Information
- Author Services

Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Journal Proposal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Fat-soluble vitamins a, d, e, and k: review of the literature and points of interest for the clinician.

1. Introduction
2. materials and methods, 3. metabolism of fat-soluble vitamins, 4. functions of fat-soluble vitamins, 5. epidemiological data on fat-soluble vitamin deficiencies, 6. clinical manifestations of fat-soluble vitamin deficiencies, 6.1. vitamin a deficiency, 6.2. vitamin d deficiency.
- Cancer, especially colorectal and breast cancer, but also prostate and lung cancer;
- Myelodysplastic syndromes;
- Arterial hypertension, with an increased risk of cardiovascular events;
- Autoimmune pathologies such as multiple sclerosis, rheumatoid arthritis, systemic lupus erythematosus, and Type 1 diabetes in children;
- Osteoarthritis;
- Schizophrenia and depression [ 10 , 11 ].
6.3. Vitamin E Deficiency
6.4. vitamin k deficiency, 6.5. multiple fat-soluble vitamin deficiencies, 7. etiologies of fat-soluble vitamin deficiencies, 7.1. dietary deficiencies, 7.2. digestive tract disorders and malabsorption, 7.3. liver diseases, 7.4. other common conditions and disorders, 7.5. etiologies of specific fat-soluble vitamin deficiencies, 8. diagnosis of fat-soluble vitamin deficiencies, 9. treatment of fat-soluble vitamin deficiencies, 10. conclusions, author contributions, conflicts of interest.
- Sauvant, P.; Azaïs-Braesco, V. Vitamines liposolubles. In Traité de Nutrition Clinique de L’adulte ; Basdevant, A., Laville, M., Lerebours, E., Eds.; Médecine-Sciences Flammarion: Paris, France, 2001; pp. 183–193. [ Google Scholar ]
- Uribe, N.G.; García-Galbis, M.R.; Espinosa, R.M.M. New Advances about the Effect of Vitamins on Human Health: Vitamins Supplements and Nutritional Aspects. In Functional Food—Improve Health through Adequate Food ; InTech: London, UK, 2017. [ Google Scholar ] [ CrossRef ]
- Youness, R.A.; Dawoud, A.; El Tahtawy, O.; Farag, M.A. Fat-soluble vitamins: Updated review of their role and orchestration in human nutrition throughout life cycle with sex differences. Nutr. Metab. 2022 , 19 , 60. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Russell, R.M. Vitamin and Trace Mineral Deficiency and Excess. In Harrison’s Principles of Internal Medicine , 16th ed.; Kasper, D.L., Braunwald, E., Fauci, A.S., Hauser, S.L., Longo, D.L., Jameson, J.L., Isselbacher, K.J., Eds.; The McGraw-Hill Companies: New York, NY, USA, 2005; pp. 403–411. [ Google Scholar ]
- Hodge, C.; Taylor, C. Vitamin A Deficiency. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK567744/ (accessed on 2 January 2023).
- Sizar, O.; Khare, S.; Goyal, A.; Givler, A. Vitamin D Deficiency. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532266/ (accessed on 17 July 2023).
- Kemnic, T.R.; Coleman, M. Vitamin E Deficiency. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519051/ (accessed on 4 July 2023).
- Eden, R.E.; Daley, S.F.; Coviello, J.M. Vitamin K Deficiency. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK536983/ (accessed on 8 September 2023).
- Reddy, P.; Jialal, I. Biochemistry, Fat Soluble Vitamins. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534869/ (accessed on 19 September 2022).
- Barker, T. Vitamins and Human Health: Systematic Reviews and Original Research. Nutrients 2023 , 15 , 2888. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, F.F.; Barr, S.I.; McNulty, H.; Li, D.; Blumberg, J.B. Health effects of vitamin and mineral supplements. BMJ 2020 , 369 , m2511. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ruggiero, C.; Tafaro, L.; Cianferotti, L.; Tramontana, F.; Macchione, I.G.; Caffarelli, C.; Virdis, A.; Ferracci, M.; Rinonapoli, G.; Mecocci, P.; et al. Targeting the Hallmarks of Aging with Vitamin D: Starting to Decode the Myth. Nutrients 2024 , 16 , 906. [ Google Scholar ] [ CrossRef ]
- Song, P.; Adeloye, D.; Li, S.; Zhao, D.; Pan, Q.; Qiu, Y.; Zhang, R.; Rudan, I.; Global Health Epidemiology Research Group (GHERG). The prevalence of vitamin A deficiency and its public health significance in children in low- and middle-income countries: A systematic review and modelling analysis. J. Glob. Health 2023 , 13 , 04084. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cui, A.; Zhang, T.; Xiao, P.; Fan, Z.; Wang, H.; Zhuang, Y. Global and regional prevalence of vitamin D deficiency in population-based studies from 2000 to 2022: A pooled analysis of 7.9 million participants. Front. Nutr. 2023 , 10 , 2023. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Terrier, B.; Resche-Rigon, M.; Andrès, E.; Bonnet, F.; Hachulla, E.; Marie, I.; Rosenthal, E.; Cacoub, P.; on behalf of the Groupe de Recherche sur les Anémies en Médecine Interne (GRAMI). Prevalence, characteristics and prognostic significance of anemia in daily practice: Results from a French nationwide cross-sectional and prospective longitudinal study. QJM 2012 , 105 , 345–354. [ Google Scholar ] [ CrossRef ]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007 , 357 , 266–281. [ Google Scholar ] [ CrossRef ]
- Fain, O. Carences en vitamine C. Rev. Med. Interne 2004 , 25 , 872–880. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- WHO. Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. Genève, Switzerland, 28 January–1 February 2002. Available online: https://www.who.int/publications-detail-redirect/924120916X (accessed on 23 May 2024).
- Andrès, E.; Serraj, K.; Fédérici, L.; Schlienger, J.L. Carences et excès en vitamine. In Diagnostics Difficiles en Médecine Interne ; Rousset, H., Vital-Durand, D., Dupond, J.L., Pavic, M., Eds.; Eds Maloine: Paris, France, 2008; pp. 951–965. [ Google Scholar ]
- Delarue, J. Carences et excès en micronutriments. In Traité de Nutrition Clinique de L’adulte ; Basdevant, A., Laville, M., Lerebours, E., Eds.; Médecine-Sciences Flammarion: Paris, France, 2001; pp. 534–550. [ Google Scholar ]
- Bertoldo, F.; Cianferotti, L.; Di Monaco, M.; Falchetti, A.; Fassio, A.; Gatti, D.; Gennari, L.; Giannini, S.; Girasole, G.; Gonnelli, S.; et al. Definition, Assessment, and Management of Vitamin D Inadequacy: Suggestions, Recommendations, and Warnings from the Italian Society for Osteoporosis, Mineral Metabolism and Bone Diseases (SIOMMMS). Nutrients 2022 , 14 , 4148. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Andrès, E.; Serraj, K.; Mecili, M.; Ciobanu, E.; Fothergill, H. Excès vitaminiques et hypervitaminoses. Médecine Thérapeutique 2010 , 16 , 21–24. [ Google Scholar ]
| Vitamins | Food Sources | Recommended Dietary Allowance | Toxic Dose | Physiological Functions |
|---|---|---|---|---|
| A | Fish oil, liver, butter, egg yolks, carrots, sweet potatoes, and spinach | 600–950 RE/day (1 μg of retinol = 3.3 IU = 6 μg of beta-carotene) | 3000 RE/day | Vision, immunity, and growth |
| D | Cod liver oil, egg yolks, fatty fish (salmon, mackerel, sardines), eggs, liver, and mushrooms | 5–10 IU/day | 1000 IU/day | Calcium homeostasis, immunity, and genomic regulation |
| E | Green vegetables, wheat germ, vegetable oils (wheat germ oil, sunflower oil), nuts and seeds (almonds, sunflower seeds), avocado, and spinach | 12 mg/day | – | Antioxidant action |
| K | Green leafy vegetables (kale, spinach, broccoli), cruciferous vegetables (cauliflower, Brussels sprouts), liver, egg yolks, soybean oil, meat, and dairy products | 0.1–1 μg/Kg/day | – | Hemostasis and bone metabolism |
| Fat-Liposoluble Vitamin Deficiencies | Typical and Frequent Clinical Manifestations |
|---|---|
| Vitamin A | Reduced night vision (night blindness, even blindness), keratomalacia, susceptibility to infection (due to impaired immunity), dry skin, hyperkeratotic papular lesions, and diarrhea (characteristic combination: ophthalmopathy and immune disorders or rickets) |
| Vitamin D | Mechanical bone pain and fractures, Looser–Milkmann striae, osteomalacia, rickets, muscular weakness, and susceptibility to falls |
| Vitamin E | Neuropathy and impaired night vision, leading to dementia and ophthalmoplegia |
| Vitamin K | Spontaneous hemorrhagic syndrome or following minor trauma, osteopenia, and muscle weakness (characteristic combination: hemorrhagic syndrome and osteopenia) |
| Fat-Soluble Vitamin Deficiency | Curative Treatment |
|---|---|
| A | 100,000 IU/day for 3 days, then 50,000 IU/day for 2 weeks |
| D | cholecalciferol 3000–10,000 IU/day (average 5000 IU/day) for 1–2 months, or cholecalciferol in a single dose of 60,000 to 150,000 IU, followed by the maintenance dose (2000 IU/day) |
| E | 50–2000 IU/day |
| K | Treatment is limited to neonates and anti-vitamin K overdoses |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Andrès, E.; Lorenzo-Villalba, N.; Terrade, J.-E.; Méndez-Bailon, M. Fat-Soluble Vitamins A, D, E, and K: Review of the Literature and Points of Interest for the Clinician. J. Clin. Med. 2024 , 13 , 3641. https://doi.org/10.3390/jcm13133641
Andrès E, Lorenzo-Villalba N, Terrade J-E, Méndez-Bailon M. Fat-Soluble Vitamins A, D, E, and K: Review of the Literature and Points of Interest for the Clinician. Journal of Clinical Medicine . 2024; 13(13):3641. https://doi.org/10.3390/jcm13133641
Andrès, Emmanuel, Noel Lorenzo-Villalba, Jean-Edouard Terrade, and Manuel Méndez-Bailon. 2024. "Fat-Soluble Vitamins A, D, E, and K: Review of the Literature and Points of Interest for the Clinician" Journal of Clinical Medicine 13, no. 13: 3641. https://doi.org/10.3390/jcm13133641
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 23 November 2021
The health effects of vitamin D supplementation: evidence from human studies
- Roger Bouillon ORCID: orcid.org/0000-0002-6446-3763 1 ,
- Despoina Manousaki 2 ,
- Cliff Rosen ORCID: orcid.org/0000-0003-3436-8199 3 ,
- Katerina Trajanoska 4 ,
- Fernando Rivadeneira ORCID: orcid.org/0000-0001-9435-9441 5 &
- J. Brent Richards 6 , 7
Nature Reviews Endocrinology volume 18 , pages 96–110 ( 2022 ) Cite this article
131k Accesses
235 Citations
391 Altmetric
Metrics details
- Endocrine system
- Endocrine system and metabolic diseases
Vitamin D supplementation can prevent and cure nutritional rickets in infants and children. Preclinical and observational data suggest that the vitamin D endocrine system has a wide spectrum of skeletal and extra-skeletal activities. There is consensus that severe vitamin D deficiency (serum 25-hydroxyvitamin D (25OHD) concentration <30 nmol/l) should be corrected, whereas most guidelines recommend serum 25OHD concentrations of >50 nmol/l for optimal bone health in older adults. However, the causal link between vitamin D and many extra-skeletal outcomes remains unclear. The VITAL, ViDA and D2d randomized clinical trials (combined number of participants >30,000) indicated that vitamin D supplementation of vitamin D-replete adults (baseline serum 25OHD >50 nmol/l) does not prevent cancer, cardiovascular events, falls or progression to type 2 diabetes mellitus. Post hoc analysis has suggested some extra-skeletal benefits for individuals with vitamin D deficiency. Over 60 Mendelian randomization studies, designed to minimize bias from confounding, have evaluated the consequences of lifelong genetically lowered serum 25OHD concentrations on various outcomes and most studies have found null effects. Four Mendelian randomization studies found an increased risk of multiple sclerosis in individuals with genetically lowered serum 25OHD concentrations. In conclusion, supplementation of vitamin D-replete individuals does not provide demonstrable health benefits. This conclusion does not contradict older guidelines that severe vitamin D deficiency should be prevented or corrected.
Vitamin D and calcium supplementation can cure nutritional rickets and can modestly decrease the risk of major fractures in older adults with poor vitamin D status or calcium intake.
Large supplementation trials recruiting vitamin D-replete adults (serum 25OHD concentration >50 nmol/l) have demonstrated no effects on the incidence of cancer, cardiovascular events or type 2 diabetes mellitus (T2DM) and no benefits in terms of bone density and the risk of falls.
Post-hoc analysis of large supplementation trials has suggested that supplementation of individuals with vitamin D deficiency modestly delays age-related bone loss and progression to T2DM, and improves lung function.
A meta-analysis suggested that vitamin D supplementation results in a modest decrease in cancer mortality.
Over 60 Mendelian randomization studies have examined causal links between genetically lower vitamin D levels and health outcomes; most studies generated null effects except four studies that demonstrated an increased risk of multiple sclerosis.
In conclusion, supplementation of vitamin D-replete individuals does not generate overall health benefits; however, correction of severe vitamin D deficiency remains essential.
Similar content being viewed by others

Vitamin D deficiency 2.0: an update on the current status worldwide
Absence of causal association between Vitamin D and bone mineral density across the lifespan: a Mendelian randomization study
Targeted 25-hydroxyvitamin d concentration measurements and vitamin d 3 supplementation can have important patient and public health benefits, introduction.
There is consensus that daily intake of 400 IU of vitamin D can prevent nutritional rickets in infants and children 1 . However, the skeletal effects of vitamin D deficiency in adults and older adults (aged >65 years), and the potential extra-skeletal effects of vitamin D are more controversial. Some people consider that vitamin D supplementation is futile 2 . By contrast, others have suggested that the vitamin D intake requirement is much higher than currently achieved by the general population and that people should aim to achieve 25-hydroxyvitamin D (25OHD, the major marker of vitamin D status) concentrations similar to those found in certain tribes in equatorial Africa with a sun exposure lifestyle that might be similar to that of early humans 3 , 4 , 5 , 6 , 7 .
The potential extra-skeletal effects of the vitamin D endocrine system (which refers to vitamin D in its active form, its precursors and metabolites, and vitamin D receptor) are based on several arguments. For example, the vitamin D receptor (VDR) and CYP27B1 (the enzyme primarily responsible for producing the active form of vitamin D, 1,25-dihydroxyvitamin D or 1,25(OH) 2 D 3 ) are widely expressed, including in tissues that are not involved in calcium or phosphate transport (Fig. 1 ). In addition, ~3% of the human and mouse genomes are under the direct or indirect control of 1,25(OH) 2 D 3 (refs 8 , 9 ). Finally, many diseases and illnesses in humans are associated with a poor vitamin D status, as measured by low serum levels of 25OHD. Therefore, one of the major clinical questions in the field is whether poor vitamin D status plays a causal role in the diseases and conditions associated with low 25OHD levels, such as cancer, impaired muscle strength and falls, and immune, metabolic or cardiovascular diseases. Furthermore, if the link is causal, the threshold serum level of 25OHD below which the risk of these diseases is increased must be identified 8 .

The potential skeletal and extra-skeletal target tissues and effects of the vitamin D endocrine system (vitamin D and vitamin D receptor) as based on preclinical and observational studies, Mendelian randomization studies and randomized controlled trials (RCTs). In vitro studies have identified many molecular and genetic targets of vitamin D action. Animal models have confirmed a variety of skeletal and extra-skeletal actions. Human observational data are largely in line with preclinical data. However, Mendelian randomization studies and RCTs have not confirmed such a widespread action profile in vitamin D-replete adults. Therefore, the health consequences of poor vitamin D status remain controversial. The strength of the relationship between the vitamin D endocrine system and health effects are indicated by the arrow thickness. FGF23, fibroblast growth factor 23; PTH, parathyroid hormone.
Up to about a decade ago, there was tremendous uncertainty about vitamin D supplementation for the maintenance of adequate health levels. Large, randomized placebo-controlled trials with clinically important outcomes and/or surrogates had yet to be performed and only a few meta-analyses of randomized controlled trials (RCTs) were available. On the other hand, many observational studies had been conducted that were confounded by multiple variables. The Institute of Medicine (IOM) guidelines were developed to provide an answer based on the best available evidence at that time 10 . The IOM Committee established minimal dosing to maintain adequate serum levels of 25OHD in young and older individuals and established the tolerable upper limits of supplementation. The Committee also examined the totality of evidence relating vitamin D supplementation to numerous outcomes, and concluded that large randomized trials were needed to establish efficacy and safety. Other societies, such as the Endocrine Society 11 , and governmental organizations also generated a variety of guidelines 12 . The minimal serum level of 25OHD that was considered to provide vitamin D sufficiency varied from 30 nmol/l (UK Scientific Advisory Committee on Nutrition 13 ), to 50 nmol/l (IOM and many other governmental guidelines) 12 , 14 , 75 nmol/l (Endocrine Society and some other societies) 11 and even >100 nmol/l (refs 12 , 14 ). Of note, serum levels of >100 nmol/l are found in people living in Africa under conditions of sun exposure supposed to be similar to that of early humans.
In this Review, we summarize the results of recent (2017–2020) RCTs as well as Mendelian randomization studies, while not reviewing observational studies, which have been well-documented previously 9 . We have chosen these two study designs because they are both types of causal inference studies and can help provide insights into the role of vitamin D in the aetiology of common diseases. The reviewed studies do not provide evidence that vitamin D supplementation prevents negative health outcomes in vitamin D-replete adults. However, all these studies reveal new suggestions for potential effects of vitamin D supplementation. Note that throughout the text vitamin D refers to vitamin D 3 unless otherwise specified.
RCTs: 2017–2020
Many small-scale RCTs have been published over the past few years. In addition, several large studies have generated a wealth of new data (Table 1 ; Supplementary Box 1 ). The new major RCTs deal with more than 35,000 study participants who have a generally better health profile than participants in older studies. These studies used higher dosages than previous studies and the volunteers were mostly vitamin D-replete at baseline. These differences might explain why these large RCTs generated mostly null results in the intention-to-treat (ITT) analysis.
The largest trial to date is the VITAL study 15 that recruited more than 25,000 adults from 44 centres in the USA and evaluated daily doses (2,000 IU) of vitamin D for a mean duration of 5.3 years. The Vitamin D Assessment Study (ViDA study) 16 evaluated the effects of monthly high-dose vitamin D supplementation in more than 5,000 adults in New Zealand followed for a mean duration of 3.3 years. The primary aim of the D2d study of 2,423 US participants was to evaluate the effects of a daily dose of vitamin D (4,000 IU per day) for a mean duration of 2.5 years on the conversion of prediabetes to type 2 diabetes mellitus (T2DM) 17 . The DO-HEALTH study evaluated the effects of vitamin D (2,000 IU per day) in 2,157 older adults in Europe for a duration of 3 years 18 . The Calgary study was not really a megatrial, as it included only 311 Canadian adults and explored the effects on bone structure and quality and the safety of daily high-dose vitamin D (4,000 and 10,000 IU versus 400 IU) for 3 years 18 , 19 , 20 .
Mendelian randomization studies
Mendelian randomization is an established genetic epidemiological method, which can be used to test whether genetically decreased 25OHD levels are associated with increased risk of disease. To do this, Mendelian randomization uses single nucleotide polymorphisms (SNPs) that are associated with 25OHD levels in genome-wide association studies (GWAS) as instruments to infer 25OHD levels. Depending on their number, these SNPs can explain from 2% to 10% of the variance in 25OHD levels. This approach offers an alternative analytical technique able to reduce bias from confounding and reverse causation present in observational studies and re-estimates observations in a framework enabling causal inference (Supplementary Box 2 ). The very large number of Mendelian randomization studies of vitamin D have also generated mostly null results; however, they have been handicapped by the low power to predict decreased serum 25OHD concentrations.
Effects of vitamin D on health outcomes
Many observational studies suggest a link between low vitamin D status and T2DM 9 .
Evidence from RCTs
In the large D2d RCT of patients with prediabetes (Table 1 ), vitamin D supplementation only showed a non-significant trend to slow down the progression of prediabetes into T2DM. The study design intentionally included people with a high risk of progression to T2DM, who received vitamin D (4,000 IU per day). In the ITT analysis, the hazard ratio for the development of T2DM in the group receiving vitamin D was 0.88 (95% CI 0.75–1.04; P = 0.12) compared with the placebo group. In a post hoc analysis, however, a significant effect was observed in individuals with a baseline BMI below 30 mg/m 2 , severe vitamin D deficiency at baseline, perfect adherence to treatment during the study or serum 25OHD above 100 nmol/l throughout the study 21 (Tables 2 , 3 ). Analysis of the combined data from the D2d trial and two other trials specifically designed and conducted to investigate the effectiveness of vitamin D supplementation in preventing T2DM showed that vitamin D supplementation (when compared with placebo) reduced the risk of developing T2DM from 23% to 13% (a 10% reduction) in persons with prediabetes not selected for vitamin D deficiency 22 . This finding is in line with two meta analyses published in 2020 dealing with eight 23 and seven 24 RCTs in people with prediabetes. These meta-analyses concluded that vitamin D supplementation decreased the risk to progress to T2DM by about 10%, especially when using doses above 1,000 IU per day and in participants without obesity. Participant-level meta-analysis of these trials might provide a better estimate of risk reduction and identify populations of patients with prediabetes who are likely to benefit the most from vitamin D supplementation.
Evidence from Mendelian randomization
Since 2015, seven large Mendelian randomization studies have investigated the causal effect of genetically altered 25OHD levels on risk of T2DM and related traits (Supplementary Box 3 ). These Mendelian randomization studies included very large numbers of participants and mostly recruited white individuals and Chinese individuals. One study 25 generated conflicting results, as part of the study using only two SNPs concluded that high predicted serum levels of 25OHD protected against T2DM (OR 0.86 of T2DM for a 25 nmol/l higher 25OHD concentration than that seen in the general population). However, in a slightly larger group of the same study that included two additional SNPs, the odds ratio became insignificant (Supplementary Box 3 ). All the other Mendelian randomization studies, including more than 500,000 volunteers, did not find a significant odds ratio for the relationship between predicted 25OHD and risk of T2DM.
Vitamin D and T2DM — summary
Although observational data have consistently confirmed lower serum 25OHD concentrations in patients with T2DM or the metabolic syndrome 9 , most Mendelian randomization studies have not supported these conclusions. Importantly, the large D2d RCT only showed a non-significant trend to slow down the progression of prediabetes into T2DM. In a small subgroup of individuals with overweight (rather than obesity) and prediabetes, supplementation provided some modest benefit, albeit lower than lifestyle modifications or metformin 26 . Furthermore, analysis of the combined results of the D2d trial and two other trials showed that vitamin D supplementation reduced the risk of developing T2DM in people with prediabetes not selected for vitamin D deficiency 22 . Additional studies or more in-depth analysis of the existing studies are needed to validate these findings. In summary, the evidence from large-scale Mendelian randomization studies and RCTs are convergent and do not support the use of vitamin D supplementation for the prevention of T2DM.
Strong preclinical data exist that link vitamin D with cell cycle control and cancer. Furthermore, many observational studies have associated poor vitamin D status with increased risk of cancer or poor prognosis 27 .
The largest RCT (VITAL) did not find an effect of daily vitamin D supplementation on invasive cancer incidence (HR 0.96, 95% CI 0.88–1.06) in US adults during a 5.3-year follow-up 15 . Further subanalysis (not statistically corrected for multiple comparisons) revealed a significant reduction in cancer risk in individuals with a normal BMI (<25 kg/m 2 ) and a trend for decreased cancer risk in African Americans. Baseline serum 25OHD concentrations did not influence cancer incidence or mortality but the number of participants with vitamin D deficiency at baseline (<50 nmol/l) was low (~10% of the total cohort) 28 . In the ViDA trial in New Zealand adults, monthly vitamin D supplementation did not modify cancer incidence (overall or specific types of cancer, excluding non-melanoma skin cancers) with an overall hazard ratio of 1.01 (95% CI 0.81–1.25) 16 .
Cancer mortality, as evaluated in a Cochrane systematic review 29 , was modestly decreased by vitamin D supplementation in four RCTs (44,492 participants), with a relative risk (RR) for cancer mortality of 0.88 (95% CI 0.78–0.98) in individuals receiving a mean daily dose of 1,146 IU (compared with no supplementation) during a mean follow-up of 6.3 years. Cancer mortality was also evaluated in several large RCTs (Supplementary Box 4 ). In the ITT analysis of the VITAL trial, a non-significant trend of reduction in total cancer mortality (HR 0.83, 95% CI 0.67–1.02) was observed in the vitamin D supplementation group. When excluding cancer deaths during the first year, or the first and second year after randomization, a significant reduction in cancer mortality was observed in the vitamin D supplementation group compared with no supplementation (HR 0.75, 95% CI 0.59–0.96). In a Kaplan–Meier plot, the cumulative increased risk of cancer mortality was visible from year 4 of follow-up onwards 28 . In the ViDA trial, however, the number of cancer deaths was not influenced by vitamin D supplementation (HR 0.97), even after exclusion of cancer deaths registered in the first year after randomization (HR 0.95) 16 . This discrepancy might be related to the short duration of follow-up. The ViDA trial lasted <4 years, whereas the effect of vitamin D supplementation in the VITAL study was only significant 4 years after randomization. An updated summary from the VITAL study 28 confirmed a small but significant effect on cancer death in vitamin D-supplemented individuals (HR 0.87, 95% CI 0.79–0.96; P = 0.005). As the final serum concentration of 25OHD in the VITAL trial (~110 nmol/l) and the ViDA trial (~125 nmol/l or 50 ng/ml) were in the high normal range it is unlikely that higher doses would be more effective.
The Ovarian Cancer Association Consortium (10,065 patients with ovarian cancer, 21,654 control individuals) 30 found a 27% increase in the risk of epithelial ovarian cancer per 20 nmol/l decrease in genetically determined 25OHD serum concentration (OR 1.27, 95% CI 1.06–1.51). However, the results were not corroborated by another Mendelian randomization study 31 which also showed no evidence of an association between 25OHD and risk of colorectal, breast, prostate, lung and pancreatic cancer or neuroblastoma. Similar findings were reported in a separate study 32 in relation to total incident cancer and cancer subtypes such as breast, colorectal and lung cancer in 23,294 women. A null effect of genetically determined 25OHD on colorectal carcinoma was confirmed in men and women after including two additional SNPs 33 . Similarly, a large-scale two-sample Mendelian randomization study (122,977 patients with breast cancer and 79,148 patients with prostate cancer) did not show any effects of genetically predicted 25OHD concentrations on these cancers (Supplementary Box 5 ). Evidence from Mendelian randomization also refutes a link between 25OHD concentrations with risk of oesophageal adenocarcinoma 34 , melanoma and non-melanoma skin cancer 35 (Supplementary Box 5 ).
Vitamin D and cancer — summary
No effects of vitamin D supplementation on cancer risk were observed in the large VITAL and ViDA trials. In line with prior studies and Mendelian randomization results, it thus seems clear that vitamin D supplementation in vitamin D-replete adults does not change cancer risk. However, a subanalysis of the VITAL trial showed that vitamin D supplementation might have some minor benefits in individuals with a normal BMI, but this finding was not corrected for multiple end point analysis 15 . In addition, several independent trials have suggested, in post hoc analysis, potential benefits of vitamin D supplementation on cancer mortality, especially when the follow-up is longer than 4 years 28 (Supplementary Box 4 ). Therefore, a link between vitamin D status and cancer incidence or mortality cannot be excluded, but will be very difficult to verify. Small changes in vitamin D status are unlikely to affect cancer incidence based on several Mendelian randomization studies.
Cardiovascular events
Major cardiovascular events.
The results of any observational studies in humans are in line with preclinical data and have demonstrated a consistent association between low vitamin D status and increased risk of cardiovascular diseases, hypertension and cardiovascular events, including ischaemic cardiac events, cardiomyopathy, congestive heart failure, stroke and even cardiovascular mortality. In a meta-analysis of nearly 850,000 individuals, low serum 25OHD concentrations were associated with an increased risk of cardiovascular events (RR 1.43, comparing individuals with the lowest vitamin D status with individuals with a better vitamin D status) 36 .
Two large RCTs (VITAL and ViDA) were designed to include cardiovascular events as one of their primary end points 15 , 37 . During the 5.3 years of follow-up in the VITAL trial, the hazard ratio for the expanded composite end point of major cardiovascular events including coronary revascularization was 0.97 (95% CI 0.85–1.12) in the vitamin D supplementation group, compared with placebo. A similar hazard ratio was found for cardiovascular death (HR 1.11, 95% CI 0.88–1.40), or death from any cause. Exclusion of cardiovascular events or deaths during the first 2 years of follow-up did not change the overall results. Similarly, in the ViDA study, the primary outcome of major cardiovascular events was not influenced by monthly vitamin D supplementation over 3.3 years 37 . The adjusted hazard ratio for a combination of major cardiovascular events in the vitamin D supplementation group was 1.02 (95% CI 0.87–1.20) compared with placebo, and such null findings also applied for a large list of secondary end points (myocardial infarction, heart failure, stroke and hypertension, among others), or cardiovascular deaths. Findings were not dependent on the baseline serum 25OHD concentration or previous cardiovascular status. When the results of these two major trials (including together more than 30,000 participants) were combined with those of previous studies evaluating the potential effects of vitamin D supplementation, a similar general conclusion of no effect of vitamin D supplementation was reached. An analysis of 21 RCTs including more than 80,000 participants showed that major cardiovascular events were not influenced by vitamin D supplementation 38 . The hazard ratios for myocardial infarction, stroke or cardiovascular death were all close to 1 and the 95% confidence intervals included the null. The results are uniformly concordant despite variation in target groups, baseline vitamin D status and vitamin dosage or regimens. Furthermore, vitamin D supplementation of largely vitamin D-replete participants did not significantly reduce first or recurrent hospitalization rates for heart failure compared with no supplementation in the VITAL Heart Failure study (HR 0.93, 95% CI 0.78–1.11; non-significant).
To date, six Mendelian randomization studies have investigated the effect of genetically altered 25OHD levels on cardiovascular events and related outcomes (Supplementary Box 6 ). These studies evaluated the effects of genetically altered 25OHD concentrations (based on two to six SNPs) in more than a million European and Chinese adults and found no significant effects on any cardiovascular event or mortality 39 , 40 , 41 , 42 . A 2020 study 43 , using a substantially larger number of SNPs (242 SNPs associated with 25OHD levels adjusted for BMI, and 232 SNPs associated to 25OHD levels without adjustment for BMI), showed a non-significant odds ratio for coronary artery disease in people with genetically lowered 25OHD levels of 0.98 (95% CI −0.06–0.02) compared with those with normal or high 25OHD level in a sample of 417,580 white British individuals from the UK Biobank.
Hypertension
Observational data also link hypertension with low vitamin D status but this apparent association could have been due to many other confounding factors (for example, related to lifestyle). Causal inference studies, such as RCTs and Mendelian randomization studies, should provide insights that reduce the risk of confounding. The data on blood pressure effects of vitamin D supplementation in the VITAL trial (VITAL Hypertension) are not yet available (NCT01653678; as of October 2021). The ViDA trial, however, studied extensively the effects of vitamin D supplementation in a subgroup of participants using a state of the art invasive technology (suprasystolic oscillometry) 44 . After a mean follow-up of 1.1 years, vitamin D supplementation generated null effects. In participants with vitamin D deficiency at baseline (<50 nmol/l), brachial systolic and diastolic blood pressure decreased by 3 mmHg to 5 mmHg (not statistically significant); however, aortic systolic blood pressure (−7.5 mmHg, P = 0.03) and other parameters (augmentation index, pulse wave velocity, peak reservoir pressure and backward pressure amplitude) improved on correction of baseline vitamin D deficiency 44 . The DO-HEALTH trial in European older adults did not find any effect of vitamin D supplementation on systolic or diastolic blood pressure 18 .
The evidence from Mendelian randomization studies on the effects of predicted serum 25OHD levels on hypertension, systolic and diastolic blood pressure is consistent across five large studies, and overall does not support any of these outcomes (Supplementary Box 6 ). Specifically, a study in 146,581 European individuals 45 , using two SNPs in the two vitamin D synthesis genes showed a marginal decrease in diastolic blood pressure of 0.29 mmHg per 10% increase in 25OHD level. There was no significant effect on systolic blood pressure, and the Mendelian randomization odds ratio for hypertension was 0.92 per 10% increase in 25OHD level (95% CI 0.87–0.97). A 2019 study, using six 25OHD-related SNPs 46 , failed to show any evidence of a causal association between 25OHD levels and systolic blood pressure, diastolic blood pressure or hypertension. Finally, using up to 252 SNPs as instruments for estimating levels of 25OHD, the most recent Mendelian randomization study in this field published in 2020 (ref. 43 ) showed a marginal effect of 25OHD levels on risk of hypertension (Mendelian randomization OR 0.97 per unit increase in rank-based inverse normal-transformed 25OHD level, 95% CI 0.94–1.0) in 417,580 White British individuals from UK Biobank. After adjusting for BMI, this association became non-significant. In non-European populations, Mendelian randomization results thus far are consistent with those in Europeans. Specifically, a Mendelian randomization study 47 on 2,591 Korean adults failed to show any causal effect of 25OHD levels on systolic blood pressure, diastolic blood pressure or risk of hypertension. A Mendelian randomization study 48 in 10,655 Chinese individuals showed equally a null effect of 25OHD on systolic and diastolic blood pressure.
Vitamin D and cardiovascular disease — summary
In summary, convergent evidence from Mendelian randomization studies and RCTs demonstrates that vitamin D supplementation does not decrease the risk of cardiovascular disease. The link between vitamin D status and a variety of cardiovascular events or risk factors was tested previously in mostly small-scale studies. The 2017–2020 megatrials (Table 1 ) and Mendelian randomization studies clearly confirm the lack of benefit of vitamin D supplementation in vitamin D-replete adults. This conclusion most likely also applies to people with vitamin D deficiency as based on subgroup analyses of the VITAL and ViDA trials. Unfortunately, both studies recruited very few participants with severe vitamin D deficiency. A dedicated detailed analysis of the ViDA trial suggested some modest benefits on central (but not peripheral) blood pressure, but the implications of this observations are limited in view of the small scale of this ViDA substudy 44 .
Musculoskeletal effects and falls
Vitamin d and bone health.
Severe vitamin D deficiency is the leading cause of nutritional rickets 1 . The importance of more modest vitamin D deficiency than seen in nutritional rickets for the skeleton of adults and older adults is disputed. Supplementation with vitamin D only is unlikely to be able to reduce fracture risk in older adults; 2 , 49 however, a combination of calcium and vitamin D supplementation can modestly reduce hip and non-vertebral fracture incidence in this population 2 , 50 , 51 . This conclusion is in line with a 2019 overview and meta-analysis on vitamin D and calcium supplementation and fractures 52 , which concluded from observational data (39,0141 participants) that a 25 nmol/l increase in the serum 25OHD concentration reduces the risk of any fracture or hip fracture by 7% and 20%, respectively (both statistically significant). A similar conclusion was reached in another meta-analysis 53 .
Several large RCTs have generated new results regarding the effects of vitamin D supplementation on the adult skeleton. The VITAL Bone Health study is an ancillary study of the VITAL trial, including a subcohort of 771 participants (men aged ≥50 years and women aged ≥55 years; not taking bone active medications) evaluated at baseline and after 2 years (89% retention), and aims to evaluate the effects of vitamin D on bone structure and architecture. Supplemental vitamin D (compared with placebo) had no effect on 2-year changes in areal bone mineral density (BMD) at the spine, femoral neck, total hip or whole body, or on measures of bone structure. This conclusion remained valid in a subgroup analysis, including individuals with the lowest vitamin D status (as measured by total 25OHD) at baseline. New technology allows the direct measurement of free (non-protein-bound) 25OHD as an alternative strategy to define vitamin D status 54 . In participants of the VITAL trial with the lowest directly measured free 25OHD concentrations, vitamin D supplementation generated a slight increase in spine areal BMD (0.75% in the vitamin D group versus 0% in the placebo group; P = 0.043) and attenuation in loss of total hip areal BMD (−0.42% in the vitamin D group versus −0.98% in the placebo group; P = 0.044), yet such results might not survive multiple testing correction 55 . The ViDA trial did not find an effect of monthly vitamin D supplementation on the incidence of non-vertebral fractures (RR 1.19, 95% CI 0.94–1.50; non-significant) compared with no supplementation 56 . In participants with baseline vitamin D deficiency (<50 nmol/l), the HR for non-vertebral fractures was 0.94 compared with that in vitamin D-replete participants (95% CI 0.58–1.52). This conclusion was confirmed in the DO-HEALTH trial 18 .
A well-validated risk factor for fracture, such as BMD, might provide more information on the possible effects of vitamin D supplementation. In a subgroup of participants in the ViDA trial ( n = 452) 57 , the loss of BMD during follow-up was about 0.5% lower in the vitamin D group compared with the control group. This difference was statistically significant for the femoral neck and total hip but not for the lumbar spine or total body BMD. However, in the small ( n = 30) group of participants with a baseline serum 25OHD concentration of <30 nmol/l, BMD of the lumbar spine increased significantly by 3.1% compared with that in controls. These data indicate that correction of severe vitamin D deficiency might improve bone density, but not when given to vitamin D-replete people. A smaller RCT in Scottish adults confirmed that vitamin D supplementation (daily dose of 1,000 IU) increased BMD in individuals with a baseline serum 25OHD concentration of <30 nmol/l but not in people with a better vitamin D status at baseline 58 . These results are also in line with a RCT in US adults randomized to receive placebo, 800 IU of vitamin D or high-dose vitamin D (50,000 IU per day for 2 weeks followed by 50,000 IU per 2 weeks for 1 year), which concluded that neither low-dose nor high-dose vitamin D improved bone density in participants with a mean baseline serum 25OHD of 50 nmol/l (ref. 59 ). The same conclusion was drawn from a RCT of vitamin D supplementation in Black American women, as increasing baseline serum 25OHD concentrations of 55 nmol/l to concentrations above 75 nmol/l by vitamin D supplementation did not change the rate of bone loss during 3 years of follow-up 60 . Similarly, Finnish children below the age of 2 years who received 1,200 IU of vitamin D per day for ~2 years did not have better bone density (measured by peripheral quantitative CT (pQCT)) compared with children receiving the standard dose of 400 IU per day 61 . This finding is not totally unexpected, as the baseline serum 25OHD concentration was higher (80 nmol/l) than expected in this study due to the introduction of vitamin D supplementation of food in Finland.
The Calgary study was designed to evaluate the effect of long-term high-dose vitamin D on bone mass and quality. A daily dose of 400 IU, 4,000 IU or 10,000 IU of vitamin D for 3 years in Canadian adults did not increase BMD, but rather slightly decreased BMD, as measured by the best available methodology (high-resolution pQCT) 19 . Indeed, BMD at the radius and tibia significantly decreased by 3.5% and 1.7 %, respectively in the 10,000 IU per day group compared with the 400 IU per day group, whereas the decrease at both sites was not statistically significant in the 4,000 IU per day group compared with the 400 IU per day group. This study does demonstrate that vitamin D supplementation in vitamin D-replete adults (baseline serum 25OHD concentration of about 75 nmol/l) does not improve bone mass or quality. Moreover, very high doses might even have negative effects, as a small percentage of participants developed hypercalciuria or hypercalcaemia, which quickly resolved after adjustment of dosing. Of course, this finding might imply that regular follow-up is desirable when using such dosages 19 , 62 .
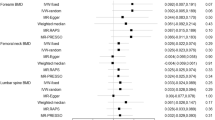
Many Mendelian randomization studies showed no causal effect of vitamin D status on a variety of bone traits in populations of European and non-European ancestry. An early Mendelian randomization study 63 found that genetically predicted one standard deviation increase in 25OHD was not associated with increased femoral neck BMD, lumbar spine BMD or estimated BMD change. Similar results were observed in relation to total body BMD 64 . A more powered Mendelian randomization analysis 65 (37,857 patients with fracture and 227,116 control individuals) also did not support a causal effect of 25OHD on fracture risk. However, a Mendelian randomization study in children 66 showed that haplotypes associating with low 25OHD were associated with low pQCT parameters (BMD, cross-sectional area and cortical density) in 2-year-old children. Finally, evidence from Mendelian randomization studies 67 refutes causal associations between predicted serum 25OHD concentrations and either BMD or bone metabolism markers found in 1,824 postmenopausal Chinese women (Supplementary Box 6 ).
Vitamin D and muscle function or falls
In mice, total deletion of VDR generates structural and functional consequences for skeletal and cardiac muscle 9 . Furthermore, humans with congenital CYP27B1 mutations or patients with severe combined deficiency of 25OHD and 1,25(OH) 2 D due to chronic renal failure develop severe muscle weakness that rapidly improves after treatment with 1,25(OH) 2 D 9 . Several meta-analyses have come to different conclusions regarding the consequences of vitamin D supplementation on muscle strength, with both positive 68 and null effects 69 . In addition, ample literature is available supporting a link between poor vitamin D status and increased risk of falls, but hesitance remains regarding causality 70 . High boluses of vitamin D, however, might transiently increase the risk of falls in older women 71 . High-dose continuous vitamin D supplementation to increase serum 25OHD concentrations to above 112 nmol/l might also induce an increased risk of falls in older men and women 72 , 73 , 74 . However, the large ViDA trial showed that monthly 100,000 IU doses of vitamin D did not reduce or increase the risk of falls. The hazard ratio for falls was 0.99 (95% CI 0.92–1.07) in the overall cohort who were treated with vitamin D compared with those receiving placebo and 1.07 (95% CI 0.91–1.25) in vitamin D-supplemented participants with baseline serum 25OHD concentrations below 50 nmol/l (ref. 56 ). The VITAL trial also looked at the effects of daily vitamin D supplementation on physical disability and falls in the SRURDY study 75 and found a non-significant (OR 0.97, 95% CI 0.91–1.25) effect of vitamin D supplementation on the risk of two falls or injurious falls requiring support from a doctor or hospital 76 . In further exploratory analysis, the same conclusion was reached when the baseline serum concentration of 25OHD was taken into account.
To our knowledge, no Mendelian randomization studies so far have examined the causal association between genetically estimated 25OHD levels and muscle traits or falls.
Vitamin D and musculoskeletal effects — summary
Of note, the 2017–2020 megatrials did not address the question of vitamin D supplementation and rickets, as there is consensus in all vitamin D guidelines from the past decade that serum 25OHD concentrations below 30 nmol/l are a risk factor for rickets or osteomalacia 12 . A daily vitamin D dose of 400 IU can prevent rickets and osteomalacia and increase serum concentrations of 25OHD well above 30 nmol/l (12 ng/ml) 77 . However, ~7% of the world population lives with severe vitamin D deficiency, with this percentage being much higher in the Middle East, North Africa and many countries in Asia 78 .
The role of vitamin D in the skeleton of adults and older adults is more disputed. The 2017–2020 megatrials were not designed to primarily evaluate the effect of vitamin D supplementation on fracture risk in older adults. These trials 15 , 16 recruited mostly vitamin D-replete adults with a fairly low risk of fracture. Even the DO-HEALTH trial in older, less vitamin D-replete, adults (compared with the other megatrials) did not find an effect on non-vertebral fractures 18 . However, the ViDA trial demonstrated that correction of severe vitamin D deficiency (<30 nmol/l) prevents age-related bone loss in adults. By contrast, the 2017–2020 megatrials demonstrate that vitamin D supplementation in vitamin D-replete adults does not improve bone mass, density or quality 16 .
Taken together, the findings indicate that supplementation with vitamin D only does not have a beneficial effect on fracture risk in vitamin D-replete, mostly white adults. However, combined calcium and vitamin D supplementation in older adults, especially those with poor vitamin D status and poor calcium intake, might decrease the risk of hip fractures and other major fractures by about 20% 51 . Therefore, most recent guidelines recommend a daily vitamin D supplement of about 800 IU of vitamin D combined with a good calcium intake (above 1,000 mg per day) in all older adults with a high risk or documented vitamin D deficiency. Of note, the Calgary study demonstrated that high daily doses of vitamin D (4,000 and especially 10,000 IU per day) might decrease BMD and bone quality 19 , 20 . Therefore, the optimal dose in vitamin D-deficient older adults should be at least 800 IU per day but not more than 4,000 IU per day.
Meta-analyses of older studies suggested a modest decrease in the risk of falls in older, mostly vitamin D-deficient, adults 79 . However, the ViDA trial did not confirm this finding as vitamin D supplementation did not change the risk of falls. The New Zealand population was younger and had a better vitamin D status than the participants in the older studies. There might also be a U-shaped relationship as very high vitamin status, especially due to high bolus doses, might increase the risk of falls 72 , 73 , 74 .
Lung function and respiratory effects
Vitamin d and respiratory infections or lung function.
The lung is increasingly recognized as an important target tissue for vitamin D. Observational data link poor vitamin D status with several inflammatory lung diseases or impaired lung function 80 , 81 , 82 . The most recent analysis published in 2019 (ref. 83 ) evaluated 10,933 participants in 25 RCTs and found a significant overall reduction in acute respiratory infections following vitamin D supplementation (OR 0.88, 95% CI 0.81–0.96) compared with no supplementation. The number needed to treat for benefit was 33. Subgroup analysis revealed that the greatest benefits were found in people with severe vitamin D deficiency (<25 nmol/l) at baseline (OR 0.58, 95% CI 0.40–0.82). Subgroup analysis revealed that intermittent (monthly or less frequent) doses of vitamin D did not generate protection, whereas daily or weekly vitamin D supplementation was more effective for preventing acute respiratory infections (OR 0.81, 95% CI 0.072–0.91). In the ViDA trial, however, no effects of vitamin D supplementation were found on acute respiratory infections in older adults 84 . This finding is not a total surprise as the lack of effects might be due to the intermittent dosing and/or adequate vitamin D status at baseline, and therefore might not contradict the findings of the 2019 meta-analysis 83 . In addition, the European DO-HEALTH trial did not show an effect on infections in general nor on upper respiratory infections 18 .
Several small-scale studies (eight RCTs) did not find an improvement in lung function (as measured in terms of forced expiratory volume in 1 s (FEV1)) in patients with chronic obstructive pulmonary disease (COPD) who were randomized to receive vitamin D supplementation 85 . A substudy of the ViDA trial, however, evaluated the effects of monthly vitamin D supplementation 86 in 442 adults treated for 1.1 years. Overall, in the ITT analysis, no significant effects were observed on FEV1. However, subgroup analysis revealed some beneficial effects, especially in subjects with existing lung problems such as asthma, COPD or a history of smoking (Table 2 ). To date, no Mendelian randomization studies have been performed that examined 25OHD levels, COPD and lung function.
Vitamin D and COVID-19
In view of the enormous health implications of the coronavirus disease 19 (COVID-19) pandemic caused by the worldwide spread of severe acute respiratory syndrome coronavirus 2, a possible link with poor vitamin D status and the risk or severity of COVID-19 has received great attention. Seven studies so far compared serum 25OHD concentrations in patients with COVID-19 compared with individuals without COVID-19 (ref. 87 ) and found a lower level (mean difference of about 12 nmol/l) in patients with COVID-19; however, in many studies the sampling did not take place at the same time in both groups. In addition, these studies were unable to control for confounding factors, a major problem due to the large number of similarities in the risk factors for vitamin D deficiency and COVID-19. About 31 studies looked at a possible link between vitamin D status and severity of the outcome of COVID-19. Lower serum concentrations of 25OHD were associated with greater mortality, greater need for intensive care treatment or increased severity of illness in general compared with better vitamin D status. However, this finding was based on observational studies. One placebo-controlled intervention study using a bolus dose of vitamin D (200,000 IU) did not reveal a beneficial effect in patients hospitalized with COVID-19 with a mean baseline 25OHD concentration of 50 nmol/l (ref. 88 ). However, one pilot study (which was not placebo-controlled) showed a marked reduction in the need for intensive care treatment in patients hospitalized for COVID-19 and treated with a high dose of 25OHD (calcifediol) at the time of admission 89 . Therefore, the link between vitamin D status and COVID-19 is unsettled so far, but many trials are ongoing that might clarify this question.
In 2021, a Mendelian randomization study assessed the causal role of serum 25OHD levels on COVID-19 susceptibility and disease severity 90 . Using data from 11,181 patients with COVID-19 and 116,456 control individuals from the Host Genetics Initiative, and six vitamin D SNPs that explain 2.5% of the variance in serum 25OHD levels, this study did not show any association between genetically decreased 25OHD and COVID-19 susceptibility or severity. These results were confirmed in a separate Mendelian randomization study using 81 25OHD SNPs that explain 4.3% of the variance in serum 25OHD levels, which also showed no effect of genetically determined 25OHD levels on risk of COVID-19-related hospitalization 91 .
Vitamin D and asthma
Research investigating the potential effects of vitamin D status on asthma has largely focused on a possible link between prenatal or maternal vitamin D status and wheezing or asthma in the offspring. A meta-analysis of four prospective studies and three RCTs concluded that vitamin D intake (~800 IU per day) by women during pregnancy is inversely related to wheezing or asthma in their offspring during up to 3 years of follow-up 92 . However, a longer follow-up did not confirm this conclusion: vitamin D supplementation during the prenatal period alone did not influence the 6-year incidence of asthma and recurrent wheeze among children who were at risk of asthma 93 . Two Mendelian randomization studies have investigated the causal association between vitamin D and asthma. A large study (n > 160,000 children and adults) 94 found odds ratios of 1.03 (95% CI 0.90–1.19) for asthma and 0.95 (95% CI 0.69–1.31) for childhood-onset asthma per standard deviation of log-transformed decrease in serum 25OHD (Supplementary Box 6 ). These findings suggest that vitamin D levels probably do not have clinically relevant effects on the risk of asthma.
Vitamin D and respiratory effects — summary
The vitamin D endocrine system influences all cells and most cytokines of the immune system 9 . The innate immune system is stimulated by 1,25(OH) 2 D and this is in line with a decreased risk of upper respiratory infections with vitamin D supplementation in individuals with vitamin D deficiency 83 . Meta-analysis of intervention studies suggested a benefit of vitamin D supplementation of participants with severe vitamin D deficiency and COPD, asthma, or similar lung diseases, and on reducing the risk of acute upper respiratory infections in severely deficient individuals 83 . However, where tested, these findings have not been supported by Mendelian randomization studies 90 . According to the results of the LUNG-ViDA trial, vitamin D supplementation might modestly improve expiratory lung function 85 . If confirmed, such data would imply that the lung is a clinically relevant target issue for vitamin D. Of note, currently there are insufficient RCTs to evaluate the potential benefit of vitamin D or calcifediol supplementation on the risk or severity of COVID-19.
Autoimmune diseases
Observational studies have, in line with preclinical data, made a link between poor vitamin D status and increased risk of infection or risk of autoimmune diseases (such as multiple sclerosis (MS), inflammatory bowel diseases or type 1 diabetes mellitus) 95 . RCTs in humans dealing with infections have mainly focused on upper respiratory infections and an overview is presented in the previous section. Unfortunately, no major RCTs have addressed the possible primary or secondary prevention of the major human autoimmune diseases. So far, the 2017–2020 megatrials (Table 1 ) have not shown results related to autoimmune diseases.
Currently, strong evidence exists that supports a causal association between genetically low serum 25OHD levels and increased risk of MS 96 , 97 , 98 , 99 . The most recent Mendelian randomization study from 2020 evaluated data from The International Multiple Sclerosis Genetics Consortium discovery phase GWAS (14,802 MS and 26,703 controls from the USA, Europe, Australia and some Asian countries) 97 using six SNPs associated with serum levels of 25OHD and found that each genetically determined unit increase in log-transformed 25(OH)D 3 was associated with an odds ratio for MS of 0.57 (95% CI 0.41–0.81; P = 0.001) (Table 4 ). This effect applies to adult-onset and childhood-onset MS.
Earlier Mendelian randomization evidence 100 did not support causality of predicted serum 25OHD levels in systemic lupus erythematosus or rheumatoid arthritis. Consistent null effects on rheumatoid arthritis were found in a 2020 Mendelian randomization study in participants from the UK Biobank, using ~220 vitamin D-associated SNPs as instruments 43 . Null effects of predicted serum 25OHD levels were also shown in Mendelian randomization studies on Crohn’s disease (odds ratio for 10 nmol/l higher 25OHD of 1.04, 95% CI 0.93–1.16) and ulcerative colitis (OR 1.13, 95% CI 1.06–1.21) 101 . Similarly, no effect on ulcerative colitis was found in participants from the UK Biobank 43 . The UK Biobank study also did not support a causal role of vitamin D on allergic rhinitis. Finally, Mendelian randomization 94 does not support causal effects of 25OHD on atopic dermatitis. A 2021 Mendelian randomization study on type 1 diabetes mellitus did not support causal effects of genetically lowered 25OHD levels on the risk of this disease 102 .
In summary, the adaptive immune system is downregulated by 1,25(OH) 2 D and therefore vitamin D deficiency might predispose to autoimmune diseases 9 . Observational studies have suggested this effect might apply to humans, but too few intervention studies have been conducted to evaluate this statement. Four independent Mendelian randomization studies agree, however, that individuals with genetically driven lower serum 25OHD concentrations have an increased risk of developing MS, either during adolescence or adulthood (Table 4 ).
Intervention studies as summarized in a Cochrane review from 2016 (ref. 103 ) dealing with 22 RCTs including 3,725 pregnant women, concluded that vitamin D supplementation significantly reduced the risk of pre-eclampsia (RR 0.48), gestational diabetes mellitus (RR 0.51) and low birthweight (<2,500 g; RR 0.55) compared with no supplementation. An update of these data 104 largely confirmed these observations. However, a large RCT in pregnant Bangladeshi women with severe vitamin D deficiency (baseline mean serum 25OHD about 25 nmol/l) supplemented from week 17–24 onwards with placebo or vitamin D (three groups receiving 4,200, 16,800 or 28,000 IU per week) until birth did not find a beneficial effect on fetal or neonatal parameters of length, weight or head circumference, either at birth or at one year of age ( n = 1,164 infants) 105 .
To date only one Mendelian randomization study 106 has examined the causal effect of predicted serum 25OHD levels on gestational hypertension and pre-eclampsia. Overall, the evidence was weak supporting a causal effect of vitamin D status on gestational hypertension (OR 0.90, 95% CI 0.78–1.03) or pre-eclampsia (OR 0.98, 95% CI: 0.89–1.07) per 10% decrease in serum 25OHD (Supplementary Box 5 ).
In summary, pregnant women more frequently have a poor vitamin D status than non-pregnant women of the same age but the absolute and relative values vary from country to country. Several meta-analyses have suggested that vitamin D supplementation might modestly decrease maternal morbidity and improve the health of their offspring 103 , 104 . However, a 2018 large RCT in Bangladeshi women with severe vitamin D deficiency did not confirm this observation 105 . Therefore, the effects of poor vitamin D status during pregnancy on pregnancy outcomes for mother and infant remains unsettled.
Patients in intensive care
Patients with severe acute illness requiring intensive care frequently have low serum concentrations of 25OHD and this poor vitamin D status is linked with increased morbidity and mortality 107 , 108 . Two major RCTs so far in patients in intensive care units (ICU) have generated conflicting results. In the VITdAL-ICU trial, patients in the ICU were randomized to either placebo ( n = 243) or high-dose oral vitamin D ( n = 249) (starting dose 540,000 IU followed by monthly maintenance doses of 90,000 IU for 5 months). Mean baseline serum 25OHD concentrations were low (33 nmol/l) and increased to ~82 nmol/l at day 3. Length of stay in the ICU or hospital, mortality in the ICU, in-hospital mortality and mortality at 6 months did not improve with the intervention. In a predefined subgroup with severe vitamin D deficiency who received the intervention (<30 nmol/l), hospital mortality (HR 0.56, 95% CI, 0.35–0.90) and 6-month mortality (HR 0.60, 95% CI, 0.39–0.93) were significantly decreased compared with patients with severe vitamin D deficiency who received placebo 107 . In the much larger Amrein ICU trial 108 , 1,059 patients in the ICU with vitamin D deficiency (<50 nmol/l) received either placebo or a single oral high dose of vitamin D (540,000 IU). This dose increased mean serum 25OHD concentration at day 3 to a mean concentration of 117 ± 58 nmol/l in comparison with the control group (mean concentration 28 ± 14 nmol/ml). The primary end point (90-day mortality) and other non-fatal outcomes were similar in the two groups. Although all patients in both studies were admitted to ICUs, the US patients in the VITdAL-ICU trial were probably less sick than those in the Amrein trial 107 as indicated by the percentage of patients requiring mechanical ventilation (32% in the US trial).
Effects of vitamin D supplementation on safety outcomes
In all vitamin D supplementation RCTs, some safety end points have been reported in addition to mortality (see next section). No effects were found on serum calcium or calciuria unless very high doses were used, such as 4,000–10,000 IU per day in the Calgary study. Even in these circumstances, hypercalcaemia was infrequent and occurred transiently after changes in treatment modality 19 , 62 . A modestly increased risk of kidney stones was observed in the WHI trial 109 , but this effect was not seen in the more recent 2017–2020 megatrials (that is, ViDA, VITAL and D2d; Table 1 ). Furthermore, no changes in kidney function were found in these large trials. Skeletal consequences were either null effects, slight (beneficial) increases in BMD in subgroups with poor vitamin D status at baseline, or a modest but significant decrease in BMD during high-dose (10,000 IU per day) therapy in the Calgary study 19 . An increased risk of fractures in patients receiving high intermittent bolus doses has been reported 71 , 110 . Similarly, an increased risk of falls has been reported when either high intermittent doses 71 or high continuous doses were used 72 , 73 . Importantly, the 2017–2020 megatrials (that is, ViDA, VITAL and D2d), with detailed evaluation of about 30,000 participants for 2–5 years, did not discover notable adverse effects. These findings indicate that a daily dose (or dose equivalent) of 2,000–4,000 IU can be considered as safe in an adult (even vitamin D-replete) population. High-dose vitamin D also did not modify arterial calcifications during a 3-year follow up in the Calgary study 111 .
Effects of vitamin D supplementation on mortality
Observational data have repeatedly linked poor vitamin D status with increased mortality. This effect was extensively documented in several NHANES studies based on representative samples of the US population and confirmed after validation of serum 25OHD concentrations according to standards generated by the US National Institute of Standards and Technology 112 . To decrease the possible effect of reverse causation, people who died within the first 3 years after 25OHD measurements were excluded from the analysis; however, the same association between poor vitamin D status and increased mortality remained 112 . Using a combination of several European prospective studies, mortality was also higher in the population with the poorest vitamin D status compared with the vitamin D-replete population 113 . A 2019 large long-term (>10 years) Finnish study concluded that people with the highest tertile of 25OHD concentrations (>50 nmol/l) had a mortality odds ratio of 0.77 (95% CI 0.71–0.84) compared with people with the lowest tertile of 25OHD concentrations, even in a multivariate model with correction of multiple co-variables 114 .
As nearly all long-term vitamin D supplementation trials include data on mortality, several meta-analyses have shown the effects of vitamin D supplementation on mortality. Extensive meta-analyses published in 2014 showed a modest decrease in overall mortality in participants randomized to vitamin D supplementation; based on 22 RCTs, the risk of death decreased by 11% 36 . A 2014 Cochrane analysis 29 evaluated 56 RCTs including 95,286 participants (mostly healthy women older than 70 years) with a mean follow-up of 4.4 years. Vitamin D supplementation significantly reduced all-cause mortality (RR 0.94, 95% CI 0.91–0.98; P = 0.002) compared with no supplementation. This finding implies that vitamin D supplementation of 150 women for 5 years prevented one additional death. Vitamin D supplementation also decreased cancer mortality (RR 0.88, 95% CI 0.78–0.98; P = 0.02) compared with no supplementation 29 .
In the 2017–2020 megatrials (that is, VITAL, ViDA and D2d), overall mortality was much lower than shown in the previous meta-analyses 29 , 36 and did not show an effect of vitamin D supplementation on overall mortality 15 . A new meta-analysis of 52 RCTs including a total of 75,454 participants concluded that vitamin D (either vitamin D 3 or D 2 ) supplementation did not change mortality (RR 0.98, 95% CI 0.95–1.02) compared with no supplementation 115 . A subanalysis, however, found that vitamin D 3 (instead of D 2 ) supplementation trials tended to reduce mortality (RR 0.95, 95% CI 1.90–1.00; P = 0.06), whereas this was not the case for vitamin D 2 supplementation trials. These new findings conflict with the 2014 reports 112 . The difference could be partly because the 2019 meta-analysis did not include ten RCTs including ~50,000 participants using a combination of vitamin D and calcium supplementation. However, the 2019 meta-analysis did include two megatrials (VITAL and ViDA) that evaluated the effects of vitamin D supplementation in a younger population of mostly vitamin D-replete participants 115 .
In a large-scale population Mendelian randomization study (10,349 deaths in 95,766 total participants) 116 , the odds ratios for a genetically determined lower 25OHD concentration was 1.30 (95% CI 1.05–1.61) for all-cause mortality, 0.77 (95% CI 0.55–1.08) for cardiovascular mortality, 1.43 (95% CI 1.02–1.99) for cancer mortality and 1.44 (95% CI 1.01–2.04) for other types of mortality. Similar point estimates and effect sizes, whose 95% confidence intervals included the null, were found for all-cause mortality in two follow-up Mendelian randomization studies 46 , 117 . Nevertheless, both studies may have been underpowered to detect existing causal associations. Finally, evidence from Mendelian randomization 118 did not support an association between 25OHD concentrations and cancer mortality in a sample of 6,998 deaths from cancer. These data provide some evidence that genetically lowered vitamin D levels might increase overall mortality risks, but the results have not been consistent across studies, or across causes of mortality.
If vitamin D supplementation exerts beneficial effects on extra-skeletal health outcomes and major diseases, then it is likely to have some effects on mortality, especially in older adults with poor vitamin D status. Large meta-analyses dealing mostly with women older than 70 years 29 , 36 showed a 6–11% reduction in mortality; however, adding the newest 2017–2020 megatrials eliminated this effect, possible because these new trials recruited a younger population.
Discordance between studies
Preclinical data are mostly in line with the very large number of observational studies linking very poor vitamin D status with skeletal and extra-skeletal health effects (Fig. 1 ). However, Mendelian randomization studies and the majority of RCTs do not confirm the causality of these associations. Several possible reasons exist for this discrepancy. Most importantly, serum 25OHD levels are a highly confounded variable. Specifically, serum 25OHD levels are affected by a host of health behaviours, the presence of obesity, socioeconomic status and education levels. Although most observational studies have attempted to control for such confounding through multivariable adjustment, such approaches depend upon the degree of accuracy of measurement of the confounders, knowledge that such confounding takes place, and most often that the nature of the confounding relationship (linear versus nonlinear) is known. Furthermore, statistical adjustment for confounding variables can only be accomplished if the confounding variables are known.
The concordance between 25OHD Mendelian randomization studies and RCTs is striking and suggests that Mendelian randomization might be a more relevant way to begin to understand the effect of 25OHD levels on risk of disease than observational studies. Perhaps the vitamin D endocrine system only has a role in these extra-skeletal effects in people with prolonged and very severe vitamin D deficiency. Studies in countries or population groups with severe vitamin D deficiency who need improved vitamin D status anyway might be the ideal approach to better understand the effect of vitamin D supplementation in individuals with severe vitamin D deficiency. Most RCTs and Mendelian randomization studies have been undertaken in individuals from the general population in which the rates of severe vitamin D deficiency are low.
Of note, the available Mendelian randomization studies were not able to predict large variations in serum 25OHD concentrations (usually only about 5% difference or less). However, this low degree of variance would affect the statistical power of a study but not introduce bias. New techniques will soon enable us to use a much larger number of SNPs than used in current studies (usually based on less than six SNPs), thereby allowing much larger variations in serum 25OHD concentrations to be predicted. Most RCTs did not last longer than 3–5 years. In such short-term scenarios, answering the question of causality is extremely difficult. This fact implies that only very long-term improvements in vitamin D status might generate beneficial effects. However, Mendelian randomization studies provide estimates of the effect of a lifetime of genetically lowered vitamin D levels and such Mendelian randomization studies have generally produced null findings.
Reverse causality remains a valid rationale to explain the discordance between observational and intervention studies. The most plausible hypothesis states that individuals with any health problems are less likely to regularly engage in outdoor activity and less exposure to sunlight results in lower vitamin D status. Another mechanism of reverse causality might be that the activity of hepatic 25-hydroxylase is decreased in many major diseases and this decrease could cause low serum 25OHD concentrations. Indeed, data in mice demonstrate that diet-induced obesity, type 1 diabetes mellitus or T2DM, fasting and exposure to glucocorticoids substantially decrease the gene and protein expression of CYP2R1, thereby decreasing the overall 25-hydroxylase activity 119 , 120 , 121 . This finding implies that decreased 25OHD concentrations are the consequence of disease, rather than involved in the origin of these metabolic diseases. Of course, these data from mice need confirmation in humans. Finally, many diseases other than those described in this Review (including brain-related diseases) are linked with poor vitamin D status; however, causality is doubtful without adequate Mendelian randomization studies or RCTs.
Future Mendelian randomization studies
Improved understanding of the genetic determinants of 25OHD has helped re-assess the role of vitamin D in the aetiology of complex diseases through Mendelian randomization. Taken together, the evidence from over 60 Mendelian randomization studies published to date assessing the role vitamin D does not support a causal role for the large majority of studied outcomes. Despite this null data, in the few cases where the evidence from Mendelian randomization supported a causal role of vitamin D status, such as in the example of MS, these results had important clinical implications. For instance, clinical care guidelines for the use of vitamin D in preventing MS in those at risk were published by the MS Society of Canada 122 .
The earlier Mendelian randomization studies used, as instruments for 25OHD levels, SNPs within the four genes related to 25OHD synthesis and metabolism ( DHCR7 , CYP2R1 , GC and CYP24A1 ), which together explained 2.4% of the variance in 25OHD levels 123 . Later Mendelian randomization studies combined the aforementioned four SNPs with two SNPs in SEC23A and AMDHD1 (both genes without clear role in the vitamin D metabolic pathway), and thereby explained ~5.3% of the variance in 25OHD levels. The identification of over 150 25OHD-associated genetic variants in 2020, which explain a considerable portion of the variance in 25OHD levels (~10.5%) 43 , has enabled a deeper understanding of the genetic determinants contributing to variation in circulating 25OHD levels. These newly identified SNPs will probably enable improved instrumentation of vitamin D in Mendelian randomization studies. Moreover, with the emergence of large-scale GWAS in densely phenotyped biobanks, we anticipate that more powerful vitamin D Mendelian randomization studies will be published that utilize the optimized set of genetic instruments. Such new studies should revisit previously studied diseases and investigate new disease outcomes, to further aid causal effect estimation.
Conclusions
In conclusion, the data generated by the 2017–2020 megatrials of vitamin D supplementation in largely vitamin D-replete adults (Table 1 ) demonstrate that increasing the serum 25OHD concentration into the high normal range (based on the IOM and most recent guidelines published over the past decade 12 , in the range of 50–125 nmol/l or 20–50 ng/ml) does not generate benefits for global health or major diseases or medical events such as cancer, cardiovascular events, T2DM, falls or fractures. Therefore, no reason exists at present to recommend vitamin D supplementation of already vitamin D-replete individuals. These data do not contradict the causal link between severe vitamin D deficiency and rickets, or the need to correct severe deficiency at any age. Similarly, the 2017–2020 trials do not contradict the probable beneficial effects of combined supplementation of calcium and vitamin D in older adults with poor vitamin D and calcium status on their risks of fracture or falls.
A few hints have emerged that vitamin D supplementation might have some extra-skeletal benefits, especially in people with severe vitamin D deficiency (such as reduced progression to T2DM, decreased numbers of infections, increased lung function and decreased cancer or overall mortality) (Tables 2 , 3 ). These suggestions are largely based on subgroup or post hoc analyses and thus should not result in the systematic recommendation of vitamin D supplements in such populations but might guide the correct design of future studies.
Arguments have been put forward that daily doses of ≥4,000 IU of vitamin D convey some risks other than simple hypercalcaemia or hypercalciuria. Such doses, or the equivalent of serum 25OHD concentrations well above 112 nmol/l or 45 ng/ml bring no benefits, but might be harmful in some people (for example, in causing loss of BMD or increasing the risk of falls). The same is true for intermittent high-dose boluses of vitamin D. Unfortunately, about 3% of the US population as screened by NHANES use such high dose vitamin D supplements.
Over the past few decades, vitamin D has been a hot topic for scientists and lay people alike, who frequently suggest that vitamin D supplementation might generate a wide variety of health benefits. The data discussed in the present Review might well dampen such enthusiasm. However, a large number of intervention studies (and most probably Mendelian randomization studies) are still ongoing, and these might help provide a better understanding of who would benefit from vitamin D supplementation.
In conclusion, it seems that far too many people with severe vitamin D deficiency (~7% of the world population) do not take or even have access to normal doses of vitamin D. About a third of the world population lives with suboptimal (below 20 ng/ml) serum 25OHD concentrations 78 . However, many vitamin D-replete people take vitamin D supplements without clear benefits. In addition, a small percentage of the population takes higher doses than the upper limit of safe intake. Therefore, we recommend that vitamin D be used wisely and “giveth to those who needeth” 7 .
Munns, C. F. et al. Global consensus recommendations on prevention and management of nutritional rickets. J. Clin. Endocrinol. Metab. 101 , 394–415 (2016).
Article CAS PubMed PubMed Central Google Scholar
Bolland, M. J., Grey, A. & Avenell, A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 6 , 847–858 (2018).
Article CAS PubMed Google Scholar
Luxwolda, M. F., Kuipers, R. S., Kema, I. P., Dijck-Brouwer, D. A. & Muskiet, F. A. Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/l. Br. J. Nutr. 108 , 1557–1561 (2012).
Luxwolda, M. F. et al. Vitamin D status indicators in indigenous populations in East Africa. Eur. J. Nutr. 52 , 1115–1125 (2013).
Holick, M. F. & Grant, W. B. Vitamin D status and ill health. Lancet Diabetes Endocrinol. 2 , 273–274 (2014).
Article PubMed Google Scholar
Bouillon, R., Lips, P. & Bilezikian, J. P. Vitamin D supplementation and musculoskeletal health. Lancet Diabetes Endocrinol. 7 , 85–86 (2019).
Lips, P., Bilezikian, J. P. & Bouillon, R. Vitamin D: giveth to those who needeth. JBMR 4 , e10232 (2020).
CAS Google Scholar
Ebeling, P. R. et al. Management of endocrine disease: therapeutics of vitamin D. Eur. J. Endocrinol. 179 , R239–R259 (2018).
Bouillon, R. et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr. Rev. 40 , 1109–1151 (2019).
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D (National Academies Press, 2011)
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96 , 1911–1930 (2011).
Bouillon, R. Comparative analysis of nutritional guidelines for vitamin D. Nat. Rev. Endocrinol. 13 , 466–479 (2017).
Scientific Advisory Committee on Nutrition (SACN). Vitamin D and health. GOV.UK https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report (2016).
Lips, P. et al. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency; a position statement of the European Calcified Tissue Society. Eur. J. Endocrinol. 180 , 23–54 (2019).
Article Google Scholar
Manson, J. E. et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N. Engl. J. Med. 380 , 33–44 (2019).
Scragg, R. et al. Monthly high-dose vitamin D supplementation and cancer risk: a post hoc analysis of the vitamin D assessment randomized clinical trial. JAMA Oncol. 4 , e182178 (2018).
Article PubMed PubMed Central Google Scholar
Pittas, A. G. et al. Vitamin D supplementation and prevention of type 2 diabetes. N. Engl. J. Med. 381 , 520–530 (2019).
Bischoff-Ferrari, H. A. et al. Effect of vitamin D supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: the DO-HEALTH Randomized Clinical Trial. JAMA 324 , 1855–1868 (2020).
Burt, L. A. et al. Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: a randomized clinical trial. JAMA 322 , 736–745 (2019).
Billington, E. O. et al. Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial. J. Clin. Endocrinol. Metab. 105 , 1261–1273 (2020).
Dawson-Hughes, B. et al. Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the Vitamin D and Type 2 Diabetes (D2d) Study. Diabetes Care 43 , 2916–2922 (2020).
Pittas, A. G., Jorde, R., Kawahara, T. & Dawson-Hughes, B. Vitamin D supplementation for prevention of type 2 diabetes mellitus: to D or not to D? J. Clin. Endocrinol. Metab. 105 , 3721–3733 (2020).
Article PubMed Central Google Scholar
Zhang, Y. et al. Effects of Vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care 43 , 1650–1658 (2020).
Barbarawi, M. et al. Effect of vitamin D supplementation on the incidence of diabetes mellitus. J. Clin. Endocrinol. Metab. 105 , 2857–2868 (2020).
Lu, L. et al. Association of vitamin D with risk of type 2 diabetes: a Mendelian randomisation study in European and Chinese adults. PLoS Med. 15 , e1002566 (2018).
Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 3 , 866–875 (2015).
Feldman, D., Krishnan, A. V., Swami, S., Giovannucci, E. & Feldman, B. J. The role of vitamin D in reducing cancer risk and progression. Nat. Rev. Cancer 14 , 342–357 (2014).
Manson, J. E., Bassuk, S. S., Buring, J. E. & Group, V. R. Principal results of the VITamin D and OmegA-3 TriaL (VITAL) and updated meta-analyses of relevant vitamin D trials. J. Steroid Biochem. Mol. Biol. 198 , 105522 (2020).
Bjelakovic, G. et al. Vitamin D supplementation for prevention of cancer in adults. Cochrane Database Syst. Rev. 6 , CD007469 (2014).
Google Scholar
Ong, J. S. et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Int. J. Epidemiol. 45 , 1619–1630 (2016).
Dimitrakopoulou, V. I. et al. Circulating vitamin D concentration and risk of seven cancers: Mendelian randomisation study. BMJ 359 , j4761 (2017).
Chandler, P. D. et al. Association between vitamin D genetic risk score and cancer risk in a large cohort of U.S. women. Nutrients 10 , 55 (2018).
He, Y. et al. Exploring causality in the association between circulating 25-hydroxyvitamin D and colorectal cancer risk: a large Mendelian randomisation study. BMC Med. 16 , 142 (2018).
Dong, J. et al. No association between vitamin D status and risk of Barrett’s esophagus or esophageal adenocarcinoma: a Mendelian randomization study. Clin. Gastroenterol. Hepatol. 17 , 2227–2235.e1 (2019).
Winslow, U. C., Nordestgaard, B. G. & Afzal, S. High plasma 25-hydroxyvitamin D and high risk of nonmelanoma skin cancer: a Mendelian randomization study of 97 849 individuals. Br. J. Dermatol. 178 , 1388–1395 (2018).
Chowdhury, R. et al. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ 348 , g1903 (2014).
Scragg, R. et al. Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the Vitamin D Assessment Study: a randomized clinical trial. JAMA Cardiol. 2 , 608–616 (2017).
Barbarawi, M. et al. Vitamin D supplementation and cardiovascular disease risks in more than 83000 individuals in 21 randomized clinical trials: a meta-analysis. JAMA Cardiol. 4 , 765–776 (2019).
Afzal, S., Brondum-Jacobsen, P., Bojesen, S. E. & Nordestgaard, B. G. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. BMJ 349 , g6330 (2014).
Manousaki, D., Mokry, L. E., Ross, S., Goltzman, D. & Richards, J. B. Mendelian randomization studies do not support a role for vitamin D in coronary artery disease. Circ. Cardiovasc. Genet. 9 , 349–356 (2016).
Larsson, S. C. et al. Serum 25-hydroxyvitamin D concentrations and ischemic stroke and its subtypes. Stroke 49 , 2508–2511 (2018).
Huang, T. et al. Vitamin D and cause-specific vascular disease and mortality: a Mendelian randomisation study involving 99,012 Chinese and 106,911 European adults. BMC Med. 17 , 160 (2019).
Revez, J. A. et al. Genome-wide association study identifies 143 loci associated with 25 hydroxyvitamin D concentration. Nat. Commun. 11 , 1647 (2020).
Sluyter, J. D. et al. Effect of monthly, high-dose, long-term vitamin D supplementation on central blood pressure parameters: a randomized controlled trial substudy. J. Am. Heart Assoc. 6 , e006802 (2017).
Vimaleswaran, K. S. et al. Association of vitamin D status with arterial blood pressure and hypertension risk: a Mendelian randomisation study. Lancet Diabetes Endocrinol. 2 , 719–729 (2014).
Meng, X. et al. Phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank study. Int. J. Epidemiol. 48 , 1425–1434 (2019).
Kwak, S. Y., Cho, Y., Oh, H. & Shin, M. J. Association of circulating 25-hydroxyvitamin D levels with hypertension and blood pressure values in Korean adults: a Mendelian randomization study on a subset of the Korea National Health and Nutrition Survey 2011-2012 population. Nutr. Res. Pract. 13 , 498–508 (2019).
Chen, C. et al. Association of 25-hydroxyvitamin D with cardiometabolic risk factors and metabolic syndrome: a Mendelian randomization study. Nutr. J. 18 , 61 (2019).
Boonen, S. et al. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 92 , 1415–1423 (2007).
Bolland, M. J., Grey, A., Gamble, G. D. & Reid, I. R. The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis. Lancet Diabetes Endocrinol. 2 , 307–320 (2014).
Avenell, A., Mak, J. C. & O’Connell, D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst. Rev. 4 , CD000227 (2014).
Yao, P. et al. Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw. Open 2 , e1917789 (2019).
Chakhtoura, M., Chamoun, N., Rahme, M. & Fuleihan, G. E. Impact of vitamin D supplementation on falls and fractures–a critical appraisal of the quality of the evidence and an overview of the available guidelines. Bone 131 , 115112 (2020).
Bikle, D., Bouillon, R., Thadhani, R. & Schoenmakers, I. Vitamin D metabolites in captivity? Should we measure free or total 25(OH)D to assess vitamin D status? J. Steroid Biochem. Mol. Biol. 173 , 105–116 (2017).
LeBoff, M. S. et al. Effects of supplemental vitamin D on bone health outcomes in women and men in the VITamin D and OmegA-3 TriaL (VITAL). J. Bone Miner. Res. 35 , 883–893 (2020).
Khaw, K. T. et al. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Lancet Diabetes Endocrinol. 5 , 438–447 (2017).
Reid, I. R. et al. Effect of monthly high-dose vitamin D on bone density in community-dwelling older adults substudy of a randomized controlled trial. J. Intern. Med. 282 , 452–460 (2017).
Macdonald, H. M. et al. 25-hydroxyvitamin D threshold for the effects of vitamin D supplements on bone density: secondary analysis of a randomized controlled trial. J. Bone Miner. Res. 33 , 1464–1469 (2018).
Hansen, K. E. et al. Treatment of vitamin D insufficiency in postmenopausal women: a randomized clinical trial. JAMA Intern. Med. 175 , 1612–1621 (2015).
Aloia, J. et al. Vitamin D supplementation in elderly black women does not prevent bone loss: a randomized controlled trial. J. Bone Miner. Res. 33 , 1916–1922 (2018).
Rosendahl, J. et al. Effect of higher vs standard dosage of vitamin D3 supplementation on bone strength and infection in healthy infants: a randomized clinical trial. JAMA Pediatrics 172 , 646–654 (2018).
Bouillon, R. Safety of high-dose vitamin D supplementation. J. Clin. Endocrinol. Metab. 105 , 1290–1291 (2020).
Larsson, S. C., Melhus, H. & Michaelsson, K. Circulating serum 25-hydroxyvitamin D levels and bone mineral density: Mendelian randomization study. J. Bone Miner. Res. 33 , 840–844 (2018).
Sun, J. Y. et al. Circulating serum vitamin D levels and total body bone mineral density: a Mendelian randomization study. J. Cell Mol. Med. 23 , 2268–2271 (2019).
Trajanoska, K. et al. Assessment of the genetic and clinical determinants of fracture risk: genome wide association and Mendelian randomisation study. BMJ 362 , k3225 (2018).
Kampe, A. et al. Genetic variation in GC and CYP2R1 affects 25-hydroxyvitamin D concentration and skeletal parameters: a genome-wide association study in 24-month-old Finnish children. PLoS Genet. 15 , e1008530 (2019).
Li, S. S. et al. Genetically low vitamin D Levels, bone mineral density, and bone metabolism markers: a Mendelian randomisation study. Sci. Rep. 6 , 33202 (2016).
Beaudart, C. et al. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 99 , 4336–4345 (2014).
Tabrizi, R. et al. The effects of vitamin D supplementation on muscle function among postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. EXCLI J. 18 , 591–603 (2019).
PubMed PubMed Central Google Scholar
Girgis, C. M., Clifton-Bligh, R. J., Hamrick, M. W., Holick, M. F. & Gunton, J. E. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr. Rev. 34 , 33–83 (2013).
Sanders, K. M. et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 303 , 1815–1822 (2010).
Bischoff-Ferrari, H. A. et al. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern. Med. 176 , 175–183 (2016).
Gallagher, J. C. Vitamin D and falls–the dosage conundrum. Nat. Rev. Endocrinol. 12 , 680–684 (2016).
Smith, L. M., Gallagher, J. C. & Suiter, C. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. J. Steroid Biochem. Mol. Biol. 173 , 317–322 (2017).
Michos, E. D. et al. Rationale and design of the Study To Understand Fall Reduction and Vitamin D in You (STURDY): a randomized clinical trial of vitamin D supplement doses for the prevention of falls in older adults. Contemp. Clin. trials 73 , 111–122 (2018).
LeBoff, M. S. et al. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. J. Clin. Endocrinol. Metab. 105 , 2929–2938 (2020).
Cashman, K. D., Ritz, C., Kiely, M. & Odin, C. Improved dietary guidelines for vitamin D: application of individual participant data (IPD)-level meta-regression analyses. Nutrients 9 , 469 (2017).
Bouillon, R. Vitamin D status in Africa is worse than in other continents. Lancet Glob. Health 8 , e20–e21 (2020).
Bischoff-Ferrari, H. A. et al. Effect of vitamin D on falls: a meta-analysis. JAMA 291 , 1999–2006 (2004).
Lange, N. E., Sparrow, D., Vokonas, P. & Litonjua, A. A. Vitamin D deficiency, smoking, and lung function in the Normative Aging Study. Am. J. Respir. Crit. Care Med. 186 , 616–621 (2012).
Janssens, W. et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax 65 , 215–220 (2010).
Maes, K., Serre, J., Mathyssen, C., Janssens, W. & Gayan-Ramirez, G. Targeting vitamin D deficiency to limit exacerbations in respiratory diseases: utopia or strategy with potential? Calcif. Tissue Int. 106 , 76–87 (2020).
Martineau, A. R. et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol. Assess. 23 , 1–44 (2019).
Camargo, C. A. et al. Effect of monthly high-dose vitamin D supplementation on acute respiratory infections in older adults: a randomized controlled trial. Clin. Infect. Dis. 71 , 311–317 (2019).
Chen, F. Y., Xiao, M., Ling, B., Liu, L. & Chen, L. Vitamin D does not improve lung function decline in COPD: a meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 23 , 8637–8644 (2019).
PubMed Google Scholar
Sluyter, J. D. et al. Effect of monthly, high-dose, long-term vitamin D on lung function: a randomized controlled trial. Nutrients 9 , 1353 (2017).
Bassatne, A. et al. The link between COVID-19 and vitamin D (VIVID): a systematic review and meta-analysis. Metabolism 119 , 15475 (2021).
Murai, I. H. et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. JAMA 325 , 1053–1060 (2021).
Entrenas Castillo, M. et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 203 , 105751 (2020).
Amin, H. & Drenos, F. No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data. BMJ Nutr. Prev. Health 4 , 42–48 (2021).
Butler-Laporte, G. et al. Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: a Mendelian randomization study. PLoS Med. 18 , e1003605 (2021).
Li, W. et al. Vitamin D supplementation during pregnancy and the risk of wheezing in offspring: a systematic review and dose-response meta-analysis. J. Asthma 56 , 1266–1273 (2019).
Litonjua, A. A. et al. Six-year follow-up of a trial of antenatal vitamin D for asthma reduction. N. Engl. J. Med. 382 , 525–533 (2020).
Manousaki, D. et al. Vitamin D levels and susceptibility to asthma, elevated immunoglobulin E levels, and atopic dermatitis: a Mendelian randomization study. PLoS Med. 14 , e1002294 (2017).
Murdaca, G. et al. Emerging role of vitamin D in autoimmune diseases: an update on evidence and therapeutic implications. Autoimmun. Rev. 18 , 102350 (2019).
Mokry, L. E. et al. Vitamin D and risk of multiple sclerosis: a mendelian randomization study. PLoS Med. 12 , e1001866 (2015).
Jacobs, B. M., Noyce, A. J., Giovannoni, G. & Dobson, R. BMI and low vitamin D are causal factors for multiple sclerosis: a Mendelian randomization study. Neurol. Neuroimmunol. Neuroinflamm 7 , e662 (2020).
Gianfrancesco, M. A. et al. Evidence for a causal relationship between low vitamin D, high BMI, and pediatric-onset MS. Neurology 88 , 1623–1629 (2017).
Rhead, B. et al. Mendelian randomization shows a causal effect of low vitamin D on multiple sclerosis risk. Neurol. Genet. 2 , e97 (2016).
Bae, S. C. & Lee, Y. H. Vitamin D level and risk of systemic lupus erythematosus and rheumatoid arthritis: a Mendelian randomization. Clin. Rheumatol. 37 , 2415–2421 (2018).
Lund-Nielsen, J. et al. Vitamin D and inflammatory bowel disease: Mendelian randomization analyses in the Copenhagen studies and UK biobank. J. Clin. Endocrinol. Metab. 103 , 3267–3277 (2018).
Manousaki, D. et al. Vitamin D levels and risk of type 1 diabetes: a Mendelian randomization study. PLoS Med. 18 , e1003536 (2021).
Palacios, C., De-Regil, L. M., Lombardo, L. K. & Pena-Rosas, J. P. Vitamin D supplementation during pregnancy: updated meta-analysis on maternal outcomes. J. Steroid Biochem. Mol. Biol. 164 , 148–155 (2016).
Palacios, C., Kostiuk, L. K. & Pena-Rosas, J. P. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 7 , CD008873 (2019).
Roth, D. E. et al. Vitamin D supplementation in pregnancy and lactation and infant growth. N. Engl. J. Med. 379 , 535–546 (2018).
Magnus, M. C. et al. Vitamin D and risk of pregnancy related hypertensive disorders: Mendelian randomisation study. BMJ 361 , k2167 (2018).
Amrein, K. et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 312 , 1520–1530 (2014).
National Heart, L. et al. Early high-dose vitamin D3 for critically ill, vitamin D-deficient patients. N. Engl. J. Med. 381 , 2529–2540 (2019).
Wactawski-Wende, J. et al. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N. Engl. J. Med. 354 , 684–696 (2006).
Smith, H. et al. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women–a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology 46 , 1852–1857 (2007).
Billington, E. O. et al. Effect of high-dose vitamin D supplementation on peripheral arterial calcification: secondary analysis of a randomized controlled trial. Osteoporos. Int. 31 , 2141–2150 (2020).
Durazo-Arvizu, R. A. et al. The reverse J-shaped association between serum total 25-Hydroxyvitamin D concentration and all-cause mortality: the impact of assay standardization. Am. J. Epidemiol. 185 , 720–726 (2017).
Gaksch, M. et al. Vitamin D and mortality: individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLoS ONE 12 , e0170791 (2017).
Mattila, T. et al. Airway obstruction, serum vitamin D and mortality in a 33-year follow-up study. Eur. J. Clin. Nutr. 73 , 1024–1032 (2019).
Zhang, Y. et al. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ 366 , l4673 (2019).
Ordonez-Mena, J. M. et al. Genetic variants in the vitamin D pathway, 25(OH)D levels, and mortality in a large population-based cohort study. J. Clin. Endocrinol. Metab. 102 , 470–477 (2016).
Aspelund, T. et al. Effect of genetically low 25-hydroxyvitamin D on mortality risk: Mendelian randomization analysis in 3 large European cohorts. Nutrients 11 , 74 (2019).
Article CAS PubMed Central Google Scholar
Ong, J. S. et al. Vitamin D and overall cancer risk and cancer mortality: a mendelian randomization study. Hum. Mol. Genet. 27 , 4315–4322 (2018).
CAS PubMed Google Scholar
Bouillon, R. & Bikle, D. Vitamin D metabolism revised: fall of dogmas. J. Bone Miner. Res. 34 , 1985–1992 (2019).
Aatsinki, S. M. et al. Fasting-induced transcription factors repress vitamin D bioactivation, a mechanism for vitamin D deficiency in diabetes. Diabetes 68 , 918–931 (2019).
Roizen, J. D. et al. Obesity decreases hepatic 25-hydroxylase activity causing low serum 25-hydroxyvitamin D. J. Bone Miner. Res. 34 , 1068–1073 (2019).
Atkinson, S. A. Recommendations on vitamin D needs in multiple sclerosis from the MS Society of Canada. Public Health Nutr. 23 , 1278–1279 (2020).
Wang, T. J. et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet 376 , 180–188 (2010).
Wu, H. X. et al. Effects of vitamin D supplementation on the outcomes of patients with pulmonary tuberculosis: a systematic review and meta-analysis. BMC Pulm. Med. 18 , 108 (2018).
Download references
Author information
Authors and affiliations.
Clinical and Experimental Endocrinology, Department of Chronic Diseases and Metabolism, KU Leuven, Leuven, Belgium
Roger Bouillon
Research Center of the Sainte-Justine University Hospital, University of Montreal, Montreal, Quebec, Canada
Despoina Manousaki
Maine Medical Center Research Institute, Scarborough, ME, USA
Cliff Rosen
Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands
Katerina Trajanoska
Translational Skeletal Genomics, Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands
Fernando Rivadeneira
Centre for Clinical Epidemiology, Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, Quebec, Canada
J. Brent Richards
Departments of Medicine, Human Genetics, Epidemiology and Biostatistics, McGill University, Montreal, Quebec, Canada
You can also search for this author in PubMed Google Scholar
Contributions
R.B., D.M. and K.T. researched data for the article. All authors contributed substantially to discussion of the content. R.B. and D.M. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Correspondence to Roger Bouillon .
Ethics declarations
Competing interests.
R.B. received modest speaking or consultancy fees from Fresenius, Abiogen, FAES Farma, Ceres and Proctor and Gamble. J.B.R. has worked as a consultant to GlaxoSmithKline and Deerfield Capital. The other authors declare no competing interests
Additional information
Peer review information.
Nature Reviews Endocrinology thanks D. Bikle, C. Carlberg, G. Jones and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions.
Reprints and permissions
About this article
Cite this article.
Bouillon, R., Manousaki, D., Rosen, C. et al. The health effects of vitamin D supplementation: evidence from human studies. Nat Rev Endocrinol 18 , 96–110 (2022). https://doi.org/10.1038/s41574-021-00593-z
Download citation
Accepted : 25 October 2021
Published : 23 November 2021
Issue Date : February 2022
DOI : https://doi.org/10.1038/s41574-021-00593-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Clinical data mining: challenges, opportunities, and recommendations for translational applications.
- Huimin Qiao
- Yijing Chen
Journal of Translational Medicine (2024)
Longitudinal analysis of vitamin D levels considering sunshine duration and suggestion for a standardised approach for vitamin D supplementation in children and adolescents with obesity
- Katja Wechsung
- Dirk Schnabel
- Susanna Wiegand
BMC Pediatrics (2024)

Association between 25 hydroxyvitamin D and serum uric acid level in the Chinese general population: a cross-sectional study
- Shu-Ting Li
- Yun-Lai Wang
BMC Endocrine Disorders (2024)
Nutritional and metabolic modulation of inflammation in critically ill patients: a narrative review of rationale, evidence and grey areas
- Anne-Françoise Rousseau
- Robert Martindale
Annals of Intensive Care (2024)
Determining the vitamin D supplementation duration to reach an adequate or optimal vitamin D status and its effect on blood lipid profiles: a longitudinal study
- Sakineh Nouri Saeidlou
- Davoud Vahabzadeh
- Fariba Babaei
Journal of Health, Population and Nutrition (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- View PDF
- Download full issue

Journal of Trace Elements in Medicine and Biology
A literature review on beneficial role of vitamins and trace elements: evidence from published clinical studies.
- Previous article in issue
- Next article in issue
Cited by (0)
- Search Close search
- Find a journal
- Search calls for papers
- Journal Suggester
- Open access publishing
We’re here to help
Find guidance on Author Services
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Vitamin D in health and disease: a literature review
Affiliation.
- 1 Center for Genetics and Inherited Diseases, Taibah University, Madinah Al-Munawara, Saudi Arabia. [email protected]
- PMID: 24400428
- DOI: 10.1080/09674845.2013.11669951
Vitamin D, a fat-soluble prohormone, is synthesised in response to sunlight. Vitamin D requires two metabolic conversions, 25-hydroxylation in the liver and 1alpha-hydroxylation in the kidney, to become active hormone. The active form, 1alpha,25-(OH)2D, binds to the vitamin D receptor (VDR) to modulate gene transcription and regulate mineral ion homeostasis. Vitamin D plays several roles in the body, influencing bone health as well as serum calcium and phosphate levels. Furthermore, vitamin D may modify immune function, cell proliferation, differentiation and apoptosis. Vitamin D deficiency has been associated with numerous health outcomes, including risk of rickets in children or osteomalacia in adults, increased risk of fractures, falls, cancer, autoimmune disease, infectious disease, type 1 and type 2 diabetes, hypertension and heart disease, and other diseases such as multiple sclerosis. Here, vitamin D physiology and metabolism, its genomic action and association of polymorphisms in vitamin D pathway genes with different diseases are reviewed by focusing on new findings published in the literature.
PubMed Disclaimer
Similar articles
- Genetic disorders of Vitamin D biosynthesis and degradation. Miller WL. Miller WL. J Steroid Biochem Mol Biol. 2017 Jan;165(Pt A):101-108. doi: 10.1016/j.jsbmb.2016.04.001. Epub 2016 Apr 6. J Steroid Biochem Mol Biol. 2017. PMID: 27060335 Review.
- Cytochrome P450 enzymes in the bioactivation of vitamin D to its hormonal form (review). Wikvall K. Wikvall K. Int J Mol Med. 2001 Feb;7(2):201-9. doi: 10.3892/ijmm.7.2.201. Int J Mol Med. 2001. PMID: 11172626 Review.
- Vitamin D pathway regulatory genes encoding 1α-hydroxylase and 24-hydroxylase are dysregulated in sinonasal tissue during chronic rhinosinusitis. Christensen JM, Cheng J, Earls P, Gunton J, Sewell W, Sacks R, Harvey RJ. Christensen JM, et al. Int Forum Allergy Rhinol. 2017 Feb;7(2):169-176. doi: 10.1002/alr.21852. Epub 2016 Sep 12. Int Forum Allergy Rhinol. 2017. PMID: 27618536
- Vitamin D activities and metabolic bone disease. Ryan JW, Anderson PH, Turner AG, Morris HA. Ryan JW, et al. Clin Chim Acta. 2013 Oct 21;425:148-52. doi: 10.1016/j.cca.2013.07.024. Epub 2013 Jul 30. Clin Chim Acta. 2013. PMID: 23911750 Review.
- Vitamin D status and gene transcription in immune cells. Morán-Auth Y, Penna-Martinez M, Shoghi F, Ramos-Lopez E, Badenhoop K. Morán-Auth Y, et al. J Steroid Biochem Mol Biol. 2013 Jul;136:83-5. doi: 10.1016/j.jsbmb.2013.02.005. Epub 2013 Feb 13. J Steroid Biochem Mol Biol. 2013. PMID: 23416105 Review.
- VDR Gene Polymorphisms ( BsmI , FokI , TaqI , ApaI ) in Total Hip Arthroplasty Outcome Patients. Rozmus D, Fiedorowicz E, Grzybowski R, Płomiński J, Cieślińska A. Rozmus D, et al. Int J Mol Sci. 2024 Jul 27;25(15):8225. doi: 10.3390/ijms25158225. Int J Mol Sci. 2024. PMID: 39125794 Free PMC article.
- Knowledge, attitudes and practices (KAP) of medical university students towards vitamin D deficiency in Saudi Arabia: a cross-sectional study. Elghazaly A, Widyan A, Alsahali S, Alshammari M, Farooqui M, Alsaloom D, Alduwirej L, Alfayizi L, Alajmi M, Alowais M. Elghazaly A, et al. J Pharm Policy Pract. 2024 Aug 5;17(1):2381699. doi: 10.1080/20523211.2024.2381699. eCollection 2024. J Pharm Policy Pract. 2024. PMID: 39109357 Free PMC article.
- Serum vitamin D levels in children with vernal keratoconjunctivitis - A study from a tertiary care pediatric hospital of North India. Wadhwani M, Sharma S, Singh R. Wadhwani M, et al. Indian J Ophthalmol. 2024 Jul 1;72(Suppl 4):S634-S638. doi: 10.4103/IJO.IJO_773_23. Epub 2024 May 20. Indian J Ophthalmol. 2024. PMID: 38770629 Free PMC article. Clinical Trial.
- Vitamin D-The Iceberg in Endometriosis-Review and Meta-Analysis. Ursache A, Lozneanu L, Bujor IE, Mandici CE, Boiculese LV, Bausic AIG, Grigore M, Socolov D, Matasariu DR. Ursache A, et al. J Pers Med. 2024 Jan 20;14(1):119. doi: 10.3390/jpm14010119. J Pers Med. 2024. PMID: 38276241 Free PMC article. Review.
- Single Nucleotide Polymorphisms in the Vitamin D Metabolic Pathway and Their Relationship with High Blood Pressure Risk. Rojo-Tolosa S, Márquez-Pete N, Gálvez-Navas JM, Pineda-Lancheros LE, Fernández-Alonso A, Membrive-Jiménez C, Ramírez-Tortosa MC, Pérez-Ramírez C, Jiménez-Morales A. Rojo-Tolosa S, et al. Int J Mol Sci. 2023 Mar 22;24(6):5974. doi: 10.3390/ijms24065974. Int J Mol Sci. 2023. PMID: 36983047 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, other literature sources.
- scite Smart Citations
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 14, Issue 9
- Efficacy of selenium supplementation for patients with Graves' hyperthyroidism during methimazole treatment: protocol for a systematic review and meta-analysis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Shuo Yuan 1 ,
- Qing Wen 2 ,
- http://orcid.org/0000-0002-9730-1357 Mingxing Li 3
- 1 Department of General Surgery , Beilun Branch of the First Affiliated Hospital of Zhejiang University , Ningbo , China
- 2 Department of Operating Theater , Ningbo Mingzhou Hospital , Ningbo , China
- 3 Department of Pharmacy , Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University , Hangzhou , China
- Correspondence to Dr Mingxing Li; mxlsrrsh18{at}zju.edu.cn ; Dr Shuo Yuan; ys123883076{at}163.com
Introduction The most common cause of hyperthyroidism, Graves' disease is a common organ-specific autoimmune disease. Selenium is an essential trace element of the human body that is mainly concentrated in the thyroid gland and is involved in the synthesis and metabolism of thyroid hormones. Most studies have shown that the level of selenium is closely related to the occurrence and development of thyroid diseases, and selenium supplementation can help improve thyroid function. This study aims to evaluate the efficacy of selenium supplementation for patients with Graves' hyperthyroidism during methimazole treatment.
Methods and analysis We will search the electronic databases including PubMed, Web of Science, Embase, the Cochrane Library, China National Knowledge Infrastructure, Wanfang Data and Chinese Biomedical Literature, and the time was deadline to December 2023. To evaluate the efficacy of methimazole combined with selenium supplementation in the treatment of Graves' hyperthyroidism, randomised controlled trials will be included. The Cochrane Collaboration’s risk of bias tool will be used to assess the quality of all included studies, and the baseline data of all the studies are extracted by the authors. A random-effects model or a fixed-effects model is used to analyse the outcomes. The primary outcomes are the levels of selenium, triiodothyronine, free thyroxine and thyroid-stimulating hormone (TSH), whereas the secondary outcomes include TSH receptor antibody, thyroid peroxidase antibody and thyroglobulin antibody.
Ethics and dissemination Ethics approval is not required since no original data will be collected. The results of this study will be published in a peer-reviewed journal.
PROSPERO registration number CRD42023410999
- Meta-Analysis
- Thyroid disease
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-081302
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This protocol strictly follows the guidelines for systematic review and meta-analysis.
Only randomised controlled trials are included and subgroup analysis is conducted to evaluate the outcomes, which enhances the credibility of the results.
A comprehensive search strategy has been developed to include all eligible studies meeting the inclusion criteria.
Study screening, selection, data extraction and assessment of the risk of bias will be completed by two independent authors.
The search strategy is not restricted by language, which may cause methodological heterogeneity.
Introduction
Known as toxic diffuse goitre, Graves' disease (GD) is an organ-specific autoimmune disease that is caused by an antibody produced by the thyroid-stimulating hormone (TSH) receptor (TSHR) on the cell membrane of the thyroid follicle. 1 The clinical symptoms of GD include diffuse goitre, eye disease or orbital disease, skin disease, tachycardia and hand tremor, high energy, fatigue, weight loss, restless sleep, rapid heartbeat, and anxiety. 2 At present, the pathogenesis of GD has not been fully clarified, but it is generally believed that the occurrence of GD is related to genetic, environmental, immune, sex and other factors, among which the immune factors are the main cause of GD. This immune system disorder is caused by the abnormal metabolism of immune cells. 3 In addition, the TSHR receptor antibody (TRAb) is the main pathogenic antibody of GD, and an excessive amount of the antibody binds with TSHR to stimulate thyroid cell hyperplasia, eventually leading to hyperthyroidism and diffuse goitre. 4 An autoimmune thyroid disease, Graves' hyperthyroidism is a common chronic endocrine and metabolic disease caused by the synthesis and excessive release of thyroid hormone (TH) by the thyroid gland, accounting for approximately 85% of all cases of hyperthyroidism. 5 Relevant statistics from foreign studies has shown that the prevalence rate of Graves’ hyperthyroidism is approximately 1.9% in women and 0.16% in men. 6 Additionally, according to an epidemiological survey in China, the data indicated that the overall incidence rate of hyperthyroidism has reached 3%, with women accounting for approximately 4.1% and men accounting for approximately 1.6% of cases. 7
Currently, the main treatment of Graves' hyperthyroidism includes radioactive iodine 131 ( 131 I), antithyroid drugs (ATDs) and surgery. 8 The purpose of treatment with 131 I is to destroy enough thyroid tissue to treat the disease through the release of β radiation, but this can cause hypothyroidism, which requires lifelong use of TH replacement therapy. 9 ATDs have always been the primary modality of therapy with radioactive iodine and surgical treatment for patients whose medical therapy has failed. The commonly used ATDs include methimazole, propylthiouracil, methylthiouracil, etc. However, their disadvantages such as long treatment cycles, high recurrence rates and low remission rates of goitres, have caused a burden on the psychology of patients seriously affecting their quality of life. Methimazole is a commonly used ATD that can inhibit the activity of thyroid peroxidase, prevent thyroxine from binding to triiodothyronine (FT3), and reduce the level of thyroxine. 10 In addition, methimazole can also reduce the synthesis of antibodies in β lymphocytes, downregulate the level of thyroid-stimulating antibodies, and inhibit the function of T cells and the synthesis of THs. Most studies have shown that methimazole alone has a significant effect on reducing the level of TH, but it has a poor effect on the treatment of Graves' hyperthyroidism. 11 12 The combination of methimazole and other drugs, such as thioureas, β-receptor blockers or antioxidants, can significantly improve thyroid function and reduce adverse reactions, thus improving the effect of the treatment of Graves’ hyperthyroidism. 13 14
Graves’ hyperthyroidism is an autoimmune disease that is usually accompanied by inflammatory reactions and oxidative stress reactions, leading to damage to thyroid function. Selenium is a necessary trace element for the human body that is involved in the synthesis and metabolism of THs. 15 A reduction in selenium levels in the thyroid is an important factor leading to chronic inflammation and abnormal immune function. Under normal physiological conditions, the level of selenium in the body is high. Once the selenium level is reduced, abnormal proteins and enzymes are produced, which leads not only to insufficient elimination of free radicals, but also to a reduction in antioxidant capacity and destruction of thyroid cells, eventually leading to the occurrence of autoimmune reactions. 16 In addition, selenium deficiency causes immune dysfunction in the body, mainly humoral immunity abnormalities, promotes the production of thyroid excitatory antibodies, stimulates the synthesis of THs and ultimately causes hyperthyroidism. 17 Results of double-blind randomised controlled trials (RCTs) have revealed that selenium supplementation significantly reduced the levels of FT3, free thyroxine (FT4) and TSH in patients taking methimazole, but had no significant effect on the recurrence of Graves’ hyperthyroidism. 18 A later study further confirmed that reaching the optimal selenium level could improve the early efficacy of methimazole in the treatment of Graves’ hyperthyroidism. 19 Other studies have found that short-term selenium supplementation has no obvious effect on the adjuvant treatment of Graves' hyperthyroidism in patients with sufficient selenium. However, for patients with selenium deficiency, long-term selenium supplementation is beneficial for the treatment of hyperthyroidism. 20
Although the combination of methimazole and selenium has a significant effect on reducing TH and autoantibody levels, the results of their treatment are still different. To comprehensively evaluate the effects of selenium supplementation on the treatment of Graves’ hyperthyroidism, we conducted this meta-analysis to summarise all the results.
Methods and analysis
This review will be reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. The start date of this study is 31 March 2023 and the end date is 31 October 2024.
Search strategy
We conducted a comprehensive literature search from databases including PubMed, Web of Science, Embase, the Cochrane Library, China National Knowledge Infrastructure, Wanfang Data and Chinese Biomedical Literature, and the time was deadline to December 2023. The search terms used are as follows: ‘Graves' disease or hyperthyroidism or Graves' hyperthyroidism’ AND ‘selenium or selenium supplementation’ AND ‘methimazole’ (without language restrictions). The details of the search strategy used in PubMed are presented in box 1 . The search strategies from other databases are described in the online supplemental materials .
Supplemental material
Details of the search strategies for pubmed.
Search number and search details
#1 ‘graves' disease’((MeSH Terms)) OR ‘hyperthyroidism’(MeSH
Terms) OR ((‘grave’((All Fields)) OR ‘grave s’((All Fields))
OR ‘gravely’((All Fields)) OR ‘graves’((All Fields)) OR
‘graves s’((All Fields))) AND ‘hyperthyroidism’(MeSH
#2 ‘selenium’((MeSH Terms)) OR ‘selenium supplementation’
((MeSH Terms))
#3 ‘methimazole’((MeSH Terms)) OR ‘methimazole’(MeSH
Terms) OR ‘methimazole’((MeSH Terms))
#4 ((#1) AND (#2)) AND (#3)
#5 (#4) AND (randomizedrandomised controlled trials((Publication Type)))
Inclusion and exclusion criteria
Studies will be included in this meta-analysis if they meet the following criteria: (1) All the participants are diagnosed with Graves’ hyperthyroidism, and have no other diseases; (2) All the included studies are RCTs, and evaluate the efficacy of selenium supplementation for patients with Graves’ hyperthyroidism during methimazole treatment; (3) All the full texts are available, and the data are sufficient. Studies will be excluded if they do not meet the above criteria.
Data extraction
The baseline characteristics of all the included studies will be extracted using an Excel table by two reviewers (SY and QW). The extracted information includes the authors, publication year, study type, number of samples, age, course of disease, intervention methods, treatment period and outcomes. The primary outcomes are the levels of selenium, FT3, FT4, TSH, whereas the secondary outcomes include TRAb, thyroid peroxidase antibody, and thyroglobulin antibody. During the process of data extraction, any discrepancies will be resolved through discussion with a third reviewer.
Quality assessment
The methodological quality of all the included studies will be evaluated using the Cochrane risk of bias tool (Cochrane Collaboration). The items include random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective outcome reporting. In addition, a funnel plot is used to assess the publication bias, and all studies are scored with the Jadad Scale, with scores ranging from 0 to 7.
Statistical analysis
All the data analyses will be conducted using RevMan software V.5.4. Heterogeneity between the studies will be evaluated using the I 2 test, and the ranges of the values of I 2 0%–25%, 25%–50% and more than 50%, will be considered to have low, medium and high heterogeneity, respectively, among the studies. In addition, significant heterogeneity will be identified when I 2 ≥25% or the value of p is ≤0.05, and a random-effects model will be used. Otherwise, a fixed-effects model will be applied because of low heterogeneity. For continuous outcomes, all the results will be represented as standard mean differences and 95% CIs. For dichotomous variables, OR and 95% CIs will be used for data synthesis. Furthermore, subgroup analysis will be conducted based on the dosage of selenium, and sensitivity analyses and Begg’s test will be conducted to assess the accuracy of all the results and the potential bias. Significant statistical difference is considered when the value of p<0.05.
Ethics and dissemination
Ethics approval is not required since no original data will be collected. The results of this study will be published in a peer-reviewed journal.
Oxidative stress plays an important role in the occurrence and development of hyperthyroidism, in which a hypermetabolic state typically leads to the release of large amounts of reactive oxygen species (ROS) in peripheral tissues, as has been reported in animal models and human studies of hyperthyroidism. 21 Interestingly, ROS release also occurs in the thyroid gland, causing damage to thyroid epithelial cells, and exposing autoantigens to the immune system, eventually leading to the deterioration of thyroid autoimmunity. 22 In addition, ROS may cause peripheral tissue damage, leading to hyperthyroidism. 23 Previous studies have confirmed that ROS can activate various downstream signalling pathways such as the mitogen-activated protein kinases/extracellular regulated protein kinases (MAPK/ERK), Phosphatidylinositol 3-kinase/protein kinase B(PI3K/AKT) and nuclear factor erythroid-2-related factor 2/heme oxygenase 1(Nrf2/HO-1) pathways, causing abnormal cell proliferation and migration, then leading to thyroid dysfunction; the inhibition of ROS production; the activation of downstream signalling pathways; the promotion of mitochondrial autophagy and ferroptosis; and the alleviation of disease progression. 24–26
Selenium has been recommended for the treatment of thyroid diseases, including GD, Graves’ orbital disease and chronic autoimmune thyroiditis, and the underlying mechanisms are related to antioxidant and immune regulation. 15 Selenoproteins have antioxidant and enzymatic capabilities and are highly expressed in the thyroid gland, affecting the balance of redox activity in cells. 27 Selenium can alleviate ROS-induced oxidative damage and mitochondrial dysfunction, and exerts anti-inflammatory and antitumour effects. 28 In addition, selenoproteins are essential for activated T cells and are involved in the regulation of T cells proliferation in response to T cells receptor stimulation. It has also been reported that selenium supplementation promotes the differentiation of CD 4+ T cells into T helper cell 1 effector rather than T helper cell 2 effector cells. In terms of immune regulation, selenoproteins increase the cytotoxicity and natural killer activity of tumour cells mediated by cytotoxic lymphocytes. 17 Currently, the main dietary sources of selenium are meat, seafood, shellfish, viscera, eggs and grains, but their bioavailability varies by food type. For example, it is low in seafood and high in grains. 29
Previous studies have revealed that the mean serum selenium level is significantly lower in patients with GD than in healthy individuals and that selenium supplementation improved patients’ quality of life and reduced their risk of disease progression. 30 31 In the past, several studies have been conducted to evaluate whether selenium supplementation alone or in mixtures of antioxidant compounds is beneficial to patients with Graves’ hyperthyroidism, in addition to taking ATDs. One study showed that the use of selenium (15 µg/day) supplementation has a better effect on biochemical and clinical control in patients with hyperthyroidism than does the use of methimazole alone. 32 In addition, among patients with hyperthyroidism with selenium deficiency, methimazole combined with selenium can reduce the thyroid level of patients and improve their thyroid activity. 33 However, for patients with sufficient selenium, selenium supplemented with methimazole does not improve thyroid function. 20
Although the combination of methimazole and selenium supplementation has a beneficial effect on reducing TH and autoantibody levels, no high-quality synthesis studies exist. Therefore, we conducted this meta-analysis to evaluate the effects of selenium supplementation on the treatment of Graves’ hyperthyroidism.
Ethics statements
Patient consent for publication.
Not applicable.
- Subekti I ,
- Stocker DJ ,
- Chou EL , et al
- Antonelli A ,
- Ferrari SM ,
- Ragusa F , et al
- Fallahi P ,
- Elia G , et al
- Scappaticcio L ,
- Trimboli P ,
- Keller F , et al
- Cooper DS , et al
- Meng Z , et al
- Shrestha A ,
- Adhikari N ,
- Devkota S , et al
- Teng D , et al
- Amouzegar A
- Amouzegar A ,
- Tohidi M , et al
- Nafrialdi N , et al
- Okosieme OE
- Menconi F ,
- Rotondo Dottore G , et al
- Winther KH ,
- Rayman MP ,
- Bonnema SJ , et al
- Kahaly GJ ,
- Konig J , et al
- Mortara L ,
- Veronesi G , et al
- Bartalena L ,
- Latrofa F ,
- Menconi F , et al
- Jeong JW , et al
- Cai Y , et al
- Zhao M , et al
- Ma C , et al
- Wei J , et al
- Bednarczuk T ,
- Schomburg L
- Gheorghiu ML ,
- Rijntjes E , et al
- Marcocci C ,
- Bartalena L
- Kim BR , et al
- Guerra LN ,
- Ríos de Molina MDC ,
- Miler EA , et al
- Ying H , et al
Contributors This article was put forward by ML. SY and ML designed this study. ML, SY and QW performed the initial experiment and wrote the manuscript. All authors reviewed the manuscript and approved this version of the article, and due care has been taken to ensure the integrity of the work. ML, SY and QW revised the protocol, assisted with study design and will help with the final manuscript. ML is the guarantor and is responsible for the overall content.
Funding This work was supported by the Traditional Chinese Medicine Science and Technology Plan Project of Zhejiang Province (Grant No. 2023ZF124).
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
One Hundred Years of Vitamins-A Success Story of the Natural Sciences
- December 2012

- University of Groningen

- DSM Food Specialities, Delft, Netherlands

- DSM Nutritional Products
- This person is not on ResearchGate, or hasn't claimed this research yet.
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Christina Herzberg
- Moritz Klein

- Gilberto Litta

- FISH SHELLFISH IMMUN
- Shichao Xie
- CHINESE J CATAL

- Caiyan Zheng

- TRENDS FOOD SCI TECH

- Andrea Baschieri
- Zongxin Jin

- Qingshan Zhu
- CHEM ENG RES DES

- Xiaojuan Yu
- Xiaogang Peng

- W. Ni Haworth

- Kenneth J. Carpenter
- H.B.F. Dixon
- B.L. Horecker
- Taizo Matsukawa
- Takeo Iwatsu
- Rudolf Grewe
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Clin Biochem
- v.28(4); 2013 Oct

Vitamin C in Disease Prevention and Cure: An Overview
Shailja chambial.
Department of Biochemistry, All India Institute of Medical Sciences, Jodhpur, 342005 Rajasthan India
Shailendra Dwivedi
Kamla kant shukla, placheril j. john.
Department of Zoology, Centre for Advanced Studies, University of Rajasthan, Jaipur, 302004 India
Praveen Sharma
The recognition of vitamin C is associated with a history of an unrelenting search for the cause of the ancient haemorrhagic disease scurvy. Isolated in 1928, vitamin C is essential for the development and maintenance of connective tissues. It plays an important role in bone formation, wound healing and the maintenance of healthy gums. Vitamin C plays an important role in a number of metabolic functions including the activation of the B vitamin, folic acid, the conversion of cholesterol to bile acids and the conversion of the amino acid, tryptophan, to the neurotransmitter, serotonin. It is an antioxidant that protects body from free radical damage. It is used as therapeutic agent in many diseases and disorders. Vitamin C protects the immune system, reduces the severity of allergic reactions and helps to fight off infections. However the significance and beneficial effect of vitamin C in respect to human disease such as cancer, atherosclerosis, diabetes, neurodegenerative disease and metal toxicity however remains equivocal. Thus further continuous uninterrupted efforts may open new vistas to understand its significance in disease management.
Introduction
Vitamins are essential nutrients that are required for various biochemical and physiological processes in the body. It is well known that most of the vitamins cannot be synthesized in the body and hence their supplementation in diet is essential. Vitamins are classified on the basis of their solubility as water soluble (C and B complexes) and fat soluble vitamins (A, D, E, K). Vitamin C or ascorbic acid (AA) was first isolated in 1923 by Hungarian biochemist and Nobel laureate Szent-Gyorgyi and synthesized by Howarth and Hirst [ 1 ]. It exists in reduced [ascorbate] and oxidized forms as dehydroascorbic acid which are easily inter-convertible and biologically active thus it acts as important antioxidant. Vitamin C is easily oxidized acid and destroyed by oxygen, alkali and high temperature. Most of the plant and animal species have the ability to synthesize vitamin C from glucose and galactose through uronic acid pathway but man and other primates cannot do so because of deficiency of enzyme gulonolactone oxidase [EC 1.1.3.8] required for it’s biosynthesis. Deficiency of this enzyme is a result of a mutation which occurred approximately 40 million years ago [ 2 ].
The body requires vitamin C for normal physiological functions. It helps in the synthesis and metabolism of tyrosine, folic acid and tryptophan, hydroxylation of glycine, proline, lysine carnitine and catecholamine. It facilitates the conversion of cholesterol into bile acids and hence lowers blood cholesterol levels. It also increases the absorption of iron in the gut by reducing ferric to ferrous state. As an antioxidant, it protects the body from various deleterious effects of free radicals, pollutants and toxins. The therapeutic effect of vitamin C was explored by Linus Pauling however his work on therapeutic role of vitamin C in his later years generated much controversy yet he was the first to introduce the concept of high doses of vitamin C for the treatment of various conditions from common cold to cancer [ 3 ]. Since then mega doses of vitamin C have been widely used in the treatment and prevention of a large number of disorders like diabetes, atherosclerosis, common cold, cataracts, glaucoma, macular degeneration, stroke, heart diseases, cancer and so on.
Deficiency of this vitamin is often associated with anemia, infections, bleeding gums, scurvy, poor wound healing, capillary haemorrhage, muscle degeneration, atherosclerotic plaques and neurotic disturbances. For the correction of deficiency, vitamin C is often supplemented in large doses and unlike fat soluble vitamins, toxicity is rare. Recently the role of vitamin C in infection and immunity has also been investigated. In view of the vast biological, physiological functions and therapeutic role of vitamin C, this review is an attempt to summarise various evidences in this context.
Dietary Sources of Vitamin C
Vitamin C is found in citrus fruits, green peppers, red peppers, strawberries, tomatoes, broccoli, brussels sprouts, turnip, Indian gooseberry and other leafy vegetables. The animal sources are poor in vitamin C content and the level is usually <30–40 mg/100 g. Therefore plant sources become important because of high content of vitamin C up to 5,000 mg/100 g. It’s absorption in the buccal cavity is by passive diffusion however in gastrointestinal tract absorption is by active sodium dependent vitamin C transporters (SVCT) [ 4 , 5 ].
Vitamin C Bioavailability
Bioavailability or the effective concentration of vitamin C essentially depends on its effective absorption from intestine and renal excretion. Vitamin C, consumed either with diet or dietary supplements, is absorbed by the epithelial cells of the small intestine by SVCT1 or, subsequently diffuses into the surrounding capillaries and then the circulatory system [ 5 – 7 ]. Circulating AA is filtered from kidney capillary bed into the Bowman’s capsule through a general filtration mechanism. AA is reabsorbed through SVCT1 transporter in proximal convoluted tubule [ 6 ]. The difference between the amount of AA filtered and reabsorbed constitutes renal excretion [ 8 ]. Together, intestinal absorption and renal excretion controls the serum level of vitamin C and thus its bioavailability. At low concentrations, most vitamin C is absorbed in the small intestine and reabsorbed from the renal tubule [ 9 ]. However, at high concentrations, SVCT1 is down regulated [ 10 ] which limits the amount of AA absorbed from the intestine and kidney [ 11 ]. This imposes a physiological restriction on the maximal effective serum vitamin C concentration (or its bioavailability) that is attainable by oral consumption [ 12 ]. This value has been determined to be 200 mmol/L [ 12 ], although “normal” physiological serum concentrations of ascorbate in healthy humans range from 60 to 100 mmol/L [ 13 ]. Vitamin C levels in circulating blood cells, such as platelets, are much higher than the plasma [ 13 ], as these cells express the SVCT2 transporter [ 14 ], which mediates intracellular ascorbate accumulation [ 15 ].
Reduced bioavailability of vitamin C is often seen in stress, alcohol intake, smoking, fever, viral illnesses, usage of antibiotics, pain killers, exposure to petroleum products or carbon monoxide, heavy metals toxicity and so on. However, the precise mechanism behind low vitamin C level in the body is not well defined. Presumably, an increased utilization of this vitamin in these conditions and/or a decreased absorption from the gut could be a cause of decreased vitamin C level [ 16 ]. In the event of high consumption, AA and its metabolites such as dehydroascorbic acid, 2,3-diketogulonic acid and oxalic acid are excreted via kidney in humans. AA is generally non-toxic but at high doses (2–6 g/day) it can cause gastrointestinal disturbances or diarrhoea [ 17 , 18 ]. The side effects are generally not serious and can be easily reversed by reducing the intake of AA. Furthermore, there is no consistent and compelling data on serious health effects of vitamin C in humans [ 18 , 19 ].
Biochemical Functions of Vitamin C
The biochemical functions of AA are largely dependent on the oxido-reduction properties of l -AA which is a co-factor for hydroxylation and activity of mono-oxygenase enzymes in the synthesis of collagen, carnitine and neurotransmitters [ 20 ]. AA accelerates hydroxylation reactions by maintaining the active centre of metal ions in a reduced state for optimal activity of enzymes hydroxylase and oxygenase. Thus, it is crucial in the maintenance of collagen which represents about one-third of the total body protein. In an experimental study AA has been shown to have involvement in synthesis and release of type IV collagen into the culture medium [ 21 ]. Further, it has also been reported that AA 2-phosphate, a long-acting vitamin C derivative, stimulates both cell growth and the expression of mRNA for type III collagen in human osteoblast-like MG-63 cells and in normal human osteoblasts, as well as in human bone marrow mesenchymal stem cells, but not the expression of type I collagen in these cells [ 22 ]. However, in another study Kishimoto et al. [ 23 ] have observed that AA induced the expression of type 1 and type 4 collagen and SVCT2 in cultured human skin fibroblasts. Collagen constitutes the principal protein of skin, bones, teeth, cartilage, tendons, blood vessels, heart valves, inter vertebral discs, cornea, eye lens. AA is essential to maintain the enzyme prolyl and lysyl hydroxylase in an active form. AA deficiency results in reduced hydroxylation of proline and lysine, thus affecting collagen synthesis. AA is also an essential co-factor for hydroxylations involved in the synthesis of muscle carnitine “β-hydroxybutyric acid” [ 24 , 25 ]. Carnitine is required for the transport and transfer of long chain fatty acids into mitochondria for energy production. Further, AA is also a co-factor for the enzyme dopamine-β-hydroxylase, which catalyzes the conversion of neurotransmitter dopamine to norepinephrine [ 19 ] and hence essential for the synthesis of catecholamines. In addition, AA catalyzes other enzymatic reactions involving amidation necessary for maximal activity of hormones oxytocin, vasopressin, cholecystokinin and alpha-melanotropin [ 26 ]. It is also involved in the transformation of cholesterol to bile acids as it modulates the microsomal 7α-hydroxylation, the rate limiting reaction of cholesterol catabolism in liver [ 27 ]. Deficiency of AA affects this conversion and as a result cholesterol accumulates in the liver leading to hypercholesterolemia [ 28 , 29 ], cholesterol gall stones formation etc [ 30 , 31 ].
Vitamin C and Common Cold
Apart from the well accepted role of vitamin C in the prevention of scurvy, the most widely known health beneficial effect of AA is in the prevention and relief of common cold. Pauling was the first to introduce the concept of high dose of vitamin C and suggested that ingestion of 1–3 g of AA effectively prevents/ameliorates common cold [ 32 ]. The role of oral vitamin C in the prevention and treatment of cold however remains controversial despite many controlled studies [ 33 ]. A number of clinical trials with varying doses of AA showed that it does not have significant prophylactic effect, but reduces the severity and duration of symptoms of cold during the period of infection. Randomized and non-randomized trials on role of vitamin C in prevention and treatment of the common cold indicated that AA in dose of 1 g/day during severe winter months produced no beneficial effect on the incidences of common cold [ 34 ]. In both preventive and therapeutic trials, there was a consistent beneficial but generally modest therapeutic effect on the duration of cold symptoms. There was no clear indication of the relative benefits of different regimes of vitamin C doses. However, in trials that tested vitamin C after cold symptoms occurred, there was some evidence of greater benefits with larger doses than with lower doses [ 34 , 35 ]. Attenuation of immunity in common cold is well known. There has been a continuous debate about the role of AA in boosting immunity during rhinitis. AA has been shown to stimulate immune system by enhancing T-cell proliferation in response to infection. These cells are capable of lysing infected targets by producing large quantities of cytokines and by helping B cells to synthesize immunoglobulins to control inflammatory reactions. Further, it has been shown that AA blocks pathways that lead to apoptosis of T-cells and thus stimulate or maintain T-cell proliferation to attack the infection. This mechanism has been proposed for the enhanced immune response observed after administration of vitamin C during rhinitis [ 36 , 37 ].
Vitamin C and Tissue Healing
It is also fairly understood that wound healing requires synthesis and accumulation of collagen and subsequent cross-linking of the fibre to give new tensile strength to the damaged tissue. An early study demonstrated that maximum tensile strength of scar tissue in guinea pig was achieved after supplementation of vitamin C [ 38 ]. Since then various studies have been carried out to evaluate the role of AA in wound repair and healing/regeneration process as it stimulates collagen synthesis. Adequate supplies of AA are necessary for normal healing process especially for post-operative patients because there is rapid utilization of AA for the synthesis of collagen at the site of wound/burns during post-operative period hence, administration of 500 mg to 1.0 g/day of AA are recommended to accelerate the healing process [ 39 ]. Of late, Jagetia et al. [ 40 ] demonstrated that AA pre-treatment was beneficial in healing of irradiated wounds and suggested a vitamin C related therapeutic strategy to accelerate wound repair in such conditions and in the cases of combined injury situation.
Vitamin C and Iron
AA is known to enhance the availability and absorption of iron from non-heme iron sources [ 41 ]. It’s supplementation is found to facilitate the dietary absorption of iron. The reduction of iron by AA has been suggested to increase dietary absorption of non-heme iron [ 42 , 43 ]. Vitamin C rich fruits such as goose berry has been reported to increase the bioavailability of iron from staple cereals and pulses [ 44 ]. Recent observations are of the view that vitamin C inhibits the expression of hepcidin and by affecting erythropoietin receptor in HepG2 cells and the bioavailability of iron provides protection against anaemia due to iron deficiency [ 45 ]. Darius Lane et al. [ 46 ], has considered ascorbate as a novel modulator for the classical transferrin Fe + uptake pathway, acting through intracellular reductive mechanism. It is also well known that AA acts as a pro-oxidant in invitro in the presence of redox-active iron and might contribute to the formation of hydroxyl radical, which eventually may lead to lipid, DNA or protein oxidation [ 47 ]. Thus vitamin C supplementation in individuals with high iron and or bleomycin detectable iron in some preterm infants could be deleterious due to the production of oxidatively damaged molecules [ 48 – 51 ]. However, Proteggente et al. [ 52 ] have observed no pro-oxidant effect of AA supplementation on DNA damage in presence or absence of iron.
Vitamin C and Fertility
Vitamin C has been used in the management of male infertility on empirical grounds, particularly in the presence of non-specific seminal infections [ 53 ]. It’s presence in the seminal plasma of healthy adults in high concentration, ranging from 2.5 to 12 mg/dL, has been reported by various authors [ 54 , 55 ]. However, the precise role of vitamin C in relation to male reproduction is not yet clear. Chinoy [ 56 ] stated that AA was essential for the structural and functional integrity of androgen-dependent reproductive organs. Low concentration of vitamin C showed marked degenerative changes in the testes, epididymis and vas deferens of scorbutic guinea pigs [ 57 ]. Besides degeneration of the spermatogenic epithelium, steroidogenesis and plasma testosterone level also showed a decline [ 58 ]. On the other hand, excessive intake of vitamin C has been reported to cause reproductive failure in the males [ 59 ]. However, Sapra et al. [ 60 ] could not observe any definite effect of vitamin C supplementation on Leydig cells in guinea pigs. AA as the principle antioxidant in seminal plasma of fertile men, contributes up to 65 % of its total chain breaking antioxidant capacity [ 61 ]. It’s concentration in seminal plasma is almost ten times higher than plasma concentration. In various studies AA content in seminal plasma of fertile and infertile men was found to be significantly different [ 62 , 63 ] and the percentage of sperm with normal morphology correlated significantly with seminal AA in both the groups [ 63 – 65 ]. AA deficiency may lead to an increase in oxidative damage induced by reactive oxygen species (ROS) and increased ROS was observed in the semen of 25–45 % of infertile men [ 66 ]. This is further corroborated by association of decreased AA with increase seminal plasma lipid peroxidation as observed in human trial [ 67 ]. Others have also observed oxidative stress induced deleterious effect on male fertility [ 68 , 69 ]. Increased free radicals in the seminal plasma of infertile subjects by lowering the effective vitamin C levels may potentiate the deleterious effects that result in abnormal sperm parameters [ 70 , 71 ]. Further studies report that supplementation of AA leads to significant reduction in ROS concentration [ 72 , 73 ], sperm membrane lipid per-oxidation [ 73 ] and sperm DNA oxidation [ 74 ] and increased sperm quality [ 72 – 74 ]. The results of a recent animal experimental study indicated that, vitamin C improves antioxidant enzymes activity and significantly reduce MDA in testis compared with the test group [ 75 ]. Vitamin C supplementation as antioxidant in dose dependent manner in men may improve sperm quality [ 76 ]. It’s supplementation also increases progesterone levels in infertile women with luteal phase defect [ 77 ].
Vitamin C and Atherosclerosis
There are several publications on the role of vitamin C in lipid metabolism and atherogenesis with diverse observations. The significance of dietary inadequacy of vitamin C in the aetiology of dyslipidemia and atherosclerosis first became apparent from the clinical studies of Myasnikova in 1947. The study showed lowering of cholesterol level by administration of AA in the hypercholesterolemic patients [ 78 ]. Since then several authors have also persuaded similar studies. One reviewed the evidence for the role of vitamin C in bile acid synthesis [ 27 ] while others gave particular emphasis on the potential involvement of vitamin C in pathogenesis of atherosclerosis [ 79 , 80 ]. There are reports indicating increase in total body cholesterol and hypercholesterolemia in acutely scorbutic guinea pigs. However, some studies could not observe any effect of vitamin C in similar animal models [ 81 ]. Das et al. [ 82 ] observed that administration of AA lowers blood cholesterol, triglycerides, lipid per-oxidation and increases HDL cholesterol. Most of the earlier studies were conducted using rabbit as an animal model for examining vitamin C deficiency. As such rabbit is not a suitable model for such studies as it can synthesize AA unlike higher primates and human beings. It is difficult to elicit vitamin C deficiency in animal models. In view of the conflicting observations based on the acutely scorbutic animal model chosen by most of the workers, Ginter et al. [ 83 ] designed a model of chronic latent vitamin C deficiency in guinea pigs. This model in contrast to others, enabled the effect of AA deficiency on lipid metabolism and atherosclerosis to be followed in long term experiments. In protracted hypovitaminosis C lasting for 10 weeks, there was a considerable accumulation of cholesterol in liver and also increased concentration in serum [ 83 – 85 ].
It was also reported that the deficiency of vitamin C leads to enhanced accumulation of cholesterol in thoracic aorta along with pathomorphological changes in blood vessels [ 83 , 86 , 87 ]. Various human trials have also indicated vitamin C induced reduction in blood lipid levels in normal and hypercholesterolemic subjects [ 88 , 89 ]. Marc and Kothari and Sharma have further observed that vitamin C administration causes significant reduction in LDL and increase in HDL [ 87 ] and there by provides protection against CAD [ 87 , 90 ]. Similar observations have been given by others also [ 91 – 96 ]. Chronic AA deficiency in man can lead to impaired cholesterol metabolism resulting in atheromatous changes in the vascular system [ 87 ]. This is further supported by the observation that vitamin C lowers cholesterol [ 88 ] and reduces the risk of developing cardiovascular disease (CHD) [ 97 , 98 ]. Numerous studies have also looked into the association between AA intake and blood lipids. A large prospective epidemiological study in Finnish men and women suggested that high intake of AA was associated with a reduced risk of death from CHD in women than in men [ 98 ]. Similarly, several other studies showed that high intake of AA in American men and women appeared to benefit only women [ 97 , 99 ]. Yet, another cohort study suggested that cardiovascular mortality was reduced in both sexes by vitamin C [ 100 ]. It is likely that cholesterol lowering effect of vitamin C is affected by several factors like initial cholesterol levels, age and sex of the subjects, dose and mode of the administration. The influence of age may be important because SAA levels have been found to be lower in elderly as compared to adolescents [ 101 , 102 ] and therefore elderly subjects could be more responsive to the administration of vitamin C. In UK, a study showed that the risk of stroke in those with highest intake of vitamin C was only half that of subjects with the lowest intake. No evidence is suggestive of lower rate of CHD in those with high vitamin C intake [ 103 ]. A recent meta-analysis study on the role of AA and antioxidant vitamins also showed no evidence of significant benefit in prevention of CHD [ 104 ]. Thus, no conclusive evidence is available on the possible protective effect of AA supplementation on CHD.
Increased attention is being paid to involvement of low density lipoprotein (LDL) in atherogenesis. There are reports indicating that lipid peroxidation and oxidative modification of LDL are implicated in development of atherosclerosis [ 105 ]. Vitamin C provides protection against oxidative changes in LDL in different types of oxidative stress including metal induced oxidative stress [ 106 ]. Addition of iron to plasma devoid of AA resulted in lipid peroxidation, whereas endogenous and exogenous AA was found to inhibit the lipid oxidation in iron-over loaded human plasma [ 107 ]. In an invitro study, when AA was added to human serum supplemented with Cu 2+ , antioxidant activity were observed rather than pro-oxidant effects [ 108 ]. AA is known as important antioxidant that scavenges free radicals and thus primarily prevents the oxidation of LDL in aqueous medium [ 109 ]. In addition, invitro studies have also shown that AA strongly inhibits LDL oxidation by vascular endothelial cells at physiological concentrations [ 110 – 112 ]. An important factor that initiates atherosclerosis is the adhesion of leukocytes to the endothelium. Invivo studies have shown that AA inhibits leukocyte-endothelial cell interactions induced by cigarette smoke [ 113 , 114 ] or oxidized LDL [ 115 ]. Further, lipophilic derivatives of AA showed protective effect on lipid-peroxide induced endothelial injury [ 116 ]. In endothelial cells, AA prevented atherogenic modification of mildly oxidized LDL [ 110 ] and preserved α-tocopherol in both cells and LDL [ 117 ]. Although AA may not reverse established atherosclerosis, it can prevent the endothelial dysfunction that is the earliest sign of many vascular inflammatory conditions. AA is responsible for increased endothelial cell proliferation and also checks tumour necrosis factor (TNF) alpha induced endothelial cell growth inhibition. Vitamin C as antioxidant helps in endothelial cell proliferation and also correlated with expression of collagen IV in endothelial cells. Study has also shown that when proliferating endothelial cells were treated with AA, increased retinoblastoma protein (Rb) phosphorylation was observed with decreased level of p53 as compared to untreated cells. Furthermore, the addition of AA to TNF-alpha-treated proliferating endothelial cells blocked both the inhibition of retinoblastoma protein phosphorylation and enhanced p53 expression induced by TNF-alpha and TNF-alpha-induced apoptosis [ 117 ].
A number of studies were carried out in humans to determine the protective effect of AA supplementation (500–100 mg/day) on invivo and exvivo lipid peroxidation in healthy individuals and smokers with inconclusive findings. AA supplementation showed reduction or no change in lipid peroxidation products [ 111 , 118 – 122 ]. There are reports where vitamin C has been found to decrease LDL peroxidation even in passive smokers [ 123 ]. In this context, it is important to note that during exvivo LDL oxidation, AA is removed at initial stage of LDL isolation from plasma therefore, no change in exvivo appears [ 124 ]. May and Li, examined the role of vitamin C in oxidation of LDL which causes endothelial dysfunction, an important early manifestation of atherosclerosis. They observed that up-regulation of endothelial cell SVCT2 expression and function may help to maintain intracellular ascorbate during oxLDL-induced oxidative stress, and that ascorbate in turn can prevent this effect [ 125 ]. Overall, both invitro and invivo experiments showed that AA protects isolated LDL and plasma lipid peroxidation induced by various radicals or oxidants generating systems. However, there are reports in experimental animals that large doses of exogenous iron and AA promote the release of iron from iron binding proteins and also enhance invitro lipid peroxidation in serum. This finding supports the hypothesis that high intake of iron along with AA could increase invivo lipid peroxidation of LDL and therefore could increase risk of atherosclerosis [ 126 ]. However, Chen et al. [ 127 ], demonstrated that ascorbic acts as an anti-oxidant towards lipids even in presence of iron load invivo systems. Vitamin C also helps in prevention of atherosclerosis by strengthening the artery walls through its participation in the synthesis of collagen and by preventing the undesirable adhesion of white blood cells to damaged arteries [ 128 – 132 ].
Vitamin C and Cancer
The notion that vitamin C may have a preventive role in cancer was first proposed in 1949. It was demonstrated by Cameron et al. [ 133 – 135 ], that high-dose vitamin C improved the survival of patients with terminal cancer. However, the first documented study in which vitamin C was administered to cancer patients was carried out in the 1970s, by Pauling and Cameron. They gave 10 g (10,000 mg) of vitamin C per day to 100 terminally ill cancer patients and compared their outcome with 1,000 cancer patients who were given conventional therapy. It was observed that 10.3 % cancer patients receiving vitamin C survived while all patients on conventional therapy without vitamin C died [ 134 ]. Other studies have also confirmed these findings. Murata and Morishige showed in a study conducted on Japanese patients with uterus cancer receiving 5–30 g of vitamin C that these patients survived six times longer than those on vitamin C <4 g per day. When comparison was made between those supplemented with or without vitamin C, survival rate was 15 % higher in those supplemented with vitamin C [ 136 ]. The overwhelming evidence supports that a high intake of vitamin C is linked with a low risk for cancer of oesophagus, oral cavity, stomach, pancreas, cervix, rectum and breast [ 137 , 138 ] and also non-hormonal cancers [ 139 ]. One of the most important amenable determinants of cancer risk is diet. Several research panels and committees have independently concluded that high fruit and vegetable intake reduces the risk of different types of cancer [ 140 , 141 ] and mortality rate was also found to be inversely related to vitamin C intake [ 142 , 143 ]. However a study involving 34,000 post-menopausal women, reported no such association between the intake of vitamins A, C and E and a reduced risk of developing breast cancer [ 144 ]. Intravenous vitamin C has also been reported to have beneficial effect in advanced cancer [ 145 ]. Several mechanisms proposed indicating involvement of vitamin C in the treatment and prevention of cancer are: enhancing the immune system; stimulating the formation of collagen; preventing metastasis (spreading) by inhibiting enzymes; preventing viruses that can cause cancer; correction of vitamin C deficiency which is often associated with cancer patients; wound healing in cancer patients after surgery; enhancing the effectiveness of chemotherapy; reducing the toxicity of chemotherapy; preventing free radical damages and neutralising some carcinogens [ 146 ].
Recently a number of experimental studies have observed that different types of cancer cells either do not grow at high vitamin C concentration or it leads to tumour shrinkage [ 147 , 148 ]. Further recent experimental studies have also found that ascorbate supplementation hinders metastasis, tumour growth and inflammatory cytokine secretion as well as enhanced encapsulation of tumours in Gulo KO mice [ 149 , 150 ]. Reports have shown that intravenous injection increases vitamin C concentration more than 70 times in relation to oral administration and effectiveness of treatment is linked to vitamin C concentration [ 12 , 145 ]. Thus controversy is because of mode, dose and duration of administration.
Newly available pharmacokinetic data improved the understanding of the regulation of vitamin C transport, and the growing evidence on the therapeutic efficacy of vitamin C. This has stimulated interest to reassess the feasibility of using vitamin C in the prevention and treatment of cancer. Though different in their methodologies, most recent studies on vitamin C and cancer have two central themes:(1) the effects of high-dose AA on the development and progression of tumours; and (2) the mechanisms of action that may contribute to the anti-cancer effect [ 144 ]. Research has also refocused on the implications and applicability of high i.v. dose of vitamin C in cancer therapy. In contrast to normal physiological concentration of AA (0.1 mmol/L) pharmacological concentrations of AA (0.3–20 mmol/L) selectively targets and kills tumour cells in invitro. This tumour-killing phenomenon is attributable to the pro-oxidant property of vitamin C, which, at high concentration mediates the production of hydrogen peroxide thus provides a potential mechanism of action for the anti-tumour effect of vitamin C and it’s implication as a pro-drug in cancer treatment [ 145 , 147 ]. However, it is difficult to assess the precise contribution of vitamin C in the clinical outcome, as subjects under examination simultaneously receive different therapeutic treatments [ 151 ]. Therefore, the therapeutic value of high-dose vitamin C administration in cancer progression or remission is not unequivocally supported but i.v. administration of vitamin C in high doses improves the health-related quality of life even at the advanced stage of the disease [ 152 ].
Vitamin C and Diabetes
Diabetes is becoming a pandemic and numbers are expected to rise to 366 million (4.4 % of the global population) by 2030 [ 153 ]. In diabetic patients, long-term damage, dysfunction, and failure of different organs, especially the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), nerves (diabetic neuropathy), heart (myocardial infarction), and blood vessels (atherosclerosis) are related to uncontrolled hyperglycaemia [ 154 – 156 ]. Hyperglycaemia induces oxidative stress [ 157 ] primarily by ROS [ 18 ]. There is convincing experimental and clinical evidence that the generation of ROS increases in both types of diabetes and that the onset of diabetes is closely associated with oxidative stress [ 158 ]. Vitamin C has been associated with decreased risk of developing diabetes mellitus (DM). In Norfolk Prospective Study the association between fruit and vegetable intake and plasma levels of vitamin C and risk of type 2 DM was established [ 159 ]. During 12-years of follow-up, 735 incident cases of diabetes were identified among nearly 21,000 participants. A significant inverse association was found between plasma levels of vitamin C and risk of diabetes (odds ratio = 0.38, 95 % confidence interval: 0.28–0.52) [ 159 ]. This is further supported by a study with longer follow up of 23 years which reported that antioxidants induced risk reduction of type 2 diabetes [ 160 ] and vitamin C level was found to be significantly lower in both insulin dependent and non dependent diabetes [ 161 , 162 ]. Vitamin C reduces fasting and postprandial oxidative stress [ 163 ]. Sharma et al. have observed reduced vitamin C levels in diabetic subjects. They further reported that vitamin C level is also associated with various components of metabolic syndrome and with the increment in component there is a sharp reduction in vitamin C level [ 164 ]. In recent experimental studies it has been found that Vitamin C and E supplementation relieves oxidative stress in the blood and tissues of diabetic aged rats by modulating the antioxidant system and lipid profile [ 165 , 166 ].
Diabetes is associated with various micro vascular and macro vascular complications. Hyperglycaemia in diabetes is responsible for micro vascular ROS generation which causes endothelial dysfunction [ 167 ] and vitamin C blocks acute hyperglycaemic impairment of endothelial function in diabetic subjects [ 168 ]. One of the most important micro vascular complications is diabetic nephropathy. According to statistical prediction, out of 30 million patients with diabetes in India, diabetic nephropathy is expected to develop in 6.66 million [ 169 ]. Qin et al. [ 170 ] reported that vitamin C supplementation significantly decreased podocyte injury in diabetic rats. Perhaps AA protects podocyte by increasing antioxidative capacity and ameliorating the renal oxidative stress [ 171 ]. The role of vitamin C in diabetic retinopathy has also been reported in various studies. Vitamin C and E supplementation reduces neovascularization, prevent the inhibition of retinal glutathione reductase, glutathione peroxidase and superoxide dismutase activities; hence vitamin C and E prevent oxidative stress induced retinopathy [ 172 – 174 ]. Neuropathy is also one of the micro vascular complications often manifested in uncontrolled DM. Some studies report that the role of vitamin C in diabetic neuropathy is not as well pronounced as other antioxidants [ 175 ]. Some suggest that the AA levels are significantly low in diabetic polyneuropathy patients [ 176 ]. Role of vitamin C and other dietary antioxidants have been reviewed by several authors with controversial findings [ 177 ].
Vitamin C and Immunity
Vitamin C affects several components of the human immune system. Vitamin C appears to play a role in a number of neutrophil functions including increased chemotaxis, increased particulate ingestion, enhanced lysozyme-mediated non-oxidative killing, protection against the toxic effects of superoxide anion radical, inhibition of the halide-peroxide-myeloperoxidase system without a pronounced bactericidal effect, and stimulation of the hexose monophosphate shunt [ 178 ].
The role of vitamin C seems to be more pronounced in cell mediated response instead of humoral immunity as the T-cell hyporesponsiveness was observed to be reversed in Crohn’s disease patients on oral supplementation of vitamin C. In the same study no effect was observed on humoral immunity [ 179 ]. Another study supports the fact that vitamin C acts with other micronutrients synergistically and enhances skin barrier function as well as protective activities of immune cells but its role in antibody protection is not as pronounced [ 180 ]. On the contrary animal studies support the role of supplementation of vitamin C in humoral immunity as it increases serum levels of antibodies [ 181 ] and C1q complement proteins [ 182 ] in guinea pigs, which cannot synthesize vitamin C like humans and hence depend on dietary supplementation. Vitamin C along with other micronutrients help in reverting potential damage caused by free radicals at cellular level and modulates immune cell functions through regulation of redox-sensitive transcription factors and affects production of cytokines and prostaglandins. Adequate intake of vitamins C along with other vitamins and micronutrients like B 6 , folate, B 12 , E, selenium, zinc, copper, and iron supports a Th1 cytokine-mediated immune response [ 183 , 184 ] with sufficient production of proinflammatory cytokines, which maintain an effective immune response. Supplementation with these micronutrients reverses the Th2 cell-mediated immune response to Th1 cytokine-regulated response with enhanced innate immunity [ 183 ].
Vitamin C inhibits the excessive activation of the immune system to prevent tissue damage. It also supports antibacterial activity, stimulates natural killer (NK) cells and differentiation of Th0 subset into Th1 subset [ 184 , 185 ]. In addition, vitamin C also modulates synthesis of proinflammatory cytokines, or expression of adhesive molecules [ 185 ].
Mikirova et al. [ 186 ] have demonstrated that intravenous vitamin C treatment reduces pro-inflammatory cytokines IL-1α, IL-2, IL-8, TNF-α, chemokine eotaxin and CRP in cancer patients. Several studies have shown that the modulation of inflammation by intravenous vitamin C correlated with decrease in tumour marker levels [ 186 – 188 ]. Studies conducted on human subjects reported that that plasma vitamin C and dietary intakes of vitamin C are inversely associated with some markers of the acute phase response and haemostasis that have been associated with greater risk of CVD and non-vascular disease. Plasma vitamin C, fruit intake, and dietary vitamin C intake were significantly and inversely associated with mean concentrations of C-reactive protein, an acute phase reactant, and tissue plasminogen activator antigen, a marker of endothelial dysfunction, even after adjustment for confounders. The findings suggest that vitamin C has anti-inflammatory effects and is associated with lower endothelial dysfunction in men with no history of CHD or diabetes [ 189 – 196 ]. Vitamin C concentrations in the plasma and leukocytes rapidly decline during infections and stress. Supplementation of vitamin C has been shown to improve components of the human immune system such as antimicrobial and NK cell activities, lymphocyte proliferation, chemotaxis, and delayed-type hypersensitivity as discussed above. Vitamin C contributes in maintenance of the redox integrity of cells and thereby protects them against ROS generated during the respiratory burst and in the inflammatory response [ 197 ].
Thus, vitamin C has diverse role as an antioxidant protecting the immune cells against intracellular ROS production during inflammatory response, acting as an enzymatic cofactor and maintaining tissue integrity and plays a crucial role in formation of skin, epithelial and endothelial barriers [ 185 ]. Of late vitamin C supplementation has been found to be beneficial in various inflammatory conditions.
Vitamin C and Heavy Metal Toxicity
Metals including iron, copper, chromium, and vanadium undergo redox cycling, while cadmium, mercury, and nickel, as well as lead deplete glutathione and protein-bound sulfhydryl groups, resulting in the production of ROS as superoxide ion, hydrogen peroxide, and hydroxyl radical. As a consequence, enhanced lipid peroxidation, DNA damage, and altered calcium and sulfhydryl homeostasis occur [ 198 ]. Various experimental studies report the beneficial effect of vitamin C against heavy metal toxicity. Lead is considered as one of the common environmental poison in which protective role of vitamin C is extensively studied. A recent experimental study based on histopathological examination revealed the diminution of detrimental effects of chronic lead intoxication on liver, kidneys, brain and testes [ 199 ]. In another study lead induced electrophysiological changes were inhibited in rat colon by AA administration [ 200 ]. The beneficial effect of AA on lead concentrations in human studies is however inconclusive. A large survey comprising of 19,578 participants (6–90 years) without prior history of lead poisoning reported that blood levels of AA are inversely related to plasma AA and recent dietary intake had no influence on blood levels. This study surmises that there may be a protective relationship between AA and lead [ 201 ].
Arsenic toxicity is essentially associated with lipid peroxidation and oxidative stress. Arsenic in drinking water may even cause chromosomal aberration leading to molecular disorders [ 202 ]. Arsenic exposure during gestation and lactation leads to significantly increased lipid peroxidation in the rat brain which was reversed by supplementation of vitamin C, E and Zn [ 203 ]. In another study arsenic induced normocytic and normochromic anemia as well as a significant increase in hemolysis, TBARS production, catalase activity, hyperlipidemia, and impairment in renal functions in mice pups during gestation and lactation which was partially reverted by the administration of AA [ 204 ]. Arsenic induced hepatotoxicity has also been reported by recent experimental studies which have suggested that vitamin C supplementation improves mitochondrial structure and function along with restriction of apoptosis due to caspase-3 inhibition in arsenic trioxide exposed rat liver. The overall report is of view that vitamin C and vitamin C rich fruits such as goose berry provides protection against metal induced hepatotoxicity [ 205 , 206 ].
Cadmium is an extremely toxic metal commonly found in industrial workplaces similar to lead and arsenic also causes lipid peroxidative changes in various tissues. An experimental study discussed protective role of vitamin C supplementation in lung and brain of rat exposed to excessive cadmium [ 207 ]. Vitamin C also reverted haematological changes in mercury and cadmium exposed Wistar rats [ 208 ]. Vitamin C was also observed to be protective against concomitant exposure to heavy metal and radiation in another experimental study [ 209 ].
Vitamin C and Neurodegenerative Disorders
Schizophrenia is one of the major neurological disorders associated with great deal of morbidity and economic burden. It is a multifactorial disease and hence has a poor outcome in spite of the best available treatments. It is worth mentioning that simple water soluble vitamin C, adequately present in fruits and vegetables had drawn attention of the psychiatrists almost seven decades ago for the treatment of schizophrenia. A study conducted on 12 schizophrenics showed that urinary excretion of vitamin C was significantly lower than healthy controls and intravenous injection of large dose of vitamin C produced improvement in mental condition in 75 % of patients [ 210 ]. In another study it was observed that vitamin C level was significantly low in plasma and urine of schizophrenics as compared to normal controls. Administration of vitamin C improved plasma vitamin C level and thus concluded that schizophrenic patients require higher levels of vitamin C than the suggested optimal AA requirement for healthy individuals [ 211 ]. Several investigators have implicated role of increased free radical generation in pathogenesis of schizophrenia. Alteration in the optimum activities of antioxidant enzymes [ 212 – 214 ] and related parameters of lipid peroxidation [ 215 , 216 ] in blood have been detected in schizophrenics. Brain contains large amount of unsaturated fatty acids, catecholamines and monoamines, which are the target molecules for lipid peroxidation [ 217 , 218 ]. Brain is rich in iron containing compounds and thus it is an easy target for lipid peroxidation through the formation of hydroxyl radicals. Monoamine and catecholamine oxidation also produces superoxide anions in the brain [ 219 ]. AA, an antioxidant vitamin, plays an important role in protecting free radical-induced damage in the brain. Dadheech et al. [ 220 ] reported the antioxidant deficit in schizophrenics and it was associated with increased MDA level in blood which is a marker for lipid peroxidation. Vitamin C is present in dopamine dominant areas at high concentrations in the brain tissue as compared to other organs [ 221 , 222 ]. Recently, Arvindakshan et al. [ 223 ] reported reduction in brief psychiatric rating scale (BPRS) and positive and negative syndrome scale score after supplementation with omega-3 fatty acids, vitamin C, and vitamin E. A decrease in the levels of tocopherol, total AA and reduced glutathione was found in schizophrenics compared to normal controls. Further a significant rise in oxidative stress and decreased antioxidant status was observed in the chronic stage of schizophrenia as compared to those in acute condition. A significant rise in dehydroascorbic acid with concomitant fall in reduced AA suggests scavenging action of AA and its utilization with increased oxidative stress as indicated by high blood malondialdehyde levels. Leucocyte AA, a better index of AA status was also found to be reduced in schizophrenics, suggesting depletion of body stores of AA and the condition worsened with advancing age [ 224 ].
Very few studies have examined the effect of vitamin C with typical antipsychotics in the treatment of schizophrenia. Oral supplementation of vitamin C with antipsychotic reverses AA levels, reduces oxidative stress, and improves BPRS score, hence both the drugs in combination can be used in the treatment of schizophrenia [ 225 ]. The findings of another study suggest that antioxidant supplement therapy as an adjuvant therapy is useful in patients with stress-induced psychiatric disorders [ 226 ]. There are also reports advocating beneficial effect of vitamin C in neurodegenerative disorders including Alzheimer’s disease. Overall there is large body of evidence supporting that maintaining healthy vitamin C level can have a protective function against age related cognitive decline but avoiding vitamin C deficiency is likely to be more beneficial than taking supplements on top of normal healthy diet [ 227 ].

IMAGES
VIDEO
COMMENTS
Vitamins are a group of organic compounds essential to physiological functions in the body. This Special Issue features systematic review and original research articles of vitamins in health and disease. Among other topics, the association of endogenous vitamin levels with disease risk, the therapeutic role of vitamin supplementation in various ...
In addition, the incidence of acute respiratory inflammation in older long-term patients has decreased by vitamin D . In addition, a prior review suggested the use of vitamin D to decrease the risks of COVID-19 infection . Moreover, the effect of vitamin D3 to reduce the influenza infection risk and COVID-19 was investigated in .
The use of vitamin, mineral, and fish oil supplements 5 is common among adults in North America (fig 1). 6 The prevalence of use has increased for some individual nutrients—for example, there was a fourfold increase in use of vitamin D supplements among US adults from 1999 to 2012, excluding intake obtained from multivitamin and mineral. 7 ...
Vitamin D has a promising role in multiple sclerosis (MS) management, and it has been found to be beneficial for patients' mental health, which is reduced in MS patients. The aim of the present study was to conduct a systematic review of the literature to assess the influence of vitamin D supplementation on mental health in MS patients.
Fat-soluble vitamins, including vitamins A, D, E, and K, are energy-free molecules that are essential to the body's functioning and life. Their intake is almost exclusively exogenous, i.e., dietary. As a result, fat-soluble vitamin deficiencies are rarer in industrialized countries than in countries with limited resources. Certain groups of people are particularly affected, such as newborns ...
The vitamins and supplement market is worth millions, and we must hope that this means more people than ever want to stay well. ... Delgado A S, Mendes J J. Vitamin D deficiency and oral health: a ...
According to the literature, it is found that the use of vitamins may be beneficial in the treatment of coronavirus [17]. Accordingly, this review aimed to investigates the role of trace elements and vitamins to boost immune system function to fight against the COVID-19 pandemic.
COVID-19 is a kind of SARS-CoV-2 viral infectious pneumonia. This research aims to perform a bibliometric analysis of the published studies of vitamins and trace elements in the Scopus database with a special focus on COVID-19 disease. To achieve the goal of the study, network and density visualizat …
The lack of vitamin C causes scurvy, a. pathological c ondition leading to blood vessel fragility and connective tissue damage due to failure in producing col lagen, and, finally, to death as ...
OR "vitamin C and covid19" OR "vitamin D and covid19" OR "vitamin E and covid19". A total of 51 articles was. assessed in this literature review. Research fi nds vitamin A plays a ...
Background: The present literature review is part of the NNR5 project with the aim of reviewing and updating the scientific basis of the 4th edition of the Nordic Nutrition Recommendations (NNR) issued in 2004. Objectives: The overall aim was to review recent scientific data on the requirements and health effects of vitamin D and to report it to the NNR5 Working Group, who is responsible for ...
This article reviews the evidence for vitamin D in prevention and treatment in primary care. METHODS: We performed a literature review of randomized controlled trials, meta-analyses, systematic reviews, and large prospective trials looking at the role of vitamin D deficiency in the most common conditions seen in primary care and the top 10 ...
This Review highlights results from large randomized clinical trials performed during the period 2017-2020 and Mendelian randomization studies on vitamin D levels. Together, findings indicate ...
In addition, the incidence of acute respiratory inflammation in older long-term patients has decreased by vitamin D [70]. In addition, a prior review suggested the use of vitamin D to decrease the risks of COVID-19 infection [71]. Moreover, the effect of vitamin D3 to reduce the influenza infection risk and COVID-19 was investigated in [72].
Vitamin B 12 and bone health have been well researched in various community settings and ethnic groups, either singly or with other B vitamins. In this review, 17 cross-sectional studies reported on association of vitamin B 12 and bone mass. 21-23, 25-33, 35-39 Of these, eight studies found a significant association between vitamin B 12 and BMD ...
INTRODUCTION. Vitamin A is an essential component of the human diet. It is derived from vitamin-A-rich foods as well as from foods containing beta-carotene, composed of two retinol molecules. 1 Retinoic acid (RA) is the active metabolite of vitamin A and is a critical signaling molecule for both the developing and adult central nervous system (CNS). RA is synthesized more by the CNS than by ...
Request PDF | A Literature Review on Beneficial Role of Vitamins and Trace Elements: Evidence from Published Clinical Studies | COVID-19 is a kind of SARS-CoV-2 viral infectious pneumonia. This ...
Chapter three concentrated on vitamin A, retinoid and the provitamin A carotenoids, and their roles in human health, with a comprehensive literature review and references. Chapter four to six introduced the other three fat soluble vitamins, D, E and K, and discussing their bioavailability, requirements, and deficiency in a constructive and ...
Abstract. Vitamin D, a fat-soluble prohormone, is synthesised in response to sunlight. Vitamin D requires two metabolic conversions, 25-hydroxylation in the liver and 1alpha-hydroxylation in the kidney, to become active hormone. The active form, 1alpha,25- (OH)2D, binds to the vitamin D receptor (VDR) to modulate gene transcription and regulate ...
However, at least six systematic review and meta-analysis studies and two systematic reviews from around the world have appeared within the past 6 months, with a general consensus that it does appear that a higher vitamin D status is generally associated with a lower susceptibility to COVID-19, and better morbidity and mortality outcomes. 239 ...
Introduction The most common cause of hyperthyroidism, Graves' disease is a common organ-specific autoimmune disease. Selenium is an essential trace element of the human body that is mainly concentrated in the thyroid gland and is involved in the synthesis and metabolism of thyroid hormones. Most studies have shown that the level of selenium is closely related to the occurrence and development ...
One Hundred Y ears of Vitamins—A. Success Story of the Natural Sciences. Essential: The discovery of vitamins was. a scientific breakthrough that changed the. world! The synthesis of vitamins on ...
A systematic review has been conducted by Holvik et al. for available literature on vitamin D status in Norway. They concluded that the vitamin D status was sufficient for the majority in the general population (25(OH)D ≥50 nmol/l was considered as optimal) and that available data suggest that the vitamin D status in Norway is better than ...
Abstract. The recognition of vitamin C is associated with a history of an unrelenting search for the cause of the ancient haemorrhagic disease scurvy. Isolated in 1928, vitamin C is essential for the development and maintenance of connective tissues. It plays an important role in bone formation, wound healing and the maintenance of healthy gums.