Quick Links
Get in touch.

Save Up to 20% Before Oct. 2!

My True Story of Alcoholism, Addiction and the Choice to Live

At 8 years old, I stared out the second-floor window of our apartment. Children my age played on the playground. The windowpane was warm. The sky was clear. I remember this day now as sharp as the edge of a knife because in that moment, I wanted to die.
By this time in my life, I had been abused by my family—sexually and emotionally—for as long as I could remember. I hadn’t even lived a decade, and I hurt so much I wished it were over already.
Twenty years later, I was an alcoholic and a meth addict.
Related: ‘I Was an Everything Addict’: The Bizarre Transformation of Andrew Zimmern
When SUCCESS asked me if I would write about my personal story of getting sober and staying sober, I agreed because I know that my rich life today—as blessed and real and challenging and joyful as it is —wouldn’t be possible without the horror and sadness and hurt that came before it. Today my life is so remarkably blessed, I probably make people sick. I’m happy. I’m loved. I’m what a lot of people would consider successful. But none of it would be what it is without the suffering—the pain caused by others and the pain I brought on myself. That kind of pain isn’t unique to me. I’ve heard stories that make my life sound like Disneyland. Some pain is soul-deep. It’s life-altering. But so is our response to that pain.
I know that my life today—as blessed and real and challenging and joyful as it is—wouldn’t be possible without the horror and sadness and hurt that came before it.
This is a story that I’ve only told in recovery meetings, a story some people who have known me for years don’t even know. I’m sharing it because I want others to see their own stories in the same way: as a starting point not as an ending.
Into the Abyss
I had my first real drink when I was 10 years old. More than just a sip out of someone’s glass, the cold beer with a lime that my new stepdad handed me was all mine. I remember lying down, getting a little woozy, and later, eating some crackers to settle my stomach. One beer was plenty for a 45-pound girl.
I grimaced as it went down, but I reveled in the layer of padding the alcohol put between me and the real world, as if someone had wrapped the block of ice constantly pressed against my soul in a fluffy towel. The pain wasn’t as acute. The constant sense of danger wasn’t as imminent.
Soon I was smuggling airline-sized bottles of booze to school and hiding them in my locker so I could sneak a sip before lunch or gym or any other point in the day when one of my two best friends, depression and anxiety, crippled me socially.
At times, I’m told, I appeared self-assured . I walked with my head up and shoulders back (thanks to years in ballet). I spoke with confidence (thanks to a love of words and theater). From the outside, I probably appeared condescendingly cool at times. But the view looking out was very different.
I was hyper-aware of other people, on constant high-alert thanks to my home life. I had a persistent belief that everyone was talking about me, plotting against me or wishing me harm. I might have looked like a turtle sunning itself on a rock, but I felt like a frog in a frying pan.
By high school, I was drinking every weekend. In my world, drinking was as normal as ordering pizza. When adults sipped iced tea with dinner at a restaurant, I was dumbfounded. How could someone over the legal drinking age not be drinking? I had no idea that most people were living a very different life from mine, a life in which alcohol did not have a daily, starring role. I had been raised to believe that adults drank just like they worked jobs, drove cars and complained about taxes. It was part of being an adult .
I now know that, for the most part, the adults in my life weren’t trying to hurt me. They were living under the same delusion that their life was normal, their insane reasoning sound, and their self-centered choices rational. They, too, endured abuse and trauma that drove them to deaden their pain. The best numbing agent they found was alcohol, so they handed it down to me.
Despite my drinking and emotional instability, I earned a full scholarship to college. I carried a flask of whiskey to treat the searing depression that gripped me as soon as I put some distance between myself and my family. I was happy when I was drunk, but I was in a crying fit at least once a week and found myself in a rage over the smallest offenses. I alternated between giving people the cold shoulder and flooding them with emotional drama. As I look back, I realize that sharing daily life with my roommate—a normal, well-loved, faith-filled human being—contrasted completely with my identity. I couldn’t help acknowledge the truth I constantly tried to run from: I was damaged and hopeless.

So I drank more. I smoked a pack of cigarettes a day. I experimented with drugs. I broke hearts and had mine broken. And I lost my scholarship.
Filling the Void
For the next five years, I did everything I could to blame my deep woundedness on something other than a withering soul caused by abuse, neglect and my own increasing self-centeredness. I switched jobs, apartments and boyfriends at regular six-month intervals. I tried turning to God. I prayed. I joined a couple of churches. I was confirmed one year, then dunked the next. I did Bible studies and learned to meditate . I prayed and yelled and pleaded with God to fix me, heal me, forgive me, do anything with me that would make me feel like a normal human being.
I tried therapy. It was during these five years that I began having panic attacks. Gradually they became more intense and more frequent. Ten times a day, fear poured over my being in a way that convinced me I was about to die. I got help. I got medication. And thankfully I got out of agoraphobia and back into the world. But I didn’t stop drinking.
Related: What Agoraphobia Taught Me About Fear Versus Facts
Drinking wasn’t the problem, as far as I could see. It was the solution. It was the cleansing release that never seemed to come from on high. I drank whiskey at the bar and gulped wine in front of the TV. I started popping tiny speed pills to keep me going after an all-day bender. I ate less and slept more. I flirted with an ulcer, fought headaches, and developed chronic pain that gripped every area of my body and gave me a reason to take pain pills.
Then at 26, I decided enough was enough and I got married. Fearing my own recklessness and lack of control, I clung to the idea that settling down would slow my drinking and having a partner would ease my emotional turmoil. But of course, a person can’t fix another person. A human can’t be a higher power. One partner can’t carry the weight meant for two. So I moved out after a year, and we divorced.
I lived in an efficiency apartment for a few months after we separated. The bleak emptiness that set in during this time was unspeakable. I felt like an utter failure. No life stretched out before me as it always had. I would be no one’s wife, no one’s mother, no one’s anything. I would have no degree, no career, no purpose. I felt like one of the corn husk dolls my grandmother gave me when I was a child: faceless and meaningless, folded over and over and over on myself.
That’s when I chose to use drugs. The moment when I knew I would kill myself if I had to wake up one more day, I made the call to a friend and asked her to give me some meth.
Most people look at addiction or alcoholism from the outside and wonder, How could they sink so low? What these well-meaning people don’t understand is that sometimes addiction and alcoholism feel like a step up from someplace worse.
The first time I used meth, I thought, Wow, I’m an addict. I didn’t fight it. I didn’t care that I couldn’t control my mind and body. It was a relief, all of it, from the lightness that took over my limbs and the smile that spread across my face to the knowledge that I was, officially and forever, an addict. Because an addict has a purpose, a reason for living, a mission in life: to use drugs. Being an addict was far and away better than being a husk.
Arrival of Grace
The day I walked into my first recovery meeting, I hadn’t worked in nearly two years. I hadn’t bathed in a month. I had no running water, phone or heat in my duplex for almost a year. I didn’t brush my teeth anymore. I had sores on my head from not washing my hair and sores on my face from a relentless obsession that meth gives you for picking at anything close by. I weighed 78 pounds and experienced frequent kidney infections, seizures and voices calling my name in the darkness. I nearly died more than once. I stayed awake for three or four days at a time, getting high and drinking myself into alcohol poisoning. I blacked out often and am still missing large chunks of my timeline.
But I remember one moment as vividly as wanting to kill myself that day when I was 8 years old: I remember the second I knew I was done.
Some say that our lives change in a moment, but really, if we think about it, the actual change happened in a heartbeat.
Some say that our lives change in a moment. We might believe it took us 10 years to quit a job or fix a marriage, but really, if we think about it, the actual change happened in a heartbeat. We might think about changing for 10 years, we might tell ourselves we should make the change for 10 years, but the real change , that decision we make like a snap, occurs within us in a fraction of an instant.
For me it happened one gray morning while sitting in a room with another addict and watching what happened as alcohol and drugs shrank this larger-than-life person into a confused, quivering ball of shame. I looked at him and saw myself clearly, starkly, suddenly. I felt the strangling denial deep down inside me switch off and a light flicker on.
I’m done , I thought.
I made a life-altering decision in the thinnest slice of eternity, as if in that messy room just before the sun came up, the divine reached out to the present moment like a crack of light under the door. I was struck hard with truth so profound and so filled with grace that I couldn’t look away. And I knew: I’m worth living for.
Silently, I asked, Now what?
Looking back, this is the first proof that I’d really changed. Unlike countless times before when I had gritted my teeth, determined to solve all of my problems myself, this time I asked for help. In my most shameful moment, rather than hiding or posturing or denying, I let people see me.
I asked, “Now what? Where do I go? What do I do? Tell me, and I’ll do it.” First the someone I asked was God. Then it was someone with a list of recovery meetings.
In the early 1800s, Johann Wolfgang von Goethe published Faust , a play about a man who makes a deal with the devil for earthly satisfaction in exchange for his soul. In it, the main character says, “Whatever you can do or believe you can do, begin it. Action has magic, grace and power in it.”
That’s the only difference between me now and me on that gray morning. Grace arrived, and I didn’t just let it in. I’ve gotten up every day since and left the door wide open.
Surviving the Flood
Living sober isn’t all rainbows and butterflies. The first years of sobriety were filled with terrible realizations, paralyzing fear and daily confusion. All of the pain I’d been trying to deny, all of the wounds I’d been trying to ignore, and all of the memories I’d been trying to repress came slithering out of the darkness. Quitting drinking and using was one thing. Staying quit was another.
It reminds me of that story about the little Dutch boy who put his finger in the dam to stop up the hole. He stayed out all night, waiting for someone to come and fix it, whistling to himself to keep up his spirits. But eventually, if no one had come, he would have taken his finger out and the water would have broken through in a torrent.
For the first few weeks in sobriety, I was a whistling Dutch boy. Then the flood came. Grief, shame, sorrow, anger, bewilderment, self-hatred and random bursts of unbridled joy. I distanced myself from my family as the truth of our codependence and their own sickness dawned on me like an unwelcome hangover. Eventually, my stepdad, who was always supportive of my sobriety, died of cancer caused by his drinking. In his final year, we were closer than ever, and I asked his forgiveness and gave it in return.
Related: How to Forgive
As I tried to ride the waves of realization that arose in my now-clear head, I threw myself into a spiritual program of recovery that sustains me even today. This means, essentially, that I follow a path carved out by countless other sober people who have braved the same floods. I pray to a God that I now know loves me beyond measure, read books written by people who understand what it’s like to live in my skin, and write spirals full of self-reflection and stark unveiling only to share all that mess with another person. I’m guided along the way by women and men who are a few steps ahead of me on the path. And I have the privilege to guide others who come behind me.
Since getting sober, I’ve learned to love myself, forgive myself , and live as the person I was created to be. I’ve earned my college degree, married an incredible man, bought a house, become a mother, created a family of choice, won an Emmy, served on the editorial staffs of seven magazines and started a thriving business I love. My chronic pain is healed, the anxiety and depression are gone, and that feeling of shame has been lifted because I’ve also gotten more therapy, ended my relationships with toxic people no matter how we’re related, and been willing to feel the worst pain in order to find the most freedom. A life like this takes a lot of work for someone like me. Maybe for all of us.
That’s the thing about asking, Now what? I actually have to listen to the answer and be willing to act. Even if it scares me or confuses me or makes me mad. Today the next right action is to share my journey with you, even though it means I cringe as I hit send to file this story; bite my nails while I wait for it to be published; and ignore the fear in my head that tells me I’ll be judged, criticized, or even unduly praised for what I’ve done, seen, and lived.
In the end, I am who I am, and I live this life instead of that old, painful one because I was desperate enough to have enough faith in someone else’s solution for my problems. I can’t really take credit for my sobriety. I believe God keeps me sober one day at a time, but I believe my connection with this higher power depends utterly on my honest and sincere and consistent action—no matter how inconvenient or uncomfortable.
This is what I want you to know: Your suffering is just a starting point. It’s up to you to move, to act and to receive the grace that accompanies even the smallest effort. I know firsthand that if you don’t know you have a choice, then you don’t have one.
Today you have a choice. You can keep asking why and allow your suffering to be the name tag on your life. Or you can start asking, Now what? You can leave the door open for grace and see what it lets in.
Related: Face Your Demons
This article originally appeared in the February 2017 issue of SUCCESS magazine .
Amy Anderson
Amy Anderson is the former senior editor of SUCCESS magazine, an Emmy Award-winning writer and founder of Anderson Content Consulting. She helps experts, coaches, consultants and entrepreneurs to discover their truth, write with confidence, and share their stories so they can transform their past into hope for others. Learn more at AmyKAnderson.com and on Facebook.
5473 Blair Road, Suite 100 PMB 30053 Dallas, TX 75231
Copyright © 2024 SUCCESS Magazine. All rights reserved.

Unlock the Latest Knowledge that Can You Help You Achieve More in Life with More Confidence
Print and Digital Options Available
- Introduction
- Conclusions
- Article Information
BMI indicates body mass index; SES, socioeconomic status.
a Variables smoking status, SES, drinking pattern, former drinker bias only, occasional drinker bias, median age, and gender were removed.
b Variables race, diet, exercise, BMI, country, follow-up year, publication year, and unhealthy people exclusion were removed.
eAppendix. Methodology of Meta-analysis on All-Cause Mortality and Alcohol Consumption
eReferences
eFigure 1. Flowchart of Systematic Search Process for Studies of Alcohol Consumption and Risk of All-Cause Mortality
eTable 1. Newly Included 20 Studies (194 Risk Estimates) of All-Cause Mortality and Consumption in 2015 to 2022
eFigure 2. Funnel Plot of Log-Relative Risk (In(RR)) of All-Cause Mortality Due to Alcohol Consumption Against Inverse of Standard Error of In(RR)
eFigure 3. Relative Risk (95% CI) of All-Cause Mortality Due to Any Alcohol Consumption Without Any Adjustment for Characteristics of New Studies Published between 2015 and 2022
eFigure 4. Unadjusted, Partially Adjusted, and Fully Adjusted Relative Risk (RR) of All-Cause Mortality for Drinkers (vs Nondrinkers), 1980 to 2022
eTable 2. Statistical Analysis of Unadjusted Mean Relative Risk (RR) of All-Cause Mortality for Different Categories of Drinkers for Testing Publication Bias and Heterogeneity of RR Estimates From Included Studies
eTable 3. Mean Relative Risk (RR) Estimates of All-Cause Mortality Due to Alcohol Consumption up to 2022 for Subgroups (Cohorts Recruited 50 Years of Age or Younger and Followed up to 60 Years of Age)
Data Sharing Statement
- Errors in Figure and Supplement JAMA Network Open Correction May 9, 2023
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Zhao J , Stockwell T , Naimi T , Churchill S , Clay J , Sherk A. Association Between Daily Alcohol Intake and Risk of All-Cause Mortality : A Systematic Review and Meta-analyses . JAMA Netw Open. 2023;6(3):e236185. doi:10.1001/jamanetworkopen.2023.6185
Manage citations:
© 2024
- Permissions
Association Between Daily Alcohol Intake and Risk of All-Cause Mortality : A Systematic Review and Meta-analyses
- 1 Canadian Institute for Substance Use Research, University of Victoria, Victoria, British Columbia, Canada
- 2 Department of Psychology, University of Portsmouth, Portsmouth, Hampshire, United Kingdom
- Correction Errors in Figure and Supplement JAMA Network Open
Question What is the association between mean daily alcohol intake and all-cause mortality?
Findings This systematic review and meta-analysis of 107 cohort studies involving more than 4.8 million participants found no significant reductions in risk of all-cause mortality for drinkers who drank less than 25 g of ethanol per day (about 2 Canadian standard drinks compared with lifetime nondrinkers) after adjustment for key study characteristics such as median age and sex of study cohorts. There was a significantly increased risk of all-cause mortality among female drinkers who drank 25 or more grams per day and among male drinkers who drank 45 or more grams per day.
Meaning Low-volume alcohol drinking was not associated with protection against death from all causes.
Importance A previous meta-analysis of the association between alcohol use and all-cause mortality found no statistically significant reductions in mortality risk at low levels of consumption compared with lifetime nondrinkers. However, the risk estimates may have been affected by the number and quality of studies then available, especially those for women and younger cohorts.
Objective To investigate the association between alcohol use and all-cause mortality, and how sources of bias may change results.
Data Sources A systematic search of PubMed and Web of Science was performed to identify studies published between January 1980 and July 2021.
Study Selection Cohort studies were identified by systematic review to facilitate comparisons of studies with and without some degree of controls for biases affecting distinctions between abstainers and drinkers. The review identified 107 studies of alcohol use and all-cause mortality published from 1980 to July 2021.
Data Extraction and Synthesis Mixed linear regression models were used to model relative risks, first pooled for all studies and then stratified by cohort median age (<56 vs ≥56 years) and sex (male vs female). Data were analyzed from September 2021 to August 2022.
Main Outcomes and Measures Relative risk estimates for the association between mean daily alcohol intake and all-cause mortality.
Results There were 724 risk estimates of all-cause mortality due to alcohol intake from the 107 cohort studies (4 838 825 participants and 425 564 deaths available) for the analysis. In models adjusting for potential confounding effects of sampling variation, former drinker bias, and other prespecified study-level quality criteria, the meta-analysis of all 107 included studies found no significantly reduced risk of all-cause mortality among occasional (>0 to <1.3 g of ethanol per day; relative risk [RR], 0.96; 95% CI, 0.86-1.06; P = .41) or low-volume drinkers (1.3-24.0 g per day; RR, 0.93; P = .07) compared with lifetime nondrinkers. In the fully adjusted model, there was a nonsignificantly increased risk of all-cause mortality among drinkers who drank 25 to 44 g per day (RR, 1.05; P = .28) and significantly increased risk for drinkers who drank 45 to 64 and 65 or more grams per day (RR, 1.19 and 1.35; P < .001). There were significantly larger risks of mortality among female drinkers compared with female lifetime nondrinkers (RR, 1.22; P = .03).
Conclusions and Relevance In this updated systematic review and meta-analysis, daily low or moderate alcohol intake was not significantly associated with all-cause mortality risk, while increased risk was evident at higher consumption levels, starting at lower levels for women than men.
The proposition that low-dose alcohol use protects against all-cause mortality in general populations continues to be controversial. 1 Observational studies tend to show that people classified as “moderate drinkers” have longer life expectancy and are less likely to die from heart disease than those classified as abstainers. 2 Systematic reviews and meta-analyses of this literature 3 confirm J-shaped risk curves (protective associations at low doses with increasing risk at higher doses). However, mounting evidence suggests these associations might be due to systematic biases that affect many studies. For example, light and moderate drinkers are systematically healthier than current abstainers on a range of health indicators unlikely to be associated with alcohol use eg, dental hygiene, exercise routines, diet, weight, income 4 ; lifetime abstainers may be systematically biased toward poorer health 5 ; studies fail to control for biases in the abstainer reference group, in particular failing to remove “sick quitters” or former drinkers, many of whom cut down or stop for health reasons 2 ; and most studies have nonrepresentative samples leading to an overrepresentation of older White men. Adjustment of cohort samples to make them more representative has been shown to eliminate apparent protective associations. 6 Mendelian randomization studies that control for the confounding effects of sociodemographic and environmental factors find no evidence of cardioprotection. 7
We published 2 previous systematic reviews and meta-analyses that investigated these hypotheses. The first of these focused on all-cause mortality, 8 finding negligible reductions in mortality risk with low-volume alcohol use when study-level controls were introduced for potential bias and confounding, such as the widespread practice of misclassifying former drinkers and/or current occasional drinkers as abstainers (ie, not restricting reference groups to lifetime abstainers). 8 Our alcohol and coronary heart disease (CHD) mortality meta-analysis of 45 cohort studies 9 found that CHD mortality risk differed widely by age ranges and sex of study populations. In particular, young cohorts followed up to old age did not show significant cardio-protection for low-volume use. Cardio-protection was only apparent among older cohorts that are more exposed to lifetime selection biases (ie, increasing numbers of “sick-quitters” in the abstainer reference groups and the disproportionate elimination of drinkers from the study sample who had died or were unwell).
The present study updates our earlier systematic review and meta-analysis for all-cause mortality and alcohol use, 8 including studies published up to July 2021 (ie, 6.5 years of additional publications). The study also investigated the risk of all-cause mortality for alcohol consumption according to (1) median ages of the study populations (younger than 56 years or 56 years and older), replicating the methods of Zhao et al 9 ; (2) the sex distribution of the study populations, and (3) studies of cohorts recruited before a median age of 51 years of age and followed up in health records until a median age of at least 60 years (ie, with stricter rules to further minimize lifetime selection biases). Because younger cohorts followed up to an age at which they may experience heart disease are less likely to be affected by lifetime selection biases, 9 we hypothesized that such studies would be less likely to show reduced mortality risks for low-volume drinkers. Finally, we reran the analyses using occasional drinkers (<1 drink per week) as the reference, for whom physiological health benefits are unlikely. Occasional drinkers are a more appropriate reference group, given evidence demonstrating that lifetime abstainers may be biased toward ill health. 10
The present study updates the systematic reviews and meta-analyses described above 8 by including studies published up to July 2021 to investigate whether the risk differed for subgroups. The study protocol was preregistered on the Open Science Framework. 11 Inclusion criteria, search strategy, study selection, data extraction, and statistical analytical methods of the study are summarized in later sections (see eAppendix in Supplement 1 for more details).
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline. 12 The review sought cohort studies of all-cause mortality and alcohol consumption. We identified all potentially relevant articles published up to July 31, 2021, regardless of language, by searching PubMed and Web of Science, through reference list cross-checking of previous meta-analyses (eFigure 1 in Supplement 1 ). There were 87 studies identified by Stockwell et al. 8 After inclusion of 20 new studies meeting inclusion criteria, there were a total of 107 cohort studies (eTable 1 in Supplement 1 ). 13 - 32
Three coders (J. Z., F. A., and J. C.) reviewed all eligible studies to extract and code data independently from all studies fulfilling the inclusion criteria. Data extracted included (1) outcome, all-cause mortality; (2) measures of alcohol consumption; (3) study characteristics, including cohort ages at recruitment and follow-up; (4) types of misclassification error of alcohol consumers and abstainers; (5) controlled variables in individual studies. Alcoholic drinks were converted into grams per day according to country-specific definitions if not otherwise defined. 33 , 34
We also assessed publication bias, heterogeneity, and confounding of covariates that might potentially affect the association of interest using several statistical approaches. 35 - 41 Relative risk (RR), including hazard ratios or rate ratios, were converted to natural log-transformed formats to deal with skewness. Publication bias was assessed through visual inspection of the funnel plot of log-RR of all-cause mortality due to alcohol consumption against the inverse standard error of log-RR 42 and Egger’s linear regression method. 36 We also plotted forest graphs of log-RR of all-cause mortality for any level of drinking to assess heterogeneity among studies. 42 The between-study heterogeneity of RRs were assessed using Cochran Q 37 and the I 2 statistic. 38 If heterogeneity was detected, mixed-effects models were used to obtain the summarized RR estimates. Mixed-effects regression analyses were performed in which drinking groups and control variables were treated as fixed-effects with a random study effect because of significant heterogeneity. 43
All analyses were weighted by the inverse of the estimated variance of the natural log relative risk. Variance was estimated from reported standard errors, confidence intervals, or number of deaths. The weights for each individual study were created using the inverse variance weight scheme and used in mixed regression analysis to get maximum precision for the main results of the meta-analysis. 42 In comparison with lifetime abstainers, the study estimated the mean RR of all-cause mortality for former drinkers (ie, now completely abstaining), current occasional (<9.1 g per week), low-volume (1.3-24.0 g per day), medium-volume (25.0-44.0 g per day), high-volume (45.0-64.0 g) and highest-volume drinkers (≥65.0 grams per day). The analyses adjusted for the potential confounding effects of study characteristics including the median age and sex distribution of study samples, drinker biases, country where a study was conducted, follow-up years and presence or absence of confounders. Analyses were also repeated using occasional drinkers as the reference group. We used t tests to calculate P values, and significance was set at .05. All statistical analyses were performed using SAS version 9.4 (SAS Institute) and the SAS MIXED procedure was used to model the log-transformed RR. 44 Data were analyzed from September 2021 to August 2022.
There were 724 estimates of the risk relationship between level of alcohol consumption and all-cause mortality from 107 unique studies 13 - 32 , 45 - 131 , including 4 838 825 participants and 425 564 deaths available for the analysis. Table 1 describes the sample characteristics of the metadata. Of 39 studies 13 , 15 , 18 , 21 , 23 - 26 , 29 , 31 , 45 - 47 , 49 , 50 , 52 - 54 , 57 - 59 , 62 , 64 , 70 , 80 , 81 , 85 , 87 , 91 , 94 , 96 , 100 , 104 , 107 , 118 , 124 , 125 , 127 , 130 reporting RR estimates for men and women separately, 33 14 , 17 , 48 , 51 , 61 , 63 , 66 , 68 , 69 , 72 , 76 , 79 , 83 , 84 , 86 , 88 , 90 , 92 , 93 , 97 , 98 , 101 , 103 , 105 , 109 - 111 , 113 - 115 , 119 , 120 , 128 were for males only, 8 16 , 65 , 73 , 99 , 102 , 108 , 112 , 123 for females only, and 30 13 , 19 - 22 , 26 - 30 , 32 , 55 , 56 , 67 , 71 , 74 , 75 , 77 , 78 , 82 , 84 , 89 , 95 , 106 , 116 , 117 , 121 , 122 , 126 , 129 for both sexes. Twenty-one studies 13 , 17 , 19 , 21 , 22 , 26 , 27 , 45 - 58 (220 risk estimates) were free from abstainer bias (ie, had a reference group of strictly defined lifetime abstainers). There were 50 studies 14 - 16 , 18 , 20 , 23 - 25 , 29 , 59 - 99 (265 risk estimates) with both former and occasional drinker bias; 28 studies 28 , 30 - 32 , 100 - 122 , 130 (177 risk estimates) with only former drinker bias; and 8 studies 123 - 129 , 131 (62 risk estimates) with only occasional drinker bias.
Unadjusted mean RR estimates for most study subgroups categorized by methods/sample characteristics showed markedly or significantly higher RRs for alcohol consumers as a group vs abstainers. Exceptions were for studies with less than 10 years of follow-up and those with some form of abstainer bias ( Table 1 ). Bivariable analyses showed that mortality risks for alcohol consumers varied considerably according to other study characteristics, such as quality of the alcohol consumption measure, whether unhealthy individuals were excluded at baseline, and whether socioeconomic status was controlled for ( Table 1 ).
No evidence of publication bias was detected either by inspection of symmetry in the funnel plot of log-RR estimates and their inverse standard errors (eFigure 2 in Supplement 1 ) or by Egger linear regression analysis (eTable 2 in Supplement 1 , all P > .05 for each study group). Significant heterogeneity was observed across studies for all drinking categories confirmed by both the Q statistic ( Q 723 = 5314.80; P < .001) and I 2 estimates (all >85.87%). (See eFigure 3 in Supplement 1 for forest plot of unadjusted risk estimates of mortality risks for the 20 newly identified studies).
Pooled unadjusted estimates (724 observations) showed significantly higher risk for former drinkers (RR, 1.22; 95% CI, 1.11-1.33; P = .001) and significantly lower risk for low-volume drinkers (RR, 0.85; 95% CI, 0.81-0.88; P = .001) compared with abstainers as defined in the included studies ( Table 2 ; eFigure 4 in Supplement 1 ). In the fully adjusted model, mortality RR estimates increased for all drinking categories, becoming nonsignificant for low-volume drinkers (RR, 0.93; 95% CI, 0.85-1.01; P = .07), occasional drinkers (>0 to <1.3 g of ethanol per day; RR, 0.96; 95% CI, 0.86-1.06; P = .41), and drinkers who drank 25 to 44 g per day (RR, 1.05; 95% CI, 0.96-1.14; P = .28). There was a significantly increased risk among drinkers who drank 45 to 64 g per day (RR, 1.19; 95% CI, 1.07-1.32; P < .001) and 65 or more grams (RR, 1.35; 95% CI, 1.23-1.47; P < .001). The Figure shows the changes in RR estimates for low-volume drinkers when removing each covariate from the fully adjusted model. In most cases, removing study-level covariates tended to yield lower risk estimates from alcohol use.
Table 2 presents the RR estimates when occasional drinkers were the reference group. In fully adjusted models, higher though nonsignificant mortality risks were observed for both abstainers and medium-volume drinkers (RR, 1.04; 95% CI, 0.94-1.16; P = .44 and RR, 1.09; 95% CI, 0.96-1.25; P = .19, respectively). There were significantly elevated risks for both high and higher volume drinkers (RR, 1.24; 95% CI, 1.07-1.44; P = .004 and RR, 1.41; 95% CI, 1.23-1.61; . P = 001, respectively).
As hypothesized, there was a significant interaction between cohort age and mortality risk ( P = .02; F 601 = 2.93) and so RR estimates for drinkers were estimated in analyses stratified by median age of the study populations at enrollment ( Table 3 ). In unadjusted and partially adjusted analyses, older cohorts displayed larger reductions in mortality risk associated with low-volume consumption than younger cohorts. However, in fully adjusted analyses with multiple covariates included for study characteristics, these differences disappeared. Younger cohorts also displayed greater mortality risks than older cohorts at higher consumption levels. Among studies in which participants were recruited at age 50 years or younger and followed up to age 60 years (ie, there was likely reduced risk of lifetime selection bias) higher RR estimates were observed for all drinking groups vs lifetime abstainers. These differences were significant in all drinking groups except low-volume drinkers (eTable 3 in Supplement 1 ).
Across all levels of alcohol consumption, female drinkers had a higher RR of all-cause mortality than males ( P for interaction = .001). As can be seen in Table 4 , all female drinkers had a significantly increased mortality risk compared with female lifetime nondrinkers (RR, 1.22; 95% CI, 1.02-1.46; P = .03). Compared with lifetime abstainers, there was significantly increased risk of all-cause mortality among male drinkers who drank 45 to 64 g per day (RR, 1.15; 95% CI, 1.03-1.28; P = .01) and drank 65 or more (RR, 1.34; 95% CI, 1.23-1.47; P < .001), and among female drinkers who drank 25 to 44 g per day (RR, 1.21; 95% CI, 1.08-1.36; P < .01), 45 to 64 g (RR, 1.34; 95% CI, 1.11-1.63; P < .01) and 65 or more grams (RR, 1.61; 95% CI, 1.44-1.80; P = .001).
In fully adjusted, prespecified models that accounted for effects of sampling, between-study variation, and potential confounding from former drinker bias and other study-level covariates, our meta-analysis of 107 studies found (1) no significant protective associations of occasional or low-volume drinking (moderate drinking) with all-cause mortality; and (2) an increased risk of all-cause mortality for drinkers who drank 25 g or more and a significantly increased risk when drinking 45 g or more per day.
Several meta-analytic strategies were used to explore the role of abstainer reference group biases caused by drinker misclassification errors and also the potential confounding effects of other study-level quality covariates in studies. 2 Drinker misclassification errors were common. Of 107 studies identified, 86 included former drinkers and/or occasional drinkers in the abstainer reference group, and only 21 were free of both these abstainer biases. The importance of controlling for former drinker bias/misclassification is highlighted once more in our results which are consistent with prior studies showing that former drinkers have significantly elevated mortality risks compared with lifetime abstainers.
In addition to presenting our fully adjusted models, a strength of the study was the examination of the differences in relative risks according to unadjusted and partially adjusted models, including the effect of removing individual covariates from the fully adjusted model. We found evidence that abstainer biases and other study characteristics changed the shape of the risk relationship between mortality and rising alcohol consumption, and that most study-level controls increased the observed risks from alcohol, or attenuated protective associations at low levels of consumption such that they were no longer significant. The reduced RR estimates for occasional or moderate drinkers observed without adjustment may be due to the misclassification of former and occasional drinkers into the reference group, a possibility which is more likely to have occurred in studies of older cohorts which use current abstainers as the reference group. This study also demonstrates the degree to which observed associations between consumption and mortality are highly dependent on the modeling strategy used and the degree to which efforts are made to minimize confounding and other threats to validity.
It also examined risk estimates when using occasional drinkers rather than lifetime abstainers as the reference group. The occasional drinker reference group avoids the issue of former drinker misclassification that can affect the abstainer reference group, and may reduce confounding to the extent that occasional drinkers are more like low-volume drinkers than are lifetime abstainers. 2 , 8 , 132 In the unadjusted and partially adjusted analyses, using occasional drinkers as the reference group resulted in nonsignificant protective associations and lower point estimates for low-volume drinkers compared with significant protective associations and higher point estimates when using lifetime nondrinkers as the reference group. In the fully adjusted models, there were nonsignificant protective associations for low-volume drinkers whether using lifetime abstainers or occasional drinkers as the reference group, though this was only a RR of 0.97 for the latter.
Across all studies, there were few differences in risk for studies when stratified by median age of enrollment above or below age 56 years in the fully adjusted analyses. However, in the subset of studies who enrolled participants aged 50 years or younger who were followed for at least 10 years, occasional drinkers and medium-volume drinkers had significantly increased risk of mortality and substantially higher risk estimates for high- and higher-volume consumption compared with results from all studies. This is consistent with our previous meta-analysis for CHD, 9 in which younger cohorts followed up to older age did not show a significantly beneficial association of low-volume consumption, while older cohorts, with more opportunity for lifetime selection bias, showed marked, significant protective associations.
Our study also found sex differences in the risk of all-cause mortality. A larger risk of all-cause mortality for women than men was observed when drinking 25 or more grams per day, including a significant increase in risk for medium-level consumption for women that was not observed for men. However, mortality risk for mean consumption up to 25 g per day were very similar for both sexes.
A number of limitations need to be acknowledged. A major limitation involves imperfect measurement of alcohol consumption in most included studies, and the fact that consumption in many studies was assessed at only 1 point in time. Self-reported alcohol consumption is underreported in most epidemiological studies 133 , 134 and even the classification of drinkers as lifetime abstainers can be unreliable, with several studies in developed countries finding that the majority of self-reported lifetime abstainers are in fact former drinkers. 135 , 136 If this is the case, the risks of various levels of alcohol consumption relative to presumed lifetime abstainers are underestimates. Merely removing former drinkers from analyses may bias studies in favor of drinkers, since former drinkers may be unhealthy, and should rightly be reallocated to drinking groups according to their history. However, this has only been explored in very few studies. Our study found that mortality risk differed significantly by cohort age and sex. It might be that the risk is also higher for other subgroups, such as people living with HIV, 137 a possibility future research should investigate.
The number of available studies in some stratified analyses was small, so there may be limited power to control for potential study level confounders. However, the required number of estimates per variable for linear regression can be much smaller than in logistic regression, and a minimum of at least 2 estimates per variable is recommended for linear regression analysis, 138 suggesting the sample sizes were adequate in all models presented. It has been demonstrated that a pattern of binge (ie, heavy episodic) drinking removes the appearance of reduced health risks even when mean daily volume is low. 139 Too few studies adequately controlled for this variable to investigate its association with different outcomes across studies. Additionally, our findings only apply to the net effect of alcohol at different doses on all-cause mortality, and different risk associations likely apply for specific disease categories. The biases identified here likely apply to estimates of risk for alcohol and all diseases. It is likely that correcting for these biases will raise risk estimates for many types of outcome compared with most existing estimates.
This updated meta-analysis did not find significantly reduced risk of all-cause mortality associated with low-volume alcohol consumption after adjusting for potential confounding effects of influential study characteristics. Future longitudinal studies in this field should attempt to minimize lifetime selection biases by not including former and occasional drinkers in the reference group, and by using younger cohorts (ie, age distributions that are more representative of drinkers in the general population) at baseline.
Accepted for Publication: February 17, 2023.
Published: March 31, 2023. doi:10.1001/jamanetworkopen.2023.6185
Correction: This article was corrected on May 9, 2023, to fix errors in the Figure and Supplement.
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Zhao J et al. JAMA Network Open .
Corresponding Author: Jinhui Zhao, PhD, Canadian Institute for Substance Use Research, University of Victoria, PO Box 1700 STN CSC, Victoria, BC V8Y 2E4, Canada ( [email protected] ).
Author Contributions: Drs Zhao and Stockwell had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Zhao, Stockwell, Naimi, Churchill, Sherk.
Acquisition, analysis, or interpretation of data: Zhao, Stockwell, Naimi, Clay.
Drafting of the manuscript: Zhao, Stockwell, Clay.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Zhao, Churchill.
Obtained funding: Zhao, Stockwell, Sherk.
Administrative, technical, or material support: Zhao, Stockwell, Naimi.
Supervision: Zhao, Stockwell, Naimi.
Conflict of Interest Disclosures: Dr Stockwell reported receiving personal fees from Ontario Public Servants Employees Union for expert witness testimony and personal fees from Alko outside the submitted work. Dr Sherk reported receiving grants from Canadian Centre on Substance Use and Addiction (CCSA) during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was partly funded by the CCSA as a subcontract for a Health Canada grant to develop guidance for Canadians on alcohol and health.
Role of the Funder/Sponsor: Health Canada had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. CCSA staff conducted a preliminary search to identify potentially relevant articles but did not participate in decisions about inclusion/exclusion of studies, coding, analysis, interpretation of results or approving the final manuscript.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: We gratefully acknowledge contributions by Christine Levesque, PhD (CCSA), and Nitika Sanger, PhD (CCSA), who conducted a preliminary literature search for potentially relevant articles. We also acknowledge the leadership of Drs Catherine Paradis, PhD (CCSA), and Peter Butt, MD (University of Saskatchewan), who cochaired the process of developing Canada’s new guidance on alcohol and health, a larger project which contributed some funds for the work undertaken for this study. We are grateful to Fariha Alam, MPH (Canadian Institute for Substance Use and Research), for her help coding the studies used in this study. None of them received any compensation beyond their normal salaries for this work.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

- NIH Grants & Funding
- Blog Policies
NIH Extramural Nexus
Case Study in Research Integrity: Alcohol and Harassment
There was that bottle of champagne in the breakroom – to be opened when a paper is accepted. Or you heard a colleague’s plan to take a special guest speaker out to dinner at the local watering hole. And, then there were those recruiting events with prospective students that sometimes ended with a happy hour. As many of us have experienced, alcohol may often be part of lab events, conferences, or other related activities. But the presence of alcohol is not an excuse to check professionalism at the door. Here, we are spotlighting this issue to encourage members of the scientific community to consider the potential risks that alcohol can have on the research environment.
Unfortunately, over the past several years we have seen numerous instances where alcohol may have contributed to inappropriate behavior and sexual harassment in the context of scientific research. We are presenting a few case studies below, which are adapted in part from real situations where we worked in tandem with the recipient institutions to address the concerns.
- A postdoctoral fellow sexually assaulted a graduate student after a lab event where alcohol was provided. This fellow was terminated from the institution (who was the recipient of the NIH grant ), and the graduate student was provided with information about how to report to law enforcement. Additionally, the recipient institution directed the principal investigator (PI) to limit alcohol at lab events, as drinking contributed to the abuse.
- A PI at a prestigious scientific conference got severely intoxicated and sexually harassed a postdoctoral fellow. Because the conference organizers made their safety plan widely available and known, the fellow knew who to contact and how to report it. The PI was subsequently removed, an action outline in a safety plan the conference organizers had in place to protect their attendees. And, the PIs institution decided to remove the person from NIH grants, an action that NIH thought appropriate.
- A lab head repeatedly encouraged and pressured their junior staff to drink alcohol and made inappropriate sexual comments while on travel. The institution removed the lab head from serving as PI on NIH awards, prohibited them from applying for new funding, and placed restrictions on travel and the use of alcohol at lab-related events. The institution also identified a new co-mentor for the junior scientists, engaged an external coach to work with the lab head on professional behavior, and began conducting quarterly climate assessments of the lab. NIH also requested regular updates from the recipient institution on their progress.
- A lab head sent abusive emails to colleagues and staff. The institution also determined that the lab head was keeping alcohol in the office and working while under the influence, which may have contributed to the inappropriate communications. The recipient institution subsequently put their employee on administrative leave for several months. Upon their return to the lab, the institution also appointed a co-Director to provide additional oversight and mentoring.
The National Academies reiterated in their 2019 report that organizational tolerance of alcohol use increases the chance of sexual or gender harassment (see also these articles from 2007 , 2005 , and 2002 ). Their report adds that such permissiveness leads some people to avoid lab related social events that involve alcohol. Furthermore, a 2019 report from an Advisory Committee to the NIH Director working group retold a story from a graduate student who was a target of sexual harassment where alcohol was involved.
This type of behavior in a professional setting violates grant policies and can even rise to a criminal offense. We are disheartened to receive reports about such unacceptable behavior, and we note that in the majority of these cases the recipient institution has taken serious actions in consultation with NIH. Based on the severity of the non-compliance, such actions included suspending personnel, removing principal investigators from NIH awards, placing restrictions around alcohol use at lab-related events, and imposing restrictions on travel and conference attendance.
While responsible inclusion of alcohol in celebrations or social outings may not pose a problem, researchers and their institutions should be mindful of how alcohol can contribute to unprofessional behaviors and sexual harassment. Also, keep in mind that purchasing alcoholic beverages is not an allowable grant-associated expense .
Relatedly, NIH-sponsored conferences must have approved safety plans . The strategies discussed in those plans aim to promote safe environments through communicating with attendees, documenting allegations and resulting actions, and other relevant steps to ensure a safe and respectful environment (see also this All About Grants podcast ). If someone at the conference is harassed, and whether or not alcohol was involved, they should feel empowered and protected to report the incident.
In our continued effort to make research environments safe , collectively we must be cognizant of situations that precipitate inappropriate behavior. Nobody should be bullied or pressured if they do not want to have a drink. All social events that include alcohol should also offer non-alcohol containing beverages for those choosing not to drink alcohol. Staff should feel comfortable attending social activities. There should not be an undercurrent or expectation to engage in activities counter to the individual’s personal choices or beliefs. For resources about what constitutes alcohol misuse and how to seek help, please see Rethinking Drinking and the Treatment Navigator from the National Institute on Alcohol Abuse and Alcoholism.
Please also visit our website to inform us if you have any concerns that harassment, discrimination, or other inappropriate conduct may be affecting NIH supported research. You can remain anonymous. More on how to ensure safe and respectful workplaces is available on this podcast .
RELATED NEWS
I would urge the author to consider reframing contents of this article to reflect decades of research indicating that sexual assault, while often involving alcohol, is a an issue of power. Blaming alcohol, as the article suggests, for sexual assaults without recognizing the role power plays in the assault risks abuses continuing, if not exacerbating, since alcohol quashes the personal and social responsibilities of consent. Frankly, this is an embarrassing article to have on the NIH website, and I’d recommend the scholar learn from women in the fields of domestic violence and sexual assault research before publishing future research on the subject.
We appreciate your point about considering how power imbalances may contribute to harassment. Appropriately recognizing and addressing that issue is something we take seriously to ensure that NIH-supported research is conducted in safe and respectful workplaces. The following post may also be of interest: https://nexus.od.nih.gov/all/2023/07/17/case-study-in-research-integrity-banned-from-supervising-cant-go-in-lab-but-no-impact-on-nih-funded-research/
Prevention is the key! Rules of conduct must be out in place and followed.
Before submitting your comment, please review our blog comment policies.
Your email address will not be published. Required fields are marked *
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Alcohol effects on family relations: a case study
Affiliation.
- 1 Minas Gerais Federal University, School of Nursing. [email protected]
- PMID: 18709271
- DOI: 10.1590/s0104-11692008000700005
Problems related to alcohol abuse have been associated to different factors, regardless of the causes attributed to this phenomenon. Alcohol consumption and dependence is considered a public health problem and deserve attention because of the social, work, family, physical, legal and violence-related risks it represents. This study aimed to identify the effects of alcoholism on family relations and, by means of case management, to encourage the recovery of these relationships. The results show that the problems caused by alcohol abuse impose profound suffering to family members, which contributes to high levels of interpersonal conflict, domestic violence, parental inadequacy, child abuse and negligence, financial and legal difficulties, in addition to clinical problems associated to it.
PubMed Disclaimer
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Scientific Electronic Library Online
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Robert’s story
Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital.
He drank all day every day until he would pass out and this was either in the town centre or just by the roadside. In addition, Robert was also incontinent and really struggled with any meaningful communication or positive decision making due to his alcohol usage. This often resulted in local services such as police, ambulance being called in to help. He had no independent living skills and was unable to function without alcohol.
In addition, and due to his lifestyle and presenting behaviours, Robert had a hostile relationship with his family and had become estranged from them for a long period of time.
Robert needed ongoing support and it was identified at the General Hospital that if he was to carry on “living” the way he currently was, then he wouldn’t survive another winter.
On the back of this, Robert was referred to Calico who organised a multi-disciplinary support package for him, which included support with housing as part of the Making Every Adult Matter programme.
After some initial challenges, Robert soon started to make some positive changes.
The intensive, multidisciplinary support package taught him new skills to support him to live independently, sustain his tenancy and make some positive lifestyle changes which in turn would improve his health and wellbeing.
This included providing daily visits in the morning to see Robert and to support him with some basic activities on a daily/weekly basis. This included getting up and dressed; support with shopping and taking to appointments; guidance to help make positive decisions around his associates; support about his benefits and managing his money. In addition, he was given critical support via accessing local groups such as RAMP (reduction and motivational programme) and Acorn (drugs and alcohol service), as well as 1 to 1 sessions with drugs workers and counsellors to address his alcohol addiction.
After six months Robert continued to do well and was leading a more positive lifestyle where he had greatly reduced his A&E attendance. He had significantly reduced his alcohol intake with long periods of abstinence and was now able to communicate and make positive decisions around his lifestyle.
Critically he had maintained his tenancy and continued to regularly attend local groups and other support for his alcohol addiction and had reconnected with some of his family members.
By being able to access these community resources and reduce his isolation he is now engaged in meaningful activities throughout the day and has been able to address some of his critical issues. A small but significant example is that Robert is now wearing his hearing aids which means that he can now interact and communicate more effectively.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Understanding alcohol use disorder.
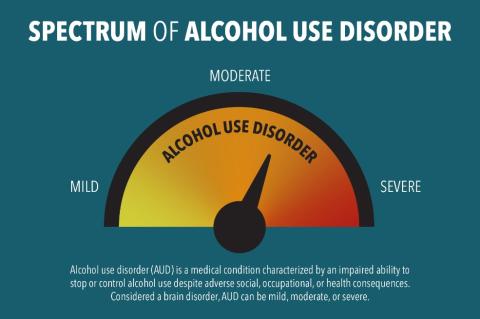
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse. The good news is that no matter how severe the problem may seem, evidence-based treatment with behavioral therapies, mutual-support groups, and/or medications can help people with AUD achieve and maintain recovery. According to the 2023 National Survey on Drug Use and Health, 28.1 million adults ages 18 and older (10.9% in this age group) had AUD in the past year. 1,2 Among youth, an estimated 757,000 adolescents ages 12 to 17 (2.9% of this age group) had AUD during this time frame. 1,2
What Increases the Risk for Alcohol Use Disorder?
A person’s risk for developing AUD depends in part on how much, how often, and how quickly they consume alcohol. Alcohol misuse—defined as drinking in a manner, situation, amount, or frequency that could cause harm to the person who drinks or to those around them—over time increases the risk of AUD. Alcohol misuse includes binge drinking and heavy alcohol use . Other factors also increase the risk of AUD, such as:
- Drinking at an early age. A recent national survey found that among people ages 26 and older, those who began drinking before age 15 were more than three times as likely to report having AUD in the past year as those who waited until age 21 or later to begin drinking. 3 The risk for females in this group is higher than that of males.
- Genetics and family history of alcohol problems. Genetics play a role, with hereditability accounting for approximately 60%; however, like other chronic health conditions, AUD risk is influenced by the interplay between a person’s genes and their environment. Parents’ drinking patterns may also influence the likelihood that a child will one day develop AUD.
- Mental health conditions and a history of trauma. A wide range of psychiatric conditions—including depression, post-traumatic stress disorder, and attention deficit hyperactivity disorder—are comorbid with AUD and are associated with an increased risk of AUD. People with a history of childhood trauma are also vulnerable to AUD.
What Are the Symptoms of Alcohol Use Disorder?
Health care professionals use criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), to assess whether a person has AUD and to determine the severity, if the disorder is present. Severity is based on the number of criteria a person meets based on their symptoms—mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria).
A health care provider might ask the following questions to assess a person’s symptoms.
In the past year, have you:
- Had times when you ended up drinking more, or longer, than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time drinking, being sick from drinking, or getting over other aftereffects?
- Wanted a drink so badly you couldn’t think of anything else?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities you found important, interesting, or pleasurable so you could drink?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or unsafe sexual behavior)?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had an alcohol-related memory blackout?
- Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, dysphoria (feeling uneasy or unhappy), malaise (general sense of being unwell), feeling low, or a seizure? Or sensed things that were not there?
Any of these symptoms may be cause for concern. The more symptoms, the more urgent the need for change.
What Are the Types of Treatment for Alcohol Use Disorder?
Several evidence-based treatment approaches are available for AUD. One size does not fit all and a treatment approach that may work for one person may not work for another. Treatment can be outpatient and/or inpatient and be provided by specialty programs, therapists, and health care providers.
Medications
Three medications are currently approved by the U.S. Food and Drug Administration to help people stop or reduce their drinking and prevent a return to drinking: naltrexone (oral and long-acting injectable), acamprosate, and disulfiram. All these medications are nonaddictive, and they may be used alone or combined with behavioral treatments or mutual-support groups.
Behavioral Treatments
Behavioral treatments—also known as alcohol counseling, or talk therapy, and provided by licensed therapists—are aimed at changing drinking behavior. Examples of behavioral treatments are brief interventions and reinforcement approaches, treatments that build motivation and teach skills for coping and preventing a return to drinking, and mindfulness-based therapies.
Mutual-Support Groups
Mutual-support groups provide peer support for stopping or reducing drinking. Group meetings are available in most communities at low or no cost, and at convenient times and locations—including an increasing presence online. This means they can be especially helpful to individuals at risk for relapse to drinking. Combined with medications and behavioral treatment provided by health care professionals, mutual-support groups can offer a valuable added layer of support.
Please note: People with severe AUD may need medical help to avoid alcohol withdrawal if they decide to stop drinking. Alcohol withdrawal is a potentially life-threatening process that can occur when someone who has been drinking heavily for a prolonged period of time suddenly stops drinking. Doctors can prescribe medications to address these symptoms and make the process safer and less distressing.
Can People With Alcohol Use Disorder Recover?
Many people with AUD do recover, but setbacks are common among people in treatment. Seeking professional help early can prevent a return to drinking. Behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Medications also can help deter drinking during times when individuals may be at greater risk of a return to drinking (e.g., divorce, death of a family member).
If you are concerned about your alcohol use and would like to explore whether you might have AUD, please visit the Rethinking Drinking website .
To learn more about alcohol treatment options and search for quality care near you, please visit the NIAAA Alcohol Treatment Navigator .
For more information about alcohol and your health, please visit: niaaa.nih.gov
1 SAMHSA, Center for Behavioral Health Statistics and Quality. 2023 National Survey on Drug Use and Health. Table 5.9A—Alcohol use disorder in past year: among people aged 12 or older; by age group, numbers in thousands, 2022 and 2023 [cited 2024 Sep 9]. Available from: https://www.samhsa.gov/data/report/2023-nsduh-detailed-tables
2 SAMHSA, Center for Behavioral Health Statistics and Quality. 2023 National Survey on Drug Use and Health. Table 5.9B—Alcohol use disorder in past year: among people aged 12 or older; by age group, percentages, 2022 and 2023 [cited 2024 Sep 9]. Available from: https://www.samhsa.gov/data/report/2023-nsduh-detailed-tables
3 Age at drinking onset: age when first drank a beverage containing alcohol (a can or bottle of beer, a glass of wine or a wine cooler, a shot of distilled spirits, or a mixed drink with distilled spirits in it), not counting a sip or two from a drink. AUD: having met two or more of the 11 AUD diagnostic criteria in the past-year according to the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) AUD risk across different ages at drinking onset is compared using the prevalence ratio weighted by the person-level analysis weight. Derived from the Center for Behavioral Health Statistics and Quality 2022 National Survey on Drug Use and Health (NSDUH-2022-DS0001) public-use file. [cited 2024 Jan 12]. Available from: https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2022-nsduh-2022-ds0001
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- When People Rebel 1857 and After Class 8 Case Study Social Science History Chapter 5
Last Updated on September 12, 2024 by XAM CONTENT
Hello students, we are providing case study questions for class 8 social science. Case study questions are the new question format that is introduced in CBSE board. The resources for case study questions are very less. So, to help students we have created chapterwise case study questions for class 8 social science. In this article, you will find case study for CBSE Class 8 Social Science History Chapter 5 When People Rebel 1857 and After. It is a part of Case Study Questions for CBSE Class 8 Social Science Series.
| When People Rebel 1857 and After | |
| Case Study Questions | |
| Competency Based Questions | |
| CBSE | |
| 8 | |
| Social Science – History | |
| Class 8 Studying Students | |
| Yes | |
| Mentioned | |
Table of Contents
Case Study Questions on When People Rebel 1857 and After Class 8
I. On 8 April 1857, a young soldier, Mangal Pandey, was hanged to death for attacking his officers in Barrackpore. Some days later, some sepoys of the regiment at Meerut refused to do the army drill using the new cartridges, which were suspected of being coated with the fat of cows and pigs. Eightyfive sepoys were dismissed from service and sentenced to ten years in jail for disobeying their officers. This happened on 9 May 1857.
Direction for question 1 to 5 given below: Based on the above passage choose the correct option:
1. Who was Mangal Pandey? (a) A British officer (b) A zamindar (c) A soldier of British army (d) A soldier of Mughal army
Difficulty Level: Easy
Ans. Option (c) is correct.
Q. 2. Why was Mangal Pandey hanged? (a) He started sepoy mutiny (b) He attacked British officer (c) He refused to use the cartridges (d) He did not pay the tax
Ans. Option (b) is correct. Explanation: Mangal Pandey, was hanged to death for attacking his officers in Barrackpore.
Q. 3. Sepoys who refused to do the army drill were from: (a) Delhi (b) Kanpur (c) Meerut (d) Awadh
Difficulty Level: Medium
Q. 4. Why did sepoys refuse to do the army drill? (a) due to low salary (b) due to poor service conditions (c) they believed that cartridges were coated with animal fat. (d) they were tired.
Q. 5. How many sepoys were dismissed (a) 82 (b) 83 (c) 84 (d) 85
Ans. Option (d) is correct.
- Agriculture Class 8 Case Study Social Science Geography Chapter 3
- Land, Soil, Water, Natural Vegetation and Wildlife Resources Class 8 Case Study Social Science Geography Chapter 2
- Judiciary Class 8 Case Study Social Science Civics Chapter 5
- Resources Class 8 Case Study Social Science Geography Chapter 1
- Understanding Laws Class 8 Case Study Social Science Civics Chapter 4
- Tribals, Dikus and the Vision of a Golden Age Class 8 Case Study Social Science History Chapter 4
- Why Do We Need A Parliament Class 8 Case Study Social Science Civics Chapter 3
- Understanding Secularism Class 8 Case Study Social Science Civics Chapter 2
- The Indian Constitution Class 8 Case Study Social Science Civics Chapter 1
- Ruling the Countryside Class 8 Case Study Social Science History Chapter 3

From Trade to Territory Class 8 Case Study Social Science History Chapter 2
How, when and where class 8 case study social science history chapter 1, you may also like.
- Assertion Reason Questions for Class 8 Social Science
- Revision Notes for Class 8 Social Science
- Assertion Reason Questions for Class 8 Science
- Assertion Reason Questions for Class 8 Maths
- Case Study Questions for Class 8 Science
- Case Study Questions for Class 8 Maths
Topics from which case study questions may be asked
Here is a list of topics from which case study questions may be asked.
- Understand the effect of policies and reforms on the Nawabs, Peasants, sepoys and on the society.
- Understand the causes and consequences of Mutiny.
- Understand the role of various leaders.
- Understand the causes of failure of the revolt of 1857.
- Understand the change in the policy of governance.
People resisted the policies of the British as they found that these policies would destroy their religion and social practices. This rebellion started with sepoy mutiny but soon it culminated into widespread massive rebellion. The British succeeded in repressing this revolt but the effect was so strong that they had to change the future policy of governance.
Frequently Asked Questions (FAQs) on When People Rebel 1857 and After Class 8 Case Study
Q1: what are case study questions.
A1: Case study questions are a type of question that presents a detailed scenario or a real-life situation related to a specific topic. Students are required to analyze the situation, apply their knowledge, and provide answers or solutions based on the information given in the case study. These questions help students develop critical thinking and problem-solving skills.
Q2: How should I approach case study questions in exams?
A2: To approach case study questions effectively, follow these steps: Read the case study carefully: Understand the scenario and identify the key points. Analyze the information: Look for clues and relevant details that will help you answer the questions. Apply your knowledge: Use what you have learned in your course to interpret the case study and answer the questions. Structure your answers: Write clear and concise responses, making sure to address all parts of the question.
Q3: What are the benefits of practicing case study questions from your website?
A3: Practicing case study questions from our website offers several benefits: Enhanced understanding: Our case studies are designed to deepen your understanding of historical events and concepts. Exam preparation: Regular practice helps you become familiar with the format and types of questions you might encounter in exams. Critical thinking: Analyzing case studies improves your ability to think critically and make connections between different historical events and ideas. Confidence: Practicing with our materials can boost your confidence and improve your performance in exams.
Q4: What are the important keywords in this chapter When People Rebel 1857 and After?
A4: Important keywords from chapter “When People Rebel 1857 and After” are given below- Firangi: Term used for foreigners as contempt. Suzerainty: The domain or area subject to a suzerain/ruler. Cartridges: A casing fitted with a bullet. Mutiny: Revolt or rebellion against constituted authority, especially by sailors and armed personnel against their officers. Sati: A rite to be performed by the Hindu woman on the death of her husband. The widow used to burn herself on the funeral pyre of her husband. Sepoy: An Indian soldier during colonial rule. Ghazis: An Arabic term which refers to a person who participates in military expeditions. Paramount: Supreme; more important than any other thing or person.
Q5: What are the important dates in this chapter “When People Rebel 1857 and After”?
A5: Important dates from chapter “When People Rebel 1857 and After” are given below- 1849: Announcement made by Lord Dalhousie that after the death of Bahadur Shah Zafar, the king’s family would be shifted out of the Red Fort and settled at some other place in Delhi. 1850: A new law was passed which made conversion into Christianity easier. 1856: (i) Governor General Canning decided that Bahadur Shah Zafar would be the last Indian king and after his death, his descendants would be recognized as mere princes and not the kings. (ii) The Company passed a new law which stated that every person who agreed to be employed in the Company’s army would have to serve overseas, if required. 8th April 1857: Mangal Pandey, an Indian soldier, was hanged for attacking British officials in Barrackpore. 9th May 1857: Sepoys revolted at several places. 10th May 1857: Sepoys moved towards Delhi from Meerut. September 1857: Delhi was reoccupied from the revolutionaries. October 1858: Mughal Emperor Bahadur Shah Zafar was imprisoned in Rangoon jail along with his wife Begum Zinat Mahal. 1858: Powers of the East India Company were transferred to the British Crown through a new Act passed by the British Parliament. November 1862: Bahadur Shah Zafar died in Rangoon jail.
Q6: Who was Nana Sahib?
A6: The adopted son of Peshwa Baji Rao II.
Q7: Who was Subedar Sitaram Pande?
A7: Sitaram Pande was a sepoy of Bengal Native Army. He was recruited in 1812 and retired in 1860. He helped the British in suppressing the rebellion, though his own was a rebel.
Q8: How did the nawabs and rajas lose their power?
A8: Since the mid-eighteenth century, there was a steady decline in the powers of the nawabs and rajas: They gradually lost their honour and authority. The residents stationed in their courts interfered in the matters of the state and also curbed the freedom of the rulers. The rulers’ armed forces were disbanded and their revenues and territories were taken away by stages. Awadh was taken away on the pretext of being misgoverned by its ruler.
Q9: What problems did the sepoys face under the British Regiment?
A9: The sepoys were unhappy with the wages and conditions of service. Some practices were against their religion.
Q10: Are there any online resources or tools available for practicing When People Rebel 1857 and After case study questions?
A10: We provide case study questions for CBSE Class 8 Social Science on our website . Students can visit the website and practice sufficient case study questions and prepare for their exams.
Related Posts

- Climate crisis
- Environment
- Global development
Transparent skin, bird flu, and why girls’ brains aged during Covid: the week in science – podcast

- Apple Podcasts
Presented by Ian Sample with Hannah Devlin ; produced by Ellie Sans; sound design by Tony Onuchukwu ; the executive producer is Ellie Bury
Thu 12 Sep 2024 05.00 BST
- Share on Facebook
- Share on Twitter
- Share via Email
Ian Sample and science correspondent Hannah Devlin discuss some of the science stories that have made headlines this week, from a new technique that uses food colouring to make skin transparent, to the first case of bird flu in a person with no known contact with sick animals, and a study looking at premature brain ageing in young people during Covid
How to listen to podcasts: everything you need to know
Clips: NBC News, KVUE
Common food dye found to make skin and muscle temporarily transparent
Missouri sees first positive bird flu case without known animal contact
Covid lockdowns prematurely aged girls’ brains more than boys’, study suggests

The Guardian is editorially independent. And we want to keep our journalism open and accessible to all. But we increasingly need our readers to fund our work.
- Science Weekly
- Coronavirus
- Neuroscience
- Young people
- Medical research
Most popular
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election results
- Google trends
- AP & Elections
- Paralympic Games
- College football
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Justin Timberlake reaches plea deal to resolve drunken driving case, AP source says
FILE - Justin Timberlake appears at the premiere of “Trolls Band Together” in Los Angeles on Nov. 15, 2023. (Photo by Richard Shotwell/Invision/AP, File)
FILE - Justin Timberlake performs at the Pilgrimage Music and Cultural Festival in Franklin, Tenn., on Sept. 23, 2017. (Photo by Amy Harris/Invision/AP, File)
FILE - Justin Timberlake appears at the Vanity Fair Oscar Party in Beverly Hills, Calif., on March 10, 2024. (Photo by Evan Agostini/Invision/AP, File)
- Copy Link copied

NEW YORK (AP) — Justin Timberlake is scheduled to enter a new plea Friday in his drunken driving case in New York’s Hamptons, prosecutors said. Details of the plea weren’t disclosed, but a person with knowledge of the deal said Timberlake has agreed to plead guilty to a less serious offense than the original charge of driving while intoxicated.
The person spoke to The Associated Press on condition of anonymity because they were not authorized to speak publicly about the case.
Timberlake’s attorney, Edward Burke, declined to comment.
The pop singer is set to appear in person on Friday in Sag Harbor Village Court to enter a plea, Suffolk County District Attorney Ray Tierney’s office confirmed Wednesday.
Timberlake was arrested in the village of Sag Harbor, on the eastern end of Long Island, on June 18 after police said he ran a stop sign in the village center, veered out of his lane and got out of his BMW smelling of alcohol. The 43-year-old Tennessee native pleaded not guilty to a misdemeanor drunken driving charge.
At a hearing last month , a judge suspended Timberlake’s right to drive in New York.
His lawyer, Burke, has maintained that Timberlake was not drunk and that the case should be dropped.
Timberlake was pulled over after leaving a Sag Harbor hotel around 12:30 a.m., according to police.
“His eyes were bloodshot and glassy, a strong odor of an alcoholic beverage was emanating from his breath, he was unable to divide attention, he had slowed speech, he was unsteady afoot and he performed poorly on all standardized field sobriety tests,” police said in a court filing.
Timberlake told the officer he had had one martini and was following some friends home, according to police. He was arrested and spent the night in custody at a police station.
The boy band singer-turned-solo star and actor’s agent and other representatives didn’t immediately respond to emails seeking comment Wednesday.
A 10-time Grammy winner, Timberlake began performing as a young Disney Mouseketeer, rose to fame as part of the boy band NSYNC and embarked on a solo recording career in the early 2000s.
Sag Harbor is a one-time whaling village mentioned in Herman Melville’s classic novel “Moby-Dick” that’s nestled amid the Hamptons, around 100 miles (160 kilometers) east of New York City.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Alcohol-induced blackouts: A review of recent clinical research with practical implications and recommendations for future studies
Reagan r. wetherill.
1 Center for Studies of Addiction, Department of Psychiatry, Perelman School of Medicine of the University of Pennsylvania, Philadelphia, PA 19104
2 Department of Psychology, University of Texas at Austin, Austin, TX 78712
Alcohol-induced blackouts, or memory loss for all or portions of events that occurred during a drinking episode, are reported by approximately 50% of drinkers and are associated with a wide range of negative consequences, including injury and death. As such, identifying the factors that contribute to and result from alcohol-induced blackouts is critical in developing effective prevention programs. Here, we provide an updated review (2010–2015) of clinical research focused on alcohol-induced blackouts, outline practical and clinical implications, and provide recommendations for future research.
A comprehensive, systematic literature review was conducted to examine all articles published between January 2010 through August 2015 that focused on examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts.
Twenty-six studies reported on alcohol-induced blackouts. Fifteen studies examined prevalence and/or predictors of alcohol-induced blackouts. Six publications described consequences of alcohol-induced blackouts, and five studies explored potential cognitive and neurobiological mechanisms underlying alcohol-induced blackouts.
Conclusions
Recent research on alcohol-induced blackouts suggests that individual differences, not just alcohol consumption, increase the likelihood of experiencing an alcohol-induced blackout, and the consequences of alcohol-induced blackouts extend beyond the consequences related to the drinking episode to include psychiatric symptoms and neurobiological abnormalities. Prospective studies and a standardized assessment of alcohol-induced blackouts are needed to fully characterize factors associated with alcohol-induced blackouts and to improve prevention strategies.
Introduction
Alcohol use is a pervasive problem with well-known deleterious effects on memory. Alcohol-induced memory impairments vary in severity, ranging from mild deficits to alcohol-induced blackouts ( Heffernan, 2008 ; White, 2003 ). Alcohol-induced blackouts are defined as amnesia, or memory loss, for all or part of a drinking episode. During a blackout, a person is able to actively engage and respond to their environment; however, the brain is not creating memories for the events. Alcohol-induced blackouts are often confused with passing out from alcohol, but blacking out and passing out are very different states of consciousness. A person experiencing a blackout is conscious and interacting with his or her environment; whereas, a person who has passed out from alcohol has lost consciousness and capacity to engage in voluntary behavior. Memory deficits during a blackout are primarily anterograde, meaning memory loss for events that occurred after alcohol consumption ( White, 2003 ). It is important to note that short-term memory remains intact during an alcohol-induced blackout, and as such, an intoxicated person is able to engage in a variety of behaviors, including having detailed conversations and other more complex behaviors like driving a vehicle, but information about these behaviors is not transferred from short-term to long-term memory, which leads to memory deficits and memory loss for these events ( White, 2003 ). There is no objective evidence that a person is in an alcohol-induced blackout ( Pressman and Caudill, 2013 ), thus it can be difficult or impossible to know whether or not a drinker is experiencing a blackout ( Goodwin, 1995 ). This is similar to the fact that one cannot know whether another person has a headache; the experience is happening inside that person’s brain, with no clear observable indices.
Based on the duration and extent of alcohol-induced memory loss, researchers have described two qualitatively distinct types of blackouts: en bloc and fragmentary ( Goodwin et al., 1969a ; Goodwin et al., 1969b ). En bloc blackouts typically occur at higher blood alcohol concentrations (BAC), have a distinct onset, and involve complete memory loss for a specific period of the drinking event. Fragmentary blackouts (also known as “brown outs” or “gray outs”), however, involve partial amnesia during a drinking episode, but one may be able to recall events of the episode with relevant cues ( Jennison and Johnson, 1994 ). Fragmentary blackouts occur more frequently than en bloc blackouts ( Goodwin et al., 1969b ; Hartzler and Fromme, 2003 ; White et al., 2004 ), but neither type appear to occur until breath alcohol concentrations (BrACs) are 0.06 g/dl or greater ( Hartzler and Fromme, 2003 ). Estimates of BrACs indicated that most blackouts occurred around 0.20 g/dl, but as low as 0.14 g/dl ( Ryback, 1970 ). According to a study of amnesia in people arrested for alcohol-related offenses ( Perry et al., 2006 ), the probability of a fragmentary or an en bloc blackout was 50/50 at a BrAC of 0.22 g/dl and the probability of an en bloc blackout was 50/50 at a BrAC of 0.31 g/dl. As such, blackouts typically occur during binge or excessive drinking episodes. Further, gulping drinks and drinking on an empty stomach ( Goodwin, 1995 ; Perry et al., 2006 ), which cause a rapid rise and high peak BAC, can also increase the likelihood of experiencing an alcohol-induced blackout.
Although alcohol-induced blackouts were previously thought to occur only in individuals who were alcohol dependent ( Jellinek, 1946 ), we now know that blackouts are quite common among healthy young adults. In fact, approximately 50% of college students who consume alcohol report having experienced an alcohol-induced blackout ( Barnett et al., 2014 ; White et al., 2002 ). Consequently, there has been increased media and research interest in alcohol-induced blackouts over the past two decades with at least three reviews describing the phenomenon ( Lee et al., 2009 ; Rose and Grant, 2010 ; White, 2003 ) a brief, descriptive section in a review on excessive alcohol use ( White and Hingson, 2013 ) and a recently published memoir that poignantly describes the phenomenology of blackouts ( Hepola, 2015 ) ( Figure 1 ). Therefore, this systematic review provides an update (2010–2015) on the clinical research focused on alcohol-induced blackouts, outlines practical and clinical implications, and provides recommendations for future research.

Number of published journal articles or reviews that evaluate alcohol-induced blackouts per year (1985 to 2015). The graph represents published articles and reviews published in English and includes both animal and human studies with the terms “blackout” and “alcohol” in the title, abstract, and/or keyword.
Materials and Methods
A Medline search was conducted in September 2015 to identify publications that included either “alcohol” or “ethanol” as one search term and at least one blackout-related search term (e.g., “blackouts”, “blacked out”). The wildcard character “*” was used to include all forms of the root word. The most recent review of blackouts was published in 2010 ( Rose and Grant, 2010 ) and there has since been extensive new research; therefore we limited our review to articles published between January 2010 and August 2015. After removing duplicates, case studies, articles that were not published in English, and studies not conducted in humans, the remaining publications were reviewed to determine whether they met inclusion criteria, namely that the study examined vulnerabilities, consequences, and possible mechanisms for alcohol-induced blackouts.
Study Characteristics
A total of 26 publications met the criteria to be included in the review (see Table 1 for study details). Fifteen studies examined prevalence and/or predictors of alcohol-induced blackouts. Six publications described consequences of alcohol-induced blackouts, and five studies explored potential cognitive and neurobiological mechanisms underlying alcohol-induced blackouts.
Characteristics of Published Studies Examining Alcohol-Induced Blackouts between 2010 and 2015
| Study reference | Design | Sample | Methods | Blackout-related findings |
|---|---|---|---|---|
| Multisite, multicohort, prospective | 1,053 first-year college students, Ages: 16–21 (M=18.4), 58% female | Blackouts and getting physically sick were most common negative consequences 54.2% of subjects endorsed a blackouts during first year of college Almost 1 in 5 drinking weeks resulted in a blackout | ||
| Cross-sectional | 307 incoming freshman college students, 59% female | Freshman who Drink to Get Drunk (DTGD) were more likely to have consumed alcohol prior to going out, participated in a drinking game, drank heavily on a non-school night, used liquor/beer, combined alcohol and drugs, experienced a hangover, vomited, passed out, and/or blacked out 50% of those who DTGD endorsed a blackout during past 30 days | ||
| Cross-sectional | 150 21-year-olds, 50% female | birthday celebration | 40% reported experiencing a blackout during their 21 birthday celebration Physical (e.g., blackout and hangover) and behavioral risks were predicted by higher estimated BACs | |
| Prospective | 166 subjects from the community who consume alcohol, Ages: 23–29 (M=25.9), 60% female | Drinking in hazardous situations, blackouts, and tolerance were most common alcohol problem Blackouts were more prevalent in whites and males Age of onset for blackouts occurred at ~19 years of age | ||
| Cross-sectional | 272 college students, Ages: 18–25 (M=19.9), 52% male | Binge drinkers were more likely to define binge drinking in an extreme manner such that the drinking results in vomiting or blacking out | ||
| Cross-sectional | 942 Australian university students participating in an Internet-based intervention trial and scored ≥8 on AUDIT, Ages: 17–24 (M=19.4), 53% male | Blackouts were one of the most frequently reported non-academic problem (44.8%) Several negative consequences, including blackouts, were rated as positive by a large proportion of the sample | ||
| Multisite, cross-sectional | 2,546 college students, 59% female | 25% of students reported blacking out during at least one occasion in which prepartying occurred in the past 30 days Greek affiliation, family history of alcohol abuse, frequency of prepartying, and both playing drinking games and consuming shots of liquor while prepartying increased the likelihood of blacking out | ||
| Prospective | 1,154 young adults, Mean age 23.8 years, 65% female | 66% of sample reported experiencing an alcohol-induced blackout Women were more likely to report blackouts than men Compared with women with a maternal family history of problematic alcohol use, men with a maternal family history of problematic alcohol use were more than twice as likely to report blackouts | ||
| Cross-sectional | 192 regularly drinking college students, Ages: 18–24 (M=19.1), 52% male | SEM analyses revealed a direct association between enhancement motives and blackouts | ||
| Prospective | 552 college students, Ages: 18–24, 57% age 21, 62% female | SEM analyses revealed an indirect association between enhancement motives at Time 1 and blackouts at Time 2 through increased levels of alcohol use at Time 2 | ||
| Prospective | 336 first-year student drinkers, Ages: 18–20 (M=18.2), 53% male | Students who reported higher levels of alcohol quantity across events were more likely to report experiencing blackout Controlling for individual differences in typical drinking, those who played drinking games more frequently were more likely to experience a blackout When women, compared to men, consumed 1 more drink than their usual amount, odds of experiencing a blackout increased by 13% | ||
| Field study | 1,222 nightclub patrons in Sao Paulo, Brazil, Ages: 51% ≤ 24, 57% male | Blackouts were more prevalent in those who engaged in binge drinking while at the nightclub | ||
| Prospective | 1,402 drinking adolescents, Ages: 15–19 (M=15.5), 60% female | In the 2 years prior to age 15, almost 30% of youth reported experiencing an alcohol-induced blackout At age 19, 74% of youth reported experiencing an alcohol-induced blackout Four latent trajectory classes were identified: Class 2 was used as a reference and predictors included female sex, higher drinking, smoking, externalizing characteristics, and estimated peer substance involvement | ||
| Multisite, cross-sectional | 757 9 and 10 grade students in Germany Ages: 15–16 (M=15.6) 50% female | Predrinking is associated with experiencing alcohol-induced blackouts | ||
| Prospective | 829 college students Mean age of 21.8 years 66% female | Alcohol dependence symptoms in Year 4 predicted increased frequency of blackouts and social/emotional consequences during the following year Blackouts during Year 4 predicted increased alcohol-related social and emotional consequences, but not alcohol dependence symptoms in Year 5 | ||
| Cross-sectional | 42,347 subjects, 54% female | Blackouts were associated with suicidal ideation and suicidal attempts in males, and suicidal ideation in females | ||
| Multisite, prospective | 954 undergraduate and graduate students, Ages: 18–41, 44% between the ages 18–20, 51% female | At baseline, 52% of males and 50% of females had experienced an alcohol-induced blackout in the past year One in eight emergency department visits over a two-year period were associated with blackouts Estimates indicated that blackout-associated emergency department visit costs ranged from $469,000–$546,000/year | ||
| Multisite, prospective | 954 undergraduate and graduate students, Ages: 18–41, 44% ages 18–20, 51% female | Approximately 7% of the sample reported experiencing 6 or more blackouts in the past year Alcohol-induced blackouts at baseline exhibited a dose-response on odds of alcohol-related injury during follow-up increasing from 1.57 among those who reported 1–2 blackouts to 2.64 for those reporting six or more blackouts | ||
| Multisite, cross-sectional | 188 AUD patients in residential alcohol treatment, Ages: 14–64, median=35, 89% male | History of alcohol-induced blackouts was predictive of comorbid MD diagnosis | ||
| Prospective | 997 incoming first year college students, Ages: 18–24 (M=18.1), 65% female | Blackout experience during the first year predicted later increases in drinking among males Blackout experience during the first year predicted decreased drinking the following year among females | ||
| Prospective | 23 heavy episodic drinking youth and 23 demographically-matched non-drinking youth, Ages: 16–18 (M=17.7), 50% female | Heavy episodic drinking youth responded with greater emotional response to the PASAT-C, but emotional responses decreased with sustained abstinence Among heavy episodic drinking youth, greater lifetime and recent alcohol consumption, alcohol-induced blackouts, and withdrawal symptoms were associated with increased negative affect with PASAT-C exposure | ||
| Cross-sectional | 64 patients with bipolar disorder and 49 controls, Ages: 18–30 (M=23), 66% female | H-MRS | In both patients and controls, reduced hippocampal-GSH was associated with blackout presence/severity | |
| Cross-sectional | 48 young adults were included in analyses (21 binge drinkers and 27 light drinkers) Ages: 18–24 ~50% female | H-MRS | Overall, binge drinkers had lower gamma amino-butyric acid and N-acetyl-aspartate in the anterior cingulate cortex than light drinkers When stratified by blackout history, binge drinkers with a history of blackouts had lower anterior cingulate cortex glutamate than light drinkers | |
| Multicohort, prospective | 60 substance-naïve youth who later transition into heavy drinking and experienced a blackout ( =20) or not ( =20) or youth who remain abstinent ( =20) Ages: 12–14 at baseline 55% male | Prior to initiating substance use, youth who later transitioned into heavy drinking and experienced blackouts showed greater activation during inhibitory processing than nondrinkers and youth who transitioned into heavy drinking but did not experience blackouts Mean activation during correct inhibitory processing in the left and right middle frontal brain regions at baseline predicted future blackout experience, after controlling for follow-up externalizing behaviors and lifetime alcohol consumption | ||
| Cross-sectional | 88 college students who consume alcohol (44 with a history of fragmentary blackouts; 44 without a history of blackouts) Ages: 21–22 (M=21.6) 50% female | Individuals with and without a history of blackouts showed similar memory performance when sober Individuals who consumed alcohol and had a positive history of fragmentary blackouts showed greater contextual memory impairments than those who had not previously experienced a blackout | ||
| Cross-sectional | 24 college students who consume alcohol (12 with a history of fragmentary blackouts and 12 without a history of fragmentary blackouts) Ages: 21–23 (M=21.3) 50% female | Groups did not show significant differences when sober Individuals with a history of fragmentary blackouts showed attenuated neural responses to contextual memory recollection in the right posterior parietal cortex and bilateral dorsolateral PFC | ||
AEQ-A, Alcohol Expectancy Questionnaire – Adolescent; BPRS, APS, Alcohol Problems Scale; AREAS, Academic Role Expectations and Alcohol Scale; AUD, alcohol use disorder; AUDIT, Alcohol Use Disorders Identification Test; BDI-II, Beck Depression Inventory-II; BIS-11, Barratt Impulsiveness Scale; BPRS, Brief Psychiatric Rating Scale; BrAC, breathe alcohol concentration; BSSS, Brief Sensation-Seeking Scale; CBCL, Child Behavior Checklist; CDDR, Customary Drinking and Drug Use Record; CIDI, Composite International Diagnostic Interview; DASS, Depression Anxiety Stress Scale; DDQ, Daily Drinking Questionnaire; ESYTC, Edinburgh Study of Youth Transitions and Crime; FHAM, Family History Assessment Module; FTQ, Family Tree Questionnaire; GNG, go-nogo; GSH, glutathione; HDRS, Hamilton Depression Rating Scale; 1 H-MRS, Proton magnetic resonance imaging spectroscopy; HSS, Health Screening Survey; IPAS, Important People and Activities Scale; IPIP-NEO, International Personality Inventory Pool form of the NEO 5-factor Personality Inventory; MD, major depression, MEPS, Medical Expenditure Panel Survey; MRI, magnetic resonance imaging; PANAS, Positive and Negative Affect Scale; PASAT-C, Paced Auditory Serial Addition Test-Computerized Version; PDS, Pubertal Development Scale; POMS, Profile of Mood States; RAPI, Rutgers Alcohol Problem Index; SCID, Structured Clinical Interview for DSM Disorders; SDQ, Strengths and Difficulties Questionnaire; SEM, Structural equation modeling; SRE, Self-ratings of the effects of alcohol; SSAGA-I, Semi-Structured Assessment for the Genetics of Alcoholism-I; STAI, State-Trait Anxiety Inventory; TLFB, Timeline Followback; TMT, Trail Making Test, WAIS-III, Wechsler Adult Intelligence Scale – 3 rd edition; WASI, Wechsler Abbreviated Scale of Intelligence; WHO-ASSIST, World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test; WMS-III, Wechsler Memory Scale – 3 rd edition; WRAT, Wide Range Achievement Test; YAACQ, Young Adult Alcohol Consequences Questionnaire; YAAPST, Youth Adult Alcohol Problems Screening Test; YMRS, Young Mania Rating Scale; YSR/ASR, Youth Self-Report/Adult Self-Report.
Prevalence and Predictors of Alcohol-Induced Blackouts
The majority of the publications identified for this review examined binge drinking and alcohol-related consequences, including blackouts, among young adults and college students and reported prevalence rates ranging from approximately 20–55% ( Barnett et al., 2014 ; Boekeloo et al., 2011 ; Brister et al., 2011 ; Chartier et al., 2011 ; Clinkinbeard and Johnson, 2013 ; Hallett et al., 2013 ; Sanchez et al., 2015 ; Wilhite and Fromme, 2015 ). Although prevalence rates were typically around 50%, one study reported a prevalence rate of only about 20%; however, this was a qualitative study examining how university students define binge drinking ( Clinkinbeard and Johnson, 2013 ). As such, participants were not directly asked whether they had experienced an alcohol-induced blackout, but rather participants were asked to describe binge drinking and then researchers categorized whether the responses described alcohol-induced blackouts. In addition to their prevalence rate of 54%, Barnett and colleagues (2014) found that college students reported experiencing an alcohol-induced blackout nearly once every five drinking weeks during the first year of college. Thus, alcohol-induced blackouts are not only common among those who consume alcohol, but also recur over time.
Using longitudinal methods, Schuckit and colleagues (2015) and Wilhite and Fromme (2015) focused specifically on prospective analyses of alcohol-induced blackouts. Schuckit and colleagues (2015) used latent class growth analysis to evaluate the pattern of occurrence of alcohol-induced blackouts across 4 time points in 1,402 drinking adolescents between the ages of 15–19. Surprisingly, 30% of the adolescents reported experiencing an alcohol-induced blackout at the age of 15, which increased to 74% at age 19. Analyses revealed 4 classes in the patterns of the occurrence for blackouts (i.e., no blackouts, blackouts rapidly increasing with age, blackouts slowly increasing, and blackouts consistently reported), with female sex, higher drinking quantities, smoking, externalizing characteristics, and estimated peer substance use predicting class membership ( Schuckit et al., 2015 ). In general, these findings are consistent with previous research ( Rose and Grant, 2010 ; White et al., 2002 ) and indicate that alcohol-induced blackouts are common even among early adolescents, which is particularly concerning given that the adolescent brain is undergoing significant developmental changes.
Wilhite and Fromme (2015) examined the associations between alcohol-induced blackouts, alcohol dependence symptoms ((as measured by the Rutgers Alcohol Problem Index ( White and Labouvie, 1989 )), and social and emotional negative consequences across 2 years among 829 young adults who were transitioning out of college. They found that alcohol dependence symptoms predicted an increased frequency of blackouts and consequences the following year. Alcohol-induced blackouts during the past three months prospectively predicted increased social and emotional negative consequences, but not alcohol dependence symptoms the following year. These findings contradict Jellinek’s theory of alcoholism, which posits that alcohol-induced blackouts are a precursor of alcoholism ( Jellinek, 1952 ).
Potential genetic influences
Behavioral genetic research suggests that there is a heritable component to experiencing alcohol-induced blackouts ( Luczak et al., 2006 ; Nelson et al., 2004 ; Slutske et al., 1999 ). Two recent studies explored genetic influences by examining the potential effects of family history of alcohol problems on blackout occurrence ( LaBrie et al., 2011 ; Marino and Fromme, 2015 ). In a study of 2,546 college students, LaBrie and colleagues (2011) found that a family history of alcohol problems increased the likelihood of blacking out. Using data from a longitudinal study of college students, Marino and Fromme (2015) explored whether maternal or paternal family history of problematic alcohol use were better predictors than a general measure of overall family history on the likelihood of experiencing an alcohol-induced blackout. They further tested whether gender moderated the association in a sample of 1,164 college students. Although prenatal alcohol exposure was not assessed and could influence findings, the researchers found that compared to women with a maternal history of problematic alcohol use, men with a maternal history of problematic alcohol use were more than twice as likely to report experiencing an alcohol-induced blackout.
Based on the Marino and Fromme (2015) findings, one could speculate that a genetic vulnerability to alcohol-induced blackouts is expressed only under certain environmental conditions, representing a possible gene by environment interaction. For example, a mother with problematic drinking habits might contribute to an environment that is characterized by lower parental monitoring and increased alcohol availability. These environmental factors, in turn, could create stress and contribute to early initiation of alcohol use and maladaptive drinking behaviors in her offspring, especially sons, who are genetically predisposed to alcohol misuse and alcohol-induced blackouts. Given the potential impact of these findings on prevention and intervention programs, additional research examining genetic and environmental factors contributing to alcohol-induced blackouts is needed.
Prepartying and drinking games
Three studies examined high-risk drinking behaviors common among young adults known as “prepartying,” “pregaming,” and “drinking games” ( LaBrie et al., 2011 ; Ray et al., 2014 ; Wahl et al., 2013 ). Typically, these drinking behaviors involve fast-paced drinking over a short period of time and can cause a rapid rise and high peak BAC, which increases the likelihood of experiencing an alcohol-induced blackout ( Goodwin, 1995 ; Perry et al., 2006 ). LaBrie and colleagues (2011) examined risk factors for blackouts among 2,546 college students who reported past month prepartying. Of these students, 25% reported blacking out during at least one occasion over the past month when prepartying had occurred. Similarly, Wahl and colleagues (2013) examined predrinking and associated behaviors among 757 German high school students and found that those who reported engaging in predrinking were more likely to experience alcohol-induced blackouts. Using an event-level approach, Ray and colleagues (2014) found that students consumed more alcohol during drinking game events compared to non-drinking game events, and all students were more likely to experience an alcohol-induced blackout during events when drinking games occurred. This provides additional support for the importance of drinking style (e.g., pace and type of alcohol), as well as amount of alcohol consumed, in the occurrence of alcohol-induced blackouts.
Drinking motives
Because drinking motives are predictors of alcohol use and consequences, recent research has also examined the association between drinking motives and alcohol-induced blackouts ( Boekeloo et al., 2011 ; Merrill and Read, 2010 ; Merrill et al., 2014 ). Merrill and Read (2010) examined whether affect-relevant motivations for alcohol use (i.e., coping: drinking to alleviate negative affect; enhancement: drinking to increase positive affect) were associated with specific types of consequences, including alcohol-induced blackouts, in 192 regularly drinking college students. Using structural equation modeling (SEM), the authors reported a direct path between enhancement motives and blackouts, suggesting that individuals who drink to increase positive affect might consume alcohol in a manner that results in a rapid increase in BAC and alcohol-induced blackouts, such as taking shots of liquor or drinking rapidly. Merrill and colleagues (2014) conducted a follow-up, longitudinal study examining whether coping and enhancement motives predicted alcohol consequences, including alcohol-induced blackouts, over the course of one year in 552 college students and reported that enhancement motives indirectly predicted blackouts the following year. Although enhancement motives did not directly predict alcohol-induced blackouts in the longitudinal study, drinking to increase positive affect seems to involve a style of drinking that increases the likelihood of blackouts.
Boekeloo and colleauges (2011) examined a different type of drinking motive -“drinking to get drunk,” which the authors defined as “pre-meditated, controlled, and intentional consumption of alcohol to reach a state of inebriation” (p. 89). They explored the prevalence and correlates of this type of drinking behavior in 307 incoming freshman who reported consuming alcohol over the past 30 days. Nearly 77% of the incoming freshmen reported drinking alcohol in a pre-meditated, intentional manner with the goal of becoming intoxicated. Compared to those who did not drink to get drunk, individuals who reported drinking to get drunk were more likely to experience an alcohol-induced blackout. Further, consistent with the prepartying and drinking games studies described previously ( LaBrie et al., 2011 ; Ray et al., 2014 ; Wahl et al., 2013 ), individuals who reported drinking to get drunk were also more likely to have prepartied and participated in drinking games.
Consequences of Alcohol-Induced Blackouts
As indicated by the research described above, alcohol-induced blackouts typically occur following a rapid rise and high peak level of alcohol intoxication, and as such, alcohol-induced blackouts are associated with and predictive of other consequences and behaviors. Using SEM, Read and colleagues (2013) examined whether alcohol-related consequences, including alcohol-induced blackouts, predicted college students’ alcohol consumption one year later and whether these associations differed between men and women. Findings revealed that alcohol-induced blackouts during the first year of college predicted alcohol use the following year, with blackouts predicting later drinking increases in men and decreases in women ( Read et al., 2013 ). Further, using data from a randomized controlled trial of screening and brief physician intervention for problem alcohol use among 954 undergraduate and graduate students, Mundt and colleagues (2012) examined whether baseline alcohol-induced blackouts prospectively identified individuals with alcohol-related injury over the subsequent 2 years after controlling for heavy drinking days ( Mundt and Zakletskaia, 2012 ; Mundt et al., 2012 ). Findings indicated that alcohol-induced blackouts at baseline predicted alcohol-related injury over time with individuals who reported experiencing 1–2 blackouts at baseline being 1.5 times more likely to experience an alcohol-related injury, and those who reported 6 or more blackouts being over 2.5 times more likely to experience an alcohol-related injury. Mundt and Zakletskaia (2012) conducted a follow-up analysis on the same sample and found that one in eight emergency department visits for alcohol-related injuries involved an alcohol-induced blackout. Thus, among young adults, experiencing a blackout increases the likelihood of having an alcohol-related injury over time, even after controlling for heavy drinking.
Recent research has also investigated the associations between alcohol-induced blackouts and psychiatric symptomatology ( Bae et al., 2015 ; Neupane and Bramness, 2013 ; Winward et al., 2014 ). Using data provided by the Korea National Health and Nutritional Examination Survey from 2007–2011, Bae and colleagues (2015) examined associations between alcohol consumption and suicidal behavior in 42,347 Korean subjects and reported that alcohol-induced blackouts were associated with suicidal ideation and suicide attempts in males and suicidal ideation in females. Further, in a sample of 188 Nepalese patients in treatment for alcohol use disorder, a history of alcohol-induced blackouts was predictive of having comorbid major depression ( Neupane and Bramness, 2013 ).
Winward and colleagues (2014) used the Paced Auditory Serial Attention Test (PASAT-C) Computer Version to examine affective reactivity, cognitive performance, and distress tolerance in relation to blackouts, during early abstinence among 23 heavy episodic drinking adolescents (ages 16–18) compared to 23 matched, non-drinking controls. Findings revealed that heavy episodic drinking adolescents responded with greater emotional response to the PASAT-C compared to controls, and among heavy episodic drinking adolescents, greater frequency of alcohol-induced blackouts during the past three months was correlated with greater increases in frustration and irritability during the PASAT-C. Overall, these findings suggest that alcohol-induced blackouts can have profound effects on an individual’s overall health and well-being, above and beyond the effects of heavy alcohol consumption.
Potential Neurobiological Mechanisms of Alcohol-Induced Blackouts
Although early theories posited that alcohol’s effects on cognition and behavior were due to alcohol’s general disruption of brain function and depression of the central nervous system, preclinical and clinical research now indicates that alcohol-induced cognitive and memory deficits are caused by alcohol’s effects on the hippocampus and related neural structures ( Figure 2 ) ( White et al., 2000 ). Briefly, the hippocampus is a brain structure involved in memory formation for events and has been found to be particularly sensitive to alcohol. Indeed, animal research published prior to the period of the current review revealed that blackouts are caused by alcohol disrupting the transfer of information from short-term to long-term memory by interfering with hippocampal, medial septal, and frontal lobe functioning ( White, 2003 ; White et al., 2000 ). Although the mechanism of alcohol-induced blackouts is now known, our understanding of the specific neurobiological vulnerability and why some individuals are more likely to experience alcohol-induced blackouts while others are not has been an area of growing interest.

General overview of alcohol’s effects on memory and alcohol-induced blackouts. Top panel: Sagittal representation of the human brain and the primary structures and associations involved in episodic memory. Bottom panel: A general model of memory formation, storage, and retrieval reproduced with permission from the National Institute on Alcohol Abuse and Alcoholism publication ( White, 2003 ). Alcohol interferes with all stages of the memory process, but the alcohol’s primary effect appears to be on the transfer of information from short-term to long-term storage. Intoxicated individuals are typically able to recall information immediately after it is presented and can keep the information active in short-term memory for one minute or more if they are not distracted. Individuals may also be able to recall long-term memories formed before they became intoxicated; however, after just one or two drinks, individuals show memory impairments. Alcohol can interfere with these memory processes so severely that once sober, the individual is not able to recall all or portions of the events that occurred during the drinking episode.
Contextual memory (often described more broadly as source memory) refers to memory for details associated with a specific event (e.g., where a person was for the event, who was at the event). These memory details facilitate recall by enabling a person to consciously re-experience past events ( Tulving, 2002 ). As such, Wetherill and Fromme (2011) examined the effects of acute alcohol consumption on contextual memory and recall among individuals with and without a history of fragmentary blackouts in an attempt to better understand why some individuals experience alcohol-induced memory impairments whereas other do not, even when these individuals have similar drinking histories and are at comparable BrACs ( Wetherill and Fromme, 2011 ). Using longitudinal data to identify 88 young adults (mean age: 21.6 years ± 0.5; alcohol consumed 3 times a week, 3 standard drinks per occasion over the past 3 months) with ( n= 44) and without ( n= 44) a history of alcohol-induced blackouts who reported comparable drinking histories, denied other illicit drug use, and were demographically matched, Wetherill and Fromme conducted an alcohol administration (target BrAC of .08 g/dl versus no alcohol) with memory assessments and found that while sober, individuals with and without a history of alcohol-induced blackouts did not differ in memory performance; however, after alcohol consumption, individuals with a history of blackouts exhibited contextual memory impairments, while those without a history of blackouts did not.
Wetherill and colleagues (2012) conducted a follow-up study that used a within subject alcohol challenge followed by two functional magnetic resonance imaging (fMRI) sessions under no alcohol and alcohol (target BrAC of .08 g/dl) conditions. During fMRI scanning, participants completed a contextual memory task. Findings again revealed that individuals with and without a history of fragmentary blackouts did not differ in contextual memory performance or neural activity while sober, yet after alcohol consumption, individuals with a history of fragmentary blackouts showed less neural activation during encoding and recollection of contextual details in prefrontal and parietal regions, suggesting that alcohol had differential effects on frontoparietal brain activity ( Wetherill et al., 2012 ).
Subsequently, Wetherill and colleagues (2013) explored whether frontoparietal abnormalities exist among substance-naïve youth who later transition into heavy drinking and experience alcohol-induced blackouts. Specifically, 60 substance-naïve youth completed fMRI scanning during a go/no-go response inhibition task shown to engage frontal and posterior parietal brain regions ( Tapert et al., 2007 ) at baseline and were followed annually. After approximately five years, youth had either remained substance-naïve ( n =20) or had transitioned into heavy drinking and were classified as either alcohol-induced blackout positive ( n =20) or alcohol-induced blackout negative ( n =20). Groups were demographically matched and youth who experienced alcohol-induced blackouts were matched on follow-up substance use. Although groups did not differ in inhibitory processing performance, prior to initiating substance use, youth who later transitioned into heavy drinking and experienced an alcohol-induced blackout showed greater neural activation during inhibitory processing in frontal and cerebellar regions compared to controls and those who did not experience alcohol-induced blackouts. Further, activation during correct inhibitory processing compared to go responses in the left and right middle frontal gyri at baseline predicted future blackout experience, after controlling for alcohol consumption and externalizing behaviors ( Wetherill et al., 2013 ). Findings from this study suggest that some individuals have inherent vulnerabilities to inhibitory processing difficulties that likely contribute to alcohol-induced memory impairments. Overall, these neuroimaging findings provide strong evidence for neurobiological vulnerabilities to alcohol-induced memory impairments and alcohol-induced blackouts that exist prior to the onset of alcohol use but become more evident after alcohol consumption.
Silveri and colleagues (2014) and Chitty and colleagues (2014) used magnetic resonance spectroscopy (MRS) to examine potential neurochemical differences among individuals who experience blackouts and those who do not. Using MRS in a sample of 23 young adults who were binge drinkers and 31 young adult light drinkers, researchers found in vivo evidence of lower frontal lobe (i.e. anterior cingulate cortex, ACC) gamma amino-butyric acid (GABA) and N-acetyl-apartate (NAA) in binge drinkers than light drinkers, with post hoc analyses revealing that these lower neurochemical profiles were driven by binge drinkers who reported a history of alcohol-induced blackouts ( Silveri et al., 2014 ). Further, in a sample of 113 18–30 year olds (64 individuals with bipolar disorder and 49 healthy comparison controls), reduced hippocampal glutathione, the brain’s most potent antioxidant, concentration was associated with blackout occurrence and severity ( Chitty et al., 2014 ). Chitty and colleagues (2014) interpreted these findings as support for the role of the hippocampus in alcohol-induced memory impairments. Together, these MRS findings indicate that binge drinking and riskier alcohol use affect the neurochemistry of some individuals more than others, which may contribute to the recurrence of and vulnerability to alcohol-induced memory impairments.
Practical and Clinical Implications of Alcohol-induced Blackouts
From a review of 26 empirical studies, Pressman and Caudill (2013) concluded that only short-term memory is impaired during a blackout and that other cognitive functions, such as planning, attention, and social skills, were not affected. Because cognitive functions other than memory are not necessarily impaired during a blackout ( Pressman and Caudill, 2013 ), a critical question is whether or not people are responsible for their behavior while in a blackout. This is often a key factor in alcohol-related crimes, when the perpetrator or victim claim to have no memory for their actions ( van Oorsouw et al., 2004 ). For example, Pressman and Caudill (2013) reference a quadruple murder in which the defendant claimed he had no memory of committing the murders because he was in an alcohol-induced blackout at the time. Applying Daubert legal standards to this case (( Daubert v. Merrell Dow Pharmaceuticals , 509 U.S. 579 (1993)), the authors concluded that the accused’s blackout could not be used as a viable defense. Equally important, however, may be the memory of a potential victim of a crime. For example, alleged victims of sexual assault may claim they have no memory for events that led up to the sexual activities (( United States v. Pease , Navy-Marine Corps Court of Criminal Appeals 201400165, (2015)). Whereas there is legal precedent to prevent voluntary intoxication and blackouts from being viable defenses against committing a crime ( Cunnien, 1986 ; Marlowe et al., 1999 ), a remaining question is the extent to which alleged victims in a blackout should be held accountable for their actions, despite their lack of memories. Unquestionably, when a victim is incapacitated from alcohol and unable to provide consent, there are grounds for a conviction of sexual assault. However, as reviewed above, blackouts can occur at BrACs well below the level of incapacitation. If people maintain their ability to make conscious decisions and execute voluntary behaviors while in a blackout, questions remain about whether or not they are responsible for their actions.
It is important to remember that when examining the impact of blackouts, the accused, victim, patient, or research subject is typically being asked to remember not remembering. This is a critical challenge to understanding and studying blackouts, and also raises questions about the accuracy of memories that are reported following a blackout. In an effort to fill in gaps in their memory because of alcohol-induced blackouts, people use a variety of strategies to reconstruct their experiences ( Nash and Takarangi, 2011 ). The most common reconstruction strategy is to ask friends who were present, and who may or may not have also been intoxicated. Consequently, in their quest to learn about their actions while in a blackout, people may be given misinformation from their friends, leading to inaccurate reconstructions of the events. People may also look for photos/videos or other types of physical evidence to help fill gaps in their memories due to blackouts. Regardless of how many different approaches a person takes in order to help reconstruct their memory of what occurred during a blackout, there is rarely a way to validate the memories as accurate because the process of memory reconstruction is inherently fallible.
The fallibility of memory, even in the absence of alcohol or blackouts, has been documented through decades of rigorous experimental and field research. Leading this research, Elizabeth Loftus has authored over 200 books and thousands of peer-reviewed articles which demonstrate the many ways in which memory for events can be distorted or contaminated during the process of recall ( Loftus and Davis, 2006 ; Morgan et al., 2013 ; Patihis et al., 2013 ). Provision of misinformation, the passage of time, and being asked or interviewed about prior events can all lead to memory distortions as the individual strives to reconstruct prior events ( Loftus and Davis, 2006 ; Nash and Takarangi, 2011 ). Consequently, the reliability or accuracy of memories that are recalled following a period of alcohol-induced amnesia are likely to be suspect.
There are also important clinical implications of blackouts, as alcohol-induced blackouts have been associated with psychiatric symptomatology ( Bae et al., 2015 ; Neupane and Bramness, 2013 ; Winward et al., 2014 ), as well as feeling embarrassed or distressed when learning about their behavior during a blackout ( White et al., 2004 ). Efforts to reconcile their intoxicated behavior with their personal values may further contribute to significant emotional angst ( Wilhite and Fromme, 2015 ). As such, educating people about the nature and consequences of alcohol-induced blackouts is needed. Although heavy episodic drinking, a common correlate of alcohol-induced blackouts, is often a focus of alcohol prevention programs, rarely are blackouts considered as a target for intervention. For example, a recent study on the effects of a motivational invention on alcohol consumption and blackouts found that the intervention decreased both alcohol consumption and the number of blackouts experienced ( Kazemi et al., 2013 ). Thus, educating people about the factors that contribute to (e.g., predrinking/prepartying; family history of alcohol problems) and consequences of blackouts may help reduce the likelihood of experiencing blackouts and related negative emotional consequences ( Wilhite and Fromme, 2015 ).
Challenges and Future Research
There are several challenges that hinder research on blackouts. First, alcohol-induced blackouts are amnestic periods, and as such, researchers are relying on self-report of alcohol consumption for a period of time that the individual cannot recall. Further, individuals who experienced a blackout often rely on other individuals to help reconstruct the events that occurred during the blackout, but the information from these other individuals is likely unreliable because they may also be consuming alcohol ( Nash and Takarangi, 2011 ). As such, future research should use alternative methodologies to better understand the phenomenology of alcohol-induced blackouts. For example, information might be obtained from a research observer, posing as a confederate, who is not drinking but is present at the drinking event. Also, because short-term memory remains intact, use of ecological momentary assessment with smart phones might also be useful for gathering information about the drinker’s experiences while he or she is in a blackout state. Subsequent interviews could then determine what aspects of those events were remembered and whether they were remembered in the same way that they were reported during the drinking event.
Another complicating factor for research on blackouts is the potential use of other drugs (illicit or prescription) that might also contribute to memory loss. Although several research studies statistically control for or exclude individuals who report co-occurring illicit drug use, research clearly indicates that some individuals who report blackouts also report other drug use ( Baldwin et al., 2011 ; Haas et al., 2015 ). Thus, researchers must be cautious and account for factors other than alcohol that might contribute to blackouts.
Perhaps the greatest impediment to rigorous tests of alcohol-induced blackouts and behavior is that researchers are not ethically permitted to provide alcohol in sufficient doses to cause a blackout to occur. BrACs of 20 g/dl and above are typically required to induce a blackout, thereby limiting the ability to safely dose research participants to the point of blackout. As such, researchers may consider conducting field studies in order to better characterize and understand alcohol-induced blackouts, as it is quite likely that the events and consequences that occur during a blackout are underestimated given the limits of laboratory research and self-report of events. Finally, given the growing literature on alcohol-induced memory impairments and blackouts, a standardized assessment for alcohol-induced blackouts is sorely needed. Most of the existing research on alcohol-induced blackouts either uses a single item from the Rutgers Alcohol Problem Index or the investigator’s own description/definition of an alcohol-induced blackout. Moreover the frequency of occurrence for blackouts is currently measured in widely different ways, including dichotomous measures (e.g., Yes/No blackouts) and proportion of times drinking that blackouts were experienced (e.g., always, sometimes, never). In an effort to better characterize blackouts, researchers should collect detailed information about past and current alcohol consumption patterns, as well as other illicit drug use. It will be important for future studies to conduct a thorough assessment of the alcohol consumption that occurred during the drinking event in which the blackout occurred (i.e., duration of drinking, type of alcohol consumed, pace of consumption), as well as gender and weight, in order to calculate more accurate estimations of BACs. Optimally, actual BrACs or blood draws could be collected to back-extrapolate peak BACs to the time of blackout. This information will enable researchers to statistically control for the direct effects of alcohol consumption and examine factors that influence alcohol-induced blackouts over and beyond the amount of alcohol consumed.
Despite the increase in research on and our understanding of alcohol-induced blackouts, additional rigorous research is still needed. Studies examining potential genetic and environmental influences, as well as their interactions, are clearly warranted given recent research findings of Marino and Fromme (2015) . Sex differences in alcohol-induced blackouts are another area in need of study. Although previous research indicates that women are more vulnerable to alcohol-induced blackouts due to the effect of sex differences in pharmacokinetics and body composition on alcohol bioavailability ( Rose and Grant, 2010 ), the influence of biological sex on alcohol-induced blackouts are inconsistent. Specifically, several studies either did not assess sex differences ( Clinkinbeard and Johnson, 2013 ; Sanchez et al., 2015 ; Wetherill and Fromme, 2011 ; Wetherill et al., 2013 ), reported no sex differences ( Barnett et al., 2014 ; Boekeloo et al., 2011 ; Brister et al., 2011 , Wilhite and Fromme, 2015 ), reported that males reported higher rates of alcohol-induced blackouts ( Chartier et al., 2011 ) or reported that being a female contributed to the likelihood of experiencing an alcohol-induced blackout ( Hallett et al., 2013 ; Schuckit et al., 2015 ). These inconsistent findings could be due in part to methodological differences across research studies and assessment of alcohol-induced blackouts, and future studies should address this issue. Additional areas for future study include interventions targeting alcohol-induced blackouts, whether the risk for alcohol-induced blackouts increases as individuals age and become more susceptible to memory deficits, and whether there is a “window of vulnerability” such that experiencing an alcohol-induced blackout increases the risk of experiencing another alcohol-induced blackout within a short time frame (akin to second impact syndrome for concussions).
The literature on alcohol-induced blackouts continues to grow, and the recent research reviewed here suggests that there are individual factors that contribute to the occurrence of alcohol-induced memory impairments beyond the amount of alcohol consumed and that alcohol-induced blackouts have consequences beyond memory loss for a drinking episode. Although our understanding of alcohol-induced blackouts has improved dramatically, additional research is clearly necessary. By fine-tuning our approach to studying blackouts, we will improve our understanding of alcohol-induced blackouts, and consequently, be better situated to improve prevention strategies.
Acknowledgments
This material is based upon work supported by the National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism under grants K23 AA023894 awarded to Reagan Wetherill and R01 AA020637 awarded to Kim Fromme.
This work was supported by National Institutes of Health grants K23AA023894 (PI: Wetherill) and R01AA020637 (PI: Fromme) from the National Institute on Alcohol Abuse and Alcoholism. The authors would like to thank Diantha LaVine for her assistance with the artwork.
Conflicts of Interest
The authors have not been involved in financial relationships that pose a conflict of interest for this work. The authors are in agreement regarding the content of this manuscript.
- Bae HC, Hong S, Jang SI, Lee KS, Park EC. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011) J Prev Med Public Health. 2015; 48 :142–150. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Baldwin K, Barrowman NJ, Farion KJ, Shaw A. Attitudes and practice of Children’s Hospital of Eastern Ontario (Ottawa, Ontario) paediatricians and residents toward literacy promotion in Canada. Paediatr Child Health. 2011; 16 :e38–42. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnett NP, Clerkin EM, Wood M, Monti PM, O’Leary Tevyaw T, Corriveau D, Fingeret A, Kahler CW. Description and predictors of positive and negative alcohol-related consequences in the first year of college. J Stud Alcohol Drugs. 2014; 75 :103–114. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boekeloo BO, Novik MG, Bush E. Drinking to Get Drunk among Incoming Freshmen College Students. Am J Health Educ. 2011; 42 :88–95. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brister HA, Sher KJ, Fromme K. 21st birthday drinking and associated physical consequences and behavioral risks. Psychol Addict Behav. 2011; 25 :573–582. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chartier KG, Hesselbrock MN, Hesselbrock VM. Alcohol problems in young adults transitioning from adolescence to adulthood: The association with race and gender. Addict Behav. 2011; 36 :167–174. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chitty KM, Lagopoulos J, Hickie IB, Hermens DF. The impact of alcohol and tobacco use on in vivo glutathione in youth with bipolar disorder: an exploratory study. J Psychiatr Res. 2014; 55 :59–67. [ PubMed ] [ Google Scholar ]
- Clinkinbeard SS, Johnson MA. Perceptions and practices of student binge drinking: an observational study of residential college students. J Drug Educ. 2013; 43 :301–319. [ PubMed ] [ Google Scholar ]
- Cunnien AJ. Alcoholic blackouts: phenomenology and legal relevance. Behav Sci Law. 1986; 4 :364–370. [ Google Scholar ]
- Goodwin DW. Alcohol amnesia. Addiction. 1995; 90 :315–317. [ PubMed ] [ Google Scholar ]
- Goodwin DW, Crane JB, Guze SB. Alcoholic “blackouts”: a review and clinical study of 100 alcoholics. Am J Psychiatry. 1969a; 126 :191–198. [ PubMed ] [ Google Scholar ]
- Goodwin DW, Crane JB, Guze SB. Phenomenological aspects of the alcoholic “blackout” Br J Psychiatry. 1969b; 115 :1033–1038. [ PubMed ] [ Google Scholar ]
- Haas AL, Wickham R, Macia K, Shields M, Macher R, Schulte T. Identifying Classes of Conjoint Alcohol and Marijuana Use in Entering Freshmen. Psychol Addict Behav 2015 [ PubMed ] [ Google Scholar ]
- Hallett J, Howat P, McManus A, Meng R, Maycock B, Kypri K. Academic and personal problems among Australian university students who drink at hazardous levels: web-based survey. Health Promot J Austr. 2013; 24 :170–177. [ PubMed ] [ Google Scholar ]
- Hartzler B, Fromme K. Fragmentary and en bloc blackouts: similarity and distinction among episodes of alcohol-induced memory loss. J Stud Alcohol. 2003; 64 :547–550. [ PubMed ] [ Google Scholar ]
- Heffernan TM. The impact of excessive alcohol use on prospective memory: a brief review. Curr Drug Abuse Rev. 2008; 1 :36–41. [ PubMed ] [ Google Scholar ]
- Hepola S. Blackout: Remembering the things I drank to forget. Grand Central Publishing; New York, NY: 2015. [ Google Scholar ]
- Jellinek EM. Phases in the drinking history of alcoholics: analysis of a survey conducted by the official organ of Alcoholics Anonymous. Quarterly Journal of Studies on Alcohol. 1946; 7 :1–88. [ PubMed ] [ Google Scholar ]
- Jellinek EM. Phases of alcohol addiction. Q J Stud Alcohol. 1952; 13 :673–684. [ PubMed ] [ Google Scholar ]
- Jennison KM, Johnson KA. Drinking-induced blackouts among young adults: results from a national longitudinal study. Int J Addict. 1994; 29 :23–51. [ PubMed ] [ Google Scholar ]
- Kazemi DM, Levine MJ, Dmochowski J, Nies MA, Sun L. Effects of motivational interviewing intervention on blackouts among college freshmen. J Nurs Scholarsh. 2013; 45 :221–229. [ PubMed ] [ Google Scholar ]
- LaBrie JW, Hummer J, Kenney S, Lac A, Pedersen E. Identifying factors that increase the likelihood for alcohol-induced blackouts in the prepartying context. Subst Use Misuse. 2011; 46 :992–1002. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee H, Roh S, Kim DJ. Alcohol-induced blackout. Int J Environ Res Public Health. 2009; 6 :2783–2792. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loftus EF, Davis D. Recovered memories. Annu Rev Clin Psychol. 2006; 2 :469–498. [ PubMed ] [ Google Scholar ]
- Luczak SE, Shea SH, Hsueh AC, Chang J, Carr LG, Wall TL. ALDH2*2 is associated with a decreased likelihood of alcohol-induced blackouts in Asian American college students. J Stud Alcohol. 2006; 67 :349–353. [ PubMed ] [ Google Scholar ]
- Marino EN, Fromme K. Alcohol-induced blackouts and maternal family history of problematic alcohol use. Addict Behav. 2015; 45 :201–206. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marlowe DB, Lambert JB, Thompson RG. Voluntary intoxication and criminal responsibility. Behav Sci Law. 1999; 17 :195–217. [ PubMed ] [ Google Scholar ]
- Merrill JE, Read JP. Motivational pathways to unique types of alcohol consequences. Psychol Addict Behav. 2010; 24 :705–711. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Merrill JE, Wardell JD, Read JP. Drinking motives in the prospective prediction of unique alcohol-related consequences in college students. J Stud Alcohol Drugs. 2014; 75 :93–102. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morgan CA, 3rd, Southwick S, Steffian G, Hazlett GA, Loftus EF. Misinformation can influence memory for recently experienced, highly stressful events. Int J Law Psychiatry. 2013; 36 :11–17. [ PubMed ] [ Google Scholar ]
- Mundt MP, Zakletskaia LI. Prevention for college students who suffer alcohol-induced blackouts could deter high-cost emergency department visits. Health Aff (Millwood) 2012; 31 :863–870. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mundt MP, Zakletskaia LI, Brown DD, Fleming MF. Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Inj Prev. 2012; 18 :44–49. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nash RA, Takarangi MK. Reconstructing alcohol-induced memory blackouts. Memory. 2011; 19 :566–573. [ PubMed ] [ Google Scholar ]
- Nelson EC, Heath AC, Bucholz KK, Madden PA, Fu Q, Knopik V, Lynskey MT, Lynskey MT, Whitfield JB, Statham DJ, Martin NG. Genetic epidemiology of alcohol-induced blackouts. Arch Gen Psychiatry. 2004; 61 :257–263. [ PubMed ] [ Google Scholar ]
- Neupane SP, Bramness JG. Prevalence and correlates of major depression among Nepalese patients in treatment for alcohol-use disorders. Drug Alcohol Rev. 2013; 32 :170–177. [ PubMed ] [ Google Scholar ]
- Patihis L, Frenda SJ, LePort AK, Petersen N, Nichols RM, Stark CE, McGaugh JL, Loftus EF. False memories in highly superior autobiographical memory individuals. Proc Natl Acad Sci U S A. 2013; 110 :20947–20952. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Perry PJ, Argo TR, Barnett MJ, Liesveld JL, Liskow B, Hernan JM, Trnka MG, Brabson MA. The association of alcohol-induced blackouts and grayouts to blood alcohol concentrations. J Forensic Sci. 2006; 51 :896–899. [ PubMed ] [ Google Scholar ]
- Pressman MR, Caudill DS. Alcohol-induced blackout as a criminal defense or mitigating factor: an evidence-based review and admissibility as scientific evidence. J Forensic Sci. 2013; 58 :932–940. [ PubMed ] [ Google Scholar ]
- Ray AE, Stapleton JL, Turrisi R, Mun EY. Drinking game play among first-year college student drinkers: an event-specific analysis of the risk for alcohol use and problems. Am J Drug Alcohol Abuse. 2014; 40 :353–358. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Read JP, Wardell JD, Bachrach RL. Drinking consequence types in the first college semester differentially predict drinking the following year. Addict Behav. 2013; 38 :1464–1471. [ PubMed ] [ Google Scholar ]
- Rose ME, Grant JE. Alcohol-induced blackout. Phenomenology, biological basis, and gender differences. J Addict Med. 2010; 4 :61–73. [ PubMed ] [ Google Scholar ]
- Ryback RS. Alcohol amnesia. Observations in seven drinking inpatient alcoholics. Q J Stud Alcohol. 1970; 31 :616–632. [ PubMed ] [ Google Scholar ]
- Sanchez ZM, Ribeiro KJ, Wagner GA. Binge Drinking Associations with Patrons’ Risk Behaviors and Alcohol Effects after Leaving a Nightclub: Sex Differences in the “Balada com Ciencia” Portal Survey Study in Brazil. PLoS One. 2015; 10 :e0133646. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schuckit MA, Smith TL, Heron J, Hickman M, Macleod J, Munafo MR, Kendler KS, Dick DM, Davey-Smith G. Latent trajectory classes for alcohol-related blackouts from age 15 to 19 in ALSPAC. Alcohol Clin Exp Res. 2015; 39 :108–116. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Silveri MM, Cohen-Gilbert J, Crowley DJ, Rosso IM, Jensen JE, Sneider JT. Altered anterior cingulate neurochemistry in emerging adult binge drinkers with a history of alcohol-induced blackouts. Alcohol Clin Exp Res. 2014; 38 :969–979. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Slutske WS, True WR, Scherrer JF, Heath AC, Bucholz KK, Eisen SA, Goldberg J, Lyons MJ, Tsuang MT. The heritability of alcoholism symptoms: “indicators of genetic and environmental influence in alcohol-dependent individuals” revisited. Alcohol Clin Exp Res. 1999; 23 :759–769. [ PubMed ] [ Google Scholar ]
- Tapert SF, Schweinsburg AD, Drummond SP, Paulus MP, Brown SA, Yang TT, Frank LR. Functional MRI of inhibitory processing in abstinent adolescent marijuana users. Psychopharmacology (Berl) 2007; 194 :173–183. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tulving E. Episodic memory: from mind to brain. Annu Rev Psychol. 2002; 53 :1–25. [ PubMed ] [ Google Scholar ]
- van Oorsouw K, Merckelbach H, Ravelli D, Nijman H, Mekking-Pompen I. Alcoholic blackout for criminally relevant behavior. J Am Acad Psychiatry Law. 2004; 32 :364–370. [ PubMed ] [ Google Scholar ]
- Wahl S, Sonntag T, Roehrig J, Kriston L, Berner MM. Characteristics of predrinking and associated risks: a survey in a sample of German high school students. Int J Public Health. 2013; 58 :197–205. [ PubMed ] [ Google Scholar ]
- Wetherill RR, Castro N, Squeglia LM, Tapert SF. Atypical neural activity during inhibitory processing in substance-naive youth who later experience alcohol-induced blackouts. Drug Alcohol Depend. 2013; 128 :243–249. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Fromme K. Acute alcohol effects on narrative recall and contextual memory: an examination of fragmentary blackouts. Addict Behav. 2011; 36 :886–889. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wetherill RR, Schnyer DM, Fromme K. Acute alcohol effects on contextual memory BOLD response: differences based on fragmentary blackout history. Alcohol Clin Exp Res. 2012; 36 :1108–1115. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res. 2013; 35 :201–218. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. J Stud Alcohol. 1989; 50 :30–37. [ PubMed ] [ Google Scholar ]
- White AM. What happened? Alcohol, memory blackouts, and the brain. Alcohol Res Health. 2003; 27 :186–196. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: results of an e-mail survey. J Am Coll Health. 2002; 51 :117–119. 122–131. [ PubMed ] [ Google Scholar ]
- White AM, Matthews DB, Best PJ. Ethanol, memory, and hippocampal function: a review of recent findings. Hippocampus. 2000; 10 :88–93. [ PubMed ] [ Google Scholar ]
- White AM, Signer ML, Kraus CL, Swartzwelder HS. Experiential aspects of alcohol-induced blackouts among college students. Am J Drug Alcohol Abuse. 2004; 30 :205–224. [ PubMed ] [ Google Scholar ]
- Wilhite ER, Fromme K. Alcohol-Induced Blackouts and Other Negative Outcomes During the Transition Out of College. J Stud Alcohol Drugs. 2015; 76 :516–524. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Winward JL, Bekman NM, Hanson KL, Lejuez CW, Brown SA. Changes in emotional reactivity and distress tolerance among heavy drinking adolescents during sustained abstinence. Alcohol Clin Exp Res. 2014; 38 :1761–1769. [ PMC free article ] [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile ...
A Case of Alcohol Abuse. The patient is a 65-year-old white woman, married for 35 years to an accountant. They have 5 grown children and 12 grandchildren. She taught elementary school for 28 years and has not worked since retiring 15 years ago.
A 54-year-old man was admitted to the hospital for alcohol withdrawal. On the fifth day, after resolution of withdrawal symptoms, he was found to be delirious, lethargic, and minimally responsive. ...
My True Story of Alcoholism, Addiction and the Choice to Live. At 8 years old, I stared out the second-floor window of our apartment. Children my age played on the playground. The windowpane was ...
This case study presents the diagnosis and treatment of a male patient with an alcohol use disorder (AUD). Although medications are helpful in AUD, nurse practitioners must be cognizant when combining them with other approaches, such as therapy. Some clinicians prefer to control AUD use before treating other issues, under the theory that alcohol can obscure and aggravate underlying physical ...
This case report discusses a 60-year-old male with severe alcohol use disorder who presented with a newly diagnosed AF with RVR, DCM, and cirrhosis. Our case demonstrates the consequential health risks of chronic alcoholism and highlights the significance of timely screening and early intervention for at-risk alcohol use.
There are studies exploring the coping styles used by the wives of alcoholic clients. Some of such studies have specifically focused on the determinants of coping styles used. Most of these studies are conducted in 80's. ... The engaged coping itself is very tiring and drains the person emotionally; however, this coping serves to maintain the ...
How would you diagnose and treat a 54-year-old man with alcohol withdrawal and altered mental status? Read this case challenge and test your knowledge.
The review identified 107 studies of alcohol use and all-cause mortality published from 1980 to July 2021. Data Extraction and Synthesis Mixed linear regression models were used to model relative risks, first pooled for all studies and then stratified by cohort median age (<56 vs ≥56 years) and sex (male vs female). Data were analyzed from ...
Results of the Singaporean study by Subramanian et al., (2017, Singapore, study #15) indicated that people with alcohol abuse were considered to be unpredictable by 65.0%, with proportions being higher for schizophrenia (77.0%) and dementia ... In the first case (Blomqvist, 2012, Sweden, study #4), respondents were asked about the person's ...
This case study is an attempt to assess the impact of psychiatric social work intervention in person with alcohol dependence. Psychiatric social work intervention (brief intervention) was provided ...
The National Academies reiterated in their 2019 report that organizational tolerance of alcohol use increases the chance of sexual or gender harassment (see also these articles from 2007, 2005, and 2002). Their report adds that such permissiveness leads some people to avoid lab related social events that involve alcohol.
Introduction and aims of the study: Despite the increasing incidence of alcohol misuse and the costs it incurs, British society continues to hold equivocal and ambiguous attitudes towards drinking, and understanding of the nature of alcohol dependence and related issues is limited. This qualitative study aimed to investigate the experiences of individuals with alcohol dependence to enhance ...
The document provides a case study of Mr. Johnson Babu, a 24-year-old man admitted to a de-addiction center for alcohol dependence. It details his personal history, including a 6-year history of daily alcohol and tobacco use. A mental status examination found him oriented with normal mood, affect, and cognition. A physical examination showed he was in overall healthy condition. The goal of his ...
This study aimed to identify the effects of alcoholism on family relations and, by means of case management, to encourage the recovery of these relationships. The results show that the problems caused by alcohol abuse impose profound suffering to family members, which contributes to high levels of interpersonal conflict, domestic violence ...
The alcohol research literature is overwhelmingly focused on risk factors, from the societal level down to the individual. Worldwide, 3.3 million deaths were attributed to alcohol misuse in 2012 (World Health Organization 2014).Excessive alcohol use is the third leading cause of death in the United States, accounting for 88,000 deaths per year (Centers for Disease Control and Prevention 2014).
Robert's story. Robert was living with an alcohol addiction and was homeless for over 25 years. He was well known in the local community and was identified as one of the top 100 A&E attendees at the Local General Hospital. He drank all day every day until he would pass out and this was either in the town centre or just by the roadside.
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism.
Hohman suggests Motivational interviewing (MI ) for person with substance abuse disorder, as a useful intervention technique, 8by applying it to a case study . A meta-analysis by Hettema et al. published in 2005 studied 72 clinical trials spanning a range of target problems, 31 of which focused on alcohol.
The high risk for heavy drinkers found in our meta-analysis of cohort studies is in line with prior research on risk for liver cirrhosis in people with alcohol use disorders.(11, 51, 52) The pooled RRs from case-control studies were much smaller; however, the more recent case-control study corresponds with the risks found in people with alcohol ...
A2: To approach case study questions effectively, follow these steps: Read the case study carefully: Understand the scenario and identify the key points. Analyze the information: Look for clues and relevant details that will help you answer the questions. Apply your knowledge: Use what you have learned in your course to interpret the case study and answer the questions.
Ian Sample and science correspondent Hannah Devlin discuss some of the science stories that have made headlines this week, from a new technique that uses food colouring to make skin transparent ...
The National Institute on Alcohol Abuse and Alcoholism is sponsoring an ongoing multisite cooperative study (Project MATCH Research Group 1993) that will have sufficient participants to test numerous hypotheses for matching clients to cognitive-behavioral treatment as well as to 12-step and motivational enhancement treatments. It is anticipated ...
NEW YORK (AP) — Justin Timberlake is scheduled to enter a new plea Friday in his drunken driving case in New York's Hamptons, prosecutors said. Details of the plea weren't disclosed, but a person with knowledge of the deal said Timberlake has agreed to plead guilty to a less serious offense than the original charge of driving while intoxicated.
According to a study of amnesia in people arrested for alcohol-related offenses (Perry et al., 2006), the probability of a fragmentary or an en bloc blackout was 50/50 at a BrAC of 0.22 g/dl and the probability of an en bloc blackout was 50/50 at a BrAC of 0.31 g/dl. As such, blackouts typically occur during binge or excessive drinking episodes.