Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- NEWS EXPLAINER
- 08 June 2021

The COVID lab-leak hypothesis: what scientists do and don’t know
- Amy Maxmen &
- Smriti Mallapaty
You can also search for this author in PubMed Google Scholar
Debate over the idea that the SARS-CoV-2 coronavirus emerged from a laboratory has escalated over the past few weeks, coinciding with the annual World Health Assembly, at which the World Health Organization (WHO) and officials from nearly 200 countries discussed the COVID-19 pandemic. After last year’s assembly, the WHO agreed to sponsor the first phase of an investigation into the pandemic’s origins, which took place in China in early 2021 .
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 594 , 313-315 (2021)
doi: https://doi.org/10.1038/d41586-021-01529-3
The Independent Panel for Pandemic Preparedness & Response COVID-19: Make it the Last Pandemic (Independent Panel, 2021).
Huang, Y. in Learning from SARS: Preparing for the Next Disease Outbreak: Workshop Summary (eds Knobler, S. et al. ) (National Academies Press, 2004).
Google Scholar
Zhou P. et al. Nature 579 , 270–273 (2020).
Article PubMed Google Scholar
Lytras, S. et al. Preprint at bioRxiv https://doi.org/10.1101/2021.01.22.427830 (2021).
Xiao, X. et al. Sci. Rep. 11, 11898 (2021).
Andersen, K. G. et al. Nature Med. 26 , 450–452 (2020).
Wu, Y. & Zhao, S. Stem Cell Res. 50 , 102115 (2020).
Peacock, T. P. et al. Preprint at bioRxiv https://doi.org/10.1101/2021.05.28.446163 (2021).
Zhou, P. et al. Nature 588 , E6 (2020).
Guo, H. et al. Preprint at bioRxiv https://doi.org/10.1101/2021.05.21.445091 (2021).
Download references
Reprints and permissions
Related Articles

- Public health
- Epidemiology

Could bird flu in cows lead to a human outbreak? Slow response worries scientists
News 17 MAY 24

Neglecting sex and gender in research is a public-health risk
Comment 15 MAY 24
Interpersonal therapy can be an effective tool against the devastating effects of loneliness
Correspondence 14 MAY 24

Bird flu in US cows: where will it end?
News 08 MAY 24

Monkeypox virus: dangerous strain gains ability to spread through sex, new data suggest
News 23 APR 24

Gut microbes linked to fatty diet drive tumour growth
News 16 MAY 24

Dual-action obesity drug rewires brain circuits for appetite
News & Views 15 MAY 24

Experimental obesity drug packs double punch to reduce weight
News 15 MAY 24
Postdoc in CRISPR Meta-Analytics and AI for Therapeutic Target Discovery and Priotisation (OT Grant)
APPLICATION CLOSING DATE: 14/06/2024 Human Technopole (HT) is a new interdisciplinary life science research institute created and supported by the...
Human Technopole
Research Associate - Metabolism
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoc Fellowships
Train with world-renowned cancer researchers at NIH? Consider joining the Center for Cancer Research (CCR) at the National Cancer Institute
Bethesda, Maryland
NIH National Cancer Institute (NCI)
Faculty Recruitment, Westlake University School of Medicine
Faculty positions are open at four distinct ranks: Assistant Professor, Associate Professor, Full Professor, and Chair Professor.
Hangzhou, Zhejiang, China
Westlake University
PhD/master's Candidate
PhD/master's Candidate Graduate School of Frontier Science Initiative, Kanazawa University is seeking candidates for PhD and master's students i...
Kanazawa University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
June 10, 2021
The COVID Lab-Leak Hypothesis: What Scientists Do and Do Not Know
An examination of the arguments that SARS-CoV-2 escaped from a lab in China and the science behind them
By Amy Maxmen , Smriti Mallapaty & Nature magazine

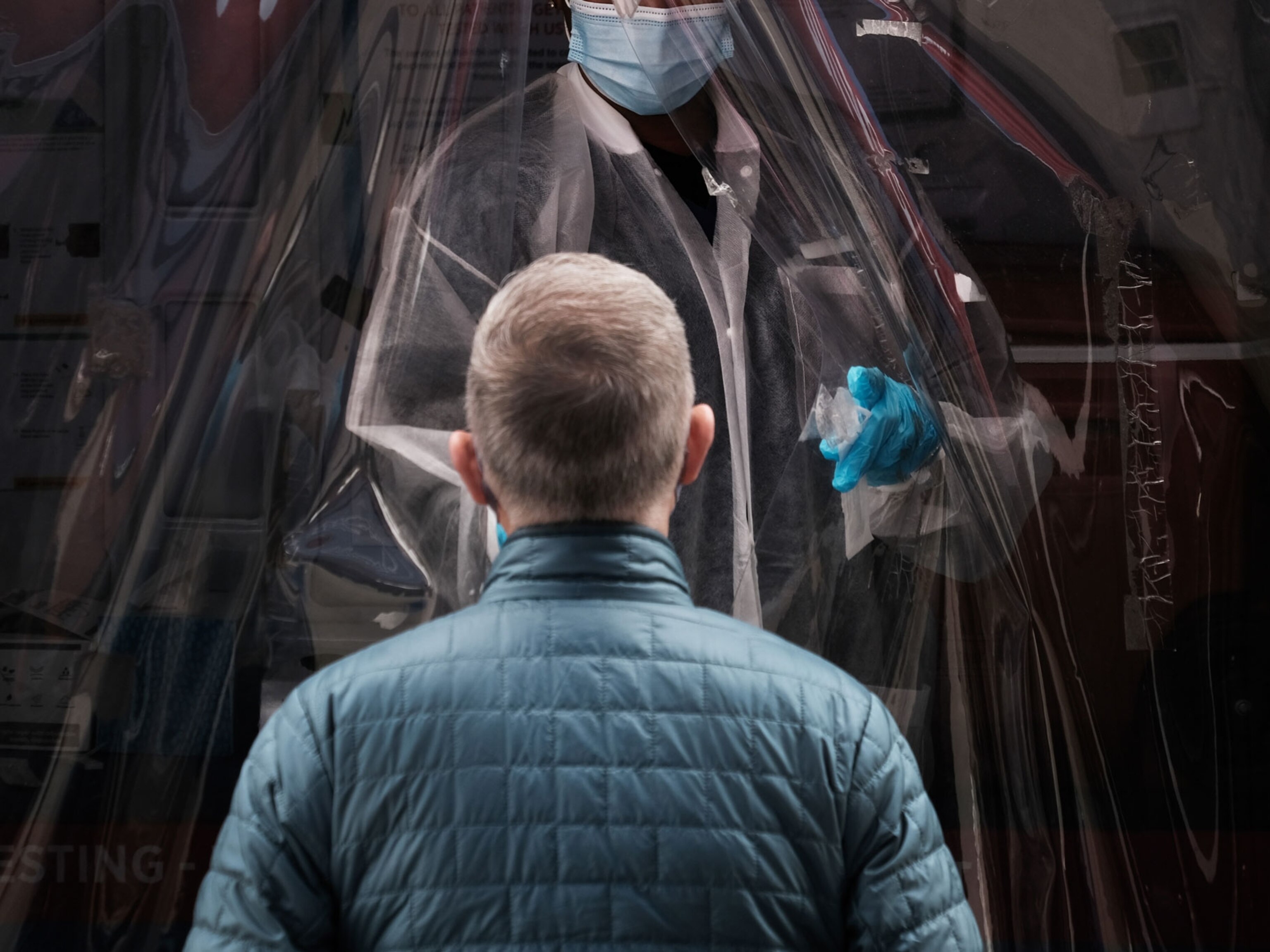
A security member keeps watch outside the Wuhan Institute of Virology.
Thomas Peter Alamy
Debate over the idea that the SARS-CoV-2 coronavirus emerged from a laboratory has escalated over the past few weeks, coinciding with the annual World Health Assembly, at which the World Health Organization (WHO) and officials from nearly 200 countries discussed the COVID-19 pandemic. After last year’s assembly, the WHO agreed to sponsor the first phase of an investigation into the pandemic’s origins, which took place in China in early 2021 .
Most scientists say SARS-CoV-2 probably has a natural origin, and was transmitted from an animal to humans. However, a lab leak has not been ruled out, and many are calling for a deeper investigation into the hypothesis that the virus emerged from the Wuhan Institute of Virology (WIV), located in the Chinese city where the first COVID-19 cases were reported. On 26 May, US President Joe Biden tasked the US Intelligence Community to join efforts to find SARS-CoV-2’s origins, whatever they might be, and report back in 90 days.
Australia, the European Union and Japan have also called for a robust investigation into SARS-CoV-2’s origins in China. The WHO has yet to reveal the next phase of its investigation. But China has asked that the probe examine other countries. Such reticence, and the fact that China has withheld information in the past, has fuelled suspicions of a ‘lab leak’. For instance, Chinese government officials suppressed crucial public-health data at the start of the COVID-19 pandemic, and during the 2002–04 severe acute respiratory syndrome (SARS) epidemic, according to high-level reports.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
At the assembly, Mike Ryan, director of health emergencies at the WHO, asked for less politicization of calls for an origin investigation , which have, in many ways, devolved into accusations. “Over the last number of days, we have seen more and more and more discourse in the media, with terribly little actual news, or evidence, or new material,” said Ryan. “This is disturbing.”
Nature looks at the key arguments that support a lab leak, and the extent to which research has answers.
There’s not yet any substantial evidence for a lab leak. Why are scientists still considering it?
Scientists don’t have enough evidence about the origins of SARS-CoV-2 to rule out the lab-leak hypothesis, or to prove the alternative — that the virus has a natural origin. Many infectious-disease researchers agree that the most probable scenario is that the virus evolved naturally and spread from a bat either directly to a person or through an intermediate animal. Most emerging infectious diseases begin with a spillover from nature, as was seen with HIV, influenza epidemics, Ebola outbreaks and the coronaviruses that caused the SARS epidemic beginning in 2002 and the Middle East respiratory syndrome (MERS) outbreak beginning in 2012.
Researchers have some leads that support a natural origin. Bats are known carriers of coronaviruses, and scientists have determined that the genome of SARS-CoV-2 is most similar to that of RATG13, a coronavirus that was first found in a horseshoe bat ( Rhinolophus affinis ) in the southern Chinese province of Yunnan in 2013. But RATG13’s genome is only 96% identical to SARS-CoV-2’s, suggesting that a closer relative of the virus—the one passed to humans—remains unknown.
Still, the possibility remains that SARS-CoV-2 escaped from a lab. Although lab leaks have never caused an epidemic, they have resulted in small outbreaks involving well-documented viruses. A relevant example happened in 2004, when two researchers were independently infected by the virus that causes SARS at a virology lab in Beijing that studied the disease. They spread the infection to seven others before the outbreak was contained.
What are the key arguments for a lab leak?
In theory, COVID-19 could have come from a lab in a few ways. Researchers might have collected SARS-CoV-2 from an animal and maintained it in their lab to study, or they might have created it by engineering coronavirus genomes. In these scenarios, a person in the lab might have then been accidentally or deliberately infected by the virus, and then spread it to others—sparking the pandemic. There is currently no clear evidence to back these scenarios, but they aren’t impossible.
People have made a number of arguments for a lab origin for SARS-CoV-2 that are currently conjecture.
One holds that it’s suspicious that, almost a year and a half into the pandemic, SARS-CoV-2’s closest relative still hasn’t been found in an animal. Another suggests it is no coincidence that COVID-19 was first detected in Wuhan, where a top lab studying coronaviruses, the WIV, is located.
Some lab-leak proponents contend that the virus contains unusual features and genetic sequences signalling that it was engineered by humans. And some say that SARS-CoV-2 spreads among people so readily that it must have been created with that intention. Another argument suggests that SARS-CoV-2 might have derived from coronaviruses found in an unused mine where WIV researchers collected samples from bats between 2012 and 2015.
So what do infectious disease researchers and evolutionary biologists say about these arguments?
Is it suspicious that no animal has been identified as transmitting the virus to humans?
Outbreak-origin investigations often take years, and some culprits remain unknown. It took 14 years to nail down the origin of the SARS epidemic, which began with a virus in bats that spread to humans, most likely through civets . To date, a complete Ebola virus has never been isolated from an animal in the region where the world’s largest outbreak occurred between 2013 and 2016.
Origin investigations are complicated because outbreaks among animals that aren't the main hosts of a particular virus, such as civets in the case of SARS, are often sporadic. Researchers must find the right animal before it dies or clears the infection. And, even if the animal tests positive, viruses found in saliva, faeces or blood are often degraded, making it difficult to sequence the pathogen’s whole genome.
Scientists have made some progress since the pandemic began, however. For example, a report, posted to the preprint server bioRxiv on 27 May, suggests that RmYN02, a coronavirus in bats in southern China, might be more closely related to SARS-CoV-2 than RATG13 is.
As for finding an intermediate host animal, researchers in China have tested more than 80,000 wild and domesticated animals; none have been positive for SARS-CoV-2. But this number is a tiny fraction of the animals in the country. To narrow the search down, researchers say, more strategic testing is needed to isolate animals that are most susceptible to infection and those that come in close contact with people. They also suggest using antibody tests to identify animals that have previously been infected with the virus.
Is it suspicious that the WIV is in Wuhan?
Virology labs tend to specialize in the viruses around them, says Vincent Munster, a virologist at the Rocky Mountain Laboratories, a division of the National Institutes of Health, in Hamilton, Montana. The WIV specializes in coronaviruses because many have been found in and around China. Munster names other labs that focus on endemic viral diseases: influenza labs in Asia, haemorrhagic fever labs in Africa and dengue-fever labs in Latin America, for example. “Nine out of ten times, when there’s a new outbreak, you’ll find a lab that will be working on these kinds of viruses nearby,” says Munster.
Researchers note that a coronavirus outbreak in Wuhan isn’t surprising, because it’s a city of 11 million people in a broader region where coronaviruses have been found. It contains an airport, train stations and markets selling goods and wildlife transported there from around the region — meaning a virus could enter the city and spread rapidly.
Does the virus have features that suggest it was created in a lab?
Several researchers have looked into whether features of SARS-CoV-2 signal that it was bioengineered. One of the first teams to do so, led by Kristian Andersen, a virologist at Scripps Research in La Jolla, California, determined that this was “improbable” for a few reasons, including a lack of signatures of genetic manipulation. Since then, others have asked whether the virus’s furin cleavage site—a feature that helps it to enter cells—is evidence of engineering, because SARS-CoV-2 has these sites but its closest relatives don’t. The furin cleavage site is important because it's in the virus's spike protein, and cleavage of the protein at that site is necessary for the virus to infect cells.
But many other coronaviruses have furin cleavage sites, such as coronaviruses that cause colds. Because viruses containing the site are scattered across the coronavirus family tree, rather than confined to a group of closely related viruses, Stephen Goldstein, a virologist at the University of Utah in Salt Lake City, says the site probably evolved multiple times because it provides an evolutionary advantage. Convergent evolution—the process by which organisms that aren’t closely related independently evolve similar traits as a result of adapting to similar environments—is incredibly common.
Another feature of SARS-CoV-2 that has drawn attention is a combination of nucleotides that underlie a segment of the furin cleavage site: CGG (these encode the amino acid arginine). A Medium article that speculates on a lab origin for SARS-CoV-2 quotes David Baltimore, a Nobel laureate and professor emeritus at the California Institute of Technology in Pasadena, as saying that viruses don’t usually have that particular code for arginine, but humans often do—a “smoking gun”, hinting that researchers might have tampered with SARS-CoV-2’s genome.
Andersen says that Baltimore was incorrect about that detail, however. In SARS-CoV-2, about 3% of the nucleotides encoding arginine are CGG, he says. And he points out that around 5% of those encoding arginine in the virus that caused the original SARS epidemic are CGG, too. In an e-mail to Nature , Baltimore says Andersen could be correct that evolution produced SARS-CoV-2, but adds that “there are other possibilities and they need careful consideration, which is all I meant to be saying”.
Is it true that SARS-CoV-2 must have been engineered, because it's perfect for causing a pandemic?
Many scientists say no. Just because the virus spreads among humans doesn't mean it was designed to do so. It also flourishes among mink and infects a host of carnivorous mammals . And it wasn’t optimally transmissible among humans for the better part of last year. Rather, new, more efficient variants have evolved around the world. To name one example, the highly transmissible variant of SARS-CoV-2 first reported in India (B.1.617.2, or Delta) has mutations in the nucleotides encoding its furin cleavage site that appear to make the virus better at infecting cells.
“This was not some supremely adapted pathogen,” says Joel Wertheim, a molecular epidemiologist at the University of California San Diego.
Did researchers collect SARS-CoV-2 from a mine?
Researchers from the WIV collected hundreds of samples from bats roosting in a mine between 2012 and 2015, after several miners working there had gotten sick with an unknown respiratory disease. (Last year, researchers reported that blood samples taken from the miners tested negative for antibodies against SARS-CoV-2, meaning that the sickness was probably not COVID-19.) Back at the lab, WIV researchers detected nearly 300 coronaviruses in the bat samples, but they were able to get whole or partial genomic sequences from fewer than a dozen , and none of those that were reported were SARS-CoV-2. During the WHO-led origins probe earlier this year, WIV researchers told investigators that they cultured only three coronaviruses at the lab, and none were closely related to SARS-CoV-2.
Although the investigators didn’t sift through freezers at the WIV to confirm this information, the low number of genomes and cultures doesn’t surprise virologists. Munster says it’s exceedingly difficult to extract intact coronaviruses from bat samples. Virus levels tend to be low in the animals, and viruses are often degraded in faeces, saliva and droplets of blood. Additionally, when researchers want to study or genetically alter viruses, they need to keep them (or synthetic mimics of them) alive, by finding the appropriate live animal cells for the viruses to inhabit in the lab, which can be a challenge.
So, for SARS-CoV-2 to have come from this mine in China, WIV researchers would have had to overcome some serious technical challenges—and they would have kept the information secret for a number of years and misled investigators on the WHO-led mission, scientists point out. There's no evidence of this, but it can't be ruled out.
What’s next for lab-leak investigations?
Biden asked the US Intelligence Community to report back to him in 90 days. Perhaps this investigation will shed light on undisclosed US intel reported by The Wall Street Journal suggesting that three staff members at the WIV were sick in November 2019, before the first cases of COVID-19 were reported in China. The article claims that US officials have different opinions on the quality of that intel. And researchers at the WIV have maintained that staff at the institute tested negative for antibodies that would indicate SARS-CoV-2 infection prior to January 2020.
Last week, Anthony Fauci, Biden’s chief medical adviser, asked Chinese officials to release the hospital records of WIV staff members. Others have asked for blood samples from WIV staff members, and access to WIV bat and virus samples, laboratory notebooks and hard drives. But it’s unclear what such asks will yield because China has not conceded to demands for a full lab investigation. A spokesperson for the Ministry of Foreign Affairs of the People's Republic of China, Zhao Lijian, said that US labs should instead be investigated, and that some people in the United States “don't care about facts or truth and have zero interest in a serious science-based study of origins”.
As Biden's investigation commences and the WHO considers the next phase in its origin study, pandemic experts are bracing themselves for a long road ahead. “We want an answer,” says Jason Kindrachuk, a virologist at the University of Manitoba in Winnipeg, Canada. “But we may have to keep piecing bits of evidence together as weeks and months and years move forward.”
This article is reproduced with permission and was first published on June 8 2021.

- CORONAVIRUS COVERAGE
What you need to know about the COVID-19 lab-leak hypothesis
Newly reported information has revived scrutiny of this possible origin for the coronavirus, which experts still call unlikely though worth investigating.
Months after a World Health Organization investigation deemed it “extremely unlikely” that the novel coronavirus escaped accidentally from a laboratory in Wuhan, China, the idea is back in the news, giving new momentum to a hypothesis that many scientists believe is unlikely, and some have dismissed as a conspiracy theory .
The renewed attention comes on the heels of President Joe Biden’s ordering U.S. intelligence agencies on May 26 to “ redouble their efforts ” to investigate the origins of the coronavirus. On May 11, Biden’s chief medical adviser, Anthony Fauci, acknowledged he’s now “ not convinced ” the virus developed naturally—an apparent pivot from what he told National Geographic in an interview last year.
Also last month, more than a dozen scientists—top epidemiologists, immunologists, and biologists—wrote a letter published in the journal Science calling for a thorough investigation into two viable origin stories: natural spillover from animal to human, or an accident in which a wild laboratory sample containing SARS-CoV-2 was accidentally released. They urged that both hypotheses “be taken seriously until we have sufficient data,” writing that a proper investigation would be “transparent, objective, data-driven, inclusive of broad expertise, subject to independent oversight,” with conflicts of interest minimized, if possible.
“Anytime there is an infectious disease outbreak it is important to investigate its origin,” says Amesh Adalja, an infectious disease physician and senior scholar at the Johns Hopkins University Center for Health Security who did not contribute to the letter in Science . “The lab-leak hypothesis is possible—as is an animal spillover,” he says, “and I think that a thorough, independent investigation of its origins should be conducted.”
Unanswered questions
The origins of SARS-CoV-2, the virus that causes COVID-19 and has infected more than 171 million people, killing close to 3.7 million worldwide as of June 4, remain unclear. Many scientists, including those that participated in the WHO’s months-long investigation, believe the most likely explanation is that that it jumped from an animal to a person—potentially from a bat directly to a human, or through an intermediate host. Animal-to-human transmission is a common route for many viruses; at least two other coronaviruses, SARS and MERS , were spread through such zoonotic spillover.
Other scientists insist it’s worth investigating whether SARS-CoV-2 escaped from the Wuhan Institute of Virology, a laboratory that has studied coronaviruses in bats for more than a decade.
For Hungry Minds
The WHO investigation —a joint effort between WHO-appointed scientists and Chinese officials—concluded it was “extremely unlikely” the highly transmissible virus escaped from a laboratory. But the WHO team suffered roadblocks that led some to question its conclusions; the scientists were not permitted to conduct an independent investigation and were denied access to any raw data. ( We still don’t know the origins of the coronavirus. Here are 4 scenarios .)
On March 30, when the WHO released its report, its director-general, Tedros Adhanom Ghebreyesus, called for further studies . “All hypotheses remain on the table,” he said at the time.
Then on May 11, Fauci told PolitiFact that while the virus most likely emerged via animal-to-human transmission, “it could have been something else, and we need to find that out.”
Recently disclosed evidence, first reported by the Wall Street Journal , has added fuel to the fire: Three researchers from the Wuhan Institute of Virology fell sick in November 2019 and sought hospital care, according to a U.S. intelligence report. In the final days of the Trump administration, the State Department released a statement that researchers at the institute had become ill with “symptoms consistent with both COVID-19 and common seasonal illness.”
You May Also Like

What is white lung syndrome? Here's what to know about pneumonia

COVID-19 is more widespread in animals than we thought

A deer may have passed COVID-19 to a person, study suggests
Most epidemiologists and virologists who have studied the novel coronavirus believe that it began spreading in November 2019. China says the first confirmed case was on December 8, 2019. During a briefing in Beijing this week, China’s foreign ministry spokesperson, Zhao Lijian, accused the U.S. of “ hyping up the theory of a lab leak ,” and asked, “does it really care about the study of origin tracing, or is it trying to divert attention?” Zhao also denied the Wall Street Journal report that three people had gotten sick.
Lab leak still ‘unlikely’
Some conservative politicians and commentators have embraced the lab-leak theory, while liberals more readily rejected it, especially early in the pandemic. The speculation has also heightened ongoing tensions between the U.S. and China.
On May 26, as the U.S. Senate passed a bill to declassify intelligence related to potential links between the Wuhan laboratory and COVID-19, Missouri Senator Josh Hawley, a Republican who sponsored the bill, said, “the world needs to know if this pandemic was the product of negligence at the Wuhan lab,” and lamented that “for over a year, anyone asking questions about the Wuhan Institute of Virology has been branded as a conspiracy theorist.”
Peter Navarro, Donald Trump’s former trade adviser, asserted in April 2020 that SARS-CoV-2 could have been engineered as a bioweapon, without citing any evidence.
The theory that SARS-CoV-2 was created as a bioweapon is “completely unlikely,” says William Schaffner, a professor of infectious diseases at Vanderbilt University Medical Center. For one thing, he explains, for a bioweapon to be successful, it must target an adversarial population without affecting one’s own. In contrast, SARS-CoV-2 “cannot be controlled,” he says. “It will spread, including back on your own population,” making it an extremely “counterproductive biowarfare agent.”
The more plausible lab-leak hypothesis, scientists say, is that the Wuhan laboratory isolated the novel coronavirus from an animal and was studying it when it accidentally escaped. “Not knowing the extent of its virulence and transmissibility, a lack of protective measures [could have] resulted in laboratory workers becoming infected,” initiating the transmission chain that ultimately resulted in the pandemic, says Rossi Hassad, an epidemiologist at Mercy College.
But Hassad adds he believes that this lab-leak theory is on the “extreme low end” of possibilities, and it “will quite likely remain only theoretical following any proper scientific investigation,” he says.
Biden ordered U.S. intelligence agencies to report back with their findings in 90 days, which would be August 26.
Based on the available information, Eyal Oren, an epidemiologist at San Diego State University, says it’s apparent why the most accepted hypothesis is that this virus originated in an animal and jumped to a human: “What is clear is that the genetic sequence of the COVID-19 virus is similar to other coronaviruses found in bats,” he says.
Some scientists remain skeptical that concrete conclusions can be drawn. “At the end, I anticipate that the question” of SARS-CoV-2’s origins “will remain unresolved,” Schaffner says.
In the meantime, science “moves much more slowly than the media and news cycles,” Oren says.
Related Topics
- CORONAVIRUS
- PUBLIC HEALTH
- WILDLIFE WATCHING

Seeking the Source of Ebola

5 things to know about COVID-19 tests in the age of Omicron
Here's what we know about the BA.2 Omicron subvariant driving a new COVID-19 wave

Humans are creating hot spots where bats could transmit zoonotic diseases

Hippos, hyenas, and other animals are contracting COVID-19
- Environment
- Perpetual Planet
History & Culture
- History & Culture
- History Magazine
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
- Ideas for Action
- Join the MAHB
- Why Join the MAHB?
- Current Associates
- Current Nodes
- What is the MAHB?
- Who is the MAHB?
- Acknowledgments

Hypothesis: The COVID-19 Pandemic is Signaling Humanity’s Global Overshoot
| February 8, 2022 | Leave a Comment

Image by Alex Borland / publicdomainpictures
Item Link: Access the Resource
File: Download
Date of Publication: April
Year of Publication: 2021
Publication City: San Francisco, CA
Publisher: Academia Inc.
Author(s): Alexander K. Lautensach, Sabina W. Lautensach
Journal: Academia Letters
Volume: Article 538
In the Anthropocene, the year 2020 marks a milestone in humanity’s learning process about how we are affecting the biosphere and how it affects us in return (Ulrich 2020). The COVID-19 pandemic is the first global event that changed every human life, if not yet actually then certainly potentially. For the first time, humanity experiences species-wide a planetary phenomenon that allows neither escape nor denial and that demands a collective response from all cultures and societies. That raises the question how this phenomenon is to be interpreted.
HYPOTHESIS:
The COVID-19 pandemic is a feedback signal from the biosphere that denotes the ecological overshoot of the human species (currently estimated at about 1.7 planets; GFN 2020). That means that efforts to control this pandemic, even if successful, will not solve the wider problem of overshoot and the prospect of further, more threatening signals or ‘transition events’ (including partial collapse) for as long as overshoot persists.
Read the full paper here or download it from the link above.
A nicotinic hypothesis for Covid-19 with preventive and therapeutic implications
Affiliations.
- 1 Institut Pasteur CNRS UMR 3571 Department of Neuroscience and Collège de France, Paris France.
- 2 Sorbonne Université, Inserm UMRS, Centre d'Immunologie et des Maladies Infectieuses (CIMI-Paris).
- 3 Assistance Publique-Hôpitaux de Paris, Groupement Hospitalier Pitié-Salpêtrière, Service de Médecine Interne 2, Maladies auto-immune et systémiques Institut E3M.
- 4 Institut Pasteur, Structural Virology Unit, Department of Virology, CNRS UMR 3569, Institut Pasteur Paris France.
- 5 Assistance Publique-Hôpitaux de Paris, Groupement Hospitalier Pitié-Salpêtrière, Département d'Immunologie, Paris, France.
- PMID: 32720486
- DOI: 10.5802/crbiol.8
Abstract in English, French
SARS-CoV-2 epidemics raises a considerable issue of public health at the planetary scale. There is a pressing urgency to find treatments based upon currently available scientific knowledge. Therefore, we tentatively propose a hypothesis which hopefully might ultimately help save lives. Based on the current scientific literature and on new epidemiological data which reveal that current smoking status appears to be a protective factor against the infection by SARS-CoV-2 [1], we hypothesize that the nicotinic acetylcholine receptor (nAChR) plays a key role in the pathophysiology of Covid-19 infection and might represent a target for the prevention and control of Covid-19 infection.
L’épidémie de SARS-Cov-2 pose un problème considérable de santé publique à l’échelle planétaire. Il y a urgence extrême de découvrir des traitements qui se fondent sur les connaissances scientifiques disponibles. Nous proposons donc une hypothèse plausible mais provisoire qui puisse le moment venu contribuer à sauver des vies. Elle se fonde sur la littérature scientifique disponible et sur des données épidémiologiques nouvelles qui révèlent que le statut de fumeur parait être un facteur de protection contre l’infection par SARS-Cov-2 [1]. Nous proposons l’hypothèse que le récepteur nicotinique de l’acétylcholine (nAChR) joue un rôle critique dans la pathophysiologie de l’infection Covid-19 et puisse représenter une cible pour la prévention et le contrôle de l’infection.
Keywords: Covid-19; clinical trials of nicotine patches; nicotinic receptors; smoking.
Publication types
- Coronavirus Infections / physiopathology*
- Coronavirus Infections / prevention & control
- Coronavirus Infections / therapy*
- Nicotine / therapeutic use*
- Nicotinic Agonists / therapeutic use*
- Pandemics / prevention & control
- Pneumonia, Viral / physiopathology*
- Pneumonia, Viral / prevention & control
- Pneumonia, Viral / therapy*
- Receptors, Nicotinic*
- Transdermal Patch
- Nicotinic Agonists
- Receptors, Nicotinic
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Supplements
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 5, Issue 6
- Hypothesis to explain the severe form of COVID-19 in Northern Italy
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-6285-7355 Luca Cegolon 1 , 2 ,
- Jennifer Pichierri 3 ,
- Giuseppe Mastrangelo 4 ,
- Sandro Cinquetti 1 ,
- Giovanni Sotgiu 5 ,
- Saverio Bellizzi 6 ,
- Giuseppe Pichierri 7
- 1 Public Health Department , Local Health Unit N. 2 "Marca Trevigiana" , Treviso , Veneto Region , Italy
- 2 IRCCS Materno Infantile Burlo Garofolo , Trieste , Friuli-Venezia Giulia Region , Italy
- 3 Children and Young People’s Diabetes , University College London Hospitals NHS Foundation Trust , London , UK
- 4 Cardiac, Thoracic and Vascular Sciences , Padua University Hospital , Padua , Veneto Region , Italy
- 5 Department of Medical, Surgical and Experimental Sciences , University of Sassari , Sassari , Sardinia Region , Italy
- 6 Partnership for Maternal, Newborn and Child Health , World Health Organization , Geneve , Switzerland
- 7 Microbiology Department , Kingston Hospital NHS Foundation Trust , Kingston upon Thames , London , UK
- Correspondence to Dr Luca Cegolon; l.cegolon{at}gmail.com
https://doi.org/10.1136/bmjgh-2020-002564
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- public health
- prevention strategies
- epidemiology
Summary box
What is already known about this subject.
Human coronaviruses are known to cause respiratory re-infections, regardless of pre-existing humoural immunity.
There is evidence suggesting that severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) had been circulating in Italy before the first COVID-19 case was detected in the country.
What are the new findings?
Prior infections with SARS-CoV-2 (or other viruses/coronaviruses) may arguably predispose to more severe forms of the disease following re-infection with SARS-CoV-2, with an immunological mechanism known as Antibody-Dependent-Enhancement, already observed with infections sustained by other coronaviruses (MERS-CoV and SARS-CoV) or other viruses such as the West Nile Virus and Dengue.
What are the recommendations for policy and practice?
If confirmed by in vivo studies, this hypothesis may have relevant implications for the treatment of severe forms of COVID-19, yet the possibility to produce an effective vaccine against SARS-CoV-2 might be hampered.
The ongoing COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), has affected 212 countries worldwide at various degrees as of 8 May 2020. 1
In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or potentially even other respiratory viruses—may predispose to more severe forms of COVID-19, following a secondary infection with SARS-CoV-2.
Most COVID-19 infections are asymptomatic or manifest with mild to moderate respiratory symptoms (fever, cough, sore throat, myalgia, fatigue and even non-severe pneumonia). Of patients with COVID-19, 14%–15% develop severe pneumonia and 5%–6% a critical condition requiring admission to intensive care unit (ICU). 2–4 Death may eventually occur after an average of 17.8 days since the onset of symptoms. 5
Among all countries, Italy (which was the first European COVID-19 cluster) presents a critical disease pattern as of 8 May 2020, having the third highest number of COVID-19 cases in the world after the USA and Spain, the fourth highest prevalence of the disease after Spain, Belgium and the USA, the third highest total number of deaths attributed to COVID-19 after the USA and the UK, and the third highest prevalence of COVID-19 mortality after Belgium and Spain, despite a current 1% rate of severe/critical disease among active cases, which has been progressively decreasing over time. 1
The cross-country discrepancies in the burden of COVID-19 observed so far across the globe cannot be explained only by differences in population age structures. 6–8 In fact, Japan has a population double that of Italy, with the proportion of subjects older than 65 being 28.8% in Japan vs 21.7% in Italy. 9 10 Nonetheless, as of 8 May 2020, the difference in COVID-19 prevalence between Japan (122 per million) and Italy (3570 per million) is massive. 1 Likewise, in Germany the percentage of individuals >65 is reportedly 22.1% (hence slightly higher than Italy), but the prevalence of COVID-19 is currently 2022 per million. 1 11 In Iran the proportion of people >65 is 5.5% (hence much younger than the Italian, German and Japanese populations), but the prevalence of COVID-19 is 1246 per million, as of 8 May 2020. 1 12
The mortality rate for COVID-19 is reportedly enhanced by 5.6%–10.5% in the presence of any comorbidities (hypertension, diabetes, cardiovascular diseases, cancer and/or chronic respiratory conditions) and becomes significantly and progressively higher after 50 years of age, 4 6 although the severe form of the disease increases linearly at any age stage. 5 Cold dry weather is a recognised risk factor for respiratory infections, rendering viruses as influenza more stable and individuals more susceptible. 13 14 This applies also to SARS-CoV-2, the viability and transmissibility of which reportedly reduce with hot and humid weather conditions. 14 Moreover, unfavourable disease progression and clinical outcomes of COVID-19 were found to be associated with cigarette smoking in a systematic review. 15
A number of factors may have contributed to enhancing the risk of infection with SARS-CoV-2 in Northern Italy. The age by which half of all young people leave parental home is higher in Italy than other European Union countries, 16 and such multigenerational cohabitation probably contributed to increase COVID-19 contagion among elderly individuals. The universal use of face masks was initially discouraged in Italy in order to preserve the limited supplies of personal protective equipment for professional use in healthcare settings; another argument initially was that face masks are ineffective in protecting against coronavirus infections. 17 Further major findings of the relevant literature have been summarised in figure 1 . An extraordinary elevated incidence of COVID-19 could have been the result of a perfect storm triggered by multiple interplaying factors. The affected areas in Northern Italy (regions of Lombardy, Emilia-Romagna, Piedmont and Veneto) are characterised by high population density 18 and recognised air pollution, 19 20 especially from fine particulate matter (PM2.5), which was found to increase the risk of death from COVID-19 in the USA. 21 Northern Italy includes several cities which, similarly to Philadelphia (USA) during the Spanish flu pandemic in 1918, 22 are historically important and densely populated, where social gatherings as well as business activities are certainly fundamental—the latter being vital to the economy of the entire country. These cultural and social dynamics might have influenced the initial resistance and reluctance of the general population to comply with the social restrictions progressively enforced by the Italian government (until full lockdown was established on 21 March). Moreover, the intense case finding in Italy was preceded by an initial overall underestimation of the COVID-19 threat by the Italian government and subsequently by the general population, who perceived the disease as just some sort of influenza, despite worrying news from the first affected country (China). 23 Thereafter SARS-CoV-2 was also going to spread to other European countries, which have also now been heavily affected by the disease. 1
- Download figure
- Open in new tab
- Download powerpoint
Conceptual framework explaining the relationships between various factors and incidence and severe/critical form of COVID-19. Established items: orange boxes; hypothetical items: blue boxes. ADE, antibody-dependent enhancement; ARDS, acute respiratory distress syndrome; COVID-19, coronavirus infectious disease 2019; IPC, infection prevention and control; SARS-CoV-2, severe acute respiratory syndrome coronavirus type.
The epidemiological investigations conducted by the Italian National Institute of Health ( Istituto Superiore di Sanità ) suggest that the vast majority of cases but the first three acquired the infection in Italy. It can therefore be reasonably argued that SARS-CoV-2 had been circulating in the country—especially in Lombardy, Emilia-Romagna, Piedmont and Veneto regions—for weeks before the first patient was found. 24 Human coronaviruses are known to cause respiratory reinfections regardless of pre-existing humoural immunity, both at the individual and community level. 25 At the same time, presumed hospital-associated transmission of SARS-CoV-2 has been reported since the initial stages of the COVID-19 outbreak in Wuhan (China) in 41% of the total number of patients, 70% of whom were healthcare staff. 26 This could have also occurred in Italy, where healthcare workers reportedly make up 9% out of all COVID-19 cases. 27 We therefore hypothesise (see blue boxes in figure 1 ) that repeated cycles of infection within a community (especially in older adults)—or even more worryingly in a healthcare setting—could have the potential to cause more severe forms of COVID-19, with acute respiratory distress syndrome (ARDS), the fundamental pathophysiology of severe viral pneumonia due to COVID-19, requiring admission to ICU. 28 ARDS associated with COVID-19 shares clinical features with the critical form of the 2003 severe acute respiratory syndrome coronavirus (SARS-CoV) epidemic, in particular lymphopaenia, massive infiltration of phagocytes and inflammation sustained by cytokines. 4 8 29
A plausible mechanistic hypothesis could be the antibody-dependent enhancement (ADE), sustained by prior exposure to SARS-CoV-2 or other viruses/coronaviruses. 8 Previous circulation and exposure to other coronaviruses similar to SARS-CoV-2 causing mild/asymptomatic cold-like symptoms shall in fact not be ruled out. 8 Binding and neutralising antibody response against other types of human coronaviruses was recently reported to increase with age in adult patients, 25 and this may explain the increased linear risk of severe COVID-19 with age, with death being significantly higher in patients older than 50. 5
Non-neutralising, subneutralising or even fully neutralising antibodies may play a key role in ADE. 30 Wan et al 30 have recently described a molecular mechanism for ADE involving the Middle East respiratory syndrome coronavirus (MERS-CoV), similar to what is already known for SARS-CoV and flaviviruses as Dengue and the West Nile virus. 31–35 While the entry of SARS-CoV into the phagocytes occurred principally through the human ACE2 receptor, the ADE mechanism was shown to be enhanced by antibodies specific for the spike (S) envelope glycoprotein binding with the macrophage receptor and subsequent enhancement of target cell infections. 33–35 Likewise, the antibody/opsonised SARS-CoV-2 particles may bind avidly with the IgFc receptors of target cells, increasing the virus yield as well as the production of cytokines. This may also explain the higher risk of thromboembolism reportedly associated with severe/critical COVID-19. 4 36 37
Anecdotal clinical reports of ‘biphasic infection’ and ‘cytokine storm’ seem to possibly point towards this direction, biphasic infection simply being the immunological result of a secondary infection by other coronaviruses or a reinfection due to SARS-CoV-2. 38–41 An early elevation of serum proinflammatory cytokines, suggesting a pathological mechanism mediated by cytokine storm, has been observed with both severe forms of SARS-CoV and MERS-CoV infections. The latter two viruses share a genomic similarity of about 79% and 50% with SARS-CoV-2, respectively. 41 42 Several Rhinolophus bats-related coronavirus strains have been found to share even higher sequence homology with SARS-CoV-2. 33 An abnormal humoural response due to ADE, in the early stages of a secondary infection by SARS-CoV-2, may delay the innate antiviral immune response relying on the production of type 1 interferon (IFN-1). This would compromise the initial antiviral response of the host, with subsequent elevated influx of proinflammatory cytokines, hyperinflammatory neutrophils and monocytes-macrophages and hypercoagulable state accountable for ARDS and typical pneumonia observed in patients affected by severe/critical COVID-19 ( figure 1 ). 4 41 43 44
If confirmed, this hypothesis would have relevant implications for the treatment of COVID-19 and the development of an effective vaccine. The licensing of a vaccine against human coronaviruses has failed thus far, partly because immunised individuals could potentially be at higher risk of ADE sustained by facilitated uptake of viral antigen-antibody complexes by target cells. 4 31 33 44 The approval of a vaccine against SARS-CoV-2 may encounter similar obstacles. Likewise, herd immunity would not be a possibility with COVID-19. WHO recommends passive immunotherapy when vaccine and antivirals are not available for emerging infections. 45 In a preliminary uncontrolled case study on five critically ill patients with COVID-19 who developed ARDS, the administration of convalescent plasma—drawn from five patients who recovered from COVID-19 and containing SARS-CoV-2-specific neutralising antibodies (IgG)—between 10 and 22 days since admission significantly improved the clinical status of all, resolving ARDS in four of them within 12 days since transfusion. 46 On the other hand, the treatment of severe COVID-19 may also benefit from monoclonal antibodies targeting proinflammatory cytokines 4 as well as supplements of IFN-1 in combination with other antiviral drugs. 47–50
Whether secondary infections from other coronaviruses or repeated community reinfections of SARS-CoV-2 may account for more severe presentations of COVID-19 observed in some countries compared with others, 8 and whether it is only a matter of time for the virus to circulate and infect a significant proportion of the population before causing reinfections and therefore more severe clinical features, are something which will require more indepth epidemiological and immunological/serological investigations. A better understanding of any underlying immunological mechanism or any additional risk factor which could explain cross-country differences in the rates of severe disease and mortality attributable to COVID-19 will help to guide international public health responses during this ongoing pandemic. It will be important to clarify if the ARDS mechanism responsible for the severe respiratory infection could potentially be attributable to ADE.
Two different in vivo strategies could be employed to endorse this hypothesis.
First (observational design), all healthcare workers and blood donors should undergo serum test for COVID-19. Individuals presenting SARS-CoV-2 IgG antibodies should be included in a local/regional/national ad-hoc register and monitored over time for the possible development of severe disease sustained by ADE, which would need to be confirmed by blood count, dosage of IFN and proinflammatory cytokines, in addition to chest CT scan. The risk of developing severe COVID-19 should be estimated and stratified by relevant risk factors, including baseline serum level of SARS-CoV-2-specific IgG antibodies, age, sex, potential occupational exposure, medical history (particularly previous infections and vaccination status), any comorbidities, area of residence and health status of household members, among others.
Second (experimental laboratory design), animal models (hamsters, rodents, palm civets, monkeys, ferrets) 33 51 52 could be infected by SARS-CoV-2 (or other viruses/coronaviruses) and subsequently re-exposed to SARS-CoV-2 to verify the possibility of onset of ARDS sustained by ADE.
- Worldometers
- World Health Organization
- Chan JF-W ,
- Kok K-H , et al
- Dorigatti I , et al
- Index Mundi
- Feng K , et al
- Vardavas CI ,
- Iacovou M ,
- Xia N , et al
- Office for National Statistics (ISTAT)
- Ghermandi G ,
- Harrison RM
- Liang S , et al
- Nethery RC ,
- Sabath BM , et al
- Hannigan T ,
- Steele C , et al
- Start Magazine
- National Institute of Health (ISS)
- Donovan MM ,
- Hu C , et al
- International Council of Nurses
- Xu J , et al
- Cheung CY ,
- Ng IHY , et al
- Sun S , et al
- Gollins SW ,
- Porterfield JS
- Urbina AN ,
- Chang MR , et al
- Yang Z-yong ,
- Werner HC ,
- Kong W-pui , et al
- Tseng S-P ,
- Yen C-H , et al
- Tirado SMC ,
- Zhao L , et al
- Thachil J ,
- Iba T , et al
- McAuley DF ,
- Brown M , et al
- Mahallawi WH ,
- Khabour OF ,
- Zhang Q , et al
- Wu AKL , et al
- Prompetchara E ,
- Li J , et al
- Pedersen SF ,
- Corapi WV ,
- Ngichabe CK , et al
- Zhao F , et al
- Sallard E ,
- Lescure F-X ,
- Yazdanpanah Y , et al
- Chen Q , et al
- Loutfy MR ,
- Siminovitch KA , et al
- Omrani AS ,
- Baig K , et al
- Cheung CY , et al
- Roberts A , et al
Handling editor Seye Abimbola
Contributors LC, JP, SB, GP and GM equally contributed to conceiving the idea and drafting the manuscript. SC and GS contributed to drafting the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement There are no data in this work.
Read the full text or download the PDF:

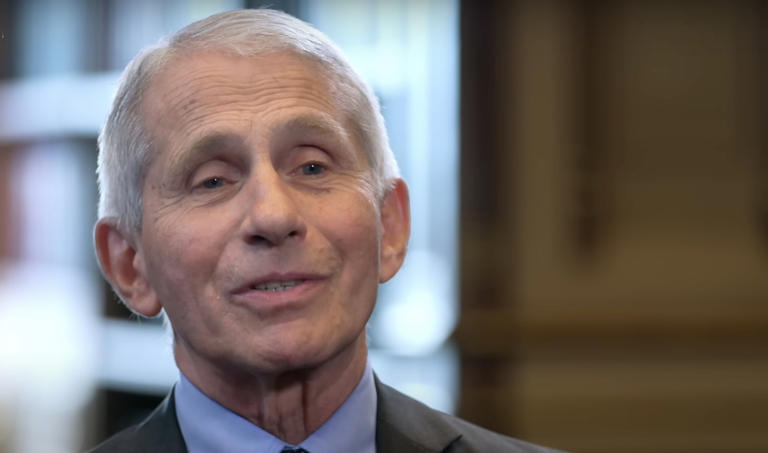
Fauci Makes Huge Admissions On Vaccine Mandates And Lab Leak Theory Legitimacy
D r. Anthony Fauci faced intense questioning from the House Select Subcommittee on the Coronavirus Pandemic, where he admitted that the six-foot social distancing rule had little scientific basis.
He also acknowledged that the lab-leak hypothesis is not a conspiracy theory and that vaccine mandates might increase hesitancy.
Despite supporting travel restrictions from China, Fauci was accused of playing down the lab-leak theory. (Trending: Clintons Scramble To Delete Embarrassing Photo, But Were Too Slow)
“It just sort of appeared,” wrote the committee, mocking Fauci with his own quote.
“Dr. Fauci acknowledged that the lab-leak hypothesis is not a conspiracy theory,” their statement continued.
“This comes nearly four years after prompting the publication of the now infamous ‘Proximal Origin’ paper that attempted to vilify and disprove the lab-leak hypothesis,” explained the committee.
The committee said Fauci still “advised American universities to impose vaccine mandates on their students.”
The committee wrote that Fauci, “played semantics with the definition of a ‘lab-leak’ in an attempt to cover up the inaccurate conclusions of ‘Proximal Origin.’”
Sen. Wenstrup said, “During his interview today, Dr. Fauci claimed that the policies and mandates he promoted may unfortunately increase vaccine hesitancy for years to come.”
“Further, the social distancing recommendations forced on Americans ‘sort of just appeared’ and were likely not based on scientific data,” he continued.
Wenstrup said the hearing “revealed systemic failures in our public health system and shed a light on serious procedural concerns with our public health authority.”
“It is clear the dissenting opinions were often not considered or suppressed completely,” lamented the lawmaker.
“Should a future pandemic arise, America’s response must be guided by scientific facts and conclusive data,” declared Wenstrup.
The committee highlighted systemic failures in public health and emphasized the need for future responses to be guided by scientific facts and conclusive data.
Most Popular:
First Moon Mission In 50 Years Blasts Off
Joe Biden Sets New Presidential Record
Fox News Star Accused Of Major Scandal
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

This article has been retracted.
Facemasks in the covid-19 era: a health hypothesis.
Many countries across the globe utilized medical and non-medical facemasks as non-pharmaceutical intervention for reducing the transmission and infectivity of coronavirus disease-2019 (COVID-19). Although, scientific evidence supporting facemasks’ efficacy is lacking, adverse physiological, psychological and health effects are established. Is has been hypothesized that facemasks have compromised safety and efficacy profile and should be avoided from use. The current article comprehensively summarizes scientific evidences with respect to wearing facemasks in the COVID-19 era, providing prosper information for public health and decisions making.
Introduction
Facemasks are part of non-pharmaceutical interventions providing some breathing barrier to the mouth and nose that have been utilized for reducing the transmission of respiratory pathogens [1] . Facemasks can be medical and non-medical, where two types of the medical masks primarily used by healthcare workers [1] , [2] . The first type is National Institute for Occupational Safety and Health (NIOSH)-certified N95 mask, a filtering face-piece respirator, and the second type is a surgical mask [1] . The designed and intended uses of N95 and surgical masks are different in the type of protection they potentially provide. The N95s are typically composed of electret filter media and seal tightly to the face of the wearer, whereas surgical masks are generally loose fitting and may or may not contain electret-filtering media. The N95s are designed to reduce the wearer’s inhalation exposure to infectious and harmful particles from the environment such as during extermination of insects. In contrast, surgical masks are designed to provide a barrier protection against splash, spittle and other body fluids to spray from the wearer (such as surgeon) to the sterile environment (patient during operation) for reducing the risk of contamination [1] .
The third type of facemasks are the non-medical cloth or fabric masks. The non-medical facemasks are made from a variety of woven and non-woven materials such as Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk. Although non-medical cloth or fabric facemasks are neither a medical device nor personal protective equipment, some standards have been developed by the French Standardization Association (AFNOR Group) to define a minimum performance for filtration and breathability capacity [2] . The current article reviews the scientific evidences with respect to safety and efficacy of wearing facemasks, describing the physiological and psychological effects and the potential long-term consequences on health.
On January 30, 2020, the World Health Organization (WHO) announced a global public health emergency of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) causing illness of coronavirus disease-2019 (COVID-19) [3] . As of October 1, 2020, worldwide 34,166,633 cases were reported and 1,018,876 have died with virus diagnosis. Interestingly, 99% of the detected cases with SARS-CoV-2 are asymptomatic or have mild condition, which contradicts with the virus name ( severe acute respiratory syndrome-coronavirus-2) [4] . Although infection fatality rate (number of death cases divided by number of reported cases) initially seems quite high 0.029 (2.9%) [4] , this overestimation related to limited number of COVID-19 tests performed which biases towards higher rates. Given the fact that asymptomatic or minimally symptomatic cases is several times higher than the number of reported cases, the case fatality rate is considerably less than 1% [5] . This was confirmed by the head of National Institute of Allergy and Infectious Diseases from US stating, “the overall clinical consequences of COVID-19 are similar to those of severe seasonal influenza” [5] , having a case fatality rate of approximately 0.1% [5] , [6] , [7] , [8] . In addition, data from hospitalized patients with COVID-19 and general public indicate that the majority of deaths were among older and chronically ill individuals, supporting the possibility that the virus may exacerbates existing conditions but rarely causes death by itself [9] , [10] . SARS-CoV-2 primarily affects respiratory system and can cause complications such as acute respiratory distress syndrome (ARDS), respiratory failure and death [3] , [9] . It is not clear however, what the scientific and clinical basis for wearing facemasks as protective strategy, given the fact that facemasks restrict breathing, causing hypoxemia and hypercapnia and increase the risk for respiratory complications, self-contamination and exacerbation of existing chronic conditions [2] , [11] , [12] , [13] , [14] .
Of note, hyperoxia or oxygen supplementation (breathing air with high partial O 2 pressures that above the sea levels) has been well established as therapeutic and curative practice for variety acute and chronic conditions including respiratory complications [11] , [15] . It fact, the current standard of care practice for treating hospitalized patients with COVID-19 is breathing 100% oxygen [16] , [17] , [18] . Although several countries mandated wearing facemask in health care settings and public areas, scientific evidences are lacking supporting their efficacy for reducing morbidity or mortality associated with infectious or viral diseases [2] , [14] , [19] . Therefore, it has been hypothesized: 1) the practice of wearing facemasks has compromised safety and efficacy profile, 2) Both medical and non-medical facemasks are ineffective to reduce human-to-human transmission and infectivity of SARS-CoV-2 and COVID-19, 3) Wearing facemasks has adverse physiological and psychological effects, 4) Long-term consequences of wearing facemasks on health are detrimental.
Evolution of hypothesis
Breathing physiology.
Breathing is one of the most important physiological functions to sustain life and health. Human body requires a continuous and adequate oxygen (O 2 ) supply to all organs and cells for normal function and survival. Breathing is also an essential process for removing metabolic byproducts [carbon dioxide (CO 2 )] occurring during cell respiration [12] , [13] . It is well established that acute significant deficit in O 2 (hypoxemia) and increased levels of CO 2 (hypercapnia) even for few minutes can be severely harmful and lethal, while chronic hypoxemia and hypercapnia cause health deterioration, exacerbation of existing conditions, morbidity and ultimately mortality [11] , [20] , [21] , [22] . Emergency medicine demonstrates that 5–6 min of severe hypoxemia during cardiac arrest will cause brain death with extremely poor survival rates [20] , [21] , [22] , [23] . On the other hand, chronic mild or moderate hypoxemia and hypercapnia such as from wearing facemasks resulting in shifting to higher contribution of anaerobic energy metabolism, decrease in pH levels and increase in cells and blood acidity, toxicity, oxidative stress, chronic inflammation, immunosuppression and health deterioration [24] , [11] , [12] , [13] .
Efficacy of facemasks
The physical properties of medical and non-medical facemasks suggest that facemasks are ineffective to block viral particles due to their difference in scales [16] , [17] , [25] . According to the current knowledge, the virus SARS-CoV-2 has a diameter of 60 nm to 140 nm [nanometers (billionth of a meter)] [16] , [17] , while medical and non-medical facemasks’ thread diameter ranges from 55 µm to 440 µm [micrometers (one millionth of a meter), which is more than 1000 times larger [25] . Due to the difference in sizes between SARS-CoV-2 diameter and facemasks thread diameter (the virus is 1000 times smaller), SARS-CoV-2 can easily pass through any facemask [25] . In addition, the efficiency filtration rate of facemasks is poor, ranging from 0.7% in non-surgical, cotton-gauze woven mask to 26% in cotton sweeter material [2] . With respect to surgical and N95 medical facemasks, the efficiency filtration rate falls to 15% and 58%, respectively when even small gap between the mask and the face exists [25] .
Clinical scientific evidence challenges further the efficacy of facemasks to block human-to-human transmission or infectivity. A randomized controlled trial (RCT) of 246 participants [123 (50%) symptomatic)] who were allocated to either wearing or not wearing surgical facemask, assessing viruses transmission including coronavirus [26] . The results of this study showed that among symptomatic individuals (those with fever, cough, sore throat, runny nose ect…) there was no difference between wearing and not wearing facemask for coronavirus droplets transmission of particles of >5 µm. Among asymptomatic individuals, there was no droplets or aerosols coronavirus detected from any participant with or without the mask, suggesting that asymptomatic individuals do not transmit or infect other people [26] . This was further supported by a study on infectivity where 445 asymptomatic individuals were exposed to asymptomatic SARS-CoV-2 carrier (been positive for SARS-CoV-2) using close contact (shared quarantine space) for a median of 4 to 5 days. The study found that none of the 445 individuals was infected with SARS-CoV-2 confirmed by real-time reverse transcription polymerase [27] .
A meta -analysis among health care workers found that compared to no masks, surgical mask and N95 respirators were not effective against transmission of viral infections or influenza-like illness based on six RCTs [28] . Using separate analysis of 23 observational studies, this meta -analysis found no protective effect of medical mask or N95 respirators against SARS virus [28] . A recent systematic review of 39 studies including 33,867 participants in community settings (self-report illness), found no difference between N95 respirators versus surgical masks and surgical mask versus no masks in the risk for developing influenza or influenza-like illness, suggesting their ineffectiveness of blocking viral transmissions in community settings [29] .
Another meta -analysis of 44 non-RCT studies (n = 25,697 participants) examining the potential risk reduction of facemasks against SARS, middle east respiratory syndrome (MERS) and COVID-19 transmissions [30] . The meta -analysis included four specific studies on COVID-19 transmission (5,929 participants, primarily health-care workers used N95 masks). Although the overall findings showed reduced risk of virus transmission with facemasks, the analysis had severe limitations to draw conclusions. One of the four COVID-19 studies had zero infected cases in both arms, and was excluded from meta -analytic calculation. Other two COVID-19 studies had unadjusted models, and were also excluded from the overall analysis. The meta -analytic results were based on only one COVID-19, one MERS and 8 SARS studies, resulting in high selection bias of the studies and contamination of the results between different viruses. Based on four COVID-19 studies, the meta -analysis failed to demonstrate risk reduction of facemasks for COVID-19 transmission, where the authors reported that the results of meta -analysis have low certainty and are inconclusive [30] .
In early publication the WHO stated that “facemasks are not required, as no evidence is available on its usefulness to protect non-sick persons” [14] . In the same publication, the WHO declared that “cloth (e.g. cotton or gauze) masks are not recommended under any circumstance” [14] . Conversely, in later publication the WHO stated that the usage of fabric-made facemasks (Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk) is a general community practice for “preventing the infected wearer transmitting the virus to others and/or to offer protection to the healthy wearer against infection (prevention)” [2] . The same publication further conflicted itself by stating that due to the lower filtration, breathability and overall performance of fabric facemasks, the usage of woven fabric mask such as cloth, and/or non-woven fabrics, should only be considered for infected persons and not for prevention practice in asymptomatic individuals [2] . The Central for Disease Control and Prevention (CDC) made similar recommendation, stating that only symptomatic persons should consider wearing facemask, while for asymptomatic individuals this practice is not recommended [31] . Consistent with the CDC, clinical scientists from Departments of Infectious Diseases and Microbiology in Australia counsel against facemasks usage for health-care workers, arguing that there is no justification for such practice while normal caring relationship between patients and medical staff could be compromised [32] . Moreover, the WHO repeatedly announced that “at present, there is no direct evidence (from studies on COVID-19) on the effectiveness face masking of healthy people in the community to prevent infection of respiratory viruses, including COVID-19” [2] . Despite these controversies, the potential harms and risks of wearing facemasks were clearly acknowledged. These including self-contamination due to hand practice or non-replaced when the mask is wet, soiled or damaged, development of facial skin lesions, irritant dermatitis or worsening acne and psychological discomfort. Vulnerable populations such as people with mental health disorders, developmental disabilities, hearing problems, those living in hot and humid environments, children and patients with respiratory conditions are at significant health risk for complications and harm [2] .
Physiological effects of wearing facemasks
Wearing facemask mechanically restricts breathing by increasing the resistance of air movement during both inhalation and exhalation process [12] , [13] . Although, intermittent (several times a week) and repetitive (10–15 breaths for 2–4 sets) increase in respiration resistance may be adaptive for strengthening respiratory muscles [33] , [34] , prolonged and continues effect of wearing facemask is maladaptive and could be detrimental for health [11] , [12] , [13] . In normal conditions at the sea level, air contains 20.93% O 2 and 0.03% CO 2 , providing partial pressures of 100 mmHg and 40 mmHg for these gases in the arterial blood, respectively. These gas concentrations significantly altered when breathing occurs through facemask. A trapped air remaining between the mouth, nose and the facemask is rebreathed repeatedly in and out of the body, containing low O 2 and high CO 2 concentrations, causing hypoxemia and hypercapnia [35] , [36] , [11] , [12] , [13] . Severe hypoxemia may also provoke cardiopulmonary and neurological complications and is considered an important clinical sign in cardiopulmonary medicine [37] , [38] , [39] , [40] , [41] , [42] . Low oxygen content in the arterial blood can cause myocardial ischemia, serious arrhythmias, right or left ventricular dysfunction, dizziness, hypotension, syncope and pulmonary hypertension [43] . Chronic low-grade hypoxemia and hypercapnia as result of using facemask can cause exacerbation of existing cardiopulmonary, metabolic, vascular and neurological conditions [37] , [38] , [39] , [40] , [41] , [42] . Table 1 summarizes the physiological, psychological effects of wearing facemask and their potential long-term consequences for health.
Physiological and Psychological Effects of Wearing Facemask and Their Potential Health Consequences.
In addition to hypoxia and hypercapnia, breathing through facemask residues bacterial and germs components on the inner and outside layer of the facemask. These toxic components are repeatedly rebreathed back into the body, causing self-contamination. Breathing through facemasks also increases temperature and humidity in the space between the mouth and the mask, resulting a release of toxic particles from the mask’s materials [1] , [2] , [19] , [26] , [35] , [36] . A systematic literature review estimated that aerosol contamination levels of facemasks including 13 to 202,549 different viruses [1] . Rebreathing contaminated air with high bacterial and toxic particle concentrations along with low O 2 and high CO 2 levels continuously challenge the body homeostasis, causing self-toxicity and immunosuppression [1] , [2] , [19] , [26] , [35] , [36] .
A study on 39 patients with renal disease found that wearing N95 facemask during hemodialysis significantly reduced arterial partial oxygen pressure (from PaO 2 101.7 to 92.7 mm Hg), increased respiratory rate (from 16.8 to 18.8 breaths/min), and increased the occurrence of chest discomfort and respiratory distress [35] . Respiratory Protection Standards from Occupational Safety and Health Administration, US Department of Labor states that breathing air with O 2 concentration below 19.5% is considered oxygen-deficiency, causing physiological and health adverse effects. These include increased breathing frequency, accelerated heartrate and cognitive impairments related to thinking and coordination [36] . A chronic state of mild hypoxia and hypercapnia has been shown as primarily mechanism for developing cognitive dysfunction based on animal studies and studies in patients with chronic obstructive pulmonary disease [44] .
The adverse physiological effects were confirmed in a study of 53 surgeons where surgical facemask were used during a major operation. After 60 min of facemask wearing the oxygen saturation dropped by more than 1% and heart rate increased by approximately five beats/min [45] . Another study among 158 health-care workers using protective personal equipment primarily N95 facemasks reported that 81% (128 workers) developed new headaches during their work shifts as these become mandatory due to COVID-19 outbreak. For those who used the N95 facemask greater than 4 h per day, the likelihood for developing a headache during the work shift was approximately four times higher [Odds ratio = 3.91, 95% CI (1.35–11.31) p = 0.012], while 82.2% of the N95 wearers developed the headache already within ≤10 to 50 min [46] .
With respect to cloth facemask, a RCT using four weeks follow up compared the effect of cloth facemask to medical masks and to no masks on the incidence of clinical respiratory illness, influenza-like illness and laboratory-confirmed respiratory virus infections among 1607 participants from 14 hospitals [19] . The results showed that there were no difference between wearing cloth masks, medical masks and no masks for incidence of clinical respiratory illness and laboratory-confirmed respiratory virus infections. However, a large harmful effect with more than 13 times higher risk [Relative Risk = 13.25 95% CI (1.74 to 100.97) was observed for influenza-like illness among those who were wearing cloth masks [19] . The study concluded that cloth masks have significant health and safety issues including moisture retention, reuse, poor filtration and increased risk for infection, providing recommendation against the use of cloth masks [19] .
Psychological effects of wearing facemasks
Psychologically, wearing facemask fundamentally has negative effects on the wearer and the nearby person. Basic human-to-human connectivity through face expression is compromised and self-identity is somewhat eliminated [47] , [48] , [49] . These dehumanizing movements partially delete the uniqueness and individuality of person who wearing the facemask as well as the connected person [49] . Social connections and relationships are basic human needs, which innately inherited in all people, whereas reduced human-to-human connections are associated with poor mental and physical health [50] , [51] . Despite escalation in technology and globalization that would presumably foster social connections, scientific findings show that people are becoming increasingly more socially isolated, and the prevalence of loneliness is increasing in last few decades [50] , [52] . Poor social connections are closely related to isolation and loneliness, considered significant health related risk factors [50] , [51] , [52] , [53] .
A meta -analysis of 91 studies of about 400,000 people showed a 13% increased morality risk among people with low compare to high contact frequency [53] . Another meta -analysis of 148 prospective studies (308,849 participants) found that poor social relationships was associated with 50% increased mortality risk. People who were socially isolated or fell lonely had 45% and 40% increased mortality risk, respectively. These findings were consistent across ages, sex, initial health status, cause of death and follow-up periods [52] . Importantly, the increased risk for mortality was found comparable to smoking and exceeding well-established risk factors such as obesity and physical inactivity [52] . An umbrella review of 40 systematic reviews including 10 meta -analyses demonstrated that compromised social relationships were associated with increased risk of all-cause mortality, depression, anxiety suicide, cancer and overall physical illness [51] .
As described earlier, wearing facemasks causing hypoxic and hypercapnic state that constantly challenges the normal homeostasis, and activates “fight or flight” stress response, an important survival mechanism in the human body [11] , [12] , [13] . The acute stress response includes activation of nervous, endocrine, cardiovascular, and the immune systems [47] , [54] , [55] , [56] . These include activation of the limbic part of the brain, release stress hormones (adrenalin, neuro-adrenalin and cortisol), changes in blood flow distribution (vasodilation of peripheral blood vessels and vasoconstriction of visceral blood vessels) and activation of the immune system response (secretion of macrophages and natural killer cells) [47] , [48] . Encountering people who wearing facemasks activates innate stress-fear emotion, which is fundamental to all humans in danger or life threating situations, such as death or unknown, unpredictable outcome. While acute stress response (seconds to minutes) is adaptive reaction to challenges and part of the survival mechanism, chronic and prolonged state of stress-fear is maladaptive and has detrimental effects on physical and mental health. The repeatedly or continuously activated stress-fear response causes the body to operate on survival mode, having sustain increase in blood pressure, pro-inflammatory state and immunosuppression [47] , [48] .
Long-Term health consequences of wearing facemasks
Long-term practice of wearing facemasks has strong potential for devastating health consequences. Prolonged hypoxic-hypercapnic state compromises normal physiological and psychological balance, deteriorating health and promotes the developing and progression of existing chronic diseases [23] , [38] , [39] , [43] , [47] , [48] , [57] , [11] , [12] , [13] . For instance, ischemic heart disease caused by hypoxic damage to the myocardium is the most common form of cardiovascular disease and is a number one cause of death worldwide (44% of all non-communicable diseases) with 17.9 million deaths occurred in 2016 [57] . Hypoxia also playing an important role in cancer burden [58] . Cellular hypoxia has strong mechanistic feature in promoting cancer initiation, progression, metastasis, predicting clinical outcomes and usually presents a poorer survival in patients with cancer. Most solid tumors present some degree of hypoxia, which is independent predictor of more aggressive disease, resistance to cancer therapies and poorer clinical outcomes [59] , [60] . Worth note, cancer is one of the leading causes of death worldwide, with an estimate of more than 18 million new diagnosed cases and 9.6 million cancer-related deaths occurred in 2018 [61] .
With respect to mental health, global estimates showing that COVID-19 will cause a catastrophe due to collateral psychological damage such as quarantine, lockdowns, unemployment, economic collapse, social isolation, violence and suicides [62] , [63] , [64] . Chronic stress along with hypoxic and hypercapnic conditions knocks the body out of balance, and can cause headaches, fatigue, stomach issues, muscle tension, mood disturbances, insomnia and accelerated aging [47] , [48] , [65] , [66] , [67] . This state suppressing the immune system to protect the body from viruses and bacteria, decreasing cognitive function, promoting the developing and exacerbating the major health issues including hypertension, cardiovascular disease, diabetes, cancer, Alzheimer disease, rising anxiety and depression states, causes social isolation and loneliness and increasing the risk for prematurely mortality [47] , [48] , [51] , [56] , [66] .
The existing scientific evidences challenge the safety and efficacy of wearing facemask as preventive intervention for COVID-19. The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks. Wearing facemasks has been demonstrated to have substantial adverse physiological and psychological effects. These include hypoxia, hypercapnia, shortness of breath, increased acidity and toxicity, activation of fear and stress response, rise in stress hormones, immunosuppression, fatigue, headaches, decline in cognitive performance, predisposition for viral and infectious illnesses, chronic stress, anxiety and depression. Long-term consequences of wearing facemask can cause health deterioration, developing and progression of chronic diseases and premature death. Governments, policy makers and health organizations should utilize prosper and scientific evidence-based approach with respect to wearing facemasks, when the latter is considered as preventive intervention for public health.
CRediT authorship contribution statement
Baruch Vainshelboim: Conceptualization, Data curation, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
WATCH TV LIVE
Former NIH Head: COVID Lab Leak Not Conspiracy Theory
By Solange Reyner | Thursday, 16 May 2024 05:14 PM EDT
Francis Collins, the top public health official during the COVID-19 pandemic, earlier this year said the lab leak hypothesis was not a conspiracy theory, according to a transcript of his testimony released Thursday by House Republicans, reported the Washington Examiner .
Collins in January of this year was called before the House Select Subcommittee to explain his role in the scientific inquiry into the origins of the COVID-19 pandemic.
Lawmakers asked him whether the coronavirus could have resulted from "a laboratory or research-related accident, a researcher doing something in the lab, getting infected with the virus, and then sparking the pandemic."
When asked if this scenario was a conspiracy theory, Collins responded "not at this point."
Collins also responded "yes" when asked by Republicans if "the origin of COVID-19" is "unsettled science."
Collins told the committee that it was in the Chinese government's best interest "for this to be unresolved."
"If it was a lab leak, they're responsible," said Collins. "If it was a natural origin in a wet market that was selling wild animals that they were not supposed to be doing, they're responsible. So they love it that this hasn't gotten resolved," he said.
FBI Director Christopher Wray last year said the bureau believes COVID-19 most likely originated in a Chinese government-controlled lab.
Solange Reyner ✉
Solange reyner is a writer and editor for newsmax. she has more than 15 years in the journalism industry reporting and covering news, sports and politics..
- Rep. Wenstrup to Newsmax: Redacted Docs Indicate COVID Cover-Up
- COVID Drug Reduces Infections in Those At-Risk
© 2024 Newsmax. All rights reserved.
Sign up for Newsmax’s Daily Newsletter
Receive breaking news and original analysis - sent right to your inbox.

- Health News
- Brain Health
- Natural Health
- Diet & Fitness
The information presented on this website is not intended as specific medical advice and is not a substitute for professional medical treatment or diagnosis. Read Newsmax Terms and Conditions of Service .
Newsmax, Moneynews, Newsmax Health, and Independent. American. are registered trademarks of Newsmax Media, Inc. Newsmax TV, and Newsmax World are trademarks of Newsmax Media, Inc.

IMAGES
COMMENTS
In theory, COVID-19 could have come from a lab in a few ways. Researchers might have collected SARS-CoV-2 from an animal and maintained it in their lab to study, or they might have created it by ...
7) Patients will become consumers. The Covid-19 pandemic literally impacts each and every one of us. The boundary between "healthy" and "sick" becomes blurred. People who have otherwise ...
Key Events in the Effort to Determine the Origins of the Covid-19 Pandemic. The joint WHO-China technical report published in March 2021 rated a zoonotic spillover as a "likely to very likely ...
COVID-19 is a new, complex, multisystem disease caused by the novel coronavirus SARS-CoV-2. In slightly over 2 years, it infected nearly 500 million and killed 6 million human beings worldwide, causing an unprecedented coronavirus pandemic. Several vaccines, developed in record time, were approved for public use (Forni and Mantovani 2021 ...
The ongoing COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), has affected 212 countries worldwide at various degrees as of 8 May 2020. 1 In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or potentially even other respiratory viruses—may predispose to more ...
COVID-19 has the potential to enter and invade the brain cells and produce different neurological symptoms. The brain has been reported to express angiotensin converting enzyme 2 (ACE2) receptors that have been detected over glial cells and neurons, which makes them a potential target of COVID-19, and could be a probable cause to develop ...
The COVID-19 pandemic has the potential to affect the human microbiome in infected and uninfected individuals, having a substantial impact on human health over the long term. This pandemic intersects with a decades-long decline in microbial diversity and ancestral microbes due to hygiene, antibiotics, and urban living (the hygiene hypothesis).
Scientists don't have enough evidence about the origins of SARS-CoV-2 to rule out the lab-leak hypothesis, ... In theory, COVID-19 could have come from a lab in a few ways. Researchers might ...
The COVID-19 pandemic has the potential to affect the human microbiome in infected and uninfected individuals, having a substantial impact on human health over the long term. This pandemic intersects with a decades-long decline in microbial diversity and ancestral microbes due to hygiene, antibiotics, and urban living (the hygiene hypothesis).
The origins of SARS-CoV-2, the virus that causes COVID-19 and has infected more than 171 million people, killing close to 3.7 million worldwide as of June 4, remain unclear. Many scientists ...
Since the outbreak of coronavirus disease 2019 (COVID-19), clinicians have tried every effort to understand the disease, and a brief portrait of its clinical features have been identified. In clinical practice, we noticed that many severe or critically ill COVID-19 patients developed typical clinical manifestations of shock, including cold extremities and weak peripheral pulses, even in the ...
on the origins of COVID-19. It also identifies areas for possible additional research. Annexes include a lexicon, additional details on methodology, and comments from outside experts. This assessment is based on information through August 2021. The IC assesses that SARS-CoV-2, the virus that causes COVID-19, probably emerged and infected humans
HYPOTHESIS: The COVID-19 pandemic is a feedback signal from the biosphere that denotes the ecological overshoot of the human species (currently estimated at about 1.7 planets; GFN 2020). That means that efforts to control this pandemic, even if successful, will not solve the wider problem of overshoot and the prospect of further, more ...
Background: Corona virus (COVID-19) is an outbreak of respiratory disease caused by a novel corona virus and declared to be a global health emergency and a pandemic by the World Health Organization (WHO) on March 11, 2020. Prevention strategies to control the transmission of the COVID-19 pandemic, such as closing of schools, refraining from gathering, and social distancing, have direct impacts ...
The null hypothesis was that there would be no difference in survey scores between Spanish and Chinese participants. The other null hypothesis was that physical symptoms resembling COVID-19, higher confidence in medical services, perceived higher chances of survival, satisfaction with health information, and adoption of precautionary measures ...
Alternative Hypotheses. Awareness of COVID-19 inflicted-death among those one knew: One possible mechanism accounting for increased willingness to vaccinate against COVID-19 was experience with the ill effects of the disease.Black Americans were disproportionately exposed to those risks (American Public Media Research Lab, Citation 2023), and this differential exposure could have increased the ...
Therefore, we tentatively propose a hypothesis which hopefully might ultimately help save lives. Based on the current scientific literature and on new epidemiological data which reveal that current smoking status appears to be a protective factor against the infection by SARS-CoV-2 [1], we hypothesize that the nicotinic acetylcholine receptor ...
The COVID-19 lab leak theory, or lab leak hypothesis, is the idea that SARS-CoV-2, the virus that caused the COVID-19 pandemic, came from a laboratory. This claim is highly controversial; most scientists believe the virus spilled into human populations through natural zoonosis (transfer directly from an infected non-human animal), similar to ...
The ongoing COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), has affected 212 countries worldwide at various degrees as of 8 May 2020.1 In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or potentially even other respiratory viruses—may predispose to more ...
The major finding was that even when a COVID-19 vaccine always produces sterilizing immunity against every SARS-CoV-2 variant, its ability to control the epidemic can be compromised by multiple common conditions. ... This hypothesis is not supported by the data on US hospital admissions. In the 20 weeks from 14 May 2022 through 24 September ...
Dr. Anthony Fauci faced intense questioning from the House Select Subcommittee on the Coronavirus Pandemic, where he admitted that the six-foot social distancing rule had little scientific basis.
Collins also responded in the affirmative when asked by Republicans if "the origin of COVID-19 still unsettled science." Regardless of whether the virus originated in the Wuhan lab or in a ...
Francis Collins, the top public health official during the COVID-19 pandemic, earlier this year said the lab leak hypothesis was not a conspiracy theory, according to a transcript of his testimony released Thursday by House Republicans, reports the Washington Examiner. Collins in January of this year was called before the House Select ...
Hypothesis. On January 30, 2020, the World Health Organization (WHO) announced a global public health emergency of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) causing illness of coronavirus disease-2019 (COVID-19) .As of October 1, 2020, worldwide 34,166,633 cases were reported and 1,018,876 have died with virus diagnosis.
Select Subcommittee seeks to uncover why the lab-leak hypothesis was suppressed and vilified. WASHINGTON — Select Subcommittee on the Coronavirus Pandemic Chairman Brad Wenstrup (R-Ohio) will hold a hearing titled "Investigating the Proximal Origin of a Cover Up" to examine the potential conflicts of interest and suppression of scientific discourse by the National Institutes of Health ...
Francis Collins, the top public health official during the COVID-19 pandemic, earlier this year said the lab leak hypothesis was not a conspiracy theory, according to a transcript of his testimony released Thursday by House Republicans, reported the Washington Examiner.. Collins in January of this year was called before the House Select Subcommittee to explain his role in the scientific ...