

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
- Visit Nurse.com on Facebook
- Visit Nurse.com on YouTube
- Visit Nurse.com on Instagram
- Visit Nurse.com on LinkedIn
Nurse.com by Relias . © Relias LLC 2024. All Rights Reserved.

Critical Thinking and Nursing Care Plans Go Together Like Chicken and Waffles | NURSING.com
.png?width=50&height=50&name=image%20(12).png)
What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Ahhhh.. chicken and waffles. They don’t sound like they should go together, but they do. They so do.
Apart they are delicious, but together.. they just make sense.

It’s the same with critical thinking and care plans.
Coming up with a nursing diagnosis, nursing interventions, and using your clinical judgment to decide upon the best way to approach how you direct your care for your patient for the day as well as how you navigate obstacles are one in the same.
What is Critical Thinking?
When I was in nursing school, I didn’t really understand what the professors meant when they said the term critical thinking . I just nodded along and pretended like it made sense to me.
I started to understand a bit more when I got into clinicals and really understood not only what it meant to think critically, but also what it felt like to critically think in the moment.
Critical thinking is something that you will do every single shift as a practicing nurse. Not one day will go by in which you do not think critically.
"Critical thinking is something that you will do every single shift as a practicing nurse"
Click to Tweet
I will take a second to describe this process, but keep in mind that it occurs much more fluidly than this description.
I liken this to learning how to shoot a layup in basketball. When you’re a beginner, you learn each step and then put them together. It looks and feels very mechanical at the beginning. However, as you get more comfortable with the process, going through it becomes much smoother and more fluid and eventually you’ll be at a point where you’re doing it without even realizing it.
- First, you will recognize a problem or issue.
- Then you will determine the best solution / nursing intervention.
- You’ll then determine if your intervention was successful and if you need to intervene again.
Example: The low oxygen saturation
(More examples at the end of the post!)
You are at the nurse’s station and see your patient’s oxygen saturation is 82%. You go into the room and see your patient is scrunched down in the bed with their nasal cannula is on the bed, labored breathing and coughing weakly.

I need them to get their oxygen saturation back up to 98%, like 3 minutes ago!
Nursing intervention
You decide to grab a coworker and have them help you boost your patient up so they are sitting straight up. You quickly reapply their nasal cannula. You hear them trying to clear their throat and grab the suction and clear a large amount of sputum that was caught in the back of their throat.
You see their oxygen saturation bounce up to 95%, and then up to 100%, and they are no longer coughing or experiencing labored breathing. They ask you what time lunch trays should arrive.
The Development of Critical Thinking
Learning how to critically think takes time. It is not something you just read in a textbook and can immediately apply. It requires foundational knowledge (like in the previous scenario, knowing what kind of troubleshooting to implement when a low oxygen saturation is occurring) and experiences.
This concept gets introduced in nursing school and you start to see it in action during clinicals. It will be mechanical at first, but eventually you will be critically thinking with the best of them. It just takes time, knowledge, and experience to really know how to see a situation (or multiple situations) and know the best plan of attack.
Practice (Not a game… practice )
(High-five to all of you Allen Iverson fans out there.. 2016 Hall of Famer – what what!)
While it does take time to become a competent critical thinker, you can begin to practice this. Whenever you have one-on-one time with a clinical instructor, physician, NP/PA, or someone else that is experienced in the field, it’s a great idea to practice this in down time. For example, if you are doing your senior year preceptorship in an intensive care unit and you’re working with one ICU nurse, you can being to ask them questions to further develop your knowledge base, learn from their experiences, and test yourself.
If you’re dealing with a septic patient in an intensive care unit, you could ask questions like..
- “So what would this patient present like in the emergency department to clue the triage nurse in to the issue of sepsis?”
- “If they weren’t responding to treatment, what would that look like… how would we respond?”
- “If his blood pressure starts to decrease, what would your first reaction be?”
- “When would you start to get concerned?”
- “I know antibiotics are important in treatment of a sepsis patient, but how would I know if the ones we’re using aren’t working?”
- “What’s the biggest complication we’re facing with this patient… how would I know that’s beginning to occur?”
What are Care Plans?
Note: There are quite a few different confusing resources for this topic floating around out there on the internet. To keep things consistent, the only resource I will use to outline care plans and definitions will come from the NANDA International website.
So now that we’ve talked about what critical thinking practically looks like, let’s chat a little bit about care plans. Going through nursing school, I felt like care plans were the least straightforward aspect of school. It took a long time for me to really feel like I kind of knew what I was doing… and I still wasn’t even sure if I got it.
Care plans are exactly what they sound like: they are a basic plan behind the care you’re going to provide.
What the heck is NANDA, NIC and NOC?
NANDA used to stand for the North American Diagnosis Association until 2002. They are now just officially known as NANDA International (or NANDA-I) because they grew quite a bit and are not limited to North America. They have basically created a standardized list of nursing diagnoses. It’s important that everyone, regardless of facility, is using the same terminology when referring to these kinds of things.
NIC stands for Nursing Intervention Classification. It’s the same concept as NANDA-I… it is a standardized list of nursing interventions.
NOC stands for the Nurse Outcomes Classification. It is a standardized list of nursing outcomes.
So to review.. NANDA-I is for diagnoses, NIC is for intervention, NOC is for outcomes.
It’s extremely helpful to have this massive, research-based, agreed-upon terminology. So if you’re working in New Jersey, you’re using the same terminology as the nurses in Hawaii. This is helpful for staff as well as patients.
There are quite a few textbooks related to nursing care plans and nursing schools may require different ones. They should include the most recent NANDA-I, NIC, and NOC approved terminology. They are the foundation of the care plans. It is imperative we are speaking the same universal language.
But before we can really dig into nursing care plans though,, we need to clearly define and discuss a few frequently used terms that all of your books will refer to over and over again. If you fully understand these, it makes the whole process much clearer.
NURSING DIAGNOSIS
When we hear the word diagnosis, we tend to assume we know what that means . Try to suspend judgement! I say this because a nursing diagnosis and a medical diagnosis are two completely different things. The medical team will make their medical diagnosis, write their progress notes, their orders, and so forth. Independently from that, the nurse will look at the patient’s medical diagnoses and entire clinical picture and develop their nursing diagnoses. These nursing diagnoses will guide how they provide and prioritize their care.
First let’s talk about what a nursing diagnosis is…
Here is the official definition of the term nursing diagnosis from the NANDA-I website:
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability.
Here is the NRSNG translation of the term nursing diagnosis :
A nursing diagnosis is something the nurse decides is a priority for their patient after they have looked at their entire clinical picture (gathered from assessment, report, and the patient’s chart). These diagnoses will guide the nurse’s care and priorities for the patient.
To come up with your nursing diagnosis, you’ll look at the patient’s subjective and objective data. This can be kind of confusing, especially when you first start looking at it. We have a really great post that helps differentiate between subjective and objective data here .
So now that we are on the same page about what a general nursing diagnosis is, let’s talk about the three kinds of nursing diagnoses. They are problem-focused, health-promotion, and risk nursing diagnoses.
Let’s define each so you fully understand each term.
Please note, the following 3 examples of different nursing diagnosis came directly from the NANDA-I website and can be found here .
PROBLEM-FOCUSED NURSING DIAGNOSIS
Here is the official definition of the term problem-focused nursing diagnosis from the NANDA-I website:
A clinical judgment concerning an undesirable human response to health conditions/life processes that exists in an individual, family, group, or community. In order to make a problem-focused diagnosis, the following must be present: defining characteristics (manifestations, signs, and symptoms) that cluster in patterns of related cues or inferences. Related factors (etiological factors) that are related to, contribute to, or antecedent to the diagnostic focus are also required.
Here is the NRSNG translation of the term problem-focused nursing diagnosis :
A nursing diagnosis that is focused on a problem the nurse identifies after considering the entire clinical picture. Defining characteristics and related factors must be present.
“I see __________ problem (diagnosis) and things that are related to the problem are ______________ (related factors), and I know this problem exists because I’ve observed/measured ____________ (defining characteristics).”
“Anxiety related to situational crises and stress (related factors) as evidenced by restlessness, insomnia, anguish and anorexia (defining characteristics).”
HEALTH PROMOTION NURSING DIAGNOSIS
Here is the official definition of the term health promotion nursing diagnosis from the NANDA website:
A clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential. These responses are expressed by a readiness to enhance specific health behaviors, and can be used in any health state. Health promotion responses may exist in an individual, family, group, or community. In order to make a health-promotion diagnosis, the following must be present: defining characteristics which begin with the phrase, “Expresses desire to enhance…”.
Here is the NRSNG translation of the term health promotion nursing diagnosis :
This diagnosis focuses on optimizing and promoting the health for that patient. We know this is an appropriate diagnosis because the patient has expressed desire from the patient to improve their health. Defining characteristics must be included.
“This patient is ready to learn more about _________ because they told me they were.”
“Readiness for enhanced self-care as evidenced by expressed desire to enhance self-care.”
RISK NURSING DIAGNOSIS
Here is the official definition of the term risk nursing diagnosis from the NANDA website:
A clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes. In order to make a risk-focused diagnosis, the following must be present: supported by risk factors that contribute to increased vulnerability.
Here is the NRSNG translation of the term risk nursing diagnosis :
A nursing diagnosis that expresses something the patient is at risk for. Risk factors must be included.
“This patient is at risk for __________ and I know this because of ___________ factors.”
“Risk for infection as evidenced by inadequate vaccination and immunosuppression (risk factors).”
A FEW MORE IMPORTANT TERMS…
- Risk factors: something that would increase the likelihood of something else. These are only in risk diagnoses.
- Related factors: something that is related to the nursing diagnosis. Examples of how you may state risk factors in your diagnosis can include “associated with, related to, contributing to,” or other. These must be included focused diagnoses and can be included in health-promotion diagnoses, but are not required.
- Defining characteristics : things you can witness yourself or measure that are related to your diagnosis. You observe defining characteristics with your 5 senses (just hopefully not taste..)
- “Patient will report pain of 4/10 within 60 minutes of medication administration and repositioning”
- Pain medication administration, reposition, pillow support to increase comfort and decrease pain level
- Use direct verbiage.. “I will _______” / “patient will _______”
- This may seem like an odd thing to include… but sometimes, you’re not able to complete the interventions you wanted to for a variety of reasons. While you had a goal with specific interventions identified, maybe the patient declined or was discharged or was at a procedure so you could not implement your interventions. That’s why they want you to say whether or not you intervened. Saying you did not does not may you a bad nurse, unless the only reason you did not intervene was because you didn’t feel like it.
- Note why something didn’t occur in the evaluation section
- “Patient reported pain scale of 6/10 in 60 minutes of intervention
- Evaluation: what this an appropriate plan?
Alright, so I’ve walked you through some of the really technical, standardized language of the nursing care plan process…
Let’s Practice Nursing Care Plans
Let me walk you through how this realistically works…
You are getting report on your patient.
(Please note, this is not full report, rather specific information from report)
Your patient has had a massive stroke and cannot move the left side of his body and doesn’t have the best control with the right side. PT tried to get him up yesterday and he just couldn’t handle it. He has a history of chronic back pain and has had a pretty consistent headache since the stroke. He’s somewhat impulsive and he’s set the bed alarm off a few times. He doesn’t eat much. It’s hard to tell if it’s because he hates his pureed food, if he has no appetite, or if he’s purposefully refusing intake.
So when I hear that in report, I start identifying problems and nursing interventions for him during my shift and some goals to evaluate whether or not my interventions were successful.
- He’s had a massive stroke and cannot move the left side of his body and doesn’t have the best control with the right side = risk for skin breakdown (PROBLEM) .. I’ve got to make sure I am on top of turning him at least every 2 hours with lots of pillow support, thoroughly assessing his skin, and making sure he’s got adequate nutrition. (INTERVENTIONS)
- Massive stroke + PT tried to get him up yesterday and he just couldn’t handle it + He’s somewhat impulsive and he’s set the bed alarm off a few times = he’s a high fall risk … I’ve got to make sure I’ve got all of my fall interventions in place. That means he’s wearing non-skid socks when he’s up, the bed alarm is on, if possible I’ve got him in a room near the nurse’s station, increase the frequency of my rounds, I reorient him if he becomes disoriented, I make sure the call bell is within reach, and evaluate if I really need any meds that may decrease his alertness.
- He doesn’t eat much. It’s hard to tell if it’s because he hates his pureed food, if he has no appetite, or if he’s purposefully refusing intake = he’s at risk for inadequate nutrition (if a patient isn’t getting proper nutrition, it’s pretty difficult for the body to heal). I’ll make sure to get any food preferences that he might have, encourage oral intake, try to figure out why he’s not eating, make sure the food is warm and he consumes it promptly after arrival, and work with the dietician to see if any dietary supplements are necessary/appropriate.
When I get towards the end of my shift, I start to evaluate if my care plan was effective… if my problems and interventions were appropriate and/or successful.
Care plans are something you decide upon at the beginning of the day and implement throughout your shift. Towards the end of your day, you document what they were and if they were progressing or not. You resolve goals that were achieved that are no longer applicable, initiate new ones if needed, and chart on existing ones that are still applicable.
I put this thought process in a chart below. What used to be this vague process in school is now second nature to me now that I do this every single shift. This is basically my thought process, not necessarily what I would document.
|
| |||
|
|
| ||
|
|
|
|
To summarize… I listen to report, check the chart, and assess my patient. Between those actions, I decide what kind of problems exist, what goals I have for the patient, and which nursing interventions would best help me achieve these goals for my patient. Throughout the shift, I implement my nursing interventions and afterwards I will evaluate whether or not we’re progressing towards the goals or if we’re not progressing.
So when you’re creating your care plans for clinical or courses, you’re basically doing the above process in a very specific format with very specific verbiage.
“This now seems straightforward.. but why is this still so difficult for me to understand?”
This is difficult for nursing students because you haven’t seen a ton of patients yet.
If you’ve never cared for patient with heart failure before, it’s hard to pick out the specific nursing diagnoses that would be appropriate for them… as well as the subsequent interventions, goals, and how to evaluate.
So if you’re not experienced with providing nursing care (and you shouldn’t be since you’re a nursing student!) … you don’t know the typical nursing diagnoses, interventions, normal responses, and normal expectations for said interventions. That’s why when you’re opening your care plan book, it looks like a foreign language. That’s why it’s hard to put these pieces together. Learning how to hear about what’s going on with a patient, meeting them, assessing them, and reading their chart and then quickly deciding how you’re going to plan your care for the day takes practice. It’s not something you can study for a few days, take an exam, and know how to do perfectly.
You’re learning in nursing school… and it takes a little while to learn how to develop this skill.
When I think back about my mental thought process during school,, I felt like it was a big performance. Every clinical, every class, every interaction was to show how much I knew… but when I look back, that’s not at all what it is or should be. It’s a time to learn how to do this stuff, not be perfect immediately.
(Sorry if that’s an obvious thing but I’m one of those who always asks “stupid” questions and needs the obvious explained to me kinda person!)
I highly advocate not waiting until the last minute to turn care plans in. They are tough to understand and it may take going to your professor’s office hours and really sitting down and talking through them to understand it.
I say all that to say – don’t think you’re stupid if this doesn’t make sense to you immediately. Please don’t become discouraged and think nursing isn’t for you if this doesn’t click after the first explanation. This takes time because there are a lot of things to think about and consider while forming these care plans.
I also recommend not looking at care plan assignments as something where you’ll get a perfect grade the first time and every time after that. I was pretty hard on myself when I’d miss little things here and there with care plans. Looking back, I really should not have been. There is a natural learning curve so expecting to pick it up immediately and never miss a point is somewhat unrealistic.
Creating a good nursing care plan isn’t just something you do quickly so you can check off you’ve done it. It truly takes time to learn how to do it correctly, which means you’re probably not going to get it right the first few times around.
Care Plans + Critical Thinking = Optimal Patient Care
When you decide upon your nursing diagnosis and start to prioritize your care by having these goals in mind. It orders your steps, in a way. You really have goals in mind to help the patient progress to discharge, rather than just getting them to the next shift.
That is the key,
The goal is for the patient to progress, not for you to complete your shift.
Just because your meds were passed, your patients were assessed and charted on and the medical team rounded, ordered new things and you implemented them doesn’t mean you provided good nursing care.
Imagine you are married to the love of your life… Alex. Oh, Alex. You’re always there. You’re the yin to my yang. The X to my Y. The Pam to my Jim. The chicken to my waffles.
Now imagine they broke their femur in a bicycling accident, had urgent surgery, and are now on an orthopedic floor. . .
(Kinda harsh, I know but bear with me..)
You’ve got Nurse A that walks in, gets report, looks at the chart and gets to work. They pass their meds on time. Give Alex IV pain meds whenever they want… draw labs when they’re ordered… help Alex to the bathroom when they ask…. Although Alex spent about 80% of the day in bed because the pain meds made them really sleepy. Nurse A answers questions when asked, but they don’t really explain anything. At the end of the day, they give the next shift report and they leave.
At the end of the day, Alex still needs pain meds frequently, felt groggy all day, barely got up, and didn’t eat much. He/she needs a decent amount of help getting up and sitting down whenever using the restroom and hasn’t seemed to improve a whole lot.
Dr. Smith, who operated on Alex right upon admission, rounded towards the end of the day, while Alex was sleeping. She wrote the following in her progress note: “Transition to oral pain meds, increase ambulation, discharge in next 72 hours.”
Successful shift… right? Everything was technically done/completed on time… doesn’t that mean they did a good job…?
You’ve got Nurse B who walks in, gets report, looks at the chart and gets to work. After report, Nurse B decides pain management, promoting mobility, and preventing skin breakdown are going to be important today to get your BFF home and doing better ASAP. Nurse B looks closely at all of the orders (meds and nursing intervention orders) to make sure to prioritize this stuff today.
Nurse B starts out the day by letting you and Alex know the plan for the day… “We’re going to try to transition from IV to oral pain meds for better, longer relief. It’s really important to get out of bed as much as possible today so we’ll get at least 2 walks in, but hopefully 3. I also want you out of bed for each meal. And we really want to make sure you’re not sitting on your butt all day because you skin can start to break down, so if you decide to sleep, let’s get some pillows and prop you up on your side, if that’s comfortable.”
Nurse B gave oral pain meds with the rest of Alex’s meds at the beginning of the shift. Nurse B made sure to get Alex up for all 3 meals and walked with him/her twice. When Alex said he wanted to take a nap during the afternoon, Nurse B came in and got him positioned up on his side. He/she slept like a rock for an hour and a half.
Dr. Smith, who operated on Alex right upon admission, rounded towards the end of the day, while Alex was up in the chair and eating dinner. She wrote the following in her progress note: “Continue current plan, discharge tomorrow.”
At the end of the shift, Alex had not needed another dose of IV pain meds despite all of the increased mobility. He/she walked twice, was up to the chair for all of the meals. Getting up the first few times was tough, but it got easier as the day progressed. By the end of the day, Alex was basically walking himself/herself to the bathroom with just the assistance of a walker and someone near by just in case.
So, which nurse had a more productive and successful shift?
They both passed their meds on time… Responded to call lights and needs verbalizing by the patient. So, all is well.. Right?
Nurse A got the tasks done for the shift, but didn’t have a plan. Nurse A did not have discharge in mind. Nurse A just wanted to get to the end of the shift. Nurse A was passive.
Nurse B had a plan. Nurse B had a care plan.
Nurse B thought about the needs of a patient with a fractured femur and prioritized care for the day. Nurse B communicated. Nurse B made sure their patient progressed towards discharge.
So, which nurse do you want caring for your loved one? Your BFF? The chicken to your waffle?
Adding Critical Thinking Back In
So imagine the above situation with Alex, but something goes wrong. Alex starts to get a fever… or gets tachycardic.. Or has sudden increasing pain uncontrollable by previous doses of pain meds…
You will use critical thinking to figure out what’s going on and the best way to address it. You’ll step back, look at the clinical picture and think. Critically, of course.
(Gosh I am on a ROLL people!)
You also use critical thinking to develop your care plan in the first place. Critical thinking enables you to figure out what’s important for this patient … why it’s important … why it’s important … how to get it done … and enables you to look at how it went at the end of the day and where the next shift needs to pick up where you left off.
Yes, This Stuff is An important Part of Being a Safe Nurse – We Promise!
I promise this is all not only important, but will be information you will you use every shift. You know how you’re sitting in class and you think, “Will I really need to know this to get through my shifts?”
Absolutely and unequivocally yes.
Real Life Critical Thinking + Nursing Care Plan Examples
Ok, let’s go through some examples of scenarios that require both critical thinking and care plan implementation!
Example 1: Falling Over You
Your patient is detoxing from alcohol. She has a really unsteady gait when they get up, weak, and have intermittent confusion. You don’t feel comfortable leaving her just sitting in the bed because if she gets up on their own, you think she may fall. You want to do all you can to prevent her from falling.. She is quite frail and you’re pretty sure she’ll break a bone if she hits the deck… So you try to think of all the little things you can do…
Critical thinking: So you make sure the bed alarm is set before you walk out of the room each time, whenever she does get up you make her put on those non-skid socks (even though she hates them), she’s in a room close to the nurse’s station, you always make sure her call bell is within reach, and you make sure to check on her a little more frequently than you technically need to just to ask if she needs to go to the bathroom or anything to drink or eat to prevent her from just getting up on her own.
Nursing diagnosis: high risk for falls related to cessation of alcohol intake as evidenced by unsteady gait, confusion, and weakness.
Patient goals : patient will remain free from falls, patient will remain free from injury, patient will utilize call bell prior to getting out of bed
Interventions: bed alarm on at all times, patient will wear non-skid socks when out of bed, ensure patient is in room close to nurse’s station, increase frequency of rounds,
Implementation: did you do your interventions.. Yes or no?
Evaluation: ⅔ goals achieved (patient did not fall and did not suffer injury), patient did not consistently use call bell despite it being in reach throughout shift. Will remind patient to use as well as reorient. All other interventions successfully implemented and helped to achieve goals.
Example 2: Dry Time
Your patient is has hyperemesis gravidarum and is dehydrated from having severe nausea and vomiting the last 3 months. When you did her assessment, she told you her mouth was really dry, as was her skin when you took her socks off to check her pedal pulses. You start to think about why she might be dry and remember that she can’t keep any food or liquids down.
Critical thinking: You decide to ask her to see if the antinausea meds are working and if the timing of them works out with her meals. You ask her if she enjoys the taste of the various oral liquids she has and if there’s anything different you can try to get her to increase consumption. You notice she has normal saline infusion at 50 ml/hr but decide to touch base with the medical team to see if it would be appropriate to increase that rate until her dry mouth/skin start to improve and she keeps more liquid down.
Nursing diagnosis: fluid volume deficit related to nausea and vomiting as evidenced by dry mucous membranes and skin, minimal oral intake.
Patient goals: patient will consume 50% of each meal, patient will report that antinausea medication regimen is effective, patient will report improvement or resolution of dry mouth
Interventions: Will assess and optimize antinausea medication schedule and time appropriately with meals, will identify 3 liquids and 3 foods the patient verbalizes do not increase nausea and order them from kitchen, discuss increasing intravenous hydration with medical team
Implementation: Zofran was given every 6 hours, Phenergan every 6 hours on an alternating schedule so that patient was receiving medication approximately every 3 hours; meds given approximately 1 hour before meal times to ensure they were at their peak when meals were hot. Three foods and liquids identified; our kitchen did not carry the brand of ginger ale she requested; spoke with partner who will bring it tonight after he gets off work. Discussed IVF with medical team.
Evaluation: Patient reported that administering the antinausea meds before nausea and vomiting became severe was much more effective; she consumed 50% of lunch and breakfast and 75% of dinner. Patient reported that having the specific foods available when meds were at their peak was also effective and increased consumption. Medical team increased ordered IVF to 100 ml/hr at approximately 1300. By shift change, patient reported her dry mouth was beginning to resolve.
Example 3: He’s Gotta Go
Your patient had back surgery 1 week ago. Prior to surgery, he was taking narcotics long-term for pain control and was being seen at a pain management clinic. Your patient has not had a bowel movement since 4 days preoperative. It has been 11 days since his last bowel movement. Post-operatively, he was on a Hydromorphone PCA for 4 days and transitioned to oral pain medications. He is taking 10 mg oxycodone every 6 hours. In report, he said he feels really constipated. He said he has only passed gas a 1-2 times a day since surgery. When you did your assessment, you noted hypoactive bowel sounds. When you looked at his chart, you noted that he was not started on a stool softener or any bowel regimen post-op.
You decide this guy needs to poop! Like, yesterday!
Critical thinking: You decide you probably should talk to the medical team about getting some meds to get his bowels going. You also noticed that he hasn’t been getting up much either. He’s been getting the same amount pain meds around the clock and wonder if he gets up and moves around regularly if he’ll need this many..or if you can mix in a Tylenol instead of so much oxycodone.
Nursing diagnosis: Constipation related to medication regimen, back surgery, and inactivity as evidenced by hypoactive bowel sounds, lack of bowel movements, decreased flatulence, and reported feelings of constipation.
Patient goals: Patient will have a bowel movement, patient will be started on a bowel regimen, patient will report increase of flatulence, patient will get out of bed for all meals and walk twice today.
Interventions: Discuss implementation of a bowel regimen and changes to pain medication schedule with medical team, get patient to chair for all 3 meals, patient will walk twice in hallway.
Evaluation: Medical team ordered 25 mg oral Dulcolax and decreased frequency of oxycodone to every 8 hours and to give 650 mg Tylenol between doses. Scheduled stool softeners were also ordered. Patient was up to the chair for breakfast and dinner and walked once with PT. Patient verbalized that he will be up for all meals and walk twice tomorrow. Patient reported increased of frequency of flatulence. Patient had large, dry, brown bowel movement after digital disimpaction.
Honestly, once you’ve got your job and are off orientation and really feel like you know what you’re doing, you’ll be creating and implementing care plans and critically thinking without even realizing it.
You’ll be helping your colleagues work through critical thinking with their patients. You’ll be critically thinking with physicians.
You’ll learn from experiences and continue to get better and faster at developing care plans critical thinking as you progress in your career.
| Welcome to the NRSNG.com Podcast. This is John Haws, RN, CCRN. Today we are talking critical thinking and care plans. Wait, before you turn off this podcast and run away because you hate those two words I want you to give this one a listen. I want you to sit back, I want you to listen to this one. |
| We’re talking with Katie Cleaver, RN, CCRN with NRSNG.com and Nurseeyeroll.com and we’re talking about what exactly is critical thinking? What are nursing care plans and how to make the two coalesce into one? How to make the two really work for you, and how to have them really make sense. You guys, we have an awesome post about this. It’s about 5,000 words. We have a ton of resources there. Videos, downloads, everything you need to get care plans and critical thinking really working because once you listen to this, you’re going to realize how the two really roll into one. That post is over at NRSNG.com/critical thinking. That’s NRSNG.com/criticalthinking. |
| I also want to tell you guys there’s actually a thunderstorm going on outside right now while me and Katie are talking on the phone so during the episode you might hear some thunder and a little bit of interruption with that. I apologize you guys for that. I hope it doesn’t get into the way too much, but I really appreciate you guys listening to the show. |
| Thank you so much for being a part of this NRSNG community. Head over to NRSNG.com/criticalthinking. You guys, this one’s going to blow you away. This whole post you really need to take a minute to head over there, read that entire post when you have some time, take some notes, print the downloads, and watch the videos. It’s really going to help you guys. Without further ado, let’s roll into the episode. |
| All right. Today we have a really good episode. I’m talking today with Katie Cleaver and we’re going to be talking about critical thinking. I know it’s almost a four-letter word in a nursing school and I remember as a nursing student how annoyed I would get every time an instructor said critical thinking because I feel like it was just left at that. It’s like, You’ve got to critically think as a nurse.” “Okay. I feel like I have a pretty decent brain in my head. Tell me what that means. Why am I not? What am I missing? What’s going on here?” |
| Today we’re going to talk with Katie. She’s put a lot of research in the last couple weeks into exactly what this means and deconstructing critical thinking and how it applies to nursing specifically so that we could give you guys something better than just saying, “You need to critically think,” or “Make sure you’re critically thinking,” or “It’s really important with nursing.” |
| What she’s done is she’s really broken it down and she’s going to lay it out for you guys on the NRSNG blog in a series of I think 8 blog posts, several videos, several podcasts just to make sure you guys understand what critically thinking really is. What she uncovered is something really interesting. We’re going to talk about that later is how critically thinking really applies to the other four-letter word in nursing school which is care plans. |
| Katie, tell us what is critical thinking and what did you discover when doing this? |
| First of all, I just have to say how much I love that they’re both four-letter words because I felt the same way in nursing school. That critical thinking is the word that they say when they don’t know what to say. The care plans I felt like it was, “This is a task that is just so not straightforward,” and they’re coming up with things that I don’t even know where they’re coming …. I don’t know. |
| Did you ever get your care plans back and be like, “What?” |
| WTF. What? Yes, I did because I would spend forever on it, and then turn it in, think it’s great, and then red marks everywhere. |
| Yeah. “I don’t even know what you’re saying.” |
| Yeah. You know what I realized especially in nursing school … Not really in nursing school. I didn’t realize this in nursing school, but care plans are not like if you think about some of your other stuff you study for in nursing school, it’s straightforward. I study this and it has this answer. |
| Even all your other courses, you memorize things and you learn concepts, but creating a care plan is like pulling from every little thing that you know to make this plan for the patient. When you haven’t seen a ton of patients, it is incredibly difficult to do that. It’s not one of those tasks that it takes you 20 minutes and you check it off or even like a paper. I know essays and research papers it takes time and you have to write stuff out, but even that is a lot more straightforward than a care plan. |
| You have to think critically about what makes the most sense for this patient. One of the things I learned was you do have the two things. You have the critical thinking, which is, “Hey, I notice a problem, and I’m going to think about my nursing knowledge of what the best way to address this problem and consider all things about the clinical picture and what I can do as a nurse before calling the physician and involving others. What can I do? Thinking critically, work through this issue to get the best case scenario for the patient or deal with this.” Then adding that piece with care plans. |
| There’s a bit of overlap definitely that I noticed that I didn’t realize until I was really researching both of them. When you think about care plans it’s like, “Okay. I have my patient that has this medical diagnosis. I’m not a physician and I couldn’t make the medical diagnosis, but what’s a really important aspect of their recovery and them getting out of the hospital and their discharge plan is me looking at their medical diagnosis. Their issues going on with them, and what are some big priorities for this patient that we have to progress through to get them out of the hospital?” |
| It takes critical thinking to really figure that stuff out and the best way to address those issues. I realized that care plans and critical thinking is really an aspect of being a successful nurse. Working as a nurse for a while, you work with those nurses that are just trying to get through their shift. They don’t care about getting the patient up to walk even though the doctor wants them to. They don’t care about weaning them off their iv pain meds or meeting goals. They’re just trying to get through the shift. |
| Technically they got all their meds passed out, they answered questions, but they didn’t progress the patient. You have to have a plan and ways to progress the patient to getting out of the hospital sooner. The way you do that is with a care plan. The way that you come up with a care plan is you think critically. |
| Absolutely. One thing that you and I have talked about, Katie, as we’ve been talking about this subject is that when you have more time working on the floor and working with the patients, you walk into a patient’s room and within two minutes you know everything that you’re going to do. It’s at that point too that we start to really laugh about how instructors made us do care plans, they’re so pointless, but I think that what we miss is that we’ve actually crossed that line of care plans just come naturally to us at that point. |
| What is this process? How does somebody get to that point of their critical thinking just flows into planning care and it just happens like that? |
| Well, it’s something that I think that you have to pay attention to these things. You have a patient that had a hip surgery and, okay, you’re learning in report about your patient or maybe you’re learning the night before because you’re going into clinical the next day. Well, what is going to be really important? Let’s stop and think instead of just go to our medications and go to this, and go to that, let’s stop and think. Just casually, “Hey, hold on. My patient, they broke their hip. You know what? It’s going to be really important that they do not fall because that can mess up their hip replacement or if they had a surgery or whatever. So I’ve got to try to figure out what I can do to keep this guy from falling.” |
| I think what people get tripped up on is the terminology. One thing I realize is it’s important to have this standardized terminology because I went to a nursing school in Iowa. I practiced in Illinois and in North Carolina. It’s all the same terminology, which is wonderful, but I think in nursing school you get so tripped up on giving it the right words and having it sound perfect, but I think what really can help nursing students understand this more is get your care plan template. A lot of nursing schools I think have their own, but write it out but don’t worry about the words. |
| “Okay, I don’t want him to fall, so no falls.” Try to just not worry about how fancy it sounds. It’s just, “Okay, I want to prevent this guy from falling. Okay. Breaking your hip hurts. He’s probably going to have some pain.” Just trying to think about it in a way that you’re not getting tripped up about the specific terminology because I think that’s the big hangup and if you can first get to the point where you can identify the issues without necessarily having to use that specific terminology then go back and say, “Okay, so he’s got a bunch of pain, so I think that would probably be a good thing to focus on. All right, so let me go back to my NANDA International book and … Okay, acute pain related to hip fracture as evidenced by self-report of pain, grimacing when walking …” those kind of things. I feel like if you work that way, it helps that come together because I think a lot of this stuff is just common sense, but we don’t realize common sense isn’t common. |
| You don’t realize you’re doing it. When we get out as nurses, we hate writing our care plans at the end of the shift, but we’ve been doing it the whole shift. Some people still struggle with getting the right words that they need to put in there, but it doesn’t mean they’re not doing it and that’s the challenge is trying. I think think that’s the best way to approach it in nursing school. Think about the patient, but don’t freak out about getting the right words right away. |
| Think about realistically what is going on and then think about your priority diagnoses or what are the three or four big issues going on with this patient? what does that have to do with it? They’ve got pain, but why do they have pain? ‘He’s a high fall risk, but why is he a high fall risk?” That’s your related-to factor. What are you seeing that is telling you this? Your as evidenced by. “All right. I know he’s in pain because the guy just told me he was. Patient reported pain.” |
| Those kinds of things if you can try and break it up like that I think it makes it flow a lot smoother, but it is important I think for students to know that it shouldn’t be easy. You haven’t seen a lot of patients. This should be challenging and something that you can’t check off right away because you really have to see a lot of patients, understand, “Hey, I’ve seen a bunch of guys that have had hip fractures. They’re really unsteady on their feet and they really have a lot of pain. They have maybe constipation, or they have anxiety, or whatever.” A realistic expectation of what their normal interventions would be. You’ve got to see a decent amount of those kind of patients before you can get this amazing plan together. |
| Sure. Your first recommendation is forget about NANDA, forget about NIC, forget about NOT and just go to common sense. Go to even though I don’t have a lot of experience with a hip fracture patient, what would this patient be going through? The pain, or the impaired skin integrity, or risk for impair. Those are the things that you just need to start thinking about first. |
| You say, “Okay, what would this patient naturally be going through?” Then from there you’re saying, “Can I work backwards? Okay, well how can I prevent that pain? How can I reduce that pain? How can I prevent skin integrity issues?” Then from you just start filling in those blanks. That’s what I would do. “What am I going to do during my shift to do that? What do I hope happens because of that?” Once you’ve done that, you can fill in the boxes on the care plan. |
| Absolutely. One thing I’ve noticed too just working as a nurse but then looking back at care planning stuff, there’s a few pretty standard common ones that’ll apply to those patients and I’m sure you’ll agree the high fall risk, the skin integrity, fluid imbalance, pain. Those are some big ones that I would argue most patients that are in the hospital are having an issue with some of those so I think it’d be good to familiarize yourself with those. |
| The ones that are the heavy hitters that it’s like, “Oh yeah, most patients in the hospital are fall risks because maybe they had an injury. Maybe they were confused, and if you get familiar with the interventions. I’m sure you could too name off all the fall risk ones. That was one thing I did not have to look up when I was writing these articles. “Non-skid socks, increase [inaudible 14:10], have a room by the nurse’s station, bed alarm on, call light within reach.” I remember that because all the neuro ICU patients are fall risks. I would really recommend getting familiarized with those very common ones. |
| Yeah, for sure. To try to help students, let’s talk about maybe what you, as an experienced nurse, would do. Let’s say you walk into a patient’s room who has heart failure. That’s all you know at this point. You walk into the patient’s room who has heart failure. Walk us through your critical thinking and then how that’s going to apply to the nursing care plan. |
| Katie hasn’t practiced this before. I’m throwing it at her right now. You walk into a heart failure room. Walk us through how this is going to go. Rather than just being that nursing student deer in the headlights, it’s a blank patient. Now you with several years experience, you’re walking in there with all this background information. What does the critical thinking and care plan process look like for you? |
| What I would normally do if I know this patient is a heart failure patient, it’s really important to know that diagnosis and then one of the things that nurses do is you think of your care plan after you have the pieces in front of you of the puzzle. You go in the room and you do an assessment. You look at your chart and this is after you’ve gotten a report, so you have all these little indicators. It’s like, “Hey, create a care plan for blank patient.” |
| It’s really important that, before you jump into that, do your assessment first. Talk tot he patient first. Those kinds of things are really important to make sure that you’re doing. That’s what I would do. “Okay, I got a report from John. Let’s see he’s a heart failure patient that …” What do I want to say about him report-wise? That is on a bumex drip and maybe he’s in the ICU or something like that, and has a history of afib. Those kinds of things. I’ll go in the room. I really think if someone has heart failure, they’re probably going to not have great fluid balance. |
| They have heart failure and what I know about the pathophysiologic about heart failure is there’s too much fluid. I’m going to look at my nursing diagnosis book and I’m going to look at my different diagnoses that have to do with fluid. I’m pretty sure there is one there that is fluid volume overload. I’m pretty sure there’s one. That would probably be my priority nursing diagnosis because the biggest deal, whether I do all the other stuff and the reason this guy’s in the hospital is heart failure, if we can work with whatever the physician has ordered to progress this guy with his heart failure to get him out of the hospital, that’s the biggest impact I’m going to make. |
| I would probably go with “Fluid volume overload related to heart failure as evidenced by,” and then I would go do my assessment. He probably has abnormal lung sounds. He’d probably have edema. His INOs wouldn’t be equal. He’d probably have 18:00] however many liters. That would be my big one. I would really focus on that and what kind of interventions can I do to make sure that I’m addressing those issues? Make sure I’m giving his meds appropriately. I’m maybe restricting his fluids and educating him appropriately. Those kinds of things. |
| Evaluating, “Did I do these things or not?” I’m sorry, implementation. “Did I do these things or not?” Then evaluation. “How did it go? Was it really ought to keep this guy restricted on fluids?” Maybe one of my interventions is going to be ambulating frequently to the bathroom to go empty his bladder as frequently as possible if he doesn’t have a Foley catheter or something like that. Those kinds of things. |
| That’s how I would. It’s really, “Okay, what is the diagnosis? What are some big issues that have to go with that diagnosis?” It’s not easy. You’re going to have to hold onto your pathophysiology knowledge. Your med surge course knowledge. Maybe pulling out those kinds of books and looking at that disease process and what kind of things go along with that. |
| Like you said in the beginning, I think what makes care plans so frustrating as a student is, you have a very minimal knowledge of heart failure and you’ve maybe only taken care of two patients. Never for a full 12 hour shift and so you don’t even see “What’s the bumex drip going to even do? What’s the end result of that? Why am I restricting? He says he’s really thirsty. Shouldn’t I give him some water?” You don’t see the full course of this stuff and so it’s okay to be frustrated by these care plans. |
| It’s okay to be really agitated by them because the knowledge that you have at this point is very limited and then your full scope of being able to see everything is very limited in Katie’s situation and why this transition you have to when critical thinking just starts happening naturally. That doesn’t happen because you learn how to think better. It happens because you have a better base knowledge and you start to understand more. |
| You see that heart failure patient from day one to the day they’re released and so you really start to see this whole picture. I think this critical thinking goes with these care plans so much because it’s getting that full picture together. I’m not just doing some things for some random patient. I’m doing specific things for a heart failure patient that has presented with all those symptoms. |
| Yeah. One think I compare this to is think about a medical student going through learning how to become a doctor and when they’re trying to figure out, “How am I going to maybe diagnose this patient?” At the beginning it’s really challenging because they haven’t seen a ton of heart failure patients. They haven’t seen a ton of patients with a stroke, or an MI, fractured femur or something. Although that one’s straightforward. It takes a while to look at all the diagnostics, look at the full clinical picture, and then get to this conclusion. |
| It’s really looking at this big picture and pulling apart the important things and it takes experience to figure out what those important things are. Of course it’s expected at the beginning that this is going to take time and that learning curve is there because you haven’t seen all these patients. I think it’s really important that students know because for me I didn’t know that. I didn’t know. |
| I thought that it was one of those things like, “You should get this right away. Why don’t you get this?” There was maybe one or two in the classroom that could pick stuff out a little bit easier, but other than that, we all were pretty much struggling with care plans, so I just want to reassure people that that’s the normal progression. It’s going to take some time to get good at this and it’s not a, “Here, do this assignment, and complete it, and then that’s it. Do you know what I mean? |
| Absolutely. I think that the post that you wrote on this and the subsequent posts are going to be huge helps and then also the care plan template that if they go to this post, read his post. Use that template, and really use the advice that you’re giving them here, it’s not going to happen overnight, but this is going to be a tremendous help. With the way that all this information’s been put together in this post and everything, it’s really going to give them the resource that’s need to make sure you’re on the right path. That you’re not like me and Katie years ago where you get a care plan back and it’s like, “I don’t even know why that’s wrong.” You’ll know where you’re going. |
| Yeah. What? |
| That was my biggest frustration was I would write my care plan, and then it would be really hard for me to come up with my care plan, and then I’d talk to my instructor and they’d be like, “Oh, this, this, this.” It’s like, “How did you come up with that?” I feel like that’s this random thing for you to pull out of it, but you realize that stuff after experience. Right now it doesn’t seem obvious, but eventually it will be. Those are encouragement that if you’re frustrated, that’s okay and that’s normal. |
| I guess one other thing I’d say too is that you’re not even going to notice it happening. You really won’t because we honestly had to go back and think about care plans in nursing school to be able to figure out how to put this information into a post and a podcast because it just happens. When you, Susan, and I all got together, we were like, “We should teach people about care plans,” and we all said, “We don’t even use care plans anymore,” and we’re like, “Wait, no, we do, we just don’t even realize it.” The thinking is all there. |
| Exactly. |
| It’s happening systematically, exactly like those boxes appear on a care plan, but it just happened |
| Right |
| You just transition to that. |
| The care plan, we do it so fluidly you don’t even think about it when you go back to the care plan because that was always that frustrating thing with work. I’m doing this work all day and I have to go back and have to turn in my care plan. It’s frustrating because it’s challenging still sometimes to put into words. The right words, the fancy words, the stuff that I just do automatically because I know how to take good care of this patient and what my goals should be because I’ve had experience at this point. I know what I need to do for my stroke patients, my seizure patients, my cabbage patients. I know what the normal post-op progression is because I’ve had experience with it. Now I have to go back and put in the work. That’s the frustrating thing, but it takes time. |
| Sure. I think one last thing I would leave with people too is in this post you talk about two different nurses on the same shift. One nurse that gives their meds on time, does what they’re supposed to do, makes sure the patient gets their meal, charts, leaves on time. Then the other nurse who listens to the patient, responds to the patient’s needs, realizes, “Okay, the patient’s sill on iv morphine, but they’re supposed to go home tomorrow. We need to start transitioning to norco and having that discussion with the patient, with the physician. It takes them a little longer to get things done and they leave a few minutes late. Which nurse really had the more successful shift? I don’t know if you want to talk about that for just a minute. |
| Yeah. When you think about that, who do you want taking care of your loved one? When, you’re learning how to be a nurse, you can technically have a shift where you got everything done, but did you really provide excellent care to that patient where they’re progressing, where they can go home sooner? I don’t think nursing students, and I know I didn’t, realize how big of an impact the proactive nurse has on patient stays. If you have proactive nurses, they significantly can reduce patient stays. How many times have you gotten a report where it’s like, “Why didn’t somebody address this three days ago?” |
| Even something as simple as, “Last bm was last Thursday.” That’s a small thing, but that’s, “Are they on [inaudible 26:24]?” “I don’t know.” Should we check on that? |
| Right. You’ll run into nurses and they’ll just do what they’re supposed to but they’re not looking at all of the orders. They’re not looking at the big picture. They’re not having a plan behind their shift. That’s the thing. That’s the difference. That’s why care plans are important because it truly is your plan of attack, your plan for the shift of how are you going to progress that patient. Like that heart failure patient, it gives you that priority. When they say priority nursing diagnosis, it’s not just, “Okay, this is the most important.” It’s like, “No, it really is [for that guy 27:01]. |
| That’s what really needs to happen today. |
| Let’s say that’s your grandpa. That’s your dad. He’s got a priority. That should be the priority to the nurse and while they might have gotten their Colace late, their fluids weren’t restricted like they were supposed to be. I think that’s the really important thing to see is that while they’re frustrating doing these care plans, if you take this seriously and understand that you have to have a plan behind the care that you provide in a 12 hour shift, that you can make this huge impact on this patient’s stay. |
| I think a lot of people go into it thinking, “Well, that’s the doctor’s job. They should tell me what to do,” and it’s like, “Well, sometimes the nurses aren’t even looking at the order.” I work in the ICU in a critical care setting and we get patients up on ventilators. It’s like, “Oh, well they put in to get them out of bed, but they’re on a ventilator so they can’t.” Yeah they can, but it’s up to the nurse to take that initiative. |
| The doctor’s there for five minutes a day and they give them these orders, but it’s up to the nurse to progress the patient and that’s what the basis of these care plans and how big a of a difference that you can make and bringing it back to, “Would you want that nurse taking care of your family?” |
| My father-in-law was in the hospital for a stroke four years ago and I could tell there were a couple of nurses that really had that care plan mindset because they were trying to progress him, and then there were those nurses. There was a nurse that was trying to give, he said he had a mild headache, trying to give him a milligram of dilaudid. Uh, no |
| No thanks. |
| You need to [inaudible 28:45] that order and get him some [inaudible 28:48] or some Tylenol. That kind of stuff. Having that mind to look at the big picture and what’s important because you have the power to do that because you are the nurse. |
| We’re trying to wrap up here, but you touched on a lot of things that I could go on for hours about. I’ll try to be as succinct as I can here. My take-away from what Katie’s saying and something I always try to say is, don’t be the nurse that just checks boxes. There’s so many boxes we have to check as a nurse and we have to check them every 15 minutes, but don’t be the nurse that’s doing their job just to check the box. |
| What happens, and you’ll see this a lot, is that a lot od hospitals will start to come out with new policies, new protocols, new this, new that because something happened. For those nurses that are critically thinking, that are really understanding what they’re doing, and really diving in, and learning, and trying to be the best nurse they can, you’ll find that … I don’t want to say this, those protocols are really for those nurses that just check boxes because they’re just trying to get through a shift and get out the door and so a new thing has to be added on because of they’re finding ways that these people are cutting corners. |
| Also I want to say that we get it, care plans are annoying. They suck, they’re hard, they’re tedious when you’re in nursing school, but I think what we’re trying to let you guys see is that learning how to incorporate these into the way that you are a nurse is going to help you be a better nurse. It’s going to help you think faster. It’s going to help you take better care of your patients, it’s going to just help you be a more well-rounded, a more holistic, a more caring nurse. |
| Lastly I want to say going along with not being a nurse that checks boxes and things like that, it can be very frustrating when you have given your all during your shift. You have a new add in the middle of the night who’s a trauma add. You get them intubated, you get everything done, but you forget to take the trash out before the day shift comes in and the nurse shows up and they neglect everything that you’ve done for this patient. “Well, the trash is still in there. You need to take the trash out.” |
| It’s like, “Are you kidding me? Forgive me for neglecting that there was a full garbage can when you can see that I have eight drips going, I have a new ventilator going, the doctor’s still in the room. We just finished CPR. Yeah, the garbage is there and it’s obviously not because I was trying to ruin your life.” Don’t just worry about those things like, “That’s the rule. You have to take the garbage out before you go home.” Don’t get so much into those things and really get that critical thinking tied into taking care of the patient and just don’t be the that nurse that’s just checking boxes. Be that nurse that actually cares. |
| I 8 million percent agree with hat. Absolutely. That’s the thing. When you realize what’s important and what’s important are care plans. What’s important are taking critical thinking and seeing those big pictures. Yeah there’s those little ticky-tack things which are really frustrating when you’ve done this great shift where you really notices all that important stuff and you forgot that stupid little thing and someone chews you out for it. |
| It’s like, “You know what? If that is what matters to this nurse, then there’s some real big learning deficits that are there,” but that’s why it’s important that you guys as nursing students learn this now and that this is the priority of us both speaking as critical care experienced nurses are saying, “Yes, these are important.” Absolutely, they’re tough but they’re worth getting used, to and getting your feet wet, and understanding. That’s where I’m at with that. |
| Agreed. When you guys get a minute, go to the post. It’s about 5,000 words long. There’s some downloads there. There’s some videos. Sorry, there’s a thunderstorm guys right now. It’s pretty big. Spend some time, dive into those resources, those videos, and really try to embrace this because we want everybody in our NRSNG family to be that nurse that gives a damn. That’s not just working for a paycheck because there is so many other jobs you could do that are a lot easier than a nurse. |
| You guys, I hope that was helpful. I hope that you can now see how much we really believe in critical thinking and care plans and how we understand care plans and critical thinking can be really annoying. I understand you hear it all the time, but listen, understanding how to do them, how to make them work, the process to them is going to make a huge difference not just in nursing school, but throughout your entire career as a nurse. Again, head over to NRSNG.com/criticalthinking. That’s NRSNG.com/criticalthinking. All right, guys. You know what time it is now. It’s time to go out and be your best self today. Happy nursing. |
How Hard is Nursing School . . . Really?
How much do nurses make | how i made over $70,000 my first year | nursing.com, similar blog posts.

Stress Overload Nursing Diagnosis and Care Plan | NURSING.com
5 Steps to Writing a (kick ass) Nursing Care Plan (plus 5 examples) | NURSING.com

How To Write the Perfect Nursing Care Plan with Examples
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
Critical Thinking in Nursing
- First Online: 02 January 2023
Cite this chapter

- Şefika Dilek Güven 3
Part of the book series: Integrated Science ((IS,volume 12))
1262 Accesses
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Thinking Critically About the Quality of Critical Thinking Definitions and Measures

Criticality in Osteopathic Medicine: Exploring the Relationship between Critical Thinking and Clinical Reasoning

A guide to critical thinking: implications for dental education
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Enhancing Critical Thinking in Clinical Practice
Implications for critical and acute care nurses.
Shoulders, Bridget MS, ACNP-BC, CCRN-CMC; Follett, Corrinne MS, FNP-BC, CCRN, RN-BC, RCIS; Eason, Joyce MS, ANP-BC, RN-BC
Bridget Shoulders, MS, ACNP-BC, CCRN-CMC , is a nurse practitioner in the cardiology department at the James A. Haley VA Hospital in Tampa, Florida.
Corrinne Follett, MS, FNP-BC, CCRN, RN-BC, RCIS, is a nurse practitioner in the cardiology department at the James A. Haley VA Hospital in Tampa, Florida.
Joyce Eason, MS, ANP-BC, RN-BC, is a nurse practitioner in the cardiology department at the James A. Haley VA Hospital in Tampa, Florida.
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
Address correspondence and reprint requests to: Bridget Shoulders, MS, ACNP-BC, 31047 Whitlock Dr, Wesley Chapel, FL 33543 ( [email protected] ).
The complexity of patients in the critical and acute care settings requires that nurses be skilled in early recognition and management of rapid changes in patient condition. The interpretation and response to these events can greatly impact patient outcomes. Nurses caring for these complex patients are expected to use astute critical thinking in their decision making. The purposes of this article were to explore the concept of critical thinking and provide practical strategies to enhance critical thinking in the critical and acute care environment.
The complexity of patients in the critical and acute care settings requires that nurses be skilled in early recognition and management of rapid changes in patient condition. The interpretation and response to these events can greatly impact patient outcomes. The purpose of this article is to explore the concept of critical thinking and provide practical strategies to enhance critical thinking in the critical and acute care environment.
The complexity of patients in the critical and acute care settings requires that nurses be skilled in early recognition and management of rapid changes in patients’ condition. Caring for patients with complex conditions, decreased length of stay, sophisticated technology, and increasing demands on time challenges new and experienced nurses alike to use astute critical thinking in clinical decision making. The decisions made directly affect patient care outcomes. 1 Bedside nurses, preceptors, and nurse leaders play a pivotal role in the development of critical thinking ability in the clinical setting. The purposes of this article were to explore the concept of critical thinking and to provide nurses with practical strategies to enhance critical thinking in clinical practice.
WHAT IS CRITICAL THINKING?
Critical thinking is a learned process 2 that occurs within and across all domains. There are numerous definitions of critical thinking in the literature, often described in terms of its components, features, and characteristics. Peter Facione, an expert in the field of critical thinking, led a group of experts from various disciplines to establish a consensus definition of critical thinking. The Delphi Report, 3 published in 1990, characterized the ideal critical thinker as “habitually inquisitive, well-informed, trustful of reason…, diligent in seeking relevant information, and persistent in seeking results.” Although this definition was the most comprehensive attempt to define critical thinking 4 at the time, it was not nursing specific.
Scheffer and Rubenfeld 4 used the Delphi technique to define critical thinking in nursing. An international panel of expert nurses in practice, education, and research provided input into what habits of the mind and cognitive skills were at the core of critical thinking. After discussion and analysis, the panel provided the following consensus statement: “Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting and transforming knowledge.” This definition expanded on the consensus definition in the Delphi Report to include the additional components of creativity and intuition.
Skilled critically thinking nurses respond quickly to changes in patients’ conditions, changing priorities of care based on the urgency of the situation. They accurately interpret data, such as subtle changes in vital signs or laboratory values. 5 They are not just looking at the numbers but also assessing the accuracy and relevancy of the findings. Critical thinking helps the nurse to recognize events as part of the bigger picture and center in on the problem.
Lack of critical thinking is evident when nurses depend heavily on structured approaches, such as protocols, to make clinical decisions. These guidelines should not be viewed as mandates because the practice is always more complex than what can be captured by pathways and protocols. 6 Without critical thinking, nurses are merely performing task-oriented care.
One example of how nurses use critical thinking is with medication administration. This task may appear to be primarily a technical process, but it requires astute critical thinking. Eisenhauer and Hurley 7 interviewed 40 nurses to illustrate their thinking processes during medication administration. The nurses described communicating with providers, sharing their interpretation of patient data to ensure safe administration of medication. They used their judgment about the timing of as-needed medication (eg, timing pain medication before physical therapy). Nurses integrated their knowledge of the patient’s laboratory values or pattern of response to medication to determine the need for a change in the drug dose or time. They assessed whether a medication was achieving the desired effect and took precautionary measures in anticipating potential side effects. It is evident in these examples that safe administration of medication involves critical thinking beyond the 5 rights that nurses are taught in the academic setting .
INTEGRATING RESEARCH, EVIDENCE-BASED PRACTICE, AND CRITICAL THINKING
Nursing research is a scientific process that validates and refines existing knowledge and generates new knowledge that influences nursing practice. 8 Evidence-based practice integrates the best available research with clinical expertise and patient’s needs and values. Different types of evidence have different strengths and weaknesses in terms of credibility. The typical evidence hierarchy places meta-analysis of randomized clinical trials at the top and expert opinion at the bottom of what counts as good evidence. 6
It is important to recognize that nursing knowledge is not always evidence based. Nurses have historically acquired knowledge through a variety of nonscientific sources such as trial and error, role modeling, tradition, intuition, and personal experiences. 8 Although these sources have been “handed down” over the years and continue to influence nursing practice, nurses are expected to use the best available evidence to guide their decision making. Evidence-based practice redirects nursing from making decisions based on tradition to practicing based on the best research evidence.
Barriers for nurses to implement evidence-based practices include lack of knowledge of research, difficulty interpreting findings and applying to practice, lack of time, and lack of autonomy to implement changes. 9 Universities can overcome these barriers by incorporating nursing research throughout all clinical and nonclinical courses. Joint endeavors between hospitals and universities to educate nurses in the use of research will increase the level of comfort with evidence-based practice. 10 Specialized research departments devoted to promotion and education of staff nurses in research evaluation, utilization, and implementation would allow nursing staff to experience an increased level of support and awareness of the need for research utilization.
Nurse leaders need to create an environment that supports transformation from outdated practices and traditions. Nurses must feel empowered to question nursing practice and have available resources to support the search for evidence. Critical thinking and evidence-based practice must be connected and integrated for nurses, starting in their basic education programs and fostered throughout their lifetime. 11
THE NURSING PROCESS AND CRITICAL THINKING
The nursing process is the nurse’s initial introduction to a thinking process used to collect, analyze, and solve patient care problems. The steps of the nursing process are similar to the scientific method. In both processes, information is gathered, observations are made, problems are identified, plans are developed, actions are taken, and processes are reviewed for effectiveness. 8 The nursing process, used as a framework for making clinical judgments, helps guide nurses to think about what they do in their practice.
Chabeli 12 described how critical thinking can be facilitated using the framework of the nursing process. During the assessment phase, the nurse systematically gathers information to identify the chief complaint and other health problems. The nurse uses critical thinking to examine and interpret the data, separating the relevant from the irrelevant and clarifying the meaning when necessary. During the diagnosis phase, nurses use the diagnostic reasoning process to draw conclusions and decide whether nursing intervention is indicated. The planning and implementation of interventions should be mutual, research based, and realistic and have measurable expected outcomes. The evaluation phase addresses the effectiveness of the plan of care and is ongoing as the patient progresses toward goal achievement. The author concludes that when the nursing process is used effectively for the intended purpose, it is a powerful scientific vehicle for facilitating critical thinking.
HOW DO WE LEARN CRITICAL THINKING IN NURSING?
Nurses initially learn to think critically in the academic environment, using assessments designed to measure critical thinking. It is conceivable that a nurse could pass an examination in the classroom but have difficulty making the transition to think critically in the clinical setting. Improving critical thinking ability should be viewed as a process and, as with the development of any skill, requires practice. 13
Most nurses develop their critical thinking ability as they gain clinical expertise. Patricia Benner 14 described the development of clinical expertise, as nurses transition from novice to expert. The beginning, or novice nurse, has theoretical knowledge as a foundation and minimal practical experiences to draw from. As similar situations are encountered, experience is accrued over time as the nurse evolves toward competency. As proficiency is developed, the nurse is able to perceive situations as a whole and recognize the significant aspects. As the proficient nurse reaches toward expertise, decision making becomes automatic, drawing from the enormous background of experience acquired over the years. Experience is more than the passage of time and is required at each stage before progressing to the next level of clinical expertise. As nurses progress along the novice-to-expert continuum and gain competence, they develop their ability to think critically. 15
Preceptors play a significant role in transitioning nurses into professional practice. It is essential that preceptors have the necessary skills to facilitate the critical thinking development of new nurses. Forneris and Peden-McAlpine 16 investigated the impact of the preceptor’s coaching component of a reflective learning intervention on novice nurses’ critical thinking skills. The following coaching strategies were used to educate preceptors: context (eg, understanding the big picture), dialogue, reflection, and time (eg, the use of past experiences to discern change over time). After completing the educational intervention, the preceptors used these strategies to coach the novice nurses in the development of their critical thinking skills. This study found that these strategies stimulated the novice nurses to engage in an intentional, reflective dialogue. The preceptors acknowledged a change in their preceptor style, moving from describing critical thinking as prioritizing and organizing task to a dialogue to share thinking and understand rationale.
Nurses must have the necessary dispositions (eg, attributes, attitudes, habits of the mind) to be effective critical thinkers. 11 Finn 17 defined thinking dispositions that influence critical thinking. Open mindedness was described as the willingness to seek out and consider new evidence or possibilities. Fair mindedness referred to an unprejudiced examination of evidence that might question beliefs or a viewpoint contrary to the nurse’s own beliefs. Reflectiveness was described as the willingness to gather relevant evidence to carefully evaluate an issue, rather than making hasty judgments. Counterfactual thinking referred to the willingness to ponder what could or would happen if the facts were considered under different conditions or perspectives. The opposite thinking styles directed toward maintaining the status quo included being close minded, biased, and rigid.
Rung-Chaung et al 18 investigated the critical thinking competence and disposition of nurses at different rankings on the clinical ladder. Using Benner’s novice to expert model as their theoretical framework, a stratified random sampling of 2300 nurses working at a medical center were classified according to their position on the clinical ladder. Ten to fifteen percent of this population were randomly selected for each ladder group, with the final sample size totaling 269. Data were collected using a modified version of the Watson-Glaser Critical Thinking Appraisal tool, designed to assess critical thinking competence in the categories of inference, recognition of assumptions, deduction, interpretation, and evaluation. The participants’ cumulative average score for critical thinking competence was 61.8 of a possible score of 100, ranking highest in interpretation and lowest in inference. Participants completed a modified version of the California Critical Thinking Disposition Inventory, designed to measure the following characteristics of critical thinking: inquisitiveness, systematic analytical approach, open mindedness, and reflective thinking. Participants scored highest in reflective thinking and lowest in inquisitiveness.
Analysis of the data indicated that older nurses with more years of experience and a more prominent position on the clinical ladder were predictive of a higher critical thinking disposition. Overall, critical thinking was shown to be only partially developed. The authors recommended training programs, such as problem-based learning, group discussion, role-playing, and concept mapping be adopted to enhance nurse critical thinking skills.
Chang el al 19 examined the relationship between critical thinking and nursing competence, using the Watson-Glaser Critical Thinking Appraisal and the Nursing Competence Scale. A total of 570 clinical nurses participated in the study. These nurses scored highest in interpretation ability and lowest in inference ability. These findings were consistent with the results reported in the Rung-Chuang study. Analysis of the data indicated that critical thinking ability was significantly higher in older nurses and nurses with more than 5 years of experience. The findings of this study indicated that critical thinking ability, working years, position/title, and education level were the 4 significant predictors of nursing competence. There were significantly positive correlations between critical thinking ability and nursing competence, indicating that the higher the critical thinking ability, the better the nursing competence is.
STRATEGIES TO ENHANCE CRITICAL THINKING ABILITY
To improve critical thinking, the learning needs of nurses must first be identified. The Performance Based Development System, a scenario-based tool, was used in a study to identify critical thinking learning needs of 2144 new and experienced nurses. 20 Results were reported as either meeting (identifying the appropriate actions) or not meeting the expectations. Most participants (74.9%) met the expectations by identifying the appropriate actions. Of the approximately 25% who did not meet the expectations, the learning needs identified included initiating appropriate nursing interventions (97.2%), differentiating urgency (67%), reporting essential clinical data (65.4%), anticipating relevant medical orders (62.8%), understanding decision rationale (62.6%), and problem recognition (57.1%). As expected, nurses with the most experience had the highest rate of identifying the appropriate actions on the Performance-Based Development System assessment. These findings were consisted with Benner’s novice to expert framework. These types of assessment tools can be used to identify learning needs and help facilitate individualized orientation. The authors acknowledged that further research is needed to identify areas of critical thinking deficiency and to test objective, educational strategies that enhance critical thinking in the nursing population.
The Institute of Medicine report on the future of nursing 21 emphasized the importance of nursing residency programs to provide hands-on experience for new graduates transitioning into practice. According to the report, these programs have been shown to help new nurses develop critical competencies in clinical decision making (eg, critical thinking) and autonomy in providing patient care. Implementing successful methods to expedite the development of critical thinking in new nurses has the potential to improve patient safety, nurse job satisfaction, and recruitment and retention of competent nurse professionals. 22
Although critical thinking skills are developed through clinical practice, there are many experienced nurses who possess less than optimal critical thinking skills. 5 As part of an initiative to elevate the critical thinking of nurses on the frontline, Berkow et al 23 reported the development of the Critical Thinking Diagnostic, a tool designed to assess critical thinking of experienced nurses. The tool includes 25 competencies, identified by nursing leaders as core skills at the heart of critical thinking. These competencies were grouped into 5 components of critical thinking: problem recognition, clinical decision making, prioritization, clinical implementation, and reflection. The potential application of this tool may enable nurse leaders to identify critical thinking strengths and individualize learning activities based on the specific needs of nurses on the frontline.
The critical thinking concepts, identified in the Delphi study of nurse experts, were used to teach critical thinking in a continuing education course. 24 The objective of the course was to help nurses develop the cognitive skills and habits of the mind considered important for practice. The course focused on the who, what, where, when, why, and how of critical thinking, using the case study approach. The authors concluded that critical thinking courses should include specific strategies for application of knowledge and opportunities to use cognitive strategies with clinical simulations.
Journal clubs encourage evidence-based practice and critical thinking by introducing nurses to new developments and broader perspectives of health care. 11 Lehna et al 25 described the virtual journal club (VJC) as an alternative to the traditional journal club meetings. The VJC uses an online blog format to post research-based articles and critiques, for generation of discussion by nurses. Recommendations for practice change derived from the analysis are forwarded to the appropriate decision-making body for consideration. The VJC not only exposes the nursing staff to scientific evidence to support changing their practice but also may lead to institutional policy changes that are based on the best evidence. The VJC overcomes the limitations of the traditional journal clubs by being available to all nurses at all times.
The integration of simulation technology in nursing exposes nursing students and nurses to complex patient care scenarios in a safe environment. Kirkman 26 reported a study to investigate nursing students’ ability to transfer knowledge and skill learned during high-fidelity simulations to the clinical setting, over time. The sample of 42 undergraduate students were rated on their ability to perform a respiratory assessment, using observation and a performance evaluation tool. The findings indicated there was a significant difference in transfer of learning demonstrated by participants over time. These results provide evidence that students were able to transfer knowledge and skills from high-fidelity simulations to the traditional clinical setting.
Jacobson et al 27 reported using simulated clinical scenarios to increase nurses’ perceived confidence and skill in handling emergency situations. During a 7-month period, the scenarios were conducted a total of 97 times with staff nurses. Each scenario presented a patient’s evolving story to challenge nurses to assess and synthesize the clinical information. The scenarios included a critical point at which the nurses needed to recognize and respond to significant deterioration in the patient’s condition. Postproject survey data found that most of the nurses perceived an improvement in their confidence and skill in managing emergency situations. More than half of the nurses reported that their critical thinking skills improved because of participation in this project.
Individual nurses can enhance critical thinking by developing a questioning attitude and habits of inquiry, where there is an appreciation and openness to other ways of doing things. Nurses should routinely reflect on the care provided and the outcomes of their interventions. Using reflection encourages nurses to think critically about what they do in everyday practice and learn from their experiences. 28 This strategy is beneficial for nurses to validate knowledge and examine nursing practice. 5 Nurses must be comfortable with asking and being asked “why” and “why not.” Seeking new knowledge and updating or refining current knowledge encourage critical thinking by practicing based on the evidence. “We’ve always done it that way” is no longer an acceptable answer. A list of other useful strategies for enhancing critical thinking is included in Table 1 .

USING THE INTERACTIVE CASE STUDY APPROACH TO ENHANCE CRITICAL THINKING
Case studies provide a means to attain experience in high-risk and complex situations in a safe environment. The purpose of a case study is to apply acquired knowledge to a specific patient situation, using actual or hypothetical scenarios. Waxman and Telles 32 discussed using Benner’s model to develop simple to complex scenarios that match the learning level of the nurse. The case study should ideally provide all the relevant information for analysis, without directing the nurse’s thinking in a particular direction. Participants are encouraged to use thinking processes similar to that used in a real situation.
A well-developed case study defines objectives and expected outcomes. The questions should be geared toward the outcomes to be met. 30 The focus of the questions should be on the underlying thought processes used to arrive at the answer, rather than the answer alone. This helps nurses identify the reasons behind why a decision is made. In some cases, the case study may build on the information shared, instead of presenting all the information at one time. At the very least, case studies should have face validity or represent what they were developed to represent. 33
Case studies can be developed for specific purposes, such as analyzing data or improving the nurse’s skill in responding to specific clinical situations. 30 This strategy can be useful in building nurses’ confidence in managing complex or emergency situations. The case can be tailored to specific patient populations or clinical events. Covering the course of care that a patient receives over time is effective in putting together the whole picture. 31 For the purpose of improving patient outcomes, the case study should represent the overall patient experience. Case studies may be used to review specific actions that led to positive outcomes or the processes that led to negative outcomes. This can help determine if the care was the most appropriate for the situation. 34
The use of case studies with simulation technology provides nurses with the opportunity to critically think through a critical situation in a controlled setting. The latest human patient simulators (HPSs) are programmed to respond to the nurse’s intervention, with outcomes determined as a result of the intervention. Howard et al 35 compared the teaching strategies of HPSs and the traditional interactive case study (ICS) approach, using scenarios with the same subject matter. A sample of 49 senior nursing students were given pretest and posttest designed to measure the students’ knowledge of the content presented and their ability to apply that content to clinical problems. Participants in the HPS group scored significantly higher on the posttest than the ICS group did. Students reported that the HPS assisted them in understanding concepts, was a valuable learning experience, and helped to stimulate their critical thinking. There was no significant difference between the HPS and ICS groups’ responses to the statement that the educational intervention was realistic.
The Figure depicts an example of a heart failure case study with the objective of applying critical thinking to a common problem encountered in practice. Expert clinical nurses would be ideal to serve as facilitators of this learning experience. Their role would be to present the scenario, describe the physiological findings, ask open-ended questions that require thinking and analysis, and guide the discussion and problem-solving process. Discussion and questioning strategies that are helpful in eliciting reflective responses during the learning experience are included in Table 2 . This case study could be tailored to meet the learning needs of the target audience.

THE INFLUENCE OF THE WORKPLACE ENVIRONMENT
The workplace environment can enhance or hinder nurses’ motivation to develop their critical thinking abilities. Cornell and Riordan 36 reported an observational study that assessed workflow barriers to critical thinking in the workplace. A total of 2061 tasks were recorded on an acute care unit during 35.7 hours of observation. The activities found to consume nearly 70% of the nurses’ time included verbal communication, walking, administering medications, treatments, and documentation. Nurse workflow was characterized by frequent task switching, interruptions, and unpredictability. The authors recommended reallocating duties, delegating appropriate task to nonnursing personnel, reducing waste, deploying technology that reduces repetitive task, and continuing education and training to help nurses cope with the complex demands of nursing.
Factors in the work environment conducive to the development of critical thinking include an atmosphere of team support, staffing patterns that allow continuity of care, and exposure to a variety of patient care situations. Creating an environment where contributions are valued, nurses feel respected, and there is comfort with asking probing questions is very important in enhancing the development of critical thinking skills.
Critical thinking is an essential skill that impacts the entire spectrum of nursing practice. Studies have shown that the higher the critical thinking ability, the better the nursing competence is. It is essential that critical thinking of new and experienced nurses be assessed and learning activities developed based on the specific needs of the nurses. The concept of critical thinking should be included in orientation, ongoing education, and preceptor preparation curriculums. These educational offerings should be designed to help nurses develop the cognitive skills and habits of the mind considered important for practice.
Bedside nurses can integrate a critical thinking approach by developing clinical expertise, making a commitment to lifelong learning, and practicing based on the evidence. Nurses should routinely reflect on the care provided and the outcomes of their interventions.
Further research is needed to identify areas of critical thinking deficiency and evaluate strategies aimed at enhancing critical thinking. These strategies will ultimately lead to improved clinical decision making and patient outcomes. Bedside nurses, preceptors, and nurse leaders are encouraged to work together collaboratively to create a culture where critical thinking is an integral part of nursing practice.
Acute care; Critical thinking; Decision making
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Assessment of clinical reasoning while attending critical care postsimulation..., nurse preceptor role in new graduate nurses' transition to practice, certified and advanced degree critical care nurses improve patient outcomes.
Nursing Care Plans (NCP) Ultimate Guide and List
Writing the best nursing care plan requires a step-by-step approach to complete the parts needed for a care plan correctly. This tutorial will walk you through developing a care plan. This guide has the ultimate database and list of nursing care plans (NCP) and nursing diagnosis samples for our student nurses and professional nurses to use—all for free! Care plan components, examples, objectives, and purposes are included with a detailed guide on writing an excellent nursing care plan or a template for your unit.
Table of Contents
Standardized care plans, individualized care plans, purposes of a nursing care plan, three-column format, four-column format, student care plans, step 1: data collection or assessment, step 2: data analysis and organization, step 3: formulating your nursing diagnoses, step 4: setting priorities, short-term and long-term goals, components of goals and desired outcomes, types of nursing interventions, step 7: providing rationale, step 8: evaluation, step 9: putting it on paper, basic nursing and general care plans, surgery and perioperative care plans, cardiac care plans, endocrine and metabolic care plans, gastrointestinal, hematologic and lymphatic, infectious diseases, integumentary, maternal and newborn care plans, mental health and psychiatric, musculoskeletal, neurological, pediatric nursing care plans, reproductive, respiratory, recommended resources, references and sources, what is a nursing care plan.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes a client’s potential needs or risks. Care plans provide a way of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
Nursing care planning begins when the client is admitted to the agency and is continuously updated throughout in response to the client’s changes in condition and evaluation of goal achievement. Planning and delivering individualized or patient-centered care is the basis for excellence in nursing practice .
Types of Nursing Care Plans
Care plans can be informal or formal: An informal nursing care plan is a strategy of action that exists in the nurse ‘s mind. A formal nursing care plan is a written or computerized guide that organizes the client’s care information.
Formal care plans are further subdivided into standardized care plans and individualized care plans: Standardized care plans specify the nursing care for groups of clients with everyday needs. Individualized care plans are tailored to meet a specific client’s unique needs or needs that are not addressed by the standardized care plan.
Standardized care plans are pre-developed guides by the nursing staff and health care agencies to ensure that patients with a particular condition receive consistent care. These care plans are used to ensure that minimally acceptable criteria are met and to promote the efficient use of the nurse’s time by removing the need to develop common activities that are done repeatedly for many of the clients on a nursing unit.
Standardized care plans are not tailored to a patient’s specific needs and goals and can provide a starting point for developing an individualized care plan .
Care plans listed in this guide are standard care plans which can serve as a framework or direction to develop an individualized care plan.
An individualized care plan care plan involves tailoring a standardized care plan to meet the specific needs and goals of the individual client and use approaches shown to be effective for a particular client. This approach allows more personalized and holistic care better suited to the client’s unique needs, strengths, and goals.
Additionally, individualized care plans can improve patient satisfaction . When patients feel that their care is tailored to their specific needs, they are more likely to feel heard and valued, leading to increased satisfaction with their care. This is particularly important in today’s healthcare environment , where patient satisfaction is increasingly used as a quality measure.
Tips on how to individualize a nursing care plan:
- Perform a comprehensive assessment of the patient’s health, history, health status, and desired goals.
- Involve the patient in the care planning process by asking them about their health goals and preferences. By involving the client, nurses can ensure that the care plan is aligned with the patient’s goals and preferences which can improve patient engagement and compliance with the care plan.
- Perform an ongoing assessment and evaluation as the patient’s health and goals can change. Adjust the care plan accordingly.
The following are the goals and objectives of writing a nursing care plan:
- Promote evidence-based nursing care and render pleasant and familiar conditions in hospitals or health centers.
- Support holistic care , which involves the whole person, including physical, psychological, social, and spiritual, with the management and prevention of the disease.
- Establish programs such as care pathways and care bundles. Care pathways involve a team effort to reach a consensus regarding standards of care and expected outcomes. In contrast, care bundles are related to best practices concerning care for a specific disease.
- Identify and distinguish goals and expected outcomes.
- Review communication and documentation of the care plan.
- Measure nursing care.
The following are the purposes and importance of writing a nursing care plan:
- Defines nurse’s role. Care plans help identify nurses’ unique and independent role in attending to clients’ overall health and well-being without relying entirely on a physician’s orders or interventions.
- Provides direction for individualized care of the client. It serves as a roadmap for the care that will be provided to the patient and allows the nurse to think critically in developing interventions directly tailored to the individual.
- Continuity of care. Nurses from different shifts or departments can use the data to render the same quality and type of interventions to care for clients, therefore allowing clients to receive the most benefit from treatment.
- Coordinate care. Ensures that all members of the healthcare team are aware of the patient’s care needs and the actions that need to be taken to meet those needs preventing gaps in care.
- Documentation . It should accurately outline which observations to make, what nursing actions to carry out, and what instructions the client or family members require. If nursing care is not documented correctly in the care plan, there is no evidence the care was provided.
- Serves as a guide for assigning a specific staff to a specific client. There are instances when a client’s care needs to be assigned to staff with particular and precise skills.
- Monitor progress. To help track the patient’s progress and make necessary adjustments to the care plan as the patient’s health status and goals change.
- Serves as a guide for reimbursement. The insurance companies use the medical record to determine what they will pay concerning the hospital care received by the client.
- Defines client’s goals. It benefits nurses and clients by involving them in their treatment and care.
A nursing care plan (NCP) usually includes nursing diagnoses , client problems, expected outcomes, nursing interventions , and rationales . These components are elaborated on below:
- Client health assessment , medical results, and diagnostic reports are the first steps to developing a care plan. In particular, client assessment relates to the following areas and abilities: physical, emotional, sexual, psychosocial, cultural, spiritual/transpersonal, cognitive, functional, age-related, economic, and environmental. Information in this area can be subjective and objective.
- Nursing diagnosis . A nursing diagnosis is a statement that describes the patient’s health issue or concern. It is based on the information gathered about the patient’s health status during the assessment.
- Expected client outcomes. These are specific goals that will be achieved through nursing interventions . These may be long and short-term.
- Nursing interventions . These are specific actions that will be taken to address the nursing diagnosis and achieve expected outcomes . They should be based on best practices and evidence-based guidelines.
- Rationales. These are evidence-based explanations for the nursing interventions specified.
- Evaluation . These includes plans for monitoring and evaluating a patient’s progress and making necessary adjustments to the care plan as the patient’s health status and goals change.
Care Plan Formats
Nursing care plan formats are usually categorized or organized into four columns: (1) nursing diagnoses, (2) desired outcomes and goals, (3) nursing interventions, and (4) evaluation. Some agencies use a three-column plan where goals and evaluation are in the same column. Other agencies have a five-column plan that includes a column for assessment cues.
The three-column plan has a column for nursing diagnosis, outcomes and evaluation, and interventions.
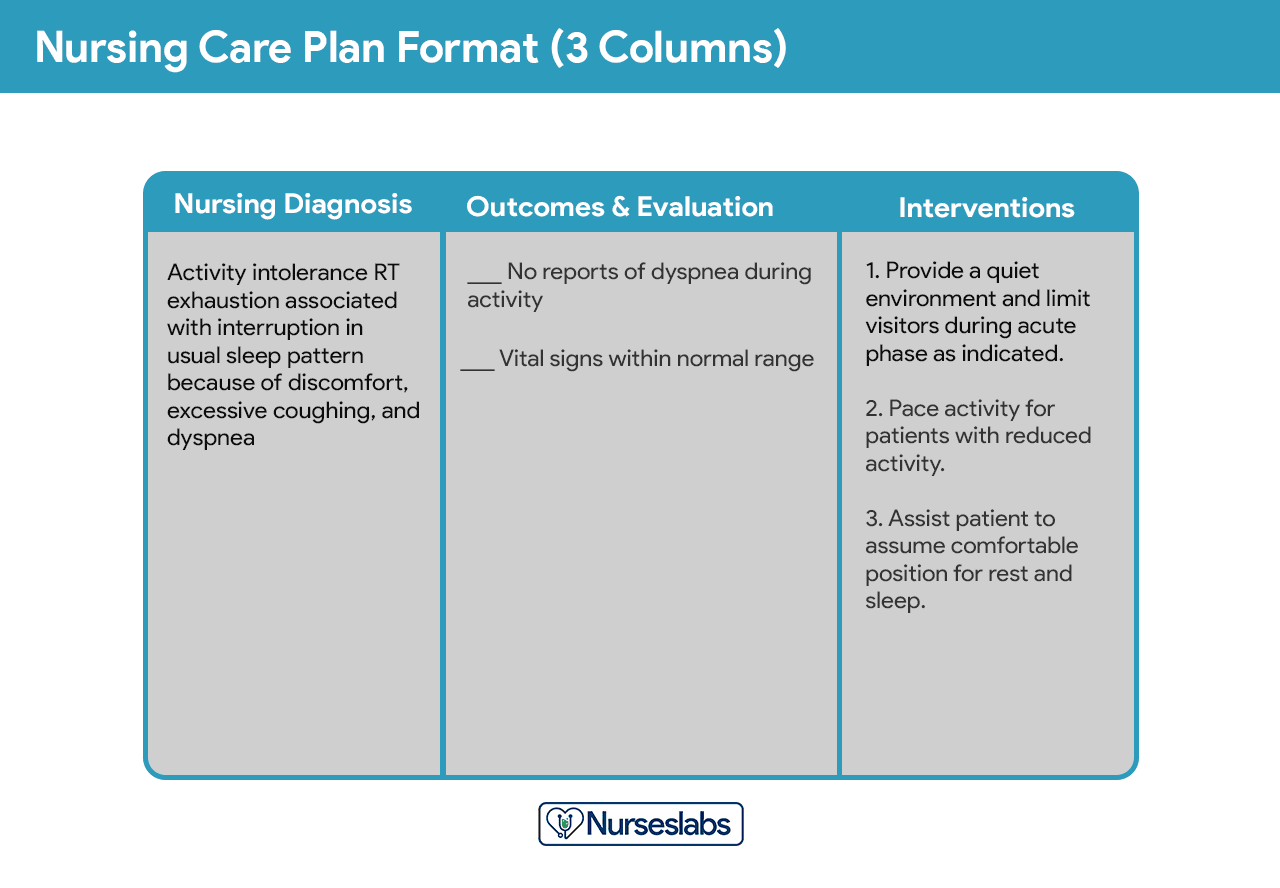
This format includes columns for nursing diagnosis, goals and outcomes, interventions, and evaluation.
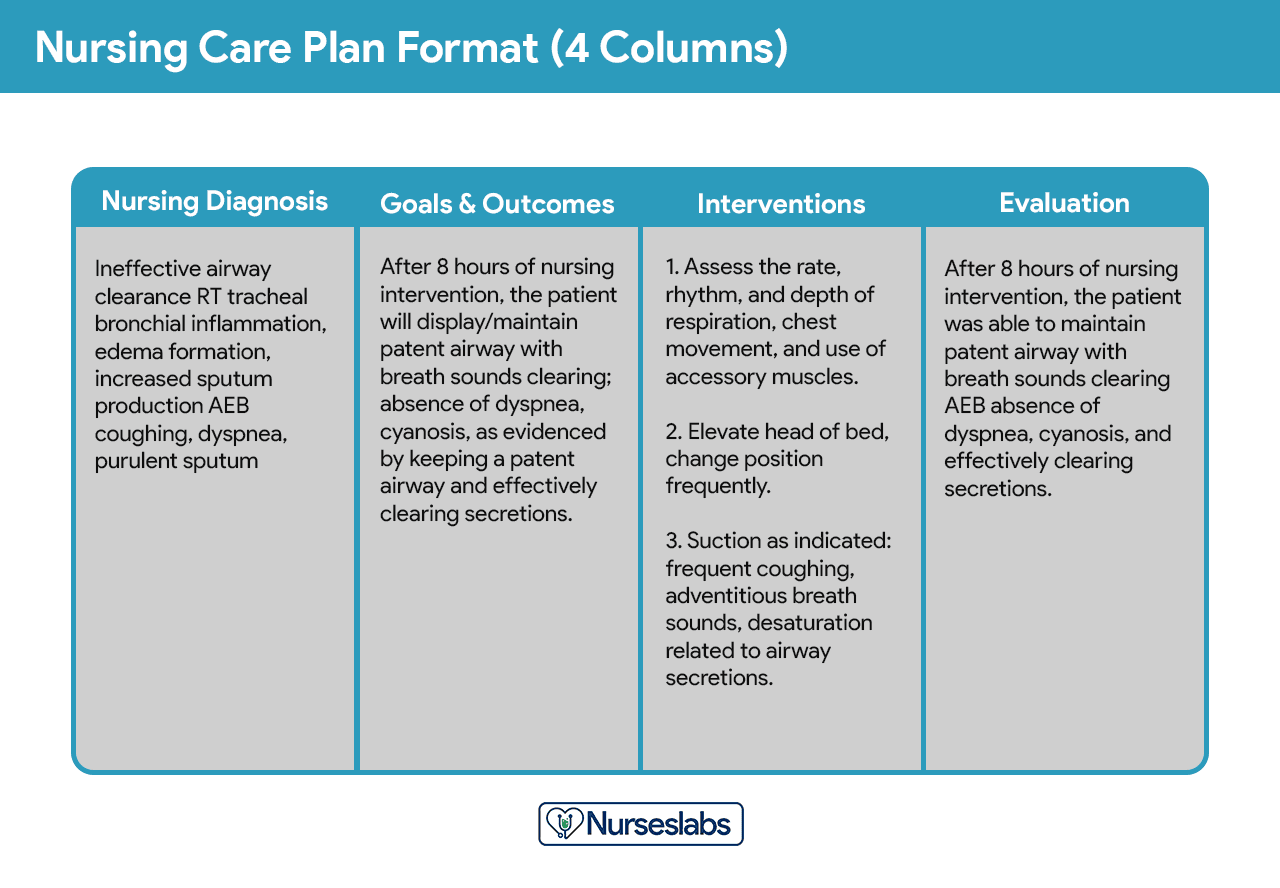
Below is a document containing sample templates for the different nursing care plan formats. Please feel free to edit, modify, and share the template.
Download: Printable Nursing Care Plan Templates and Formats
Student care plans are more lengthy and detailed than care plans used by working nurses because they serve as a learning activity for the student nurse.
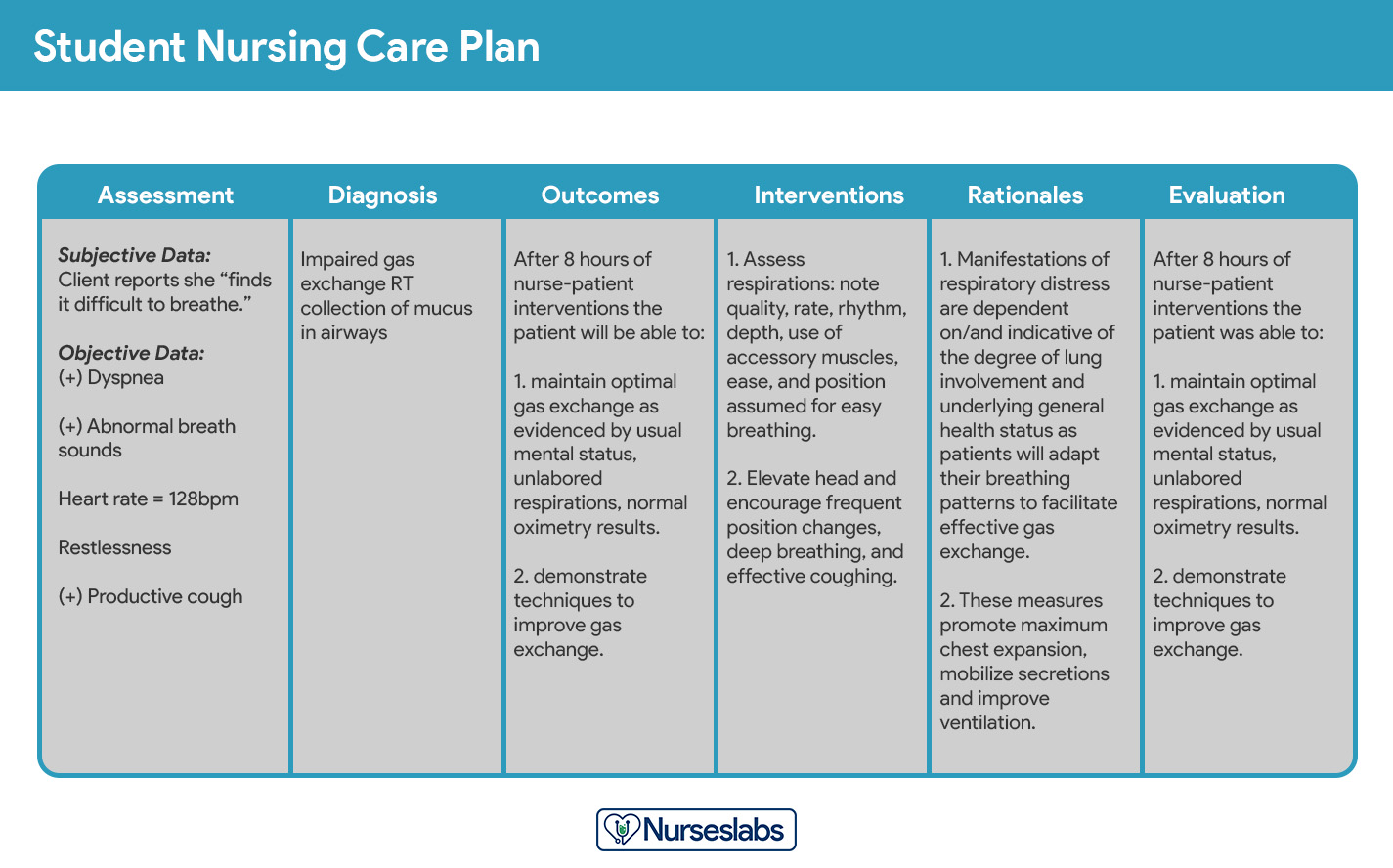
Care plans by student nurses are usually required to be handwritten and have an additional column for “Rationale” or “Scientific Explanation” after the nursing interventions column. Rationales are scientific principles that explain the reasons for selecting a particular nursing intervention.
Writing a Nursing Care Plan
How do you write a nursing care plan (NCP)? Just follow the steps below to develop a care plan for your client.
The first step in writing a nursing care plan is to create a client database using assessment techniques and data collection methods ( physical assessment , health history , interview, medical records review, and diagnostic studies). A client database includes all the health information gathered . In this step, the nurse can identify the related or risk factors and defining characteristics that can be used to formulate a nursing diagnosis. Some agencies or nursing schools have specific assessment formats you can use.
Critical thinking is key in patient assessment, integrating knowledge across sciences and professional guidelines to inform evaluations. This process, crucial for complex clinical decision-making , aims to identify patients’ healthcare needs effectively, leveraging a supportive environment and reliable information
Now that you have information about the client’s health, analyze, cluster, and organize the data to formulate your nursing diagnosis, priorities, and desired outcomes.
Nursing diagnoses are a uniform way of identifying, focusing on and dealing with specific client needs and responses to actual and high-risk problems. Actual or potential health problems that can be prevented or resolved by independent nursing intervention are termed nursing diagnoses.
We’ve detailed the steps on how to formulate your nursing diagnoses in this guide: Nursing Diagnosis (NDx): Complete Guide and List .
Setting priorities involves establishing a preferential sequence for addressing nursing diagnoses and interventions. In this step, the nurse and the client begin planning which of the identified problems requires attention first. Diagnoses can be ranked and grouped as having a high, medium, or low priority. Life-threatening problems should be given high priority.
A nursing diagnosis encompasses Maslow’s Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved, such as self-esteem and self-actualization. Physiological and safety needs are the basis for implementing nursing care and interventions. Thus, they are at the base of Maslow’s pyramid, laying the foundation for physical and emotional health.
Maslow’s Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure ) (ABCs), sleep , sex, shelter, and exercise.
- Safety and Security: Injury prevention ( side rails , call lights, hand hygiene , isolation , suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety ( therapeutic relationship ), patient education (modifiable risk factors for stroke , heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation ( bullying ), employ active listening techniques, therapeutic communication , and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one’s physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one’s maximum potential.
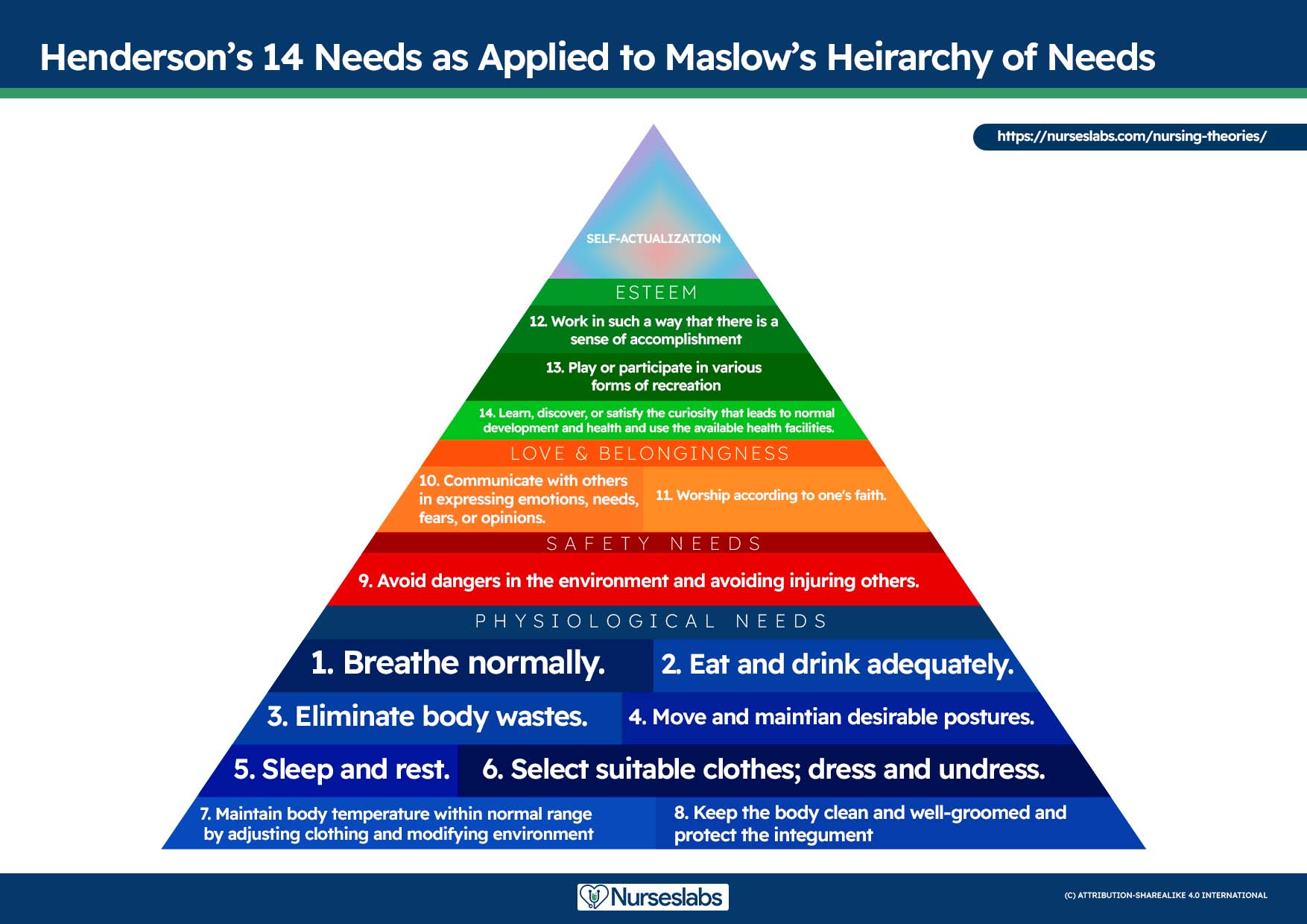
The client’s health values and beliefs, priorities, resources available, and urgency are factors the nurse must consider when assigning priorities. Involve the client in the process to enhance cooperation.
Step 5: Establishing Client Goals and Desired Outcomes
After assigning priorities for your nursing diagnosis, the nurse and the client set goals for each determined priority. Goals or desired outcomes describe what the nurse hopes to achieve by implementing the nursing interventions derived from the client’s nursing diagnoses. Goals provide direction for planning interventions, serve as criteria for evaluating client progress, enable the client and nurse to determine which problems have been resolved, and help motivate the client and nurse by providing a sense of achievement.
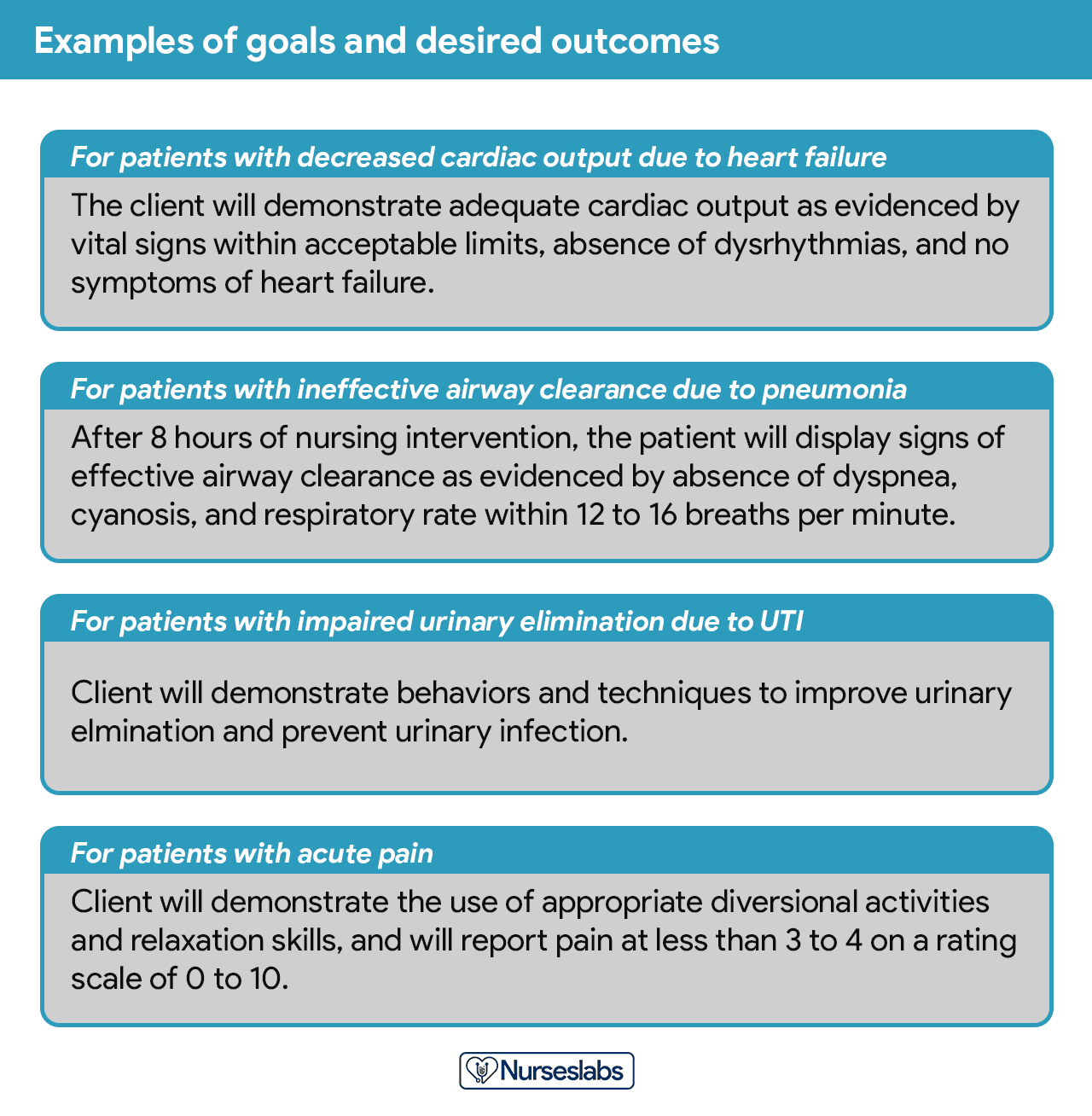
One overall goal is determined for each nursing diagnosis. The terms “ goal outcomes “ and “expected outcome s” are often used interchangeably.
According to Hamilton and Price (2013), goals should be SMART . SMART stands for specific, measurable, attainable, realistic, and time-oriented goals.
- Specific. It should be clear, significant, and sensible for a goal to be effective.
- Measurable or Meaningful. Making sure a goal is measurable makes it easier to monitor progress and know when it reaches the desired result.
- Attainable or Action-Oriented. Goals should be flexible but remain possible.
- Realistic or Results-Oriented. This is important to look forward to effective and successful outcomes by keeping in mind the available resources at hand.
- Timely or Time-Oriented. Every goal needs a designated time parameter, a deadline to focus on, and something to work toward.
Hogston (2011) suggests using the REEPIG standards to ensure that care is of the highest standards. By this means, nursing care plans should be:
- Realistic. Given available resources.
- Explicitly stated. Be clear about precisely what must be done, so there is no room for misinterpretation of instructions.
- Evidence-based. That there is research that supports what is being proposed.
- Prioritized. The most urgent problems are being dealt with first.
- Involve. Involve both the patient and other members of the multidisciplinary team who are going to be involved in implementing the care.
- Goal-centered. That the care planned will meet and achieve the goal set.
Goals and expected outcomes must be measurable and client-centered. Goals are constructed by focusing on problem prevention, resolution, and rehabilitation. Goals can be short-term or long-term . Most goals are short-term in an acute care setting since much of the nurse’s time is spent on the client’s immediate needs. Long-term goals are often used for clients who have chronic health problems or live at home, in nursing homes, or in extended-care facilities.
- Short-term goal . A statement distinguishing a shift in behavior that can be completed immediately, usually within a few hours or days.
- Long-term goal . Indicates an objective to be completed over a longer period, usually weeks or months.
- Discharge planning . Involves naming long-term goals, therefore promoting continued restorative care and problem resolution through home health, physical therapy, or various other referral sources.
Goals or desired outcome statements usually have four components: a subject, a verb, conditions or modifiers, and a criterion of desired performance.
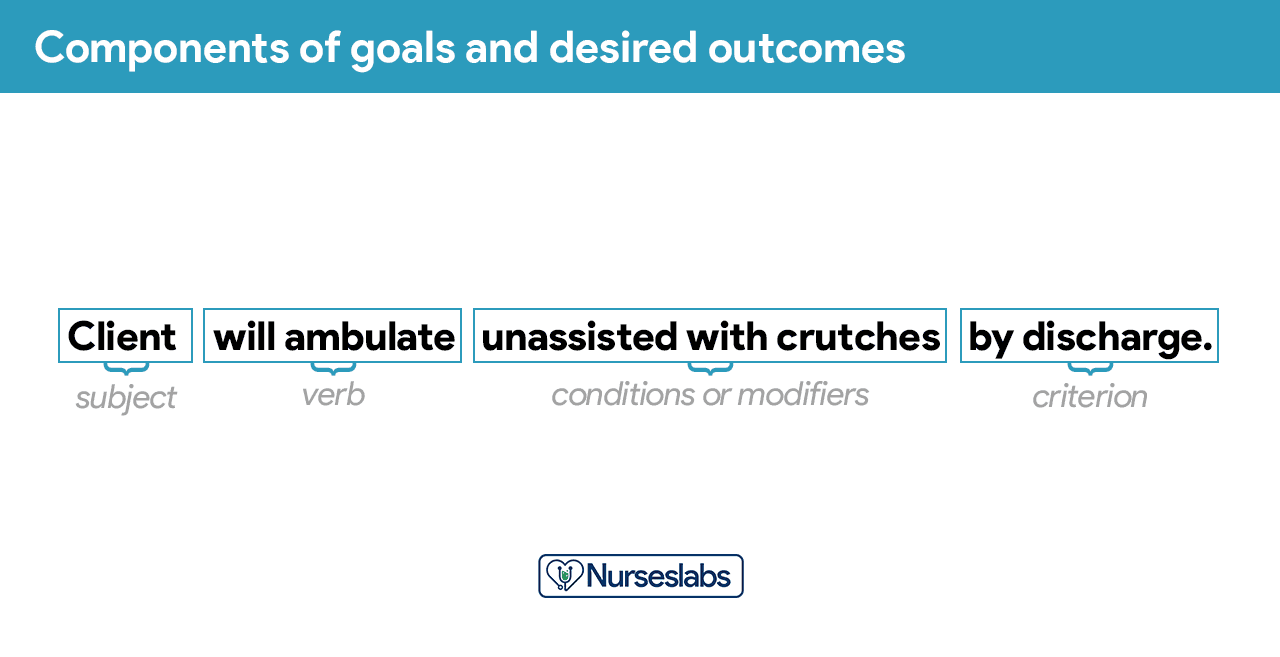
- Subject. The subject is the client, any part of the client, or some attribute of the client (i.e., pulse, temperature, urinary output). That subject is often omitted in writing goals because it is assumed that the subject is the client unless indicated otherwise (family, significant other ).
- Verb. The verb specifies an action the client is to perform, for example, what the client is to do, learn, or experience.
- Conditions or modifiers. These are the “what, when, where, or how” that are added to the verb to explain the circumstances under which the behavior is to be performed.
- Criterion of desired performance. The criterion indicates the standard by which a performance is evaluated or the level at which the client will perform the specified behavior. These are optional.
When writing goals and desired outcomes, the nurse should follow these tips:
- Write goals and outcomes in terms of client responses and not as activities of the nurse. Begin each goal with “Client will […]” help focus the goal on client behavior and responses.
- Avoid writing goals on what the nurse hopes to accomplish, and focus on what the client will do.
- Use observable, measurable terms for outcomes. Avoid using vague words that require interpretation or judgment of the observer.
- Desired outcomes should be realistic for the client’s resources, capabilities, limitations, and on the designated time span of care.
- Ensure that goals are compatible with the therapies of other professionals.
- Ensure that each goal is derived from only one nursing diagnosis. Keeping it this way facilitates evaluation of care by ensuring that planned nursing interventions are clearly related to the diagnosis set.
- Lastly, make sure that the client considers the goals important and values them to ensure cooperation.
Step 6: Selecting Nursing Interventions
Nursing interventions are activities or actions that a nurse performs to achieve client goals. Interventions chosen should focus on eliminating or reducing the etiology of the priority nursing problem or diagnosis. As for risk nursing problems, interventions should focus on reducing the client’s risk factors. In this step, nursing interventions are identified and written during the planning step of the nursing process ; however, they are actually performed during the implementation step.
Nursing interventions can be independent, dependent, or collaborative:
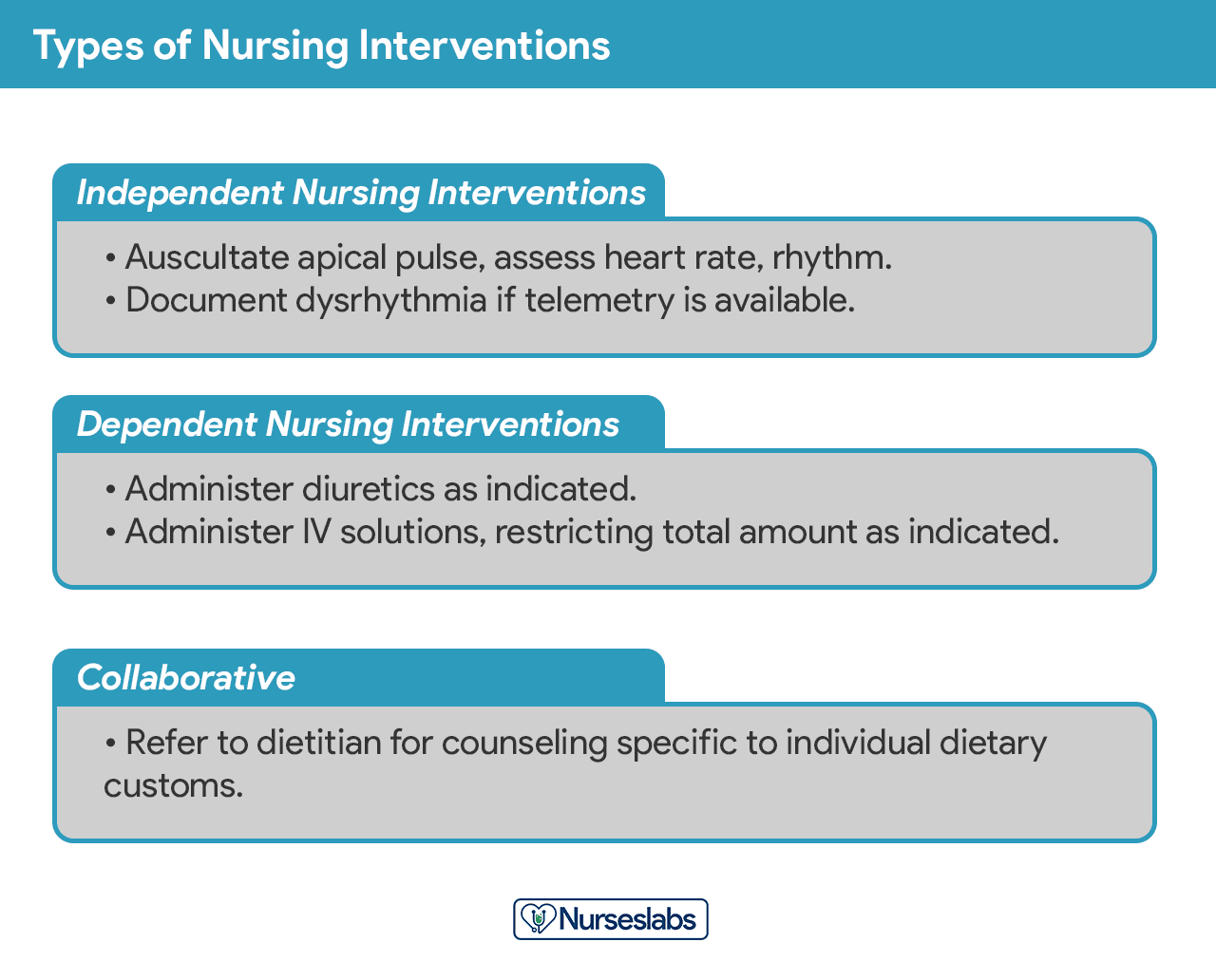
- Independent nursing interventions are activities that nurses are licensed to initiate based on their sound judgement and skills. Includes: ongoing assessment, emotional support, providing comfort , teaching, physical care, and making referrals to other health care professionals.
- Dependent nursing interventions are activities carried out under the physician’s orders or supervision. Includes orders to direct the nurse to provide medications, intravenous therapy , diagnostic tests, treatments, diet, and activity or rest. Assessment and providing explanation while administering medical orders are also part of the dependent nursing interventions.
- Collaborative interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, dietitians, and therapists. These actions are developed in consultation with other health care professionals to gain their professional viewpoint.
Nursing interventions should be:
- Safe and appropriate for the client’s age, health, and condition.
- Achievable with the resources and time available.
- Inline with the client’s values, culture, and beliefs.
- Inline with other therapies.
- Based on nursing knowledge and experience or knowledge from relevant sciences.
When writing nursing interventions, follow these tips:
- Write the date and sign the plan. The date the plan is written is essential for evaluation, review, and future planning. The nurse’s signature demonstrates accountability.
- Nursing interventions should be specific and clearly stated, beginning with an action verb indicating what the nurse is expected to do. Action verb starts the intervention and must be precise. Qualifiers of how, when, where, time, frequency, and amount provide the content of the planned activity. For example: “ Educate parents on how to take temperature and notify of any changes,” or “ Assess urine for color, amount, odor, and turbidity.”
- Use only abbreviations accepted by the institution.
Rationales, also known as scientific explanations, explain why the nursing intervention was chosen for the NCP.
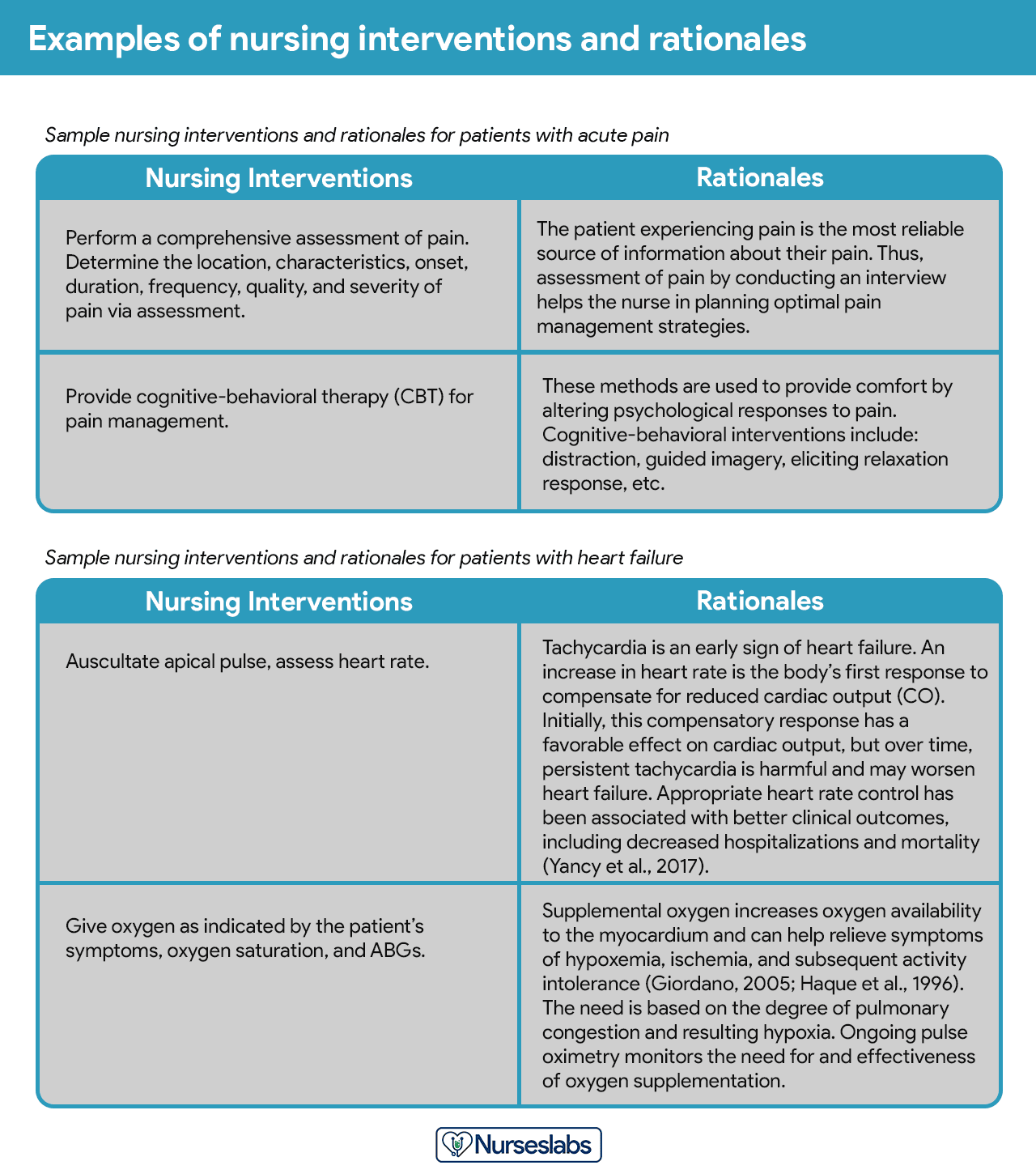
Rationales do not appear in regular care plans. They are included to assist nursing students in associating the pathophysiological and psychological principles with the selected nursing intervention.
Evaluation is a planned, ongoing, purposeful activity in which the client’s progress towards achieving goals or desired outcomes is assessed, and the effectiveness of the nursing care plan (NCP). Evaluation is an essential aspect of the nursing process because the conclusions drawn from this step determine whether the nursing intervention should be terminated, continued, or changed.
The client’s care plan is documented according to hospital policy and becomes part of the client’s permanent medical record, which may be reviewed by the oncoming nurse. Different nursing programs have different care plan formats. Most are designed so that the student systematically proceeds through the interrelated steps of the nursing process , and many use a five-column format.
Nursing Care Plan List
This section lists the sample nursing care plans (NCP) and nursing diagnoses for various diseases and health conditions. They are segmented into categories:
Miscellaneous nursing care plans examples that don’t fit other categories:
Care plans that involve surgical intervention .
| Surgery and Perioperative Care Plans |
|---|
Nursing care plans about the different diseases of the cardiovascular system :
| Cardiac Care Plans |
|---|
Nursing care plans (NCP) related to the endocrine system and metabolism:
| Endocrine and Metabolic Care Plans |
|---|
| Acid-Base Imbalances |
|---|
| Electrolyte Imbalances |
|---|
Care plans (NCP) covering the disorders of the gastrointestinal and digestive system :
| Gastrointestinal Care Plans |
|---|
Care plans related to the hematologic and lymphatic system:
| Hematologic & Lymphatic Care Plans |
|---|
NCPs for communicable and infectious diseases:
| Infectious Diseases Care Plans |
|---|
All about disorders and conditions affecting the integumentary system:
| Integumentary Care Plans |
|---|
Nursing care plans about the care of the pregnant mother and her infant. See care plans for maternity and obstetric nursing:
| Maternal and Plans |
|---|
Care plans for mental health and psychiatric nursing:
| Mental Health and Psychiatric Care Plans |
|---|
Care plans related to the musculoskeletal system:
| Musculoskeletal Care Plans |
|---|
Nursing care plans (NCP) for related to nervous system disorders:
| Neurological Care Plans |
|---|
Care plans relating to eye disorders:
| Care Plans |
|---|
Nursing care plans (NCP) for pediatric conditions and diseases:
| Pediatric Nursing Care Plans |
|---|
Care plans related to the reproductive and sexual function disorders:
| Reproductive Care Plans |
|---|
Care plans for respiratory system disorders:
| Respiratory Care Plans |
|---|
Care plans related to the kidney and urinary system disorders:
| Urinary Care Plans |
|---|
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Recommended reading materials and sources for this NCP guide:
- Björvell, C., Thorell-Ekstrand, I., & Wredling, R. (2000). Development of an audit instrument for nursing care plans in the patient record. BMJ Quality & Safety , 9 (1), 6-13. [ Link ]
- DeLaune, S. C., & Ladner, P. K. (2011). Fundamentals of nursing: Standards and practice . Cengage learning .
- Freitas, F. A., & Leonard, L. J. (2011). Maslow’s hierarchy of needs and student academic success . Teaching and learning in Nursing , 6 (1), 9-13.
- Hamilton, P., & Price, T. (2007). The nursing process, holistic. Foundations of Nursing Practice E-Book: Fundamentals of Holistic Care , 349.
- Lee, T. T. (2004). Evaluation of computerized nursing care plan: instrument development . Journal of Professional Nursing , 20 (4), 230-238.
- Lee, T. T. (2006). Nurses’ perceptions of their documentation experiences in a computerized nursing care planning system . Journal of Clinical Nursing , 15 (11), 1376-1382.
- Rn , B. O. C., Rn, H. M., Rn, D. T., & Rn, F. E. (2000). Documenting and communicating patient care : Are nursing care plans redundant?. International Journal of Nursing Practice , 6 (5), 276-280.
- Stonehouse, D. (2017). Understanding the nursing process . British Journal of Healthcare Assistants , 11 (8), 388-391.
- Yildirim, B., & Ozkahraman, S. (2011). Critical thinking in nursing process and education . International journal of humanities and social science , 1 (13), 257-262.
69 thoughts on “Nursing Care Plans (NCP) Ultimate Guide and List”
This page is helpful!
Thank you! Hope we’ve helped you write better nursing care plans!
Will definitely use this site to help write care plans. How should I cite this link when using APA format. Thank You
HI Can some one help me to do assignment on Impaired renal perfusion. 1.Goal 2.Related Action 3.Rational 4.Evaluate outcome
Wow God bless plenty Nurseslabs really relieve my burdens 😊😊
Thank you for all this useful info! I have been looking for something like this online.
You’re welcome! :)
Quite educative thank you
The notes were indeed useful
I hope to learn more and improve my skills towards nursing
Thank you so so much! This website is of great assistance to me. God bless you.
It’s so great for nursing student
Very beautiful ,Good work keep it up
Nice work. Well done
Very helpful
Great job,thank you
Thanks so much , it’s of much support for students .
Risk for ineffective thermoregulation would be a good one for you to do next for newborn.
Hi, i have learnt a lot THANK YOU. i would kindly like to learn more on paper 1 since am yet to sit for my nursing council exams and feel challenged on the paper.please do assist me thank you.
This site is a total lifesaver!
What is a nursing care plan a mother in second stage of labour?
Please see: 36 Labor Stages, Induced and Augmented Labor Nursing Care Plans
What is the nursing care plan for pulmonary oedema?
I m interest in receiving a blank nursing care plan template for my students to type on. I was wondering if it was available and if so can you please direct me on where to find it?
Hi! You can download it here: Nursing Care Plan Template
I love this website!!! Is there a textbook version of the Nurseslabs that I can purchase??
Thank you Nurseslabs. This is a wonderful note you’ve prepared for all nurses. I would like a pdf of this. Thanks.
I wish I had had this resource when i was in nursing school 2008!!
Yeah! It’s nice
Thanks for this information!
God bless you sis…Thank you for all this useful info!
This is the kind of step-by-step guidance that I needed. Thank you!
Thank you. I have learned a lot!
Wow! This is a hidden treasure!
Thanks a lot for this, it is really helpful!
Hi Matt! I would like to purchase a textbook of your nursing care plan. Where I can purchase pls help!
Hi Criselda,
Sorry, we don’t have a textbook. All of our resources are here on the website and free to use.
Good day, I would like to know how can I use your website to help students with care plans.
Sincerely, Oscar A. Acosta DNP, RN
Oh I love your works. Your explanations
I’m glad I’ve met your website. It helps me a lot. Thank you
I love this, so helpful.
These care plans are great for using as a template. I don’t have to reinvent the wheel, and the information you provided will ensure that I include the important data without leaving things out. Thanks a million!
Hi, I have learnt a lot, this is a wonderful note you’ve prepared for all nurses thank you.
Matt, this page is very informative and I especially appreciate seeing care plans for patients with neurological disorders. I notice, though, that traumatic brain injury is not on your list. Might you add a care plan page for this?
Thanks alot I had gained much since these are detailed notes 🙏🙏
OMG, this is amazing!
Wow very helpful.thank you very much🙏🙏
Hi, is there a downloadable version of this, pdf or other files maybe this is awesome!
Hi Paul, on your browser go to File > Print > Save as PDF. Hope that helps and thanks for visiting Nurseslabs!
Matt, I’m a nursing instructor looking for tools to teach this. I am interested in where we can find “rules” for establishing “related to” sections…for example –not able to utilize medical diagnosis as a “related to” etc. Also, resources for nursing rationale.
Hello, please check out our guide on how to write nursing diagnoses here: https://nurseslabs.com/nursing-diagnosis/
Nursing care plan is very amazing
Thanks for your time. Nursing Care Plan looks great and helpful!
complete knowledge i get from here
great resource. puts it all together. Thank for making it free for all
Hello Ujunwa, Thanks a lot for the positive vibes! 🌟 It’s super important to us that everyone has access to quality resources. Just wondering, is there any specific topic or area you’d love to see more about? We’re always looking to improve and add value!
Great work.
Hi Abbas, Thank you so much! Really glad to hear you found the nursing care plans guide useful. If there’s a specific area or topic you’re keen on exploring more, or if you have any suggestions for improvement, feel free to share. Always aiming to make our resources as helpful as possible!
It has been good time me to use these nursing guides.
What is ncp for acute pain
For everything you need to know about managing acute pain, including a detailed nursing care plan (NCP), definitely check out our acute pain nursing care plan guide . It’s packed with insights on assessment, interventions, and patient education to effectively manage and alleviate acute pain.
Good morning. I love this website
what is working knowledge on nursing standard, and Basic Life Support documentation?
Thank you for the website, it is awesome. I just have one question about the 1st set of ABG (Practice Exam) – The following are the values: pH 7.3, PaCO2 68 mm Hg, HCO3 28 mmol/L, and PaO2 60 mm Hg…Definitely Respiratory Acidosis, but the HC03 is only 28 mmol/L..I thought HC03 of 28 mmol/L would be within the normal range and thus, no compensation, but the correct answer has partial compensation because of the HC03 value. What value ranges are you using for HC03. Thanks, EK Mickley, RN BSN
welcome to you can get the best way to days after the holiest month
Intra operative care ncp
Leave a Comment Cancel reply
Nursing Care Plans Explained: Types, Tutorial & Examples

Nursing care plans are written tools that outline nursing diagnoses , interventions, and goals. Care plans are especially useful for student nurses as they learn to utilize the nursing process. By creating a nursing care plan based on a patient’s assessment, the nurse learns how to prioritize, plan goals and interventions, and evaluate outcomes related to specific disease processes. Care plans are essential for communication between nurses and other care team members in order to provide high-quality, continuous, evidence-based care.
In this article:
- What is a Nursing Care Plan?
- Why Use Nursing Care Plans?
- Types of Nursing Care Plans
- Nursing Care Plan Considerations
- Creating SMART Goals
- Nursing Interventions
- Tips for Effective Care Planning
- Nursing Care Plan Examples
Nursing care plans are a structured framework for delivering patient care. Nursing care plans are often called the “plan of care” and provide directions to nurses and the interprofessional team. Care plans are often described as the roadmap of patient care 2 , as they help nurses plan, prioritize, rationalize, and evaluate interventions.
Listed below are some of the benefits of using care plans in nursing practice.
1. Follows the client from admission to discharge . Care plans are continually updated depending on the patient’s status, goals, and outcomes and follow the patient across facility transfers and to different care settings.
2. Helps nurses plan interventions and revise care . Care plans provide structure to interventions, allowing the nurse to assess the intervention’s outcome and potentially revise care based on the outcome.
3. Evaluates interventions . Care plans include a combination of short and long-term goals that are specific, measurable, and timely. The nurse can evaluate if interventions are effective by evaluating goal progression.
4. Communication and continuity between nurses . The plan of care is a document that assists nurses in providing continuous and consistent care, working toward shared goals.
5. Coordinates other disciplines . The care plan may include input or interventions other interdisciplinary team members provide. A care plan communicates priorities between interprofessional team members to coordinate on common goals.
6. Engage with the patient/patient-centered care . Whenever possible, the patient should be involved in creating their plan of care. Nursing care plans are best used collaboratively with patients and families to account for a patient’s preferences, values, culture, and lifestyle. 2
7. Documentation purposes . Care plans are an opportunity for nurses to demonstrate that safe and ethical care was provided in accordance with professional regulations. Documentation may be used for communication, quality improvement, research, or legal proceedings.
8. Offers a framework for consistent care. A nursing diagnosis supports the care plan and outlines appropriate interventions. Nursing diagnoses should align with a NANDA-I nursing diagnosis, creating consistency in nursing diagnosis terminology and facilitating effective communication. 1
9. Prevents future health hazards. Some care plans may include nursing diagnoses the patient is at risk for, like falls or infection. Care plan interventions and goals can be created to prevent complications.
There is some variation in how care plans are used in practice. The structure and format of a care plan depend on the purpose of the care plan and the care setting.
Formal vs. Informal Care Planning
Generally, informal care plans are not formally documented. Informal care plans might include the nurse’s goals for their shift. These goals can be modified depending on the day’s priorities or changes in the patient’s condition.
Formal care plans are documented as part of the patient record used to coordinate, prioritize, and maintain continuity of care. While formal care plans are also modifiable depending on new priorities or the outcomes of interventions, they are often related to the longer-term goals of the patient. The formal care plan might include goals to meet before discharge from the hospital or the service. Both formal and informal care plans are used within the framework of the nursing process.
Standardized vs. Individualized Care Planning
Care plans can be either standardized or individualized for the patient. Many care settings will use standardized care plans for specific patient conditions to deliver consistent care. One example of a standardized care plan is the post-operative care pathway used in post-surgical units. These post-operative care plans outline expected goals for each post-operative day. However, standardized care plans should be tailored when possible to the needs of the individual patient.
In contrast, individualized care plans are created for individual patient needs. Individualized care plans should include input from the patient whenever possible to create personalized goals and support patient adherence. When creating an individualized care plan, consider the patient’s health status, history, and motivational factors and inquire about what matters most to them.
The Nursing Process
Care plans enter the nursing process at the planning stage but are influenced by all other steps. The steps of the nursing process can be remembered with the acronym ADPIE. 3
- Implementation/Interventions
Here is a breakdown of the nursing process:
1. Assessment: Assessing the client’s needs, gathering data In the assessment phase of the nursing process, the nurse collects and analyzes objective and subjective data . Then, the nurse uses their nursing knowledge and critical thinking skills to decide if further assessments are necessary to identify a nursing diagnosis.
2. Diagnosis: What’s going on? Crafting a nursing diagnosis Based on data collected during the assessment phase, the nurse crafts a nursing diagnosis that can be used to direct care planning. 4 The nurse should assign a nursing diagnosis using the standardized terminology laid out by NANDA-I. A nursing diagnosis is a clinical judgment that describes actual or potential health problems or opportunities for health improvement of a patient, family, or community.
3. Planning: Time to create goals In step three of the nursing process, the nurse, ideally in collaboration with the patient, creates goals of care based on the nursing diagnosis. A care plan, including interventions and expected outcomes, is created to achieve these goals.
4. Implementation: Time to act In the implementation phase of the nursing process, the nurse takes actions and performs the interventions described in the care plan to achieve the goals of care. The nurse uses their knowledge, experience, and critical thinking to decide which interventions are a priority. Often, interventions are based on orders from the physician.
5. Evaluate: What are the outcomes? In the evaluation phase of the nursing process, the nurse reassesses the patient to determine if the intervention has the desired outcome. Next, the nurse should evaluate if the goals of care have been met or require more time. If the intervention does not have the desired effect, the nurse should consider if the care plan needs revision or if the goals of care need to be updated.
Nursing Process Example
Here is an example of how the steps of the nursing process fit together.
The nurse assesses the client who was in a motor vehicle accident. The client reports a pain level of 9/10 in their right shoulder. Through an x-ray, the client is determined to have a dislocated shoulder, and the nursing diagnosis of acute pain is applied. The nurse begins planning treatment and goals to reduce pain and instill comfort. The nurse administers IV pain medication as ordered and supports the right arm with pillows. The nurse evaluates the effectiveness of interventions by asking the client to rate their pain on a scale of 0-10. Depending on the outcome, the nurse may determine that the intervention was successful or requires revision.

How To Write a Nursing Care Plan
With experience, nursing care plans become second nature as part of nursing practice. Since nursing care planning can be formal or informal, a nursing care plan may look very different depending on the care context and the patient’s needs. While informal care plans may not be written in the patient chart, writing effective formal care plans takes practice. Formal care plans are important for communicating significant changes in the patient’s condition to the care team.
Care plans will appear differently depending on each electronic health record, computer platform, setting (home health, doctor’s office, etc.), and nursing specialty (case management, PACU, etc.). Regardless, the nursing process stays the same. One way to improve the skill of care plan writing is to read examples of high-quality care plans. Nurses can also ask experienced colleagues for feedback on their care plans. Some care settings will have templates of expected formal care plans.
Overall, the care plan should flow seamlessly as part of the nursing process, taking into account relevant nursing diagnoses, expected outcomes, and the effectiveness of the planned interventions. If necessary, goals are revised, and the care plan is repeated until goals are met or are no longer applicable.
While rationales are not included in traditional nursing care plans, they are used in student care plans. When learning to write care plans, adding the rationale behind the diagnosis and interventions can be helpful. Students can explain the pathophysiology behind their assessment and why their intervention is necessary to guide their understanding.
Consider the hierarchy of needs.
In any care setting, there are often competing priorities that nurses must handle. When deciding on how to prioritize care needs for patients, a useful framework to organize care is Maslow’s hierarchy of needs. 5 The highest priority needs are at the bottom of the pyramid including physiological needs such as air, nutrition, and sleep. The nurse must prioritize physical needs over those closer to the top of the pyramid, such as the need for a sense of connection.
S.M.A.R.T. goals are specific, measurable, attainable, realistic, and time-bound. SMART goals are helpful in care planning because they increase the likelihood that the goal created will be practical and achievable. Conversely, goals that are too vague or not realistic are less likely to be achieved, which can discourage the goal-setter.
Specific Specific goals are not overly broad. A shared goal of “walking more” is not specific. However, “Walk three laps of the unit three times a day” is specific.
Measurable Related to being specific, there should be some way to measure whether the goal has been met or is at least progressing. There should be a benchmark that signals that the goal has been met. Benchmarks could be behavioral, physical, or expressed by the patient.
Attainable Goals might take work to meet, but attainable goals are within reach. Goals that are too difficult or require multiple steps to reach are more likely to discourage rather than encourage.
Realistic An achievable goal is also realistic. Attainable goals are possible to meet, while realistic goals take into consideration the context and potential barriers to meeting the goal.
Time-bound Setting a time limit on the goal grounds the goal in reality and allows for measurement. The chosen period should depend on the goal’s size and should support progress and focus.
Examples of Collaborative SMART Goals
Here are two examples of how SMART goals can be used in care planning:
Goal: “The client will rate their pain three or less on a scale of 0-10 by discharge.”
- Specific: The goal includes an exact number on the pain scale acceptable to the patient.
- Measurable: The goal can be tracked over time and measured on the pain scale.
- Attainable: This depends on the specific patient context, but for the example, we will assume this is an achievable goal for the patient.
- Realistic: Similarly, this goal must be realistic, which will depend on the patient’s pain tolerance.
- Time-bound: In the inpatient setting, ‘by discharge’ is an appropriate time frame.
Goal: The patient will demonstrate independently using a glucometer to check their blood sugar and how to self-administer necessary insulin after three diabetes education sessions.
- Specific: The goal includes specific behaviors and outcomes of the education sessions.
- Measurable: The nurse can assess if the goal is complete by asking the patient to demonstrate their skills.
- Attainable: The patient has the motor and cognitive ability to learn these skills.
- Realistic: Enough time has been given for practice and education so that the patient feels comfortable and confident.
- Time-bound: This goal is set to be achieved after three education sessions. At the end of the third session, the nurse can assess if the goal has been met or if more support or time is needed to meet this goal.
Short vs. Long-Term Goals
When creating goals of care, it can be helpful to categorize goals into short-term or long-term goals. Short-term goals are commonly found in acute care settings, where care interactions are shorter than in the community. However, both long and short-term goals are used across care settings.
Short-term goals can be completed within a few hours or days. Although there is no precise cut-off for what makes a short-term care goal, short-term goals tend to focus on issues that need to be immediately addressed. An example of a short-term care goal is to improve the patient’s shortness of breath by identifying the cause and administering an intervention to relieve the shortness of breath.
In contrast, long-term goals are usually completed over weeks or months. Long-term care goals tend to be aimed at more chronic health challenges, prevention, and improvement. While important, they may be less urgent than short-term care goals. An example of a long-term care goal is the reduction of HbA1c over several months for a patient at risk for diabetes.
Once goals and a plan of care are established, the nurse will perform interventions. There are three main categories of nursing interventions :
Independent: Independent nursing interventions are within the nurse’s scope of practice and do not require the participation of another health professional, such as a physician, to carry out the intervention. Nurses can initiate, implement, and evaluate independent nursing interventions. An example of an independent nursing intervention is providing patient education.
Dependent: Dependent nursing interventions require the participation of another health professional to carry out the intervention. Dependent interventions are often ordered by physicians and then implemented by nurses. Collecting blood work that a physician has ordered is an example of a dependent nursing intervention.
Collaborative: Collaborative nursing interventions are carried out with other healthcare professionals through collaboration or consultation. Collaborating with a physical therapist on exercises to improve patient mobility is an example of a collaborative nursing intervention.
1. Create goals with the patient when possible. The patient should be included in their care plan to ensure goals are congruent with their lifestyle, values, and preferences. This includes patient involvement in planning interventions and defining the intervention’s successful outcome. Including the patient in the care planning process will increase their motivation to actively participate in their care.
2. Revise goals if necessary. If the goal is not met within the original timeframe, the goal may need revision to ensure that it is achievable and realistic, or the timeframe may need to be extended.
3. Continue to assess and reassess the patient. It is essential to continually evaluate the patient’s status to ensure that the goals and interventions are still appropriate for their condition.
4. If a goal is not met, assess why. Interventions that are not working or care plan goals that are not met require revision. This may include revising the interventions, updating the goals of care, reviewing the patient diagnosis, assessing the client’s motivation or lack thereof, and furthering patient education.
5. Ensure that progress towards a goal is recognized even if a goal is not met . In some situations, the goal’s timeline may need to be extended for a goal to be met. Consider that a goal may be ‘met’ even if the outcome is not what was intended.
Below you’ll find a list of over 400 care plans. All our care plans are written and reviewed by registered nurses.
- Atrial Fibrillation
- Bradycardia
- Cardiomyopathy
- Chest Pain (Angina)
- Coronary Artery Disease
- Heart Failure
- Hypertension
- Hypotension
- Myocardial Infarction
- Pulmonary Embolism
- Tachycardia
- Tetralogy of Fallot
Endocrine & Metabolic
- Diabetes Mellitus
- Diabetic Foot Ulcer
- Diabetic Ketoacidosis
- Hyperglycemia
- Hyperlipidemia
- Hypocalcemia & Hypercalcemia
- Hypoglycemia
- Hypokalemia & Hyperkalemia
- Hyponatremia & Hypernatremia
- Hypothyroidism
- Malnutrition
- Metabolic Acidosis
- Metabolic Alkalosis
- Syndrome of inappropriate antidiuretic hormone (SIADH)
Gastrointestinal
- Abdominal Pain
- Appendicitis
- Bowel Perforation
- Clostridioides Difficile
- Colon Cancer
- Colostomy & Ileostomy
- Crohn’s Disease
- Diverticulitis
- Gastrointestinal Bleed
- Liver Cirrhosis
- Nausea & Vomiting
- Pancreatic Cancer
- Pancreatitis
- Paralytic Ileus
- Peritonitis
- Small Bowel Obstruction
- Ulcerative Colitis
Genitourinary
- Acute Kidney Injury
- Benign Prostatic Hyperplasia (BPH)
- Chronic Kidney Disease
- End Stage Renal Disease (ESRD)
- Kidney Stones
- Pyelonephritis
- Urinary Tract Infection
Hematologic & Lymphatic
- Anaphylaxis
- Blood Transfusion
- Deep Vein Thrombosis
- Low Hemoglobin
- Neutropenia
- Peripheral Vascular Disease
- Sickle Cell Anemia
- Thrombocytopenia
Infectious Diseases
- Human Immunodeficiency Virus (HIV)
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Respiratory syncytial virus (RSV)
- Tuberculosis
Integumentary
- Pressure Ulcers
- Wound Care & Infection
Maternal & Newborn
- Breastfeeding
- Hyperemesis Gravidarum
- Labor and Delivery
- Placenta Previa
- Postpartum Hemorrhage
- Preeclampsia
- Preterm Labor
Mental Health & Psychiatric
- Attention deficit hyperactivity disorder (ADHD)
- Altered Mental Status
- Antisocial Personality Disorder
- Bipolar Disorder
- Major Depression
- Mental Health
- Obsessive-Compulsive Disorder (OCD)
- Psychosocial
- Post-traumatic stress disorder (PTSD)
- Schizophrenia
- Substance Abuse
Musculoskeletal
- Compartment Syndrome
- Hip Fracture
- Knee Replacement Surgery
- Myasthenia Gravis
- Osteoarthritis
- Osteomyelitis
- Osteoporosis
- Rhabdomyolysis
- Rheumatoid Arthritis
- Spinal Cord Injury
Neurological
- Cerebral Palsy
- Diabetic Neuropathy
- Encephalopathy
- Headache & Migraine
- Multiple Sclerosis
- Parkinson’s Disease
- Peripheral Neuropathy
- Stroke (CVA)
- Transient Ischemic Attack (TIA)
- Traumatic Brain Injury
Respiratory
- Acute Respiratory Failure
- Acute respiratory distress syndrome (ARDS)
- Chest Tube Insertion
- Chronic obstructive pulmonary disease (COPD)
- Cystic Fibrosis
- Pleural Effusion
- Pneumothorax
- Pulmonary Edema
- Tracheostomy
Other Care Plans
Anything that didn’t match a specific category you’ll find here:
- Alcohol Withdrawal Syndrome
- Breast Cancer
- Chemotherapy
- Community Health
- End-of-Life (Hospice) Care
- Hearing Loss
- Sleep Apnea
- NANDA International. Our Story. Accessed January 7, 2023. https://nanda.org/who-we-are/our-story/
- Capriotti T, eBook Nursing Collection – Worldwide, Books@Ovid Purchased eBooks. Nursing Care Planning Made Incredibly Easy! Third. Wolters Kluwer; 2018. https://go.exlibris.link/P281xmcS
- Toney-Butler T, Thayer J. Nursing Process. Published 2022. https://www.ncbi.nlm.nih.gov/books/NBK499937/
- Carpenito LJ, Books@Ovid Purchased eBooks. Handbook of Nursing Diagnosis. 15th ed. Wolters Kluwer; 2017.
- Hayre-Kwan S, Quinn B, Chu T, Orr P, Snoke J. Nursing and Maslow’s Hierarchy; A Health Care Pyramid Approach to Safety and Security During a Global Pandemic. Nurse Lead. 2021;19(6):590-595. doi:10.1016/j.mnl.2021.08.013

We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them)
By Hannah Meinke on 07/05/2021
The nursing profession tends to attract those who have natural nurturing abilities, a desire to help others, and a knack for science or anatomy. But there is another important skill that successful nurses share, and it's often overlooked: the ability to think critically.
Identifying a problem, determining the best solution and choosing the most effective method to solve the program are all parts of the critical thinking process. After executing the plan, critical thinkers reflect on the situation to figure out if it was effective and if it could have been done better. As you can see, critical thinking is a transferable skill that can be leveraged in several facets of your life.
But why is it so important for nurses to use? We spoke with several experts to learn why critical thinking skills in nursing are so crucial to the field, the patients and the success of a nurse. Keep reading to learn why and to see how you can improve this skill.
Why are critical thinking skills in nursing important?
You learn all sorts of practical skills in nursing school, like flawlessly dressing a wound, taking vitals like a pro or starting an IV without flinching. But without the ability to think clearly and make rational decisions, those skills alone won’t get you very far—you need to think critically as well.
“Nurses are faced with decision-making situations in patient care, and each decision they make impacts patient outcomes. Nursing critical thinking skills drive the decision-making process and impact the quality of care provided,” says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing.
For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they must evaluate which patients should be treated first. While they rely on their training to measure vital signs and level of consciousness, they must use critical thinking to analyze the consequences of delaying treatment in each case.
No matter which department they work in, nurses use critical thinking in their everyday routines. When you’re faced with decisions that could ultimately mean life or death, the ability to analyze a situation and come to a solution separates the good nurses from the great ones.
How are critical thinking skills acquired in nursing school?
Nursing school offers a multitude of material to master and upholds high expectations for your performance. But in order to learn in a way that will actually equip you to become an excellent nurse, you have to go beyond just memorizing terms. You need to apply an analytical mindset to understanding course material.
One way for students to begin implementing critical thinking is by applying the nursing process to their line of thought, according to Vest. The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation.
“One of the fundamental principles for developing critical thinking is the nursing process,” Vest says. “It needs to be a lived experience in the learning environment.”
Nursing students often find that there are multiple correct solutions to a problem. The key to nursing is to select the “the most correct” solution—one that will be the most efficient and best fit for that particular situation. Using the nursing process, students can narrow down their options to select the best one.
When answering questions in class or on exams, challenge yourself to go beyond simply selecting an answer. Start to think about why that answer is correct and what the possible consequences might be. Simply memorizing the material won’t translate well into a real-life nursing setting.
How can you develop your critical thinking skills as a nurse?
As you know, learning doesn’t stop with graduation from nursing school. Good nurses continue to soak up knowledge and continually improve throughout their careers. Likewise, they can continue to build their critical thinking skills in the workplace with each shift.
“To improve your critical thinking, pick the brains of the experienced nurses around you to help you get the mindset,” suggests Eileen Sollars, RN ADN, AAS. Understanding how a seasoned nurse came to a conclusion will provide you with insights you may not have considered and help you develop your own approach.
The chain of command can also help nurses develop critical thinking skills in the workplace.
“Another aid in the development of critical thinking I cannot stress enough is the utilization of the chain of command,” Vest says. “In the chain of command, the nurse always reports up to the nurse manager and down to the patient care aide. Peers and fellow healthcare professionals are not in the chain of command. Clear understanding and proper utilization of the chain of command is essential in the workplace.”
How are critical thinking skills applied in nursing?
“Nurses use critical thinking in every single shift,” Sollars says. “Critical thinking in nursing is a paramount skill necessary in the care of your patients. Nowadays there is more emphasis on machines and technical aspects of nursing, but critical thinking plays an important role. You need it to understand and anticipate changes in your patient's condition.”
As a nurse, you will inevitably encounter a situation in which there are multiple solutions or treatments, and you'll be tasked with determining the solution that will provide the best possible outcome for your patient. You must be able to quickly and confidently assess situations and make the best care decision in each unique scenario. It is in situations like these that your critical thinking skills will direct your decision-making.
Do critical thinking skills matter more for nursing leadership and management positions?
While critical thinking skills are essential at every level of nursing, leadership and management positions require a new level of this ability.
When it comes to managing other nurses, working with hospital administration, and dealing with budgets, schedules or policies, critical thinking can make the difference between a smooth-running or struggling department. At the leadership level, nurses need to see the big picture and understand how each part works together.
A nurse manager , for example, might have to deal with being short-staffed. This could require coaching nurses on how to prioritize their workload, organize their tasks and rely on strategies to keep from burning out. A lead nurse with strong critical thinking skills knows how to fully understand the problem and all its implications.
- How will patient care be affected by having fewer staff?
- What kind of strain will be on the nurses?
Their solutions will take into account all their resources and possible roadblocks.
- What work can be delegated to nursing aids?
- Are there any nurses willing to come in on their day off?
- Are nurses from other departments available to provide coverage?
They’ll weigh the pros and cons of each solution and choose those with the greatest potential.
- Will calling in an off-duty nurse contribute to burnout?
- Was this situation a one-off occurrence or something that could require an additional hire in the long term?
Finally, they will look back on the issue and evaluate what worked and what didn’t. With critical thinking skills like this, a lead nurse can affect their entire staff, patient population and department for the better.
Beyond thinking
You’re now well aware of the importance of critical thinking skills in nursing. Even if you already use critical thinking skills every day, you can still work toward strengthening that skill. The more you practice it, the better you will become and the more naturally it will come to you.
If you’re interested in critical thinking because you’d like to move up in your current nursing job, consider how a Bachelor of Science in Nursing (BSN) could help you develop the necessary leadership skills.
EDITOR’S NOTE: This article was originally published in July 2012. It has since been updated to include information relevant to 2021.
- Share on Facebook
- Share on Twitter
- Share on Pinterest
- Share on LinkedIn
Request More Information
Talk with an admissions advisor today.
Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid (for those who qualify)
- Customized Support Services
- Detailed Program Plans
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- 10 digits with no dashes or spaces
- No country code (e.g. "1" for USA)
There is an error in ZIP code. Make sure your answer has only 5 digits.
We offer tuition savings for many employers—see if yours is one of them.
Please enter Corporate Employer.
Can’t find your employer? Select "Other Employer Not In List" or "Not Employed".
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Hannah Meinke

Posted in General Nursing
- nursing education
Related Content

Brianna Flavin | 05.07.2024

Brianna Flavin | 03.19.2024

Robbie Gould | 11.14.2023

Noelle Hartt | 11.09.2023
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.
ADPIE – The Five Stages of The Nursing Process
ADPIE is an acronym for assessment, diagnosis, planning, implementation, and evaluation.
The ADPIE process helps medical professionals remember the process and order of the steps they need to take to provide proper care for the individuals they are treating.
This process is essential as it provides a practical and thorough framework for patient care.
It also helps medical professionals develop critical thinking and problem-solving skills.
By following the ADPIE process, medical professionals can improve their work efficiency and promptly develop more accurate decisions.
Process Overview
The purpose of ADPIE is to help improve an individual’s mental, emotional, and physical health through analysis, diagnosis, and treatment.
The ADPIE process allows medical professionals to identify potential problems, develop solutions, and monitor the results individually.
Nurses must reevaluate, adjust and correct the process if it does not improve the patient’s condition.
Here is an explanation detailing each step of the process:
Assessment is the first step of the ADPIE process.
During the assessment phase, medical professionals will attempt to identify the problem and establish a database.
Interviewing the patient and family members, observing behavior, and performing examinations help with the assessment.
This step focuses heavily on collecting/recording data, validating information, and listing any abnormalities in the data.
Nurses collect assessment data in one of two ways, subjective or objective.
You cannot measure subjective data directly.
It includes verbal information like asking questions, obtaining verbal feedback, interviewing people, and collecting/gathering a patient’s health history data.
Subjective data is symptomatic because nurses cannot measure or observe it directly.
Objective data is measurable because nurses can see, hear, feel, or smell it.
It includes measuring a patient’s weight, blood pressure, heart rate, and body temperature.
Because objective data is measurable, nurses refer to it as signs.
Gathering as much data as possible during the assessment phase is essential.
While gathering data, Identify if the data is accurate, concise, consistent, and straightforward.
Once you’ve gathered enough accurate data, you can form a conclusion about the patient’s condition.
After that, move on to the next phase of the ADPIE process, diagnosis.
The process’s diagnosis phase is where the medical professional develops a theory or hypothesis about the individual’s situation based on the information collected while performing an assessment.
Although registered nurses cannot form a professional diagnosis, they can develop critical thinking and communicate their clinical judgments to their team members.
Nurses have a standardized language for communicating their clinical judgments, which comes from NANDA international .
That said, certified nurse practitioners can diagnose medical conditions and act as primary care providers for their patients.
Examples of Medical Language Nurse Use Include:
- Activity intolerance
- Constipation
- Decreased cardiac output
- Fluid volume deficit
- Hypothermia
- Sleep deficit
The diagnostic process allows medical professionals to decide on the individual they treat.
That determination determines whether the patient is dealing with a physiological, mental, or emotional condition.
And while nurses cannot give a professional diagnosis , they can identify actual or potential medical /health risks.
After performing a diagnosis, nurses must place risks that can cause complications or harm in order.
Organize the highest risks as the top priority (life-threatening).
Accordingly, nurses should label lower risks in descending order (non-life-threatening/minor/future well-being).
Nurses must identify, address and correct new problems that affect other priorities.
Therefore, nurses must perform assessments regularly to approach patient problems adequately.
After identifying and prioritizing the concerns, the next phase of the process is planning.
Planning involves developing a plan and establishing SMART goals to achieve the desired outcome.
For example, adequate planning helps reduce a patient’s pain or improve cardiovascular function.
SMART goals are specific, measurable, attainable, realistic/relevant, and time-restricted.
SMART goals provide the individual with focused activities designed to improve their condition.
They also provide medical professionals with a plan to measure and evaluate the individual’s improvements.
Goals may be short-term or long-term, singular in nature, and focus on the individual outcome.
Nurses must determine whether the SMART goals benefit the patient.
They must also make sure that the SMART goals are attainable.
In addition to SMART goals, nurses must develop and communicate a care plan and intervention strategies to the team.
It helps maximize the success of the goals.
The care plan involves the steps and strategies needed to achieve the desired goal.
Along with the care plan, developing intervention strategies keeps the individual on track.
Nurses communicate the care plan and intervention strategies to the patient and medical team as part of the treatment.
After nurses establish the care plan, interventions, and SMART goals, they must implement them into patient care.
Implementation
The implementation phase is the actionable part of the process.
It’s where the medical team implements the care plan, SMART goals, and interventions to achieve their goals.
Accordingly, nurses can evaluate and measure this process.
The implementation phase uses a combination of direct care and indirect care.
Direct care involves giving patients physical or verbal aid.
Direct care includes assisting the patient with mobility, performing physical maintenance, range of motion exercises, and assisting with daily living activities.
It may also include coaching, counseling, and providing feedback to the individual.
Indirect care involves actions performed while away from the patient.
Indirect care may include monitoring/supervising the medical staff, delegating responsibilities, and advocating on behalf of the patients.
While implementing the care plan, the nurse/team needs to use critical judgment.
They must also question care plan procedures to ensure it meets the demands/concerns of the people receiving the care.
Steps or procedures that appear inappropriate, non-actionable, or questionable should be questioned and reevaluated with the medical staff.
Moreover, nurses must communicate with those receiving the care plan to ensure it is safe and aligns with the medical teams/individuals’ goals.
The last phase of the process is the evaluation phase.
It’s where the medical professionals assess and evaluate the success of the planning and implementation processes.
This phase ensures that the individual is making progress towards their goals and is achieving the desired outcome.
Healthcare professionals must evaluate if the process works and identify what brings the individual closer to their goals.
Nurses must reassess the problem if it isn’t working and determine whether it needs to be modified or eliminated.
Nurses must regularly perform evaluations during the ADPIE process to assess the plan and make adjustments.
By performing regular evaluations, medical professionals can determine the appropriate course of action, identify potential errors, and ensure that the process works as smoothly as possible.
ADPIE Recap
The ADPIE process assists medical professionals in identifying and addressing potential medical concerns.
By implementing the process, medical professionals can assess the patient’s condition and ensure they receive adequate care.
The assessment process begins through the collection of subjective and objective data.
This data allows medical to develop a diagnosis based on the collected information.
With the diagnosis, nurses can create a plan with interventions and SMART goals for the patient to follow.
The process is then implemented into action to achieve the plan’s goals.
Nurses must evaluate the process during and after implementation to ensure the individual achieves their goals.
ADPIE is an excellent way to improve critical thinking.
It helps nurses create, evaluate, and reevaluate procedures.
It also helps them implement and modify processes until they reach the desired outcome.
What Are The Five Stages of The Nursing Process?
The five stages of the nursing process are assessment, diagnosis, planning, implementation, and evaluation.
In other words, the five stages of the nursing process are ADPIE, which I explained earlier in this article.
Nurses follow these five stages to ensure proper patient care from the beginning of treatment until the end.
Consequently, It allows nurses to utilize a systematic approach to observing, analyzing, taking action, and reevaluating goals, strategies, and outcomes.
Overall this helps nurses perform their best and account for potential mistakes and errors throughout patient treatment.
The ADPIE nursing process is an essential component of clinical care.
It improves critical thinking and decision-making by breaking down processes into simplified and organized steps.
Each concurrent step builds upon the previous one throughout the process until nurses develop and implement a good approach.
With that said, numerous nurses lack experience applying the ADPIE nursing process.
It’s partially due to a shortage of information/resources and busy work schedules making it difficult to implement.
However, new processes are continually developing, allowing current/future nurses to incorporate these processes into their daily work.
Without processes like ADPIE and others, nurses would have more difficulty approaching complex patient care scenarios.
ADPIE isn’t well known among some nurses.
However, there are many well-known, and implemented processes nurses utilize.
Critical Thinking and the Nursing Process
In today’s health care arena, the nurse is faced with increasingly complex issues and situations resulting from advanced technology, greater acuity of patients in hospital and community settings, an aging population, and complex disease processes, as well as ethical and cultural factors. Traditionally, nurses have used a problem-solving approach in planning and providing nursing care. Today the decision-making part of problem solving has become increasingly complex and requires critical thinking.
Definition of Critical thinking
Critical thinking is a multidimensional skill, a cognitive or mental process or set of procedures. It involves reasoning and purposeful, systematic, reflective, rational, outcome-directed thinking based on a body of knowledge, as well as examination and analysis of all available information and ideas. Critical thinking leads to the formulation of conclusions and the most appropriate, often creative, decisions, options, or alternatives. Critical thinking includes metacognition, the examination of one’s own reasoning or thought processes while thinking, to help strengthen and refine thinking skills. Independent judgments and decisions evolve from a sound knowledge base and the ability to synthesize information within the context in which it is presented. Nursing practice in today’s society mandates the use of high-level critical thinking skills within the nursing process. Critical thinking enhances clinical decision making, helping to identify patient needs and to determine the best nursing actions that will assist the patient in meeting those needs. Critical thinking and critical thinkers have distinctive characteristics. As indicated in the above definition, critical thinking is a conscious, outcome-oriented activity; it is purposeful and intentional. The critical thinker is an inquisitive, fair-minded truth seeker with an open-mindedness to the alternative solutions that might surface.
Critical thinking Process: Rationality and Insight
Critical thinking is systematic and organized. The skills involved in critical thinking are developed over time through effort, practice, and experience. Skills needed in critical thinking include interpretation, analysis, evaluation, inference, explanation, and self-regulation. Critical thinking requires background knowledge and knowledge of key concepts as well as standards of good thinking. The critical thinker uses reality-based deliberation to validate the accuracy of data and the reliability of sources, being mindful of and questioning inconsistencies. Interpretation is used to determine the significance of data that are gathered, and analysis is used to identify patient problems indicated by the data. The nurse uses inference to draw conclusions. Explanation is the justification of actions or interventions used to address patient problems and to help a patient move toward desired outcomes. Evaluation is the process of determining whether outcomes have been or are being met, and self-regulation is the process of examining the care provided and adjusting the interventions as needed. Critical thinking is also reflective, involving metacognition, active evaluation, and refinement of the thinking process. The critical thinker considers the possibility of personal bias when interpreting data and determining appropriate actions. The critical thinker must be insightful and have a sense of fairness and integrity, the courage to question personal ethics, and the perseverance to strive continuously to minimize the effects of egocentricity, ethnocentricity, and other biases on the decision making process.
Components of Critical thinking
Certain cognitive or mental activities can be identified as key components of critical thinking. When thinking critically, a person will do the following:
- Ask questions to determine the reason why certain developments have occurred and to see whether more information is needed to understand the situation accurately.
- Gather as much relevant information as possible to consider as many factors as possible.
- Validate the information presented to make sure that it is accurate (not just supposition or opinion), that it makes sense, and that it is based on fact and evidence.
- Analyze the information to determine what it means and to see whether it forms clusters or patterns that point to certain conclusions.
- Draw on past clinical experience and knowledge to explain what is happening and to anticipate what might happen next, acknowledging personal bias and cultural influences.
- Maintain a flexible attitude that allows the facts to guide thinking and takes into account all possibilities.
- Consider available options and examine each in terms of its advantages and disadvantages.
- Formulate decisions that reflect creativity and independent decision making.
Critical thinking requires going beyond basic problem solving into a realm of inquisitive exploration, looking for all relevant factors that affect the issue, and being an “out-of-the-box” thinker. It includes questioning all findings until a comprehensive picture emerges that explains the phenomenon, possible solutions, and creative methods for proceeding. Critical thinking in nursing practice results in a comprehensive patient plan of care with maximized potential for success.
Critical thinking In Nursing Practice
Using critical thinking to develop a plan of nursing care requires considering the human factors that might influence the plan. The nurse interacts with the patient, family, and other health care providers in the process of providing appropriate, individualized nursing care. The culture, attitude, and thought processes of the nurse, the patient, and others will affect the critical thinking process from the data-gathering stage through the decision-making stage; therefore, aspects of the nurse-patient interaction must be considered. Nurses must use critical thinking skills in all practice settings—acute care, ambulatory care, extended care, and in the home and community. Regardless of the setting, each patient situation is viewed as unique and dynamic. The unique factors that the patient and nurse bring to the health care situation are considered, studied, analyzed, and interpreted. Interpretation of the information presented then allows the nurse to focus on those factors that are most relevant and mostsignificant to the clinical situation. Decisions about what to do and how to do it are then developed into a plan of action.
Fonteyn (1998) identified 12 predominant thinking strategies used by nurses, regardless of their area of clinical practice:
Recognizing a pattern
- Setting priorities
- Searching for information
- Generating hypotheses
- Making predictions
- Forming relationships
- Stating a proposition (“if–then”)
- Asserting a practice rule
- Making choices (alternative actions)
- Judging the value
- Drawing conclusions
- Providing explanations
Fonteyn further identified other, less prominent thinking strategies the nurse might use:
- Posing a question
- Making assumptions (supposing)
- Making generalizations
These thought processes are consistent with the characteristics of critical thinking and cognitive activities discussed earlier. Fonteyn asserted that exploring how these thinking strategies are used in various clinical situations, and practicing using the strategies, might assist the nurse–learner in examining and refining his or her own thinking skills.
Throughout the critical thinking process, a continuous flow of questions evolves in the thinker’s mind. Although the questions will vary according to the particular clinical situation, certain general inquiries can serve as a basis for reaching conclusions and determining a course of action. When faced with a patient situation, it is often helpful to seek answers to some or all of the following questions in an attempt to determine those actions that are most appropriate:
- What relevant assessment information do I need, and how do I interpret this information? What does this information tell me?
- To what problems does this information point? Have I identified the most important ones? Does the information point to any other problems that I should consider?
- Have I gathered all the information I need (signs/symptoms, laboratory values, medication history, emotional factors, mental status)? Is anything missing?
- Is there anything that needs to be reported immediately? Do I need to seek additional assistance?
- Does this patient have any special risk factors? Which ones are most significant? What must I do to minimize these risks?
- What possible complications must I anticipate?
- What are the most important problems in this situation? Do the patient and the patient’s family recognize the same problems?
- What are the desired outcomes for this patient? Which have the highest priority? Does the patient see eye to eye with me on these points?
- What is going to be my first action in this situation? How can I construct a plan of care to achieve the goals?
- Are there any age-related factors involved, and will they require some special approach? Will I need to make some change in the plan of care to take these factors into account?
- How do the family dynamics affect this situation, and will this have an affect on my actions or the plan of care?
- Are there cultural factors that I must address and consider?
- Am I dealing with an ethical problem here? If so, how am I going to resolve it?
- Has any nursing research been conducted on this subject?
Related Posts
Historical evolution of nursing, loss and grief, leavell and clark’s three levels of prevention.

Clinical Reasoning In Nursing (Explained W/ Example)

Last updated on August 19th, 2023
In this article, we will cover:
What is Clinical Reasoning?
Definition of clinical reasoning in nursing.
- What is the concept of clinical reasoning?
Why is Clinical Reasoning Important in Nursing?
What are the types of clinical reasoning, what are the three elements of clinical reasoning, what are the steps of clinical reasoning, what is the importance of clinical reasoning and judgement in nursing, what is the difference between critical thinking and clinical reasoning, clinical reasoning in nursing example.
Clinical reasoning refers to the cognitive process that healthcare professionals, such as doctors, nurses, and other clinicians, use to analyze and make decisions about a patient’s condition and appropriate treatment.
It’s a complex and dynamic process that involves gathering and interpreting information from various sources, including patient history, physical examinations, laboratory tests, imaging studies, and the clinician’s own experience and knowledge.
Medicine, physical therapy, and occupational therapy were the first to introduce clinical reasoning to the healthcare disciplines. Since then, the nursing profession has used these strategies to improve patient care.
What is Clinical Reasoning in Nursing?
Clinical reasoning in nursing is dynamic and adaptive, as nurses continuously gather new information and adjust care plans based on patient responses.
It’s a crucial skill that guides nurses in providing safe, effective, and patient-centered care. Clinical reasoning involves the integration of clinical knowledge, critical thinking , and experience to address the complex and dynamic nature of patient situations.
It involves balancing medical knowledge with critical thinking , empathy, and ethical considerations to provide comprehensive and compassionate patient care.
Clinical reasoning in nursing refers to the cognitive process that nurses use to collect and assess patient information, analyze data, make informed judgments, and develop appropriate care plans.
What is the Concept of Clinical Reasoning?
Clinical reasoning is the cognitive process used by healthcare professionals to make informed decisions regarding patient care.
It encompasses tasks such as collecting information, analyzing data, identifying patterns, generating hypotheses, and making judgments for diagnosis and treatment.
Clinical reasoning blends science and intuition in medical practice. It combines evidence-based knowledge with experience-derived judgment to attain accurate diagnoses and treatments while addressing uncertainties.
As an essential component of clinical practice, clinical reasoning guides healthcare providers in delivering safe and effective patient care.
Clinical reasoning is important in nursing for several reasons. Some reasons are listed below.
Patient-Centered Care:
Clinical reasoning helps nurses tailor care plans to individual patients, considering their unique needs, preferences, and circumstances, leading to more personalized and effective care.
Safe and Effective Care:
It ensures that nurses make well-informed decisions based on thorough assessments, reducing the risk of errors and promoting patient safety.
Optimal Outcomes:
Through clinical reasoning, nurses can identify early signs of complications, make timely interventions, and contribute to better patient outcomes.
Nurtured Critical Thinking:
Clinical reasoning cultivates nurses’ critical thinking abilities, empowering them to dissect complex situations, appraise evidence, and make rational choices.
Efficient Resource Utilization:
It helps nurses prioritize care tasks, allocate resources effectively, and manage time efficiently, enhancing workflow and patient care delivery.
Evidence-Based Practice:
Nursing practice is constantly evolving with new research and evidence. Clinical reasoning involves integrating the latest evidence-based knowledge into decision-making, ensuring that care plans are aligned with the best available practices.
Complex Cases:
Nurses often encounter intricate patient cases; clinical reasoning equips them to navigate complexity, address multiple issues, and make comprehensive care plans.
Interdisciplinary Collaboration:
Effective clinical reasoning supports collaboration with other healthcare professionals, promoting well-rounded patient care.
Adaptation to Change:
In rapidly changing healthcare environments, clinical reasoning enables nurses to adapt to new information, technologies, and practices.
Critical Decision-Making:
Nurses face complex situations where quick and accurate decisions are critical. Clinical reasoning equips them with the ability to analyze data, identify patterns, and generate hypotheses. This enables nurses to make informed decisions about interventions, medications, and treatments, leading to effective care.
Early Detection and Prevention:
Through clinical reasoning, nurses can detect subtle changes in a patient’s condition that might signal complications or deterioration. This allows for early interventions, preventing potential health crises and improving patient prognosis.
Error Reduction:
Clinical reasoning encourages systematic thinking, reducing the likelihood of errors in administering medications, performing procedures, and assessing patients. This promotes patient safety and prevents adverse events.
Holistic Care:
Patient’s health is influenced by various factors beyond just medical conditions. Clinical reasoning enables nurses to consider the social, emotional, and psychological aspects of patients, promoting holistic care and overall well-being.
Ethical Dilemmas:
Nursing often involves ethical challenges. Clinical reasoning guides nurses in making ethically sound decisions by considering patients’ autonomy, values, and cultural beliefs.
Communication and Collaboration:
Clinical reasoning enhances nurses’ ability to communicate effectively with patients, families, and other healthcare professionals. It fosters collaboration by enabling nurses to articulate their assessments, interventions, and rationales clearly.
Professional Growth:
Developing strong clinical reasoning skills enhances nurses’ professional growth. It increases their confidence, competence, and ability to take on more complex patient cases and leadership roles.
In summary , clinical reasoning is an important component of nursing practice, allowing nurses to provide safe, effective, and patient-centered care.
It enables nurses to make informed decisions, improve patient outcomes, and navigate the dynamic and complex healthcare setting.
Clinical reasoning involves three key elements that healthcare professionals integrate to make informed decisions about patient care:
1. Patient Information:
This element encompasses all the relevant data about the patient’s medical history, current condition, symptoms, physical examination findings, diagnostic test results, and social and contextual factors.
Gathering comprehensive and accurate patient information is essential for forming an accurate understanding of the patient’s health status and needs.
2. Clinical Knowledge and Expertise:
Healthcare professionals draw upon their extensive medical knowledge, clinical experience, and expertise to interpret patient information.
This knowledge includes an understanding of anatomy, physiology, pathophysiology, pharmacology, and medical guidelines.
Clinical expertise is built over years of practice, exposure to a variety of cases, and ongoing learning.
3. Critical Thinking and Decision-Making Skills:
Critical thinking involves the analytical and logical thought processes that healthcare professionals use to evaluate patient information in the context of their clinical knowledge.
It includes the ability to identify patterns, assess potential diagnoses, consider alternative explanations, and weigh the pros and cons of different treatment options.
Effective decision-making is the outcome of critical thinking , as healthcare professionals choose the most appropriate course of action based on the available information.
These three elements are interdependent and work together to form the foundation of clinical reasoning.
Healthcare professionals integrate patient information with their clinical knowledge and expertise while applying critical thinking skills to reach accurate diagnoses, develop effective treatment plans, and provide high-quality patient care.
The balance between these elements varies based on the complexity of the clinical situation and the healthcare provider’s level of experience and expertise.
8 Stages of the Clinical Reasoning Cycle
Clinical reasoning involves several key steps:
1. Data Collection: Gathering relevant information about the patient’s medical history, symptoms, physical examination findings, and any diagnostic tests that have been conducted.
2. Pattern Recognition: Recognizing patterns and relationships in the collected data to identify potential diagnoses or issues. This involves comparing the patient’s presentation to previous cases and medical knowledge.
3. Hypothesis Generation: Formulating hypotheses or possible explanations for the patient’s condition based on the patterns and information observed. This step often involves generating a list of potential diagnoses that fit the available evidence.
4. Differential Diagnosis: Narrowing down the list of potential diagnoses by considering the likelihood of each condition and ruling out less likely options. This is where critical thinking and medical knowledge come into play.
5. Testing and Validation: Ordering further diagnostic tests or investigations to confirm or rule out specific diagnoses. This could include blood tests, imaging studies, biopsies, or other procedures.
6. Synthesis: Integrating the results of diagnostic tests and additional information to refine the diagnosis and treatment plan. This may involve adjusting the initial hypotheses based on new data.
7. Treatment Planning: Developing a comprehensive treatment plan that addresses the diagnosed condition, the patient’s unique circumstances, preferences, and any potential risks or benefits of various treatment options.
8. Monitoring and Adaptation: Continuously monitoring the patient’s progress and adjusting the treatment plan as needed based on how the patient responds and any new information that emerges.
Clinical reasoning requires a deep understanding of medical science, anatomy, physiology, and pathology, as well as the ability to apply this knowledge to real-world clinical scenarios.
It also involves critical thinking skills , logical reasoning, and the ability to handle uncertainty, as medical situations can be complex and patients may present with atypical symptoms.
Overall, clinical reasoning is a crucial skill for healthcare professionals, as it forms the foundation for making accurate diagnoses and providing effective patient care.
Clinical reasoning and judgment are of paramount importance in nursing for several reasons:
- Accurate Diagnosis and Treatment: Effective clinical reasoning enables nurses to accurately assess patients’ conditions, identify potential problems, and make informed decisions about appropriate interventions and treatments. Accurate diagnosis and treatment are crucial for improving patient outcomes and preventing complications.
- Patient Safety: Sound clinical judgment helps nurses recognize potential risks and make timely interventions to ensure patient safety. By identifying early signs of deterioration or complications, nurses can take appropriate actions to prevent adverse events.
- Individualized Care: Clinical reasoning allows nurses to tailor care plans to each patient’s unique needs, preferences, and circumstances. This patient-centered approach improves patient satisfaction and contributes to better treatment outcomes.
- Early Detection of Changes: Nurses often spend the most time with patients, which puts them in a prime position to notice subtle changes in a patient’s condition. Strong clinical reasoning skills enable nurses to detect these changes early and respond appropriately.
- Effective Communication: Nurses with strong clinical reasoning skills can communicate more effectively with patients, families, and interdisciplinary healthcare teams. They can convey complex medical information, treatment plans, and concerns in a clear and organized manner.
- Ethical Decision-Making: Clinical reasoning includes ethical considerations in decision-making. Nurses must weigh the ethical implications of their actions and decisions, especially when faced with complex situations that involve moral dilemmas.
- Resource Utilization: Effective clinical reasoning helps nurses allocate resources efficiently. By accurately assessing patient needs and prioritizing care, nurses can optimize the use of time, personnel, and equipment.
- Adaptation to Change: Healthcare is dynamic, and patients’ conditions can change rapidly. Nurses with strong clinical reasoning skills can adapt quickly to changing situations, making necessary adjustments to care plans and interventions.
- Continuity of Care: Nurses often play a critical role in ensuring continuity of care as patients transition between different healthcare settings. Effective clinical reasoning facilitates clear communication of patient information and ensures a smooth transition of care.
- Professional Growth: Developing clinical reasoning and judgment skills enhances a nurse’s professional growth. These skills are transferrable and applicable across various healthcare settings, allowing nurses to provide high-quality care regardless of the environment.
- Confidence and Job Satisfaction: Nurses who feel confident in their clinical reasoning abilities experience greater job satisfaction. Confidence comes from knowing that decisions are based on a solid foundation of knowledge, experience, and critical thinking.
- Advocacy: Nurses with strong clinical reasoning skills can effectively advocate for their patients, ensuring that their needs are met, their voices are heard, and their rights are respected within the healthcare system.
- Quality Improvement: Clinical reasoning plays a role in quality improvement efforts by identifying areas for improvement in patient care processes and outcomes.
In summary, clinical reasoning and judgment are essential for nurses to provide safe, effective, and patient-centered care.
These skills underpin the entire nursing process, enabling nurses to make informed decisions, communicate effectively, and positively impact patient outcomes and experiences.
Critical Thinking :
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information, ideas, and arguments to make reasoned judgments and decisions.
It is a broader skill applicable to various aspects of life and professions, encouraging logical, evidence-based thinking and minimizing biases.
Critical thinking aims to enhance problem-solving, decision-making, and analytical abilities in a wide range of contexts beyond healthcare.
Clinical Reasoning:
Clinical reasoning, on the other hand, is a specialized form of critical thinking that is primarily focused on healthcare and clinical situations.
It specifically pertains to the cognitive process healthcare professionals, especially nurses and doctors, use to collect, assess, analyze, and apply information to make informed clinical judgments and decisions.
Clinical reasoning is crucial for providing safe and effective patient care, as it integrates medical knowledge, patient assessments, ethical considerations, and treatment planning.
Critical Thinking vs. Clinical Reasoning
| The ability to analyze, evaluate, and synthesize information, ideas, and arguments to make reasoned judgments and decisions. | The cognitive process of collecting, assessing, analyzing, and applying information to make informed clinical judgments and decisions. | |
| Broadly applicable to various aspects of life and professions. | Primarily focused on healthcare and clinical situations. | |
| Applied to diverse contexts and disciplines. | Applied specifically to patient care scenarios, diagnostics, and treatment planning in healthcare. | |
| Applies beyond the clinical setting. | Primarily relevant within the healthcare context. | |
| Enhances general problem-solving, decision-making, and analytical skills. | Supports safe and effective patient care by integrating medical knowledge, assessments, and ethical considerations. | |
| Can be developed and honed through practice, reflection, and exposure to various ideas. | Developed through clinical experience, education, and applying knowledge to actual patient cases. | |
| Evaluating the credibility of news sources, identifying fallacies in arguments, and analyzing the pros and cons of an issue. | Diagnosing a patient’s condition based on symptom presentation, medical history, and diagnostic tests. | |
| Encourages logical, evidence-based thinking, minimizing bias, and informed decision-making. | Leads to appropriate and well-informed interventions, improved patient outcomes, and enhanced patient safety. |
Clinical reasoning can be categorized into different types or approaches. Each of which represents a particular way of thinking and making decisions in clinical practice.
Some of the commonly recognized types of clinical reasoning include:
- Deductive Reasoning: This type of reasoning starts with a general principle or theory and applies it to a specific case. Healthcare professionals use deductive reasoning to make predictions or decisions based on established medical knowledge. For example, if a patient presents with a set of symptoms consistent with a well-known disease, the clinician may deduce that the patient likely has that disease.
- Inductive Reasoning: In contrast to deductive reasoning, inductive reasoning involves making generalizations or conclusions based on specific observations or cases. Clinicians use inductive reasoning to form hypotheses or theories from individual patient experiences. For instance, a nurse may notice a pattern of symptoms in several patients and develop a hypothesis about a potential new condition.
- Abductive Reasoning: Abductive reasoning combines elements of both deductive and inductive reasoning. It involves making educated guesses or hypotheses to explain observations or data that don’t fit neatly into established patterns. Clinicians use abductive reasoning when they encounter cases that don’t seem to fit existing diagnoses or models, and they generate plausible explanations to guide further investigation.
- Analytical Reasoning: This type of reasoning involves systematically breaking down a complex situation or problem into smaller parts to understand its components and relationships. Healthcare professionals use analytical reasoning to dissect complex patient cases, focusing on details and relationships to arrive at a diagnosis or treatment plan.
- Intuitive Reasoning: Intuitive reasoning relies on a healthcare professional’s experience, intuition, and gut feeling. It involves drawing on one’s own clinical experience and recognizing patterns that may not be immediately apparent. Intuitive reasoning is often employed in situations where rapid decision-making is necessary.
- Procedural Reasoning: Procedural reasoning focuses on the steps or processes needed to manage a clinical situation. It involves thinking about the sequence of actions required to address a patient’s needs. For example, a nurse may use procedural reasoning when administering medications, performing wound care, or carrying out other routine clinical procedures.
- Narrative Reasoning: Narrative reasoning involves considering the patient’s story, values, and context as essential components of clinical decision-making. It emphasizes understanding the patient’s perspective and tailoring care plans to the individual’s unique circumstances.
- Hypothetico-Deductive Reasoning: This approach involves generating and testing hypotheses systematically to arrive at a diagnosis. Healthcare professionals consider various possible diagnoses, then order specific tests to confirm or rule out each hypothesis.
- Pattern Recognition Reasoning: This type of reasoning relies on recognizing familiar patterns based on clinical experience and knowledge. Healthcare providers quickly identify common clinical presentations and apply established treatment protocols.
Emily Davis, a 68-year-old woman, is admitted to the medical unit with a diagnosis of Acute Exacerbation of COPD. She has a history of chronic obstructive pulmonary disease (COPD) and has been experiencing increased shortness of breath, cough, and decreased oxygen saturation levels.
How does your understanding of nursing fundamentals influence your clinical reasoning?
Nursing Action:
• Reflect on the nursing care provided to patients with COPD and respiratory distress.
• Review the pharmacologic treatments that will improve the patient’s COPD.
• Reflect the non-pharmacologic measures that will help to improve the patient’s respiratory distress.
• Determine the most appropriate assessments and interventions for managing respiratory distress in patients with COPD.
Implementation of Interventions:
• Assess Emily’s respiratory rate, depth, and effort, as well as oxygen saturation levels.
• Administer prescribed bronchodilators, and nebulization to improve airway patency.
• Elevate the head of the bed to promote better lung expansion.
• Encourage deep breathing exercises and effective coughing techniques.
• Consult with the physician to determine pharmacologic therapy
• Monitor Emily’s response to interventions and adjust care as needed. How does your understanding of pathophysiology guide your clinical reasoning?
• Knowledge of COPD’s pathophysiology helps anticipate complications and tailor interventions.
In this scenario, the nurse’s grasp of nursing fundamentals enables them to provide appropriate care for a patient with COPD.
By considering the patient’s history and symptoms, the nurse takes action to manage respiratory distress.
Implementing interventions such as bronchodilators and elevation of the head of the bed aligns with nursing knowledge.
Additionally, understanding the pathophysiology of COPD aids in predicting potential complications and choosing interventions to support the patient’s respiratory function.
- What is Critical Thinking in Nursing? (Explained W/ Examples)
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What Are Socratic Questions?
- What is the “5 Whys” Technique?
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
Clinical reasoning in nursing involves the skillful integration of medical knowledge, critical thinking , and patient assessment to make informed decisions about patient care.
It enables nurses to provide safe, effective, and patient-centered interventions while considering individual needs and complex healthcare situations.
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Nursing care plans versus concept maps in the enhancement of critical thinking skills in nursing students enrolled in a baccalaureate nursing program
Affiliation.
- 1 D'Youville College in Buffalo, New York, USA. [email protected]
- PMID: 22856062
- DOI: 10.1891/1078-4535.18.2.78
Appropriate and effective critical thinking and problem solving is necessary for all nurses in order to make complex decisions that improve patient outcomes, safety, and quality of nursing care. With the current emphasis on quality improvement, critical thinking ability is a noteworthy concern within the nursing profession. An in-depth review of literature related to critical thinking was performed. The use of nursing care plans and concept mapping to improve critical thinking skills was among the recommendations identified. This study compares the use of nursing care plans and concept mapping as a teaching strategy for the enhancement of critical thinking skills in baccalaureate level nursing students. The California Critical Thinking Skills Test was used as a method of comparison and evaluation. Results indicate that concept mapping enhances critical thinking skills in baccalaureate nursing students.
PubMed Disclaimer
Similar articles
- The influence of concept mapping on critical thinking in baccalaureate nursing students. Wheeler LA, Collins SK. Wheeler LA, et al. J Prof Nurs. 2003 Nov-Dec;19(6):339-46. doi: 10.1016/s8755-7223(03)00134-0. J Prof Nurs. 2003. PMID: 14689390 Clinical Trial.
- Critical thinking dispositions and skills of senior nursing students in associate, baccalaureate, and RN-to-BSN programs. Shin K, Jung DY, Shin S, Kim MS. Shin K, et al. J Nurs Educ. 2006 Jun;45(6):233-7. doi: 10.3928/01484834-20060601-08. J Nurs Educ. 2006. PMID: 16780012
- Concept maps as an assessment tool in a nursing course. Hsu L, Hsieh SI. Hsu L, et al. J Prof Nurs. 2005 May-Jun;21(3):141-9. doi: 10.1016/j.profnurs.2005.04.006. J Prof Nurs. 2005. PMID: 16021557
- Using a conceptual approach with concept mapping to promote critical thinking. Vacek JE. Vacek JE. J Nurs Educ. 2009 Jan;48(1):45-8. doi: 10.3928/01484834-20090101-11. J Nurs Educ. 2009. PMID: 19227756 Review.
- Concept mapping: an effective, active teaching-learning method. Clayton LH. Clayton LH. Nurs Educ Perspect. 2006 Jul-Aug;27(4):197-203. Nurs Educ Perspect. 2006. PMID: 16921805 Review.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ingenta plc
- Ovid Technologies, Inc.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)
- PMC10779280

Teaching Strategies for Developing Clinical Reasoning Skills in Nursing Students: A Systematic Review of Randomised Controlled Trials
Associated data.
Data are contained within the article.
Background: Clinical reasoning (CR) is a holistic and recursive cognitive process. It allows nursing students to accurately perceive patients’ situations and choose the best course of action among the available alternatives. This study aimed to identify the randomised controlled trials studies in the literature that concern clinical reasoning in the context of nursing students. Methods: A comprehensive search of PubMed, Scopus, Embase, and the Cochrane Controlled Register of Trials (CENTRAL) was performed to identify relevant studies published up to October 2023. The following inclusion criteria were examined: (a) clinical reasoning, clinical judgment, and critical thinking in nursing students as a primary study aim; (b) articles published for the last eleven years; (c) research conducted between January 2012 and September 2023; (d) articles published only in English and Spanish; and (e) Randomised Clinical Trials. The Critical Appraisal Skills Programme tool was utilised to appraise all included studies. Results: Fifteen papers were analysed. Based on the teaching strategies used in the articles, two groups have been identified: simulation methods and learning programs. The studies focus on comparing different teaching methodologies. Conclusions: This systematic review has detected different approaches to help nursing students improve their reasoning and decision-making skills. The use of mobile apps, digital simulations, and learning games has a positive impact on the clinical reasoning abilities of nursing students and their motivation. Incorporating new technologies into problem-solving-based learning and decision-making can also enhance nursing students’ reasoning skills. Nursing schools should evaluate their current methods and consider integrating or modifying new technologies and methodologies that can help enhance students’ learning and improve their clinical reasoning and cognitive skills.
1. Introduction
Clinical reasoning (CR) is a holistic cognitive process. It allows nursing students to accurately perceive patients’ situations and choose the best course of action among the available alternatives. This process is consistent, dynamic, and flexible, and it helps nursing students gain awareness and put their learning into perspective [ 1 ]. CR is an essential competence for nurses’ professional practice. It is considered crucial that its development begin during basic training [ 2 ]. Analysing clinical data, determining priorities, developing plans, and interpreting results are primary skills in clinical reasoning during clinical nursing practise [ 3 ]. To develop these skills, nursing students must participate in caring for patients and working in teams during clinical experiences. Among clinical reasoning skills, we can identify communication skills as necessary for connecting with patients, conducting health interviews, engaging in shared decision-making, eliciting patients’ concerns and expectations, discussing clinical cases with colleagues and supervisors, and explaining one’s reasoning to others [ 4 ].
Educating students in nursing practise to ensure high-quality learning and safe clinical practise is a constant challenge [ 5 ]. Facilitating the development of reasoning is challenging for educators due to its complexity and multifaceted nature [ 6 ], but it is necessary because clinical reasoning must be embedded throughout the nursing curriculum [ 7 ]. Such being the case, the development of clinical reasoning is encouraged, aiming to promote better performance in indispensable skills, decision-making, quality, and safety when assisting patients [ 8 ].
Nursing education is targeted at recognising clinical signs and symptoms, accurately assessing the patient, appropriately intervening, and evaluating the effectiveness of interventions. All these clinical processes require clinical reasoning, and it takes time to develop [ 9 ]. This is a significant goal of nursing education [ 10 ] in contemporary teaching and learning approaches [ 6 ].
Strategies to mitigate errors, promote knowledge acquisition, and develop clinical reasoning should be adopted in the training of health professionals. According to the literature, different methods and teaching strategies can be applied during nursing training, as well as traditional teaching through lectures. However, the literature explains that this type of methodology cannot enhance students’ clinical reasoning alone. Therefore, nursing educators are tasked with looking for other methodologies that improve students’ clinical reasoning [ 11 ], such as clinical simulation. Clinical simulation offers a secure and controlled setting to encounter and contemplate clinical scenarios, establish relationships, gather information, and exercise autonomy in decision-making and problem-solving [ 12 ]. Different teaching strategies have been developed in clinical simulation, like games or case studies. Research indicates a positive correlation between the use of simulation to improve learning outcomes and how it positively influences the development of students’ clinical reasoning skills [ 13 ].
The students of the 21st century utilise information and communication technologies. With their technological skills, organisations can enhance their productivity and achieve their goals more efficiently. Serious games are simulations that use technology to provide nursing students with a safe and realistic environment to practise clinical reasoning and decision-making skills [ 14 ] and can foster the development of clinical reasoning through an engaging and motivating experience [ 15 ].
New graduate nurses must possess the reasoning skills required to handle complex patient situations. Aware that there are different teaching methodologies, with this systematic review we intend to discover which RCTs published focus on CR in nursing students, which interventions have been developed, and their effectiveness, both at the level of knowledge and in increasing clinical reasoning skills. By identifying the different techniques used during the interventions with nursing students in recent years and their effectiveness, it will help universities decide which type of methodology to implement to improve the reasoning skills of nursing students and, therefore, obtain better healthcare results.
This study aims to identify and analyse randomised controlled trials concerning clinical reasoning in nursing students. The following questions guide this literature review:
Which randomised controlled trials have been conducted in the last eleven years regarding nursing students’ clinical reasoning? What are the purposes of the identified RCTs? Which teaching methodologies or strategies were used in the RCTs studies? What were the outcomes of the teaching strategies used in the RCTs?
2. Materials and Methods
This review follows the PRISMA 2020 model statement for systematic reviews. That comprises three documents: the 27-item checklist, the PRISMA 2020 abstract checklist, and the revised flow diagram [ 16 ].
2.1. Search Strategy
A systematic literature review was conducted on PubMed, Scopus, Embase, and the Cochrane Controlled Register of Trials (CENTRAL) up to 15th October 2023.
The PICOS methodology guided the bibliographic search [ 17 ]: “P” being the population (nursing students), “I” the intervention (clinical reasoning), “C” comparison (traditional teaching), “O” outcome (dimension, context, and attributes of clinical reasoning in the students’ competences and the results of the teaching method on nursing students), and “S” study type (RCTs).
The search strategy used in each database was the following: (“nursing students” OR “nursing students” OR “pupil nurses” OR “undergraduate nursing”) AND (“clinical reasoning” OR “critical thinking” OR “clinical judgment”). The filters applied were full text, randomised controlled trial, English, Spanish, and from 1 January 2012 to 15 October 2023. The search strategy was performed using the same process for each database. APP performed the search, and AZ supervised the process.
During the search, the terms clinical reasoning, critical thinking, and clinical judgement were used interchangeably since clinical judgement is part of clinical reasoning and is defined by the decision to act. It is influenced by an individual’s previous experiences and clinical reasoning skills [ 18 ]. Critical thinking and clinical judgement involve reflective and logical thinking skills and play a vital role in the decision-making and problem-solving processes [ 19 ].
The first search was conducted between March and September 2022, and an additional search was conducted during October 2023, adding the new articles published between September 2022 and September 2023, following the same strategy. The search strategy was developed using words from article titles, abstracts, and index terms. Parallel to this process, the PRISMA protocol was used to systematise the collection of all the information presented in each selected article. This systematic review protocol was registered in the international register PROSPERO: CRD42022372240.
2.2. Eligibility Criteria and Study Selection
The following inclusion criteria were examined: (a) clinical reasoning, clinical judgment, and critical thinking in nursing students as a primary aim; (b) articles published in the last eleven years; (c) research conducted between January 2012 and September 2023; (d) articles published only in English and Spanish; and (e) RCTs. On the other hand, the exclusion criteria were studies conducted with students from other disciplines other than nursing, not random studies or review articles.
2.3. Data Collection and Extraction
After this study selection, the following information was extracted from each article: bibliographic information, study aims, teaching methodology, sample size and characteristics, time of intervention, and conclusions.
2.4. Risk of Bias
The two reviewers, APP and AZ, worked independently to minimise bias and mistakes. The titles and abstracts of all papers were screened for inclusion. All potential articles underwent a two-stage screening process based on the inclusion criteria. All citations were screened based on title, abstract, and text. Reviewers discussed the results to resolve minor discrepancies. All uncertain citations were included for full-text review. The full text of each included citation was obtained. Each study was read thoroughly and assessed for inclusion following the inclusion and exclusion criteria explained in the methodology. The CASP tool was utilised to appraise all included studies. The CASP Randomized Controlled Trial Standard Checklist is an 11-question checklist [ 20 ], and the components assessed included the appropriateness of the objective and aims, methodology, study design, sampling method, data collection, reflexivity of the researchers, ethical considerations, data analysis, rigour of findings, and significance of this research. These items of the studies were then rated (“Yes” = with three points; “Cannot tell” = with two points; “No” = with one point). The possible rates for every article were between 0 and 39 points.
2.5. Ethical Considerations
Since this study was a comprehensive, systematic review of the existing published literature, there was no need for us to seek ethical approval.
3.1. Search Results
The initial search identified 158 articles using the above-mentioned strategy (SCOPUS ® n = 72, PUBMED ® n = 56, CENTRAL ® n = 23, and EMBASE ® n= 7), and the results are presented in Figure 1 . After retrieving the articles and excluding 111, 47 were selected for a full reading. Finally, 17 articles were selected. To comply with the methodology, the independent reviewers analysed all the selected articles one more time after the additional search, and they agreed to eliminate two of them because this study sample included nursing students as well as professional nurses. Therefore, to have a clear outcome focused on nursing students, two articles were removed, and the very final sample size was fifteen articles, following the established selection criteria ( Figure 1 ). The reasons for excluding studies from the systematic review were: nurses as targets; other design types of studies different from RCTs; focusing on other health professionals such as medical students; review studies; and being published in full text in other languages other than Spanish or English.

Flowchart of screening of clinical reasoning RCTs that underwent review.
3.2. Risk of Bias in CASP Results
All studies included in the review were screened with the CASP tool. Each study was scored out of a maximum of 39 points, showing the high quality of the randomised control trial methodology. The studies included had an average score of 33.1, ranging from 30 to 36 points. In addition, this quantitative rate of the items based on CASP, there were 13 studies that missed an item in relation to assessing/analysing outcome/s ‘blinded or not’ or not, and 11 studies that missed the item whether the benefits of the experimental intervention outweigh the harms and costs.
3.3. Data Extraction
Once the articles had undergone a full reading and the inclusion criteria were applied, data extraction was performed with a data extraction table ( Appendix A ). Their contents were summarised into six different cells: (1) CASP total points result, (2) purpose of this study, (3) teaching strategy, (4) time of intervention, (5) sample size, and (6) author and year of publication. After the review by the article’s readers, fifteen RCTs were selected. Of the fifteen, the continent with the highest number of studies was Asia, with 53.33% of the studies (n = 8) (Korea n = 4, Taiwan n = 2, and China n = 2), followed by Europe with 26.66% (n = 4) (Turkey n = 2, Paris n = 1, and Norway n = 1), and lastly South America with 20% (n = 3), all of them from Brazil.
3.4. Teaching Strategies
Different teaching strategies have been identified in the reviewed studies: simulation methods (seven articles) and learning programmes (eight articles). There are also two studies that focus on comparing different teaching methodologies.
3.4.1. Clinical Simulation
The simulation methods focused on in the studies were virtual simulation (based on mobile applications), simulation games, and high-fidelity clinical simulation. Of the total number of nursing students in the studies referring to clinical simulations, 43.85% were in their second year, while 57.1% were senior-year students. The most used method in the clinical simulation group was virtual simulation, and 57.14% of studies included only one-day teaching interventions.
Virtual simulations were used to increase knowledge about medication administration and nasotracheal suctioning in different scenarios [ 21 ], to evaluate the effect of interactive nursing skills, knowledge, and self-efficacy [ 11 ], and to detect patient deterioration in two different cases [ 22 ]. Simulation game methodology was used to improve nursing students’ cognitive and attention skills, strengthen judgment, time management, and decision-making [ 14 ].
Clinical simulation was used to develop nursing students’ clinical reasoning in evaluating wounds and their treatments [ 12 ], to evaluate and compare the perception of stressors, with the goal of determining whether simulations promote students’ self-evaluation and critical-thinking skills [ 23 ], and also to evaluate the impact of multiple simulations on students’ self-reported clinical decision-making skills and self-confidence [ 24 ].
3.4.2. Learning Programs
Different types of learning programmes have been identified in this systematic review: team-based learning, reflective training programs, person-centred educational programmes, ethical reasoning programmes, case-based learning, mapping, training problem-solving skills, and self-instructional guides. Of the total number of nursing students in the studies referring to learning programs, 57.1% were junior-year students, while 43.85% were in their senior year.
Team-based learning is a learner-centred educational strategy that promotes active learning to improve students’ problem-solving, knowledge, and practise performance. It can be implemented in small or large groups divided into teams with an instructor and reading material based on case scenarios [ 25 ]. Reflective training is based on a new mentoring practise to explore, think about, and solve problems actively during an internship. During the reflective training program, the mentors lead students to uncover clinical nursing problems through conversations with them and discussing feedback for their professional portfolios [ 26 ]. The person-centred educational programme focuses on how nursing students perceive individualised care, using design thinking to improve their perception. The use of design thinking gave the students opportunities to apply their theoretical knowledge of the person-centred program to plan innovative solutions that may effectively resolve real-life situations [ 27 ]. Another educational programme identified is the ethical reasoning program, and the aim of this is to improve nursing students’ handling of ethical decision-making situations [ 28 ], engaging the students in complex ethical clinical situations based on real cases.
Case-based learning was used to explore and demonstrate the feasibility of implementing unfolding cases in lectures to develop students’ critical-thinking abilities [ 29 ]. The web-based concept mapping of nursing students was also investigated to determine its impact on critical-thinking skills [ 30 ]. Training problem-solving skills were used to find out how it affected the rate of self-handicapping among nursing students [ 31 ]. And the last article evaluated the effect of the self-instructional guide to improve clinical reasoning skills on diagnostic accuracy in undergraduate nursing students [ 32 ].
4. Discussion
Although 158 studies were initially identified, only 15 articles were finally included in this review. The excluded articles were mainly from other disciplines other than nursing and used a less rigorous study design than RCT.
The three longest interventions were developed in Asia [ 26 , 28 , 29 ]. The longest was 300 h in duration, through one year [ 30 ]. These interventions were based on learning programs, case-based learning, person-centred care (PCC), and reflective training programs. However, it is important to take into account that Asian nursing curriculum programmes are different from European or United States curriculum because their internship is carried out only during the last academic degree year, while in Europe, following the European directive 2005/36/CE, 2013/55/UE nursing education requirements of 4600 h (2300 h of clinical practice) is carried out along the 3–4 years of the academic degree [ 33 ]. On the other hand, the intervention with the biggest sample was 419 nursing students [ 30 ], 210 in the experimental group, and 209 in the control group, and the one with the lowest sample was 51, with 24 students in the control group and 27 in the intervention group [ 32 ]. Therefore, all the included studies had a good sample size.
This systematic review has detected different methodologies to help nursing students improve their reasoning and decision-making skills. Virtual simulation was the most frequently used teaching method, both as a mobile application and as a serious game. In terms of its effectiveness in a study carried out in Taiwan, the use of a mobile application resulted in significantly higher knowledge scores, better skill performance, and higher satisfaction in students than traditional paper materials [ 21 ]. Virtual simulation [ 11 , 14 , 21 ] has also proven to be an effective tool for enhancing knowledge and confidence in recognising and responding to rapidly deteriorating patients, but studies that combined two educational strategies were more effective [ 29 ], like clinical simulation combined with another teaching strategy such as lectures or videos [ 12 ].
An interactive learner-centred nursing education mobile application with systematic contents effectively allowed students to experience positive practical nursing skills [ 11 ]. However, in a study comparing serious game simulation versus traditional teaching methods, no significant difference was found immediately or in the month following the training [ 22 ], but serious games can improve nursing students’ cognitive skills to detect patient deterioration and to make safe decisions about patient care [ 14 ]. Although the innovative teaching method was well received by the students, who expressed higher levels of satisfaction and motivation [ 22 ]. We can affirm that the development of a mobile application and its application can be effectively used by nursing students at all levels [ 11 ]. However, the performance of all these studies was measured on its short-term outcomes, only 40 min [ 21 ], 2 h [ 22 ], and 1 week [ 11 , 14 ] of intervention, and was performed with a mean sample size of 97 nursing students.
The data obtained in a study developed in Brazil [ 12 ] confirm that clinical simulation is effective for the development of nursing students’ clinical reasoning in wound evaluation and treatment and that clinical simulation in conjunction with other educational methods promotes the acquisition of knowledge by facilitating the transition from what the student knows to rational action. Moreover, the high-fidelity simulation strategy increases the perception of stressors related to a lack of competence and interpersonal relationships with patients, multidisciplinary teams, and colleagues compared with the conventional practice class in the skill laboratory. This increase was related to the students’ capacity for self-evaluation and critical reflection, concerning their learning responsibility and the need to acquire the required skills for patient care [ 23 ]. However, in the case of the effect of multiple simulations on students, there are no differences found between the double-versus single-scenario simulations [ 24 ]. The intervention time in these three studies was 30 min [ 23 ], 3.5 h [ 12 ], and 4 days [ 24 ]; then the time used to implement the intervention can determine the results obtained.
The different learning methods have an impact on various learning outcomes and students’ variables. Team-based learning [ 25 ], reflective training [ 26 ], the person-centred education programme [ 27 ], web-based concept mapping [ 30 ], and teaching cognitive-behavioural approaches [ 31 ] have proven to be effective in enhancing problem-solving abilities, knowledge, and reasoning processes and consequently improving the quality of nursing practical education. Team-based learning increased problem-solving ability scores significantly, while those in the control group decreased [ 25 ]. Reflective training, developed in China based on the new mentoring approach, was effective in encouraging nursing students to explore, think about, and solve problems actively during an internship, consequently improving their disposition for critical thinking [ 26 ]. A person-centred education programme using design thinking can effectively improve how nursing students perceive individualised care. Using design thinking allowed the students to apply their theoretical knowledge of the programme to plan innovative solutions that may effectively resolve real health problems [ 27 ]. These programmes were developed in 5 or 6 days [ 27 , 31 ], 1 week or 3 weeks [ 25 , 30 ], and 1 year [ 26 ].
The education programme focused on improving ethical decision-making had statistically significant improvements in nursing students’ self-efficacy in communication confidence, complex ethical decision-making skills, and decreased communication difficulty [ 28 ]. Case-based learning was more effective with lectures than without them in developing students’ critical thinking abilities [ 29 ]. This study was one of the longest developed with 300 h during one school year. This long-term learning intervention could have a positive impact on this study sample. Therefore, the time of the learning intervention could be a limitation in the studied RCTs. The one-time self-instruction guide was ineffective in impacting students’ diagnostic accuracy in solving case studies [ 32 ], and it is possible that only one day of intervention is not enough.
Studies have shown that problem- and team-based learning [ 25 , 31 ] are more beneficial than traditional teaching [ 29 ], as they enhance nursing skills and improve problem-solving abilities, clinical performance, communication competencies, critical thinking, and self-leadership.
Researchers generally agree that clinical reasoning is an important ability and one of the most important competencies for good nursing practise to ensure optimal patient outcomes [ 29 ] and to recognise and address patient deterioration effectively. However, effective communication is crucial in clinical reasoning. It is required to establish a rapport with patients, conduct health evaluations, make collaborative decisions, and discuss clinical cases with colleagues and supervisors. Developing clinical reasoning skills during training is essential to improving nursing professionals’ practice. To enhance clinical reasoning abilities, nursing schools should integrate simulations at every level of education to ultimately improve patient care. Improving nursing students’ preparation will impact the quality of patient care. In addition, new innovative teaching methodologies based on the use of technology could be a motivational driver in nursing clinical reasoning [ 22 ].
5. Limitations
This systematic review did not perform a search on CINAHL. Although most of the journals included in this database are included in MEDLINE, this should be addressed in the future because of the relevance of the database to nursing research. The results of the included studies could have also been influenced by the different times of the interventions and the different contexts. In addition, the reviewers have identified other studies published in languages other than those required by the inclusion criteria. It seems that many articles are published by Asian researchers, but some of them are not in English, so they cannot be analysed.
6. Conclusions
As society progresses, the new generation of nursing students poses a challenge; new technologies are ingrained in their daily lives with access to increasingly advanced technologies like artificial intelligence, and we must adapt training to capture their interest and increase their learning skills. The utilisation of mobile apps, digital simulations, and learning games has a positive impact on the clinical reasoning abilities of nursing students and their motivation. Incorporating new technologies into problem-solving-based learning and decision-making can also enhance nursing students’ reasoning skills. As a result, it is crucial to incorporate these tools into the learning process to maintain students’ interest, motivation, and satisfaction in education. Clinical simulation is particularly important in the training of students in terms of clinical performance. Still, it is necessary to add another teaching method to increase the efficacy of clinical simulations. Therefore, nursing schools should evaluate their current teaching methods and consider integrating or modifying new technologies and methodologies that can help enhance students’ learning, improve their clinical reasoning and cognitive skills, and potentially improve nursing students’ ability to affect patient care positively. By doing so, students will be better equipped to provide high-quality patient care in the future.
| Study | Sample Size | Time Intervention | Teaching Strategies | Purpose of the RCTs | CASP |
|---|---|---|---|---|---|
| Maurício et al., 2022 [ ] | n = 51 | 1 day | Self-Instructional Guide | To evaluate the effect of the Self-Instructional Guide for Clinical Reasoning on the diagnostic accuracy of undergraduate nursing students. | 36 |
| Calik and Kapucu 2022 [ ] | n = 60 | 1 week | Simulation game | Evaluated the efficacy of serious games using pre- and post-tests. | 36 |
| Zhang et al., 2017 [ ] | n = 157 | 12 months | Reflective training program | To evaluate the effects of reflective training for nursing students on their critical thinking disposition. | 35 |
| Chang et al., 2021 [ ] | n = 110 | 40 min | Mobile application | To test the hypothesis that nursing students who used a mobile learning app would have significantly higher levels of knowledge about nasotracheal suctioning and medication administration and a better development of skill performance in medication administration. | 35 |
| (Virtual simulation) | |||||
| Blanié et al., 2020 [ ] | n= 146 | 2 h | Gaming and traditional methods | To compare a traditional teaching method with gaming to improve the clinical reasoning skills necessary to help nursing students detect patient deterioration. | 35 |
| Bilik et al., 2020 [ ] | n = 419 | 1 week | Web-based concept mapping education | To investigate the impact of web-based concept mapping education on nursing students’ critical-thinking and concept-mapping skills. | 34 |
| Zarshenas et al., 2019 [ ] | n = 90 | 2 h for 6 days | Problem-solving | To investigate how training problem-solving skills affected the rate of self-handicapping among nursing students. | 33 |
| Svellingen et al., 2021 [ ] | n = 146 | 4 days in 3 years | Clinical simulation | To evaluate the impact of multiple simulations on students’ self-reported clinical decision-making skills and self-confidence. | 33 |
| Kim and Suh 2018 [ ] | n = 72 | 1 week | Mobile application | To determine if a mobile application improved students’ skills and knowledge. | 33 |
| (virtual simulation) | |||||
| Park et al., 2021 [ ] | n = 105 | 2 h for 5 days | Education program | To develop a feasibility programme for providing foundational knowledge and skills about patient-centred care to fourth-year undergraduate nursing students using the design-thinking approach. | 32 |
| Pai et al., 2022 [ ] | n = 101 | 8 h for 14 weeks | Person-centred education program | To investigate the impact of an ethical decision-making framework on ethical decision-making and communication self-efficacy in nursing students. | 32 |
| Silva et al., 2020 [ ] | n = 78 | 3.5 h for one day | Clinical simulation | To analyse the effect of clinical simulation on the development of clinical reasoning and on nursing students’ acquisition of knowledge of wound evaluation and treatment. | 31 |
| Boostel et al., 2018 [ ] | n = 52 | 30 min | Clinical simulation | To compare and evaluate the perception of stressors by nursing students before and after a high-fidelity conventional laboratory practise class or clinical simulation. | 30 |
| Hong and Yu, 2017 [ ] | n = 122 | 300 h | Cased-based learning | To compare and explore the effectiveness of two styles of case-based learning methods, unfolding nursing cases and unusual nursing cases, implemented in lectures for developing nursing students’ critical-thinking abilities. | 30 |
| Kim et al., 2016 [ ] | n = 63 | 2 h weekly for 3 weeks | Team-based learning | To examine the effects of TBL on learning outcomes and the problem-solving ability (knowledge and clinical performance) of Korean nursing students. | 30 |
Funding Statement
This research received external funding from the European programme Eramus +2021-1-BE02-KA220-HED-000023194.
Author Contributions
Conceptualisation, A.P.-P. and A.Z.; methodology, A.P.-P. and A.Z.; formal analysis, A.P.-P.; writing—original draft preparation, A.P.-P.; writing—review and editing, A.Z.; visualisation, A.Z.; supervision, A.Z. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Critical thinking enables you to evaluate all available information, consider potential outcomes, and choose the most appropriate interventions. It improves decision-making. Effective decision-making in nursing involves selecting the best options among various alternatives. Critical thinking allows nurses to weigh the pros and cons of different ...
Real Life Critical Thinking + Nursing Care Plan Examples. Ok, let's go through some examples of scenarios that require both critical thinking and care plan implementation! Example 1: Falling Over You. Your patient is detoxing from alcohol. She has a really unsteady gait when they get up, weak, and have intermittent confusion.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient's preferences, medical history, and evidence-based practices.
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers in nursing exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, openmindedness, perseverance, and reflection.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Critical thinking makes the nurse a professional achiever who picks, integrates, analyzes, and utilizes knowledge. Nurses' actions in the caregiving process are realized with critical thinking skills. Critical thinking in nursing practice helps make an inclusive care plan with considerable potential for success.
24 Strategies to improve critical thinking skills in nursing. You may also want to check out: 15 Attitudes of Critical Thinking in Nursing ... Through attentive listening, a nurse uncovers a patient's underlying concerns, leading to an informed care plan that addresses both medical needs and emotional well-being.
The tool includes 25 competencies, identified by nursing leaders as core skills at the heart of critical thinking. These competencies were grouped into 5 components of critical thinking: problem recognition, clinical decision making, prioritization, clinical implementation, and reflection.
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
A formal nursing care plan is a written or computerized guide that organizes the client's care information. ... Critical thinking in nursing process and education. International journal of humanities and social science, 1(13), 257-262. Share.
• In nursing, critical thinking is a cognitive process that represents the capacity to reflect upon reasoning with the aim of minimizing the errors in decision-making (Chao, Liu, Wu, Clark, & Tan, 2013; Shinnick & Woo, 2013; Alfaro-LeFevre, 2016) ... • Plan care for each patient that is unique to the problem and situation
By creating a nursing care plan based on a patient's assessment, the nurse learns how to prioritize, plan goals and interventions, and evaluate outcomes related to specific disease processes. ... Then, the nurse uses their nursing knowledge and critical thinking skills to decide if further assessments are necessary to identify a nursing ...
Nursing critical thinking skills drive the decision-making process and impact the quality of care provided," says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing. For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they ...
The nursing process functions as a systematic guide to client-centered care with 5 sequential steps. These are assessment, diagnosis, planning, implementation, and evaluation. Assessment. Assessment is the first step and involves critical thinking skills and data collection; subjective and objective. Subjective data involves verbal statements ...
The care plan involves the steps and strategies needed to achieve the desired goal. ... The ADPIE nursing process is an essential component of clinical care. It improves critical thinking and decision-making by breaking down processes into simplified and organized steps.
Critical thinking in nursing practice results in a comprehensive patient plan of care with maximized potential for success. Critical thinking In Nursing Practice. Using critical thinking to develop a plan of nursing care requires considering the human factors that might influence the plan. The nurse interacts with the patient, family, and other ...
Clinical reasoning in nursing is dynamic and adaptive, as nurses continuously gather new information and adjust care plans based on patient responses. It's a crucial skill that guides nurses in providing safe, effective, and patient-centered care. Clinical reasoning involves the integration of clinical knowledge, critical thinking, and ...
With the current emphasis on quality improvement, critical thinking ability is a noteworthy concern within the nursing profession. An in-depth review of literature related to critical thinking was performed. The use of nursing care plans and concept mapping to improve critical thinking skills was among the recommendations identified.
The person-centred educational programme focuses on how nursing students perceive individualised care, using design thinking to improve their perception. The use of design thinking gave the students opportunities to apply their theoretical knowledge of the person-centred program to plan innovative solutions that may effectively resolve real ...