NCSBN Research Projects Significant Nursing Workforce Shortages and Crisis
CHICAGO – Today, NCSBN unveiled its research, titled “Examining the Impact of the COVID-19 Pandemic on Burnout & Stress Among U.S. Nurses,” in a panel titled “Nursing at the Crossroads: A Call to Action” in Washington, D.C. at the National Press Club at 9:30 am EST.
For the first time, the research findings reveal how the nursing workforce was impacted by the pandemic and how many left the workforce in this period, and forecast how many nurses in the U.S. have an intent to leave the workforce. The research also examined the personal and professional characteristics of nurses experiencing heightened workplace burnout and stress due to the COVID-19 pandemic.
The study is considered to be the most comprehensive and only research in existence, uncovering the alarming data points which have far reaching implications for the health care system at large and for patient populations. The research was gathered as part of a biennial nursing workforce study conducted by NCSBN and the National Forum of State Nursing Workforce Centers.
Key findings include:
- Approximately 100,000 registered nurses (RNs) left the workforce during the COVID-19 pandemic in the past two years due to stress, burnout and retirements.
- Another 610,388 RNs reported an “intent to leave” the workforce by 2027 due to stress, burnout and retirement.
- 188,962 additional RNs younger than 40 years old reported similar intentions.
- Altogether, about one-fifth of RNs nationally are projected to leave the health care workforce.
- 62% of the sample reported an increase in their workload during the pandemic.
- A quarter to half of nurses reported feeling emotionally drained (50.8%), used up (56.4%), fatigued (49.7%), burned out (45.1%), or at the end of the rope (29.4%) “a few times a week” or “every day.”
- These issues were most pronounced with nurses with 10 or fewer years of experience, driving an overall 3.3% decline in the U.S. nursing workforce in the past two years.
- Licensed practical/vocational nurses, who generally work in long-term care settings caring for the most vulnerable populations, have seen their ranks decline by 33,811 since the beginning of the pandemic. This trend continues.
Research also suggested that nurses’ workloads and unprecedented levels of burnout during the COVID-19 pandemic played key roles in accelerating these workforce trends and threatening the future of the U.S. nursing workforce, particularly for younger, less experienced RNs. Further, high levels of turnover were seen with the potential for even further declines in a post-pandemic nursing workplace as disruptions in prelicensure nursing programs have also raised concerns about the supply and clinical preparedness of new nurse graduates. Early career data for new entrants into the profession suggest decreased practice and assessment proficiency. Coupled with large declines among nursing support staff, NCSBN calls for significant action to foster a more resilient and safe U.S. nursing workforce moving forward.
“The data is clear: the future of nursing and of the U.S. health care ecosystem is at an urgent crossroads,” said Maryann Alexander, PhD, RN, FAAN, NCSBN Chief Officer of Nursing Regulation. “The pandemic has stressed nurses to leave the workforce and has expedited an intent to leave in the near future, which will become a greater crisis and threaten patient populations if solutions are not enacted immediately. There is an urgent opportunity today for health care systems, policymakers, regulators and academic leaders to coalesce and enact solutions that will spur positive systemic evolution to address these challenges and maximize patient protection in care into the future.”
The research findings and proposed solutions were presented in a panel discussion today at the National Press Club in Washington, D.C.
Panelists included:
- Antonia Villarruel, Dean of Nursing at University of Pennsylvania
- Gay Landstrom, Senior Vice President and Chief Nursing Officer at Trinity Health System
- Congresswoman Lisa Blunt Rochester, U.S. Representative of Delaware
- Robyn Begley, CEO of the American Organization for Nursing Leadership and CNO/Sr. VP for the American Hospital Association
- Rayna M. Letourneau, Board of Directors, National Forum for State Workforce Centers
A recording of the panel discussion is available on ncsbn.org .
To request interviews with NCSBN or view the entire research, please contact [email protected] or visit ncsbn.org .
Research Methodology: The study examines a subset of the 2022 National Nursing Workforce Study for analysis. Reported trends represent population-based estimates. There were 29,472 registered nurses (including advanced registered nurses [APRN]) and 24,061 licensed practical nurses/vocational nurses across 45 states included.
About NCSBN Empowering and supporting nursing regulators across the world in their mandate to protect the public, NCSBN is an independent, not-for-profit organization. As a global leader in regulatory excellence, NCSBN champions regulatory solutions to borderless health care delivery, agile regulatory systems and nurses practicing to the full scope of their education, experience and expertise. A world leader in test development and administration, NCSBN’s NCLEX® Exams are internationally recognized as the preeminent nursing examinations.
NCSBN’s membership is comprised of the nursing regulatory bodies (NRBs) in the 50 states, the District of Columbia and four U.S. territories. There are five exam user members and 25 associate members that are either NRBs or empowered regulatory authorities from other countries or territories.
The statements and opinions expressed are those of NCSBN and not individual members.

Nursing in 2023: How hospitals are confronting shortages
When we tabulated the results of our first nationwide nursing survey almost two years ago , we were surprised to see such a high reported likelihood of nurses planning to leave their jobs—and we did not expect this trend to persist for such an extended period of time.
About the authors
This article is a collaborative effort by Gretchen Berlin , Faith Burns, Connor Essick, Meredith Lapointe, and Mhoire Murphy , representing views from McKinsey’s Healthcare Practice.
But that is what has happened in the wake of the COVID-19 pandemic. In fact, we have seen some of this reported anticipated turnover actually occur, as well as a decrease in the overall active nursing workforce. And there is still cause for concern: today, 31 percent of nurses still say they may leave their current direct patient care jobs in the next year, according to our most recent survey. That said, we are cautiously optimistic that some of the practices implemented by healthcare organizations to improve the experience of nurses are bearing fruit.
In this article, we share the latest data from our September 2022 frontline nursing survey of 368 frontline nurses providing direct patient care in the United States (see sidebar, “About the research”). We offer these insights as resources for organizations as they continue their journeys of attracting, supporting, and retaining a vibrant workforce, as well as promoting longer-term workforce stability.
What’s been happening in the nursing workforce
About the research.
Nursing turnover continues to be a substantial challenge for healthcare organizations as the number of individuals with the intent to leave their jobs remains high. In our most recent nursing survey, 31 percent of respondents indicated they were likely to leave their current role in direct patient care, a figure that has stabilized over the past six to 12 months yet is still higher than the 22 percent rate observed in our first survey in February 2021 (Exhibit 1). 1 Gretchen Berlin, Meredith Lapointe, and Mhoire Murphy, “ Surveyed nurses consider leaving direct patient care at elevated rates ,” McKinsey, February 17, 2022; Gretchen Berlin, Meredith Lapointe, Mhoire Murphy, and Molly Viscardi, “ Nursing in 2021: Retaining the healthcare workforce when we need it most ,” McKinsey, May 11, 2021. Our research further shows that the intent to leave varies across settings. For example, inpatient registered nurses (RNs) have consistently reported a higher intent to leave than the average of all surveyed RNs. In our most recent pulse survey of inpatient RNs, we saw intent to leave rise again, from 35 percent in fall 2022 to over 40 percent in March 2023.
Recent analysis of studies comparing intent to leave to actual turnover show that both jumped meaningfully over the course of 2021. A study from Nursing Solutions Inc. (NSI) showed that actual reported hospital and staff RN turnover increased from 18 percent in fiscal year 2020 to 27 percent in fiscal year 2021; the same March 2022 study reported that the workforce lost about 2.5 percent of RNs in 2021. 2 2022 NSI national health care retention & RN staffing report , NSI Nursing Solutions, March 2022. In the latest NSI report (March 2023), turnover reduced to 23 percent in fiscal year 2022 but still remains elevated compared with prepandemic levels. 3 2023 NSI national health care retention & RN staffing report , March 2023. A Health Affairs study published in April 2022 found that the RN workforce fell by about 100,000 by the end of 2021, which is a “far greater drop than ever observed over the past four decades.” This decline was particularly pronounced among midtenure nurses (aged 35 to 49). 4 David Auerbach, Peter Buerhaus, Karen Donelan, and Douglas Staiger, “A worrisome drop in the number of young nurses,” Health Affairs Forefront, April 13, 2022. In terms of where they are going, nurses are both leaving the profession entirely as well as simply changing employers or roles. About 35 percent of respondents to our most recent survey who indicated they were likely to leave said they would remain in direct patient care (that is, at a different employer or role). The remainder said they intended to leave the bedside for nondirect patient care roles to pursue different career paths or education or to exit the workforce entirely.
With this persistently high turnover and the corresponding gathering storm in US healthcare , it is more important than ever for healthcare organizations to design and deploy initiatives that respond to and address workforce needs. Most healthcare organizations have learned that attracting and retaining nursing talent in the postpandemic era will require a more nuanced understanding of what nurses are looking for in a profession and an employer.
Our four frontline nursing surveys over the past two years have enabled us to glean insights into factors contributing to both attrition and retention. Frontline nursing respondents have consistently ranked elements of flexibility, meaning, and balance as the most important factors affecting their decision to stay in direct patient care (Exhibit 2). Recognition, open lines of communication, and embedding breaks into the operating model (for example, during shifts, between shifts, and formal paid time off) have consistently been rated as the top initiatives to support well-being.
The nursing workforce has evolved over the course of the pandemic, and the strategies aimed at attracting and retaining tomorrow’s workforce have evolved as well. To start, structural solutions that help to ensure a manageable workload—for example, consistent support staff, a safe environment, reduced documentation and administrative requirements, predictability of schedule, and ability to take paid time off—continue to be critical. Surveyed nurses who left a direct patient care role in the past 18 months indicated that not being valued, unmanageable workloads, and inadequate compensation were the top factors in their decision to exit (Exhibit 3). There are no one-size-fits-all solutions, but many healthcare organizations have adapted their approaches and carried out interventions that appear to be yielding results.
What stakeholders can do in the short term
Our most recent survey found that 75 percent of nurses who left a job in the past 18 months reported that not being valued by their organization was a factor in their decision. In addition, 56 percent of total respondents reported that appropriately recognizing nurses for their contributions was the most effective initiative to support well-being. Surveyed nurses suggested various ways to respond to the recognition gap, including simple acknowledgement, appreciation of excellence, and reinforcement through broader workplace culture and support in the field.
Many healthcare systems have found ways to implement the nurses’ suggestions. While more research is needed to understand the full impact of these efforts, they may be helpful short-term starting points in the attempt to show support for the workforce.
At the Orlando VA Medical Center, “Employee Well-Being Centers” were set up to address the burnout and stress caused by the pandemic. Setting up a dedicated quiet space with amenities like virtual-reality headsets, aroma therapy, and sound machines, as well as snacks and beverages, resulted in a measurable positive impact on Employee Whole Health engagement scores and decreased feelings of burnout, higher retention, and increased overall well-being. As a result of these improvements, the program has expanded to more than ten medical centers across the Veterans Health Administration network. 5 “Employee well-being centers and carts,” VA Diffusion Marketplace, accessed April 2023.
Some health systems have employed digital tools to ensure that tailored recognition can be delivered in a timely and meaningful way. For example, nurse managers at the Orange Coast Medical Center in Fountain Valley, California, were using sticky notes, mining emails, spreadsheets, and other manual processes to remind them which nurses did what to deserve recognition or to schedule meetings to help other nurses improve their work. While meaningful, these recognition processes were time-consuming for nurse managers. 6 “Frontline nurses are burning out. This digital health start-up is trying to change that," Laudio, May 13, 2022.
To sustain both this type of in-the-moment recognition and to reward bigger milestones, Orange Coast implemented the Laudio technology platform, which enables frontline leaders to monitor and manage team activity and performance. Use of this system has shown that one meaningful, or high quality, interaction per team member per month can reduce turnover by 36 percent. 7 “Frontline nurses are burning out. This digital health start-up is trying to change that," Laudio, May 13, 2022. In addition to keeping track of events and alerting managers about matters to engage in with specific nurses, Laudio can send digital cards and notes to nurses to acknowledge high performance.
Safety is also increasingly top of mind for nurses, as troubling incidents involving visitors and patients have risen. 8 Christine Porath and Adrienne Boissy, “Frustrated patients are making health care workers’ jobs even harder,” Harvard Business Review , May 14, 2021. In our most recent survey, 42 percent of nurses indicated that not having a safe working environment was an extremely or very important factor affecting their decision to leave direct patient care, up from 24 percent in March 2022.
To address safety concerns and incivility, UMass Memorial Medical Center in Worcester, Massachusetts, developed a patient and visitor code of conduct. At the entrances to facilities, visitors are asked to sign an agreement to adhere to a code of conduct that formalizes parameters and expectations of behavior. In addition, UMass created talking points for employees to use to respond to and de-escalate contentious situations. In just over a month of piloting the program, the hospital collected 56,000 signed agreements and only asked four visitors to leave the premises. 9 Christine Porath, “Frontline work when everyone is angry,” Harvard Business Review , November 9, 2022.
In addition to deploying more effective strategies to support and retain employees, healthcare executives can look at ways to better attract talent in the near term. To recruit staff, health systems should ensure that their value proposition is aligned to the workplace elements that nurses consider most important—especially when differentiating on compensation is less feasible. Aya Healthcare, a healthcare-talent software and staffing company, found that hospitals seen as a great place to work paid less to secure talent throughout the pandemic. In fact, hospitals seen as great places to work had labor compensation rates 11 percent lower than those without this advantage. 10 April Hansen, “The value of a good reputation (or the cost of a bad one…),” The Staffing Stream, April 8, 2021.
What stakeholders can do in the medium term
In the medium term, finding ways to incorporate flexibility into work schedules is an initiative that 63 percent of surveyed nurses ranked as the most effective for their well-being. We saw similar responses regarding nurses’ decision to stay in their current position: 86 percent cited a flexible work schedule as the reason, which ranked second after “doing meaningful work.” The nature of nurses’ work—typically specialized and always in demand—may make providing schedule flexibility seem daunting. But health systems have pursued several creative ways to address the issue.
The nature of nurses’ work—typically specialized and always in demand—may make providing schedule flexibility seem daunting.
For example, the Mercy health system launched Mercy Works on Demand, a systemwide on-demand platform that allows its full- and part-time nurses as well as other experienced nurses to select when they work. Through the platform, Mercy has hired about 1,100 individuals they are calling gig nurses and have improved overall fill rates by two percentage points. 11 Kelly Gooch, “How Mercy embraced a gig mindset for nursing,” Becker’s Hospital Review, December 5, 2022. But flexibility means different things to different people, which has increased complexity for employers. Charting a path forward will require a nuanced understanding of the employee value proposition as well as what options resonate with the workforce.
Job flexibility is at the center of many health systems’ strategies to not only attract new talent but also to welcome back nurses who left during the pandemic. Henry Ford Health has been able to bring back 25 percent of the nurses who left by offering flexible opportunities. Nursing leaders worked closely with Henry Ford Health’s human resources department to design flexible options such as the ability to work in different settings (for example, inpatient, outpatient, or virtual) or to work only on weekends. The health system also created fixed-term positions for nurses who didn’t want full-time permanent jobs, with the option to transition to permanent roles once their term was up. 12 Mackenzie Bean and Erica Carbajal, “How Henry Ford rehired 25% of nurses who left during the pandemic,” Becker’s Hospital Review, February 15, 2023.
As in other industries, the flexibility to work remotely has become increasingly important to some nurses. Trinity Health launched a virtual-care model, allowing more experienced nurses to continue providing patient care but away from the bedside. The new virtual model opens the door to nurses who may be physically tired from the demands of in-person care and to those who prefer to work from home. In addition, this program has enabled the virtual nurses to provide support to teams at the bedside and to improve patient experience by giving them more chances to interact with a nurse. The program is being rolled out across Trinity’s 88 hospitals nationwide. 13 Giles Bruce, “Trinity Health plans to institute virtual nurses across its 88 hospitals in 26 states,” Becker’s Hospital Review, January 13, 2023.
What stakeholders can do in the long term
As health systems look beyond retaining the current workforce and meeting the expected demand for nursing talent, they could have a role to play in building a longer-term pipeline through investing in new-graduate nurses and in the infrastructure required to ensure successful onboarding into the profession.
For example, Dignity Health has invested heavily in longer-term pipeline building through a joint venture between Dignity Health Global Education and Global University Systems. The partnership offers online academic degrees to further the education, training, and development of the healthcare workforce. The joint venture spans technical, professional, executive, and leadership training and provides a range of flexible, accessible, and affordable education opportunities for healthcare workers to advance their careers. It also has a scholarship fund to remove financial barriers for education and to increase equity in healthcare. Dignity Health Global Education now has one of the most comprehensive nursing residency programs, available in 21 states. 14 “Dignity Health and Global University Systems announce joint venture to expand global education for health professionals,” Global University Systems press release, January 30, 2019.
The commitment to building a longer-term talent pipeline has expanded beyond individual health systems. Many city and regional partnerships have developed across the United States, bringing together critical stakeholders across the healthcare ecosystem to train and upskill unemployed and underemployed job seekers into healthcare occupations. For example, the Birmingham Region Health Partnership, the result of close collaboration among government, healthcare employers, and other community partners, including Birmingham Business Alliance and Innovate Birmingham, won a $10.8 million grant from the Good Jobs Challenge to train and place over 1,000 jobseekers in the region. 15 “Birmingham receives $10.8 million ‘Good Jobs Challenge’ grant,” Birmingham City Council press release, August 3, 2022. Similar collaborative partnerships exist in Chicago, Baltimore, Philadelphia, among others, to build a pipeline of healthcare workers and to create meaningful career opportunities for historically excluded job seekers. 16 BACH Quarterly Newsletter , Baltimore Alliance for Careers in Healthcare, accessed April 2023; “Cutting the ribbon on new West Philadelphia Skills Initiative Headquarters,” University City District, March 29, 2023; CHWC Overview & Update - February 2021, Chicagoland Healthcare Workforce Collaborative, updated March 10, 2021.
Other stakeholders are taking action at a national level. In 2022, the US Department of Labor budgeted $80 million to encourage not-for-profit organizations, educational institutions, and tribal organizations to apply for grants of up to $6 million each to train current and former nurses to become nursing educators and frontline healthcare workers to train for nursing careers. 17 “DOL Nursing Expansion Grant Program: Total funding available: Up to $80 million,” US Department of Labor Employment and Training Administration, 2022. The program emphasizes increasing workforce diversity and building partnerships with community-based organizations and training institutions.
Retaining the current nursing workforce while looking ahead to the longer-term talent pipeline will be critical to meeting the projected shortfall in registered nurses. There isn’t one answer to the challenges confronting healthcare organizations, and indeed, they have begun taking steps to address nurses’ stated needs through short-, medium-, and longer-term strategies that attract, strengthen, and grow a vibrant nurse workforce. There is more to be done, especially in taking account of the voices of the front line and addressing the core drivers behind why nurses are planning to leave. We are optimistic that the issues facing the nursing profession can be addressed, but this will require consistent and dedicated attention from many parties.
Gretchen Berlin , RN, is a senior partner in McKinsey’s Washington, DC, office, where Faith Burns is a consultant; Meredith Lapointe is a partner in the Bay Area office, where Connor Essick is a consultant; and Mhoire Murphy is a partner in the Boston office.
The authors wish to thank the nurses, physicians, and staff on the front lines who are caring for patients and communities. They also wish to thank Beth Bravo, Stephanie Hammer, Thomas Pu, Brooke Tobin, and Catherine Wilkosz for their contributions to this article.
Explore a career with us
Related articles.

Around the world, nurses say meaningful work keeps them going

Surveyed nurses consider leaving direct patient care at elevated rates

Nurses and the Great Attrition
Nursing Shortage Fact Sheet
The U.S. is projected to experience a shortage of Registered Nurses (RNs) that is expected to intensify as Baby Boomers age and the need for health care grows. Compounding the problem is the fact that nursing schools across the country are struggling to expand capacity to meet the rising demand for care. The American Association of Colleges of Nursing (AACN) is working with schools, policy makers, nursing organizations, and the media to bring attention to this healthcare concern. AACN is leveraging its resources to shape legislation, identify strategies, and form collaborations to address the shortage.
Download Fact Sheet [PDF]
Current and Projected Shortage Indicators
- According to the Bureau of Labor Statistics’ Employment Projections 2022-2032, the Registered Nursing (RN) workforce is expected to expand by 6% over the next decade. The RN workforce is anticipated to grow from 3.1 million in 2022 to 3.3 million in 2032, an increase of 177,440 nurses. The Bureau also projects 193,100 openings for RNs each year through 2032 when nurse retirements and workforce exits are factored into the number of nurses needed in the U.S.
- The Advanced Practice Registered Nurse (APRN) workforce, including Nurse Practitioners, Nurse Anesthetists, and Nurse Midwives, is expected to grow much faster than average for all occupations, by 38% from 2022 through 2032, according to the BLS’ Occupational Outlook Handbook. Approximately 29,200 new APRNs, which are prepared in master’s and doctoral programs, will be needed each year through 2032 to meet the rising demand for primary and specialty care.
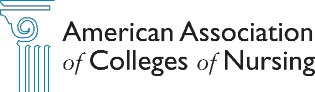
- According to a Health Workforce Analysis published by the Health Resources and Services Administration (HRSA) in November 2022, federal authorities project a shortage of 78,610 full-time RNs in 2025 and a shortage of 63,720 full-time RNs in 2030. The ten states with the largest projected nursing shortage in 2035 are Washington (26%), Georgia (21%), California (18%), Oregon (16%), Michigan (15%), Idaho (15%), Louisiana (13%), North Carolina (13%), New Jersey (12%), and South Carolina (11%). Data for each state may be accessed through HRSA’s Workforce Projections Dashboard .
- In April 2022, Dr. David Auerbach and colleagues published a nursing workforce analysis in Health Affairs , which found that total supply of RNs decreased by more than 100,000 from 2020 to 2021 – the largest drop than ever observed over the past four decades. A significant number of nurses leaving the workforce were under the age of 35, and most were employed in hospitals.
- The Institute of Medicine in its landmark report on The Future of Nursing called for increasing the number of baccalaureate-prepared nurses in the workforce to at least 80% to enhance patient safety. The current nursing workforce falls short of this recommendation, though more than two-thirds of RNs are educated at the baccalaureate or graduate level. The exact percentage has been reported as 69% by HRSA and 71.7% by the National Council of State Boards of Nursing .
- In March 2023, the International Council of Nurses (ICN) released a report calling for the worldwide shortage of nurses to be treated as a global health emergency. The report, titled Recover to Rebuild: Investing in the Nursing Workforce for Health System Effectiveness , details the impact that the pandemic had on the world’s nursing workforce, nurse burnout, and access to care. The authors call for protecting and investing in nurses as key to health system recovery.
Contributing Factors Impacting the Nursing Shortage
Nursing school enrollment is not growing fast enough to meet the projected demand for RN and APRN services.
Though enrollment in entry-level baccalaureate programs in nursing increased by 0.3% in 2023, AACN did report drops in both PhD and master’s nursing programs by 3.1% and 0.9%, respectively. These trends are raising concerns about the capacity of nursing schools to meet the projected demand for nursing services, including the need for more nurse faculty, researchers, and primary care providers.
A shortage of nursing school faculty is restricting nursing program enrollments.
- According to AACN’s report on 2023-2024 Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing , U.S. nursing schools turned away 65,766 qualified applications (not applicants) from baccalaureate and graduate nursing programs in 2023 due to insufficient number of faculty, clinical sites, classroom space, and clinical preceptors, as well as budget constraints.
- According to a Special Survey on Vacant Faculty Positions released by AACN in October 2023, a total of 1,977 full-time faculty vacancies were identified in a survey of 922 nursing schools with baccalaureate and/or graduate programs across the country (84.6% response rate). Besides the vacancies, schools cited the need to create an additional 103 faculty positions to accommodate student demand. The data show a national nurse faculty vacancy rate of 7.8%. Most of the vacancies (79.8%) were faculty positions requiring or preferring a doctoral degree.
A significant segment of the nursing workforce is nearing retirement age.
- According to the 2022 National Sample Survey of Registered Nurses , 23% of RNs working in outpatient, ambulatory, and clinical settings have retired or plan to retire over the next 5 years. While hospitals had the lowest share of nurses who have retired or plan to retire over the next 5 years (15.1%), nurses employed in this setting had the lowest levels of job satisfaction.
- Published October 4, 2023, by the Journal of the American Medical Association , Dr. Melissa Suran published an article titled Overworked and Understaffed, More Than 1 in 4 US Nurses Say They Plan to Leave the Profession . The author looks at the latest data on nurses’ intent to leave their positions and how burnout and understaffing are impacting the workforce.
- In a Health Affairs blog posted in May 2017, Dr. Peter Buerhaus and colleagues project than more than 1 million registered nurses will retire from the workforce by 2030.
Changing demographics signal a need for more nurses to care for our aging population.
- The U.S. Census Bureau reported that number of Americans aged 65 and older is projected to increase from 58 million in 2022 to 82 million by 2050 (23% of the population). With larger numbers of older adults, there will be an increased need for geriatric care, including care for individuals with chronic diseases and comorbidities.
Amplified by the pandemic, insufficient staffing is raising the stress level of nurses, impacting job satisfaction, and driving many nurses to leave the profession.
- According to data published in Nurse.com’s 2022 Nurse Salary Research Report , 29% of nurses across all license types considering leaving in 2021, compared with 11% in 2020.Among nurses who are considering leaving the profession, higher pay was the most influential motivation to stay, followed by better support for work-life balance and more reasonable workload.
- In March 2022, the American Nurses Foundation and the American Nurses Association released the results of its COVID-19 Impact Assessment Survey , which found that 52% of nurses are considering leaving their current position due primarily to insufficient staffing, work negatively affecting health and well-being, and inability to deliver quality care. In addition, 60% of acute care nurses report feeling burnt out, and 75% report feeling stressed, frustrated, and exhausted.
- In September 2021, the American Association of Critical-Care Nurses reported survey findings which show 66% of acute care nurses have considered leaving nursing after their experiences during the pandemic.
Impact of Nurse Staffing on Patient Care
Many scientific studies point to the connection between adequate levels of registered nurse staffing and safe patient care.
- In November 2021, new research in Nursing Outlook examined Variations in Nursing Baccalaureate Education and 30-day Inpatient Surgical Mortality . Researchers found that having a higher proportion of baccalaureate-prepared nurses (BSN) in hospital settings, regardless of educational pathway, is associated with lower rates of 30-day inpatient surgical mortality. The findings support promoting multiple BSN educational pathways.
- In the July 2017 issue of BMJ Quality & Safety , the international journal of healthcare improvement, Dr. Linda Aiken and her colleagues released findings from a study of acute care hospitals in Belgium, England, Finland, Ireland, Spain, and Switzerland, which found that a greater proportion of professional nurses at the bedside is associated with better outcomes for patients and nurses. Reducing nursing skill mix by adding assistive personnel without professional nurse qualifications may contribute to preventable deaths, erode care quality, and contribute to nurse shortages.
- In a study published in the journal BMJ Quality & Safety in May 2013, researcher Heather L. Tubbs-Cooley and colleagues observed that higher patient loads were associated with higher hospital readmission rates. The study found that when more than four patients were assigned to an RN in pediatric hospitals, the likelihood of hospital readmissions increased significantly.
- In the August 2012 issue of the American Journal of Infection Control , Dr. Jeannie Cimiotti and colleagues identified a significant association between high patient-to-nurse ratios and nurse burnout with increased urinary tract and surgical site infections. In this study of Pennsylvania hospitals , the researchers found that increasing a nurse’s patient load by just one patient was associated with higher rates of infection. The authors conclude that reducing nurse burnout can improve both the well-being of nurses and the quality of patient care.
- In a study publishing in the April 2011 issue of Medical Care , Dr. Mary Blegen and her colleagues from the University of California, San Francisco found that higher nurse staffing levels were associated with fewer deaths, lower failure-to-rescue incidents, lower rates of infection, and shorter hospital stays.
- In March 2011, Dr. Jack Needleman and colleagues published findings in the New England Journal of Medicine , which indicate that insufficient nurse staffing was related to higher patient mortality rates. These researchers analyzed the records of nearly 198,000 admitted patients and 177,000 eight-hour nursing shifts across 43 patient-care units at large academic health centers. The data show that the mortality risk for patients was about 6% higher on units that were understaffed as compared with fully staffed units. In the study titled Nurse Staffing and Inpatient Hospital Mortality , the researchers also found that when a nurse’s workload increases because of high patient turnover, mortality risk also increases.
- A growing body of research clearly links baccalaureate-prepared nurses to lower mortality and failure-to-rescue rates. The latest studies published in the journals Health Services Research in August 2008 and the Journal of Nursing Administration in May 2008 confirm the findings of several previous studies which link education level and patient outcomes. Efforts to address the nursing shortage must focus on preparing more baccalaureate-prepared nurses in order to ensure access to safe patient care.
- In March 2007, a comprehensive report initiated by the Agency for Healthcare Research and Quality was released on Nursing Staffing and Quality of Patient Care . Through this meta-analysis, the authors found that the shortage of registered nurses, in combination with an increased workload, poses a potential threat to quality. Increases in registered nurse staffing was associated with reductions in hospital-related mortality and failure to rescue as well as reduced length of stays.
- A shortage of nurses prepared at the baccalaureate level is affecting health care quality and patient outcomes. In a study published September 24, 2003 , in the Journal of the American Medical Association (JAMA), Dr. Linda Aiken and her colleagues at the University of Pennsylvania identified a clear link between higher levels of nursing education and better patient outcomes. This extensive study found that surgical patients have a “substantial survival advantage” if treated in hospitals with higher proportions of nurses educated at the baccalaureate or higher degree level. In hospitals, a 10% increase in the proportion of nurses holding BSN degrees decreased the risk of patient death and failure to rescue by 5%.
- AACN is committed to working with the higher education and healthcare community to prepare more highly educated nurses in sufficient numbers to meet the needs of the nation’s diverse patient population. To address the nursing shortage, AACN is advocating for federal legislation and increased funding for nursing education ( Title VIII , Future Advancement of Academic Nursing Act ); promoting a post-baccalaureate nurse residency program to aid in nurse retention; encouraging innovation in nursing programs, including the development of fast-track programs (second-degree BSN and MSN programs; baccalaureate to doctoral); and working with partner organizations to highlight careers in nursing, including those requiring graduate level preparation.
- Since 2010, AACN has operated NursingCAS, the nation’s centralized application service for nursing education programs that prepare nurses for entry-level and advanced roles. One of the primary reasons for launching NursingCAS was to ensure that all vacant seats in schools of nursing are filled to better meet the nation’s need for RNs, APRNs, and nurse faculty.
Efforts to Address the Nursing Shortage
- In June 2022, the National Council of State Legislatures issued a brief profiling different legislative approaches states are using to address the nursing shortage, including adapting scope of practice laws and offering financial incentives for preceptors.
- In a report on How To Ease the Nursing Shortage in America released in May 2022, the Center for American Progress calls for bold policies toward solving the nursing shortage to ensure that more patients with access to safe, high-quality nursing services. The report highlights how federal and state policymakers can address the shortage through coordinated planning, action, and investment.
- Many statewide initiatives are underway to address both the shortage of RNs and nurse educators. For example, in October 2022, the University of Minnesota and Minnesota State joined forces to create Coalition for Nursing Equity and Excellence, which will work with every school of nursing in the state, healthcare providers, and others to increase enrollment in nurse education programs, expand equity in the nursing workforce, and increase student success. Additional initiatives are also underway in Connecticut , Florida , Louisiana , Missouri , and other states.
- Nursing schools are forming strategic partnerships and seeking private support to help expand student capacity. For example, Shenandoah University announced in March 2023 a new collaboration with Valley Health and the Virginia Hospital and Healthcare Association to address the region’s nursing shortage through a program that leverages retiring nurses and simulation to create a sustainable pathway into nursing. See also efforts launched by Idaho State University and Kootenai Health; Illinois College and Memorial Health; Emory University and the Georgia Nursing Leadership Coalition; Washington State University and Providence Health & Services; and the University of Oklahoma and area schools.
Recent Articles on the Nursing Shortage
- Buerhaus, P.I., Staiger, D.O., Auerbach, D.I., Yates, C., & Donelan, K. (2022, January). Nurse employment during the first fifteen months of the COVID-19 pandemic. Health Affairs , 41(1).
- Buerhaus, P.I. (2021, September/October). Current nursing shortages could have long-lasting consequences: Time to change our present course. Nursing Economics , 39(5), 247-250.
- Firth, S. (2022, May 16). More Support Needed to Shore Up Nurse Pipeline, Experts Say . MedPage Today .
- Suran, M. (2023, October 23). Overworked and Understaffed, More Than 1 in 4 US Nurses Say They Plan to Leave the Profession . JAMA Medical News , 330(16), 1512-1514. doi:10.1001/jama.2023.10055
Updated: May 2024
Robert Rosseter [email protected]
Health Equity
News | Video
Sorting Out Fact and Fiction of a National Nursing Shortage
Penn ldi virtual seminar eyes hospital working conditions that drive nurses from the workplace.
- Hoag Levins
- Share this page on Twitter
- Share this page on Facebook
- Share this page on LinkedIn
The unwillingness of large numbers of nurses to work in facilities that maintain poor nurse working conditions is creating a critical labor shortage across the U.S. hospital and long-term care industry. As she opened a December 1 Penn LDI virtual seminar on the topic, moderator and LDI Executive Director Rachel M. Werner, MD, PhD , asked the four panelists: “How did the labor market become so broken for nurses, and how do we come back from that?”

The panelists were: David Benton, PhD, RN , an Adjunct Lecturer in the Harvard Global Nursing Leadership Program and former Chief Executive Officer of the National Council of State Boards of Nursing; Bianca Frogner, PhD , Professor at the University of Washington’s Center for Health Workforce Studies; Gopi Shah Goda, PhD , Senior Fellow at the Stanford University Institute for Economic Policy Research and former Senior Economist at the White House Council of Economic Advisers; and Karen Lasater, PhD, RN , LDI Senior Fellow and Term Chair of Nursing and Health Policy at the University of Pennsylvania School of Nursing.
“This is not a case of the work being difficult,” said Lasater, “rather it’s about the organizational failures that are hindering nurses from doing their work effectively that drive nurses to feel burnt out. In a recent study, we asked nurses ‘What would be the most important intervention that your hospital could do to prevent your burnout or reduce your burnout?’ The vast majority of respondents said improving nurse staffing levels was the most important intervention that hospital administrators could take. So, there is a real mismatch between what hospitals think they should do and what nurses want them to do. Nurses say appointing clinician wellness champions is not effective. Providing resiliency training and throwing pizza parties is not effective. What nurses want and need are manageable, safe workloads.”
Workplace Nursing Shortage
Like many other nurse scientists who have been researching the issue for years, Lasater is frustrated that the press and policymakers continue to cite a “nursing shortage” that causes the public to assume that in absolute numbers, there aren’t enough nurses across the country. Her and her team’s research at the University of Pennsylvania School of Nursing’s Center for Health Outcomes and Policy Research (CHOPR) have documented that this is not the case. In fact, the current U.S. population of 4.7 million licensed registered nurses is more than the country has ever had and more are coming out of school every year.

The problem, in this age of the industrialized and massively consolidated medicine enterprises, is that so many hospitals have created seriously understaffed, high-stress working environments that large numbers of nurses simply refuse to work in. And those who are working in them continue to experience the constant chaos and stress that has caused at least 100,000 of them to bail out of hospital nursing altogether in the past two years. Surveys have found that 600,000 more say they intend to leave the hospital employment by 2027.
A Vicious Cycle
“It is a vicious cycle,” Lasater said. “Nurses work in bad environments. They leave, they tell other nurses, ‘Don’t go work in that hospital.’ And that results in the nurses who stay there having even worse working conditions and even lower morale. If I were a hospital administrator, I would try to be proactive and address the reasons why nurses are leaving. This is a nurse retention issue. It’s not a nurse pipeline issue.”
Another frustration for nursing researchers is that the poor working conditions that are driving out nurses isn’t just a labor issue. Investigations have shown that the quality of patient care is significantly worse in the same poor nursing environments staffed by inadequate numbers of licensed nurses. But most policymaker comments and press reports fail to connect hospitals’ poor nursing working conditions with the direct harm done to patients who fail to receive adequate care.

Discussing the economics of significantly expanding a hospital’s nursing staff, Shah Goda asked, “Why are hospital administrators not investing more in this workforce? We need to understand what the barriers are to that. If it turns out that there are some market failures here that we need to correct with government policy, then we need to identify those.”
Economics of Staff Expansion
“This is a market heavily driven by reimbursement rates from Medicaid,” Shah Goda continued. “There’s some evidence in very high-quality research studies that suggest that increases in Medicaid reimbursement rates do seem to be causally related to an increase in the number of skilled nurses per patient. So that points to a policy lever that could be something to talk about in terms of what could actually impact what we think might be a labor supply shortage of nurses.”
Frogner agreed that hospitals are struggling financially as they come out of the pandemic but said “that burden should not be borne by the employees. The burden should go back to the federal or state governments that need to step in to help fill the gaps or figure out what are the best mechanisms to make the supporting of workers more sustainable.”

“There are also other things that have value for nurses, such as child care,” said Frogner. “Our health workforce is very female dominated and many of those women are also the primary caregivers in their homes. So, is there something that hospitals can do to support childcare, whether it be subsidizing it or providing childcare on site? Can they help to subsidize transportation costs? Can they make sure nurses are not paying for parking? These all seem like small things, but when you start adding up those costs, they have real wage consequences.”
Lack of Political Will
“The question isn’t just ‘Why aren’t hospitals or skilled nursing facilities doing something,’ but rather, ‘Why aren’t policymakers doing more?'” Frogner continued. “In long term care, that’s been particularly surprising given just what a mess it has just been throughout the pandemic. I think part of it is this question of political will–where is the political will to make some of the changes happen?”
Frogner also noted how hospitals’ intense use of travel nurse agencies during the pandemic demonstrated how nurses eagerly flocked to positions offering more flexible hours and higher wages in temporary nurse service. She said that hospitals’ use of travel nurses continues to decline post-pandemic, but it’s been difficult to extract insights about the dynamics of that because of the lack of data. “We don’t have good national data on either nurse travel agencies or detailed hospital data on workforce to help us understand what has been happening. I know the Centers for Medicare and Medicaid Services (CMS) is making a real effort to try to collect data and put it out there on a more real time basis, and we could probably benefit from that across more health care settings.”
Nursing Licensure Policies
Benton focused on the overarching efforts of the National Council of State Boards of Nursing (NCSBN) to establish more standardized rules for licensure policies enabling nurses to easily practice or move across state lines or collaborate in high-tech, networked delivery systems.

“We need to start to be much more creative in our workforce models that don’t just focus on a name like a ‘nurse’ or ‘physician,’ but actually think about the competencies,” Benton said. “So, having a resource that actually interfaces with multiple intensive care units, not just across a state, but potentially across several states, how do we actually plan workforce practices for some of that as well?”
“The variation between scopes of practice in different states is becoming less and less of an issue as the NCSBN introduced things like the Nurse Licensure Compact and the Model Act & Rules that are now being based on evidence rather than opinion,” Benton said. “We’re starting to see states migrating toward a more standardized approach. And we’re looking at how the pandemic drove a massive increase in the provision of services through telehealth technologies. So, the way that we start to plan a workforce for the future is not simply about the local labor market, but it’s about how that labor market will be deployed potentially more widely through, for example, the internet of things.”
Recommendations
As the session ended, Werner asked each panelist to recommend a state or federal policy change that might meaningfully address the nursing workforce issue:
- Lasater: “My policy change would be either state or federal requirements for minimum safe staffing in hospitals. I’m pretty optimistic about this because there are more and more states pushing for this legislation, including Pennsylvania where the Patient Safety Act has passed in the House and is on its way to the Senate. Also, the American Nurses Association has endorsed this legislation at the federal level, which represents a major historic shift in their position.”
- Shah Goda: “I would add on to what has been said in terms of minimum staffing ratios, perhaps also tied with some kind of funding source like increasing Medicaid reimbursement rates or having some kind of dedicated financial incentives to help companies and hospitals do that. I’m optimistic on the staffing ratios, but I don’t know if people are really having the conversations about where the funding is going to come from.”
- Frogner: “I think we need to figure out how to leverage the voice of the actual workers themselves and maybe this is where professional organizations can play a role, helping to train their members to do lobbying work and advocating for their needs. I think it’s also about getting nurses the tools they need to also take advantage of new technologies. I hate to put it back on the nurse, but they are such a large occupational group and have such power. People are listening. This is their time and their moment.”
- Benton: “For me, it’s about a long-term solution for what we know the long-term problems are going to be. If you look at the 2050 projections for the numbers of individuals we will have in the various age bands, the current model is simply not sustainable. We have to fundamentally rethink how we deliver care and educate practitioners. There are many things that policymakers could do, but they’ve got to stop using Band-Aid solutions that are only about their next election cycle instead of about the health and well-being of citizens into the future.”

Editor, Digital Publications
More ldi news.

How Well Do Fetal Care Centers Meet the Needs of Highly Complex Patients and Families?
A Penn Study Creates a Person-Centered Care Measurement Instrument

Population Health
Andy Tan to Co-Lead $9.6 Million Tobacco Communications Study
Will Evaluate the Impact of Current Government Anti-Tobacco Messaging

Penn LDI CICADA Initiative Names Researchers for 2024-2025 Cohort
Seventh Year of Program that Recruits, Mentors and Develops Junior Faculty for Health Services Research

Improving Care for Older Adults
How Do Ownership Changes Affect Nursing Home Quality?
After Acquisition, Staffing Declines Lead to a Small Negative Impact on Overall Quality
- Chris Tachibana, PhD, MS

In Their Own Words
Health Care Access & Coverage
How A Nonprofit’s Closure Could Harm Children’s Health and Threaten Many Families’ Finances
The Sudden Shutdown of Benefits Data Trust Is a Wakeup Call For Philly and Beyond, LDI Experts Write
- Aditi Vasan, MD, MSHP
- George Dalembert, MD, MSHP
- and Madeline DeMarco, MPP

Penn, Harvard and Columbia All Chose Doctors To Lead Anxious Campuses
LDI Senior Fellow Guy David Has Taught Leadership To Over 2,000 Clinicians. He Lays Out Why Doctors Can Make Great Leaders In a Stat News Op-Ed
- Guy David, PhD

University Administration
- Careers @ USA
- For Current Students
- Request Information
- Master of Occupational Therapy (MOT)
- Doctor of Occupational Therapy (OTD)
- Post-Professional Doctor of Occupational Therapy (PPOTD)
- Master of Health Administration (MHA)
- Doctor of Education (EdD)
- Graduate Certificates
- Clinical Orthopedic Residency (OCS)
- Orthopaedic Manual Physical Therapy Fellowship (OMPT)
- Continuing Professional Education (CPE)
- Doctor of Physical Therapy (DPT)
- Non-Degree Physical Therapy Online Courses
- Master of Science in Speech-Language Pathology (MS-SLP)
- Post-Graduate Nursing Certificates
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Browse All Degree-Programs
- Admissions & Aid Home
- Scholarships & Grants
- How to Apply
- Cost of Attendance
- Financial Aid
- Application Deadlines
- Academic Calendar
- Financial Aid FAQ
- Admissions FAQs
- Catalog/Handbook
- Our History
- Accreditation
- B Corp Certified
- Change of Ownership
- Student Achievement Data
- Institutional Learning Outcomes (ILOs)
- Diversity & Inclusion
- San Marcos, California
- St. Augustine, Florida
- Miami, Florida
- Austin, Texas
- Dallas, Texas
- Our Faculty
- Board of Directors

Nursing MSN & DNP
| 25 May 2021
The 2021 American Nursing Shortage: A Data Study

The United States is in the midst of a critical nursing shortage that is expected to continue through 2030. ((Edward Mehdaova, “Strategies to Overcome the Nursing Shortage,” Walden University, 2017: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=5933&context=dissertations )) In this post, we examine how this complex issue came about, what the statistics reveal, and what strategies nurses can use to move through the challenges it brings.
The Growing Nursing Shortage
“Nursing is what I was called to at a very young age, and I cannot imagine doing anything else— but I am very tired.” —Heather Josey Thomas, MSN-Ed, RN, CCRN, DNP student at USAHS
The bravery and dedication of America’s nurses have been displayed in front-page newspaper stories across the country throughout the COVID-19 pandemic. However, the pandemic has also been a huge strain on nurses and the healthcare system, due in part to limited staff and resources. The nursing shortage facing America began long before the pandemic propelled it into the headlines once again.
The United States has experienced nursing shortages periodically since the early 1900s. Multiple factors led to each shortage, from world wars to economic recessions. But the magnitude of the current nursing shortage, announced in 2012, is greater than ever before in this country. ((Linda Workman, “Confronting the Nursing Shortage,” Nurse Key: https://nursekey.com/confronting-the-nursing-shortage/ ))
Given the growing demand for healthcare services across a multitude of specialties , reports project that 1.2 million new registered nurses (RNs) will be needed by 2030 to address the current shortage. Nursing schools and graduate nursing programs are working to accommodate the rising demand for skilled nurses and nurse leaders, but they also face challenges.
Nursing Shortage Statistics
To create a visualization of the American nursing shortage, we compared each state’s population to the most recent statistics on the employment of RNs in that state to calculate the number of working RNs currently available per 1,000 residents.
How does your state rank?
Registered nurses available by state
Click on a state to reveal the statistics or use the dropdown menu below.
Why Is There a Nursing Shortage?
High demand and low supply have created the current nursing shortage, and a multitude of factors have led us to this point.
Demand Is on the Rise
As of February 2021, registered nursing was the fifth-most in-demand job in the American workforce, according to LinkedIn. ((Mike Irvine, LinkedIn Talent Blog, “The Most In-Demand Jobs Right Now,” March 15, 2021: https://business.linkedin.com/talent-solutions/blog/trends-and-research/2020/most-in-demand-jobs )) Healthcare facilities are searching for skilled RNs because they are facing increased patient demand for care.
The country has a larger population over the age of 65 than ever before in its history, composed primarily of baby boomers (those born between 1946 and 1964). This 65+ demographic has grown rapidly, jumping from 41 million people in 2011 to 71 million in 2019—a whopping 73% increase. (( Lisa Haddad et al., “Nursing Shortage,” StatPearls Publishing, Dec. 14, 2020: https://www.ncbi.nlm.nih.gov/books/NBK493175/ )) And the U.S. Census Bureau projected that number to continue to rise, estimating it will reach 73 million by 2030. ((U.S. Census Bureau, Population Division, “Projected Age Groups and Sex Composition of the Population: Projections for the United States, 2017–2060,” U.S. Census Bureau, Population Division, Sept. 2018: https://www2.census.gov/programs-surveys/popproj/tables/2017/2017-summary-tables/np2017-t2.xlsx ))
With better and more accessible healthcare, the growing population of seniors requires more health services due to age-related conditions. Lengthened lifespans stretch out the timeframe when patients require services, thus adding pressure to an already strained healthcare system.
The Retirement Drain
“When COVID hit, many people retired or were given an early retirement package… Now they are so understaffed that they are paying bonuses for people not to call out or use their vacation for the next three months.” —Beverly Banez, BSN, RN, MSN student at USAHS
The population surge from the baby boomer generation has led not only to a greater number of aging patients but also means that a large portion of the nursing workforce is heading toward retirement. Between 2000 and 2018, the average age of employed registered nurses increased from 42.7 to 47.9 years old. And nearly half (47.5%) of all RNs are now over the age of 50. ((U.S. Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis, “Brief Summary of Results from the 2018 National Sample Survey of Registered Nurses,” 2019: https://data.hrsa.gov/DataDownload/NSSRN/GeneralPUF18/nssrn-summary-report.pdf ))
A 2015 study predicted that over one million RNs will retire from the workforce between now and 2030. ((David Auerbach et al., “Will the RN Workforce Weather the Retirement of the Baby Boomers?” Medical Care , Oct. 2015: https://journals.lww.com/lww-medicalcare/Abstract/2015/10000/Will_the_RN_Workforce_Weather_the_Retirement_of.3.aspx )) As they go, they take with them their invaluable amount of accumulated knowledge and nursing experience.
It’s important to note that COVID-19 created a wave of artificial early retirements due to the extended period of limited access for both patients and staff to medical facilities. Because hospitals stopped doing elective surgeries and patients stayed away from the hospital, hospitals had less income and needed to reduce staff to stay afloat. In response, many hospitals forced furloughs on their employees, leading some people to opt to retire who wouldn’t have planned to otherwise. ((Alia Paavola, “266 hospitals furloughing workers in response to COVID-19,” Becker’s Hospital Review , Aug. 31, 2020: https://www.beckershospitalreview.com/finance/49-hospitals-furloughing-workers-in-response-to-covid-19.html ))
The Location Factor
When reviewing nursing shortage data at the state and national level, the numbers can be confusing. The Bureau of Health Workforce projects that California will face the largest nursing shortage of any state, with a projected shortfall of 44,500 nurses by 2030. In contrast, the state of Florida will have a projected surplus of more than 53,000 RNs by 2030. Looking only at states better off can lead one to falsely assume that the problem has blown over or never even existed. ((U.S. Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis, “Supply and Demand Projections of the Nursing Workforce: 2014-2030,” 2017: https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/nchwa-hrsa-nursing-report.pdf ))
Rural communities absorb greater impacts of the nursing shortage than do metropolitan areas. Only 16 percent of RNs live in rural areas, where they serve over 52 million Americans who reside there. ((Health Resources and Services Administration, National Center for Health Workforce Analysis, “The U.S. Nursing Workforce: Trends in Supply and Education,” April 2013: https://www.ruralhealthinfo.org/assets/1206-4974/nursing-workforce-nchwa-report-april-2013.pdf ))
The Educator Exodus
Nurses need to be taught by other nurses. As the average age of the RN population has increased, so has the age of RNs who have stepped into the role of educator. They, too, are looking toward retirement, leaving nursing schools without a strong pipeline of teachers to take their place.
According to the American Association of the College of Nursing, faculty shortages at nursing schools across the country are limiting student capacity. Budget constraints, an aging faculty, and increasing job competition from clinical sites have contributed to this crisis. ((American Association of Colleges of Nursing, “Nursing Faculty Shortage,” https://www.aacnnursing.org/news-data/fact-sheets/nursing-faculty-shortage )) As a result of the ongoing decrease in faculty numbers, fewer nursing graduates will be joining the workforce.
Stress of the Job
The heightened stress levels of today’s nurses are due to more than just the pandemic, more than just the need to make urgent life-altering decisions, and more than just working long hours. It is all of these things and more, combined, that weigh on the shoulders of many RNs.
Ongoing budget tightening has led many healthcare facilities to cut staffing levels, leaving a major imbalance in the workloads for remaining nursing staff. This has been especially true during the pandemic. Many hospital employees were asked to move from their usual departments and roles to assist with the intensive care of COVID-19 patients. (( Nancy Cleeland, “Hospitals Face Staffing Shortages, Reduced Budgets in Coronavirus Pandemic,” SHRM, April 7, 2020: https://www.shrm.org/resourcesandtools/hr-topics/employee-relations/pages/hospitals-face-staffing-shortages-reduced-budgets-in-coronavirus-pandemic.aspx )) Most nurses are dedicated to helping patients however they can; however, it’s stressful to be thrown into a new area of nursing on short notice—especially an area as demanding as critical care.
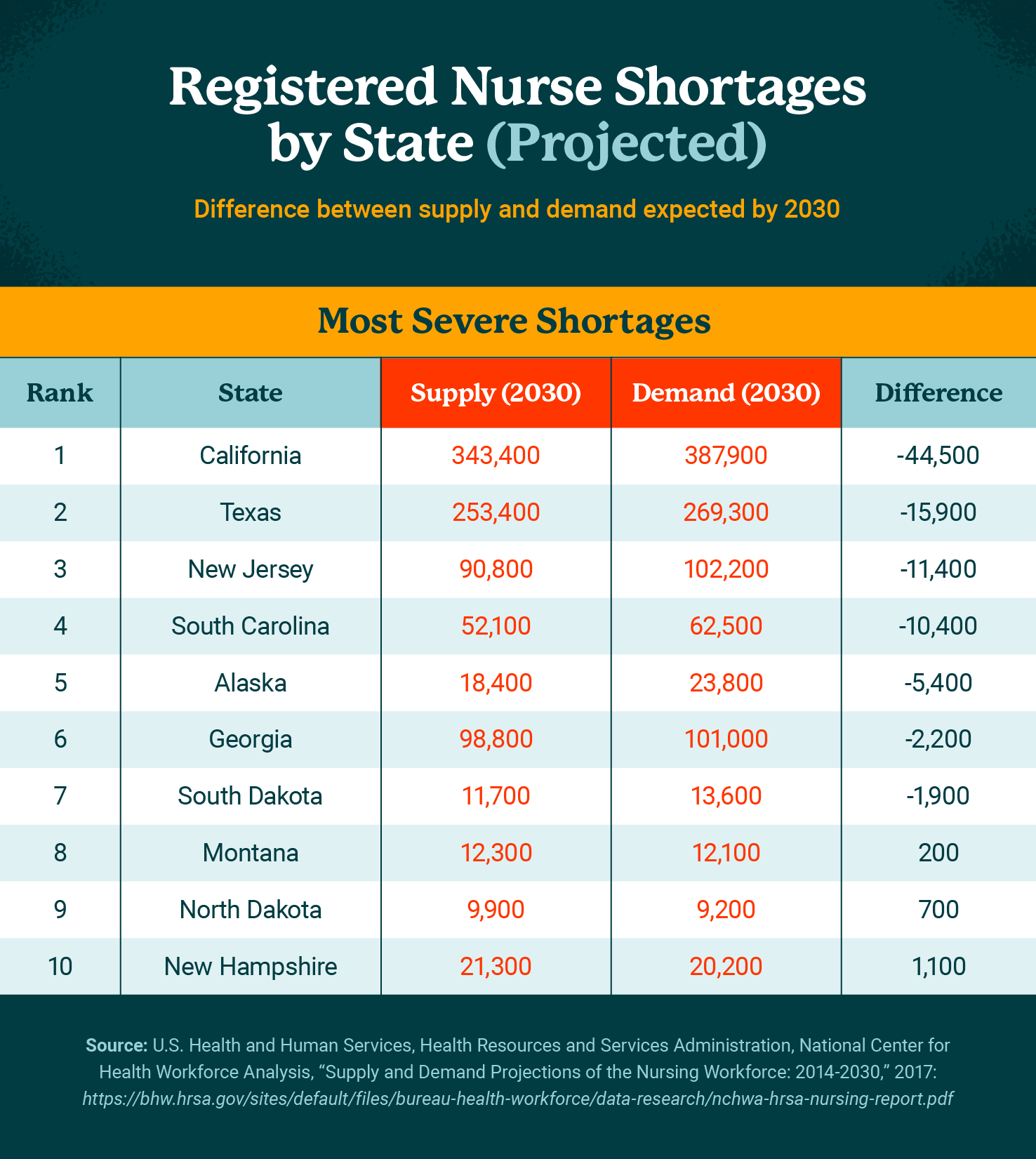
The Impact of the Nursing Shortage
Source: Pascale Carayon and Ayse Gurses, “Chapter 30: Nursing Workload and Patient Safety—A Human Factors Engineering Perspective,” Patient Safety and Quality: An Evidence-Based Handbook for Nurses: https://www.ncbi.nlm.nih.gov/books/NBK2657/
The shortage of skilled nurses entering and staying in the workforce affects both patient care and other healthcare workers on the team. Nurses are so important to healthcare delivery that any challenge they face impacts us all.
Higher Risk of Nurse Burnout
“I have missed kids’ school events, I have been short-tempered when I shouldn’t have been, and I have compromised my own health at times due to my inability to say ‘no’ to the extra shifts even on days when I knew I should.” —Heather Josey Thomas
Overwhelmed frontline-working RNs have been running a constant risk of developing nurse burnout . The phrase struggles to encompass the depth of the physical and emotional exhaustion nurses experience as the result of heavy workloads, long hours, and the stress of treating critically ill patients.
Pandemic or not, having fewer nurses available to spread the workload is guaranteed to add layers of stress onto other staff. The weight of life-altering decisions needing to be made on a constant basis and the knowledge that there is never enough time to provide your patients can undermine staff efficacy and exacerbate personnel shortages.
Higher Risk of Medication Errors and Deaths
A 2019 study revealed that a patient’s risk of post-care-associated infection increased by 15% in facilities with low hospital staffing levels. ((Jingjing Shang et al., “Nurse Staffing and Healthcare-Associated Infection Unit-Level Analysis,” The Journal of Nursing Administration, May 2019: https://pubmed.ncbi.nlm.nih.gov/31008835/ )) Another study conducted in California correlated an 8.9% decrease in pneumonia infections among surgical patients to an increase of one additional work hour per patient per RN. ((Pascale Carayon and Ayse Gurses, “Chapter 30: Nursing Workload and Patient Safety—A Human Factors Engineering Perspective,” Patient Safety and Quality: An Evidence-Based Handbook for Nurses: https://www.ncbi.nlm.nih.gov/books/NBK2657/ ))
Longer Wait Times and Shorter Visits
The fewer staff members available at a given facility due to the nursing shortage, the longer patients must wait to be seen by the staff on site. And with more and more patients coming for medical assessments and treatments due to the aging U.S. population, extensive wait times and brief visits with the nurse and doctor become more and more typical.
Solutions for the Nursing Shortage
For such a complex problem, there is no simple solution. But there are strategies and practices that we can examine and put into play today. Advances in nursing education, in the workplace, and at the policy level may spark the change we need.
Greater Access to Education
“I hope that more people choose nursing as a career and that I can continue to be involved in teaching and growing them. After all, they will be the ones caring for me and my family someday!” —Heather Josey Thomas
Education is the bedrock for growing the population of skilled nurses. Creating programs that incentivize students to enroll in nursing school, complete their studies, and continue their education to up-level their skills and careers is one strategy for increasing enrollments. Registered nurses with a Bachelor of Science in Nursing (BSN) degree typically have stronger job prospects than nurses without the degree.
Naturally, encouraging nurses to earn their graduate-level credentials, such as a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) degree, will add to the pool of highly skilled nurses and improve patient outcomes. Nurses with graduate degrees can serve in leadership roles , in advanced levels of patient care, or as educators themselves.
Flexible options for schooling, such as online programs, are critical to recruiting and retaining engaged students—especially working nurses who need to fit school into their busy schedules.
Strategic Workplace Accommodations and Flexibility
“The hospital where I work part-time as a direct-care ICU nurse hired many travelers and/or agency staff. They also offered a huge COVID differential, essentially doubling everyone’s hourly salary, but eventually, even that couldn’t entice people to come in to work extra shifts because we were just so tired.” —Heather Josey Thomas
Nurse executives are responsible for creating a workplace culture that supports nursing staff and entices experienced nurses to remain on staff. For example, beyond simply improving compensation and benefits packages, executives can empower nurses to create their own schedules and reward senior nursing staff for mentoring new nurses; programs like this can have a major impact on employee retention at a time when it’s needed most.
As modern technology continues to shape healthcare delivery, the flexibility of telehealth and travel nursing creates new paths for some nurses to continue doing their good work in creative ways. Increased opportunities for career development and growth in nursing will help maintain nursing as an attractive, desirable job opportunity.
Lobbying and Advocacy
Everyone who benefits from the skilled hands and minds of RNs across the country should be encouraged to advocate during the policymaking process at both the state and federal levels. For example, the American Nursing Association (ANA) currently works with legislators on a variety of key topics, such as workplace health and safety, appropriate staffing, and reducing gun violence. The ANA even provides an RN Activist Toolkit to help get you started. ((American Nursing Association, “Federal Issues”: https://www.nursingworld.org/practice-policy/advocacy/federal/ ))
Opportunities Created by the Nursing Shortage
“The nursing shortage gave me a chance to work in another department for better hours and for a new experience.” —Beverly Banez
Thankfully, the current nursing shortage has a positive side: opportunities for career growth. The healthcare industry is considered to be recession-proof, which translates to potential long-term job security.
- According to U.S. News & World Report’s list of the 100 Best Jobs in America for 2021, nurse practitioner takes third place as an optimal career path. In fact, 13 of the top 20 Best Jobs are in the healthcare field, including speech-language pathologist (#7) and occupational therapist (#19). ((U.S. News & World Report, “100 Best Jobs,” 2021: https://money.usnews.com/careers/best-jobs/rankings/the-100-best-jobs ))
- Opportunities for nurse educators abound. A report from the American Association of Colleges of Nursing in 2018 found that 56% of the educational institutions they surveyed had full-time vacant teaching positions open. ((American Association of Colleges of Nursing, “Special Survey on Vacant Faculty Positions for Academic Year 2018-2019,” 2018: https://www.aacnnursing.org/Portals/42/News/Surveys-Data/Vacancy18.pdf ))
No healthcare system can function without skilled nurses. Nursing shortages are being documented around the globe, with a recent report from the World Health Organization noting that the world may be short 5.7 million nurses by 2030. ((Mackenzie Bean, “World may be short 5.7M nurses by 2030: 4 report takeaways,” Becker’s Hospital Review, April 9, 2020: https://www.beckershospitalreview.com/nursing/world-may-be-short-5-7m-nurses-by-2030-4-report-takeaways.html )) The United States’ experience with the pandemic has placed the reality of our current nursing shortage into the spotlight. With a better understanding of what challenges the shortage brings, how we can improve the situation, and how nurses can take advantage of the opportunities it brings, we can hope to shift the tide.
The University of St. Augustine for Health Sciences (USAHS) offers a Master of Science in Nursing (MSN) program, a Doctor of Nursing Practice (DNP) program, and Post-Graduate Nursing Certificates designed for working nurses. Our degrees are offered online, with optional on-campus immersions.* Role specialties include Family Nurse Practitioner (FNP), Nurse Educator,** and Nurse Executive. The MSN has several options to accelerate your time to degree completion. Earn your advanced nursing degree while keeping your work and life in balance. *The FNP role specialty includes two required hands-on clinical intensives as part of the curriculum. **The Nurse Educator role specialty is not available for the DNP program.
ARE YOU INSPIRED?
There could be an article about you here one day. Take charge of your own life-story!
Take charge of your own life-story
More Nursing MSN & DNP Articles

Dr. Elisabeth McGee Discusses USAHS’ Driving Role in Future-Focused Healthcare

Nurse Practitioner vs. Physician Assistant: Key Differences
85 Nursing Quotes: Words of Wisdom for Nurses
Upcoming nursing msn & dnp events.

Post Professional Doctor of Occupational Therapy (OTD) Webinar - September 10 | USAHS

Occupational Therapy Programs (OTD, OTD Flex, MOT, & MOT Flex) - Admissions Webinar - September 16 | USAHS

Doctor of Physical Therapy (DPT) - Admissions Webinar - September 17 @ 4:00 pm PDT
The Nursing Shortage and Work Expectations Are in Critical Condition: Is Anyone Listening?
- Standard View
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Annette M. Bourgault; The Nursing Shortage and Work Expectations Are in Critical Condition: Is Anyone Listening?. Crit Care Nurse 1 April 2022; 42 (2): 8–11. doi: https://doi.org/10.4037/ccn2022909
Download citation file:
- Ris (Zotero)
- Reference Manager
Working conditions have worsened for many nurses and health care professionals across the globe during the COVID-19 pandemic. 1 – 3 During the Omicron wave, the US Department of Health and Human Services has reported critical staffing shortages in 24% of US hospitals, 4 and military medical personnel have been deployed to assist hospitals in at least 8 states. 5 As I write this editorial in January 2022, health care workers have also been asked to return to the work setting 5 days after testing positive for COVID-19. Consequently, many nurses are working 12-hour shifts with an increased patient load, increased patient acuity, and, for some, added mandatory overtime while recovering from illness. These expectations are not reasonable.
- The Reality
Nurses and other health care workers have been saddled with the burden of the pandemic by first being asked to work in unsafe conditions without proper protective personal equipment and then asked to work in crisis mode after crisis mode, as the various waves of the pandemic hit. 6 And the pandemic is not over. How much more can nurses and other health care professionals be asked to take on? I speak mostly about nurses because this journal is Critical Care Nurse , yet I recognize that nurse leaders, physicians, and other allied health providers are also exhausted and working in crisis mode.
In late January 2022, the incidence of Omicron in US communities is beginning to fall, yet many hospital systems remain burdened by unprecedented high patient volumes and COVID-19–related deaths. Hospital-acquired infections, pressure injuries, and patient falls have increased since the pandemic began. 7 These adverse outcomes are a consequence of the current work environment—a health system issue. Some nurses who may have cared for 2 critically ill patients in the past are now being asked to care for 3 or 4 critically ill patients. Anyone who has worked at the bedside in critical care knows these high staffing ratios are a recipe for failure. 8 , 9 Nurses cannot provide optimal care if they are assigned to too many patients. Some patients may not receive all of the necessary elements of evidence-based care, and some patient needs will not be attended to. This situation is not the fault of the nurse—it is a system failure.
The ideal nurse-to-patient ratio can change instantly, especially in critical care. Patients in the intensive care unit (ICU) have fluctuating requirements; they need a nurse who has flexibility in their assignment and is available to run to their room when they have a critical need. The American Association of Critical-Care Nurses (AACN) developed the Synergy Model to illustrate the importance for patient needs to drive nurse competencies. 10 Appropriate staffing is much more than just a number.
Consider a nurse who may have 3 critically ill patients. This situation can be difficult to manage even if all 3 patients remain stable. What happens if one patient’s blood pressure becomes unstable? This scenario is common in critical care and can involve a large amount of nursing time to assess the cause, alert other health care providers, determine the appropriate interventions, and perform or assist with diagnostic testing and/or interventions to monitor and stabilize the patient. This sudden change in workload takes a lot of time and energy. While the nurse is busy stabilizing this patient, who is looking after the other 2 patients? If every nurse has a high patient load, who has flexibility to assist other patients or other nurses during times of critical need? In health care, we may have little or no control over the timing of critical needs or adverse patient events.
Not all patient needs are critical, but they are all important. For example, a patient who is intubated and ventilated may be scared and anxious. Leaving this patient in a room by themselves for extended periods of time without someone there to reassure them that everything will be OK—is that the kind of health care environment we want? There is little flexibility in the system when nurses are overassigned. This situation can be incredibly stressful for the nurses and extremely unsafe for the patients. Natasha Williams, an emergency department nurse in New York City, said she felt like she was “being pulled in too many directions at once.” These constant interruptions may also lead to unsafe work environments. 11
Insufficient staffing levels were associated with poor outcomes before the pandemic. 8 , 9 A study of 422 730 surgical patients in 9 European countries showed that patients were more likely to die within 30 days of admission when the nurses’ workload was increased by 1 patient. 12 This study included hospitalized patients with common surgical diagnoses and did not appear to include ICU staffing. If 1 extra patient per nurse on a medical/surgical unit can affect mortality, imagine the implications of adding 1 or 2 patients to the assignment of an ICU nurse.
Global health care staffing costs are projected to reach $47.8 billion by 2026. 13 Some hospitals have started cutting nursing hours to save money, but excellent health care costs money. I am not just referring to the cost of nurses’ salaries, but the cost of adequate and safe staffing levels. We should not allow our institutions to use terminology such as nonproductive time to refer to the valuable time spent by nurses obtaining professional development such as learning how to use a new medical device or working on collaborative evidence-based practices. 14 Just because the nurse is not physically touching a patient, it does not mean that their work is not important. Thinking and educational time is valuable. Nurses need to make critical lifesaving decisions. The public and our health care institutions must be prepared to spend the money necessary to obtain the kind of health care that is expected and desired. No one wants to be on a discount budget plan when they are a patient in the ICU. An inadequate staffing budget can lead only to poor outcomes.
Many nurses are angry and leaving the profession early. Jessica Fink left ICU nursing to focus more on preventative, primary care. 15 She said, “I worry for America’s nurses, and I am angry. The problems they face are inflicting a deep and lasting wound.” 15 As the public gets angry about pandemic issues such as delayed elective surgeries, they need to realize that these delays are caused by systems in crisis. Hospitals in almost half of the US states postponed surgeries during the Omicron wave. 16 If customers are angry about long waiting times for hospital admission or delayed and canceled surgeries, they should also be upset and angry about the type of work environments that nurses are currently working in. If our customers want to receive excellent health care for themselves and their loved ones, they need to support changes to the nursing work environment, such as safe and flexible nurse-to-patient ratios and healthy work environments. I think customers expect safe and appropriate staffing in health care.
Prepandemic research identified 2 major reasons for understaffing of nursing care: (1) poor workplace conditions and (2) inadequate staffing models and flexibility. 17 Dr Linda Aiken, a top researcher on nursing workforce issues, blames inadequate staffing on lack of government legislation, especially at the state level 17 ; she believes that states can assist by mandating staffing ratios. Dr Mary Ann Fuchs, president of the American Organization for Nursing Leadership, says that decisions around flexible staffing should be driven by professional nursing judgment. 18 According to Dr Fuchs, 18 “To truly commit to patient safety—always the number one priority— nurses[,] not legislators[,] need to be empowered with flexibility to determine appropriate staffing for the needs of their patients.” Dr Aiken also highlights the importance of nurses and says that “health care leaders must fund enough positions for nurses and create reasonable working conditions so that nurses will be there to care for us all.” 17
Policies must be in place to help safely manage nurse-to-patient ratios. It is one thing to say that health care systems can adjust staffing as needed during times of crisis, but when the crisis continues 2 years after the start of the COVID-19 pandemic, enough is enough. Nurses and other health care professionals are human. As they have cared for all of us, many nurses have fallen ill with COVID-19 and too many nurses have died. Some of the nurses are still recovering. We tell nurses to look after themselves to maintain health and resiliency, but how can they do that when their scheduled days off are canceled due to mandatory overtime or they are begged to come into work on their days off? Nurses cannot authentically engage in self-care if they feel guilty about saying no to working when their colleagues are short staffed and overworked. Many nurses are exhausted and our system is failing them. We cannot afford to lose or harm more nurses. Action needs to happen and it needs to happen soon because our health care system is in crisis.
- Is Anyone Listening?
The answer is Yes! Although I have written about some of the deplorable realities of the current work conditions for many nurses around the globe, I feel hopeful that meaningful and substantive changes will be made to nurse staffing and healthy work environments. We have seen positive changes during the pandemic such as enhanced, interdisciplinary teamwork and expansion of the scope of practice for advanced practice nurses. 1 AACN and other organizations such as the American Nurses Association (ANA), American Organization for Nursing Leadership, Healthcare Financial Management Association, and the Institute for Healthcare Improvement are collaborating to develop strategies for positive change in the health care environment. 19 These organizations will work hard to push for action in a timely manner.
Hopefully, by the time you read this editorial, many nurses will have joined ANA’s initiative to send a strong message to state representatives in Congress. 20 The ANA letter states that “… it’s time for Congress and the Administration to take concrete steps towards finally addressing the nursing shortage to ensure that we have a robust workforce now and in the future.” 20 Nurses can personalize their message to describe the difficult work situations they have been enduring.
We need to create an environment in which nurses can autonomously use their nursing skills at the highest level. We need to create a system where nurses want to work and feel proud about the excellent care that they can deliver. Great health care costs money, and that money should be spent where it is most needed, at the bedside.
Nurses, if you are asked what you would like for Nurses Week in May, I suggest asking one of your hospital administrators to shadow a critical care nurse for a day. This exercise may lead to administrators gaining a greater understanding of the nursing role and the extraordinary demands being placed on nurses.
We have an opportunity to create change, so let us make it happen and soon—before we lose or harm more nurses and other health care professionals. As AACN president Beth Wathen 21 says, “The future of nursing starts now.”
To purchase electronic and print reprints, contact the American Association of Critical-Care Nurses, 27071 Aliso Creek Rd, Aliso Viejo, CA 92656. Phone, (800) 809-2273 or (949) 362-2050 (ext 532); fax, (949) 362-2049; email, [email protected] .
The statements and opinions contained in this editorial are solely those of the Editor.

- Previous Article
- Next Article
Data & Figures

Supplements
Email alerts, affiliations.
- About Critical Care Nurse
- CE Articles
- Individual Subscriptions
- Institutional Subscriptions
- Sign up for Alerts
- Submit an Article
- Online ISSN 1940-8250
- Print ISSN 0279-5442
- AACN Advanced Critical Care (ACC)
- American Journal of Critical Care (AJCC)
- Critical Care Nurse (CCN)
- AACN Membership
- Privacy Policy
- Advertising
- Permissions
- Tel: (800) 899-1712
- Tel: (949) 362-2000
- Cookie Policy
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright 2024 American Association of Critical-Care Nurses
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Data, AI, & Machine Learning
- Managing Technology
- Social Responsibility
- Workplace, Teams, & Culture
- AI & Machine Learning
- Diversity & Inclusion
- Big ideas Research Projects
- Artificial Intelligence and Business Strategy
- Responsible AI
- Future of the Workforce
- Future of Leadership
- All Research Projects
- AI in Action
- Most Popular
The Truth Behind the Nursing Crisis
- Coaching for the Future-Forward Leader
Measuring Culture
Our summer 2024 issue highlights ways to better support customers, partners, and employees, while our special report shows how organizations can advance their AI practice.
- Past Issues
- Upcoming Events
- Video Archive
- Me, Myself, and AI
- Three Big Points

The Real Issues Driving the Nursing Crisis
Our analysis of nurses’ employer reviews reveals the true source of burnout and why nurses are leaving the field. here’s how health care leaders can improve nurse job satisfaction to fight a looming nursing shortage..
- Workplace, Teams, & Culture
- Talent Management
- Organizational Behavior

Health care leaders face a daunting set of challenges — rising costs, the transition to digital health, and shifting payment models, to name just a few. But according to a recent survey from the American College of Healthcare Executives, the No. 1 problem hospital CEOs face is staff shortages and burnout. 1 Ninety percent of the CEOs surveyed cited nursing shortages as a particularly acute pain point.
In 2021, the total number of registered nurses working in the U.S. dropped by the largest amount in 40 years, with younger nurses leading the exodus. 2 By 2025, the U.S. health care system could suffer a shortfall of up to 450,000 nurses, or 20% fewer than the nursing workforce required for patient care. 3
Get Updates on Transformative Leadership
Evidence-based resources that can help you lead your team more effectively, delivered to your inbox monthly.
Please enter a valid email address
Thank you for signing up
Privacy Policy
High levels of job dissatisfaction and burnout are driving nurses from the profession. The COVID-19 pandemic placed tremendous pressure on all health care workers, but dissatisfaction and burnout among nurses have not improved since the pandemic ended. And by some measures, it might be getting worse: In 2021, nearly two-thirds of registered nurses would have encouraged others to become a nurse, but only half said they would recommend nursing as a profession two years later. 4
One of the richest sources of insight on dissatisfaction among nurses is how they describe their job, in their own words, on employment sites like Indeed and Glassdoor. This information is voluminous but difficult to synthesize because most of it takes the form of unstructured free text. To understand the challenges nurses face, we analyzed how 150,000 of them had described their employers in Glassdoor reviews since the beginning of the pandemic. (See “The Research.”) In this article, we share key insights from that analysis and offer advice to health care leaders about how they can address nurses’ most pressing issues.
Health Care Leaders Are Out of Touch
Nurses view their managers as out of touch with the daily realities of patient care. We categorized their comments about managers into nearly 50 leadership traits. The second most frequently cited trait described managers as being unaware of the challenges that nurses struggle with in the workplace. When nurses discussed how managers understood life at the bedside, their comments were negative 9 times out of 10.
Nurses are particularly critical of members of the senior executive team for their disconnectedness. The top team was 10 times more likely than front-line supervisors and middle managers to be criticized for being out of touch. Our results reinforce a separate survey in which nearly half of hospital nurses said they believe management does not listen to their concerns. 5
To address dissatisfaction and burnout, health care leaders must first understand what’s happening at the bedside. This can be challenging, particularly in large health care systems with thousands of nurses working across multiple sites and specialties.
Historically, leaders have struggled to systematically analyze the gold mine of insights into nurses’ frustrations that can be gleaned from their comments in employee surveys or external reviews. Reading, understanding, and analyzing huge volumes of unstructured textual data has simply not been practical. However, recent advances in artificial intelligence make it possible to identify deep patterns in large bodies of text and understand feedback at scale. Leaders can now mine free text to gain a nuanced understanding of the issues driving dissatisfaction and burnout among nurses and use that insight to improve life at work for their nursing staffs. (See “Getting Started With Text Analytics.”)
Identify Relative Strengths and Opportunities Through Benchmarking
Nursing satisfaction varies widely across employers. We identified 200 of the largest health care employers in the United States, including hospitals and health care systems, home health care providers, operators of senior living facilities, and staffing agencies. For each employer, we calculated how highly nurses rated the organization and senior leadership on Glassdoor from the beginning of the COVID-19 pandemic through June 2023. 6
Among large employers, nurses’ Glassdoor ratings ran the gamut from poor (2.6) to nearly perfect (4.9) on a 5-point scale. Nurses’ assessments of how well senior leadership has performed during and after the pandemic were even more varied, ranging from 2.1 to 4.9 on the same 5-point scale. The wide variance in Glassdoor ratings is consistent with a separate survey in which the percentage of dissatisfied nurses ranged from 2% to 48% across 60 U.S. hospitals. 7
Employees of the 200 large health care organizations can use our interactive tool to see how their organization ranks against others. The index is sortable by nurses’ overall ratings, their assessments of the top leadership, and the four most powerful predictors of nurses’ satisfaction: compensation, workload, organizational support, and toxic culture.
Nurses who work for staffing agencies (who are sometimes referred to as travel nurses) are, on average, much more satisfied than other nurses. The five highest-ranked employers in our sample (and six of the top 10) are staffing agencies.
Higher compensation, of course, accounts for part of this difference, but not all of it. We compared how positively nurses working with staffing agencies spoke about 200 topics compared with their counterparts employed by hospitals and health care systems. (See “Staffing Agencies Rate Better on Many Key Factors.”) While compensation was viewed more favorably by agency nurses, issues around solving nurses’ problems and open, honest communication had a larger sentiment gap between the two groups. By focusing on nurses as clients, staffing agencies excel at practices that improve satisfaction beyond simply paying higher wages. Other health care leaders can learn from their example, and we’ll make some concrete recommendations below.
Prioritize Drivers of Job Satisfaction
To understand the drivers of job satisfaction among nurses, we analyzed the free text of all reviews that had been written by the nurses in our sample since the beginning of the COVID-19 pandemic and classified the text into nearly 200 topics. 8 We then clustered topics into two dozen broader themes and used those themes to predict nurses’ overall ratings of their employers. We then compared each theme’s relative importance in predicting ratings. (See “Top and Bottom Predictors of Nurses’ Job Satisfaction.”)
Compensation was the top predictor of satisfaction among nurses reviewing their current employer, which is not surprising, given that inflation eroded the purchasing power of take-home pay during the period we analyzed. The importance of workload, the second-most-important driver, jibes with findings from a separate large-scale survey that found insufficient staffing was the strongest predictor of nurses’ job dissatisfaction, burnout, and intent to quit. 9
Workload and compensation are root causes of the nursing crisis that must be addressed, but they are not the only factors influencing nurses’ job satisfaction. Our analysis surfaced other aspects of the work environment, including toxic culture, organizational support, work schedules, communication, and learning and development opportunities, that leaders can focus on to improve nurses’ work lives.
This analysis also highlights areas that are unlikely to move the needle in improving the workplace experience for nurses. Perks are nice, but they will not compensate for a punishing workload or wages that fail to keep pace with inflation. Highlighting the corporate mission to promote patient health won’t help much either. Nurses already know that their job serves a higher purpose; that’s why most of them became nurses in the first place.
Mine Free Text for Actionable Insights
Many health care organizations rely on annual employee surveys, with dozens of items rated on a 5-point scale and a few open-ended questions tacked on as an afterthought. Faced with a long list of multiple-choice questions, employees are prone to switching to autopilot and assigning similar scores to very different items. The choice of questions constrains what employees can discuss, and there is seldom room to expand on why they chose a particular numeric response.
Open-ended, free-text feedback provides a rich source of nuanced and actionable insights. When nurses can decide which topics to write about, they use their freedom to discuss what matters most to them. Open-ended questions provide nurses with the space to expand on their concerns in their own words, offer crucial context, and propose concrete and actionable fixes to the problems they face. Individual free-text responses can be aggregated into broader themes to prioritize where leaders could focus their attention and limited resources to achieve the largest improvements in nurses’ satisfaction.
While organizational averages are useful, it is important to remember that distinctive subcultures can coexist within the same organization. This is particularly true among large health care systems that have grown through mergers and acquisitions. One national hospital chain, for example, has ratings that range from 1.9 to 3.9 across nearly 50 sites. Rather than relying on organizational averages alone, health care leaders must measure and analyze differences across locations, departments, functions, teams, and individual leaders.
Women, underrepresented minorities, and older employees can also experience organizational culture very differently from other employees. 10 It’s crucial to understand the drivers of job satisfaction and burnout across diverse employee populations.
It’s crucial to understand the drivers of job satisfaction and burnout across diverse employee populations.
Leaders can mine the free text for detailed insights about the most critical pain points for specific groups and tailor their interventions accordingly. Schedules, for example, have a significant impact on nurses’ job satisfaction, but which aspects of scheduling matter most will depend on the specific position. Flexibility in scheduling shifts and the ability to take uninterrupted work breaks is very important for nurses in hospitals and primary care practices, while home health care nurses place a premium on predictable schedules. 11
Nurses’ comments provide a treasure trove of practical suggestions to improve the workplace and patient care. The Glassdoor reviews we studied, for example, include dozens of actionable suggestions for how employers can improve scheduling. Some are easy-to-implement actions, such as using an app to make it easier to pick up or swap shifts, or paying a $20 to $50 bonus to nurses who pick up shifts at the last minute. Others are more systemic changes, like including nurses on a committee established to set schedules or ensuring that employees who receive tuition assistance are able to schedule work around their classes.
Listen to Nurses Who Leave Your Organization
Most organizations limit their surveys to current employees. Exit interviews are administered haphazardly, if at all, and the feedback from former employees is too often dismissed as the rantings of malcontents. But ignoring feedback from former employees is a big mistake.
Interviewing or surveying former employees can surface the reasons for their departure and pinpoint the most effective actions to retain talent. Free of the threat of retaliation, nurses who are leaving (or have left) an organization are more likely to provide candid feedback, even about taboo issues that current employees are reluctant to discuss. By collecting feedback from those who have left, organizations can uncover potential blind spots.
More than one-third of the Glassdoor reviews in our sample were written by former employees and provide insights on what mattered most to nurses who voted with their feet. 12 The bars on the left side of the figure “Top and Bottom Predictors of Nurses’ Job Satisfaction” rank the factors that predict how nurses who quit rank their former employers, and it sheds light on a critical reason nurses might head for the exits.
In an earlier article , we argued that five behavioral attributes — disrespectful, noninclusive, unethical, cutthroat, and abusive — mark an organizational culture as toxic. 13 Among nurses who quit, toxic culture is more than twice as predictive of their overall satisfaction than compensation or workload. The importance of toxic workplaces among nurses who quit is consistent with earlier research that found toxicity to be the strongest predictor of industry-adjusted attrition during the first six months of the Great Resignation. 14
Toxic culture has become more important for nurses in the post-pandemic era. When we compared which factors best predict how nurses rated their employer before and after the pandemic, toxic culture experienced the largest gain in relative importance post-COVID-19 (followed by workload, well-being, and compensation). If your organization suffers from cultural toxicity, another article of ours, “ How to Fix a Toxic Culture ,” presents several evidence-based interventions health care leaders can use to detox their own organization.
Learn From Staffing Agency Practices
As the figure “Staffing Agencies Rate Better on Many Key Factors” shows, nurses are very positive about the processes staffing agencies have in place to resolve problems quickly and efficiently. Of nurses who mentioned the efficiency of staffing agencies’ processes, 75% were positive, compared with 23% expressing positive sentiment for health care systems. For travel nurses, common process issues include onboarding, obtaining required credentials and licenses, contract negotiation, and reimbursement. The best staffing agencies listen to feedback, develop a deep understanding of the typical problems travel nurses face, and optimize their work processes to address these issues.
Many of the pain points encountered by staff nurses will differ from those of agency nurses. Health care systems, home health agencies, and long-term care providers could, however, adopt a similar approach to capture and analyze nurses’ feedback, prioritize the most common and frustrating challenges they face, and work with staff members to address these issues.
Consistently listening to and acting on feedback can also build trust with the nursing staff. Staffing agency nurses are more positive about having the psychological safety to speak up about difficult issues and be heard than are nurses working in hospitals and health care systems.
The benefits of psychological safety are blunted, however, if management is slow to respond to issues that nurses raise. Nurses speak highly of how quickly staffing agencies respond to their questions and concerns. In contrast, nurses frequently complain that other types of employers are slow to respond to emails raising issues, if they get a reply at all. Nurses also place a high value on having multiple channels of communication with their supervisors, including text, email, Facebook, Jabber, and a 24/7 hotline.
Another insight from our research is that nurses value honesty and transparency. They understand the challenges health care faces as well as anyone, and they expect honest communication about what is happening in the organization, how it affects them, and why decisions were made. Triage, a staffing agency and the fourth most highly rated large employer we studied, places honest communication at the center of its value proposition: “We tell it like it is so you won’t be surprised by how it goes.” 15
Health care systems can learn from staffing agencies, but they can also leverage their own distinctive advantages to attract and retain nurses. Nurses in full-time staff positions rate hospitals and health care systems higher than staffing agencies on three important aspects of organizational life: learning and development (including promotion opportunities and reimbursement for training), benefits, and colleagues. Those three factors are among the top 10 predictors of how nurses rate their employers. Health care systems should invest in their comparative advantages and emphasize them when communicating their value proposition to potential and current employees.
Health care systems can learn from staffing agencies, but they can also leverage their own distinctive advantages to attract and retain nurses.
Translate Feedback Into Action to Build Trust
It’s one thing to collect employee feedback, but it’s another to consistently act on those insights. Employees are less likely to surface issues or propose potential solutions if they believe that managers will not act. 16 Worse yet, employees are more likely to quit if they believe that management lacks the power, resources, or interest to make changes based on their suggestions. 17 Nearly half of nurses believe that management will not fix problems that clinical staff members bring to their attention. 18
Organizations need to put in place structures to consistently act on employee feedback. One well-known example is Kaiser Permanente’s unit-based teams (UBTs), which consist of clinical staff members and managers who regularly work together in a specific unit or department. 19 The teams, which meet at least once per month, are responsible for their unit’s performance and are co-led by a manager, a labor representative, and, typically, a clinical staff member.
The UBTs identify opportunities to improve along four dimensions: quality (including patient outcomes), patient service, affordability, and employee experience. The teams use employee feedback to identify and prioritize improvement opportunities. Next, the teams develop and test solutions using best practices and evidence-based methods. Once a solution has been deemed effective, it is implemented across the unit, department, or, in some cases, the entire organization. The UBTs then monitor the impact of these changes in terms of patient outcomes, employee satisfaction, and cost reduction.
Our study of 150,000 reviews written by U.S. nurses since the onset of COVID-19 reveals wide variation in how nurses rate their employers as a whole, and specifically in terms of compensation, workload, toxic culture, and organizational support — the four factors that most shape nurses’ job satisfaction. In our view, this variation offers a message of hope. Despite the structural challenges that all health care organizations face, it is possible to provide an environment where nurses look forward to going to work every day.
Many organizations, including some of the largest employers of nurses, have significant room for improvement. These rankings are not designed to “name and shame” but rather to make health care leaders aware of the magnitude of the gap between their organization’s performance and what is possible when it comes to providing a healthy workplace for nurses. We also hope that the objective data on how health care organizations rank on factors that matter most to nurses can provide their leaders with the impetus to make improvements and the evidence to convince all stakeholders of the urgent need for change.
Related Articles
What leaders should not do is ask nurses to work harder and endure more frustration and stress while failing to understand and address the organizational factors that make life miserable for many of them. Leaders who continue business as usual should not be surprised when staff members quit, workers unionize, and state and federal legislators dictate regulations to protect the interests of nurses.
To improve the work lives of nurses, and indeed all health care workers, leaders must collect and act on their feedback, recognizing that different parts of the organization and different populations will face distinctive challenges and issues. Listening to nurses demonstrates that there are meaningful steps health care leaders can take to fix the nursing crisis. The single most important step is to listen to them in the first place.

About the Authors
Donald Sull ( @culturexinsight ) is a senior lecturer at the MIT Sloan School of Management and a cofounder of CultureX. Charles Sull is a cofounder of CultureX.
1. “ Survey: Workforce Challenges Cited by CEOs as Top Issue Confronting Hospitals in 2022 ,” American College of Healthcare Executives, Feb. 13, 2023, www.ache.org.
2. D.I. Auerbach, P.I. Buerhaus, K. Donelan, et al., “ A Worrisome Drop in the Number of Young Nurses ,” Health Affairs Forefront, April 13, 2022, www.healthaffairs.org.
3. B. Martin, N. Kaminski-Ozturk, C. O’Hara, et al., “ Examining the Impact of the COVID-19 Pandemic on Burnout and Stress Among U.S. Nurses ,” Journal of Nursing Regulation 14, no. 1 (April 2023): 4-12; and G. Berlin, M. Lapointe, M. Murphy, et al., “ Assessing the Lingering Impact of COVID-19 on the Nursing Workforce ,” McKinsey & Co., May 11, 2022, www.mckinsey.com.
4. R.A. Smiley, R.L. Allgeyer, Y. Shobo, et al., “ The 2022 National Nursing Workforce Survey ,” Journal of Nursing Regulation 14, no. 1, sup. 2 (April 2023): S1-S90.
5. L.H. Aiken, K.B. Lasater, D.M. Sloane, et al., “ Physician and Nurse Well-Being and Preferred Interventions to Address Burnout in Hospital Practice: Factors Associated With Turnover, Outcomes, and Patient Safety ,” JAMA Health Forum 4, no. 7 (July 2023): table 2.
6. We selected the largest 200 employers based on the number of U.S. Glassdoor ratings by nurses from April 1, 2020, through June 30, 2023.
7. Aiken et al., “Physician and Nurse Well-Being,” table 1.
8. This methodology is similar to that employed by M. Jura, J. Spetz, and D.-M. Liou in “ Assessing the Job Satisfaction of Registered Nurses Using Sentiment Analysis and Clustering Analysis ,” Medical Care Research and Review 79, no. 4 (August 2022): 585-593.
9. Aiken et al., “Physician and Nurse Well-Being,” table 3.
10. M.A. McCord, D.L. Joseph, L.Y. Dhanani, et al., “ A Meta-Analysis of Sex and Race Differences in Perceived Workplace Mistreatment ,” Journal of Applied Psychology 103, no. 2 (February 2018): 137-163; and K. Aquino and S. Thau, “ Workplace Victimization: Aggression From the Target’s Perspective ,” Annual Review of Psychology 60 (February 2009): 717-741.
11. A. Bergman, H. Song, G. David, et al., “ The Role of Schedule Volatility in Home Health Nursing Turnover ,” Medical Care Research and Review 79, no. 3 (June 2022): 382-393.
12. Nurses quitting (versus being fired) accounted for 96% of all separations from hospitals in 2021. See “ 2021 NSI National Health Care Retention & RN Staffing Report ” (East Petersburg, Pennsylvania: NSI Nursing Solutions, March 2021): 3.
13. D. Sull, C. Sull, W. Cipolli, et al., “ Why Every Leader Needs to Worry About Toxic Culture ,” MIT Sloan Management Review, March 16, 2022, https://sloanreview.mit.edu.
14. D. Sull, C. Sull, and B. Zweig, “ Toxic Culture Is Driving the Great Resignation ,” MIT Sloan Management Review, Jan. 11, 2022, https://sloanreview.mit.edu.
15. “We Tell It Like It Is So You Won’t Be Surprised by How It Goes,” Triage, accessed April 24, 2023, https://triagestaff.com.
16. E.W. Morrison, “ Employee Voice and Silence ,” Annual Review of Organizational Psychology and Organizational Behavior 1 (March 16, 2014): 173-197.
17. E.J. McClean, E.R. Burris, and J.R. Detert, “ When Does Voice Lead to Exit? It Depends on Leadership ,” Academy of Management Journal 56, no. 2 (April 2013): 525-548.
18. Aiken et al., “Physician and Nurse Well-Being,” table 2.
19. “ Unit-Based Team Overview ” and “ UBT Roles ,” Labor Management Partnership, accessed Aug. 30, 2023, www.lmpartnership.org.
i. We ran models for the pre- and post-COVID-19 samples by current employees, former employees, and all employees for a total of six models. The average out-of-sample adjusted R2 across a tenfold validation ranged between 0.29 and 0.39 for all models. A model using structural attributes of employers, including ownership, type of organization (health care system, nursing home, or specialty hospital), and location, however, together explained less than 5% of the variance in how nurses rated their employers. Our analysis of structural attributes included seven ownership types, 17 organizational types, and 50 U.S. states. For the structural model, the average out-of-sample adjusted R2 across a tenfold cross-validation was 4.2%.
More Like This
Add a comment cancel reply.
You must sign in to post a comment. First time here? Sign up for a free account : Comment on articles and get access to many more articles.
The Nursing Shortage Explained
What is the nursing shortage, why is there a nursing shortage.
- Is the Nursing Shortage Getting Worse?
How Do We Solve the Nursing Shortage?

The nursing shortage is a growing problem in the United States, with the U.S. Bureau of Labor Statistics (BLS) projecting that a 6% growth rate in the demand for registered nurses will result in a need for 3.3 million nurses by 2031. But, how much of that will need will actually be met?
Unfortunately, the Covid-19 pandemic has only exacerbated this issue as front-line nurses feel the strain of increased workloads and decreased staffing levels. This has led to higher rates of nurse burnout due to long hours and high-stress levels.
The nursing shortage is impacting the care that nurses are able to provide for patients and stretching their ability to cope with having to do more work with less help.
But why is there a nursing shortage? And can anything be done about it? Keep reading to learn about the causes and possible solutions of the nursing shortage based on findings from our own 2023 State of Nursing report and other findings from the AACN.
>> Download the 2023 State of Nursing Report
According to the American Association of Colleges of Nursing (AACN) , the nursing shortage is a chronic and escalating problem created by several interrelated factors:
- Nursing school enrollment not keeping up with the demand for nurses
- Shortage of nurse faculty restricting nursing school enrollments
- A large number of nurses are retiring or approaching retirement
- Increase in the aging population and therefore nursing services
- Insufficient staffing causes nurses to leave the profession
Interestingly, many of the top reasons nurses cited as causes of the nursing shortage are not included in the AACN’s list. When asked “What do you think are the primary causes of the nursing shortage?” these were the most popular responses from the 2023 State of Nursing survey:
- Nurses are burned out - 74%
- Poor working conditions - 58%
- Inadequate pay for nurses - 57%
- Lack of appreciation for nurses - 34%
The greater number of patients due to an aging population, changes to the medicare/healthcare system, and lack of nursing school educators/faculty got the least amount of responses from nurses. Indicating that, while these systemic factors may be contributing to the overall nursing shortage, that’s not what nurses are feeling on a day-to-day basis, and not what’s ultimately prompting many nurses to think about leaving the bedside, or even the profession altogether.

Popular Online Master of Science in Nursing (MSN) Programs

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals. GCU offers a full spectrum of nursing degrees, from a pre-licensure BSN degree to a Doctor of Nursing Practice (DNP) program.
Enrollment: Nationwide
- MSN - Family NP
- MSN - Adult Gerontology Acute Care NP
- MSN - Nursing Education
- MSN - Health Informatics
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MBA & MSN - Nursing Leadership in Health Care Systems
- See more GCU nursing programs

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management
Enrollment: Nationwide, excluding NY, RI and CT. Certain programs have additional state restrictions. Check with Walden for details.
- MSN - Psychiatric-Mental Health NP
- MSN - Adult/Gerontology Acute Care NP
- MSN - Adult/Gerontology Primary Care NP
- MSN - Pediatric NP - Primary Care
- MSN - Nursing Informatics

As a working RN, you need a flexible, transfer-friendly program to help you save time and money as you take the next step in your nursing career. In our CCNE-accredited4 RN to BSN program, you can transfer in up to 134 credits—which is nearly 75% of program requirements. Your transfer credits can be reviewed in one business day (on average).
Enrollment: FL
- MSN - Adult-Gerontology NP - Primary Care
- MSN - Nursing Leadership & Admin
- MSN - Healthcare Tech, Simulation & Informatics
- See more Rasmussen nursing programs
Is the Nursing Shortage Getting Worse?
While a nursing shortage has existed for decades, 91% of nurses believe the nursing shortage is getting worse. Other reports support this as well.
For example, a 2022 report by McKinsey consulting and advisory firm warns that the “nursing shortage will become dire by 2025” due to a projected shortage of 200,000 to 450,000 nurses—roughly 10% to 20% of the nurses required to provide all patient care.
Already some nurses describe having to “ration care” due to inadequate nurse-patient ratios so they can focus on keeping patients “alive”, often at the expense of meeting patients’ other basic needs such as helping them with a much-needed bath.
When asked “What do you think would make the biggest impact on the nursing shortage” 71% of nurses replied that improved staffing ratios would have the biggest impact, followed by better pay (64%) and better working conditions (41%).

But ultimately, addressing the nursing shortage will require a multi-faceted approach that includes both short-term solutions to improve nurses' daily lives and long-term strategies to address the underlying issues.
1. Increasing Funding to Improve Nurse-Patient Ratios and Retain Nurses
Hospitals and healthcare facilities need to start listening to nurses if they want to retain them and improving staffing ratios was the number one factor that nurses thought could positively impact the nursing shortage.
New York state nurses described “abysmal working conditions” as they went on strike in January 2023 but were told “There’s no money in the budget” to improve working conditions and ensure safe nursing staff levels. Hospital administrators and those that control the purse strings of healthcare facility budgets need to reevaluate their budget priorities if they want to retain and attract nurses and protect patients.
2. Paying Higher Salaries to All Nurses, Particularly to Recruit and Retain Nursing Faculty
As we saw above, 64% of nurses believe that better pay would help lessen the nursing shortage. When we asked nurses how they felt about their current pay, 75% of nurses said they felt underpaid.
In addition, a major reason for the shortage of nursing faculty is low salaries. While the average salary of an advanced nurse practitioner with a master’s degree is $120,680 , master’s prepared nursing faculty were paid just $87,325/year in 2022.
With the average nursing faculty salary being $33,372/year less than what nurses earn in clinical and private-sectors positions, it’s hard to attract and retain faculty. Therefore, nursing faculty salaries need to be increased substantially if nursing schools want to attract and retain faculty.
3. Better Working Conditions
Being able to do things like take breaks and feeling that they’re able to turn down extra shifts may seem like basics that all nurses should be getting, but our survey shows that they are not. 72% of nurses don’t have adequate backup, 53% of nurses are unable to take sick days, and 36% feel that they can’t turn down extra shifts at work.
4. Providing Funding for More Master’s and Doctoral Nursing Student Enrollments
According to the AACN, “Master’s and doctoral programs in nursing are not producing a large enough pool of potential nurse educators to meet the demand.”
For example, although enrollment in entry-level baccalaureate nursing programs increased by 3.3% in 2021, enrollment in master’s and PhD nursing programs dropped by 7% and 3.8%, respectively.
Therefore, more funding and recruitment need to be directed at graduate-level nursing programs to help prepare more nursing faculty and create more advanced practice nurses.
5. Designing Nursing Positions That Offer Better Work-Life Balance
And finally, nurse leaders need to start creating nursing positions that allow nurses to have a better work-life balance if they want to attract and retain nurses in these positions.
The high levels of nurse burnout and chronic stress in nursing are simply unacceptable and cannot continue if the nursing shortage is to be significantly reduced. 81% of nurses said they’ve felt burnt out in the past year, according to our survey.
Nurses will continue to leave the profession and their jobs in search of a more manageable lifestyle and less stressful work.
By making a commitment to listen to nurses and implement these changes, policymakers, facility administrators, and nurse leaders can reverse this nursing shortage and ensure that our healthcare system has enough nurses to meet the needs of patients now and into the future.

Leona Werezak BSN, MN, RN is the Director of Business Development at NCLEX Education. She began her nursing career in a small rural hospital in northern Canada where she worked as a new staff nurse doing everything from helping deliver babies to medevacing critically ill patients. Learning much from her patients and colleagues at the bedside for 15 years, she also taught in baccalaureate nursing programs for almost 20 years as a nursing adjunct faculty member (yes! Some of those years she did both!). As a freelance writer online, she writes content for nursing schools and colleges, healthcare and medical businesses, as well as various nursing sites.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Nursing Shortage Solutions for the Future
Written by: applied nursing research editorial team • may 19, 2024.

The nursing profession has long stood as a pillar of healthcare systems worldwide. Nurses act as the backbone, offering compassionate care, executing vital medical tasks, and serving as the bridge between patients and doctors. Despite their essential role, a looming crisis threatens healthcare: the nursing shortage. In this article, we delve deep into understanding the nursing shortage, its implications, and why it is a pressing concern for all of us.
What is the nursing shortage?
A nursing shortage refers to a situation where the demand for registered nurses (RNs) and other nursing roles exceeds the supply—locally, nationally, or globally. This deficit isn’t a new phenomenon. In fact, sporadic shortages have been recorded over the decades. However, the current and impending scarcity is unparalleled in its reach and potential impact.
There are two types of shortages to consider:
Global shortages: These are broad in nature, affecting many countries simultaneously. Factors like global health crises, universal trends in education, and collective shifts in population age can contribute.
Regional shortages: These can be isolated to specific areas, often exacerbated by unique local factors. For instance, rural areas might suffer more due to the lack of educational institutions or attractive job opportunities.
Why is the nursing shortage important?
The implications of a nursing shortage reverberate throughout the entire healthcare system:
Impact on Patient Care and Safety: An inadequate number of nurses can lead to oversights in patient care. With fewer hands on deck, essential tasks like monitoring patients, administering medication, and responding to emergencies can be delayed or overlooked.
Economic Implications: Hospitals and healthcare systems face financial strain due to overtime costs, the need for temporary staffing, and potential lawsuits arising from medical oversights or mistakes. Additionally, a stretched-thin staff may lead to longer hospital stays for patients, further increasing costs.
Effects on Current Nursing Staff: Nurses working in understaffed facilities face significant stress. Their shifts become longer, their patient loads increase, and their chances of burnout skyrocket. This not only affects their mental and physical health but can also lead to higher turnover rates, exacerbating the shortage.
Future of Healthcare: In the longer term, a persistent nursing shortage can diminish the quality of healthcare. Prospective medical procedures or treatments might be delayed or canceled due to lack of staff. Moreover, as the frontline caregivers, nurses offer valuable insights into patient care optimization. A shortage means fewer voices to champion patient needs or to innovate in care delivery.
Challenges surrounding the nursing shortage
The nursing shortage isn’t merely an issue of insufficient recruitment. It’s a multifaceted challenge, with roots in various areas:
Rising Demand Due to an Aging Population
As the global population ages, there’s an increased demand for healthcare services. Elderly individuals often have complex medical needs, necessitating more frequent and specialized care. This increased demand strains an already under-resourced nursing workforce.
Burnout and High Turnover Rates
Nursing, while rewarding, is also emotionally and physically taxing. Long hours, the emotional toll of patient care, and the high-stress nature of the job can lead to burnout. This results in nurses leaving the profession or seeking less demanding roles.
Educational Bottlenecks
Nursing education institutions are grappling with their challenges, including a shortage of faculty and limited classroom space. This restricts the number of students they can admit, despite a growing list of qualified applicants.
Economic Challenges
In some regions, the compensation for nursing roles isn’t commensurate with the demands of the job. When alternative professions offer better pay, benefits, or work-life balance, nursing can lose its appeal to potential recruits.
Migration Patterns
The migration of nurses from low-income to high-income countries, or from rural to urban areas, further aggravates localized shortages. While migration can offer individual nurses better opportunities, it can also drain resources from already vulnerable areas.
Solutions for the nursing shortage
Addressing the nursing shortage requires a multi-pronged approach, tailored to the unique challenges presented:
Increasing Educational Opportunities:
Partnering with Colleges: Establishing partnerships with colleges and universities can create fast-track nursing programs, enabling students to enter the workforce more rapidly.
Online and Distance Learning: Digital platforms can accommodate more students, bypassing the traditional limitations of physical space. This also allows students from remote areas to access quality education.
Financial Incentives:
Scholarships and Loan Forgiveness: Offering financial aid can incentivize students to choose nursing as a career and help them graduate without burdensome debt.
Competitive Pay and Benefits: Reviewing and restructuring compensation packages can make nursing roles more attractive, retaining current staff and attracting new recruits.
Creating a Supportive Work Environment:
Reducing Nurse-to-Patient Ratios: Fewer patients per nurse can significantly reduce workload, ensuring patients get quality care while reducing nurse burnout.
Professional Development: Offering opportunities for career advancement, training, and mentorship can motivate nurses and improve job satisfaction.
Addressing Burnout: Implementing mental health support, wellness programs, and flexible scheduling can help nurses manage the demands of their roles.
Nursing shortage outlook
While the current situation paints a grim picture, understanding the future landscape of the nursing shortage is vital for proactive planning:
Predictions for the Future: Forecasts suggest that unless significant measures are taken, the nursing shortage will continue to grow over the next two decades.
Potential Shifts: Global events, such as pandemics or economic downturns, can either exacerbate or temporarily alleviate shortages. For instance, economic crises might see more individuals turning to nursing as a stable profession, but this can be offset by the increased healthcare demands during such periods.
Technological Advancements: Innovations in healthcare technology, such as AI-driven diagnostics or robotic assistance, might reduce some of the demand on nurses. However, the human touch and expertise that nurses provide will remain irreplaceable.
Nursing Shortage FAQ
As the nursing shortage continues to be a topic of concern, several frequently asked questions arise that help shed light on its intricacies.
Q: How severe is the current nursing shortage?
The severity varies by region, but many parts of the world, particularly in the West, face acute shortages. The World Health Organization (WHO) estimates a global deficit of nearly six million nurses, making it a pressing issue on a global scale.
Q: Why can’t we just train more nurses?
While training more nurses sounds like a straightforward solution, there are underlying challenges. First, nursing schools often face faculty shortages, limiting their ability to admit more students. Second, nursing is a demanding profession, both physically and emotionally. Not everyone interested in healthcare chooses or is suited for nursing, making recruitment a challenge.
Q: Are there countries unaffected by the nursing shortage?
Most countries experience some level of nursing shortage, but the severity varies. Some nations have mitigated the issue through targeted policies, international recruitment, or offering better incentives for nursing professionals. However, no country is entirely immune.
Q: What are the health risks associated with a nursing shortage?
A shortage can lead to compromised patient care, increased risk of medical errors, longer hospital stays, and overall strain on the healthcare system. It also leads to increased stress and burnout among the existing nursing staff, potentially impacting their own health and well-being.
Q: How do nursing shortages affect other medical professionals?
The entire healthcare system is interconnected. A shortage of nurses increases the workload on other professionals, from doctors to medical technicians. It can cause delays in treatment, diagnosis, and overall patient care.
Q: Are there any positive side effects of a nursing shortage?
While the effects of a nursing shortage are primarily negative, it does bring attention to systemic issues within the healthcare system. This increased attention can lead to policy changes, innovations in training, and heightened public awareness about the value of nurses.
The nursing shortage is more than a staffing issue; it’s a complex, multifaceted challenge that touches every corner of the healthcare system. From the well-being of individual patients to the overall efficacy of global health initiatives, the role of nurses is paramount. Addressing the nursing shortage requires collaborative efforts from governments, institutions, communities, and the nurses themselves.
While the road ahead is fraught with challenges, there’s also room for hope. The spotlight on the nursing shortage has led to innovations in education, technology, and healthcare policy. By continuing to prioritize the well-being and professional development of nurses, we not only ensure their rightful place in the healthcare ecosystem but also uphold the highest standards of patient care. The future of global health hinges on the steps we take today to value and support our nursing professionals.
Related Articles
May 19, 2024 May 19, 2024
Mental Health Guide for Nurses
Nurse practitioner vs. physician's assistant: what's the difference , rn vs np: registered nurse vs nurse practitioner .
- Accreditation
- -Associates
- -Doctorates
- -Certificates
- Your favorite state, in photos
- Sign up to follow compelling stories of Californians in pictures.
- Environment
- California Voices
Should California community colleges offer bachelor’s degrees in nursing? Universities say no

Share this:
- Click to share on X (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on WhatsApp (Opens in new window)

Lawmakers approved two bills to allow some community colleges to provide bachelor’s degrees in nursing. That’s setting up another conflict with the California State University, which already offers these bachelor’s degrees.
Lea esta historia en Español
Is there a nursing shortage in California? Now, yes, though in a few years, probably not.
By 2027, the state is projected to have as many nurses as it needs because of a rise in nursing program enrollment, according to UC San Francisco projections compiled for the state agency that regulates nursing programs. The report was published last year.
But there are other sub-shortages in California’s nursing workforce. Two bills passed by the Legislature last week focus on one of those: nurses with bachelor’s degrees.
Both target a growing demand for nurses to possess bachelor’s degrees by allowing some community colleges to issue them. Presently the colleges only provide associate degrees — generally the minimum degree needed to be a registered nurse.
The bills are the latest developments in the state’s ongoing quest to tweak the educational offerings of colleges and universities to address cultural and workforce needs, from requiring ethnic studies courses to permitting colleges and universities to issue degrees they haven’t before. But the bills also underscore the complexity of both identifying a labor force problem — a nursing shortage — and the role that community colleges and universities play in graduating skilled workers.
One is Senate Bill 895 by Sen. Richard Roth, a Democrat from Riverside. The other is Assembly Bill 2104 by Assemblymember Esmeralda Soria, a Democrat from Merced.
The California State University opposes both bills, viewing them as undermining a promise lawmakers made two years ago that community colleges wouldn’t issue bachelor’s degrees that duplicate existing Cal State programs, among other worries. Private colleges oppose the bills, as well. The University of California doesn’t officially oppose the bills but raised similar concerns .
Understanding the nursing shortages
Even as the state may not have an industry-wide nursing shortage by 2027, there are still stubborn sub-shortages.
While California has seen the number of nursing education program slots grow by 3,000 between 2018 and 2023 , virtually all of that was at private nonprofit and for-profit campuses . Available slots at the more affordable public colleges and universities have remained flat.
There are regional differences, too, with California’s Central Valley and the Central Coast lacking enough nursing program slots to meet demand. “Those would be the regions that I would point to as having the biggest challenges,” said Joanne Spetz, a researcher at UC San Francisco who studies the state’s nursing sector and co-wrote the projections report
Yet another micro-shortage stems from the fact that more hospitals prefer — or require — hiring nurses with bachelor’s degrees . That makes sense: Several academic studies concluded that hospitals that increased their share of nurses with bachelor’s degrees saw lower rates of patient death and shorter hospital stays .
And an overall shortage may still persist past 2027 due to “high rates of burnout” that “may lead to greater turnover and departures from nursing,” the projections report said.
What the two bills will do
Enter the two bills the Legislature passed last week.
Will they lead to more registered nurses? Speaking of his bill in July, Roth said no. But it would help produce more nurses with bachelor’s degrees — which more hospitals say they want, he said.
The bill authors — as well as their community college and hospital backers — say some community colleges should be allowed to issue bachelor’s degrees in nursing for other reasons, too.
Students who live too far from a California State University or University of California nursing program could enroll at a community college and avoid long commutes to the public universities or much more expensive private colleges . There are more than 70 community colleges in California that offer associate degrees in nursing and 21 public universities — mostly through the Cal State system — that award bachelor’s degrees in nursing . And while some universities offer online programs, not every student has fast-enough internet or enough computing power at home, Roth told lawmakers .
Students with associate and bachelor’s degrees take the same licensure exam. Typically a bachelor’s degree in nursing requires about 30 more units of coursework, which takes about a year to complete.
An overall shortage may still persist past 2027 due to “high rates of burnout” that “may lead to greater turnover and departures from nursing.” UC San Francisco projections report
Both bills seek to form pilot programs that each allow just 10 community college districts — out of the state’s 73 — to offer bachelor’s degrees in nursing.
But they vary in other ways. Soria’s bill places an emphasis on pilots in the Central Valley , which has a chronic nursing shortage. Roth’s bill is aimed at the whole state, though it would focus on the Central Valley and other regions by prioritizing pilot programs in underserved communities. Both would require the Legislative Analyst’s Office to evaluate the pilots, but Roth’s bill would have the pilot programs last until 2034 while under Soria’s bill the programs would run until 2031.
Roth’s bill requires colleges in the pilot to have national accreditation, which can take several years to accomplish. Soria’s bill doesn’t specify that. Still, 28 community colleges already have national accreditation, according to a July legislative bill analysis.
Learn more about legislators mentioned in this story.
Josh Newman
Democrat, State Senate, District 29 (Fullerton)
Richard Roth
Democrat, State Senate, District 31 (Riverside)
Esmeralda Soria
Democrat, State Assembly, District 27 (Merced)
The differences raise questions about how Gov. Gavin Newsom may reconcile the two bills.
That’s one reason why the California Community Colleges Chancellor’s Office is “recommending the governor sign SB 895” over Soria’s bill, wrote Melissa Villarin, a spokesperson for the California Community Colleges Chancellor’s Office, in an email Wednesday. She also noted that either bill getting Newsom’s signature would be a “major victory.”
The chancellor’s office prefers Roth’s bill because it was sponsored by statewide groups close to the central office, including the Community College League of California, which represents community college administrators and trustees. Roth’s legislation is also a “bill where more attention and efforts (in terms of negotiating amendments) have been focused throughout the legislative process,” she wrote.
Why Cal State opposes bachelors degrees at community colleges
Both bills are creating a panic for Cal State leadership and the system’s nursing programs. There’s the fear that the community colleges will eat Cal State’s enrollment lunch by offering bachelor’s degrees that are cheaper than what Cal States charge.
Roth’s bill “will siphon off the students” who’d “otherwise come to a CSU nursing degree program,” said Rehman Attar , director of health care workforce development at the Cal States, during a July legislative hearing. He said the same about Soria’s bill .
Forming new bachelor’s programs at community colleges is expensive, he argued. Cal State’s online bachelor’s programs and the system’s fast-track bachelor’s degree programs with 37 existing community colleges can meet the bills’ goals, he said in an interview. More of these partnership programs are pending, he added .

California’s health care workers are burning out. These universities want to help.
There’s also a philosophical battle brewing over the distinct roles of each higher education segment in California. For decades, the state’s 1960 Master Plan for Higher Education stipulated that the community colleges offer certificates and associate degrees; Cal States chiefly provide bachelor’s degrees and master’s degrees; and the UCs focus on research by offering bachelor’s, master’s and doctoral degrees.
But in recent years, the Legislature has permitted the community colleges to award bachelor’s degrees, with the proviso that those degrees don’t duplicate the degrees already offered at Cal States. Both systems have fought over the practicalities of that détente , but the bills proposed by Roth and Soria would knowingly blow up that public policy peace by allowing the community colleges to offer the same nursing bachelor’s degrees the Cal States already provide.
“Our overall opposition is, of course, we’re opposed to duplication,” Attar said in an interview. Both bills received wide bipartisan support. However, a few Democrats — who have a supermajority in the Legislature — expressed reservations about the emerging mission creep of the community colleges.
Among those is Sen. Josh Newman, a Democrat from Fullerton who is chair of the Senate’s education committee. During a hearing on Soria’s bill , he said that the master plan assumed a “division of labor, if you will, between the segments. And largely because of geographical and workforce needs, we’re seeing that erode. I believe that is problematic.”
Roth’s bill would also create new layers of pricing. It would cap tuition for the pilot nursing bachelor’s degrees to be no more expensive than other community college courses — $46 a unit — wrote Villarin.
“The only way to pursue a bachelor’s degree, if you’re in some of those communities, is to either do an online program, some of which are excellent and some of which are not so good, or to relocate to do a bachelor’s degree.” Joanne Spetz, researcher at UCSF
Existing bachelor’s degrees at community colleges have tuition charges that are capped at $10,560, excluding course and campus fees, so Roth’s bill would make a nursing bachelor’s roughly half that. Meanwhile, Cal State systemwide tuition, excluding fees, is now more than $6,000 a year and will grow by 5% annually through 2028-29 .
Spetz of UC San Francisco said the lack of public bachelor’s degree programs in nursing is a real barrier to Californians in remote parts of the state where there’s no nearby university.
“The only way to pursue a bachelor’s degree, if you’re in some of those communities, is to either do an online program, some of which are excellent and some of which are not so good, or to relocate to do a bachelor’s degree, which just seems kind of silly and isn’t possible for many people,” she said.
She’d recommend limiting the pilot programs to community colleges that are particularly far from a public university with a nursing program. “I think having a distance threshold and really focusing on regions where there is not a public bachelor’s degree opportunity for folks …is a reasonable thing to test.”

Tired of the waiting lists for California’s public universities, nursing students increasingly turn to expensive private programs

California needs thousands of nurses, but leaders can’t agree on how to fill jobs
Mikhail zinshteyn higher education reporter.
Mikhail Zinshteyn reports on higher education for CalMatters. His coverage tackles state legislation, financial aid, labor issues, student demands, campus housing and college affordability. His work on... More by Mikhail Zinshteyn

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Registered nurses’ perceptions on the factors affecting nursing shortage in the Republic of Vanuatu Hospitals: A qualitative study
Adel tutuo tamata.
1 Vanuatu College of Nursing Education, Ministry of Health, Port Vila, Vanuatu
Masoud Mohammadnezhad
2 School of Public Health and Primary Care, Fiji National University, Suva, Fiji
Ledua Tamani
Associated data.
Data can be found at the Open Science Framework (OSF): Factors affecting nursing shortage in Vanuatu (Mohammadnezhad, 2021) (DOI: 10.17605/OSF.IO/W7G8E ).
Registered nurse has a vital role in delivering healthcare services to individual, family and community. One of the main challenges that health system facing globally is the shortage of nursing workforce. Vanuatu as a Pacific county is also facing the shortage issue and the impact on the registered nurses’ performance.
A qualitative study was used to collect data from 25 registered nurses in three randomly selected hospitals in Vanuatu between 4 th to 14 th September, 2020. A semi-structured open-ended questionnaire was used to collect data using face-to-face in-depth interviews. The data were transcribed and analyzed using thematic analysis process.
Four themes were identified including; Difficult working conditions, Reinforcing factors and Perceived risks. Sub themes for difficult working condition were heavy workload, lack of workforce and unusual working hours. Sub themes for reinforcing factors were lack of support, lack of opportunities and advancement in nursing practice. Sub themes for perceived risks were stress, physical and mental risk, and social and family risks.
This study has identify factors affected shortage of current nursing workforce and the impact it has on registered nurses. Broad themes and sub-themes were identified which highlighted the impact of nursing shortage to registered nurses and the effects on their performance which includes stress or moral distress from work overload and lengthy hours shift which impact the nurses’ physical, psychological, social, and family relationship, and lack of leadership support. The findings can be helpful to policy makers at the decision-making level to resolve the nursing workforce shortage and its effects in the future by refining and developing relevant policies that will address and strengthen the nursing workforce to meet the demand and improve delivery of quality health services to all individual.
Introduction
Registered Nurses (RNs) are valued professionals and constitute the largest proportion of nursing population. They play a very significant role to ensure that effective quality care is provided in improving the health system [ 1 ]. In order to improve the health coverage and achievements of health targets, adequate nurses are crucial as the effectiveness of the patient care depend on the availability of more nurses [ 2 , 3 ].
While the world has acknowledged nursing profession as vital in delivering healthcare services, one of the main challenges faced today globally is the shortage of nursing workforce which has major impact on nurses and causes severe effects on the nurses’ performance to provide quality of health care services and improving well-being of the global population [ 3 – 5 ]. The nursing shortage caused severe stress or burned out which aggravate the problems on nurses to leave their job [ 1 ].
According to the World Health Organization (WHO), it was estimated that there will be a shortage of 7.2 million health workers to deliver healthcare services worldwide and by 2035 the demand of nursing will reach 12.9 million [ 6 ]. The inadequate supply of nurses has notably created many negative impacts not only on RNs but also on patient health-related outcome as well as challenges to fight diseases and improving health, which causes increase workload on nurses and later results in decreasing the quality of nursing care [ 7 , 8 ].
There are many factors affecting the healthcare system as a result of shortage of nursing workforce. These include decreased number of student nurse’s enrolment in nursing program and increase number of early retirement due to health problem [ 3 , 9 ]. However, one of the main factors reported in many countries is inadequate policies and workforce planning [ 10 , 11 ].
In the Pacific Island Countries (PICs), the shortage in nursing workforce is becoming a common problem [ 9 ]. In Solomon Islands, Papua New Guinea and Vanuatu, the health worker density per 1,000 populations (mainly nurses and midwives) is far below the minimum threshold density (4.45 per 1,000 populations) to sustain basic health services [ 12 ]. In countries such as Tonga, Samoa and Fiji, the main factors that trigger shortage of nursing staff includes very high rate of nurses’ migration to other countries, especially to Australia and New Zealand for better working conditions and for other potential opportunities. This has created challenges and gaps that needed to be identified to better explore the extent of the nursing shortage and to address it promptly and efficiently [ 13 ].
In Vanuatu, nurses constitute only 58% or 12.0 per 10,000 populations, which is below the WHO recommended ratio of 45 nurses per 10,000 populations [ 14 ]. According to the Vanuatu Ministry of Health (MoH) Annual Report (2018), the number of retiree nurses in the next 10 years will continue to rise but will be disproportionate to the qualified nurses graduated from the Vanuatu College of Nursing Education (VCNE) which becoming a major problem for Vanuatu MoH to fill the vacant positions. This will create more workload for nurses which will impact their performance. This study sets out to explore RNs’ perceptions on the impact of nursing shortage of nurses and their performance in providing quality care in Republic of Vanuatu in 2020.
Methodology
Study design and setting.
A qualitative study was used to gather information using face-to-face in-depth interviews from RNs in three hospitals in Vanuatu between 4 th to 14 th September, 2020. The three hospitals were randomly selected among six hospitals that included Vila Central Hospital (VCH) in Shefa Province, Northern Provincial Hospital (NPH) in Sanma Province and Lenakel hospital in Tafea Province. In-depth interviews are very powerful methods to allow participants to express their view freely regarding their detailed personal experiences [ 15 , 16 ].
Study population and sample
All RNs in Vanuatu were considered as the study population and those who were currently working at the three selected hospitals with at least 6 months’ work experience were included in this study. Those who were not willing to participate in the study were non-respondent. A purposive sampling was used to choose study participants. The RNs were interviewed using face-to-face, in-depth interviews until data saturation is reached. A total of 25 RNs were involved in this study.
Data collection tool
In-depth face-to-face interviews was conducted using a semi-structured open-ended questionnaire to probe elicit information from the identified participants from both the target populations. Open-ended questions aimed for participants to express their personal experience freely [ 17 ]. The interview questions developed is based on relevant literatures and research studies that will fulfill the aim and the research question of the study. Seven questions were prepared and asked during in-depth interview to enable the participants to explain or discuss their perceptions about the research topic.
The demographic information form was also used to collect demographic characteristics regarding their gender, age, marital status, education level, work station and years of experience. The interview questions were checked by 3 experts in the relevant filed and also by 3 RNs to make sure they are understandable and are in line with the research questions before conducting the interviews.
Study procedures
Following the ethic approvals, all potential RNs in three selected hospitals were informed about the aim of study and were invited to participate. An information sheet was used to inform the participants about the purpose, procedure and nature of the study; duration of interview; the right to participate; benefits and risks of the study; notification for decline or withdrawal at any time from participating; informed consent and the interview procedure. They were informed that their information will be confidential and they are allowed to leave the study at any time. Those who met the study criteria and were willing to participate were asked to sign a consent form. An arrangement was made about the date, time and venue of the interview. A trained bi-lingual interviewer who signed a consent form was employed to conduct interviews. Participants were asked about their preferred language to do interview before the interview. Those who preferred to speak in local language were interviewed in Bislama language otherwise the English language was chosen for the interviews. All interviews were audio-taped for transcription later.
Data management and analysis
Cross translation was applied for translating the interviews that were in Bislama to English. All the interviews were transcribed by the main researcher and were checked by the research assistant to make sure they are transcribed accurately. The data were manually analyzed using thematic analysis process to identify the final themes. Thematic analysis is a method which involves identifying, analyzing, and reporting patterns of data and is widely used for analyzing qualitative research [ 18 ]. The participants’ answers were read and re-read closely by the main researcher to divide into key words or phrases into their similar meanings and create codes. The transcribed results were later transferred to A4 paper. Then the coded data were sorted into themes and sub-themes based on the similar issues which formed the result of the study.
Ethics approval
Before proceeding to data collection, ethic approvals were obtained from the College Health Research Ethics Committee (CHREC) in Fiji National University (FNU) and from the Research Ethics Committee in Vanuatu MoH. All participate were provided a consent form and the information sheet. The participants were informed about the purpose of the study and ensures that their identities are anonymous and the participants ‘data and any other information would be kept confidential and protected.
Demographic characteristics of participants
Twenty-five participants were involved in the in-depth interview (12 males and 13 females). With respect of age, 14 with age range <40 and 6 of the participant with the age range from 40–49, and 5 age ≥50, and 18 of them were married. Their educational level, 21 of them had their undergraduate qualification and 4 had their highest qualification as post graduate level which includes post graduate diploma ( Table 1 ).
| Frequency | Percentage | ||
|---|---|---|---|
| Sex | Male | 12 | 48 |
| Female | 13 | 52 | |
| Age (YR) | <40 | 14 | 56 |
| 40–49 | 6 | 24 | |
| ≥50 | 5 | 20 | |
| Marital Status | Single | 2 | 8 |
| Married | 18 | 72 | |
| Others | 5 | 20 | |
| Work Experience (YR) | <10 | 10 | 40 |
| 10–19 | 7 | 28 | |
| ≥20 | 8 | 32 | |
| Education Level (Profession) | Undergraduate | 21 | 84 |
| Post graduate | 4 | 16 |
*De Factor 2, Divorce 3
Themes and sub-themes
The thematic analysis found three major themes emerging; 1) Difficult working condition, 2) Reinforcing Factors, and 3) Perceived risks. Each theme had several sub-themes ( Table 2 ). The participants’ reflection for each theme and sub-theme are further expanded and compared with other published studies. In this section, participants are presented with a “P” and cardinal number like P1, P2.
| THEMES | SUB-THEMES |
|---|---|
| Difficult working conditions | • Heavy workload |
| • Lack of workforce | |
| • Unusual working hours | |
| Reinforcing factors | • Lack of support |
| • Lack of opportunities and advancement in nursing practice. | |
| Perceived risks | • Stress |
| • Physical and mental risk | |
| • Medical risk | |
| • Social and family risk |
Difficult working conditions
The nurses believe that the conditions where nurses’ work can have a major influence on their performance and the quality of care provided to patients include “heavy workload”, “lack of workforce” and “unusual working hours”.
1. Heavy workload
All the participants (25) working in the hospitals have confirmed that workload has been a challenge when there are extremely limited nurses to manage the patients on each shift. P3 stated that shortage of nursing and workload is seen throughout the hospital wards which exceed the number of nurses working per shift.
“Shortage of nursing is seen throughout the hospital wards and is a long-term issue where workload exceeds the number of nurses working in one shift” .P3 (a 56-year-old female RN).
All the participants (25) also reported that the workload is increasing because of the high number of patients’ admitted. P16 compared the population in the past with the current and stated that when the population increased, diseases also increased that caused workload on nurses.
“In the past , the population was less but now the population increases due to the high number of disease cases that causes more patients’ admission and more workload to us nurses” .P16 (a 32-year-old male RN)
Some of the participants (15) reported an inadequate number of nurses working in each shift also create challenges due to workload when other nurses on sick calls or annual leave. P6 expressed the workload when only one nurse worked to cover for nurses who were on various leaves.
“Workload is too much as most of the time only two nurses working in each shift is not enough , if one staff on sick leave or annual leave then we must double the shift” . P6 (a 34-year-old male RN)
Four participants stressed the ratio of nurses to patients admitted in the hospital in Vanuatu as a huge difference which affects nurses’ performance compared to the other countries. P14 stated:
“Uh… . when we look at the ratio of nurses to patients in Vanuatu which is 1 : 10 or 1 : 15 compared to other countries of which they have 1 : 4 , there is a huge difference . One ward receives on average of 20 to 30 patients at one time but only 2 to 3 nurses work on one shift which is too much for one nurse to perform his or her duty effectively” .P14 (a 33-year-old male RN)
Twenty participants have the same responses due to the nursing shortage they experienced in their workstation, that they neglected a lot of their duties and responsibilities as a registered nurse. P8 reported that the impact of shortage prevents him to perform his duties and responsibilities such as home visits and other bedside nursing care which also affects the quality of care the patients required.
“Impact of shortage prevents me from performing some of my duties and responsibilities such as home visits and follow-up care to patients with chronic illnesses . Bedside nursing and wound care or wound management are also not done regularly , which can have a great impact on patients’ health” . P8 (a 43-year-old male RN)
2. Lack of workforce
Increased workload compared to less number of nurses working in the hospitals causes nurses’ physical exhaustion leading to job dissatisfaction as expressed by all 25 participants. P11 expressed the result of lack of workforce to his well-being.
“Workload is too much in the hospital wards and we cannot do all our work at one time……I normally experienced tiredness and exhaustion and not interested to work due to incomplete jobs seen each day” . P11 (a 37-year-old male RN)
Thirteen of the participants responded that the increased workload does not correspond with the number of nursing staff in the health facilities especially with increased number of patients admitted and less number of nurses working. P8 stated that the number of workforce does not match with the number of workload from increased admission.
“Few nurses do not match with the increased workload today . For example , increased number of admissions with only 2 staff working per shift is a great challenge to us” .P8 (a 43-year-old male RN)
Other participant added:
“Shortage in my ward with only 2 nurses in one shift is not enough compared to the number of patients admitted especially when we have the critical patients that need close supervision in the ward” . P22 (a 53-year-old female RN).
Furthermore, eight participants stated that training and enrolment have significant effects to the shortage on the nursing workforce due to a single nursing college in the country with limited number of student nurses’ enrolment. P6 said that lack of workforce is due to inadequate enrolment from the nursing college each year.
“ One nursing college is not enough to train more nurses to have an adequate number of nurses in the workforce . Furthermore , the decreased number of intakes to only 30 per year is not enough” . P6 (a 34-year-old male RN)
Conversely, seven participants stated that lack of nursing workforce is due to irregular nursing enrollment in the nursing college in the past.
“The reason for having a shortage of nurses frequently is due to uhm……no regular nursing intake from the VCNE each year . In the past 15 years , nursing college always have regular intakes each year even if the number of intakes is less , we still have continuous graduation of nurses each year with a good supply of nurses in the hospital to work and provide care . Nowadays , the intake occur every 2 or 3 years . P20 (a 33-year-old female RN)
Few of the participants (4), reported that the other reasons for lack of workforce is nurse turnover. P24 stated that the workforce is affected especially when nurses leave their profession and look for other jobs elsewhere due to too much pressure from work.
“Workforce is affected when nurses leave their profession and look for other jobs elsewhere . They left due to too much work load and not enough time to rest” . P24 (a 42-year-old female RN).
3. Unusual working hours
Working long shift hours up to 12 to 16 hours or double the shift due to not enough staff to do shift work especially when staff on sick leave or on annual leave causes physical and emotional exhaustion and also affects quality patients’ care. P21 expressed the reasons for long hours shift and its impact to the nurses and to the patient.
“Most of the time we spend long shift hours of work e . g . 12 to 16 hours or we double the shift due to not enough staff in the ward to do shift work when we don’t have enough staff and when staff are on sick leave . It is so tiring and causes a lot of stress to most of us who work long hours which also affect the quality care provided to patient” .P21 (a 42-year-old female RN)
Fifteen of the participants who normally work shift stated that they used to work double shift especially during the night where only few nurses were working. P17, an experienced nurse expressed that double shifts especially at night is common in the hospital wards when nurses on duty unexpectedly on sick leave which significantly affect the nurses’ physical well-being.
“Double shift is a common practice in the wards especially when there are not enough nurses to work or when a working colleague is on sick leave . This causes much stress to us nurses due to tiredness” . P17 (a 64-year-old female RN)
Five senior nurses responded that occasionally they work 24 hours to assist nurses in the ward when more critical patients are admitted or during an epidemic. P3 stated that as a senior in charge nurse, they committed to work 24 hours when lack of nurses to take care of increased patient admission
“It is our duty as senior nurses to assist the nurses in the wards when more critical patients are admitted or during disease outbreak and work for 24 hours . It is quite tiring but we have no choice because it is part of our responsibilities” . P3 (a 56-year-old male RN)
Three participants responded that during natural disasters, where a lot of nurses are unable to attend work and more patients admitted, they have to work extra hours during the day and during the night. P22 expressed her experience during natural disasters where she has to work on unusual hours to care for the casualties and assist nurses in the wards.
I have experienced spending all day and night for one whole week during tropical cyclones to look after patients as more nurses were unable to come to work” . P22 (a 53-year-old female RN).
Reinforcing factors
The nurses quoted during the interviews that “lack of support” and “lack of development opportunities and advancement in nursing practice” were reasons for low motivations in their performance and job retention.
1. Lack of support
Most respondents (13) reported that lack of support from the leaders causes low working morale and low motivation. P15 stated that the leaders in the hospital management haven’t provide much support to the nurses.
“We always confront our nursing managers or clinical supervisors concerning problems in our work place such as poor working equipment needing replacement and poor working environment but they always give excuses and no action taken seriously which affects our morale of work ….” P15 (a 35-year-old male RN)
Another participant added:
“We hardly see the managers or supervisors doing regular visitation to support nursing staff and to assess nurses work performance , this causes low staff motivation” . P14 (a 33-year-old male RN)
All nurses (25) responded that lack of family support is common due to working overtime and coming home late from work. One participant (P21) reported that they don’t receive any support from the family especially when they came home late from work
“When I came home very late from work my family got angry with me . I don’t receive any support from my family . They even forced me to quit my job due to coming home late from work every day” . P21 (a 42-year-old female RN)
“Even my family don’t want to give me food due to frustration of continuously coming home late from work . ” P16 (a 32-year-old male RN)
Most of the participants (15) have expressed their frustration due to lack of financial support from the MoH especially special allowance for working overtime and others. P1 stressed that she has been working for more than 20 years but she hasn’t received any financial support concerning their overtime package or other allowance or incentives apart from their normal wages which affect their motivation to perform duty effectively.
“I work for many years but I don’t receive any financial support from the health authorities apart from my little salary regarding extra responsibility allowances or overtime allowances or any incentives” . P1 (a 56-year-old female RN)
“Even our working status is on contract bases for so long due to positions not budgeted for which affects our benefits and job insecurity” . P11 (a 37-year-old male RN)
2. Lack of development opportunities and advancement in nursing practice
All participants (25) stated that lack of development opportunities to advance in nursing practices and career pathways are common problems that cause disappointment within the working environment. P24 expressed her disappointment that she works for quite a long time in the hospital but chances to advance in her knowledge is very slim and don’t have the opportunity to expand her knowledge and skills in nursing practice.
“I am very disappointed because I worked in the hospital for many years doing the same routine job as usual and I still remain the same usual nurse… . I don’t receive any promotion because I don’t have any opportunities to advance in knowledge and skills in nursing practices” . P24 (a 42-year-old female RN)
“I haven’t seen any effective career pathway for nurses developed by managers for further trainings to upgrade nurses’ knowledge and skills for advancement in our clinical practice” . P4 (a 34-year-old male RN)
All the participants stated that most of them don’t have any chances for professional development. P18 responded that most nurses perused their training from the Vanuatu nursing college with a diploma level and haven’t had any chances to upgrade to a higher level of qualification.
“ Most of us nurses graduated from the nursing college with a diploma of nursing but we don’t have changes to upgrade to a higher level of qualification or to up skill our-selves” . P18 (a 30-year-old female RN)
“Our skills in nursing practice need to be upgraded in order for us to advance with our clinical practices . It is very good to have regular in-service training but it never happens on regular bases , in order to keep us updated with our nursing practice skills ”. P2 (a 34-year-old male RN)
Other nurses reported that specialty training is also necessary to up skill nurses and advance in their clinical practice in the speciality area but only few nurses had given the chances in the past to attend those training.
“Vanuatu needs more specialized nurses to provide quality care to different types of patients however , only few nurses had been given the chances to take up those training which is still needed for more nurses to take specialize training to provide effective and quality care needed” . P3 (a 56-year-old female RN)
Perceived risk
The nurses quoted during interviews that “stress” and “physical and medical risks” were reasons that affect nurses and increased the chances to quit their profession.
Majority of the participants (20) have worked in the hospital for more than 5 years and reported that they have experienced the impact of shortage of nursing personally. P5 reported that stress causes a major effect on nurses due to workload and also threatens her job.
“I experienced tiredness , stress and not satisfied with my job each day due to work overload . I normally go home late due to long hours of work and no time for my family which affects my family relationship . Even my family asked me to look for another health facility to work which has less workload” . P5 (a 31-year-old female RN)
Four of the participants stressed the effects of work overload and overtime due to nursing shortage causes stress and frustration and violence at home.
“Work overload and work for long hours causes a lot of stress and frustration where I don’t have enough rest , no time to relax , and not enough quality time for my family which causes frustration and violence in my home” . P23 (a 53-year-old female RN)
O ther participants (12) added:
“Stress is the result of tiredness and not enough rest especially when the ward is full and less nurses working and you have to double the shift” . P12 (a 40-year-old female RN)
2. Physical and mental risks
Some participants (6) stated that work overload and work for long hours causes more physical and medical risks
“Shortage of nurses affects our physical body very badly . We experienced back pain and back injury for trolleying patients to the theatre and to other diagnostic units……and we felt tired and cannot provide the best quality nursing care to our patients” . P20 (a 33-year-old female RN)
Other physical risks which was reported by all participants (25) is when they don’t have enough time to rest and eat or drink due to too much work load and limited nurses. P24 expressed that they don’t have enough time to rest and eat during busy times which affect her physical body and her health.
“Most of the time our ward is busy and those times I don’t have enough time to rest and eat or even drink which affects my physical health” . P24 (a 42-year-old female RN)
Workload with only few nurses causes a lot of medical risks on nurses’ health and clinical performance which leads to early retirement or were granted early retirement due to medical reasons. One participant stated:
“A lot of nurses in our hospital leave their job and most of them were granted early retirement due to medical health reasons which prevent them to continue with their job” . P11 (a 37-year-old-female)
“I worked almost 20 years now and I have medical issues which affect both my lower extremities and I have requested to take my early retirement because I won’t be able to work with the current health conditions . My health conditions will not only affect my well-being but will also affect my clinical nursing performance” . P7 (40-year-old-female RN)
Most nurses (15) reported that high job demands increase physical and mental health problems. P9 mentioned the impact of stress to physical and mental problem on nurses
“Stress affects our mental health when we are exhausted due to work overload which prevents us to think properly which also increases the chances to make mistakes” . P9 (a 56-year-old female RN)
“When we have too many patients and lack of skills especially for us inexperienced nurses , it affects us psychologically as well which can affect our performance” . P5 (a 31-year-old male RN)
3. Medical risk
One of the respondents stated that medical errors are one of the common risks that occur due to stress from working long hours or work overload.
“I have experienced the result of stress that causes high chances of errors in our work station which threaten the lives of the patient . Some prevented errors are the result of work overload and long hours of work which prevent nurses from perform their duties effectively and increase the chances to make mistakes” . P2 (a 34-year-old male RN)
Four participants reported that medical errors were seen in their work station due to physical and psychological stress where they gave incorrect medication to the patients.
“Few times I gave incorrect medication to patients because I can’t think properly due to tiredness and exhaustion or sometimes I gave the correct medication but I don’t explain it well to the patient especially the dose , time and route of administration” . P4 (a 34-year-old male)
“Most of the time due to frustration and too much workload I don’t practice infection control rules and regulations which cause more medical risk to my patients” . P11 (a 37-year-old male RN)
4. Social and family risk
Nurses experienced social and family risks when they have high volume of pressure and when patients are not receiving services immediately, they cause mischief to nurses and their families. P12 expressed his fear when patient and relatives were frustrated due to patients’ not receiving care or service immediately and threaten her family.
“I experienced most times especially when we have less nurses working in one shift in the emergency department when I and even my family were threatened when patients’ relatives got angry with me for not attending to them immediately or not treating them well as expected . Sometimes they threatened me and my family as well” . P12 (a 40-year-old female RN)
“Occasionally I get frustrated from work due to pressure and when I bring frustration to my home , it causes domestic violence in my home . This causes much risk to my family” . P6 (a 34-year-old male RN)
Prompted by the findings from the RNs in Vanuatu on the nursing shortage, it impacted the health service delivery throughout the Vanuatu population [ 14 ]. Although the Vanuatu MoH has been implementing strategies in the past to address the issues, the shortage of nursing is still evident with the current nursing workforce shortage of more than 400 where Vanuatu MoH is still unable to fill the shortage gaps [ 14 ]. The current study findings have reported the impact of nursing shortage on the nurses and their performance in providing quality care.
The working conditions for nurses have major influence on the nurse’s performance and the quality of care provided to patients due to job dissatisfaction. The findings emerged with the condition which includes workload due to high patients’ admission, lack of workforce and unusual working hours. Several studies have shown that job dissatisfaction always emerged along with poor working conditions due to workload and lack of workforce [ 19 , 20 ].
It is obvious that the workload in the health facilities within the MoH health system has been a long-term issue and become a challenge when few or limited number of nurses who care for the large number of patients admitted, and workload exceeds the number of nurses working in each shift. The maximum number of nurses working per shift is 2 to 3 nurses according to the findings, which is not effective to provide a quality care needed for nurses and patient’s safety. Although the managers within the hospital setting are aware of the workload issues, they have no better solutions to address the workforce shortage as it become a major challenge across the country that needs effective planning and policy directions from the policy makers at the government level. Studies stressed that work load is becoming a major factor when there are inadequate number of nurses working compared to the demand [ 21 , 22 ]. Other studies from other developed countries also reported that inadequate policy direction and planning has huge impact on nursing population including nurses’ workload [ 5 , 23 ]. The difference is that our study participants have experienced shortage and its impact while working in the hospital and might have limited knowledge about the policy and planning direction of Vanuatu MoH.
With few number of nursing staff compared to high workload, causes a lot of pressure and physical exhaustion to nurses. There are factors that contributed to lack of workforce identified by participants who include low student nurse enrolment or irregular training provided by the nursing college. Although the nursing college enrolled nurses continuously for the last 30 years, the number of output is so limited and does not match with the increased demand. Other health leaders also supported the fact that low enrolment in the nursing college is becoming obvious when looking at the current increase number of aging population of nurse within the MoH. Studies from other countries stated that low enrolment have significantly contributed to lack of workforce which affect nursing and their profession in the future [ 4 , 24 ]. The shortage were identified by the participants from the low number of nurses distributed and work in each of the hospital.
In this study it was found that most of the nurses working in the hospital had experienced long shift hours up to 12 to 16 hours or double the shift due to not enough staff to do shift work or when other nursing staff on sick calls or annual leave. The nurses stated that long working hours is very stressful which affects their work performance and as well as their social and family relationship. The nursing managers and senior clinical supervisors aware that nurses normally work on unusual hours when not enough staff to do shift work, and have noticed moral distress on nurses which affects nurses’ motivation to perform the job effectively. In other industrialized countries, one third of the nursing workforce has irregular or unusual working hours which significantly affects the nurses’ health and patient outcome [ 25 ]. Furthermore, pressure of working long hours contributed to nurses leaving their profession from job dissatisfaction and poor working environment. Study have shown that nurses leave their job due dissatisfaction with working condition in a stressed environment such as irregular working hours [ 26 , 27 ].
Findings shows that lack of support and lack of development opportunities and advancement in nursing practice were reasons for low motivations which affects nurses’ performance.
Most nurses reported that lack of support from the managers and supervisors causes low working morale and low motivation to perform duties effectively. Although the nursing managers and senior clinical staff are experienced in their position, nurses still haven’t received full support for the leaders. This includes no regular visits and no actions to nursing staff complaints or grievance. It is evident due to areas that yet to be resolved and need urgent actions from the managers. Studies show that nurses needed attention from the managers and supervisors to identify areas that needs urgent or serious attention or early detection of any problems that might occur among nurses and their work performance [ 20 , 28 ].
Most of the nurses stated that lack of development opportunities to advance in nursing practices is one of the common issues that create disappointment on nursing staff within their working environments. Nurses believed that when opportunities to advance is left too long or no attention from their superiors, it causes low motivation that leads to low performance that will certainly allow nurses to leave their job. Although the HR at the national level develop career pathway for nurses, most nurses are not given any chances to advance in their profession or capacity building as part of their professional development, which is also reflected on the level of Education on demographic information where the highest level for most nurses is diploma of nursing. A study in Iran has shown that lack of opportunities to advance in nursing and lack of professional vision towards nursing, cause discrimination among nurses and dissatisfaction which causes nurses intended to leave their profession [ 21 ]. According to the RNs personal characteristics, more than 50% have completed undergraduate studies with diploma of nursing as their highest level of nursing which reflect lack of professional vision to upgrade nurses to higher level which might results to low motivation in the workplace.
The findings perceived that stress and medical risks impact nurses that increase the chances to quit nursing profession.
Stress has major effect on nurses not only with physical exhausted but also has an effect on social and family relationship. Stress affected nurses due to workload and overwork which significantly affect the quality of care provided to patients as well. Majority of the RNs who work in the hospital might experience the impact of shortage of nursing personally because they have worked for more than five years. If stress was managed promptly, it will prevent burnout, job satisfaction and improve patients’ quality care. Although studies have shown that stress affect all nurses due to worldwide nursing shortage, the nursing managers and leaders in Vanuatu, who have in contact with nurses regularly must have better understanding of stress and its relationship and also its symptoms in order to manage stress effectively [ 29 , 30 ]. It is important for Vanuatu MoH to adopt stress management process by other countries in order to identify and management stress among nurses effectively.
Findings have shown that work overload and long hours’ work causes serious threats to nurse’s physical health. Furthermore, finding shows that nurses experienced injuries and other medical conditions while performing service. Furthermore, majority of the RNs have been granted early retirement due to medical reasons that might be due to work overload or poor working conditions. The challenges of having nurses gone on early retirement is when not enough nurses for replacement, however nurses with medical reasons need to leave their profession as they will negatively impact patient’s care and also their well-being. Studies supported that mental and physical health of nurses has significant effects on the quality of care provided to the patient [ 30 , 31 ]. On the other hand, other studies supported that senior nurses leave their profession before their retirement age due to medical reason and is necessary for patients’ safety to decrease mortality [ 32 , 33 ].
Furthermore, stress associated with nursing shortage has a significant impact on patients’ care in the hospital which causes much health risks and increase the risk of medical errors and lack of quality care up to a required standard. Findings show that, Vanuatu nurses were able to work under pressure, but medical errors can still be experienced at the workplace. Studies confirmed that medical errors are associated with nurses’ psychological stress and other health risks due to work overload [ 8 , 31 ].
Study strengths
The study is a high quality study and the first study that was conducted in the Republic of Vanuatu among the registered nurses. The study rigors was followed from conducting the study, data collection and data analysis. The study will benefit the Vanuatu ministry of health by enabling the policy makers to refine and develop relevant policies to address and strengthen the nursing workforce to meet the demand and improve delivery of quality health services to all individuals in both urban and rural settings.
Study limitations
There were some logistic limitations in terms of conducting interviews or reach the study participants easily due to was unable to Covid-19 pandemic. It was not possible to study other hospitals in Vanuatu to extract more information due to time limitation.
This study has identified many key factors that contributed to the shortage current nursing workforce and the impact it has on RNs which needs to be addressed promptly to resolve the shortage of nursing workforce Vanuatu in the coming years. Broad themes and sub-themes were identified which highlighted the impact of nursing shortage to RNs and the effects on their performance. The studies showed that stress or moral distress from work overload and lengthy hours shift impact the nurses’ physical, psychological, social, and family relationship.
The recommendation to assist the Vanuatu government through the Ministry of health to address chronic shortage of nurses is, the government should invest on establishing a much bigger nursing college to increase its yearly intake in nursing, to have interim plan to address the current shortage of nurses and review the whole nursing situation and nurses distribution, and to promote nursing in all the secondary levels of education.
Acknowledgments
We would like to thank all the study participants and those who were very supportive for their valuable time and participation in the interview.
Funding Statement
The authors received no specific funding for this work.
Data Availability
San Jose Inside

San Jose Inside (https://www.sanjoseinside.com)
CSU Opposes Bills to Expand Ability of Community Colleges to Offer Nursing BA Degrees
By mikhail zinshteyn / 2 hours ago 0.

Graduating nursing students wait for the commencement ceremony to begin at Southwestern College in Chula Vista in May. Photo by Adriana Heldiz, CalMatters
Is there a nursing shortage in California? Now, yes, though in a few years, probably not.
By 2027, the state is projected to have as many nurses as it needs because of a rise in nursing program enrollment, according to UC San Francisco projections compiled for the state agency that regulates nursing programs. The report was published last year.
But there are other sub-shortages in California’s nursing workforce. Two bills passed by the Legislature last week focus on one of those: nurses with bachelor’s degrees.
Both target a growing demand for nurses to possess bachelor’s degrees by allowing some community colleges to issue them. Presently the colleges only provide associate degrees — generally the minimum degree needed to be a registered nurse.
The bills are the latest developments in the state’s ongoing quest to tweak the educational offerings of colleges and universities to address cultural and workforce needs, from requiring ethnic studies courses to permitting colleges and universities to issue degrees they haven’t before. But the bills also underscore the complexity of both identifying a labor force problem — a nursing shortage — and the role that community colleges and universities play in graduating skilled workers.
One is Senate Bill 895 by Sen. Richard Roth, a Democrat from Riverside. The other is Assembly Bill 2104 by Assemblymember Esmeralda Soria, a Democrat from Merced.
The California State University opposes both bills, viewing them as undermining a promise lawmakers made two years ago that community colleges wouldn’t issue bachelor’s degrees that duplicate existing Cal State programs, among other worries. Private colleges oppose the bills, as well. The University of California doesn’t officially oppose the bills but raised similar concerns .
Understanding the nursing shortages
Even as the state may not have an industry-wide nursing shortage by 2027, there are still stubborn sub-shortages.
While California has seen the number of nursing education program slots grow by 3,000 between 2018 and 2023 , virtually all of that was at private nonprofit and for-profit campuses . Available slots at the more affordable public colleges and universities have remained flat.
There are regional differences, too, with California’s Central Valley and the Central Coast lacking enough nursing program slots to meet demand. “Those would be the regions that I would point to as having the biggest challenges,” said Joanne Spetz, a researcher at UC San Francisco who studies the state’s nursing sector and co-wrote the projections report
Yet another micro-shortage stems from the fact that more hospitals prefer — or require — hiring nurses with bachelor’s degrees . That makes sense: Several academic studies concluded that hospitals that increased their share of nurses with bachelor’s degrees saw lower rates of patient death and shorter hospital stays .
And an overall shortage may still persist past 2027 due to “high rates of burnout” that “may lead to greater turnover and departures from nursing,” the projections report said.
What the two bills will do
Enter the two bills the Legislature passed last week.
Will they lead to more registered nurses? Speaking of his bill in July, Roth said no. But it would help produce more nurses with bachelor’s degrees — which more hospitals say they want, he said.
The bill authors — as well as their community college and hospital backers — say some community colleges should be allowed to issue bachelor’s degrees in nursing for other reasons, too.
Students who live too far from a California State University or University of California nursing program could enroll at a community college and avoid long commutes to the public universities or much more expensive private colleges . There are more than 70 community colleges in California that offer associate degrees in nursing and 21 public universities — mostly through the Cal State system — that award bachelor’s degrees in nursing . And while some universities offer online programs, not every student has fast-enough internet or enough computing power at home, Roth told lawmakers .
Students with associate and bachelor’s degrees take the same licensure exam. Typically a bachelor’s degree in nursing requires about 30 more units of coursework, which takes about a year to complete.
Both bills seek to form pilot programs that each allow just 10 community college districts — out of the state’s 73 — to offer bachelor’s degrees in nursing.
But they vary in other ways. Soria’s bill places an emphasis on pilots in the Central Valley , which has a chronic nursing shortage. Roth’s bill is aimed at the whole state, though it would focus on the Central Valley and other regions by prioritizing pilot programs in underserved communities. Both would require the Legislative Analyst’s Office to evaluate the pilots, but Roth’s bill would have the pilot programs last until 2034 while under Soria’s bill the programs would run until 2031.
Roth’s bill requires colleges in the pilot to have national accreditation, which can take several years to accomplish. Soria’s bill doesn’t specify that. Still, 28 community colleges already have national accreditation, according to a July legislative bill analysis.
The differences raise questions about how Gov. Gavin Newsom may reconcile the two bills.
That’s one reason why the California Community Colleges Chancellor’s Office is “recommending the governor sign SB 895” over Soria’s bill, wrote Melissa Villarin, a spokesperson for the California Community Colleges Chancellor’s Office, in an email Wednesday. She also noted that either bill getting Newsom’s signature would be a “major victory.”
The chancellor’s office prefers Roth’s bill because it was sponsored by statewide groups close to the central office, including the Community College League of California, which represents community college administrators and trustees. Roth’s legislation is also a “bill where more attention and efforts (in terms of negotiating amendments) have been focused throughout the legislative process,” she wrote.
Why Cal State opposes bachelors degrees at community colleges
Both bills are creating a panic for Cal State leadership and the system’s nursing programs. There’s the fear that the community colleges will eat Cal State’s enrollment lunch by offering bachelor’s degrees that are cheaper than what Cal States charge.
Roth’s bill “will siphon off the students” who’d “otherwise come to a CSU nursing degree program,” said Rehman Attar , director of health care workforce development at the Cal States, during a July legislative hearing. He said the same about Soria’s bill .
Forming new bachelor’s programs at community colleges is expensive, he argued. Cal State’s online bachelor’s programs and the system’s fast-track bachelor’s degree programs with 37 existing community colleges can meet the bills’ goals, he said in an interview. More of these partnership programs are pending, he added .
There’s also a philosophical battle brewing over the distinct roles of each higher education segment in California. For decades, the state’s 1960 Master Plan for Higher Education stipulated that the community colleges offer certificates and associate degrees; Cal States chiefly provide bachelor’s degrees and master’s degrees; and the UCs focus on research by offering bachelor’s, master’s and doctoral degrees.
But in recent years, the Legislature has permitted the community colleges to award bachelor’s degrees, with the proviso that those degrees don’t duplicate the degrees already offered at Cal States. Both systems have fought over the practicalities of that détente , but the bills proposed by Roth and Soria would knowingly blow up that public policy peace by allowing the community colleges to offer the same nursing bachelor’s degrees the Cal States already provide.
“Our overall opposition is, of course, we’re opposed to duplication,” Attar said in an interview. Both bills received wide bipartisan support. However, a few Democrats — who have a supermajority in the Legislature — expressed reservations about the emerging mission creep of the community colleges.
Among those is Sen. Josh Newman, a Democrat from Fullerton who is chair of the Senate’s education committee. During a hearing on Soria’s bill , he said that the master plan assumed a “division of labor, if you will, between the segments. And largely because of geographical and workforce needs, we’re seeing that erode. I believe that is problematic.”
Roth’s bill would also create new layers of pricing. It would cap tuition for the pilot nursing bachelor’s degrees to be no more expensive than other community college courses — $46 a unit — wrote Villarin.
Existing bachelor’s degrees at community colleges have tuition charges that are capped at $10,560, excluding course and campus fees, so Roth’s bill would make a nursing bachelor’s roughly half that. Meanwhile, Cal State systemwide tuition, excluding fees, is now more than $6,000 a year and will grow by 5% annually through 2028-29 .
Spetz of UC San Francisco said the lack of public bachelor’s degree programs in nursing is a real barrier to Californians in remote parts of the state where there’s no nearby university.
“The only way to pursue a bachelor’s degree, if you’re in some of those communities, is to either do an online program, some of which are excellent and some of which are not so good, or to relocate to do a bachelor’s degree, which just seems kind of silly and isn’t possible for many people,” she said.
She’d recommend limiting the pilot programs to community colleges that are particularly far from a public university with a nursing program. “I think having a distance threshold and really focusing on regions where there is not a public bachelor’s degree opportunity for folks …is a reasonable thing to test.”
Mikhail Zinshteyn is a reporter with CalMatters.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

IMAGES
VIDEO
COMMENTS
A systematic review study on the factors affecting shortage ...
The same nursing shortage that has been a concern for decades is now wreaking havoc on the U.S. health care system. The research findings are undeniable: Our country's urgent shortage of nurses has reached catastrophic proportions. While dire, the problem has solutions that we can begin to implement now.
NCSBN Research Projects Significant Nursing Workforce ...
83% feel their mental health has suffered. 77% feel unsupported at work. 61% feel unappreciated. 60% have felt uncomfortable having to work outside of their comfort zone in the past year. 58% of nurses have felt frustrated with their patients. 58% of nurses have felt unsafe at work in the past year. The numbers don't lie.
Addressing the Nursing Shortage in the United States
Nursing Shortage - StatPearls
Nursing in 2023: How hospitals are confronting shortages
It has been projected that nursing will be one of the top profes- sions for job growth until the year 2029. It's expected that the RN workforce will increase by 7%, or 221,900 nurses, in the 10-year period from 2019 to 2029. This is in addition to 175,900 projected RN jobs each year until 2029.
Nursing Shortage Fact Sheet
Addressing the Nursing Shortage: The Voices of Nurses
Sorting Out Fact and Fiction of a National Nursing Shortage
graduate nursing programs in 2018 due to insufficient resources, such as a lack of faculty and clinical sites. 12. Two contributing factors to the shortage of nursing faculty members are: many are approaching retirement, and not enough nurses are opting for a career in nursing education to replace the retirees. 13 . Clearly, there is a need
When reviewing nursing shortage data at the state and national level, the numbers can be confusing. The Bureau of Health Workforce projects that California will face the largest nursing shortage of any state, with a projected shortfall of 44,500 nurses by 2030. In contrast, the state of Florida will have a projected surplus of more than 53,000 ...
The Nursing Shortage and Work Expectations Are in Critical ...
Nursing Workforce Challenges in the Postpandemic World
Nursing Shortage Projected to Be Worse By State in 2030
The Real Issues Driving the Nursing Crisis
The Nursing Shortage Explained | Causes & Solutions
A nursing shortage refers to a situation where the demand for registered nurses (RNs) and other nursing roles exceeds the supply—locally, nationally, or globally. This deficit isn't a new phenomenon. In fact, sporadic shortages have been recorded over the decades. However, the current and impending scarcity is unparalleled in its reach and ...
Nursing shortage: Nursing shortage is the struggle to expand capacity to meet the. rising supply and demand for nursing workforce nationally (Mee, 2014). Registered nurses (RNs): RNs provide and coordinate patient care, educate. patients and the public about various health conditions, and provide advice and emotional.
A 'shortage' is therefore not merely about a numbers game or an economic model, it is about individual and collective decision-making and choice (Buchan 2000, 2006). The 'shortage' is not necessarily a shortage of individuals with nursing qualifications, it is a shortage of nurses willing to work as nurses in the present conditions.
nursing shortage. This qualitative multiple case study sought to identify specific and effective strategies used by nursing managers to manage nursing shortages. The sample for this study was eight nurse managers who demonstrate effective strategies to manage the nursing shortage in the Midwest, such as Illinois, Indiana, and Kansas, and who
Even as the state may not have an industry-wide nursing shortage by 2027, there are still stubborn sub-shortages. While California has seen the number of nursing education program slots grow by 3,000 between 2018 and 2023, virtually all of that was at private nonprofit and for-profit campuses. Available slots at the more affordable public ...
Conclusion. This study has identify factors affected shortage of current nursing workforce and the impact it has on registered nurses. Broad themes and sub-themes were identified which highlighted the impact of nursing shortage to registered nurses and the effects on their performance which includes stress or moral distress from work overload and lengthy hours shift which impact the nurses ...
Understanding the nursing shortages. Even as the state may not have an industry-wide nursing shortage by 2027, there are still stubborn sub-shortages. While California has seen the number of nursing education program slots grow by 3,000 between 2018 and 2023, virtually all of that was at private nonprofit and for-profit campuses. Available ...