Gastrointestinal | Appendagitis, Epiploic, Abdominal pain, CT abdomen | |
| Gastrointestinal | CT abdomen, Small bowel obstruction, SBO | |
| Gastrointestinal | cathine, cathione, khat, hepatitis, cathionine | |
| Gastrointestinal | rectal foreign body, FB | |
| Gastrointestinal | abdominal compartment syndrome, intra-abdominal pressure, intra-abdominal hypertension, IAH, ACS | |
| Hematology | fibrinolytic, VTE, Wells, PERC | |
| Hematology | factor VIIa, rFVIIa, novoseven | |
| Hematology | Critical Bleeding, Massive Transfusion, Tranexamic Acid, TxA, MTP | |
| Hematology | Dyshemoglobinemia, Acute myeloid leukemia, AML | |
| Immunological | angiodema, angioedema, lip sweliing | |
| Immunological | frusemide, furosemide, lasix, sulfa, | |
| Immunological | wegener, GPA, granulomatosis, palpable purpura | |
| Obstetric | amniotic fluid embolism, DIC, obstetric complication, disseminated intravascular coagulation, schistocytes, | |
| Microbial | CSF, Meningococcal meningitis, | |
| Microbial | fulminant bacterial pneumonia, septic shock, Pneumococcus, Streptococcus pyogenes, urinary pneumococcal antigen, | |
| Microbial | Legionella, community acquired pneumonia | |
| Microbial | Staphylococcal toxic shock syndrome, Toxic-shock syndrome | |
| Microbial | ||
| Microbial | ||
| Microbial | Norovirus | |
| Toxicology | Coma, similie, metaphor, flashcard, toxidromes, anticholinergic, cholinergic, PHAILS, OTIS CAMPBELL, PACED, FAST, COOLS, CT SCAN | |
| Neurology | HIV, Mass effect, CNS lesion, Brain lesion | |
| Neurology | pancoast, argyll robertson, holmes-adie, coma, pinpoint, pin-point, horner syndrome | |
| Neurology | rule of 4, rules of four, brainstem, weber syndrome, wallenberg | |
| Neurology | rule of 4, rules of four, brainstem, Nothnagel syndrome, benedikt, claude, | |
| Neurology | ||
| Neurology | ||
| Neurology | ||
| Neurology | Unilateral internuclear ophthalmoplegia, medial longitudinal fasciculus, MLF, INO, one-and-a-half syndrome | |
| Neurology | GSW, gunshot wound, bullet, TBI, Codman ICP monitor, Trans-cranial doppler, Near-infrared spectroscopy, NIRS, cerebral microdialysis catheter | |
| Neurology | BPPV, Benign Paroxysmal Positional Vertigo, Dix-Hallpike test, semont, epley, dix hallpike, brandt-daroff | |
| Neurology | Anti-NMDA Receptor Encephalitis, teratoma | |
| To err is human | cognitive error, bias, entrapment | |
| To err is human | rule of thumb, heuristic, satisficing, cognitive bias, metacognition | |
| To err is human | | Anchoring Bias, confirmation, satisficing, clustering bias |
| Cardiology | ||
| Paediatric | pediatric |
Compendium of Clinical Cases
LITFL Top 100 Self Assessment Quizzes
Browse by collection
- Anaesthesia
- Clinical pharmacology
- Critical care
- Dentistry and oral medicine
- Dermatology
- Ear, nose and throat
- Emergency medicine
- Endocrinology
- Gastroenterology
- General practice and family medicine
- Geriatric medicine
- Global health
- Haematology
- Images in...
- Infectious diseases
- Nutrition and metabolism
- Obstetrics and gynaecology
- Open access
- Ophthalmology
- Orthopaedics
- Paediatrics
- Palliative care
- Rehabilitation medicine
- Renal medicine
- Respiratory medicine
- Rheumatology
- Sexual health
- Sports and exercise medicine
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to write a medical...
How to write a medical case report
- Related content
- Peer review
- Seema Biswas , editor-in-chief, BMJ Case Reports, London, UK ,
- Oliver Jones , student editor, BMJ Case Reports, London, UK
Two BMJ Case Reports journal editors take you through the process
This article contains...
- Choosing the right patient
- Choosing the right message
- Before you begin - patient consent
- How to write your case report
- How to get published
During medical school, students often come across patients with a unique presentation, an unfamiliar response to treatment, or even an obscure disease. Writing a case report is an excellent way of documenting these findings for the wider medical community—sharing new knowledge that will lead to better and safer patient care.
For many medical students and junior doctors, a case report may be their first attempt at medical writing. A published case report will look impressive on your curriculum vitae, particularly if it is on a topic of your chosen specialty. Publication will be an advantage when applying for foundation year posts and specialty training, and many job applications have points allocated exclusively for publications in peer reviewed journals, including case reports.
The writing of a case report rests on skills that medical students acquire in their medical training, which they use throughout their postgraduate careers: these include history taking, interpretation of clinical signs and symptoms, interpretation of laboratory and imaging results, researching disease aetiology, reviewing medical evidence, and writing in a manner that clearly and effectively communicates with the reader.
If you are considering writing a case report, try to find a senior doctor who can be a supervising coauthor and help you decide whether you have a message worth writing about, that you have chosen the correct journal to submit to (considering the format that the journal requires), that the process is transparent and ethical at all times, and that your patient is not compromised in your writing. Indeed, try to include your patient in the process from the …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Can Chiropr Assoc
- v.52(4); 2008 Dec
Guidelines to the writing of case studies
Dr. brian budgell.
* Département chiropratique, Université du Québec à Trois-Rivières, 3351, boul des Forges, Trois-Rivières, Qc, Canada G9A 5H7

Dr. Brian Budgell, DC, PhD, JCCA Editorial Board
- Introduction
Case studies are an invaluable record of the clinical practices of a profession. While case studies cannot provide specific guidance for the management of successive patients, they are a record of clinical interactions which help us to frame questions for more rigorously designed clinical studies. Case studies also provide valuable teaching material, demonstrating both classical and unusual presentations which may confront the practitioner. Quite obviously, since the overwhelming majority of clinical interactions occur in the field, not in teaching or research facilities, it falls to the field practitioner to record and pass on their experiences. However, field practitioners generally are not well-practised in writing for publication, and so may hesitate to embark on the task of carrying a case study to publication. These guidelines are intended to assist the relatively novice writer – practitioner or student – in efficiently navigating the relatively easy course to publication of a quality case study. Guidelines are not intended to be proscriptive, and so throughout this document we advise what authors “may” or “should” do, rather than what they “must” do. Authors may decide that the particular circumstances of their case study justify digression from our recommendations.
Additional and useful resources for chiropractic case studies include:
- Waalen JK. Single subject research designs. J Can Chirop Assoc 1991; 35(2):95–97.
- Gleberzon BJ. A peer-reviewer’s plea. J Can Chirop Assoc 2006; 50(2):107.
- Merritt L. Case reports: an important contribution to chiropractic literature. J Can Chiropr Assoc 2007; 51(2):72–74.
Portions of these guidelines were derived from Budgell B. Writing a biomedical research paper. Tokyo: Springer Japan KK, 2008.
General Instructions
This set of guidelines provides both instructions and a template for the writing of case reports for publication. You might want to skip forward and take a quick look at the template now, as we will be using it as the basis for your own case study later on. While the guidelines and template contain much detail, your finished case study should be only 500 to 1,500 words in length. Therefore, you will need to write efficiently and avoid unnecessarily flowery language.
These guidelines for the writing of case studies are designed to be consistent with the “Uniform Requirements for Manuscripts Submitted to Biomedical Journals” referenced elsewhere in the JCCA instructions to authors.
After this brief introduction, the guidelines below will follow the headings of our template. Hence, it is possible to work section by section through the template to quickly produce a first draft of your study. To begin with, however, you must have a clear sense of the value of the study which you wish to describe. Therefore, before beginning to write the study itself, you should gather all of the materials relevant to the case – clinical notes, lab reports, x-rays etc. – and form a clear picture of the story that you wish to share with your profession. At the most superficial level, you may want to ask yourself “What is interesting about this case?” Keep your answer in mind as your write, because sometimes we become lost in our writing and forget the message that we want to convey.
Another important general rule for writing case studies is to stick to the facts. A case study should be a fairly modest description of what actually happened. Speculation about underlying mechanisms of the disease process or treatment should be restrained. Field practitioners and students are seldom well-prepared to discuss physiology or pathology. This is best left to experts in those fields. The thing of greatest value that you can provide to your colleagues is an honest record of clinical events.
Finally, remember that a case study is primarily a chronicle of a patient’s progress, not a story about chiropractic. Editorial or promotional remarks do not belong in a case study, no matter how great our enthusiasm. It is best to simply tell the story and let the outcome speak for itself. With these points in mind, let’s begin the process of writing the case study:
- Title: The title page will contain the full title of the article. Remember that many people may find our article by searching on the internet. They may have to decide, just by looking at the title, whether or not they want to access the full article. A title which is vague or non-specific may not attract their attention. Thus, our title should contain the phrase “case study,” “case report” or “case series” as is appropriate to the contents. The two most common formats of titles are nominal and compound. A nominal title is a single phrase, for example “A case study of hypertension which responded to spinal manipulation.” A compound title consists of two phrases in succession, for example “Response of hypertension to spinal manipulation: a case study.” Keep in mind that titles of articles in leading journals average between 8 and 9 words in length.
- Other contents for the title page should be as in the general JCCA instructions to authors. Remember that for a case study, we would not expect to have more than one or two authors. In order to be listed as an author, a person must have an intellectual stake in the writing – at the very least they must be able to explain and even defend the article. Someone who has only provided technical assistance, as valuable as that may be, may be acknowledged at the end of the article, but would not be listed as an author. Contact information – either home or institutional – should be provided for each author along with the authors’ academic qualifications. If there is more than one author, one author must be identified as the corresponding author – the person whom people should contact if they have questions or comments about the study.
- Key words: Provide key words under which the article will be listed. These are the words which would be used when searching for the article using a search engine such as Medline. When practical, we should choose key words from a standard list of keywords, such as MeSH (Medical subject headings). A copy of MeSH is available in most libraries. If we can’t access a copy and we want to make sure that our keywords are included in the MeSH library, we can visit this address: http://www.ncbi.nlm.nih.gov:80/entrez/meshbrowser.cgi
A narrative abstract consists of a short version of the whole paper. There are no headings within the narrative abstract. The author simply tries to summarize the paper into a story which flows logically.
A structured abstract uses subheadings. Structured abstracts are becoming more popular for basic scientific and clinical studies, since they standardize the abstract and ensure that certain information is included. This is very useful for readers who search for articles on the internet. Often the abstract is displayed by a search engine, and on the basis of the abstract the reader will decide whether or not to download the full article (which may require payment of a fee). With a structured abstract, the reader is more likely to be given the information which they need to decide whether to go on to the full article, and so this style is encouraged. The JCCA recommends the use of structured abstracts for case studies.
Since they are summaries, both narrative and structured abstracts are easier to write once we have finished the rest of the article. We include a template for a structured abstract and encourage authors to make use of it. Our sub-headings will be:
- Introduction: This consists of one or two sentences to describe the context of the case and summarize the entire article.
- Case presentation: Several sentences describe the history and results of any examinations performed. The working diagnosis and management of the case are described.
- Management and Outcome: Simply describe the course of the patient’s complaint. Where possible, make reference to any outcome measures which you used to objectively demonstrate how the patient’s condition evolved through the course of management.
- Discussion: Synthesize the foregoing subsections and explain both correlations and apparent inconsistencies. If appropriate to the case, within one or two sentences describe the lessons to be learned.
- Introduction: At the beginning of these guidelines we suggested that we need to have a clear idea of what is particularly interesting about the case we want to describe. The introduction is where we convey this to the reader. It is useful to begin by placing the study in a historical or social context. If similar cases have been reported previously, we describe them briefly. If there is something especially challenging about the diagnosis or management of the condition that we are describing, now is our chance to bring that out. Each time we refer to a previous study, we cite the reference (usually at the end of the sentence). Our introduction doesn’t need to be more than a few paragraphs long, and our objective is to have the reader understand clearly, but in a general sense, why it is useful for them to be reading about this case.
The next step is to describe the results of our clinical examination. Again, we should write in an efficient narrative style, restricting ourselves to the relevant information. It is not necessary to include every detail in our clinical notes.
If we are using a named orthopedic or neurological test, it is best to both name and describe the test (since some people may know the test by a different name). Also, we should describe the actual results, since not all readers will have the same understanding of what constitutes a “positive” or “negative” result.
X-rays or other images are only helpful if they are clear enough to be easily reproduced and if they are accompanied by a legend. Be sure that any information that might identify a patient is removed before the image is submitted.
At this point, or at the beginning of the next section, we will want to present our working diagnosis or clinical impression of the patient.
It is useful for the reader to know how long the patient was under care and how many times they were treated. Additionally, we should be as specific as possible in describing the treatment that we used. It does not help the reader to simply say that the patient received “chiropractic care.” Exactly what treatment did we use? If we used spinal manipulation, it is best to name the technique, if a common name exists, and also to describe the manipulation. Remember that our case study may be read by people who are not familiar with spinal manipulation, and, even within chiropractic circles, nomenclature for technique is not well standardized.
We may want to include the patient’s own reports of improvement or worsening. However, whenever possible we should try to use a well-validated method of measuring their improvement. For case studies, it may be possible to use data from visual analogue scales (VAS) for pain, or a journal of medication usage.
It is useful to include in this section an indication of how and why treatment finished. Did we decide to terminate care, and if so, why? Did the patient withdraw from care or did we refer them to another practitioner?
- Discussion: In this section we may want to identify any questions that the case raises. It is not our duty to provide a complete physiological explanation for everything that we observed. This is usually impossible. Nor should we feel obligated to list or generate all of the possible hypotheses that might explain the course of the patient’s condition. If there is a well established item of physiology or pathology which illuminates the case, we certainly include it, but remember that we are writing what is primarily a clinical chronicle, not a basic scientific paper. Finally, we summarize the lessons learned from this case.
- Acknowledgments: If someone provided assistance with the preparation of the case study, we thank them briefly. It is neither necessary nor conventional to thank the patient (although we appreciate what they have taught us). It would generally be regarded as excessive and inappropriate to thank others, such as teachers or colleagues who did not directly participate in preparation of the paper.
A popular search engine for English-language references is Medline: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi
- Legends: If we used any tables, figures or photographs, they should be accompanied by a succinct explanation. A good rule for graphs is that they should contain sufficient information to be generally decipherable without reference to a legend.
- Tables, figures and photographs should be included at the end of the manuscript.
- Permissions: If any tables, figures or photographs, or substantial quotations, have been borrowed from other publications, we must include a letter of permission from the publisher. Also, if we use any photographs which might identify a patient, we will need their written permission.
In addition, patient consent to publish the case report is also required.
Running Header:
- Name, academic degrees and affiliation
Name, address and telephone number of corresponding author
Disclaimers
Statement that patient consent was obtained
Sources of financial support, if any
Key words: (limit of five)
Abstract: (maximum of 150 words)
- Case Presentation
- Management and Outcome
Introduction:
Provide a context for the case and describe any similar cases previously reported.
Case Presentation:
- Introductory sentence: e.g. This 25 year old female office worker presented for the treatment of recurrent headaches.
- Describe the essential nature of the complaint, including location, intensity and associated symptoms: e.g. Her headaches are primarily in the suboccipital region, bilaterally but worse on the right. Sometimes there is radiation towards the right temple. She describes the pain as having an intensity of up to 5 out of ten, accompanied by a feeling of tension in the back of the head. When the pain is particularly bad, she feels that her vision is blurred.
- Further development of history including details of time and circumstances of onset, and the evolution of the complaint: e.g. This problem began to develop three years ago when she commenced work as a data entry clerk. Her headaches have increased in frequency in the past year, now occurring three to four days per week.
- Describe relieving and aggravating factors, including responses to other treatment: e.g. The pain seems to be worse towards the end of the work day and is aggravated by stress. Aspirin provides some relieve. She has not sought any other treatment.
- Include other health history, if relevant: e.g. Otherwise the patient reports that she is in good health.
- Include family history, if relevant: e.g. There is no family history of headaches.
- Summarize the results of examination, which might include general observation and postural analysis, orthopedic exam, neurological exam and chiropractic examination (static and motion palpation): e.g. Examination revealed an otherwise fit-looking young woman with slight anterior carriage of the head. Cervical active ranges of motion were full and painless except for some slight restriction of left lateral bending and rotation of the head to the left. These motions were accompanied by discomfort in the right side of the neck. Cervical compression of the neck in the neutral position did not create discomfort. However, compression of the neck in right rotation and extension produced some right suboccipital pain. Cranial nerve examination was normal. Upper limb motor, sensory and reflex functions were normal. With the patient in the supine position, static palpation revealed tender trigger points bilaterally in the cervical musculature and right trapezius. Motion palpation revealed restrictions of right and left rotation in the upper cervical spine, and restriction of left lateral bending in the mid to lower cervical spine. Blood pressure was 110/70. Houle’s test (holding the neck in extension and rotation for 30 seconds) did not produce nystagmus or dizziness. There were no carotid bruits.
- The patient was diagnosed with cervicogenic headache due to chronic postural strain.
Management and Outcome:
- Describe as specifically as possible the treatment provided, including the nature of the treatment, and the frequency and duration of care: e.g. The patient undertook a course of treatment consisting of cervical and upper thoracic spinal manipulation three times per week for two weeks. Manipulation was accompanied by trigger point therapy to the paraspinal muscles and stretching of the upper trapezius. Additionally, advice was provided concerning maintenance of proper posture at work. The patient was also instructed in the use of a cervical pillow.
- If possible, refer to objective measures of the patient’s progress: e.g. The patient maintained a headache diary indicating that she had two headaches during the first week of care, and one headache the following week. Furthermore the intensity of her headaches declined throughout the course of treatment.
- Describe the resolution of care: e.g. Based on the patient’s reported progress during the first two weeks of care, she received an additional two treatments in each of the subsequent two weeks. During the last week of care she experienced no headaches and reported feeling generally more energetic than before commencing care. Following a total of four weeks of care (10 treatments) she was discharged.
Discussion:
Synthesize foregoing sections: e.g. The distinction between migraine and cervicogenic headache is not always clear. However, this case demonstrates several features …
Summarize the case and any lessons learned: e.g. This case demonstrates a classical presentation of cervicogenic headache which resolved quickly with a course of spinal manipulation, supportive soft-tissue therapy and postural advice.
References: (using Vancouver style) e.g.
1 Terret AGJ. Vertebrogenic hearing deficit, the spine and spinal manipulation therapy: a search to validate the DD Palmer/Harvey Lillard experience. Chiropr J Aust 2002; 32:14–26.
Legends: (tables, figures or images are numbered according to the order in which they appear in the text.) e.g.
Figure 1: Intensity of headaches as recorded on a visual analogue scale (vertical axis) versus time (horizontal axis) during the four weeks that the patient was under care. Treatment was given on days 1, 3, 5, 8, 10, 12, 15, 18, 22 and 25. Headache frequency and intensity is seen to fall over time.

Writing a Case Report
This page is intended for medical students, residents or others who do not have much experience with case reports, but are planning on writing one.
What is a case report? A medical case report, also known as a case study, is a detailed description of a clinical encounter with a patient. The most important aspect of a case report, i.e. the reason you would go to the trouble of writing one, is that the case is sufficiently unique, rare or interesting such that other medical professionals will learn something from it.
Case reports are commonly of the following categories :
- Rare diseases
- Unusual presentation of disease
- Unexpected events
- Unusual combination of diseases or conditions
- Difficult or inconclusive diagnosis
- Treatment or management challenges
- Personal impact
- Observations that shed new light on a disease or condition
- Anatomical variations
It is important that you recognize what is unique or interesting about your case, and this must be described clearly in the case report.
Case reports generally take the format of :
1. Background
2. Case presentation
3. Observations and investigation
4. Diagnosis
5. Treatment
7. Discussion
Does a case report require IRB approval?
Case reports typically discuss a single patient. If this is true for your case report, then it most likely does not require IRB approval because it not considered research. If you have more than one patient, your study could qualify as a Case Series, which would require IRB review. If you have questions, you chould check your local IRB's guidelines on reviewing case reports.
Are there other rules for writing a case report?
First, you will be collecting protected health information, thus HIPAA applies to case reports. Spectrum Health has created a very helpful guidance document for case reports, which you can see here: Case Report Guidance - Spectrum Health
While this guidance document was created by Spectrum Health, the rules and regulations outlined could apply to any case report. This includes answering questions like: Do I need written HIPAA authorization to publish a case report? When do I need IRB review of a case report? What qualifies as a patient identifier?
How do I get started?
1. We STRONGLY encourage you to consult the CARE Guidelines, which provide guidance on writing case reports - https://www.care-statement.org/
Specifically, the checklist - https://www.care-statement.org/checklist - which explains exactly the information you should collect and include in your case report.
2. Identify a case. If you are a medical student, you may not yet have the clinical expertise to determine if a specific case is worth writing up. If so, you must seek the help of a clinician. It is common for students to ask attendings or residents if they have any interesting cases that can be used for a case report.
3. Select a journal or two to which you think you will submit the case report. Journals often have specific requirements for publishing case reports, which could include a requirement for informed consent, a letter or statement from the IRB and other things. Journals may also charge publication fees (see Is it free to publish? below)
4. Obtain informed consent from the patient (see " Do I have to obtain informed consent from the patient? " below). Journals may have their own informed consent form that they would like you to use, so please look for this when selecting a journal.
Once you've identified the case, selected an appropriate journal(s), and considered informed consent, you can collect the required information to write the case report.
How do I write a case report?
Once you identify a case and have learned what information to include in the case report, try to find a previously published case report. Finding published case reports in a similar field will provide examples to guide you through the process of writing a case report.
One journal you can consult is BMJ Case Reports . MSU has a multi-year open access publishing agreement with the publisher BM J , and an institutional fellowship with BMJ Case Reports which allows MSU faculty, staff and students to publish in this journal for free. See this page for a link to the journal and more information on publishing- https://lib.msu.edu/collections/scholcomm/support
There are numerous other journals where you can find published case reports to help guide you in your writing.
Do I have to obtain informed consent from the patient?
The CARE guidelines recommend obtaining informed consent from patients for all case reports. Our recommendation is to obtain informed consent from the patient. Although not technically required, especially if the case report does not include any identifying information, some journals require informed consent for all case reports before publishing. The CARE guidelines recommend obtaining informed consent AND the patient's perspective on the treatment/outcome (if possible). Please consider this as well.
If required, it is recommended you obtain informed consent before the case report is written.
An example of a case report consent form can be found on the BMJ Case Reports website, which you can access via the MSU library page - https://casereports.bmj.com/ . Go to "Instructions for Authors" and then "Patient Consent" to find the consent form they use. You can create a similar form to obtain consent from your patient. If you have identified a journal already, please consult their requirements and determine if they have a specific consent form they would like you to use.
Seek feedback
Once you have written a draft of the case report, you should seek feedback on your writing, from experts in the field if possible, or from those who have written case reports before.
Selecting a journal
Aside from BMJ Case Reports mentioned above, there are many, many journals out there who publish medical case reports. Ask your mentor if they have a journal they would like to use. If you need to select on your own, here are some strategies:
1. Do a PubMed search. https://pubmed.ncbi.nlm.nih.gov/
a. Do a search for a topic, disease or other feature of your case report
b. When the results appear, on the left side of the page is a limiter for "article type". Case reports are an article type to which you can limit your search results. If you don't see that option on the left, click "additional filters".
c. Review the case reports that come up and see what journals they are published in.
2. Use JANE - https://jane.biosemantics.org/
3. Check with specialty societies. Many specialty societies are affiliated with one or more journal, which can be reviewed for ones that match your needs
4. Search through individual publisher journal lists. Elsevier publishes many different medical research journals, and they have a journal finder, much like JANE ( https://journalfinder.elsevier.com/ ). This is exclusive to Elsevier journals. There are many other publishers of medical journals for review, including Springer, Dove Press, BMJ, BMC, Wiley, Sage, Nature and many others.
Is it free to publish ?
Be aware that it may not be free to publish your case report. Many journals charge publication fees. Of note, many open access journals charge author fees of thousands of dollars. Other journals have smaller page charges (i.e. $60 per page), and still others will publish for free, with an "open access option". It is best practice to check the journal's Info for Authors section or Author Center to determine what the cost is to publish. MSU-CHM does NOT have funds to support publication costs, so this is an important step if you do not want to pay out of pocket for publishing
*A more thorough discussion on finding a journal, publication costs, predatory journals and other publication-related issues can be found here: https://research.chm.msu.edu/students-residents/finding-a-journal
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. 2013. The CARE guidelines: Consensus-based clinical case reporting guideline development. Glob Adv Health Med . 2:38-43. doi: 10.7453/gahmj.2013.008
Riley DS, Barber MS, Kienle GS, AronsonJK, von Schoen-Angerer T, Tugwell P, Kiene H, Helfand M, Altman DG, Sox H, Werthmann PG, Moher D, Rison RA, Shamseer L, Koch CA, Sun GH, Hanaway P, Sudak NL, Kaszkin-Bettag M, Carpenter JE, Gagnier JJ. 2017. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol . 89:218-234. doi: 10.1016/j.jclinepi.2017.04.026
Guidelines to writing a clinical case report. 2017. Heart Views . 18:104-105. doi: 10.4103/1995-705X.217857
Ortega-Loubon C, Culquichicon C, Correa R. The importance of writing and publishing case reports during medical education. 2017. Cureus. 9:e1964. doi: 10.7759/cureus.1964
Writing and publishing a useful and interesting case report. 2019. BMJ Case Reports. Link to document
Camm CF. Writing an excellent case report: EHJ Case Reports , Case of the Year 2019. 2020. European Heart Jounrnal. 41:1230-1231. https://doi.org/10.1093/eurheartj/ehaa176
*content developed by Mark Trottier, PhD
- Utility Menu
harvardchan_logo.png

Harvard T.H. Chan School of Public Health Case-Based Teaching & Learning Initiative
Teaching cases & active learning resources for public health education, case library.
The Harvard Chan Case Library is a collection of teaching cases with a public health focus, written by Harvard Chan faculty, case writers, and students, or in collaboration with other institutions and initiatives.
Use the filters at right to search the case library by subject, geography, health condition, and representation of diversity and identity to find cases to fit your teaching needs. Or browse the case collections below for our newest cases, cases available for free download, or cases with a focus on diversity.
Using our case library
Access to cases.
Many of our cases are available for sale through Harvard Business Publishing in the Harvard T.H. Chan case collection . Others are free to download through this website .
Cases in this collection may be used free of charge by Harvard Chan course instructors in their teaching. Contact Allison Bodznick , Harvard Chan Case Library administrator, for access.
Access to teaching notes
Teaching notes are available as supporting material to many of the cases in the Harvard Chan Case Library. Teaching notes provide an overview of the case and suggested discussion questions, as well as a roadmap for using the case in the classroom.
Access to teaching notes is limited to course instructors only.
- Teaching notes for cases available through Harvard Business Publishing may be downloaded after registering for an Educator account .
- To request teaching notes for cases that are available for free through this website, look for the "Teaching note available for faculty/instructors " link accompanying the abstract for the case you are interested in; you'll be asked to complete a brief survey verifying your affiliation as an instructor.
Using the Harvard Business Publishing site
Faculty and instructors with university affiliations can register for Educator access on the Harvard Business Publishing website, where many of our cases are available . An Educator account provides access to teaching notes, full-text review copies of cases, articles, simulations, course planning tools, and discounted pricing for your students.

What's New
Atkinson, M.K. , 2023. Organizational Resilience and Change at UMass Memorial , Harvard Business Publishing: Harvard T.H. Chan School of Public Health. Available from Harvard Business Publishing Abstract The UMass Memorial Health Care (UMMHC or UMass) case is an examination of the impact of crisis or high uncertainty events on organizations. As a global pandemic unfolds, the case examines the ways in which UMMHC manages crisis and poses questions around organizational change and opportunity for growth after such major events. The case begins with a background of UMMHC, including problems the organization was up against before the pandemic, then transitions to the impact of crisis on UMMHC operations and its subsequent response, and concludes with challenges that the organization must grapple with in the months and years ahead. A crisis event can occur at any time for any organization. Organizational leaders must learn to manage stakeholders both inside and outside the organization throughout the duration of crisis and beyond. Additionally, organizational decision-makers must learn how to deal with existing weaknesses and problems the organization had before crisis took center stage, balancing those challenges with the need to respond to an emergency all the while not neglecting major existing problem points. This case is well-suited for courses on strategy determination and implementation, organizational behavior, and leadership.
The case describes the challenges facing Shlomit Schaal, MD, PhD, the newly appointed Chair of UMass Memorial Health Care’s Department of Ophthalmology. Dr. Schaal had come to UMass in Worcester, Massachusetts, in the summer of 2016 from the University of Louisville (KY) where she had a thriving clinical practice and active research lab, and was Director of the Retina Service. Before applying for the Chair position at UMass she had some initial concerns about the position but became fascinated by the opportunities it offered to grow a service that had historically been among the smallest and weakest programs in the UMass system and had experienced a rapid turnover in Chairs over the past few years. She also was excited to become one of a very small number of female Chairs of ophthalmology programs in the country.
Dr. Schaal began her new position with ambitious plans and her usual high level of energy, but immediately ran into resistance from the faculty and staff of the department. The case explores the steps she took, including implementing a LEAN approach in the department, and the leadership approaches she used to overcome that resistance and build support for the changes needed to grow and improve ophthalmology services at the medical center.
This case describes efforts to promote racial equity in healthcare financing from the perspective of one public health organization, Community Care Cooperative (C3). C3 is a Medicaid Accountable Care Organization–i.e., an organization set up to manage payment from Medicaid, a public health insurance option for low-income people. The case describes C3’s approach to addressing racial equity from two vantage points: first, its programmatic efforts to channel financing into community health centers that serve large proportions of Black, Indigenous, People of Color (BIPOC), and second, its efforts to address racial equity within its own internal operations (e.g., through altering hiring and promotion processes). The case can be used to help students understand structural issues pertaining to race in healthcare delivery and financing, to introduce students to the basics of payment systems in healthcare, and/or to highlight how organizations can work internally to address racial equity.
Kerrissey, M.J. & Kuznetsova, M. , 2022. Killing the Pager at ZSFG , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract This case is about organizational change and technology. It follows the efforts of one physician as they try to move their department past using the pager, a device that persisted in American medicine despite having long been outdated by superior communication technology. The case reveals the complex organizational factors that have made this persistence possible, such as differing interdepartmental priorities, the perceived benefits of simple technology, and the potential drawbacks of applying typical continuous improvement approaches to technology change. Ultimately the physician in the case is not able to rid their department of the pager, despite pursuing a thorough continuous improvement effort and piloting a viable alternative; the case ends with the physician having an opportunity to try again and asks students to assess whether doing so is wise. The case can be used in class to help students apply the general concepts of organizational change to the particular context of technology, discuss the forces of stasis and change in medicine, and to familiarize students with the uses and limits of continuous improvement methods.
Yatsko, P. & Koh, H. , 2021. Dr. Joan Reede and the Embedding of Diversity, Equity, and Inclusion at Harvard Medical School , Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract For more than 30 years, Dr. Joan Reede worked to increase the diversity of voices and viewpoints heard at Harvard Medical School (HMS) and at its affiliate teaching hospitals and institutes. Reede, HMS’s inaugural dean for Diversity and Community Partnership, as well as a professor and physician, conceived and launched more than 20 programs to improve the recruitment, retention, and promotion of individuals from racial and ethnic groups historically underrepresented in medicine (UiMs). These efforts have substantially diversified physician faculty at HMS and built pipelines for UiM talent into academic medicine and biosciences. Reede helped embed the promotion of diversity, equity, and inclusion (DEI) not only into Harvard Medical School’s mission and community values, but also into the DEI agenda in academic medicine nationally. To do so, she found allies and formed enduring coalitions based on shared ownership. She bootstrapped and hustled for resources when few readily existed. And she persuaded skeptics by building programs using data-driven approaches. She also overcame discriminatory behaviors and other obstacles synonymous with being Black and female in American society. Strong core values and sense of purpose were keys to her resilience, as well as to her leadership in the ongoing effort to give historically marginalized groups greater voice in medicine and science.
Cases Available for Free Download
Johnson, P. & Gordon, R. , 2014. Dr. Sam Thenya: A Women's Health Pioneer , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case tracks Dr. Sam Thenya’s challenges in establishing and sustaining two Kenyan health organizations for women’s health. Thenya founded the Gender Violence Recovery Centre (GVRC) and the Nairobi Women’s Hospital (NWH) Medical Training College. In particular, the case focuses on the choices made as he expanded these two closely connected enterprises even though the GVRC was a non-profit enterprise while the NWH was a for-profit enterprise. Students consider how he led change to improve women’s health at both the population and system levels. They reflect on his leadership and lessons learned as he sought to change the face of women’s health care in Kenya and shift societal attitudes about gender-based violence (GBV). Students analyze how Dr. Thenya scaled up his innovative model, and the subsequent decisions he made to sustain his enterprise. They consider the ways in which he adapted his vision in order to provide GBV services free of charge and expand the reach of these services. This case also provides a Kenyan context in which to discuss health care delivery, and explores general attitudes and issues surrounding GBV.
Gender-based analysis in public health is a systematic examination of the differences and similarities in the lives of women and men, as shaped by systems of gender relations, and the causes and consequences of these differences and similarities with respect to population health, policies and laws, programs and services, research priorities, and public discourse. As the Harvard School of Public Health Interdisciplinary Concentration on Women, Gender, and Health (WGH) states:
"Addressing issues of women, gender, and health requires the study of the health of women and girls—and men and boys—throughout the lifecourse, with gender, gender inequality, and biology understood as important and interacting determinants of well-being and disease.
"Also included are the study of gender and gender inequality in relation to individuals’ treatment by and participation in health and medical care systems, the physical, economic, and social conditions in which they live, and their ability to promote the health of their families, their communities, and themselves.
"Inherent in this definition is recognition of diversity and inequality among women—and men—in relation to race/ethnicity, nationality, class, sexuality, gender identity and age, and that protection of human rights is fundamental to health."
The WGH 207 teaching example assignment provides students with the opportunity to create brief teaching examples to expose students in non-WGH courses to gender-based analysis. Students work in pairs to create teaching examples based on the substantive material presented by guest speakers throughout the term (e.g., reproductive technologies). Teaching examples focus on cultivating a key technical skill within public health (e.g., Directed Acylic Graphs) through the exploration of a central issue in gender-based analysis (e.g., challenging simplistic conflations of gender and sex). Beyond building the pedagogical skills of WGH 207 students, the assignment has yielded—and continues to yield—teaching examples that can introduce the concept of gender-based analysis into core courses across all departments at HSPH.
This assignment was originally developed by course instructors Jerel P. Calzo, PhD, and Sabra L. Katz-Wise, PhD.
To cite an individual teaching example, please reference the author(s) and year of publication on the first page of the document.
Teaching examples available for download:
Measuring and Analyzing Gender:
- Sex and Gender Analysis within a Demonstration of Effect Measure Modification versus Confounding and supplemental materials
- Gender-Based Analysis and Directed Acyclic Graphs
- Unbiased Sampling Methods for Sexual and Gender Minorities and supplemental materials
- Gender-Based Analysis for Variable Selection in Logistic Model Building and supplemental materials
- Gender-Based Analysis in Sample Size and Power for Binomial Proportions
- Gender Analysis, Effect Modification, & Environmental/Occupational Exposures
- Exploring Model Specification Options for Adolescent Gender Expression and supplemental materials
- Supplementary materials
Intimate Partner Violence:
- Sex and Gender Analysis of Intimate Partner Violence
- Intimate Partner Violence Mock Trial
- Gender Analysis of Intimate Partner Violence in “High Risk” Behavior Epidemiology
Gender, Policy, and the Law:
- Gender-Based Analysis and Op-Ed Writing: The Example of Sexual Minority Reproductive Health , supplemental materials , and supplemental slides
- Using Gender-Based Analysis in a Policy Brief on Paid Family and Medical Leave
- Public Health Law Teaching Example: Forced Sterilization Law & Policy
- Gender Analysis of COVID-19 Response
- Sex/Gender, COVID-19, and DAGs: A 60-Minute Teaching Module for Introductory Epidemiology Lab
Other Topics:
- Gender Analysis and Social Support
- Gender Analysis for Winter Session Travel Course
- Incorporating Gender and an Intersectional Lens: Implications for Research on Racial/Ethnic Inequities in Hypertension and supplemental materials
- Constrained Choice Theory and Factors Impacting the Education of Adolescent Girls in Sub-Saharan Africa
- Gender Analysis in Health Communication and supplemental materials
- Disentangling the Effects of Sex vs. Gender across Neurodegenerative Disease
- Gender-Based Analysis of Alcohol Use
- Incorporating Gender-Based Analysis to Reproductive Health: Polycystic Ovary Syndrome
Cash, R., et al. , 2009. Casebook on ethical issues in international health research , World Health Organization. Publisher's Version Abstract This casebook published by the World Health Organization contains 64 case studies, each of which raises an important and difficult ethical issue connected with planning, reviewing, or conducting health-related research. Available for download free of charge from the World Health Organization in English, Arabic, Russian, and Spanish.
Kane, N.M. & Alidina, S. , 2008. Attacking Heart Disease in Suffolk County , Harvard T.H. Chan School of Public Health case collection. Download free of charge Abstract “Suffolk County is experiencing elevated cardiovascular disease mortality relative to New York State,” explained Dr. Humayun Chaudhry, Commissioner for the Department of Health Services of Suffolk County. Given the general affluence of the area, he finds the CVD mortality rates "a paradoxical situation. We need to determine strategies to address this high priority health issue for our county." Teaching note available for faculty/instructors .
Weinberger, E. , 2014. The Governor Is Very Interested, or, Cost-Effectiveness Analysis for School Health Screenings , Harvard T.H. Chan School of Public Health: Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED). Download free of charge Abstract Nefertiti Nelson, a senior official at the Columbia Department of Public Health (CDPH) in the fictitious U.S. state of Columbia, has been asked by the governor’s office to examine the cost-effectiveness of administering BMI and eating disorders screenings in schools. To carry out the project, Nefertiti and her team of CDPH colleagues join forces with the consulting firm, Datamon; yet, as the analysis begins questions quickly arise about the logistics and costliness of implementing the screenings, potential outcome measures, and the interests and concerns of respective stakeholders. Teaching note available for faculty/instructors .
Focus on Diversity, Equity, and Inclusion
Guerra, I., et al. , 2019. SALUDos: Healthcare for Migrant Seasonal Farm Workers , Harvard University: Social Medicine Consortium. Download free of charge Abstract The SALUDos program began in 2008 as a response to an influx of migrant seasonal farm workers (MSFWs) at a mobile medical unit serving homeless persons in Santa Clara County in Northern California. The program offered patients free and low-cost primary care services, linkage to resources, and advocacy. As the farm workers involved in this program became more involved in their primary care, they advocated for evening hours, transportation, linkage to coverage programs, and health education resources to better understand their medical and psychological conditions. During continual modifications of the SALUDos program, the team sought to understand and address large-scale social forces affecting migrant health through interventions to mitigate health inequities. Teaching note available for faculty/instructors.
Chai, J., Gordon, R. & Johnson, P. , 2013. Malala Yousafzai: A Young Female Activist , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case traces the story of Malala Yousafzai who has advocated passionately for girls’ right to education. In October 2012, a militant group with ties to the Taliban shot 14-year-old Yousafzai in the head as she was riding the school bus home after a day of classes. Yousafzai recovered and became the youngest recipient of the Nobel Peace Prize in 2014. This case explores the social factors that made such an attack possible and why there continue to be such barriers to educational opportunities for girls. "Malala Yousafzai: A Young Female Activist" is a part of a case series on violence against women that illustrate the critical role for leadership through an examination of how factors within a society influence women’s health. Students analyze the situations described by considering the circumstances that placed each protagonist in vulnerable positions. Participants examined the commonalities and differences of these situations in an effort to understand the circumstances that affect women’s well-being. Additionally, using the cases as a framework, students analyzed the connections between collective outrage, reactive action, and leadership.
Jessie Gaeta, the chief medical officer for Boston Health Care for the Homeless Program (BHCHP), learned on April 7, 2020 that the City of Boston needed BHCHP to design and staff in 48 hours one half of Boston Hope, a 1,000-bed field hospital for patients infected with COVID-19. The mysterious new coronavirus spreading around the world was now running rampant within BHCHP's highly vulnerable patient population: people experiencing homelessness in Boston. A nonprofit community health center, BHCHP for 35 years had been the primary care provider for Boston's homeless community. Over the preceding month, BHCHP's nine-person incident command team, spearheaded by Gaeta and CEO Barry Bock, had spent long hours reorganizing the program. (See Boston Health Care for the Homeless (A): Preparing for the COVID-19 Pandemic.) BHCHP leaders now confronted the most urgent challenge of their long medical careers. Without previous experience in large-scale disaster medicine, Gaeta and her colleagues had in short order to design and implement a disaster medicine model for COVID-19 that served the unique needs of people experiencing homelessness.
This case study recounts the decisive actions BHCHP leaders took to uncover unexpectedly widespread COVID-19 infection among Boston's homeless community in early April 2020. It details how they overcame their exhaustion to quickly design, staff, and operate the newly erected Boston Hope field hospital for the city's homeless COVID-19 patients. It then shows how they adjusted their disaster medicine model when faced with on-the-ground realities at Boston Hope regarding patients' psychological needs, limited English capabilities, substance use disorders, staff stress and burnout, and other issues.
Al Kasir, A., Coles, E. & Siegrist, R. , 2019. Anchoring Health beyond Clinical Care: UMass Memorial Health Care’s Anchor Mission Project , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract As the Chief Administrative Officer of UMass Memorial Health Care (UMMHC) and president of UMass Memorial (UMM) Community Hospitals, Douglas Brown had just received unanimous and enthusiastic approval to pursue his "Anchor Mission" project at UMMHC in Worcester, Massachusetts. He was extremely excited by the board's support, but also quite apprehensive about how to make the Anchor Mission a reality. Doug had spearheaded the Anchor Mission from its earliest exploratory efforts. The goal of the health system's Anchor Mission-an idea developed by the Democracy Collaborative, an economic think tank-was to address the social determinants of health in its community beyond the traditional approach of providing excellent clinical care. He had argued that UMMHC had an obligation as the largest employer and economic force in Central Massachusetts to consider the broader development of the community and to address non-clinical factors, like homelessness and social inequality that made people unhealthy. To achieve this goal, UMMHC's Anchor Mission would undertake three types of interventions: local hiring, local sourcing/purchasing, and place-based community investment projects. While the board's enthusiasm was palpable and inspiring, Doug knew that sustaining it would require concrete accomplishments and a positive return on any investments the health system made in the project. The approval was just the first step. Innovation and new ways of thinking would be necessary. The bureaucracy behind a multi-billion-dollar healthcare organization would need to change. Even the doctors and nurses would need to change! He knew that the project had enormous potential but would become even more daunting from here.
This teaching case study examines psychological trauma in a community context and the relevance, both positive and negative, of social determinants of health. Healthy People 2020 views people residing in communities with large-scale psychological trauma as an emerging issue in mental health and mental health disorders (Healthy People, 2016). The case study, which focuses on Newark, New Jersey, addresses three of the five key determinants of health: social and community context, health and health care, and neighborhood and built environment. The three key determinants are addressed using psychological trauma as an exemplar in the context of trauma-informed systems. The social and community context is addressed using concepts of social cohesion, civic participation, and discrimination. Access to health and health care are addressed with discussion of access to mental health and primary care services, health literacy, and the medical home model. Neighborhood and built environment are viewed through the lens of available government and NGO programs and resources to improve the physical environment with a focus on quality of housing, crime and violence, and environmental conditions. Upstream interventions designed to improve mental health and well-being that support trauma-informed systems are analyzed. The use of Newark as the case study setting allows a real-life exploration of each of these three key determinants of health.
This case study has four sections – introduction, case study, side bar, and vignettes. Learners should work through the case, access appropriate resources, and work in a team for successful completion.
Filter cases
Author affiliation.
- Harvard T.H. Chan School of Public Health (98) Apply Harvard T.H. Chan School of Public Health filter
- Harvard Business School (22) Apply Harvard Business School filter
- Global Health Education and Learning Incubator at Harvard University (12) Apply Global Health Education and Learning Incubator at Harvard University filter
- Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) (11) Apply Strategic Training Initiative for the Prevention of Eating Disorders (STRIPED) filter
- Social Medicine Consortium (8) Apply Social Medicine Consortium filter
- Harvard Kennedy School of Government (1) Apply Harvard Kennedy School of Government filter
- Harvard Malaria Initiative (1) Apply Harvard Malaria Initiative filter
- Women, Gender, and Health interdisciplinary concentration (1) Apply Women, Gender, and Health interdisciplinary concentration filter
Geographic focus
- United States (63) Apply United States filter
- Massachusetts (14) Apply Massachusetts filter
- International/multiple countries (11) Apply International/multiple countries filter
- California (6) Apply California filter
- Mexico (4) Apply Mexico filter
- India (3) Apply India filter
- Israel (3) Apply Israel filter
- New York (3) Apply New York filter
- Bangladesh (2) Apply Bangladesh filter
- Colorado (2) Apply Colorado filter
- Guatemala (2) Apply Guatemala filter
- Haiti (2) Apply Haiti filter
- Japan (2) Apply Japan filter
- Kenya (2) Apply Kenya filter
- South Africa (2) Apply South Africa filter
- Uganda (2) Apply Uganda filter
- United Kingdom (2) Apply United Kingdom filter
- Washington state (2) Apply Washington state filter
- Australia (1) Apply Australia filter
- Cambodia (1) Apply Cambodia filter
- China (1) Apply China filter
- Connecticut (1) Apply Connecticut filter
- Egypt (1) Apply Egypt filter
- El Salvador (1) Apply El Salvador filter
- Honduras (1) Apply Honduras filter
- Liberia (1) Apply Liberia filter
- Louisiana (1) Apply Louisiana filter
- Maine (1) Apply Maine filter
- Michigan (1) Apply Michigan filter
- Minnesota (1) Apply Minnesota filter
- New Jersey (1) Apply New Jersey filter
- Nigeria (1) Apply Nigeria filter
- Pakistan (1) Apply Pakistan filter
- Philippines (1) Apply Philippines filter
- Rhode Island (1) Apply Rhode Island filter
- Turkey (1) Apply Turkey filter
- Washington DC (1) Apply Washington DC filter
- Zambia (1) Apply Zambia filter
Case availability & pricing
- Available for purchase from Harvard Business Publishing (73) Apply Available for purchase from Harvard Business Publishing filter
- Download free of charge (50) Apply Download free of charge filter
- Request from author (4) Apply Request from author filter
Case discipline/subject
- Healthcare management (55) Apply Healthcare management filter
- Social & behavioral sciences (41) Apply Social & behavioral sciences filter
- Health policy (35) Apply Health policy filter
- Global health (28) Apply Global health filter
- Multidisciplinary (16) Apply Multidisciplinary filter
- Child & adolescent health (15) Apply Child & adolescent health filter
- Marketing (15) Apply Marketing filter
- Environmental health (12) Apply Environmental health filter
- Human rights & health (11) Apply Human rights & health filter
- Social innovation & entrepreneurship (11) Apply Social innovation & entrepreneurship filter
- Women, gender, & health (11) Apply Women, gender, & health filter
- Finance & accounting (10) Apply Finance & accounting filter
- Population health (8) Apply Population health filter
- Social medicine (7) Apply Social medicine filter
- Epidemiology (6) Apply Epidemiology filter
- Nutrition (6) Apply Nutrition filter
- Technology (6) Apply Technology filter
- Ethics (5) Apply Ethics filter
- Life sciences (5) Apply Life sciences filter
- Quality improvement (4) Apply Quality improvement filter
- Quantative methods (3) Apply Quantative methods filter
- Maternal & child health (1) Apply Maternal & child health filter
Health condition
- Cancer (3) Apply Cancer filter
- COVID-19 (3) Apply COVID-19 filter
- Obesity (3) Apply Obesity filter
- Breast cancer (2) Apply Breast cancer filter
- Disordered eating (2) Apply Disordered eating filter
- Ebola (2) Apply Ebola filter
- Influenza (2) Apply Influenza filter
- Injury (2) Apply Injury filter
- Malaria (2) Apply Malaria filter
- Alcohol & drug use (1) Apply Alcohol & drug use filter
- Asthma (1) Apply Asthma filter
- Breast implants (1) Apply Breast implants filter
- Cardiovascular disease (1) Apply Cardiovascular disease filter
- Cervical cancer (1) Apply Cervical cancer filter
- Cholera (1) Apply Cholera filter
- Food poisoning (1) Apply Food poisoning filter
- HPV (1) Apply HPV filter
- Malnutrition (1) Apply Malnutrition filter
- Meningitis (1) Apply Meningitis filter
- Opioids (1) Apply Opioids filter
- Psychological trauma (1) Apply Psychological trauma filter
- Road traffic injury (1) Apply Road traffic injury filter
- Sharps injury (1) Apply Sharps injury filter
- Skin bleaching (1) Apply Skin bleaching filter
Diversity and Identity
- Female protagonist (13) Apply Female protagonist filter
- Health of diverse communities (11) Apply Health of diverse communities filter
- Protagonist of color (5) Apply Protagonist of color filter
Supplemental teaching material
- Teaching note available (70) Apply Teaching note available filter
- Multi-part case (18) Apply Multi-part case filter
- Additional teaching materials available (12) Apply Additional teaching materials available filter
- Simulation (2) Apply Simulation filter
- Teaching pack (2) Apply Teaching pack filter
- Teaching example (1) Apply Teaching example filter
Browse our case library
This case describes the challenges facing Jon Moussally, the CEO of TraumaLink, a four-year-old social venture that provided trauma first aid to victims of traffic injuries in Bangladesh, a country that had some of the most dangerous highways in the world but no formal emergency response system. Jon, a practicing emergency room physician and public health student, had been shocked by the chaotic traffic that he observed during a trip to Dhaka, Bangladesh, for a course on global health issues. Over the next 18 months, Jon and three partners—two fellow students and the Bangladeshi head of a local social venture organization—decided on a three-pronged approach: they would train community-based volunteers who lived or worked close to the highway to provide free basic trauma first aid; they would develop an easy-to-use 911-type software system to deploy volunteers quickly to a crash scene; and they planned to raise operating funds by selling advertising or subscriptions to companies in Bangladesh whose workers travelled the dangerous highways daily.
By the fall of 2017, TraumaLink had been successfully launched along two sections of particularly dangerous highways. Their trained volunteers had been able to quickly and effectively provide first aid to victims of traffic injuries. The software had worked well to notify and deploy volunteers and collect data. However, Jon and his partners had not yet found sustainable, long-term sources of revenue, despite almost four years of trying. After an initial pilot phase in November 2014, the organization had been awarded $142,500 by the US Agency for International Development, but these funds would run out by the end of 2018, with little chance of another round.
TraumaLink had proven that they could deliver emergency services and save lives, but could Jon and his partners figure out how to become financially sustainable so that they could continue to support and expand their services within Bangladesh and possibly beyond?
"The foundation of Integrated Health Services is the relentless pursuit of value. Our fundamental purpose is to help IBM win in the marketplace through the health and productivity of our workforce." ---Martín Sepúlveda
Martín Sepúlveda, Vice President of Integrated Health Services at IBM, had played a central role in establishing IHS as a vital and ongoing contributor to the corporation's success. IBM's IHS organization, as it had come to be known in 2008, was a global team of approximately 250 occupational medicine, industrial hygiene, safety, health benefits and wellness professionals responsible for ensuring the health and well-being of IBM's over 400,000 employees worldwide. This case, set in 2011, highlights the many challenges and his team faced in developing strategies and approaches to creating a culture of health within IBM, and maintain its commitment to the well-being of every employee.
Siegrist, R. , 2014. Eastern Cape Clinic (Parts A, B, & C) , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract Thandeka Sisulu had just been hired as the new administrative director for the Eastern Cape Clinic, located in the outskirts of the South African city of East London. The Clinic had opened about 18 months ago with support from the government and from two anonymous donor groups. Those funds would soon run out and Thandeka faced the dual challenge of helping the Clinic become self-sufficient and dealing with the long wait times for patients to be seen. She knew that the budget for this year projected a loss, so she decided to better understand the financial problem first.
Moon, S. & Gordon, R. , 2014. Ensuring Vaccine Supply for the Next Pandemic Flu , Harvard University: Global Health Education and Learning Incubator. Access online Abstract This case highlights the challenges of managing externalities and sovereignty through the example of pandemic flu. Recent outbreaks of both the H5N1 and H1N1 influenza strains have illustrated that the global institutions charged with preventing and responding to these pandemics are not up to the task. With both, there were significant problems with the development, production, and distribution of flu vaccines. Indeed, stemming a modern day pandemic depends on the rapid development, sufficient production, and equitable, timely access to influenza vaccines, all within a complex global context. Compounding these challenges are the disease-specific “unknowns” related to the emergence of a new virus, including severity levels, transmission ease, human immunity, and drug vulnerability. Specific themes covered in "Ensuring Vaccine Supply for the Next Pandemic Flu: Will the World Be Ready?" include issues of sovereignty; the legitimacy, authority, and credibility of the World Health Organization (WHO); uncertainty and risk; world dependence on private vaccine manufacturers for an essential public health good; health as a security issue; and equity issues in vaccine distribution.
2018. Western Public Health Casebooks: Cases from the Schulich Interfaculty Program in Public Health , Western University: Schulich School of Medicine & Dentistry. Access online Abstract A collection of cases written by MPH students of the Schulich Interfaculty Program in Public Health at Western University, Canada. These casebooks--from 2015, 2016, 2017, and 2018--may be copied and used free of charge without permission for any educational uses by an accredited educational institution.
Solomon, C. & Kane, N.M. , 2016. Strategic Change at Whitman-Walker Health , Harvard Business Publishing: Harvard T.H. Chan School of Public Health case collection. Available from Harvard Business Publishing Abstract In the seven years since Don Blanchon was hired as the Chief Executive Officer of Whitman-Walker Health, it had transitioned into a primary care-based community health center and a patient-centered medical home serving a diverse population in a rapidly changing area of Washington, DC. The Affordable Care Act of 2010 would, in Blanchon’s view, increase access to providers for WWH’s patient population, thereby increasing the competition. The implications of this change left senior management with unresolved strategic questions. Should WWH pursue a “hybrid FQHC model,” a new location, new services, or a future strategic partnership with a large health system? What should the next direction be for WWH, and how should it get there?
In February 2015, technical staff reviewed the results from a jointly conducted study on malaria control. This study had major implications for malaria in Zambia—and elsewhere. The preliminary analysis strongly suggested that the study’s Mass Drug Administration (MDA) strategy was reducing the incidence of malaria disease. In addition, MDA seemed to be driving down the infection reservoir among asymptomatic people in the study area of the Southern Province of Zambia. Further analysis with mathematical models indicated that if the intervention was sustained so current trends continued, then the MDA strategy would make it possible to eliminate malaria in the Southern Province.
If malaria could be eliminated in one region of Zambia, that would provide new evidence and motivation to work towards elimination throughout the country, an ambitious goal. But it would not be easy to move from conducting one technical study in a single region to creating a national strategy for malaria elimination. The scientists realized that their new data and analyses—of malaria infections, mosquito populations, and community health worker activities—were not enough. A national malaria elimination effort would require mobilizing many partners, national and local leaders, and community members, and convincing them to get on board with this new approach.
Teaching note available for faculty/instructors .
On February 1, 2020, Jessie Gaeta, the chief medical officer for Boston Health Care for the Homeless Program (BHCHP), received news that a student in Boston had tested positive for the novel coronavirus virus that causes COVID-19 disease. Since mid-January, Gaeta had been following reports of the mysterious virus that had been sickening people in China. Gaeta was concerned. Having worked for BHCHP for 18 years, she understood how vulnerable people experiencing homelessness were to infectious diseases. She knew that the nonprofit program, as the primary medical provider for Boston’s homeless population, would have to lead the city’s response for that marginalized community. She also knew that BHCHP, as the homeless community’s key medical advocate, not only needed to alert local government, shelters, hospitals, and other partners in the city’s homeless support network, but do so in a way that spurred action in time to prevent illness and death.
The case study details how BHCHP’s nine-person incident command team quickly reorganized the program and built a detailed response, including drastically reducing traditional primary care services, ramping up telehealth, and redeploying and managing staff. It describes how the team worked with partners and quickly designed, staffed, and made operational three small alternative sites for homeless patients, despite numerous challenges. The case then ends with an unwelcome discovery: BHCHP’s first universal testing event at a large city shelter revealed that one-third of nearly 400 people there had contracted COVID-19, that most of the infected individuals did not report symptoms, and that other large city shelters were likely experiencing similar outbreaks. To understand how BHCHP and its partners subsequently popped up within a few days a 500-bed field hospital, which BHCHP managed and staffed for the next two months, see Boston Health Care for the Homeless (B): Disaster Medicine and the COVID-19 Pandemic.
- Education Home
- Medical Education Technology Support
- Graduate Medical Education
- Medical Scientist Training Program
- Public Health Sciences Program
- Continuing Medical Education
- Clinical Performance Education Center
- Center for Excellence in Education
- Research Home
- Biochemistry & Molecular Genetics
- Biomedical Engineering
- Cell Biology
- Genome Sciences
- Microbiology, Immunology, & Cancer Biology (MIC)
- Molecular Physiology & Biological Physics
- Neuroscience
- Pharmacology
- Public Health Sciences
- Office for Research
- Clinical Research
- Clinical Trials Office
- Funding Opportunities
- Grants & Contracts
- Research Faculty Directory
- Cancer Center
- Cardiovascular Research Center
- Carter Immunology Center
- Center for Behavioral Health & Technology
- Center for Brain Immunology & Glia
- Center for Diabetes Technology
- Center for Immunity, Inflammation & Regenerative Medicine
- Center for Membrane & Cell Physiology
- Center for Research in Reproduction
- Myles H. Thaler Center for AIDS & Human Retrovirus Research
- Child Health Research Center (Pediatrics)
- Division of Perceptual Studies
- Research News: The Making of Medicine
- Core Facilities
- Virginia Research Resources Consortium
- Center for Advanced Vision Science
- Charles O. Strickler Transplant Center
- Keck Center for Cellular Imaging
- Institute of Law, Psychiatry & Public Policy
- Translational Health Research Institute of Virginia
- Clinical Home
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopaedic Surgery
- Otolaryngology
- Physical Medicine & Rehabilitation
- Plastic Surgery, Maxillofacial, & Oral Health
- Psychiatry & Neurobehavioral Sciences
- Radiation Oncology
- Radiology & Medical Imaging
- UVA Health: Patient Care
- Diversity Home
- Diversity Overview
- Student Resources
- GME Trainee Resources
- Faculty Resources
- Community Resources
- Medical Student Case Studies
Each student is required to prepare a teaching case to present to his/her colleagues and the course director. Past examples provided below.
General Diagnostic Case Studies
- Arteriovenous Fistula Secondary to Trauma
- Chylothorax, Cellulitis, Gas Gangrene
- Ectopic ACTH-Secreting Tumor
- Epiphrenic Diverticula
- Incidental Mediastinal Hilar Lymphadenopathy
- Liver Metastasis
- Neurocystercircosis
- Pneumoperitoneum
- Pneumothorax
- Posterior Urethralcutaneous Fistula
- Renal Cysts
- Rocky Mountain Spotted Fever
- Septic Emboli to the Brain
- Submassive Bilateral PE
- Tailgut Duplication Cyst
- Tension Pneumocephalus
- Tracheo-Esophageal Fistula
- Vestibular Schwannoma
Radiology Pathology Correlation Case Studies
- Adenoid Cystic Carcinoma
- Cholangiocarcinoma
- Cryptococcal PNA
- Disseminated Histoplasmosis
- Lung Adenocarcinoma
- Marginal Zone B-cell Lymphoma
- Metastatic Urothelial Carcinoma
- Mixed Clear Cell Papillary RCC
- Ovarian Carcinoma
- Pancreatic Adenocarcinoma
- Squamous Cell Carcinoma of the Lung
- Squamous Cell Carcinoma
- Uterine Leiomyosarcoma
- Cervical Adenosquamous Carcinoma
- Clear Cell Renal Cell Carcinoma
- Esophageal Adenocarcinoma
- Metastic Esophageal Gastrointestinal Stomal Tumor
- Ocular Melanoma with Mets to Liver
- Pancreatic Metatasis
- Papillary Thyroid Carcinoma
- Papillary Thyroid Carcinoma #2
- Renal Transplant Rejection
- Small Cell Lung Cancer
- Urothelial Carcinoma Lung Met
- Yolk Sac Tumor
- Burkitt’s Lymphoma
- Ewing Sarcoma
- Hepatocellular Carcinoma
- Hepatocellular Carcinoma #2
- High-grade Serous Ovarian Carcinoma
- Metastatic Duodenal Adenocarcinoma
- Metastatic Melanoma
- Ovarian Cancer
- Papillary Thyroid Carcinoma #3
- Papillary Thyroid Carcinoma with Nodal Involvement
- Well Differentiated Hepatocellular Carcinoma
- How to Apply
- Alexander (Sasha) Sytov, MD
- Alexander Zhang, MD
- Anna Osment, MD
- Connor Sleeth, MD
- Eric Fromke, MD
- Hannah Clode, MD
- Jenna Pollock, MD
- Jineet Patel, MD
- Joshua Hunsaker, MD
- Joshua Ravicz, MD
- Julia Kariher, MD
- Kaelin Cockrell, MD
- Maclean Cook, MD
- Marissa Boettcher, MD
- Nabeel Mirza, MD
- Nathan Leaphart, MD
- Qi (Phoebe) Dong, MD
- Samantha Epstein, MD
- Tyler Dalton, MD
- Vatsal Lal, MD
- Warren Campbell IV, MD, PhD
- Wayne Dell, MD
- Zachary Miller, MD, PhD
- Salary and Benefits
- Resident Lifestyle
- Early Specialization in Interventional Radiology (ESIR)
- Diagnostic Radiology/Nuclear Medicine (DR/NM) Pathway
- Diagnostic Radiology Research Track
- Current IR Residents
- Where Are They Now?
- Letter from the Chief Residents
- Former Residents
- Your UVA Interview Day
- Living in Charlottesville
- Participating Residents
- Program News and Updates
- Make a Gift
- Current Representatives
- Ladyologists – Supporting Each Other
- 4th-year Medical Students Scholarship
- Radiology Electives
- Radiology Interest Group
- Abdominal Imaging
- Breast Imaging
- Cardiothoracic Imaging
- Diagnostic Neuroradiology
- Musculoskeletal Imaging
- Nuclear Radiology
- Pediatric Radiology
- Angiography and Interventional Radiology Observership
- Breast Imaging International Visiting Scholars
- Why Choose Structured Education?
- Program Directors
- Verification of Graduate Medical Education Training and Faculty Appointment
- Online Training Resources
- Case report
- Open access
- Published: 14 August 2024
Doege-Potter syndrome due to a solitary fibrous tumor of the pleura: a case report
- Juan Estrada-Maya ORCID: orcid.org/0000-0003-3543-6958 1 , 2 ,
- Juan Sebastián Montejo ORCID: orcid.org/0000-0002-1598-5637 1 , 2 ,
- Katerin Dayana Báez López ORCID: orcid.org/0000-0002-9182-9417 3 &
- Juan Carlos Garzón 4
Journal of Medical Case Reports volume 18 , Article number: 383 ( 2024 ) Cite this article
160 Accesses
Metrics details
Doege-Potter syndrome is a rare paraneoplastic phenomenon associated with solitary fibrous tumors of the pleura (SFTPs). It is characterized by the presence of severe, sustained, and treatment-refractory hypoglycemia. Hypoglycaemia, which may be the sole symptom at disease onset, is mediated by the secretion of high-molecular-weight insulin-like growth factor (IGF-2). Most tumors exhibit benign behavior, with a 100% survival rate at 5 years. However, 10% of these tumors may display aggressive behavior with local or metastatic recurrence. We present a clinical case of a patient with a benign solitary fibrous tumor of the pleura who presented with symptomatic hypoglycemia and required pulmonary and pleural surgical resection to control the paraneoplastic phenomenon.
Case presentation
A Hispanic 46-year-old man presented with a 15-day history of transient alterations in consciousness worsened by fasting. The relevant medical history included obstructive sleep apnea treated with continuous positive air pressure (CPAP) and previous smoking. In-hospital studies revealed noninsulinemic hypoglycemia and a benign SFTP. Complete surgical resection was performed while the patient received dextrose fluids and corticosteroids perioperatively for hypoglycemia. Subsequently, the hypoglycemia resolved, and the patient was followed-up without disease recurrence.
Doege-Potter syndrome is challenging to recognize. However, effective treatment can be achieved with a high survival rate. Raising awareness among healthcare professionals about the recognition of this paraneoplasic syndrome patients will improve diagnostic suspicion, biochemical confirmation, the development of diagnostic and therapeutic guidelines, and the creation of predictive indices for aggressive presentations requiring closer monitoring.
Peer Review reports
Non-Islet Cell Tumor Hypoglycemia (NICTH) is an uncommon paraneoplastic condition caused by the synthesis of insulin-like growth factor type 2 (IGF-2) by benign and malignant nonpancreatic tumors [ 1 ]. This condition, first described by Karl Doege and Roy Potter in 1930 is characterized by recurrent and refractory hypoglycemia in the presence of an intrathoracic solitary fibrous tumor [ 2 ]. Doege-Potter syndrome is attributed to non-insulin-induced hypoglycemia caused on by fibrous tumors, while it can also be seen in mesotheliomas, liposarcoma, rhabdomyosarcoma, leukemia, lymphoma, and teratoma [ 3 ].
Solitary fibrous tumors are mesenchymal neoplasms that make up 2% of soft tissue tumors [ 4 ]. While they typically develop in the pleura, they can also affect the peritoneum, pericardium, and mediastinum [ 5 ]. Although rare, they occur at a rate of 2.8 per 100,000 people and usually have an indolent and benign course in 90% of cases [ 6 ]. However, about 5% of patients develop difficult-to-manage non-insulin-induced hypoglycemia [ 7 , 8 ].
Doege-Potter syndrome patients are difficult to identify since their condition is rarely taken into account while making a differential diagnosis of hypoglycemia. Case reports and short series make up the majority of the literature on Doege-Potter syndrome [ 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ]. By sharing our experience and highlighting interesting aspects of the pathophysiology, our case report seeks to advance understanding of this syndrome.
We present the case of a Hispanic 46-year-old male from Bogotá, Colombia, with a 15-day history of disorientation, altered thought content, stereotyped movements of the upper limbs, and episodes of heteroaggressive behavior. The patient, who was diagnosed with obstructive sleep apnea (OSA) using continuous positive air pressure (CPAP), had a history of smoking cessation (5 pack-years) and a recently identified suspicious right lung mass on outpatient chest computed tomography (CT). There was no other relevant personal or family history.
Upon admission to the CardioInfantil Foundation-Cardiology Institute, the patient was in good condition with all vital signs at normal ranges. Physical examination revealed digital clubbing (Fig. 1 ) in both hands, skin thickening between the eyes, also known as pachydermoperiostosis, absence of breath sounds in the right hemithorax, and a normal neurological examination.

Image of the patient highlighting physical examination findings: digital clubbing indicated by a red arrow. The patient's face has been obscured to protect his identity
Mixed delirium was considered the initial working diagnosis. The admission laboratory results are presented in Table 1 . Neurologic services ruled out structural central nervous system components through cranial CT and contrast-enhanced cerebral magnetic resonance imaging (MRI), both of which were normal. Twelve-hour electroencephalography showed no ictal activity. According to the described history and semiological findings, a chest X-ray (Fig. 2 ) revealed a radiopaque mass occupying the right hemithorax. Thoracic surgeons indicated that an incisional biopsy after a chest CT scan (Fig. 3 ) revealed a pleura-dependent mass affecting the right hemithorax and compressing the ipsilateral lung parenchyma.

Anteroposterior (AP) and lateral chest radiographs, highlighting a radiodense space-occupying lesion with ill-defined borders and mild ipsilateral pleural effusion, accompanied by subsegmental atelectasis in the ipsilateral hilar regions
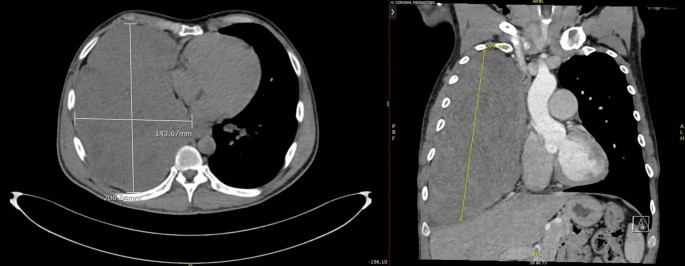
Chest computerized tomography (CT) of axial (left) and coronal (right) sections revealed a large solid mass with extrapulmonary features, demonstrating mild heterogeneous enhancement and some coarse calcifications in its lower portion, measuring approximately 229 by 204 by 124 mm, occupying nearly the entire right hemithorax. An apparent vascular supply was observed from branches of the right middle adrenal artery and right internal mammary artery
During the procedure, the patient experienced a relapse of neurological symptoms, including stupor, upwards gaze deviation, and profuse diaphoresis, which were identical to what family members had reported. A glucometer reading of 35 mg/dl indicated severe symptomatic hypoglycemia. Intravenous correction with 10% dextrose in distilled water resulted in full symptom reversal, recovery of consciousness with amnesia of the incident, and further biochemical investigations (Table 1 ).
Despite a constant intravenous 10% dextrose infusion rate of 20 cc/h, the patient continued to experience episodes of hypoglycemia. The addition of 10 mg of prednisolone resulted in the remission of neuroglycopenic episodes and glycemic control (Fig. 4 ).

Hospitalized serum fasting glucose patterns
An open approach involving right thoracotomy was used for tumor removal, and paraneoplastic phenomena due to the intrathoracic mass were considered. Nonanatomic lung resection of the anterobasal segment of the right lower lobe was used to remove the entire tumor. The infiltrative involvement and secondary adhesions of the tumor pose difficulties for surgical treatment, especially when releasing the vascular pedicle. In the end, a total resection of the 25 × 18 × 20 cm mass was obtained (Fig. 5 ). A solitary fibrous tumor of the pleura was confirmed by histopathological investigation (Fig. 6 ) and classified as low risk by modified risk stratification criteria proposed by DEMICCO et al. in 2017 [ 17 ].
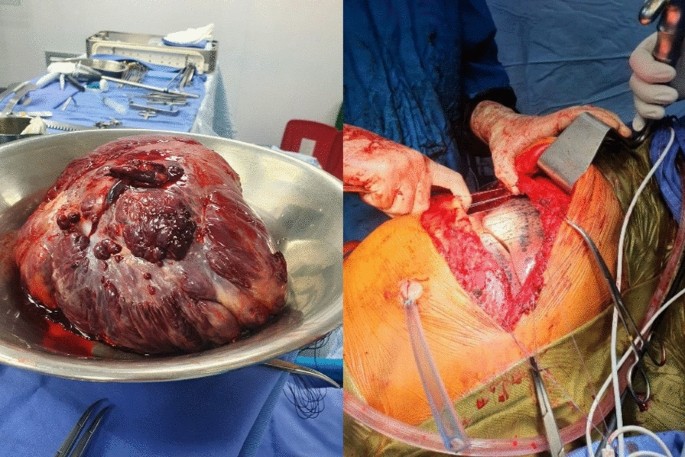
(Left) Large right intrathoracic mass measuring 25 by 18 by 20 cm, originating from the medial and subpulmonary aspects of the right lower lobe, with multiple adhesions. (Right) Complete lung expansion after mass removal without lung compromise
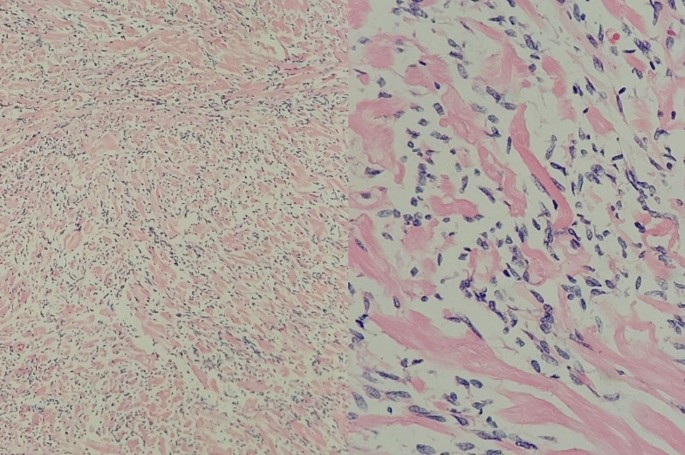
Fusocellular tumors with moderately dense collagenous stroma, delicate and branching vasculature, devoid of mitotic activity, necrosis, cellular atypia, or areas of hypercellularity. Low-risk solitary fibrous tumor stratification was performed according to the 2017 DEMICCO et al. [ 17 ] criteria
Adequate lung re-expansion was observed on postoperative chest X-ray (Fig. 7 ). The patient maintained good glycemic control during the postoperative period. Consequently, he was discharged after 5 days with a nasal cannula for oxygen after five days, along with orders for follow-up visits with Thoracic Surgery, Endocrinology, and Pulmonology. The patient had a Follow-up check up at3, 6, and 12 months post-discharge, during which blood glucose levels were evaluated and found to be within normal range. Additionally, there was an improvement in digital clubbing (Fig. 8 ), as evidenced by the previously described images. The patient was still free of tumor recurrence.
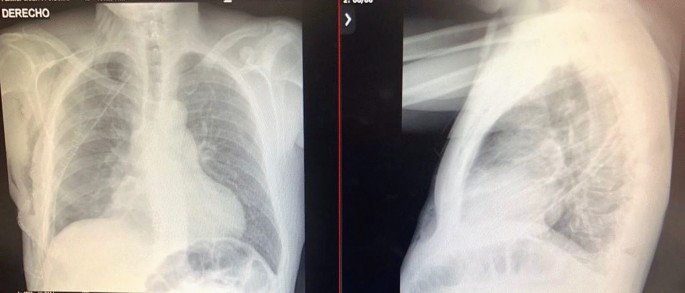
Postoperative anteroposterior (AP) and lateral chest radiography demonstrating lung re-expansion, with clear costophrenic and cardiophrenic angles

Image of the patient during the ambulatory follow-up period, revealing evidence of resolution of cutaneous changes
A classic instance of Doege-Potter syndrome was documented, with a solitary fibrous tumor of the pleura causing difficult-to-treat severe symptomatic hypoglycemia. Despite having all neuroglycopenic (behavioral changes, drowsiness, confusion), adrenergic (anxiety, tremor, palpitations), and autonomic (hunger, diaphoresis) symptoms, hypoglycemia is rarely diagnosed in non-diabetic patients [ 15 ]. And if it is suspected, generally it is considered to have more common causes outside of insulin, like drug side effects (sulfonylureas, antibiotics), alcohol, malnutrition, liver or kidney failure, and endocrine causes (endogenous hyperinsulinism and adrenal insufficiency) [ 15 ]. As a result, non-pancreatic malignancies are seldom considered to cause hypoglycemia, yet it can be the only manifestation of the disease [ 12 ].
Solitary fibrous tumors (SFTs) are rare soft tissue neoplasms that develop from submesothelial mesenchymal cells with fibroblastic differentiation [ 18 ]. Although first described as intrathoracic, the majority of instances come from the visceral pleura, accounting for less than 5% of all pleural malignancies. They may additionally arise within the lungs from the parenchyma, mediastinum, or diaphragm. Other common tumor sites are the retroperitoneum, pelvis, liver, and mediastinum [ 18 , 19 ]. They are typically benign tumors with slow growth that become symptomatic only when they reach a significant size, resulting in cough, dyspnea, chest discomfort, pleural effusion, or digital clubbing [ 16 ], as shown in our instance.
Hypoglycemia associated with these tumors is infrequent and is known as Doege-Potter syndrome, accounting for less than 5% of all cases [ 5 , 20 ]. In this condition, changes in IGF-2 folding result in the generation of bigger peptides, which impede cellular receptors signaling pathways of counterregulatory hormones, favoring hypoglycemia states [ 21 ]. However, the presence of "large" IGF-2 does not guarantee a relationship with NICTH episodes. Lloyd et al. found that 83.3% of fibrous tumors expressed IGF-2 mRNA, while only 7.1% of patients experienced hypoglycemia [ 22 ]. Predictors for the biochemical diagnosis of NICTH include an IGF-2/IGF-1 ratio greater than 3 and inhibition of IGF-1 expression [ 14 , 23 ]. Although these tests were not done on our patient due to study constraints, other non-insulin-induced hypoglycemia diagnostic criteria, such as reduced insulin levels and undetectable C-peptide, were present [ 20 , 24 , 25 ].
Currently, there are no clinical practice guidelines for NICTH patients. The initial therapy is usually symptomatic, with an intravenous dextrose bolus or infusion while waiting for surgery. In this example, a continuous infusion of dextrose fluids was employed to treat hypoglycemia as an interim measure for tumor removal. Previous research found that corticosteroids at dosages greater than 25 mg/day of prednisolone reduced hypoglycemia episodes by 75% in medically treated individuals by decreasing "large" IGF-2 [ 26 ]. Bourciguax et al. demonstrated the efficacy of combination corticosteroid and growth hormone therapy in treating hypoglycemic episodes [ 27 ]. The use of glucagon is more controversial, with inconsistent outcomes [ 14 ].
The definitive treatment is a full surgical excision of the tumor with clear margins [ 18 , 25 ]. The histological report of the neoplasia has no bearing on the curative surgical technique. Tumor size determines the type of surgery performed: thoracotomy for large tumors orthoracoscopy for small tumors. Complete mass excision has a 5-year survival rate of 100%, with a recurrence risk of 20% [ 28 ]. In our case, nonanatomic excision of the anterobasal portion of the lower right lobe was done by thoracotomy. Vascular pedicle inscision was made for total tumor mass release and subsequent linear mechanical suturing. Adequate postprocedural lung re-expansion was demonstrated, indicating the likelihood of total excision (Fig. 2 ). Other therapeutic options for cytoreduction, such as glucocorticoids, chemotherapy, and radiotherapy, were not investigated in this case, as surgery was provided as a curative attempt [ 25 ]. Anthracycline-based chemotherapy regimens [ 29 ] are available for individuals whose cancers are unresectable or have metastatic disease. In other cases, combination therapy with temozolomide and bevacizumab may be recommended [ 20 ]. There is currently insufficient data to support the use of radiotherapy, and there are few descriptive studies and case reports using brachytherapy and photodynamic therapy during the preoperative period [ 25 ].
When compared to other recorded Doege-Potter syndrome cases around the world and in Colombia, some epidemiological points stand out. The patient's age at clinical presentation was lower than that documented in the literature, with the disease peaking between the sixth and eighth decades of life [ 10 ]. Furthermore, this is the first recorded male incidence in Colombia in contrast to two prior cases in females [ 15 , 16 ], for a syndrome in which it is uncertain if women are more affected than men [ 9 ]. Additionally, it is a case of non-insulin-induced hypoglycemia (NICTH) caused by a benign tumor, which is generally associated with malignancies in up to 56% of situations [ 14 ]. Finally, a right-sided pleural tumor with a right-to-left ratio larger than 2 was found, which is indicative of a tumor linked to hypoglycemia [ 14 ].
Regarding the strengths and limitations of our approach, it is worth noting that the previous medical record of lung mass skewed the initial approach, which aimed to rule out intracerebral metastases while overlooking metabolic causes on admission analytics. Yet, once hypoglycemia was identified, interdisciplinary collaboration across internal medicine, thoracic surgery, and endocrinology allowed recognition and medical attention of Doege-Potter syndrome, highlighting the value of teamwork. We acknowledge that the measurement of IGF-2 was not performed, and this laboratory result could have supported the diagnosis and served as a prognostic biomarker to define the risk of recurrence in light of the available literature. Aside from that, we believe our experience will be extremely beneficial to other healthcare professionals by raising awareness of Doege-Potter syndrome, enhancing early detection and effective patient management, and motivating future clinical research for evidence-based treatment guidelines.
Conclusions
As previously stated, NICTH is a difficult metabolic illness characterized by aggressive disease behavior, local recurrence, and metastatic involvement [ 26 ]. Counterregulatory hormones are frequently used to offset the endogenous activity of paraneoplastic hormones, but there is limited evidence. The relevance of prognostic biochemical, histological, and imaging parameters, such as IGF-2 levels, vimentin, CD34, bcl-2, or CD99 positivity but cytokeratin negativity, and tumor size > 10 cm, is unclear [ 13 ]. Raising knowledge among healthcare providers about Doege-Potter syndrome patients may serve to improve diagnostic suspicion, biochemical confirmation, and the creation of diagnostic and treatment guidelines. Future advancements are expected in developing models that can forecast aggressive disease presentations that necessitate closer monitoring.
Availability of data and materials
All data generated and analysed during the current study are included in this published article [and its supplementary information files].
Abbreviations
Continuous positive air pressure
Computed tomography
Insulin-like growth factor
Magnetic resonance imaging
Nonislet cell tumor hypoglycemia
Solitary fibrous tumors of the pleura
Solitary fibrous tumors
de Groot JW, Rikhof B, van Doorn J, et al . Non-islet cell tumourinduced hypoglycaemia: a review of the literature including two new cases. Endocr Relat Cancer. 2007;14:979–93.
Article PubMed Google Scholar
Baldwin RS. Hypoglycemia with neoplasia (Doege-Potter Syndrome). Wis Med J. 1965;64:185–9.
CAS PubMed Google Scholar
Bodnar TW, Acevedo MJ, Pietropaolo M. Clinical review: management of non-islet-cell tumor hypoglycemia: a clinical review. J Clin Endocrinol Metab. 2014;99(3):713.
Article CAS PubMed Google Scholar
Davanzo B, Emerson RE, Lisy M, Koniaris LG, Kays JK. Solitary fibrous tumor. Transl Gastroenterol Hepatol. 2018;21(3):94.
Article Google Scholar
Santos S.M. Fernandez R. Canto H. Doege-Potter syndrome: What hypoglycemia hid. Rev Clin Esp. 2018.
Gold JS, Antonescu CR, Hadju C, Ferrone CR, Hussain M, Lewis JJ, et al . Clinicopathologic correlates of solitary fibrous tumors. Cancer. 2002;94:1057–68.
Eastman RC, Carson RE, Orloff DG, et al . Glucose utilization in a patient with hepatoma and hypoglycaemia. Assessment by a positron emission tomography. J Clin Invest. 1992;89(6):1958–63.
Article CAS PubMed PubMed Central Google Scholar
Tietge UJ, Schofl C, Ocran KW, et al . Hepatoma with severe non-islet cell tumor hypoglycemia. Am J Gastroenterol. 1998;93(6):997–1000.
Kinoshita T, Ishii K, Higashiiwai H, et al . Malignant solitary fibrous tumour of the peritoneum. Clin Radiol. 2000;55:157–60.
Kalebi AY, Hale MJ, Wong ML, et al . Surgically cured hypoglycemia secondary to pleural solitary fibrous tumour: case report and update review on the Doege-Potter syndrome. J Cardiothorac Surg. 2009;4:45.
Article PubMed PubMed Central Google Scholar
Fukuda I, Hizuka N, Ishikawa Y, et al . Clinical features of insulinlike growth factor-II producing non-islet-cell tumor hypoglycemia. Growth Horm IGF Res. 2006;16:211–6.
Hizuka N, Fukuda I, Takano K, Okubo Y, Asakawa-Yasumoto K, Demura H. Serum insulin-like growth factor II in 44 patients with non-islet cell tumor hypoglycemia. Endocr J. 1998;45(Suppl):S61–5.
Miraki-Moud F, et al . A rapid method for analyzing serum pro-insulin-like growth factor-II in patients with non-islet cell tumor hypoglycemia. J Clin Endocrinol Metab. 2005;90(7):3819–23.
Han G, Zhang Z, Shen X, Wang K, Zhao Y, He J, Gao Y, Shan X, Xin G, Li C, Liu X. Doege-Potter syndrome: a review of the literature including a new case report. Medicine. 2017;96(27):e7417.
Sandoval-Alzate HF, Parra-Gamboa JM, Angulo-Casalis A. Doege-Potter syndrome. Acta Medica Colombiana. 2020;45(3):78–81.
Google Scholar
Muñoz-Gómez C, Almanza-Hurtado A, Rodríguez-Yáñez T, Suárez-Romero B, Rodríguez J, Remolina C, Castañeda O. Síndrome de Doege Potter. Acta Médica Colombiana. 2023;48(1S).
Demicco EG, Wagner MJ, Maki RG, Gupta V, Iofin I, Lazar AJ, Wang WL. Risk assessment in solitary fibrous tumors: validation and refinement of a risk stratification model. Mod Pathol. 2017;30(10):1433–42. https://doi.org/10.1038/modpathol.2017.54 .
Olson NJ, Linos K. Dedifferentiated solitary fibrous tumor: a concise review. Arch Pathol Lab Med. 2018;142(6):761–6. https://doi.org/10.5858/arpa.2016-0570-RS .
Sathyanarayanan SP, Añel-Tiangco RML, Tiangco NDL. Doege-Potter syndrome in a patient with solitary fibrous tumor of the lung: a rare cause of recurrent hypoglycemia. J Clin Transl Endocrinol Case Rep. 2022. https://doi.org/10.1016/j.jecr.2022.100112 .
Ogunsakin A, Hilsenbeck H, Portnoy D, Nyenwe E. Recurrent severe hypoinsulinemic hypoglycemia responsive to temozolomide and bevacizumab in a patient with Doege-Potter syndrome. Am J Med Sci. 2018;356(2):181–4. https://doi.org/10.1016/j.amjms.2018.01.008 .
Daughaday WH, Trivedi B, Baxter RC. Serum “big insulin-like growth factor II” from patients with tumor hypoglycemia lacks normal E-domain O-linked glycosylation, a possible determinant of normal propeptide processing. Proc Natl Acad Sci USA. 1993;90:5823–7.
Lloyd RV, Erickson LA, Nascimento AG, et al . Neoplasms causing nonhyperinsulinemic hypoglycemia. Endocr Pathol. 1999;10:291–7.
Rosseel L, De Leu N, Van Hecke W, et al . A rare case of hypoglycemia in a patient with elevated right hemidiaphragm. BMJ Case Rep. 2012;2012:bcr0320125972.
Cameselle R, Delfín Vázquez M, Piñeiro L, Fernández Martín R, MartínezVázquez C, García RVG. Tumor endotorácico hipoglucemiante síndrome de doege-potter. Arch Bronconeumol. 1990;26(7):317–9. https://doi.org/10.1016/s0300-2896(15)31576-3 .
Fernández-Trujillo L, Bolaños JE, Álvarez C, Giraldo J, Velásquez M, Zúñiga-Restrepo V, Pérez B, Sua LF. Doege-Potter syndrome and hypoglycemia associated with solitary fibrous tumor of the pleura: two case reports. Clin Med Insights Circ Respir Pulm Med. 2020;13(14):1179548420964759. https://doi.org/10.1177/1179548420964759 .
Santos RS, Haddad R, Lima CE, et al . Patterns of recurrence and longterm survival after curative resection of localized fibrous tumors of the pleura. Clin Lung Cancer. 2005;7:197–201.
Bourcigaux N, Arnault-Ouary G, Christol R, et al . Treatment of hypoglycemia using combined glucocorticoid and recombinant human growth hormone in a patient with a metastatic non-islet cell tumor hypoglycemia. Clin Ther. 2005;27:246–51.
Fabiana P, Pablo DRJ, Nebil L, Germán E, Shigeru K. Tumor fibroso solitario y síndrome Doege-Potter. Medicina (B Aires). 2018;78(1):47–9.
Stacchiotti S, Libertini M, Negri T, Palassini E, Gronchi A, Fatigoni S, Poletti P, Vincenzi B, Dei Tos AP, Mariani L, Pilotti S, Casali PG. Response to chemotherapy of solitary fibrous tumour: a retrospective study. Eur J Cancer. 2013;49(10):2376–83. https://doi.org/10.1016/j.ejca.2013.03.017 .
Download references
Acknowledgements
The authors wish to thank the Research Center of Fundación Cardioinfantil-Instituto de Cardiología, Bogotá, Colombia, for their contribution to the publication costs of this manuscript.
There was no funding for the work associated with this publication.
Author information
Authors and affiliations.
Internal Medicine, Fundación Cardioinfantil-Instituto de Cardiología, Calle 163ª#13B-60, Bogotá, Colombia
Juan Estrada-Maya & Juan Sebastián Montejo
School of Medicine and Health Sciences, Universidad del Rosario, Bogotá, Colombia
General Medicine, Fundación Cardioinfantil-Instituto de Cardiología, Bogotá, Colombia
Katerin Dayana Báez López
Thoracic Surgery, Fundación Cardioinfantil-Instituto de Cardiología, Bogotá, Colombia
Juan Carlos Garzón
You can also search for this author in PubMed Google Scholar
Contributions
JSM and DKB were responsible for patient care, obtaining images, and reviewing the case literature. The JCG was the attending surgeon in the patient's care and provided the surgical descriptions and images. JPE designed the case report and led the manuscript development along with JSM and DKB. All the authors have read and approved the final manuscript.
Corresponding author
Correspondence to Juan Estrada-Maya .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent for case publication was obtained following the outlined procedure.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Estrada-Maya, J., Montejo, J.S., Báez López, K.D. et al. Doege-Potter syndrome due to a solitary fibrous tumor of the pleura: a case report. J Med Case Reports 18 , 383 (2024). https://doi.org/10.1186/s13256-024-04658-1
Download citation
Received : 23 February 2024
Accepted : 02 May 2024
Published : 14 August 2024
DOI : https://doi.org/10.1186/s13256-024-04658-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Solitary fibrous tumor
- Hypoglycemia
- Insulin-like growth factor II
- Doege-Potter syndrome
- Paraneoplastic syndrome
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
What happened in the Kolkata rape case that triggered doctors’ protests?
Activists and doctors in India demand better safeguarding of women and medical professionals after a trainee medic was raped and murdered in Kolkata.

Activists and doctors across India continued to protest on Wednesday to demand justice for a female doctor, who was raped and murdered while on duty in a hospital in the eastern city of Kolkata.
Feminist groups rallied on the streets in protests titled “Reclaim the Night” in Kolkata overnight on Wednesday – on the eve of India’s independence day – in solidarity with the victim, demanding the principal of RG Kar Medical College resign. Some feminist protesters also marched well beyond Kolkata, including in the capital Delhi.
Keep reading
Doctors across india protest rape and murder of medic in kolkata, india supreme court to monitor investigations into manipur sexual violence, goals not guns: how a girls football team in india’s manipur beats violence, four arrested after spanish blogger on india motorcycle tour gangraped.
While the protests were largely peaceful, a small mob of men stormed the medical college and vandalised property. This group was dispersed by the police.
This comes after two days of nationwide protests by doctors following the incident at RG Kar Medical College in West Bengal’s capital city. “Sit-in demonstrations and agitation in the hospital campus will continue,” one of the protesting doctors, identified as Dr Mridul, told Al Jazeera.
Services in some medical centres were halted indefinitely, and marches and vigils shed light on issues of sexual violence, as well as doctors’ safety in the world’s most populous nation.
What happened to the doctor in Kolkata?
A 31-year-old trainee doctor’s dead body, bearing multiple injuries, was found on August 9 in a government teaching hospital in Kolkata.
The parents of the victim were initially told “by hospital authorities that their daughter had committed suicide,” lawyer and women’s rights activist Vrinda Grover told Al Jazeera. But an autopsy confirmed that the victim was raped and killed.
Grover has appeared for victims in sexual violence cases in India in the past, including Bilkis Bano , a Muslim woman who was gang-raped during the 2002 Gujarat riots, and Soni Sori, a tribal activist based in Chhattisgarh state.
Thousands of doctors marched in Kolkata on Monday, demanding better security measures and justice for the victim.
On Tuesday, the Kolkata High Court transferred the case to the Central Bureau of Investigation (CBI).
The Federation of Resident Doctors Association (FORDA) called for a nationwide halting of elective services in hospitals starting on Monday. Elective services are medical treatments that can be deferred or are not deemed medically necessary.

On Tuesday, FORDA announced on its X account that it is calling off the strike after Health Minister Jagat Prakash Nadda accepted protest demands.
One of these demands was solidifying the Central Protection Act, intended to be a central law to protect medical professionals from violence, which was proposed in the parliament’s lower house in 2022, but has not yet been enacted.
FORDA said that the ministry would begin working on the Act within 15 days of the news release, and that a written statement from the ministry was expected to be released soon.
Press release regarding call off of strike. In our fight for the sad incident at R G Kar, the demands raised by us have been met in full by the @OfficeofJPNadda , with concrete steps in place, and not just verbal assurances. Central Healthcare Protection Act ratification… pic.twitter.com/OXdSZgM1Jc — FORDA INDIA (@FordaIndia) August 13, 2024
Why are some Indian doctors continuing to protest?
However, other doctors’ federations and hospitals have said they will not back down on the strike until a concrete solution is found, including a central law to curb attacks on doctors.
Those continuing to strike included the Federation of All India Medical Associations (FAIMA), Delhi-based All India Institute Of Medical Sciences (AIIMS) and Indira Gandhi Hospital, local media reported.
Ragunandan Dixit, the general secretary of the AIIMS Resident Doctors’ Association, said that the indefinite strike will continue until their demands are met, including a written guarantee of the implementation of the Central Protection Act.
Medical professionals in India want a central law that makes violence against doctors a non-bailable, punishable offence, in hopes that it deters such violent crimes against doctors in the future.
Those continuing to protest also call for the dismissal of the principal of the college, who was transferred. “We’re demanding his termination, not just transfer,” Dr Abdul Waqim Khan, a protesting doctor told ANI news agency. “We’re also demanding a death penalty for the criminal,” he added.
“Calling off the strike now would mean that female resident doctors might never receive justice,” Dr Dhruv Chauhan, member of the National Council of the Indian Medical Association’s Junior Doctors’ Network told local news agency Press Trust of India (PTI).
Which states in India saw doctors’ protests?
While the protests started in West Bengal’s Kolkata on Monday, they spread across the country on Tuesday.
The capital New Delhi, union territory Chandigarh, Uttar Pradesh capital Lucknow and city Prayagraj, Bihar capital Patna and southern state Goa also saw doctors’ protests.

Who is the suspect in the Kolkata rape case?
Local media reported that the police arrested suspect Sanjoy Roy, a civic volunteer who would visit the hospital often. He has unrestricted access to the ward and the police found compelling evidence against him.
The parents of the victim told the court that they suspect that it was a case of gang rape, local media reported.
Why is sexual violence on the rise in India?
Sexual violence is rampant in India, where 90 rapes were reported on average every day in 2022.
Laws against sexual violence were made stricter following a rape case in 2012, when a 22-year-old physiotherapy intern was brutally gang-raped and murdered on a bus in Delhi. Four men were hanged for the gang rape, which had triggered a nationwide protests.
But despite new laws in place, “the graph of sexual violence in India continues to spiral unabated,” said Grover.
She added that in her experience at most workplaces, scant attention is paid to diligent and rigorous enforcement of the laws.
“It is regrettable that government and institutions respond only after the woman has already suffered sexual assault and often succumbed to death in the incident,” she added, saying preventive measures are not taken.
In many rape cases in India, perpetrators have not been held accountable. In 2002, Bano was raped by 11 men, who were sentenced to life imprisonment. In 2022, the government of Prime Minister Narendra Modi authorised the release of the men, who were greeted with applause and garlands upon their release.
However, their remission was overruled and the Supreme Court sent the rapists back to jail after public outcry.
Grover believes that the death penalty will not deter rapists until India addresses the deeply entrenched problem of sexual violence. “For any change, India as a society will have to confront and challenge, patriarchy, discrimination and inequality that is embedded in our homes, families, cultural practices, social norms and religious traditions”.
What makes this case particularly prominent is that it happened in Kolkata, Sandip Roy, a freelance contributor to NPR, told Al Jazeera. “Kolkata actually prided itself for a long time on being really low in the case of violence against women and being relatively safe for women.”
A National Crime Records Bureau (NCRB) report said that Kolkata had the lowest number of rape cases in 2021 among 19 metropolitan cities, with 11 cases in the whole year. In comparison, New Delhi was reported to have recorded 1, 226 cases that year.
Prime Minister Modi’s governing Bharatiya Janata Party (BJP) has called for dismissing the government in West Bengal, where Kolkata is located, led by Mamata Banerjee of All India Trinamool Congress (AITC). Banerjee’s party is part of the opposition alliance.
Rahul Gandhi, the leader of the opposition in parliament, also called for justice for the victim.
“The attempt to save the accused instead of providing justice to the victim raises serious questions on the hospital and the local administration,” he posted on X on Wednesday.
Roy spoke about the politicisation of the case since an opposition party governs West Bengal. “The local government’s opposition will try to make this an issue of women’s safety in the state,” he said.

Have doctors in India protested before?
Roy explained to Al Jazeera that this case is an overlap of two kinds of violence, the violence against a woman, as well as violence against “an overworked medical professional”.
Doctors in India do not have sufficient workplace security, and attacks on doctors have started protests in India before.
In 2019, two junior doctors were physically assaulted in Kolkata’s Nil Ratan Sircar Medical College and Hospital (NRSMCH) by a mob of people after a 75-year-old patient passed away in the hospital.
Those attacks set off doctors’ protests in Kolkata, and senior doctors in West Bengal offered to resign from their positions to express solidarity with the junior doctors who were attacked.
More than 75 percent of Indian doctors have faced some form of violence, according to a survey by the Indian Medical Association in 2015.
What happens next?
The case will now be handled by the CBI, which sent a team to the hospital premises to inspect the crime scene on Wednesday morning, local media reported.
According to Indian law, the investigation into a case of rape or gang rape is to be completed within two months from the date of lodging of the First Information Report (police complaint), according to Grover, the lawyer.
The highest court in West Bengal, which transferred the case from the local police to the CBI on Tuesday, has directed the central investigating agency to file periodic status reports regarding the progress of the investigation.
The FIR was filed on August 9, which means the investigation is expected to be completed by October 9.
Bengal women will create history with a night long protest in various major locations in the state for at 11.55pm on 14th of August’24,the night that’ll mark our 78th year as an independent country. The campaign, 'Women, Reclaim the Night: The Night is Ours', is aimed at seeking… pic.twitter.com/Si9fd6YGNb — purpleready (@epicnephrin_e) August 13, 2024
News from Brown
Brain-computer interface allows man with als to ‘speak’ again.
In a clinical trial and study supported by Brown scientists and alumni, a participant regained nearly fluent speech using a brain-computer interface that translates brain signals into speech with up to 97% accuracy.
The new BCI system allowed Casey Harrell, a 45-year-old person with ALS, to communicate his intended speech effectively within minutes of activation. Photo provided by University of California Regents
PROVIDENCE, R.I. [Brown University] — Scientists with the BrainGate research consortium have developed a brain-computer interface that translates brain signals into speech with up to 97% accuracy, offering a significant breakthrough for individuals with speech impairments due to conditions like amyotrophic lateral sclerosis.
The technology involves using implanted sensors in the brain to interpret brain signals when a user attempts to speak. These signals are then converted into text, which is read aloud by a computer.
The work is described in a new study in the New England Journal of Medicine published on Wednesday, Aug. 14, that was led by neurosurgeon David Brandman and neuroscientist Sergey Stavisky, both of whom are Brown University alumni and faculty members at UC Davis Health.
“Our BCI technology helped a man with paralysis to communicate with friends, families and caregivers,” Brandman said. “Our paper demonstrates the most accurate speech neuroprosthesis ever reported.”
ALS, also known as Lou Gehrig's disease, affects nerve cells controlling muscle movement, leading to the gradual loss of mobility and speech. BCI technology aims to restore communication for those who have lost the ability to speak due to paralysis or neurological disorders.
The system allowed Casey Harrell, a 45-year-old person with ALS, to communicate his intended speech effectively within minutes of activation. The powerful moment brought tears to Harrell and his family. Harrell, reflecting on his experience with the technology, described the impact that regaining the ability to communicate could have on others facing similar challenges.
“Not being able to communicate is so frustrating and demoralizing. It is like you are trapped,” Harrell said. “Something like this technology will help people back into life and society.”
The first time Harrell tried the system, he cried with joy as the words he was trying to say correctly appeared on-screen. Photo provided by University of California Regents
The study is part of the BrainGate clinical trial, directed by Dr. Leigh Hochberg, a critical care neurologist and a professor at Brown University’s School of Engineering who is affiliated with the University’s Carney Institute for Brain Science .
“Casey and our other BrainGate participants are truly extraordinary,” Hochberg said. “They deserve tremendous credit for joining these early clinical trials. They do this not because they’re hoping to gain any personal benefit, but to help us develop a system that will restore communication and mobility for other people with paralysis.”
It is the latest in a series of advances in brain-computer interfaces made by the BrainGate consortium, which along with other work using BCIs has been developing systems for several years that enable people to generate text by decoding the user’s intent. Last year, the consortium described how a brain-computer interface they developed enabled a clinical trial participant who lost the ability to speak to create text on a computer at rates that approach the speed of regular speech, just by thinking of saying the words.
“The field of brain computer interface has come remarkably far in both precision and speed,” said John Ngai, director of the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies ® Initiative (The BRAIN Initiative®) , which funded earlier phases of the BrainGate consortium. “This latest development brings technology closer to helping people, ‘locked in’ by paralysis, regain their ability to communicate with friends and loved ones, and enjoy the best quality of life possible.”
In July 2023, the team at UC Davis Health implanted the BCI device, consisting of four microelectrode arrays, into Harrell’s left precentral gyrus, a brain region responsible for coordinating speech. These arrays record brain activity from 256 cortical electrodes and detect their attempt to move their muscles and talk.
“We are recording from the part of the brain that’s trying to send these commands to the muscles,” Stavisky said. “We are basically listening into that, and we’re translating those patterns of brain activity into a phoneme — like a syllable or the unit of speech — and then the words they’re trying to say.”
BCI allows man to 'speak’
A new brain-computer interface translates brain signals into speech with up to 97% accuracy — the most accurate system of its kind.
The study reports on 84 data collection sessions over 32 weeks. In total, Harrell used the speech BCI in self-paced conversations for over 248 hours to communicate in person and over video chat. The system showed decoded words on a screen and read them aloud in a voice synthesized from Harrell’s pre-ALS voice samples.
In the first session, the system achieved 99.6% word accuracy with a 50-word vocabulary in just 30 minutes. In another session with a vocabulary expanded to 125,000 words, the system achieved 90.2% accuracy after an additional 1.4 hours of training data. After continued data collection, the BCI has maintained 97.5% accuracy.
“At this point, we can decode what Casey is trying to say correctly about 97% of the time, which is better than many commercially available smartphone applications that try to interpret a person’s voice,” Brandman said. “This technology is transformative because it provides hope for people who want to speak but can’t.”
The research included funding from the National Institutes of Health.
This story was adapted from a news release published by Nadine Yehya at UC Davis Health.
CAUTION: Investigational device. Limited by federal law to investigational use.
Related news:
Rhode island high schoolers embrace stem lessons at icerm’s girls get math program, new study unveils 16,000 years of climate history in the tropical andes, isabel tribe: examining ancient sediment to predict earth’s future.
- Introduction
- Conclusions
- Article Information
eFigure. Cardiac magnetic resonance image for a patient with myocarditis.
- JAMA Network Journals’ Articles of the Year 2021 JAMA Medical News & Perspectives December 28, 2021 This Medical News article is our fifth-annual roundup of the top-viewed articles from each of the JAMA Network Journals. Jennifer Abbasi
- Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021 JAMA Original Investigation January 25, 2022 This descriptive study compares the effect of mRNA-based COVID-19 vaccination with BNT162b2 (Pfizer-BioNTech) vs mRNA-1273 (Moderna) on the reported cases of myocarditis in the US after each vaccination dose. Matthew E. Oster, MD, MPH; David K. Shay, MD, MPH; John R. Su, MD, PhD, MPH; Julianne Gee, MPH; C. Buddy Creech, MD, MPH; Karen R. Broder, MD; Kathryn Edwards, MD; Jonathan H. Soslow, MD, MSCI; Jeffrey M. Dendy, MD; Elizabeth Schlaudecker, MD, MPH; Sean M. Lang, MD; Elizabeth D. Barnett, MD; Frederick L. Ruberg, MD; Michael J. Smith, MD, MSCE; M. Jay Campbell, MD, MHA; Renato D. Lopes, MD, PhD, MHS; Laurence S. Sperling, MD; Jane A. Baumblatt, MD; Deborah L. Thompson, MD, MSPH; Paige L. Marquez, MSPH; Penelope Strid, MPH; Jared Woo, MPH; River Pugsley, PhD, MPH; Sarah Reagan-Steiner, MD, MPH; Frank DeStefano, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA
- Myocarditis Following a Third BNT162b2 Vaccination Dose in Military Recruits in Israel JAMA Research Letter April 26, 2022 This study assessed whether a third vaccine dose was associated with the risk of myocarditis among military personnel in Israel. Limor Friedensohn, MD; Dan Levin, MD; Maggie Fadlon-Derai, MHA; Liron Gershovitz, MD; Noam Fink, MD; Elon Glassberg, MD; Barak Gordon, MD
- JAMA Network Articles of the Year 2022 JAMA Medical News & Perspectives December 27, 2022 This Medical News article is our annual roundup of the top-viewed articles from all JAMA Network journals. Melissa Suran, PhD, MSJ
- Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination JAMA Cardiology Brief Report October 1, 2021 This study describes 4 patients who presented with acute myocarditis after mRNA COVID-19 vaccination. Han W. Kim, MD; Elizabeth R. Jenista, PhD; David C. Wendell, PhD; Clerio F. Azevedo, MD; Michael J. Campbell, MD; Stephen N. Darty, BS; Michele A. Parker, MS; Raymond J. Kim, MD
- Temporal Associations Between Immunization With the COVID-19 mRNA Vaccines and Myocarditis JAMA Cardiology Editorial October 1, 2021 Ann Marie Navar, MD, PhD; Elizabeth McNally, MD, PhD; Clyde W. Yancy, MD, MSc; Patrick T. O’Gara, MD; Robert O. Bonow, MD, MS
- Myocarditis Occurring After Immunization With mRNA-Based COVID-19 Vaccines JAMA Cardiology Editorial October 1, 2021 David K. Shay, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA; Frank DeStefano, MD, MPH
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Montgomery J , Ryan M , Engler R, et al. Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol. 2021;6(10):1202–1206. doi:10.1001/jamacardio.2021.2833
Manage citations:
© 2024
- Permissions
Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military
- 1 Immunization Healthcare Division, Defense Health Agency, Falls Church, Virginia
- 2 Walter Reed National Military Medical Center, Bethesda, Maryland
- 3 Naval Medical Center, San Diego, California
- 4 Uniformed Services University of the Health Sciences, Bethesda, Maryland
- 5 Womack Army Medical Center, Fort Bragg, North Carolina
- 6 Wilford Hall Ambulatory Surgical Center, Lackland Air Force Base, San Antonio, Texas
- 7 Naval Hospital Bremerton, Bremerton, Washington
- 8 Marine Expeditionary Forces, Okinawa, Japan
- 9 Mayo Clinic, Jacksonville, Florida
- Editorial Temporal Associations Between Immunization With the COVID-19 mRNA Vaccines and Myocarditis Ann Marie Navar, MD, PhD; Elizabeth McNally, MD, PhD; Clyde W. Yancy, MD, MSc; Patrick T. O’Gara, MD; Robert O. Bonow, MD, MS JAMA Cardiology
- Editorial Myocarditis Occurring After Immunization With mRNA-Based COVID-19 Vaccines David K. Shay, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA; Frank DeStefano, MD, MPH JAMA Cardiology
- Medical News & Perspectives JAMA Network Journals’ Articles of the Year 2021 Jennifer Abbasi JAMA
- Original Investigation Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021 Matthew E. Oster, MD, MPH; David K. Shay, MD, MPH; John R. Su, MD, PhD, MPH; Julianne Gee, MPH; C. Buddy Creech, MD, MPH; Karen R. Broder, MD; Kathryn Edwards, MD; Jonathan H. Soslow, MD, MSCI; Jeffrey M. Dendy, MD; Elizabeth Schlaudecker, MD, MPH; Sean M. Lang, MD; Elizabeth D. Barnett, MD; Frederick L. Ruberg, MD; Michael J. Smith, MD, MSCE; M. Jay Campbell, MD, MHA; Renato D. Lopes, MD, PhD, MHS; Laurence S. Sperling, MD; Jane A. Baumblatt, MD; Deborah L. Thompson, MD, MSPH; Paige L. Marquez, MSPH; Penelope Strid, MPH; Jared Woo, MPH; River Pugsley, PhD, MPH; Sarah Reagan-Steiner, MD, MPH; Frank DeStefano, MD, MPH; Tom T. Shimabukuro, MD, MPH, MBA JAMA
- Research Letter Myocarditis Following a Third BNT162b2 Vaccination Dose in Military Recruits in Israel Limor Friedensohn, MD; Dan Levin, MD; Maggie Fadlon-Derai, MHA; Liron Gershovitz, MD; Noam Fink, MD; Elon Glassberg, MD; Barak Gordon, MD JAMA
- Medical News & Perspectives JAMA Network Articles of the Year 2022 Melissa Suran, PhD, MSJ JAMA
- Brief Report Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination Han W. Kim, MD; Elizabeth R. Jenista, PhD; David C. Wendell, PhD; Clerio F. Azevedo, MD; Michael J. Campbell, MD; Stephen N. Darty, BS; Michele A. Parker, MS; Raymond J. Kim, MD JAMA Cardiology
Question Should myocarditis be considered a potential adverse event following immunization with messenger RNA (mRNA) COVID-19 vaccines?
Findings In this case series of 23 male patients, including 22 previously healthy military members, myocarditis was identified within 4 days of receipt of a COVID-19 vaccine. For most patients (n = 20), the diagnosis was made after the second dose of mRNA COVID-19 vaccine; these episodes occurred against the backdrop of 2.8 million doses of mRNA COVID-19 vaccines administered.
Meaning Vigilance for rare adverse events, including myocarditis, after COVID-19 vaccination is warranted but should not diminish overall confidence in vaccination during the current pandemic.
Importance Myocarditis has been reported with COVID-19 but is not clearly recognized as a possible adverse event following COVID-19 vaccination.
Objective To describe myocarditis presenting after COVID-19 vaccination within the Military Health System.
Design, Setting, and Participants This retrospective case series studied patients within the US Military Health System who experienced myocarditis after COVID-19 vaccination between January and April 2021. Patients who sought care for chest pain following COVID-19 vaccination and were subsequently diagnosed with clinical myocarditis were included.
Exposure Receipt of a messenger RNA (mRNA) COVID-19 vaccine between January 1 and April 30, 2021.
Main Outcomes and Measures Clinical diagnosis of myocarditis after COVID-19 vaccination in the absence of other identified causes.
Results A total of 23 male patients (22 currently serving in the military and 1 retiree; median [range] age, 25 [20-51] years) presented with acute onset of marked chest pain within 4 days after receipt of an mRNA COVID-19 vaccine. All military members were previously healthy with a high level of fitness. Seven received the BNT162b2-mRNA vaccine and 16 received the mRNA-1273 vaccine. A total of 20 patients had symptom onset following the second dose of an appropriately spaced 2-dose series. All patients had significantly elevated cardiac troponin levels. Among 8 patients who underwent cardiac magnetic resonance imaging within the acute phase of illness, all had findings consistent with the clinical diagnosis of myocarditis. Additional testing did not identify other etiologies for myocarditis, including acute COVID-19 and other infections, ischemic injury, or underlying autoimmune conditions. All patients received brief supportive care and were recovered or recovering at the time of this report. The military administered more than 2.8 million doses of mRNA COVID-19 vaccine in this period. While the observed number of myocarditis cases was small, the number was higher than expected among male military members after a second vaccine dose.
Conclusions and Relevance In this case series, myocarditis occurred in previously healthy military patients with similar clinical presentations following receipt of an mRNA COVID-19 vaccine. Further surveillance and evaluation of this adverse event following immunization is warranted. Potential for rare vaccine-related adverse events must be considered in the context of the well-established risk of morbidity, including cardiac injury, following COVID-19 infection.
Myocarditis is a heterogeneous disease with diverse clinical patterns, etiologies, and therapeutic responses, reflecting inflammatory injury to myocardial tissue in the absence of ischemia. 1 While viral infections, now including SARS-CoV-2, are the most common triggers of the disease, some myocarditis cases are associated with certain drugs and vaccine exposures. 1 With the exception of cases following live-attenuated smallpox vaccine in the military population, 2 myocarditis as an adverse event following immunization is described in rare published case reports and infrequent submissions to the Vaccine Adverse Events Reporting System (VAERS). 3 , 4
Serious adverse events associated with receipt of new vaccines targeting COVID-19 are of high interest to the public and to public health vaccine safety surveillance. We describe a series of 23 individuals who developed probable hypersensitivity myocarditis in temporal association with COVID-19 messenger RNA (mRNA) vaccination.
The US military initiated COVID-19 vaccination following US Centers for Disease Control and Prevention (CDC)–defined phased distribution in December 2020. Adverse events following immunizations were identified from referrals to Defense Health Agency clinical specialists and through review of VAERS reports. Retrospective review of cases was conducted in accordance with the Walter Reed National Military Medical Center Institutional Review Board–approved protocol, “Adverse Events Following Immunization: Case Definitions and Outcomes Retrospective Review,” and exempt from formal consent procedures.
A total of 23 male patients (22 currently serving in the military and 1 retiree; median [range] age, 25 [20-51] years) were evaluated between January and April 2021 for acute-onset chest pain following mRNA COVID-19 vaccination. Care was provided in 15 distinct geographic locations globally with varying diagnostic evaluations. Each patient had a final diagnosis of myocarditis without infectious, ischemic, or autoimmune etiologies identified. Diagnoses were reviewed by an adjudication process and met the CDC case definition criteria for probable myocarditis ( Table 1 ). A total of 8 patients had cardiac magnetic resonance imaging (cMRI) with T2 weighting showing subepicardial late gadolinium enhancement and/or focal myocardial edema, consistent with Lake Louise criteria for myocarditis. 1 The eFigure in the Supplement exemplifies cMRI findings for one of these patients.
The demographic and clinical characteristics of patients are summarized in Table 2 . All military service members were physically fit by military standards and lacking any known history of cardiac disease, significant cardiac risk factors, or exposure to cardiotoxic agents. All patients presented with acute chest pain and significantly elevated cardiac troponin levels (10-fold to 400-fold the upper limits of their respective reference ranges). Their symptoms began within 12 to 96 hours following immunization with an mRNA COVID-19 vaccine. Sixteen had received the mRNA-1273 vaccine (Moderna), and 7 had received the BNT162b2-mRNA vaccine (Pfizer-BioNTech). For all but 3 patients, the second dose of vaccine preceded their myocarditis presentations. Among the 3 patients presenting after an initial vaccine dose, all had confirmed COVID-19 infection more than 2 months prior to vaccination.
All patients underwent electrocardiography and echocardiography ( Table 2 ). Abnormal electrocardiography findings were recorded in 19 patients (83%); findings included ST-segment elevations, T-wave inversions, and nonspecific ST changes. Echocardiography in 4 patients (17%) demonstrated reduced left ventricular ejection fractions (40% to 50%). No structural abnormalities were noted on any echocardiograms. A total of 16 patients underwent coronary artery imaging (11 had cardiac catheterization and 5 had coronary computed tomography angiography); none showed evidence of coronary artery disease.
Nineteen patients had respiratory specimens tested for SARS-CoV-2 by polymerase chain reaction at the time of presentation; none had evidence of acute SARS-CoV-2 infection. There were no positive findings among 13 patients who were tested for other infections, nor among 9 patients who were tested for autoimmune diseases.
Cardiac symptoms resolved within 1 week of onset for 16 patients. Seven patients continued to have chest discomfort at the time of this report; follow-up is ongoing.
The number of doses of mRNA COVID-19 vaccine administered by the Military Health System through April 30, 2021, is shown in Table 3 . Overall, 2 810 000 doses were administered; 1 065 000 second doses were administered; 544 000 second doses were administered to military service members; and 436 000 second doses were administered to male military service members. The expected number of myocarditis cases occurring in a 30-day period after vaccination may be estimated using an international incidence of 22 cases per 100 000 person-years 5 or a US incidence of 1 to 10 cases per 100 000 person-years. 6 Observed numbers of myocarditis in the Military Health System were higher than some estimates of expected numbers, especially when considering the subset of the population who were military service members who received second doses of an mRNA COVID-19 vaccine ( Table 3 ).
In this case series, we describe 23 patients with clinical evidence of myocarditis following mRNA COVID-19 vaccination and meeting the CDC case definition for probable myocarditis. Eight patients had cMRI findings consistent with myocarditis. All patients in this series reflect substantial similarities in demographic characteristics, proximate vaccine dose, onset interval, and character of vaccine-associated myocarditis. The consistent pattern of clinical presentation, rapid recovery, and absence of evidence of other causes support the diagnosis of hypersensitivity myocarditis. Without myocardial biopsy, histology cannot be defined, but the clinical course suggests eosinophilic hypersensitivity myocarditis as described in the context of other drug-associated and vaccine-associated myocarditis. 1 - 3 Presentation after second vaccine dose or, in 3 patients, when vaccination followed SARS-CoV-2 infection, suggests that prior exposure was relevant in the hypersensitivity response.
With the exception of the smallpox vaccine, immunizations are rarely associated with hypersensitivity myocarditis. The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition. 7 In contrast to passive case finding, Engler et al 2 reported a significantly higher incidence of myocarditis and pericarditis after smallpox vaccination through active prospective follow-up of vaccinated participants. They noted that 60% of these patients would not have sought medical care for symptoms outside of the study protocol. 2 Recognition of vaccine-associated myocarditis is clinically important since diagnosis impacts management, recommendations for exercise, and monitoring for cardiomyopathy. 8
Notably, myocarditis cases were not reported following vaccination in clinical trials of current COVID-19 vaccines. 9 , 10 Adverse cardiac events of any kind were reported in less than 0.1% of trial participants, and rates were not higher in recipients of vaccine compared with placebo. The inability to identify rare adverse events is understandable in preauthorization testing since fewer than 20 000 participants received a vaccine in each trial.
Background rates of myocarditis in the general population are variable and may be challenging to determine. As noted, a global estimate of incidence is 22 cases per 100 000 person-years. 5 More recent estimates of US incidence are lower (1 to 10 cases per 100 000 person-years) and may be more appropriate for estimating expected rates of diagnoses in evaluations of immunization safety. 6 Applying both the US and global background incidence to the population vaccinated by the US military yields a range of expected numbers of cases of myocarditis in this period ( Table 3 ). The observed number of male military members who experienced myocarditis after their second dose of mRNA vaccine, while relatively small, is substantially higher than the expected number.
Finally, it is important to frame concerns about potential vaccine-associated myocarditis within the context of the current pandemic. Infection with SARS-CoV-2 is a clear cause of serious cardiac injury in many patients. 11 The mechanism of injury may be direct infection, an immune-mediated response, or a combination of direct or indirect effects. Prevalence of cardiac injury may be as high as 60% in seriously ill patients. Notably, nearly 1% of highly fit athletes with mild COVID-19 infection have evidence of myocarditis on cMRI. 12 , 13 Given that COVID-19 vaccines are remarkably effective at preventing infection, any risk of rare adverse events following immunization must be carefully weighed against the very substantial benefit of vaccination.
Important limitations to this case series should be considered. Passive surveillance, even when stimulated by global attention on vaccine safety, may not identify all cases. The patients described in this report were identified in a brief period of observation after vaccine implementation from a cohort of essential workers who are not necessarily representative of the general population. Clinical evaluations varied and did not include complete testing in some patients who received care in different hospitals and in different countries. In particular, consistent application of cMRI and thorough viral testing would have strengthened clinical conclusions. This early report is also unable to describe longer-term outcomes among these patients. Despite limitations of this review, it is notable that the clinical presentations of these 23 patients appear consistent with other recent case reports of myocarditis after second doses of mRNA COVID-19 vaccines. 14 , 15
We report a case series of probable hypersensitivity myocarditis with consistent temporal association to receipt of an mRNA COVID-19 vaccine. While the true incidence of this adverse event is unknown at this time, the presentation pattern and clinical course suggest an association with an inflammatory response to vaccination. Increased attention to myocarditis as a potential adverse event following immunization is warranted. Recognition of the substantial morbidity associated with COVID-19 infection, including risk of cardiac injury, and the strong effectiveness of immunization in preventing infection provide important context for this topic. Concerns about rare adverse events following immunization should not diminish overall confidence in the value of vaccination.
Accepted for Publication: June 1, 2021.
Published Online: June 29, 2021. doi:10.1001/jamacardio.2021.2833
Corresponding Author: Jay Montgomery, MD, Walter Reed National Military Medical Center, 4954 N Palmer Rd, Bldg 19, Room 4026, Bethesda, MD 20889 ( [email protected] ); Margaret Ryan, MD, MPH, Naval Medical Center San Diego, 34800 Bob Wilson Dr, Bldg 6, Room 4V7C1, San Diego, CA 92134 ( [email protected] ).
Author Contributions: Drs Montgomery and Ryan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design : Montgomery, Ryan, McClenathan, Collins, Hrncir, Herring.
Acquisition, analysis, or interpretation of data : Montgomery, Ryan, Engler, Hoffman, McClenathan, Loran, Hrncir, Herring, Platzer, Adams, Sanou, Cooper.
Drafting of the manuscript : Montgomery, Ryan, Engler, Cooper.
Critical revision of the manuscript for important intellectual content : All authors.
Statistical analysis : Ryan, McClenathan.
Administrative, technical, or material support : Montgomery, Ryan, Engler, Hoffman, McClenathan, Collins, Loran, Hrncir, Herring, Platzer, Adams, Sanou.
Study supervision : Montgomery, Ryan, Cooper.
Conflict of Interest Disclosures: Dr Cooper has received personal fees from Bristol Myers Squibb, Cantargia, CardioPath, Kiniksa Pharmaceuticals, and Cardiol Therapeutics. No other disclosures were reported.
Disclaimer: The views expressed are those of the authors and do not necessarily reflect official policy of the Department of Defense or the US government.
Additional Contributions: We thank the eldest patient for granting permission to publish identifiable information. We appreciate the contributions of the many clinicians who provided care or consultation for these patients worldwide, including, but not limited to, Todd Looney, MD; Matthew Needleman, MD; J. Edwin Atwood, MD; Carlie Cerne, MD; P. Gabriel Peterson, MD; Benjamin St. Clair, MD; and Nathan Boggs, MD (Walter Reed National Military Medical Center, Bethesda, Maryland); and Michael Romero, HM1, USN. We appreciate the support of Col Tonya Rans, USAF, MC; Laurie Duran, MSN; Laurie Housel, MSN; Ann Morse, MSN; Catherine Skerrett, MSN (Immunization Healthcare Division, Defense Health Agency, Falls Church, Virginia); and the Clinical Immunization Safety Assessment professionals at the US Centers for Disease Control and Prevention.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 9, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Study finds baked potatoes can improve heart health for diabetics
by Steven Slivka, University of Nevada, Las Vegas

The potato is small enough to fit inside a person's hand yet contains enough nutrients to whittle waistlines and lower blood sugar in adults with type 2 diabetes. Yet, despite the fact that potatoes—particularly the skins—are packed with health-boosting nutrients, they routinely get a bad rap among dieters.
That may soon change, thanks to new research by Neda Akhavan, assistant professor in the Department of Kinesiology and Nutrition Sciences within UNLV's School of Integrated Health Sciences. Akhavan recently presented her findings on the cardiovascular benefits of potatoes for those living with Type 2 diabetes to the Alliance for Potato Research and Education.
"I like doing research on food items that are highly stigmatized in the nutrition world," she said. "Most people associate the potato as something that is mostly fried or has a lot of fat, and we wanted to shine a light on how a potato—when prepared properly—can be both functional and healthy."
Putting potatoes to the test
Akhavan enlisted 24 participants for the study , all of whom had Type 2 diabetes that was well controlled with medication. This is believed to be the first study of its kind to scientifically measure the cardiovascular benefits of potatoes for adults with diabetes.
Participants in the study group were each given a pre-prepared baked potato with the skin measured to 100g, with only 20 grams of carbohydrates, roughly enough to fit in one hand to incorporate as a snack or side with meals daily. The control group was given a similar potion of white rice with the same number of calories and carbohydrates. The study ran daily for 12 weeks, which is considered the minimum time needed to see changes in indices of glycemic control and cardiometabolic health.
Study participants were permitted to add herbs or spices to the potatoes, or up to ½ tbsp of butter, but they were advised not to fry their potato.
Key takeaways and recommendations
A modest decrease in fasting blood glucose levels was present for study participants who ate potatoes. Study participants also showed improvements in body composition, waist circumference, and a decrease in resting heart rate.
"The results from our study provide evidence that white potatoes can be healthfully incorporated in the diet of individuals with Type 2 diabetes when substituted for other foods with a high glycemic load, such as long-grain white rice," Akhavan said.
"Additionally, there were no harmful effects on measured health outcomes , and some cardiometabolic health benefits were shown, which aligned with what we expected to see. Therefore, diabetics should not shy away from potatoes."
Akhavan says that just like all foods, moderation—and preparation methods—are key.
"Potatoes are a very versatile food and can be eaten with most types of cuisines, but you want to make sure to incorporate them into a well-rounded diet," she said.
"For those tight on time, consider making a large batch of baked or roasted potatoes and meal prep to last you a while. I'm not against boiling potatoes, but you want to keep as much of the potassium from the skin as you can, and you lose some of that when you boil them."
Making the case for potatoes
Potatoes are the richest source of dietary potassium in Western diets, and high potassium diets have been shown to prevent high blood pressure and Type 2 diabetes development. Additionally, potato skins contain a certain type of fiber called "resistance starch," which have been shown to improve glucose control, lipid profiles, and satiety. Because of these added health benefits, Akhavan recommends eating potatoes with the skin.
So, the next time you want to reach for a banana, she added, reach for that potato instead.
"A lot of people are shocked to learn that a potato has a higher level of potassium than a banana," she said. "Believe it or not, a baked potato is one of the most satiating foods consumed within the western diet. And, when it is consumed baked, it increases our ability to feel fuller throughout the day."
Akhavan intends to expand the study in the coming months to include a larger and more diverse participant population, and incorporation of potatoes within a Mediterranean dietary pattern. She also plans to explore the role of potato consumption and its effects on dietary patterns and related health benefits.
Explore further
Feedback to editors

Preclinical study shows potential of Manuka honey as a nutraceutical for breast cancer
8 hours ago

Low cortisol and hair-trigger stress response in the brain may underlie long COVID, study finds
9 hours ago

Study finds potential link between DNA markers and aging process

Platelets under control: Protecting the heart and brain more effectively after an infarction
10 hours ago

Study finds constipation is a significant risk factor for major cardiac events
12 hours ago

Study shows macrophages form in eye before birth, offering hope for diabetic retinopathy treatment

Examining Alzheimer's disease drug impact on tissue samples from people with Down syndrome: Study raises safety concerns
13 hours ago

Researchers discover new way to control the sense of touch

Generative AI can not yet reliably read and extract information from clinical notes in medical records, finds study

Circadian rhythms appear to influence vulnerability to malaria parasites
14 hours ago
Related Stories

Defending potatoes
Aug 9, 2024

It's not them, it's you: Why potatoes don't deserve their bad reputation
Dec 5, 2022
Pass the potatoes, or take a pass? Here's expert advice
Nov 22, 2023

Potatoes can be part of a healthy diet
Nov 17, 2022

Sweet potatoes are a holiday dish to be thankful for
Nov 25, 2019

Figuring out how to make the healthiest potato chips on the planet
Jun 19, 2023
Recommended for you

Improving access to heart-failure screening with a low-cost saliva test
21 hours ago

Better transplantations with 'heart-in-a-box': Study finds method reduces early heart failure risk
Aug 16, 2024

Intervention for cleaning shared health care equipment could significantly reduce health care–associated infections

Study unveils impact of cardiovascular risk factors on genetic predisposition to heart disease
Aug 15, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Advertisement
Supported by
How Did Mpox Become a Global Emergency? What’s Next?
The virus is evolving, and the newest version spreads more often through heterosexual populations. Sweden reported the first case outside Africa.
- Share full article

By Apoorva Mandavilli
Apoorva Mandavilli covered the 2022 mpox outbreak and the Covid-19 pandemic.
Faced once again with a rapidly spreading epidemic of mpox, the World Health Organization on Wednesday declared a global health emergency. The last time the W.H.O. made that call was in 2022, when the disease was still called monkeypox.
Ultimately the outbreak affected nearly 100,000 people worldwide, primarily gay and bisexual men, including more than 32,000 in the United States.
The W.H.O.’s decision this time was prompted by an escalating crisis of mpox concentrated in the Democratic Republic of Congo. It recently spread to a dozen other African countries. If it is not contained, the virus again may rampage all over the world, experts warned.
On Thursday, Sweden reported the first case of a deadlier form of mpox outside Africa , in a person who had traveled to the continent. “Occasional imported cases like the current one may continue to occur,” the country’s public health agency warned.
“There’s a need for concerted effort by all stakeholders, not only in Africa, but everywhere else,” Dr. Dimie Ogoina, a Nigerian scientist and chair of the W.H.O.’s mpox emergency committee, said on Wednesday.
Congo alone has reported 15,600 mpox cases and 537 deaths, most of them among children under 15, indicating that the nature of the disease and its mode of spread may have changed.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Watch CBS News
Details emerge after doctor raped and murdered in India as thousands protest
August 15, 2024 / 6:32 AM EDT / CBS/AFP
Thousands took to the streets of Kolkata early Thursday to condemn the rape and murder of a local doctor , demanding justice for the victim and an end to the chronic issue of violence against women in Indian society.
The discovery of the 31-year-old's brutalized body last week at a state-run hospital has sparked nationwide protests, with Prime Minister Narendra Modi demanding swift punishment for those who commit "monstrous" deeds against women.
Large crowds marched through the streets of Kolkata in West Bengal to condemn the killing, with a candlelight rally at midnight coinciding with the start of India's independence day celebrations on Thursday.
The protesters in Kolkata, who marched under the slogan "reclaim the night", called for a wider tackling of violence against women and held up handwritten signs demanding action.
"We want justice," read one sign at the rally. "Hang the rapist, save the women," read another.

"The atrocities against women do not stop," midnight marcher Monalisa Guha told Kolkata's The Telegraph newspaper.
"We face harassment almost on a daily basis," another marcher, Sangeeta Halder, told the daily. "But not stepping out because of fear is not the solution."
"Monstrous behavior against women"
Modi, speaking in New Delhi on Thursday morning at independence day celebrations, did not specifically reference the Kolkata murder, but expressed his "pain" at violence against women.
"There is anger for atrocities committed against our mothers and sisters, there is anger in the nation about that," he said.
"Crimes against women should be quickly investigated; monstrous behavior against women should be severely and quickly punished," he added. "That is essential for creating deterrence and confidence in the society."
Doctors are also demanding swift justice and better workplace security in the wake of the killing, with those in government hospitals across several states on Monday halting elective services "indefinitely" in protest.
Protests have since occurred in several other hospitals across the country, including in the capital.
"Doctors nationwide are questioning what is so difficult about enacting a law for our security," Dhruv Chauhan, from the Indian Medical Association's Junior Doctors' Network, told the Press Trust of India news agency. "The strike will continue until all demands are formally met."
The Telegraph on Thursday praised the "spirited public protests" across India.
"Hearteningly, doctors and medical organizations are not the only ones involved," it said in an editorial. "The ranks of the protesters have been swelled by people from all walks of life."
Police accused of mishandling case
Indian media have reported the murdered doctor was found in the teaching hospital's seminar hall, suggesting she had gone there for a brief rest during a long shift.
An autopsy has confirmed sexual assault, and in a petition to the court, the victim's parents have said that they suspected their daughter was gang-raped, according to Indian broadcaster NDTV.
Though police have detained a man who worked at the hospital helping people navigate busy queues, officers have been accused of mishandling the case.
Kolkata's High Court on Tuesday transferred the case to the elite Central Bureau of Investigation (CBI) to "inspire public confidence."
In the early hours of Thursday, a mob of some 40 people angry at authorities' handling of the case stormed the grounds of the R.G. Kar Medical College and Hospital, the site of the murder.
The men smashed property and hurled stones at police, who fired tear gas in response, authorities said.

West Bengal lawmaker Abhishek Banerjee, from the Trinamool Congress party, condemned the "hooliganism and vandalism," but said "the demands of the protesting doctors are fair and justified."
History of sexual violence in India
Sexual violence against women is a widespread problem in India. An average of nearly 90 rapes a day were reported in India in 2022, according to data from the National Crime Records Bureau.
That year, police arrested 11 people after the alleged brutal gang rape and torture of a young woman that included her being paraded through the streets of Dehli. Also in 2022, a police officer in India was arrested after being accused of raping a 13-year-old girl who went to his station to report she had been gang-raped.
In March 2024, multiple Indian men were arrested after the gang rape of a Spanish tourist on a motorbike trip with her husband.
For many, the gruesome nature of the attack has invoked comparisons with the horrific 2012 gang rape and murder of a young woman on a Delhi bus.
The woman became a symbol of the socially conservative country's failure to tackle sexual violence against women.
Her death sparked huge, and at times violent, demonstrations in Delhi and elsewhere.
Under pressure, the government introduced harsher penalties for rapists, and the death penalty for repeat offenders.
Several new sexual offences were also introduced, including stalking and jail sentences for officials who failed to register rape complaints.
- Sexual Violence
More from CBS News

Alabama's third nitrogen execution set for November

A new generation of protestors takes on the 2024 DNC in Chicago

Suspect identified in 1980 cold case killing of UT nursing student

Harris-Walz ticket sharpens contrast with Trump-Vance on health care
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
News releases.
News Release
Thursday, August 15, 2024
The antiviral tecovirimat is safe but did not improve clade I mpox resolution in Democratic Republic of the Congo
NIH-cosponsored study examined tecovirimat in mpox-endemic country.

The antiviral drug tecovirimat did not reduce the duration of mpox lesions among children and adults with clade I mpox in the Democratic Republic of the Congo (DRC), based on an initial analysis of data from a randomized, placebo-controlled trial. However, the study’s 1.7% overall mortality among enrollees, regardless of whether they received the drug or not, was much lower than the mpox mortality of 3.6% or higher reported among all cases in the DRC. This shows that better outcomes among people with mpox can be achieved when they are hospitalized and provided high-quality supportive care. The trial is sponsored by the National Institutes of Health’s (NIH) National Institute of Allergy and Infectious Diseases (NIAID) and co-led through a government-to-government partnership with the DRC’s Institut National de Recherche Biomédicale (INRB). Further analyses and detailed results will be released through scientific channels.
“These findings are disappointing, but they give us essential information and reinforce the need to identify other therapeutic candidates for mpox while we continue research on tecovirimat use in other populations with mpox,” said NIAID Director Jeanne Marrazzo, M.D., M.P.H. “We remain committed to developing safe and effective interventions, including treatments and vaccines, that can ease the devastating mpox burden in Central Africa and address the milder form of the virus that is circulating globally.”
Mpox has occurred in West, Central and East Africa for decades, with the first human case identified in 1970. Two types of the virus that causes mpox have been identified. Clade I, studied in this trial, is endemic in Central Africa and can cause severe illness. Clade II, endemic in West Africa, tends to result in milder illness. A clade II subtype virus caused a global mpox outbreak in 2022. People with compromised immune systems, children, and people who are pregnant are especially vulnerable to severe mpox regardless of the virus clade.
Reports of clade I mpox are increasing in Central African countries, particularly in the DRC. A recent report from the Centers for Disease Control and Prevention (CDC) indicated that 67% of suspected DRC mpox cases and 78% of suspected mpox deaths have occurred in people aged 15 years and younger. Tecovirimat , also known as TPOXX, was initially developed and approved by the Food and Drug Administration to treat smallpox — a virus closely related to, but far more serious than, mpox—but the drug’s safety and efficacy as an mpox treatment have not been established. It is currently available for mpox treatment in the United States as part of a separate NIAID-sponsored trial called STOMP and through a CDC expanded access Investigational New Drug (EA-IND) request process. Tecovirimat is authorized in Europe and the United Kingdom for the treatment of smallpox, mpox, and other indications.
In October 2022, NIAID and INRB launched the PALM007 trial to examine the safety and efficacy of tecovirimat for mpox treatment in adults and children. The study enrolled 597 people with laboratory-confirmed mpox at two sites in the DRC. Study participants were randomly assigned to receive tecovirimat or placebo and were admitted to a hospital for at least 14 days, where they were monitored closely for safety and resolution of mpox lesions. All participants received supportive care including nutrition, hydration, and treatment for secondary infections.
Tecovirimat was well-tolerated with no drug-related serious adverse events. Overall, mortality was lower, and lesions resolved faster than anticipated regardless of whether participants received tecovirimat or placebo. Study participants are being notified of the initial results and offered the opportunity to participate in an ongoing extension study providing further supportive medical care. Additional analyses are planned to better understand outcomes observed in the study, including whether there were any significant differences in clinical outcomes by days of symptoms prior to enrollment, severity of clinical disease, participant characteristics, or the genetic variant of mpox being treated.
“This study delivered urgently needed evidence to guide the mpox response in Central Africa” said co-principal investigator Jean-Jacques Muyembe-Tamfum, M.D., Ph.D., director-general of INRB and professor of microbiology at Kinshasa University Medical School in Kinshasa, DRC. “Although not what we had hoped for, the results show that study clinicians provided exceptional supportive care to all participants, which is a testament to the knowledge and skill that Congolese clinicians have acquired on managing mpox-related disease.”
“The PALM007 study demonstrated the importance and value of testing investigational mpox treatments through robust clinical trials in the DRC’s endemic setting,” said Lori Dodd, Ph.D., NIAID’s PALM project lead for the DRC. “We’ll continue to evaluate the trial data to determine whether additional studies of tecovirimat in patient subgroups are warranted.
The PALM007 trial is led by co-principal investigators Professor Muyembe-Tamfum and Placide Mbala, M.D., Ph.D., operations manager of the PALM clinical research partnership, and head of the Epidemiology and Global Health Department and the Pathogen Genomic Laboratory at INRB. NIAID’s Veronique Nussenblatt, M.D. and Olivier Tshiani, M.D. of Leidos Biomedical Research were protocol co-chairs. The trial was implemented in Tunda (Maniema province) and Kole (Sankuru province) with support from Congolese staff, the Mitchell Group and the NIH’s Frederick National Laboratory for Cancer Research. Collaborating institutions include the U.S. CDC, the Institute of Tropical Medicine Antwerp (ITM) , the aid organization Alliance for International Medical Action (ALIMA) and the World Health Organization (WHO). The U.S. Embassy in the DRC and DRC-based U.S. CDC staff supported logistics and operations for shipments, travel and regional security. SIGA Technologies, Inc., based in New York, provided tecovirimat for the study.
The “Pamoja Tulinde Maisha” or “PALM” clinical research partnership was established in response to the 2018 Ebola outbreak in DRC. The collaboration has continued as a multilateral clinical research program composed of NIAID, the DRC Ministry of Health, INRB and INRB’s partners.
NIAID and the INRB thank the extraordinary team of individuals who carried out this study in remote regions of the DRC, the members of the independent study Data and Safety Monitoring Board, and most importantly, the study participants and their families. For more information about PALM007, please visit ClinicalTrials.gov using the study identifier NCT05559099 .
“Given the differences in populations affected by the two mpox clades, the types of clinical disease that are appearing and the ongoing spread of both clades, it’s very important that we continue with the STOMP trial and other related studies, so that we can develop treatments that benefit all people with mpox,” said Dr. Marrazzo.
The international STOMP trial is examining the safety and efficacy of tecovirimat against clade II mpox. For more information about the STOMP trial, please visit ClinicalTrials.gov using the study identifier NCT05534984 . An additional study, UNITY, sponsored by ANRS Emerging Infectious Disease, is evaluating tecovirimat with a similar study design to STOMP in Argentina, Brazil and Switzerland. More information about the UNITY study can also be found on ClinicalTrials.gov using the identifier NCT05597735 . Both studies will continue to enroll participants and work in close collaboration.
NIAID conducts and supports research—at NIH, throughout the United States, and worldwide—to study the causes of infectious and immune-mediated diseases, and to develop better means of preventing, diagnosing and treating these illnesses. News releases, fact sheets and other NIAID-related materials are available on the NIAID website .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit www.nih.gov .
NIH…Turning Discovery Into Health ®
Connect with Us
- More Social Media from NIH

IMAGES
COMMENTS
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-1062. Crossref
Journal of Medical Case Reports publishes original case reports and research on case reporting from all medical disciplines. Learn about the journal's aims, scope, editorial policies, submission guidelines, and latest articles on COVID-19 and other topics.
A widely accepted evidence-based treatment approach used in patients with early HER2-positive breast cancer is surgery, followed by adjuvant therapy, for patients with clinical stage T1N0 disease ...
The largest online collection of medical case reports. Validation period: 8/19/2024, 10:43:28 AM - 8/19/2024, 4:43:28 PM. Subscribe Login. Latest content Archive For authors About Help. Email alerts. Search the world's largest collection of clinical case reports ... Every year BMJ Case Reports selects authors of global health case reports to ...
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant ...
Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091-m1091. PubMed
The LITFL Clinical Case Collection includes over 250 Q&A style clinical cases to assist 'Just-in-Time Learning' and 'Life-Long Learning'. Cases are categorized by specialty and can be interrogated by keyword from the Clinical Case searchable database. Search by keywords; disease process; condition; eponym or clinical features….
SAGE Open Medical Case Reports is a peer-reviewed, open access journal, which focusses on providing a publication home for short case reports and case series, which often do not find a place in traditional primary research journals, but provide key insights into real medical cases that are essential for physicians, and may ultimately help to improve patient outcomes.
Editorial. Introduction. Case reports and case series or case study research are descriptive studies to present patients in their natural clinical setting. Case reports, which generally consist of three or fewer patients, are prepared to illustrate features in the practice of medicine and potentially create new research questions that may contribute to the acquisition of additional knowledge ...
Learn how to turn an interesting case or unusual presentation into an educational report with this guide from two doctors. Find out how to get consent, gather information, write up, title, research, and conclude your case report.
Clinical Case Reports is an open access journal aiming to improve global health outcomes by conveying important best practice messages and sharing clinical knowledge with medical case reports, clinical images, and procedural videos. As part of Wiley's Forward Series, this journal offers a streamlined, faster publication experience with a ...
A journal publishing case reports in all medical disciplines, including general medicine, drug interaction and adverse reactions. The largest online collection of medical case reports. Subscribe Login. Latest content Archive For authors About Help. Home / Browse by collection. Email alerts. Browse by collection. Anaesthesia;
Publish with Oxford Medical Case Reports. Oxford Medical Case Reports is an open access, peer-reviewed journal publishing original and educationally valuable case reports that expand the field of medicine. To understand more about why OMCR is a great fit for your research, head to our 'Why Publish With Us?' page here.
Learn the skills and steps to write a case report for medical journals, from choosing the right patient and message to getting published. This article by BMJ Case Reports editors provides guidance and tips for medical students and junior doctors.
While case studies cannot provide specific guidance for the management of successive patients, they are a record of clinical interactions which help us to frame questions for more rigorously designed clinical studies. Case studies also provide valuable teaching material, demonstrating both classical and unusual presentations which may confront ...
Clinical Case Studies (CCS), peer-reviewed & published bi-monthly electronic only, is the only journal devoted entirely to innovative psychotherapy case studies & presents cases involving individual, couples, & family therapy.The easy-to-follow case presentation format allows you to learn how interesting & challenging cases were assessed & conceptualized, & how treatment followed such ...
Dr. Pavan K. Bendapudi: I was involved in the care of this patient and am aware of the diagnosis in this case. The patient presented with skin mottling and a rapidly progressive reticular rash ...
A medical case report, also known as a case study, is a detailed description of a clinical encounter with a patient. The most important aspect of a case report, i.e. the reason you would go to the trouble of writing one, is that the case is sufficiently unique, rare or interesting such that other medical professionals will learn something from it.
The Harvard Chan Case Library is a collection of teaching cases with a public health focus, written by Harvard Chan faculty, case writers, and students, or in collaboration with other institutions and initiatives. Use the filters at right to search the case library by subject, geography, health condition, and representation of diversity and identity to find cases to fit your teaching needs.
Radiology Pathology Correlation Case Studies. 2017-2018. 2018-2019. 2019-2020. Early Specialization in Interventional Radiology (ESIR) Diagnostic Radiology/Nuclear Medicine (DR/NM) Pathway. Angiography and Interventional Radiology Observership. Verification of Graduate Medical Education Training and Faculty Appointment. Each student is required ...
Doege-Potter syndrome is a rare paraneoplastic phenomenon associated with solitary fibrous tumors of the pleura (SFTPs). It is characterized by the presence of severe, sustained, and treatment-refractory hypoglycemia. Hypoglycaemia, which may be the sole symptom at disease onset, is mediated by the secretion of high-molecular-weight insulin-like growth factor (IGF-2).
Medical professionals in India want a central law that makes violence against doctors a non-bailable, punishable offence, in hopes that it deters such violent crimes against doctors in the future.
In a clinical trial and study supported by Brown scientists and alumni, a participant regained nearly fluent speech using a brain-computer interface that translates brain signals into speech with up to 97% accuracy. The new BCI system allowed Casey Harrell, a 45-year-old person with ALS, to communicate his intended speech effectively within ...
The spectrum of clinical presentation and reliance on patients seeking health care and on health care professionals recognizing a rare vaccine-associated adverse event limits determination of the true incidence of this condition. 7 In contrast to passive case finding, Engler et al 2 reported a significantly higher incidence of myocarditis and ...
Making the case for potatoes Potatoes are the richest source of dietary potassium in Western diets, and high potassium diets have been shown to prevent high blood pressure and Type 2 diabetes ...
Five weeks earlier, nausea, vomiting, diarrhea, chills, and fever had developed. CT revealed bilateral pelvic masses; examination of a peripheral-blood smear revealed schistocytes, anisocytosis ...
Several studies have shown that antibodies prompted by the Jynneos vaccine wane and may be undetectable within a year. But other research has found that two doses effectively prevent severe ...
In the early hours of Thursday, a mob of some 40 people angry at authorities' handling of the case stormed the grounds of the R.G. Kar Medical College and Hospital, the site of the murder.
Mpox has occurred in West, Central and East Africa for decades, with the first human case identified in 1970. Two types of the virus that causes mpox have been identified. ... are being notified of the initial results and offered the opportunity to participate in an ongoing extension study providing further supportive medical care. Additional ...
Candlelight memorial for the victim. On 9 August 2024, Moumita Debnath, a trainee doctor at RG Kar Medical College in Kolkata, West Bengal, India was raped and murdered.Her dead body was found on campus. The incident has amplified debate about the safety of women and doctors in India, and has sparked significant outrage, nationwide protests, and demands for a thorough investigation.