LOGIN

Annual Report
- Board of Directors
- Nomination Process
- Organizational Structure
- ATS Policies
- ATS Website
- MyATS Tutorial
- ATS Experts
- Press Releases
Member Newsletters
- ATS in the News
- ATS Conference News
- Embargo Policy
ATS Social Media
Breathe easy podcasts, ethics & coi, health equity, industry resources.
- Value of Collaboration
- Corporate Members
- Advertising Opportunities
- Clinical Trials
- Financial Disclosure
In Memoriam
Global health.
- International Trainee Scholarships (ITS)
- MECOR Program
- Forum of International Respiratory Societies (FIRS)
- 2019 Latin American Critical Care Conference
Peer Organizations
Careers at ats, affordable care act, ats comments and testimony, forum of international respiratory societies, tobacco control, tuberculosis, washington letter.
- Clinical Resources
- ATS Quick Hits
- Asthma Center
Best of ATS Video Lecture Series
- Coronavirus
- Critical Care
- Disaster Related Resources
- Disease Related Resources
- Resources for Patients
- Resources for Practices
- Vaccine Resource Center
- Career Development
- Resident & Medical Students
- Junior Faculty
- Training Program Directors
- ATS Reading List
- ATS Scholarships
- ATS Virtual Network
ATS Podcasts
- ATS Webinars
- Professional Accreditation
Pulmonary Function Testing (PFT)
- Calendar of Events
Patient Resources
- Asthma Today
- Breathing in America
- Fact Sheets: A-Z
- Fact Sheets: Topic Specific
- Patient Videos
- Other Patient Resources
Lung Disease Week
Public advisory roundtable.
- PAR Publications
- PAR at the ATS Conference
Assemblies & Sections
- Abstract Scholarships
- ATS Mentoring Programs
- ATS Official Documents
- ATS Interest Groups
- Genetics and Genomics
- Medical Education
- Terrorism and Inhalation Disasters
- Allergy, Immunology & Inflammation
- Behavioral Science and Health Services Research
- Clinical Problems
- Environmental, Occupational & Population Health
- Pulmonary Circulation
- Pulmonary Infections and Tuberculosis
- Pulmonary Rehabilitation
- Respiratory Cell & Molecular Biology
- Respiratory Structure & Function
- Sleep & Respiratory Neurobiology
- Thoracic Oncology
- Joint ATS/CHEST Clinical Practice Committee
- Clinicians Advisory
- Council of Chapter Representatives
- Documents Development and Implementation
- Drug/Device Discovery and Development
- Environmental Health Policy
- Ethics and Conflict of Interest
- Health Equity and Diversity Committee
- Health Policy
- International Conference Committee
- International Health
- Members In Transition and Training
- View more...
- Membership Benefits
- Categories & Fees
- Special Membership Programs
- Renew Your Membership
- Update Your Profile
- ATS DocMatter Community
- Respiratory Medicine Book Series
- Elizabeth A. Rich, MD Award
- Member Directory
- ATS Career Center
- Welcome Trainees
- ATS Wellness
- Thoracic Society Chapters
- Chapter Publications
- CME Sponsorship
Corporate Membership
Clinical cases, professionals.
- Respiratory Health Awards
- Clinicians Chat
- Ethics and COI
- Pulmonary Function Testing
- ATS Resources
- Live from the CCD
- Pediatric Division Directors

The ATS Clinical Cases are a series of cases devoted to interactive clinical case presentations on all aspects of pulmonary, critical care and sleep medicine. They are designed to provide education to practitioners, faculty, fellows, residents, and medical students in the areas of pulmonary, critical care and sleep medicine.
Currently, we are not accepting new cases for this series, as there are several other venues for publishing cases. For cases that can be written as brief, image-based quesitons, consider submitting them as to Quick Hits . For other cases, please contact your assembly web director regarding other opportunities to publish or highlight cases.
ATS Clinical Cases Designated by the Assemblies
Assembly on Allergy, Immunology, and Inflammation
- A Case Of Diffuse Miliary Pulmonary Infiltrates In A 35 Year-Old Man
- The Mighty Eosinophil
- Persistent Dyspnea in a Patient with Down’s Syndrome
- A 20 Year-Old with a Mediastinal Mass
- A Transsexual with Acute Dyspnea and Diffuse Infiltrates
- Use of Endobronchial Ultrasound to Diagnose an Incidental Lung Nodule
- Persistent Dyspnea Despite Maximal Medical Therapy in COPD
- Uncontrolled asthma, recurrent rhinosinusitis, and infertility in a young woman
- A case of progressive dyspnea and abnormal chest x-ray
- A 27 year old with a non resolving cavitary lung lesion
- ARDS Following Autologous Hematopoietic Stem Cell Transplantation for Multiple Myeloma
- Sudden Onset of Wheezing at Work
- Difficult-to-Control Asthma in a 49-Year-Old Man
- Dyspnea and wheezing in a pregnant patient
- Mediastinal Lymphadenopathy and Interstitial Lung Disease in a Cancer Patient
- Diffuse Infiltrates Following Hematopoietic Stem Cell Transplantation
- Difficult-to-control asthma in 13-year-old boy
- Stable Mild Persistent Asthma in a Young Adult
- Dyspnea in a college athlete
Assembly on Behavioral Science and Health Services Research
- Challenges in Caring for the Child with Asthma: Enlisting Community Services
- A 60-Year-Old Man with Acute Respiratory Failure and Mental Status Changes
- Young Man with Recent Onset Hypertension and Acute Onset Dyspnea
- Hoarseness and Hemoptysis in a 28-Year-Old Pregnant Woman
Assembly on Critical Care
- 60-Year-Old Man with Non-resolving Pneumonia
- Egg Shell Calcifications in a 69 Year Old Woman
- Cavitating Lung Lesion in a 59 year-old man.
- Intracerebral Hemorrhage in a Young Adult Male Patient
- A 39 Year Old Woman with Fever and Myalgia
- Septic Shock Following an Ulcerative Colitis Flare
- A 67-Year-Old Man with Massive Hemoptysis
- Chest Pain After Sexual Intercourse
- Liver dysfunction and severe lactic acidosis in a previously healthy man
Assembly on Clinical Problems
- Clinical Considerations for Individuals with Cystic Fibrosis
- An Unusual Cause of Chest Pain
- A 5 year old girl with Prader-Willi syndrome and worsening snoring during growth hormone therapy
- Dry Cough and Clubbing in a 45-Year-Old Woman
- Near-Complete Opacification of the Right Hemithorax
- Sudden Onset Chest Pain in a Young Man
- Intrapulmonary Shunting Through Tumor Causing Refractory Hypoxemia
Assembly on Environmental, Occupational and Population Health
- Progressive Dyspnea in an Appalachian Coal Miner
- Workplace Spirometry: Early Detection Benefits Individuals, Worker Groups and Employers
- “Horse play and the Lung” – a possible cobalt effect?
- Nonspecific Interstitial Pneumonitis or Hypersensitivity Pneumonitis?
Assembly on Microbiology, Tuberculosis and Pulmonary Infections
- Acute Respiratory Distress Syndrome Secondary to an Unusual Infection
- A Pregnant Woman with Fever and Respiratory Failure
- Cavitating Lung Lesion and Recurrent Chest Infections
- Bronchiectasis and recurrent pulmonary infections
Assembly on Pediatrics
- A six year-old child with cough and facial swelling
Assembly on Pulmonary Circulation
- A Cystic Fibrosis Patient with Hemoptysis From an Unusual Cause
- A 57 Year Old Woman with Pulmonary Hypertension Suffering Worsening Dyspnea on Endothelin Receptor Antagonist Therapy
- 70- Year-Old Woman with Progressive Dyspnea and Dilated Pulmonary Arteries
- An 18-year-old woman with severe dyspnea, hypoxia and abnormal chest findings
Assembly on Pulmonary Rehabilitation
- Pre- and Postoperative Pulmonary Rehabilitation for a COPD Patient Undergoing Bilateral Lung Transplant
Assembly on Sleep and Respiratory Neurobiology
- Central Hypersomnolence: History is the Key
- Persistent Sleepiness in Obstructive Sleep Apnea
- A case of Sleep Disordered Breathing after Coronary Artery Bypass Graft Surgery.
- Postoperative Respiratory Failure in a Child — A Diagnostic Dilemma
- A Case of “Complex” Sleep Apnea?
- Hypersomnolent, Hypercapnic, and Morbidly Obese
- Sleepy Since Adolescence

The American Thoracic Society improves global health by advancing research, patient care, and public health in pulmonary disease, critical illness, and sleep disorders. Founded in 1905 to combat TB, the ATS has grown to tackle asthma, COPD, lung cancer, sepsis, acute respiratory distress, and sleep apnea, among other diseases.
AMERICAN THORACIC SOCIETY 25 Broadway New York, NY 10004 United States of America Phone: +1 (212) 315-8600 Fax: +1 (212) 315-6498 Email: [email protected]
Privacy Statement | Term of Use | COI Conference Code of Conduct

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- MedEdPORTAL

“I Have a Cough”: An Interactive Virtual Respiratory Case-Based Module
Nelia afonso.
1 Professor, Foundation Medical Studies, Oakland University William Beaumont School of Medicine
Arati Kelekar
2 Assistant Professor, Internal Medicine, Oakland University William Beaumont School of Medicine and Beaumont Health System
Anjali Alangaden
3 Third-Year Medical Student, Wayne State University School of Medicine
Associated Data
- Facilitator Guide.docx
- PowerPoint for Facilitator.pptx
- SP Case Development Tool.docx
- Telemedicine Encounter SP Feedback Checklist.doc
- Student Worksheet Postsession.docx
- Student Survey Postsession.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Introduction
The COVID-19 pandemic has radically disrupted traditional models of medical education, forcing rapid evolution in the delivery of clinical training. As a result, clinical educators must quickly transition away from in-person sessions and develop effective virtual learning opportunities instead. This virtual resource was designed to replace a clinical simulation session for the physical examination course for medical students in the preclinical years.
We designed an online interactive module in three sections for preclinical (first- or second-year) medical students who had not yet learned the respiratory physical exam. The first section incorporated demonstration and practice of the components of the respiratory physical exam that could be effectively taught via videoconferencing software. Following this, students conducted a telemedicine encounter with a standardized patient and received patient-centered feedback evaluating their communication skills. The final segment involved a case discussion and clinical reasoning component.
These sessions were implemented for 122 first-year medical students. The module was well received by the students. A majority felt that it helped improve their telemedicine communication skills (93%), interpretation of physical exam findings (84%), development of differential diagnosis (95%), and correlation of clinical and basic science content (93%).
Our pilot educational session demonstrates that this virtual instruction method is an effective tool for teaching basic clinical skills during medical school. Virtual learning resources allow remote instruction to take place and can be a supplement when face-to-face clinical teaching is not possible.
Educational Objectives
By the end of this activity, learners will be able to:
- 1. Describe the components of a thorax/lung exam and practice basic percussion and auscultation techniques.
- 2. Elicit a comprehensive history from a standardized patient during a telemedicine encounter and develop a differential diagnosis with supportive evidence from the history and physical examination.
- 3. Practice a telehealth encounter.
- 4. Recommend appropriate diagnostic testing for a patient with suspected pneumonia.
- 5. Demonstrate knowledge specific to community-acquired pneumonia and COVID-19.
Clinical skills education is deeply rooted in face-to-face history taking, hands-on physical examination, and collaborative clinical reasoning with faculty coaching and feedback. However, these traditional tenets of clinical skills training for medical students have been entirely upended by the COVID-19 pandemic, and educators have had to quickly adapt. As a result of the pandemic, many medical schools have suspended or curtailed in-person sessions, and virtual alternatives have become essential.
Clinical skills directors have been challenged to create virtual training interactions to ensure students are comfortable with and competent at history taking and physical examination skills.
Although medical student interaction with patients was suspended in March 2020 in accordance with AAMC guidelines, many clinical rotations continued to provide educational opportunities via virtual morning reports and telemedicine visits. 1 – 3 Hoffman, Harding, Youm, and Wiechmann were even able to virtually bring students into the hospital rooms of COVID-19 patients, allowing the students to learn directly from both patients personally experiencing the disease and the team members caring for them. 4 Shih, Chan, Chen, and Lai adapted face-to-face demonstrations of techniques for preclinical students by a clinical tutor to Zoom-based small-group tutorials. 5 Hannon, Lappe, Griffin, Roussel, and Colbert-Getz utilized videoconferencing software to convert in-person objective structured clinical examinations to remote ones, allowing for the continued assessment of students. 6
Medical students have also challenged educators to use the current circumstances as a learning experience and expressed the desire that medical education should be continually adapted to meet their educational goals and prepare them for their eventual role as frontline workers. 7 However, currently, there is a paucity of fully developed resources available for virtual clinical skills training. 8 – 15
We designed this online interactive case-based learning module to teach students how to evaluate a patient with respiratory concerns and perform some components of a respiratory exam. As the COVID-19 pandemic came to dominate the cultural conversation at all levels, we found it to be a remarkable diagnosis to center the module around. Additionally, as this virus is an entirely novel disease entity, diagnosis of the condition had not been previously taught in the clinical skills curriculum, making it an engaging, timely, and unique manner in which to train students in history taking and respiratory examination.
Session Design
Prior to the developing the module, faculty discussed the content that was imperative to include in the standardized patient (SP) presentation and case discussion. After identifying the most important pulmonary complaints commonly seen in the primary care setting, we focused on a patient presenting with cough and fever.
In particular, we incorporated the components of the respiratory physical exam that could be effectively taught and demonstrated via videoconferencing software. These real-time teaching sessions provided immediate feedback to students and served as supplementation to several other online teaching resources, such as physical exam video demonstrations and step-by-step written guides.
The SP portrayed the role of a patient presenting to a clinic with cough and fever who was anxious that the symptoms could be COVID-19. The ensuing physical exam presentation, differential diagnoses, and discussion centered around the clinical features of community-acquired pneumonia (CAP) and, in particular, COVID-19.
This session was designed to allow several interactions to take place between the following:
- 1. Faculty and students—during the demonstration of percussion and auscultation.
- 2. Students, SP, and faculty—during a telemedicine patient encounter with patient-centered feedback from the SP on students' communication skills and “web-side” manner. Faculty also provided communication skills feedback.
- 3. Faculty and students—during the clinical reasoning and case discussion session.
At the conclusion of the session, students were encouraged to complete an optional four-question survey to measure their satisfaction with the demonstration of the respiratory physical exam, clinical reasoning exercises, and overall correlation with basic science content. The survey was administered through the school's learning management platform (Moodle).
- • Detailed facilitator guide ( Appendix A ): contains instructions for faculty preceptors.
- • PowerPoint presentation ( Appendix B ): reveals case details and related questions sequentially as the case unfolds. Relevant teaching slides were included to illustrate important or difficult concepts.
- • SP case (Madison Lopez) training material ( Appendix C ).
- • Telemedicine encounter SP feedback checklist ( Appendix D ).
- • Student worksheet ( Appendix E ).
- • Postsession student survey ( Appendix F ).
Facilitator Training
All faculty facilitators attended a 90-minute training session held via videoconferencing software (Google Meet). During this training, the clinical skill course director familiarized facilitators with the learning objectives and case materials, demonstrated the relevant physical exam techniques, and coached instructors on guiding discussion among students. The director also reviewed session logistics, postencounter debriefing, and the importance of delivering meaningful feedback to students on their communication skills and empathy.
Additionally, as this videoconferencing platform was unfamiliar to many facilitators, the training session focused on features like screen sharing, muting nonparticipants, free-text typing, and answering student queries. Doing so preemptively addressed many potential issues and ensured that sessions flowed smoothly with minimal technical difficulties. The training session improved the comfort level of facilitators and ensured that content delivery was standardized.
SP Training
Sp training for portrayal of madison lopez.
An SP trainer instructed SPs on the specific symptoms, concerns, and appropriate physical behaviors to portray for Madison Lopez, a patient presenting with respiratory concerns. SPs were also instructed to give patient-centered feedback using the feedback checklist ( Appendix D ). Feedback focused on students' communication behavior and telemedicine web-side manner.
SP training for the student session
The SP training lasted 2 hours and was conducted via the same virtual platform used during the actual student sessions (Google Meet). The SPs were familiarized with session logistics, including using the videoconferencing software, specific times to log in, and when to provide feedback.
Presession Assignments for Students
We instructed students to review the physical exam of the lungs and thorax and accompanying videos from their required text. 16 , 17 They were also required to develop three illness scripts for conditions that could cause a patient to present with fever and cough: CAP (including COVID-19), acute bronchitis, and upper respiratory infection. 18
Session Delivery
Each session was facilitated by clinical faculty who taught in the clinical skills course. Each group was assigned an SP who called in for the telemedicine encounter.
Following the suspension of face-to-face teaching, these sessions were implemented for 122 first-year medical students during in their respiratory unit. Each session included six to eight students. Five clinical faculty ran 18 small-group sessions, each lasting 90 minutes. All sessions took place during the same week in April 2020. A postsession survey ( Appendix F ) was also given to participants.
Feedback to Students
Students received feedback both from SPs and from the clinical facilitator running their session. The SPs used a structured communication feedback tool (see Appendix D ) to evaluate students directly following the telemedicine portion of the session. Clinical faculty also provided feedback to students on the clinical content of their interaction with the SP.
A total of 122 first-year medical students participated in this session.
Student Satisfaction Survey
The voluntary survey was completed by 57 of 122 students (47%) who participated in the sessions. The majority of students felt that this session helped to improve their telemedicine communication skills (93%), interpretation of physical exam findings (84%), development of differential diagnosis (95%), and correlation of clinical and basic science content (93%). (See the Table for more details.)

Twenty-two of the 57 students who completed the survey wrote comments. Key themes identified were session format, student perception of learning, technology issues, and suggestions. These are listed below with representative quotes.
Format of session
- • “Small group setting is also great. I feel like I get a lot more out of these sessions compared to in-person ones that are larger.”
- • “I really loved this! I feel like I learn so much more by having the physician watch the interview take place and then going through the physical exam findings and talking about the case as we go. It helps me get a better picture of everything and it is more cohesive.”
- • “Good alternative to current dilemma.”
Student perceptions of learning (i.e., history taking, physical exam, case discussion)
- • “I thought it was helpful to incorporate telemedicine into our curriculum as it will likely be a part of our practice moving forward.”
- • “I like the idea of interviewing the patient in these group settings, with 1–2 students taking the lead. I have incorporated some questions into my own routine that I would not have otherwise asked by watching my peers ask those questions.”
- • “I think they are extremely helpful in ensuring we are taking a proper, thorough history as well as improving our medical reasoning.”
- • “I think this solidified my knowledge, in both the respiratory topics, but also the importance of being able to take a good history.”
- • “I thought that it was really helpful to go through certain aspects of the respiratory exam since we weren't able to practice in person.”
Technology issues
- • “There were some technological issues that made it difficult to hear at certain points in session.”
Suggestions
- • “I think it would be great if we were allowed to have a willing and quiet family member, housemate or fellow classmate with us… and get real-time feedback from [clinical skills course] faculty.”
This pilot educational session demonstrated that this method of virtual instruction is an effective educational tool for teaching basic clinical skills during medical school. However, we do not believe these sessions should replace dedicated curricular time for hands-on clinical teaching. We propose that creating virtual learning resources allows remote instruction to take place and can be a supplement to face-to-face clinical teaching in extraordinary situations.
Limitations
This module was developed at short notice following the abrupt cessation of in-person clinical skills teaching. Teaching of physical examination skills was certainly limited, but clinical faculty were still able to demonstrate selected techniques and discuss the pathophysiologic correlations of abnormal findings. The module also offered faculty an opportunity to coach small student groups and refine clinical reasoning. We believe that creating such resources allows remote instruction to take place within the current physical distancing needs and can be a supplement to face-to-face clinical teaching without suspension of that clinical teaching.
Using additional technology such as a digital stethoscope during teaching would augment demonstrations of the physical exam for these sessions. As this was only a single session, we did not assess student knowledge. We plan to repeat the session during the upcoming academic year and to create more robust assessment.
Lessons Learned
Session flow and faculty guide.
To ensure that adequate time was afforded to each section, the faculty guide provided facilitators with detailed time-management guidelines, in addition to direction on session content. When screen sharing, clinical instructors were unable to see the faces and reactions of learners, making it difficult to maintain the same level of engagement as during an in-person session. For that reason, providing instructors with skills to facilitate meaningful participation was something we focused on during the faculty training session.
Faculty preparation
Faculty were reminded to include all participants in the conversations and discussions, ideally by assigning roles prior to the telemedicine SP encounter. This ensured the smooth flow of the interview, especially considering multiple students were working with the same SP. When data gathering was noted to be suboptimal, observing students were encouraged to participate at the end of the interview to obtain additional information. As the faculty instructors were in the unique position of being able to observe the interview without any distractions, they were also encouraged to record and provide feedback on the students' communication skills independent of that provided by the SPs.
Numerous online modules for teaching various clinical skills like communication, physical examination, and clinical reasoning have been previously published and are available, but they tend to focus on each skill in isolation. MedEdPORTAL has several e-leaning resources and telemedicine SP cases, but none involve multimodal teaching strategies. 8 – 15 Our module integrates a telemedicine encounter, guided virtual practice of basic physical examination techniques, and delivery of relevant medical content and clinical reasoning with faculty educators who provide real-time coaching and feedback during each of these components.
Several medical schools and training programs have transitioned face-to-face clinical skills teaching and assessment to remote delivery. 2 – 6 Similar to Hannon and colleagues, 6 this remote educational session delivery enabled us to observe core clinical skills like history taking, documentation, and clinical reasoning. The students also took a proactive role in their educational experience since there was an element of self-directed learning that preceded the interactive session.
This session was effective in bringing together small groups of classmates and giving them an opportunity to interact even when not physically together. Additionally, we anticipate that for students who had already learned this content, progression and enhancement of these skills may be quicker and easier when they return to the Clinical Skills Center for face-to-face instruction. This module can easily be implemented by clinical skills courses and utilized by other medical schools.
Disclosures
None to report.
Funding/Support
Ethical approval.
The Oakland University Institutional Review Board approved this study.
- LOGIN / FREE TRIAL

‘Racism absolutely must not be tolerated’
STEVE FORD, EDITOR
- You are here: COPD
Diagnosis and management of COPD: a case study
04 May, 2020
This case study explains the symptoms, causes, pathophysiology, diagnosis and management of chronic obstructive pulmonary disease
This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient’s associated pathophysiology. Diagnosis involves spirometry testing to measure the volume of air that can be exhaled; it is often performed after administering a short-acting beta-agonist. Management of chronic obstructive pulmonary disease involves lifestyle interventions – vaccinations, smoking cessation and pulmonary rehabilitation – pharmacological interventions and self-management.
Citation: Price D, Williams N (2020) Diagnosis and management of COPD: a case study. Nursing Times [online]; 116: 6, 36-38.
Authors: Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
The term chronic obstructive pulmonary disease (COPD) is used to describe a number of conditions, including chronic bronchitis and emphysema. Although common, preventable and treatable, COPD was projected to become the third leading cause of death globally by 2020 (Lozano et al, 2012). In the UK in 2012, approximately 30,000 people died of COPD – 5.3% of the total number of deaths. By 2016, information published by the World Health Organization indicated that Lozano et al (2012)’s projection had already come true.
People with COPD experience persistent respiratory symptoms and airflow limitation that can be due to airway or alveolar abnormalities, caused by significant exposure to noxious particles or gases, commonly from tobacco smoking. The projected level of disease burden poses a major public-health challenge and primary care nurses can be pivotal in the early identification, assessment and management of COPD (Hooper et al, 2012).
Grace Parker (the patient’s name has been changed) attends a nurse-led COPD clinic for routine reviews. A widowed, 60-year-old, retired post office clerk, her main complaint is breathlessness after moderate exertion. She scored 3 on the modified Medical Research Council (mMRC) scale (Fletcher et al, 1959), indicating she is unable to walk more than 100 yards without stopping due to breathlessness. Ms Parker also has a cough that produces yellow sputum (particularly in the mornings) and an intermittent wheeze. Her symptoms have worsened over the last six months. She feels anxious leaving the house alone because of her breathlessness and reduced exercise tolerance, and scored 26 on the COPD Assessment Test (CAT, catestonline.org), indicating a high level of impact.
Ms Parker smokes 10 cigarettes a day and has a pack-year score of 29. She has not experienced any haemoptysis (coughing up blood) or chest pain, and her weight is stable; a body mass index of 40kg/m 2 means she is classified as obese. She has had three exacerbations of COPD in the previous 12 months, each managed in the community with antibiotics, steroids and salbutamol.
Ms Parker was diagnosed with COPD five years ago. Using Epstein et al’s (2008) guidelines, a nurse took a history from her, which provided 80% of the information needed for a COPD diagnosis; it was then confirmed following spirometry testing as per National Institute for Health and Care Excellence (2018) guidance.
The nurse used the Calgary-Cambridge consultation model, as it combines the pathological description of COPD with the patient’s subjective experience of the illness (Silverman et al, 2013). Effective communication skills are essential in building a trusting therapeutic relationship, as the quality of the relationship between Ms Parker and the nurse will have a direct impact on the effectiveness of clinical outcomes (Fawcett and Rhynas, 2012).
In a national clinical audit report, Baxter et al (2016) identified inaccurate history taking and inadequately performed spirometry as important factors in the inaccurate diagnosis of COPD on general practice COPD registers; only 52.1% of patients included in the report had received quality-assured spirometry.
Pathophysiology of COPD
Knowing the pathophysiology of COPD allowed the nurse to recognise and understand the physical symptoms and provide effective care (Mitchell, 2015). Continued exposure to tobacco smoke is the likely cause of the damage to Ms Parker’s small airways, causing her cough and increased sputum production. She could also have chronic inflammation, resulting in airway smooth-muscle contraction, sluggish ciliary movement, hypertrophy and hyperplasia of mucus-secreting goblet cells, as well as release of inflammatory mediators (Mitchell, 2015).
Ms Parker may also have emphysema, which leads to damaged parenchyma (alveoli and structures involved in gas exchange) and loss of alveolar attachments (elastic connective fibres). This causes gas trapping, dynamic hyperinflation, decreased expiratory flow rates and airway collapse, particularly during expiration (Kaufman, 2013). Ms Parker also displayed pursed-lip breathing; this is a technique used to lengthen the expiratory time and improve gaseous exchange, and is a sign of dynamic hyperinflation (Douglas et al, 2013).
In a healthy lung, the destruction and repair of alveolar tissue depends on proteases and antiproteases, mainly released by neutrophils and macrophages. Inhaling cigarette smoke disrupts the usually delicately balanced activity of these enzymes, resulting in the parenchymal damage and small airways (with a lumen of <2mm in diameter) airways disease that is characteristic of emphysema. The severity of parenchymal damage or small airways disease varies, with no pattern related to disease progression (Global Initiative for Chronic Obstructive Lung Disease, 2018).
Ms Parker also had a wheeze, heard through a stethoscope as a continuous whistling sound, which arises from turbulent airflow through constricted airway smooth muscle, a process noted by Mitchell (2015). The wheeze, her 29 pack-year score, exertional breathlessness, cough, sputum production and tiredness, and the findings from her physical examination, were consistent with a diagnosis of COPD (GOLD, 2018; NICE, 2018).
Spirometry is a tool used to identify airflow obstruction but does not identify the cause. Commonly measured parameters are:
- Forced expiratory volume – the volume of air that can be exhaled – in one second (FEV1), starting from a maximal inspiration (in litres);
- Forced vital capacity (FVC) – the total volume of air that can be forcibly exhaled – at timed intervals, starting from a maximal inspiration (in litres).
Calculating the FEV1 as a percentage of the FVC gives the forced expiratory ratio (FEV1/FVC). This provides an index of airflow obstruction; the lower the ratio, the greater the degree of obstruction. In the absence of respiratory disease, FEV1 should be ≥70% of FVC. An FEV1/FVC of <70% is commonly used to denote airflow obstruction (Moore, 2012).
As they are time dependent, FEV1 and FEV1/FVC are reduced in diseases that cause airways to narrow and expiration to slow. FVC, however, is not time dependent: with enough expiratory time, a person can usually exhale to their full FVC. Lung function parameters vary depending on age, height, gender and ethnicity, so the degree of FEV1 and FVC impairment is calculated by comparing a person’s recorded values with predicted values. A recorded value of >80% of the predicted value has been considered ‘normal’ for spirometry parameters but the lower limit of normal – equal to the fifth percentile of a healthy, non-smoking population – based on more robust statistical models is increasingly being used (Cooper et al, 2017).
A reversibility test involves performing spirometry before and after administering a short-acting beta-agonist (SABA) such as salbutamol; the test is used to distinguish between reversible and fixed airflow obstruction. For symptomatic asthma, airflow obstruction due to airway smooth-muscle contraction is reversible: administering a SABA results in smooth-muscle relaxation and improved airflow (Lumb, 2016). However, COPD is associated with fixed airflow obstruction, resulting from neutrophil-driven inflammatory changes, excess mucus secretion and disrupted alveolar attachments, as opposed to airway smooth-muscle contraction.
Administering a SABA for COPD does not usually produce bronchodilation to the extent seen in someone with asthma: a person with asthma may demonstrate significant improvement in FEV1 (of >400ml) after having a SABA, but this may not change in someone with COPD (NICE, 2018). However, a negative response does not rule out therapeutic benefit from long-term SABA use (Marín et al, 2014).
NICE (2018) and GOLD (2018) guidelines advocate performing spirometry after administering a bronchodilator to diagnose COPD. Both suggest a FEV1/FVC of <70% in a person with respiratory symptoms supports a diagnosis of COPD, and both grade the severity of the condition using the predicted FEV1. Ms Parker’s spirometry results showed an FEV1/FVC of 56% and a predicted FEV1 of 57%, with no significant improvement in these values with a reversibility test.
GOLD (2018) guidance is widely accepted and used internationally. However, it was developed by medical practitioners with a medicalised approach, so there is potential for a bias towards pharmacological management of COPD. NICE (2018) guidance may be more useful for practice nurses, as it was developed by a multidisciplinary team using evidence from systematic reviews or meta-analyses of randomised controlled trials, providing a holistic approach. NICE guidance may be outdated on publication, but regular reviews are performed and published online.
NHS England (2016) holds a national register of all health professionals certified in spirometry. It was set up to raise spirometry standards across the country.
Assessment and management
The goals of assessing and managing Ms Parker’s COPD are to:
- Review and determine the level of airflow obstruction;
- Assess the disease’s impact on her life;
- Risk assess future disease progression and exacerbations;
- Recommend pharmacological and therapeutic management.
GOLD’s (2018) ABCD assessment tool (Fig 1) grades COPD severity using spirometry results, number of exacerbations, CAT score and mMRC score, and can be used to support evidence-based pharmacological management of COPD.

When Ms Parker was diagnosed, her predicted FEV1 of 57% categorised her as GOLD grade 2, and her mMRC score, CAT score and exacerbation history placed her in group D. The mMRC scale only measures breathlessness, but the CAT also assesses the impact COPD has on her life, meaning consecutive CAT scores can be compared, providing valuable information for follow-up and management (Zhao, et al, 2014).
After assessing the level of disease burden, Ms Parker was then provided with education for self-management and lifestyle interventions.
Lifestyle interventions
Smoking cessation.
Cessation of smoking alongside support and pharmacotherapy is the second-most cost-effective intervention for COPD, when compared with most other pharmacological interventions (BTS and PCRS UK, 2012). Smoking cessation:
- Slows the progression of COPD;
- Improves lung function;
- Improves survival rates;
- Reduces the risk of lung cancer;
- Reduces the risk of coronary heart disease risk (Qureshi et al, 2014).
Ms Parker accepted a referral to an All Wales Smoking Cessation Service adviser based at her GP surgery. The adviser used the internationally accepted ‘five As’ approach:
- Ask – record the number of cigarettes the individual smokes per day or week, and the year they started smoking;
- Advise – urge them to quit. Advice should be clear and personalised;
- Assess – determine their willingness and confidence to attempt to quit. Note the state of change;
- Assist – help them to quit. Provide behavioural support and recommend or prescribe pharmacological aids. If they are not ready to quit, promote motivation for a future attempt;
- Arrange – book a follow-up appointment within one week or, if appropriate, refer them to a specialist cessation service for intensive support. Document the intervention.
NICE (2013) guidance recommends that this be used at every opportunity. Stead et al (2016) suggested that a combination of counselling and pharmacotherapy have proven to be the most effective strategy.
Pulmonary rehabilitation
Ms Parker’s positive response to smoking cessation provided an ideal opportunity to offer her pulmonary rehabilitation (PR) – as indicated by Johnson et al (2014), changing one behaviour significantly increases a person’s chance of changing another.
PR – a supervised programme including exercise training, health education and breathing techniques – is an evidence-based, comprehensive, multidisciplinary intervention that:
- Improves exercise tolerance;
- Reduces dyspnoea;
- Promotes weight loss (Bolton et al, 2013).
These improvements often lead to an improved quality of life (Sciriha et al, 2015).
Most relevant for Ms Parker, PR has been shown to reduce anxiety and depression, which are linked to an increased risk of exacerbations and poorer health status (Miller and Davenport, 2015). People most at risk of future exacerbations are those who already experience them (Agusti et al, 2010), as in Ms Parker’s case. Patients who have frequent exacerbations have a lower quality of life, quicker progression of disease, reduced mobility and more-rapid decline in lung function than those who do not (Donaldson et al, 2002).
“COPD is a major public-health challenge; nurses can be pivotal in early identification, assessment and management”
Pharmacological interventions
Ms Parker has been prescribed inhaled salbutamol as required; this is a SABA that mediates the increase of cyclic adenosine monophosphate in airway smooth-muscle cells, leading to muscle relaxation and bronchodilation. SABAs facilitate lung emptying by dilatating the small airways, reversing dynamic hyperinflation of the lungs (Thomas et al, 2013). Ms Parker also uses a long-acting muscarinic antagonist (LAMA) inhaler, which works by blocking the bronchoconstrictor effects of acetylcholine on M3 muscarinic receptors in airway smooth muscle; release of acetylcholine by the parasympathetic nerves in the airways results in increased airway tone with reduced diameter.
At a routine review, Ms Parker admitted to only using the SABA and LAMA inhalers, despite also being prescribed a combined inhaled corticosteroid and long-acting beta 2 -agonist (ICS/LABA) inhaler. She was unaware that ICS/LABA inhalers are preferred over SABA inhalers, as they:
- Last for 12 hours;
- Improve the symptoms of breathlessness;
- Increase exercise tolerance;
- Can reduce the frequency of exacerbations (Agusti et al, 2010).
However, moderate-quality evidence shows that ICS/LABA combinations, particularly fluticasone, cause an increased risk of pneumonia (Suissa et al, 2013; Nannini et al, 2007). Inhaler choice should, therefore, be individualised, based on symptoms, delivery technique, patient education and compliance.
It is essential to teach and assess inhaler technique at every review (NICE, 2011). Ms Parker uses both a metered-dose inhaler and a dry-powder inhaler; an in-check device is used to assess her inspiratory effort, as different inhaler types require different inhalation speeds. Braido et al (2016) estimated that 50% of patients have poor inhaler technique, which may be due to health professionals lacking the confidence and capability to teach and assess their use.
Patients may also not have the dexterity, capacity to learn or vision required to use the inhaler. Online resources are available from, for example, RightBreathe (rightbreathe.com), British Lung Foundation (blf.org.uk). Ms Parker’s adherence could be improved through once-daily inhalers, as indicated by results from a study by Lipson et al (2017). Any change in her inhaler would be monitored as per local policy.
Vaccinations
Ms Parker keeps up to date with her seasonal influenza and pneumococcus vaccinations. This is in line with the low-cost, highest-benefit strategy identified by the British Thoracic Society and Primary Care Respiratory Society UK’s (2012) study, which was conducted to inform interventions for patients with COPD and their relative quality-adjusted life years. Influenza vaccinations have been shown to decrease the risk of lower respiratory tract infections and concurrent COPD exacerbations (Walters et al, 2017; Department of Health, 2011; Poole et al, 2006).
Self-management
Ms Parker was given a self-management plan that included:
- Information on how to monitor her symptoms;
- A rescue pack of antibiotics, steroids and salbutamol;
- A traffic-light system demonstrating when, and how, to commence treatment or seek medical help.
Self-management plans and rescue packs have been shown to reduce symptoms of an exacerbation (Baxter et al, 2016), allowing patients to be cared for in the community rather than in a hospital setting and increasing patient satisfaction (Fletcher and Dahl, 2013).
Improving Ms Parker’s adherence to once-daily inhalers and supporting her to self-manage and make the necessary lifestyle changes, should improve her symptoms and result in fewer exacerbations.
The earlier a diagnosis of COPD is made, the greater the chances of reducing lung damage through interventions such as smoking cessation, lifestyle modifications and treatment, if required (Price et al, 2011).
- Chronic obstructive pulmonary disease is a progressive respiratory condition, projected to become the third leading cause of death globally
- Diagnosis involves taking a patient history and performing spirometry testing
- Spirometry identifies airflow obstruction by measuring the volume of air that can be exhaled
- Chronic obstructive pulmonary disease is managed with lifestyle and pharmacological interventions, as well as self-management
Related files
200506 diagnosis and management of copd – a case study.
- Add to Bookmarks
Related articles

Nurse-led cognitive behavioural therapy for respiratory patients
Anxiety and depression are common comorbidities of chronic obstructive pulmonary disease. This…

Issues of home-based non-invasive ventilation
Non-invasive ventilation is increasingly used to manage patients with COPD at home,…

Improving outcomes with online COPD self-care
An innovative approach to the self-management of chronic obstructive pulmonary disease is…

An audit of care provided to patients with COPD
Nationwide audit of COPD care reveals many aspects of provision have improved,…
Have your say
Sign in or Register a new account to join the discussion.
Interactive Case Studies In Respiratory Care
Sep 24, 2014
430 likes | 604 Views
Interactive Case Studies In Respiratory Care. Doug Pursley , M.Ed., RRT Program Director Ozarks Technical Community College Springfield, MO. Case 1. A 74 year old female with COPD is admitted to the ED with mild chest pain. She is on her portable liquid system at 3 l/m.
Share Presentation
- 40 ventimask
- paco2 40 30
- 40 ventimask running 6

Presentation Transcript
Interactive Case Studies In Respiratory Care Doug Pursley, M.Ed., RRT Program Director Ozarks Technical Community College Springfield, MO
Case 1 • A 74 year old female with COPD is admitted to the ED with mild chest pain. She is on her portable liquid system at 3 l/m. • B/S, CXR clear, pt. is alert and oriented • ABGs: pH 7.32, PaCO2 84, HCO2 42, BE +15, PaO2 68 • The physician sees the initial ABG and wants to place the patient on BiPAP.
The RCP disagreed and convinced the physician that BiPAP is not indicated at this timesince the patient is not in respiratory distress and has “classic” chronic hypercarbia. • She is moved to a regular room from triage to await labs and speak with the physician • 30 minutes later the physician pops his head in the door and finds the patient lethargic and on 10 l/m per nasal cannula. • ABG at this time is: pH 7.20, PaCO2 110, HCO3 41, BE +13, PaO2 117
Now she is BiPAPed 10/5 and 40% • Next ABG shows: 7.22, PaCO2 103, HCO3 41, BE +13, PaO2 64 • The patient’s BiPAP settings are changed to 15/5 and she is transferred to the MICU. • She is removed from BiPAP a few hours later and had the following ABG on 3 l/m: pH 7.30, PaCO2 87, HCO3 41, BE +14, PaO2 61 • Obviously a case of oxygen-induced hypercarbia
Case 2 • A 53 year old female with diabetes and COPD is admitted to the ED. • She walks in under her own power and has the following ABG drawn 10 minutes later: pH 6.65, PaCO2 76, HCO3 8, BD -25 • Glucose 620, increased WBCs • She is placed on BiPAP 20/15, 100% for a few minutes and then intubated • She develops asystole as she is being intubated and is resuscitated unsuccessfully for 45 minutes.
Case 3 • The patient is a 34 year old male that has just been brought to the ETC after a narcotic overdose. He is currently being mechanically ventilated. What is your recommendation after seeing his CXR?
Case 4 • 450 lb. 45 year male is brought to a local ETC (PB 730 mmHg) in acute respiratory distress. Someone places him on a nasal cannula but they forget to turn the O2 on. He is also placed on a pulse oximeter and ABG’s are drawn.
Good pleth waveforms are seen on the pulse oximeter which measured 81% at the time the ABG was drawn. Ten minutes later, you arrive, turn the oxygen on, and titrate the O2 achieving an SpO2 of 94%. • The patient’s vital signs improve and he says he is less short of breath.
ABGs on room air were: FI02 .21 pH 7.33 PaC02 64 HCO3 32.6 Base +7 Pa02 84 Sp02 81% (at time of blood draw)
What is your recommendation after seeing the ABG?
Case 5 • K.B. is a 55 kg., 72 year old documented CO2 retainer with end-stage COPD who also has a history of severe air trapping and dynamic flow limitation.
Admitted the previous day for exacerbation of his COPD. • Intubated and placed on a ventilator after failing NIV. • Current ventilator settings are: PRVC, 500 X 16 (total f 16), Set PEEP 5, and FIO2 0.35 • Total PEEP is measured at 10 cmH2O
ABG’s on those settings are: • pH 7.50 • PaCO2 40 mmHg • HCO3 30.1 • BE +6 • PaO2 65 • SaO2 94% • Hb 18 g%
What is your recommendation?
Case 6 • An 8 year old boy is brought to the ETC after being hit by a car while walking across a Walmart parking lot. • He was intubated prior to arrival and is currently being manually ventilated. • A chest x-ray is taken with the boy in the supine position.
The CXR shows an ETT just inside the RMS and fractures of the 4th and 5th posterior ribs on the right. What other major finding is seen on the CXR?
What is the major finding? • Left pleural effusion • Right pneumothorax • Left pneumonia • Pulmonary edema
His ABG’s are: pH 7.19, PaCO2 60, HCO3 22. Interpretation?
Case 7 • You are taking care of a post-op cholecystectomy patient on a 40% ventimask. The recommended flow stamped on the device is 6 l/m, which is what the device is set for.
On further examination, you notice that the patient’s work of breathing seems to be slightly increased and that her SpO2 is 88% • You then perform a quick calculation and determine that the total flow exiting a 40% ventimask running @ 6 l/m is 24 l/m (3:1 ratio) and remember your old instructor in school saying that a normal, resting inspiratory flowrate for an adult is about 25-35 l/m.
What is the most appropriate action to take at this time?
Most appropriate action? • Take her off the venti and place her on a 6 l/m cannula • Increase the FIO2 on the ventimask to 50% • Increase the flow on the 40% ventimask • Do nothing. The stamped flow says 6therefore it has to be set on 6.
Case 8 • A nurse hears cries of help from a 64 year old female COPD, lung cancer patient. She is on oxygen. • When she gets to the patient’s room, she finds the O2 tubing, pillow, and patient’s hair on fire. • She quickly extinguishes the fire but the patient suffered burns to the face, neck, right shoulder, and upper back while trying to light a cigarette. • The patient is then transferred to the Burn Unit.
According to data from the Consumer Product Safety Commission, approximately how many medical oxygen related thermal burns were seen in US emergency rooms in the four years from Jan 1,2003 to Dec 31, 2006? FIRES AND BURNS INVOLVING HOME MEDICAL OXYGEN Marty Ahrens Fire Analysis and Research Division National Fire Protection Association August 2008
How many O2 induced thermal burns do you think were reported in the US from Jan 1, 2003-Dec 31, 2006? • 1,000 • 5,000 • 25,000 • 100,000
Case 9 • A 76 year-old, 58 kg IBW, male is admitted with extreme hypothermia
Vitals on admission • Temperature 30 C • Pulse 74 • f 41 and shallow • Crackles • Atrial fibrillation
76 year-old, 58 kg IBW • In the ER he is placed on a ventilator with the following settings: PC, pressure 23 cmH20, f 12, PEEP 8, FIO2 0.35, exhaled tidal volume 570 ml. • ABG’s reported at 37 C are: • pH 7.40 • PaCO2 40 • PaO2 80
Because he was hypothermic when the blood gas was drawn, the physician requested that the lab correct the ABG to 30 C. • The corrected ABG is: • pH 7.50 • PaCO2 30 • PaO2 54
The ER doc asks for your opinion on what ventilator changes to make. • What is your recommendation at this time?
What is your recommendation? • Decrease rate from 12 to 8 • Increase FIO2 from 0.35 to 0.60 • Increase PEEP from 8 to 15 • Do all three • Make no changes at this time 37 C30 C pH 7.40 7.50 PaCO2 40 30 PaO2 80 54
Case 10 • A 64 year old male presents to the ED with extreme shortness of breath. A CXR is obtained.
What immediate treatment is indicated? • IPV • Bilalateral chest tubes • Bronchoscopy • Albuterol and CPT Q2 • CPAP and 40 mg of Lasix
Case 11 • A 37 year old male presents with bronchial breath sounds and crackles in the left lower lobe, E to A egophony on the left, increased tactile fremitus on the left, dull percussion note on the left, and decreased chest expansion on the left.
What do the findings suggest? • Pneumothorax • Pneumonia • Pleural effusion • Bronchitis • Asthma
Case 12 • A 40 kg., 32 year old female MVA is being ventilated and has a 6.0 ETT in place. • She is currently being suctioned with a 14 F catheter. • You and a co-worker get into a discussion about the proper size of catheter to use on a 6.0 ETT
What is the ideal suction catheter size for a 6.0 ETT? • 1. 10 F • 2. 12 F • 3. 14 F • 4. Doesn’t matter
Case 13 • Just as you are about to go home for the day, you notice a group of people in the ED gathered around the lateral neck x-ray of a 13 year old male just admitted for extreme shortness of breath.
The lateral neck x-ray shows: • Epiglottitis • Croup • Foreign body obstruction • Retropharyngeal abscess • Cervical fracture
- More by User
Respiratory Care
Respiratory Care. Who, What, Where, When?. Mission Statement.
801 views • 11 slides
INTERACTIVE BIBLE STUDIES
INTERACTIVE BIBLE STUDIES. Definition.
530 views • 28 slides

???????????????????. ?????????????????? (intubation) ??????????????????????????????????? ?????????????????? ??????????????????????????????????????? (humidity and aerosol therapy)?????????????????????????? (tracheobronchial suction)????????????????????????? (chest physical therapy). ??????????????
1.26k views • 95 slides
979 views • 59 slides

RESPIRATORY CARE
RESPIRATORY CARE. A Great Career That Makes A Difference. What is Respiratory Care?. A health profession that specializes in the evaluation, treatment, education and rehabilitation of patients with lung and heart disease, under the direction of a physician
1.03k views • 35 slides

WebPath Respiratory Case Studies
WebPath Respiratory Case Studies. Dr. Spencer Gilbert. Laboratory Part I. CASE 1:. Clinical History:
1.51k views • 125 slides
RESPIRATORY CARE. Careers in Respiratory Care. The Respiratory Therapist’s Main Goal:. To help clients breathe more easily. Best Way: by preventing and treating disease. Two Main Levels of Practice:. CRT-Certified Respiratory Therapist (entry level position)
1.13k views • 48 slides
Respiratory Care. A Life and Breath Career for You!. Respiratory Care Makes a Difference. At 9:32 am, Lori Moreno brought a newborn baby struggling to breathe back to life… What have you accomplished today? Lori is a recent graduate of a respiratory therapist educational program.
590 views • 29 slides
Respiratory (A&P, ABG’s, Assessment) Respiratory case studies
Respiratory (A&P, ABG’s, Assessment) Respiratory case studies. Ron Pinkston, RRT Respiratory Therapist Staff Educator/ Team Leader. Chest Tubes. Chest Tubes. COPD. Indications for Oxygen Therapy. Hypoxemia Excessive Work of Breathing Excessive Work of Heart. Oxygen Delivery Devices.
1.72k views • 56 slides
Respiratory Care. Understanding the Organizations that Serve Our Profession. In Respiratory Care. American Association for Respiratory Care The professional association Committee on Accreditation for Respiratory Care Programs The accrediting body for schools
408 views • 15 slides
Interactive Case Studies in Lead Extraction
Interactive Case Studies in Lead Extraction. John Andriulli, DO, FACC Assistant Professor of Medicine Director of Arrhythmia Device Program Cooper University Hospital. CASE 1. CASE 2. CASE 3. 84 y/o M ICM EF 25% ICD implant 2007 Leads: 4076, 4194, 6949
298 views • 10 slides
Respiratory Care. A Life and Breath Career for You!. What is Respiratory Care?. Respiratory Care is the health profession that specializes in the promotion of optimum cardiopulmonary function and health. What is The Role of The Respiratory Care Practitioner .
386 views • 22 slides
Respiratory Care. Arterial Blood Gas Interpretation. Reference – Egan’s Fundamentals of Respiratory Care 8 th Edition. Normal Values for ABG. pH = 7.40 pCO 2 = 40 mmHg pO 2 = 90 mmHg Bicarb = 24 mEq/L Base Excess = 0 mEq/L S a O 2 = >90%. Normal Ranges. pH = 7.35 – 7.45
755 views • 30 slides
Respiratory Care. A Life and Breath Career for You!. What is Respiratory Care?. Respiratory Care is the health profession that specializes in the promotion of optimum cardiopulmonary function and health. What is The Role of The Respiratory Care Practitioner.
504 views • 22 slides
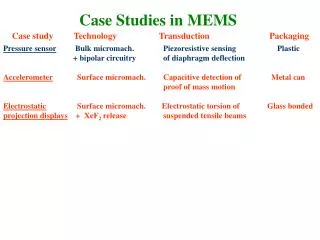
Case Studies in MEMS
Case Studies in MEMS. Case study Technology Transduction Packaging. Pressure sensor Bulk micromach. Piezoresistive sensing Plastic + bipolar circuitry of diaphragm deflection
1.25k views • 36 slides
Interactive case studies
Interactive case studies. Swisstransfusion, 6 September 2013 Haemovigilance M. Jutzi, M.Rüesch Clinical Reviewer Haemovigilance, Swissmedic. Case 1.
762 views • 62 slides
Respiratory Care Issues in Disasters
Texas State Guard Texas Medical Rangers HMRG - Galveston Company. Respiratory Care Issues in Disasters. Prepared by: CPT A. Amin, RRT, RCP and CPT W. Williams, RRT, RCP HMRG - Galveston Company. Texas State Guard Texas Medical Rangers HMRG - Galveston Company.
482 views • 35 slides
Respiratory Care in Neuromuscular Disease
Respiratory Care in Neuromuscular Disease. Cori Daines, MD Pediatric Pulmonary Medicine University of Arizona. Neuromuscular Disease. Duchenne’s muscular dystrophy Becker’s muscular dystrophy Limb-Girdle muscular dystrophy Spinal muscular atrophy Myotonic dystrophy. Neuromuscular Disease.
1.09k views • 59 slides
Respiratory Protection in Primary Care
Respiratory Protection in Primary Care. Deborah Gold, MPH, CIH [email protected] January, 2010. California Aerosol Transmissible Disease Standard. Became effective August 5, 2009 Applies in most health care environments, including primary care
643 views • 46 slides
204 views • 15 slides
Cultural Competence in Respiratory Care
Cultural Competence in Respiratory Care. Terry S. LeGrand, PhD, RRT Department of Respiratory Care The University of Texas at San Antonio. Why be Culturally Competent?. Many cultures populate our country Vast array of customs, beliefs, practices
307 views • 29 slides
- Subscriptions
- Advanced search

Advanced Search
Bronchiectasis: a case-based approach to investigation and management
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- Figures & Data
- Info & Metrics
Bronchiectasis is a chronic respiratory disease characterised by a syndrome of productive cough and recurrent respiratory infections due to permanent dilatation of the bronchi. Bronchiectasis represents the final common pathway of different disorders, some of which may require specific treatment. Therefore, promptly identifying the aetiology of bronchiectasis is recommended by the European Respiratory Society guidelines. The clinical history and high-resolution computed tomography (HRCT) features can be useful to detect the underlying causes. Despite a strong focus on this aspect of treatment a high proportion of patients remain classified as “idiopathic”. Important underlying conditions that are treatable are frequently not identified for prolonged periods of time.
The European Respiratory Society guidelines for bronchiectasis recommend a minimal bundle of tests for diagnosing the cause of bronchiectasis, consisting of immunoglobulins, testing for allergic bronchopulmonary aspergillosis and full blood count. Other testing is recommended to be conducted based on the clinical history, radiological features and severity of disease. Therefore it is essential to teach clinicians how to recognise the “clinical phenotypes” of bronchiectasis that require specific testing.
This article will present the initial investigation and management of bronchiectasis focussing particularly on the HRCT features and clinical features that allow recognition of specific causes.
Bronchiectasis is a heterogeneous disease with diverse clinical presentation. Careful history, review of radiological features and laboratory testing are required to identify the underlying diagnosis. http://ow.ly/RDF730koTxu
- Introduction
Bronchiectasis is a progressive respiratory disease characterised by permanent dilatation of the bronchi and associated with a clinical syndrome of cough, sputum production and recurrent respiratory infections [ 1 ]. The causes of bronchiectasis are varied with important differences between the presentation and natural history of the disease depending on aetiology.
Bronchiectasis is increasing in prevalence with current rates estimated between 53 and 566 cases per 100 000 inhabitants depending on the population studied [ 2 , 3 ]. These differences in reported prevalence may be due to the long period of neglect and growing awareness or could represent a true rise in prevalence. It should therefore be expected that cases of bronchiectasis will be encountered more frequently by the general physician, as well as the respiratory specialist. Bronchiectasis is a heterogenous disease with many causes and associations. The most commonly associated conditions are shown in table 1 . Although the final clinical syndrome is similar, there are many clinical and radiological features which give clues as to aetiology. The presentation of post-infective bronchiectasis can be very different to the presentation of chronic obstructive pulmonary disease (COPD)-related bronchiectasis and the features of a computed tomography (CT) scan of post-tuberculous bronchiectasis are different to the features seen with nontuberculous mycobacteria (NTM) related disease, for example. Identifying the underlying cause accurately and quickly is a key recommendation of international guidelines, as many causes of bronchiectasis are treatable or have specific prognostic implications ( table 1 ).
- View inline
Aetiologies of bronchiectasis
Our understanding of the pathophysiology of bronchiectasis is limited. The so-called “vicious cycle hypothesis” first proposed in 1986 by C ole [ 4 ] remains central to our understanding. The key components of the disease are chronic inflammation, impaired mucociliary clearance, chronic bronchial infection and structural lung damage. Chronic airways infection, most frequently with Haemophilus influenzae and Pseudomonas aeruginosa , stimulates and sustains lung neutrophilic inflammation and is related with a higher frequency of exacerbations, worse quality of life and increased mortality [ 5 ]. This is particularly the case with P. aeruginosa infection where chronic infection is associated with a three-fold increase in mortality and seven-fold increase in hospitalisation [ 6 ].
Recognised aetiologies include post-infection, COPD, primary ciliary dyskinesia (PCD), allergic bronchopulmonary aspergillosis (ABPA), NTM infections, immune deficiencies and connective tissue diseases [ 7 ]. However, despite extensive testing, up to 53% of patients may have no identifiable cause and the diagnosis of idiopathic bronchiectasis remains common [ 8 ].
The recent European Respiratory Society (ERS) guidelines suggest the following minimum bundle of aetiological tests to perform in adults with a new diagnosis of bronchiectasis: measurement of differential blood count, immunoglobulins (IgA, IgM and IgG) and screening for ABPA (total IgE, specific IgE to Aspergillus , IgG to Aspergillus and eosinophil count). Additional tests may be appropriate in specific clinical features or in patients with severe or rapidly progressive disease. Sputum culture is recommended for monitoring bacterial infections and when NTM infection is suspected [ 9 ]. Standardised tests are important to seek causes of underlying bronchiectasis because they lead to a change in treatment in 7–37% of cases [ 7 , 8 , 10 , 11 ].
Chest high-resolution computed tomography (HRCT) features can be useful to detect the underlying causes. HRCT is now the accepted standard to establish the diagnosis of bronchiectasis [ 1 ]. The prerequisite is the identification of dilation of the airways, seen as an increased ratio between the internal lumen of a bronchus and its immediately adjacent pulmonary artery. The lack of normal tapering, mucus plugging, nodules, bronchial wall thickening, “tree-in-bud” pattern, lung volume loss and mosaicism pattern are all additional features useful to support a diagnosis of bronchiectasis. Furthermore, all these signs can be associated with particular distributions of bronchiectasis and can guide us to a specific cause [ 12 ].
As the ERS guidelines recommend only a small number of tests are performed routinely, it is important that clinicians know how to recognise other treatable causes and “phenotypes”, as listed in table 1 . This article presents examples of clinical phenotypes, integrating history and HRCT features to illustrate the importance of identifying the underlying cause of bronchiectasis and key components of management.
Case 1 is a 42-year-old man. He works as a gardener but has been finding it difficult to maintain his business recently due to recurrent respiratory infections. He has had a long history of respiratory problems starting in early childhood. He thinks he was told that he had asthma and previously used an inhaler but stopped due to it being ineffective. He struggled at school due to frequent absence due to “chest infections”. He is unaware of any neonatal issues but believes that he was born at home without complications and is unsure of any previous tests he has had as he is now estranged from his parents. He believes he has a cousin with a “lung disease”.
He tends to cough most days and has three to four significant chest infections per year. He has often struggled to gain weight. He is married but has not had any children.
His initial screening blood tests did not reveal any abnormalities. His CT scan showed extensive cystic and varicose bronchiectasis affecting all lobes including the upper lobes ( figure 1 ). His sputum culture taken in clinical stability grew P. aeruginosa . No previous cultures are available to determine the duration of this infection. Due to his family history, infertility, severity of disease and young age of onset cystic fibrosis (CF) genetics were performed. His genotype was F508del/R117H, with a sweat chloride of 73 mEq·L −1 . A diagnosis of CF was made.
- Download figure
- Open in new tab
- Download powerpoint
Varicose and cystic bronchiectasis with mucus plugging in upper lobes.
Cystic fibrosis
CF is the most common life-threatening autosomal recessive disease in the USA and Europe [ 13 , 14 ].
CF is a multisystem disorder caused by mutations in the gene that encodes the CF transmembrane conductance regulator (CFTR) protein, a chloride channel expressed in epithelial cells [ 15 ]. More than 2000 CFTR mutations have been identified to date, but only the functional importance of a small number is known to cause the disease [ 16 ].
Clinical manifestations of CF can be very different between patients according to their genotype and the consequent highly variable levels of CFTR dysfunction [ 15 , 17 ].
Bronchiectasis associated with cough, sputum production and recurrent respiratory infections are the hallmark of CF lung disease. An upper lobe predominant distribution of cylindrical, cystic and varicose bronchiectasis associated with airway wall thickening, mucus plugging and parenchymal opacities on a HRCT scan should raise the suspicion of CF disease [ 18 ]. The presence of nasal polyposis and/or chronic rhinosinusitis, recurrent pancreatitis, malabsorption, diabetes, osteoporosis and male infertility are other typical features of CF and the diagnosis of CF should be considered in any adult who presents with these signs and symptoms, especially if they started in childhood.
According to the recent guidelines published by the Cystic Fibrosis Foundation in the USA [ 19 ], CF is diagnosed when an individual has both a clinical presentation of the disease and evidence of biochemical and genetic markers of CFTR dysfunction. If an individual with clinical features of the disease has a concentration of chloride >60 mmol·L −1 at the sweat test or a concentration in the intermediate range (30–59 mmol·L −1 ) but two disease-causing CFTR mutations the diagnosis of CF can be made. If the CFTR genotype is undefined, CFTR physiologic tests, such as nasal potential difference and intestinal current measurement, should be performed.
However, because of widespread CF newborn screening based on the measurement of immunoreactive trypsinogen in blood spots, 55.5–73% of new CF diagnoses in Europe now occur in asymptomatic or minimally symptomatic infants [ 20 – 22 ], so that it has become unusual to diagnose CF in patients with classic symptoms of respiratory disease and emaciation at an advanced age [ 23 ]. Nevertheless, the diagnosis can be challenging or inconclusive in some individuals [ 24 ]. For positive screened individuals with inconclusive CFTR functional and genetic testing the CFTR - related metabolic syndrome definition should be used, whereas for non-screened individuals presenting with monosymptomatic clinical entity associated with CFTR dysfunction that does not fulfil the diagnostic criteria for CF, a diagnosis of CFTR-related disorder should be considered [ 19 ].
Diagnosing CF is an important goal in adults with bronchiectasis. Around 7% of patients with CF are diagnosed as adults [ 23 ]. Patients affected by CF should be referred to a CF specialist centre because CF has a distinct pathophysiology, prognosis and treatment pathway. In many countries, CF patients have more access to respiratory therapies than patients with non-CF bronchiectasis. Furthermore, new CFTR modulator therapies can be provided to patients with specific mutations in order to improve their clinical outcomes.
The presence of a single CFTR mutation in the presence of a normal sweat test is relatively common in bronchiectasis and its clinical significance is uncertain.
The authors' current practice is to screen for CF in all patients presenting with bronchiectasis before the age of 50 years, as in this case, and all patients with bronchiectasis symptoms onset during childhood irrespective of the age of presentation. In addition, the presence of upper lobe disease, Staphylococcus aureus or P. aeruginosa in sputum, or extrapulmonary features such as malabsorption, pancreatitis or infertility should also prompt CF testing irrespective of the age of the patient.
Case 2 is a 45-year-old architect. He has had asthma since childhood. It has generally been well controlled throughout most of his adult life with only one or two exacerbations and no hospital admissions. In recent years he has noticed a decline in his exercise tolerance and an increase in cough which has become productive of purulent sputum with occasional thick/solid components. He has had several significant respiratory exacerbations which have not responded well to standard steroid and antibiotic treatment. One of these episodes was so severe he required emergency hospital admission due to respiratory distress. This improved when he managed to expectorate some very thick sputum. He was noted to have variable pulmonary infiltrates on chest radiographs during these episodes.
He attended a general respiratory clinic. A CT scan showed significant central bronchiectasis ( figure 2 ). He was noted to have a marked eosinophilia on initial blood tests. This prompted Aspergillus serological testing. His total IgE was >2000 IU·mL −1 , his Aspergillus IgE was 750 IU·mL −1 and Aspergillus IgG was 45 IU·mL −1 . A diagnosis of ABPA was made and he was commenced on high-dose oral corticosteroids.
Central tubular bronchiectasis in upper lobes.
Allergic bronchopulmonary aspergillosis
ABPA is an inflammatory disease caused by hypersensitivity to the ubiquitous fungus Aspergillus fumigatus. [ 25 ].
ABPA occurs most commonly in patients with asthma [ 26 ] and CF [ 27 ], but many patients do not have a history of asthma. ABPA is the cause of 1–10% of cases of bronchiectasis [ 8 , 28 , 29 ], but it can also complicate pre-existing bronchiectasis. Most ABPA cases occur in the third and fourth decade without a sex predilection.
Clinically, patients affected by ABPA may present with symptoms such as malaise, weight loss, low-grade fever, cough, purulent sputum containing brownish-black mucus plugs, pleuritic chest pains and haemoptysis [ 30 ].
There is not a single test to diagnose ABPA or a universally recognised set of criteria. Integration of patient's history, clinical, radiological and serological features is used to diagnose ABPA. When ABPA is suspected, total IgE, specific IgE to Aspergillus or Aspergillus skin prick testing, IgG to Aspergillus and eosinophil count should be performed [ 9 ]. Total serum IgE levels >1000 IU·mL −1 are the hallmark of ABPA and total IgE levels are also the most useful test for follow-up [ 30 ]. Caution is recommended in interpreting total IgE levels in patients recently treated with oral corticosteroids as “partially treated” ABPA may result in lower levels. A. fumigatus -specific IgE levels are also elevated and more sensitive than skin-prick test to Aspergillus antigen [ 31 ]. Peripheral eosinophilia and raised IgG antibodies against Aspergillus are also supportive of diagnosis [ 30 ].
HRCT is particularly useful in identifying ABPA as central bronchiectasis is a classical finding, even though peripheral bronchiectasis may occur [ 32 ] . The upper lobes are most frequently affected [ 33 ] but bronchiectasis may be present in all lobes [ 34 ]. Additional findings on HRCT are mucus plugging with “finger-in-glove” appearance, transient consolidation, centrilobular nodules associated with tree-in-bud, atelectasis, mosaicism due to air trapping on expiration and fibrosis in end-stage disease [ 30 ]. In some cases though, ABPA without bronchiectasis can be recognised [ 35 ] . Distinguishing between ABPA diagnosed serologically (ABPA-S) and ABPA with central bronchiectasis (ABPA-CB) may have prognostic implications: ABPA-S may be a more benign phenotype of ABPA, but most experts consider it a precursor of ABPA-CB [ 36 ].
The clinical course of ABPA is variable. There are five recognised stages of ABPA: stage I defines new, active ABPA; stage II is clinical and serological remission; stage III is recurrent active ABPA; stage IV defines patients with chronic, steroid-dependent ABPA; and stage V is end-stage disease with fibrocavitary lesions [ 37 ]. ABPA is important to identify as progressive lung damage occurs rarely once treatment is started [ 36 ].
Many drugs have been tried in the treatment of ABPA, such as: systemic and inhaled corticosteroids with the aim to reduce the inflammatory response; antifungal agents, that decrease the antigen burden and subsequent immune response; and omalizumab, a monoclonal antibody directed against IgE [ 38 ]. The initial treatment for ABPA is usually with oral corticosteroids [ 1 ]. Treatment is typically started at high doses, e.g. 40 or 50 mg daily, with weaning of the dose over several months with monitoring of total IgE and clinical symptoms.
ABPA remission is defined by improvement in symptoms, decrease in total serum IgE level, resolution of radiographic infiltrates and improvement in lung function [ 39 ]. Failure to respond to therapy should prompt consideration of comorbidities or alternative diagnoses. Infective exacerbations of bronchiectasis are associated with cough, wheeze and mucus plugging so that it may be challenging to discern if the primary driver of sputum is bacterial or allergic.
The role of antifungal treatment in ABPA is controversial. A double-blind randomised controlled trial previously demonstrated that treatment response, defined as a reduction of corticosteroid dose of >50%, was more rapid in patients taking a combination of steroids plus itraconazole compared to corticosteroids alone. This study suggests that itraconazole can be used as a steroid sparing agent [ 40 ]. Many clinicians use itraconazole in combination with corticosteroids as initial therapy for ABPA. Evidence for this approach is limited. A recent randomised controlled trial with 131 patients included found a similar rate of response in terms of IgE and exacerbations with initial therapy using prednisolone alone versus itraconazole alone, which does suggest that reducing fungal burden may be important alongside reducing inflammation [ 41 ]. We do not currently advocate treatment with antifungals alone. Concerns with antifungals include liver toxicity, photosensitivity and drug–drug interactions. Patients taking itraconazole should not take proton-pump inhibitors since they require an acidic environment to be absorbed.
Case 3 is a 19-year-old student. He arrived in the UK from Pakistan aged 13 years. He has had respiratory problems since early childhood. His grandparents describe him as a small child with chronic cough since birth, as well as recurrent ear and sinus infections which have led to partial hearing loss. His brother and one of his cousins are similarly affected. His parents are first cousins. Since arriving in the UK he has had two hospital admissions with pneumonia. He has had a provisional diagnosis of asthma due to frequent symptoms even when well, but standard treatment has not been effective.
Examination revealed dextrocardia which was confirmed on radiographs and CT. CT scans also showed minor lingula bronchiectasis ( figure 3 ). He grew H. influenzae on several occasions on sputum culture. Due to his age and family history, he was screened for CF (which was negative) and PCD. His nasal nitric oxide (nNO) was inconclusive and he went on to have a high-speed video analysis (HSVA) examination of nasal epithelial cells. This demonstrated static cilia. Electron microscopy and genetic testing revealed an outer dynein arm defect and biallelic pathogenic mutations in DHAH5 which confirmed the diagnosis of PCD. His sibling was also later diagnosed.
a) Chest radiograph showing dextrocardia. b) High-resolution computed tomography showing cylindrical bronchiectasis in the lingula.
Primary ciliary dyskinesia
PCD is a rare genetic disorder with an estimated prevalence of 1:10 000 [ 42 ]. PCD is caused by recessive autosomal or X-linked mutations in one of more than 35 genes which lead to functional and/or structural defects of cilia [ 43 ]. Motile cilia are specialised structures present in many tissues, so their immotility or ineffective beating results in a systemic disease with heterogeneous features. In upper and lower respiratory airways, failure of motile cilia leads to poor mucociliary clearance, which triggers a vicious cycle of inflammation and infection that leads to chronic rhinosinusitis and otitis media, progressive airway obstruction, bronchiectasis and ultimately respiratory failure [ 44 ]. A history of neonatal respiratory distress is often reported [ 45 ]. Since embryonic nodal cilia can also be defective, ∼50% of patients have situs inversus totalis or heterotaxy. When situs inversus is accompanied by chronic sinusitis and bronchiectasis, this is known as Kartagener's syndrome [ 44 ]. Sperm flagella and cilia of the fallopian tubes share common axonemal structures with motile cilia, so a proportion of PCD-affected males and females are infertile and female patients that are fertile are at a higher risk of complications such as ectopic pregnancy [ 46 ].
The PCD diagnostic pathway is complex and some of its tests are very expensive or require a high level of expertise, so only a few tertiary centres can perform all of them. According to the 2017 ERS PCD guidelines, a diagnostic PCD step-wise approach includes firstly the measurement of nNO and the performance of nasal brushing for the evaluation of ciliary beat frequency and pattern with HSVA. The evaluation of ciliary ultrastructural defects with transmission electron microscopy or genetic testing can be used to confirm the diagnosis. Neither modality is able to detect all cases of PCD, with ∼80% and 70% of specificity, respectively. Therefore, in cases where diagnosis remains inconclusive, repeating the high-speed video microscopy on a new sample or after in vitro culture of the airway epithelium is suggested. Detection of presence or absence of ciliary proteins on ciliated respiratory epithelial cells by immunofluorescence is also increasingly used [ 47 ]. In the ERS bronchiectasis guidelines, testing for PCD is limited to patients with clinical features consistent with the disease (persistent productive cough since childhood, chronic rhinosinusitis, chronic middle ear disease with or without hearing loss, situs anomalies, congenital cardiac defects and a history of neonatal respiratory distress or neonatal intensive care admittance in term infants) [ 9 ]. All these clinical factors are included in the PICADAR score, a simple diagnostic tool to predict whether symptomatic patients have PCD [ 48 ]. PICADAR score and nNO are suitable and easy-to-perform tests in respiratory clinics, whereas further tests should be performed in PCD or tertiary centres with high expertise. Importantly, although nNO is often used as a screening test, it can be normal or inconclusive in some cases of PCD, as in this case. Therefore, where there is a high index of suspicion as in this case, further investigations should be performed irrespective of the nNO result.
HRCT features may be helpful in raising the suspicion of PCD. Bronchiectasis in PCD is predominantly in the middle lobe, lingula and lower lobes, with a central or diffuse distribution. As expected from the underlying pathophysiology of the disease, the severity of bronchiectasis increases with age, whereas data regarding the correlation between HRCT features and pulmonary function are conflicting [ 49 , 50 ] . Besides lung parenchymal alterations, situs inversus, heterotaxy and congenital heart disease could support the suspicion of PCD. Pectus excavatum is identified in 9% of cases [ 49 ].
Investigation and diagnosis of PCD is an important goal because it is a multi-system disease which benefits from a specific and multidisciplinary team approach, including genetic and reproductive counselling, in a PCD referral centre [ 1 ]. Although airway clearance is an important aspect of the management of all bronchiectasis patients , it is particularly emphasised in the management of patients with PCD. The importance of making the diagnosis is emphasised by data showing worse lung function and higher rates of P. aeruginosa infection the later patients are diagnosed [ 51 – 55 ].
Case 4 is a 77-year-old retired librarian. She has had cough for many years, although she has only sought medical attention recently as she has developed more systemic symptoms. Her new symptoms are fatigue, weight loss and fever. A chest CT scan was performed looking for a possible occult malignancy and bronchiectasis was found ( figure 4 ).
Cylindrical bronchiectasis and tree-in-bud pattern in lower lobes and middle lobe.
Following the CT scan features of cylindrical bronchiectasis and tree-in-bud pattern in middle and lower lobes, she attended a respiratory clinic. A sputum sample was sent and a positive acid-alcohol-fast bacilli staining was found. After 4 weeks Mycobacterium avium complex (MAC) grew on the culture. Several subsequent cultures were also positive. As NTM can complicate pre-existing bronchiectasis as well as being a cause of bronchiectasis, further testing for immunodeficiency, ABPA and other causes was performed. No abnormalities were found. In view of the clinical history, radiological findings and absence of an alternative cause, a diagnosis of bronchiectasis due to NTM lung disease was made.
Nontuberculous mycobacteria
NTM are ubiquitous organisms in the environment and can be inhaled or ingested from water, soil and dust with different consequences according to individual and organism characteristics.
The exact prevalence of NTM disease is difficult to obtain because reporting these infections is not mandatory in many countries and discriminating between colonisation and active infection can be challenging. Certainly, the recovery of NTM from the respiratory tract is increasing as a result of a real growing prevalence of pulmonary disease due to these organisms [ 56 ], but also because of improving microbiological techniques and the increasing attention to this topic. In a systematic review, the overall prevalence of NTM in patients with bronchiectasis was 9.3%, with higher rates in larger cohorts and in Asian populations [ 57 ]. The most frequent species is MAC (which includes M. intracellulare , M. avium and M. chimaera ), with a percentage up to 80% of all NTM lung disease cases [ 58 , 59 ] whereas the isolation of other species, e.g. M. abscessus , M. kansasii , M. chelonae and M. fortuitum , varies from study to study.
The outcome of respiratory exposure to NTM, colonisation or pulmonary disease, probably depends on a complex relationship between host-related factors (genetics, immune status and lung damage), exposure-related factors (duration, number of organisms, inhaled or ingested particle size) and organism-related factors (capability of mycobacteria to cause pulmonary disease, e.g. M. malmoense has more pathogenicity than M. chelonae [ 60 ]). NTM can be both a cause and a consequence of bronchiectasis. NTM can cause bronchiectasis by destroying the bronchial wall and bronchiectasis can predispose to NTM colonisation/disease due to an impairment of bronchial anatomy and local host defence [ 61 , 62 ].
The diagnosis of NTM pulmonary disease is based on the presence of clinical criteria (respiratory symptoms consistent with the diagnosis), radiological features consistent with NTM, exclusion of other diagnoses and microbiological criteria (a positive culture from one bronchial lavage, at least two NTM-positive sputum cultures or a lung biopsy with mycobacterial histopathologic features plus a NTM-positive culture) [ 63 ]. NTM pulmonary disease is often challenging to diagnose, due to the presence of organisms in the environment and the consequent possibility of sample contamination and the wide spectrum of clinical manifestations. If a diagnosis of NTM pulmonary disease is difficult in healthy individuals, it is even more difficult in bronchiectasis patients, where distinguishing between bronchiectasis-related and NTM-related symptoms can be challenging. According to the ERS guidelines, three sequential daily sputum cultures for mycobacteria or a single bronchoalveolar lavage should be considered in patients with persistent fever, weight loss, haemoptysis, symptoms non-responsive to standard therapy or rapid clinical deterioration [ 9 ]. Up to 50% of patients will not produce sputum spontaneously and such patients should be investigated by bronchoscopy or sputum induction.
HRCT features should also be investigated when NTM pulmonary disease is suspected. Two major radiological patterns are related to NTM infection: the nodular/bronchiectatic and fibrocavitary forms. The first one is characterised by multiple small centrilobular nodules and cylindrical bronchiectasis, especially localised in middle lobe and lingula. [ 64 ]. This pattern is frequently associated with MAC infection [ 65 ] and with the “Lady Windermere syndrome”: women with elderly age, low body mass index and chronic cough [ 66 ]. The fibrocavitary form is characterised by increased opacity areas and cavitations, usually in the upper lobes, with or without calcifications. In addition, apical pleural thickening and fibrosis with volume loss can be found. Pleural effusion, adenopathies and lower lobes involvement are uncommon [ 67 ]. This pattern is frequently associated with M. abscessus , M. chelonae and M. kansasii infections [ 65 ] . The underlying pulmonary disease in these patients is often advanced COPD.
Once a diagnosis of NTM disease is established, the institution of therapy is not always mandatory. Since NTM treatment is usually prolonged and based on multiple drugs with significant side effects, a careful evaluation of risks and benefits should be made. Considering NTM species, patient's conditions, radiological pattern and disease severity is crucial in the decision-making process. In the case of NTM treatment, patients should be closely monitored with visits, sputum cultures, lung function and blood tests to assess the response to therapy and possible side effects. Follow-up should also be prolonged after treatment since relapse or new infections are possible and the underlying bronchiectasis requires long-term management. In case of no treatment, patients should be monitored to evaluate disease progression.
This patient was treated with rifampicin 600 mg daily, ethambutol 15 mg·kg −1 daily and clarithromycin 500 mg twice daily. This, sometimes with the addition of intravenous amikacin for 3 months or nebulised amikacin, is the regimen recommended for severe MAC pulmonary disease where acid-fast bacilli is smear positive or there are severe symptoms of systemic illness or cavitation. Intermittent therapy three times per week (rifampicin 600 mg three times per week, ethambutol 25 mg·kg −1 three times per week and azithromycin or clarithromycin three times per week) are recommended in patients with mild disease who are smear negative with the absence of cavitation and no systemic symptoms. Patients who have intolerance to drugs or refractory disease should be referred to an NTM speciality clinic.
A 66-year-old woman with established idiopathic bronchiectasis has had three to four exacerbations per year for the past 3 years despite performing daily chest physiotherapy. Testing for NTM, ABPA and other complications were negative, but sputum shows persistent infection with P. aeruginosa . She produces large volumes of sputum daily despite performing the active cycle of breathing technique.
This is one of the most common presentations of bronchiectasis, as exacerbations are one of the most important manifestations of bronchiectasis and P. aeruginosa is the most frequent organism in severe bronchiectasis worldwide. This patient could present any of the CT scans shown above ( figure 5 ).
Different radiological “phenotypes” of bronchiectasis. a) Tubular bronchiectasis in lower lobes, b) varicose bronchiectasis in lower lobes, c) cystic bronchiectasis in right lower lobe, d) cystic bronchiectasis with tree-in-bud pattern and mucus plugging in lower lobes (cavitation in right lower lobe), e) mucus plugging and tree-in-bud pattern in lower lobes, f) varicose bronchiectasis in upper lobes and lingula.
Cylindrical bronchiectasis is the most common morphological pattern identified on CT scans [ 68 ] and is recognised by an abnormal dilatation of bronchus with uniform calibre and lack of tapering at the periphery, producing a tramline (tram track sign) ( figure 5a ). Varicose bronchiectasis has no regular form or size, with distortion and irregular bulging ( figure 5b ), whereas cystic bronchiectasis is a saccular dilatation with ballooned cutline that can be traced almost to the pleura ( figure 5c ). In the context of bronchiectasis cavitation can also be seen, especially in NTM pulmonary disease or previous M. tuberculosis infection ( figure 5d ). Another frequent finding is mucus plugging, the presence of mucoid secretions in peripheral airways ( figure 5e ), that can produce V- and Y-opacities, the so-called tree-in-bud pattern ( figures 5d and e). The distribution and extension of bronchiectasis are also key components in bronchiectasis evaluation. For instance, localised bronchiectasis, especially in a single lobe, should raise the suspicion of obstructive or post-infective bronchiectasis ( figure 5f ).
Management of frequent exacerbations
Frequent exacerbations should prompt a review of all aspects of management including reviewing current airway clearance regime, repeat sputum microbiology and repeat testing for NTM, ABPA and ensuring the all possible treatable causes and comorbidities have been identified.
Intensification of treatment should address all aspects of the vicious cycle including targeting airway infection, airway clearance and airway structural damage. Interventions that have been shown to reduce exacerbations and improve quality of life in either controlled trials or observational studies include macrolides [ 69 – 71 ], inhaled antibiotics [ 72 – 74 ], mucoactive drugs ( e.g. hypertonic saline) [ 75 , 76 ], airway clearance [ 77 , 78 ] and pulmonary rehabilitation [ 79 , 80 ]. All of these interventions were recommended in appropriate patients in the 2017 ERS guidelines [ 9 ].
The first-line recommendation for P. aeruginosa with frequent exacerbations is an inhaled antibiotic [ 9 ] and this patient was commenced on twice daily colistin treatment. Airway clearance was optimised through an appointment with a respiratory physiotherapy and nebulised saline was added to her daily regimen. She was referred to and completed pulmonary rehabilitation. These interventions resulted in a reduction of her exacerbation frequency and an improvement in quality of life. Important issues with inhaled antibiotics include an approximately 10% risk of bronchospasm [ 72 ] and the burden of administering a daily nebulised therapy that takes some time. Antibiotic resistance is also a theoretical risk with any long-term antimicrobial treatment. Treatment of these patients with multiple nebulised therapies plus airway clearance results in a large burden of treatment and increases the risk of non-adherence. Macrolides are a reasonable alternative with a lower treatment burden but have less evidence in the context of chronic P. aeruginosa infection [ 69 – 71 ]. Furthermore, it is important to exclude NTM prior to commencing macrolide therapy to avoid inducing resistance. A detailed discussion of management of bronchiectasis is beyond the scope of this review. Further information on treatment including antibiotic therapy, thoracic surgery, physiotherapy management and treatment of acute exacerbations can be found in the 2017 ERS guidelines [ 9 ].
Bronchiectasis is no longer a neglected disease. Interest and awareness are increasing in scientific and patient communities. Chest physiotherapy and antibiotic treatment when an exacerbation occurs remain the cornerstone of bronchiectasis therapy. Discovering the underlying aetiology of bronchiectasis could make a real difference in the management and prognosis of patients and could delay the progression of lung involvement when treated. Since routine testing of all patients for all possible underlying disorders has not been shown to be cost-effective, current guidelines recommend using clinical judgement and recognition of patient phenotypes to guide testing for disorders such as CF, PCD, NTM and others. Therefore, physicians should be familiar with the key clinical history and CT features that can raise the suspicion of a specific cause of bronchiectasis and lead to improved treatment.
Provenance: Commissioned article, peer reviewed.
Conflict of interest: J.D. Chalmers reports grants and personal fees (for COPD) from GlaxoSmithKline, Boehringer Ingelheim and Pfizer, grants (for COPD) from AstraZeneca, grants and personal fees (for research into bronchiectasis) from Bayer Healthcare and Grifols, and personal fees (for consultancy) from Napp, outside the submitted work.
- Received February 23, 2018.
- Accepted June 4, 2018.
- Copyright ©ERS 2018.
ERR articles are open access and distributed under the terms of the Creative Commons Attribution Non-Commercial Licence 4.0.
- Pasteur MC ,
- Ringshausen FC ,
- de Roux A ,
- Pletz MW , et al.
- Millett ER ,
- Joshi M , et al.
- McDonnell MJ ,
- Aliberti S ,
- Goeminne PC , et al.
- Abo-Leyah H , et al.
- Shoemark A ,
- Ozerovitch L ,
- Helliwell SM ,
- Houghton SJ , et al.
- Polverino E ,
- Goeminne PC ,
- McDonnell MJ , et al.
- Worthy SA , et al.
- Chalmers JD ,
- Cartier Y ,
- Kavanagh PV ,
- Johkoh T , et al.
- ↵ Cystic Fibrosis Foundation . Understanding changes in life expectancy . www.cff.org/Research/Researcher-Resources/Patient-Registry/2016-Patient-Registry-Reports/ Date last accessed: June 19 2018.
- O'Sullivan BP ,
- Freedman SD
- ↵ CFTR2 . https://cftr2.org/ Date last accessed: June 19 2018.
- Konstan MW ,
- Schluchter MD , et al.
- Hansell DM ,
- Strickland B
- Farrell PM ,
- Ren CL , et al.
- ↵ Cystic Fibrosis Trust . Reporting and resources . www.cysticfibrosis.org.uk/the-work-we-do/uk-cf-registry/reporting-and-resources
- Registro Italiano Fibrosi Cistica . www.registroitalianofibrosicistica.it/ Date last accessed: June 19 2018.
- ↵ Cystic Fibrosis Data Network . Cystic Fibrosis Reports: France . www.cysticfibrosisdata.org/ReportsFrance.html
- Bienvenu T , et al.
- Petren K , et al.
- Garrett J ,
- Milne D , et al.
- Stevens DA ,
- Kurup VP , et al.
- Paquin R , et al.
- Patterson K ,
- Patterson KC ,
- Davies ML ,
- Cowan MD , et al.
- Goodman LR ,
- Gurney JW , et al.
- Mitchell TA ,
- Hamilos DL ,
- Lynch DA , et al.
- Patterson R ,
- Greenberger PA ,
- Halwig JM , et al.
- Miller TP ,
- Roberts M , et al.
- Radin RC , et al.
- Agarwal R ,
- Aggarwal AN ,
- Sehgal IS , et al.
- Schwartz HJ ,
- Lee JY , et al.
- Dhooria S ,
- Singh Sehgal I , et al.
- Kuehni CE ,
- Barbato A ,
- Frischer T ,
- Kuehni CE , et al.
- Sannuti A , et al.
- Fitzgerald DA ,
- Jaffe A , et al.
- Vanaken GJ ,
- Bassinet L ,
- Boon M , et al.
- Collins SA , et al.
- Dimitrov BD ,
- Kennedy MP ,
- Leigh MW , et al.
- Irving SJ ,
- Davies G , et al.
- Marthin JK ,
- Petersen N ,
- Skovgaard LT , et al.
- Ellerman A ,
- MacNeill SJ , et al.
- Gremmo ML ,
- Shapiro AJ ,
- Zariwala MA ,
- Ferkol T , et al.
- Kendall BA ,
- Winthrop KL
- Xiao H , et al.
- Mirsaeidi M ,
- Ericsoussi B , et al.
- Wickremasinghe M ,
- Griffith DE ,
- Bonaiti G ,
- Marruchella A , et al.
- Aksamit T ,
- Brown-Elliott BA , et al.
- Erasmus JJ ,
- McAdams HP ,
- Farrell MA , et al.
- Hsu CL , et al.
- Kwon OJ , et al.
- Carr DH , et al.
- Jayaram L ,
- Karalus N , et al.
- Serisier DJ ,
- Martin ML ,
- McGuckin MA , et al.
- Altenburg J ,
- de Graaff CS ,
- Stienstra Y , et al.
- Haworth CS ,
- Foweraker JE ,
- Wilkinson P , et al.
- Murray MP ,
- Doherty CJ , et al.
- De Soyza A , et al.
- Kellett F ,
- Barker AF , et al.
- Pentland JL ,
- Nicolini A ,
- Cardini F ,
- Landucci N , et al.
- Cecins N , et al.
- Adamo D , et al.

- Table of Contents
- Index by author
Thank you for your interest in spreading the word on European Respiratory Society .
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- CF and non-CF bronchiectasis
- Tweet Widget
- Facebook Like
- Google Plus One
More in this TOC Section
- Protecting healthcare workers from SARS-COV-2 infections
- A European regulatory perspective on cystic fibrosis
Related Articles

COPD Case Study: Patient Diagnosis and Treatment (2024)
by John Landry, BS, RRT | Updated: May 16, 2024
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that affects millions of people around the world. It is primarily caused by smoking and is characterized by a persistent obstruction of airflow that worsens over time.
COPD can lead to a range of symptoms, including coughing, wheezing, shortness of breath, and chest tightness, which can significantly impact a person’s quality of life.
This case study will review the diagnosis and treatment of an adult patient who presented with signs and symptoms of this condition.
25+ RRT Cheat Sheets and Quizzes
Get access to 25+ premium quizzes, mini-courses, and downloadable cheat sheets for FREE.
COPD Clinical Scenario
A 56-year-old male patient is in the ER with increased work of breathing. He felt mildly short of breath after waking this morning but became extremely dyspneic after climbing a few flights of stairs. He is even too short of breath to finish full sentences. His wife is present in the room and revealed that the patient has a history of liver failure, is allergic to penicillin, and has a 15-pack-year smoking history. She also stated that he builds cabinets for a living and is constantly required to work around a lot of fine dust and debris.

Physical Findings
On physical examination, the patient showed the following signs and symptoms:
- His pupils are equal and reactive to light.
- He is alert and oriented.
- He is breathing through pursed lips.
- His trachea is positioned in the midline, and no jugular venous distention is present.
Vital Signs
- Heart rate: 92 beats/min
- Respiratory rate: 22 breaths/min
Chest Assessment
- He has a larger-than-normal anterior-posterior chest diameter.
- He demonstrates bilateral chest expansion.
- He demonstrates a prolonged expiratory phase and diminished breath sounds during auscultation.
- He is showing signs of subcostal retractions.
- Chest palpation reveals no tactile fremitus.
- Chest percussion reveals increased resonance.
- His abdomen is soft and tender.
- No distention is present.
Extremities
- His capillary refill time is two seconds.
- Digital clubbing is present in his fingertips.
- There are no signs of pedal edema.
- His skin appears to have a yellow tint.
Lab and Radiology Results
- ABG results: pH 7.35 mmHg, PaCO2 59 mmHg, HCO3 30 mEq/L, and PaO2 64 mmHg.
- Chest x-ray: Flat diaphragm, increased retrosternal space, dark lung fields, slight hypertrophy of the right ventricle, and a narrow heart.
- Blood work: RBC 6.5 mill/m3, Hb 19 g/100 mL, and Hct 57%.
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD) .
The key findings that point to this diagnosis include:
- Barrel chest
- A long expiratory time
- Diminished breath sounds
- Use of accessory muscles while breathing
- Digital clubbing
- Pursed lip breathing
- History of smoking
- Exposure to dust from work
What Findings are Relevant to the Patient’s COPD Diagnosis?
The patient’s chest x-ray showed classic signs of chronic COPD, which include hyperexpansion, dark lung fields, and a narrow heart.
This patient does not have a history of cor pulmonale ; however, the findings revealed hypertrophy of the right ventricle. This is something that should be further investigated as right-sided heart failure is common in patients with COPD.
The lab values that suggest the patient has COPD include increased RBC, Hct, and Hb levels, which are signs of chronic hypoxemia.
Furthermore, the patient’s ABG results indicate COPD is present because the interpretation reveals compensated respiratory acidosis with mild hypoxemia. Compensated blood gases indicate an issue that has been present for an extended period of time.
What Tests Could Further Support This Diagnosis?
A series of pulmonary function tests (PFT) would be useful for assessing the patient’s lung volumes and capacities. This would help confirm the diagnosis of COPD and inform you of the severity.
Note: COPD patients typically have an FEV1/FVC ratio of < 70%, with an FEV1 that is < 80%.
The initial treatment for this patient should involve the administration of low-flow oxygen to treat or prevent hypoxemia .
It’s acceptable to start with a nasal cannula at 1-2 L/min. However, it’s often recommended to use an air-entrainment mask on COPD patients in order to provide an exact FiO2.
Either way, you should start with the lowest possible FiO2 that can maintain adequate oxygenation and titrate based on the patient’s response.
Example: Let’s say you start the patient with an FiO2 of 28% via air-entrainment mask but increase it to 32% due to no improvement. The SpO2 originally was 84% but now has decreased to 80%, and his retractions are worsening. This patient is sitting in the tripod position and continues to demonstrate pursed-lip breathing. Another blood gas was collected, and the results show a PaCO2 of 65 mmHg and a PaO2 of 59 mmHg.
What Do You Recommend?
The patient has an increased work of breathing, and their condition is clearly getting worse. The latest ABG results confirmed this with an increased PaCO2 and a PaO2 that is decreasing.
This indicates that the patient needs further assistance with both ventilation and oxygenation .
Note: In general, mechanical ventilation should be avoided in patients with COPD (if possible) because they are often difficult to wean from the machine.
Therefore, at this time, the most appropriate treatment method is noninvasive ventilation (e.g., BiPAP).
Initial BiPAP Settings
In general, the most commonly recommended initial BiPAP settings for an adult patient include this following:
- IPAP: 8–12 cmH2O
- EPAP: 5–8 cmH2O
- Rate: 10–12 breaths/min
- FiO2: Whatever they were previously on
For example, let’s say you initiate BiPAP with an IPAP of 10 cmH20, an EPAP of 5 cmH2O, a rate of 12, and an FiO2 of 32% (since that is what he was previously getting).
After 30 minutes on the machine, the physician requested another ABG to be drawn, which revealed acute respiratory acidosis with mild hypoxemia.
What Adjustments to BiPAP Settings Would You Recommend?
The latest ABG results indicate that two parameters must be corrected:
- Increased PaCO2
- Decreased PaO2
You can address the PaO2 by increasing either the FiO2 or EPAP setting. EPAP functions as PEEP, which is effective in increasing oxygenation.
The PaCO2 can be lowered by increasing the IPAP setting. By doing so, it helps to increase the patient’s tidal volume, which increased their expired CO2.
Note: In general, when making adjustments to a patient’s BiPAP settings, it’s acceptable to increase the pressure in increments of 2 cmH2O and the FiO2 setting in 5% increments.
Oxygenation
To improve the patient’s oxygenation , you can increase the EPAP setting to 7 cmH2O. This would decrease the pressure support by 2 cmH2O because it’s essentially the difference between the IPAP and EPAP.
Therefore, if you increase the EPAP, you must also increase the IPAP by the same amount to maintain the same pressure support level.
Ventilation
However, this patient also has an increased PaCO2 , which means that you must increase the IPAP setting to blow off more CO2. Therefore, you can adjust the pressure settings on the machine as follows:
- IPAP: 14 cmH2O
- EPAP: 7 cmH2O
After making these changes and performing an assessment , you can see that the patient’s condition is improving.
Two days later, the patient has been successfully weaned off the BiPAP machine and no longer needs oxygen support. He is now ready to be discharged.
The doctor wants you to recommend home therapy and treatment modalities that could benefit this patient.
What Home Therapy Would You Recommend?
You can recommend home oxygen therapy if the patient’s PaO2 drops below 55 mmHg or their SpO2 drops below 88% more than twice in a three-week period.
Remember: You must use a conservative approach when administering oxygen to a patient with COPD.
Pharmacology
You may also consider the following pharmacological agents:
- Short-acting bronchodilators (e.g., Albuterol)
- Long-acting bronchodilators (e.g., Formoterol)
- Anticholinergic agents (e.g., Ipratropium bromide)
- Inhaled corticosteroids (e.g., Budesonide)
- Methylxanthine agents (e.g., Theophylline)
In addition, education on smoking cessation is also important for patients who smoke. Nicotine replacement therapy may also be indicated.
In some cases, bronchial hygiene therapy should be recommended to help with secretion clearance (e.g., positive expiratory pressure (PEP) therapy).
It’s also important to instruct the patient to stay active, maintain a healthy diet, avoid infections, and get an annual flu vaccine. Lastly, some COPD patients may benefit from cardiopulmonary rehabilitation .
By taking all of these factors into consideration, you can better manage this patient’s COPD and improve their quality of life.
Final Thoughts
There are two key points to remember when treating a patient with COPD. First, you must always be mindful of the amount of oxygen being delivered to keep the FiO2 as low as possible.
Second, you should use noninvasive ventilation, if possible, before performing intubation and conventional mechanical ventilation . Too much oxygen can knock out the patient’s drive to breathe, and once intubated, these patients can be difficult to wean from the ventilator .
Furthermore, once the patient is ready to be discharged, you must ensure that you are sending them home with the proper medications and home treatments to avoid readmission.

Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
- Faarc, Kacmarek Robert PhD Rrt, et al. Egan’s Fundamentals of Respiratory Care. 12th ed., Mosby, 2020.
- Chang, David. Clinical Application of Mechanical Ventilation . 4th ed., Cengage Learning, 2013.
- Rrt, Cairo J. PhD. Pilbeam’s Mechanical Ventilation: Physiological and Clinical Applications. 7th ed., Mosby, 2019.
- Faarc, Gardenhire Douglas EdD Rrt-Nps. Rau’s Respiratory Care Pharmacology. 10th ed., Mosby, 2019.
- Faarc, Heuer Al PhD Mba Rrt Rpft. Wilkins’ Clinical Assessment in Respiratory Care. 8th ed., Mosby, 2017.
- Rrt, Des Terry Jardins MEd, and Burton George Md Facp Fccp Faarc. Clinical Manifestations and Assessment of Respiratory Disease. 8th ed., Mosby, 2019.
Recommended Reading
How to prepare for the clinical simulations exam (cse), faqs about the clinical simulation exam (cse), 7+ mistakes to avoid on the clinical simulation exam (cse), copd exacerbation: chronic obstructive pulmonary disease, epiglottitis scenario: clinical simulation exam (practice problem), guillain barré syndrome case study: clinical simulation scenario, drugs and medications to avoid if you have copd, the pros and cons of the zephyr valve procedure, the 50+ diseases to learn for the clinical sims exam (cse).

- Al-Ansari K, Sakran M, Davidson BL, El Sayyed R, Mahjoub H, Ibrahim K. Nebulized 5% or 3% hypertonic or 0.9% saline for treating acute bronchiolitis in infants. J Pediatrics. 2010;157:630-634.
- Gadomski AM, Brower M. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2010;12CD001266.
- Hartling L, Fernandes RM, Bialy L, et al. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ. 2011;342:d1714.
- Martinón-Torres F, Rodríguez-Núñez A, Martinón-Sánchez JM. Nasal continuous positive airway pressure with heliox versus air oxygen in infants with acute bronchiolitis: a crossover study. Pediatrics. 2007;121:e1190-e1195.
- Liet JM, Ducruet T, Gupta V, Cambonie G. Heliox inhalation therapy for bronchiolitis in infants. Cochrane Database Syst Rev. 2010;4:CD006915.
- Ermers MJ, Rovers MM, van Woensel JB, Kimpen JL, Bont LJ; RSV Corticosteroid Study Group. The effect of high dose inhaled corticosteroids on wheeze in infants after respiratory syncytial virus infection: randomised double blind placebo controlled trial. BMJ. 2009;338:b897.
- Committee on Infectious Disease. From the American Academy of Pediatrics: Policy statement -- modified recommendations for use of palivizumab for prevention of respiratory syncytial virus infections. Pediatrics. 2009;124:1694-1701. Abstract
Faculty and Disclosures
NAPNAP Disclaimer Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any medications, diagnostic procedures, or treatments discussed in this publication should not be used by clinicians or other health care professionals without first evaluating their patients' conditions, considering possible contraindications or risks, reviewing any applicable manufacturer's product information, and comparing any therapeutic approach with the recommendations of other authorities.

Respiratory Syncytial Virus Bronchiolitis: A Case Study
View abbreviations used in this activity.
Case Presentation
"JV" is a previously healthy, 4-month-old boy who presented to the pediatric nurse practitioner (PNP) at the emergency department (ED) with rhinorrhea and tachypnea for the past 4 days. A fever that developed during the night prompted his mother to bring him to the ED. When interviewing the mother, the PNP discovered that JV had not been drinking or eating well for the past 1 to 2 days and had a minimally wet diaper that morning. He has had no vomiting or diarrhea. He has had no cough, but his mother reported that when he breathes, he sounds “funny” and his chest looks funny. He has been recently exposed to other sick children at his daycare center.
In reviewing JV's general wellness, the PNP discovered that he was born at 34 weeks and 5 days prematurely. His birth weight was 2.6 kg (5.73 lb). He was hospitalized in the special care nursery for 1 week with an oxygen requirement for several days. He was discharged home with no medications or other therapies. He usually consumes 30 ounces of breastmilk/day. He usually has 4 to 6 wet diapers per day; his stools are brown and he has soft stool every day. He rolls over from front to back. His height, weight, and head circumference are all at the 50 th percentile. His immunizations are up to date to 4 months, and he has not received immunoprophylaxis with palivizumab.
JV lives with his married parents, a 4-year-old sister, and a pet dog in an apartment. He and his sister attend daycare 5 days/week. There are no smokers at home, although the neighbors smoke. There is a family history of asthma in the mother.
JV undergoes a physical examination by the PNP (Table).
Table. Physical Examination Findings
| , 91% on room air |
Based on the examination findings, the PNP orders oxygen 2 L per nasal cannula to treat the desaturation, placement of a peripheral intravenous catheter followed by a fluid bolus for dehydration, albuterol via nebulizer for the wheezing, and a diagnostic respiratory viral panel. After the fluid bolus, the infant's physical examination findings are unchanged, and the bolus is repeated with improvement. The oxygen brings his saturations up to 93%. His wheezing is unchanged, but the work of breathing appears slightly improved after the albuterol nebulizer treatment.
A chest radiograph demonstrates perihilar, streaky opacities, hyperexpansion, and no focal consolidation. The decision is made to admit JV to an inpatient unit with the diagnosis of bronchiolitis. While awaiting a bed on the inpatient unit, JV develops an increased oxygen requirement and is transitioned to face mask oxygen at a fraction of inspired oxygen of 0.35.
JV is transferred to the ward and is evaluated by the provider team. He is found to have moderate work of breathing, poor aeration, and wheezing. The team discusses using a bronchodilator to improve his wheezing. Information from the emergency department (ED) is reviewed and it is discovered that JV's wheezing did not improve with the albuterol therapy. A racemic epinephrine nebulizer treatment is given instead, with limited improvement of his condition. At this time, the results of the respiratory viral panel are available and indicate that JV has respiratory syncytial virus (RSV) infection as the cause of his bronchiolitis.
JV's therapeutic plan is as follows: intravenous fluids for hydration, nothing per mouth, oxygen support, cardiac and respiratory monitoring, ventilation monitoring with a noninvasive device, antipyretics for fever, and isolation to decrease the risk of spreading the RSV infection.
Approximately 24 hours after admission (day 5 of illness), JV experiences increases in his respiratory rate (74 breaths per minute), pulse (182 beats per minute), work of breathing, and a fever (39.4 degrees C [102.92 degrees F]). He is given an antipyretic. After 1 hour, his fever persists and his work of breathing, respiratory rate and pulse remain elevated. Now, his oxygen saturation has fallen to 90%. His supplemental oxygen is increased and a call is made to the rapid response team to assess him.
On arrival of the rapid response team, JV is lethargic with severe work of breathing and oxygen desaturation of 88%. His supplemental oxygen is increased. His lung examination demonstrates wheezing with poor aeration. A hypertonic saline nebulizer treatment is given, with some improvement in his distress.
A decision was made to transfer JV to the pediatric intensive care unit (PICU), where he was quickly connected to the cardiorespiratory monitor, pulse oximetry, and ventilation measurement device. His arterial carbon dioxide level was 54 mm Hg. He was placed on continuous positive airway pressure (CPAP) via a nasal mask at 5 cm H 2 O pressure. Approximately 30 minutes later, he remained tachypneic with severe work of breathing; the CPAP was increased to 8 cm H 2 O pressure and a helium-oxygen (heliox) gas mixture was added.
Discussion: Managing Bronchiolitis
In 2010, Al-Ansari and colleagues [1] studied the effectiveness of hypertonic saline (5% and 3%) compared with normal saline for the treatment of bronchiolitis in infants. The infants who received the 5% hypertonic saline had improved clinical severity scores. However, there was no impact on length of hospital stay. A systematic analysis of bronchodilators in the treatment of bronchiolitis in infants found no benefit, although some of the trials included in this analysis demonstrated an improvement in clinical severity scores. [2] Subsequently, a meta-analysis by Hartling and colleagues [3] demonstrated that epinephrine with or without corticosteroids had a positive impact on clinical severity score but not on length of stay.
The use of nasal CPAP combined with air or heliox delivery in infants and toddlers with bronchiolitis was studied by Martinón-Torres and colleagues. [4] They found that the use of CPAP with air decreased clinical severity scores and that there was additional improvement when heliox was used instead of air. A systematic review found that clinical severity scores were improved with the use of heliox in infants with bronchiolitis. [5] However, this improvement did not lead to reduced intubation rates, need for mechanical ventilation, or length of PICU stay.
Case Presentation, Continued
Because of the severity of JV's illness, the provider team in the PICU discussed the possibility of corticosteroids. A review of the literature revealed conflicting evidence for the use of corticosteroids and that corticosteroids have not been shown to decrease hospitalization in infants with RSV bronchiolitis. In addition, a trial of inhaled corticosteroids in infants who had had RSV bronchiolitis found no difference in wheezing 3 months posthospitalization. [6]
JV continued to require CPAP with heliox for several days and then began to improve. He responded to the nebulized hypertonic saline that he had received for several days and was able to tolerate enteral feeds by nasogastric tube. He was weaned from his supportive therapies and was transitioned to a standard nasal cannula on PICU day 4. On PICU day 5, he was transferred to the ward. He was weaned from supplemental oxygen and was prepared for discharge home with no therapies on hospital day 8.
Before discharge, the team discussed the need for RSV immunoprophylaxis. According to the American Academy of Pediatrics revised guidelines, JV should have had RSV immunoprophylaxis initiated at birth before his discharge from the hospital. [7] He met the age criteria (32 weeks 0 days to 34 weeks 6 days) with the risk factors of living with a sibling younger than 5 years and attending daycare. [7] The team contacted JV's primary care provider, gave a summary of his hospitalization, and requested that RSV immunoprophylaxis be considered for JV, henceforth.
Respiratory syncytial virus bronchiolitis is a common pediatric illness with thousands of children each year requiring hospitalization secondary to severe illness. While many of affected children never require hospitalization, some are sick enough to be hospitalized in the intensive care unit. The children requiring intensive care are typically young infants and those with comorbid conditions. While these children can be severely ill and require intubation and mechanical ventilation, most of the children recover and very few succumb to the disease.
Supported by an independent educational grant from MedImmune Inc.
- Abbreviations
The material presented here does not necessarily reflect the views of Medscape, LLC, or companies that support educational programming on medscape.org. These materials may discuss therapeutic products that have not been approved by the US Food and Drug Administration and off-label uses of approved products. A qualified healthcare professional should be consulted before using any therapeutic product discussed. Readers should verify all information and data before treating patients or employing any therapies described in this educational activity.
Medscape Education © 2012 Medscape, LLC

Quick Search

| , Tayfun Caliskan, Kadir Cano�lu, �zge At��, Mustafa �ark�� | | | ||
| , Gauri Gadge, Sweta Chourasia, Parimal Deshpande, Swapnil Bakamwar | | ||
| Esra Arslan Aksu, , O�uz Uzun | | ||
| , Fatma Tokgoz Akyil, Neslihan Fener | | ||
| , Ege G�le� Balbay, Mustafa Bo�an, Ali Can Kara | | ||
| , Mustafa �olak, Ali Karak�l��, Zafer Erol, Nurhan Sarioglu | | | ||
| Nalan Kozac�, , Tu��e Er�ahin, B��ra Ta�k�ran | | ||
| | | | ||
| Nurhan Atilla, Burcu Akk�k, Fulsen Bozku�, | | --> | ||
| | | ||
This site is intended for health professionals only

- Newsletter sign up
- Nursing in Practice 365
CPD: Case by case – measles and whooping cough

- The characteristic presenting symptoms of measles and whooping cough in children and adults, and how to distinguish them from other potential infectious diseases
- How cases should be diagnosed and managed in primary care, including appropriate treatment for suspected or confirmed cases
- Appropriate public health measures to take if suspected cases of measles or whooping cough present to you, including infection and prevention control measures and how to notify appropriate bodies
- Prevention of measles and whooping cough through vaccination; why and when vaccinations are recommended and how to advise patients who have missed their vaccinations

See how our symptom tool can help you make better sense of patient presentations Click here to search a symptom

Receive the latest news, clinical updates and case studies straight to your inbox.
SIGN UP TODAY
Related articles

Most Popular
1 Supporting lung cancer screening in the community
2 Another baby dies from whooping cough as cases surpass 10,000
3 Festival nursing: ‘You can have so much fun doing something you love’
4 Use school nurses to deliver immunisations, think-tank report urges

IMPORTANT LINKS
- Subscribe to newsletters
- Privacy policy
- Terms and conditions
- Yellow Card reporting
MORE FROM COGORA
- Pulse Today
- The Pharmacist
- Management in Practice
- Healthcare Leader
- Hospital Healthcare Europe
- Hospital Pharmacy Europe
© Cogora 2024 Cogora Limited. 1 Giltspur Street, London EC1A 9DD Registered in the United Kingdom. Reg. No. 2147432
Nursing in Practice newsletters
Sign up today to receive the latest news, business insight, blogs and case studies via newsletters as it happens.
- Preferences

Respiratory Case Study Discussions - PowerPoint PPT Presentation

Respiratory Case Study Discussions
... in lung bases, and negative for asymmetry of fremitus or dullness to percussion. ... for fremitus in rll with rales (crackles) and dullness to percussion. ... – powerpoint ppt presentation.
- Chest film shadows of x-ray energy
- Radiopaque dense materials (metal or bone) appear as white
- Radiolucent materials with little density (air or fat) appear as dark
- Variations in density (soft tissue or fluid) appear as shades of gray
- Border interface between densities
- Posterior-Anterior
- Anterior-Posterior (portable)
- Bryan Mann, MD
- Fort Hays State University
- Department of Nursing
- 2 Soft Tissue
- Adds dimension
- Note clear areas substernal retrocardiac
- Penetration
- Overexposed too dark, under interpretation
- Underexposed too light, over interpretation
- Inspiratory breath
- Count 10 ribs above diaphram
- Symmetry alignment
- Compare clavicles for rotation
- Sharp costophrenic angles
- AP (heart may appear enlarged)
- Right patient
- Mediastinum (midline)
- Hilar markings
- Lung markings
- Diaphragm gastric bubble
- Costophrenic angles
- A 23 year old male presents with a 6 day history of cough productive of scant white mucous, and intermittent low grade fevers, without high fever spikes. Past medical history is negative. Lung exam is positive for bilateral scattered crackles with occasional expiratory wheezes in lung bases, and negative for asymmetry of fremitus or dullness to percussion.
- Assessment considerations
- A 64 year old man with a 30 pack year smoking history and a 3 year history of difficulty starting his urinary stream presents with shortness of breath on exertion and a new cough. Lung exam is positive for scattered wheezes and rhonchi bilaterally.
- A 54 year old man with history of alcoholism presents with a complaint of fever, night sweats, chills, shortness of breath and a cough productive of green sputum. His temperature is 101.2 degrees F. Lung exam is positive for decreased breath sounds and dullness to percussion in right upper lobe.
- A 19 year old male presents with sudden onset of shortness of breath. Past history is negative. Lung exam is positive for dullness to percussion and decreased breath sounds over the left lateral lung field.
- a 26 year old female presents with a history of sudden onset of purulent sputum (rust-tinged), fevers to 102.4 degrees F, shortness of breath and chills. Past history negative. Lung exam is positive for fremitus in RLL with rales (crackles) and dullness to percussion.
PowerShow.com is a leading presentation sharing website. It has millions of presentations already uploaded and available with 1,000s more being uploaded by its users every day. Whatever your area of interest, here you’ll be able to find and view presentations you’ll love and possibly download. And, best of all, it is completely free and easy to use.
You might even have a presentation you’d like to share with others. If so, just upload it to PowerShow.com. We’ll convert it to an HTML5 slideshow that includes all the media types you’ve already added: audio, video, music, pictures, animations and transition effects. Then you can share it with your target audience as well as PowerShow.com’s millions of monthly visitors. And, again, it’s all free.
About the Developers
PowerShow.com is brought to you by CrystalGraphics , the award-winning developer and market-leading publisher of rich-media enhancement products for presentations. Our product offerings include millions of PowerPoint templates, diagrams, animated 3D characters and more.

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
A rare case: adenomatoid odontogenic tumor mimicking follicular cyst in a young patient.

1. Introduction
2. case description, 3. discussion, 4. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- WHO. Classification of Tumours Editorial Board. Head and Neck Tumours , 5th ed.; WHO Classification of Tumours Series; International Agency for Research on Cancer: Lyon, France, 2022; Volume 9, Available online: https://publications.iarc.fr/ (accessed on 20 August 2024).
- Abrahams, J.M.; McClure, S.A. Pediatric Odontogenic Tumors. Oral Maxillofac. Surg. Clin. N. Am. 2016 , 28 , 45–58. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tamiolakis, P.; Thermos, G. Demographic and clinical characteristics of 5294 jaw cysts: A retrospective study of 38 years. Head Neck Pathol. 2019 , 13 , 587–596. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McLean, A.C.; Vargas, P.A. Cystic Lesions of the Jaws: The Top 10 Differential Diagnoses to Ponder. Head. Neck Pathol. 2023 , 17 , 85–98. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Steensland, H.S. Epithelioma adamantinum. J. Exper Med. 1905 , 6 , 377–389. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- WHO; El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.; Slootweg, P.J. (Eds.) World Health Organization Classification of Head and Neck Tumours ; IARC Press: Lyon, France, 2017; p. 348. [ Google Scholar ]
- Vered, M.; Wright, J.M. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Odontogenic and Maxillofacial Bone Tumours. Head. Neck Pathol. 2022 , 16 , 63–75. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Coura, B.P.; Bernardes, V.F.; de Sousa, S.F.; França, J.A.; Pereira, N.B.; Pontes, H.A.R.; Batista, A.C.; da Cruz Perez, D.E.; Albuquerque, R.L.C., Jr.; de Souza, L.B.; et al. KRAS mutations drive adenomatoid odontogenic tumor and are independent of clinicopathological features. Mod. Pathol. 2019 , 32 , 799–806. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chaves, R.R.M.; Júnior, A.A.C.P.; Gomes, C.C.; de Castro, W.H.; Gomez, R.S. Multiple adenomatoid odontogenic tumors in a patient with Schimmelpenning syndrome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020 , 129 , e12–e17. [ Google Scholar ] [ CrossRef ]
- Konouchi, H.; Asaumi, J.; Yanagi, Y.; Hisatomi, M.; Kishi, K. Adenomatoid odontogenic tumor: Correlation of MRI with histopathological findings. Eur. J. Rad. 2002 , 44 , 19–23. [ Google Scholar ] [ CrossRef ]
- Ide, F.; Muramatsu, T.; Ito, Y.; Kikuchi, K.; Miyazaki, Y.; Saito, I.; Kusama, K. An expanded and revised early history of the adenomatoid odontogenic tumor. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013 , 115 , 646–651. [ Google Scholar ] [ CrossRef ]
- Scholl, R.J.; Kellett, H.M.; Neumann, D.P.; Lurie, A.G. Cysts and cystic lesions of the mandible: Clinical and radiologic-histopathologic review. Radiographics 1999 , 19 , 1107–1124. [ Google Scholar ] [ CrossRef ]
- Speight, P.; Fantasia, F.E.; Neville, B.W. Dentigerous cyst. In WHO Classification of Head and Neck Tumours , 4th ed.; El-Naggar, A.K., Chan, J.K.C., Grandis, J.R., Takata, T., Slootweg, P.J., Eds.; International Agency for Research on Cancer: Lyon, France, 2017; pp. 234–235. [ Google Scholar ]
- Jones, A.; Craig, G.; Franklin, C. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J. Oral Pathol. Med. 2006 , 35 , 500–507. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hajj, R.; Dagher, J.; Nasseh, I. Infrequent radiological features of a dentigerous cyst—A case report. Int. Dent. Med. J. Adv. Res. 2019 , 5 , 1–5. [ Google Scholar ]
- McKinney, S.L.; Lukes, S.M. Dentigerous cyst in a young child: A case report. Can. J. Dent. Hyg. 2021 , 55 , 177–181. [ Google Scholar ] [ PubMed ] [ PubMed Central ]
- Tuwirqi, A.A.; Khzam, N. What do we know about dentigerous cysts in children: A review of literature. J. Res. Med. Dent. Sci. 2017 , 5 , 67–79. [ Google Scholar ] [ CrossRef ]
- Philipsen, H.P.; Reichart, P.A. Adenomatoid odontogenic tumour: Facts and figures. Oral Oncol. 1999 , 35 , 125–131. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chrcanovic, B.R.; Gomez, R.S. Adenomatoid odontogenic tumor: An updated analysis of the cases reported in the literature. J. Oral Pathol. Med. 2019 , 48 , 10–16. [ Google Scholar ] [ CrossRef ]
- Batra, P.; Prasad, S.; Parkash, H. Adenomatoid odontogenic tumour: Review and case report. J. Can. Dent. Assoc. 2005 , 71 , 250–253. [ Google Scholar ] [ PubMed ]
- Prakasam, M.; Tiwari, S.; Satpathy, M.; Banda, V.R. Adenomatoid odontogenic tumour. BMJ Case Rep. 2013 , 27 , bcr2013010212. [ Google Scholar ] [ CrossRef ]
- Barnts, K.; Feng, J.Q.; Qin, C.; Zhang, H.; Cheng, Y.L. Adenomatoid odontogenic tumor: Evidence for a mixed odontogenic tumor. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022 , 133 , 675–683. [ Google Scholar ] [ CrossRef ]
- Zhou, C.-X.; Gao, Y. Adenomatoid odontogenic tumor: A report of a rare case with recurrence. J. Oral Pathol. Med. 2007 , 36 , 440–443. [ Google Scholar ]
Click here to enlarge figure
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Petroni, G.; Zaccheo, F.; Di Gioia, C.R.T.; Adotti, F.; Cicconetti, A. A Rare Case: Adenomatoid Odontogenic Tumor Mimicking Follicular Cyst in a Young Patient. Appl. Sci. 2024 , 14 , 7554. https://doi.org/10.3390/app14177554
Petroni G, Zaccheo F, Di Gioia CRT, Adotti F, Cicconetti A. A Rare Case: Adenomatoid Odontogenic Tumor Mimicking Follicular Cyst in a Young Patient. Applied Sciences . 2024; 14(17):7554. https://doi.org/10.3390/app14177554
Petroni, Giulia, Fabrizio Zaccheo, Cira Rosaria Tiziana Di Gioia, Flavia Adotti, and Andrea Cicconetti. 2024. "A Rare Case: Adenomatoid Odontogenic Tumor Mimicking Follicular Cyst in a Young Patient" Applied Sciences 14, no. 17: 7554. https://doi.org/10.3390/app14177554
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

IMAGES
VIDEO
COMMENTS
An 81-year-old man presented with fever, cough, and shortness of breath. Within a few hours after presentation, chest pain and respiratory distress developed. A chest radiograph showed bilateral pa...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
History. A 60-year-old man presented to the emergency department complaining of persistent right-sided chest pain and cough. The chest pain was pleuritic in nature and had been present for the last month. The associated cough was productive of yellow sputum without hemoptysis. He had unintentionally lost approximately 30 pounds over the last 6 ...
ATS Clinical Cases. The ATS Clinical Cases are a series of cases devoted to interactive clinical case presentations on all aspects of pulmonary, critical care and sleep medicine. They are designed to provide education to practitioners, faculty, fellows, residents, and medical students in the areas of pulmonary, critical care and sleep medicine.
Presentation of Case. ... the respiratory rate 25 breaths per minute, and the oxygen saturation 95% while he was receiving oxygen through a mechanical ventilator (positive end-expiratory pressure ...
Respirology Case Reports (RCR) is an international open access journal publishing original clinical case reports, case series, clinical images, and clinical videos in all fields of respiratory medicine. We facilitate the international exchange between clinicians and researchers of experiences in diagnosing and treating uncommon diseases or diseases with unusual presentations.
1. Describe the components of a thorax/lung exam and practice basic percussion and auscultation techniques. 2. Elicit a comprehensive history from a standardized patient during a telemedicine encounter and develop a differential diagnosis with supportive evidence from the history and physical examination. 3.
American Journal of Respiratory and Critical Care Medicine; 196: 4, 438-446. Lozano R et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet; 380: 9859, 2095-2128. Lumb AB (2016) Nunn's Applied Respiratory Physiology ...
Interactive Case Studies In Respiratory Care Doug Pursley, M.Ed., RRT Program Director Ozarks Technical Community College Springfield, MO. Case 1 • A 74 year old female with COPD is admitted to the ED with mild chest pain. She is on her portable liquid system at 3 l/m. • B/S, CXR clear, pt. is alert and oriented • ABGs: pH 7.32, PaCO2 84, HCO2 42, BE +15, PaO2 68 • The physician sees ...
Bronchiectasis is a progressive respiratory disease characterised by permanent dilatation of the bronchi and associated with a clinical syndrome of cough, sputum production and recurrent respiratory infections [ 1 ]. The causes of bronchiectasis are varied with important differences between the presentation and natural history of the disease ...
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD). The key findings that point to this diagnosis include: Barrel chest. Tachypnea. A long expiratory time. Diminished breath sounds. Use of accessory muscles while breathing. Digital clubbing. Pursed lip breathing.
Approximately 24 hours after admission (day 5 of illness), JV experiences increases in his respiratory rate (74 breaths per minute), pulse (182 beats per minute), work of breathing, and a fever (39.4 degrees C [102.92 degrees F]). He is given an antipyretic. After 1 hour, his fever persists and his work of breathing, respiratory rate and pulse ...
Respiratory Case Reports 2024 Volume: 13 Issue: 2: CASE REPORT: 1. INTERACTIVE CASE: Brucellosis Mimicking Lung Cancer: A Case Report Gokce Kulah, Tayfun Caliskan, Kadir Canoğlu, Özge Atış, Mustafa Çarkçı doi: 10.5505/respircase.2024.68335 Pages 67 - 70.
Presentation of Case Dr. Kathy M. Tran: A 74-year-old man with mantle-cell lymphoma was admitted to this hospital during the coronavirus disease 2019 (Covid-19) pandemic because of acute ...
The document presents a case of respiratory distress syndrome (RDS) in a 3-day-old male infant. Key details include: 1. The infant presented with difficulty breathing, fast breathing rate, and was born prematurely at low birth weight. 2. Physical examination found signs of respiratory distress including a fast heart rate and blue skin discoloration. 3. The infant was diagnosed with RDS, likely ...
In this case-based module, Dr Toni Hazell discusses the diagnosis, treatment and prevention of measles and whooping cough, including how to identify and manage suspected cases, what appropriate treatment should be given in primary care and how to support improved uptake of vaccination against these serious infectious diseases. Learning objectives With the concerns about ongoing outbreaks of ...
Hydropneumothorax
Presentation of Case Dr. Sarita U. Patil (Allergy and Immunology): A 9-year-old boy was admitted to this hospital because of fever, cough, respiratory distress, and chest pain.
In most cases, this failure may lead to death if it's not treated quickly. • The incidence rate of acute respiratory failure worldwide per year was found to be at 88.6 per 100,000 population. On the other hand, the mortality rates of acute respiratory failure worldwide per year were found to be at 42.7% (ICU Mortality) and 41% (90-day ...
Case 3. A 54 year old man with history of alcoholism. presents with a complaint of fever, night sweats, chills, shortness of breath and a cough. productive of green sputum. His temperature is. 101.2 degrees F. Lung exam is positive for. decreased breath sounds and dullness to. percussion in right upper lobe.
Study design and methods ... Peer-Reviewed • More info Atypical Presentations of Myasthenia Gravis as Acute Respiratory Failure: A Rare Case Bingu ... article as: Reddy B, Jadhav U, Wagh P, et al. (August 23, 2024) Atypical Presentations of Myasthenia Gravis as Acute Respiratory Failure: A Rare Case. Cureus 16(8): e67635. doi:10.7759/cureus ...
Presentation of Case Dr. Lila M. Martin: A 73-year-old man was transferred to the intensive care unit (ICU) of an academic health center in Boston for acute hypoxemic respiratory failure
Acute pulmonary embolism (PE) is a common manifestation of venous thromboembolic disease, responsible for over 100,000 deaths worldwide in 2018 alone. 1 Patients with acute PE can have a variety of presentations, ranging from no symptoms to obstructive shock leading to right heart failure and death. 2,3 Clinical presentation is directly linked to the severity of the acute PE.
The objective of this study is to present an uncommon case of adenomatoid odontogenic tumor (AOT) with an impacted maxillary canine, initially mimicking a follicular cyst. AOT is a rare odontogenic tumor, accounting for approximately 1% to 9% of all odontogenic tumors. It primarily occurs in the maxilla and is often associated with an unerupted permanent tooth. Follicular cysts, also known as ...