Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
Information & authors, metrics & citations, view options, insights into mechanisms related to cocaine addiction using a novel imaging method for dopamine neurons, treatment implications of understanding brain function during early abstinence in patients with alcohol use disorder, relatively low amounts of alcohol intake during pregnancy are associated with subtle neurodevelopmental effects in preadolescent offspring, increased comorbidity between substance use and psychiatric disorders in sexual identity minorities, trends in nicotine use and dependence from 2001–2002 to 2012–2013, conclusions, information, published in.

- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues

Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
NEXT ARTICLE
Request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- Reasons to publish with us
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction.
- < Previous
Understanding reasons for drug use amongst young people: a functional perspective
- Article contents
- Figures & tables
- Supplementary Data
Annabel Boys, John Marsden, John Strang, Understanding reasons for drug use amongst young people: a functional perspective, Health Education Research , Volume 16, Issue 4, August 2001, Pages 457–469, https://doi.org/10.1093/her/16.4.457
- Permissions Icon Permissions
This study uses a functional perspective to examine the reasons young people cite for using psychoactive substances. The study sample comprised 364 young poly-drug users recruited using snowball-sampling methods. Data on lifetime and recent frequency and intensity of use for alcohol, cannabis, amphetamines, ecstasy, LSD and cocaine are presented. A majority of the participants had used at least one of these six drugs to fulfil 11 of 18 measured substance use functions. The most popular functions for use were using to: relax (96.7%), become intoxicated (96.4%), keep awake at night while socializing (95.9%), enhance an activity (88.5%) and alleviate depressed mood (86.8%). Substance use functions were found to differ by age and gender. Recognition of the functions fulfilled by substance use should help health educators and prevention strategists to make health messages about drugs more relevant and appropriate to general and specific audiences. Targeting substances that are perceived to fulfil similar functions and addressing issues concerning the substitution of one substance for another may also strengthen education and prevention efforts.
The use of illicit psychoactive substances is not a minority activity amongst young people in the UK. Results from the most recent British Crime Survey show that some 50% of young people between the ages of 16 and 24 years have used an illicit drug on at least one occasion in their lives (lifetime prevalence) ( Ramsay and Partridge, 1999 ). Amongst 16–19 and 20–24 year olds the most prevalent drug is cannabis (used by 40% of 16–19 year olds and 47% of 20–24 year olds), followed by amphetamine sulphate (18 and 24% of the two age groups respectively), LSD (10 and 13%) and ecstasy (8 and 12%). The lifetime prevalence for cocaine hydrochloride (powder cocaine) use amongst the two age groups is 3 and 9%, respectively. Collectively, these estimates are generally comparable with other European countries ( European Monitoring Centre for Drugs and Drug Addiction, 1998 ) and the US ( Johnston et al ., 1997 , 2000 ).
The widespread concern about the use of illicit drugs is reflected by its high status on health, educational and political agendas in many countries. The UK Government's 10-year national strategy on drug misuse identifies young people as a critical priority group for prevention and treatment interventions ( Tackling Drugs to Build a Better Britain 1998 ). If strategies to reduce the use of drugs and associated harms amongst the younger population are to be developed, particularly within the health education arena, it is vital that we improve our understanding of the roles that both licit and illicit substances play in the lives of young people. The tendency for educators, practitioners and policy makers to address licit drugs (such as alcohol) separately from illegal drugs may be unhelpful. This is partly because young illicit drug users frequently drink alcohol, and may have little regard for the illicit and licit distinction established by the law. To understand the roles that drug and alcohol use play in contemporary youth culture, it is necessary to examine the most frequently used psychoactive substances as a set.
It is commonplace for young drug users to use several different psychoactive substances. The terms `poly-drug' or `multiple drug' use have been used to describe this behaviour although their exact definitions vary. The term `poly-drug use' is often used to describe the use of two or more drugs during a particular time period (e.g. over the last month or year). This is the definition used within the current paper. However, poly-drug use could also characterize the use of two or more psychoactive substances so that their effects are experienced simultaneously. We have used the term `concurrent drug use' to denote this pattern of potentially more risky and harmful drug use ( Boys et al. 2000a ). Previous studies have reported that users often use drugs concurrently to improve the effects of another drug or to help manage its negative effects [e.g. ( Power et al ., 1996 ; Boys et al. 2000a ; Wibberley and Price, 2000 )].
The most recent British Crime Survey found that 5% of 16–29 year olds had used more than one drug in the last month ( Ramsay and Partridge, 1999 ). Given that 16% of this age band reported drug use in the month prior to interview, this suggests that just under a third of these individuals had used more than one illicit substance during this time period. With alcohol included, the prevalence of poly-drug use is likely to be much higher.
There is a substantial body of literature on the reasons or motivations that people cite for using alcohol, particularly amongst adult populations. For example, research on heavy drinkers suggested that alcohol use is related to multiple functions for use ( Edwards et al ., 1972 ; Sadava, 1975 ). Similarly, research with a focus on young people has sought to identify motives for illicit drug use. There is evidence that for many young people, the decision to use a drug is based on a rational appraisal process, rather than a passive reaction to the context in which a substance is available ( Boys et al. 2000a ; Wibberley and Price, 2000 ). Reported reasons vary from quite broad statements (e.g. to feel better) to more specific functions for use (e.g. to increase self-confidence). However, much of this literature focuses on `drugs' as a generic concept and makes little distinction between different types of illicit substances [e.g. ( Carman, 1979 ; Butler et al ., 1981 ; Newcomb et al ., 1988 ; Cato, 1992 ; McKay et al ., 1992 )]. Given the diverse effects that different drugs have on the user, it might be proposed that reasons for use will closely mirror these differences. Thus stimulant drugs (such as amphetamines, ecstasy or cocaine) will be used for reasons relating to increased nervous system arousal and drugs with sedative effects (such as alcohol or cannabis), with nervous system depression. The present study therefore selected a range of drugs commonly used by young people with stimulant, sedative or hallucinogenic effects to examine this issue further.
The phrase `instrumental drug use' has been used to denote drug use for reasons specifically linked to a drug's effects ( WHO, 1997 ). Examples of the instrumental use of amphetamine-type stimulants include vehicle drivers who report using to improve concentration and relieve tiredness, and people who want to lose weight (particularly young women), using these drugs to curb their appetite. However, the term `instrumental substance use' seems to be used when specific physical effects of a drug are exploited and does not encompass use for more subtle social or psychological purposes which may also be cited by users. In recent reports we have described a `drug use functions' model to help understand poly-substance use phenomenology amongst young people and how decisions are made about patterns of consumption ( Boys et al ., 1999a , b , 2000a ). The term `function' is intended to characterize the primary or multiple reasons for, or purpose served by, the use of a particular substance in terms of the actual gains that the user perceives that they will attain. In the early, 1970s Sadava suggested that functions were a useful means of understanding how personality and environmental variables impacted on patterns of drug use ( Sadava, 1975 ). This work was confined to functions for cannabis and `psychedelic drugs' amongst a sample of college students. To date there has been little research that has examined the different functions associated with the range of psychoactive substances commonly used by young poly-drug users. It is unclear if all drugs with similar physical effects are used for similar purposes, or if other more subtle social or psychological dimensions to use are influential. Work in this area will help to increase understanding of the different roles played by psychoactive substances in the lives of young people, and thus facilitate health, educational and policy responses to this issue.
Previous work has suggested that the perceived functions served by the use of a drug predict the likelihood of future consumption ( Boys et al ., 1999a ). The present study aims to develop this work further by examining the functional profiles of six substances commonly used by young people in the UK.
Patterns of cannabis, amphetamine, ecstasy, LSD, cocaine hydrochloride and alcohol use were examined amongst a sample of young poly-drug users. Tobacco use was not addressed in the present research.
Sampling and recruitment
A snowball-sampling approach was employed for recruitment of participants. Snowball sampling is an effective way of generating a large sample from a hidden population where no formal sampling frame is available ( Van Meter, 1990 ). A team of peer interviewers was trained to recruit and interview participants for the study. We have described this procedure in detail elsewhere and only essential features are described here ( Boys et al. 2000b ). Using current or ex-drug users to gather data from hidden populations of drug using adults has been found to be successful ( Griffiths et al ., 1993 ; Power, 1995 ).
Study participants
Study participants were current poly-substance users with no history of treatment for substance-related disorders. We excluded people with a treatment history on the assumption that young people who have had substance-related problems requiring treatment represent a different group from the general population of young drug users. Inclusion criteria were: aged 16–22 years and having used two or more illegal substances during the past 90 days. During data collection, the age, gender and current occupation of participants were recorded and monitored to ensure that sufficient individuals were recruited to the groups to permit subgroup analyses. If an imbalance was observed in one of these variables, the interviewers were instructed to target participants with specific characteristics (e.g. females under the age of 18) to redress this imbalance.
Study measures
Data were collected using a structured interviewer-administered questionnaire developed specifically for the study. In addition to recording lifetime substance use, questions profiled consumption patterns of six substances in detail. Data were collected between August and November 1998. Interviews were audiotaped with the interviewee's consent. This enabled research staff to verify that answers had been accurately recorded on the questionnaire and that the interview had been conducted in accordance with the research protocol. Research staff also checked for consistency across different question items (e.g. the total number of days of drug use in the past 90 days should equal or exceed the number of days of cannabis use during the same time period). On the few occasions where inconsistencies were identified that could not be corrected from the tape, the interviewer was asked to re-contact the interviewee to verify the data.
Measures of lifetime use, consumption in the past year and past 90 days were based on procedures developed by Marsden et al . ( Marsden et al ., 1998 ). Estimated intensity of consumption (amount used on a typical using day) was recorded verbatim and then translated into standardized units at the data entry stage.
Functions for substance use scale
The questionnaire included a 17-item scale designed to measure perceived functions for substance use. This scale consisted of items developed in previous work ( Boys et al ., 1999a ) in addition to functions derived from qualitative interviews ( Boys et al ., 1999b ), new literature and informal discussions with young drug users. Items were drawn from five domains (Table I ).
Participants were asked if they had ever used a particular drug in order to fulfil each specific function. Those who endorsed the item were then invited to rate how frequently they had used it for this purpose over the past year, using a five-point Likert-type scale (`never' to `always'; coded 0–4). One item differed between the function scales used for the stimulant drugs and for alcohol and cannabis. For the stimulant drugs (amphetamines, cocaine and ecstasy) the item `have you ever used [named drug] to help you to lose weight' was used, for cannabis and alcohol this item was replaced with `have you ever used [drug] to help you to sleep?'. (The items written in full as they appeared in the questionnaire are shown in Table III , together with abbreviations used in this paper.)
Statistical procedures
The internal reliability of the substance use functions scales for each of the six substances was judged using Chronbach's α coefficient. Chronbach's α is a statistic that reflects the extent to which each item in a measurement scale is associated with other items. Technically it is the average of correlations between all possible comparisons of the scale items that are divided into two halves. An α coefficient for a scale can range from 0 (no internal reliability) to 1 (complete reliability). Analyses of categorical variables were performed using χ 2 statistic. Differences in scale means were assessed using t -tests.
The sample consisted of 364 young poly-substance users (205 males; 56.3%) with a mean age of 19.3 years; 69.8% described their ethnic group as White-European, 12.6% as Black and 10.1% were Asian. Just over a quarter (27.5%) were unemployed at the time of interview; a third were in education, 28.8% were in full-time work and the remainder had part-time employment. Estimates of monthly disposable income (any money that was spare after paying for rent, bills and food) ranged from 0 to over £1000 (median = £250).
Substance use history
The drug with the highest lifetime prevalence was cannabis (96.2%). This was followed by amphetamine sulphate (51.6%), cocaine hydrochloride (50.5%) (referred to as cocaine hereafter) and ecstasy (48.6%). Twenty-five percent of the sample had used LSD and this was more common amongst male participants (χ 2 [1] = 9.68, P < 0.01). Other drugs used included crack cocaine (25.5%), heroin (12.6%), tranquillizers (21.7%) and hallucinogenic mushrooms (8.0%). On average, participants had used a total of 5.2 different psychoactive substances in their lives (out of a possible 14) (median = 4.0, mode = 3.0, range 2–14). There was no gender difference in the number of different drugs ever used.
Table II profiles use of the six target drugs over the past year, and the frequency and intensity of use in the 90 days prior to interview.
There were no gender differences in drug use over the past year or in the past 90 days with the exception of amphetamines. For this substance, females who had ever used this drug were more likely to have done so during the past 90 days than males (χ 2 [1] = 4.14, P < 0.05). The mean number of target drugs used over the past 90 days was 3.2 (median = 3.0, mode = 3.0, range 2–6). No gender differences were observed. Few differences were also observed in the frequency and intensity of use. Males reported drinking alcohol more frequently during the three months prior to interview ( t [307] = 2.48, P < 0.05) and using cannabis more intensively on a `typical using day' ( t [337] = 3.56, P < 0.001).
Perceived functions for substance use
There were few differences between the functions endorsed for use of each drug `ever' and those endorsed for use during `the year prior to interview'. This section therefore concentrates on data for the year prior to interview. We considered that in order to use a drug for a specific function, the user must have first hand knowledge of the drug's effects before making this decision. Consequently, functions reported by individuals who had only used a particular substance on one occasion in their lives (i.e. with no prior experience of the drug at the time they made the decision to take it) were excluded from the analyses. Table III summarizes the proportion of the sample who endorsed each of the functions for drugs used in the past year. Roman numerals have been used to indicate the functions with the top five average scores. Table III also shows means for the total number of different items endorsed by individual users and the internal reliability of the function scales for each substance using Chronbach's α coefficients. There were no significant gender differences in the total number of functions endorsed for any of the six substances.
The following sections summarize the top five most popular functions drug-by-drug together with any age or gender differences observed in the items endorsed.
Cannabis use ( n = 345)
Overall the most popular functions for cannabis use were to `RELAX' (endorsed by 96.8% of people who had used the drug in the last year), to become `INTOXICATED' (90.7%) and to `ENHANCE ACTIVITY' (72.8%). Cannabis was also commonly used to `DECREASE BOREDOM' (70.1%) and to `SLEEP' (69.6%) [this item was closely followed by using to help `FEEL BETTER' (69.0%)]. Nine of the 17 function items were endorsed by over half of those who had used cannabis on more than one occasion in the past year. There were no significant gender differences observed, with the exception of using to `KEEP GOING', where male participants were significantly more likely to say that they had used cannabis to fulfil this function in the past year (χ 2 [1] = 6.10, P < 0.05).
There were statistically significant age differences on four of the function variables: cannabis users who reported using this drug in the past year to help feel `ELATED/EUPHORIC' or to help `SLEEP' were significantly older than those who had not used cannabis for these purposes (19.6 versus 19.0; t [343] = 3.32, P < 0.001; 19.4 versus 19.0; t [343] = 2.01, P < 0.05). In contrast, those who had used cannabis to `INCREASE CONFIDENCE' and to `STOP WORRYING' tended to be younger than those who did not (19.0 versus 19.4; t [343] = –2.26, P < 0.05; 19.1 versus 19.5; t [343] = –1.99, P < 0.05).
Amphetamines ( n = 160)
Common functions for amphetamine use were to `KEEP GOING' (95.6%), to `STAY AWAKE' (91.3%) or to `ENHANCE ACTIVITY' (66.2%). Using to help feel `ELATED/EUPHORIC' (60.6%) and to `ENJOY COMPANY' (58.1%) were also frequently mentioned. Seven of the 17 function items were endorsed by over half of participants who had used amphetamines in the past year. As with cannabis, gender differences were uncommon: females were more likely to use amphetamines to help `LOSE WEIGHT' than male participants (χ 2 [1] = 21.67, P < 0.001).
Significant age differences were found on four function variables. Individuals who reported using amphetamines in the past year to feel `ELATED/EUPHORIC' were significantly older than those who did not (19.9 versus 19.0; t [158] = 2.87, P < 0.01). In contrast, participants who used amphetamines to `STOP WORRYING' (18.8 versus 19.8; t [158] = –2.77, P < 0.01), to `DECREASE BOREDOM' (19.2 versus 19.9; t [158] = –2.39, P < 0.05) or to `ENHANCE ACTIVITY' (19.3 versus 20.1; t [158] = –2.88, P < 0.01) were younger than those who had not.
Ecstasy ( n = 157)
The most popular five functions for using ecstasy were similar to those for amphetamines. The drug was used to `KEEP GOING' (91.1%), to `ENHANCE ACTIVITY' (79.6%), to feel `ELATED/EUPHORIC' (77.7%), to `STAY AWAKE' (72.0%) and to get `INTOXICATED' (68.2%). Seven of the 17 function items were endorsed by over half of those who had used ecstasy in the past year. Female users were more likely to use ecstasy to help `LOSE WEIGHT' than male participants (Fishers exact test, P < 0.001).
As with the other drugs discussed above, participants who reported using ecstasy to feel `ELATED/EUPHORIC' were significantly older than those who did not (19.8 versus 18.9; t [155] = 2.61, P < 0.01). In contrast, those who had used ecstasy to `FEEL BETTER' (19.3 versus 20.0; t [155] = –2.29, P < 0.05), to `INCREASE CONFIDENCE' (19.2 versus 19.9; t [155] = –2.22, P < 0.05) and to `STOP WORRYING' (19.0 versus 19.9; t [155] = –2.96, P < 0.01) tended to be younger.
LSD ( n = 58)
Of the six target substances examined in this study, LSD was associated with the least diverse range of functions for use. All but two of the function statements were endorsed by at least some users, but only five were reported by more than 50%. The most common purpose for consuming LSD was to get `INTOXICATED' (77.6%). Other popular functions included to feel `ELATED/EUPHORIC' and to `ENHANCE ACTIVITY' (both endorsed by 72.4%), and to `KEEP GOING' and to `ENJOY COMPANY' (both endorsed by 58.6%). Unlike the other substances examined, no gender or age differences were observed.
Cocaine ( n = 168)
In common with ecstasy and amphetamines, the most widely endorsed functions for cocaine use were to help `KEEP GOING' (84.5%) and to help `STAY AWAKE' (69.0%). Consuming cocaine to `INCREASE CONFIDENCE' and to get `INTOXICATED' (both endorsed by 66.1%) were also popular. However, unlike the other stimulant drugs, 61.9% of the cocaine users reported using to `FEEL BETTER'. Ten of the 17 function items were endorsed by over half of those who had used cocaine in the past year.
Gender differences were more common amongst functions for cocaine use than the other substances surveyed. More males reported using cocaine to `IMPROVE EFFECTS' of other drugs (χ 2 [1] = 4.00, P < 0.05); more females used the drug to help `STAY AWAKE' (χ 2 [1] = 12.21, P < 0.001), to `LOSE INHIBITIONS' (χ 2 [1] = 9.01, P < 0.01), to `STOP WORRYING' (χ 2 [1] = 8.11, P < 0.01) or to `ENJOY COMPANY' of friends (χ 2 [1] = 4.34, P < 0.05). All participants who endorsed using cocaine to help `LOSE WEIGHT' were female.
Those who had used cocaine to `FEEL BETTER' (18.9 versus 19.8; t [166] = –3.06, P < 0.01), to `STOP WORRYING' (18.6 versus 19.7; t [166] = –3.86, P < 0.001) or to `DECREASE BOREDOM' (18.9 versus 19.6; t [166] = –2.52, P < 0.05) were significantly younger than those who did not endorse these functions. Similar to the other drugs, participants who had used cocaine to feel `ELATED/EUPHORIC' in the past year tended to be older than those who had not (19.6 versus 18.7; t [166] = 3.16, P < 0.01).
Alcohol ( n = 312)
The functions for alcohol use were the most diverse of the six substances examined. Like LSD, the most commonly endorsed purpose for drinking was to get `INTOXICATED' (89.1%). Many used alcohol to `RELAX' (82.7%), to `ENJOY COMPANY' (74.0%), to `INCREASE CONFIDENCE' (70.2%) and to `FEEL BETTER' (69.9%). Overall, 11 of the 17 function items were endorsed by over 50% of those who had drunk alcohol in the past year. Male participants were more likely to report using alcohol in combination with other drugs either to `IMPROVE EFFECTS' of other drugs (χ 2 [1] = 4.56, P < 0.05) or to ease the `AFTER EFFECTS' of other substances (χ 2 [1] = 7.07, P < 0.01). More females than males reported that they used alcohol to `DECREASE BOREDOM' (χ 2 [1] = 4.42, P < 0.05).
T -tests revealed significant age differences on four of the function variables: those who drank to feel `ELATED/EUPHORIC' were significantly older (19.7 versus 19.0; t [310] = 3.67, P < 0.001) as were individuals who drank to help them to `LOSE INHIBITIONS' (19.6 versus 19.0; t [310] = 2.36, P < 0.05). In contrast, participants who reported using alcohol just to get `INTOXICATED' (19.2 versus 20.3; t [310] = –3.31, P < 0.001) or to `DECREASE BOREDOM' (19.2 versus 19.6; t [310] = –2.25, P < 0.05) were significantly younger than those who did not.
Combined functional drug use
The substances used by the greatest proportion of participants to `IMPROVE EFFECTS' from other drugs were cannabis (44.3%), alcohol (41.0%) and amphetamines (37.5%). It was also common to use cannabis (64.6%) and to a lesser extent alcohol (35.9%) in combination with other drugs in order to help manage `AFTER EFFECTS'. Amphetamines, ecstasy, LSD and cocaine were also used for these purposes, although to a lesser extent. Participants who endorsed the combination drug use items were asked to list the three main drugs with which they had combined the target substance for these purposes. Table IV summarizes these responses.
Overall functions for drug use
In order to examine which functions were most popular overall, a dichotomous variable was created for each different item to indicate if one or more of the six target substances had been used to fulfil this purpose during the year prior to interview. For example, if an individual reported that they had used cannabis to relax, but their use of ecstasy, amphetamines and alcohol had not fulfilled this function, then the variable for `RELAX' was scored `1'. Similarly if they had used all four of these substances to help them to relax in the past year, the variable would again be scored as `1'. A score of `0' indicates that none of the target substances had been used to fulfil a particular function. Table V summarizes the data from these new variables.
Over three-quarters of the sample had used at least one target substance in the past year for 11 out of the 18 functions listed. The five most common functions for substance use overall were to `RELAX' (96.7%); `INTOXICATED' (96.4%); `KEEP GOING' (95.9%); `ENHANCE ACTIVITY' (88.5%) and `FEEL BETTER' (86.8%). Despite the fact that `SLEEP' was only relevant to two substances (alcohol and cannabis), it was still endorsed by over 70% of the total sample. Using to `LOSE WEIGHT' was only relevant to the stimulant drugs (amphetamines, ecstasy and cocaine), yet was endorsed by 17.3% of the total sample (almost a third of all female participants). Overall, this was the least popular function for recent substance use, followed by `WORK' (32.1%). All other items were endorsed by over 60% of all participants.
Gender differences were identified in six items. Females were significantly more likely to have endorsed the following: using to `INCREASE CONFIDENCE' (χ 2 [1] = 4.41, P < 0.05); `STAY AWAKE' (χ 2 [1] = 5.36, P < 0.05), `LOSE INHIBITIONS' (χ 2 [1] = 4.48, P < 0.05), `ENHANCE SEX' (χ 2 [1] = 5.17, P < 0.05) and `LOSE WEIGHT' (χ 2 [1] = 29.6, P < 0.001). In contrast, males were more likely to use a substance to `IMPROVE EFFECTS' of another drug (χ 2 [1] = 11.18, P < 0.001).
Statistically significant age differences were identified in three of the items. Those who had used at least one of the six target substances in the last year to feel `ELATED/EUPHORIC' (19.5 versus 18.6; t [362] = 4.07, P < 0.001) or to `SLEEP' (19.4 versus 18.9; t [362] = 2.19, P < 0.05) were significantly older than those who had not used for this function. In contrast, participants who had used in order to `STOP WORRYING' tended to be younger (19.1 versus 19.7; t [362] = –2.88, P < 0.01).
This paper has examined psychoactive substance use amongst a sample of young people and focused on the perceived functions for use using a 17-item scale. In terms of the characteristics of the sample, the reported lifetime and recent substance use was directly comparable with other samples of poly-drug users recruited in the UK [e.g. ( Release, 1997 )].
Previous studies which have asked users to give reasons for their `drug use' overall instead of breaking it down by drug type [e.g. ( Carman, 1979 ; Butler et al ., 1981 ; Newcomb et al ., 1988 ; Cato, 1992 ; McKay et al ., 1992 )] may have overlooked the dynamic nature of drug-related decision making. A key finding from the study is that that with the exception of two of the functions for use scale items (using to help sleep or lose weight), all of the six drugs had been used to fulfil all of the functions measured, despite differences in their pharmacological effects. The total number of functions endorsed by individuals for use of a particular drug varied from 0 to 15 for LSD, and up to 17 for cannabis, alcohol and cocaine. The average number ranged from 5.9 (for LSD) to 9.0 (for cannabis). This indicates that substance use served multiple purposes for this sample, but that the functional profiles differed between the six target drugs.
We have previously reported ( Boys et al. 2000b ) that high scores on a cocaine functions scale are strongly predictive of high scores on a cocaine-related problems scale. The current findings support the use of similar function scales for cannabis, amphetamines, LSD and ecstasy. It remains to be seen whether similar associations with problem scores exist. Future developmental work in this area should ensure that respondents are given the opportunity to cite additional functions to those included here so that the scales can be further extended and refined.
Recent campaigns that have targeted young people have tended to assume that hallucinogen and stimulant use is primarily associated with dance events, and so motives for use will relate to this context. Our results support assumptions that these drugs are used to enhance social interactions, but other functions are also evident. For example, about a third of female interviewees had used a stimulant drug to help them to lose weight. Future education and prevention efforts should take this diversity into account when planning interventions for different target groups.
The finding that the same functions are fulfilled by use of different drugs suggests that at least some could be interchangeable. Evidence for substituting alternative drugs to fulfil a function when a preferred drug is unavailable has been found in other studies [e.g. ( Boys et al. 2000a )]. Prevention efforts should perhaps focus on the general motivations behind use rather than trying to discourage use of specific drug types in isolation. For example, it is possible that the focus over the last decade on ecstasy prevention may have contributed inadvertently to the rise in cocaine use amongst young people in the UK ( Boys et al ., 1999c ). It is important that health educators do not overlook this possibility when developing education and prevention initiatives. Considering functions that substance use can fulfil for young people could help us to understand which drugs are likely to be interchangeable. If prevention programmes were designed to target a range of substances that commonly fulfil similar functions, then perhaps this could address the likelihood that some young people will substitute other drugs if deterred from their preferred substance.
There has been considerable concern about the perceived increase in the number of young people who are using cocaine in the UK ( Tackling Drugs to Build a Better Britain 1998 ; Ramsay and Partridge, 1999 ; Boys et al. 2000b ). It has been suggested that, for a number of reasons, cocaine may be replacing ecstasy and amphetamines as the stimulant of choice for some young people ( Boys et al ., 1999c ). The results from this study suggest that motives for cocaine use are indeed similar to those for ecstasy and amphetamine use, e.g. using to `keep going' on a night out with friends, to `enhance an activity', `to help to feel elated or euphoric' or to help `stay awake'. However, in addition to these functions which were shared by all three stimulants, over 60% of cocaine users reported that they had used this drug to `help to feel more confident' in a social situation and to `feel better when down or depressed'. Another finding that sets cocaine aside from ecstasy and amphetamines was the relatively common existence of gender differences in the function items endorsed. Female cocaine users were more likely to use to help `stay awake', `lose inhibitions', `stop worrying', `enjoy company of friends' or to help `lose weight'. This could indicate that women are more inclined to admit to certain functions than their male counterparts. However, the fact that similar gender differences were not observed in the same items for the other five substances, suggests this interpretation is unlikely. Similarly, the lack of gender differences in patterns of cocaine use (both frequency and intensity) suggests that these differences are not due to heavier cocaine use amongst females. If these findings are subsequently confirmed, this could point towards an inclination for young women to use cocaine as a social support, particularly to help feel less inhibited in social situations. If so, young female cocaine users may be more vulnerable to longer-term cocaine-related problems.
Many respondents reported using alcohol or cannabis to help manage effects experienced from another drug. This has implications for the choice of health messages communicated to young people regarding the use of two or more different substances concurrently. Much of the literature aimed at young people warns them to avoid mixing drugs because the interactive effects may be dangerous [e.g. ( HIT, 1996 )]. This `Just say No' type of approach does not take into consideration the motives behind mixing drugs. In most areas, drug education and prevention work has moved on from this form of communication. A more sophisticated approach is required, which considers the functions that concurrent drug use is likely to have for young people and tries to amend messages to make them more relevant and acceptable to this population. Further research is needed to explore the motivations for mixing different combinations of drugs together.
Over three-quarters of the sample reported using at least one of the six target substances to fulfil 11 out of the 18 functions. These findings provide strong evidence that young people use psychoactive drugs for a range of distinct purposes, not purely dependent on the drug's specific effects. Overall, the top five functions were to `help relax', `get intoxicated', `keep going', `enhance activity' and `feel better'. Each of these was endorsed by over 85% of the sample. Whilst all six substances were associated to a greater or lesser degree with each of these items, there were certain drugs that were more commonly associated with each. For example, cannabis and alcohol were popular choices for relaxation or to get intoxicated. In contrast, over 90% of the amphetamine and ecstasy users reported using these drugs within the last year to `keep going'. Using to enhance an activity was a common function amongst users of all six substances, endorsed by over 70% of ecstasy, cannabis and LSD users. Finally, it was mainly alcohol and cannabis (and to a lesser extent cocaine) that were used to `feel better'.
Several gender differences were observed in the combined functions for recent substance use. These findings indicate that young females use other drugs as well as cocaine as social supports. Using for specific physical effects (weight loss, sex or wakefulness) was also more common amongst young women. In contrast, male users were significantly more likely to report using at least one of the target substances to try to improve the effects of another substance. This indicates a greater tendency for young males in this sample to mix drugs than their female counterparts. Age differences were also observed on several function items: participants who had used a drug to `feel elated or euphoric' or to `help sleep' tended to be older and those who used to `stop worrying about a problem' were younger. If future studies confirm these differences, education programmes and interventions might benefit from tailoring their strategies for specific age groups and genders. For example, a focus on stress management strategies and coping skills with a younger target audience might be appropriate.
Some limitations of the study need to be acknowledged. The sample for this study was recruited using a snowball-sampling methodology. Although it does not yield a random sample of research participants, this method has been successfully used to access hidden samples of drug users [e.g. ( Biernacki, 1986 ; Lenton et al ., 1997 )]. Amongst the distinct advantages of this approach are that it allows theories and models to be tested quantitatively on sizeable numbers of subjects who have engaged in a relatively rare behaviour.
Further research is now required to determine whether our observations may be generalized to other populations (such as dependent drug users) and drug types (such as heroin, tranquillizers or tobacco) or if additional function items need to be developed. Future studies should also examine if functions can be categorized into primary and subsidiary reasons and how these relate to changes in patterns of use and drug dependence. Recognition of the functions fulfilled by substance use could help inform education and prevention strategies and make them more relevant and acceptable to the target audiences.
Structure of functions scales
| Domain . | Item . |
|---|---|
| Changing mood | Make yourself feel better when down or depressed |
| Help you stop worrying about a problem | |
| Help you to relax | |
| Help you feel elated or euphoric | |
| Just get really stoned or intoxicated | |
| Physical effects | Enhance feelings when having sex |
| Help you to stay awake | |
| Help you lose weight | |
| Help you to sleep | |
| Social purposes | Help you enjoy the company of your friends |
| Help you feel more confident or more able to talk to people in a social situation | |
| Help you lose your inhibitions | |
| Help you keep going on a night out with friends | |
| Facilitate activity | Help you to concentrate or to work or study |
| Enhance an activity such as listening to music or playing a game or sport | |
| Help make something you were doing less boring | |
| Manage effects from other substances | Improve the effects of other substances |
| Help ease the after effects of other substances |
| Domain . | Item . |
|---|---|
| Changing mood | Make yourself feel better when down or depressed |
| Help you stop worrying about a problem | |
| Help you to relax | |
| Help you feel elated or euphoric | |
| Just get really stoned or intoxicated | |
| Physical effects | Enhance feelings when having sex |
| Help you to stay awake | |
| Help you lose weight | |
| Help you to sleep | |
| Social purposes | Help you enjoy the company of your friends |
| Help you feel more confident or more able to talk to people in a social situation | |
| Help you lose your inhibitions | |
| Help you keep going on a night out with friends | |
| Facilitate activity | Help you to concentrate or to work or study |
| Enhance an activity such as listening to music or playing a game or sport | |
| Help make something you were doing less boring | |
| Manage effects from other substances | Improve the effects of other substances |
| Help ease the after effects of other substances |
Profile of substance use over the past year and past 90 days ( n = 364)
| Substance (lifetime users) . | Lifetime users consuming in past year (%) . | Lifetime usersconsuming in past 90 days (%) . | Mean days used in past 90 days (range) . | Average amount on typical using day[SD (range)] . |
|---|---|---|---|---|
| Grams. | ||||
| Number of tablets. | ||||
| Number of units (1 unit = 8 g ethanol approximately). | ||||
| One respondent reported smoking 21.3 g of cannabis on a typical using day. This outlying value was recoded to the next highest intensity recorded (10.6 g). | ||||
| Two alcohol users reported consuming 48.0 and 50.0 units of alcohol on a typical using day respectively. These outlying values were recoded to the next highest intensity recorded in the sample (42.0 units per day) to ensure a more representative measure of mean intensity. | ||||
| Cannabis ( 350) | 98.6 | 98.3 | 55.2 (1–90) | 1.9 (1.49; 0.11–10.7) |
| Amphetamines ( 188) | 87.8 | 79.3 | 7.7 (1–70) | 0.9 (0.54; 0.02–2.5) |
| Ecstasy ( 177) | 93.8 | 87.6 | 9.0 (1–51) | 1.7 (1.07; 0.5–5.0) |
| LSD ( 91) | 68.1 | 50.5 | 5.3 (1–39) | 1.3 (0.67; 0.5–4.0) |
| Cocaine ( 184) | 93.5 | 85.3 | 11.3 (1–80) | 0.8 (0.53; 0.01–3.5) |
| Alcohol ( 327) | 95.4 | 94.5 | 39.7 (1–90) | 9.8 (6.74; 0.5–42.0) |
| Substance (lifetime users) . | Lifetime users consuming in past year (%) . | Lifetime usersconsuming in past 90 days (%) . | Mean days used in past 90 days (range) . | Average amount on typical using day[SD (range)] . |
|---|---|---|---|---|
| Grams. | ||||
| Number of tablets. | ||||
| Number of units (1 unit = 8 g ethanol approximately). | ||||
| One respondent reported smoking 21.3 g of cannabis on a typical using day. This outlying value was recoded to the next highest intensity recorded (10.6 g). | ||||
| Two alcohol users reported consuming 48.0 and 50.0 units of alcohol on a typical using day respectively. These outlying values were recoded to the next highest intensity recorded in the sample (42.0 units per day) to ensure a more representative measure of mean intensity. | ||||
| Cannabis ( 350) | 98.6 | 98.3 | 55.2 (1–90) | 1.9 (1.49; 0.11–10.7) |
| Amphetamines ( 188) | 87.8 | 79.3 | 7.7 (1–70) | 0.9 (0.54; 0.02–2.5) |
| Ecstasy ( 177) | 93.8 | 87.6 | 9.0 (1–51) | 1.7 (1.07; 0.5–5.0) |
| LSD ( 91) | 68.1 | 50.5 | 5.3 (1–39) | 1.3 (0.67; 0.5–4.0) |
| Cocaine ( 184) | 93.5 | 85.3 | 11.3 (1–80) | 0.8 (0.53; 0.01–3.5) |
| Alcohol ( 327) | 95.4 | 94.5 | 39.7 (1–90) | 9.8 (6.74; 0.5–42.0) |
Proportion (%) of those who have used [substance] more than once, who endorsed each functional statement for their use in the past year
| Used [substance] to... . | Cannabis ( 345) . | Amphetamines ( 160) . | Ecstasy ( 357) . | LSD ( 58) . | Cocaine ( 168) . | Alcohol ( 312) . |
|---|---|---|---|---|---|---|
| Abbreviations for these items shown in brackets are used in the text of this paper. | ||||||
| Indication of rank according to item scores on Likert scales. | ||||||
| Make yourself feel better when down or depressed (FEEL BETTER) | 69.0 | 43.1 | 48.4 | 20.7 | 61.9 | 69.9 |
| Help you `keep going' on a night out with friends (KEEP GOING) | 35.9 | 95.6 | 91.1 | 58.6 | 84.5 | 66.7 |
| Help you feel elated or euphoric (ELATED/EUPHORIC) | 46.1 | 60.6 | 77.7 | 72.4 | 57.1 | 51.3 |
| Just get really stoned or intoxicated (INTOXICATED) | 90.7 | 55.0 | 68.2 | 77.6 | 66.1 | 89.1 |
| Help you lose weight (LOSE WEIGHT) | – | 23.1 | 7.0 | – | 6.0 | – |
| Help you enjoy the company of your friends (ENJOY COMPANY) | 66.4 | 58.1 | 63.1 | 58.6 | 61.3 | 74.0 |
| Help you to relax (RELAX) | 96.8 | 13.1 | 29.9 | 17.2 | 28.6 | 82.7 |
| Help you feel more confident or more able to talk to people in a social situation (INCREASE CONFIDENCE) | 36.5 | 53.1 | 42.0 | 10.3 | 66.1 | 70.2 |
| Improve the effects of other substances (IMPROVE EFFECTS) | 44.3 | 37.5 | 27.4 | 29.3 | 26.2 | 41.0 |
| Help ease the after effects of other substances (AFTER EFFECTS) | 64.6 | 11.9 | 8.3 | 3.4 | 12.5 | 35.9 |
| Help you to stay awake (STAY AWAKE) | 7.5 | 91.3 | 72.0 | 50.0 | 69.0 | 10.6 |
| Help you lose your inhibitions (LOSE INHIBITIONS) | 28.1 | 41.9 | 49.7 | 36.2 | 41.1 | 51.0 |
| Enhance feelings when having sex (ENHANCE SEX) | 27.8 | 31.9 | 63.1 | 25.9 | 52.4 | 32.1 |
| Help you stop worrying about a problem (STOP WORRYING) | 57.7 | 22.5 | 32.5 | 15.5 | 41.7 | 55.1 |
| Help make something you were doing less boring (DECREASE BOREDOM) | 70.1 | 45.6 | 36.3 | 44.8 | 53.6 | 60.6 |
| Help you to sleep (SLEEP) | 69.6 | – | – | – | – | 30.4 |
| Help you to concentrate or to work or study (WORK) | 20.9 | 29.4 | 3.2 | 1.7 | 6.0 | 6.4 |
| Enhance an activity such as listening to music or playing a game or sport (ENHANCE ACTIVITY) | 72.8 | 66.2 | 79.6 | 72.4 | 60.7 | 51.6 |
| Total number of items in the scale | 17 | 17 | 17 | 16 | 17 | 17 |
| Chronbach's α for scale items | 0.78 | 0.74 | 0.76 | 0.73 | 0.78 | 0.84 |
| Mean total number of different functions endorsed for use of [substance] (range) | 9.0 (0–17) | 7.8 (0–16) | 8.0 (0–16) | 5.9 (0–15) | 7.9 (0–17) | 8.8 (0–17) |
| Used [substance] to... . | Cannabis ( 345) . | Amphetamines ( 160) . | Ecstasy ( 357) . | LSD ( 58) . | Cocaine ( 168) . | Alcohol ( 312) . |
|---|---|---|---|---|---|---|
| Abbreviations for these items shown in brackets are used in the text of this paper. | ||||||
| Indication of rank according to item scores on Likert scales. | ||||||
| Make yourself feel better when down or depressed (FEEL BETTER) | 69.0 | 43.1 | 48.4 | 20.7 | 61.9 | 69.9 |
| Help you `keep going' on a night out with friends (KEEP GOING) | 35.9 | 95.6 | 91.1 | 58.6 | 84.5 | 66.7 |
| Help you feel elated or euphoric (ELATED/EUPHORIC) | 46.1 | 60.6 | 77.7 | 72.4 | 57.1 | 51.3 |
| Just get really stoned or intoxicated (INTOXICATED) | 90.7 | 55.0 | 68.2 | 77.6 | 66.1 | 89.1 |
| Help you lose weight (LOSE WEIGHT) | – | 23.1 | 7.0 | – | 6.0 | – |
| Help you enjoy the company of your friends (ENJOY COMPANY) | 66.4 | 58.1 | 63.1 | 58.6 | 61.3 | 74.0 |
| Help you to relax (RELAX) | 96.8 | 13.1 | 29.9 | 17.2 | 28.6 | 82.7 |
| Help you feel more confident or more able to talk to people in a social situation (INCREASE CONFIDENCE) | 36.5 | 53.1 | 42.0 | 10.3 | 66.1 | 70.2 |
| Improve the effects of other substances (IMPROVE EFFECTS) | 44.3 | 37.5 | 27.4 | 29.3 | 26.2 | 41.0 |
| Help ease the after effects of other substances (AFTER EFFECTS) | 64.6 | 11.9 | 8.3 | 3.4 | 12.5 | 35.9 |
| Help you to stay awake (STAY AWAKE) | 7.5 | 91.3 | 72.0 | 50.0 | 69.0 | 10.6 |
| Help you lose your inhibitions (LOSE INHIBITIONS) | 28.1 | 41.9 | 49.7 | 36.2 | 41.1 | 51.0 |
| Enhance feelings when having sex (ENHANCE SEX) | 27.8 | 31.9 | 63.1 | 25.9 | 52.4 | 32.1 |
| Help you stop worrying about a problem (STOP WORRYING) | 57.7 | 22.5 | 32.5 | 15.5 | 41.7 | 55.1 |
| Help make something you were doing less boring (DECREASE BOREDOM) | 70.1 | 45.6 | 36.3 | 44.8 | 53.6 | 60.6 |
| Help you to sleep (SLEEP) | 69.6 | – | – | – | – | 30.4 |
| Help you to concentrate or to work or study (WORK) | 20.9 | 29.4 | 3.2 | 1.7 | 6.0 | 6.4 |
| Enhance an activity such as listening to music or playing a game or sport (ENHANCE ACTIVITY) | 72.8 | 66.2 | 79.6 | 72.4 | 60.7 | 51.6 |
| Total number of items in the scale | 17 | 17 | 17 | 16 | 17 | 17 |
| Chronbach's α for scale items | 0.78 | 0.74 | 0.76 | 0.73 | 0.78 | 0.84 |
| Mean total number of different functions endorsed for use of [substance] (range) | 9.0 (0–17) | 7.8 (0–16) | 8.0 (0–16) | 5.9 (0–15) | 7.9 (0–17) | 8.8 (0–17) |
Combined functional substance use reported by the sample over the past year
| . | Cannabis ( 153) . | Amphetamines ( 60) . | Ecstasy ( 43) . | LSD ( 17) . | Cocaine ( 44) . | Alcohol ( 128) . |
|---|---|---|---|---|---|---|
| Used with [substance] to improve its effects | ||||||
| cannabis | – | 16 | 18 | 8 | 14 | 93 |
| amphetamines | 37 | – | 20 | 7 | 3 | 29 |
| ecstasy | 55 | 39 | – | 11 | 19 | 45 |
| LSD | 24 | 10 | 9 | – | 3 | 6 |
| cocaine | 42 | 4 | 5 | 1 | – | 45 |
| alcohol | 110 | 38 | 23 | 4 | 29 | – |
| hallucinogenic mushrooms | 2 | 0 | 0 | 1 | 0 | 1 |
| . | Cannabis ( 153) . | Amphetamines ( 60) . | Ecstasy ( 43) . | LSD ( 17) . | Cocaine ( 44) . | Alcohol ( 128) . |
|---|---|---|---|---|---|---|
| Used with [substance] to improve its effects | ||||||
| cannabis | – | 16 | 18 | 8 | 14 | 93 |
| amphetamines | 37 | – | 20 | 7 | 3 | 29 |
| ecstasy | 55 | 39 | – | 11 | 19 | 45 |
| LSD | 24 | 10 | 9 | – | 3 | 6 |
| cocaine | 42 | 4 | 5 | 1 | – | 45 |
| alcohol | 110 | 38 | 23 | 4 | 29 | – |
| hallucinogenic mushrooms | 2 | 0 | 0 | 1 | 0 | 1 |
| . | Cannabis ( 223) . | Amphetamines ( 19) . | Ecstasy ( 15) . | LSD ( 3) . | Cocaine ( 23) . | Alcohol ( 112) . |
|---|---|---|---|---|---|---|
| Used to help ease after effects of [substance] | ||||||
| cannabis | – | 5 | 2 | 0 | 4 | 18 |
| amphetamines | 83 | – | 6 | 1 | 1 | 47 |
| ecstasy | 114 | 7 | – | 3 | 10 | 59 |
| LSD | 29 | 0 | 5 | – | 0 | 13 |
| cocaine | 80 | 1 | 1 | 0 | – | 34 |
| alcohol | 70 | 18 | 7 | 0 | 14 | – |
| . | Cannabis ( 223) . | Amphetamines ( 19) . | Ecstasy ( 15) . | LSD ( 3) . | Cocaine ( 23) . | Alcohol ( 112) . |
|---|---|---|---|---|---|---|
| Used to help ease after effects of [substance] | ||||||
| cannabis | – | 5 | 2 | 0 | 4 | 18 |
| amphetamines | 83 | – | 6 | 1 | 1 | 47 |
| ecstasy | 114 | 7 | – | 3 | 10 | 59 |
| LSD | 29 | 0 | 5 | – | 0 | 13 |
| cocaine | 80 | 1 | 1 | 0 | – | 34 |
| alcohol | 70 | 18 | 7 | 0 | 14 | – |
Percentage of participants who reported having used at least one of the target substances to fulfil each of the different functions over the past year ( n = 364)
| Used at least one target substance to... . | Male (%) ( 205) . | Female (%) ( 159) . | Total (%) ( 364) . | χ . |
|---|---|---|---|---|
| < 0.05, < 0.01; < 0.001. | ||||
| 1. RELAX | 96.1 | 97.5 | 96.7 | 0.54 |
| 2. INTOXICATED | 96.1 | 96.9 | 96.4 | 0.15 |
| 3. KEEP GOING | 95.6 | 96.2 | 95.9 | 0.09 |
| 4. ENHANCE ACTIVITY | 90.2 | 86.2 | 88.5 | 1.46 |
| 5. FEEL BETTER | 84.9 | 89.3 | 86.8 | 1.54 |
| 6. ENJOY COMPANY | 83.4 | 86.2 | 84.6 | 0.52 |
| 7. DECREASE BOREDOM | 82.0 | 84.3 | 83.0 | 0.34 |
| 8. INCREASE CONFIDENCE | 79.0 | 87.4 | 82.7 | 4.41 |
| 9. STAY AWAKE | 78.0 | 87.4 | 82.1 | 5.36 |
| 10. FEEL ELATED/EUPHORIC | 77.1 | 74.2 | 75.8 | 0.40 |
| 11. STOP WORRYING | 71.7 | 79.9 | 75.3 | 3.21 |
| 12. SLEEP | 73.7 | 67.9 | 71.2 | 1.43 |
| 13. AFTER EFFECTS | 71.2 | 65.4 | 68.7 | 1.41 |
| 14. LOSE INHIBITIONS | 62.4 | 73.0 | 67.0 | 4.48 |
| 15. ENHANCE SEX | 57.6 | 69.2 | 62.6 | 5.17 |
| 16. IMPROVE EFFECTS | 65.9 | 48.4 | 58.2 | 11.18 |
| 17. WORK | 33.7 | 30.2 | 32.1 | 0.49 |
| 18. LOSE WEIGHT | 7.8 | 29.6 | 17.3 | 29.6 |
| Used at least one target substance to... . | Male (%) ( 205) . | Female (%) ( 159) . | Total (%) ( 364) . | χ . |
|---|---|---|---|---|
| < 0.05, < 0.01; < 0.001. | ||||
| 1. RELAX | 96.1 | 97.5 | 96.7 | 0.54 |
| 2. INTOXICATED | 96.1 | 96.9 | 96.4 | 0.15 |
| 3. KEEP GOING | 95.6 | 96.2 | 95.9 | 0.09 |
| 4. ENHANCE ACTIVITY | 90.2 | 86.2 | 88.5 | 1.46 |
| 5. FEEL BETTER | 84.9 | 89.3 | 86.8 | 1.54 |
| 6. ENJOY COMPANY | 83.4 | 86.2 | 84.6 | 0.52 |
| 7. DECREASE BOREDOM | 82.0 | 84.3 | 83.0 | 0.34 |
| 8. INCREASE CONFIDENCE | 79.0 | 87.4 | 82.7 | 4.41 |
| 9. STAY AWAKE | 78.0 | 87.4 | 82.1 | 5.36 |
| 10. FEEL ELATED/EUPHORIC | 77.1 | 74.2 | 75.8 | 0.40 |
| 11. STOP WORRYING | 71.7 | 79.9 | 75.3 | 3.21 |
| 12. SLEEP | 73.7 | 67.9 | 71.2 | 1.43 |
| 13. AFTER EFFECTS | 71.2 | 65.4 | 68.7 | 1.41 |
| 14. LOSE INHIBITIONS | 62.4 | 73.0 | 67.0 | 4.48 |
| 15. ENHANCE SEX | 57.6 | 69.2 | 62.6 | 5.17 |
| 16. IMPROVE EFFECTS | 65.9 | 48.4 | 58.2 | 11.18 |
| 17. WORK | 33.7 | 30.2 | 32.1 | 0.49 |
| 18. LOSE WEIGHT | 7.8 | 29.6 | 17.3 | 29.6 |
We gratefully acknowledge research support from the Health Education Authority (HEA). The views expressed in this paper are those of the authors and do not necessarily reflect those of the HEA. We would also like to thank the anonymous referees for helpful comments and suggestions on an earlier draft of this paper.
Biernacki, P. (1986) Pathways from Heroin Addiction: Recovery without Treatment . Temple University Press, Philadelphia, PA.
Boys, A., Marsden, J., Griffiths, P., Fountain, J., Stillwell, G. and Strang, J. ( 1999 ) Substance use among young people: the relationship between perceived functions and behavioural intentions. Addiction , 94 , 1043 –1050.
Boys, A., Marsden, J., Fountain, J., Griffiths, P., Stillwell, G. and Strang, J. ( 1999 ) What influences young people's use of drugs? A qualitative study of decision-making. Drugs: Education, Prevention and Policy , 6 , 373 –389.
Boys, A., Marsden, J. and Griffiths. P. ( 1999 ) Reading between the lines: is cocaine becoming the stimulant of choice for urban youth? Druglink , 14 , 20 –23.
Boys, A., Fountain, J., Marsden, J., Griffiths, P., Stillwell, G. and Strang, J. (2000a) Drug Decisions: A Qualitative Study of Young People , Drugs and Alcohol . Health Education Authority, London.
Boys, A., Marsden, J., Griffiths, P. and Strang, J. ( 2000 ) Drug use functions predict cocaine-related problems. Drug and Alcohol Review , 19 , 181 –190.
Butler, M. C., Gunderson, E. K. E. and Bruni, J. R. ( 1981 ) Motivational determinants of illicit drug use: an assessment of underlying dimensions and their relationship to behaviour. International Journal of the Addictions , 16 , 243 –252.
Carman, R. S. ( 1979 ) Motivations for drug use and problematic outcomes among rural junior high school students. Addictive Behaviors , 4 , 91 –93.
Cato, B. M. ( 1992 ) Youth's recreation and drug sensations: is there a relationship? Journal of Drug Education , 22 , 293 –301.
Edwards, G., Chandler, J. and Peto, J. ( 1972 ) Motivation for drinking among men in a London suburb, Psychological Medicine , 2 , 260 –271.
European Monitoring Centre for Drugs and Drug Addiction (1998) Annual Report on the State of the Drugs Problem in the European Union . EMCDDA, Lisbon.
Griffiths, P., Gossop, M., Powis, B. and Strang, J. ( 1993 ) Reaching hidden populations of drug users by privileged access interviewers: methodological and practical issues. Addiction , 88 , 1617 –1626.
HIT (1996) Chill Out: A Clubber's Guide—The Second Coming . HIT, Liverpool.
Johnston, L. D., O'Malley, P. M. and Bachman J. G. (1997) National Survey Results on Drug Use from the Monitoring the Future Study , 1975–1996: Secondary School Students . US DHHS, National Institute on Drug Abuse, Rockville, MD.
Johnston, L. D., O'Malley, P. M. and Bachman J. G. (2000) The Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings 1999 . US DHHS, National Institute on Drug Abuse, Rockville, MD.
Lenton, S., Boys, A. and Norcross, K. ( 1997 ) Raves, drugs and experience: drug use by a sample of people who attend raves in Western Australia. Addiction , 92 , 1327 –1337.
Marsden, J., Gossop, M., Stewart, D., Best, D., Farrell, M., Edwards, C., Lehmann, P. and Strang, J. ( 1998 ) The Maudsley Addiction Profile (MAP): a brief instrument for assessing treatment outcome. Addiction , 93 , 1857 –1867.
McKay, J. R., Murphy, R. T., McGuire, J., Rivinus, T. R. and Maisto, S. A. ( 1992 ) Incarcerated adolescents' attributions for drug and alcohol use. Addictive Behaviors , 17 , 227 –235.
Newcomb. M. D., Chou, C.-P., Bentler, P. M. and Huba, G. J. ( 1988 ) Cognitive motivations for drug use among adolescents: longitudinal tests of gender differences and predictors of change in drug use. Journal of Counselling Psychology , 35 , 426 –438.
Power, R. ( 1995 ) A model for qualitative action research amongst illicit drug users. Addiction Research , 3 , 165 –181.
Power, R., Power, T. and Gibson, N. ( 1996 ) Attitudes and experience of drug use amongst a group of London teenagers. Drugs: Education, Prevention and Policy , 3 , 71 –80.
Ramsay, M. and Partridge, S. (1999) Drug Misuse Declared in 1998: Results from the British Crime Survey . Home Office, London.
Release (1997) Release Drugs and Dance Survey: An Insight into the Culture . Release, London.
Sadava, S. ( 1975 ) Research approaches in illicit drug use: a critical review. Genetic Psychology Monographs , 91 , 3 –59.
Tackling Drugs to Build a Better Britain (1998) The Government's 10-year Strategy on Drug Misuse. Central Drugs Co-ordinating Unit, London.
Van Meter, K. M. (1990) Methodological and design issues: techniques for assessing the representatives of snowball samples. In Lambert, E. Y. (ed.), The Collection and Interpretation of Data from Hidden Populations . US DHHS, National Institute on Drug Abuse, Rockville, MD, pp. 31–33.
Wibberley, C. and Price, J. ( 2000 ) Patterns of psycho-stimulant drug use amongst `social/operational users': implications for services. Addiction Research , 8 , 95 –111.
WHO (1997) Amphetamine-type Stimulants: A Report from the WHO Meeting on Amphetamines , MDMA and other Psychostimulants , Geneva, 12–15 November 1996. Programme on Substance Abuse, Division of Mental Health and Prevention of Substance Abuse, WHO, Geneva.
| Month: | Total Views: |
|---|---|
| November 2016 | 106 |
| December 2016 | 26 |
| January 2017 | 130 |
| February 2017 | 438 |
| March 2017 | 566 |
| April 2017 | 809 |
| May 2017 | 444 |
| June 2017 | 106 |
| July 2017 | 66 |
| August 2017 | 193 |
| September 2017 | 474 |
| October 2017 | 647 |
| November 2017 | 787 |
| December 2017 | 3,578 |
| January 2018 | 4,050 |
| February 2018 | 4,172 |
| March 2018 | 6,061 |
| April 2018 | 5,699 |
| May 2018 | 4,355 |
| June 2018 | 3,217 |
| July 2018 | 2,979 |
| August 2018 | 3,640 |
| September 2018 | 3,719 |
| October 2018 | 3,989 |
| November 2018 | 4,227 |
| December 2018 | 4,056 |
| January 2019 | 3,401 |
| February 2019 | 3,752 |
| March 2019 | 5,071 |
| April 2019 | 5,171 |
| May 2019 | 5,669 |
| June 2019 | 4,881 |
| July 2019 | 4,563 |
| August 2019 | 4,036 |
| September 2019 | 5,248 |
| October 2019 | 6,512 |
| November 2019 | 5,277 |
| December 2019 | 3,308 |
| January 2020 | 3,569 |
| February 2020 | 4,416 |
| March 2020 | 3,889 |
| April 2020 | 3,668 |
| May 2020 | 1,868 |
| June 2020 | 2,416 |
| July 2020 | 2,215 |
| August 2020 | 2,612 |
| September 2020 | 3,276 |
| October 2020 | 4,074 |
| November 2020 | 4,599 |
| December 2020 | 4,431 |
| January 2021 | 4,464 |
| February 2021 | 5,133 |
| March 2021 | 6,737 |
| April 2021 | 6,184 |
| May 2021 | 6,006 |
| June 2021 | 3,161 |
| July 2021 | 2,094 |
| August 2021 | 2,075 |
| September 2021 | 3,467 |
| October 2021 | 3,660 |
| November 2021 | 4,289 |
| December 2021 | 3,412 |
| January 2022 | 2,564 |
| February 2022 | 3,176 |
| March 2022 | 4,355 |
| April 2022 | 3,891 |
| May 2022 | 3,911 |
| June 2022 | 2,572 |
| July 2022 | 1,851 |
| August 2022 | 1,795 |
| September 2022 | 2,353 |
| October 2022 | 3,057 |
| November 2022 | 3,443 |
| December 2022 | 2,281 |
| January 2023 | 2,672 |
| February 2023 | 3,068 |
| March 2023 | 3,993 |
| April 2023 | 3,083 |
| May 2023 | 2,959 |
| June 2023 | 2,196 |
| July 2023 | 1,591 |
| August 2023 | 1,532 |
| September 2023 | 1,746 |
| October 2023 | 2,315 |
| November 2023 | 1,881 |
| December 2023 | 1,302 |
| January 2024 | 1,584 |
| February 2024 | 1,504 |
| March 2024 | 1,875 |
| April 2024 | 1,702 |
| May 2024 | 1,406 |
| June 2024 | 599 |
| July 2024 | 443 |
| August 2024 | 388 |
| September 2024 | 246 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Understanding the Demand for Illegal Drugs (2010)
Chapter: 1 introduction, 1 introduction.
A merica’s problem with illegal drugs seems to be declining, and it is certainly less in the news than it was 20 years ago. Surveys have shown a decline in the number of users dependent on expensive drugs (Office of National Drug Control Policy, 2001), an aging of the population in treatment (Trunzo and Henderson, 2007), and a decline in the violence related to drug markets (Pollack et al., 2010). Still, research indicates that illegal drugs remain a concern for the majority of Americans (Caulkins and Mennefee, 2009; Gallup Poll, 2009).
There is virtually no disagreement that the trafficking in and use of cocaine, heroin, and methamphetamine continue to cause great harm to the nation, particularly to vulnerable minority communities in the major cities. In contrast, there is disagreement about marijuana use, which remains a part of adolescent development for about half of the nation’s youth. The disagreement concerns the amount, source, and nature of the harms from marijuana. Some note, for example, that most of those who use marijuana use it only occasionally and neither incur nor cause harms and that marijuana dependence is a much less serious problem than dependence on alcohol or cocaine. Others emphasize the evidence of a potential for triggering psychosis (Arseneault et al., 2004) and the strengthening evidence for a gateway effect (i.e., an opening to the use of other drugs) (Fergusson et al., 2006). The uncertainty of the causal mechanism is reflected in the fact that the gateway studies cannot disentangle the effect of the drug itself from its status as an illegal good (Babor et al., 2010).
The federal government probably spends $20 billion per year on a wide array of interventions to try to reduce drug consumption in the United States, from crop eradication in Colombia to mass media prevention programs aimed at preteens and their parents. 1 State and local governments spend comparable amounts, mostly for law enforcement aimed at suppressing drug markets. 2 Yet the available evidence, reviewed in detail in this report, shows that drugs are just as cheap and available as they have ever been.
Though fewer young people are starting to use drugs than in some previous years, for each successive birth cohort that turns 21, approximately half have experimented with illegal drugs. The number of people who are dependent on cocaine, heroin, and methamphetamine is probably declining modestly, 3 and drug-related violence has appears to have declined sharply. 4 At the same time, injecting drug use is still a major vector for HIV transmission, and drug markets blight parts of many U.S. cities.
The declines in drug use that have occurred in recent years are probably mostly the natural working out of old epidemics. Policy measures— whether they involve prevention, treatment, or enforcement—have met with little success at the population level (see Chapter 4 ). Moreover, research on prevention has produced little evidence of any targeted interventions that make a substantial difference in initiation to drugs when implemented on a large scale. For treatment programs, there is a large body of evidence of effectiveness and cost-effectiveness (reviewed in Babor et al., 2010), but the supply of treatment facilities is inadequate and,
|
| The official estimate from the Office of National Drug Control Policy of $14.8 billion in fiscal 2009 excludes a number of major items, such as the cost of prosecuting and incarcerating those arrested by federal agencies for violations of drug laws. See Carnevale (2009) for a detailed analysis of the limits of the official estimate of the federal drug budget. |
|
| The only estimates of drug-related expenditures by state and local governments are for 1990 and 1991 (Office of National Drug Control Policy, 1993). Given the number of people prosecuted and incarcerated each year for drug offenses, that estimate remains a plausible but unsubstantiated claim. |
|
| The most recent published estimates only extend through 2000 (Office of National Drug Control Policy, 2001). |
|
| There are no specific indices that measure drug-related violence. The assumption of reduced violence reflects an inference from (1) the aging of the populations that are dependent on cocaine, heroin, and methamphetamine as reflected in the Treatment Episode Data Set, maintained by the Substance Abuse and Mental Health Administration of the U.S. Department of Health and Human Services; (2) the declining share of arrests of drug users that are for violent crimes, as reflected in the Surveys of Prison and Jail Inmates (Pollack et al., 2010); (3) the 70 percent decline in homicides since 1991; and (4) the increasing share of drug transactions that are conducted in nonpublic settings. |
perversely, not enough of those who need treatment are persuaded to seek it (see Chapter 4 ). Efforts to raise the price of drugs through interdiction and other enforcement programs have not had the intended effects: the prices of cocaine and heroin have declined for more than 25 years, with only occasional upward blips that rarely last more than 9 months (Walsh, 2009).
STUDY PROJECT AND GOALS
Given the persistence of drug demand in the face of lengthy and expensive efforts to control the markets, the National Institute of Justice asked the National Research Council (NRC) to undertake a study of current research on the demand for drugs in order to help better focus national efforts to reduce that demand. In response to that request, the NRC formed the Committee on Understanding and Controlling the Demand for Illegal Drugs. The committee convened a workshop of leading researchers in October 2007 and held two follow-up meetings to prepare this report. The statement of task for this project is as follows:
An ad hoc committee will conduct a workshop-based study that will identify and describe what is known about the nature and scope of markets for illegal drugs and the characteristics of drug users. The study will include exploration of research issues associated with drug demand and what is needed to learn more about what drives demand in the United States. The committee will specifically address the following issues:
What is known about the nature and scope of illegal drug markets and differences in various markets for popular drugs?
What is known about the characteristics of consumers in different markets and why the market remains robust despite the risks associated with buying and selling?
What issues can be identified for future research? Possibilities include the respective roles of dependence, heavy use, and recreational use in fueling the market; responses that could be developed to address different types of users; the dynamics associated with the apparent failure of policy interventions to delay or inhibit the onset of illegal drug use for a large proportion of the population; and the effects of enforcement on demand reduction.
Drawing on commissioned papers and presentations and discussions at a public workshop that it will plan and hold, the committee will prepare a report on the nature and operations of the illegal drug market in the United States and the research issues identified as having potential for informing policies to reduce the demand for illegal drugs.
The committee drew on economic models and their supporting data, as well as other research, as one part of the evidentiary base for this
report. However, the context for and content of this report were informed as well by the general discussion and the presentations in the workshop. The committee was not able to fully address task 2 because research in that area is not strong enough to give an accurate description of consumers across different markets nor to address the questions about why markets remain robust despite the risks associated with buying and selling. The discussion at the workshop underscored the point that neither the available ethnographic research nor the limited longitudinal research on drug-seeking behavior is strong enough to inform these questions related to task 2. With regard to task 3, the committee benefitted considerably from the paper by Jody Sindelar that was presented at the workshop and its discussion by workshop participants.
This study was intended to complement Informing America’s Policy on Illegal Drugs: What We Don’t Know Keeps Hurting Us (National Research Council, 2001) by giving more attention to the sources of demand and assessing the potential of demand-side interventions to make a substantial difference to the nation’s drug problems. This report therefore refers to supply-side considerations only to the extent necessary to understand demand.
The charge to the committee was extremely broad. It could have included reviewing the literature on such topics as characteristics of substance users, etiology of initiation of use, etiology of dependence, drug use prevention programs, and drug treatments. Two considerations led to narrowing the focus of our work. The first was substantive. Each of the topics just noted involves a very large field of well-developed research, and each has been reviewed elsewhere. Moreover, each of these areas of inquiry is currently expanding as a result of new research initiatives 5 and new technologies (e.g., neuroimaging, genetics). The second consideration was practical: given the available resources, we could not undertake a complete review of the entire field.
Thus, we decided to focus our work and this report tightly on demand models in the field of economics and to evaluate the data needs for advancing this relatively undeveloped area of investigation. That is, this area has a relatively shorter history of accumulated findings than the more clinical, biological, and epidemiological areas of drug research. Yet it is arguably better situated to inform government policy at the national level. A report on economic models and supporting data seemed to us more timely than a report on drug consumers and drug interventions.
The rest of this chapter briefly lays out some concepts that provide a basis for understanding the committee’s work and the rest of the report.
|
| These include the National Epidemiologic Survey on Alcohol and Related Conditions and the Community Epidemiology Work Group of the National Institute on Drug Abuse. |
Chapter 2 presents the economic framework that seems most useful for studying the phenomenon of drug demand. It emphasizes the importance of understanding the responsiveness of demand and supply to price, which is the intermediate variable targeted by the principal government programs in the United States, namely, drug law enforcement. Chapter 3 then examines changes in the consumption of drugs and assesses the various indicators that are available to measure that consumption. Chapter 4 turns to the program type that most focuses specifically on reducing drug demand, the treatment of dependent users. It considers how well these programs work and how the treatment system might be expanded to further reduce consumption. Finally, Chapter 5 presents our recommendations for how the data and research base might be built to improve understanding of the demand for drugs and policies to reduce it.
PROGRAM CONCEPTS
A standard approach to considering drug policy is to divide programs into supply side and demand side. This approach accepts that drugs, as commodities, albeit illegal ones, are sold in markets. Supply-side programs aim to reduce drug consumption by making it more expensive to purchase drugs through increasing costs to producers and distributors. Demand-side programs try to lower consumption by reducing the number of people who, at a given price, seek to buy drugs; the amount that the average user wishes to consume; or the nonmonetary costs of obtaining the drugs. This approach has value, but it also raises questions.
The value of this framework is that it allows systematic evaluation of programs. A successful supply-side program will raise the price of drugs, as well as reduce the quantity available, while a demand-side program will lower both the number of users and the quantity consumed, as well as eventually reducing the price. As noted above, this report is primarily focused on improving understanding of the sources of demand.
There are two basic objections to this approach. First, some programs have both demand- and supply-side effects. Since many dealers are themselves heavy users, drug treatment will reduce supply, just as incarceration of drug dealers lowers demand. Second, there is a collection of programs that do not attempt to reduce demand or supply; rather, their goal is to reduce the damage that drug use and drug markets cause society, which are generally referred to as “harm-reduction” programs (Iversen, 2005; National Institute on Drug Abuse, 2010). 6 Nonetheless, the classifi-
|
| An expanded classification to include harm-reduction programs is common in the drug control strategies of other countries, including Australia, Switzerland, and the United Kingdom. |
cation of interventions into demand reduction and supply reduction is a very helpful heuristic for policy purposes, as well as being written into the legislation under which the Office of National Drug Control Policy operates.
What determines the demand for drugs? Clearly, many different factors play a role: cultural, economic, and social influences are all important. At the individual level, a rich set of correlates have been explored, either in large-scale cross-sectional surveys (such as the National Survey on Drug Use and Health and the National Household Survey on Drug Abuse) or in small-scale longitudinal studies (see, e.g., Wills et al., 2005). Below we briefly summarize the complex findings of those studies.
Less has been done at the population level. It is known that rich western countries differ substantially in the extent of drug use, in ways that do not seem to reflect policy differences. For example, despite the relatively easy access to marijuana in the Netherlands, that nation has a prevalence rate that is in the middle of the pack for Europe, while Britain, despite what may be characterized as a pragmatic and relatively evidence-oriented drug policy, has Europe’s highest rates of cocaine and heroin addiction (European Monitoring Center for Drugs and Drug Addiction, 2007). There is only minimal empirical research that has attempted to explain those differences. Similarly, there is very little known about why epidemics of drug use occur at specific times. In the United States, for example, there is no known reason for the sudden spread of methamphetamine from its long-term West Coast concentration to the Midwest that began in the early 1990s. There are only the most speculative conjectures as to the proximate causes.
A DYNAMIC AND HETEROGENEOUS PROCESS
The committee’s starting point is that drug use is a dynamic phenomenon, both at the individual and community levels. In the United States there is a well-established progression of use of substances for individuals, starting with alcohol or cigarettes (or both) and proceeding through marijuana (at least until recently) possibly to more dangerous and expensive drugs (see, e.g., Golub and Johnson, 2001). Such a progression seems to be a common feature of drug use, although the exact sequence might not apply in other countries and may change over time. For example, cigarettes may lose their status as a gateway drug because of new restrictions on their use. 7 Recently, abuse of prescription drugs has emerged as a possible gateway, with high prevalence rates reported for youth aged 18-25;
|
| In Amsterdam, people can smoke marijuana at indoor cafes but not marijuana mixed with tobacco. |
however, because of limited economic research on this phenomenon, this report’s focus is on completely illegal drugs.
At the population level, there are epidemics, in which, like a fashion good, a new drug becomes popular rapidly in part because of its novelty and then, often just as rapidly, loses its appeal to those who have not tried it. For addictive substances (including marijuana but not hallucinogens, such as LSD), that leaves behind a cohort of users who experimented with the drug and then became habituated to it.
An important and underappreciated element of the demand for illegal drugs is its variation in many dimensions. For example, the demand for marijuana may be much more responsive to price changes than the demand for heroin because fewer of those who use marijuana are drug dependent (Iversen, 2005; National Institute on Drug Abuse, 2010). Users who are employed, married, and not poor may be more likely to desist than users of the same drug who are unemployed, not part of an intact household, and poor. There may be differences in the characteristics of demand associated with when the specific drug first became available in a particular community, that is, whether it is early or late in a national drug “epidemic.”
There are also unexplained long-term differences in the drug patterns in cities that are close to each other. In Washington, DC, in 1987 half of all those arrested for a criminal offense (not just for drugs) tested positive for phencyclidine, while in Baltimore, 35 miles away, the drug was almost unknown. Although the Washington rate had fallen to approximately 10 percent in 2009 (District of Columbia Pretrial Services Agency, 2009), it remains far higher than in other cities. More recently, the spread of methamphetamine has shown the same unevenness: in San Antonio only 2.3 percent of arrestees tested positive for methamphetamine in 2002; in Phoenix, the figure was 31.2 percent (National Institute of Justice, 2003). These differences had existed for more than 10 years.
The implication of this heterogeneity is that programs that work for a particular drug, user type, place, or period may be much less effective under other circumstances, which substantially complicates any research task. It is hard to know how general are findings on, say, the effectiveness of a prevention program aimed at methamphetamine use by adolescents in a city where the drug has no history. Will this program also be effective for trying to prevent cocaine use among young adults in cities that have long histories of that drug?
This report does not claim to provide the answers to such ambitious questions. It does intend, however, to equip policy officials and the public to understand what is known and what needs to be done to provide a more sound base for answering them.
Arseneault, L., M. Cannon, J. Witten, and R. Murray. (2004). Causal association between cannabis and psychosis: Examination of the evidence. British Journal of Psychiatry, 184 , 110-117.
Babor, T., J. Caulkins, G. Edwards, D. Foxcroft, K. Humphreys, M.M. Mora, I. Obot, J. Rehm, P. Reuter, R. Room, I. Rossow, and J. Strang. (2010). Drug Policy and the Public Good . New York: Oxford University Press.
Carnevale, J. (2009). Restoring the Integrity of the Office of National Drug Control Policy. Testimony at the hearing on the Office of National Drug Control Policy’s Fiscal Year 2010 National Drug Control Budget and the Policy Priorities of the Office of National Drug Control Policy Under the New Administration. The Domestic Policy Subcommittee of the House Committee on Oversight and Government Reform. May 19, 2009. Available: http://carnevaleassociates.com/Testimony%20of%20John%20Carnevale%20May%2019%20-%20FINAL.pdf [accessed August 2010].
Caulkins, J., and R. Mennefee. (2009). Is objective risk all that matters when it comes to drugs? Journal of Drug Policy Analysis , 2 (1), Art. 1. Available: http://www.bepress.com/jdpa/vol2/iss1/art1/ [accessed August 2010].
District of Columbia Pretrial Services Agency. (2009). PSA’s Electronic Reading Room—FOIA. Available: http://www.dcpsa.gov/foia/foiaERRpsa.htm [accessed May 2009].
European Monitoring Center for Drugs and Drug Addiction. (2007). 2007 Annual Report: The State of the Drug Problem in Europe. Lisbon, Portugal. Available: http://www.emcdda.europa.eu/publications/annual-report/2007 [accessed May 2009].
Fergusson, D.M., J.M. Boden, and L.J. Horwood. (2006). Cannabis use and other illicit drug use: Testing the cannabis gateway hypothesis. Addiction, 6 (101), 556-569.
Gallup Poll. (2009). Illegal Drugs . Available: http://www.gallup.com/poll/1657/illegal-drugs.aspx [accessed April 2010].
Golub, A., and B. Johnson. (2001). Variation in youthful risks of progression from alcohol and tobacco to marijuana and to hard drugs across generations. American Journal of Public Health, 91 (2), 225-232.
Iversen, L. (2005). Long-term effects of exposure to cannabis. Current Opinion in Pharmacology, 5 (1), 69-72. Available: http://www.safeaccessnow.org/downloads/long%20term%20cannabis%20effects.pdf [accessed July 2010].
National Institute of Justice. (2003). Preliminary Data on Drug Use & Related Matters Among Adult Arrestees & Juvenile Detainees 2002 . Washington, DC: U.S. Department of Justice.
National Institute on Drug Abuse. (2010). NIDA InfoFacts: Heroin . Available: http://www.drugabuse.gov/infofacts/heroin.html [accessed August 2010].
National Research Council. (2001). Informing America’s Policy on Illegal Drugs: What We Don’t Know Keeps Hurting Us. Committee on Data and Research for Policy on Illegal Drugs, C.F. Manski, J.V. Pepper, and C.V. Petrie (Eds.). Committee on Law and Justice and Committee on National Statistics. Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press.
Office of National Drug Control Policy. (1993). State and Local Spending on Drug Control Activities . NCJ publication no. 146138. Washington, DC: Executive Office of the President.
Office of National Drug Control Policy. (2001). What America’s Users Spend on Illegal Drugs 1988–2000 . W. Rhodes, M. Layne, A.-M. Bruen, P. Johnston, and L. Bechetti. Washington, DC: Executive Office of the President.
Pollack, H., P. Reuter., and P. Sevigny. (2010). If Drug Treatment Works So Well, Why Are So Many Drug Users in Prison? Paper presented at the meeting of the National Bureau of Economic Research on Making Crime Control Pay: Cost-Effective Alternatives to Incarceration, July, Berkeley, CA. Available: http://www.nber.org/chapters/c12098.pdf [accessed August 2010].
Trunzo, D., and L. Henderson. (2007). Older Adult Admissions to Substance Abuse Treatment: Findings from the Treatment Episode Data Set . Paper presented at the meeting of the American Public Health Association, November 6, Washington, DC. Available: http://apha.confex.com/apha/135am/techprogram/paper_160959.htm [accessed August 2010].
Walsh, J. (2009). Lowering Expectations: Supply Control and the Resilient Cocaine Market. Available: http://www.eluniversal.com.mx/graficos/pdf09/wolareportcocaine.pdf [accessed August 2010].
Wills, T., C. Walker, and J. Resko. (2005). Longitudinal studies of drug use and abuse. In Z. Slobada (Ed.), Epidemiology of Drug Abuse (pp. 177-192). New York: Springer.
This page intentionally left blank.
Despite efforts to reduce drug consumption in the United States over the past 35 years, drugs are just as cheap and available as they have ever been. Cocaine, heroin, and methamphetamines continue to cause great harm in the country, particularly in minority communities in the major cities. Marijuana use remains a part of adolescent development for about half of the country's young people, although there is controversy about the extent of its harm.
Given the persistence of drug demand in the face of lengthy and expensive efforts to control the markets, the National Institute of Justice asked the National Research Council to undertake a study of current research on the demand for drugs in order to help better focus national efforts to reduce that demand.
This study complements the 2003 book, Informing America's Policy on Illegal Drugs by giving more attention to the sources of demand and assessing the potential of demand-side interventions to make a substantial difference to the nation's drug problems. Understanding the Demand for Illegal Drugs therefore focuses tightly on demand models in the field of economics and evaluates the data needs for advancing this relatively undeveloped area of investigation.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Open access
- Published: 13 November 2021
Risk and protective factors of drug abuse among adolescents: a systematic review
- Azmawati Mohammed Nawi 1 ,
- Rozmi Ismail 2 ,
- Fauziah Ibrahim 2 ,
- Mohd Rohaizat Hassan 1 ,
- Mohd Rizal Abdul Manaf 1 ,
- Noh Amit 3 ,
- Norhayati Ibrahim 3 &
- Nurul Shafini Shafurdin 2
BMC Public Health volume 21 , Article number: 2088 ( 2021 ) Cite this article
149k Accesses
118 Citations
20 Altmetric
Metrics details
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was adopted for the review which utilized three main journal databases, namely PubMed, EBSCOhost, and Web of Science. Tobacco addiction and alcohol abuse were excluded in this review. Retrieved citations were screened, and the data were extracted based on strict inclusion and exclusion criteria. Inclusion criteria include the article being full text, published from the year 2016 until 2020 and provided via open access resource or subscribed to by the institution. Quality assessment was done using Mixed Methods Appraisal Tools (MMAT) version 2018 to assess the methodological quality of the included studies. Given the heterogeneity of the included studies, a descriptive synthesis of the included studies was undertaken.
Out of 425 articles identified, 22 quantitative articles and one qualitative article were included in the final review. Both the risk and protective factors obtained were categorized into three main domains: individual, family, and community factors. The individual risk factors identified were traits of high impulsivity; rebelliousness; emotional regulation impairment, low religious, pain catastrophic, homework completeness, total screen time and alexithymia; the experience of maltreatment or a negative upbringing; having psychiatric disorders such as conduct problems and major depressive disorder; previous e-cigarette exposure; behavioral addiction; low-perceived risk; high-perceived drug accessibility; and high-attitude to use synthetic drugs. The familial risk factors were prenatal maternal smoking; poor maternal psychological control; low parental education; negligence; poor supervision; uncontrolled pocket money; and the presence of substance-using family members. One community risk factor reported was having peers who abuse drugs. The protective factors determined were individual traits of optimism; a high level of mindfulness; having social phobia; having strong beliefs against substance abuse; the desire to maintain one’s health; high paternal awareness of drug abuse; school connectedness; structured activity and having strong religious beliefs.
The outcomes of this review suggest a complex interaction between a multitude of factors influencing adolescent drug abuse. Therefore, successful adolescent drug abuse prevention programs will require extensive work at all levels of domains.
Peer Review reports
Introduction
Drug abuse is a global problem; 5.6% of the global population aged 15–64 years used drugs at least once during 2016 [ 1 ]. The usage of drugs among younger people has been shown to be higher than that among older people for most drugs. Drug abuse is also on the rise in many ASEAN (Association of Southeast Asian Nations) countries, especially among young males between 15 and 30 years of age. The increased burden due to drug abuse among adolescents and young adults was shown by the Global Burden of Disease (GBD) study in 2013 [ 2 ]. About 14% of the total health burden in young men is caused by alcohol and drug abuse. Younger people are also more likely to die from substance use disorders [ 3 ], and cannabis is the drug of choice among such users [ 4 ].
Adolescents are the group of people most prone to addiction [ 5 ]. The critical age of initiation of drug use begins during the adolescent period, and the maximum usage of drugs occurs among young people aged 18–25 years old [ 1 ]. During this period, adolescents have a strong inclination toward experimentation, curiosity, susceptibility to peer pressure, rebellion against authority, and poor self-worth, which makes such individuals vulnerable to drug abuse [ 2 ]. During adolescence, the basic development process generally involves changing relations between the individual and the multiple levels of the context within which the young person is accustomed. Variation in the substance and timing of these relations promotes diversity in adolescence and represents sources of risk or protective factors across this life period [ 6 ]. All these factors are crucial to helping young people develop their full potential and attain the best health in the transition to adulthood. Abusing drugs impairs the successful transition to adulthood by impairing the development of critical thinking and the learning of crucial cognitive skills [ 7 ]. Adolescents who abuse drugs are also reported to have higher rates of physical and mental illness and reduced overall health and well-being [ 8 ].
The absence of protective factors and the presence of risk factors predispose adolescents to drug abuse. Some of the risk factors are the presence of early mental and behavioral health problems, peer pressure, poorly equipped schools, poverty, poor parental supervision and relationships, a poor family structure, a lack of opportunities, isolation, gender, and accessibility to drugs [ 9 ]. The protective factors include high self-esteem, religiosity, grit, peer factors, self-control, parental monitoring, academic competence, anti-drug use policies, and strong neighborhood attachment [ 10 , 11 , 12 , 13 , 14 , 15 ].
The majority of previous systematic reviews done worldwide on drug usage focused on the mental, psychological, or social consequences of substance abuse [ 16 , 17 , 18 ], while some focused only on risk and protective factors for the non-medical use of prescription drugs among youths [ 19 ]. A few studies focused only on the risk factors of single drug usage among adolescents [ 20 ]. Therefore, the development of the current systematic review is based on the main research question: What is the current risk and protective factors among adolescent on the involvement with drug abuse? To the best of our knowledge, there is limited evidence from systematic reviews that explores the risk and protective factors among the adolescent population involved in drug abuse. Especially among developing countries, such as those in South East Asia, such research on the risk and protective factors for drug abuse is scarce. Furthermore, this review will shed light on the recent trends of risk and protective factors and provide insight into the main focus factors for prevention and control activities program. Additionally, this review will provide information on how these risk and protective factors change throughout various developmental stages. Therefore, the objective of this systematic review was to determine the risk and protective factors of drug abuse among adolescents worldwide. This paper thus fills in the gaps of previous studies and adds to the existing body of knowledge. In addition, this review may benefit certain parties in developing countries like Malaysia, where the national response to drugs is developing in terms of harm reduction, prison sentences, drug treatments, law enforcement responses, and civil society participation.
This systematic review was conducted using three databases, PubMed, EBSCOhost, and Web of Science, considering the easy access and wide coverage of reliable journals, focusing on the risk and protective factors of drug abuse among adolescents from 2016 until December 2020. The search was limited to the last 5 years to focus only on the most recent findings related to risk and protective factors. The search strategy employed was performed in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) checklist.
A preliminary search was conducted to identify appropriate keywords and determine whether this review was feasible. Subsequently, the related keywords were searched using online thesauruses, online dictionaries, and online encyclopedias. These keywords were verified and validated by an academic professor at the National University of Malaysia. The keywords used as shown in Table 1 .
Selection criteria
The systematic review process for searching the articles was carried out via the steps shown in Fig. 1 . Firstly, screening was done to remove duplicate articles from the selected search engines. A total of 240 articles were removed in this stage. Titles and abstracts were screened based on the relevancy of the titles to the inclusion and exclusion criteria and the objectives. The inclusion criteria were full text original articles, open access articles or articles subscribed to by the institution, observation and intervention study design and English language articles. The exclusion criteria in this search were (a) case study articles, (b) systematic and narrative review paper articles, (c) non-adolescent-based analyses, (d) non-English articles, and (e) articles focusing on smoking (nicotine) and alcohol-related issues only. A total of 130 articles were excluded after title and abstract screening, leaving 55 articles to be assessed for eligibility. The full text of each article was obtained, and each full article was checked thoroughly to determine if it would fulfil the inclusion criteria and objectives of this study. Each of the authors compared their list of potentially relevant articles and discussed their selections until a final agreement was obtained. A total of 22 articles were accepted to be included in this review. Most of the excluded articles were excluded because the population was not of the target age range—i.e., featuring subjects with an age > 18 years, a cohort born in 1965–1975, or undergraduate college students; the subject matter was not related to the study objective—i.e., assessing the effects on premature mortality, violent behavior, psychiatric illness, individual traits, and personality; type of article such as narrative review and neuropsychiatry review; and because of our inability to obtain the full article—e.g., forthcoming work in 2021. One qualitative article was added to explain the domain related to risk and the protective factors among the adolescents.
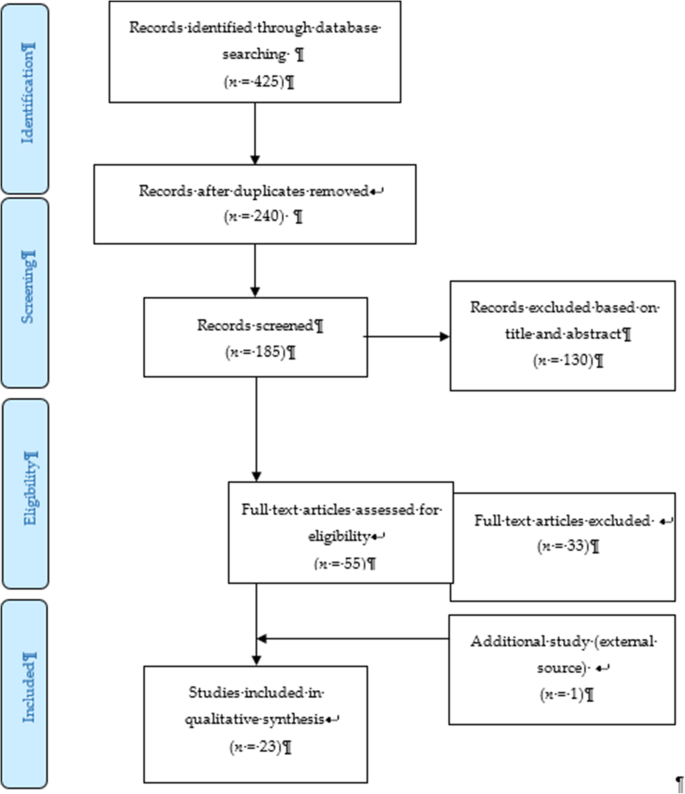
PRISMA flow diagram showing the selection of studies on risk and protective factors for drug abuse among adolescents.2.2. Operational Definition
Drug-related substances in this context refer to narcotics, opioids, psychoactive substances, amphetamines, cannabis, ecstasy, heroin, cocaine, hallucinogens, depressants, and stimulants. Drugs of abuse can be either off-label drugs or drugs that are medically prescribed. The two most commonly abused substances not included in this review are nicotine (tobacco) and alcohol. Accordingly, e-cigarettes and nicotine vape were also not included. Further, “adolescence” in this study refers to members of the population aged between 10 to 18 years [ 21 ].
Data extraction tool
All researchers independently extracted information for each article into an Excel spreadsheet. The data were then customized based on their (a) number; (b) year; (c) author and country; (d) titles; (e) study design; (f) type of substance abuse; (g) results—risks and protective factors; and (h) conclusions. A second reviewer crossed-checked the articles assigned to them and provided comments in the table.
Quality assessment tool
By using the Mixed Method Assessment Tool (MMAT version 2018), all articles were critically appraised for their quality by two independent reviewers. This tool has been shown to be useful in systematic reviews encompassing different study designs [ 22 ]. Articles were only selected if both reviewers agreed upon the articles’ quality. Any disagreement between the assigned reviewers was managed by employing a third independent reviewer. All included studies received a rating of “yes” for the questions in the respective domains of the MMAT checklists. Therefore, none of the articles were removed from this review due to poor quality. The Cohen’s kappa (agreement) between the two reviewers was 0.77, indicating moderate agreement [ 23 ].
The initial search found 425 studies for review, but after removing duplicates and applying the criteria listed above, we narrowed the pool to 22 articles, all of which are quantitative in their study design. The studies include three prospective cohort studies [ 24 , 25 , 26 ], one community trial [ 27 ], one case-control study [ 28 ], and nine cross-sectional studies [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. After careful discussion, all reviewer panels agreed to add one qualitative study [ 46 ] to help provide reasoning for the quantitative results. The selected qualitative paper was chosen because it discussed almost all domains on the risk and protective factors found in this review.
A summary of all 23 articles is listed in Table 2 . A majority of the studies (13 articles) were from the United States of America (USA) [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], three studies were from the Asia region [ 32 , 33 , 38 ], four studies were from Europe [ 24 , 28 , 40 , 44 ], and one study was from Latin America [ 35 ], Africa [ 43 ] and Mediterranean [ 45 ]. The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. There were a wide range of drugs assessed in the quantitative articles, with marijuana being mentioned in 11 studies, cannabis in five studies, and opioid (six studies). There was also large heterogeneity in terms of the study design, type of drug abused, measurements of outcomes, and analysis techniques used. Therefore, the data were presented descriptively.
After thorough discussion and evaluation, all the findings (both risk and protective factors) from the review were categorized into three main domains: individual factors, family factors, and community factors. The conceptual framework is summarized in Fig. 2 .
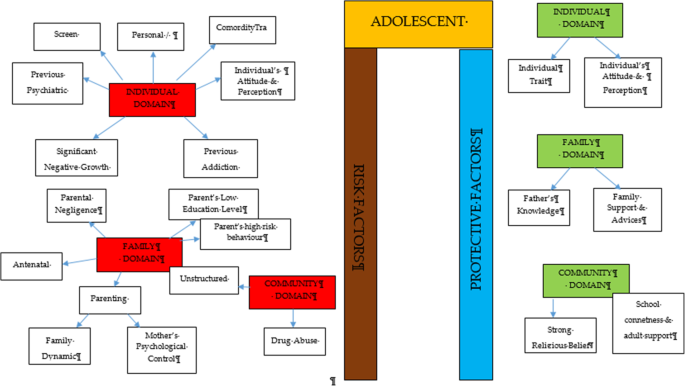
Conceptual framework of risk and protective factors related to adolescent drug abuse
DOMAIN: individual factor
Risk factors.
Almost all the articles highlighted significant findings of individual risk factors for adolescent drug abuse. Therefore, our findings for this domain were further broken down into five more sub-domains consisting of personal/individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance history, comorbidity and an individual’s attitude and perception.
Personal/individual traits
Chuang et al. [ 29 ] found that adolescents with high impulsivity traits had a significant positive association with drug addiction. This study also showed that the impulsivity trait alone was an independent risk factor that increased the odds between two to four times for using any drug compared to the non-impulsive group. Another longitudinal study by Guttmannova et al. showed that rebellious traits are positively associated with marijuana drug abuse [ 27 ]. The authors argued that measures of rebelliousness are a good proxy for a youth’s propensity to engage in risky behavior. Nevertheless, Wilson et al. [ 37 ], in a study involving 112 youths undergoing detoxification treatment for opioid abuse, found that a majority of the affected respondents had difficulty in regulating their emotions. The authors found that those with emotional regulation impairment traits became opioid dependent at an earlier age. Apart from that, a case-control study among outpatient youths found that adolescents involved in cannabis abuse had significant alexithymia traits compared to the control population [ 28 ]. Those adolescents scored high in the dimension of Difficulty in Identifying Emotion (DIF), which is one of the key definitions of diagnosing alexithymia. Overall, the adjusted Odds Ratio for DIF in cannabis abuse was 1.11 (95% CI, 1.03–1.20).
Significant negative growth exposure
A history of maltreatment in the past was also shown to have a positive association with adolescent drug abuse. A study found that a history of physical abuse in the past is associated with adolescent drug abuse through a Path Analysis, despite evidence being limited to the female gender [ 25 ]. However, evidence from another study focusing at foster care concluded that any type of maltreatment might result in a prevalence as high as 85.7% for the lifetime use of cannabis and as high as 31.7% for the prevalence of cannabis use within the last 3-months [ 30 ]. The study also found significant latent variables that accounted for drug abuse outcomes, which were chronic physical maltreatment (factor loading of 0.858) and chronic psychological maltreatment (factor loading of 0.825), with an r 2 of 73.6 and 68.1%, respectively. Another study shed light on those living in child welfare service (CWS) [ 35 ]. It was observed through longitudinal measurements that proportions of marijuana usage increased from 9 to 18% after 36 months in CWS. Hence, there is evidence of the possibility of a negative upbringing at such shelters.
Personal psychiatric diagnosis
The robust studies conducted in the USA have deduced that adolescents diagnosed with a conduct problem (CP) have a positive association with marijuana abuse (OR = 1.75 [1.56, 1.96], p < 0.0001). Furthermore, those with a diagnosis of Major Depressive Disorder (MDD) showed a significant positive association with marijuana abuse.
Previous substance and addiction history
Another study found that exposure to e-cigarettes within the past 30 days is related to an increase in the prevalence of marijuana use and prescription drug use by at least four times in the 8th and 10th grades and by at least three times in the 12th grade [ 34 ]. An association between other behavioral addictions and the development of drug abuse was also studied [ 29 ]. Using a 12-item index to assess potential addictive behaviors [ 39 ], significant associations between drug abuse and the groups with two behavioral addictions (OR = 3.19, 95% CI 1.25,9.77) and three behavioral addictions (OR = 3.46, 95% CI 1.25,9.58) were reported.
Comorbidity
The paper by Dash et al. (2020) highlight adolescent with a disease who needs routine medical pain treatment have higher risk of opioid misuse [ 38 ]. The adolescents who have disorder symptoms may have a risk for opioid misuse despite for the pain intensity.
Individual’s attitudes and perceptions
In a study conducted in three Latin America countries (Argentina, Chile, and Uruguay), it was shown that adolescents with low or no perceived risk of taking marijuana had a higher risk of abuse (OR = 8.22 times, 95% CI 7.56, 10.30) [ 35 ]. This finding is in line with another study that investigated 2002 adolescents and concluded that perceiving the drug as harmless was an independent risk factor that could prospectively predict future marijuana abuse [ 27 ]. Moreover, some youth interviewed perceived that they gained benefits from substance use [ 38 ]. The focus group discussion summarized that the youth felt positive personal motivation and could escape from a negative state by taking drugs. Apart from that, adolescents who had high-perceived availability of drugs in their neighborhoods were more likely to increase their usage of marijuana over time (OR = 11.00, 95% CI 9.11, 13.27) [ 35 ]. A cheap price of the substance and the availability of drug dealers around schools were factors for youth accessibility [ 38 ]. Perceived drug accessibility has also been linked with the authorities’ enforcement programs. The youth perception of a lax community enforcement of laws regarding drug use at all-time points predicted an increase in marijuana use in the subsequent assessment period [ 27 ]. Besides perception, a study examining the attitudes towards synthetic drugs based on 8076 probabilistic samples of Macau students found that the odds of the lifetime use of marijuana was almost three times higher among those with a strong attitude towards the use of synthetic drugs [ 32 ]. In addition, total screen time among the adolescent increase the likelihood of frequent cannabis use. Those who reported daily cannabis use have a mean of 12.56 h of total screen time, compared to a mean of 6.93 h among those who reported no cannabis use. Adolescent with more time on internet use, messaging, playing video games and watching TV/movies were significantly associated with more frequent cannabis use [ 44 ].
Protective factors
Individual traits.
Some individual traits have been determined to protect adolescents from developing drug abuse habits. A study by Marin et al. found that youth with an optimistic trait were less likely to become drug dependent [ 33 ]. In this study involving 1104 Iranian students, it was concluded that a higher optimism score (measured using the Children Attributional Style Questionnaire, CASQ) was a protective factor against illicit drug use (OR = 0.90, 95% CI: 0.85–0.95). Another study found that high levels of mindfulness, measured using the 25-item Child Acceptance and Mindfulness Measure, CAMM, lead to a slower progression toward injectable drug abuse among youth with opioid addiction (1.67 years, p = .041) [ 37 ]. In addition, the social phobia trait was found to have a negative association with marijuana use (OR = 0.87, 95% CI 0.77–0.97), as suggested [ 31 ].
According to El Kazdouh et al., individuals with a strong belief against substance use and those with a strong desire to maintain their health were more likely to be protected from involvement in drug abuse [ 46 ].
DOMAIN: family factors
The biological factors underlying drug abuse in adolescents have been reported in several studies. Epigenetic studies are considered important, as they can provide a good outline of the potential pre-natal factors that can be targeted at an earlier stage. Expecting mothers who smoke tobacco and alcohol have an indirect link with adolescent substance abuse in later life [ 24 , 39 ]. Moreover, the dynamic relationship between parents and their children may have some profound effects on the child’s growth. Luk et al. examined the mediator effects between parenting style and substance abuse and found the maternal psychological control dimension to be a significant variable [ 26 ]. The mother’s psychological control was two times higher in influencing her children to be involved in substance abuse compared to the other dimension. Conversely, an indirect risk factor towards youth drug abuse was elaborated in a study in which low parental educational level predicted a greater risk of future drug abuse by reducing the youth’s perception of harm [ 27 , 43 ]. Negligence from a parental perspective could also contribute to this problem. According to El Kazdouh et al. [ 46 ], a lack of parental supervision, uncontrolled pocket money spending among children, and the presence of substance-using family members were the most common negligence factors.
While the maternal factors above were shown to be risk factors, the opposite effect was seen when the paternal figure equipped himself with sufficient knowledge. A study found that fathers with good information and awareness were more likely to protect their adolescent children from drug abuse [ 26 ]. El Kazdouh et al. noted that support and advice could be some of the protective factors in this area [ 46 ].
DOMAIN: community factors
- Risk factor
A study in 2017 showed a positive association between adolescent drug abuse and peers who abuse drugs [ 32 , 39 ]. It was estimated that the odds of becoming a lifetime marijuana user was significantly increased by a factor of 2.5 ( p < 0.001) among peer groups who were taking synthetic drugs. This factor served as peer pressure for youth, who subconsciously had desire to be like the others [ 38 ]. The impact of availability and engagement in structured and unstructured activities also play a role in marijuana use. The findings from Spillane (2000) found that the availability of unstructured activities was associated with increased likelihood of marijuana use [ 42 ].
- Protective factor
Strong religious beliefs integrated into society serve as a crucial protective factor that can prevent adolescents from engaging in drug abuse [ 38 , 45 ]. In addition, the school connectedness and adult support also play a major contribution in the drug use [ 40 ].
The goal of this review was to identify and classify the risks and protective factors that lead adolescents to drug abuse across the three important domains of the individual, family, and community. No findings conflicted with each other, as each of them had their own arguments and justifications. The findings from our review showed that individual factors were the most commonly highlighted. These factors include individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance and addiction history, and an individual’s attitude and perception as risk factors.
Within the individual factor domain, nine articles were found to contribute to the subdomain of personal/ individual traits [ 27 , 28 , 29 , 37 , 38 , 39 , 40 , 43 , 44 ]. Despite the heterogeneity of the study designs and the substances under investigation, all of the papers found statistically significant results for the possible risk factors of adolescent drug abuse. The traits of high impulsivity, rebelliousness, difficulty in regulating emotions, and alexithymia can be considered negative characteristic traits. These adolescents suffer from the inability to self-regulate their emotions, so they tend to externalize their behaviors as a way to avoid or suppress the negative feelings that they are experiencing [ 41 , 47 , 48 ]. On the other hand, engaging in such behaviors could plausibly provide a greater sense of positive emotions and make them feel good [ 49 ]. Apart from that, evidence from a neurophysiological point of view also suggests that the compulsive drive toward drug use is complemented by deficits in impulse control and decision making (impulsive trait) [ 50 ]. A person’s ability in self-control will seriously impaired with continuous drug use and will lead to the hallmark of addiction [ 51 ].
On the other hand, there are articles that reported some individual traits to be protective for adolescents from engaging in drug abuse. Youth with the optimistic trait, a high level of mindfulness, and social phobia were less likely to become drug dependent [ 31 , 33 , 37 ]. All of these articles used different psychometric instruments to classify each individual trait and were mutually exclusive. Therefore, each trait measured the chance of engaging in drug abuse on its own and did not reflect the chance at the end of the spectrum. These findings show that individual traits can be either protective or risk factors for the drugs used among adolescents. Therefore, any adolescent with negative personality traits should be monitored closely by providing health education, motivation, counselling, and emotional support since it can be concluded that negative personality traits are correlated with high risk behaviours such as drug abuse [ 52 ].
Our study also found that a history of maltreatment has a positive association with adolescent drug abuse. Those adolescents with episodes of maltreatment were considered to have negative growth exposure, as their childhoods were negatively affected by traumatic events. Some significant associations were found between maltreatment and adolescent drug abuse, although the former factor was limited to the female gender [ 25 , 30 , 36 ]. One possible reason for the contrasting results between genders is the different sample populations, which only covered child welfare centers [ 36 ] and foster care [ 30 ]. Regardless of the place, maltreatment can happen anywhere depending on the presence of the perpetrators. To date, evidence that concretely links maltreatment and substance abuse remains limited. However, a plausible explanation for this link could be the indirect effects of posttraumatic stress (i.e., a history of maltreatment) leading to substance use [ 53 , 54 ]. These findings highlight the importance of continuous monitoring and follow-ups with adolescents who have a history of maltreatment and who have ever attended a welfare center.
Addiction sometimes leads to another addiction, as described by the findings of several studies [ 29 , 34 ]. An initial study focused on the effects of e-cigarettes in the development of other substance abuse disorders, particularly those related to marijuana, alcohol, and commonly prescribed medications [ 34 ]. The authors found that the use of e-cigarettes can lead to more severe substance addiction [ 55 ], possibly through normalization of the behavior. On the other hand, Chuang et al.’s extensive study in 2017 analyzed the combined effects of either multiple addictions alone or a combination of multiple addictions together with the impulsivity trait [ 29 ]. The outcomes reported were intriguing and provide the opportunity for targeted intervention. The synergistic effects of impulsiveness and three other substance addictions (marijuana, tobacco, and alcohol) substantially increased the likelihood for drug abuse from 3.46 (95%CI 1.25, 9.58) to 10.13 (95% CI 3.95, 25.95). Therefore, proper rehabilitation is an important strategy to ensure that one addiction will not lead to another addiction.
The likelihood for drug abuse increases as the population perceives little or no harmful risks associated with the drugs. On the opposite side of the coin, a greater perceived risk remains a protective factor for marijuana abuse [ 56 ]. However, another study noted that a stronger determinant for adolescent drug abuse was the perceived availability of the drug [ 35 , 57 ]. Looking at the bigger picture, both perceptions corroborate each other and may inform drug use. Another study, on the other hand, reported that there was a decreasing trend of perceived drug risk in conjunction with the increasing usage of drugs [ 58 ]. As more people do drugs, youth may inevitably perceive those drugs as an acceptable norm without any harmful consequences [ 59 ].
In addition, the total spent for screen time also contribute to drug abuse among adolescent [ 43 ]. This scenario has been proven by many researchers on the effect of screen time on the mental health [ 60 ] that leads to the substance use among the adolescent due to the ubiquity of pro-substance use content on the internet. Adolescent with comorbidity who needs medical pain management by opioids also tend to misuse in future. A qualitative exploration on the perspectives among general practitioners concerning the risk of opioid misuse in people with pain, showed pain management by opioids is a default treatment and misuse is not a main problem for the them [ 61 ]. A careful decision on the use of opioids as a pain management should be consider among the adolescents and their understanding is needed.
Within the family factor domain, family structures were found to have both positive and negative associations with drug abuse among adolescents. As described in one study, paternal knowledge was consistently found to be a protective factor against substance abuse [ 26 ]. With sufficient knowledge, the father can serve as the guardian of his family to monitor and protect his children from negative influences [ 62 ]. The work by Luk et al. also reported a positive association of maternal psychological association towards drug abuse (IRR 2.41, p < 0.05) [ 26 ]. The authors also observed the same effect of paternal psychological control, although it was statistically insignificant. This construct relates to parenting style, and the authors argued that parenting style might have a profound effect on the outcomes under study. While an earlier literature review [ 63 ] also reported such a relationship, a recent study showed a lesser impact [ 64 ] with regards to neglectful parenting styles leading to poorer substance abuse outcomes. Nevertheless, it was highlighted in another study that the adolescents’ perception of a neglectful parenting style increased their odds (OR 2.14, p = 0.012) of developing alcohol abuse, not the parenting style itself [ 65 ]. Altogether, families play vital roles in adolescents’ risk for engaging in substance abuse [ 66 ]. Therefore, any intervention to impede the initiation of substance use or curb existing substance use among adolescents needs to include parents—especially improving parent–child communication and ensuring that parents monitor their children’s activities.
Finally, the community also contributes to drug abuse among adolescents. As shown by Li et al. [ 32 ] and El Kazdouh et al. [ 46 ], peers exert a certain influence on other teenagers by making them subconsciously want to fit into the group. Peer selection and peer socialization processes might explain why peer pressure serves as a risk factor for drug-abuse among adolescents [ 67 ]. Another study reported that strong religious beliefs integrated into society play a crucial role in preventing adolescents from engaging in drug abuse [ 46 ]. Most religions devalue any actions that can cause harmful health effects, such as substance abuse [ 68 ]. Hence, spiritual beliefs may help protect adolescents. This theme has been well established in many studies [ 60 , 69 , 70 , 71 , 72 ] and, therefore, could be implemented by religious societies as part of interventions to curb the issue of adolescent drug abuse. The connection with school and structured activity did reduce the risk as a study in USA found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity and social activity [ 73 ]. The school activity should highlight on the importance of developmental perspective when designing and offering school-based prevention programs [75].
Limitations
We adopted a review approach that synthesized existing evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in different settings, there are some potential limitations to this work. We may have missed some other important factors, as we only included English articles, and article extraction was only done from the three search engines mentioned. Nonetheless, this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and cigarettes, thereby making this paper more focused.
Conclusions
This review has addressed some recent knowledge related to the individual, familial, and community risk and preventive factors for adolescent drug use. We suggest that more attention should be given to individual factors since most findings were discussed in relation to such factors. With the increasing trend of drug abuse, it will be critical to focus research specifically on this area. Localized studies, especially those related to demographic factors, may be more effective in generating results that are specific to particular areas and thus may be more useful in generating and assessing local control and prevention efforts. Interventions using different theory-based psychotherapies and a recognition of the unique developmental milestones specific to adolescents are among examples that can be used. Relevant holistic approaches should be strengthened not only by relevant government agencies but also by the private sector and non-governmental organizations by promoting protective factors while reducing risk factors in programs involving adolescents from primary school up to adulthood to prevent and control drug abuse. Finally, legal legislation and enforcement against drug abuse should be engaged with regularly as part of our commitment to combat this public health burden.
Data availability and materials
All data generated or analysed during this study are included in this published article.
Nation, U. World Drug Report 2018 (United Nations publication, Sales No. E.18X.XI.9. United Nation publication). 2018. Retrieved from https://www.unodc.org/wdr2018
Google Scholar
Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–64. https://doi.org/10.1016/S2215-0366(15)00508-8 Elsevier Ltd.
Article PubMed Google Scholar
Ritchie H, Roser M. Drug Use - Our World in Data: Global Change Data Lab; 2019. https://ourworldindata.org/drug-use [10 June 2020]
Holm S, Sandberg S, Kolind T, Hesse M. The importance of cannabis culture in young adult cannabis use. J Subst Abus. 2014;19(3):251–6.
Luikinga SJ, Kim JH, Perry CJ. Developmental perspectives on methamphetamine abuse: exploring adolescent vulnerabilities on brain and behavior. Progress Neuro Psychopharmacol Biol Psychiatry. 2018;87(Pt A):78–84. https://doi.org/10.1016/j.pnpbp.2017.11.010 Elsevier Inc.
Article CAS Google Scholar
Ismail R, Ghazalli MN, Ibrahim N. Not all developmental assets can predict negative mental health outcomes of disadvantaged youth: a case of suburban Kuala Lumpur. Mediterr J Soc Sci. 2015;6(1):452–9. https://doi.org/10.5901/mjss.2015.v6n5s1p452 .
Article Google Scholar
Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. https://doi.org/10.1016/j.pbb.2006.12.001 .
Article CAS PubMed Google Scholar
Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2). https://doi.org/10.1007/bf03391702 Technosdar Ltd.
Somani, S.; Meghani S. Substance Abuse among Youth: A Harsh Reality 2016. doi: https://doi.org/10.4172/2165-7548.1000330 , 6, 4.
Book Google Scholar
Drabble L, Trocki KF, Klinger JL. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: findings from the National Alcohol Survey. Drug Alcohol Depend. 2016;161:127–34. https://doi.org/10.1016/j.drugalcdep.2016.01.022 .
Article PubMed PubMed Central Google Scholar
Goliath V, Pretorius B. Peer risk and protective factors in adolescence: Implications for drug use prevention. Soc Work. 2016;52(1):113–29. https://doi.org/10.15270/52-1-482 .
Guerrero LR, Dudovitz R, Chung PJ, Dosanjh KK, Wong MD. Grit: a potential protective factor against substance use and other risk behaviors among Latino adolescents. Acad Pediatr. 2016;16(3):275–81. https://doi.org/10.1016/j.acap.2015.12.016 .
National Institutes on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse (NIDA); 2003. Retrieved from https://www.drugabuse.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
Nguyen NN, Newhill CE. The role of religiosity as a protective factor against marijuana use among African American, White, Asian, and Hispanic adolescents. J Subst Abus. 2016;21(5):547–52. https://doi.org/10.3109/14659891.2015.1093558 .
Schinke S, Schwinn T, Hopkins J, Wahlstrom L. Drug abuse risk and protective factors among Hispanic adolescents. Prev Med Rep. 2016;3:185–8. https://doi.org/10.1016/j.pmedr.2016.01.012 .
Macleod J, Oakes R, Copello A, Crome PI, Egger PM, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–88. https://doi.org/10.1016/S0140-6736(04)16200-4 .
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3 .
Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–94. https://doi.org/10.1177/0269881105049040 .
Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the united states: A social ecological perspective. J Stud Alcohol Drugs. 2015;76(1):5–20. https://doi.org/10.15288/jsad.2015.76.5 .
Guxensa M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007;21(3):252–60. https://doi.org/10.1157/13106811 .
Susan MS, Peter SA, Dakshitha W, George CP. The age of adolescence. Lancet Child Adolesc Health. 2018;2(Issue 3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1 .
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
McHugh ML. Interrater reliability: The kappa statistic. Biochem Med. 2012;22(3):276–82. https://doi.org/10.11613/bm.2012.031 .
Cecil CAM, Walton E, Smith RG, Viding E, McCrory EJ, Relton CL, et al. DNA methylation and substance-use risk: a prospective, genome-wide study spanning gestation to adolescence. Transl Psychiatry. 2016;6(12):e976. https://doi.org/10.1038/tp.2016.247 Nature Publishing Group.
Article CAS PubMed PubMed Central Google Scholar
Kobulsky JM. Gender differences in pathways from physical and sexual abuse to early substance use. Child Youth Serv Rev. 2017;83:25–32. https://doi.org/10.1016/j.childyouth.2017.10.027 .
Luk JW, King KM, McCarty CA, McCauley E, Stoep A. Prospective effects of parenting on substance use and problems across Asian/Pacific islander and European American youth: Tests of moderated mediation. J Stud Alcohol Drugs. 2017;78(4):521–30. https://doi.org/10.15288/jsad.2017.78.521 .
Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, Hawkins JD. The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prev Sci. 2019;20(2):235–45. https://doi.org/10.1007/s11121-018-0882-9 .
Dorard G, Bungener C, Phan O, Edel Y, Corcos M, Berthoz S. Is alexithymia related to cannabis use disorder? Results from a case-control study in outpatient adolescent cannabis abusers. J Psychosom Res. 2017;95:74–80. https://doi.org/10.1016/j.jpsychores.2017.02.012 .
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74:41–7. https://doi.org/10.1016/j.addbeh.2017.05.021 .
Gabrielli J, Jackson Y, Brown S. Associations between maltreatment history and severity of substance use behavior in youth in Foster Care. Child Maltreat. 2016;21(4):298–307. https://doi.org/10.1177/1077559516669443 .
Khoddam R, Jackson NJ, Leventhal AM. Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 2016;169:48–55. https://doi.org/10.1016/j.drugalcdep.2016.10.007 .
Li SD, Zhang X, Tang W, Xia Y. Predictors and implications of synthetic drug use among adolescents in the gambling Capital of China. SAGE Open. 2017;7(4):215824401773303. https://doi.org/10.1177/2158244017733031 .
Marin S, Heshmatian E, Nadrian H, Fakhari A, Mohammadpoorasl A. Associations between optimism, tobacco smoking and substance abuse among Iranian high school students. Health Promot Perspect. 2019;9(4):279–84. https://doi.org/10.15171/hpp.2019.38 .
Miech RA, O’Malley PM, Johnston LD, Patrick ME. E-cigarettes and the drug use patterns of adolescents. Nicotine Tob Res. 2015;18(5):654–9. https://doi.org/10.1093/ntr/ntv217 .
Schleimer JP, Rivera-Aguirre AE, Castillo-Carniglia A, Laqueur HS, Rudolph KE, Suárez H, et al. Investigating how perceived risk and availability of marijuana relate to marijuana use among adolescents in Argentina, Chile, and Uruguay over time. Drug Alcohol Depend. 2019;201:115–26. https://doi.org/10.1016/j.drugalcdep.2019.03.029 .
Traube DE, Yarnell LM, Schrager SM. Differences in polysubstance use among youth in the child welfare system: toward a better understanding of the highest-risk teens. Child Abuse Negl. 2016;52:146–57. https://doi.org/10.1016/j.chiabu.2015.11.020 .
Wilson JD, Vo H, Matson P, Adger H, Barnett G, Fishman M. Trait mindfulness and progression to injection use in youth with opioid addiction. Subst Use Misuse. 2017;52(11):1486–93. https://doi.org/10.1080/10826084.2017.1289225 .
Dash GF, Feldstein Ewing SW, Murphy C, Hudson KA, Wilson AC. Contextual risk among adolescents receiving opioid prescriptions for acute pain in pediatric ambulatory care settings. Addict Behav. 2020;104:106314. https://doi.org/10.1016/j.addbeh.2020.106314 Epub 2020 Jan 11. PMID: 31962289; PMCID: PMC7024039.
Osborne V, Serdarevic M, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Age of first use of prescription opioids and prescription opioid non-medical use among older adolescents. Substance Use Misuse. 2020;55(14):2420–7. https://doi.org/10.1080/10826084.2020.1823420 .
Zuckermann AME, Qian W, Battista K, Jiang Y, de Groh M, Leatherdale ST. Factors influencing the non-medical use of prescription opioids among youth: results from the COMPASS study. J Subst Abus. 2020;25(5):507–14. https://doi.org/10.1080/14659891.2020.1736669 .
De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. https://doi.org/10.1089/lgbt.2016.0132 .
Spillane NS, Schick MR, Kirk-Provencher KT, Hill DC, Wyatt J, Jackson KM. Structured and unstructured activities and alcohol and marijuana use in middle school: the role of availability and engagement. Substance Use Misuse. 2020;55(11):1765–73. https://doi.org/10.1080/10826084.2020.1762652 .
Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun state, Nigeria. Int J Adolesc Med Health. 2016;29(3). https://doi.org/10.1515/ijamh-2015-0096 .
Doggett A, Qian W, Godin K, De Groh M, Leatherdale ST. Examining the association between exposure to various screen time sedentary behaviours and cannabis use among youth in the COMPASS study. SSM Population Health. 2019;9:100487. https://doi.org/10.1016/j.ssmph.2019.100487 .
Afifi RA, El Asmar K, Bteddini D, Assi M, Yassin N, Bitar S, et al. Bullying victimization and use of substances in high school: does religiosity moderate the association? J Relig Health. 2020;59(1):334–50. https://doi.org/10.1007/s10943-019-00789-8 .
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Substance Abuse Treat Prevent Policy. 2018;13(1):–31. https://doi.org/10.1186/s13011-018-0169-y .
Sussman S, Lisha N, Griffiths M. Prevalence of the addictions: a problem of the majority or the minority? Eval Health Prof. 2011;34(1):3–56. https://doi.org/10.1177/0163278710380124 .
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. https://doi.org/10.1016/j.cpr.2009.11.004 .
Ricketts T, Macaskill A. Gambling as emotion management: developing a grounded theory of problem gambling. Addict Res Theory. 2003;11(6):383–400. https://doi.org/10.1080/1606635031000062074 .
Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cogn Ther Res. 2012;36(5):451–7. https://doi.org/10.1007/s10608-011-9384-9 .
National Institutes on Drug Abuse. Drugs, brains, and behavior the science of addiction national institute on drug abuse (nida). 2014. Retrieved from https://www.drugabuse.gov/sites/default/files/soa_2014.pdf
Hokm Abadi ME, Bakhti M, Nazemi M, Sedighi S, Mirzadeh Toroghi E. The relationship between personality traits and drug type among substance abuse. J Res Health. 2018;8(6):531–40.
Longman-Mills S, Haye W, Hamilton H, Brands B, Wright MGM, Cumsille F, et al. Psychological maltreatment and its relationship with substance abuse among university students in Kingston, Jamaica, vol. 24. Florianopolis: Texto Contexto Enferm; 2015. p. 63–8.
Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychol Trauma Theory Res Pract Policy. 2014;6(1):25–33. https://doi.org/10.1037/a0031920 .
Krishnan-Sarin S, Morean M, Kong G, et al. E-Cigarettes and “dripping” among high-school youth. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-3224 .
Adinoff B. Neurobiologic processes in drug reward and addiction. Harvard review of psychiatry. NIH Public Access. 2004;12(6):305–20. https://doi.org/10.1080/10673220490910844 .
Kandel D, Kandel E. The gateway hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica. 2014;104(2):130–7.
Dempsey RC, McAlaney J, Helmer SM, Pischke CR, Akvardar Y, Bewick BM, et al. Normative perceptions of Cannabis use among European University students: associations of perceived peer use and peer attitudes with personal use and attitudes. J Stud Alcohol Drugs. 2016;77(5):740–8.
Cioffredi L, Kamon J, Turner W. Effects of depression, anxiety and screen use on adolescent substance use. Prevent Med Rep. 2021;22:101362. https://doi.org/10.1016/j.pmedr.2021.101362 .
Luckett T, NewtonJohn T, Phillips J, et al. Risk of opioid misuse in people with cancer and pain and related clinical considerations:a qualitative study of the perspectives of Australian general practitioners. BMJ Open. 2020;10(2):e034363. https://doi.org/10.1136/bmjopen-2019-034363 .
Lipari RN. Trends in Adolescent Substance Use and Perception of Risk from Substance Use. The CBHSQ Report. Substance Abuse Mental Health Serv Admin. 2013; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27656743 .
Muchiri BW, dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Substance Abuse. 2018;13(1):24. https://doi.org/10.1186/s13011-018-0163-4 .
Becoña E, Martínez Ú, Calafat A, Juan M, Fernández-Hermida JR, Secades-Villa R. Parental styles and drug use: a review. In: Drugs: Education, Prevention and Policy: Taylor & Francis; 2012. https://doi.org/10.3109/09687637.2011.631060 .
Berge J, Sundel K, Ojehagen A, Hakansson A. Role of parenting styles in adolescent substance use: results from a Swedish longitudinal cohort study. BMJ Open. 2016;6(1):e008979. https://doi.org/10.1136/bmjopen-2015-008979 .
Opara I, Lardier DT, Reid RJ, Garcia-Reid P. “It all starts with the parents”: a qualitative study on protective factors for drug-use prevention among black and Hispanic girls. Affilia J Women Soc Work. 2019;34(2):199–218. https://doi.org/10.1177/0886109918822543 .
Martínez-Loredo V, Fernández-Artamendi S, Weidberg S, Pericot I, López-Núñez C, Fernández-Hermida J, et al. Parenting styles and alcohol use among adolescents: a longitudinal study. Eur J Invest Health Psychol Educ. 2016;6(1):27–36. https://doi.org/10.1989/ejihpe.v6i1.146 .
Baharudin MN, Mohamad M, Karim F. Drug-abuse inmates maqasid shariah quality of lifw: a conceotual paper. Hum Soc Sci Rev. 2020;8(3):1285–94. https://doi.org/10.18510/hssr.2020.83131 .
Henneberger AK, Mushonga DR, Preston AM. Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev. 2020;6(1):57–73. https://doi.org/10.1007/s40894-019-00130-0 Springer.
Gomes FC, de Andrade AG, Izbicki R, Almeida AM, de Oliveira LG. Religion as a protective factor against drug use among Brazilian university students: a national survey. Rev Bras Psiquiatr. 2013;35(1):29–37. https://doi.org/10.1016/j.rbp.2012.05.010 .
Kulis S, Hodge DR, Ayers SL, Brown EF, Marsiglia FF. Spirituality and religion: intertwined protective factors for substance use among urban American Indian youth. Am J Drug Alcohol Abuse. 2012;38(5):444–9. https://doi.org/10.3109/00952990.2012.670338 .
Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the national comorbidity survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–7. https://doi.org/10.1097/00004583-200009000-00020 .
Moon SS, Rao U. Social activity, school-related activity, and anti-substance use media messages on adolescent tobacco and alcohol use. J Hum Behav Soc Environ. 2011;21(5):475–89. https://doi.org/10.1080/10911359.2011.566456 .
Simone A. Onrust, Roy Otten, Jeroen Lammers, Filip smit, school-based programmes to reduce and prevent substance use in different age groups: what works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev. 2016;44:45–59. https://doi.org/10.1016/j.cpr.2015.11.002 .
Download references
Acknowledgements
The authors acknowledge The Ministry of Higher Education Malaysia and The Universiti Kebangsaan Malaysia, (UKM) for funding this study under the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). We also thank the team for their commitment and tireless efforts in ensuring that manuscript was well executed.
Financial support for this study was obtained from the Ministry of Higher Education, Malaysia through the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Community Health, Universiti Kebangsaan Malaysia, Cheras, 56000, Kuala Lumpur, Malaysia
Azmawati Mohammed Nawi, Mohd Rohaizat Hassan & Mohd Rizal Abdul Manaf
Centre for Research in Psychology and Human Well-Being (PSiTra), Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Rozmi Ismail, Fauziah Ibrahim & Nurul Shafini Shafurdin
Clinical Psychology and Behavioural Health Program, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Noh Amit & Norhayati Ibrahim
You can also search for this author in PubMed Google Scholar
Contributions
Manuscript concept, and drafting AMN and RI; model development, FI, NI and NA.; Editing manuscript MRH, MRAN, NSS,; Critical revision of manuscript for important intellectual content, all authors. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Rozmi Ismail .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Secretariat of Research Ethics, Universiti Kebangsaan Malaysia, Faculty of Medicine, Cheras, Kuala Lumpur (Reference no. UKMPPI/111/8/JEP-2020.174(2). Dated 27 Mac 2020.
Consent for publication
Not applicable.
Competing interests
The authors AMN, RI, FI, MRM, MRAM, NA, NI NSS declare that they have no conflict of interest relevant to this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nawi, A.M., Ismail, R., Ibrahim, F. et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 21 , 2088 (2021). https://doi.org/10.1186/s12889-021-11906-2
Download citation
Received : 10 June 2021
Accepted : 22 September 2021
Published : 13 November 2021
DOI : https://doi.org/10.1186/s12889-021-11906-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug abuse, substance, adolescent
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Research articles

Unexplored therapeutic opportunities in the human genome
In 2014, the Illuminating the Druggable Genome programme was launched to promote the exploration of currently understudied but potentially druggable proteins. This article discusses how the systematic collection and processing of a wide array of biological and chemical data as part of this programme has enabled the development of evidence-based criteria for tracking the target development level of human proteins, which indicates a substantial knowledge deficit for approximately one out of three proteins in the human proteome. It also highlights the nature of the unexplored therapeutic opportunities for major protein families.
- Tudor I. Oprea
- Cristian G. Bologa
- Gergely Zahoránszky-Köhalmi
Drug discovery effectiveness from the standpoint of therapeutic mechanisms and indications
Shih and colleagues analyse comprehensive industry-wide data on drug development projects pursued during the past 20 years, classified according to the mechanism and indication for each project. Their findings indicate several points and trends that may be useful in understanding and improving the productivity of the pharmaceutical industry, including areas with substantial success or failure and the relative extent of novelty in completed and ongoing projects.
- Hsin-Pei Shih
- Xiaodan Zhang
- Alex M. Aronov

Trends in GPCR drug discovery: new agents, targets and indications
G protein-coupled receptors (GPCRs) are the most intensively studied class of drug targets. This article presents a pioneering analysis of all GPCR-targeted drugs and agents that are currently in clinical trials, and discusses the trends across molecule types, drug targets and therapeutic indications.
- Alexander S. Hauser
- Misty M. Attwood
- David E. Gloriam
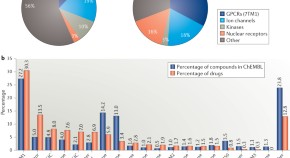
A comprehensive map of molecular drug targets
The success of mechanism-based drug discovery depends on the definition of the drug target, but targets are often poorly defined in the literature. Here, Overington and colleagues present a comprehensive map of the molecular targets of approved drugs, and explore aspects including the footprint of target classes across disease areas, the success of privileged target families and drug target orthologues across standard model organisms.
- Rita Santos
- John P. Overington
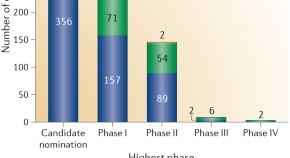
An analysis of the attrition of drug candidates from four major pharmaceutical companies
Attempts to reduce the number of efficacy- and safety-related failures that may be linked to the physicochemical properties of small-molecule drug candidates have been inconclusive owing to the limited size of data sets from individual companies. Waring and colleagues analyse the largest data set compiled so far on the causes of attrition for oral, small-molecule drug candidates, derived from a pioneering data-sharing effort by AstraZeneca, Eli Lilly and Company, GlaxoSmithKline and Pfizer.
- Michael J. Waring
- John Arrowsmith
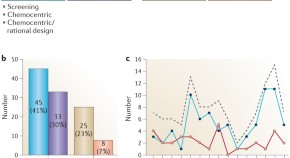
The discovery of first-in-class drugs: origins and evolution
Previous analyses of new drug approvals have suggested that phenotypic screening strategies have been more productive than target-based approaches in the discovery of first-in-class small-molecule drugs. Eder and colleagues analysed the origins of the first-in-class drugs approved by the US Food and Drug Administration from 1999 to 2013, and found that target-based approaches have had a substantial impact in more recent years. They discuss the implications for drug discovery strategies, including viewing phenotypic screening as a novel discipline rather than as a neoclassical approach.
- Richard Sedrani
- Christian Wiesmann
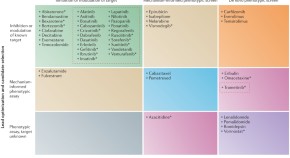
Phenotypic screening in cancer drug discovery — past, present and future
There has been a resurgence of interest in the use of phenotypic screens in drug discovery as an alternative to target-focused approaches. Moffat and colleagues investigated the contribution of phenotypic assays in oncology by analysing the origins of the new small-molecule cancer drugs approved by the US Food and Drug Administration over the past 15 years. They also discuss technical and biological advances that could empower phenotypic drug discovery in oncology by enabling the development of mechanistically informed phenotypic screens.
- John G. Moffat
- Joachim Rudolph
- David Bailey
The role of ligand efficiency metrics in drug discovery
Ligand efficiency metrics quantify the molecular properties required to gain binding affinity for a drug target. This article discusses the application of such metrics in the selection and optimization of fragments, hits and leads, highlighting how optimizing ligand efficiency metrics based on both molecular mass and lipophilicity, when set in the context of the specific target, has the potential to increase the quality of drug candidates.
- Andrew L. Hopkins
- György M. Keserü
- Charles H. Reynolds

Objective assessment of cancer genes for drug discovery
Effectively selecting therapeutic targets from the sizeable lists that are emerging from large-scale multi-omics initiatives is a key challenge in drug discovery. This article describes an objective, systematic computational assessment of biological and chemical space that can be applied to any human gene set to prioritize targets for further evaluation, and demonstrates its use on a set of 479 cancer-associated genes to identify new opportunities for drug discovery and repurposing.
- Mishal N. Patel
- Mark D. Halling-Brown
- Bissan Al-Lazikani
Quantifying factors for the success of stratified medicine
Co-developing a drug with a diagnostic to create a stratified medicine — a therapy that is targeted to a specific patient population on the basis of a clinical biomarker — presents challenges for product developers, regulators, payers and physicians. With the aim of developing a shared framework and tools for addressing these challenges, this article presents an analysis using data from case studies in oncology and Alzheimer's disease, coupled with integrated computational modelling of clinical outcomes and economic value, to quantify the effects of decisions on key issues such as the design of clinical trials.
- Mark R. Trusheim
- Breon Burgess
- Michael C. Palmer
The influence of the 'organizational factor' on compound quality in drug discovery
In the past 15 years, it has become clear that physicochemical properties of drug candidates, such as lipophilicity and molecular mass, have an important influence on the likelihood of compound-related attrition during development. By analysing the properties of compounds described in patents from leading pharmaceutical companies between 2000 and 2010, this article indicates that a substantial part of the industry has not modified its drug design practices accordingly and is still producing compounds with suboptimal physicochemical profiles.
- Paul D. Leeson
- Stephen A. St-Gallay
Trends in the exploitation of novel drug targets
Schiöth and colleagues examine the drugs approved by the US Food and Drug Administration over the past 30 years and analyse the interactions of these drugs with therapeutic targets encoded by the human genome, identifying 435 effect-mediating drug targets. They also analyse trends in the introduction of drugs that modulate previously unexploited targets, and discuss the network pharmacology of the drugs in the data set.
- Mathias Rask-Andersen
- Markus Sällman Almén
- Helgi B. Schiöth

How were new medicines discovered?
To investigate whether some strategies have been more successful than others in the discovery of new drugs, this article analyses the discovery strategies and the molecular mechanism of action for 259 new drugs that were approved by the US Food and Drug Administration between 1999 and 2008. Observations from this analysis — such as the fact that the contribution of phenotypic screening to the discovery of first-in-class small-molecule drugs exceeded that of target-based approaches in an era in which the major focus was on target-based approaches — could have important implications for efforts to increase the productivity of drug research and development.
- David C. Swinney
- Jason Anthony
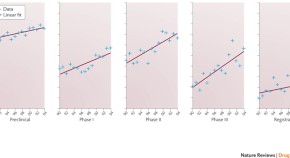
The productivity crisis in pharmaceutical R&D
Although investment in pharmaceutical research and development (R&D) has increased substantially in recent decades, the lack of a corresponding increase in the output in terms of new drugs being approved indicates that therapeutic innovation has become more challenging. Here, using a large database that contains information on R&D projects for more than 28,000 compounds investigated since 1990, Riccaboni and colleagues examine the factors underlying the decline in R&D productivity, which include an increasing concentration of R&D investments in areas in which the risk of failure is high.
- Fabio Pammolli
- Laura Magazzini
- Massimo Riccaboni
Probing the links between in vitro potency, ADMET and physicochemical parameters
A common assumption in current drug discovery strategies is that compounds with high in vitro potency at their target(s) have a greater potential to translate into successful, low-dose therapeutics, which is reflected in screening cascades with in vitro potency embedded as an early filter. This analysis of the publicly available ChEMBL database, which includes more than 500,000 drug discovery and marketed oral drug compounds, suggests that the perceived benefit of high in vitro potency may be negated by poorer absorption, distribution, metabolism, elimination and toxicity (ADMET) properties.
- M. Paul Gleeson
- Anne Hersey
- John Overington
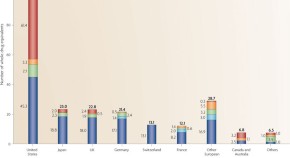
The importance of new companies for drug discovery: origins of a decade of new drugs
Understanding the factors that promote drug innovation is important both for improvements in health care and the future of organizations engaged in the field. To investigate these factors, Kneller identifies the inventors of 252 new drugs approved by the US Food and Drug Administration from 1998 to 2007 and their places of work, and classifies these drugs according to innovativeness. This article presents a comprehensive analysis of these data, which highlight the strong contribution of biotechnology companies, particularly in the United States, to innovative drug discovery, and discusses potential contributing factors to the trends observed.
- Robert Kneller
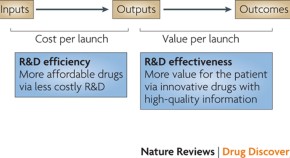
How to improve R&D productivity: the pharmaceutical industry's grand challenge
Improving R&D productivity is crucial to ensuring the future viability of the pharmaceutical industry and advances in health care. This article presents a detailed analysis, based on comprehensive, recent, industry-wide data, to identify the relative contributions of each of the steps in the drug discovery and development process to overall R&D productivity, and proposes strategies that could have the most substantial impact in enhancing R&D productivity.
- Steven M. Paul
- Daniel S. Mytelka
- Aaron L. Schacht
Lessons from 60 years of pharmaceutical innovation
This article investigates pharmaceutical innovation by analysing data on the companies that introduced the ∼1,200 new drugs that have been approved by the US FDA since 1950. Implications of this analysis — which shows that the rate of new drug output in this period has essentially been constant despite the huge increases in R&D investment — are discussed, as well as options to achieve sustainability for the pharmaceutical industry.
- Bernard Munos
Can literature analysis identify innovation drivers in drug discovery?
Here, the authors use bibliometrics and related data-mining methods to analyse PubMed abstracts, literature citation data and patent filings. The analyses are used to identify trends in disease-related scientific activity that are likely to give new therapeutic opportunities.
- Pankaj Agarwal
- David B. Searls
Community-wide assessment of GPCR structure modelling and ligand docking: GPCR Dock 2008
The recent determination of several crystal structures of G protein-coupled receptors (GPCRs) is providing new opportunities for structure-based drug design. This article analyses the state of the art in the prediction of GPCR structure and the docking of potential ligands on the basis of a community-wide, blind prediction assessment — GPCR Dock 2008 — that was carried out in coordination with the publication of the human adenosine A 2A receptor structure in 2008 and public release of the three-dimensional coordinates.
- Mayako Michino
- Enrique Abola
- Raymond C. Stevens
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Focus (Am Psychiatr Publ)
- v.17(2); Spring 2019

Substance Use Among College Students
Substance use among college students is associated with negative outcomes, and several risk factors, such as academic and peer pressure, are specific to this population. This article describes specific challenges and approaches to treatment for this population, including screening tests and interventions for specific substances and evidence-based programming.
U.S. college campuses have witnessed a national increase of cannabis, stimulant, and illicit drug use among students over the past decade. Substance use among college students is associated with numerous negative outcomes including lower academic performance, a higher probability of unemployment after graduation, and an increased risk of committing and experiencing sexual assault. Several risk factors for substance use are specific to this population, including an affiliation with Greek life, perception of high academic pressure, and peer pressure. Students with problematic substance use also face unique challenges in planning treatment, including aspects of confidentiality, financial constraints, and potential university oversight and involvement. This article highlights the prevalence of substance use on college campuses and describes some of the specific challenges and approaches to treatment in this population, including screening tests and interventions for specific substances used on college campuses and evidence-based substance use programming for college students.
For many youths, college enrollment is a distinct life event that symbolizes the transition from adolescence to independence and adulthood. It also represents a vulnerable period for increased exposure to a variety of illicit and prescribed substances.
Clinical Context
Substance use on college campuses.
Although attending college has historically been considered a protective factor against the development of substance use disorders, in recent decades substance use has become one of the most widespread health problems on college campuses in the United States ( 1 ). In a study by Caldeira et al. ( 2 ), nearly half of 946 college students who were followed from freshman to junior year met criteria for at least one substance use disorder during that time. Students who regularly use substances are more likely to have lower GPAs, spend fewer hours studying, miss significantly more class time, and fail to graduate or to be unemployed postgraduation ( 3 – 6 ). Substance use is also associated with significant general medical and psychiatric morbidity and mortality for many students ( 7 , 8 ).
One of the most significant challenges with addressing substance use on college campuses is related to its history of integration into the normative tradition and fabric of the college experience. Alcohol use is a prime example. National survey data indicate that over 60% of full-time college students have consumed alcohol, and a staggering 39% report engaging in binge drinking (consuming five or more drinks) over the past month ( 9 ). Surprisingly, both past-month and past-year alcohol use are higher for college attendees than for age-matched cohorts who do not attend college ( 1 ). Binge drinking can lead to dangerously elevated blood alcohol levels and is associated with an increased risk of illicit drug use ( 10 ). The challenges associated with beginning college life, such as separation from family members, participation in new social networks, and more intense academic pressures, may significantly contribute to increased alcohol consumption.
The escalation and normative acceptance of the use of prescription stimulants for cognitive enhancement purposes have also increased on college campuses over the past decade ( 1 ). Annual prevalence of nonmedical dextroamphetamine (Adderall) use among college students is higher (9.9%) than for age-matched youths not enrolled in college (6.2%) ( 1 ). College students often seek out dextroamphetamine prescriptions from mental health practitioners, with the intention of enhancing their ability to focus and study for exams. This presents a unique challenge for prescribers, who must ensure that those who need stimulant medication for a diagnosed condition receive it while not overprescribing to those who may be using it for nontherapeutic purposes.
The use of cocaine among college students presents another challenge to health care providers. According to the 2016 Monitoring the Future survey, 4.0% of full-time college students surveyed used cocaine in the past year, and 1.4% used cocaine in the past month ( 1 ). A longitudinal study of 1,253 college students found that more than 20% were exposed to opportunities for cocaine use in the past year ( 11 ). The substantial presence of stimulants on college campuses warrants the continued attention of clinicians and school administrators.
The percentage of college students using cannabis daily has increased, nearly doubling between 2007 and 2014 ( 1 ). According to the 2016 National Survey on Drug Use and Health, 20% of full-time college students reported using marijuana in the past month ( 12 ). There is considerable evidence of the short-term impact of heavy cannabis use on memory and learning, and it plays a negative role in academic and health outcomes on college campuses ( 4 , 13 ). The likelihood of cannabis use increases during the college years, with some studies demonstrating an escalation in prevalence with each successive year ( 14 ).
Fortunately, tobacco use has been on the decline over the past 20 years across U.S. college campuses. However, campuses have witnessed a relative explosion of electronic cigarette/vaporizer devices, which offer the ability to use more concentrated amounts of nicotine ( 15 ), as well as cannabis oil (sometimes known as “dab pens”). Although college students are still somewhat less likely than noncollege cohorts to use vaporizer devices (6.9% versus 9%), the trend suggests that use of electronic vaporizer devices represents a new and potentially more discrete means of acquiring physiologic nicotine dependence ( 1 ). For example, the Juul is a very small and popular vaporizer device sold online, advertising its compact nature and colorful nicotine pods to youths as fun and convenient (including a charging station that fits onto the side of a laptop computer). One pod contains as much nicotine as a full pack of traditional cigarettes. Relatively short-term use can lead to significant symptoms of nicotine withdrawal. Youths who initiate experimentation with electronic cigarettes are also more likely than those who do not to progress to tobacco products ( 16 ). In some cases, youths are also experimenting with alternative modes of cannabis delivery with vaporizing devices. Cannabis oil cartridge sales have escalated in states where cannabis is legal, such as California, while traditional sales of the cannabis plant product have simultaneously declined ( 17 ).
MDMA, LSD, and other psychedelic drugs are also gaining popularity in the club and rave scenes among college students. The annual prevalence of MDMA use among college students more than doubled from 2004 to 2016 ( 1 ), and the rate of emergency room visits resulting from MDMA use in this age group continues to increase ( 18 ). College students reported taking hallucinogens and MDMA for reasons such as curiosity, a desire to escape or to achieve a novel experience, and social pressures ( 19 , 20 ). In recent years, “microdosing” has also gained popularity among college students. Microdosing describes the act of consuming a small amount of hallucinogen in order to achieve a subtle psychedelic effect but not to fully alter consciousness. Research on the prevalence and potential adverse effects of microdosing is unfortunately scarce ( 21 ).
In the midst of the opioid crisis, college students are particularly vulnerable to opioid misuse. According to the National Survey on Drug Use and Health, young adults ages 18 to 25 report the highest past-year opioid use prevalence of all age groups ( 22 ). The risk for opioid use disorders commonly begins during adolescence and young adulthood ( 23 , 24 ), coinciding with the college years. Results from a recent study suggest that opioid misuse among college students is associated with several factors, such as living off campus and having a low GPA ( 25 ). Unfortunately, individuals in this age group are often reluctant to enter treatment. Even for those who receive treatment, retention rates are lower than for older adults ( 26 – 28 ). Unfortunately, although the American Academy of Pediatrics supports the use of medication-assisted treatment for opioid use disorder, prescribing rates remain relatively low for young adults ( 24 ). Buprenorphine-naloxone is approved for patients ages 16 and older and has been found to be a cost-effective treatment in this age group. Methadone or extended-release injectable naltrexone may also be options; however, some have cautioned about the perceived stigma of methadone in this age group ( 29 ), and to date there is limited data directly supporting extended injectable naltrexone in this population ( 30 , 31 ).
Risk Factors Specific for Substance Use on College Campuses
In addition to general risk factors, such as certain psychiatric conditions and family history of substance use disorders ( 32 , 33 ), there are a number of risk factors for substance use specific to the college campus. Figure 1 summarizes these factors. Peer influence and the perception of harm play a significant role in the decision to engage in substance use on college campuses. This is especially true during the first year of college, with less of an effect in each consecutive year ( 34 ). Students who perceive substance use by their peers to be normative are more likely to be at risk themselves of developing a substance use disorder ( 35 ). This perception is confounded by a general overestimation of peer substance use within the college-age population ( 35 – 37 ). According to the American College Health Association, among 26,139 undergraduate students from 52 schools, 9% had used cigarettes in the past 30 days, yet most believed that about 71% of their counterparts had smoked cigarettes in the past 30 days ( 36 ). The results were also similar for cannabis use. The drastic overestimation of peer use has been found to be present in nearly all categories of substance use.

College campus–specific risk factors for substance use
Members of fraternities and sororities have some of the highest rates of substance use on college campuses. Compared with nonmembers, fraternity and sorority members are more likely to use alcohol, cannabis, and other drugs, as well as binge drink more frequently and smoke cigarettes, ( 38 , 39 ). Members also suffer from more negative consequences from substance use compared with nonmembers, including a higher prevalence of driving under the influence, being physically injured, experiencing memory loss, and having unprotected sex ( 40 , 41 ). Males who live in fraternity houses during college not only have a heightened risk of binge drinking but are also at higher risk of an alcohol use disorder later in adulthood (45% reporting symptoms that meet criteria) ( 42 ). Living in a fraternity or sorority house is also associated with a higher prevalence of cigarette smoking ( 38 ). Students who engage in substance use behaviors during high school are more likely to join fraternities and sororities when they enter college ( 43 ). Male students demonstrate a greater increase in alcohol use after pledging into fraternities, compared with nonmembers ( 44 ). Members who are more actively involved or who have taken leadership positions are also more likely to hold positive thoughts about alcohol use, including the facilitation of bonding between brothers, having fun, and enhancing sexual appeal ( 45 ). Not surprisingly, students who later disaffiliate with Greek life demonstrate a decrease in heavy drinking and alcohol-related consequences ( 46 ).
The relative ubiquity of prescription stimulant medication on college campuses places at risk students who are academically underperforming or experiencing significant academic pressure. A recent longitudinal study found that approximately one-third of students were offered stimulants for nonmedical use in the past year. Of those who were offered stimulants, more than one-third misused them ( 47 ). In 2016, approximately one in ten college students reported nonmedical use of dextroamphetamine-amphetamine (Adderall) in the past 12 months ( 1 ). The risk is especially elevated for female college students, who are twice as likely as their noncollege female counterparts to use stimulant medications for nonmedical purposes ( 1 ). The risk is also higher among college students with lower GPAs and those who have skipped more classes ( 14 ). The number of first-time stimulant users typically peaks in April and November, coinciding with college final-exam weeks ( 48 ). Despite popular beliefs by college students that the nonmedical use of stimulants will facilitate earning higher grades ( 49 ), nonmedical use has not been found to be associated with an improvement in academic performance as reflected by GPA ( 50 ).
Substance Use and Sexual Assault
Sexual assault is a significant problem on college campuses. Alcohol and other drug use is a strong predictor of an increased risk of committing and experiencing sexual assault among college students ( 51 ). Unfortunately, being involved in Greek life and binge drinking are added risk factors for experiencing a sexual assault in college ( 52 ). Among a survey of 23,980 college women, 4.7% endorsed having been raped since the beginning of the school year ( 53 ). Three-quarters reported being intoxicated when the perpetration happened. Female students who reported binge drinking (defined by the investigator as having six or more drinks on one occasion) at least monthly were more than twice as likely as those who did not report monthly binge drinking to experience a sexual assault ( 52 ). The amount of alcohol consumed is also linearly correlated with the perpetrator’s aggressiveness ( 54 ). Unfortunately, alcohol consumption by victims can impair their ability to stay alert to the perpetrator’s intent and makes it harder to resist or escape the sexual assault.
Treatment Strategies and Evidence
Each clinical situation requires a specific treatment plan that is tailored to an individual’s current set of circumstances, level of motivation for treatment, and financial and social resources. Table 1 provides a summary of screening tests and treatment recommendations by substance category. Many of these screening tools provide a simple and straightforward way of assessing a college student’s risk of developing a substance use disorder. Additional information to determine the severity of substance use should be obtained by an interview if a student’s screen indicates an elevated risk.
Recommended screening tests and interventions for specific substances used on college campuses
| Alcohol | Fraternity and sorority membership, students who used heavily in high school | CRAFFT (for adolescents; car, relax, alone, forget, friends, trouble), CAGE Questionnaire (cut down, annoyed, guilty, eye opener), AUDIT (Alcohol Use Disorders Identification Test), TAPS Tool (tobacco, alcohol, prescription medication and other substance use), NM ASSIST (NIDA-Modified Alcohol, Smoking and Substance Involvement Screening Test) | BASICS Program; College Drinker's Check-up (CDCU); motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change | Detoxification when withdrawal symptoms are present; referral for individual therapy, self-help groups, or pharmacotherapy (i.e., naltrexone or acamprosate) for alcohol use disorders; close monitoring around academic performance and necessary accommodations |
| Tobacco, nicotine | Fraternity and sorority membership, existing mental health difficulties | NM ASSIST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change | Nicotine replacement therapy; no evidence that vaporizing devices lead to reduced risk of relapse (may escalate use); behavioral therapy referral |
| Stimulants | Academic difficulties, preexisting ADHD, midterms | DAST (Drug Abuse Screening Test), TAPS Tool, NM ASSIST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change; warn of risk of using cocaine with alcohol. | No evidenced-based pharmacological intervention at this time; balance risk of prescribing stimulants with need, if indicated; cognitive-behavioral therapy and 12-step programming may be helpful; close monitoring of academic performance and necessary accommodations |
| Opioids | Withdrawal from social interactions, poor academic performance, existing mental health difficulties | DAST, TAPS Tool, NM ASSIST | Motivational interviewing not advised; thoroughly assess for signs of withdrawal and acute safety concerns | Significant risk of overdose; consider detoxification setting or residential treatment setting for regular use; buprenorphine-naloxone and long-acting injectable naltrexone are considered first-line treatment; close monitoring of academic performance and necessary accommodations |
| Marijuana, cannabis | Low perception of harm of marijuana use, peers who use, poor academic performance, existing mental health concerns | World Health Organization ASSIST (Alcohol, Smoking and Substance Involvement Screening Test), how many times have you used marijuana in the past 90 days, TAPS Tool, NM ASSIST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change; marijuana eCHECKUP TO GO | N-acetylcysteine 1,200 mg twice daily may reduce cravings and risk of relapse among motivated individuals up to age 21 in addition to contingency management; behavioral therapy referral; close monitoring of academic performance and necessary accommodations |
| Hallucinogens | Frequent attendance at “rave parties” or club settings | DAST, TAPS Tool, NM ASSIST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change; provide information about potential risks of “microdosing” ( ) | Inform of risk of tolerance formation after only one use, as well as flashbacks; develop a plan for abstinence or reduction; referral for individual therapy |
| Benzodiazepines | Existing mental health difficulties, combining benzodiazepines and alcohol in party setting | DAST, TAPS Tool, NM ASSIST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change; provide psychoeducation about dangers of using benzodiazepines in combination with alcohol and other substances | Assess for withdrawal symptoms and consider detoxification if present, followed by residential treatment or long-term program; outpatient management is not recommended unless use is infrequent |
| Inhalants | Existing mental health difficulties, expressed need for escape and dissociation | DAST, NM ASSIST | Provide psychoeducation about the acute and long-term dangers of use | Significant health concerns and risk with acute intoxication; long-term use can lead to depression and brain damage; consider higher level of care, such as inpatient or partial program. |
| Over-the-counter medications (dextromethorphan, antihistamines) | Existing mental health difficulties, expressed need for escape and dissociation | DAST | Motivational interviewing to address discrepancy between problematic use and values and to assess readiness for change | Risk of significant impairment from acute intoxication; inpatient hospitalization for any accompanying suicidality, paranoia, or persistent hallucinations. |
Prevention and Brief intervention
Multiple prevention and intervention strategies have been implemented for selected at-risk students on college campuses. The Substance Abuse and Mental Health Services Administration has created a national registry of evidence-based programs and practices designed for substance use–related interventions. The database contains several programs tailored to the college student population. One example includes the Brief Alcohol Screening and Intervention for College Students (BASICS) program, which is based on a motivational-interviewing style of interaction that uses cognitive-behavioral therapy skills to reduce alcohol consumption among college students who are at risk of alcohol-related problems ( 55 ). BASICS consists of two 1-hour interviews and an online survey assessment ( 56 ). BASICS aims to motivate students to reduce risky behaviors and has been shown to be effective in reducing alcohol use among heavy-drinking students ( 57 , 58 ). The College Drinker's Check-up (CDCU) is a 90-minute computer-based brief intervention targeted toward college students who are episodic drinkers. The CDCU has demonstrated effectiveness in reducing heavy alcohol use among college students ( 59 ). Additional prevention and intervention programs that target college students are described in Table 2 ( 60 – 84 ).
Evidence-based substance use programming for college students a
| AlcoholEdu for College ( – ) | Online | A 1- to 3-hour interactive multimedia online course that consists of a baseline survey and four modules | Reduce alcohol use and alcohol-related negative consequences | Contact the program supplier for pricing information (everfi.com) |
| Alcohol Literacy Challenge ( , ) | Classroom based | A 50-minute group-delivered classroom session that incorporates slides and videos | Reduce alcohol use by correcting erroneous beliefs about its positive and negative effects | $5,000 onsite training and $1 per student per year licensing fee ( ) |
| Brief Alcohol Screening and Intervention for College Students (BASICS) ( , , , , ) | In person | Two 1-hour one-on-one interviews with a BASICS facilitator and one online survey | Motivate high-risk students to reduce alcohol consumption; prompt students to change their drinking patterns; teach coping skills | $4,500 onsite training and $1,000 licensing fee; annual licensing fee for online assessment varies ( ) |
| Challenging College Alcohol Abuse ( ) | Campaign | Social media campaign that places advertisements in the school newspaper and other media and provides minigrants to support nonalcohol social activities | Reduce binge drinking by challenging misconceptions about peer use; reduce the negative impact of heavy alcohol use on campus | Free |
| College Drinker’s Check-up ( , , ) | Computer-based software and online version | A 45-minute Web-based brief motivational interview that includes screening, assessment, feedback, and setting a plan; optional follow-up sessions are also available | Reduce alcohol consumption among heavy, episodic drinkers; give at risk students personalized feedback and invite them to participate in the intervention module | One-time fee $2,500 for colleges with fewer than 15,000 students and $4,500 for colleges with more than 15,000 students ( ) |
| InShape Prevention Plus Wellness ( ) | In person | A 30-minute session, including a baseline screen, a one-on-one consultation, and a behavioral goal plan | Reduce alcohol, tobacco, and illicit drug use; promote healthy eating, exercise, and other positive changes | $499 teacher’s manual; optional online and in-person webinars and workshops ( ) |
| Kognito At-Risk for College Students ( , ) | Online | A 30-minute interactive training simulation with virtual avatars | Increase knowledge and awareness about mental health; identify warning signs of psychological distress; promote help-seeking | Starting at $2,000 per year; price depends on size of the institution ( ) |
| PRIME for Life ( , ) | In person | A motivational risk reduction program delivered by instructors and group leaders | Change drinking and drug use behaviors of high-risk individuals; typically used by agencies serving individuals who have violated some type of substance use policy | Contact the program supplier for pricing information |
| Safer California Universities Study (SAFER) ( , ) | Online | An alcohol risk management prevention strategy that includes action plans for enforcing alcohol control measures on and around college campuses | Reduce heavy drinking on and around campus; reduce alcohol-related risky behaviors, such as driving while intoxicated | Free ( ) |
| Say It Straight (SIS) ( – ) | Classroom-based | Five to ten 45- to 50-minute sessions led by one or two trainers; sessions are action oriented and involve components such as role-plays | Prevent risky or destructive behaviors (i.e., substance use, violence, and dropout) and promote positive changes through drug refusal skill practices and communication training | $750 per participant in training workshop; $750 certification; $250 trainer manual in addition to workbooks and posters ( ) |
Treatment Considerations
The true confidentiality of patient records can be complicated in this patient population. When treating an adolescent under age 18, a parent or guardian has the right to obtain copies of the medical record without the patient’s consent. For young adults, written consent must be obtained from the identified patient (with special consent required to obtain substance use history and treatment) in order to share any information. Because many students remain under their parent or guardian’s insurance plan at this age, itemized billing statements and summaries of coverage may be disclosed to the subscriber of the insurance plan, placing an additional barrier to completely confidential treatment.
Screening and evaluation of substance use are important, given the relatively low rates of help-seeking behaviors within the transitional youth population (the prevalence of help seeking among those with a substance use disorder is estimated to be only about 8%) ( 2 ). Screening also provides an opportunity for early intervention and education for those who need it, given the low perceived risk of harm from trying substances once or twice and the relative ease of access to substances on the college campus ( 85 ).
Campus Recovery Programs
Students in recovery may feel as though they are missing out on their college experience by needing to avoid high-risk social situations and certain school-related functions, in addition to having to attend treatment. Collegiate Recovery Programs (CRPs) or Collegiate Recovery Communities are college-based drug and alcohol–free programs that provide recovery support to students and an outlet to socialize in safe settings ( 86 ). These supports often include access to substance-free housing, in-person meetings, group activities, support during recovery-related crises, and overall guidance in navigating college life while abstinent. CRPs vary in size, funding capability, and level of supervision from employed staff members ( 87 ), but they share the goals of creating posttreatment communities that help to prevent relapse and promote abstinence. As of 2014, a total of 600 students were enrolled in 33 CRPs across the United States ( 86 ). A national survey of 29 CRPs demonstrated that students enrolled in these programs had a mean age of 26.2. Over a third of these individuals had spent time in jail or prison, and three-quarters had been treated for chronic mental health problems ( 88 ). Students have been found to participate in CRPs for an average of seven semesters, with approximately half already enrolled when they started college ( 64 ). CRPs have also demonstrated encouraging outcomes both in terms of relapse rates and academic performance ( 86 , 89 ). According to Texas Tech University, of the 80 students enrolled in its CRP, 82.5% had a GPA higher than 2.75, and nearly half of the students planned to pursue a professional degree after graduation ( 87 ). Another study found that 87.5% of the CRP alumni had no relapse following graduation ( 90 ). However, more research needs to be conducted to elucidate the ideal characteristics of these programs, compare recovery outcomes of students in these programs versus those not enrolled, and examine longer-term follow up data.
Special Circumstances
There are additional considerations when treating students in a college mental health facility. In certain circumstances, a student may have to agree to allow sharing of protected information between practitioner and the dean of the college in order to maintain good academic standing. Students may understandably be reluctant to share information about their substance use history with a practitioner who works in a health services facility on campus with this type of arrangement, although the same federal laws of confidentiality and consent technically apply in these cases. However, if the college or university already has knowledge of an identified mental health or substance use concern within its student body, it can compel students to receive treatment under the threat of expulsion and may require students to meet contingencies in order to return to school. This may include mandatory urine drug screens, a medical leave of absence, or designated mental health visits in the student mental health center on campus. If the individual is an international student in the United States on a visa, a request for a medical leave of absence can be obtained in most cases (either for treatment within the United States or abroad). Students treated near their college or university may encounter additional challenges over the summer months when school is not in session, especially if they live geographically far from campus.
Questions and Controversy
Two of the most common questions that colleges and universities have faced include how to approach alcohol use on campus and how to control the nonmedical use of prescription stimulants. In an effort to reduce morbidity and mortality, some colleges have banned alcohol consumption for all students on campus, regardless of their age. Colleges with alcohol bans have been found to have higher rates of abstinence, compared with other colleges without such policies (29% versus 16%) ( 91 ). However, students who choose to consume alcohol at colleges with alcohol bans have similar rates of quantity and frequency of alcohol consumption. Implementing alcohol-free fraternity and sorority housing has not been found to be effective in reducing overall alcohol use ( 92 , 93 ). Despite the effort to restrict alcohol use inside fraternity and sorority houses, members will often seek alternative drinking settings off campus ( 92 ).
The focus on preventive measures for the nonmedical use of prescription stimulants on college campuses has been less uniform across the United States. However, certain universities and colleges have implemented policies in their designated mental health facilities in an effort to reduce overprescribing and availability. Some college mental health facilities have stopped offering testing to establish new attention-deficit hyperactivity disorder (ADHD) diagnoses because of the high volume of requests. Others require significant documentation of a current diagnosis in order to provide prescriptions (including prior neuropsychological testing), and the institutions often closely monitor supplies, without permitting early refills ( 94 , 95 ). Many have also started no-prescription policies for controlled stimulant medication, without exception. If patients with a history of substance use require prescription stimulants for a medical indication, clinicians should closely monitor their prescription use and consider providing smaller supplies in an effort to reduce the risk of diversion or personal nonmedical use. Switching to a nonstimulant option (atomoxetine) for treatment of ADHD is another reasonable option for this population.
Although drug testing is not uncommon in other settings in colleges and universities, such as for college athletes and medical and dental school admissions, it is relatively rare for undergraduate universities to require students to take drug tests. The implementation of mandatory universal drug screening has resulted in a class-action lawsuit and a ruling by a federal appeals court that this form of testing is unconstitutional ( 96 ). In addition, mandatory drug testing can be viewed as an invasion of privacy and consumes a significant portion of school resources. One can argue that college students over age 18 should be allowed to make decisions for themselves, even if such decisions might result in severe consequences. Conversely, drug testing allows schools to identify at-risk students and intervene at an early stage to protect them from unnecessary risks, such as alcohol-related accidents and overdose. Whether colleges and universities should be allowed to implement mandatory drug testing remains controversial. However, urine drug screening should be a routine part of any clinical mental health assessment when working with this higher-risk population. Urine drug screening is often most beneficial when used as part of daily practice and not ordered only following suspicion of substance use or a known substance-related incident.
Recommendations
Even though problematic substance use has a marked presence on college campuses, many struggling students continue to go unrecognized. Treatment of this population presents specific challenges, but it can also be highly rewarding. Summary recommendations are provided below for psychiatrists working with the college-age youths both on and off college campuses.
Recommendation 1: Be Clear About Confidentiality Limitations
Offer a clear explanation of confidentiality limitations, especially as they apply to college students who are still under their parents’ insurance plans. This is the best way to begin to foster trust and to strategize with the patient about how to best protect his or her health information moving forward. Consider referral to an off-campus provider if the student understands the confidentiality protections but is still concerned about disclosing information to an on-campus provider. Because most college students presenting for a mental health evaluation will not express concern about a primary substance use disorder, it is important to carefully screen for co-occurring substance use (both concurrent and past use).
Recommendation 2: Screen for Past Sexual Assault and Violence
Screening for past sexual assault and violence is important when assessing a student who has a history of any substance use, particularly alcohol. Although most young adults will not typically volunteer information about prior sexual encounters during a general interview, sensitive but direct questioning about potential past assault (“Have you ever been taken advantage of when under the influence?”) increases the probability that the individual will report this information. Those who report past sexual assault and violence should be offered the option of further medical screening for sexually transmitted diseases, as well as a thorough safety assessment and assistance with law/campus enforcement, when appropriate.
Recommendation 3: Consider the Student’s Time Constraints in Treatment Planning
Treatment planning should take into consideration whether a student is willing or able to take time off from his or her education to pursue more intensive options. For example, an intensive outpatient program, in conjunction with a 12-step program in the evenings, might be more feasible than a medical leave of absence for some students. Universities and colleges often require that a student taking a medical leave of absence take off more than a single semester of study, which can delay graduation and thereby incur additional financial burden.
Recommendation 4: Formalize the Procedure for Planning a Medical Leave of Absence
If medical leave is being considered for longer-term treatment, it is important to have a clear plan (i.e., referral to a designated residential treatment facility and stipulation of what the treatment goals are while on leave). A written request by the treating clinician can be submitted to the academic department within the school to allow the student to suspend his or her enrollment for a designated period. Some schools may allow a treatment re-entry plan that can reduce the required time of medical leave (i.e., one versus two semesters).
Recommendation 5: Specify Treatment Site for International Students Taking Medical Leave
To request a medical leave of absence for international students, the clinician must specify where the treatment is to occur. The request should be communicated to the designated office of international services or student affairs, as well as to the student’s specific academic department.
Recommendation 6: Plan Ahead for Treatment Occurring Outside the Academic Year
Clinicians should plan ahead for alternative treatment arrangements over the summer months if the student lives out of state, as well as create a plan for handling any crises that may arise outside of the academic year. If a student is receiving a controlled substance, consider a required local check-in with an out-of-state provider, as well as review of any available Prescription Drug Monitoring System (PDMP). Many states are now linking viewable access to out-of-state prescription fills.
Recommendation 7: Discuss Tuition Insurance With Families
Families have the option of purchasing tuition insurance if there is concern that a chronic illness may interrupt the process of completing the semester at school and inflict additional financial cost. Substance use disorders are no exception, and a recommendation to purchase tuition insurance should be considered for identified at-risk students.
Future Directions
Colleges are facing continued challenges around students’ high rates of binge drinking, nonmedical use of stimulants for performance enhancement, and nicotine use. Psychiatrists have the opportunity to influence their local colleges and universities to integrate evidence-based practices. Although promising prevention and treatment programs are available, more research is needed to better inform university administrators about the effectiveness of various programs targeted to college students.
There is a need to develop prevention programming targeted toward specific high-risk subgroups, such as fraternity and sorority members. These members play a pivotal role in influencing the substance use culture on campus. Colleges and universities should communicate and collaborate with the National Panhellenic Conference and the North-American Interfraternity Conference when enforcing substance use policies. The National Panhellenic Conferences has a strict policy on the ban of alcohol use in sorority houses.
Campus recovery programs are increasing and are a way to provide support to students who have a history of problematic substance use. The Association of Recovery in Higher Education has compiled a list of participating CRC universities ( https://collegiaterecovery.org/collegiate-recovery-programs ), and clinicians can work with the association to create a CRC program at their institution.
The Drug Enforcement Administration also provides resources, such as the Campus Drug Prevention ( https://www.campusdrugprevention.gov ), to universities and colleges. The resources include information on how to identify illicit substances and a list of federal, state, and law enforcement resources.
Clinicians should closely monitor new drug-related trends that are increasing in popularity in this age group, such as vaping and microdosing. Despite lack of conclusive long-term data about the impact of these substances on health and psychological well-being, patients should still be cautioned about potential risks of addiction and associated medical complications. These complications may include respiratory damage and physiologic nicotine dependence with vaping, and neurotoxicity with LSD microdosing. Clinicians can commit to continuing medical education on this topic and contribute to the solution by creating new prevention and intervention programs for college campuses or by providing scientific support to existing programs.
Preparation of this article was financially supported by grant R21 DA046738 from the National Institute on Drug Abuse.
Dr. Welsh reports receipt of consulting fees from GW Pharmaceuticals and training fees from Chestnut Health Systems. The other authors report no financial relationships with commercial interests.

Stay up to date with the latest developments in therapeutics by reading the world’s most respected source of authoritative drug information. For over 50 years Drugs has been the definitive journal of drugs and therapeutics, promoting optimum pharmacotherapy by publishing reviews and original clinical research authored by leading international clinicians and researchers to support clinical decision-making.
Through a rigorous and comprehensive program of peer-reviewed evaluations, Drugs provides detailed and objective analysis covering the full spectrum of new and established drug therapies in all disease areas.
As a hybrid journal, Drugs does not charge authors to publish using the traditional subscription-based publishing route, but does offer the option to publish accepted articles open access if authors so wish or if their funders require ( more information ).
Drugs offers a range of additional features designed to increase the visibility, readership and educational value of the journal’s content ( more information ).
- Dene Peters

Latest issue
Volume 84, Issue 8
Latest articles
Slowing the progression of chronic kidney disease in patients with type 2 diabetes using four pillars of therapy: the time to act is now.
- Panagiotis I. Georgianos
- Vasilios Vaios
- Vassilios Liakopoulos
Donanemab: First Approval
- Connie Kang

Long-Term Safety and Efficacy Evaluation of Travoprost Intracameral Implant Based on Pooled Analyses from Two Phase III Trials
- I. Paul Singh
- John P. Berdahl
- Tomas Navratil

Dose Individualisation of Antimicrobials from a Pharmacometric Standpoint: The Current Landscape
- Tim Preijers
- Anouk E. Muller
- Sebastiaan D. T. Sassen

Impact of CYP2C19 Genotype Status on Clinical Outcomes in Patients with Symptomatic Coronary Artery Disease, Stroke, and Peripheral Arterial Disease: A Systematic Review and Meta-Analysis
- Dominique P. M. S. M. Maas
- Loes H. Willems
- Michiel C. Warlé

Journal updates
Digital features.
Drugs is able to host a range of digital features, with a number of options available to authors.
50 Years of Drugs Infographic

Journal information
- CAB Abstracts
- Chemical Abstracts Service (CAS)
- Current Contents/Clinical Medicine
- Current Contents/Life Sciences
- Google Scholar
- Japanese Science and Technology Agency (JST)
- OCLC WorldCat Discovery Service
- Pathway Studio
- Science Citation Index Expanded (SCIE)
- Semantic Scholar
- TD Net Discovery Service
- UGC-CARE List (India)
Rights and permissions
Editorial policies
© Springer Nature Switzerland AG
- Find a journal
- Publish with us
- Track your research
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- All Summits
- STATUS List
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Pfizer drug shows promise in cancer-related condition that causes weight loss and weakness
Cachexia is an under-recognized syndrome that needs further research.
- Manage alerts for this article
- Email this article
- Share this article

By Andrew Joseph
Sept. 14, 2024
Europe Correspondent
BARCELONA, Spain — Patients with advanced cancers often develop a secondary condition that causes them to shed weight, making it even harder to tolerate their cancer treatments. Called cachexia, it’s an under-recognized syndrome that researchers are still trying to tease out, and one that’s attracting more interest from drugmakers.
On Saturday, Pfizer reported that an experimental antibody not only helped cancer patients with cachexia regain some weight versus placebo, but that it also seemed to increase their muscle mass and activity levels, signaling that the added weight translated into meaningful benefits.
advertisement
“The weight gain compared to patients on placebo is very important, but showing a consequence of that weight gain in patient wellness is also very important, and that’s what we set out to do,” Charlotte Allerton, Pfizer’s head of discovery and early development, told STAT.
STAT+ Exclusive Story
Already have an account? Log in

This article is exclusive to STAT+ subscribers
Unlock this article — plus daily coverage and analysis of the biotech sector — by subscribing to stat+..
Totals $468 per year
for 3 months, then $399/year
Then $399/year
Savings start at 25%!
Annually per user
$300 Annually per user
Get unlimited access to award-winning journalism and exclusive events.
About the reporting
STAT’s investigation is based on interviews with nearly 100 people around the country, including incarcerated patients and grieving families, prison officials, and legal and medical experts. Reporter Nicholas Florko also filed more than 225 public records requests and combed through thousands of pages of legal filings to tell these stories. His analysis of deaths in custody is based on a special data use agreement between STAT and the Department of Justice.
You can read more about the reporting for this project and the methodology behind our calculations.
The series is the culmination of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by The Commonwealth Fund.
Andrew Joseph
Andrew Joseph covers health, medicine, and the biopharma industry in Europe.
More on Long Covid

STAT Plus: As Humira biosimilars take over the market, CVS has created a new ploy: the drug ‘rebate credit’

Your guide to the annual European Society for Medical Oncology Congress
Your data will be processed in accordance with our Privacy Policy and Terms of Service . You may opt out of receiving STAT communications at any time.

A new era for drug development and research
Recommended

STAT Plus: Incyte’s checkpoint inhibitor staves off disease progression in anal cancer trial

STAT Plus: Lung cancer drug from iTeos, GSK shows response, boosting TIGIT as a viable target

Can GLP-1 drugs help with type 1 diabetes?

STAT Plus: Can iTeos and GSK solve TIGIT’s troubles?

Moderna cuts spending, and Sarepta’s ‘curse’ on Califf
Subscriber picks, stat plus: with a win in lung cancer, biotech’s wealthiest outsider surfs to new heights, stat plus: a new drug offers a rare option for brain cancer treatment — and inspires hopes for more, stat plus: former verily executives hatch plan to invest millions in high-tech medical data, stat plus: how pfizer ended up passing on my glp-1 work back in the early ’90s, stat plus: ‘sarepta’s like a curse on me’: fda commissioner dismisses controversy over elevidys.
- Environment
- Science & Technology
- Business & Industry
- Health & Public Welfare
- Topics (CFR Indexing Terms)
- Public Inspection
- Presidential Documents
- Document Search
- Advanced Document Search
- Public Inspection Search
- Reader Aids Home
- Office of the Federal Register Announcements
- Using FederalRegister.Gov
- Understanding the Federal Register
- Recent Site Updates
- Federal Register & CFR Statistics
- Videos & Tutorials
- Developer Resources
- Government Policy and OFR Procedures
- Congressional Review
- My Clipboard
- My Comments
- My Subscriptions
- Sign In / Sign Up
- Site Feedback
- Search the Federal Register
This site displays a prototype of a “Web 2.0” version of the daily Federal Register. It is not an official legal edition of the Federal Register, and does not replace the official print version or the official electronic version on GPO’s govinfo.gov.
The documents posted on this site are XML renditions of published Federal Register documents. Each document posted on the site includes a link to the corresponding official PDF file on govinfo.gov. This prototype edition of the daily Federal Register on FederalRegister.gov will remain an unofficial informational resource until the Administrative Committee of the Federal Register (ACFR) issues a regulation granting it official legal status. For complete information about, and access to, our official publications and services, go to About the Federal Register on NARA's archives.gov.
The OFR/GPO partnership is committed to presenting accurate and reliable regulatory information on FederalRegister.gov with the objective of establishing the XML-based Federal Register as an ACFR-sanctioned publication in the future. While every effort has been made to ensure that the material on FederalRegister.gov is accurately displayed, consistent with the official SGML-based PDF version on govinfo.gov, those relying on it for legal research should verify their results against an official edition of the Federal Register. Until the ACFR grants it official status, the XML rendition of the daily Federal Register on FederalRegister.gov does not provide legal notice to the public or judicial notice to the courts.
Design Updates: As part of our ongoing effort to make FederalRegister.gov more accessible and easier to use we've enlarged the space available to the document content and moved all document related data into the utility bar on the left of the document. Read more in our feature announcement .
Electronic Common Technical Document; Data Standards; Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research Supporting Electronic Common Technical Document Version 4.0
A Notice by the Food and Drug Administration on 09/16/2024
This document has been published in the Federal Register . Use the PDF linked in the document sidebar for the official electronic format.
- Document Details Published Content - Document Details Agencies Department of Health and Human Services Food and Drug Administration Agency/Docket Number Docket No. FDA-2018-D-1216 Document Citation 89 FR 75545 Document Number 2024-20897 Document Type Notice Pages 75545-75546 (2 pages) Publication Date 09/16/2024 Published Content - Document Details
- View printed version (PDF)
- Document Dates Published Content - Document Dates Dates Text Support for eCTDv4.0 electronic submissions begins September 16, 2024. FDA will also continue to support eCTDv3.2.2 electronic submissions. Submit either electronic or written comments at any time. Published Content - Document Dates
This table of contents is a navigational tool, processed from the headings within the legal text of Federal Register documents. This repetition of headings to form internal navigation links has no substantive legal effect.
Electronic Submissions
Written/paper submissions, for further information contact:, supplementary information:.
This feature is not available for this document.
Additional information is not currently available for this document.
- Sharing Enhanced Content - Sharing Shorter Document URL https://www.federalregister.gov/d/2024-20897 Email Email this document to a friend Enhanced Content - Sharing
- Print this document
Document page views are updated periodically throughout the day and are cumulative counts for this document. Counts are subject to sampling, reprocessing and revision (up or down) throughout the day.
This document is also available in the following formats:
More information and documentation can be found in our developer tools pages .
This PDF is the current document as it appeared on Public Inspection on 09/13/2024 at 8:45 am.
It was viewed 2 times while on Public Inspection.
If you are using public inspection listings for legal research, you should verify the contents of the documents against a final, official edition of the Federal Register. Only official editions of the Federal Register provide legal notice of publication to the public and judicial notice to the courts under 44 U.S.C. 1503 & 1507 . Learn more here .
Document headings vary by document type but may contain the following:
- the agency or agencies that issued and signed a document
- the number of the CFR title and the number of each part the document amends, proposes to amend, or is directly related to
- the agency docket number / agency internal file number
- the RIN which identifies each regulatory action listed in the Unified Agenda of Federal Regulatory and Deregulatory Actions
See the Document Drafting Handbook for more details.
Department of Health and Human Services
Food and drug administration.
- [Docket No. FDA-2018-D-1216]
Food and Drug Administration, HHS.
The Food and Drug Administration's (FDA or Agency) Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research are announcing support for Electronic Common Technical Document (eCTD) Version 4.0 (v4.0)-based electronic submissions.
Support for eCTDv4.0 electronic submissions begins September 16, 2024. FDA will also continue to support eCTDv3.2.2 electronic submissions. Submit either electronic or written comments at any time.
You may submit comments as follows:
Submit electronic comments in the following way:
- Federal eRulemaking Portal: https://www.regulations.gov . Follow the instructions for submitting comments. Comments submitted electronically, including attachments, to https://www.regulations.gov will be posted to the docket unchanged. Because your comment will be made public, you are solely responsible for ensuring that your comment does not include any confidential information that you or a third party may not wish to be posted, such as medical information, your or anyone else's Social Security number, or confidential business information, such as a manufacturing process. Please note that if you include your name, contact information, or other information that identifies you in the body of your comments, that information will be posted on https://www.regulations.gov .
- If you want to submit a comment with confidential information that you do not wish to be made available to the public, submit the comment as a written/paper submission and in the manner detailed (see “Written/Paper Submissions” and “Instructions”).
Submit written/paper submissions as follows:
- Mail/Hand Delivery/Courier (for written/paper submissions): Dockets Management Staff (HFA-305), Food and Drug Administration, 5630 Fishers Lane, Rm. 1061, Rockville, MD 20852.
- For written/paper comments submitted to the Dockets Management Staff, FDA will post your comment, as well as any attachments, except for information submitted, marked and identified, as confidential, if submitted as detailed in “Instruction.”
Instructions: All submissions received must include the Docket No. FDA-2018-D-1216 for “Electronic Common Technical Document; Data Standards; Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research Supporting Electronic Common Technical Document Version 4.0.” Received comments will be placed in the docket and, except for those submitted as “Confidential Submissions,” publicly viewable at https://www.regulations.gov or at the Dockets Management Staff between 9 a.m. and 4 p.m., Monday through Friday, 240-402-7500.
- Confidential Submissions—To submit a comment with confidential information that you do not wish to be ( print page 75546) made publicly available, submit your comments only as a written/paper submission. You should submit two copies total. One copy will include the information you claim to be confidential with a heading or cover note that states “THIS DOCUMENT CONTAINS CONFIDENTIAL INFORMATION.” The Agency will review this copy, including the claimed confidential information, in its consideration of comments. The second copy, which will have the claimed confidential information redacted/blacked out, will be available for public viewing and posted on https://www.regulations.gov . Submit both copies to the Dockets Management Staff. If you do not wish your name and contact information to be made publicly available, you can provide this information on the cover sheet and not in the body of your comments and you must identify this information as “confidential.” Any information marked as “confidential” will not be disclosed except in accordance with 21 CFR 10.20 and other applicable disclosure law. For more information about FDA's posting of comments to public dockets, see 80 FR 56469 , September 18, 2015, or access the information at: https://www.govinfo.gov/content/pkg/FR-2015-09-18/pdf/2015-23389.pdf .
Docket: For access to the docket to read background documents or the electronic and written/paper comments received, go to https://www.regulations.gov and insert the docket number, found in brackets in the heading of this document, into the “Search” box and follow the prompts and/or go to the Dockets Management Staff, 5630 Fishers Lane, Rm. 1061, Rockville, MD 20852, 240-402-7500.
Jonathan Resnick, Center for Drug Evaluation and Research, Food and Drug Administration, [email protected] ; or James Myers, Center for Biologics Evaluation and Research, Food and Drug Administration, Bldg. 71, Rm. 7301, Silver Spring, MD 20993-0002, 240-402-7911.
According to the guidance for industry entitled “Providing Regulatory Submissions in Electronic Format—Certain Human Pharmaceutical Product Applications and Related Submissions Using the eCTD Specifications” (available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/providing-regulatory-submissions-electronic-format-certain-human-pharmaceutical-product-applications ), submissions subject to section 745A(a) of the Federal Food, Drug, and Cosmetic Act ( 21 U.S.C. 379k-1(a) ) must be submitted in eCTD format using the version of eCTD currently supported by FDA unless such submission is exempt from the electronic submission requirements or if FDA has granted a waiver. The version of eCTD currently supported by FDA is specified in the FDA Data Standards Catalog (available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/data-standards-catalog ). FDA plans to update the FDA Data Standards Catalog to add eCTDv4.0 upon publication of this notice. FDA will support both eCTDv3.2.2 and eCTDv4.0 submissions before eventually only supporting eCTDv4.0 submissions. FDA will provide advance notice of when the Agency will begin supporting electronic submission only in eCTDv4.0. Specifications for eCTDv3.2.2 and v4.0 are available on FDA's eCTD web page (available at: https://www.fda.gov/drugs/electronic-regulatory-submission-and-review/electronic-common-technical-document-ectd ).
Dated: September 10, 2024.
Lauren K. Roth,
Associate Commissioner for Policy.
[ FR Doc. 2024-20897 Filed 9-13-24; 8:45 am]
BILLING CODE 4164-01-P
- Executive Orders
Reader Aids
Information.
- About This Site
- Legal Status
- Accessibility
- No Fear Act
- Continuity Information

IMAGES
VIDEO
COMMENTS
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
It starts with merely. smoking of cigarettes and gradually drowns the person into the trap of drug abuse. Stress, anxiety, peer pressure, poverty are some of the main causes of drug abuse.As is ...
This article examines the reasons young poly-drug users cite for using alcohol, cannabis, amphetamines, ecstasy, LSD and cocaine. It identifies 18 substance use functions and how they differ by age and gender.
Introduction. Social determinants of health (SDOH) are "the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks." [] There is a growing recognition in the fields of public health and medicine that SDOH play a key role in driving health inequities and ...
The current paper highlights the causes of drug abuse, and describes the treatment and prevention of drug abuse and addiction for proper management of the problem. Discover the world's research 25 ...
Introduction. An estimated 271 million people used an internationally scheduled ('illicit') drug in 2017, corresponding to 5.5% of the global population aged 15 to 64. 1 Despite decades of investment, policies aimed at reducing supply and demand have demonstrated limited effectiveness. 2 3 Moreover, prohibitive and punitive drug policies have had counterproductive effects by contributing ...
A drug is any substance capable of altering the functioning of a person's body and mind. In this paper, a deterministic nonlinear model was adapted to investigate the behavior of drug abuse and ...
Abstract. The current opioid epidemic is one of the most severe public health crisis in US history. Responding to it has been difficult due to its rapidly changing nature and the severity of its associated outcomes. This review examines the origin and evolution of the crisis, the pharmacological properties of opioids, the neurobiology of opioid ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
The characterisation of the role of glia and the extracellular matrix (ECM) in drug-induced synaptic plasticity is an exciting emerging field of drug addiction research as it comes with promising ...
Drawing on commissioned papers and presentations and discussions at a public workshop that it will plan and hold, the committee will prepare a report on the nature and operations of the illegal drug market in the United States and the research issues identified as having potential for informing policies to reduce the demand for illegal drugs ...
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA ...
At the National Institute on Drug Abuse (NIDA), we believe that increased understanding of the basics of addiction will empower people to make informed choices in their own lives, adopt science-based policies and programs that reduce drug use and addiction in their communities, and support scientific research that improves the Nation's well ...
Research Topics. En español. The National Institute on Drug Abuse (NIDA) is the largest supporter of the world's research on substance use and addiction. Part of the National Institutes of Health, NIDA conducts and supports biomedical research to advance the science on substance use and addiction and improve individual and public health.
Methamphetamine Research Report. | En español. | Provides an overview of the latest scientific findings on methamphetamine, including short- and long-term health consequences, effects on pregnancy, and potential prevention and treatment options. Research Report.
The Relationship Between Crime. and Drugs: What W e Ha ve. Learned in Recent Decades. David Deitch, Ph.D.*; Igor Koutsenok M.D.** & Amanda Ruiz, M.D.***. Abstract —The focus of this article is ...
This analysis of the publicly available ChEMBL database, which includes more than 500,000 drug discovery and marketed oral drug compounds, suggests that the perceived benefit of high in vitro ...
Research on the prevalence and potential adverse effects of microdosing is unfortunately scarce . In the midst of the opioid crisis, college students are particularly vulnerable to opioid misuse. According to the National Survey on Drug Use and Health, young adults ages 18 to 25 report the highest past-year opioid use prevalence of all age ...
For over 50 years Drugs has been the definitive journal of drugs and therapeutics, promoting optimum pharmacotherapy by publishing reviews and original clinical research authored by leading international clinicians and researchers to support clinical decision-making. Through a rigorous and comprehensive program of peer-reviewed evaluations ...
Drug use is one of the most common sources of referrals of students to police [Citation 80]. And recent estimates show that over a third of all U.S. school districts with middle or high schools had student drug testing policies [Citation 81-83]. Drug war policies also impact higher education, which is integral to economic mobility [Citation 84].
This monograph is based on the papers and discussion from a technical review on "Drug Abuse Prevention intervention Research: Methodological Issues," held on May 22-23, 1989, in Rockville, MD. ... clarity with a description of a drug abuse prevention research evaluation model that includes three levels of evaluation: (1) process evaluation ...
Abstract. Drug discovery is a dynamic field constantly evolving with the aim of identifying novel. therapeutic agents to combat various diseases. In this review, we present an overview of recent ...
Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year.
Pfizer drug shows promise in cancer-related condition that causes weight loss and weakness Cachexia is an under-recognized syndrome that needs further research Manage alerts for this article
The Food and Drug Administration's (FDA or Agency) Center for Drug Evaluation and Research and Center for Biologics Evaluation and Research are announcing support for Electronic Common Technical Document (eCTD) Version 4.0 (v4.0)-based electronic submissions. ... For written/paper comments submitted to the Dockets Management Staff, FDA will ...
June 14-15, 2024 Montreal, Canada. After three years of virtual meetings, the 2024 NIDA International Forum returned to an in-person format. The meeting, which was held on June 14 and 15 in Montreal in conjunction with the College on Problems of Drug Dependence (CPDD) Annual Scientific Meeting, was cochaired by NIDA International Program's leadership, Dr. Tom Clarke and Dr. Lindsey Friend.