Find a Surgeon
Search by U.S. State, Procedure and Insurance Search by Country and Procedure Browse the Global Surgeon Maps

Gender Surgeons in Germany
Dr. juergen schaff.

Dr. Schaff offers gender reassignment surgery in Germany, both MTF and FTM procedures, including the fibula flap phalloplasty.
Dr. Laszlo Szalay

Dr. Klaus Exner
Dr. michael sohn, dr. tobias s. pottek, dr. ute ebert, dr. hendrik schöll, dr. susanne morath, dr. jens christian wallmichrath.

Dr. Robert Kampmann
Dr. markus krankenhaus, dr. cornelius klein, dr. wolf j. holtje, dr. wolfgang muhlbauer, dr. hans-georg luhr, dr. hans-peter howaldt, dr. cvetan taskov, dr. michael krueger, dr. jutta krocker, dr. andree faridi, dr. marcus küntscher, dr. jens diedrichson.

Dr. Wolfgang Funk
Dr. kay arne klemenz.

- Abdominal Surgery
- Dermatology and Venereology
- Endocrine Surgery
- Foot and Ankle Surgery
- Gastroenterology
- General and Internal Medicine
- Gynaecology
- Hand Surgery
- Neurosurgery
- Ophthalmology
- Orthopaedic / Trauma Surgery
- Otorhinolaryngology
- Paediatrics
- Paediatric Surgery
- Plastic / Cosmetic Surgery
- ReconstructiveSurgery
- Rheumatology
- Spinal Diseases
- Sports Medicine
- Transgender Surgery
- Vascular Surgery, Venous Disorders
- MEOCHECK Superior Programme
- MEOCHECK Premium Programme
- MEOCHECK Basis Programme
- International patients
Private practice Transgender Surgery Meoclinic Berlin

Transgender Surgery at the MEOCLINIC in Berlin-Mitte
Our medical expert team in berlin-mitte is available for short-notice appointments..
A sex reassignment surgery is a big step for you as a patient. We will be happy to assist you in this process and help you fulfill your wish.
A sex reassignment procedure is always preceded by a detailed indication consultation at the MEOCLINIC private practices where you can clarify all medical and personal questions. Your doctor will inform you in detail about individual surgical steps and techniques and provide explanations on possible risks and complications.
Appointment
Our experts.

Dr. med. Paul Jean Daverio
Facharzt für Plastische- und Wiederherstellungs-Chirurgie, Mikrochirurgie
Schwerpunkt geschlechtsangleichende Operationen
Mehr erfahren
Our treatment scope.
- Sex Reassignment Female to Male (FtM)
- Sex Reassignment Male to Female (MtF)
- Erectile Prosthetics and Scrotoplasty
- Secondary Surgery in case of complications
Our goal is to provide the best possible result for you as a patient. Sex reassignment surgery aims for natural aesthetics as well as optimal function and sensitivity.
We will gladly discuss all further details with you in a personal consultation session. We look forward to you contacting us.
If you wish to learn more about the treatment in advance, please find detailed information (in German) here .
Spezialsprechstunden
Endokrine Chirurgie
Eine Störung im Ablauf der Hormonproduktion führt zu einer Über- oder Unterfunktion der endokrinen Organe, infolge dessen es zu Bluthochdruck, Herzrhythmusstörungen aber auch der Ausbildung von Tumoren kommen kann.
Endocrine surgery
Bei uns sind sie in guten händen.
Kurzfristige Terminvergabe
Parken im Haus
Wohlfühlatmosphäre
Professionelle Ärzte
The Forgotten History of the World's First Trans Clinic
The Institute for Sexual Research in Berlin would be a century old if it hadn’t fallen victim to Nazi ideology
By Brandy Schillace
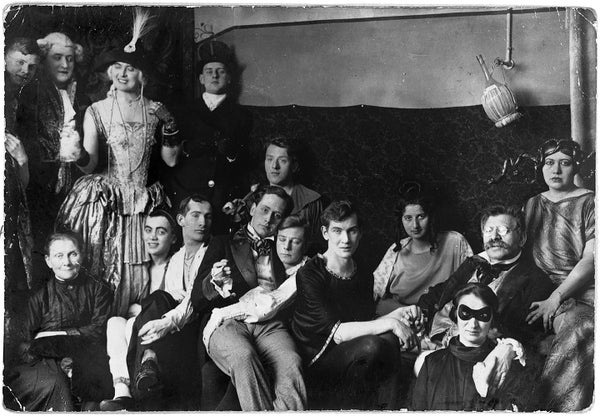
Costume party at the Institute for Sexual Research in Berlin, date and photographer unknown. Magnus Hirschfeld ( in glasses ) holds hands with his partner, Karl Giese ( center ).
Magnus-Hirschfeld-Gesellschaft e.V., Berlin
Late one night on the cusp of the 20th century, Magnus Hirschfeld, a young doctor, found a soldier on the doorstep of his practice in Germany. Distraught and agitated, the man had come to confess himself an Urning —a word used to refer to homosexual men. It explained the cover of darkness; to speak of such things was dangerous business. The infamous “Paragraph 175” in the German criminal code made homosexuality illegal; a man so accused could be stripped of his ranks and titles and thrown in jail.
Hirschfeld understood the soldier’s plight—he was himself both homosexual and Jewish—and did his best to comfort his patient. But the soldier had already made up his mind. It was the eve of his wedding, an event he could not face . Shortly after, he shot himself.
The soldier bequeathed his private papers to Hirschfeld, along with a letter: “The thought that you could contribute to [a future] when the German fatherland will think of us in more just terms,” he wrote, “sweetens the hour of death.” Hirschfeld would be forever haunted by this needless loss; the soldier had called himself a “curse,” fit only to die, because the expectations of heterosexual norms, reinforced by marriage and law, made no room for his kind. These heartbreaking stories, Hirschfeld wrote in The Sexual History of the World War , “bring before us the whole tragedy [in Germany]; what fatherland did they have, and for what freedom were they fighting?” In the aftermath of this lonely death, Hirschfeld left his medical practice and began a crusade for justice that would alter the course of queer history.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Hirschfeld sought to specialize in sexual health, an area of growing interest. Many of his predecessors and colleagues believed that homosexuality was pathological, using new theories from psychology to suggest it was a sign of mental ill health. Hirschfeld, in contrast, argued that a person may be born with characteristics that did not fit into heterosexual or binary categories and supported the idea that a “third sex” (or Geschlecht ) existed naturally. Hirschfeld proposed the term “sexual intermediaries” for nonconforming individuals. Included under this umbrella were what he considered “situational” and “constitutional” homosexuals—a recognition that there is often a spectrum of bisexual practice—as well as what he termed “transvestites.” This group included those who wished to wear the clothes of the opposite sex and those who “from the point of view of their character” should be considered as the opposite sex. One soldier with whom Hirschfeld had worked described wearing women’s clothing as the chance “to be a human being at least for a moment.” He likewise recognized that these people could be either homosexual or heterosexual, something that is frequently misunderstood about transgender people today.
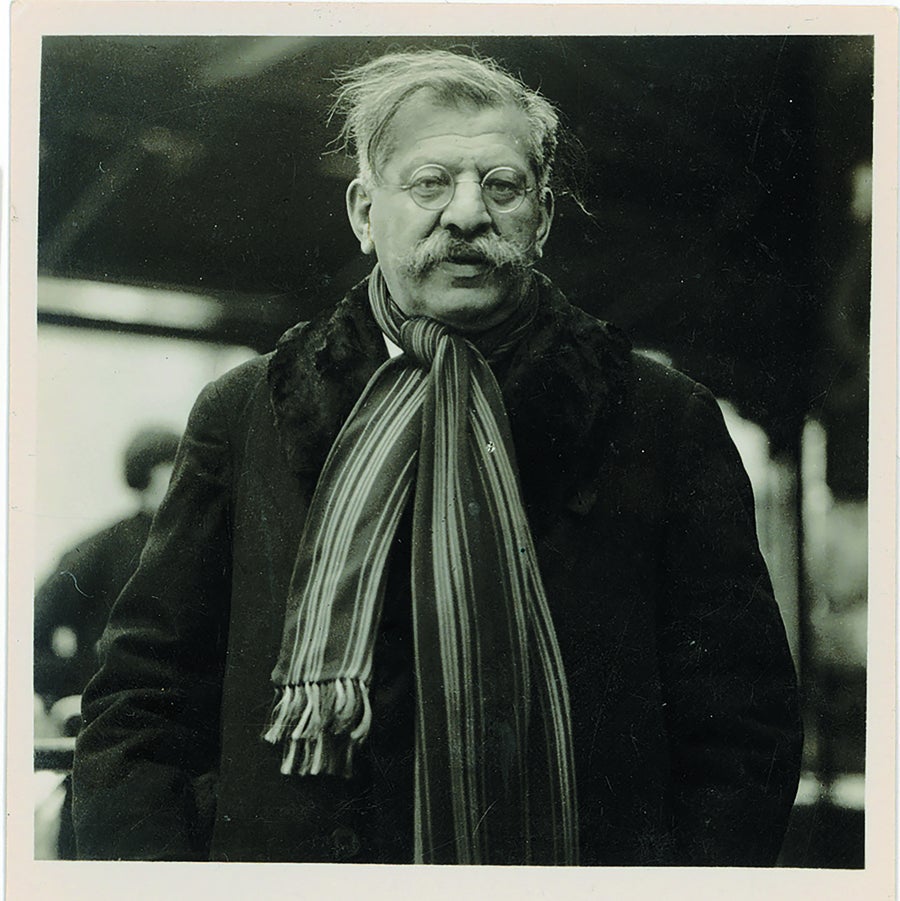
Magnus Hirschfeld, director of the Institute for Sexual Research, in an undated portrait. Credit: Magnus-Hirschfeld-Gesellschaft e.V., Berlin
Perhaps even more surprising was Hirschfeld’s inclusion of those with no fixed gender, akin to today’s concept of gender-fluid or nonbinary identity (he counted French novelist George Sand among them). Most important for Hirschfeld, these people were acting “in accordance with their nature,” not against it.
If this seems like extremely forward thinking for the time, it was. It was possibly even more forward than our own thinking, 100 years later. Current anti-trans sentiments center on the idea that being transgender is both new and unnatural. In the wake of a U.K. court decision in 2020 limiting trans rights, an editorial in the Economist argued that other countries should follow suit , and an editorial in the Observer praised the court for resisting a “disturbing trend” of children receiving gender-affirming health care as part of a transition.
Related: The Disturbing History of Research into Transgender Identity
But history bears witness to the plurality of gender and sexuality. Hirschfeld considered Socrates, Michelangelo and Shakespeare to be sexual intermediaries; he considered himself and his partner Karl Giese to be the same. Hirschfeld’s own predecessor in sexology, Richard von Krafft-Ebing, had claimed in the 19th century that homosexuality was natural sexual variation and congenital.
Hirschfeld’s study of sexual intermediaries was no trend or fad; instead it was a recognition that people may be born with a nature contrary to their assigned gender. And in cases where the desire to live as the opposite sex was strong, he thought science ought to provide a means of transition. He purchased a Berlin villa in early 1919 and opened the Institut für Sexualwissenschaft (the Institute for Sexual Research) on July 6. By 1930 it would perform the first modern gender-affirmation surgeries in the world.
A Place of Safety
A corner building with wings to either side, the institute was an architectural gem that blurred the line between professional and intimate living spaces. A journalist reported it could not be a scientific institute, because it was furnished, plush and “full of life everywhere.” Its stated purpose was to be a place of “research, teaching, healing, and refuge” that could “free the individual from physical ailments, psychological afflictions, and social deprivation.” Hirschfeld’s institute would also be a place of education. While in medical school, he had experienced the trauma of watching as a gay man was paraded naked before the class, to be verbally abused as a degenerate.
Hirschfeld would instead provide sex education and health clinics, advice on contraception, and research on gender and sexuality, both anthropological and psychological. He worked tirelessly to try to overturn Paragraph 175. Unable to do so, he got legally accepted “transvestite” identity cards for his patients, intended to prevent them from being arrested for openly dressing and living as the opposite sex. The grounds also included room for offices given over to feminist activists, as well as a printing house for sex reform journals meant to dispel myths about sexuality. “Love,” Hirschfeld said, “is as varied as people are.”
The institute would ultimately house an immense library on sexuality, gathered over many years and including rare books and diagrams and protocols for male-to-female (MTF) surgical transition. In addition to psychiatrists for therapy, he had hired Ludwig Levy-Lenz, a gynecologist. Together, with surgeon Erwin Gohrbandt, they performed male-to-female surgery called Genitalumwandlung —literally, “transformation of genitals.” This occurred in stages: castration, penectomy and vaginoplasty. (The institute treated only trans women at this time; female-to-male phalloplasty would not be practiced until the late 1940s.) Patients would also be prescribed hormone therapy, allowing them to grow natural breasts and softer features.
Their groundbreaking studies, meticulously documented, drew international attention. Legal rights and recognition did not immediately follow, however. After surgery, some trans women had difficulty getting work to support themselves, and as a result, five were employed at the institute itself. In this way, Hirschfeld sought to provide a safe space for those whose altered bodies differed from the gender they were assigned at birth—including, at times, protection from the law.

1926 portrait of Lili Elbe, one of Hirschfeld's patients. Elbe's story inspired the 2015 film The Danish Girl . Credit: https://wellcomeimages.org/indexplus/image/L0031864.html (CC BY 4.0)
Lives Worth Living
That such an institute existed as early as 1919, recognizing the plurality of gender identity and offering support, comes as a surprise to many. It should have been the bedrock on which to build a bolder future. But as the institute celebrated its first decade, the Nazi party was already on the rise. By 1932 it was the largest political party in Germany, growing its numbers through a nationalism that targeted the immigrant, the disabled and the “genetically unfit.” Weakened by economic crisis and without a majority, the Weimar Republic collapsed.
Adolf Hitler was named chancellor on January 30, 1933, and enacted policies to rid Germany of Lebensunwertes Leben , or “lives unworthy of living.” What began as a sterilization program ultimately led to the extermination of millions of Jews, Roma, Soviet and Polish citizens—and homosexuals and transgender people.
When the Nazis came for the institute on May 6, 1933, Hirschfeld was out of the country. Giese fled with what little he could. Troops swarmed the building, carrying off a bronze bust of Hirschfeld and all his precious books, which they piled in the street. Soon a towerlike bonfire engulfed more than 20,000 books, some of them rare copies that had helped provide a historiography for nonconforming people.
The carnage flickered over German newsreels. It was among the first and largest of the Nazi book burnings. Nazi youth, students and soldiers participated in the destruction, while voiceovers of the footage declared that the German state had committed “the intellectual garbage of the past” to the flames. The collection was irreplaceable.
Levy-Lenz, who like Hirschfeld was Jewish, fled Germany. But in a dark twist, his collaborator Gohrbandt, with whom he had performed supportive operations, joined the Luftwaffe as chief medical adviser and later contributed to grim experiments in the Dachau concentration camp. Hirschfeld’s likeness would be reproduced on Nazi propaganda as the worst kind of offender (both Jewish and homosexual) to the perfect heteronormative Aryan race.
In the immediate aftermath of the Nazi raid, Giese joined Hirschfeld and his protégé Li Shiu Tong, a medical student, in Paris. The three would continue living together as partners and colleagues with hopes of rebuilding the institute, until the growing threat of Nazi occupation in Paris required them to flee to Nice. Hirschfeld died of a sudden stroke in 1935 while still on the run. Giese died by suicide in 1938. Tong abandoned his hopes of opening an institute in Hong Kong for a life of obscurity abroad.
Over time their stories have resurfaced in popular culture. In 2015, for instance, the institute was a major plot point in the second season of the television show Transparent , and one of Hirschfeld’s patients, Lili Elbe, was the protagonist of the film The Danish Girl . Notably, the doctor’s name never appears in the novel that inspired the movie, and despite these few exceptions the history of Hirschfeld’s clinic has been effectively erased. So effectively, in fact, that although the Nazi newsreels still exist, and the pictures of the burning library are often reproduced, few know they feature the world’s first trans clinic. Even that iconic image has been decontextualized, a nameless tragedy.
The Nazi ideal had been based on white, cishet (that is, cisgender and heterosexual) masculinity masquerading as genetic superiority. Any who strayed were considered as depraved, immoral, and worthy of total eradication. What began as a project of “protecting” German youth and raising healthy families had become, under Hitler, a mechanism for genocide.

One of the first and largest Nazi book burnings destroyed the library at the Institute for Sexual Research. Credit: Ullstein Bild and Getty Images
A Note for the Future
The future doesn’t always guarantee progress, even as time moves forward, and the story of the Institute for Sexual Research sounds a warning for our present moment. Current legislation and indeed calls even to separate trans children from supportive parents bear a striking resemblance to those terrible campaigns against so-labeled aberrant lives.
Studies have shown that supportive hormone therapy, accessed at an early age, lowers rates of suicide among trans youth. But there are those who reject the evidence that trans identity is something you can be “born with.” Evolutionary biologist Richard Dawkins was recently stripped of his “humanist of the year” award for comments comparing trans people to Rachel Dolezal , a civil rights activist who posed as a Black woman, as though gender transition were a kind of duplicity. His comments come on the heels of legislation in Florida aiming to ban trans athletes from participating in sports and an Arkansas bill denying trans children and teens supportive care.
Looking back on the story of Hirschfeld’s institute—his protocols not only for surgery but for a trans-supportive community of care, for mental and physical healing, and for social change—it’s hard not to imagine a history that might have been. What future might have been built from a platform where “sexual intermediaries” were indeed thought of in “more just terms”? Still, these pioneers and their heroic sacrifices help to deepen a sense of pride—and of legacy—for LGBTQ+ communities worldwide. As we confront oppressive legislation today, may we find hope in the history of the institute and a cautionary tale in the Nazis who were bent on erasing it.
Brandy Schillace is editor in chief of BMJ's Medical Humanities journal and author of the recently released book Mr. Humble and Doctor Butcher , a biography of Robert White, who aimed to transplant the human soul.
Transsexuality
Male is male and female is female! This is true for the vast majority of us – despite all individual differences. That is why hardly anyone can imagine what it means when this is not the case. In fact, according to estimates, at least 0.005% of all people are born in the “wrong body”. The reasons that lead to transsexuality (transidentity) are not yet finally researched, but much speaks for genetic (hereditary) causes.
Life as a transsexual person For those affected, transsexuality often means severe psychological suffering, exclusion from society, as well as a long and painful path to the long-awaited surgical gender reassignment.
Transgender surgery at Klinik Sanssouci Surgical gender reassignment procedures have been performed at Klinik Sanssouci for over 20 years.
While many clinics perform these gender reassignments in several individual surgeries, we prefer that the respective steps required for gender reassignment are combined in a single surgery (“All in One”). This reduces the duration of the entire gender reassignment and healing process.
This requires not only careful organization before, during and after surgery, but also the coordination of multiple surgical teams, as the individual surgical steps must be perfectly coordinated.
Due to the large number of gender reassignment surgeries that have already been performed at our clinic, Klinik Sanssouci can look back on a considerable amount of experience in this area – from preventive care to aftercare:
The pre-operative discussions, the preliminary examinations as well as the inpatient and also outpatient aftercare also take place in our clinic. In addition, our patients find support with many other questions on the subject of gender reassignment.
Our surgeons are renowned experts in their respective fields. After Dr. Paul Daverio, who has led the transgender surgery department from the beginning, moved to a new place of work at the age of 74 after his successful work with us, the medical leadership of the team has been in the hands of Dr. Olivier Bauquis from Lausanne, Switzerland, since 2018. Dr. Bauquis has been performing transgender surgeries for many years and accordingly has a great expertise and reputation.
In addition, we were able to gain Dr. Jürgen Schaff, another internationally renowned surgeon, for our clinic in 2020. Dr. Jürgen Schaff had previously performed man-to-woman operations in Munich at Klinikum Rechts der Isar with great dedication and success. In doing so, he has continuously refined the classical and well-known surgical methods and developed them into his so-called combined method.
We are very pleased to be able to offer our patients an even broader range of services in the field of TS surgery with two experienced specialists in transgender surgery.
Female-to-Male
Female-to-male surgery: phalloplasty Phalloplasty, penoid reconstruction as part of female-to-male (ftm) gender reassignment surgery, is arguably the most challenging and complex operation in the field of transsexual surgery.
The technique developed by Dr. Paul Daverio, in which the penoid (“artificial penis”) is formed in a microsurgical operation from skin and subcutaneous tissue including nerves and blood vessels of the forearm (so-called forearm flap), is nowadays considered the standard procedure for gender reassignment worldwide. It leads to the best optical and functional results and has been practiced at Klinik Sanssouci for over 20 years.
Surgical technique: The steps of surgical gender reassignment. Female-to-male surgical gender reassignment is performed under general anesthesia. This procedure takes about seven to nine hours and includes:
- the removal of the breasts (mastectomy)
- removal of the uterus (hysterectomy)
- removal of the ovaries and fallopian tubes (ovarectomy, adnectomy)
- removal of the vagina (colpectomy)
- the shaping of the penoid including the new urethra (neo-urethra)
- the plastic reconstruction of a glans (glansplasty)
- the lengthening of the female urethra with the labia minora
- the relocation of the penoid from the left forearm to the pubic area. The arteries (arteries) and veins (veins) of the penoid are connected to the corresponding blood vessels of the thigh. At the same time, the inguinal nerves are connected to the penoid nerves, as well as the lengthened urethra to the newly formed urethra.
- covering the tissue defect on the forearm with skin obtained either from the groin or from the excess skin of the breast.
- the preparation of the labia majora, where the artificial testicles will be implanted later.
Important: The clitoris (clit) remains at the base of the penoid and is not removed, only its covering epidermis. Thus, the ability to orgasm is preserved.
After the surgery
- After the surgery, intensive supervision with monitoring takes place. There will be several daily visits as well as regular dressing changes and wound inspections by our doctors.
- You may get up for the first time on the 6th day after the surgery.
- The bladder catheter is removed on the 12th day. From this moment on you can urinate standing up.
- Usually, you can leave the clinic on the 14th to 16th day.
- Further treatment after female-to-male gender reassignment can be performed by your doctors at your place of residence.
- Depending on your professional situation, you can expect to be unable to work for about 6 weeks.
Complications Female-to-male gender reassignment surgery, especially penoid reconstruction (phalloplasty), is a complex procedure and therefore prone to complications. At Klinik Sanssouci, complications occur with about 5% of our patients.
Possible complications of phalloplasty include:
Stenosis This is a constriction at the connection between the urethra and the newly formed urethra (neo-urethra). This complication can usually be corrected by simple bougienage (widening) by the urologist. Only in 1 to 2% of cases is a minor second surgery required, often under local anesthesia, to widen this constriction.
Fistula This is a connection between the urethra and the skin surface through which urine can leak out. Fistulas usually close spontaneously after two to three months. If this does not occur, the fistula can be closed in a minor procedure under local anesthesia. Serious complications such as complete penoid loss (flap loss) are very rare.
Erectile prosthesis / testicular replacement A second procedure is necessary if an erectile prosthesis is to be installed. This surgery is possible if there is feeling in the penoid, which is usually about eight to ten months after the phalloplasty surgery.
As erectile prosthesis we use a so-called hydraulic implant from American Medical Systems (AMS) with a pump (AMS 700), which is placed in the newly formed scrotum (neoscrotum). A reservoir is surgically placed under the abdominal wall muscles. We place two inflatable silicone rods into the penoid. An erection is then possible by means of this pumping system. We also implant silicone testicles in the scrotum.
Male-to-female
Surgical technique The surgical male-to-female sex adjustment is performed under general anesthesia and takes about 4-5 hours. If desired, we can perform augmentation at the same time (insertion of a silicone implant for breast augmentation or augmentation with autologous fat). At the same time, a thyroid cartilage reduction is also possible.
For sex adjustment, we offer two different methods (Classic penile inversion and combined method), both of which provide excellent results, but differ in several ways.
Classic penile inversion involves the following surgical steps:
Removal of the testicles (orchidectomy)
- plastic construction of a neovagina with an island flap plasty
- plastic construction of a sensitive neoclitoris
- plastic construction of labia from scrotum
- shortening of the urethra
- cavernous body removal
- plastic construction of pubic mound
- breast reconstruction if necessary
- if necessary, reduction of the thyroid cartilage
In the combined method, additional skin grafts and the original urethra are used to build up a neovagina. Due to the special incision in this method, a more natural vulvoplasty (plastic reconstruction of the labia) is possible.
The following surgical steps are performed:
- removal of the testicles (orchidectomy)
- plastic construction of a neovagina with a combined island flap plasty, free skin graft from the skin of the scrotum as well as pedicled urethral skin
- plastic construction of labia and clitoral hood from parts of penile shaft skin
Due to the special incision, a second surgery is mandatory for the combined method. This involves some fine plastic work that cannot technically be implemented in the first surgery. Usually, the desired breast augmentation and other optional plastic procedures are also performed during this second surgery.
In direct comparison, each method has its own strengths and weaknesses, which we will be happy to discuss with you in a personal consultation in order to select the optimal treatment strategy for you.
After surgery
- after the surgery, intensive supervision with monitoring takes place. There are several daily rounds as well as regular dressing changes and wound checks by our doctors
- you can already get up on the 1st day and also go to the toilet
- the urinary catheter is removed on day 6 to 8
- Usually you can leave the clinic on the 8th to 12th day
- further treatment after male-to-female gender reassignment surgery can be performed by your doctors at your place of residence
- depending on the professional situation, an inability to work of approx. 4 weeks is to be expected
- in the combined method, bougienage (dilatation) of the neovagina must be performed – written instructions for bougienage after discharge can be found here (PDF, 39k).
Complications Complications occur in less than 5% of our patients.
- postoperative bleeding approx. 1 %
- narrowing (stenosis) of the urethral opening 1-2 %
- narrowing (stenosis) of the neovagina approx. 1 %
- we were not able to record any serious complications
- in about 30% of our patients, we perform corrective surgery after about 3-6 months, when the vaginal entrance is constricted by a small fold formed during invagination (invagination) of the original penile skin.
Requirements
For female-to-male or male-to-female gender reassignment, the following medical as well as legal requirements are necessary at Klinik Sanssouci:
- You should have undergone opposite-sex hormone treatment for at least six to eight months.
- We also need two expert opinions from you that confirm your transsexuality (transidentity). These can be, for example, the expert opinions that you obtained as part of your change of first name and civil status.
Of course, we will be happy to advise you in a personal preliminary consultation about the exact procedure of the operation and answer your questions. You can make an appointment with us, please use our contact form.
Costs / Cost coverage
In general, a transsexual patient has the right to a gender reassignment surgery. Usually, this is not declined by the health insurances. However, there is no obligation for the statutory health insurance companies to cover the costs of treatment in a private clinic.
The vast majority of our transsexual patients have statutory or private health insurance and have been granted reimbursement for an operation in our clinic on a case-by-case basis. Private health insurances usually reimburse partial amounts. We will be happy to assist you with the application process. In particular, you will need a cost estimate from us, which you will receive from us during your consultation appointment.
International patients who have to pay their costs in advance as self-payers should also obtain a cost estimate.
Please feel free to contact us with any questions you may have regarding the details of reimbursement and billing.
Frequently asked questions
Female-to-male
What methods of phalloplasty do you use and what are the functional results? We perform phalloplasty with a so-called free forearm flap. The patient can urinate standing up after the operation on the 12th day. Sexual sensitivity is preserved because the clitoris (clit) is not removed in our method. All surgical steps are performed in one session.
Why do you perform all surgical steps in one session? This procedure, the all-in-one surgery, significantly reduces the duration of the entire inpatient stay, and of course also the number of surgeries. An essential consideration is also the rapid restoration of full working capacity. It is always claimed that the risks increase due to multiple surgery, but with careful organization, good teamwork and very great experience, it is possible to perform individual surgical steps with several surgical teams at the same time without extending the total surgical time. One-stage surgery also avoids scarring adhesions in the vaginal area, which are disadvantageous in a second operation. If the breast is removed at the same time, we can use the excess skin for coverage and, if necessary, do without other skin removal sites (fewer scars). Not to be forgotten are stress factors that are eliminated when the patient has to undergo surgery only once.
Do you work with microsurgery? Yes. In phalloplasty, the penoid is formed from skin and subcutaneous tissue, including nerves and blood vessels of the forearm (called the forearm flap) in a microsurgical surgery.
How many surgeries are necessary until a final result? At Klinik Sanssouci Potsdam, two surgeries are necessary for complete female-to-male gender reassignment: The first surgery includes removal of the uterus (hysterectomy), removal of the ovaries and fallopian tubes (ovarectomy, adnectomy), removal of the breast (mastectomy), removal of the vagina (colpectomy), and penoid reconstruction (phalloplasty). In a second surgery (about eight to ten months after the first surgery), an erectile prosthesis and a silicone testicle are implanted into the newly formed scrotum.
How long does a patient have to stay in the clinic? For the first surgery, during which the penoid reconstruction (phalloplasty) takes place, you will need to plan for about 14 to 16 days of hospitalization.
What is the sensitivity of the penoid (neophallus)? The sensitivity, i.e. the sensation of the penoid, corresponds to normal skin sensitivity, comparable to the sensitivity of the skin on the forearm. Sensitivity is achieved by the ingrowth of nerves about eight to ten months after the initial surgery. Some erotic sensitivity, starting from nerves of the clitoris, is also possible.
What happens to the clitoris? Will it be removed or how will this important organ be preserved? During the phalloplasty surgery we preserve the clitoris completely and with it the sensitivity and sexual experience. We achieve this by only removing (deepithelializing) the clitoris from its epidermis, placing it at the base of the penoid and only covering it with skin so that arousal is possible as before the procedure. We do not consider the removal of the clitoris to be useful.
Have serious problems occurred at the forearm collection site? No. In the first days and weeks after the phalloplasty surgery, the hand may swell a little and become thicker. Then you should keep it elevated. We also recommend regular exercise of the hand. Serious, for example motor (movement) problems have not occurred – even fine motor movements of the hand are not affected.
Where are scars found on the penoid and are they visible? The only scar that will be visible on the penis is on the back of the penoid, so it will not be visible from the front.
Is there an acorn buildup? And when does it take place? Yes, glans reconstruction (glansplasty) is performed as standard together with phalloplasty in the first procedure.
Will a sensitive clitoris be created and how is it done? Microsurgically, while preserving the blood vessels, a clitoris is constructed from a portion of the glans (penis) in such a way that it is sexually aroused and placed in a typical location.
Are additional surgeries performed at the same time and what are they often? If desired, we perform breast reconstruction, i.e. implantation of a silicone prosthesis, in the same session. If desired, a thyroid cartilage reduction is also possible. These procedures extend the total operation time only insignificantly.
Will follow-up procedures be necessary and how often? Due to invagination of the original penile skin for the construction of the neovagina, there is often a fold at the posterior vaginal entrance, which we leave intraoperatively in order not to endanger blood circulation and thus good healing of the penile skin in the pelvis. Therefore, in about 30% of our patients we perform a widening of the vaginal entrance about 3-6 months after the initial procedure. During this procedure, small labia are formed at the same time and, if desired, the clitoris is reduced in size. As a rule, the clitoris is created during the initial operation in such a way that the safety of blood circulation and sensitivity are ensured, so that for many patients the clitoris primarily appears to be somewhat large. This is corrected during the follow-up surgery.
Are other procedures performed in your clinic for optical adaptation to the female gender? Reduction of the larynx can be performed. Likewise, nose correction and other procedures from the repertoire of aesthetic plastic surgery are possible.
When is sexual intercourse possible after surgery? There is no set rule, but medically it is possible to have normal sexual intercourse about 6 weeks after surgery.
Where are visible scars found? There are scars only on the labia majora, which are formed by reduction of the scrotum.
At what point is vaginal dilatation possible and do you use a so-called stent? After surgery, a loose tamponade is inserted into the neovagina, which is replaced on the 5th to 6th day. Careful stretching with a small dildo is possible about 10 to 14 days after surgery. It is not necessary to use a stent.
Can there be problems with sexual intercourse after surgery? Every transsexual patient should keep in mind that the pelvis of a man is much smaller and narrower than usually the pelvis of a so-called biological woman. In addition, the pelvic floor muscles are usually more strongly developed and not as soft and stretchy as in bio-women. For these reasons, it is not uncommon for muscular constriction to occur, which can persist over a longer period of time and can also lead to difficulties during sexual intercourse. Consistent stretching and relaxation is helpful in this case.
Specialist in Plastic and Reconstructive Surgery
Specialist in Gynecology and Obstetrics
Specialist in Surgery Specialist in Plastic and Cosmetic Surgery Specialist in Hand Surgery
Specialist in Plastic and Aesthetic Surgery Hand Surgeon
Physician Assistant
Dr. med. Olivier Bauquis
www.olivierbauquis.ch
Specializations Transsexuality surgery
Range of Medical Services Gender reassignment surgery female-to-male and male-to-female
Contact / Consultation Hours Consultation Center Potsdam Helene-Lange-Straße 11 14469 Potsdam ✆ +49 (0) 331 280 87 200 🖷 +49 (0) 331 280 87 209 📧 [email protected]
More Information „Transsexualität: Im falschen Körper“ mit Dr. Olivier Bauquis (in German, SRF)
- Senior physician at the University Hospital of Lausanne, Switzerland
- Co-director of the transgender network Vaud-Genève since 2017
- Medical expert for transgender surgery
- Stays abroad: 2011, Montréal, Canada, Dr. P. Brassard: surgery of transsexuality 2014, Ghent, Belgium, Prof. S. Monstrey: surgery of transsexuality
- 2006 Start of specialization in surgery of transsexuality
- Conference president “Transsexualité” at the Women’s Health Congress, 2012
- Session chair: “Surgery of gender reassignment” at the annual congress of the Swiss Society of Surgery, 2013
- Article “Gender reassignment surgery” in the Swiss Med Forum (PDF in German, 921k)
- Article „Chaque semaine au CHUV un patient change de sexe“ in VAUD (JPEG in French, 803k)
Memberships
- Swiss Medical Association (FMH)
- Swiss Society for Hand Surgery
- Swiss Society for Plastic and Reconstructive Surgery
- European Society for Surgery of Transsexuality
Dr. med. Florian Müller
www.krankenhaus-waldfriede.de
Specializations Minimally invasive gynecological procedures
Contact / Consultation Hours Krankenhaus Waldfriede Gynäkologie, Haus A, 3. OG Argentinische Allee 40 14163 Berlin ✆ +49 (0) 30 81 810 245 oder ✆ +49 (0) 30 81 810 207 🖷 +49 (0) 30 81 810-77245 📧 [email protected]
More Information Chief Physician of the Department of “Gynecology and Obstetrics” at Waldfriede Hospital
Dr. med. Jürgen Schaff
www.drschaff.de
Range of Medical Services Male-to-female feminization surgery, feminizing breast surgery, facial feminization.
More Information
- 1988 Beginning of specialization in surgery of transsexuality
- Medical practice at the Klinikum Rechts der Isar TU Munich until 1994
- Chief physician at Amperklinikum Dachau until 2004
- Head physician Red Cross Clinic Munich and Praxisklinik until 2019
- 2006 Foundation of the Quality Circle Transsexuality in Munich with Dr. Werner Ettmeier, 3-4 events per year
- 2008 Foundation of a symposium for transsexual surgery, annual events at different locations
- Foundation of the Working Group Transsexuality of the German Society of Plastic Reconstructive and Aesthetic Surgeons
- Expert witness for transgender surgery
- Live surgeries at several hospitals in Germany and abroad
- Development of several new surgical techniques and surgical standards
- German Society for Surgery
- German Society of Plastic, Reconstructive and Aesthetic Surgeons (DGPRÄC)
- Association of German Aesthetic Plastic Surgeons (VDÄPC)
- Interplast Germany
- World Professional Association for Transgender Health (WPATH)
Priv.-Doz. Dr. med. Andreas E. Steiert
www.steiert.berlin
Specializations Surgery of transsexuality
Range of Medical Services Plastic surgery and microsurgery with a focus on gender reassignment surgery female-to-male and male-to-female
Contact / Consultation Hours Sprechstundenzentrum Potsdam Helene-Lange-Straße 11 14469 Potsdam ✆ +49 (0) 331 280 87 200 🖷 +49 (0) 331 280 87 209 📧 [email protected]
More information General surgery training at the Charité and the RWTH-Aachen.
Publications: Author of numerous publications on various topics in internationally renowned journals:
- Aesthetic Surgery Journal (Official Journal of The American Society for Aesthetic Plastic Surgery).
- Aesthetic Plastic Surgery Journal (Springer-Verlag)
- Journal of Biomedical Materials Type A
- Journal of Surgical Research
- Medical Devices
- Journal of Plastic, Reconstructive and Aesthetic Surgery
and is the author of several book chapters, including “Facelift” in “Praxis der Plastischen Chirurgie, edited by Prof. Peter M. Vogt, Springer Verlag.
10/2001 Clinic for Plastic, Hand and Reconstructive Surgery, Hanover Medical School Univ.-Prof. Dr. P.M. Vogt
06/2007 Appointment as senior physician of the clinic Clinic for Plastic, Hand and Reconstructive Surgery, Hanover Medical School Univ.-Prof. Dr. P.M. Vogt
04/2011 Appointment as Managing Senior Physician of the Clinic, Deputy of the Clinic Director Clinic for Plastic, Hand and Reconstructive Surgery, Hanover Medical School Univ.-Prof. Dr. P.M. Vogt
12/2012 Additional qualification in hand surgery
09/2015 Habilitation Award of the Venia Legendi for Plastic and Aesthetic Surgery
- International Confederation for Plastic Reconstructive & Aesthetic Surgery (IPRAS)
- German Society for Senology (DGS)
- German Society for Surgery (DGCH)
- Professional Association of German Surgeons (BDC)
Contact our transgender division
- What We Treat
- Consultation Center
- Anesthesiologists
- Physician Assistants
- Contact People
- [email protected]
- TEL 0331 – 280 87 0 FAX 0331 – 280 40 86
- Klinik Sanssouci Potsdam Helene-Lange-Straße 13 14469 Potsdam
© 2024 Klinik Sanssouci. Alle Rechte vorbehalten.
Datenschutz
Please choose the relevant department and send us a message..
Appointment request with* Dr. med. Bernd Dreithaler Dr. med. Holm Edelmann Prof. Dr. med. Peter Hertel Dr. med. Joh.-Stephan von Ruediger Dr. med. Jürgen Schaff Prof. Dr. med. Markus Scheibel
Not sure who the right contact person is?
DIRECTO EN INSTAGRAM: 26 de junio, a las 19 h, "Hablemos de cirugía de afirmación de género" con el Dr Ivan Mañero. / 3 de julio, a las 13h, "Sexualidad después de la vaginoplastia" con la Dra. Labanca.

WORLD LEADER IN GENDER REASSIGNMENT SURGERY
The most advanced clinic in Europe
Gender reassignment surgery, what is gender reassignment surgery.
Gender reassignment surgery, confirmation surgery or sex reassignment surgery means a variety of procedures that allow people transition to their self-identified gender. These surgical treatments modify a physical person’s appearance and sexual characteristics to approach their identified gender.
The most common treatments are feminization surgeries are vaginoplasty, breast augmentation or facial aesthetic procedures. In the cases FTM, phalloplasty, breast reduction or facial masculinization operations are the most demanded surgeries.
Our gender affirming treatments and procedures
We offer a wide range of gender confirmation procedures to help our patients to achieve the results they are looking for, supporting and providing professional advice throughout the transformation process.
Feminisation surgery
MTF Vaginoplasty

Facial feminization

BREAST AUGMENTATION

MTF body surgery

FEMINIZING VOICE SURGERY

AESTHETIC MEDICINE
Masculinisation surgery.

Phalloplasty

Metoidioplasty
FTM top surgery

FTM Hysterectomy

Body Masculinization
OTHER MASCULINIZATION
Before and after gender-affirming surgery results.
Knowing the results of some sex reassignment surgeries could be helpful to make a decision and to have an idea about what to expect.
Dr. Ivan Mañero, a reference
Dr. Ivan Mañero, reconstructive and aesthetic plastic surgeon, is an international leader in gender affirmation surgery (ies) for trans people. He has been performing and perfecting gender reassignment surgeries for more than two decades, both inside and outside our borders.
His professionalism has led him to be internationally known and sought after, participating and moderating events in conferences. From the beginning of his professional career, he has always advocated for specialized and sensitive care for trans people. However, in the beginning, he had to deal with other peers who did not understand why a specialist like him cared about this matter.
A pioneer in unique surgical techniques for gender reassignment, Dr. Ivan Mañero has collaborated with various administrations to ensure that this type of a surgeries re included within the public health service in Spain. . In order to be able to offer greater and better care to trans people who require it.
The IM GENDER team, led by Dr Ivan Mañero, is a leading international reference in sex reassignment surgery and genital reassignment surgery.
World leader in gender reassignment surgery
The IM GENDER Gender Unit opened its doors over twenty years ago and has become an international benchmark in Gender Reassignment Surgery. IM GENDER has cared for more than 3,000 trans people who have decided to carry out some treatment or surgical procedure at the Unit, whether genital affirmation surgery – vaginoplasty, phalloplasty, metoidioplasty -, body surgery – mastectomy, breast augmentation, feminizing liposculpture, among others -, facial surgery – facial feminization, thyroplasty, masculinization of features, etc.- or other plastic surgery procedures.
IM GENDER offers all the advantages of IM CLINIC, a pioneering clinic for its concept of understanding healthcare in a global and personalized way. Our clinic confers differentiating characteristics that allow us to offer a high quality of care.
At IM GENDER you will find a clear commitment to the most cutting-edge and reliable technology, with technologically cutting-edge operating rooms and the most innovative equipment in the sector. All this, added to a medical team expert in gender surgery with more than two decades of experience led by Dr. Ivan Mañero, the most recognized plastic surgeon specialized in gender reassignment surgery in Europe and even internationally. In addition, Dr. Mañero was a pioneer in unique/specific surgical techniques for genital affirmation, such as vaginoplasty with graft.
The entire human team that makes up IM GENDER, from Patient Care to medical, health professionals, psychologists and physiotherapists, are trained in health care based on human rights, respect and privacy of all patients. Our goal is to offer all the necessary information before, during and after the surgery through close treatment and personalized attention.
YEARS OF EXPERIENCE
Im gender specialists.
THEIR EXPERIENCE COULD BE YOURS
Meet IM GENDER’s true stars and learn about their personal experiences, from preoperative consultations to postoperative follow-up care. Discover how our comprehensive approach to gender-affirming surgery, (ies) coupled with our psychological support and family guidance, has made a difference in their lives.
At IM GENDER, we understand that every patient’s journey is unique, and we are committed to providing personalised care that caters to individual needs. Our testimonials are a testament to our dedication to patient satisfaction, and we are proud to share the stories of our satisfied clients with you.
We invite you to explore our website and learn more about our services, team, and testimonials. Our team is available to answer any questions or concerns you may have and to help you start your journey towards gender affirmation.
REQUEST AN APPOINTMENT
Type of consultation: Physical appointment Online consultation
I read and accept the privacy law
IM CLINIC FACILITIES
IM GENDER is the Gender Unit at IM CLINIC, one of the most advanced sex reassignment surgery centers Internationally. A new concept of clinic born from our commitment to experience in the field. IM GENDER is a team of highly qualified professionals, who all believe in the same philosophy of exquisite patient care.
Prepare for your surgery
(18 years in Spain)
Are you 18 years or older?
Home - Transgender
Transgender – sex reassignment surgery
When a person cannot identify with the gender assigned at birth, that person’s status is referred to as transgender (formerly transsexuality). Primarily, transgender is not a problem per se, but simply the certainty of feeling you belong to a sex other than the one assigned to you, or to neither, and the wish to be acknowledged in that affiliation both socially and juridically. There are a number of possible gender identities that come under the umbrella term ‘trans’ or stand alone. Ultimately, each of them is a very individual, alterable identity. The road to sex reassignment has now been smoothed, though it does still feature some bureaucratic hurdles. Talk to us about it. We’ll help you find your own individual way forward, and we’ll be at your side to advise you. Given that the medical services at the place where they live are often limited, many transident individuals are prepared to travel long distances, sometimes even going abroad, to adapt their phenotype, though the aftercare in such cases may not necessarily be assured to an appropriate degree. If you have already had surgery, we can offer post-operational care here at the practice and will advise you if there are any complications. In Germany, the diagnosis of the transgender characteristic is geared to the International Statistical Classification of Diseases and associated health problems (ICD – transsexualism according to ICD F64.0) issued by the World Health Organisation (WHO). Many transgender and non-binary individuals feel hurt when their gender feeling is classified as a disease or disorder. However, categorisation in ICD-10 and recognition as a disease pursuant to SGB V (Book V of the German Social Security Code) do at least have the advantage for those concerned that the health insurance providers meet the costs for diagnostics and treatment once the diagnosis has been confirmed. If you are considering applying for the costs of sex reassignment surgery to be borne by your statutory health insurance provider, there are as a rule some conditions that need to be fulfilled. Having said that, we would like to draw your attention to the fact that in our practice clinic we cannot perform any operations with reimbursement for out-patient care services as defined by the statutory health insurance providers (on the so-called standard assessment scale [EBM]). In individual cases, however, you may be able to come to a special agreement with your provider. For direct payers and privately insured patients, (depending on their individual contract profile), these restrictions do not apply. As a rule, paramount to sex reassignment surgery is the removal of the protruding chest with the aim of adapting to an appearance that corresponds to the patient’s gender perception, or the construction of a protruding chest. A chest that does not fit in with the person’s sexual identity often constitutes the greatest visible stigma for the patient. Which surgical procedures are suitable in your particular case depends on your initial findings. We can offer you either realignment to a flat chest for trans people assigned female at birth (AFAB), or the creation of a protruding chest for trans people assigned male at birth (AMAB). We can perform all the operations that are necessary to achieve an optimum result for you, so that you can get just that little bit closer to your long awaited goal of uniting your body with the way you feel. We work together with a network of microsurgeons, gynaecologists, urologists and endocrinologists who will also advise and assist you. In a detailed consultation, we can talk about the gender reassignment measures which will achieve the result that is best for you.
FAQs on the law on self-determination with regard to gender entry (SBGG)
The Self-Determination Act, which was passed by the German Bundestag on 12 April 2024, is intended to make it easier for transgender, intersex and non-binary people to change their gender entry. The website of the Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (BMFSFJ) provides an overview of the most important FAQs on the draft law. Find out more here.
Ask our advice.
We’ll be glad to provide you with detailed information about this treatment. Simply get in touch with us now and obtain advice at an individual and absolutely personal level. +49 30 - 94 041 144

Wolff & Edusei Practice Clinic
Specialist practice for plastic and aesthetic surgery Taubenstraße 26 10117 Berlin (Mitte)
- +49 30 - 94 041 144
- [email protected]
Follow us on Social Media
Site notice | Privacy policy
- Testimonials
- Book a Botulinal toxin consultation
- Botulinal toxin
- Hyaluronic acid
- Biostimulation
- Thread lift
- Chemical skin peel
- Lipofilling
- Surgical needling
- Dermabrasion
- Breast correction
- Breast removal
- Breast lift
- Breast augmentation by fat transfer
- Breast augmentation with implants
- Breast reduction
- Nipple correction
- Breast reconstruction
- Breast operations for him
- Labial reduction
- Correction of the mons pubis
- Transgender
- Eyelid lift
- Volume replenishment
- Facial injuries
- Hair transplantation
- Abdominal wall lift
- Liposuction
- Buttock lift
- Upper arm lift
- Excessive perspiration
- Skin alterations
- Microsurgical scar correction
- FAQ Breast surgery
- FAQ Breast augmentation
- FAQ Breast reduction & breast lift
- FAQ Tubular breast deformity
- FAQ Breast implants
- FAQ Intimate surgery
- FAQ Beauty & Wrinkle Injections
- FAQ Anesthesia
- FAQ Gender reassignment
- Make an appointment on line Dr. med. Andrea Wolff
- Make an appointment on line Dr. med. Isabel Edusei
- Book an appointment for your botulinum toxin and glow consultation!

Online appointments
You can make an appointment on line at any time quickly and easily via the free ‘Doctolib’ doctor booking platform.
Contact form
Outside our opening hours, you can also get in touch with us via our contact form. We will get back to you as soon as possible.
Terminvereinbarung online
Über die Arzt-Buchungsplattform »Doctolib« können Sie jederzeit schnell, einfach und kostenlos einen Termin online vereinbaren.
Kontaktformular
Our Response to COVID-19 →
Medical Tourism
Best countries in the world for gender reassignment surgery.
Gender reassignment surgery (GRS) is a life-changing medical procedure that can help individuals align their physical appearance with their gender identity. Across the globe, various countries have gained recognition for offering top-notch GRS procedures, comprehensive healthcare, and experienced medical professionals. In this article, we will delve into the best countries in the world for gender reassignment surgery, shedding light on the remarkable destinations where individuals can embark on their transformative journey.
Thailand: Pioneering Excellence
Thailand has earned a reputation as a pioneer in gender reassignment surgery. Renowned for its world-class medical facilities and a cadre of skilled surgeons, Thailand offers a safe and comfortable environment for individuals seeking GRS. The country's medical tourism infrastructure is well-developed, with Bangkok serving as a hub for transformative surgeries.
Germany: Leading the Way in Europe
Germany stands out as a prominent European destination for gender reassignment surgery. The country boasts cutting-edge technology, rigorous medical standards, and an array of experienced surgeons. Berlin, in particular, is recognized for its excellence in GRS procedures, drawing patients from around the world.
United States: A Hub of Expertise
The United States, with its vast healthcare network and innovative medical centers, remains a popular choice for gender reassignment surgery. Cities like New York, San Francisco, and Los Angeles have world-renowned gender clinics that offer a wide range of procedures and comprehensive care.
Canada: A Compassionate Approach
Canada's inclusive healthcare system and commitment to LGBTQ+ rights make it a compassionate choice for gender reassignment surgery. Major cities like Toronto and Vancouver provide access to skilled surgeons and supportive medical facilities, ensuring patients receive top-tier care throughout their journey.
Brazil: Combining Beauty and Expertise
Known for its stunning landscapes and a reputation for cosmetic surgery, Brazil also shines in the realm of gender reassignment surgery. The country boasts experienced surgeons who are well-versed in GRS procedures, making it a sought-after destination for those seeking comprehensive transformations.
Belgium: Precision and Expertise
Belgium stands out as a hub for precision and expertise in GRS. The country's surgeons are renowned for their attention to detail, ensuring the best possible outcomes for patients. Brussels, the capital, is a prominent location for gender reassignment surgeries.
India: Affordable Excellence
For those seeking affordability without compromising on quality, India emerges as a viable choice for gender reassignment surgery. The country offers world-class medical facilities, experienced surgeons, and competitive pricing, making it an attractive option for international patients.
Argentina: Advocating Inclusivity
Argentina has made significant strides in advocating for LGBTQ+ rights and gender-affirming healthcare. Buenos Aires, in particular, boasts a thriving transgender community and skilled medical professionals who specialize in gender reassignment surgery.
South Korea: Excellence in Aesthetic
South Korea, renowned for its expertise in aesthetic procedures, has also gained recognition in the field of gender reassignment surgery. The country's commitment to precision and advanced medical techniques makes it a standout destination for those seeking facial feminization surgeries and other GRS procedures.
Embarking on a gender reassignment journey is a profound and life-changing decision. Choosing the right destination for gender reassignment surgery is crucial for ensuring a safe, supportive, and successful experience. The countries mentioned in this article have distinguished themselves as some of the best in the world for GRS, offering exceptional medical facilities, skilled surgeons, and inclusive environments where individuals can achieve their desired transformations. Before making a decision, it is essential to conduct thorough research, consult with healthcare professionals, and consider personal preferences and needs. Ultimately, the journey towards aligning one's gender identity with their physical appearance should be met with understanding, compassion, and excellence in medical care.
To receive a free quote for this procedure please click on the link: https://www.medicaltourism.com/get-a-quote
For those seeking medical care abroad, we highly recommend hospitals and clinics who have been accredited by Global Healthcare Accreditation (GHA). With a strong emphasis on exceptional patient experience, GHA accredited facilities are attuned to your cultural, linguistic, and individual needs, ensuring you feel understood and cared for. They adhere to the highest standards, putting patient safety and satisfaction at the forefront. Explore the world's top GHA-accredited facilities here . Trust us, your health journey deserves the best.
Unveiling the Power of Social Media Marketing in Medical Tourism
Korea: turning the focus to an emerging global leader in medical tourism, exploring the surge of cosmetic tourism: trends and considerations in aesthetic procedures abroad, holistic healing: exploring integrative medicine and wellness retreats, meeting the surge: the growing demand for knee replacement surgeries and advances in the field, bridging culture and care: insights from dr. heitham hassoun, chief executive of cedars-sinai international, mastercard and the medical tourism association join forces to revolutionize cross-border healthcare payments, in pursuit of excellence: ceo spotlight with ms. artirat charukitpipat, stem cells show promise for hair thickening, stem cell injection for back and neck pain, continue reading, south korea, a medical tourism leader pioneering the future of medicine , best countries for stomach cancer treatment: a global perspective, ponderas academic hospital: elevating medical tourism with jci accreditation and personalized care, featured reading, medical tourism magazine.
The Medical Tourism Magazine (MTM), known as the “voice” of the medical tourism industry, provides members and key industry experts with the opportunity to share important developments, initiatives, themes, topics and trends that make the medical tourism industry the booming market it is today.
- For authors
- Ärztestellen
- English Edition
Review article
Hormonal gender reassignment treatment for gender dysphoria, meyer, g ; boczek, u ; bojunga, j.
- Figures & Tables
Background: No data are available at present on the prevalence of gender dysphoria (trans-identity) in Germany. On the basis of estimates from the Netherlands, it can be calculated that approximately 15 000 to 25 000 persons in Germany are affected. Persons suffering from gender dysphoria often experience significant distress and have a strong desire for gender reassignment treatment.
Method: This review is based on pertinent publications retrieved by a selective search in the PubMed database employing the searching terms “transsexualism,” “transgender,” “gender incongruence,” “gender identity disorder,” “gender-affirming hormone therapy,” and “gender dysphoria.”
Results: In view of its far-reaching consequences, some of which are irreversible, hormonal gender reassignment treatment should only be initiated after meticulous individual consideration, with the approval of the treating psychiatrist/psychotherapist and after extensive information of the patient by an experienced endocrinologist. Before the treatment is begun, the patient must be extensively screened for risk factors. The contraindications include severe preexisting thromboembolic diseases (mainly if untreated), hormone-sensitive tumors, and uncontrolled preexisting chronic diseases such as arterial hypertension and epilepsy. Finding an appropriate individual solution is the main objective even if contraindications are present. Male-to-female treatment is carried out with 17β-estradiol or 17β-estradiol valerate in combination with cyproterone acetate or spironolactone as an antiandrogen, female-to-male treatment with transdermal or intramuscular testosterone preparations. The treatment must be monitored permanently with clinical and laboratory follow-up as well as with gynecological and urological early-detection screening studies. Prospective studies and a meta-analysis (based on low-level evidence) have documented an improvement in the quality of life after gender reassignment treatment. Female-to-male gender-incongruent persons often have difficulty being accepted in a gynecological practice as a male patient.
Conclusion: Further prospective studies for the quantification of the risks and benefits of hormonal treatment would be desirable. Potential interactions of the hormone preparations with other medications must always be considered.
Gender dysphoria—or gender incongruence or transsexuality–is characterized by a mismatch between the biological sex and the inner sense of gender (gender identity). A transgender woman is a biologically male person with female gender identity; correspondingly, a transgender man is a biologically female person with male gender identity. In the Netherlands, the prevalence of gender dysphoria is estimated to be 0.02–0.03% ( 1 ). For Germany, no estimates have yet been published. Based on the above figures, it can be assumed that approximately 15 000 to 25 000 people are affected. While earlier studies ( 1 , e1 , e2 ) reported a gender ratio of transgender women to transgender men of approximately 2 : 1, more recent studies found increasingly similar proportions ( e3 ) or even a reversal of this ratio ( 2 ).
With the onset of puberty, transgender persons typically experience significant psychological distress (gender dysphoria) and consequently seek gender-affirming—or gender reassignment—treatment ( e4 ). With 9% to 11% and 1.5% to 2%, the rates of suicide attempts ( 3 ) and committed suicides ( 4 ), respectively, are increased among people with gender dysphoria compared to the general population. In 2010, a meta-analysis found a decrease in mental and physical complaints as well as an increase in quality of life after the start of gender-affirming hormone therapy (GAHT) ( 5 ), but the data quality of this study was limited. However, later prospective studies confirmed these findings ( 6 , e5 ). The two-year follow-up after GAHT revealed the following differences compared to the pre-treatment status:
- Decrease in depressive symptoms (Beck Depression Inventory [BDI] II scores: transgender women −1.41, p<0.001; transgender men −1.31, p<0.001)
- Reduction in body uneasiness (Body Uneasiness Test [BUT] index: transgender women −0.24, p<0.001; transgender men −0.24, p = 0.001)
- Decrease in gender dysphoria (GIDYQ AA score: transgender women −0.06, p 6 ).
For persons with gender dysphoria, treatment with cross-sex hormones delivers a sense of identity. However, since gender-affirming hormone therapy has a significant effect on a person’s hormonal balance, it is associated with a risk of adverse effects which is particularly high in the event of unsupervised treatment or overdosing.
Using treatment data from a large Dutch gender identity clinic collected in the period from 1980 to 2015, Wiepjes et al. demonstrated a 20-fold increase in newly started GAHT ( 1 ). Similarly, many treatment providers in Germany have observed an increase in the number of affected persons in recent years (personal communication from colleagues of other institutes). Factors potentially contributing to this trend include growing societal acceptance and a significant increase in public attention and media coverage ( e6 , e7 , e8 , e9 , e10 ). Nevertheless, in Germany, too, those affected do frequently not receive optimal care ( 7 , 8 , e4 , e11 ).
The aim of this article is to provide up-to-date insights into and recommendations for gender-affirming hormone therapy (GAHT) as well as information about special aspects that should be taken into account by general practitioners and specialists involved in the care of transgender persons.
Overall, the evidence from studies on the effects and risks of GAHT—which also forms the basis of the guidelines of the Endocrine Society which were initially created under US and European co-authorship in 2009 and then updated in 2017 ( 9 )—is weak. Most studies are retrospective data analyses, frequently based on comparatively few cases. Prospective studies are scarce. There are no randomized controlled trials and, ultimately, it is difficult to imagine that studies designed will ever be conducted, not least for ethical reasons. A German or European guideline on GAHT has not yet been created.
This review is based on a selective search of the PubMed database for original publications and review articles up to December 2019. The following search terms were used: “transsexualism”, “transgender”, “gender incongruence“, “gender identity disorder“, “gender affirming hormone therapy“, “gender dysphoria”.
Requirements
Treatment with GAHT quickly causes marked and partly irreversible changes. Thus, prior to the start of treatment, it is critical to confirm the diagnosis and to ensure that a clear, written indication for GAHT is established by a psychotherapist or psychiatrist ( 9 , 10 , 11 , e12 ). There are no strict requirements for the duration of preceding psychotherapy and, given the very different circumstances and needs of the affected individuals, any such requirement may not be helpful after all.
GAHT can be started at about age 16 years, provided a written, documented informed consent is obtained from the adolescent’s parents or guardian and the adolescent is mature enough to make this decision. In gender-dysphoric younger children and adolescents, a reversible puberty-suppressing therapy with gonadotropin-releasing hormone (GnRH) analogs can be initiated with the onset of puberty ( 9 ). In minors, confirmation of the indication by an independent second therapist should be required ( 9 ). Prior to the initiation of treatment, the patient must be informed in detail about the treatment effects, their course over time, the limitations of the treatment and potential adverse effects ( 9 , 10 ).
Medical diagnostic work-up prior to treatment initiation
A comprehensive pre-treatment risk screening, including thorough medical history, family history and physical examination as well as clinical chemistry testing of relevant parameters is required to identify potential contraindications and risk factors. This screening also helps to adapt the planned treatment to a patient’s individual risk profile (Box).
Many healthcare payers require that a somatic variation of sex development is ruled out before treatment is started ( e13 ). These differential diagnostic conditions, such as Klinefelter syndrome and complete androgen resistance syndrome, are rare and can be excluded based on the medical history, physical examination and measuring of basal hormone levels. Only in the presence of major clinical abnormalities and grossly abnormal laboratory findings, further diagnostic work-up, including chromosomal analysis, should be performed.
Pre-existing conditions, such as arterial hypertension, diabetes, dyslipidemia, and HIV, require adequate treatment. Adequately controlled, they are not considered absolute contraindications. In the presence of elevated liver enzyme levels, a pre-existing hepatic condition should be ruled out. Further diagnostic testing may be required.
GAHT is so essential for patients with gender dysphoria that priority even over contraindications can be given to this treatment on an individual basis after detailed discussion of associated risks. The decision to provide the treatment should also be broadly supported by all clinicians involved in the patient’s care. Absolute contraindications are very rare. Unsupervised self-medication is associated with high risks. Thus, instead of withholding therapeutically controlled hormone treatment in patients with contraindications, ideally an experienced endocrinologist should carefully evaluate each case individually to find a personalized solution.
Male-to-female gender dysphoria
Treatment recommendations
GAHT of male-to-female transsexuals is based on the oral or transdermal administration of 17ß-estradiol or 17ß-estradiol valerate ( 9 ). Because of the significantly more unfavorable risk profile, treatment with ethinyl estradiol is obsolete ( 12 , 13 , 14 ). Since thromboembolic complications are more common with oral estradiol treatment ( 15 ), preference is given to the transdermal route of application if additional risk factors, such as overweight, older age and smoking, are present.
Since reducing androgen levels is another important requirement for the desired feminization of the body ( 16 , e14 ), patients also receive supplementary anti-androgen therapy. Here, the standard treatment is the administration of cyproterone acetate ( 17 ). Alternatively, treatment with spironolactone may be considered. Administration of a GnRH analog is another treatment option, but the significantly higher costs of this approach need to be taken into consideration. Anti-androgen treatment is discontinued, at the latest, once orchiectomy has been performed as part of the gender-affirming surgical procedure. An additional benefit on breast development by supplemental progesterone treatment has not yet been confirmed ( 18 , 19 ). There is a lack of randomized controlled trials evaluating this aspect. Given the increased risk of breast cancer and thromboembolic events associated with hormone replacement therapy in postmenopausal women ( e15 ), additional administration of progesterone in transgender women is currently not recommended ( 9 ). Information about the medications used for GAHT and their standard dosing schedules is provided in Table 1.
Course and limitations of treatment
Table 2 gives an overview of the course of treatment over time and its limitations. GAHT cannot alter the size and shape of the male larynx and consequently the pitch of the voice. While body and facial hear growth are diminished, they usually do not stop completely; consequently, epilation treatment is required in most cases.
Adverse reactions and risks
Table 3 gives an overview of adverse reactions and risks. The development of venous thromboembolism (VTE) is a relevant risk. Older, retrospective data from the time when ethinyl estradiol (today considered obsolete) was still commonly used show a significant increase in the risk of thromboembolism with the occurrence of a VTE in 5.5% to 6.3% of ethinyl estradiol-treated patients ( 12 , 20 ). With the advent of modern treatment regimens, the prevalence of VTEs has declined to about 0.6% to 2% ( 21 , 22 ). To date, no studies evaluating the perioperative risk of thromboembolism have been conducted in patients receiving feminizing hormone therapy. Studies investigating this risk in postmenopausal women receiving hormone replacement therapy found heterogeneous results ( e16 , e17 , e18 ). Transdermal estradiol therapy without co-administration of progestin appears to be no significant additive risk factor in this patient population. The potential negative effect of temporarily discontinuing GAHT on mind and body, the risk profile and the treatment used have to be taken into consideration when making recommendations on the perioperativen management of GAHT ( 23 ). Most treating clinicians currently recommend to discontinue the hormone therapy for two weeks prior to scheduled surgical interventions ( 24 ).
Occasionally, weight gain of 3 to 4 kg, on average, is observed ( 25 , 26 ). In addition, older studies showed an increase in triglycerides ( 26 , 27 ) from 76 mg/dL to 128 mg/dL, on average, (p 12 ). When transdermal estradiol formulations are used, unfavorable changes in these laboratory parameters are significantly less common ( 27 ) or levels even decrease to the female reference range ( 17 ).
Long-term data on cardiovascular risk are scarce. However, a recent study found an increased occurrence of cerebral ischemia in transgender individuals receiving GAHT compared to age-matched women (2.4-fold risk increase) and men (1.8-fold risk increase) ( 28 ). The rate of myocardial infarction was higher compared to biological women but comparable with the rate in age-matched men ( 28 , 29 ). From about age 50 years onwards, it is recommended to reduce the estradiol dose, mimicking the normal age-related hormonal changes ( 30 ). Nevertheless, it may be useful to continue treatment with a low maintenance dose beyond the statistical age of menopause to preserve bone density ( 31 ). If additional risk factors for osteoporosis are present and especially in the rare cases where GAHT is not continued after orchiectomy, e.g. because of contraindications, it is recommended to measure bone density using dual-energy X-ray absorptiometry (DXA) ( 9 ). However, the costs of DXA for this indication are not covered by German statutory health insurance funds.
While, especially in patients receiving high doses of estradiol, mild increases in prolactin levels are common and considered acceptable, relevant increases of prolactin levels >2x ULN may require an adjustment of the estradiol dose, once functional causes of hyperprolactinemia (e.g. preceding palpation of the breast) have been ruled out. If elevated levels persist, magnetic resonance imaging (MRI) of the pituitary gland should be performed since isolated cases of prolactinoma have been reported among patients receiving long-term high-dose estradiol therapy ( 32 ). In a recent Dear Doctor letter (“Rote-Hand-Brief”), a dose-dependent increase in the risk of meningioma occurrence has been described for patients treated with cyproterone acetate.
GAHT leads to testicular atrophy and over the course of treatment potentially to irreversible infertility ( 33 ). Information about theses consequences of the therapy and the options for preserving fertility (eBox) should be an integral part of the informed consent discussion.
Female-to-male gender dysphoria
Gender-affirming hormone therapy of female-to-male transsexual persons is based on testosterone administered as a transdermal gel or intramuscular depot preparation. A progestin can be added temporarily to the regimen to suppress menstruation until adequate suppression of the gonadotropic axis is achieved by testosterone ( 9 ). Progestin preparations need to be taken very regularly to ensure reliable menstrual suppression. Typically, treatment is started with a low dose taken once daily. If this is not successful, the dose can be increased to twice daily or, alternatively, a GnRH analog may be used. Further information about the preparations used and the recommended doses is presented in Table 1.
Table 2 gives an overview of the course of treatment over time and its limitations.
Adverse reactions and risks are listed in Table 3. Acne is the most common adverse reaction of testosterone therapy ( 17 , 34 ). Depending on the severity and form of acne, topical retinoids, benzoyl peroxide, adapalene, azelaic acid, or clindamycin are used. Systemic treatment with retinoids or antibiotics is reserved for severe forms of acne ( e19 ). Combination oral contraceptives with anti-androgenic progestin component are not suitable for the treatment of transgender men ( 35 ). In transgender men receiving retinoid treatment who are sexually active with biological men, reliable contraception has to be ensured because of the teratogenicity of the drug.
In the experience of the authors, an increase in aggressive behavior is occasionally reported. This issue should already be addressed prior to the start of treatment and regularly discussed over the course of therapy.
Because of the effect of testosterone on erythropoiesis, up to 11% to 17% of these patients develop erythrocytosis. This risk increases with increasing duration of the hormone therapy and the size of the testosterone dose, but essentially even patients with normal testosterone levels are at risk ( 17 , 36 ). If side effects occur, the dose of testosterone should be reduced or the injection interval extended. Currently there is no reliable answer to the question whether erythrocytosis in transgender men increases the risk of thrombosis to an extent which is similar to that seen in patients with myeloproliferative disorders ( 24 ).
Body weight can increase by 2 kg to 4 kg on average ( 25 , 26 ); however, an increase in muscle mass is also noted. While some studies indicated an unfavorable effect on lipid metabolism (increase in LDL cholesterol and decrease in HDL cholesterol) ( 25 , 26 ), other studies found that blood lipid levels rather tend to align with the male reference range ( 17 ). Overall, there is some evidence indicating a somewhat increased risk of cardiovascular events ( 28 , 29 ). It appears that if modern, guideline-based treatment regimens are used, relevant increases in liver enzyme levels occur significantly less frequently ( 17 , 27 ) compared to the rates reported in earlier studies ( 12 ).
Contraception/fertility
Testosterone therapy alone does not provide adequate contraception before gonadectomy is performed. Safe contraceptive options which can be used in combination with GAHT include barrier methods, oral progestins as well as hormone-free or progestin-releasing intrauterine devices ( 37 ). In the informed consent discussion, the issue of contraception as well as the options for preserving fertility (eBox) must be addressed.
Follow-up examinations
After the initiation of treatment, a regular clinical and laboratory follow-up of the patients is required ( 9 ). During the first year, checks at three-month intervals are useful; in the long term, checks should be performed every 6 to 12 months and be continued even after the patient underwent gender-affirming surgery. It is useful to measure serum sex hormone levels to assess the required dosing and, above all, to prevent overtreatment. In transgender women, the goal should be to achieve estradiol levels in the middle of the reference range for premenopausal women ( 17 , 18 , 38 ). Increasing the estradiol dose beyond the normal limit does not result in further growth of the breast, but increases the risk of adverse long-term effects of the hormone therapy.
In transgender men, the goal is to achieve a testosterone level within the male reference range (approx. 250–840 ng/dL). Hemoglobin and hematocrit are important markers of the effect of testosterone ( 17 , 36 ) and should be regularly monitored over the course of treatment because of the risk of erythrocytosis, among others.
In addition, patients should be screened for potential adverse reactions and risks on a regular basis. During screening, patients should be asked about risk factors and possible co-medications. Furthermore, body weight, blood pressure, liver enzyme levels, lipid status, blood count, and, in patients receiving feminizing treatment, also prolactin levels should be checked ( 9 ).
Gynecological and urological care
In a retrospective analysis of more than 2000 transgender women receiving feminizing GAHT, a recent study from the Netherlands has shown a 46-fold increase in breast cancer risk among transgender women compared to men. However, with a standardized incidence ratio of 0.3, the incidence of breast cancer in transgender women remains below the incidence observed in biological women ( 39 ). It is recommended that transgender women attend the standard gynecological screening program ( 9 ).
Since the prostate gland is not removed during genital gender-affirming surgery but remains in situ and sporadic cases of benign prostatic hyperplasia ( 40 ) and prostate cancer ( e21 ) have been reported in transgender women receiving hormone therapy, annual checks of prostate-specific antigen (PSA) levels and clinical examinations of the prostate gland are recommended ( 9 ).
Since testosterone is aromatized to estradiol, patients receiving GAHT are in principle still at risk for hormone-dependent cancers. While related data are scarce, overall hysterectomy with bilateral salpingo-oophorectomy is recommended. It is also recommended that until patients have undergone this procedure, or as an alternative if no surgery is performed, they should attend regular gynecological screening examinations ( 9 ).
Despite their importance, these screening examinations are frequently not or only irregularly attended. The psychological barrier for transgender men to undergo a gynecological examination is often high. Reports of transgender men finding it very difficult to be accepted by a gynecologist’s practice are not uncommon ( 7 ). It is critical that transgender men have access to gynecological care—even after their legal sex status has been changed and their registered gender is male.
Treatment of pre-existing chronic conditions and intercurrent diseases
Attention should be paid to a few peculiarities and potential drug interactions (Table 4).
In memory of Dr. Sophinette Becker, 1950–2019, former Head of the Sexual Medicine Outpatient Clinic of the Frankfurt University Hospital, longstanding co-publisher of the “Zeitschrift für Sexualforschung“ and co-founder of the Rhein-Main Working Group on Transidentity.
Conflict of interest The authors declare no conflict of interest.
Manuscript received on16 January 2020, revised version accepted on 25 June 2020
Translated from the original German by Ralf Thoene, MD.
Corresponding author Dr. med. Gesine Meyer Fachärztin für Innere Medizin, Endokrinologie und Diabetologie Universitätsklinikum Frankfurt Theodor-Stern-Kai 7 60596 Frankfurt am Main
Germany [email protected]
Cite this as: Meyer G, Boczek U, Bojunga J: Hormonal gender reassignment treatment for gender dysphoria. Dtsch Arztebl Int 2020; 117: 725–32. DOI: 10.3238/arztebl.2020.0725
► Supplementary material
For eReferences please refer to: www.aerzteblatt-international.de/ref4320
eBox: www.aerzteblatt-international.de/20m0725
| 1. | Wiepjes CM, Nota NM, de Blok CJM, et al.: The Amsterdam Cohort of Gender Dysphoria Study (1972–2015): Trends in prevalence, treatment, and regrets. J Sex Med 2018; 15: 582–90 |
| 2. | Meyer G, Mayer M, Mondorf A, Herrmann E, Bojunga J: Increasing normality–persisting barriers: current socio-demographic characteristics of 350 individuals diagnosed with gender dysphoria. Clin Endocrinol (Oxf) 2020; 92: 241–6 |
| 3. | Bauer GR, Scheim AI, Pyne J, Travers R, Hammond R: Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada Health behavior, health promotion and society. BMC Public Health 2015; 15: 525 |
| 4. | Wierckx K, Elaut E, Declercq E, et al.: Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: a case-control study. Eur J Endocrinol 2013; 169: 471–8 |
| 5. | Murad MH, Elamin MB, Garcia MZ, et al.: Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf) 2010; 72: 214–31 |
| 6. | Fisher AD, Castellini G, Ristori J, et al.: Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab 2016; 101: 4260–9 |
| 7. | Jaffee KD, Shires DA, Stroumsa D: Discrimination and delayed health care among transgender women and men implications for improving medical education and health care delivery. Med Care 2016; 54: 1010–6 |
| 8. | Safer JD, Tangpricha V: Care of transgender persons. N Engl J Med 2019; 381: 2451–60 |
| 9. | Hembree WC, Cohen-Kettenis PT, Gooren L, et al.: Endocrine treatment of gender-dysphoric/gender-incongruent persons: an endocrine societyclinical practice guideline. J Clin Endocrinol Metab 2017; 102: 3869–903 |
| 10. | Coleman E, Bockting W, Botzer M, et al.: Standards of care for the health of transsexual, transgender, and gender nonconforming people, Version 7. Int J Transgenderism 2012; 13: 165–232 |
| 11. | AWMF-Register-Nr. 138|001: Geschlechtsinkongruenz, Geschlechtsdysphorie und Trans-Gesundheit. https://www.awmf.org/uploads/tx_szleitlinien/138-001l_S3_Geschlechtsdysphorie-Diagnostik-Beratung-Behandlung_2019-02.pdf (last accessed on 9 June 2020). |
| 12. | van Kesteren PJM, Asscheman H, Megens JAJ, Gooren LJG: Mortality and morbidity in transsexual subjects treated with cross-sex hormones. Clin Endocrinol (Oxf) 1997; 47: 337–42 |
| 13. | Asscheman H, Giltay EJ, Megens JAJ, De Ronde W, Van Trotsenburg MAA, Gooren LJG: a long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 2011; 164: 635–42 |
| 14. | Toorians AWFT, Thomassen MCLGD, Zweegman S, et al.: Venous thrombosis and changes of hemostatic variables during cross-sex hormone treatment in transsexual people. J Clin Endocrinol Metab 2003; 88: 5723–9 |
| 15. | Sweetland S, Beral V, Balkwill A, et al.: Venous thromboembolism risk in relation to use of different types of postmenopausal hormone therapy in a large prospective study. J Thromb Haemost 2012; 10: 2277–86 |
| 16. | Gooren LJ, Giltay EJ, Bunck MC: Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience. J Clin Endocrinol Metab 2008; 93: 19–25 |
| 17. | Meyer G, Mayer M, Mondorf A, Fluegel AK, Herrmann E, Bojunga J: Safety and rapid efficacy of guideline-based gender affirming hormone therapy: an analysis of 388 individuals diagnosed with gender dysphoria. Eur J Endocrinol 2020; 182: 149–56 |
| 18. | Wierckx K, Gooren L, T’Sjoen G: Clinical review: Breast development in trans women receiving cross-sex hormones. J Sex Med 2014; 11: 1240–7 |
| 19. | Seal LJ: A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria. Ann Clin Biochem 2016; 53: 10–20 |
| 20. | Asscheman H, T’Sjoen G, Lemaire A, et al.: Venous thrombo-embolism as a complication of cross-sex hormone treatment of male-to-female transsexual subjects: a review. Andrologia 2014; 46: 791–5 |
| 21. | Defreyne J, Van de Bruaene LDL, Rietzschel E, Van Schuylenbergh J, T’Sjoen GGR: Effects of gender-affirming hormones on lipid, metabolic, and cardiac surrogate blood markers in transgender persons. Clin Chem 2019; 65: 119–34 |
| 22. | Arnold JD, Sarkodie EP, Coleman ME, Goldstein DA: Incidence of venous thromboembolism in transgender women receiving oral estradiol. J Sex Med 2016; 13: 1773–7 |
| 23. | Boskey ER, Taghinia AH, Ganor O: Association of surgical risk with exogenous hormone use in transgender patients: a systematic review. JAMA Surg 2019; 154: 159–69 |
| 24. | Shatzel JJ, Connelly KJ, DeLoughery TG: Thrombotic issues in transgender medicine: a review. Am J Hematol 2017; 92: 204–8 |
| 25. | Pelusi C, Costantino A, Martelli V, et al.: Effects of three different testosterone formulations in female-to-male transsexual persons. J Sex Med 2014; 11: 3002–11 |
| 26. | Elbers JMH, Giltay EJ, Teerlink T, et al.: Effects of sex steroids on components of the insulin resistance syndrome in transsexual subjects. Clin Endocrinol (Oxf) 2003; 58: 562–71 |
| 27. | Wierckx K, Van Caenegem E, Schreiner T, et al.: Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: results from the European network for the investigation of gender incongruence. J Sex Med 2014; 11: 1999–2011 |
| 28. | Nota NM, Wiepjes CM, De Blok CJM, Gooren LJG, Kreukels BPC, Den Heijer M: Occurrence of acute cardiovascular events in transgender individuals receiving hormone therapy results from a large cohort study. Circulation 2019; 139: 1461–2 |
| 29. | Getahun D, Nash R, Flanders WD, et al.: Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med 2018; 169: 205–13 |
| 30. | Tangpricha V, den Heijer M: Oestrogen and anti-androgen therapy for transgender women. Lancet Diabetes Endocrinol 2017; 5: 291–300 |
| 31. | Gooren LJ, T’Sjoen G: Endocrine treatment of aging transgender people. Rev Endocr Metab Disord 2018; 19: 253–62 |
| 32. | Cunha FS, Domenice S, Câmara VL, et al.: Diagnosis of prolactinoma in two male-to-female transsexual subjects following high-dose cross-sex hormone therapy. Andrologia 2015; 47: 680–4 |
| 33. | Jindarak S, Nilprapha K, Atikankul T, et al.: Spermatogenesis abnormalities following hormonal therapy in transwomen. Biomed Res Int 2018; 2018: 7919481 |
| 34. | Giltay EJ, Gooren LJG: Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females. J Clin Endocrinol Metab 2000; 85: 2913–21 |
| 35. | Motosko CC, Zakhem GA, Pomeranz MK, Hazen A: Acne: a side-effect of masculinizing hormonal therapy in transgender patients. Br J Dermatol 2019; 180: 26–30 |
| 36. | Defreyne J, Vantomme B, Van Caenegem E, et al.: Prospective evaluation of hematocrit in gender-affirming hormone treatment: results from european network for the investigation of gender incongruence. Andrology 2018; 6: 446–54 |
| 37. | Francis A, Jasani S, Bachmann G: Contraceptive challenges and the transgender individual. Womens Midlife Health 2018; 4: 12 |
| 38. | De Blok CJM, Klaver M, Wiepjes CM, et al.: Breast development in transwomen after 1 year of cross-sex hormone therapy: Results of a prospective multicenter study. J Clin Endocrinol Metab 2018; 103: 532–8 |
| 39. | De Blok CJM, Wiepjes CM, Nota NM, et al.: Breast cancer risk in transgender people receiving hormone treatment: Nationwide cohort study in the Netherlands. BMJ 2019; 365: 11652 |
| 40. | Casella R, Bubendorf L, Schaefer DJ, Bachmann A, Gasser TC, Sulser T: Does the prostate really need androgens to grow? Transurethral resection of the prostate in a male-to-female transsexual 25 years after sex-changing operation. Urol Int 2005; 75: 288–90 |
| e1. | Fisher AD, Bandini E, Casale H, et al.: Sociodemographic and clinical features of gender identity disorder: an Italian multicentric evaluation. J Sex Med 2013; 10: 408–19 |
| e2. | Gómez-Gil E, Trilla A, Salamero M, Godás T, Valdés M: Sociodemographic, clinical, and psychiatric characteristics of transsexuals from Spain. Arch Sex Behav 2009; 38: 378–92 |
| e3. | Garrels L, Kockott G, Michael N, et al.: Sex ratio of transsexuals in Germany: the development over three decades. Acta Psychiatr Scand 2000; 102: 445–8 |
| e4. | Safer JD, Coleman E, Feldman J, et al.: Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes 2016; 23: 168–71 |
| e5. | Colizzi M, Costa R, Pace V, Todarello O: Hormonal treatment reduces psychobiological distress in gender identity disorder, independently of the attachment style. J Sex Med 2013; 10: 3049–58 |
| e6. | New Health Guidelines Propel Transgender Rights: Human Rights Watch. www.hrw.org/news/2019/05/27/new-health-guidelines-propel-transgender-rights (last accessed on 23 December 2019). |
| e7. | Tessa Ganserer – Transfrau im Landtag: „Ich verlange, dass dieser Staat mich akzeptiert” – SPIEGEL ONLINE. www.spiegel.de/politik/deutschland/tessa-ganserer-transfrau-im-landtag-ich-verlange-dass-dieser-staat-mich-akzeptiert-a-1302193.html (last accessed on 23 December 2019). |
| e8. | The Lancet: Creating respectful health care for trans patients. Lancet 2019; 394 (10192): 2. doi: 10.1016/S0140–6736(19)31522–3 |
| e9. | Duvivier RJ, Wiley E: WHO’s slow progress on transgender and gender diverse health. Lancet 2019; 394: 1901 |
| e10. | Hackl AM, Becker AB, Todd ME: “I Am Chelsea Manning”: Comparison of gendered representation of private manning in U.S. and international news media. J Homosex 2016; 63: 467–86 |
| e11. | Sineath RC, Woodyatt C, Sanchez T, et al: Determinants of and barriers to hormonal and surgical treatment receipt among transgender people. Transgender Heal 2016; 1: 129–36 |
| e12. | Medizinischer Dienst des Spitzenverbandes Bund der Krankenkassen e.V. (MDS): Begutachtungsanleitung Geschlechtsangleichende Maßnahmen bei Transsexualität. Grundlagen der Begutachtung. 2009. www.mds-ev.de (last accessed on 9 June 2020). |
| e13. | Cools M, Nordenström A, Robeva R, et al.: Caring for individuals with a difference of sex development (DSD): a consensus statement. Nat Rev Endocrinol 2018; 14: 415–29 |
| e14. | Moore E, Wisniewski A, Dobs A: Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab 2003; 88: 3467–73 |
| e15. | Manson JAE, Chlebowski RT, Stefanick ML, et al.: Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the women’s health initiative randomized trials. Obstet Gynecol Surv 2014; 69: 83–5 |
| e16. | Mohammed K, Abu Dabrh AM, Benkhadra K, et al.: Oral vs transdermal estrogen therapy and vascular events: a systematic review and Meta-analysis. J Clin Endocrinol Metab 2015; 100: 4012–20 |
| e17. | Marjoribanks J, Farquhar C, Roberts H, Lethaby A, Lee J: Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst Rev 2017; 1: CD004143 |
| e18. | Vinogradova Y, Coupland C, Hippisley-Cox J: Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ 2019; 364: k4810 |
| e19. | Nast A, Dréno B, Bettoli V, et al.: European evidence-based (S3) guideline for the treatment of acne–update 2016–short version. J Eur Acad Dermatol Venereol 2016; 30: 1261–8 |
| e20. | Cheng PJ, Pastuszak AW, Myers JB, Goodwin IA, Hotaling JM: Fertility concerns of the transgender patient. Transl Androl Urol 2019; 8: 209–18 |
| e21. | Miksad RA, Bubley G, Church P, et al.: Prostate cancer in a transgender woman 41 years after initiation of feminization. JAMA 2006; 296: 2316–7 |

- PDF-Version
- Table of contents
- German version
- Request permissions
Specialities
- Endocrinology / Diabetology
- Internal Medicine
- Psychosomatic Medicine and Psychotherapy
Citation manager
- Reference Manager
Select site language
- Slovenščina
Access to sex reassignment surgery
Key aspects.
- In thirteen out of twenty-eight Member States, general surgery rules apply as regards the age at which children can request a sex reassignment surgery. In this context, the age requirement for access to medical treatment without the consent of the parents or of a public authority is 18 years in Bulgaria, Cyprus, Greece, France, Hungary, Romania and Slovakia , and 15 years in Slovenia . In the United Kingdom the age requirement ranges from 16 in Scotland to 17 in England and 18 in Wales . In Belgium, Estonia, Germany and Luxembourg the child’s maturity is assessed.
- In Austria , Czechia, Croatia, Denmark, Finland, Italy, Latvia, Lithuania , the Netherlands , Poland, Portugal, Spain and Sweden the minimum age requirement to request sex reassignment surgery is explicitly set at the age of 18.
- Overall, twenty Member States (and Wales ) only allow sex reassignment surgeries in individuals over the age of 18. Out of these, twelve Member States also set 18 as the age requirement for transgender hormone therapy, while in the case of sex reassignment surgery, eight countries ( Czechia, Denmark, Finland , the Netherlands, Latvia, Poland, Spain and Sweden ) ask for a higher age than for transgender hormone therapy.
- In Ireland and Malta , the age requirement for sex reassignment surgery is 16 years.
- Croatia allows children to have sex reassignment surgery before the age of 18 if they have parental consent, without laying down any specific minimum age requirement.
Language English
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dtsch Arztebl Int
- v.111(47); 2014 Nov
Satisfaction With Male-to-Female Gender Reassignment Surgery
Jochen hess.
1 Department of Urology at the University Hospital Essen
Roberto Rossi Neto
2 Clinica Urologia, General Hospital Ernesto Simoes Filho, Salvador, Brasilien
Herbert Rübben
Wolfgang senf.
3 Department of Psychosomatic Medicine and Psychotherapy, University of Essen
The frequency of gender identity disorder is hard to determine; the number of gender reassignment operations and of court proceedings in accordance with the German Law on Transsexuality almost certainly do not fully reflect the underlying reality. There have been only a few studies on patient satisfaction with male-to-female gender reassignment surgery.
254 consecutive patients who had undergone male-to-female gender reassignment surgery at Essen University Hospital’s Department of Urology retrospectively filled out a questionnaire about their subjective postoperative satisfaction.
119 (46.9%) of the patients filled out and returned the questionnaires, at a mean of 5.05 years after surgery (standard deviation 1.61 years, range 1–7 years). 90.2% said their expectations for life as a woman were fulfilled postoperatively. 85.4% saw themselves as women. 61.2% were satisfied, and 26.2% very satisfied, with their outward appearance as a woman; 37.6% were satisfied, and 34.4% very satisfied, with the functional outcome. 65.7% said they were satisfied with their life as it is now.
The very high rates of subjective satisfaction and the surgical outcomes indicate that gender reassignment surgery is beneficial. These findings must be interpreted with caution, however, because fewer than half of the questionnaires were returned.
Culturally, gender is considered an obvious, unambiguous dichotomy. The term “gender identity” denotes the consistency of one’s emotional and cognitive experience of one’s own gender and the objective manifestations of a particular gender. In gender identity disorder, one’s own anatomical sex is objectively perceived but is felt to be alien, whereas the term “gender incongruence” refers to a difference between an individual’s gender identity and prevailing cultural norms. Finally, gender dysphoria is the suffering that results. The treatment guidelines of the World Professional Association of Transgender Health (WPATH) state that gender identity need not coincide with anatomical sex as determined at birth. Transgender identity should therefore be considered neither negative nor pathological ( 1 ). Unfortunately, gender incongruence often leads to discrimination against the affected individual, which can favor the development of psychological complaints such as anxiety disorders and depression ( 2 – 4 ). While some transgender individuals are able to realize their gender identity without surgery, for many gender reassignment surgery is an essential, medically necessary step in the treatment of their gender dysphoria ( 5 ). Research conducted to date has shown that gender reassignment surgery has a positive effect on subjective wellbeing and sexual function ( 2 , 6 , 7 ). The surgical procedure (penile inversion with sensitive clitoroplasty) is described in eBox 1 .
Surgical procedure for penile inversion vaginoplasty
- Open the scrotum.
- Remove both testicles, including the spermatic cord, from the superficial inguinal ring.
- Make a circular cut around the skin of the shaft of the penis under the glans and prepare the skin of the shaft of the penis as far as the base of the penis.
- Separate the urethra from the erectile tissue.
- Separate the neurovascular bundle from the erectile tissue.
- Perform bilateral resection of the erectile tissue.
- Create a space for the neovagina between the rectum and urethra or prostate (the prostate is left intact).
- Invert the skin of the shaft of the penis and close the distal end.
- Insert a placeholder into the neovagina (= the inverted skin of the shaft of the penis).
- Create passages for the neoclitoris (former glans penis) and urethra and then fix in place.
- Inject fibrin glue into the neovagina.
- Position the neovagina, including the placeholder.
- Adjust the labia majora.
- During a second operation six to eight weeks after the first, the vaginal entrance is constructed and minor plastic corrections are made if necessary.
Surgery lasts an average of approximately 3.5 hours. Preservation of the neurovascular bundle results in a sensitive clitoroplasty. The most common complications in short-term postoperative recovery include superficial wound healing problems around the external sutures. In the medium and long term there is a risk of loss of depth ( 23 , 24 , 30 , e15 , e23 , e25 ) or breadth ( 24 , 30 , e11 , e19 , e25 ) of the neovagina in particular. These problems usually result from inconsistent dilatation ( e27 ).
No official figures are available on the prevalence of transgender or gender-nonconforming individuals, and it is very difficult to arrive at a realistic estimate. There is no central reporting register in Germany. Furthermore, figures for those who seek medical help for gender dysphoria would in any case give only an imprecise idea of the true prevalence. The global prevalence of transgender individuals has been estimated at approximately 1 per 11 900 to 1 per 45 000 for male-to-female individuals and approximately 1 per 30 400 to 1 per 200 000 for female-to-male individuals ( 1 ). Weitze and Osburg estimate prevalence in Germany at 1 per 42 000 ( 8 ). In contrast, De Cuypere et al. ( 9 ) suppose a prevalence of 1 per 12 900 for Belgium. Biosnich et al. ( 10 ) estimate prevalence among US veterans at 1 per 4366. This compares to an estimated prevalence of 1 per 23 255 in the general population. Even if percentages of transgender individuals in different parts of the world are comparable, it is highly likely that cultural differences will lead to differing behavior and expression of gender identity, resulting in differing levels of gender dysphoria ( 1 ). The ratio of male-to-female to female-to-male transgender individuals varies greatly. Although it was given as approximately 3:1 by van Kesteren ( 11 ), it is 2.3:1 according to Weitze and Osburg ( 8 ) and 1.4:1 according to Dhejne ( 3 ). Garrels ( 12 ) found a gradual decrease in the difference between the two figures in Germany, with the ratio decreasing from 3.5:1 (in the 1950s and 60s) to 1.2:1 (1995 to 1998) ( Table 1 ).
| Author | Year | Country | MTF | FTM | MTF:FTM ratio (rounded) |
|---|---|---|---|---|---|
| (per 100000) | |||||
| Pauly ( ) | 1968 | USA | 1.0 | 0.25 | 4:1 |
| Walinder ( ) | 1968 | Sweden | 2.7 | 1.0 | 3:1 |
| Hoenig and Kenna ( ) | 1974 | UK | 3.0 | 0.93 | 3:1 |
| Ross et al. ( ) | 1981 | Australia | 4.2 | 0.67 | 6:1 |
| O’Gorman ( ) | 1982 | Ireland | 1.9 | – | 3:1 |
| Tsoi ( ) | 1988 | Singapore | 35.1 | 12.0 | 3:1 |
| Ekland et al. ( ) | 1988 | Netherlands | 18 | 54 | 3:1 |
| van Kesteren et al. ( ) | 1996 | Netherlands | 8.8 | 3.2 | 3:1 |
| Landén et al. ( ) | 1996 | Sweden | – | – | 3:1 |
| Weitze and Osburg ( ) | 1996 | Germany | 2.4 | 1.0 | 2:1 |
| Wilson et al. ( ) | 1999 | Scotland | 13.4 | 3.2 | 4:1 |
| Garrels et al. ( ) | 2000 | Germany | – | – | 1:1 |
| Haraldsen and Dahl ( ) | 2000 | Norway | – | – | 1:1 |
| Olsson and Moller ( ) | 2003 | Sweden | – | – | 2:1 |
| Gomez-Gil et al. ( ) | 2006 | Spain | 4.7 | 2.1 | 2:1 |
| de Cuypere et al. ( ) | 2007 | Belgium | 7.7 | 3.0 | 3:1 |
| Vujovic et al. ( ) | 2009 | Serbia | 0.9 | 0.9 | 1:1 |
| Coleman et al. ( ) | 2012 | Global | 8.4 | 2.2 | 4:1 |
MTF: male-to-female; FTM: female-to-male
Criteria for diagnosis
Transsexualism is primarily a problem of gender identity (transidentity) or gender role (transgenderism) rather than of sexuality ( 13 ). In Germany, it is diagnosed according to ICD-10 (10 th revision of the International Statistical Classification of Diseases and Related Health Problems).
Criteria for diagnosis include the following:
- Feeling of unease or not belonging to biological gender
- Desire to live and be accepted as a member of the opposite sex
- Presence of this desire for at least two years persistently
- Wish for hormonal treatment and surgery
- Not a symptom of another mental disorder
- Not associated with intersex, genetic, or gender chromosomal abnormalities.
Psychological aspects of transsexualism
According to Senf, no disruption to an individual’s identity is comparable in scale to the development of transsexualism ( 14 ). Transsexualism is a dynamic, biopsychosocial process which those affected cannot escape. An affected individual gradually becomes aware that he or she is living in the wrong body. The feeling of belonging to the opposite sex is experienced as an unchangeable, unequivocal identity ( 14 , 15 ). The individual therefore strives to change his or her inner identity. This change is associated with a change in psychosocial role, and in most cases with hormonal and/or surgical reassignment of the body to the desired gender ( 14 ). Coping with the development of transsexualism poses enormous challenges to those affected and often leads to a considerable psychological burden. In some cases this results in mental illness. Transsexualism itself need not lead to a mental disorder ( 14 ). Psychotherapeutic support is beneficial and is a major part of standard treatment and the examination of transsexual individuals in Germany ( 15 ).
This study aimed to evaluate the effect of male-to-female gender reassignment surgery on the satisfaction of transgender patients.
Data collection
Retrospective inquiry involved consecutive inclusion of 254 patients who had undergone male-to-female gender reassignment surgery involving penile inversion vaginoplasty at Essen University Hospital’s Department of Urology between 2004 and 2010. All patients received a questionnaire ( eBox 2 ) by post, with a franked return envelope. The questions were contained within a follow-up questionnaire developed by Essen University Hospital’s Department of Urology ( 16 ). Because the process was anonymized, patients who had not sent back the questionnaire could not be contacted. The diagnosis of “transidentity” had been made previously following specialized medical examination and in accordance with ICD-10.
Questionnaire
1. How satisfied are you with your outward appearance?
A) Very satisfied
B) Satisfied
C) Dissatisfied
D) Very dissatisfied
2. How satisfied were you with the gender reassignment surgery process?
C) Mostly satisfied
D) Dissatisfied
E) Very dissatisfied
3. How satisfied are you with the aesthetic outcome of your surgery?
4. How satisfied are you with the functional outcome of your surgery?
5. How satisfied are you with your life now, on a scale from 1 (very dissatisfied) to 10 (very satisfied)?
6. How do you see yourself today?
A) As a woman
B) More female than male
C) More male than female
D) As a man
7. Do you feel accepted as a woman by society?
A) Yes, completely
D) No/Not sure
8. Has your life become easier since surgery?
B) Somewhat easier
C) Somewhat harder
9. Have your expectations of life as a woman been fulfilled?
C) Mostly not
D) Not at all
10. How easy is it for you to achieve orgasm?
A) Very easy
B) Usually easy
C) Rarely easy
D) Never achieve orgasm
11. If you compare your orgasm earlier as a man and now as a woman, what is your orgasm like now?
A) More intense
B) Equally/Roughly equally intense
C) Less intense
Statistical evaluation was performed using SPSS (Statistical Package for the Social Sciences, 17.0). Correlation analyses were performed using SAS (Statistical Analysis System, 9.1 for Windows). The distribution of categorical and ordinal data was described using absolute and relative frequencies. Fisher’s exact test was used to compare categorical and ordinal variables in independent samples. The Mann–Whitney U-test was used to compare satisfaction scale distribution of two independent samples. This nonparametric test was used in preference to the t -test because the Shapiro–Wilk test indicated that distribution was not normal. Spearman’s correlation analysis was performed.
A total of 119 completed questionnaires were returned, all of which were included in the evaluation. This represents a response rate of 46.9%. Because the questionnaires were anonymous, no data on patients’ ages could be obtained. The average age of a comparable cohort of patients at Essen University Hospital’s Department of Urology between 1995 and 2008 ( 17 ) was 36.7 years (16 to 68 years). The median time since surgery was 5.05 years (standard deviation: 1.6 years; range: 1 to 7 years). Not all patients had completed the questionnaire in full, so for some questions the total number of responses is not 119.
Following surgery, 63 of 103 patients (61.2%) were satisfied with their outward appearance as women, and a further 27 (26.2%) were very satisfied ( Figure 1 ). 45.5% ( n = 50) were very satisfied with the gender reassignment surgery process, 30% ( n = 33) satisfied, 22.7% ( n = 25) mostly satisfied, and 1.8% ( n = 2) dissatisfied. Figure 2 shows the high rates of subjective satisfaction with the aesthetic outcome of surgery. Overall, approximately three-quarters (70 of 94 responses) reported that they were satisfied or very satisfied. A further 21 (22.3%) were mostly satisfied. Figures for satisfaction with the functional outcome of surgery were similar ( Figure 3 ). A total of 67 of 93 respondents (72%) were satisfied or very satisfied. A further 18 patients (19.4%) were mostly satisfied. Table 2 compares the rates of subjective satisfaction with aesthetic and functional outcome with other studies.

How satisfied are you with your outward appearance? (103 responses)

How satisfied are you with the aesthetic outcome of your surgery? (94 responses)

How satisfied are you with the functional outcome of your surgery? (93 responses)
| Author | Year | No. (MTF/FTM) | Country | Satisfaction (%) | Response rate (%) | ||
|---|---|---|---|---|---|---|---|
| Functional | Aesthetic | Overall | |||||
| Imbimbo et al. ( ) | 2009 | 139 (139/0) | Italy | 56 | 78 | 94 | – |
| Hess et al. | 2014 | 119 (119/119) | Germany | 91 | 97 | 96 | 47 |
| Perovic et al. ( ) | 2000 | 89 (89/0) | Serbia | 87 | 87 | – | – |
| Happich et al. ( ) | 2006 | 56 (33/23) | Germany | – | 82 | >90 | 48 |
| Löwenberg et al. ( ) | 2010 | 52 (52/0) | Germany | 84 | 94 | 69 | 49 |
| Salvador et al. ( ) | 2012 | 52 (52/0) | Brazil | 88 | – | 100 | 75 |
| Johansson et al. ( ) | 2010 | 42 (25/17) | Sweden | – | – | 95 | 70 |
| Hepp et al. ( ) | 2002 | 33 (22/11) | Switzerland | 80 | 75 | – | 70 |
| de Cuypere et al. ( ) | 2005 | 32 (32/0) | Belgium | 79 | 86 | – | – |
| Krege et al. ( ) | 2001 | 31 (31/0) | Germany | 76 | 94 | – | 67 |
| Amend et al. ( ) | 2013 | 24 (24/0) | Germany | 100 | 100 | – | – |
| Blanchard et al. ( ) | 1987 | 22 (22/0) | Canada | 73 | 90 | – | – |
| Giraldo et al. ( ) | 2004 | 16 (16/0) | Spain | 100 | 100 | – | – |
*1 Functional satisfaction includes satisfaction with depth and breadth of the neovagina and satisfaction with penetration or intercourse
*2 Aesthetic satisfaction includes satisfaction with appearance of external genitalia
In order to gather information on patients’ general satisfaction with their lives, they were asked to place themselves on a Likert scale ranging from 1 (“very dissatisfied”) to 10 (“very satisfied”). Of the total of 102 respondents, 7 (6.9 percent) selected scores from 1 to 3 (2 × 1, 1 × 2, 4 × 3) and 39 (38.2%) scores from 4 to 7 (4 × 4, 16 × 5, 8 × 6, 11 × 7). 56 patients (54.9%) placed themselves in the top third (32 × 8, 13 × 9, 11 × 10). 88 of 103 participants (85.4%) felt completely female following surgery, and 11 (10.7%) mostly female ( Figure 4 ). 69 of 102 women (67.6%) saw themselves as fully accepted as women by society, 25 (24.5%) mostly, and 6 (5.9%) rarely. Two women (2.0%) were not sure of their answer to this question. Of 95 respondents, 65 (68.4%) answered with a clear “Yes” that their life had become easier since surgery. 14 (14.7%) found life somewhat easier, 9 (9.5%) somewhat harder, and 7 (7.4%) harder. Expectations of life as a woman were completely fulfilled for 51 of 102 (50.0%) women, and mostly for 41 (40.2%). The expectations of 6 (5.9%) patients were mostly not fulfilled, and those of 4 (3.9%) were not fulfilled at all.

How do you see yourself today? (103 responses)
There was a correlation between self-perception as a woman (“How do you see yourself today?”) and perceived acceptance by society ( r = 0.495; p <0.01). There was also a correlation between self-perception and answers to whether life had become easier since surgery ( r = 0.375; p <0.01) and whether expectations of life as a woman had been fulfilled ( r = 0.419; p <0.01). Patients who saw themselves completely as women reported higher scores for current satisfaction with their lives than patients who only saw themselves as more female than male ( r = 0.347; p <0.01).
Patients were asked how easy they found it to achieve orgasm. A total of 91 participants answered this question: 75 (82.4%) reported that they could achieve orgasm. Of these, 19 (20.9%) still achieved orgasm very easily, 39 (42.9%) usually easily, and 17 (18.7%) rarely easily. Participants were also asked to compare their experience of orgasm before and after surgery (more intense/the same/less intense). Over half of those who answered this question (43 of 77, 55.8%) experienced more intense orgasm postoperatively, and 16 patients (20.8%) experienced the same intensity.
According to Sohn et al. ( 18 ), subjective satisfaction rates of 80% can be expected following gender reassignment surgery. Löwenberg ( 19 ) reported 92% general satisfaction with the outcome of gender reassignment surgery. The study by Imbimbo et al. ( 20 ) found a similarly high satisfaction rate (94%); however, subjective assessment of general satisfaction and the question of whether or not patients regretted the decision to undergo gender reassignment surgery were queried in one combined question. It is likely that most patients do not actually regret their decision to undergo surgery, even though general postoperative satisfaction is limited. Löwenberg’s figures also show this ( 19 ): 69% of those asked were satisfied with their overall life situation, but 96% would opt for surgery again. In the authors’ own study population, general satisfaction with surgery was achieved in 87.4% of patients. Regardless of surgical results, over half of patients (54.9%) were in the top third (“completely satisfied”) and a further 38.2% in the middle third (“fairly satisfied”) of the general life satisfaction scale.
A retrospective survey performed by Happich ( 21 ) found more than 90% satisfaction with gender reassignment. Sexual experience following surgery is a very important factor in satisfaction with gender reassignment. It depends essentially on the functionality of the neovagina. Figures for satisfaction with functional outcome range from 56% to 84% ( 16 , 19 , 20 , 22 , 23 ). In the authors’ population, satisfaction with function was 72% (“very satisfied” and “satisfied”) or 91.4% (including also “mostly satisfied”). According to Happich ( 21 ), satisfaction with sexual experience is positively correlated with satisfaction with outcome of surgery. Other studies ( 16 , 23 – 25 ) have also found surgical outcome to be one of the essential factors in postoperative satisfaction. Löwenberg ( 19 ) also found a correlation between satisfaction with surgery and satisfaction with aesthetic appearance of the external genitalia. In our study, almost all patients (98.2%) were satisfied with the gender reassignment surgery process ( n = 50, 45.5% “very satisfied”; n = 33, 30% “satisfied”; n = 25, 22.7% “mostly satisfied”).
The Imbimbo et al. working group ( 20 ) reported 78% satisfaction with aesthetic appearance of the neogenitalia (36% “very satisfied,” 32% “satisfied,” 10% “mostly satisfied”). Happich found 82.1% satisfaction with outcome of surgery (46 of 56 patients). Of these, 33.9% of patients reported high satisfaction and 48.2% good to medium satisfaction ( 21 ). A similar value was obtained in the survey by Hepp et al. ( 22 ). Löwenberg ( 19 ) found higher values (94%) for satisfaction with aesthetic outcome of surgery. This population included 106 male-to-female transgender individuals who underwent surgery at Essen University Hospital’s Department of Urology between 1997 and 2003. In the population described here (254 patients, 2004 to 2010) satisfaction with aesthetic outcome was still higher (96.8%).
Orgasm was possible for 82.4% of study participants. The ability to achieve orgasm was lower than in an earlier study population ( 16 ). Figures in the literature vary widely (29% to 100%) and sometimes include small case numbers ( Table 3 ). Overall, the figures for this study match those of comparable studies of a similar size. Finally, it is not clear why more than half the participants experienced orgasm more intensely following surgery than preoperatively. One possible explanation is that postoperatively patients were able to experience orgasm in a body that matched their perception.
| Author | Year | No. of patients (n) | Able to achieve orgasm (%) |
|---|---|---|---|
| Lawrence ( ) | 2005 | 232 | 85 |
| Lawrence ( ) | 2006 | 226 | 78 |
| Hess et al. | 2014 | 119 | 82 |
| Perovic et al. ( ) | 2000 | 89 | 82 |
| Goddard et al. ( ) | 2007 | 64 | 48 |
| Hage and Karim ( ) | 1996 | 59 | 80 |
| Salvador et al. ( ) | 2012 | 52 | 88 |
| Eicher et al. ( ) | 1991 | 50 | 82 |
| Bentler ( ) | 1976 | 42 | 67 |
| Jarrar et al. ( ) | 1996 | 37 | 60 |
| de Cuypere et al. ( ) | 2005 | 32 | 50 |
| Krege et al. ( ) | 2001 | 31 | 87 |
| Selvaggi et al. ( ) | 2007 | 30 | 85 |
| Rehman et al. ( ) | 1999 | 28 | 79 |
| Amend et al. ( ) | 2013 | 24 | 96 |
| van Noort and Nicolai ( ) | 1993 | 22 | 82 |
| Blanchard et al. ( ) | 1987 | 22 | 82 |
| Eldh ( ) | 1993 | 20 | 100 |
| Schroder and Carroll ( ) | 1999 | 17 | 66 |
| Rakic et al. ( ) | 1996 | 16 | 63 |
| Ross and Need ( ) | 1989 | 14 | 85 |
| Lief and Hubschman ( ) | 1993 | 14 | 29 |
| Giraldo et al. ( ) | 2004 | 16 | 100 |
| Lindemalm et al. ( ) | 1986 | 13 | 46 |
| Rubin ( ) | 1993 | 13 | 92 |
| Stein et al. ( ) | 1990 | 10 | 80 |
| Freandt et al. ( ) | 1993 | 10 | 70 |
Limitations
The response rate of less than 50% must be mentioned as a shortcoming of this study. This may have led to a bias in the results. If all patients who did not take part in the survey were dissatisfied, up to 50.1% and 54.6% would be dissatisfied with aesthetic or functional outcome respectively. According to Eicher, the suicide rate in transgender individuals following successful surgery is no higher than in the general population ( 26 ), so suicide is a very unlikely reason for nonparticipation. Contacting transfemale patients for long-term follow-up after successful surgery is generally difficult (2, 3, 22, 23, 25, 27, 28). This may be because a patient has moved since successful surgery, for example, ( 21 ). Postoperative contact is particularly difficult in countries such as Germany which have no central registers. Response rates to surveys in retrospective research are between 19% ( 28 ) and 79% ( 29 ). Goddard et al. obtained a response rate of 30% in a retrospective survey following gender reassignment surgery ( 30 ). A follow-up survey performed by Löwenberg et al. had a similar response rate, 49% ( 19 ). It is also possible that the positive results of our survey represent patients’ wish for social desirability rather than the real situation. However, this cannot be verified retrospectively.
Taking into account the limitations mentioned above, the high rates of subjective satisfaction with outward female appearance and with aesthetic and functional outcome of surgery indicate that the study participants benefited from gender reassignment surgery.
Key Messages
- At the core of the transsexual experience lies the awareness that one is a member of a realistically perceived anatomical sex (matching of genotype and phenotype), but a subjective feeling of belonging to the other gender.
- Change to the gender inwardly identified with is associated with a change in psychosocial role and in most cases with hormonal and surgical reassignment of the body to the desired gender.
- Although transsexualism itself is not a mental disorder, it can favor the development of mental problems.
- Transsexualism is a dynamic, biopsychosocial process which affected individuals cannot escape.
- The high rates of subjective satisfaction with outward female appearance and with aesthetic and functional outcome of surgery indicate that study participants benefited from gender reassignment surgery.
Acknowledgments
Translated from the original German by Caroline Devitt, M.A.
Conflict of interest statement
Dr. Hess has received reimbursement of conference fees and travel expenses from AMS American Medical Systems.
The other authors declare that no conflict of interest exists.
In the News
- Israel-Hamas War Live Updates
- Lebanon Pager Blasts
- Netanyahu-Sa'ar
- Israel-Hezbollah
- Laura Loomer
- Israeli Hostages
- Israelis Dead
Recalling the First Sex Change Operation in History: A German-Israeli Insurance Salesman
The long-forgotten story of a German Jew who was born as Martha and escaped the Nazis as Karl, rediscovered by a Tel Aviv University student.
“Karl Meir Baer, 1956,” says the simple headstone on a grave at Tel Aviv's Kiryat Shaul Cemetery.
Pager Blasts Humiliated Hezbollah, but They Won't Win Any Wars for Israel
Four israeli soldiers killed in gaza fighting; sirens activated across northern israel, the government has declared war on israeli citizens, does israel's sleepy opposition even want to bring down netanyahu's coalition, only a kahanist kind of judaism has no room for compassion toward children, learn how to optimize your home solar system, what made an israeli student work for iranian intelligence, fear of israel's occupation of gaza pushes egypt closer to turkey, israeli gov't's apocalyptic vision: turning gaza into west bank, and west bank into gaza, israeli society has truly fallen to cruelty, violence and apathy. just look at us, why a jewish writer canceled by the progressive left is leaving america, top psychiatrist working with october 7 victims has a warning for israel.
PERSPECTIVE article
Healthcare for trans*gender people in germany: gaps, challenges, and perspectives.

- 1 Department of Psychiatry and Psychotherapy, University of Tübingen, Tübingen, Germany
- 2 Graduate Training Centre of Neuroscience, University of Tübingen, Tübingen, Germany
- 3 Emotion Neuroimaging Lab, Max Planck Institute for Human Cognitive and Brain Sciences, Leipzig, Germany
- 4 International Max Planck Research School on Neuroscience of Communication: Function, Structure, and Plasticity, Leipzig, Germany
- 5 Department of Psychiatry, Psychotherapy and Psychosomatics, RWTH Aachen University, Aachen, Germany
- 6 Institute of Neuroscience and Medicine, JARA-Institute Brain Structure Function Relationship (INM 10), Research Center Jülich, Jülich, Germany
- 7 LEAD Graduate School and Research Network, University of Tübingen, Tübingen, Germany
- 8 International Max Planck Research School for Cognitive and Systems Neuroscience, University of Tübingen, Tübingen, Germany
- 9 TübingenNeuroCampus, University of Tübingen, Tübingen, Germany
People whose gender does not correspond to the binary gender system, i.e., trans ∗ gender people, face two main problems when it comes to healthcare in Germany: (1) They often suffer from general psychiatric comorbidities as well as specific and significant mental distress due to gender dysphoria, and (2) the German healthcare system lacks sufficiently educated and clinically experienced medical personnel who are able to provide specialized healthcare. Aside from transition, it often is extremely difficult for trans ∗ gender people to get access to and be integrated into the medical system. Stigmatization and pathologization in treatment are widespread, as are long waiting times for specialized healthcare providers who are often only accessible to those trans ∗ gender people willing to travel long distances. Frequently, trans ∗ gender people face further difficulties and barriers after transition, as some healthcare professionals fail to provide suitable care (e.g., gynecological consultation for transmen). The ICD-11 German Modification (ICD-11-GM), which should be routinely used by 2022, implements a depathologization of trans ∗ gender people in the medical system. This paper compares the issues related to health and healthcare of trans ∗ gender people in Germany with those in other European countries. We review the care offered by specialized centers with regard to treatment of and support for trans ∗ gender people. We conclude with specific proposals that may contribute to establish an improved, up-to-date, gender-sensitive healthcare system.
Introduction – Gaps and Challenges
Modern societies are widely dominated by a hegemonic binary view of people’s gender identity as well as a heteronormative understanding of relationships. Even in liberal democracies, where a pluralist understanding of different sexual, religious and lifestyle orientations are commonly accepted, trans ∗ gender people are confronted with this “heterosexual matrix” ( Butler, 1991 ) on a daily basis. Correspondingly, the healthcare systems in these societies have institutionalized an exclusive binarity: medicine largely operates with the classification “male” and “female” as the only expected expression of gender, with most of the current models for mental disorders still relying on male data only ( Shansky, 2019 ). This is especially problematic when it comes to healthcare for non-binary people. They face insufficient medical care, which is aggravated by treatment providers’ lack of awareness of their concerns and insufficient knowledge of gender-sensitive medicine. People whose gender identity does not correspond to the perceived norm are negatively affected by this lack of knowledge with some of them facing severe stress and discomfort. Unsurprisingly, trans ∗ gender individuals are at higher risk to report mental health problems than cisgender individuals. For example, a recent comparative study of mental health issues among cisgender and trans ∗ gender people indicated that 77% of the included trans ∗ gender participants were diagnosed with a mental disorder vs. 37,8% in cisgender participants ( Hanna et al., 2019 ). Several studies show an elevated risk for affective disorders, anxiety disorders, and addictive disorders in trans ∗ gender people compared to cisgender individuals ( Reisner et al., 2016 ; Bouman et al., 2017 ; De Freitas et al., 2020 ). In addition, increased suicidality for trans ∗ gender people compared to the cisgender population has been reported ( Goldblum et al., 2012 ; Bailey et al., 2014 ; Reisner et al., 2016 ; Adams et al., 2017 ; Yüksel et al., 2017 ). This increased risk of comorbidities could be replicated in several countries worldwide, including data from the Lebanon ( Ibrahim et al., 2016 ), the United States ( Hanna et al., 2019 ), and the Republic of Côte d’Ivoire ( Scheim et al., 2019 ). Consequently, mental health issues do not result from gender incongruence and stress/rejection/discomfort experienced by the individuals alone but are possibly further promoted by the binary-gendered thinking and treatment routines of the healthcare systems as they exist in most societies around the globe.
Interestingly, the question why trans ∗ gender people have increased comorbidity rates can still be considered unanswered ( Reisner et al., 2016 ). Some authors refer to the model of internalized homonegativity in order to explain increased risk and high prevalence of mental comorbidities in trans ∗ gender people ( Bockting et al., 2013 , Bockting, 2015 ; Breslow et al., 2015 ). Internalized homonegativity describes how non-heterosexual people internalize socio-culturally predetermined negative attitudes and images ( Göth and Kohn, 2014 ). This model is in line with societies’ heteronormativity as it explains how predominant socio-culturally norms can lead to self-pathologizing ( Rauchfleisch et al., 2002 ; Günther et al., 2019 ) which in turn can cause psychological distress and may finally result in mental health conditions ( Bockting et al., 2013 ; Breslow et al., 2015 ; Perez-Brumer et al., 2015 ; Scandurra et al., 2018 ). This internalization process can be applied correspondingly to trans ∗ gender persons inasmuch as gender identities are conceived of as stable, binary and invariant personality traits. Accordingly, this can be conceptualized as internalized transphobia ( Bockting et al., 2013 ; Bockting, 2015 ; Breslow et al., 2015 ). The notion that mental comorbidities solely arise due to gender incongruence and dysphoria therefore seems decidedly too one-dimensional, ignoring the underlying complexity.
The Evolution and Current Healthcare for Trans ∗ gender in Germany
Trans ∗ gender healthcare in Germany has a centennial history already. In 1922, the German sexologist Magnus Hirschfeld, founder of the first Institute for Sexology, carried out the worldwide first sex reassignment surgery in Berlin ( Bhinder and Upadhyaya, 2021 ). In the post-war German society, the situation of trans ∗ gender persons was recognized only very haltingly. The so-called “transsexual law” (TSG) from 1980 implemented changes of personal and civil status. The law since required trans ∗ gender persons to undergo surgical alteration of their genitals in order to have key identity documents changed. This was declared unconstitutional only in 2011.
Besides the legal framework there were no regulations for medical and psychotherapeutic healthcare for trans ∗ gender people whatsoever until the publication of the German Standards for the Treatment and Diagnostic Assessment of Transsexuals (1997) ( Nieder and Strauß, 2015 ). These standards provided temporal and diagnostic frameworks and concrete guidelines according to which gender-affirming procedures may take place. Stemming from the desire to enable trans ∗ gender people to follow a self-determined and individualized transition, the new S3 guidelines from 2018 [“Gender incongruence, gender dysphoria, and trans health: S3 guideline on diagnosis, counseling, and treatment” ( Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften [AWMF], 2019 )] have been developed in collaboration with experts and interest groups. In contrast to the precursor from 1997, the new guidelines take a less directive and more participatory approach ( Nieder and Strauß, 2019 ). Hence, treatment seekers and treatment providers are now able to find individual solutions together on equal terms. Access restrictions should no longer exist. Thus, gender-affirming hormone treatment can already be used after diagnosis, at the beginning of the transition. Psychotherapy should no longer be a prerequisite for gender-affirming therapy but should accompany the transition and promote self-acceptance and stability ( Nieder and Strauß, 2019 ). However, the report guidelines of the medical service of the health insurance funds (MDS) contradict the S3 guidelines by continuing to set strict framework conditions for the treatment costs to be covered by the public health insurance funds. Also, the guidelines for the diagnosis of trans ∗ gender criteria from the ICD-10 catalog are less flexible and more stigmatizing than the S3 guidelines. Trans ∗ gender is coded as “transsexualism” ( Graubner, 2013 ). There, the main criterion is the desire of a person to belong to the binary opposite gender. This may include the desire to change sex characteristics (primary or secondary) and to be recognized as belonging to this gender. The desire must be constant for 2 years and must not result from mental disorder. The ICD-10 defines transsexualism as a disorder, subclassified in the section of disorders of adult personality and behavior ( Graubner, 2013 ).
Therefore, practitioners in Germany find themselves in a field of tension between the prevailing strict conditions imposed by health insurance and the ICD-10 catalog and attempts to loosen the regulations in accordance with the individual needs of trans ∗ gender people. This also explains ambivalent reactions and uncertainties on the part of the practitioners to the S3 guidelines ( Nieder and Strauß, 2019 ). In this constellation, it is expected that the new ICD-11 catalog 2022 will bring further change, as transsexualism will be coded in the section “Conditions affecting sexual health,” thus separating trans ∗ gender from somatic or mental illness ( Jakob, 2018 ). This was already successfully implemented in the Diagnostic and Statistical Manual of Mental Disorders-V (DSM-V), according to which it is only possible to speak of a disorder when there is relevant suffering due to the gender incongruence (dysphoria) ( American Psychiatric Association, 2013 ). According to MDS the assessment instructions will have to be revised after ICD-11 has been established.
Trans ∗ gender healthcare in Germany is provided in different institutions. Usually, medical services are provided in private practices. In addition, interdisciplinary healthcare supplies are available via outpatient care, such as the regional “Qualitätszirkel.” These are regional associations of multidisciplinary trans ∗ gender healthcare specialists. There are hardly any centers that offer multiprofessional treatment. The interdisciplinary care center at the University Hospital of Hamburg plays a pioneering role in this area. Some university hospitals offer specialized consultation hours, such as the specialized outpatient clinic for transsexuality and trans ∗ gender in Tübingen, which was established in October 2020. This service is primarily aimed at trans ∗ gender people before and during transition. To the best of our knowledge, there are no central registers for medical services for trans ∗ gender people. Online, there are lists of addresses maintained by interest groups. Figure 1 depicts the institutions providing treatment in Germany and the “Qualitätszirkel” (individual practices or clinics that only cover somatic needs are not listed). They offer various services: psychotherapeutic support, indication letters, medical reports to the TSG and partly interdisciplinary services. Healthcare services offered to trans ∗ gender persons are covered by the health insurance and thus are covered publically, as was decided in 1987 by the Federal Social Court, the Bundessozialgericht (BSG 3 RK 15/86). However, letters of indication from experts are necessary in order that services (e.g., hormonal treatment, surgery) are covered by the health insurance.
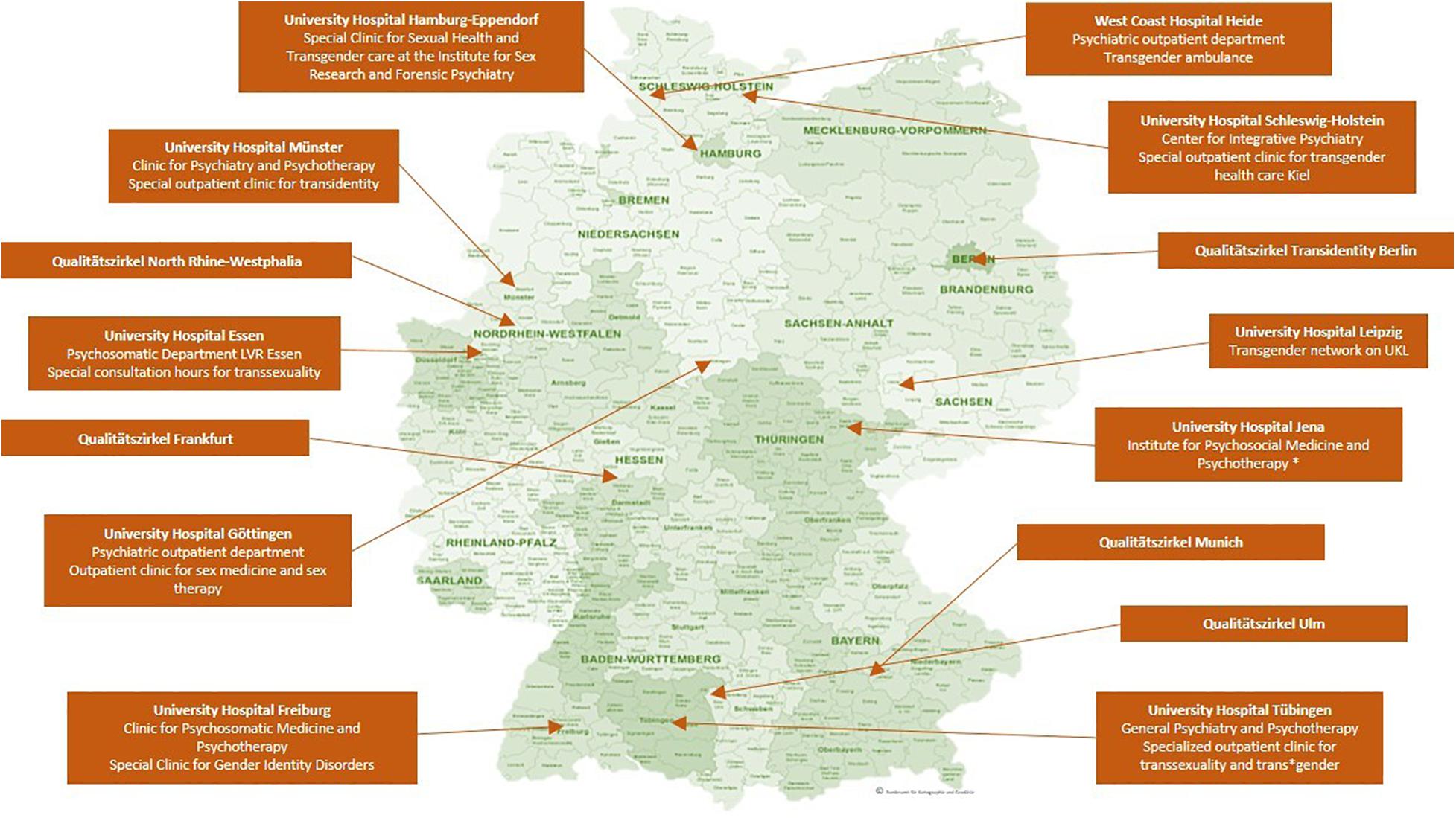
Figure 1. Institutions providing specialized trans ∗ gender healthcare in Germany. The map shows the location of clinics and regional associations of multidisciplinary healthcare specialists (“Qualitätszirkel”) that offer specialized trans ∗ gender healthcare in Germany, without claiming to be exhaustive. ∗ : According to the clinic‘s website only expert opinions are issued. However, this is listed differently on the website of https://transmann.de . © Bundesamt für Kartographie und Geodäsie.
How Does the Healthcare System Understand Trans ∗ gender Nowadays?
Trans ∗ gender people experience incongruence between the sex assigned at birth and their gender identity. Sex assignment is based on the external genital, which are usually defined in medical literature as indicators of the so-called biological sex. To avoid classifying non-binary gender identities as a deviation from the biological sex, the terminology “assigned gender” or “assignment gender” seems more suitable than the term “biological sex” ( Günther et al., 2019 ). Gender identity describes a person’s certainty and conviction to belong to a certain gender ( Eckloff, 2012 ). This develops during the course of a person’s life and is shaped by biological and social conditions equally ( Göth and Kohn, 2014 ). In trans ∗ gender people, gender identity does not develop in accordance with the assigned sex; the result can be a binary or a non-binary form of gender identity: Binary trans ∗ gender indicates that individuals experience themselves as belonging to the binary opposite gender (i.e., transman or transwoman). However, there are also people who feel they belong to neither the female nor the male gender and/or experience their gender on a continuum between the sexes ( Günther et al., 2019 ).
In terms of prevalence rates in European countries, similar rates have been reported, always indicating a slightly higher prevalence rate for trans ∗ women. The prevalence of the ICD-10 diagnosis of transsexualism is estimated at 1:12000 for trans ∗ women and 1:30000 for trans ∗ men in Germany ( Schneider et al., 2007 ). In Belgium, 1:12900 trans ∗ women have undergone gender-affirming surgery, while in men this ratio is approximately 1:33800 in trans ∗ men ( De Cuypere et al., 2007 ). Netherlands show similar prevalence rates (1:11900 for trans ∗ women and 1:30400 for trans ∗ men) ( Bakker et al., 1993 ). However, an increase in prevalence has been reported in several countries: in Germany, for example, a 2.6-fold increase in the number of inpatients who were diagnosed with a gender identity disorder between 2000 and 2014 has been reported (data of the German Federal Statistical Office) ( Brunner et al., 2017 ). Brunner et al. (2017) discuss the increased amount of informational martials and the facilitated access to gender-affirming therapy as a cause of the reported increase in prevalence. Whether and how destigmatization of trans ∗ gender individuals further contributes to the increased prevalence rates needs to be investigated. Unfortunately, standardized prevalence rates of trans ∗ gender individuals are rarely to be found ( Collin et al., 2016 ), as different definitions of trans ∗ gender samples lead to different results in prevalence, obscuring the systematic investigation. Furthermore, the prevalence might be underestimated, as not all trans ∗ gender persons seek gender affirming therapy ( De Freitas et al., 2020 ). After the introduction of the new ICD-11, it should be possible to record comparable prevalence rates of the diagnosis gender dysphoria instead of transsexualism.
The Healthcare System’s Influence on the Emergence and Maintenance of Suffering of Trans ∗ gender People Focused on the Situation in Germany
The German medical system has institutionalized stigmatization of non-binary people, which has to be especially considered a substantial factor of trans ∗ gender persons’ healthcare situation. This mainly applies to non-trans ∗ gender specific medical care, but also partly to trans ∗ gender healthcare. The variety of experiences of discrimination within the healthcare system have already been pointed out ( Franzen and Sauer, 2010 ; Grant et al., 2011 ; LesMigras, 2012 ; Bradford et al., 2013 ; Roberts and Fantz, 2014 ; Günther et al., 2019 ). However, since discrimination refers to distinctions that lead to, produce, or give rise to disadvantage ( Scherr et al., 2017 ), it often seems more appropriate to speak of stigmatization in the context of trans-specific healthcare in Germany. Stigmatization means the designation and marking of a deviation from a norm which is given or desired within a society ( Goffman, 1963 ). Stigmatized persons are denied the status of a normal member of society because of an attribution of characteristics marked as a deviation. Institutional stigmatization occurs within social systems or organizations, where routines in communication and actions perpetuate “normality,” which force the presentation and treatment of deviations from this norm as explicit deviations. Trans ∗ gender people experience this institutional stigmatization in modern medicine in Germany and worldwide ( Franzen and Sauer, 2010 ; Fuchs et al., 2012 ; LesMigras, 2012 ).
In itself, the structure of the healthcare system in Germany can be experienced as exclusionary by trans ∗ gender individuals: Identification documents, such as health insurance cards, may not match the gender, cause confusion in providers and can lead to misgendering which in turn is experienced as stigmatizing ( Roberts and Fantz, 2014 ). In the context of medical treatment in Germany, they presumably experience not so much discriminatory disadvantage as invalidation of their gender identity. Günther et al., suggest that exposition to the healthcare system may trigger internalized transphobia among trans ∗ gender people, due to the fact that it occasionally puts the trans ∗ gender individual under pressure to legitimize their own gender identity ( Günther et al., 2019 ).
Because of experienced and/or feared stigmatization, some people are not willing to utilize the medical system. Studies from different countries show that the use of the healthcare system in trans ∗ gender people is reduced due to fear of discrimination ( Bauer et al., 2014 ). In the US-American “national transgender survey” stigmatization experiences of trans ∗ gender persons were documented. One of the key findings reports a high likelihood of discrimination if the medical provider knows about their patients trans ∗ gender identity. They also identify a lack of knowledge by the medical providers, so most of trans ∗ gender people themselves have to inform their doctors about trans ∗ gender healthcare ( Grant et al., 2011 ). In Germany trans ∗ gender persons report that their experiences with the healthcare system depend on whether their trans ∗ identity remains hidden or becomes visible ( LesMigras, 2012 ). Stigmatizing experiences in the healthcare system are among the most common negative experiences of trans ∗ gender persons in Germany, after discrimination at the workplace ( LesMigras, 2012 ). As a result, the health of this group of people is under-supplied, as they typically leave the health system after negative experiences and seek help elsewhere ( Mizock and Lewis, 2008 ).
Due to the deeply embedded heteronormativity in Germany’s society, it is unsurprising that medical areas that are not primarily oriented toward trans ∗ gender healthcare show an unprofessional handling when they face gender identities that do not correspond to this supposed norm. Correspondingly, a study in North-Rhine-Westphalia (Germany) shows that trans ∗ gender persons were hardly satisfied with their psychotherapeutic support ( Fuchs et al., 2012 ). The same study reveals the administrative and treatment burdens caused by the MDS review procedure. It has also been shown, that the institutional pathologizing of trans ∗ identity is experienced as a tremendous burden by trans ∗ gender people ( LesMigras, 2012 ). As outlined in section “The Evolution and Current Healthcare for Trans ∗ gender in Germany,” the German healthcare system has been developing new ways of dealing with trans ∗ gender healthcare. It is in a transition period between strict regulation and self-determination of the trans ∗ gender community. Studies on the fears and wishes of the trans ∗ gender community for multiprofessional treatment centers (as the one in Hamburg) show that also on the part of the treatment providers this development is being worked on and the offers are being adapted to the needs of the trans ∗ gender community ( Eysell et al., 2017 ).
Trans ∗ gender people depend on the healthcare system as they require medical professionals before, during and after gender affirming therapy. Even after a successful transition, psychotherapeutic and somatic care must be ensured. Due to hormone therapy, trans ∗ gender persons have a different lifetime risk profile for cardiovascular diseases ( Aranda et al., 2019 ; Dutra et al., 2019 ; Pyra et al., 2020 ). The risk for sex-hormone dependent cancers is not higher during gender-affirming hormone therapy, but the cancer screening recommendations have to be considered in trans ∗ gender people as well, i.e., prostate cancer screening in transwomen or breast and cervical cancer screening in transmen ( McFarlane et al., 2018 ). Because of this need, it is alarming that the stigmatization in the healthcare system increases the chance for trans ∗ gender people to avoid medical care and balk preventive measures, such as cancer screenings ( Günther et al., 2019 ; Weyers et al., 2021 ).
In addition, studies show that after gender-affirming therapy, psychological stress can also occur, which may lead to increased suicidality ( Rolle et al., 2015 ; Wiepjes et al., 2020 ). The lifetime prevalence of suicidality is also affected – amongst other variables – by negative experience with medical providers ( Haas et al., 2014 ).
Psychotherapeutic services should also strive to offer gender-sensitive counseling in order to adequately address internalized transphobia, specific role conflicts, and so forth. The need for specialized counseling usually is not met after transition, as trans ∗ gender persons are constantly confronted with their minority status in a binary, heterosexual environment ( Verbeek et al., 2020 ). Unfortunately, specialized training programs for psychotherapists are hardly established. Since medical professionals are usually not trained in gender-sensitive medicine and may be out of their depth with regard to the healthcare of trans ∗ gender persons, this ongoing stigmatization comes as no surprise. Therefore, gender sensitive medicine must become a part of the medical curriculum. There seems to be an interest on the part of medical students ( Turner et al., 2014 ). Finally, gender sensitive medicine has to be implemented in the standard medical care in Germany ( Chase et al., 2014 ).
Medical Care Services and Barriers for Trans ∗ gender Individuals in Europe
As we propose, the institutionally co-generated psychological strain on trans ∗ gender persons, promotes comorbidities and further increases economic costs. It seems imperative that stigma-free and need-oriented trans-specific treatment is provided by trained personnel. Only then can we reasonably expect that the psychological distress due to gender dysphoria can be minimized and fused conflicts can be addressed e.g., via psychotherapy. There is evidence for a reduction of distress through access to gender-affirming therapy ( Bränström and Pachankis, 2020 ; Almazan and Keuroghlian, 2021 ).
The mission statement of the European Professional Association for Transgender Health (EPATH), a sub-organization of the World Professional Association for Transgender Health (WPATH), envisions the establishment of uniform European healthcare for trans ∗ gender persons. By drafting a “standard of care” position paper, EPATH tries to formulate a uniform guideline for trans ∗ gender sensitive health care beyond transition. The guideline furthermore establishes basic principles, addressing medical professionals. There is a consensus that healthcare providers worldwide should adhere to these basic principles, regardless of socio-cultural norms and legal requirements of their respective country. Inter alia , EPATH urges medical personnel to treat trans ∗ gender persons respectfully and in a non-pathologizing manner. Access to treatment options should be ensured and medical personnel should be further trained in gender-sensitive medicine ( Coleman et al., 2012 ).
However, uniform and comprehensive care for trans ∗ gender persons is far from guaranteed in Europe, as the legal and medical situation is highly diverse: While some countries have been trying to ensure appropriate treatment of trans ∗ gender persons in the legal and medical domain, trans ∗ gender people in other countries are faced with persecution and discrimination ( ILGA Europe Annual Review, 2021d ). Apart from that, a legal and medical situation that considers the needs of trans ∗ gender people does not necessarily imply that sufficient medical care is provided or that medical staff are sufficiently informed. While there are specialized treatment centers in many European countries nowadays, trans ∗ gender individuals generally face the problem of long waiting times due to the structural lack of healthcare providers in the area of gender-affirming treatment services. In Netherlands treatment options (i.e., diagnostic classification, subsequent gender-affirming therapy such as hormone therapy, gender-affirming surgery) are offered in health centers (Amsterdam UMC, Groningen UMC and Radboud UMC Nijmegen). Like the center in Hamburg, they provide an interdisciplinary treatment – the so-called “gender team.” However, these centers are far from meeting the demand and a lack of healthcare providers in Netherlands has been pointed out recently ( Verbeek et al., 2020 ). In Belgium, care is also provided in healthcare centers (Belgien Universitär ziekenhuis Ghent, Université libre de Bruxelles and Le centre hospitalier universitaire de Liège), with the center in Ghent offering interdisciplinary care ( Elaut, 2014 ). In contrast to Germany, hormonal treatment in Belgium is already possible during full-time real-life experience ( Steinmetzer and Groß, 2008 ). Here, too, the long waiting times have been pointed out as problematic and as an obstacle to the access of appropriate services ( Motmans et al., 2010 ). Specialized care centers in England, Scotland, and Northern Ireland are listed by Vincent (2018) . He points out that trans ∗ gender persons have the longest waiting times of all patients in need of specialized treatment services. In Spain, the healthcare is installed in multidisciplinary gender units in different communities all over the country and the Canary Islands ( Gómez-Gil et al., 2019 ). New healthcare models deviate from the central multidisciplinary gender units, for example by offering gender-affirming healthcare without psychological assessment. These new healthcare models are the subject of controversy, because the decentralization can be considered a missed opportunity: (a) for research and (b) to collected data to evaluate the quality of healthcare ( Gómez-Gil et al., 2020a , b ).
The procedure for gender-affirming surgery in Denmark is prescribed by the Danish Health Authority and is centralized in three clinics (e.g., The Sexological Clinic, Ringshospitalet Copenhagen) ( ILGA Europe Annual Review, 2021c ). Italy is a positive example of a publicly accessible database of medical care professionals. On the website https://www.infotrans.it/ , published in 2020, trans ∗ gender people can find out about treatment services ( ILGA Europe Annual Review, 2021b ).
The situation in Poland stands out as a negative example in a discrepancy to the, as not sufficiently marked, but existing care situation in most European countries. There, no medical care for trans ∗ gender persons is guaranteed. In addition, there is talk of a hate campain against the LGBTIQ community ( ILGA Europe Annual Review, 2021a ).
Overall, healthcare in Europe is taking important steps toward depathologization, and many countries are attempting to establish the requirements of WPATH/EPATH. Worldwide, however, conditions remain poor and self-determination rights are denied to the trans ∗ gender community. In some countries trans ∗ gender persons are still criminalized (e.g., Indonesia, Niger, Malaysia, United Arab Emirates).
Key Findings
The article reviews the medical care situation for trans ∗ gender people nowadays and it provides a more detailed description of the situation in Germany. Three main deficiencies were identified, that are linked to medical care for trans ∗ gender persons in the German healthcare system: (1) A lack of specialized medical care to support transition. Mental comorbidities could be reduced by individualized support during transition. However, this is usually hindered by significant organizational and institutional barriers. Deficits in the structure of specialized healthcare services in Germany and Europe have been pointed out. There is a lack of specialized care offers that ensure a safe place for good care and that alleviate individual suffering through a professionally accompanied transition. (2) A lack of gender-sensitive psychotherapeutic support before and after transition, which could address the trans ∗ gender specific dysfunctional internalization processes in a patient-oriented, professional manner. (3) A lack of sensitivity to special treatment needs in post-transition healthcare. We elaborated that even after transition, a non-discriminatory integration into the healthcare system remains necessary. Due to exclusively binary gender thinking, medicine is prone to institutional stigmatization. Accordingly, trans ∗ gender people are frequently confronted with deficits and hurdles with the safeguard of their health. The multifactorial condition of suffering is modeled in Figure 2 .
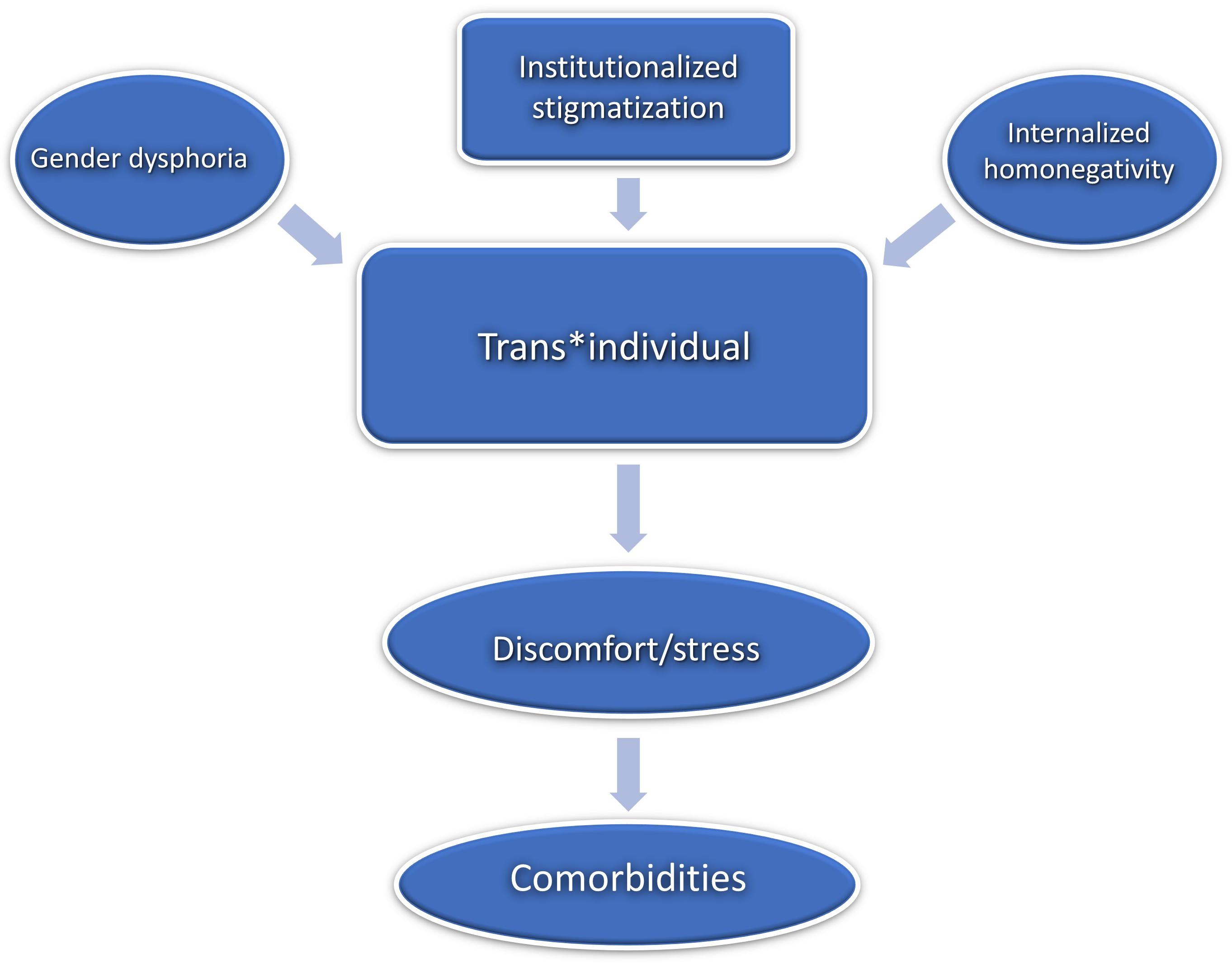
Figure 2. Multifactorial condition of suffering. © Bundesamt für Kartographie und Geodäsie.
Perspective
We see an urgent need for the establishment of comprehensive gender-affirmative healthcare. We propose three starting points: (1) A nationwide structure of specialized treatment centers for trans ∗ gender healthcare is needed. In particular, the problem of unacceptably long waiting times must be addressed. (2) Specific sexual medicine training at an early stage (i.e., at university level during education and later on in specialist training) should lay the groundwork to minimize the institutional stigmatization of trans ∗ gender individuals. (3) Finally, we call for the establishment of psychotherapeutic specialization as well as further education programs to support appropriate treatment of the diverse and multifactorial psychological issues of trans ∗ gender people.
It should be pointed out, that through increased cooperation between medical providers and advocacy groups (e.g., Transgender Europe, TGEU), the European healthcare system can be transformed into a system based on self-determination and informed consent. It is time to face and address the many faceted barriers trans ∗ gender people are facing when confronted with the healthcare system in different European countries (and probably world-wide).
In Germany we see a significant progression within the medical system toward the recognition of the trans ∗ gender community and its needs in the recent years. The implementation of the new S3 guidelines is becoming more and more important and the trans ∗ gender community is becoming more and more involved. Unfortunately, this development has not yet reached all areas. The new ICD catalog in 2022 will be an important step to further improving healthcare of trans ∗ gender individuals. We hope to contribute to establishing improved, gender-sensitive medical care in line with the variable demands of trans ∗ gender people.
Data Availability Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Author Contributions
NG prepared the first draft of the manuscript. All authors contributed to critically revising and editing the content of the manuscript and approved the final version of the manuscript for submission.
MG, CL, UH, and BD were supported by the German Research Association (DFG, DE2319/2-4).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Janina Richter, Tobias Schwippel, and Rebecca Popp for their valuable input. Also, a special thanks to Philipp Rhein, who helped reviewing the topic from a sociological perspective.
Adams, N., Hitomi, M., and Moody, C. (2017). Varied reports of adult transgender suicidality: synthesizing and describing the peer-reviewed and gray literature. Transgender Health 2, 60–75. doi: 10.1089/trgh.2016.0036
PubMed Abstract | CrossRef Full Text | Google Scholar
Almazan, A. N., and Keuroghlian, A. S. (2021). Association Between Gender-Affirming Surgeries and Mental Health Outcomes. JAMA Surg. 2021:952. doi: 10.1001/jamasurg.2021.0952
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5§). Am. Psychiatric Pub.
Google Scholar
Aranda, G., Mora, M., Hanzu, F. A., Vera, J., Ortega, E., and Halperin, I. (2019). Effects of sex steroids on cardiovascular risk profile in transgender men under gender affirming hormone therapy. Endocrinología, Diabetes y Nutrición 66, 385–392. doi: 10.1016/j.endien.2019.07.001
CrossRef Full Text | Google Scholar
Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften [AWMF] (2019). Staändige Kommission Leitlinien. AWMF-Regelwerk Geschlechtsinkongruenz, Geschlechtsdysphorie und Trans-Gesundheit: S3-Leitlinie zur Diagnostik, Beratung und Behandlung“. Überarbeitete Fassung 27.02.2019. Available online at: https://www.awmf.org/uploads/tx_szleitlinien/138-001l_S3_Geschlechtsdysphorie-Diagnostik-Beratung-Behandlung_2019-02.pdf [Accessed 05 May 2021]
Bailey, L., Ellis, S., and Mcneil, J. (2014). Suicide risk in the UK Trans population and the role of gender transition in decreasing suicidal ideation and suicide attempt. Mental Health Rev. J. 19, 209–220. doi: 10.1108/MHRJ-05-2014-0015
Bakker, A., Van Kesteren, P. J., Gooren, L. J., and Bezemer, P. D. (1993). The prevalence of transsexualism in The Netherlands. Acta Psychiatr. Scand. 87, 237–238. doi: 10.1111/j.1600-0447.1993.tb03364.x
Bauer, G. R., Scheim, A. I., Deutsch, M. B., and Massarella, C. (2014). Reported emergency department avoidance, use, and experiences of transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. Ann. Emerg. Med. 63, 713–720. doi: 10.1016/j.annemergmed.2013.09.027
Bhinder, J., and Upadhyaya, P. (2021) “Brief history of gender affirmation medicine and surgery,” in Urological Care for the Transgender Patient , eds D. Nikolavsky and S. A. Blakely (Cham: Springer), 249–254. doi: 10.1007/978-3-030-18533-6_19
Bockting, W. (2015). Internalized transphobia. Internat. Encyclop. Human Sexual. 583–625.
Bockting, W. O., Miner, M. H., Swinburne Romine, R. E., Hamilton, A., and Coleman, E. (2013). Stigma, mental health, and resilience in an online sample of the US transgender population. Am. J. Public Health 103, 943–951. doi: 10.2015/AJPH.2013.301241
Bouman, W. P., Claes, L., Brewin, N., Crawford, J. R., Millet, N., Fernandez-Aranda, F., et al. (2017). Transgender and anxiety: a comparative study between transgender people and the general population. Internat. J. Transgend. 18, 16–26. doi: 10.1080/15532739.2016.1258352
Bradford, J., Reisner, S. L., Honnold, J. A., and Xavier, J. (2013). Experiences of transgender-related discrimination and implications for health: results from the Virginia Transgender Health Initiative Study. Am. J. Public Health 103, 1820–1829. doi: 10.2015/AJPH.2012.300796
Bränström, R., and Pachankis, J. E. (2020). Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study. Am. J. Psychiatry 177, 727–734. doi: 10.1176/appi.ajp.2019.19010080
Breslow, A. S., Brewster, M. E., Velez, B. L., Wong, S., Geiger, E., and Soderstrom, B. (2015). Resilience and collective action: Exploring buffers against minority stress for transgender individuals. Psychol. Sexual Orient. Gender Div. 2:253. doi: 10.1037/sgd0000117
Brunner, F., Koops, T., Nieder, T. O., Reed, G. M., and Briken, P. (2017). Stationäre Krankenhausbehandlungen ausgewählter sexueller Störungen. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 60, 987–998. doi: 10.1007/s00103-017-2592-z
Butler, J. (1991). Das Unbehagen der Geschlechter. edition suhrkamp. Frankfurt am Main. Milton Park: Routledge
Chase, D. P., Mitar, I., Oertelt-Prigione, S., Hess, N., and Amelung, V. E. (2014). Gender Medicine And Health Insurance Policy: An Empirical Study In Germany. Value Health 17:A149. doi: 10.1016/j.jval.2014.03.866
Coleman, E., Bockting, W., Botzer, M., Cohen-Kettenis, P., Decuypere, G., Feldman, J., et al. (2012). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Internat. J. Transgend. 13, 165–232. doi: 10.1080/15532739.2011.700873
Collin, L., Reisner, S. L., Tangpricha, V., and Goodman, M. (2016). Prevalence of Transgender Depends on the “Case” Definition: A Systematic Review. J. Sexual Med. 13, 613–626. doi: 10.1016/j.jsxm.2016.02.001
De Cuypere, G., Van Hemelrijck, M., Michel, A., Carael, B., Heylens, G., Rubens, R., et al. (2007). Prevalence and demography of transsexualism in Belgium. Eur. Psychiatry 22, 137–141. doi: 10.1016/j.eurpsy.2006.10.002
De Freitas, L. D., Léda-Rêgo, G., Bezerra-Filho, S., and Miranda-Scippa, Â (2020). Psychiatric disorders in individuals diagnosed with gender dysphoria: A systematic review. Psychiatry Clin. Neurosci. 74, 99–104. doi: 10.1111/pcn.12947
Dutra, E., Lee, J., Torbati, T., Garcia, M., Merz, C. N. B., and Shufelt, C. (2019). Cardiovascular implications of gender-affirming hormone treatment in the transgender population. Maturitas 129, 45–49. doi: 10.1016/j.maturitas.2019.08.010
Eckloff, T. (2012). Die Geschlechtlichkeit des Menschen: Wie sexuelle Orientierung, Geschlechtsidentität und Geschlechtsrolle zusammenhängt. Riga: AK Akademikerverlag.
Elaut, E. (2014). Transgender health care in Belgium. Available online at: https://epath.eu/wp-content/uploads/2014/07/Transgender-health-care-in-Belgium_Els-Elaut_20150313.pdf [Accessed May19 2021].
Eysell, J., Koehler, A., Dekker, A., Sehner, S., and Nider, T. O. (2017). Nedds and concerns of transger individuals regarding interdisciplinary transgender healthcare: A non-clinical online survey. PLoS One 12:e0183014. doi: 10.1371/journal.pone.0183014
Franzen, J., and Sauer, A. (2010). Benachteiligung von Trans ∗ -Personen, insbesondere im Arbeitsleben. Expertise für die Antidiskriminierungsstelle des Bundes, Berlin. [Discrimination against trans ∗ persons, especially in employment. Expertise for the Federal Anti-Discrimination Agency, Berlin]. Available online at: https://static1.squarespace.com/static/572347337da24f738c352ec7/t/588e15708419c2ec3fdbfbc7/1485706613853/benachteiligung_von_trans_personen_insbesondere_im_arbeitsleben.pdf [Accessed July 22, 2021].
Fuchs, W., Ghattas, D. C., Reinert, D., and Widmann, C. (2012). Studie zur Lebenssituation von Transsexuellen in Nordrhein-Westfalen. [study on the quality of life of trans ∗ gender in Nordrhein-Westfalen.]. Available online at: https://www.lsvd.de/fileadmin/pics/Dokumente/TSG/Studie_NRW.pdf [Accessed July 25, 2021]
Goffman, E. (1963). Stigma. Notes on the Management of Spoiled Identity. Harmondsworth: Penguin, 1963.
Goldblum, P., Testa, R. J., Pflum, S., Hendricks, M. L., Bradford, J., and Bongar, B. (2012). The relationship between gender-based victimization and suicide attempts in transgender people. Prof. Psychol. 43:468. doi: 10.1037/a0029605
Gómez-Gil, E., Esteva de Antonio, I., Almaraz Almaraz, M., Asenjo Araque, N., Fernández Rodríguez, M., Hurtado Murillo, F., et al. (2019). Atención sanitaria en Espana a personas transexuales y con variantes de género: Historia y evolución. [New care models for transgender people in the Spanish Health System: demands, controversies and reflections.]. Psicosomatica y psiquiatría 11, 63–75.
Gómez-Gil, E., Esteva de Antonio, I., Fernández Rodríguez, M., Almaraz Almaraz, M., Hurtado Murillo, F., Gómez Blaguer, M., et al. (2020a). Nuevos modelos de atención sanitaria para las personas transgénero en el Sistema Sanitario Espanol: demandas, controversias y reflexiones [New care models for transgender people in the Spanish Health System: demands, controversies and reflections.]. Rev. Esp. Salud Publica 94:e202011123.
Gómez-Gil, E., Flo, M., Fernández, R., Esteva, I., and Gómez-Gil, F. J. (2020b). Spanish research in gender diysphoria: Areview of more than 20 years biomedical literature. Actas espanolas de pisquiatria 48, 271–286.
Göth, M., and Kohn, R. (2014). Sexuelle Orientierung: in Psychotherapie und Beratung. New York, NY: Springer-Verlag.
Grant, J. M., Mottet, L., Tanis, J. E., Harrison, J., Herman, J., and Keisling, M. (2011). Injustice at every turn: A report of the national transgender discrimination survey. Washington, DC: National Center for Transgender Equality.
Graubner, B. (2013). ICD-10-GM Version 2014 Systematisches Verzeichnis. Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme, 10. Revision-German Modification. Cologne: Deutscher Ärzteverlag GmbH.
Günther, M., Teren, K., and Wolf, G. (2019). Psychotherapeutische Arbeit mit trans ∗ Personen: Handbuch für die Gesundheitsversorgung. Munich: Ernst Reinhardt Verlag.
Haas, A. P., Rodgers, P. L., and Herman, J. L. (2014). Suicide attempts among transgender and gender non-conforming adults. Work 50:59.
Hanna, B., Desai, R., Parekh, T., Guirguis, E., Kumar, G., and Sachdeva, R. (2019). Psychiatric disorders in the US transgender population. Ann. Epidemiol. 39, 1–7. doi: 10.1016/j.annepidem.2019.09.009
Ibrahim, C., Haddad, R., and Richa, S. (2016). Psychiatric comorbidities in transsexualism: study of a Lebanese transgender population. L’encephale 42, 517–522. doi: 10.1016/j.encep.2016.02.011
ILGA Europe Annual Review (2021a). ANNUAL REVIEW OF THE HUMAN RIGHTS SITUATION OF LESBIAN, GAY, BISEXUAL, TRANS, AND INTERSEX PEOPLE IN POLAND COVERING THE PERIOD OF JANUARY TO DECEMBER 2020. Available online at: https://www.ilga-europe.org/sites/default/files/2021/poland.pdf [Accessed July 15, 2021]
ILGA Europe Annual Review (2021b). ANNUAL REVIEW OF THE HUMAN RIGHTS SITUATION OF LESBIAN, GAY, BISEXUAL, TRANS, AND INTERSEX PEOPLE IN ITALY COVERING THE PERIOD OF JANUARY TO DECEMBER 2020. Available online at: https://www.ilga-europe.org/sites/default/files/2021/italy.pdf [Accessed July 15, 2021]
ILGA Europe Annual Review (2021c). ANNUAL REVIEW OF THE HUMAN RIGHTS SITUATION OF LESBIAN, GAY, BISEXUAL, TRANS, AND INTERSEX PEOPLE IN DENMARK COVERING THE PERIOD OF JANUARY TO DECEMBER 2020. Available online at: https://www.ilga-europe.org/sites/default/files/2021/denmark.pdf [Accessed July 15, 2021]
ILGA Europe Annual Review (2021d). ANNUAL REVIEW OF THE HUMAN RIGHTS SITUATION OF LESBIAN, GAY, BISEXUAL, TRANS, AND INTERSEX PEOPLE IN EUROPE AND CENTRAL ASIA 2021. Available online at: http://rainbow-europe.org/sites/default/files/annual-report/Annual-Review-Full-2021.pdf [Accessed July 15, 2021]
Jakob, R. (2018). ICD-11–Anpassung der ICD an das 21. Jahrhundert. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 61, 771–777. doi: 10.1007/s00103-018-2755-6
LesMigras (2012). not so seizable but still real”. A quantitative and qualitative study on violence and (multiple) discrimination of lesbian, bisexual women and trans ∗ in Germany. Berlin: Lebensberatung.
McFarlane, T., Zajac, J. D., and Cheung, A. S. (2018). Gender-affirming hormone therapy and the risk of sex hormone-dependent tumours in transgender individuals—A systematic review. Clin. Endocrinol. 89, 700–711. doi: 10.1111/cen.13835
Mizock, L., and Lewis, T. K. (2008). Trauma in Transgender-Population: Risiko, Resilienz und klinische Versorgung. J. Emot. Abuse 8, 33 5–354.
Motmans, J., De Boilley, I., and Debunne, S. (2010). Being transgender in Belgium: Mapping the social and legal situation of transgender people. Brussels: Instituut voor de gelijkheid van vouwen en mannen.
Nieder, T. O., and Strauß, B. (2015). Transgender health care in Germany: Participatory approaches and the development of a guidline. Internat. Rev. Psychiatry 27, 416–426. doi: 10.3109/09540261.2015.1074562
Nieder, T. O., and Strauß, B. (2019). S3-Leitlinie zur Diagnostik, Beratung und Behandlung im Kontext von Geschlechtsinkongruenz, Geschlechtsdysphorie und Trans-Gesundheit. Zeitschrift für Sexualforschung 32, 70–79. doi: 10.1055/a-0895-8176
Perez-Brumer, A., Hatzenbuehler, M. L., Oldenburg, C. E., and Bockting, W. (2015). Individual-and structural-level risk factors for suicide attempts among transgender adults. Behav. Med. 41, 164–171. doi: 10.1080/08964289.2015.1028322
Pyra, M., Casimiro, I., Rusie, L., Ross, N., Blum, C., Keglovitz Baker, K., et al. (2020). An Observational Study of Hypertension and Thromboembolism Among Transgender Patients Using Gender-Affirming Hormone Therapy. Transgender Health 5, 1–9. doi: 10.1089/trgh.2019.0061
Rauchfleisch, U., Fossard, J., Waser G., Wiesendanger, K., and Roth, W. (2002). Coming-out, ein lebenslanger Prozess. Gleich und doch anders. Psychotherapie und Beratung von Lesben, Schwulen, Bisexuellen und ihren Angehörigen. 38–52. Stuttgart: Klett-Cotta.
Reisner, S. L., Poteat, T., Keatley, J., Cabral, M., Mothopeng, T., Dunham, E., et al. (2016). Global health burden and needs of transgender populations: a review. Lancet 388, 412–436. doi: 10.1016/S0140-6736(16)00684-X
Roberts, T. K., and Fantz, C. R. (2014). Barriers to quality health care for the transgender population. Clin. Biochem. 47, 983–987. doi: 10.1016/j.clinbiochem.2014.02.009
Rolle, L., Ceruti, C., Timpano, M., Falcone, M., and Frea, B. (2015). Quality of life after sexual reassignment surgery in Management of Gender Dysphoria. New York, NY: Springer, 193–203. doi: 10.1007/)78-88-470-5696-1_23
Scandurra, C., Bochicchio, V., Amodeo, A. L., Esposito, C., Valerio, P., Maldonato, N. M., et al. (2018). Internalized Transphobia, Resilience, and Mental Health: Applying the Psychological Mediation Framework to Italian Transgender Individuals. Internat. J. Env. Res. Public H ealth 15:508. doi: 10.3390/ijerph15030508
Scherr, A., El-Mafaalani, A., and Yüksel, G. (2017). Handbuch Diskriminierung. New York, NY: Springer.
Scheim, A., Lyons, C., Ezouatchi, R., Liestman, B., Drame, F., Diouf, D., et al. (2019). Sexual behavior stigma and depression among transgender women and cisgender men who have sex with men in Côte d’Ivoire. Ann. Epidemiol. 33, 79–83. doi: 10.1016/j.annepidem.2019.03.002
Schneider, H. J., Schaaf, L., and Stalla, G. K. (2007). “Transsexualität,” in Medizinische Therapie 2007 | 2008 , ed. J. Schölmerich (Berlin: Springer).
Shansky, R. M. (2019). Are hormones a “female problem” for animal research? Science 364, 825–826. doi: 10.1126/science.aaw7570
Steinmetzer, J., and Groß, D. (2008). Der Umgang mit Transsexualität in der Europäischen Union unter besonderer Berücksichtigung von Belgien. Normal—anders—krank. ed. D. Groß (Aachen: Medizinisch Wissenschaftliche Verlagsgesellschaft). 153–169.
Turner, D., Jopt, K., Nider, T. O., and Briken, P. (2014). German medical students’ interest in and knowledge about human sexuality in 1972 and 2012. J. Sexual Med. 11, 1914–1926. doi: 10.1111/jsm.12595
Verbeek, M. J., Hommes, M. A., Stutterheim, S. E., Van Lankveld, J. J., and Bos, A. E. (2020). Experiences with stigmatization among transgender individuals after transition: A qualitative study in the Netherlands. Internat. J. Transgend. Health 21, 220–233. doi: 10.1080/26895269.2020.1750529
Vincent, B. (2018). Transgender health: A practitioner’s guide to binary and non-binary trans patient care. London: Jessica Kingsley Publishers.
Weyers, S., Garland, S., Cruickshank, M., Kyrgiou, M., and Arbyn, M. (2021). Cervical cancer prevention in transgender men: a review. BJOG 128, 822–826. doi: 10.1111/1471-0528.16503
Wiepjes, C. M., den Heijer, M., Bremmer, M. A., Nota, N. M., de Blok, C. J., Coumou, B. J., et al. (2020). Trends in suicide death risk in transgender people: results from the Amsterdam cohort of gender dysphoria study (1972–2017). Acta Psychiatrica Scandinavica 141, 486–491. doi: 10.1111/acps.13164
Yüksel, Ş, Aslantaş Ertekin, B., Öztürk, M., Bikmaz, P. S., and Oğlağu, Z. (2017). A Clinically Neglected Topic: Risk of Suicide in Transgender Individuals. Noro psikiyatri arsivi 54, 28–32. doi: 10.5152/npa.2016.10075
Keywords : transgender, transidentity, transsexualism, healthcare, internalized homonegativity, gender-affirmative healthcare
Citation: Guethlein N, Grahlow M, Lewis CA, Bork S, Habel U and Derntl B (2021) Healthcare for Trans*gender People in Germany: Gaps, Challenges, and Perspectives. Front. Neurosci. 15:718335. doi: 10.3389/fnins.2021.718335
Received: 31 May 2021; Accepted: 11 August 2021; Published: 07 September 2021.
Reviewed by:
Copyright © 2021 Guethlein, Grahlow, Lewis, Bork, Habel and Derntl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nora Guethlein, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- For Journalists
- News Releases
- Latest Releases
- News Release
Age restriction lifted for gender-affirming surgery in new international guidelines
'Will result in the need for parental consent before doctors would likely perform surgeries'
Media Information
- Release Date: September 16, 2022
Media Contacts
Kristin Samuelson
- (847) 491-4888
- Email Kristin
- Expert can speak to transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage, how the U.S. gender regulations compare to other countries, more
CHICAGO --- The World Professional Association for Transgender Health (WPATH) today today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
Alithia Zamantakis (she/her), a member of the Institute of Sexual & Gender Minority Health at Northwestern University Feinberg School of Medicine, is available to speak to media about the new guidelines. Contact Kristin Samuelson at [email protected] to schedule an interview.
“Lifting the age restriction will greatly increase access to care for transgender adolescents, but will also result in the need for parental consent for surgeries before doctors would likely perform them,” said Zamantakis, a postdoctoral fellow at Northwestern, who has researched trans youth and resilience. “Additionally, changes in age restriction are not likely to change much in practice in states like Alabama, Arkansas, Texas and Arizona, where gender-affirming care for youth is currently banned.”
Zamantakis also can speak about transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage and how U.S. gender regulations compare to other countries.
Guidelines are thorough but WPATH ‘still has work to do’
“The systematic reviews conducted as part of the development of the standards of care are fantastic syntheses of the literature on gender-affirming care that should inform doctors' work,” Zamantakis said. “They are used by numerous providers and insurance companies to determine who gets access to care and who does not.
“However, WPATH still has work to do to ensure its standards of care are representative of the needs and experiences of all non-cisgender people and that the standards of care are used to ensure that individuals receive adequate care rather than to gatekeep who gets access to care. WPATH largely has been run by white and/or cisgender individuals. It has only had three transgender presidents thus far, with Marci Bower soon to be the second trans woman president.
“Future iterations of the standards of care must include more stakeholders per committee, greater representation of transgender experts and stakeholders of color, and greater representation of experts and stakeholders outside the U.S.”
Transgender individuals’ right to bodily autonomy
“WPATH does not recommend prior hormone replacement therapy or ‘presenting’ as one's gender for a certain period of time for surgery for nonbinary people, yet it still does for transgender women and men,” Zamantakis said. “The reality is that neither should be requirements for accessing care for people of any gender.
“The recommendation of requiring documentation of persistent gender incongruence is meant to prevent regret. However, it's important to ask who ultimately has the authority to determine whether individuals have the right to make decisions about their bodily autonomy that they may or may not regret? Cisgender women undergo breast augmentation regularly, which is not an entirely reversible procedure, yet they are not required to have proof of documented incongruence. It is assumed that if they regret the surgery, they will learn to cope with the regret or will have an additional surgery. Transgender individuals also deserve the right to bodily autonomy and ultimately to regret the decisions they make if they later do not align with how they experience themselves.”
A Teen Gender-Care Debate Is Spreading Across Europe
Doubts have now come to the Netherlands, where the most-contested interventions for children and adolescents were developed.
As Republicans across the U.S. intensify their efforts to legislate against transgender rights, they are finding aid and comfort in an unlikely place: Western Europe, where governments and medical authorities in at least five countries that once led the way on gender-affirming treatments for children and adolescents are now reversing course, arguing that the science undergirding these treatments is unproven, and their benefits unclear.
The about-face by these countries concerns the so-called Dutch protocol, which has for at least a decade been viewed by many clinicians as the gold-standard approach to care for children and teenagers with gender dysphoria. Kids on the protocol are given medical and mental-health assessments; some go on to take medicines that block their natural puberty and, when they’re older, receive cross-sex hormones and eventually surgery. But in Finland, Sweden, France, Norway, and the U.K., scientists and public-health officials are warning that, for some young people, these interventions may do more harm than good.
European health authorities are not reversing themselves on broader issues of trans rights, particularly for adults. But this turn against the Dutch protocol has inflamed activists and politicians in the United States. Republicans who have worked to ban its recommended treatments claim that the shifts in Europe prove they’re right. Their opponents argue that any doubts at all about the protocol, raised in any country whatsoever, are simply out of step with settled science: They point to broad endorsements by the American Medical Association, the American Psychiatric Association, and the American Academy of Pediatrics, among other groups; and they assert that when it comes to the lifesaving nature of gender-affirming care, “ doctors agree .”
But doctors do not agree, particularly in Europe, where no treatments have been banned but a genuine debate is unfurling in this field. In Finland, for example, new treatment guidelines put out in 2020 advised against the use of puberty-blocking drugs and other medical interventions as a first line of care for teens with adolescent-onset dysphoria . Sweden’s National Board of Health and Welfare followed suit in 2022, announcing that such treatments should be given only under exceptional circumstances or in a research context. Shortly after that, the National Academy of Medicine in France recommended la plus grande réserve in the use of puberty blockers. Just last month, a national investigatory board in Norway expressed concerns about the treatment. And the U.K.’s only national gender clinic for children, the Tavistock, has been ordered to close its doors after a government-commissioned report found, among other problems, that its Dutch-protocol-based approach to treatment lacked sufficient evidence.
These changes in Europe have so far been fairly localized: Health authorities in many countries on the continent—among them Austria, Denmark, Germany, Italy, and Spain—have neither subjected the Dutch approach to formal scrutiny nor advised against its use. Yet questions about the protocol seem to be spreading. At the end of March, for example, a Belgian TV report described a 42-fold increase in patients at a leading gender clinic in Ghent and raised questions about the right approach to care. Doubts about the protocol have even come to the country that invented it, at the Center of Expertise on Gender Dysphoria in Amsterdam. “Until I began noticing the developments in other EU countries and started reading the scientific literature myself, I too thought that the Dutch gender care was very careful and evidence-based,” Jilles Smids, a postdoctoral researcher in medical ethics at Erasmus University in the Netherlands, told me via email. “But now I don’t think that any more.”
Kirsten Visser, a Netherlands-based advocate and consultant for parents of trans teens, says her own son, Sietse, started receiving “definitely lifesaving” care at the Amsterdam center in 2012, at the age of 11. Around the time that Sietse showed up at the clinic, the Dutch protocol was becoming established internationally, largely through the work of a child and adolescent psychiatrist there named Annelou de Vries.
After completing a Ph.D. on gender dysphoria in Dutch adolescents, de Vries published two seminal papers with the clinical psychologist Peggy Cohen-Kettenis and other colleagues, in 2011 and 2014. The former looked at the psychological effects of puberty suppression on 70 young people over a period of two years, on average; the latter tracked outcomes for 55 of those people who had gone on to receive gender-reassignment surgery, over an average of six years. Taken together, the studies found that the teens showed fewer symptoms of depression after having their puberty suppressed, as well as a decrease in behavioral and emotional problems; and that the ones who went on to take gender-affirming hormones and have surgery grew into “well-functioning young adults.” De Vries’s expertise has since been widely recognized within the field: She served as a co-lead on the revision of the adolescent section of care guidelines recently published by the World Professional Association for Transgender Health, and is now president-elect of the European equivalent, EPATH.
But in the years after her two studies were released, research done in other European countries led to concerns about their relevance. In 2015, for example, Finnish researchers described a phenomenon that “ called for clinical attention ,” as they put it: More children were reporting gender dysphoria, and a greater proportion of them had been assigned female at birth. The fact that three-quarters of those Finnish teens had been diagnosed with separate and severe psychiatric conditions appeared to be at odds with the data from the Netherlands, the paper argued. The Dutch studies had found that just one-third of adolescents with gender dysphoria experienced other psychiatric issues, suggesting they were in far better mental health.
In Sweden, too, clinicians grew alarmed by the sudden increase in the number of teenagers seeking gender care. Mikael Landén, a professor of psychiatry at the University of Gothenburg, told me that this population has increased 17-fold since 2010. One explanation for that change—that more open-minded attitudes around gender have emboldened kids to seek the help they need—just doesn’t ring true to him. He’d studied those views in his early work, he said, and found that, on the whole, Swedish attitudes toward transgender people have been very positive for a long time.
When the government asked Landén and a group of other scientists to write an evidence-based review of hormone-based treatments for young people, their verdict, after two years of study, was expressed definitively: The original research findings from de Vries were outdated, and do not necessarily apply to the group of teens who have been coming forward in more recent years. The Dutch protocol had been “a valuable contribution,” he told me, and “it was reasonable to start using it” in Sweden. But times had changed, and so had the research literature. In 2021, for instance, a team based at the U.K.’s Tavistock clinic published research showing no detectable improvements in the mental health of youngsters who had been put on puberty blockers and followed for up to three years.
Read: The war on trans kids is totally unconstitutional
De Vries acknowledged some concerns about the research when we spoke in February. “Our early outcomes studies were really from another time and comprised small samples,” she told me, and they looked only at trans youth who had experienced gender dysphoria from childhood. She granted that there is some research to suggest that kids who don’t arrive at the clinic until they’re older are worse off, psychologically, than their younger peers; but she also said her team has run studies including 16-year-olds, and that their findings were “not worrisome.” She agrees that other researchers have not replicated the long-term follow-up research on kids who went through the Dutch protocol, but she pointed out that the short-term benefits of such treatment have indeed been seen in other studies. Research conducted in the U.S., and published earlier this year, found that a group of 315 trans and nonbinary youth were on average less depressed and anxious , and better-functioning, after two years of hormonal treatment.
In the meantime, de Vries and her colleagues have urged clinicians in other countries to do more of their own investigation, in part because the youngsters who receive care at gender clinics in the Netherlands seem to be in comparatively good mental health from the get-go. It’s not yet clear, she told me, that studies of this group will be applicable to youth in other countries. “Every doctor or psychologist who is involved in transgender care should feel the obligation to do a good pre- and post-test,” one of de Vries’s co-authors on the 2011 and 2014 studies said to a Dutch newspaper in 2021. “The rest of the world is blindly adopting our research.”
De Vries is now working on a research project, funded by an $864,000 grant, that will try to answer newly forming doubts about the Dutch protocol. Her proposal for the grant, filed in 2021, described its subject as a “once so welcomed but now sharp[ly] criticized approach.”
That such criticisms are becoming mainstream even in her own country is itself a startling development. After all, the Netherlands has long been at the vanguard of progressive health-care practices. When the Dutch approach to transgender care for adults first started taking shape during the 1970s (many years before the protocol for kids would be established), the country’s politics were dominated by a steadfast opposition to taboos. James Kennedy, an American-born professor of modern Dutch history at Utrecht University, has described this as the country’s “compassionate culture”: In a radical departure from its traditional Christian conservatism, long-standing policies were being spurned; and even touchy subjects such as death and sex were made the subject of broad public-policy debates. Sex work, for example, was widely tolerated , then legalized in 2000. Similarly, the Royal Dutch Medical Association offered formal guidelines for the practice of euthanasia in the 1980s, and a corresponding national law—one of the world’s first—codified the rules in 2002.
Against this backdrop of openness, in which doctors were seen as authoritative figures who were well equipped to decide what was best for their patients, one of the first dedicated clinics for transgender people was established in Amsterdam in 1972. It offered an array of services—blood tests, hormone therapy, and surgeries—to trans adults. According to a recent book by the historian Alex Bakker, Dutch surgeons, some of them inspired by their Christian beliefs, developed techniques that would reduce patients’ psychological suffering. “Helping those in need trumped ‘taboos’ about the sanctity of life or fixed gender roles,” Kennedy told me. The Dutch protocol for treating gender dysphoria in children, as established in the 1990s, reflected a further extension of this philosophy, aiming to smooth adult transitions by intervening early.
Read: Take detransitioners seriously
Nevertheless, in December, a journalist named Jan Kuitenbrouwer and a sociologist named Peter Vasterman published an opinion piece in a leading daily newspaper, NRC , that took aim at the Dutch protocol and its “shaky” scientific foundations, and alluded to the international scrutiny of the past few years. “It is remarkable that the media in our neighboring countries report extensively on this reconsideration,” the article said, “but the Dutch hardly ever do.” Like critics elsewhere, Kuitenbrouwer and Vasterman pointed to the rising numbers of children seeking care, from 60 to 1,600 in the Netherlands across a dozen years, and the unaccounted rise in those assigned female at birth; and they suggested that this new generation of people seeking treatment is not analogous to those included in the studies conducted by de Vries a decade ago. De Vries and some colleagues countered that their more recent research addresses this concern. “Scientific evaluation has always been an integral part of this challenging model of care, where young people make early decisions about medical interventions with lifelong implications,” they wrote in the same newspaper.
Also in December, a clinical psychologist at Radboud University’s gender clinic in Nijmegen named Chris Verhaak told a different Dutch outlet that puberty blockers affect children’s bones, and maybe also their brain development. “It is not nothing,” she said. Verhaak is currently running a government-funded study to understand the source and nature of the increase in the number of patients. (Results are due to be presented to the Dutch House of Representatives this year.) In another interview that month, she said that for up to half of cases, the gains in suppressing puberty are not clear. “I worry about that,” she told the newsweekly De Groene Amsterdammer . “Especially because we also experience enormous pressure to provide these puberty inhibitors as quickly as possible.”
Verhaak’s comments in particular sparked dismay among trans groups, which saw them as promoting destructive narratives about social contagion. Verhaak and her direct collaborators say that they are no longer speaking to the media until their study is released, but Hedi Claahsen, a professor and principal clinician on the Radboud center’s gender team, told me that practitioners are cautious and follow national guidelines. When I asked if her center’s approach differed from the one used in Amsterdam, she told me, “No clinic is exactly the same.” Individual providers, who are working at different institutions, may end up providing care that reflects “a different vision.”
Another, more significant round of criticism arrived at the end of February, when another widely read Dutch newspaper, de Volkskrant , published a 5,000-word article under a headline reading: “The treatment of transgender youth in the Netherlands was praised. Now the criticism of ‘the Dutch approach’ is growing.” The authors spoke with Iris, a 22-year-old woman who spent five years on testosterone and had a double mastectomy that she now regrets; they pointed to a new population of kids assigned female at birth seeking care only in their teens; and they noted reservations about the protocol in Finland and Sweden. “Is the ‘Dutch approach’ still the way to go?” the story asked.
The article prompted debate on Twitter, where Michiel Verkoulen, a health economist working with the government of the Netherlands to address the long-standing problem of ever-expanding waiting lists and their impact on young people’s mental health, accused the Dutch protocol’s critics of ignoring what he described as the elephant in the room. “What to do with the people for whom transgender care is critical?” he asked. “You can put every research aside, keep asking for more, and argue that diagnostics and treatments should be stricter … But the question remains: W hat then ?”
“In the Netherlands there are more and more people saying that gender diversity is woke and it’s nonsense and it’s bullshit,” Visser, the consultant for parents of trans teens, told me. Sam van den Berg, a spokesperson for an Utrecht-based trans-rights organization called Transvisie, argued that this debate does not need to happen. The quality of care for children with gender dysphoria is better in the Netherlands than almost anywhere else, she said. “We don’t feel it’s necessary to change anything.” Indeed, doctors in the Netherlands are still free to provide gender-affirming care as they see fit. The same is true of their colleagues in Finland, Sweden, France, Norway, and the U.K., where new official guidelines and recommendations are not binding. No legal prohibitions have been put in place in Europe, as they have been in more than a dozen U.S. states, where physicians risk losing their medical license or facing criminal sanctions for prescribing certain forms of gender-affirming care.
But the trend toward more conservative application of the Dutch protocol is likely to have real effects in European countries, in terms of which kids get treatment, and of what kind. Louise Frisén, an associate professor at Karolinska Institute and a pediatric psychiatrist at the child and adolescent mental-health clinic in Stockholm, Sweden, told me she worries that under her country’s new guidelines, many of her teenage patients will find it harder to access medical care. The benefits of treatment are clear, she said, and she further claimed that the policy change has caused anguish for some patients who are panicking at the looming prospect of puberty.
As for de Vries, when I spoke with her a few weeks before the article in de Volkskrant was published, she agreed that clinicians should be cautious, but not to the point where treatment becomes inaccessible. Outcomes for those with later-onset dysphoria do need to be investigated further, she acknowledged, but “if we are going to wait ’til the highest-standard medical evidence provides us the answers, we will have to stop altogether.” In that sense, Europe’s brewing disagreement over treatment could turn into paralysis. “That’s what worries me,” she said. “You will always have to work with uncertainties in this field.”
About the Author
More Stories
A Mysterious Syndrome Can Strike Decades After Polio

IMAGES
VIDEO
COMMENTS
Dr. Juergen Schaff. Dr. Schaff has performed MTF surgery for over 15 years and has worked with over 200 FTM clients. He is a member of the following Professional Organizations: Dr. Schaff performs the following SRS procedures: For a consultation, call the number listed above.
Dr. Schaff offers gender reassignment surgery in Germany, both MTF and FTM procedures, including the fibula flap phalloplasty.
Meoclinic Berlin. Transgender Surgery at the MEOCLINIC in Berlin-Mitte. Our medical expert team in Berlin-Mitte is available for short-notice appointments. A sex reassignment surgery is a big step for you as a patient. We will be happy to assist you in this process and help you fulfill your wish. A sex reassignment procedure is always preceded ...
Opinion. Late one night on the cusp of the 20th century, Magnus Hirschfeld, a young doctor, found a soldier on the doorstep of his practice in Germany. Distraught and agitated, the man had come to ...
Transgender surgery at Klinik Sanssouci. Surgical gender reassignment procedures have been performed at Klinik Sanssouci for over 20 years. While many clinics perform these gender reassignments in several individual surgeries, we prefer that the respective steps required for gender reassignment are combined in a single surgery ("All in One").
The IM GENDER Gender Unit opened its doors over twenty years ago and has become an international benchmark in Gender Reassignment Surgery. IM GENDER has cared for more than 3,000 trans people who have decided to carry out some treatment or surgical procedure at the Unit, whether genital affirmation surgery - vaginoplasty, phalloplasty, metoidioplasty -, body surgery - mastectomy, breast ...
In Germany, the diagnosis of the transgender characteristic is geared to the International Statistical Classification of Diseases and associated health problems (ICD - transsexualism according to ICD F64.0) issued by the World Health Organisation (WHO). ... As a rule, paramount to sex reassignment surgery is the removal of the protruding ...
Germany stands out as a prominent European destination for gender reassignment surgery. The country boasts cutting-edge technology, rigorous medical standards, and an array of experienced surgeons. Berlin, in particular, is recognized for its excellence in GRS procedures, drawing patients from around the world.
The Evolution and Current Healthcare for Trans ∗ gender in Germany. Trans ∗ gender healthcare in Germany has a centennial history already. In 1922, the German sexologist Magnus Hirschfeld, founder of the first Institute for Sexology, carried out the worldwide first sex reassignment surgery in Berlin (Bhinder and Upadhyaya, 2021).In the post-war German society, the situation of trans ∗ ...
For persons with gender dysphoria, treatment with cross-sex hormones delivers a sense of identity. However, since gender-affirming hormone therapy has a significant effect on a person's hormonal ...
The United Kingdom is among several countries in Europe that are rethinking minors' access to gender-affirming care. Chase, a transgender teenager who identifies as non-binary, has been trying to ...
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
In Ireland and Malta, the age requirement for sex reassignment surgery is 16 years. Croatia allows children to have sex reassignment surgery before the age of 18 if they have parental consent, without laying down any specific minimum age requirement. 19 October 2018. Excel file: Minimum age requirements concerning children's rights in the EU ...
Results from studies imply that sex reassignment surgery on the one hand has positive effects in terms of partial aspects of quality of life, such as mental health, sexuality, and life satisfaction, and, on the other hand, on quality of life overall. Because of the studies' high dropout rates (12-77%; median 56%), the results should be ...
Dora Rudolfine Richter [3] (16 April 1892 - 26 April 1966) was a German trans woman and the first known person to undergo complete male-to-female gender-affirming surgery. [4] She was one of a number of transgender people in the care of sex-research pioneer Magnus Hirschfeld at Berlin's Institute for Sexual Research during the 1920s and early 1930s. She underwent surgical removal of the ...
Transgender rights in the Federal Republic of Germany are regulated by the Transsexuellengesetz ("Transsexual law") [1] since 1980, and indirectly affected by other laws like the Abstammungsrecht ("Law of Descent"). [2] The law initially required transgender people to undergo sex-reassignment surgery in order to have key identity documents changed.
Research conducted to date has shown that gender reassignment surgery has a positive effect on subjective wellbeing and sexual function (2, 6, 7). The surgical ... Garrels found a gradual decrease in the difference between the two figures in Germany, with the ratio decreasing from 3.5:1 (in the 1950s and 60s) to 1.2:1 (1995 to 1998) (Table ...
Karl M. Baer, who underwent a female-to-male sex-change operation in Germany in 1906. Credit: 'Memoirs of a Man's Maiden Years' Ofer Aderet. Dec 5, 2015. ... before Baer, but he was the first who underwent surgery. "He was unusual in that he used medical technology and surgical means to change his gender," she says.
The Evolution and Current Healthcare for Trans ∗ gender in Germany. Trans ∗ gender healthcare in Germany has a centennial history already. In 1922, the German sexologist Magnus Hirschfeld, founder of the first Institute for Sexology, carried out the worldwide first sex reassignment surgery in Berlin (Bhinder and Upadhyaya, 2021).
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
The World Professional Association for Transgender Health (WPATH) today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
April 28, 2023. As Republicans across the U.S. intensify their efforts to legislate against transgender rights, they are finding aid and comfort in an unlikely place: Western Europe, where ...