Join our Newsletter
Get helpful tips and the latest information

CBT for Depression: How It Works, Examples, & Effectiveness
Author: Renee Skedel, LPC
Renee Skedel LPCC
Renee Skedel, LPCC, has extensive experience in crisis resolution, suicide risk assessment, and severe mental illness, utilizing CBT and DBT approaches. She’s worked in diverse settings, including hospitals and jails.
Cognitive behavioral therapy (CBT) for depression effectively targets negative thought patterns. It’s a short-term therapy for clinical depression that reduces symptoms by helping people recognize unhelpful thoughts and behaviors and replace them with healthier thinking and reacting.
How Does CBT Help Depression?
Cognitive behavioral therapy (CBT) is a type of psychotherapy that uses a combination of cognitive and behavioral approaches to reduce depression . 1 CBT therapy for depression focuses on changing a person’s feelings to help improve their thoughts and behaviors. CBT therapists may challenge depressive thinking patterns that lead to inaction or self-harming behaviors.
Cognitive Methods to Change Depressive Thinking Patterns
Cognitive methods teach you to challenge negative or irrational thoughts, eventually reducing their power over you. Techniques like cognitive restructuring can help you understand your thought patterns, the emotion behind them, and the actual reality of the situation. A therapist can help present a more realistic perspective to help reduce cognitive distortions . You can also use the free CBT for depression worksheet below to practice cognitive restructuring.
A common cognitive distortion among those with depression is “mind reading,” where you believe you know what others are thinking. By challenging this and other depressive thoughts, you can build a healthier pattern of thinking and self-talk. 1, 2
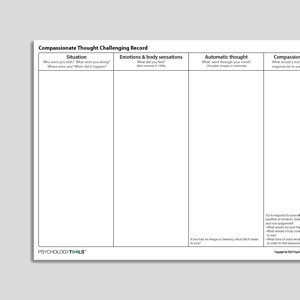
Cognitive Restructuring for Depression Worksheet
You can recognize unhealthy thought patterns that are making your depression symptoms worse by practicing cognitive restructuring with this worksheet.
Find a Supportive Therapist Who Specializes in CBT.
BetterHelp has over 30,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $65 per week. Take a free online assessment and get matched with the right therapist for you.
Types of CBT for Depression
Cognitive behavioral therapy is not only a treatment type, but it is also the main branch for a number of different therapy styles. There are three common types of CBT used for depression symptoms and episodes.
Along with standard CBT, here are three other common types of CBT used for depression:
Acceptance & Commitment Therapy (ACT)
ACT engages a number of techniques to increase someone’s mental flexibility. ACT for depression can help with reducing the difficulties of negative thoughts and self-talk, anxiety, and judgment, and increase the individual’s ability to focus.
ACT techniques include strategies for each of these pillars: 9
- Acceptance : allowing a thought or feeling to exist without judging it or pushing it away
- Mindfulness: encouraging the individual to be able to focus on the present
- Commitment to behavioral change: if something is not in line with the meaning or values the individual holds, then change this behavior to meet that value
Dialectical Behavioral Therapy (DBT)
Similar to ACT, DBT helps people learn how to accept difficult feelings and thoughts. In addition, DBT for depression teaches how to balance between the ability to accept and address irrational thoughts and behaviors to be able to make healthy and maintainable changes in their ability to cope with life’s stressors. 9
DBT is most frequently used to treat those with borderline personality disorder (BPD). However, it was initially developed to treat people who had frequent suicidal thoughts . In addition, those with BPD or bipolar disorder engage in significant amounts of self-harm—regardless of suicidal intent—that can be seen in depressive episodes across disorders.
Rational Emotive Behavior Therapy (REBT)
In treating depression, rational emotive behavioral therapy (REBT) uses the approach of utilizing the desire to feel happy or fulfilled to reduce depressive symptoms. The REBT approach uses many CBT techniques for depression to help people change their thought processes, helping to create healthier behavior patterns, and eventually helping someone move out of their depressive thoughts and behaviors. 10
REBT was created with the idea that individuals make choices in their lives to meet needs that allow them to survive and feel fulfilled. In turn, REBT teaches individuals how to address irrational and unhealthy behaviors and thoughts so that they can change them for a more functional and fulfilling life.
Behavioral Methods
Behavioral methods are highly effective in treating depression. They typically involve rewarding yourself for small behavioral changes. For example, depression can cause a lack of motivation or low energy. By rewarding yourself for engaging in a task like putting away a dish or two, you change the chemical outputs in your brain. Adding a reward makes you more likely to repeat the behavior in the future. 1
CBT employs several methods to reduce the power of not engaging in behaviors as well, like reducing self-harming or self-sabotaging behaviors that often accompany depression.
What Types of Depression Can CBT Treat?
Cognitive behavioral therapy for depression can be an effective treatment for various depressive disorders and episodes that may be impacting your life, especially in the mild to moderate range of symptoms. 3
CBT can be effective in treating these types of depression: 3
- Major depressive disorder (clinical depression)
- Persistent depressive disorder (PDD)
- Seasonal affective disorder
- Postpartum depression
- The depressive episodes of bipolar disorder
- Situational depression
- Schizoaffective disorder, depressive type
9 Common CBT Techniques for Depression
Common CBT techniques used for depression include cognitive restructuring, thought journaling, and mindful meditation. Many of these techniques are used together to show the connections between thoughts, emotions, and behaviors.
Here are nine common CBT techniques for depression: 2
1. Cognitive Restructuring
In challenging your thought patterns, tone, and self-talk, you learn about potential cognitive distortions and unhealthy thought patterns that could be increasing depressive emotions or suicidal thoughts. Cognitive restructuring , sometimes called reframing, forms healthier thought patterns, reduces cognitive errors, and helps you practice ways to rationalize distortions and untrue beliefs.
Here’s how to try the five steps to cognitive restructuring:
- Set up your list: draw a line down the middle of a piece of paper. Title the left-hand column “Unproductive Thoughts” and title the right-hand column “Replacement Thoughts.”
- Write down your unproductive thoughts: on the left-hand side of your paper, list your negative and self-critical thoughts, or any automatic thoughts you have regularly that make you unhappy, something like “I can’t do anything right.”
- Identify your replacement thoughts: for each of your unproductive thoughts, create a replacement thought and write it down on the right side of your paper, such as “Here’s a project I did well.”
- Review your list regularly: so you begin to memorize the unproductive thoughts and their replacement thoughts.
- Notice your thoughts in real time: pay attention to your thoughts throughout each day. When you think of one of your unproductive thoughts, stop yourself and remind yourself of the replacement thought. With practice, you’ll begin to challenge your unproductive thoughts and naturally start to replace them with rational ones.
2. Activity Scheduling
Activity scheduling involves rewarding yourself for scheduling activities that encourage positive experiences and self-care. By scheduling these activities and rewards, you learn to motivate yourself to complete necessary tasks even when you are feeling low. It also increases the chances of continuing to complete these tasks after you end your formal therapy sessions.
3. Thought Journaling
By journaling for mental health , exploring things like your emotions, thoughts, and behaviors, you create a space to process and identify any potential triggers, as well as how your thoughts have been influencing your behavior. This can increase self-awareness and help you learn coping techniques to use in the future. 4 You can also use specific journal prompts for depression to understand more where your beliefs and moods have been coming from.
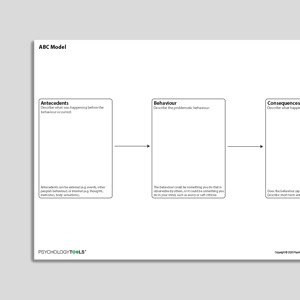
4. ABC Analysis
Similar to journaling, the ABC model is solely focused on breaking down the behaviors that are related to depression, like snapping at people or sleeping all day. In analyzing your triggers and consequences, you can explore the “consequential” behaviors and look to find common causes in your depressive triggers.
The ABC model works by using the following structure:
- The “Activating” event
- Your “Beliefs” about that event
- The “Consequences” of the event, including your feelings and behaviors surrounding the event
5. Fact-checking
Fact-checking encourages you to review your thoughts and understand that, while you may be stuck in a depressive or harmful thought pattern, these thoughts are not facts but opinions based on your emotions (e.g., “I am a failure”). Fact-checking can also help you identify what behaviors you engage in due to your opinions or emotions instead of the actual facts.
6. Successive Approximation or “Breaking It Down”
Breaking down large tasks into smaller goals will help you feel less overwhelmed. By practicing successive approximation, you will be more likely to complete your goals and be better able to cope with large tasks in the future, even during times when your depression is heightened.
7. Mindful Meditation
By engaging in meditation for depression , you will learn to reduce focus on negative thoughts and increase your ability to remain in the present. Meditation can help you recognize and learn to accept your negative thought patterns and detach from them instead of letting them take over.
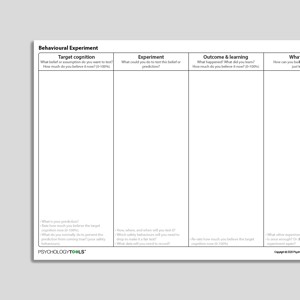
8. Behavioral Experiments
Therapists use behavioral experiments as a tool for challenging irrational thought patterns that may be contributing to your depression. You’ll learn how to replace these thoughts with healthier thoughts. By engaging in these experiments, you can spot and learn to stop catastrophic thinking and develop a more realistic view of the world.
9. Role Play
Your therapist may have you role play a specific situation you find challenging. You will act out the situation alongside the therapist, while learning to practice healthier responses and depression coping mechanisms . Role playing helps you gain a better understanding of your emotional responses and how to manage your reactions in a real-life situation.
Talkspace - Online Therapy and Medication Management
Your therapist can help you process thoughts and feelings, understand motivations, and develop coping skills. Covered by most major insurance plans. Try Talkspace
Examples of CBT for Depression
CBT uses cognitive and behavioral techniques to improve depression symptoms , but the exact CBT treatment plan for depression might depend on the type of depression someone is experiencing.
CBT For Major Depressive Disorder (MDD) Example
Jody, a 35-year-old female, has recently started to feel tired all the time. This began about two and a half weeks ago. Along with “sleeping all the time,” she reports these other symptoms that all started around the same time.
Those symptoms include:
- Experiencing negative thoughts
- Constantly worrying about different aspects of her life
- Finding it difficult to stay still
- Does not have an appetite
- Has generally been feeling sad, hopeless, irritable, and numb
She reports that she had also felt this way in her teens and mid-20’s; and she also experienced brief suicidal thoughts in her 20’s.
Jody began meeting with her therapist and the therapist diagnosed major depressive disorder after they finished their assessment. During sessions, her therapist began asking her to think about what thoughts are making her feel sad and to change her thought process. She also recommended journaling every day.
Part of the journaling homework includes documenting something that she chose to do to make her feel happy or productive daily, a CBT technique called behavioral activation. When Jody started reporting an increase in her worry and rumination , the therapist encouraged her to add meditation to her daily work, to help reduce the incessant worrying and increase calm in Jody’s mind. 1, 5
CBT For Persistent Depressive Disorder (PDD) Example
Matt, a 28-year-old male, has been experiencing a low and depressed mood, difficulty sleeping, low self-esteem , and difficulty with concentration for the last two and a half years. He works a difficult job and felt it was related, but was informed by family that they noticed this low-grade depression even when he was in less stressful positions.
Matt reached out to a therapist, who diagnosed him with persistent depressive disorder (dysthymia) . 1, 5, 6, 7 His therapist began working with him on journaling about his day on a regular basis, especially if something made him happy. The therapist encouraged him to write down and challenge his negative and irrational thoughts.
Matt and his therapist also worked on noting triggers for aggressive thoughts towards himself to increase his awareness. Matt’s therapist began encouraging him to engage in problem-solving tasks to help him function and build resilience when his depressive symptoms flared up. 1
CBT For Seasonal Affective Disorder (SAD) & Situational Depression Example
Jamie, a 37-year-old male, began experiencing depressive moods, difficulty concentrating, increased fatigue, lowered energy, feeling tense, and negative thoughts in his early 20’s. He reports that he never reached out for help because even if the symptoms tended to start in October to November almost every year, they always stopped around March.
This year, Jamie’s symptoms began around the same time, although he noticed that his negative thoughts were worse than normal and that his sleep schedule was off. As a result, he reached out to a local therapist, who diagnosed Jamie with “unspecified depressive disorder with seasonal pattern,” which is more commonly known as seasonal affective disorder (SAD) . 7
Jamie’s therapist began working with him to reduce the impact of his symptoms by having him engage in regular meditation to reduce his anxiety and challenge his thoughts outside of session to reduce the negative thought patterns impacting his perspective.
They also worked together to create a daily schedule of activities to help increase self-fulfillment and self-care , and journaling to increase acknowledgement of positive things during the difficult season, as well as to track Jamie’s mood. 1, 5, 7
CBT For Postpartum Depression Example
Julia, a 32-year-old female, had her baby about three weeks ago. About two weeks ago, Julia began experiencing significant levels of anxiety, panic attacks, low mood, feelings of depression and worthlessness, and loneliness . This was Julia’s first child and she had never experienced these feelings before, nor had anyone else in her family. 1, 7
Julia sought out a therapist to figure out her feelings and was diagnosed with “unspecified depressive disorder with peripartum onset,” more commonly known as postpartum depression . Her therapist knew that research indicated that CBT had improved long- and short-term symptoms of depression and had some impact on anxiety in postnatal depression. 8
Julia’s therapist encouraged her to journal her feelings each day to increase awareness as well as acknowledge the positive things she was doing.
She also had her engage in a daily short meditation and breathing regulation technique to lower anxiety and panic attacks, engage in gratitude practices with her journaling to increase her mood and lower depressive symptoms, and to discuss her emotional concerns with her support system and partner to allow herself time to meet her own needs.
Julia was encouraged to explore her thought patterns influencing the anxious thoughts, especially leading up to panic attacks, to help reduce anxiety and become more aware of her triggers to be able to feel comfortable with her baby. 4, 9
How Effective Is CBT for Depression?
Cognitive therapy can be as effective as depression medication in initially treating moderate to severe depression, although its success often relies on the therapist’s level of experience. Studies show that when CBT is delivered by skilled therapists, it can lead to substantial improvements in depressive symptoms. 11
Other research studies have proven the effectiveness of CBT for depression:
- Studies show that the behavioral activation techniques used in CBT are useful in the treatment of those with severe depression. 5
- When compared to antidepressant medication, CBT alone may be effective in continued recovery for depression. 5
- Cognitive therapy shares efficacy with medication in treating moderate to severe major depressive disorder, although this can be impacted by the level of the therapist’s experience with CT/CBT. 11
- CBT was found to be an effective intervention in lowering depressive symptoms and depression relapse rates, especially in comparison with a control group. 12
- A study on bipolar disorder, including depressive episodes and symptoms, found that the group with CBT treatment had fewer bipolar episodes, shorter bipolar episodes, and less hospitalization admissions. In addition, this group’s depressed mood and mania symptoms were noted to be significantly lower. 13
Would You Like to Try CBT Therapy?
What to Expect During CBT Treatment
Those seeking CBT for depression will typically attend 12-20 weekly sessions, although many will experience improvements after just a few sessions. CBT treatments can be done in-person or with a CBT therapist online. 14 Most insurance companies cover CBT to help reduce the cost, but if paying out of pocket, you can expect to pay between $100 and $200 per session.
While CBT may involve some rigor and homework, CBT treatment was intended to be short-term to allow people to thrive with the help of their therapist, but then on their own. Each CBT session will generally last about 50 to 55 minutes, and happen once a week. The format of each session is usually quite structured.
Each CBT session consists of: 13
- Setting a goal or a problem to process for that day
- Working on the problem reported (this might include processing barriers in the problem as well as the person’s thoughts on these)
- Creating an action plan to address the problem in and out of session
- Measuring the person’s movement on the problem (like discussing homework, a reported issue, communication, etc.)
While this may not always be the case in a CBT treatment plan or the model of every single session, this is the expectation for treatment. Your therapist may take some different approaches, but CBT treatment tends to be short-term and active in attempting to reduce the impact of your mental health symptoms on your life.
How to Find a CBT Therapist
If you’re wondering how to choose a therapist , ask your primary care provider or a trusted loved one for a list of recommendations. You can also search a local therapist directory to find a licensed CBT provider in your state who specializes in CBT for depression. Many therapists now offer video-based therapy that has enabled many people to get CBT online .
If you’re ready to begin online CBT, Online-Therapy.com is an excellent choice for those without insurance. There are also several online therapy options that take insurance .
At-Home Cognitive Behavioral Therapy Exercises For Depression
While you should always seek help from a professional if you think you may have depression, there are CBT exercises you can try on your own or through the use of CBT apps to help relieve mild symptoms, like journaling, scheduling out activities you enjoy, and starting a gratitude practice. A therapist can also help you develop these techniques so you’ll be prepared when depressive symptoms arise.
Here are some at-home CBT exercises for depression: 3
Even if you aren’t seeing a therapist, keeping a journal of your thoughts, feelings, and behaviors can be helpful. Through writing in a notebook or through a journaling app like the Sensa app , you may begin to learn more about yourself and identify difficulties that regularly impact you. This way, you can prepare for them in the future. 4
Schedule Enjoyable Activities
Have events scheduled that improve your mood, like concerts, lunch dates with friends, or road trips. Even on a smaller scale like making a general to-do list, scheduling can inspire you to keep moving forward.
Try Meditation
Meditation can be helpful in managing your emotions, decompressing, and even falling asleep. It has been proven to help with addiction, depressive disorders, anxiety disorders, and more. If you’re not sure where to start, using meditation apps and free videos available online can help you clear your mind and connect to the present.
Practice Challenging Your Thoughts
You might want to start this practice in a journal, but it is also helpful to challenge or reframe your thinking in the moment. By reframing thoughts or saying affirmations in your head, you may be able to learn to stop negative thoughts in their tracks.
Start a Gratitude Practice
It might feel difficult at times, but it’s helpful to identify the positives in your life. One study showed that the use of gratitude helped to significantly reduce continuous negative thought processes (and reduced the risk of negative thoughts in individuals experiencing anxiety and depression ). 14 It can help to try writing three things you’re grateful for every day.
In My Experience
“In my experience, CBT can help with depression symptoms in many ways. In accessing CBT services, whether through a therapist or by practicing at-home skills, you can start feeling a bit better and getting back to the things that are most important to you.”
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy .
Cognitive behavioral therapy EXERCISES Los ANGELES: CBT INTERVENTIONS. (2020). Retrieved from https://cogbtherapy.com/cognitive-behavioral-therapy-exercises
Fenn, K., & Byrne, M. (2013). The key principles of cognitive behavioural therapy. InnovAiT, 6(9), 579–585. https://doi.org/10.1177/1755738012471029
Gautam, M., Tripathi, A., Deshmukh, D., & Gaur, M. (2020). Cognitive Behavioral Therapy for Depression. Indian Journal of Psychiatry, 62(8), 223. https://doi.org/10.4103/psychiatry.indianjpsychiatry_772_19
Utley, A., & Garza, Y. (2011). The therapeutic use of journaling with adolescents. Journal of Creativity in Mental Health, 6(1), 29-41.
Chand, S. P., & Maerov, P. J. (2019, March 28). Using CBT effectively for treating depression and anxiety. Retrieved from https://www.mdedge.com/psychiatry/article/82695/anxiety-disorders/using-cbt-effectively-treating-depression-and-anxiety/page/0/2
Publishing, H. (2014, March). Dysthymia. Retrieved from https://www.health.harvard.edu/newsletter_article/dysthymia
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (5th ed.). American Psychiatric Publishing.
Huang, L., Zhao, Y., Qiang, C., & Fan, B. (2018). Is cognitive behavioral therapy a better choice for women with postnatal depression? A systematic review and meta-analysis. PLOS ONE, 13(10), e0205243. https://doi.org/10.1371/journal.pone.0205243
Mike, D. (2016, February 8). Know the 3 Major Types of Therapy – CBT, ACT, DBT. Boca Raton Psychiatrist | Florida Psychologists. Retrieved November 13, 2021, from https://drmikemd.com/understanding-the-3-major-types-of-therapy-cbt-act-dbt
Ellis, A., & Joffe Ellis, D. (2019). Introduction. Rational Emotive Behavior Therapy (2nd Ed.)., 3–7. https://doi.org/10.1037/0000134-001
DeRubeis, R. J., Hollon, S. D., Amsterdam, J. D., Shelton, R. C., Young, P. R., Salomon, R. M., O’Reardon, J. P., Lovett, M. L., Gladis, M. M., Brown, L. L., & Gallop, R. (2005). Cognitive Therapy vs Medications in the Treatment of Moderate to Severe Depression. Archives of General Psychiatry, 62(4), 409. https://doi.org/10.1001/archpsyc.62.4.409
Li, J. M., Zhang, Y., Su, W. J., Liu, L. L., Gong, H., Peng, W., & Jiang, C. L. (2018). Cognitive behavioral therapy for treatment-resistant depression: A systematic review and meta-analysis. Psychiatry Research, 268, 243–250. https://doi.org/10.1016/j.psychres.2018.07.020
Lam, D. H., Watkins, E. R., Hayward, P., Bright, J., Wright, K., Kerr, N., Parr-Davis, G., & Sham, P. (2003). A Randomized Controlled Study of Cognitive Therapy for Relapse Prevention for Bipolar Affective Disorder. Archives of General Psychiatry, 60(2), 145. https://doi.org/10.1001/archpsyc.60.2.145
What is a CBT Session Like? (2021, August 3). Beck Institute Cares. Retrieved November 16, 2021, from https://cares.beckinstitute.org/about-cbt/what-are-sessions-like/
We regularly update the articles on ChoosingTherapy.com to ensure we continue to reflect scientific consensus on the topics we cover, to incorporate new research into our articles, and to better answer our audience’s questions. When our content undergoes a significant revision, we summarize the changes that were made and the date on which they occurred. We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here .
Your Voice Matters
Can't find what you're looking for.
Request an article! Tell ChoosingTherapy.com’s editorial team what questions you have about mental health, emotional wellness, relationships, and parenting. The therapists who write for us love answering your questions!
Leave your feedback for our editors.
Share your feedback on this article with our editors. If there’s something we missed or something we could improve on, we’d love to hear it.
Our writers and editors love compliments, too. :)
Frequently Asked Questions
How much does cbt cost.
CBT sessions generally cost about $100 to $200 out of pocket. Your insurance may cover it depending on their coverage for mental health treatments. If covered, insurance can reduce CBT sessions to around $25 to $75 each. If you’re considering CBT group therapy , the cost can be significantly lower. Group sessions tend to range from $25 to $50 per person, depending on the provider.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
Talk Therapy
Online-Therapy.com – Get support and guidance from a licensed therapist. Online-Therapy.com provides 45 minute weekly video sessions and unlimited text messaging with your therapist for only $64/week. Get Started
Online Psychiatry
Hims / Hers If you’re living with anxiety or depression, finding the right medication match may make all the difference. Connect with a licensed healthcare provider in just 12 – 48 hours. Explore FDA-approved treatment options and get free shipping, if prescribed. No insurance required. Get Started
Depression Newsletter
A free newsletter from Choosing Therapy for those impacted by depression. Get helpful tips and the latest information. Sign Up
Learn Anti-Stress & Relaxation Techniques
Mindfulness.com – Change your life by practicing mindfulness. In a few minutes a day, you can start developing mindfulness and meditation skills. Free Trial
Choosing Therapy Directory
You can search for therapists by specialty, experience, insurance, or price, and location. Find a therapist today.
Online Depression Test
A few questions from Talkiatry can help you understand your symptoms and give you a recommendation for what to do next.
Best Online Psychiatry Services
Online psychiatry, sometimes called telepsychiatry, platforms offer medication management by phone, video, or secure messaging for a variety of mental health conditions. In some cases, online psychiatry may be more affordable than seeing an in-person provider. Mental health treatment has expanded to include many online psychiatry and therapy services. With so many choices, it can feel overwhelming to find the one that is right for you.
CBT for Depression Infographics
Find a therapist in your state
Get the help you need from a therapist near you
California Connecticut Colorado Florida Georgia Illinois Indiana Kentucky Maryland Massachusetts Michigan New Jersey New York North Carolina Ohio Pennsylvania Texas Virginia
Are you a Therapist? Get Listed Today
A free newsletter for those impacted by depression. Get helpful tips and the latest information.
FOR IMMEDIATE HELP CALL:
Medical Emergency: 911
Suicide Hotline: 988
© 2024 Choosing Therapy, Inc. All rights reserved.
| published: | 2 Sep 2022 |
|---|---|
| updated: | 8 Jun 2024 |
- Psychology & Counseling Tools
9 CBT Worksheets and Tools for Anxiety and Depression

CBT is one of the most effective psychological treatments when it comes to managing anxiety and depression, and can be a highly useful approach to apply in online therapy.
If you help clients tackle cognitive distortions and unhelpful thinking styles, we’ve compiled a list of essential worksheets that should be part of your therapy toolbox.
How To Use CBT Worksheets in Therapy
Cognitive-behavioral therapy (CBT) is based on the idea that thoughts, feelings, physical sensations and behaviors are interlinked, and that changing negative thought patterns can enhance the way we act and feel.
It encompasses a variety of techniques and interventions that have been proven effective in the treatment of many mental disorders.
Besides anxiety and depression, a few examples include: [1]
- Panic disorder
- Bipolar disorder
- Borderline personality disorder, and
- Obsessive-compulsive disorder.
With the advent of online therapy, guided online CBT has become an increasingly popular way for mental health professionals to help clients manage behavioral health conditions without the need to meet in person as often.
CBT worksheets, exercises, and activities play a large role in these treatments to encourage further progress between sessions, in the same way that face-to-face CBT involves between-session practice. [2]
The Importance of Tailoring CBT Worksheets to Individual Needs
While CBT worksheets are effective tools, it is crucial to tailor these resources to the unique needs of each client.
Every individual’s experience with anxiety and depression is different, and a one-size-fits-all approach may not be as effective. Personalization involves understanding the specific triggers, thought patterns, and behaviors of a client.
For instance, a client struggling with social anxiety may benefit more from worksheets focusing on exposure and social skills training, while someone with generalized anxiety disorder might need tools aimed at managing worry and improving relaxation techniques.
Customizing worksheets also means considering the client’s cultural background, personal preferences, and level of cognitive functioning.
This tailored approach not only enhances the therapeutic alliance but also ensures that the interventions are more impactful, leading to better outcomes.
Therapists should regularly review and adjust the worksheets to keep them relevant and aligned with the client’s progress and evolving needs.
5 Example Tools For Treating Anxiety
So what types of online CBT worksheets can be used to help clients cope better with symptoms of anxiety ?
There is a wide spectrum of therapeutic approaches that range from self-help activities to guided interventions, and all of them focus on identifying and changing unhelpful thoughts, feelings, and behaviors.
Here are a few of the best-known techniques that can be applied with the right tools.
Identifying cognitive distortions
Recognizing and identifying maladaptive automatic thoughts is a main goal of CBT.
Recognizing and identifying maladaptive automatic thoughts is a main goal of CBT. Cognitive distortions describe inaccurate or exaggerated perceptions, beliefs, and thoughts that can contribute to or increase anxiety, so increasing a client’s awareness of these is the first step to unraveling them and feeling better.
Quenza’s Unhelpful Thinking Styles – “Shoulding” and “Musting” worksheet, shown below, is an example exercise that can help clients recognize the damaging impacts of using “should” and “must” statements to place unreasonable demands or unnecessary pressure on themselves.

Cognitive restructuring
Cognitive restructuring involves disputing the distortions that underpin a client’s challenges. Various techniques that can be helpful here include Socratic questioning, decatastrophizing, and disputing troublesome thoughts with facts.
One example CBT exercise is the Cognitive Restructuring Expansion shown below, which can help clients identify automatic thoughts and substitute them with more fair, rational ways of thinking.

Journaling and thought records
Journaling is a form of self-monitoring that helps clients identify their thought patterns and emotional tendencies, as shown by the Stress Diary Expansion below.

Journals can involve logging negative thoughts or feelings as homework, with the aim of positioning clients to manage them successfully.
Stress Reduction Techniques
Stress reduction exercises such as deep breathing, meditation, and progressive muscle relaxation can all be effective CBT tools for managing anxiety.
The example below is Quenza’s Progressive Muscle Relaxation exercise, which clients can practice to increase their sense of control and calm when stressed or anxious.

Breathing Exercises
Diaphragmatic breathing is another useful relaxation exercise often used in CBT for anxiety.
With this mindfulness practice, clients learn to regulate their breath and activate their body’s relaxation response, as shown in Quenza’s audio Diaphragmatic Breathing exercise below.

CBT Worksheets for Depression (PDF)
CBT worksheets are useful resources for therapists helping clients manage depression, because they can be used to encourage your clients’ progress between sessions.
If you are a mental health professional, the following worksheets can be shared as homework. Each is available as a customizable Quenza Expansion for easy sharing with clients with a $1, 30-day Quenza trial .
The ABC Model of Helpful Behavior
ABC is an acronym for Antecedents, Behavior, and Consequences, and the ABC model proposes that behavior can be learned and unlearned based on association, reward, and punishment.
This CBT worksheet allows clients to reflect on adaptive behavior, thus building their awareness of the triggers for and consequences of this behavior.
After introducing the ABC Model of Behavior and the ABC Model of Helpful Behavior, the exercise asks clients to try it out themselves by:
- Describing a recent personal problem
- Recalling a helpful behavior that they carried out that contributed to the problem in a positive way.
- Recalling the Antecedents of the helpful Behavior – where they were, who they were with, and what they were doing, thinking, and feeling
- Considering the short- and long-term Consequences of that behavior – how they felt, what happened, and what others said or did.
Unhelpful Thinking Styles – Emotional Reasoning
This worksheet invites clients to identify and decrease the negative impact of a specific cognitive bias known as “Emotional Reasoning,” which can be common in clients with depression.
As an introduction, clients learn about the negative impacts of regarding emotions as evidence of the truth, or basing one’s view of situations, yourself, or others on how they feel at a certain moment.
They are then invited to reflect on a time when they used emotional reasoning and describe the situation as well as their thoughts and emotions at the time.
Through self-reflection, this therapy exercise aims to help the user separate their feelings from their thoughts so that they can reduce the negative effect of emotional reasoning on their wellbeing.
De-Catastrophizing
As we’ve seen, patients with symptoms of depression often experience negative thoughts that result from faulty thinking rather than accurate experiences of reality.
Catastrophizing is amplifying the importance of adverse events and situations while minimizing their positive aspects or outcomes. The Decatastrophizing Expansion can be an impactful cognitive restructuring technique to help with this cognitive distortion when it is practiced over time.
Clients are asked to describe the situation that they are currently catastrophizing about before answering a series of questions to challenge their thinking:
- What is the worst that can happen?
- What three events would have to take place for the worst to happen?
- How likely is it that all three of these events will take place?
- What is a more likely outcome, given what you know about the situation?
Here’s an example of the PDF copy that you or your clients can download of these exercises: Decatastrophizing CBT worksheet
To customize these CBT worksheets for depression and browse more, take a look at the $1, 30-day Quenza trial .
Can CBT Help Build Self Esteem?
Studies have shown CBT to be useful in developing a client’s self-esteem so that they start to perceive themselves as more worthy and deserving. [3]
Cognitive restructuring is particularly can equip them with the skills to challenge or refute negative self-talk. This involves:
- Helping clients explore repetitive negative self-talk can be damaging to their sense of self-worth
- Challenging harmful cognitive distortions
- Supporting in the development of a more balanced, positive self-perspective.

Quenza’s Challenging Unhelpful Thoughts , pictured above, is an example CBT worksheet for self-esteem with the following prompts and questions:
- Describe a negative thought that keeps coming back.
- On a scale of 1 to 10, how strongly do you believe this thought to be true?
- What evidence supports this thought?
- What evidence do you have against the thought?
- What would you tell a friend (to help them) who would have the same thought?
Integrating Technology with CBT Worksheets for Enhanced Engagement
The advent of technology has significantly transformed the landscape of psychological treatments, including CBT.
Digital tools and applications can greatly enhance the engagement and effectiveness of CBT worksheets.
Interactive platforms allow clients to complete worksheets on their devices, providing instant feedback and progress tracking.
Additionally, gamification elements, such as rewards for completing tasks or interactive scenarios, can make the therapy process more engaging and motivating for clients.
Teletherapy platforms can integrate these digital worksheets, allowing therapists to monitor their clients’ progress in real time and make adjustments as needed.
Moreover, digital tools often include additional resources like videos, guided meditations, and forums for peer support, which can complement the worksheets and provide a more holistic approach to treatment.
By leveraging technology, therapists can ensure that CBT remains a dynamic and accessible option for clients, regardless of their location or schedule.
CBT Toolbox for Online Therapists
Once you’ve found the most useful tools for your programs and are ready to start treating clients, it’s time to organize them for easy, convenient delivery.
Without a centralized library of digital materials – and the ability to quickly personalize and share them – it’s easy to spend more time than is necessary on the admin side of helping others.
With the right CBT app , you should have an entire toolbox of CBT worksheets plus the tools you need to deliver them:
- Activity design tools: for efficiently creating online CBT interventions
- Customizable templates: e.g., Quenza Expansions that include personalizable science-based exercises and activities
- Documentation tools: e.g., Quenza Notes – A secure, convenient way to create and store session notes and collaborate with clients
- Pathway builder tools: which help you assemble separate worksheets and tools into programs and mental health treatment plans
- Real-time results tracking: to securely collect and store client responses and results
- A free client app: so that clients can easily receive, complete, and return your CBT resources and assemble a library of their finished activities.
Whether you’re new to the world of online therapy or coaching or simply looking to increase your impact, our free 30-page guide is a great place to start.
This PDF will give you an easy-to-understand introduction to the essentials of digital practice: how to create and share your own CBT interventions, keep clients engaged in their treatment, and improve your clients’ results while growing and scaling your business.
Click here to download your copy of Coach, This Changes Everything .

Final Thoughts
Practicing CBT online for the first time may take some adapting, but the ability to help more clients with less work is always worth the payoff.
Hopefully, these worksheets and resources give you a solid starting point for building your CBT toolkit. Let your fellow practitioners know how you use them – leave a comment and join in the conversation below!
- ^ NHS. (2022). Overview - Cognitive behavioural therapy (CBT). Retrieved from https://www.nhs.uk/mental-health/talking-therapies-medicine-treatments/talking-therapies-and-counselling/cognitive-behavioural-therapy-cbt/overview/
- ^ Harvard Health Publishing. (2015). Online cognitive-behavioral therapy: The latest trend in mental health care. Retrieved from https://www.health.harvard.edu/blog/online-cognitive-behavioral-therapy-the-latest-trend-in-mental-health-care-201511048551
- ^ McKay, M., & Fanning, P. (2016). Self-esteem. New Harbinger.
Leave a reply Cancel
Your email address will not be published.

Download free guide (PDF)
Discover how to engage your clients on autopilot while radically scaling your coaching practice.
Coach, This Changes Everything (Free PDF)
.st0{fill:none;stroke:#000;stroke-width:2;stroke-linecap:round;stroke-linejoin:round;stroke-miterlimit:10} Filter
Resource type
Therapy tool.

Cognitive Distortions – Unhelpful Thinking Styles (Extended)
Information handouts

Cognitive Distortions – Unhelpful Thinking Styles (Common)

Assertive Communication

Therapy Blueprint (Universal)

Subjugation
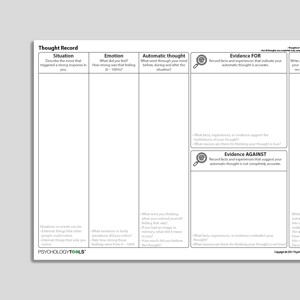
Thought Record (Evidence For And Against)

Embracing Uncertainty

Choosing Your Values

Intolerance Of Uncertainty
Audio Collection: Psychology Tools For Developing Self-Compassion

Insufficient Self-Control

Assertive Responses

Unhelpful Thinking Styles (Archived)

Activity Menu

Valued Domains

Using Behavioral Activation To Overcome Depression

Emotions Motivate Actions

Behavioral Activation Activity Diary

Behavioral Experiment (Portrait Format)

Mistrust/Abuse

Values: Connecting To What Matters

Punitiveness

Abandonment
Evaluating Unhelpful Automatic Thoughts
Compassionate Thought Challenging Record

What Keeps Depression Going?
Behavioral Experiment

Exploring Valued Domains

What Is Rumination?
Audio Collection: Psychology Tools For Mindfulness
CBT Appraisal Model

Failure To Achieve

Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (Second Edition): Client Workbook
Treatments That Work™

Emotional Deprivation

Changing Avoidance (Behavioral Activation)

Understanding Depression

Negative Thoughts - Self-Monitoring Record

Behavioral Activation Activity Planning Diary

Core Belief Magnet Metaphor

Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (Second Edition): Therapist Guide

Emotional Inhibition
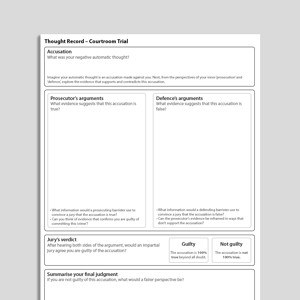
Thought Record – Courtroom Trial

Thought-Action Fusion
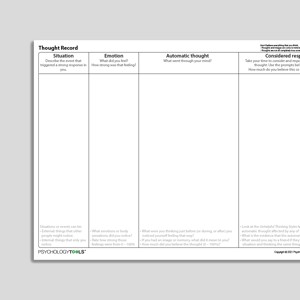
Thought Record (Considered Response)

Social Comparison

Defectiveness
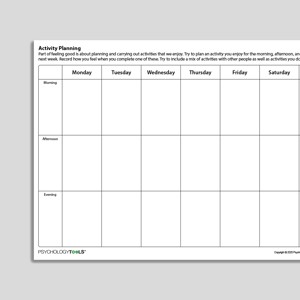
Activity Planning

Emotional Reasoning

Activity Diary (Hourly Time Intervals)

"Should" Statements

Thoughts And Depression
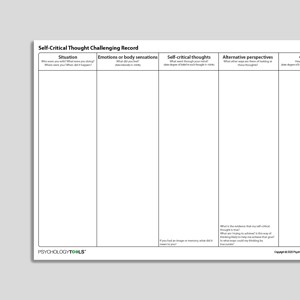
Self Critical Thought Challenging Record
Approval-/Admiration-Seeking
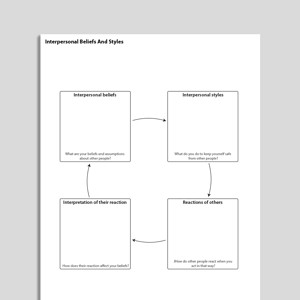
Interpersonal Beliefs And Styles

All-Or-Nothing Thinking

Self-Monitoring Record (Universal)

Boundaries - Self-Monitoring Record

Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)

Dependence / Incompetence

Overcoming Depression (Second Edition): Workbook

Entitlement

Uncertainty Beliefs – Experiment Record

Developing Psychological Flexibility

Catching Your Thoughts (CYP)
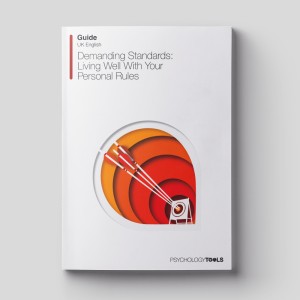
Demanding Standards – Living Well With Your Personal Rules

Discounting In Perfectionism – The Ratchet Effect

Schema Bias
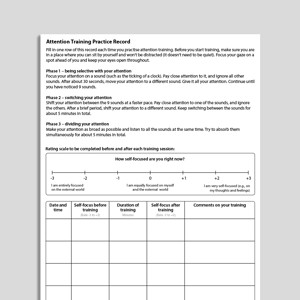

Attention Training Practice Record

A Guide To Emotions (Psychology Tools For Living Well)
Books & Chapters

Disqualifying The Positive

Intrusive Memory Record

What Is Imagery Rescripting?

Overcoming Depression (Second Edition): Therapist Guide

Depression - Self-Monitoring Record

Rumination - Self-Monitoring Record

Being With Difficulty (Audio)

Hindsight Bias

What Is Burnout?
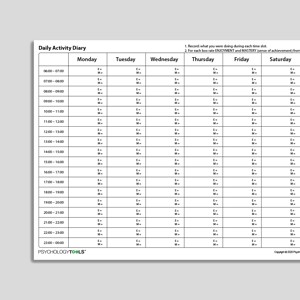
CBT Daily Activity Diary With Enjoyment And Mastery Ratings

Functional Analysis With Intervention Planning
Body Scan (Audio)
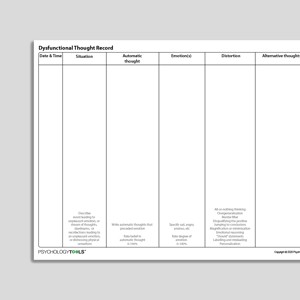
Dysfunctional Thought Record

Mind Reading

Mindfulness Of Breath (Short Version) (Audio)

Externalizing
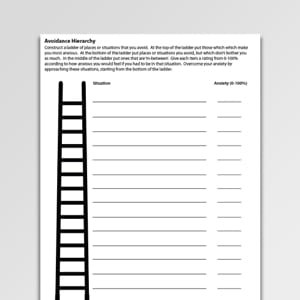
Avoidance Hierarchy (Archived)

Court Trial Thought Challenging Record (Archived)

What Do People Think About Themselves (CYP)?

Challenging Your Negative Thinking (Archived)

Mastery And Pleasure Activity Diary

Mental Filter

Fortune Telling

Magnification And Minimization

Personalizing

Exercise For Mental Health

Disqualifying Others
Links to external resources.
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
- Valued Living Questionnaire (Version 2) | Wilson, Groom | 2002 Download Archived Link
- Scale Download Primary Link Archived Link
- Scale Download Archived Link
- Zimmerman, M., Chelminski, I., McGlinchey, J. B., & Posternak, M. A. (2008). A clinically useful depression outcome scale. Comprehensive psychiatry, 49(2), 131-140.
- Reference Zung, W. W. (1965). A self-rating depression scale. Archives of General Psychiatry, 12(1), 63-70.
- Scale – Adult Download Primary Link Archived Link
- Scale – Child Age 11-17 Download Primary Link Archived Link
- Scale phqscreeners.com Download Primary Link
- Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatric annals, 32(9), 509-515.
- MADRS Score Card Download Archived Link
- Montgomery, S.A., Asberg, M. (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry, 134 (4): 382–89.
- Hamilton M. (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry, 23, 56–62.
- Scale Download Primary Link
- Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782-786.
Case Conceptualization / Case Formulation
- Developing and using a case formulation to guide cognitive behaviour therapy | Persons | 2015 Download Primary Link Archived Link
- Cognitive conceptualisation (excerpt from Basics and Beyond) | J. Beck Download Archived Link
Guides and workbooks
- Mood And Substance Use | NDARC: Mills, Marel, Baker, Teesson, Dore, Kay-Lambkin, Manns, Trimingham | 2011 Download Primary Link
Information Handouts
- What Is Depression? Download Primary Link Archived Link
- What Causes Depression? Download Primary Link Archived Link
- Psychotherapy for Depression Download Primary Link Archived Link
- Vicious Cycle of Depression Download Primary Link Archived Link
- Behavioural Activation: Fun and Achievement Download Primary Link Archived Link
- Fun Activities Catalogue Download Primary Link Archived Link
- Improving How You Feel Download Primary Link Archived Link
- Thinking and Feeling Download Primary Link Archived Link
- Analysing Your Thinking Download Primary Link Archived Link
- Changing Your Negative Thinking Download Primary Link Archived Link
- Unhelpful Thinking Styles Download Primary Link Archived Link
- What Are Core Beliefs? Download Primary Link Archived Link
- Problem Solving Download Primary Link Archived Link
- Staying Healthy Download Primary Link Archived Link
- Grief and Bereavement Download Primary Link Archived Link
Information (Professional)
- Get out of the TRAP and back on TRAC (for rumination and worry) | GoodMedicine Download Primary Link Archived Link
Self-Help Programmes
- Introduction to BA for depression Download Archived Link
- Monitoring Activity And Mood Download Archived Link
- Roadmap: The Activation Plan Download Archived Link
- Finding Direction: Values, Flow, And Strengths Download Archived Link
- Avoidance And Depression TRAPs Download Archived Link
- Thinking Habits Download Archived Link
- Next Steps Download Archived Link
- Module 1: Overview of Depression Download Primary Link Archived Link
- Module 2: Behavioural Strategies for Managing Depression Download Primary Link Archived Link
- Module 3: The Thinking-Feeling Connection Download Primary Link Archived Link
- Module 4: The ABC Analysis Download Primary Link Archived Link
- Module 5: Unhelpful Thinking Styles Download Primary Link Archived Link
- Module 6: Detective Work and Disputation Download Primary Link Archived Link
- Module 7: The End Result Download Primary Link Archived Link
- Module 8: Core Beliefs Download Primary Link Archived Link
- Module 9: Self-Management Download Primary Link Archived Link
- Module 1: Overview Of Depression Download Primary Link
- Module 2: Behavioral Strategies For Managing Depression Download Primary Link
- Module 3: The Thinking-Feeling Connection Download Primary Link
- Module 4: The ABC Analysis Download Primary Link
- Module 5: Unhelpful Thinking Styles Download Primary Link
- Module 6: Detective Work And Disputation Download Primary Link
- Module 7: The End Result Download Primary Link
- Module 8: Core Beliefs Download Primary Link
- Module 9: Self Management Download Primary Link
Treatment Guide
- Depression In Adults: Treatment And Management (NICE Guideline) | NICE | 2022 Download Primary Link
- Behavioural activation treatment for depression (BATD) manual | Lejuez, Hopko & Hopko | 2001 Download Archived Link
- Suicide and self injury: a practitioners guide | Forensic Psychology Practice Ltd | 1999 Download Archived Link
- Behavioural activation treatment for depression – revised (BATD-R) manual | Lejuez, Hopko, Acierno, Daughters, Pagoto | 2011 Download Archived Link
- Metacognitive Training For Depression (D-MCT) Manual | Jelinek, Schneider, Hauschild, Moritz | 2023 Download Primary Link Archived Link
- Module 1: Thinking and reasoning 1 Download Primary Link Archived Link
- Module 2: Memory Download Primary Link Archived Link
- Module 3: Thinking and reasoning 2 Download Archived Link
- Module 4: Self-worth Download Primary Link Archived Link
- Module 5: Thinking and reasoning 3 Download Primary Link Archived Link
- Module 6: Behaviors and strategies Download Primary Link Archived Link
- Module 7: Thinking and reasoning 4 Download Primary Link Archived Link
- Module 8: Perception of feelings Download Primary Link Archived Link
- Cognitive-behavioral therapy for depression in young people: a modular treatment manual | Orygen | 2015 Download Primary Link Archived Link
- Group therapy manual for cognitive behavioral treatment of depression | Muñoz, Miranda | 1993 Download Archived Link
- CBT For Depression In Veterans And Military Service Members – Therapist Manual | Wenzel, Brown, Carlin | 2011 Download Primary Link Archived Link
- Cognitive behaviour therapy for depression in young people: manual for therapists | Improving Mood with Psychoanalytic and Cognitive Therapies (IMPACT) Study CBT Sub-Group | 2010 Download Primary Link Archived Link
- Cognitive-Behavioural Therapy (CBT) Group Program For Depression | Milner, Tischler, DeSena, Rimer Download Primary Link Archived Link
- Manual for group cognitive-behavioral therapy of major depression: a reality management approach (Instructor’s manual) | Muñoz, Ippen, Rao, Le, Dwyer | 2000 Download Primary Link
- Individual therapy manual for cognitive-behavioural treatment of depression | Ricardo Muñoz, Jeanne Miranda | 1996 Download Primary Link Archived Link
- Depression In Adults: Recognition And Management | National Institute for Health and Care Excellence (NICE) guidelines | 2009 Download Primary Link Archived Link
- Symptoms of Depression Download Primary Link Archived Link
- Behavioural Activation Download Primary Link Archived Link
- My Behavioural Antidepressants Download Primary Link Archived Link
- Weekly Activity Schedule Download Primary Link Archived Link
- Weekly Goals Record Download Primary Link Archived Link
- Making the Connection (Between Thoughts and Feelings) Download Primary Link Archived Link
- Thought Diary 1 Download Primary Link Archived Link
- Thought Diary 2 Download Primary Link Archived Link
- Thought Diary 3 Download Primary Link Archived Link
- Thought Diary (Tri-fold) Download Primary Link Archived Link
- Core Beliefs Worksheet Download Primary Link Archived Link
- Healthy Me Download Primary Link Archived Link
- Goal Setting (End of Therapy) Download Primary Link Archived Link
Recommended Reading
- Behavioural activation treatment for depression: returning to contextual roots | Jacobson, Martell, Dimidjian | 2001 Download Primary Link Archived Link
What Is Depression?
Signs and symptoms of depression.
To meet DSM-5 diagnostic criteria for major depressive disorder an individual must have experienced five of the following symptoms for at least two weeks:
- a depressed mood that is present most of the day, nearly every day
- diminished interest in activities which were previously experienced as pleasurable
- fatigue or a loss of energy
- sleep disturbance (insomnia or hypersomnia)
- feelings of worthlessness, self-reproach, or excessive guilt
- a diminished ability to think or concentrate, or indecisiveness
- recurrent thoughts of death or suicide, or suicidal behavior
- changes in appetite marked by a corresponding weight change
- psychomotor agitation or retardation to a degree which is observable by others
Psychological Models and Theory of Depression
Beck’s cognitive theory of depression (Beck, Rush, Shaw, & Emery, 1979) forms the basis for cognitive behavioral approaches for the treatment of depression. Beck’s theory proposes that there are different levels of cognition that can be dysfunctional in depression: core beliefs, rules and assumptions, and negative automatic thoughts. CBT aims to balance negatively biased cognition with more rational and accurate thoughts, beliefs, and assumptions. CBT also systematically aims to increase levels of rewarding activity.
Acceptance and commitment therapy (ACT) proposes that distress, including symptoms of depression, are the result of psychological inflexibility (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). Indicators of psychological inflexibility include:
- ‘buying in’ to negative thoughts and narratives;
- engaging in worry or rumination that takes us away from the present moment;
- losing contact with our values—what is important to us.
Evidence-Based Psychological Approaches for Working with Depression
Many psychological therapies have an evidence base for working with depression:
- Cognitive behavioral therapy (CBT)
- Behavioral activation (BA)
- Acceptance and commitment therapy (ACT)
- Mindfulness-based cognitive therapy (MBCT) for preventing relapse
- Interpersonal therapy (IPT)
Resources for Working with Depression
Psychology Tools resources available for working therapeutically with depression may include:
- psychological models of depression
- information handouts for depression
- exercises for depression
- CBT worksheets for depression
- self-help programs for depression
- Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression . New York: Guilford Press.
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy , 44 (1), 1–25.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Psychiatry
- v.62(Suppl 2); 2020 Jan
Cognitive Behavioral Therapy for Depression
Manaswi gautam.
Consultant Psychiatrist Gautam Hospital and Research Center, Jaipur, Rajasthan, India
Adarsh Tripathi
1 Department of Psychiatry, King George's Medical University, Lucknow, Uttar Pradesh, India
Deepanjali Deshmukh
2 MGM Medical College, Aurangabad, Maharashtra, India
Manisha Gaur
3 Consultant Psychologist, Gaur Mental Health Clinic, Ajmer, Rajasthan, India
INTRODUCTION
Depressive disorders are one of the most common psychiatric disorders that occur in people of all ages across all world regions. Although it may present at any age however adolescence to early adults is the most common age of onset, and females are affected two times more in comparison to the males. Depressive disorders can occur as heterogeneous conditions in clinical scenario ranging from transient minor symptoms to severe and debilitating clinical conditions, causing severe social and occupational impairments. Usually, it presents with constellations of cognitive, emotional, behavioral, physiological, interpersonal, social, and occupational symptoms. The illness can be of various severities, and a significant proportion of the patients can have recurrent illness. Depression is also highly comorbid with several psychiatric and medical illnesses such as anxiety disorders, substance use, obsessive–compulsive disorder, diabetes, hypertension, and cardiovascular illnesses.
Major depressive disorders accounted for around 8.2% global years lived with disability (YLD) in 2010, and it was the second leading cause of the YLDs. In addition, they also contribute to the burden of several other disorders indirectly such as suicide and ischemic heart disease.[ 1 ]
EVIDENCE BASE FOR COGNITIVE BEHAVIORAL THERAPY IN DEPRESSION
Cognitive behavioral therapy (CBT) is one of the most evidence-based psychological interventions for the treatment of several psychiatric disorders such as depression, anxiety disorders, somatoform disorder, and substance use disorder. The uses are recently extended to psychotic disorders, behavioral medicine, marital discord, stressful life situations, and many other clinical conditions.
A sufficient number of researches have been conducted and shown the efficacy of CBT in depressive disorders. A meta-analysis of 115 studies has shown that CBT is an effective treatment strategy for depression and combined treatment with pharmacotherapy is significantly more effective than pharmacotherapy alone.[ 2 ] Evidence also suggests that relapse rate of patient treated with CBT is lower in comparison to the patients treated with pharmacotherapy alone.[ 3 ]
Treatment guidelines for the depression suggest that psychological interventions are effective and acceptable strategy for treatment. The psychological interventions are most commonly used for mild-to-moderate depressive episodes. As per the prevailing situations of India with regards to significant lesser availability of trained therapist in most of the places and patients preferences, the pharmacological interventions are offered as the first-line treatment modalities for treatment of depression.
Indication for Cognitive behavior therapy as enlisted in table 1 .
Indications for cognitive behavioral therapy (situations that can call for preferred use of the psychological interventions) are
| 1. Client’s preference |
| 2. Availability and accessibility of the trained therapist |
| 3. Special situations like children and adolescents, pregnancy, lactation, female in fertile age group planning for pregnancy, medical comorbidities, etc. |
| 4. Inability to tolerate psychopharmacological treatments |
| 5. The presence of significant psychosocial factors, intrapsychic conflicts, and interpersonal difficulties |
CONTRAINDICATIONS FOR COGNITIVE BEHAVIORAL THERAPY
There is no absolute contraindication to CBT; however, it is often reported that clients with comorbid severe personality disorders such as antisocial personality disorders and subnormal intelligence are difficult to manage through CBT. Special training and expertise may be needed for the treatment of these clients.
Patient with severe depression with psychosis and/or suicidality might be difficult to manage with CBT alone and need medications and other treatment before considering CBT. Organicity should be ruled out using clinical evaluation and relevant investigations, as and when required.
There are many advantages of CBT in depression as given in table 2
Advantages of cognitive behavioral therapy in depression
| 1. It is used to reduce symptoms of depression as an independent treatment or in combination with medications |
| 2. It is used to modify the underlying schemas or beliefs that maintain the depression |
| 3. It can be used to address various psychosocial problems, for example, marital discord, job stress which can contribute to the symptoms |
| 4. Reduce the chances of recurrence |
| 5. Increase the adherence to recommended medical treatment |
CHOICE OF TREATMENT SETTINGS
CBT can be done on an Out Patient Department (OPD) basis with regular planned sessions. Each session lasts for about 45 min–1 h depending on the suitability for both patients and therapists. In specific situations, the CBT can be delivered in inpatient settings along with treatment as usual such as adjuvant treatment in severe depression, high risk for self-harm or suicidal patients, patients with multiple medical or psychiatric comorbidities and in patients hospitalized due to social reasons.
ASSESSMENT AND EVALUATION FOR THE THERAPY
A detail diagnostic assessment is needed for the assessment of psychopathology, premorbid personality, diagnosis, severity, presence of suicidal ideations, and comorbidities. Baseline assessment of severity using a brief scale will be helpful in mutual understanding of severity before starting therapy and also to track the progress. Clients during depressive illness often fail to recognize early improvement and undermine any positive change. Objective rating scale hence helps in pointing out the progress and can also help in determining agenda during therapy process. Beck Depression Inventory (A. T. Beck, Steer, and Brown, 1996), the Depression Anxiety Stress Scales (Lovibond and Lovibond, 1995), Montgomery-Asberg Depression Rating Scale, Hamilton Rating Scale for Depression are useful rating scales for this purpose. The assessment for CBT in depression is, however, different from diagnostic assessment.
THE USE OF COGNITIVE BEHAVIORAL THERAPY ACCORDING TO SEVERITY OF DEPRESSION
Various trials have shown the benefit of combined treatment for severe depression.
Combined therapy though costlier than monotherapy it provides cost-effectiveness in the form of relapse prevention.
Number of sessions depends on patient responsiveness.
Booster sessions might be required at the intervals of the 1–12 th month as per the clinical need.
A model for reference is given in table 3
The use of cognitive behavioral therapy according to the severity of depression
| Type of depression | First line | Adjunctive | Number of sessions |
|---|---|---|---|
| Mild | CBT or medication | CBT or medication | 8–12 |
| Moderate | CBT or medication | CBT or medication | 8–16 |
| Severe | Medication or/and Somatic treatment | CBT | 16 or more |
| Chronic depression and recurrent depression | CBT or medication | CBT or medication | 16 or more and booster sessions up to 1–2 years |
The general outline of CBT for depression has been discussed in table 4
Overview of cognitive behavioral therapy for depression
| 1. Mutually agreed on problem definition by therapist and client |
| 2. Goal settings |
| 3. Explaining and familiarizing client with five area model of CBT |
| 4. Improving awareness and understanding on one’s cognitive activity and behavior |
| 5. Modification of thoughts and behavior - using principles of Socratic dialogue, guided discovery, and behavioral experiments/exposure exercise |
| 6. Application and consolidation of new skills and strategies in therapy sessions and homework sessions to generalize it across situations |
| 7. Relapse prevention |
| 8. End of the therapy |
CBT – Cognitive behavioral therapy
COGNITIVE MODEL FOR DEPRESSION
Cognitive theory conceptualizes that people are not influenced by the events rather the view they take of the events. It essentially means that individual differences in the maladaptive thinking process and negative appraisal of the life events lead to the development of dysfunctional cognitive reactions. This cognitive dysfunction is in turn is responsible for the rest of the symptoms in affective and behavioral domains.
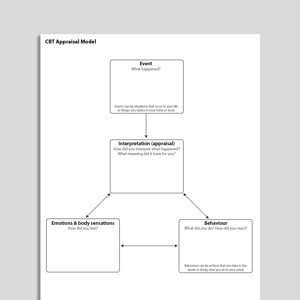
Aaron beck proposed a cognitive model of depression, and it is detailed in Figure 1 . Cognitive dysfunctions are of the following categories.

Cognitive behavioral therapy model of depression
- Schema - stable internal structure of information usually formed during early life, also include core belief about self
- information processing and intermediate belief are usually interpreted as rules of living and usually expressed in terms of “if and then” sentences
- Automatic thoughts - proximally related to everyday events and in depression, often reflects cognitive triad, i.e., negative view of oneself, world, and future.
Negative cognitive triad of depression as given beck is as following:
- I am helpless (helplessness)
- The future is bleak (hopelessness)
- I am worthless (worthlessness).
CHOICE OF THE PATIENT
Patient-related factors that facilitated response are.
- Psychological mindedness of patients: Patients who are able to understand and label their feelings and emotions generally respond better to CBT. Although some patients in the course of treatment learn those skills during treatment
- Intellectual level of the patient might also affect the overall effectiveness of the treatment
- Willingness and motivation on the part of patients: Although it is not prerequisite, patients who are motivated to analyze their feelings and ready to undergo various homework show a better response to treatment
- Patient preference is single most important factor: After initial assessment of the patient those who prefer psychological treatment can be offered CBT alone or in combination depending on type of depression
- Those with mild to moderate depression CBT can be recommended as a first line of treatment
- Patients with severe depression might need combination of both CBT and medications (and or other treatments)
- Special situations such as children and adolescents, pregnancy, lactation, female in fertile age group planning for pregnancy, medical comorbidities
- Inability to tolerate psychopharmacological treatment
- The presence of significant psychosocial factors, intrapsychic conflicts, and interpersonal difficulties.
Therapist related factors
- Availability of cognitive behavioral therapist/psychiatrist
- The ability of therapist to form therapeutic alliance with the patient.
CLINICAL INTERVIEW FOR COGNITIVE BEHAVIORAL THERAPY
Symptoms and associated cognitions.
Negative automatic thoughts both trigger and enhance depression. It might be helpful to identify unhealthy automatic thoughts associated with symptoms of depression.
Some common symptoms and associated automatic thoughts are given in table 5 .
Symptoms of depression and associated cognitions
| Serial number | Symptoms | Automatic thoughts |
|---|---|---|
| 1 | Behavioral: lower activity levels | I cants do it. It is too much for me |
| 2 | Guilt | I am letting everybody down |
| 3 | Shame | What everyone must be thinking about me |
Impact on functioning
it is important to know the extent and effect of depression on the overall functioning and interpersonal relationships.
Coping strategies
Sometimes patients with depression might have adapted a coping strategies which make them feel good for short duration (e.g., alcohol consumption) but might be unhealthy in long term.
Onset of current symptoms
Patient's perception about the situation at the onset of symptoms might provide useful information about underlying cognitive distortions.
Background information
Detailed history of patient is necessary, including patients premorbid personality.
The therapist should be able to do the cognitive case conceptualization for the patient as given in Figure 2 .

Case conceptualization for the cognitive model of depression
MANAGING TREATMENT
An outline of the breakup of typical session of CBT is given in table 6 .
Session structure of cognitive behavioral therapy
| Serial number | Component | Time (min) |
|---|---|---|
| 1 | Beginning of the session | |
| Mood check | 5–10 | |
| Agenda setting | ||
| Reviewing homework | ||
| 2 | Discussion of agenda items/problems | 35–40 |
| Description of occurrence of specific problem | ||
| Elicitation and confirmation of elements of the cognitive model | ||
| Collaborative discussion regarding how to approach a problem | ||
| Rationale for the introduction of intervention | ||
| Assessment of the efficacy of intervention | ||
| Summary by patient | ||
| Collaborative action plan in writing | ||
| Planning and discussing a homework and how to approach it | ||
| 3 | Feedback to the therapist | 1–2 |
Starting treatment
First treatment interview has mainly four objectives:
- To establish a warm collaborative therapeutic alliance
- To list specific problem set and associated goals
- To psycho-educate patient regarding the cognitive model and vicious cycle that maintains the depression
- Give the patient idea about further treatment procedures.
CBT can be explained in the following headings
- Behavioral interventions
Working with negative automatic thoughts
- Ending session.
The first treatment interview has four main objectives:
- To establish a warm, collaborative therapeutic alliance
- To list specific problems and associated goals, and select a first problem to tackle
- To educate the patient about the cognitive model, especially the vicious circle that maintains depression
- To give the patient first-hand experience of the focused, workman-like, empirical style of CBT.
These convey two important messages: (1) It is possible to make sense of depression; (2) there is something the patient can do about it. These messages directly address hopelessness and helplessness.
- Identifying problems and goals:-The various problems faced by patients should be included in a list which can include symptoms of depression or social problems (e.g., family conflict). Developing this list at the end of the first session helps in planning treatment goals
- Introducing cognitive model of depression:- In the first session at least a basic idea about how our cognitions affect our emotions and behavior is taught to the patient. The data provided by patient can be used to give insight into behaviors
- Where to start:-Common treatment goal is agreed upon by patient and therapist, therapeutic alliance is of key importance in CBT. Appropriate homework assignment should be given to patient according to predecided goal.
Behavioural interventions
Reducing ruminations.
It has been seen that depressed patients spend a significant amount of time and attention focusing on their shortcomings. Making patient aware of those negative ruminations and consciously diverting attention toward certain positive aspects can be taught to patients.
Monitoring activities
Loss of interest in day to day activities is central to the depression. It has been seen that early behavioral intervention has been increased sense of autonomy in the patients.
Patients are taught to record each and every activity hour by hour on the activity schedule. Each activity is rated 0–10 for Pleasure (P) and Mastery (M). P ratings indicate how enjoyable the activity was, and M ratings how much of an achievement it was. Mostly depressed patients feel low on achievement all the time. Hence, M should be explained as “achievement how you felt at the time of doing.” Patients are instructed to rate activities immediately and not retrospectively.
Example of activity schedule is
Activity Chart Write in each box, activity performed and depression rating from 0-100% (0-minimal, 100-maximum)
| 6-7 AM | |||||||
| 7-8 AM | |||||||
| 8-9 AM* | Breakfast, talk with wife, 40% | Breakfast alone, 60% | Walk, 30% | Breakfast with son, 50% | Talk with friend on phone, 20% | Breakfast alone, 60% | Breakfast with everyone in family, 20% |
| 10-11 PM | Hourly rating from waking up till time to sleep | What everyone must be thinking about me |
Planning activities
Once the patient learns to self-monitor activities each day is planned in advance.
This helps patients by:
- This provides a structure and helps with setting priorities
- This avoids the need to keep making decisions about what to do next
- This changes perception from chaos to manageable tasks
- This increases the chances that activities will be carried out
- This enhances patients’ sense of control.
A plan for activities is made in such a way that both pleasure and mastery are balanced (e.g., ironing cloths followed by listening to music). The tasks which are generally avoided by patient can be divided into graded tasks.
The patient is taught to evaluate each and every day in detail also encouraged to keep the record of unhelpful negative thoughts regarding tasks.
Other important behavioral activities are:-
- Mindfulness meditation: Helps people stay grounded in the present by keeping away from ruminations
- Successive approximation: Breaking larger tasks into smaller tasks which are easy to accomplish
- Visualizing the best part of the day
- Pleasant activity scheduling.
Scheduling an activity in near future which one can look on with mastery and with sense of achievement.
The main tool for this negative automatic thought record.
Thought Record -1
| Situation (write down exact details of specific situation) | Emotions (Rate 0-100%) | Behaviour | Physical reactions | Automatic thoughts/ images (Identify most important thought) |
Thought Record – 2
| Situation (write down exact details of specific situation) | Emotions (Rate 0-100%) | Automatic thoughts/ images (Identify most important thought) | Evidence for automatic thoughts | Evidence against automatic thoughts | Balanced thought | Rate emotion now (0-100%) |
Identifying negative automatic thoughts
Patients learn to record upsetting incidents as soon as possible after they occur (delay makes it difficult to recall thoughts and feelings accurately). They learn:
- To identify unpleasant emotions (e.g., despair, anger, guilt), signs that negative thinking is present. Emotions are rated for intensity on a 0–100 scale. These ratings (though the patient may initially find them difficult) help to make small changes in emotional state obvious when the search for alternatives to negative thoughts begins. This is important since change is rarely all-or-nothing, and small improvements may otherwise be missed
- To identify the problem situation. What was the patient doing or thinking about when the painful emotion occurred (e.g., “waiting at the supermarket checkout,” “worrying about my husband being late home”)?
- To identify negative automatic thoughts associated with the unpleasant emotions. Sessions direct the therapist towards asking: “And what went through your mind at that moment?” Patients become aware of thoughts, images, or implicit meanings that are present when emotional shifts occur, and record. Belief in each thought is also rated on a 0%–100%.
Questioning negative automatic thoughts
Therapist can help patient to discover dysfunctional automatic thoughts through “guided discovery.”
- What is evidence?
- What are alternative views?
- What are advantages and disadvantages of this way of thinking?
- What are my thinking biases?
Common cognitive distortions are
- Black– and– white (also called all– or– nothing, polarized, or dichotomous thinking): Situations viewed in only two categories instead of on a continuum. Example: “If I don’t top the exams. I’m a failure”
- Fortune-telling (also called catastrophizing): Future is predicted negatively without considering other possible, more likely outcomes. Example: “I ll be so upset, i won’t be able to function at all”
- Disqualifying or discounting the positive: The person unreasonably tell oneself that positive experiences, deeds, or qualities do not count. Example: “I cracked the examl, but that doesn’t mean I’m competent; It was a fluke”
- Emotional reasoning: One thinks something must be true because he/she “feels” (actually believe) it so strongly, ignoring or discounting evidence to the contrary. Example: “I know I successfully complete most of my tasks, but I still feel like I’ m incompetent”
- Labeling: One puts a fixed, global label on oneself or others without considering that the evidence might more reasonably lead to a less disastrous conclusion. Example: “I’m a failure. He's not good enough”
- Magnification/minimization: When one evaluates oneself, another person, or a situation, one unreasonably magnifies the negative and/or minimizes the positive. Example: “Getting a C Grade in exams proves how mediocre I am. Getting high marks doesn’t mean I’m smart”
- Selective abstraction (also called mental filter): One pays undue attention to one's negative detail instead of seeing the whole picture. Example: “Because I got just passing marks in one subject in my examinations (which also contained distinctions in other subjects) it means I’m not a good student”
- Mind reading: One believes that he/she knows what others are thinking, failing to consider other, more likely possibilities. Example: “He assumes that his boss thinks that he is a novice for this assignment”
- Overgeneralization: One makes a negative conclusion that goes far beyond the current situation. Example: “(Because I felt uncomfortable at the meeting) I don’t have what it takes to be a group leader”
- Personalization: O ne believes others are behaving negatively because of him/her, without exploring alternative explanations for their behavior. Example: “The watchman didn’t smile at me because I did something wrong”
- Imperatives (also called “Should” and “must” statements): One has a precise, fixed idea of how one or others should behave, and they overestimate how bad it is that these expectations are not met with. Example: “It's terrible that I sneeze as I am a Gym Trainer”
- Tunnel vision: One only views the negative aspects of a situation. Example: “My subordinate can’t do anything right. He's callous, casual and insensitive towards his job.”
Testing negative automatic thoughts: What can I do now?
It is important that cognitive changes that are brought out by questioning are consolidated by behavior experiments.
Ending the treatment
CBT is time-limited goal-directed form of therapy. Hence, the patient is made aware about end of treatment in advance. This can be done through the following stages.
Dysfunctional assumptions identification
Consolidating learning blueprint.
- Preparation for the setback.
Once the patient is able to identify negative automatic thoughts. Before ending treatment patient patients should be made aware about dysfunctional assumptions.
- Where did this rule come from? Identifying the source of a dysfunctional assumption (e.g., parental criticism) often helps to encourage distance by suggesting that its development is understandable, though it may no longer be relevant or useful
- In what ways is the rule unrealistic? Dysfunctional assumptions do not fit the way the world works. They operate by extremes, which are reflected in their language (always/never rather than some of the time; must/should/ought rather than want/prefer/would like)
- In what ways is the rule helpful? Dysfunctional assumptions are not usually wholly negative in their effects. For example, perfectionism may lead to genuine, high-quality performance. If such advantages are not recognized and taken into account when new assumptions are formulated, the patient may be reluctant to move forward
- In what ways is the rule unhelpful? The advantages of dysfunctional assumptions are normally outweighed by their costs. Perfectionism leads to rewards, but it also undermines satisfaction with achievements and stops people learning from constructive criticism
- What alternative rule might be more realistic and helpful? Once the old assumption has been undermined, it is helpful to formulate an explicit alternative (e.g., "It is good to do things well, but I am only human-sometimes I make mistakes"). This provides a new guideline for living, rather than simply undermining the old system
- What needs to be done to consolidate the new rule? As with negative automatic thoughts, re-evaluation is best made real through experience: Behavioral experiments.
The patient should be able to summarize whatever he has learned throughout the sessions.
The following questions might help to set the framework:
- How did my problems develop? (unhelpful beliefs and assumptions, the experiences that led to their formation, events precipitating onset)
- What kept them going? (maintenance factors)
- What did I learn from therapy that helped? Techniques (e.g., activity scheduling) and Ideas (e.g., "I can do something to influence my mood")
- What were my most unhelpful negative thoughts and assumptions? What alternatives did I find to them? (summarized in two columns)
- How can I build on what I have learned? (a solid, practical, clearly specified action plan).
Preparation for the setback
Since depression is recurring illness patient should be made aware about the possibility of relapse.
- What might lead to a setback for me? For example, future losses (e.g., children leaving home) and stresses (e.g., financial difficulties), i.e., events which impinge on patients’ vulnerabilities and are thus liable to be interpreted negatively
- What early warning signs do I need to be alert for?
- Feelings, behaviors, and symptoms that might indicate the beginning of another depression are identified and listed
- If I notice that I am becoming depressed again, what should I do? Clear simple instructions, which will make sense despite low mood, are needed here. Specific ideas and techniques summarized earlier in the blueprint should be referred to.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
How to Design Homework in CBT That Will Engage Your Clients

Take-home assignments provide the opportunity to transfer different skills and lessons learned in the therapeutic context to situations in which problems arise.
These opportunities to translate learned principles into everyday practice are fundamental for ensuring that therapeutic interventions have their intended effects.
In this article, we’ll explore why homework is so essential to CBT interventions and show you how to design CBT homework using modern technologies that will keep your clients engaged and on track to achieving their therapeutic goals.
Before you continue, we thought you might like to download our three Positive CBT Exercises for free . These science-based exercises will provide you with a detailed insight into positive CBT and give you the tools to apply it in your therapy or coaching.
This Article Contains:
Why is homework important in cbt, how to deliver engaging cbt homework, using quenza for cbt: 3 homework examples, 3 assignment ideas & worksheets in quenza, a take-home message.
Many psychotherapists and researchers agree that homework is the chief process by which clients experience behavioral and cognitive improvements from CBT (Beutler et al., 2004; Kazantzis, Deane, & Ronan, 2000).
We can find explanations as to why CBT homework is so crucial in both behaviorist and social learning/cognitive theories of psychology.
Behaviorist theory
Behaviorist models of psychology, such as classical and operant conditioning , would argue that CBT homework delivers therapeutic outcomes by helping clients to unlearn (or relearn) associations between stimuli and particular behavioral responses (Huppert, Roth Ledley, & Foa, 2006).
For instance, imagine a woman who reacts with severe fright upon hearing a car’s wheels skidding on the road because of her experience being in a car accident. This woman’s therapist might work with her to learn a new, more adaptive response to this stimulus, such as training her to apply new relaxation or breathing techniques in response to the sound of a skidding car.
Another example, drawn from the principles of operant conditioning theory (Staddon & Cerutti, 2003), would be a therapist’s invitation to a client to ‘test’ the utility of different behaviors as avenues for attaining reward or pleasure.
For instance, imagine a client who displays resistance to drawing on their support networks due to a false belief that they should handle everything independently. As homework, this client’s therapist might encourage them to ‘test’ what happens when they ask their partner to help them with a small task around the house.
In sum, CBT homework provides opportunities for clients to experiment with stimuli and responses and the utility of different behaviors in their everyday lives.
Social learning and cognitive theories
Scholars have also drawn on social learning and cognitive theories to understand how clients form expectations about the likely difficulty or discomfort involved in completing CBT homework assignments (Kazantzis & L’Abate, 2005).
A client’s expectations can be based on a range of factors, including past experience, modeling by others, present physiological and emotional states, and encouragement expressed by others (Bandura, 1989). This means it’s important for practitioners to design homework activities that clients perceive as having clear advantages by evidencing these benefits of CBT in advance.
For instance, imagine a client whose therapist tells them about another client’s myriad psychological improvements following their completion of a daily thought record . Identifying with this person, who is of similar age and presents similar psychological challenges, the focal client may subsequently exhibit an increased commitment to completing their own daily thought record as a consequence of vicarious modeling.
This is just one example of how social learning and cognitive theories may explain a client’s commitment to completing CBT homework.
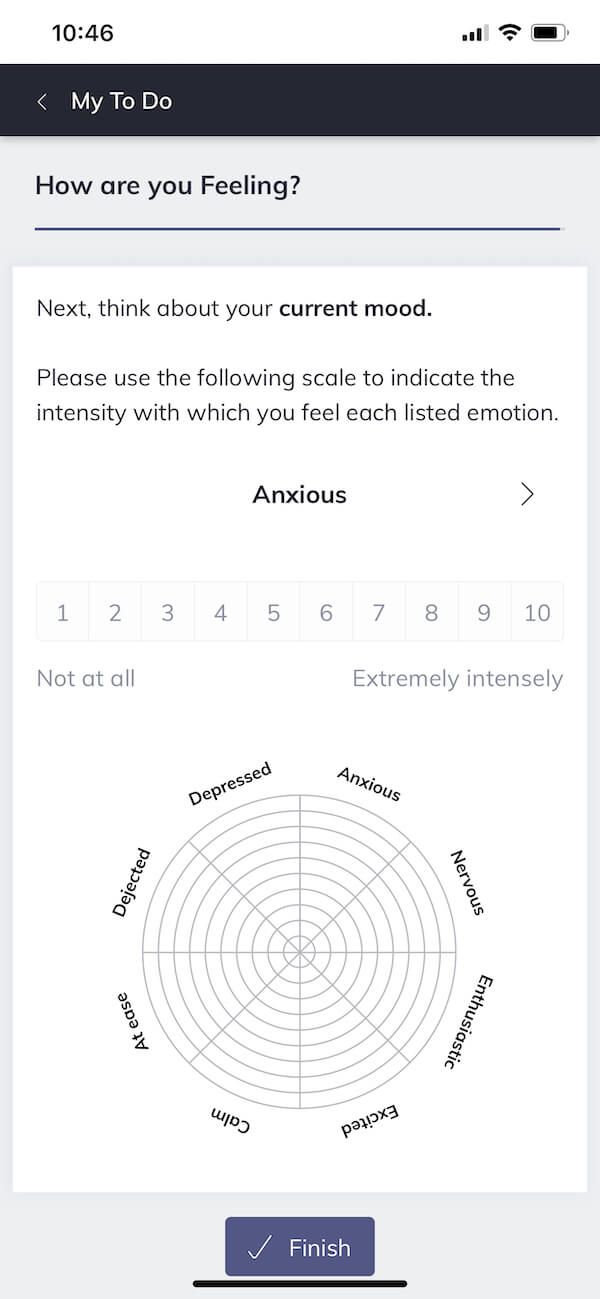
Let’s now consider how we might apply these theoretical principles to design homework that is especially motivating for your clients.
In particular, we’ll be highlighting the advantages of using modern digital technologies to deliver engaging CBT homework.
Designing and delivering CBT homework in Quenza
Gone are the days of grainy printouts and crumpled paper tests.
Even before the global pandemic, new technologies have been making designing and assigning homework increasingly simple and intuitive.
In what follows, we will explore the applications of the blended care platform Quenza (pictured here) as a new and emerging way to engage your CBT clients.
Its users have noted the tool is a “game-changer” that allows practitioners to automate and scale their practice while encouraging full-fledged client engagement using the technologies already in their pocket.
To summarize its functions, Quenza serves as an all-in-one platform that allows psychology practitioners to design and administer a range of ‘activities’ relevant to their clients. Besides homework exercises, this can include self-paced psychoeducational work, assessments, and dynamic visual feedback in the form of charts.
Practitioners who sign onto the platform can enjoy the flexibility of either designing their own activities from scratch or drawing from an ever-growing library of preprogrammed activities commonly used by CBT practitioners worldwide.
Any activity drawn from the library is 100% customizable, allowing the practitioner to tailor it to clients’ specific needs and goals. Likewise, practitioners have complete flexibility to decide the sequencing and scheduling of activities by combining them into psychoeducational pathways that span several days, weeks, or even months.
Importantly, reviews of the platform show that users have seen a marked increase in client engagement since digitizing homework delivery using the platform. If we look to our aforementioned drivers of engagement with CBT homework, we might speculate several reasons why.
- Implicit awareness that others are completing the same or similar activities using the platform (and have benefitted from doing so) increases clients’ belief in the efficacy of homework.
- Practitioners and clients can track responses to sequences of activities and visually evidence progress and improvements using charts and reporting features.
- Using their own familiar devices to engage with homework increases clients’ self-belief that they can successfully complete assigned activities.
- Therapists can initiate message conversations with clients in the Quenza app to provide encouragement and positive reinforcement as needed.
The rest of this article will explore examples of engaging homework, assignments, and worksheets designed in Quenza that you might assign to your CBT clients.
Download 3 Free Positive CBT Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to find new pathways to reduce suffering and more effectively cope with life stressors.
Download 3 Free Positive CBT Tools Pack (PDF)
By filling out your name and email address below.
Let’s now look at three examples of predesigned homework activities available through Quenza’s Expansion Library.
Urge Surfing
Many of the problems CBT seeks to address involve changing associations between stimulus and response (Bouton, 1988). In this sense, stimuli in the environment can drive us to experience urges that we have learned to automatically act upon, even when doing so may be undesirable.
For example, a client may have developed the tendency to reach for a glass of wine or engage in risky behaviors, hoping to distract themselves from negative emotions following stressful events.
Using the Urge Surfing homework activity, you can help your clients unlearn this tendency to automatically act upon their urges. Instead, they will discover how to recognize their urges as mere physical sensations in their body that they can ‘ride out’ using a six-minute guided meditation, visual diagram, and reflection exercise.
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Moving From Cognitive Fusion to Defusion
Central to CBT is the understanding that how we choose to think stands to improve or worsen our present emotional states. When we get entangled with our negative thoughts about a situation, they can seem like the absolute truth and make coping and problem solving more challenging.
The Moving From Cognitive Fusion to Defusion homework activity invites your client to recognize when they experience a negative thought and explore it in a sequence of steps that help them gain psychological distance from the thought.
Finding Silver Linings
Many clients commencing CBT admit feeling confused or regretful about past events or struggle with self-criticism and blame. In these situations, the focus of CBT may be to work with the client to reappraise an event and have them look at themselves through a kinder lens.
The Finding Silver Linings homework activity is designed to help your clients find the bright side of an otherwise grim situation. It does so by helping the user to step into a positive mindset and reflect on things they feel positively about in their life. Consequently, the activity can help your client build newfound optimism and resilience .

As noted, when you’re preparing homework activities in Quenza, you are not limited to those in the platform’s library.
Instead, you can design your own or adapt existing assignments or worksheets to meet your clients’ needs.
You can also be strategic in how you sequence and schedule activities when combining them into psychoeducational pathways.
Next, we’ll look at three examples of how a practitioner might design or adapt assignments and worksheets in Quenza to help keep them engaged and progressing toward their therapy goals.
In doing so, we’ll look at Quenza’s applications for treating three common foci of treatment: anxiety, depression, and obsessions/compulsions.
When clients present with symptoms of generalized anxiety, panic, or other anxiety-related disorders, a range of useful CBT homework assignments can help.
These activities can include the practice of anxiety management techniques, such as deep breathing, muscle relaxation, and mindfulness training. They can also involve regular monitoring of anxiety levels, challenging automatic thoughts about arousal and panic, and modifying beliefs about the control they have over their symptoms (Leahy, 2005).
Practitioners looking to support these clients using homework might start by sending their clients one or two audio meditations via Quenza, such as the Body Scan Meditation or S.O.B.E.R. Stress Interruption Mediation . That way, the client will have tools on hand to help manage their anxiety in stressful situations.
As a focal assignment, the practitioner might also design and assign the client daily reflection exercises to be completed each evening. These can invite the client to reflect on their anxiety levels during the day by responding to a series of rating scales and open-ended response questions. Patterns in these responses can then be graphed, reviewed, and used to facilitate discussion during the client’s next in-person session.
As with anxiety, there is a range of practical CBT homework activities that aid in treating depression.
It should be noted that it is common for clients experiencing symptoms of depression to report concentration and memory deficits as reasons for not completing homework assignments (Garland & Scott, 2005). It is, therefore, essential to keep this in mind when designing engaging assignments.
CBT assignments targeted at the treatment of depressive symptoms typically center around breaking cycles of negative events, thinking, emotions, and behaviors, such as through the practice of reappraisal (Garland & Scott, 2005).
Examples of assignments that facilitate this may include thought diaries , reflections that prompt cognitive reappraisal, and meditations to create distance between the individual and their negative thoughts and emotions.
To this end, a practitioner looking to support their client might design a sequence of activities that invite clients to explore their negative cognitions once per day. This exploration can center on responses to negative feedback, faced challenges, or general low mood.
A good template to base this on is the Personal Coping Mantra worksheet in Quenza’s Expansion Library, which guides clients through the process of replacing automatic negative thoughts with more adaptive coping thoughts.
The practitioner can also schedule automatic push notification reminders to pop up on the client’s device if an activity in the sequence is not completed by a particular time each day. This function of Quenza may be particularly useful for supporting clients with concentration and memory deficits, helping keep them engaged with CBT homework.
Obsessions/compulsions
Homework assignments pertaining to the treatment of obsessive-compulsive disorder typically differ depending on the stage of the therapy.
In the early stages of therapy, practitioners assigning homework will often invite clients to self-monitor their experience of compulsions, rituals, or responses (Franklin, Huppert, & Roth Ledley, 2005).
This serves two purposes. First, the information gathered through self-monitoring, such as by completing a journal entry each time compulsive thoughts arise, will help the practitioner get clearer about the nature of the client’s problem.
Second, self-monitoring allows clients to become more aware of the thoughts that drive their ritualized responses, which is important if rituals have become mostly automatic for the client (Franklin et al., 2005).
Therefore, as a focal assignment, the practitioner might assign a digital worksheet via Quenza that helps the client explore phenomena throughout their day that prompt ritualized responses. The client might then rate the intensity of their arousal in these different situations on a series of Likert scales and enter the specific thoughts that arise following exposure to their fear.
The therapist can then invite the client to complete this worksheet each day for one week by assigning it as part of a pathway of activities. A good starting point for users of Quenza may be to adapt the platform’s pre-designed Stress Diary for this purpose.
At the end of the week, the therapist and client can then reflect on the client’s responses together and begin constructing an exposure hierarchy.
This leads us to the second type of assignment, which involves exposure and response prevention. In this phase, the client will begin exploring strategies to reduce the frequency with which they practice ritualized responses (Franklin et al., 2005).
To this end, practitioners may collaboratively set a goal with their client to take a ‘first step’ toward unlearning the ritualized response. This can then be built into a customized activity in Quenza that invites the client to complete a reflection.
For instance, a client who compulsively hoards may be invited to clear one box of old belongings from their bedroom and resist the temptation to engage in ritualized responses while doing so.
17 Science-Based Ways To Apply Positive CBT
These 17 Positive CBT & Cognitive Therapy Exercises [PDF] include our top-rated, ready-made templates for helping others develop more helpful thoughts and behaviors in response to challenges, while broadening the scope of traditional CBT.
Created by Experts. 100% Science-based.
Developing and administering engaging CBT homework that caters to your client’s specific needs or concerns is becoming so much easier with online apps.
Further, best practice is becoming more accessible to more practitioners thanks to the emergence of new digital technologies.
We hope this article has inspired you to consider how you might leverage the digital tools at your disposal to create better homework that your clients want to engage with.
Likewise, let us know if you’ve found success using any of the activities we’ve explored with your own clients – we’d love to hear from you.
We hope you enjoyed reading this article. For more information, don’t forget to download our three Positive CBT Exercises for free .
- Bandura, A. (1989). Human agency in social cognitive theory. American Psychologist , 44 (9), 1175–1184.
- Beutler, L. E., Malik, M., Alimohamed, S., Harwood, T. M., Talebi, H., Noble, S., & Wong, E. (2004). Therapist variables. In M. J. Lambert (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change (5th ed.) (pp. 227–306). Wiley.
- Bouton, M. E. (1988). Context and ambiguity in the extinction of emotional learning: Implications for exposure therapy. Behaviour Research and Therapy , 26 (2), 137–149.
- Franklin, M. E., Huppert, J. D., & Roth Ledley, D. (2005). Obsessions and compulsions. In N. Kazantzis, F. P. Deane, K. R., Ronan, & L. L’Abate (Eds.), Using homework assignments in cognitive behavior therapy (pp. 219–236). Routledge.
- Garland, A., & Scott, J. (2005). Depression. In N. Kazantzis, F. P. Deane, K. R., Ronan, & L. L’Abate (Eds.), Using homework assignments in cognitive behavior therapy (pp. 237–261). Routledge.
- Huppert, J. D., Roth Ledley, D., & Foa, E. B. (2006). The use of homework in behavior therapy for anxiety disorders. Journal of Psychotherapy Integration , 16 (2), 128–139.
- Kazantzis, N. (2005). Introduction and overview. In N. Kazantzis, F. P. Deane, K. R., Ronan, & L. L’Abate (Eds.), Using homework assignments in cognitive behavior therapy (pp. 1–6). Routledge.
- Kazantzis, N., Deane, F. P., & Ronan, K. R. (2000). Homework assignments in cognitive and behavioral therapy: A meta‐analysis. Clinical Psychology: Science and Practice , 7 (2), 189–202.
- Kazantzis, N., & L’Abate, L. (2005). Theoretical foundations. In N. Kazantzis, F. P. Deane, K. R., Ronan, & L. L’Abate (Eds.), Using homework assignments in cognitive behavior therapy (pp. 9–34). Routledge.
- Leahy, R. L. (2005). Panic, agoraphobia, and generalized anxiety. In N. Kazantzis, F. P. Deane, K. R., Ronan, & L. L’Abate (Eds.), Using homework assignments in cognitive behavior therapy (pp. 193–218). Routledge.
- Staddon, J. E., & Cerutti, D. T. (2003). Operant conditioning. Annual Review of Psychology , 54 (1), 115–144.
Share this article:
Article feedback
Let us know your thoughts cancel reply.
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

The Positive CBT Triangle Explained (+11 Worksheets)
Cognitive behavioral therapy (CBT) is a popular and highly effective intervention model for dealing with multiple mental health conditions (Early & Grady, 2017; Yarwood et [...]

Fundamental Attribution Error: Shifting the Blame Game
We all try to make sense of the behaviors we observe in ourselves and others. However, sometimes this process can be marred by cognitive biases [...]

Halo Effect: Why We Judge a Book by Its Cover
Even though we may consider ourselves logical and rational, it appears we are easily biased by a single incident or individual characteristic (Nicolau, Mellinas, & [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (21)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (37)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (39)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)
3 Positive CBT Exercises (PDF)
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
What's the Difference Between DBT and CBT?
:max_bytes(150000):strip_icc():format(webp)/JoyEmehsheadshot1-JoyEmeh-ef67f56eb29e4a81a9f66d80745aea82.jpg)
- Similarities
- Differences
- How To Choose
Olga Rolenko / Getty Images
Experts estimate that more than one in five adults in the United States live with a mental health condition with varying degrees of severity. These mental health conditions require treatment, and healthcare providers recommend therapies like dialectical behavior therapy (DBT) or cognitive behavioral therapy (CBT) to help you feel better.
CBT and DBT are two forms of psychotherapy or talk therapy where you work with a mental health provider to gain more insight about yourself, understand your condition, and learn skills that help you cope with and manage your symptoms.
While CBT and DBT share some similarities, they are two different therapeutic approaches to treating conditions like anxiety, depression, personality disorders, and posttraumatic stress disorder (PTSD).
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) combines two therapeutic approaches—cognitive therapy and behavioral therapy—to identify harmful or destructive thinking patterns and replace them with positive or more desirable ones. The concept behind CBT is that the way you feel, your behavior, your thoughts, and how other people make you feel are all interconnected and affect your mental health.
Distressing thought patterns and negative conclusions about things or people can cause you to feel bad about yourself, unhappy, depressed, rejected, and isolated. CBT uses different techniques to teach you to face your fears, identify those negative thoughts, find solutions to manage them, focus on the solutions, and develop a greater sense of confidence in your own abilities.
Unlike therapies like psychoanalysis, which is interested in dealing with your past and understanding why you have negative or intrusive thoughts in the first place, CBT is more problem-oriented and is focused on helping you deal with your current issues as soon as possible. This form of therapy has been effective in treating mental health-related conditions like:
- Substance use disorder (SUD)
- Obsessive-compulsive disorder (OCD)
- Marital challenges
People with physical conditions, such as rheumatism, tinnitus , and chronic pain, may also benefit from CBT, as there's evidence that therapy can help some people manage physical symptoms.
Dialectical Behavioral Therapy
Dialectical behavior therapy (DBT) is an evidence-based treatment specially adapted for people who experience emotions intensely. While this treatment was developed based on the principles of CBT, it emphasizes fixing emotional dysregulation .
Instead of focusing on changing atypical or maladaptive behaviors, thoughts, and feelings, DBT encourages you to be realistic about your thoughts, accept them as they are, and teach you healthy coping mechanisms in the process.
Most therapists who practice DBT teach their clients strategies like how to cope with stress, be mindful, regulate their emotions , live in the moment, and form healthy relationships with others. They may employ techniques like:
- Individual psychotherapy: One-on-one face-to-face (in-person or online) sessions with your therapist
- Telephone consultation: Sessions with your therapist via phone call
- Skills training group: Learning skills like emotional regulation and mindfulness in a group setting
DBT is the only treatment effective in treating borderline personality disorder (BPD), a mental health condition that causes long-term patterns of unstable moods, difficulty maintaining relationships, and turbulent emotions.
It may also help treat other mental health conditions like generalized anxiety disorder (GAD), bipolar disorder, schizophrenia, substance use disorder (SUD), and eating disorders.
Similarities Between DBT and CBT
DBT is considered a modified form of CBT, as it uses the principles of CBT. So, both therapies share some overlapping strategies and techniques. DBT and CBT both:
- Rely on the basic principle that people's behavior, cognition, and emotions are interlinked
- Believe that changing disruptive behaviors can significantly reduce emotional distress
- Teach coping skills and management strategies
- Focus on the present experience (rather than past traumas) to deal with current challenges
Key Differences Between DBT and CBT
The goals and principles of CBT and DBT are similar, but some differences are evident in the actual techniques and strategies that both therapies adopt.
CBT focuses on changing people’s beliefs and thoughts, while DBT focuses on emotional regulation. Unlike CBT, DBT also addresses mindfulness , interpersonal relationships, and distress tolerance (managing difficult situations).
Mode of Approach
CBT views dysfunctional behaviors, thoughts, and feelings as “unhelpful” and tries to change them or help people build skills to redirect those thoughts. This approach can make it hard for people to accept their beliefs as reasonable or real.
DBT, on the other hand, incorporates the concept of radical acceptance and validation. Your thoughts and behaviors are not judged, but you learn to accept and tolerate painful thoughts and situations.
Suitable Applications
DBT is more strongly recommended for people with self-destructive behaviors, intense emotion dysregulation, and strong urges for self-harm. Healthcare providers recommend people living with borderline personality disorder try DBT first.
CBT is the first line of treatment for most other mental health conditions (such as substance use disorder, depression, and anxiety) and is a more popular treatment option than DBT.
Therapy Time-Frame
While there is no “standard” duration of treatment for mental health conditions, CBT is often considered more of a short-term treatment, as sessions are usually once a week and last about 12 weeks on average. DBT, however, is often a year-long (or longer) intensive treatment.
How To Choose the Right Therapy
CBT and DBT are both effective treatments for mental health conditions. However, your healthcare provider will work with you to determine which therapy option is best for you. The ideal therapy will depend on your specific condition, its symptoms, their severity, and what you want to achieve from your treatment. In some cases, therapists can combine aspects of CBT and DBT together to best fit your needs.
For instance, DBT was originally designed for treating borderline personality disorder and is recommended for treating people with ongoing suicidal or self-harm behaviors. It may also be ideal for you if you are experiencing intense emotional dysregulation. On the other hand, CBT may be best suited for you if you want to understand how your thinking patterns may affect your life and want to work on them to overcome your life’s stressors.
To learn which therapy is right for you:
- Have an honest and open discussion with your healthcare provider. They can talk to you about your symptoms and treatment goals and refer you to a therapist.
- Search for a therapist on the Clinical Resource Directory or American Psychological Association Psychologist Locator.
- Explore local sources, such as asking someone you trust for a recommendation or using your school’s counseling center.
A Quick Review
Cognitive behavior therapy and dialectical behavior therapy are both evidence-based interventions that help treat different mental health conditions, such as depression, anxiety, and post-traumatic stress disorder.
There are several similarities, but CBT focuses on recognizing and reframing negative thoughts and behaviors. DBT encourages you to accept your thoughts and behaviors and learn healthy ways to cope with your emotions.
If you're interested in either form of therapy, it's important to choose a mental health professional you trust, one who is a good match for you, and one with whom you are comfortable.
:max_bytes(150000):strip_icc():format(webp)/sr-a21a100afbf343f481150ff49b3a733e.jpeg)
National Institute of Mental Health. Mental illness .
Bass C, van Nevel J, Swart J. A comparison between dialectical behavior therapy, mode deactivation therapy, cognitive behavioral therapy, and acceptance and commitment therapy in the treatment of adolescents . International Journal of Behavioral Consultation and Therapy . 2014;9(2):4-8. doi:10.1037/h0100991
InformedHealth.org [Internet]. In brief: Cognitive behavioral therapy (CBT) . Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2022.
American Psychological Association. What is Cognitive Behavioral Therapy? .
Nourisaeed A, Ghorban-Shiroudi S, Salari A. Comparison of the effect of cognitive-behavioral therapy and dialectical behavioral therapy on perceived stress and coping skills in patients after myocardial infarction . ARYA Atherosclerosis . 2021;17(2):1-9. doi:10.22122/arya.v17i0.2188
May JM, Richardi TM, Barth KS. Dialectical behavior therapy as treatment for borderline personality disorder . The Mental Health Clinician . 2016;6(2):62-67. doi:10.9740/mhc.2016.03.62
Linehan MM, Wilks CR. The Course and Evolution of Dialectical Behavior Therapy . American Journal of Psychotherapy. 2015;69(2):91-239. doi:10.1176/appi.psychotherapy.2015.69.2.97
Afshari B, Jafarian Dehkordi F, Asgharnejad Farid AA, et al. Study of the effects of cognitive behavioral therapy versus dialectical behavior therapy on executive function and reduction of symptoms in generalized anxiety disorder . Trends in Psychiatry and Psychotherapy. 2022;44:e20200156. doi:10.47626/2237-6089-2020-0156
Røysamb E, Kendler KS, Tambs K, et al. The joint structure of DSM-IV Axis I and Axis II disorders . Journal of Abnormal Psychology . 2011;120(1):198-209. doi:10.1037/a0021660
Substance Abuse and Mental Health Services Administration. DSM-5 Changes: Implications for Child Serious Emotional Disturbance . In: Substance Abuse and Mental Health Services Administration (US); 2016.
McMain SF, Chapman AL, Kuo JR. et al. The effectiveness of 6 versus 12-months of dialectical behaviour therapy for borderline personality disorder: the feasibility of a shorter treatment and evaluating responses (FASTER) trial protocol . BMC Psychiatry 2018;18(230). doi:10.1186/s12888-018-1802-z
Related Articles
- Open access
- Published: 31 August 2024
Effectiveness of a cognitive behavioural therapy (CBT)-based intervention for reducing anxiety among adolescents in the Colombo District, Sri Lanka: cluster randomized controlled trial
- Sinha De Silva ORCID: orcid.org/0000-0003-4578-5019 1 ,
- Renuka Peris 2 ,
- Sudharshi Senaviratne 3 &
- Dulani Samaranayake 4
Child and Adolescent Psychiatry and Mental Health volume 18 , Article number: 108 ( 2024 ) Cite this article
Metrics details
Anxiety disorders are found to be the most prevalent psychological problems among children and adolescents. Cognitive behaviour therapy (CBT) was found to be effective at reducing anxiety. The purpose of this study was to assess the effectiveness of a universal school-based intervention for reducing anxiety among Grade 9 schoolchildren. A randomized controlled cluster trial was conducted by randomly assigning 36 schools in the Colombo district in Sri Lanka into study and control arms, each comprising 18 schools with 360 students. The levels of anxiety, self-esteem and depression status were assessed using the validated Screen for Child Anxiety Related Disorders (SCARED) tool and the Rosenberg self-esteem scale, respectively, and the Depression, Anxiety and Stress Scale 21 (DASS-21) at baseline, after intervention, and after 3 months. A CBT-based universal intervention package was administered weekly by a trained teacher for eight weeks with a one-month self-practice period to a randomly selected Grade 9 class in each school in the study arm. The control arm received routine care. Anxiety and self-esteem scores and depression status were compared between the two arms after the intervention and at 3 months of follow-up using the generalized estimation equation (GEE), controlling for confounding and clustering. The nonresponse and loss to follow-up rates were < 1%. When comparing the study arm with the control arm using GEE, anxiety levels were significantly lower [β = (-0.096), 95% CI = (-0.005) − (-0.186), p = 0.038] at follow-up but not postintervention [β = (-0.024), 95% CI = 0.006 − (-0.055), p = 0.115]. There were no significant differences in depression status after intervention (OR = 0.257, 95% CI =0.052–1.286; p = 0.098) or follow-up (OR = 0.422, 95% CI 0.177–1.008; p = 0.052), and self-esteem significantly increased after intervention (β = 0.811, 95% CI = 0.314–1.309; p = 0.001) but not at follow-up [β=0.435, 95% CI=(-0.276)-1.145, p=0.231]. This study revealed that the universal package based on CBT is effective at reducing anxiety and improving self-esteem among adolescents. The trial registration number and date were SLCTR/2018/018 and 19th of June 2018 respectively.
Introduction
Anxiety is defined as the anticipation of upcoming threats and is associated with muscle tension and vigilance in preparation for future danger and continuous or avoidant behavior [ 1 ]. It is recognized as a normal adaptive response to a stimulus that one will try to avoid. It is a brain response to something that is happening or might happen in the future. Anxiety becomes pathological, regardless of the individual’s age, when it is persistent or excessive and associated with subjective distress or impairment [ 2 ]. Individuals with any anxiety disorder (AD) may exhibit similar psychological, physical, and behavioral characteristics. These disorders are categorized based on the object or situation that induces fear, anxiety, and/or distress and avoidance behavior [ 2 ].
Anxiety disorders are the most prevalent form of psychopathology among adolescents [ 3 , 4 , 5 ]. Despite notable variations in prevalence estimates, likely due to methodological differences, the lifetime prevalence of ‘any anxiety disorder’ in studies with children or adolescents is approximately 15–20%. Period prevalence estimates, such as 1-year or 6-month rates, are not considerably lower than lifetime estimates [ 2 ]. A longitudinal study revealed significant linear associations between having anxiety disorders in adolescence and developing a range of adverse outcomes in early adulthood, including mental health problems like major depression, nicotine dependence, alcohol dependence, illicit drug dependence, and suicidal behavior [ 6 ].
Behavioral therapy plays a pivotal role in preventing and managing anxiety disorders. A review by Compton et al. (2004) of 21 randomized controlled trials concluded that cognitive behavioral therapy (CBT) is the treatment of choice for anxiety in children and adolescents, showing medium to large effect sizes for symptom reduction. CBT is favored due to its lack of adverse side effects, withdrawal problems, and association with a lower rate of subsequent relapse. Additionally, CBT can enhance self-esteem and foster an increased sense of agency [ 7 , 8 ].
Anxiety prevention measures can be directed at individuals or groups. Evidence suggests that group-targeted preventive measures are more effective than those targeting individuals. Prevention programs targeting a group may be universal, selective, or indicated. Universal interventions are directed at the entire population regardless of risk status. Selective interventions involve people identified as at risk for psychological problems, while indicated interventions target those identified as having mild to moderate symptoms. Universal prevention strategies include elements of primordial, primary, secondary, and tertiary prevention, whereas selective programs focus on primary prevention, and indicated programs concentrate on secondary prevention [ 9 ].
There are several benefits associated with universal prevention programs compared to selective and targeted programs. Universal interventions can address people with limited access to treatment, ensuring no one is omitted. People with limited access to treatment show low dropout rates, which can help avoid the stigma associated with participating in selective or targeted interventions [ 9 ]. A systematic review of universal interventions for reducing anxiety and depressive symptoms in school-aged children revealed small but significant effects on reducing these symptoms. The goal of prevention is to reduce the likelihood of future negative outcomes by reducing relevant risk factors and strengthening protective factors [ 10 ]. When developed as prevention programs, these programs are designed to build skills rather than provide therapy, meaning strategies are learned for common situations rather than specific individual difficulties [ 11 ].
Despite the established effectiveness of school-based interventions for reducing anxiety, there is a scarcity of evidence, particularly in Southeast Asia. The importance of this study becomes increasingly evident when considering the unique interaction between interventions designed to reduce anxiety and contextual factors influencing their efficacy. These factors play a central role, particularly in educational settings characterized by distinct regional attributes. The educational environments of our region have unique characteristics that can significantly impact the effectiveness of these interventions. Therefore, it is crucial to conduct this intervention study tailored to our specific context. By doing so, we can gain a deeper understanding of how these unique environmental characteristics influence anxiety reduction strategies, allowing us to fine-tune the intervention in a contextually relevant manner.
This study was conducted to assess the effectiveness of a universal CBT-based intervention for reducing anxiety among adolescents in Sri Lanka. The study was carried out in the Sri Jayewardenepura Education Zone in the Colombo district, targeting Grade 9 schoolchildren. We employed a randomized controlled cluster trial, randomly assigning 36 schools into intervention and control arms. The intervention, delivered by trained teachers, consisted of eight weekly CBT sessions followed by a one-month practice period. Outcomes were assessed using validated tools at baseline, post-intervention, and three months follow-up.
By focusing on the effectiveness of a universal CBT-based intervention within the unique cultural and educational context of Sri Lanka, this study aims to provide insights into how contextual factors influence anxiety reduction strategies, thereby enhancing the relevance and applicability of the intervention in similar settings.
Materials and methods
Study design and participants.
We conducted a randomized controlled multicenter trial in the Sri Jayewardenepura Education Zone in the Colombo district, Sri Lanka. The target population was children in grade nine (aged 13–15 years). Each school was considered a cluster, and a randomly selected class of nine grades was selected from each school for the study. The average number of students per group was 20. The sample size and number of groups for each arm were decided using a formula proposed by Hayes Moulton (2017) for an individually randomized trial with inflation for the design effect for a cluster randomized trial [ 12 ]. The values for the true mean and standard deviation of the outcome variable in the presence (µ 1 = 7.35, σ 1 = 6.93) and absence (µ 0 = 9.58, σ 0 = 6.44) of intervention were informed by Barrett and Turner (2001) in their study on reducing anxiety using a CBT-based package. For alpha (Z α ) and beta (Z β ) errors, the values used were Z α = 1.96 for α = 0.05 and Z β = 0.84 for β = 0.80 [ 13 ]. According to Shackleton et al. (2016), the ICC for psychological outcomes ranges from 0.01 to 0.07; we used the higher end of this range, setting ICC (ρ) at 0.07 to maximize sample size [ 14 ]. All Sinhala medium schools with year nine classes were invited to participate in the study; 37 schools agreed upon the study, and one school withdrew prior to randomization. A total of 720 students from 36 schools and their parents provided assent and informed written consent, respectively.
The trial was registered in the Sri Lanka Clinical Trial Register (SLCTR/2018/018) and was approved by the Ethics Review Committee of the Faculty of Medicine, University of Kelaniya (P/19/01/2018). Administrative approval was obtained from the Ministry of Education, Sri Lanka.
Randomization and masking
The consented schools were stratified by school gender type, i.e., male, female, or mixed. Within each stratum, schools were randomized to the universal intervention group based on CBT or the control group using the block randomization method to ensure allocation of schools in a 1:1 ratio to two groups (Fig. 1 ). Schools, students, and the research team were masked in the allocation.
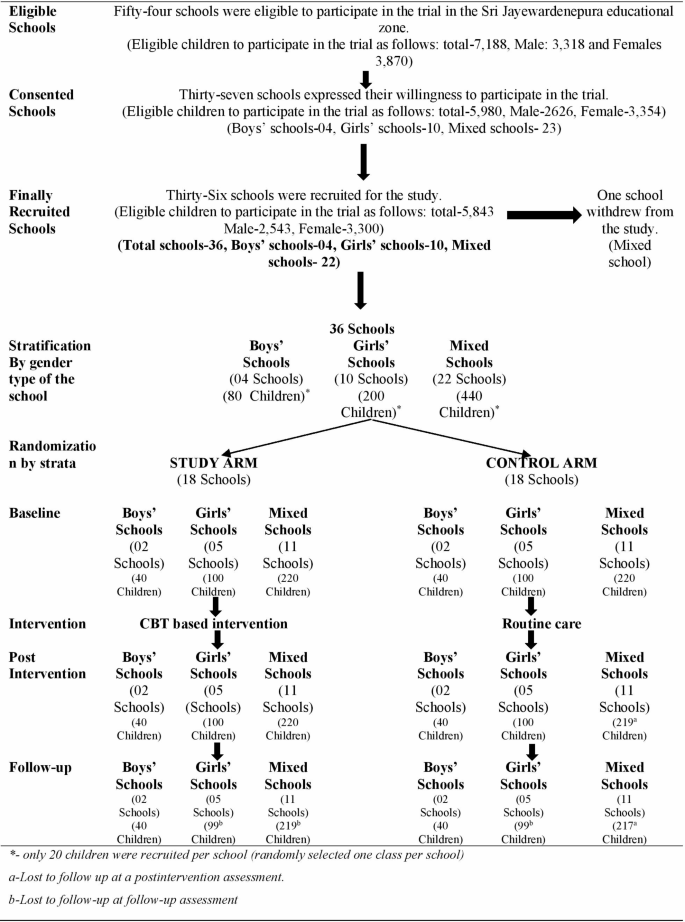
Student progress through the trial– CONSORT flow chart
Intervention arm
Schools that were randomized into the intervention arm received a universal CBT-based intervention package that was developed based on the UK Medical Research Council guidance by De Silva et al. [ 15 ]. The intervention was delivered by a teacher who underwent a comprehensive training program covering CBT principles, specific techniques, and strategies for engaging students. To ensure consistency, the training included role-playing exercises, peer reviews, and feedback sessions. Teachers were provided with a detailed handbook outlining session plans and activities. The delivery of the intervention was monitored using a fidelity monitoring framework involving regular supervision by experienced mental health professionals. Teachers submitted weekly reports, and random observations were conducted to assess adherence to the intervention protocol. Any deviations were addressed through additional support and training, aiming to minimize variations and maintain the integrity of the intervention across different schools. Each teacher delivered the intervention package to randomly selected classes in the intervention arm in a 40-minute session per week for eight consecutive weeks and for a subsequent one-month duration to practice what they learned. An additional session was arranged for students who missed a session prior to the next session. During these eight sessions, the children were trained in CBT-based skills that were aimed at reducing anxiety and relaxing. The outline of the intervention package is shown in Table 1 , and its details are published elsewhere by De Silva et al. (2023) [ 15 ]. They were instructed to practice these skills under the close and distant supervision of the teacher.
A 40-minute session was held for parents by the same teachers, overlapping with the routine parent meeting. Parents were educated about anxiety, anxiety disorders, how to identify them, and how to adapt to reduce anxiety. This session aimed to support parents in practicing the anxiety reduction skills learned by their children at home. Materials included the Teachers’ Handbook, the Workbook for Children, and a monitoring tool for students’ practice, along with a leaflet for parents. The intervention was monitored using the process evaluation framework (PEF) at the school level [ 15 ]. The PEF of the intervention group is provided in Additional File 1 Table S1 .
We acknowledge the potential for performance bias due to the lack of blinding among intervention deliverers and participants. While blinding presents challenges in school-based interventions, several measures were taken to minimize bias and ensure the study’s internal validity. The rigorous training, monitoring procedures, and use of validated assessment tools, such as the SCARED tool for anxiety and the Rosenberg self-esteem scale, helped reduce subjective bias. Despite the difficulties in implementing blinding, these steps significantly contributed to the robustness of our findings. Future studies should explore feasible blinding strategies to further strengthen internal validity.
Control arm
Routine schoolwork was carried out in randomly selected classes from the control arm. The participants were assessed at baseline, after the intervention, and at follow-up.
Outcomes and measures
Both groups were assessed at baseline using a self-administered questionnaire consisting of sociodemographic questions, a tool to measure the level of anxiety, the state of depression, and the level of self-esteem. The participants’ level of anxiety, depression status and self-esteem were assessed postintervention, as well as at three months of follow-up, using the same tools as follows.
Level of anxiety
The child version of the Screen for Child Anxiety Related Disorders (SCARED) is a 41-item instrument rated on a 3-point Likert scale. This instrument has been validated for assessing children aged 8–18 years [ 16 , 17 ]. The translated and validated questionnaire, which has high reliability according to Cronbach’s alpha (0.87) and test-retest correlation coefficient (0.74), was used to assess the level of anxiety [ 18 ]. A higher score indicates a greater level of anxiety.
Status of depression
Depression scales of the validated DAS-21 questionnaire were used in the local setting among adolescents by Weerasinghe in 2012. This approach has been validated for use in Sinhalese adolescents, as it has good psychometric properties. All the subscales had good reliability (Cronbach’s alpha > 0.7). Its cut-off value for the depression subscale was 19, with a sensitivity = 80% and specificity = 83%. [ 19 ]. The state of depression was determined using this tool.
Self-esteem
The Rosenburg self-esteem instrument was validated for use among adolescents internationally. The NRS-2002 is a 10-item scale that measures global self-worth by measuring both positive and negative feelings about the self. The scale is believed to be unidimensional. All the items are answered using a four-point Likert scale ranging from strongly agreeing to strongly disagreeing. The scores were on a continuous scale ranging from 10 to 40. A higher score indicates greater self-esteem [ 20 , 21 ].
Statistical analysis
All the analyses were based on intention-to-treat principles. All baseline categorical variables are presented as numbers and percentages, and all numerical variables are presented as the means and standard deviations (Table 2 ). As the first step of the pre specified statistical analysis plan (SAP), all the outcome variables were compared between two groups using conventional statistics with their effect sizes. Those results are presented in the (Additional File 1 Table S2 to Table S4 ).
The outcome variables were analysed to determine the effectiveness of the intervention using marginal linear regression with coefficients estimated by the generalized estimating equation (GEE). This approach allowed us to control for the effect of clustering and adjust for imbalanced covariates and probable confounders identified at the beginning of the study. Specifically, we considered several covariates and confounding variables, including sex, age, ethnicity, religion, permanent and current residence, school functional type, attendance at tuition classes, engagement in extracurricular activities, having siblings, anxiety sensitivity, behavioral inhibition, mother’s level of education, mother’s and father’s occupation, and perceived parenting style of the mother. By adjusting for these covariates, we aimed to isolate the effect of the intervention from other factors that might affect anxiety, depression, and self-esteem levels among the participants, thereby minimizing bias and improving the internal validity of our findings. The marginal models allow the effect of the explanatory variables on the outcome, and the correlation between observations is modelled separately. Each outcome variable was analysed after the intervention and at the follow-up; in other words, separate marginal models were used for each outcome variable after the intervention and at the follow-up. Only the relevant anxiety levels from the outcome tables are shown here (Tables 3 and 4 ), and the anxiety levels for depression status and self-esteem are shown in the supplementary material. In each marginal model, the scores of the outcome variable were used as the dependent variable, the arm of the study (intervention or control), the baseline value of the outcome variable and the baseline covariates that needed to be adjusted were used as predictors. Clusters were used as subjects to control for the nested/cluster effect. SPSS 22 was used for the data analysis.
Thirty-six clusters were recruited, and all the clusters remained throughout the study. Clusters were randomized into intervention and control arms as shown in Fig. 1 . At the initial assessment before the beginning of the study, there were 720 students in both arms. At the postintervention assessment, only one student in the control arm was lost to follow-up, which was a 99.86% ( n = 719) response rate. At the end of the three-month follow-up, only two students were lost to follow-up in the intervention arm, and four were lost to follow-up in the control arm (99.16%; n = 714). At both points of measurement, less than 0.9% of the patients were lost to follow-up. A comparison of the baseline sociodemographic and other selected characteristics between the study arm and the control arm was performed as follows (Table 2 ):
The standardized mean difference (Cohen’s d) between the levels of anxiety in the two groups at post-intervention was calculated to be 0.12. The estimated regression coefficients of a marginal model with robust standard error to show the effects of the intervention arm on the outcome, the SCARED Child Sinhala score postintervention, after adjustment for the baseline SCARED Child score and other selected covariates/factors while controlling for the clustering effect are shown in Table 3 .
The standardized mean difference (Cohen’s d) between the levels of anxiety in the two groups at follow-up was calculated to be 0.32.The estimated regression coefficient of a marginal model with robust standard error was used to show the effects of the intervention arm on the outcome, the SCARED Child score at follow-up, after adjustment for the baseline SCARED Child score, and other selected covariates/factors controlling for the clustering effect (Table 4 ).
The standardized mean differences (Cohen’s d) in depression levels between the intervention and control groups were 0.04 at post-intervention and 0.06 at follow-up. The generalized estimating equation was used with clusters as the subject variables, a robust estimator as the covariance matrix, AR as the working correlation matrix structure, a binomial logit as the ordinal response under the type of model, and predictors that included the arm of the intervention, baseline DASS-21 Depression Scale score at baseline and some selected covariates. The status of depression, that is, having or not having depression at the postintervention time point and follow-up, was assessed as the dependent variable in two separate models (Additional File 1 Table S5 and Table S6 ). The results suggest that the study arm participants had lower odds of having depression after the intervention time point, with an OR of 0.257 (95% CI 0.05–1.27) and an OR of 0.422 (95% CI 0.177–1.008) at the follow-up time point than did the control arm participants; however, these differences were not statistically significant, with p = 0.098 and p = 0.052, respectively, when adjustments were made for imbalance correlates/confounders at baseline and for the effect of clustering in two separate models.
Level of self-esteem
The standardized mean differences (Cohen’s d) in self-esteem levels between the intervention and control groups were 0.3 at post-intervention and 0.2 at follow-up. The regression coefficients were estimated from two different marginal models with robust standard errors to show the effects of the intervention on the Rosenberg self-esteem scale scores after the intervention and at follow-up after adjustment for the Rosenberg self-esteem scale scores at baseline and other selected covariates/factors while controlling for the cluster effect (Additional File 1 Table S7 and Table S8 ). The results suggest that the participants in the study arm had significantly greater Rosenberg self-esteem scale scores at the postintervention time point (i.e., high self-esteem) (0.811 points; 95% CI = 0.314 to 1.309, p = 0.001) than did the participants in the control arm; however, the participants in the study arm had greater Rosenberg self-esteem scale scores at the follow-up time point (i.e., high self-esteem) [0.435; 95% CI = (-0.276) to 1.145] than did the participants in the control arm did, but it was not statistically significant, as the p value was 0.231 when adjustments were made for imbalanced correlates at baseline and for the effect of clustering.
We examined the effectiveness of teacher-provided universal CBT-based interventions for reducing anxiety among adolescents in a school setting. The loss to follow-up was minimal, and good compliance with the intervention was reported. The baseline variables were comparable between the two arms.
There was a reduction in the level of anxiety (SCARED Child score) after the intervention and at the follow-up, but it was statistically significant only at the follow-up in the intervention arm compared to the control arm. Depression status was also reduced in the intervention arm than in the control arm at both postintervention and follow-up. The level of self-esteem (the Rosenberg self-esteem tool score) was greater in the intervention arm than in the control arm at both postintervention and follow-up but was statistically significant only at postintervention assessment.
A systematic review by Corrieri et al. 2014 of 28 RCTs conducted after the year 2000 in which outcomes were measured as continuous variables with self-reported instruments, focusing on school-based prevention interventions for anxiety and depression with the aim of exploring their effectiveness, revealed that 15 studies [ 10 ] were reported to be effective (73%), and 16 (67%) out of 24 studies reported effective outcomes for anxiety and depression [ 22 ]. Furthermore, Werner-Seidler et al. (2017) revealed that psychological program-based interventions are effective at reducing anxiety and depression after intervention and at follow-up in a systematic review that included 81 studies with 31,794 participants [ 23 ]. Similar findings to those of the present study were explored in a cluster randomized controlled trial with a universal school-based intervention based on CBT administered in 10 weekly sessions among 638 children aged 9–12 years in 14 schools in Germany, where anxiety level was assessed using a self-reported instrument (SCAS). A statistically significant reduction in anxiety was observed at follow-up ( p < 0.05) but not postintervention [ 24 ].
Despite the fact that CBT-based interventions were effective at significantly reducing the level of depression, as shown by systematic reviews, the present study did not show a significant effect on reducing depression. Furthermore, a reduction in the level of depression was shown in the intervention arm, and a follow-up arm comparison became nonsignificant at p = 0.52. These differences may be due to an inadequate sample size for detecting changes with respect to the level of depression.
Like in the current study, a CBT-based RCT conducted by Amin et al. (2020) among 76 adolescents aged 13–16 years in Pakistan with a study arm and a control arm, with the objective of evaluating its effectiveness in increasing self-esteem using the Rosenberg self-esteem scale for outcome evaluation, revealed a statistically significant increase in self-esteem levels in the study arm compared to the control arm ( p < 0.001) [ 25 ].
Therefore, it could be concluded that the findings of the present intervention study align with the global literature. Furthermore, from a practical point of view, the importance of this study is manifold. First and foremost, it was carried out by the teachers themselves, seamlessly integrating into the existing educational framework. This approach not only emphasizes the feasibility of the study but also highlights its minimal intrusion into the regular schedule, preserving the quality of academic hours. In addition, the enthusiastic participation of students serves as a testament to the study’s engagement and relevance to their needs. The fact that the tool was well received by the student body not only adds to its credibility but also demonstrates its practical value in real-world educational settings. In essence, this study provides an example of how educational research can be conducted effectively and efficiently, with direct benefits for both educators and students. Therefore, universal CBT-based interventions are effective at reducing anxiety and increasing self-esteem among schoolchildren in Sri Lanka.
In order to address the delay in achieving statistical significance, it is important to consider multiple contributing factors. While the time taken by participants to practice learned skills is a key element, other potential influences must be acknowledged. Individual differences in response to the intervention, such as varying levels of baseline anxiety and differing capacities for skill acquisition and application, likely played a role. Contextual factors, including the school environment and external stressors, may have impacted the effectiveness of the intervention. Additionally, methodological limitations, such as potential biases in self-report measures and the challenges of maintaining consistency across different school settings, could have influenced the outcomes. Recognizing these factors provides a more comprehensive understanding of the intervention’s effectiveness over time and highlights areas for future research to further optimize CBT-based interventions in similar contexts. Also, in view of addressing the discrepancy in detecting changes in depression levels, several factors need to be considered. The intensity and duration of the intervention might not have been sufficient to produce a measurable effect on depression within the study period. Future research should explore longer intervention durations, increased intensity, and tailored approaches to address depression more effectively in similar populations.
The observed improvement in self-esteem among participants in the intervention arm can be attributed to several factors inherent in CBT techniques, which are particularly relevant within the cultural and educational context of Sri Lanka. CBT emphasizes the identification and restructuring of negative thought patterns, leading to a more positive self-view and enhanced self-esteem. In the Sri Lankan context, where students often face high academic pressures and societal expectations, learning to manage stress and develop a healthier cognitive outlook can significantly impact their self-esteem. Additionally, the group-based nature of the intervention facilitated peer support and interaction, providing a sense of community and shared experience among students. This is particularly important in the collectivist culture of Sri Lanka, where community and social relationships play a crucial role in individual well-being. The involvement of teachers, who are respected authority figures, in delivering the intervention likely contributed to its effectiveness by reinforcing the importance and credibility of the skills being taught. Future research should continue to explore these dimensions to further optimize the effectiveness of CBT-based interventions in diverse settings.
Conclusions
Universal CBT-based interventions delivered by schoolteachers are effective at reducing anxiety and increasing self-esteem among schoolchildren. The observed improvements, although statistically significant, reflect a modest effect size, indicating that while the intervention is beneficial, its impact may vary among individuals. The sustainability of these effects over the long term remains a crucial area for further research, as continued practice and reinforcement of CBT skills are likely necessary to maintain these benefits.
From a practical standpoint, this approach can be easily incorporated into existing educational systems with minimal external resources, making it a feasible and scalable option for improving mental health at the school level. However, implementing such interventions in real-world settings presents challenges, including ensuring fidelity to the intervention protocol, providing adequate training and support for teachers, and addressing varying levels of resource availability across different schools. Future studies should focus on these aspects to enhance the practicality and effectiveness of CBT-based interventions in diverse educational contexts.
Limitations
The study acknowledged several limitations. Performance bias due to the lack of blinding among intervention deliverers and participants was a potential issue, despite measures taken to minimize it. The sample size may have been inadequate to detect significant changes in depression levels. The delay in achieving statistical significance could be attributed to multiple factors, including the time taken by participants to practice learned skills, individual differences in response to the intervention, contextual factors such as the school environment and external stressors, and methodological limitations like potential biases in self-report measures and consistency challenges across different school settings. Additionally, the intensity and duration of the intervention might not have been sufficient to produce measurable effects on depression within the study period. The sustainability of the intervention’s effects over the long term remains uncertain, requiring continued practice and reinforcement of CBT skills. Finally, practical challenges in implementing such interventions in real-world settings include ensuring fidelity to the intervention protocol, providing adequate training and support for teachers, and addressing varying levels of resource availability across different schools.
Availability of data and materials
The data that support the findings of this study is available from the authors upon reasonable request.
Roehr B. American psychiatric association explains dsm-5. BMJ. 2013;346. https://www.bmj.com/content/346/bmj.f3591 . Accessed 23 Jan 2024.
Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524 accessed on 23rd of January 2024.
Article PubMed PubMed Central Google Scholar
Bell-Dolan DJ, Last CG, Strauss CC. Symptoms of anxiety disorders in normal children. J Am Acad Child Adolesc Psychiatry. 1990;29(5):759–65 Accessed on 23rd of January 2024.
Article PubMed CAS Google Scholar
Bernstein GA, Borchardt CM, Perwien AR. Anxiety disorders in children and adolescents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1996;29(5):759–65 accessed on 23rd of January 2024.
Google Scholar
Kashani JH, Orvaschel H. A community study of anxiety in children and adolescents. Am J Psychiatry. 1990;147(3):313–8. https://pubmed.ncbi.nlm.nih.gov/2309948/ . Accessed on 23rd of January 2024.
Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001;40(9):1086–93 accessed on 23rd of January 2024.
Otto MW, Henin A, Hirshfeld-Becker DR, Pollack MH, Biederman J, Rosenbaum JF. Posttraumatic stress disorder symptoms following media exposure to tragic events: impact of 9/11 on children at risk for anxiety disorders. J Anxiety Disord. 2007;21(7):888–902. https://pubmed.ncbi.nlm.nih.gov/17276653/ . Accessed on 23rd of January 2024.
Article PubMed Google Scholar
Wehry AM, Beesdo-Baum K, Hennelly MM, Connolly SD, Strawn JR. Assessment and treatment of anxiety disorders in children and adolescents. Curr Psychiatry Rep. 2015;17(7):52. https://pubmed.ncbi.nlm.nih.gov/25980507/ . Accessed 23 Jan 2024.
Haggerty RJ, Mrazek PJ. Reducing risks for mental disorders: frontiers for preventive intervention research. National Academies; 1994. https://pubmed.ncbi.nlm.nih.gov/25144015/ . Accessed on 23rd of January 2024. URL.
Coie JD, Miller-Johnson S, Bagwell C. Prevention science. Handbook of developmental psychopathology. URL: Springer; 2000. pp. 93–112. https://eclass.edc.uoc.gr/modules/document/file.php/DEA101/Handbook%20of%20Developmental%20Psychopathology%20%282014%2C%20Springer%20US%29.pdf . Accessed on 23rd of January 2024.
Lowry-Webster HM, Barrett PM, Lock S. A universal prevention trial of anxiety symptomology during childhood: results at 1-year follow-up. Behav Change. 2003;20(1):25. https://psycnet.apa.org/record/2003-08839-003 . Accessed on 23rd of January 2024.
Article Google Scholar
Hayes RJ, Moulton LH. Cluster randomized trials. CRC press; 2017. URL: https://www.taylorfrancis.com/books/mono/10.4324/9781315370286/cluster-randomised-trials-richard-hayes-lawrence-moulton
Barrett P, Turner C. Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial. Br J Clin Psychol. 2001;40(4):399–410.
Shackleton N, Hale D, Bonell C, Viner RM. Intraclass correlation values for adolescent health outcomes in secondary schools in 21 European countries. SSM-population Health. 2016;2:217–25.
Article PubMed PubMed Central CAS Google Scholar
De Silva S, Seneviratne S, Samaranayake D. Development of a complex public health intervention to reduce the anxiety of children aged 13–15 years attending government Sinhala Medium Schools in Colombo District, Sri Lanka. IJPSAT. 2023;39(2):49–59. https://ijpsat.org/index.php/ijpsat/article/view/5444 . Accessed on 23rd of January 2024.
Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–53 Accessed on 23rd of January 2024.
Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–6. https://pubmed.ncbi.nlm.nih.gov/10517055/ . Accessed 23rd Jan 2024.
De Silva S, Senevirathne S, Samaranayake D. Screen for child anxiety related disorders (SCARED)-child version: validity and reliability assessment among children aged 13–15 years. JCCPSL. 2022;28(2):583–91 Accessed on 23rd of January 2024.
Weerasinghe W. Adaptation and validation of DASS 21 for use in Sri Lanka among adolescents. Colombo: PGIM; 2012.
Franck E, De Raedt R, Barbez C, Rosseel Y. Psychometric properties of the Dutch Rosenberg self-esteem scale. Psychol Belg. 2008;48(1):25–35. https://psychologicabelgica.com/articles/10.5334/pb-48-1-25 .
Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg self-esteem scale: overall and across demographic groups living within the United States. Eval Health Prof. 2010;33(1):56–80 Accessed on 23rd of January 2024.
Corrieri S, Heider D, Conrad I, Blume A, König HH, Riedel-Heller SG. School-based prevention programs for depression and anxiety in adolescence: a systematic review. Health Promot Int. 2014;29(3):427–41. https://pubmed.ncbi.nlm.nih.gov/23376883/ . Accessed on 24th of January 2024.
Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev. 2017;51:30–47. https://pubmed.ncbi.nlm.nih.gov/27821267/ . Accessed 23 Jan 2024.
Essau CA, Conradt J, Sasagawa S, Ollendick TH. Prevention of anxiety symptoms in children: results from a Universal School-based trial. Behav Ther. 2012;43(2):450–64 Accessed on 23rd of January 2024.
Amin R, Iqbal A, Naeem F, Irfan M. Effectiveness of a culturally adapted cognitive behavioural therapy-based guided self-help (CACBT-GSH) intervention to reduce social anxiety and enhance self-esteem in adolescents: a randomized controlled trial from Pakistan. Behav Cogn Psychother. 2020;1–12. https://pubmed.ncbi.nlm.nih.gov/32450939/ . Accessed 24 Jan 2024.
Download references
Acknowledgements
Our sincere thanks go to all the participants for their generous enthusiasm for participating in the trial. We are very much grateful to the Ministry of Education, School principals and the teachers who voluntarily participated in delivering the intervention. Additionally, our sincere appreciation goes to the Regional Director of Health Services, Colombo district; all the Medical Officers of Health; and their staff in the Colombo district for providing support in conducting this study. Furthermore, all the authors of the tools used in this study, including Dr. Boris Birmaher, MD, and the team, were included.
Self-funded.
Author information
Authors and affiliations.
PGIM, University of Colombo, Colombo, Sri Lanka
Sinha De Silva
Ministry of Education (Retired), Colombo, Sri Lanka
Renuka Peris
The Central Queensland Hospital and Health Service (CQHHS), Queensland, Australia
Sudharshi Senaviratne
Faculty of Medicine, University of Colombo, Colombo, Sri Lanka
Dulani Samaranayake
You can also search for this author in PubMed Google Scholar
Contributions
“SDS designed, implemented the study and prepared the manuscript. DS supervised the overall project from the design stage until the preparation of this manuscript. SS and RP provided technical supervision throughout the project related to their technical expertise i.e., psychiatry and education respectively. All the authors reviewed the final manuscript and approved it. “.
Corresponding author
Correspondence to Sinha De Silva .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Ethics Review Committee of the Faculty of Medicine, University of Kelaniya, Sri Lanka (P/19/01/2018). Informed written assent and consent were obtained from children and their parents respectively. The trial was registered in the Sri Lanka Clinical Trial Register (SLCTR/2018/018).
Consent for publication
All authors declare that they consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
De Silva, S., Peris, R., Senaviratne, S. et al. Effectiveness of a cognitive behavioural therapy (CBT)-based intervention for reducing anxiety among adolescents in the Colombo District, Sri Lanka: cluster randomized controlled trial. Child Adolesc Psychiatry Ment Health 18 , 108 (2024). https://doi.org/10.1186/s13034-024-00799-9
Download citation
Received : 23 January 2024
Accepted : 20 August 2024
Published : 31 August 2024
DOI : https://doi.org/10.1186/s13034-024-00799-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]

COMMENTS
Depression is a mental illness that affects people of all ages. Despite sharing the same symptoms as adults, depression in children often goes unnoticed and untreated. Children who are depressed may be misunderstood as being shy, difficult, or misbehaved. The Childhood Depression: Info for Caregivers worksheet teaches parents and caregivers the ...
Here's a list of 25 cognitive behavioral therapy techniques, CBT interventions, and exercises. ... there are a few more CBT activities and exercises that may be helpful for you or your clients that we'd like to cover. 1. Mindfulness meditation ... Effectiveness of cognitive behavioral therapy on depression and self-efficacy among out-patient ...
During Depression: (1) If I avoid challenges, I'll be okay, but if I try to do hard things I'll fail. (2) If I avoid asking for help, my incompetence won't show but if I do ask for help, people will see how incompetent I am. SITUATION #2 Thinking of asking son for help in revising resume SITUATION #1 Thinking about bills SITUATION #3
2 Group Therapy Worksheets. Delivering CBT in a group therapy format is sometimes recommended for those who may benefit from a group to relate to when dealing with symptoms and situations specific to depression.. Individuals may also benefit from group cohesion and can potentially use the group as an arena for challenging their negative thoughts and behavior (Thimm & Antonsen, 2014).
Here are nine common CBT techniques for depression: 2. 1. Cognitive Restructuring. In challenging your thought patterns, tone, and self-talk, you learn about potential cognitive distortions and unhealthy thought patterns that could be increasing depressive emotions or suicidal thoughts.
CBT helps you identify and challenge negative thought patterns that contribute to depression. Cognitive behavioral therapy (CBT) is a widely used and effective treatment for several psychiatric ...
CBT Worksheets for Depression and Anxiety. Cognitive-Behavioral Therapy is a form of psychotherapy that combines cognitive therapy with behavioral therapy ... Reinforcing healthy, enjoyable activities can go a long way in helping a depressed individual feel better. Sometimes getting going is the hardest part, but with some structure in place ...
CBT can help you to learn ways to stop spiraling down into feelings of depression. This illustration shows that "giving in" to the "slowed-down" feeling that often comes with depression leads to a . downward spiral: do less, feel worse, do even less, etc. In therapy, you will learn ways of stopping this
Embark on a transformative journey toward emotional well-being by exploring our free online Cognitive Behavioral Therapy workbook tailored to address anxiety and depression. This comprehensive resource is designed to empower you with practical CBT interventions and exercises rooted in evidence-based therapeutic techniques. Dive into a self ...
Dr. Judith S. Beck as a setting for state-of-the-art psychotherapy and professional training in CBT. In our 25-year history, Beck Institute has built exceptional in-person and online trainings in CBT, trained thousands of professionals from around the world, and created a global community of CBT practitioners. ONLINE RESOURCES:
• Using between-session assignments. Practice changes the brain, little by little! "But my depression is 'situational!'" Yes, it is true that often depression is set in motion by difficult events that happen to us. If you are dealing with a big loss, stressful situation, or change in your life, feelings of depression could be a result.
depression. CBT-D is based on years of research and has been shown to be very effective with nearly all types of people and age groups. Over 75% of people treated with CBT-D show improvement. This treatment is at least as effective as medications, although both CBT-D and medications can be helpful in the treatment of depression for some people ...
9 CBT Worksheets and Tools for Anxiety and Depression. CBT is one of the most effective psychological treatments when it comes to managing anxiety and depression, and can be a highly useful approach to apply in online therapy. If you help clients tackle cognitive distortions and unhelpful thinking styles, we've compiled a list of essential ...
worksheet. 12. Cognitive Behavioral Therapy (CBT) requires clients to have a strong understanding of the cognitive model before they attempt to identify and challenge their negative thoughts. This CBT worksheet will help you teach your clients about the relationship between thoughts, emotions, and behaviors through the use of several examples ...
Explore our range of CBT worksheets, exercises, information handouts, self-help guides, audio therapy tools, and the Treatments That Work™ series. Translations are available in over 70 languages, and many of our resources are downloadable in multiple formats to suit your therapy style. 100 of 515 resources. Sort by Recommended.
Cognitive behavioral therapy is the culmination of years of scientific research into the mind and what makes us feel better. Unlike traditional talk therapy, CBT interventions make use of a number of exercises and skills to reduce anxiety, depression, and many other psychological problems. These exercises have been the subject of much study and ...
8-session Depression Prevention Course and the 12-session Group CBT manual retained the three-pronged focus on activities, thoughts, and people from the manuals of the original study, because these are key areas that influence depressed mood, and thus can be used to treat it.
The cognitive triangle illustrates how thoughts, emotions, and behaviors affect one another. This idea forms the basis of cognitive behavior therapy (CBT). Perhaps most important to CBT, when a person changes their thoughts, they will also change their emotions and behaviors. By targeting irrational or maladaptive thoughts, mood and behavior ...
Therapist Materials. Cheat Sheet - Depression. N2K (Need to Know) Behavioral Activation Sheet. N2K (Need to Know) Changing Unhelpful Cognitions Sheet. Socratic Techniques for Changing Unhelpful Thoughts.
Depression is characterized by an extended period of low mood, anhedonia, and reduction in activity. Dysthymia (persistent depressive disorder) is characterized by a depressed mood that occurs for most of the day, more days than not, and has been present for at least two years. Depression is a heterogeneous condition with many different ...
Cognitive behavioral therapy (CBT) is one of the most evidence-based psychological interventions for the treatment of several psychiatric disorders such as depression, anxiety disorders, somatoform disorder, and substance use disorder. The uses are recently extended to psychotic disorders, behavioral medicine, marital discord, stressful life ...
As with anxiety, there is a range of practical CBT homework activities that aid in treating depression. It should be noted that it is common for clients experiencing symptoms of depression to report concentration and memory deficits as reasons for not completing homework assignments (Garland & Scott, 2005).
Cognitive Behavioral Therapy . ... CBT is the first line of treatment for most other mental health conditions (such as substance use disorder, depression, and anxiety) and is a more popular ...
Anxiety disorders are found to be the most prevalent psychological problems among children and adolescents. Cognitive behaviour therapy (CBT) was found to be effective at reducing anxiety. The purpose of this study was to assess the effectiveness of a universal school-based intervention for reducing anxiety among Grade 9 schoolchildren. A randomized controlled cluster trial was conducted by ...