- Introduction
- Conclusions
- Article Information
Cirrhosis leads to intrahepatic resistance, which causes portal hypertension and, at later stages, hepatic insufficiency, which disrupts the liver’s normal metabolic functions. Together these features cause gut-barrier disruption and portosystemic shunting, resulting in the multisystem complications of cirrhosis, eg, hepatic encephalopathy, sarcopenia, ascites, and kidney injury.
The presence of cirrhosis is associated with an increased risk of complications such as liver cancer and decompensation including ascites, hepatic encephalopathy, and variceal hemorrhage. It is important to evaluate for the presence of cirrhosis in people with risk factors or any diagnosed chronic liver disease. While physical examination findings may be suggestive, it is recommended to stratify risk for all using the FIB-4 followed by elastography for at-risk patients. After identifying patients with cirrhosis, optimal care may involve referral to a hepatologist, liver cancer screening, and consideration of endoscopy for varices screening and/or initiation of nonselective β-blockers. BMI indicates body mass index.
a Terry nails identified by white discoloration, absent lunula, and dark pink tips.
b Biopsy is of highest value when the diagnosis of the underlying liver disease is unclear or noninvasive tests yield indeterminate or discordant results. The role of biopsy is also based on patient preference and clinical context.
The consequences of cirrhosis are depicted on a timeline from the development of compensated cirrhosis to death or transplant. Biomarkers associated with lower risk of decompensation and death are shown in green, those of indeterminate significance in yellow, and biomarkers and events associated with a higher risk of decompensation and death in red; disease-modifying measures and interventions are shown in blue. The liver stiffness measures are shown in kilopascals and are derived from vibration-controlled transient elastography.
a Ten to 19 kPa denotes intermediate risk, 15 kPa is the threshold for assuming cirrhosis, 20 kPa is high risk, and 25 kPa is highest risk and assumes clinical portal hypertension.
- Vibration-Controlled Transient Elastography for Diagnosing Cirrhosis and Staging Hepatic Fibrosis JAMA JAMA Diagnostic Test Interpretation November 20, 2018 A 68-year-old man has an undetectable hepatitis C (HCV) viral load, normal liver function tests, and an elevated vibration-controlled transient elastography (VCTE) measure after 12 weeks of antiviral treatment for HCV with stage 2 fibrosis by biopsy. How do you interpret the results? Julius Wilder, MD, PhD; Steve S. Choi, MD; Cynthia A. Moylan, MD, MHS
- Patient Information: What Is Cirrhosis? JAMA JAMA Patient Page July 25, 2023 This JAMA Patient Page describes liver cirrhosis, its signs and symptoms, potential complications, and treatment options. Kristin L. Walter, MD, MS
- Diagnosis and Treatment of Cirrhosis—Reply JAMA Comment & Response September 12, 2023 Elliot B. Tapper, MD; Neehar D. Parikh, MD, MS
- Diagnosis and Treatment of Cirrhosis JAMA Comment & Response September 12, 2023 Alain Braillon, MD
- County-Level Variation in Cirrhosis-Related Mortality in the US, 1999-2019 JAMA Network Open Research Letter February 2, 2022 This cross-sectional study characterizes cirrhosis mortality by metropolitan categories and potential disparities among the various rural and urban demographic subgroups using the US Centers for Disease Control and Prevention WONDER database. Audrey Y. Ha; Michael H. Le, MS; Linda Henry, PhD; Yee Hui Yeo, MD, MSc; Ramsey C. Cheung, MD; Mindie H. Nguyen, MD, MAS

See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Tapper EB , Parikh ND. Diagnosis and Management of Cirrhosis and Its Complications : A Review . JAMA. 2023;329(18):1589–1602. doi:10.1001/jama.2023.5997
Manage citations:
© 2024
- Permissions
Diagnosis and Management of Cirrhosis and Its Complications : A Review
- 1 Division of Gastroenterology and Hepatology, University of Michigan, Ann Arbor
- JAMA Diagnostic Test Interpretation Vibration-Controlled Transient Elastography for Diagnosing Cirrhosis and Staging Hepatic Fibrosis Julius Wilder, MD, PhD; Steve S. Choi, MD; Cynthia A. Moylan, MD, MHS JAMA
- JAMA Patient Page Patient Information: What Is Cirrhosis? Kristin L. Walter, MD, MS JAMA
- Comment & Response Diagnosis and Treatment of Cirrhosis—Reply Elliot B. Tapper, MD; Neehar D. Parikh, MD, MS JAMA
- Comment & Response Diagnosis and Treatment of Cirrhosis Alain Braillon, MD JAMA
- Research Letter County-Level Variation in Cirrhosis-Related Mortality in the US, 1999-2019 Audrey Y. Ha; Michael H. Le, MS; Linda Henry, PhD; Yee Hui Yeo, MD, MSc; Ramsey C. Cheung, MD; Mindie H. Nguyen, MD, MAS JAMA Network Open
Importance Cirrhosis affects approximately 2.2 million adults in the US. From 2010 to 2021, the annual age-adjusted mortality of cirrhosis increased from 14.9 per 100 000 to 21.9 per 100 000 people.
Observations The most common causes of cirrhosis in the US, which can overlap, include alcohol use disorder (approximately 45% of all cases of cirrhosis), nonalcoholic fatty liver disease (26%), and hepatitis C (41%). Patients with cirrhosis experience symptoms including muscle cramps (approximately 64% prevalence), pruritus (39%), poor-quality sleep (63%), and sexual dysfunction (53%). Cirrhosis can be diagnosed by liver biopsy but may also be diagnosed noninvasively. Elastography, a noninvasive assessment of liver stiffness measured in kilopascals, can typically confirm cirrhosis at levels of 15 kPa or greater. Approximately 40% of people with cirrhosis are diagnosed when they present with complications such as hepatic encephalopathy or ascites. The median survival time following onset of hepatic encephalopathy and ascites is 0.92 and 1.1 years, respectively. Among people with ascites, the annual incidence of spontaneous bacterial peritonitis is 11% and of hepatorenal syndrome is 8%; the latter is associated with a median survival of less than 2 weeks. Approximately 1% to 4% of patients with cirrhosis develop hepatocellular carcinoma each year, which is associated with a 5-year survival of approximately 20%. In a 3-year randomized clinical trial of 201 patients with portal hypertension, nonselective β-blockers (carvedilol or propranolol) reduced the risk of decompensation or death compared with placebo (16% vs 27%). Compared with sequential initiation, combination aldosterone antagonist and loop diuretics were more likely to resolve ascites (76% vs 56%) with lower rates of hyperkalemia (4% vs 18%). In meta-analyses of randomized trials, lactulose was associated with reduced mortality relative to placebo (8.5% vs 14%) in randomized trials involving 705 patients and reduced risk of recurrent overt hepatic encephalopathy (25.5% vs 46.8%) in randomized trials involving 1415 patients. In a randomized clinical trial of 300 patients, terlipressin improved the rate of reversal of hepatorenal syndrome from 39% to 18%. Trials addressing symptoms of cirrhosis have demonstrated efficacy for hydroxyzine in improving sleep dysfunction, pickle brine and taurine for reducing muscle cramps, and tadalafil for improving sexual dysfunction in men.
Conclusions and Relevance Approximately 2.2 million US adults have cirrhosis. Many symptoms, such as muscle cramps, poor-quality sleep, pruritus, and sexual dysfunction, are common and treatable. First-line therapies include carvedilol or propranolol to prevent variceal bleeding, lactulose for hepatic encephalopathy, combination aldosterone antagonists and loop diuretics for ascites, and terlipressin for hepatorenal syndrome.
Cirrhosis affects approximately 2.2 million adults in the US 1 and is associated with mortality rates of 21.9 per 100 000 people. 2 , 3 Cirrhosis is defined as the fibrotic replacement of liver tissue that can result from any chronic liver disease. Most prevalent cases of cirrhosis are caused by alcohol use disorder (approximately 45% of all cirrhosis cases), hepatitis C (41%), and nonalcoholic fatty liver disease (26%), with many patients having overlapping causes. 4 However, hepatitis C is now curable with direct-acting antivirals and most newly diagnosed cirrhosis is due to nonalcoholic fatty liver disease (NAFLD) (accounting for 61.8% of incident cases) and alcohol use disorder (accounting for 20.0%). 5
Outcomes for patients with cirrhosis can be improved with evidence-based therapies directed toward both the etiology of cirrhosis 6 - 12 and its complications. 13 - 21 Recent innovations include noninvasive risk stratification of cirrhosis 22 , 23 as well as interventions that improve survival by preventing or reducing the complications of cirrhosis. 24 Such complications include variceal hemorrhage, ascites, and hepatic encephalopathy. People with cirrhosis have reduced quality of life. 25 Poor quality of life is associated with many common symptoms 26 such as muscle cramps, 27 , 28 poor-quality sleep, 29 pruritus, 30 , 31 and sexual dysfunction, 32 , 33 which can be improved with therapy.
This review summarizes the current evidence regarding the diagnosis and management of cirrhosis and its complications ( Box ).
Common Questions on the Management and Complications of Cirrhosis
Does my patient need a liver biopsy to diagnose cirrhosis?
No. Cirrhosis can be accurately diagnosed using sequential noninvasive testing such as the fibrosis-4 index followed by a liver stiffness measurement obtained by elastography (eg, vibration-controlled transient elastography or magnetic resonance elastography). Because liver stiffness measurements are also prognostic, they can be used, for example, to determine which patients need endoscopy to screen for esophageal varices.
What is the most common cause of cirrhosis?
Most prevalent cases of cirrhosis in the US are caused by alcohol use disorder, nonalcoholic fatty liver disease (NAFLD), and hepatitis C infection. Most incident cases of cirrhosis are caused by NAFLD; however, there is also an increase in alcohol-related cirrhosis, particularly among young people.
What can be done to improve survival among patients with compensated cirrhosis?
Survival for patients with cirrhosis is improved with control of their underlying chronic liver disease (eg, alcohol use disorder, viral hepatitis, NAFLD). Beyond that, screening for liver cancer with biannual ultrasound and α-fetoprotein is associated with higher rates of curative treatment when cancer is detected. When patients develop portal hypertension, nonselective β-blockers (particularly carvedilol or propranolol) are associated with lower rates of decompensation or death.
We searched PubMed (January 1, 2000, to March 10, 2023) for systematic reviews, meta-analyses, randomized clinical trials (RCTs), and relevant guidelines. We prioritized recent RCTs of higher quality based on rigor of study design, sample size, and length of follow-up. Of 8887 articles retrieved, 115 were included, consisting of 9 practice guidelines, 3 consensus statements, 25 RCTs, 17 meta-analyses, 7 systematic reviews (without meta-analysis), and 54 observational cohort studies.
The causes of cirrhosis vary by context and many overlap. In a study of 68 673 patients from a national sample of patients in the Veterans Administration (2020-2021), the causes of cirrhosis were hepatitis C (24.0%), alcohol related (27.9%), hepatitis C and alcohol related (17.4%), NAFLD related (25.9%), and due to other conditions (3.7%). 4 Patients diagnosed with cirrhosis typically have a mean age of 59.5 to 62.4 years. 34 , 35 Patients with NAFLD cirrhosis often present at a mean age of 67 years. 34 However, cirrhosis is now more common among younger patients. The incidence of cirrhosis by age 35 years was 46.9 per 100 000 people among those born during or after 1980 compared with 32.6 per 100 000 born between 1945 and 1960. 36 A total of 54% to 60% of cirrhosis cases occur among men. 35 - 37 Between 2010 and 2021, age-adjusted mortality from cirrhosis increased from 14.9 to 21.9 per 100 000 people. 2 , 3 Cirrhosis mortality increased from 1.1 to 3.3 per 100 000 people aged 25 to 34 years from 2010 to 2020 3 due to increases in alcohol-related liver disease. 2 The epidemiology of cirrhosis and its complications are described further in Table 1 . 24 , 34 , 36 , 38 - 56
Chronic inflammatory liver injury causes activation of hepatic myofibroblasts and macrophages, which increase collagen accumulation (fibrosis) in the extracellular matrix. This process disrupts the connection between hepatocytes and sinusoids where blood flows, leads to formation of nodules of fibrosis, and impedes portal inflow resulting in portal venous hypertension. Chronic liver injury results in increased vasoconstrictor signaling (such as endothelin-1) and decreased production of vasodilators (such as nitric oxide), further restricting sinusoidal flow. Inflammatory injury from alcohol or steatosis also increases vascular resistance. In both NAFLD and alcohol-related liver disease, heritable factors in lipid metabolism have been associated with progression of liver disease. 57 In addition, chronic liver injury causes hepatocyte loss and reduces the liver’s capacity for metabolic activity including protein synthesis, detoxification, nutrient storage, and bilirubin clearance. Proteins synthesized by the liver include albumin, hormones (eg, thrombopoietin [responsible for platelet production]), and hemostatic factors (procoagulants and anticoagulants). 58 The multisystem impact of these processes is depicted in Figure 1 .
Over time, patients may progress from compensated cirrhosis without clinical manifestations to decompensated cirrhosis with variceal hemorrhage, ascites, or hepatic encephalopathy. Portal hypertension, defined as a pressure gradient between the hepatic and portal vein of 10 mm Hg or greater, promotes development of varices (collateral vessels that shunt portal blood to systemic veins and often result in dilated esophagogastric channels prone to hemorrhage). Disrupted portal flow causes decreased cardiac return and decreased central blood volume, leading to increased plasma renin activity, increased renal-tubular affinity for sodium, peripheral volume expansion, and kidney vasoconstriction, predisposing patients to ascites, hyponatremia, and kidney injury, particularly in the setting of volume depletion, infection, or hemorrhage. Increasing portal pressure induces ascites from hepatic sinusoids. Increased sinusoidal pressure causes increased lymph production, which extravasates into the peritoneum when lymphatic drainage capacity is exceeded. Gut-derived toxins, such as ammonia and bacterial products that induce systemic inflammation, cause hepatic encephalopathy. Hepatic encephalopathy can develop at low ammonia levels in the context of infection. 59 While the mechanisms are incompletely characterized, the presence of hepatic fibrosis and hepatic injury from inflammation contribute to the genetic and epigenetic aberrations that lead to the development of hepatocellular carcinoma.
Medical history and physical examination can identify patients with or at risk for cirrhosis. Patients with cirrhosis frequently experience muscle cramps (64% prevalence) and pruritus (39%), 26 poor-quality sleep (63%), 60 and sexual dysfunction (53%). 61 Risk factors, such as diabetes or alcohol use, and symptoms, such as muscle cramps, pruritus, sleep disorder, and sexual dysfunction, are neither sensitive nor specific for the diagnosis of cirrhosis. 62 Most physical examination findings are not sensitive for cirrhosis but some offer specificity greater than 90%: these include Terry nails (white discoloration, absent lunula, dark pink at tip), gynecomastia, caput medusa, facial telangiectasia, palmar erythema, decreased body hair, testicular atrophy, and jaundice. 62
Screening for cirrhosis in the general population is not currently recommended. 63 However, patients with established chronic liver disease with abnormal liver enzymes, hepatic steatosis on imaging, or viral hepatitis should be evaluated for cirrhosis. Liver biopsy is considered the criterion standard to diagnose cirrhosis, although it is being increasingly replaced by noninvasive methods for fibrosis assessment. Biopsy is reserved for patients with noninvasive testing that is inconclusive or technically inadequate or when the underlying chronic liver disease is unclear.
Serologic measures and imaging-based indices are used to diagnose cirrhosis. Compared with biopsy, these measures are less expensive, safer, and simpler to follow longitudinally ( Figure 2 ). The most common serologic tests capture indirect signs of liver fibrosis and dysfunction (eg, thrombocytopenia, reflecting reduced platelet production and splenic sequestration and a higher ratio of aspartate aminotransferase to alanine aminotransferase). 62 The fibrosis-4 index (FIB-4; age, alanine aminotransferase, aspartate aminotransferase, platelet count) is a widely accepted risk-stratification tool that, for people with either NAFLD or alcohol-related liver disease, classifies scores as low (<1.30), intermediate (1.30-2.67), and high (>2.67). Age increases the FIB-4; for patients older than 65 years, the lower risk threshold is 2.0 or less (while high-risk thresholds remain the same). 64 Cutoffs such as less than 1.45 and greater than 3.25 have been developed for hepatitis C. FIB-4 has high negative predictive value (96%) but low positive predictive value (63%) for cirrhosis. 65 Risk stratification using FIB-4, for which values less than 1.3 offer a negative likelihood ratio of 0.4 for advanced fibrosis, 66 is recommended by societal guidelines in patients with known NAFLD (or risk factors such as diabetes or obesity). 63
Additional testing is needed in the setting of an elevated FIB-4 score (eg, ≥1.3 for patients with NAFLD, ≥2.0 for patients >65 years old). 63 Sequential testing of patients with liver disease risk factors using FIB-4 followed by elastography can provide posterior probabilities of cirrhosis of 89% or greater. 66 Elastography provides a liver stiffness measurement (LSM; measured in kilopascals [kPa]) that correlates with the abundance of fibrosis. 66 LSM of 15 kPa or greater by vibration-controlled transient elastography (VCTE), an ultrasound-based method that uses a handheld probe for point-of-care assessments, identified cirrhosis with 95.5% specificity (62% positive predictive value) in a cohort of 5648 patients with both VCTE and liver biopsy. Conversely, LSM of 10 kPa or greater had a sensitivity of 74.9% (88% negative predictive value). 22 , 67 Magnetic resonance elastography has fewer technical failures than VCTE in patients with high (>40) body mass index (calculated as weight in kilograms divided by height in meters squared). However, cost and access limit widespread use of magnetic resonance elastography. Liver inflammation (ie, alanine aminotransferase >120 IU/L 68 ) and central venous congestion from heart failure can also increase liver stiffness, generating false-positives from elastography.
Portal pressures can be estimated using a transjugular catheter to determine the hepatic venous pressure gradient, a measure of the pressure gradient across the liver. Clinically significant portal hypertension (CSPH) is defined as a gradient of 10 mm Hg or greater (normal <5 mm Hg). 22 In a study of 213 patients with pressure gradients less than 10 mm Hg, approximately 90% remained decompensation free for at least 4 years. 69 Pressure measurements, though safe, are costly; can only be obtained in specialized units; and have high (26%) within-individual variance. 70 The optimal noninvasive alternative for identifying patients with CSPH involves a combination of liver stiffness from VCTE and platelet counts. 71 Thrombocytopenia (ie, platelet count <110 × 10 9 /L) in patients with liver disease is both highly suggestive of cirrhosis 62 and associated with a patient’s risk of ascites and variceal bleeding. 72 Among 518 persons with cirrhosis from Europe and Canada, a nomogram based on LSM and platelet counts was developed to predict CSPH. 71 For example, patients with an LSM of 25 kPa or greater and any platelet count have a prevalence of CSPH of at least 66%, increasing to 90% or more for patients with platelet counts of 110 × 10 9 /L or less. 71
All patients with varices have CSPH. Because portal pressures are not routinely measured, it is recommended to screen for varices in patients with cirrhosis every year if decompensated or every 2 to 3 years if compensated (2 years if the patient is actively drinking alcohol or chronic liver disease is uncontrolled, eg, untreated hepatitis B or C or autoimmune hepatitis). 23 However, guidelines also suggest that noninvasive tests can rule out CSPH 22 , 23 and therefore obviate the need for endoscopy. Among 7387 patients pooled from 26 studies, LSM less than 20 kPa and platelet count greater than 150 × 10 9 /L provided a negative likelihood ratio of 0.09 for high-risk (large and/or thin-walled) varices. 73 According to these data, only 2.2% of high-risk varices were missed if endoscopy was not performed. 73
The diagnosis of ascites can be made using abdominal ultrasonography or cross-sectional imaging. Flank dullness, shifting dullness, and fluid wave elicited by physical examination offer 94%, 83%, and 50% sensitivity and 29%, 56%, and 82% specificity, respectively. 74 Spontaneous bacterial peritonitis is diagnosed after paracentesis with ascites concentrations of neutrophil count greater than 250/μL. 75 Up to one-third of patients with spontaneous bacterial peritonitis do not have fever or pain. Therefore, diagnostic paracentesis is recommended for all hospitalized patients with cirrhosis and ascites. 53 , 76 Hepatorenal syndrome is defined as kidney injury in the presence of large-volume ascites if there is a 50%, or 0.3 mg/dL, or greater increase in serum creatinine within 7 days from the last measure that does not respond to 2 days of intravenous fluids to establish normal intravascular volume. 53
Hepatic encephalopathy is a clinical diagnosis. It presents as a spectrum on the West Haven Criteria scale (0 to 4 scale, where 0 indicates no deficits and 4 indicates coma). Overt hepatic encephalopathy (grades ≥2) presents with asterixis, disorientation, lethargy, and coma. Covert hepatic encephalopathy (grades ≤1) may present as deficits in executive function, sleep disorder, vegetative behavior, and gait disturbance. The criterion-standard diagnostic for covert hepatic encephalopathy is greater than or equal to 4 SDs below healthy control performance on the 5-test paper-pencil battery called the Psychometric Hepatic Encephalopathy Score. This battery can be replaced by some bedside measures 42 including the Animal Naming Test (in a prospective cohort of 327 patients, <15 and <10 animals per minute offered sensitivities for diagnosing hepatic encephalopathy of 70% and 15%, respectively, and specificities of 63% and 92%, respectively) or the EncephalApp Stroop Test (>198 seconds on a computerized version of the Stroop test of attention offered 80% sensitivity and 61% specificity in a prospective cohort of 277 patients). 42 Covert hepatic encephalopathy can also present as recent falls (40% within the prior year for those diagnosed with covert hepatic encephalopathy vs 12.9% for those without) 77 and poor-quality sleep (mean of 10.3 vs 7.6 on the Pittsburgh Sleep Quality Index where >5 reflects poor sleep). 78 An algorithm based on age, sex, and self-reported loss of balance, irritability/impatience, anorexia, and disinterest in physical activity can identify covert hepatic encephalopathy with a sensitivity of 80% and specificity of 79%. 42
Although randomized trials of screening for hepatocellular carcinoma (HCC) are lacking, screening with biannual abdominal ultrasound and serum α-fetoprotein is recommended by the American Association for the Study of Liver Diseases to improve early HCC detection in patients with cirrhosis, regardless of etiology. 76 , 79 In a meta-analysis of 32 observational studies that included 13 367 patients, screening for HCC was associated with early-stage detection (58.8% vs 27.0%) and increased rates of curative therapies (58.2% vs 34.0%) in comparison with no screening. 80 Longer screening intervals (ie, annual screening) have not been prospectively compared with semiannual screening.
Patients with cirrhosis and a greater than 1.0-cm mass on screening ultrasound or with a rising or elevated α-fetoprotein level (cutoff >20 ng/mL) should undergo further diagnostic workup to evaluate for HCC. Though biopsy is diagnostic, multiphasic contrast-enhanced cross-sectional imaging can be used to make the diagnosis. 79 A solid lesion exhibiting specific features (eg, arterial-phase hyperenhancement and portal venous phase washout) in a patient with cirrhosis can be diagnosed as HCC. 79
Although survival varies with age at diagnosis and extrahepatic comorbidities, 81 patients with compensated cirrhosis have a median survival of 12 years according to a pooled analysis of 806 prospectively followed up patients. 82 Survival is reduced after any decompensation ( Figure 3 ). Patients with compensated cirrhosis and small varices have a 6% 1-year risk of bleeding, while patients with large varices and decompensated cirrhosis have a 42% to 76% 1-year risk of bleeding. 83 In-hospital mortality after variceal hemorrhage is approximately 14.5% overall and as low as 0% for patients with previously compensated cirrhosis. 84 Ascites in the setting of cirrhosis was associated with a median survival of 1.1 years in a cohort of 13 265 patients enrolled in Medicare. 46 Median survival time following incident overt hepatic encephalopathy was 0.92 years in a study of 49 164 patients with cirrhosis enrolled in Medicare. 37 , 44 Compared with patients with cirrhosis without any hepatic encephalopathy, covert hepatic encephalopathy was also associated with worse outcomes. Such outcomes included a higher 1-year risk of car crashes (17% of 97 patients with covert hepatic encephalopathy vs 3% of 70 without) 85 and, in a cohort of 170 patients with cirrhosis (56% with covert hepatic encephalopathy), higher rates of hospitalization (47% vs 15%) and death (18% vs 3%). 43
Factors associated with reduced survival include lower serum levels of albumin, higher international normalized ratios (INRs), and elevated bilirubin levels. These are 3 components of the Child-Turcotte-Pugh (CTP) score, which also includes ascites and hepatic encephalopathy. Bilirubin and INR are included in the Model for End-stage Liver Disease–Sodium (MELD-Na) score along with creatinine and sodium levels. The CTP ranges from 5 (75% 5-year survival) to 15 (20% 5-year survival if >12) 86 ; the MELD-Na ranges from 6 (1.9% 90-day mortality) to 40 (71.3% 90-day mortality). 87 MELD is best suited to short-term prognostication for patients with decompensated cirrhosis and it is used to prioritize organ allocation on the transplant waitlist; the CTP is used for long-term prognostics and complements MELD by describing the patient’s compensation status. When patients with cirrhosis require hospitalization, patients with acute-on-chronic liver failure have an increased rate of near-term mortality. 88 Organ failures include severe hepatic encephalopathy (disorientation and/or coma), shock, requirement for mechanical ventilation, and kidney failure requiring dialysis. Thirty-day survival is 95% for patients with decompensated cirrhosis and no organ failure. 88 Survival is reduced for patients with organ failures and infections. For patients with 2 organ failures, survival with or without infection is 62% or 84%, respectively; for those with 4 organ failures, survival is 0% or 24%. 88
Cirrhosis is associated with multiple common physical and psychological symptoms that can be improved with treatment ( Table 2 ). 13 - 21 , 24 , 27 - 33 , 53 , 89 - 94 In an RCT of 80 patients, compared with tap water, 1 sip of pickle brine at cramp onset significantly reduced cramp severity at 28-day follow-up (2.3- vs 0.4-point reduction on a 10-point visual analog scale). 27 In a 2-week randomized, double-blind, crossover trial of 30 patients, compared with placebo, 1000 mg of taurine twice daily significantly reduced leg cramping (7 fewer cramps compared with placebo). 28 Cholestyramine (4-16 g daily) is considered first-line therapy for pruritus given its safety profile but randomized trials in cirrhosis are lacking. 30 In a 4-week RCT of 16 patients with cirrhosis, naltrexone significantly improved pruritus compared with placebo with a mean (SD) 54% (10%) reduction in pruritus severity compared with an 8% (10%) increase as measured by a 100-mm visual analog scale. 31 In a 10-day RCT of 35 patients with sleep disorder, compared with placebo, hydroxyzine, 25 mg, nightly was associated with a significant 40% improvement from baseline on a 10-point visual analog scale of sleep quality (vs 0% for placebo). 29 One patient in the hydroxyzine group developed overt hepatic encephalopathy (disorientation). Alcohol cessation may improve sexual function, with 25% of 60 men abstinent for 6 months or longer achieving self-reported normal sexual function. 32 In a 12-week, randomized trial of 140 men, compared with placebo, tadalafil, 10 mg, improved erectile function based on patient report (63% vs 30%). 33
Patients with cirrhosis of any cause may benefit from evaluation for liver transplant when they have developed a decompensation or HCC. 76 However, control of the underlying etiology improves the prognosis of cirrhosis by slowing its progression and may reverse fibrosis. For example, after 12 months of follow-up, 43% of 37 patients with cirrhosis and hepatitis C cured with direct-acting antivirals experienced regression to a lower fibrosis stage. 95 Among 96 patients with hepatitis B cirrhosis treated with tenofovir and followed up for 240 weeks, 28% no longer had cirrhosis on biopsy. 96 Alcohol use can worsen the prognosis of any chronic liver disease; alcohol use disorder should be identified and treated. 97 In an observational longitudinal study of 33 682 patients with cirrhosis and alcohol use disorder from the Veterans Administration, behavioral or pharmacotherapy (eg, naltrexone) for alcohol use disorder was associated with significantly reduced 180-day mortality (2.6% vs 3.9%) and cirrhosis decompensation (6.5% vs 11.6%). 98 Etiology-specific therapies and their effects on cirrhosis outcomes are provided in Table 3 . 6 - 12 , 99 - 104
Nonselective β-blockers (eg, carvedilol or propranolol) reduce portal pressure by reducing splanchnic blood flow. Because of its α-blocking effects, carvedilol also reduces intrahepatic resistance. 22 β-Blockers are standard of care for people with large varices or prior bleeding. 58 , 76 If large varices are encountered on endoscopy, carvedilol (optimally dosed at 12.5 mg daily) is preferred to other β-blockers (grade B evidence, strong recommendation) according to the Baveno VII consensus statement. 22 In an RCT of 152 patients, compared with band ligation every 2 weeks until variceal eradication, participants randomized to carvedilol (without banding) had lower rates (10% vs 23%) of variceal bleeding after 20 months of follow-up. 105 Esophageal ulcers caused by the band ligation resulted in bleeding in about 8% of patients in the band ligation group. 105 Patients with portal hypertension alone also benefited from β-blockers. In a 3-year, placebo-controlled, RCT of 201 patients with CSPH, propranolol (or carvedilol for those who did not respond to propranolol) reduced the risk of decompensation or death (16% vs 27%). 24 , 48 Variceal bleeding should be treated with band ligation during timely endoscopy (<24 hours after presentation), 106 vasoactive medications (compared with placebo, octreotide was associated with higher rates of hemostasis at 5 days [77% vs 58%] in a meta-analysis of randomized trials), 17 and prophylactic antibiotics (associated with reduced short-term mortality to 18.5% vs 22.2% with placebo in a meta-analysis of randomized trials 18 ). In a randomized trial of 63 patients with acute variceal bleeding who achieved initial hemostasis, transjugular intrahepatic portosystemic shunt (TIPS, a stent placed in a tract created to connect branches of the hepatic and portal veins) performed within 72 hours (compared with no TIPS placement) improved 1-year survival (61% vs 86%). 19
In an RCT of 100 patients that compared sequential therapy with aldosterone antagonists followed by the addition of loop diuretics to a guideline-recommended combination of both diuretics, ascites resolved at a higher rate with combination therapy (76% vs 56%) and was associated with lower rates of hyperkalemia (4% vs 18%). 16 , 53 Sodium restriction (<2 g/d) is recommended because greater intake may be associated with worse ascites. 53 However, sodium restriction must be carefully monitored, ideally under the care of a nutritionist. Sodium restriction may not improve the effectiveness of diuretics (as seen in a clinical trial of 115 hospitalized patients randomized to daily sodium intake of 2760 mg or 920 mg resulting in rates of refractory ascites of 5.7% vs 4.8%, respectively). 107 Further, many patients who successfully restrict sodium do not meet daily calorie and protein goals. 53
Paracentesis is associated with temporary relief for patients with symptomatic ascites. Multiple paracenteses, despite attempts to optimize diuretic dosage, should prompt referral for TIPS. In a meta-analysis of 305 patients in randomized trials, compared with treatment without TIPS, TIPS was associated with reduced risk of recurrent ascites (42% vs 89%) and reduced 2-year mortality (51% vs 65%), but more hepatic encephalopathy episodes per year (mean [SD], 1.1 [1.9] vs 0.63 [1.2]). 108 While the risk of TIPS rises with MELD score and age, rather than using an absolute MELD cutoff for TIPS candidacy, expert consensus recommends a multidisciplinary approach and shared decision-making (level of evidence, 2a). 109
Hyponatremia (<135 meq/L) is common among patients with decompensated cirrhosis, affecting up to 31% of a national sample of 13 940 patients undergoing liver transplant evaluation. 87 Though evidence supporting its management is limited, hyponatremia is treated by addressing volume depletion (if present) and optimizing diuretic doses; fluid restriction is reserved for patients with levels less than 125 mmol/L despite optimization. 53
Because hypoalbuminemia (<3.5 g/dL) is common among patients with ascites, an open-label RCT enrolling 431 patients with ascites refractory to diuretics and hypoalbuminemia investigated the role of weekly infusions of 40 g of 25% human albumin solution compared with no infusions 110 ; 18-month survival was higher in the albumin group (77%) compared with the no infusion group (66%). 110 However, albumin infusion is not yet recommended for clinical care. 53 In an open-label randomized trial enrolling 777 hospitalized patients with cirrhosis and albumin level less than 3.0 g/dL, albumin infusions (mean dose, 200 g) targeted to increase the albumin level to more than 3.0 g/dL did not improve the rate of a composite outcome (new infection, kidney dysfunction, or death) for up to 14 days (29.7% vs 30.2% for the standard care group). The rate of pulmonary edema (4% vs 1%) was higher for the albumin group. 92
Spontaneous bacterial peritonitis should be treated with guideline-recommended third-generation cephalosporins such as ceftriaxone, 2 g, daily and intravenous albumin. 53 In an RCT of 126 patients, compared with antibiotics alone, 25% albumin (1.5 g/kg on day 1, 1 g/kg on day 2) reduced mortality from 41% to 22% at 3-month follow-up. 20 After a first episode of spontaneous bacterial peritonitis, patients should receive secondary prophylaxis with suppressive oral antibiotics (eg, trimethoprim/sulfamethoxazole or ciprofloxacin). 53 Primary prophylaxis may not be effective given the prevalence of resistant organisms in the community. Antibiotic use is associated with adverse events (eg, trimethoprim-related hyperkalemia, antibiotic-related diarrhea, or Clostridioides difficile infection). 53
Optimal therapy for hepatorenal syndrome includes carefully monitored volume expansion with intravenous albumin and vasoconstrictor therapy to increase mean arterial pressure and kidney perfusion. In an RCT of 300 patients, compared with placebo, terlipressin improved kidney function (creatinine ≤1.5 mg/dL; 39% vs 18%) but was associated with an increased risk of death due to respiratory failure (11% vs 2% with placebo). 21 In a meta-analysis, norepinephrine, 0.5 to 3 mg/h, was noninferior to terlipressin with a 50% pooled rate of kidney injury reversal. 111
Despite low platelet counts or prolonged INR, bleeding after low-risk procedures (eg, paracentesis, endoscopy) is rare. For example, the rate of major bleeding was 0.2% in a pooled analysis of 2113 patients with INR greater than 1.5 and/or platelet count less than 50 × 10 9 /L undergoing paracentesis. 112 In guidelines from the American Association for the Study of Liver Diseases and the Society of Interventional Radiology, neither prophylactic plasma, platelet transfusions, nor vitamin K supplementation is recommended. 58 , 112
Patients who present with clinically manifest hepatic encephalopathy (grade ≥2) should be evaluated for infection, gastrointestinal bleeding, dehydration, and receipt of psychoactive medications. 76 Patients should receive intravenous hydration and lactulose, starting at a dose of 60 cc, followed by 20 cc of lactulose every 1 to 2 hours until a bowel movement occurs, followed by maintenance with sufficient lactulose to achieve 2 to 3 soft bowel movements per day. 43 After the acute episode resolves, secondary prophylaxis also includes rifaximin, 550 mg, twice a day. 13 In a meta-analysis of 705 patients with hepatic encephalopathy, compared with placebo, lactulose was associated with reduced mortality (8.5% vs 14%). 14 Compared with placebo, lactulose was associated with reduced recurrent overt hepatic encephalopathy (25.5% vs 46.8%) in a meta-analysis of RCTs enrolling 1415 patients with hepatic encephalopathy. 14 In a meta-analysis of 3 clinical trials of 126 participants receiving lactulose, lactulose was associated with an improvement of 6.92 (95% CI, 6.66-7.18) in the Sickness Impact Profile (ranges from 0 [best] to 68 [worst]; clinically important differences are >4). 113 In a 6-month placebo-controlled, double-blind RCT, rifaximin reduced hospitalization for hepatic encephalopathy from 22.6% to 13.6% among 299 patients with prior hepatic encephalopathy taking lactulose. 13 Guidelines recommend that all patients should receive education about nutrition, including consumption of 1 g of protein per kilogram of actual body weight, 30 to 40 kCal/kg, and a nighttime snack, as overnight fasting exacerbates catabolism ( Table 2 ). 114 , 115
This review has several limitations. First, this was not a systematic review. Second, some relevant research may have been missed. Third, the quality of the included evidence was not formally assessed.
Approximately 2.2 million US adults have cirrhosis. Many symptoms such as muscle cramps, poor sleep, pruritus, and sexual dysfunction are common and treatable. First-line therapies include carvedilol or propranolol to prevent variceal bleeding, lactulose for hepatic encephalopathy, combination aldosterone antagonists and loop diuretics for ascites, and terlipressin for hepatorenal syndrome.
Accepted for Publication: March 27, 2023.
Corresponding Author: Elliot B. Tapper, MD, Division of Gastroenterology and Hepatology, University of Michigan, 3912 Taubman, 1500 E Medical Center Dr, Ann Arbor, MI 48109 ( [email protected] ).
Conflict of Interest Disclosures: Dr Tapper reported grants from Salix Pharmaceuticals and consulting fees from Madrigal Pharmaceuticals and Novo Nordisk, all paid to his institution, and consulting fees from Bausch Health, Mallinckrodt Pharmaceuticals, Axcella Health, Novo Nordisk, Ambys Medicines, Lipocine, Kaleido, and Takeda Pharmaceutical Company. Dr Parikh reported receiving grants from Exact Sciences, Genentech, Glycotest Inc, and Target PharmaSolutions and personal fees from Eli Lilly, Freenome, Eisai, Gilead Sciences, Bayer, Exelixis, and Fujifilm Medical.
Funding: This study was funded by a grant from the National Institutes of Health (U01DK130113).
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Search Menu
- Sign in through your institution
- Why Publish with Gastroenterology Report
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Gastroenterology Report
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Etiological overlap must receive attention in lc, hepatic and systemic inflammation should be evaluated for lc, non-invasive measurements should be developed for lc diagnosis, lc stage and liver function classification must be accurately estimated, measures of hepatic venous pressure gradient (hvpg) should be recommended, etiological treatment is vital, maintenance of a sufficient blood supply of the portal vein, strengthening nutritional support therapy, endoscopic sequential therapy is able to eradicate gastroesophageal varices and reduce the death rate of rebleeding, early diagnosis and early treatment are pivotal for lc-supervened hcc, standardized follow-up and management, as well as health education, are important for lc patients, integrating palliative care into routine clinical management is a contentious issue for lc, conflict of interest, critical issues in the diagnosis and treatment of liver cirrhosis.
- Article contents
- Figures & tables
- Supplementary Data
Xing Wang, Bin Wu, Critical issues in the diagnosis and treatment of liver cirrhosis, Gastroenterology Report , Volume 7, Issue 4, August 2019, Pages 227–230, https://doi.org/10.1093/gastro/goz024
- Permissions Icon Permissions
Liver cirrhosis (LC) is a worldwide health problem that is associated with various complications and high mortality. Although, in the past four decades, the incidence of hepatitis B continuously decreased and a promising cure for hepatitis C was developed, LC remains a formidable challenge in clinical practice due to the ever-increasing incidences of alcoholic and non-alcoholic fatty liver diseases, autoimmune-related liver disease and drug-induced liver disease [ 1–3 ]. Our survey data showed a significant increase in the inpatient percentages of alcoholic LC and autoimmune LC, with concomitant decreases in viral hepatitis LC, which contributes to the overall increasing incidence of LC in China [ 4 ]. As a spacious country with a large population, a discrepancy exists in medical specialties and several topics should therefore receive more attention in the management of LC. To aid broad gastroenterologists and heatologists as well as physicians, we identified the following critical issues in the diagnosis and treatment of LC.
Cirrhosis with two or more mixed etiologies should be carefully identified, despite high prevalences of hepatitis B virus (HBV) and hepatitis C virus (HCV) cirrhosis. We conducted a large-scale, cross-sectional study and found that the proportions of LC inpatients with HBV/HCV coinfection, HBV/alcohol coexistence and HBV/HCV/alcohol coexistence were 0.58%, 4.81% and 0.14%, respectively [ 4 ]. We also observed cases of HBV with fatty liver disease, cases of HBV with Wilson’s disease and cases of HBV with hemochromatosis; cases with as many as four overlapping etiologies were not rare. HBV/HCV coinfection has been reported to be associated with higher rates of severe liver disease and with a 2- to 5-fold increased risk of hepatic decompensation [ 5 ], whereas multicenter studies have shown that alcohol abuse significantly increased long-term incidences of hepatocellular carcinoma (HCC) in HBV-related and HCV-related cirrhotic patients [ 6 ]. When considering the fact that multi-etiologic cirrhosis may result in a worse prognosis, treatments that target all of the underlying etiologies are necessary to achieve favorable curative effects.
Activated Kupffer cells and monocytes initially induce inflammatory reactions in LC, after which the levels of TNF-α and other pro-inflammatory cytokines increase, and natural killer cells, natural killer T cells and macrophages are activated to aggravate systemic inflammation [ 7 ]. Inflammatory evaluations have always been ignored when staging fibrosis, but the measurement of liver stiffness is emphasized. Instead, more attention should be focused on the focal inflammation of the liver parenchyma by liver biopsies and on systemic inflammation by the detection of serum or humoral inflammatory biomarkers. The control of the liver parenchyma and systemic inflammation has been observed to be able to slow the progression of decompensated LC or even reverse fibrosis to some extent [ 8 ].
Cirrhosis usually develops from chronic hepatitis and transitions into compensated cirrhosis, after which there is a progression into decompensated cirrhosis. The early diagnosis of LC is difficult due to the absence of overt symptoms, the patient’s neglect and a lack of appropriate biomarkers. Traditional liver biopsies have been widely accepted as the gold standard for the evaluation of liver fibrosis and liver parenchymal inflammation. Although liver biopsies are very safe with the use of ultrasonic guidance, these biopsies are still invasive procedures. Non-invasive serum fibrosis biomarkers are highly applicable and easily repeatable, and newly developed markers, including procollagen type III N-terminal peptide (PIIINP) and YKL-40, have been demonstrated to be of great value in detecting advanced fibrosis or cirrhosis with both a sensitivity and specificity of approximately 80%. However, none of the fibrotic markers is liver-specific; thus, these markers may be influenced by non-hepatic inflammation. On the other hand, numbers of composite score models combining multiple serum markers have been developed to accurately evaluate the degree of liver fibrosis. As two of the most validated models, the AST-platelet ratio index and fibrosis-4 (FIB-4) index have shown comparable results in excluding advanced, but not moderate, fibrosis [ 9 ]. Liver-specific markers and new score models are being exploited and show promise for more specific diagnoses in the near future. With regard to imaging methods for the diagnosis of liver fibrosis, routine ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) is not accurate enough for early diagnoses, whereas FibroScan and FibroTouch tests have certain reference values but are subject to inter-observer variation. Increasing amounts of data have shown that real-time shear wave elastography and magnetic resonance elastography are the most promising and efficient evaluations for the early diagnosis of LC with respect to multi-sectional inspection, objectivity, sensitivity for early fibrosis and the ability to examine the entire liver [ 10 , 11 ]. Recent studies have observed that the ultrasound measurements of the stiffnesses of the liver or spleen are promising tools for detecting clinically significant portal hypertension and for excluding severe portal hypertension, although these methods were limited by heterogeneous values and an inapplicability in hepatic decompensation [ 12 ].
The Child-Pugh-Turcotte classification system is still of clinical value and has long been regarded as the most convenient measurement for LC clinical staging, although the score may be influenced by inter-observer variance. The Model for End-Stage Liver Disease (MELD) score incorporates serum creatinine levels, serum bilirubin levels and the international normalized ratio (INR); thus, it is likely to be more accurate in evaluating the disease severity and in predicting prognoses. Furthermore, the MELD score is crucial in assessing the need for liver transplantations. The Metavir score system has been widely used for the staging of liver fibrosis, with scores ranging from F0 (no fibrosis) to F4 (cirrhosis), and ultrasound elastography has been increasingly accepted as a non-invasive and valuable approach for distinguishing patients with no or minimal fibrosis (F0/F1), as well as those with severe fibrosis or cirrhosis (F3/F4) [ 13 ].
HVPG is the best indicator for portal pressure. A HVPG ≥10 mmHg is associated with an increased risk of developing gastroesophageal varices (GEV), whereas a HVPG ≥12 mmHg can identify a risk of bleeding and a HVPG ≥20 mmHg can predict the failure to control acute variceal bleeding, early rebleeding and bleeding-related deaths [ 14 ]. Hepatic vein catheterization with the use of a balloon-tipped catheter is currently the preferred technique in determining HVPG, which is highly recommended in qualified liver care centers. Given that HVPG measurements are invasive, costly and difficult in terms of obtaining real-time continuous surveillance, the Baveno VI guideline recommended a combination of liver stiffness that is less than 20 kPa in transient elastography and a peripheral platelet count that is higher than 150,000/µL to preclude the risk of a variceal hemorrhage [ 15 ]. Non-invasive HVPG measurements have been introduced; however, these measurements are pending until they can be proved to be effective in clinical practice and practically accurate, non-invasive approaches for HVPG measurements are highly expected.
The etiological treatment of LC is critical, although it is usually ignored in the decompensated stage. Patients should be initially treated with a direct-acting antiviral (DAA) treatment as soon as HCV is identified. Hepatitis B cirrhosis is the predominant etiology in China and mounting data have shown that the early use of antiviral therapy may alleviate cirrhotic progression and reduce the risk of HCC [ 16 ]. Moreover, both the American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of the Liver (EASL) guidelines advocate that the patient should undergo antiviral therapy regardless of the levels of HBV-DNA and alanine aminotransferase, as well as the HBeAg status, when the patient has a positive result for HBV-DNA test [ 17 , 18 ]. Alcohol cessation is the key issue for alcoholic LC treatment, whereas psychological interventions may be essential for alcohol addicts. Adequate physical exercise, the treatment of comorbid metabolic syndrome and an early referral to a dietician are helpful for patients with non-alcoholic fatty liver disease that is related to LC. With regard to AIH-related LC, physicians should optimize a therapy of steroids and immunosuppressants for the etiological treatment.
Given that the liver is an organ with a dual blood supply from the portal vein and the hepatic artery, the maintenance of sufficient perfusion is significant for ensuring the nourishment of this organ. Injuries to the portal vein, which may occur as a result of devascularization surgery, a surgical portosystemic shunt, a splenectomy, an endoscopic tissue glue injection or radio-interventional therapy, should be carefully avoided to reduce the possibility of a portal vein thrombosis (PVT). PVTs have long been a difficult clinical problem. Although warfarin has been a traditionally efficient treatment, the dose titration highly relies on repeated INR tests and may result in poor patient compliance [ 19 ]. New generations of oral anticoagulants, including rivaroxaban and dabigatran, have been proved to be effective, but they are also expensive. Failed cases that result from the use of anticoagulation therapy should consider the use of interventional portal vein recanalization techniques, including balloon angioplasty, stent-placement, thrombectomy and thrombolysis [ 20 ].
Malnutrition occurs in up to 80% of overall cirrhotic patients and in nearly all decompensated patients [ 21 ]. This complication comprises protein malnutrition, energy malnutrition and mixed malnutrition, which are highly related to insufficient intake, absorption dysfunction and a high catabolic status. Impaired nutritional situations will induce ascites and infection, will aggravate variceal bleeding and will increase mortality; therefore, cirrhotic patients should adhere to an adequate diet of sufficient calories and protein. Food supplements involving essential amino acids are able to promote protein synthesis and improve the outcomes of malnutrition, whereas proper physical exercise also helps in energy intake and nutritional rehabilitation [ 22 ].
As the most lethal complication of LC, gastroesophageal variceal bleeding (GEVB) occurs in 0%–40% of compensated cirrhosis and in 70%–80% of decompensated cirrhosis. Moreover, 20%–50% of patients will rebleed after the first bleeding episode and this proportion of patients is associated with 20% of 6-week mortality and 15% of in-hospital mortality [ 23 ]. When considering that LC patients also have intestinal variceal bleeding risks due to portal hypertension, early endoscopy screening should be advocated for the evaluation of the bleeding risk of not only GEV, but also of the small intestinal and colorectal varices. The endoscopic management of GEV has been proven to be effective and has been widely used in primary hospitals. However, it is common in China that patients will attend one or two treatment sessions for acute bleeding but will not attend subsequent follow-up sessions until recurrent bleeding occurs. Our preliminary data from a cirrhotic cohort showed that, after variceal eradication by endoscopic sequential therapy that combined band ligation, tissue glue injection and sclerotherapy, the 5-year occurrence rate of rebleeding and all-cause death rate were reduced to 9.6% and 3.4%, respectively (data not shown). Furthermore, endoscopic treatments should be repeated and sequenced until complete variceal eradication occurs, after which the patients should receive follow-ups with regular 6- to 12-month intervals.
Primary liver cancer contributes to 4.7% of global malignancies and 8.2% of cancer mortalities. Cancer statistics in China showed that the incidence of liver cancer ranks third in men and sixth in women, and the mortality ranks third in men and fourth in women [ 24 ]. Early interventions with DAA drugs may prevent cancerization and may prolong the cancer-free survival period. The early diagnosis rate of HCC is still low, which is partially due to asymptomatic features and neglect by the patients. Ultrasound screening is still the first choice that is applicable for primary healthcare institutions, whereas CT/MRI is more accurate but costly. Biomarkers represent a promising direction. However, even though alpha-fetoprotein (AFP) is a classical marker, its sensitivity and specificity are not high. We recently identified a novel biomarker (Lnc-PCDH9-13: 1) that has >80% of sensitivity and >98% of specificity for early HCC diagnoses, and the biomarker is detectable in both serum and saliva. Therefore, the use of this biomarker is more convenient for clinic follow-ups and community surveys than traditional AFP detection [ 25 ]. For every LC patient, ultrasound should be administered every 6 months and a subsequent CT/MRI is necessary when a suspicious carcinoma is discovered. Regular surveillance will promote early detection and may benefit subsequent treatments.
Regular follow-ups involving clinic visits and laboratory tests are able to monitor disease progression and modulate the timely use of therapies. Patients should undergo complete blood counts, liver biochemistry tests, electrolyte tests, coagulation measurements, AFP measurements and tests for viral loads of HBV and/or HCV every 3 months. Nutritional evaluation should also be carried out every 3 months to investigate the risk of hypoalbuminemia, as well as to treat malnourishment. Ultrasonic examination should be performed every 6 months to examine the liver parenchyma and to detect changes in the portal vein, in order for occurrences of HCC and PVT to be quickly identified. Furthermore, an annual CT or MRI is necessary for the surveillance of cirrhosis progression and HCC. Regular endoscopic examinations of the upper and lower gastrointestinal tract are recommended to investigate the variceal situation and bleeding risk. The medical center should establish a comprehensive follow-up database to systematically manage patients. In addition, health education for the patients themselves, as well as their family members, is also important to guide rehabilitation, to improve the quality of life and to increase the survival of LC patients.
End-stage liver disease (ESLD), encompassing advanced liver disease, liver failure and decompensated cirrhosis, is associated with a high mortality and a high degree of symptom burden and it affects approximately 6 million people in the USA [ 26 ]. Palliative care (PC) as an approach for improving the quality of life of patients and families who are facing a life-limiting illness has become an emerging debated issue in the field of ESLD treatment. Increasing amounts of data have shown beneficial effects of PC, including the alleviation of patient-reported symptoms, a reduction in the overall cost of care and even prolonged survival. However, PC consultation is still underused in cirrhotic patients and only approximately 5% of hospitalized patients with decompensated cirrhosis received this kind of service [ 27 ]. The broader implementation of PC is hindered by a shortage of qualified providers, a lack of public reimbursement, the misconceptions of patients and healthcare providers, and a dearth of relevant research. Access to PC services is mainly limited to Western countries and little is known about the clinical application of PC in developing countries, including China. Better organization and financing of PC services are greatly needed and more data focusing on how to best integrate PC into the ESLD workflow are highly needed in the future.
The study was supported in part by grants from the National Natural Science Foundation of China (U1501224), the Natural Science Foundation Team Project of Guangdong Province (2018B03031200), the Science and Technology Developmental Foundation of Guangdong Province (2017B020226003) and the Science and Technology Program of Guangzhou City (201604020118).
The authors declare that they have no conflicts of interest.
Allen AM , Kim WR , Moriarty JP et al. Time trends in the health care burden and mortality of acute on chronic liver failure in the United States . Hepatology 2016 ; 64 : 2165 – 72 .
Google Scholar
Tapper EB , Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study . BMJ 2018 ; 362 : k2817.
GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 . Lancet 2018 ; 392 : 1015 – 35 .
Wang X , Lin SX , Tao J et al. Study of liver cirrhosis over ten consecutive years in Southern China . World J Gastroenterol 2014 ; 20 : 13546 – 55 .
Mavilia MG , Wu GY. HBV-HCV coinfection: viral interactions, management, and viral reactivation . J Clin Transl Hepatol 2018 ; 6 : 296 – 305 .
Lin CW , Lin CC , Mo LR et al. Heavy alcohol consumption increases the incidence of hepatocellular carcinoma in hepatitis B virus-related cirrhosis . J Hepatol 2013 ; 58 : 730 – 5 .
Noor MT , Manoria P. Immune dysfunction in cirrhosis . J Clin Transl Hepatol 2017 ; 5 : 50 – 8 .
Bernardi M , Caraceni P. Novel perspectives in the management of decompensated cirrhosis . Nat Rev Gastroenterol Hepatol 2018 ; 15 : 753 – 64 .
Lurie Y , Webb M , Cytter-Kuint R et al. Non-invasive diagnosis of liver fibrosis and cirrhosis . World J Gastroenterol 2015 ; 21 : 11567 – 83 .
Wang K , Lu X , Zhou H et al. Deep learning radiomics of shear wave elastography significantly improved diagnostic performance for assessing liver fibrosis in chronic hepatitis B: a prospective multicentre study . Gut 2019 ; 68 : 729 – 41 .
Procopet B , Berzigotti A. Diagnosis of cirrhosis and portal hypertension: imaging, non-invasive markers of fibrosis and liver biopsy . Gastroenterol Rep (Oxf) 2017 ; 5 : 79 – 89 .
Song J , Huang J , Huang H et al. Performance of spleen stiffness measurement in prediction of clinical significant portal hypertension: a meta-analysis . Clin Res Hepatol Gastroenterol 2018 ; 42 : 216 – 26 .
Li C , Li R , Zhang W. Progress in non-invasive detection of liver fibrosis . Cancer Biol Med 2018 ; 15 : 124 – 36 .
Garcia-Tsao G , Abraldes JG , Berzigotti A et al. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases . Hepatology 2017 ; 65 : 310 – 35 .
de Franchis R ; Baveno VI Faculty. Expanding consensus in portal hypertension: report of the Baveno VI Consensus Workshop: stratifying risk and individualizing care for portal hypertension . J Hepatol 2015 ; 63 : 743 – 52 .
Marcellin P , Gane E , Buti M et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study . Lancet 2013 ; 381 : 468 – 75 .
Terrault NA , Lok ASF , McMahon BJ et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance . Hepatology 2018 ; 67 : 1560 – 99 .
European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection . J Hepatol 2017 ; 67 : 370 – 98 .
Hanafy AS , Abd-Elsalam S , Dawoud MM. Randomized controlled trial of rivaroxaban versus warfarin in the management of acute non-neoplastic portal vein thrombosis . Vascul Pharmacol 2019 ; 113 : 86 – 91 .
Priyanka P , Kupec JT , Krafft M et al. Newer oral anticoagulants in the treatment of acute portal vein thrombosis in patients with and without cirrhosis . Int J Hepatol 2018 ; 2018 : 8432781.
European Association for the Study of the Liver. EASL clinical practice guidelines on nutrition in chronic liver disease . J Hepatol 2019 ; 70 : 172 – 93 .
Moctezuma-Velazquez C , Garcia-Juarez I , Soto-Solis R et al. Nutritional assessment and treatment of patients with liver cirrhosis . Nutrition 2013 ; 29 : 1279 – 85 .
Cabrera L , Tandon P , Abraldes JG. An update on the management of acute esophageal variceal bleeding . Gastroenterol Hepatol 2017 ; 40 : 34 – 40 .
Bray F , Ferlay J , Soerjomataram I et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries . CA Cancer J Clin 2018 ; 68 : 394 – 424 .
Xie Z , Zhou F , Yang Y et al. Lnc-PCDH9-13:1 is a hypersensitive and specific biomarker for early hepatocellular carcinoma . EBioMedicine 2018 ; 33 : 57 – 67 .
Potosek J , Curry M , Buss M et al. Integration of palliative care in end-stage liver disease and liver transplantation . J Palliat Med 2014 ; 17 : 1271 – 7 .
Rush B , Walley KR , Celi LA et al. Palliative care access for hospitalized patients with end-stage liver disease across the United States . Hepatology 2017 ; 66 : 1585 – 91 .
| Month: | Total Views: |
|---|---|
| June 2019 | 37 |
| July 2019 | 24 |
| August 2019 | 251 |
| September 2019 | 276 |
| October 2019 | 294 |
| November 2019 | 334 |
| December 2019 | 242 |
| January 2020 | 221 |
| February 2020 | 165 |
| March 2020 | 110 |
| April 2020 | 85 |
| May 2020 | 79 |
| June 2020 | 113 |
| July 2020 | 138 |
| August 2020 | 185 |
| September 2020 | 164 |
| October 2020 | 152 |
| November 2020 | 196 |
| December 2020 | 137 |
| January 2021 | 138 |
| February 2021 | 165 |
| March 2021 | 272 |
| April 2021 | 244 |
| May 2021 | 164 |
| June 2021 | 114 |
| July 2021 | 138 |
| August 2021 | 90 |
| September 2021 | 166 |
| October 2021 | 228 |
| November 2021 | 197 |
| December 2021 | 104 |
| January 2022 | 86 |
| February 2022 | 104 |
| March 2022 | 160 |
| April 2022 | 119 |
| May 2022 | 120 |
| June 2022 | 81 |
| July 2022 | 80 |
| August 2022 | 87 |
| September 2022 | 101 |
| October 2022 | 134 |
| November 2022 | 131 |
| December 2022 | 84 |
| January 2023 | 112 |
| February 2023 | 136 |
| March 2023 | 126 |
| April 2023 | 113 |
| May 2023 | 74 |
| June 2023 | 62 |
| July 2023 | 88 |
| August 2023 | 106 |
| September 2023 | 137 |
| October 2023 | 104 |
| November 2023 | 92 |
| December 2023 | 98 |
| January 2024 | 84 |
| February 2024 | 111 |
| March 2024 | 94 |
| April 2024 | 126 |
| May 2024 | 94 |
| June 2024 | 55 |
| July 2024 | 94 |
| August 2024 | 49 |
| September 2024 | 10 |
Email alerts
Citing articles via, affiliations.

- Online ISSN 2052-0034
- Copyright © 2024 Oxford University Press and Sixth Affiliated Hospital of Sun Yat-Sen University
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
An evidence-based treatment approach
Casler, Kelly DNP, APRN, FNP-BC, EBP-C, CHSE; Chaney, Amanda DNP, APRN, FNP-BC, FAANP
Kelly Casler is an assistant professor of clinical nursing at The Ohio State University College of Nursing, Columbus, Ohio, and FNP at The Healthcare Connection, Lincoln Heights, Ohio.
Amanda Chaney is Chair of the Advanced Practice Provider Subcommittee and senior NP at the Department of Transplant at the Mayo Clinic, Jacksonville, Fla.
The authors and planners have disclosed no potential conflicts of interests, financial or otherwise.
The NP's role in managing cirrhosis is increasing due to the growing prevalence of the disease. The purpose of this article is to review the pathophysiology, diagnosis, and management of patients with cirrhosis with an emphasis on interdisciplinary collaboration and evidence-based practice. Cirrhosis complications are also discussed.

Cirrhosis is reported to be one of the most challenging chronic conditions healthcare providers must manage, yet evidence suggests that primary care providers (PCPs) will take on more of the burden of care as the disease becomes more prevalent. 1 Therefore, it is imperative that NPs understand the challenges and best practices of managing this common chronic disease.
Epidemiology
Cirrhosis prevalence has increased over the last 20 years with higher disease rates seen in impoverished and Black patients. 2,4 It is the 12th leading cause of death in the US, causing at least 1 million deaths annually. 3,4 Underdiagnosis is common; over two-thirds of patients are unaware that they have liver disease. This is concerning given that cirrhosis confers a higher risk of mortality than many other chronic diseases. 1,4 Annually, 30 billion dollars are spent on care of patients with cirrhosis. 2
Pathophysiology
Cirrhosis starts with an initial injury or inciting event to the liver that triggers an inflammatory response. The most common inciting events in the US are viral infections (hepatitis B or C), nonalcoholic steatohepatitis (caused by excess carbohydrates and calories), and alcoholic liver disease (excess alcohol) (see Chronic liver conditions that can lead to cirrhosis ). 5,6 In response to inflammation, new blood vessels form, extracellular matrix proliferates, and new hepatocytes migrate to the area, replicating excessively. Angiogenesis becomes abnormal and fibrosis develops. The fibrosis coalesces, causing nodules to replace normal liver tissue. 7 Fibrosis then advances from mild to severe, with the most severe fibrosis leading to cirrhosis. During this time, the liver attempts to regenerate normal functioning liver tissue in between diseased areas and these regenerative nodules give the cirrhotic liver its hallmark lumpy appearance (see Progression to cirrhosis and its complications ). Recovery and regression of early fibrosis is usually possible if the damaging event is removed. However, liver transplant has been traditionally thought of as the only cure once cirrhosis develops. 7 But new research is exploring the reversibility of liver cirrhosis. 8,9 Since progression toward cirrhosis is slow, taking 2 to 3 decades, cirrhosis is most often diagnosed in the fourth or fifth decade of life. However, recent data reveal that diagnosis is occurring at younger ages than in past decades. 2,4
A healthy liver performs a wide range of functions including carbohydrate and lipid metabolism; breakdown of medications, ammonia, and bilirubin; and synthesis of albumin and coagulation factors. 10 Kupffer cells help with immune system regulation and hepatocytes produce bile, which is critical for digestion and absorption of fat-soluble vitamins. 10 Cirrhosis can cause dysfunction affecting one or more of these primary liver functions. Additionally, persistent alterations in cellular homeostasis during cirrhosis can lead to increased propensity for hepatocellular neoplasm. 8

Cirrhosis of the liver also alters the hepatic vasculature, which results in portal hypertension, a state of increased pressure in the portal venous system. As the pressure inside the liver increases, blood flow is restricted, and blood vessels become congested and engorged with blood. As this occurs over months to years, this pressure increase can cause damage to the vessel walls and chronic inflammation. Ultimately, portal hypertension can lead to complications of esophageal varices, portal hypertensive gastropathy, and ascites. Additionally, patients may develop portal vein thrombosis that can further complicate blood flow to and from the portal circulation.
Cirrhosis is classified as either compensated or decompensated. Compensated cirrhosis is often asymptomatic and may therefore go undetected. 1 Conversely, decompensated cirrhosis is manifested by complications; the most common are ascites, esophageal varices, and hepatic encephalopathy. Comorbidities, such as diabetes, predispose a patient to a higher likelihood of decompensation. 11 Prognosis is poor following decompensation. 12 While life expectancy estimate for compensated cirrhosis is 12 or more years, life expectancy for decompensated cirrhosis is approximately 2 years. 12 Therefore, when a patient moves from compensated to decompensated cirrhosis, referral to a transplant center for liver transplant evaluation is warranted.
Evaluation of patients with cirrhosis
As with any chronic illness, a thorough history, physical exam, and diagnostic evaluation is important. During this time, the NP may evaluate for signs of cirrhosis, identify the underlying etiology of liver disease, and intervene for improved outcomes (see Signs and symptoms of cirrhosis and underlying pathophysiology ). For example, treatment of hepatitis C and abstinence from alcohol can improve complication rates and life expectancy in patients with cirrhosis. 8,13
Two of the most common lab tests to monitor and evaluate cirrhosis are alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Although it is frequently assumed that both AST and ALT are elevated in patients with cirrhosis, their levels can be normal during compensated cirrhosis and even sometimes, decompensated cirrhosis. 12,14 Consequently, although these tests are frequently referred to as “liver function tests,” they should actually be referred to as liver enzymes or liver transaminases, since they do not reflect how well the liver is functioning. 14 True “liver function tests” include albumin, prothrombin time (PT)/international normalized ratio (INR), and bilirubin. However, even these tests may not show variation until late in decompensated cirrhosis, at which point albumin levels will be reduced and PT/INR will be elevated. Thrombocytopenia can be an early lab clue to cirrhosis, since it can occur in the early stages of portal hypertension. 12,15 Patients should be evaluated for possible cirrhosis when platelet levels fall below 160,000/mm 3 . 13

Several diagnostic tests are used in the evaluation and monitoring of cirrhosis. Ultrasound will often show splenomegaly during cirrhosis and portosystemic collateral veins with worsening cirrhosis. 15 The gold standard to diagnose fibrosis and cirrhosis is liver biopsy, but the invasiveness of the procedure limits its usefulness. Therefore, transient liver elastography is frequently used to evaluate for advanced fibrosis. 16 Other mechanisms for fibrosis and cirrhosis diagnosis, such as serum biomarkers, are being studied, but not yet FDA-approved.
Evaluation and management of cirrhosis complications
Ascites, hepatic encephalopathy, and esophageal/gastric varices are the three most common complications seen in decompensated cirrhosis. However, there are several other possible complications that require monitoring (see Monitoring for complications of cirrhosis ).
Ascites . Ascites is the most common complication of cirrhosis with almost one half of patients with compensated cirrhosis developing it over a 10-year period. 13,17 Sometimes, the diagnosis of ascites is the first clue to prompt the identification of cirrhosis. Ascites is thought to occur due to disrupted equilibrium between the intravascular and extravascular space when portal hypertension results in elevated hydrostatic pressure and hypoalbuminemia results in decreased osmotic pressure. As a consequence, fluid accumulates in the peritoneal space. 10,15
Evaluation of patients with ascites may show a positive fluid wave test. A fluid wave test is performed by having the patient lay supine and push down on the midline of their abdomen with their hands. The NP then places one hand on each side of the patient's flank area and alternates tapping each flank, feeling for an impulse that transmits across the abdomen. However, ascites may be hard to diagnose in this manner, especially in patients with large abdominal girth or only a small amount of ascitic fluid. An ultrasound can confirm ascites. 17,18

Diet and medication can help manage ascites. A dietary sodium restriction of 2,000 mg per day is recommended, though evidence for its success is low. 17,19,20 Two diuretics, spironolactone (a potassium-sparing diuretic) and furosemide (a loop diuretic), are often used together to manage ascites while maintaining a normal potassium level. Single morning dosing will help avoid nocturia and increase the likelihood of compliance. It is important to closely monitor kidney function and watch for hyponatremia when initiating and titrating doses and prescribing high doses. Even a small increase in creatinine within the normal range, such as 0.3 mg/dL, can signal acute kidney injury. Diuretics should be stopped in the presence of hepatic encephalopathy, sodium level less than 120 mEq/L, or a creatinine level more than 2.0 mg/dL. 19
Another method of ascites management is paracentesis. Current clinical guidelines suggest that patients should have a paracentesis as soon as possible (within 1 month) of the first episode of ascites in order to evaluate the fluid. 18,21 Paracentesis may also be needed for ascites that is refractory to diuretics and sodium restriction. In order to provide renal protection from volume loss, albumin infusion is suggested following paracentesis when more than 5L of fluid is removed. 17 If paracentesis is required frequently, it may be a clue to worsening decompensation or inability to adhere to sodium restriction or diuretics. 13,17 Other methods for ascites management include a transjugular intrahepatic portosystemic shunt (TIPS) (see Transjugular intrahepatic portosystemic shunt ), which is more effective than paracentesis for severe or refractory ascites. 22

Spontaneous bacterial peritonitis
Spontaneous bacterial peritonitis can be a complication of ascites and is usually caused by a translocation of bacteria from the gut to the ascitic fluid. It is defined by a polymorphonuclear leukocyte count of at least 250 cells/mm 3 in ascitic fluid and/or positive ascitic fluid cultures. 13 This diagnosis should be suspected when a patient develops fever, abdominal pain, and/or leukocytosis. When this happens, it is important to perform paracentesis as soon as possible (within 12 hours of first suspicion) to confirm the diagnosis and collect cultures since prompt treatment is associated with better patient outcomes. 13
Hepatic encephalopathy
Hepatic encephalopathy (HE) is another common cirrhosis complication, and perhaps the most complex complication to identify. 13,23 Although the pathophysiology of HE is not fully understood, it is thought to develop due to excess accumulation of ammonia in the bloodstream, which then crosses the blood brain barrier and becomes neurotoxic. Normally, hepatocytes break down the ammonia produced by intestinal bacteria, a process that is impaired in cirrhosis. Portosystemic shunting can also cause HE since it hinders the delivery of ammonia to hepatocytes for detoxification. 10
The course of HE is often unpredictable and the diagnosis is challenging. 24 This is partially due to variability and the subtle nature of symptoms. 24 HE can be categorized as covert and overt; the West Haven criteria are also used to categorize HE from Grade 0 (no symptoms) through 4 (coma). 24,25 (See Resources for NPs caring for patients with cirrhosis .) Symptoms may be overlooked during early stages and covert HE due to their subtle nature. These subtle symptoms include attention deficits, psychomotor slowing, insomnia, daytime sleepiness, apathy, and mild hypokinesia. 13,23,25 NPs should engage the patient's caregiver in discussions involving history to achieve accurate evaluation since patients tend to avoid specific questions and “hide” their confusion. The psychometric hepatic encephalopathy score (PHES), the critical flicker frequency (CFF), and the Trail Making test are useful objective tests to supplement the physical exam and identify covert HE. 13 Other tools, such as online applications, are available for diagnostic guidance. Patients with overt HE are more easily diagnosed as they may exhibit asterixis or hyperactive deep tendon reflexes. 13 Further complicating diagnosis, HE can be episodic, recurrent, or persistent and may either be spontaneous or precipitated by problems such as a urinary tract infection (UTI), medication noncompliance, or electrolyte imbalances. 25

HE is a clinical diagnosis and the nonspecific signs and symptoms associated with it necessitate ruling out alternate diagnoses. 25 Diagnostic evaluation should include evaluation for a precipitating event; the most common are infection and electrolyte abnormalities. Usual workup should include electrolyte evaluation and infection evaluation (that is, lactate, two sets of blood cultures, a urinalysis if patient presents symptoms of UTI, and stool studies if there is presence of diarrhea). 13,26-28,30 Although traditionally used in the evaluation of HE, recent research shows that ammonia lacks sufficient sensitivity and specificity to be helpful in HE diagnosis and monitoring and is no longer recommended as a diagnostic tool. 26,27
Treatment options for HE focus on intestinal elimination of ammonia before it makes its way to the bloodstream or reduction of intestinal ammonia production. Lactulose is a nonabsorbable disaccharide that alters the pH of the colon and reduces the absorption of ammonia. It causes frequent, loose stools. Once HE is resolved, doses are titrated toward a goal of two to three bowel movements per day to prevent future HE episodes. Lactulose is continued indefinitely, but there is increased risk of dehydration and hypernatremia when bowel movements exceed five per day. 27-29 Adverse reactions of lactulose include bloating, diarrhea, dehydration, electrolyte abnormalities, cramping, nausea, and/or vomiting.
Antibiotics are added to lactulose therapy in the case of continued recurrent HE episodes. Rifaximin is an antibiotic that targets bacteria in the intestines, reducing ammonia production. 25,28 Drawbacks to rifaximin include high cost and prior authorization requirements. Less commonly used antibiotics include neomycin, metronidazole, and vancomycin.
HE management includes correcting electrolyte imbalances and optimizing nutrition with a high protein diet to avoid HE exacerbation. 24,25 Additionally, NPs caring for patients with a diagnosis of HE will want to consider referral to a fitness-to-drive assessment performed by occupational therapists or state agencies to ensure that it is safe for patients to operate vehicles. 30
Esophageal and gastric varices
Esophageal and gastric varices are concerning sequelae to the congestion of portal hypertension. They can ooze or burst causing severe blood loss, anemia, and multiorgan failure. Therefore, all patients should be screened for varices within 12 months of cirrhosis diagnosis using esophagogastroduodenoscopy (EGD). 21
The goal in management of varices is to prevent bleeding. When bleeding does occur, patients require hospitalization, most often in the ICU where they are administered blood products to maintain hemoglobin greater than 7 g/dL. 13,31 Beta-blockers are used to prevent bleeding from existing varices, but they are not effective at preventing the formation of varices. 13 Nonselective beta-blockers like propranolol, nadolol, and carvedilol should be chosen since optimized blood flow occurs from beta-2 effects rather than beta-1 effects. 15 Carvedilol is unique in that it also exhibits some anti-alpha-1 adrenergic effects allowing for beneficial vasodilation in intrahepatic circulation. 15 Beta-blockers should be discontinued in the presence of any of the following: mean arterial pressure (MAP) less than 80 mm Hg, systolic BP less than 100 mm Hg, sodium concentration less than 120 mEq/L, refractory ascites, hepatorenal syndrome (HRS), or episodes of spontaneous bacterial peritonitis. 13
Endoscopic variceal ligation is also used to manage varices. This procedure is completed at the time of initial EGD and involves placing rubber bands around the varices to cut off the blood supply. Unfortunately, varices often recur after banding since there is no underlying treatment of the portal hypertension. In these cases, patients can also undergo local therapies such as injection of a cyanoacrylate glue or sclerotherapy. Additionally, patients with severe decompensated cirrhosis and varices may undergo TIPS. 15
Other complications of cirrhosis
Other complications of cirrhosis such as hepatopulmonary syndrome, hepatic hydrothorax, and portopulmonary hypertension cause respiratory dysfunction and often require supplemental oxygen. Hepatopulmonary syndrome results from intrapulmonary vascular dilation and altered alveolar-arterial oxygen exchange and is diagnosed by combined testing with arterial blood gas and echocardiogram showing a PaO 2 less than 60 to 80 mm Hg and the presence of an intrapulmonary shunt, respectively. 32 Liver transplant is the only effective treatment for hepatopulmonary syndrome. Hepatic hydrothorax occurs when ascitic fluid moves into the right pleural space from a defect in the right diaphragm. Initial treatment options are the same as those for ascites. 13 Thoracentesis is an option for those with large volume effusions and/or severe symptoms. 19 Portopulmonary hypertension is defined by cirrhosis-associated pulmonary hypertension and causes fatigue, exertional dyspnea, orthopnea, and sometimes respiratory failure. Each of these complications exhibits specific clinical signs/symptoms with distinct recommendations for management.
HRS is a consequence of splanchnic vasodilation and subsequent decreased kidney perfusion. These patients also exhibit ascites and, usually, hyponatremia. 33 Hypovolemia and acute kidney injury should be ruled out prior to diagnosing HRS. 13 HRS is prevented through avoidance of nephrotoxic medications and hypotension. Volume expansion with albumin is recommended as first-line treatment; if no response is seen after 48 hours, vasoactive medications like midodrine and octreotide may be used. 19
Hepatocellular carcinoma (HCC) is a final complication of cirrhosis that warrants discussion. Globally, HCC is the fifth most common tumor and the fourth leading cause of cancer-related death. 34,35 Patients with cirrhosis are at high-risk for developing HCC, regardless of cirrhosis etiology; 80% of newly diagnosed HCC cases are in patients with cirrhosis. HCC prognosis is more favorable when the disease is diagnosed in early stages. HCC can be treated by resection, radiofrequency ablation, or chemoembolization. Transplant is also a potential option for those who meet criteria. Screening for HCC should be completed twice annually, although recent research has questioned whether screening improves mortality rates. 34-36
Management of the patient with cirrhosis
Care coordination . Care coordination between PCPs, hepatology/gastroenterology specialists, and other healthcare professionals results in improved patient outcomes and reduced hospital readmission rates for patients with cirrhosis. 13 However, patients perceive that communication and coordination among healthcare professionals is poor. 37 Thus, it is important for healthcare providers to work together to achieve quality of care. The care coordination process should focus on monitoring for changes in prognosis, patient and family education and support, health promotion, nutrition, and medication reconciliation and monitoring. Patients should be referred to hepatology or gastroenterology specialists as soon as possible after cirrhosis is suspected. After any hospitalization for cirrhosis decompensation, patients should follow up with their PCP within a week of discharge, although this recommendation is extrapolated from heart failure research. 17
Patients with cirrhosis should be routinely monitored for changes in prognosis. One method for monitoring prognosis and need for liver transplant is calculation of the Model for End-stage Liver Disease-Sodium (MELD-Na). 38 The MELD-Na Score uses INR, bilirubin, creatinine, serum sodium, and the need for dialysis to predict severity of disease and risk for poor outcomes. 39,40 An online calculator to determine the patient's MELD-Na score is available (see Resources for NPs caring for patients with cirrhosis ). Specialists begin liver transplant planning once the MELD score rises above 17 or a patient develops a cirrhotic complication. 17,26 Liver transplant planning is also indicated when medical interventions for complications become ineffective. 38
Palliative care and hospice services should be considered for patients with cirrhosis and are often underutilized. 41 All patients with cirrhosis qualify for palliative care and should be educated on its premise. 37 Palliative care can provide important interdisciplinary team members and an additional support system to reduce symptoms and improve quality of life. 41 Another important aspect of palliative care is the assistance of social workers in helping the patient and family make advanced care planning decisions. If a patient meets criteria for a liver transplant, but is unable to safely proceed, then a hospice referral is recommended. Other indications for hospice referrals are oliguria and refractory or recurrent cirrhosis complications. 41
Communication with the patient and caregivers while supporting and educating them is essential. Caregivers of patients with cirrhosis experience significant stress and, therefore, the importance of supporting them cannot be understated. 41 Patient education is important since patients lack the knowledge needed to manage their illness successfully and specifically need education on the symptoms and how they relate to the diagnosis and its complications. 37,42 Patients also usually have inadequate knowledge to manage the special nutrition needs of cirrhosis, so involvement of a registered dietitian is beneficial especially since malnutrition occurs in over 80% of patients, including patients with an elevated body mass index. 13,20,43,44 Patients should be advised about the hypermetabolic state seen in cirrhosis, choosing high-protein foods, and consuming a high-protein diet (1.0 to 1.5 grams of protein per kilogram of body weight per day). 13 Late evening meals with protein or protein nutritional supplements may help achieve this goal. Additional nutrition education is warranted based on other complications (that is, low sodium for ascites, fluid restriction for hyponatremia, and low carbohydrate for diabetes). 13
NPs should assure health promotion for patients with cirrhosis based on their age, gender, and other comorbidities. Additionally, all patients with cirrhosis should be vaccinated for hepatitis A and B to prevent new insults to the liver in the future. 21 Immunization for pneumococcal disease with pneumococcal polysaccharide vaccine (PPSV23) is also required regardless of age. 45 Alcohol avoidance is important since alcohol cessation can help stabilize cirrhosis symptoms and intake is linked to cirrhosis decompensation. 15,17
Astute medication management is important in cirrhosis. Some medication dosages may need to be reduced since cirrhosis results in decreased metabolism of drugs. 46 Additionally, medications should be evaluated for hepatotoxicity using resources such as LiverTox. 47 Unlike chronic kidney disease, for which glomerular filtration rate guides dosage adjustment, there is no single lab value available to reflect the severity of cirrhosis for medication dose adjustments. Prescribing references often suggest dosage adjustments based on the Child-Turcotte-Pugh score. 46 Pharmacist consultation is also helpful to determine optimal dosages.
Management of comorbidities
Cardiovascular disease is a common comorbidity that poses unique patient management concerns. Despite popular belief, statins can and should be continued during compensated cirrhosis. In fact, statins improve liver function by enhancing hepatic blood flow through intrahepatic vessel dilation. 15 Statins also partially reverse the endothelial dysfunction and fibrosis that is seen in portal hypertension. 15 The benefit of aspirin to prevent cerebrovascular accident and/or myocardial infarction should be carefully balanced with the increased risk for azotemia or gastrointestinal bleeding seen in cirrhosis. Additionally, all nonsteroidal anti-inflammatory drugs should be used with caution, and avoided if possible, due to decreased urinary sodium excretion and azotemia risks. 19 BP should be closely monitored in hypertensive patients, because patients may transition from hypertension to normotension, and possibly hypotension. As portal hypertension progresses, systemic vasodilation, increased nitric oxide release, and splenic artery vasodilation all create excessive blood vessel relaxation. Initially, the body compensates by increasing its vasoconstrictors, but over time it loses this compensatory mechanism. 17 When a patient's BP starts trending down, NPs should consider discontinuing antihypertensive medications since an MAP less than 80 mm Hg has been associated with poorer health outcomes and decreased survival in patients with cirrhosis. 13,17
Patients with cirrhosis may complain of pruritus; management of this complaint has mainly been studied in those with primary sclerosing cholangitis and primary biliary cholangitis. 48,49 Antihistamines are ineffective since the itch occurs from cholestasis rather than histamine release. 49 Cholestyramine is a first-line approach, but is an off-label use of the medication. Doses should be taken before or with a meal and at least 4 hours prior to other medications because of potential drug interactions. 48,49 Naltrexone and sertraline may be used if cholestyramine is ineffective, although this is an off-label use of these medications. Patients should also be counseled to use moisturizing lotion and cooling ointments (menthol, for example) twice a day and to keep nails trimmed short to prevent injury from scratching.
As many as 30% of patients with cirrhosis may experience depression. 50 Anxiety and insomnia are also common. Selective serotonin reuptake inhibitors are the safest class of medication to treat depression and anxiety in this group. Since medication clearance is reduced in cirrhosis, NPs should aim for a maintenance dose that is half of the usual dose. 50 Benzodiazepines should be avoided due to an increased risk of HE. Hydroxyzine or trazadone at bedtime may be safe, effective choices for insomnia although this is an off-label use. Refer to package inserts for guidance on appropriate dosing. Agents such as zolpidem and diphenhydramine should be avoided as they are related to increased HE risk. 13
Pain management for patients with cirrhosis can be challenging. Acetaminophen up to 2 grams a day is safe, though some patients may need stronger pain relievers. 13,51 The risk of opioid toxicity is increased in patients with cirrhosis and caution is advised. If opioids are used, medications to prevent constipation should be coprescribed, and only immediate-release forms should be given. For neuropathic pain management, medications such as gabapentin and pregabalin may be considered since they are not metabolized in the liver. 51
Osteoporosis occurs more frequently in patients with cirrhosis than in the normal population due to physiologic alterations of hypogonadism and poor nutrition. 38,52 Additionally, patients with autoimmune causes of cirrhosis are at increased risk for osteoporosis due to the need for daily corticosteroid use. Therefore, all patients should be counseled on adequate vitamin D and calcium intake. Further, NPs should assess the patient for other osteoporosis risk factors like postmenopausal status or smoking. Screening densitometry is warranted in these patients. 53 Patients undergoing liver transplant should also receive densitometry testing. 38 If indicated based on densitometry results, bisphosphonates, like weekly alendronate and monthly ibandronate, may be used in patients with cirrhosis. 53
The management of patients with cirrhosis is complex and requires a team approach. Understanding pathophysiology, diagnosis, and management strategies helps NPs become more adept at caring for patients afflicted with this common chronic disease.
- Cited Here |
- PubMed | CrossRef
- View Full Text | PubMed | CrossRef
- View Full Text | PubMed
cirrhosis; collaboration; evidence-based practice; interdisciplinary; NP
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Aprn transition to practice: program development tips, th</sup> annual aprn legislative update', 'phillips susanne j. dnp aprn fnp-bc', 'the nurse practitioner', 'january 20, 2017', '42', '1' , 'p 18-46');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">29 th annual aprn legislative update, th</sup> annual aprn legislative update: improving access to healthcare one state at a time', 'phillips susanne j. dnp aprn fnp-bc faanp', 'the nurse practitioner', 'january 15, 2018', '43', '1' , 'p 27-54');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">30 th annual aprn legislative update: improving access to healthcare one state..., idiopathic pulmonary fibrosis: a guide for nurse practitioners, antidepressant use in breastfeeding women.

ANDREW SMITH, MD, KATRINA BAUMGARTNER, MD, AND CHRISTOPHER BOSITIS, MD
Am Fam Physician. 2019;100(12):759-770
Author disclosure: No relevant financial affiliations.
Cirrhosis is the 12th leading cause of death in the United States. Newer research has established that liver fibrosis is a dynamic process and that early cirrhosis may be reversible. Only one in three people with cirrhosis knows they have it. Most patients with cirrhosis remain asymptomatic until the onset of decompensation. When clinical signs, symptoms, or abnormal liver function tests are discovered, further evaluation should be pursued promptly. The most common causes of cirrhosis are viral hepatitis, alcoholic liver disease, and nonalcoholic steatohepatitis. Initial workup includes viral hepatitis serologies, ferritin, transferrin saturation, and abdominal ultrasonography as well as complete blood count, liver function tests, and prothrombin time/international normalized ratio, if not already ordered. Additional testing is based on demographics and risk factors. Common serum and ultrasound-based screening tests to assess fibrosis include the aspartate transaminase to platelet ratio index score, Fibrosis 4 score, FibroTest/FibroSure, nonalcoholic fatty liver fibrosis score, standard ultrasonography, and transient elastography. Generally, noninvasive tests are most useful in identifying patients with no to minimal fibrosis or advanced fibrosis. Chronic liver disease management includes directed counseling, laboratory testing, and ultrasound monitoring. Treatment goals are preventing cirrhosis, decompensation, and death. Varices are monitored with endoscopy and often require prophylaxis with nonselective beta blockers. Ascites treatment includes diuresis, salt restriction, and antibiotic prophylaxis for spontaneous bacterial peritonitis, when indicated. Hepatic encephalopathy is managed with lifestyle and nutritional modifications and, as needed, with lactulose and rifaximin. Hepatocellular carcinoma screening includes ultrasound screening every six months for patients with cirrhosis.
Cirrhosis is a diffuse process of liver damage considered irreversible in its advanced stages. In 2016, more than 40,000 Americans died because of complications related to cirrhosis, making it the 12th leading cause of death in the United States. 1 Recent projections suggest that this number is likely to grow. 2 An estimated 630,000 Americans have cirrhosis, yet less than one in three knows it. 3 Important racial and socioeconomic disparities exist, with prevalence highest among non-Hispanic blacks, Mexican Americans, and those living below the poverty level. 3 Cirrhosis and advanced liver disease cost the United States between $12 billion and $23 billion dollars in health care expenses annually. 4 , 5
WHAT'S NEW ON THIS TOPIC
Estimates suggest that nonalcoholic steatohepatitis will become the leading cause of cirrhosis in U.S. patients awaiting liver transplantation sometime between 2025 and 2035.
Liver biopsy remains the reference standard; however, transient elastography has become more widely available and is rapidly replacing biopsy as the preferred method for liver fibrosis staging.
Newer guidelines suggest targeted screening for esophageal varices in patients with clinically significant portal hypertension rather than screening all patients with cirrhosis.
| , | Expert opinion and consensus guidelines in the absence of clinical trials | |
| Expert opinion and consensus guidelines with low-quality trials | ||
| Randomized controlled trials demonstrate acceptable survival benefits based on clinical criteria and Model for End-Stage Liver Disease results with some variability | ||
| Data from multiple randomized controlled trials demonstrate more benefit than harm regarding patient comfort and reduced hospitalization times | ||
| , , , | Randomized controlled trials and meta-analyses comparing nonselective beta blockers, endoscopic band ligation, and placebo or no therapy, which generally show a reduction in variceal hemorrhage | |
| Low-quality randomized controlled trials that demonstrate less recurrence of hepatic encephalopathy using lactulose and/or rifaximin | ||
| , , , | Multiple randomized controlled trials demonstrate a reduction in bacterial infections as well as mortality | |
| should be screened for gastroesophageal varices with endoscopy. Repeat endoscopy should be performed every one to two years if small varices are found and every two to three years if no varices are found. | Expert opinion, consensus guidelines, and unpublished studies in progress |
The most common causes of cirrhosis in the United States are viral hepatitis (primarily hepatitis C virus [HCV] and hepatitis B virus [HBV]), alcoholic liver disease, and non-alcoholic steatohepatitis. HCV remains the leading cause of cirrhosis in patients awaiting liver transplant. With an increasing prevalence of nonalcoholic fatty liver disease (NAFLD) in the United States, estimates suggest that non-alcoholic steatohepatitis, a severe progression of NAFLD characterized by inflammatory steatohepatitis, will become the leading cause of cirrhosis in patients awaiting liver transplant sometime between 2025 and 2035. 6 , 7 Table 1 lists common etiologies of cirrhosis. 8
| Viral hepatitis (hepatitis B, hepatitis C) |
| Alcoholic liver disease |
| Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis |
| Storage diseases |
| Hemochromatosis |
| Wilson disease |
| Alpha -antitrypsin deficiency |
| Immune mediated |
| Autoimmune hepatitis (types 1, 2, and 3) |
| Primary biliary cholangitis |
| Primary sclerosing cholangitis |
| Immunoglobulin G4 cholangiopathy |
| Cardiovascular |
| Veno-occlusive disease (Budd-Chiari syndrome) |
| Congestive heart failure |
| Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease) |
| Chronic biliary disease |
| Recurrent bacterial cholangitis |
| Bile duct stenosis |
| Other |
| Medications (e.g., methotrexate, amiodarone) |
| Erythropoietic protoporphyria |
| Sarcoidosis |
| Schistosomiasis |
Pathophysiology and Natural History of Cirrhosis
Chronic liver injury causes inflammation and hepatic fibrosis. Regardless of the cause, this can lead to the formation of fibrous septae and nodules, collapse of liver structures, and distortion of hepatic parenchyma and vascular architecture. Progressive fibrosis and cirrhosis subsequently result in decreased metabolic and synthetic hepatic function, causing a rise in bilirubin and decreased production of clotting factors and thrombopoietin, as well as splenic platelet sequestration, increased portal pressure, and the development of ascites and esophageal varices.
Cirrhosis can result from chronic liver damage of any cause. In patients with the three most common causes of liver disease, 10% to 20% will develop cirrhosis within 10 to 20 years. 9 Factors associated with an increased risk of progression to cirrhosis include increased age, medical comorbidities (particularly patients coinfected with HIV and HCV), and male sex (except in alcoholic liver disease, where females progress more rapidly). 10 The point at which this process becomes irreversible, however, is not clear. Newer research has established that liver fibrosis is a dynamic process and that even early cirrhosis is reversible. 11 Studies have demonstrated biopsy-proven fibrosis improvement rates as high as 88% after antiviral treatment in patients with HBV and HCV and as high as 85% after bariatric surgery in patients with nonalcoholic steatohepatitis. 12 , 13
After cirrhosis is established, a patient may remain clinically stable, or compensated, for years. Patients with compensated cirrhosis caused by HBV, HCV, and alcoholic liver disease develop clinical signs of decompensation, which include ascites, hepatic encephalopathy, jaundice, or bleeding, at a rate of 4% to 10% per year. 14 Variability of disease progression is influenced by the underlying cause and the presence or absence of treatment and ongoing liver injury. The median survival for those with compensated cirrhosis is 12 years, compared with two years once decompensation occurs. 15
Clinical Presentation
Most patients with compensated cirrhosis remain asymptomatic. When symptoms occur, they include fatigue, weakness, loss of appetite, right upper quadrant discomfort, and unexplained weight loss. With the onset of decompensation, patients may report symptoms of impaired liver function such as jaundice, portal hypertension (including ascites and peripheral edema), and hepatic encephalopathy (such as confusion and disordered sleep).
PHYSICAL EXAMINATION
Physical examination findings that may be present in patients with advanced liver disease (cirrhosis) are summarized in Table 2 . 16 , 17 The Stanford Medicine 25 website is a good resource for photos and instructional videos that demonstrate findings associated with cirrhosis ( http://stanfordmedicine25.stanford.edu/the25/liverdisease.html ). 16 , 17
| General | Muscle wasting |
| Central nervous system | Asterixis (tremor of the hand with wrist extension) |
| Drowsiness, confusion | |
| Head | Fetor hepaticus: sweet odor of the breath attributable to increased concentrations of dimethyl sulfide |
| Jaundice: may see yellowing of mucous membranes beneath the tongue | |
| Parotid enlargement | |
| Scleral icterus | |
| Spider nevi | |
| Chest | Gynecomastia |
| Spider nevi | |
| Thinning axillary hair | |
| Abdomen | Ascites |
| Caput medusae (engorged superficial epigastric veins radiating from the umbilicus) | |
| Contracted or enlarged liver | |
| Hemorrhoids | |
| Splenomegaly | |
| Hands and nails | Clubbing |
| Dupuytren contracture (progressive fibrosis of palmar fascia, resulting in limited extension of the fingers) | |
| Palmar erythema | |
| Terry nails (whiteness of proximal half of nail plate) | |
| Genitourinary (male) | Testicular atrophy |
| Lower extremities | Distal erythema |
| Edema | |
| Petechiae |
INITIAL LABORATORY FINDINGS
In early compensated disease, laboratory findings may be normal. Incidentally elevated liver enzymes or evidence of hepatic disease on imaging may prompt the initial suspicion of chronic liver injury. Findings suggestive of cirrhosis include low albumin (less than 3.5 g per dL [35 g per L]), thrombocytopenia (platelet count less than 160 × 10 3 per μL [160 × 10 9 per L]), aspartate transaminase (AST):alanine transaminase (ALT) ratio greater than 1, elevated bilirubin, and a prolonged prothrombin time (PT)/elevated international normalized ratio (INR). 18
Evaluation of Chronic Liver Disease
When chronic liver disease is suspected, a history should be conducted, reviewing any potentially hepatotoxic medications, alcohol consumption, and family history of liver disease. Basic laboratory tests, including complete blood count, ALT, AST, albumin, alkaline phosphatase, gamma-glutamyl transferase, total bilirubin, and PT/INR, should be ordered.
For those with clinical signs or symptoms of liver disease or abnormal liver function test results, regardless of duration, further evaluation to determine the potential etiology should be pursued promptly. 19 , 20 Viral hepatitis serologies, ferritin, transferrin saturation, and abdominal ultrasonography should be performed; complete blood count, liver function tests, and PT/INR should be completed, if not already ordered. If risk factors for NAFLD exist, testing of fasting lipid levels and A1C should be done. For patients with risk factors or demographics with concern for autoimmune hepatitis, antinuclear antibodies and smooth muscle antibodies should be tested. Table 3 lists additional suggested tests based on risk factors and clinical findings. 19 , 21 , 22
| Alcoholic liver disease | Positive screening tests for alcohol use disorder | Aspartate transaminase ≥ 2 times alanine transaminase level in 70% of patients, especially if 3 times |
| History of excessive alcohol intake | Elevated glucose tolerance test and/or mean corpuscular volume [corrected] | |
| Ultrasonography may show fatty change | ||
| Alpha -antitrypsin deficiency | Autosomal recessive trait | Alpha -antitrypsin phenotype |
| European ancestry | ||
| All other evaluations unrevealing | ||
| Autoimmune hepatitis | Young and middle-aged women (in type 1, the most common) | Antinuclear antibody and/or antismooth muscle antibody positive in titers ≥ 1:80 |
| Total serum immunoglobulin G (polyclonal hypergammaglobulinemia > 1.5 times the upper limit of normal supports diagnosis) | ||
| Hemochromatosis | Autosomal recessive trait | Ferritin ≥ 250 to 300 ng per mL in men, ≥ 200 ng per mL in women |
| Northern European ancestry | Transferrin saturation (serum iron × 100/total iron-binding capacity) ≥ 45% | |
| If ferritin or transferrin saturation is abnormal, order human hemochromatosis protein gene mutation analysis | ||
| Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis | Obesity, diabetes mellitus | Lipids, A1C (not needed for diagnosis) |
| Improvement with weight loss | Ultrasonography may show fatty change | |
| May need biopsy to diagnose nonalcoholic steatohepatitis | ||
| Primary biliary cholangitis (primary biliary cirrhosis) | Associated with other autoimmune disorders (80% with Sjögren syndrome; 5% to 10% with autoimmune hepatitis) Middle-aged women | Cholestasis (elevated alkaline phosphatase and glucose tolerance test) Antimitochondrial antibody positive |
| Primary sclerosing cholangitis | Middle-aged men | Cholestasis (elevated alkaline phosphatase and glucose tolerance test) |
| Associated with inflammatory bowel disease (70%) | Perinuclear antineutrophil cytoplasmic antibodies positive in 70% of patients Frequently positive antinuclear antibodies, antismooth muscle antibodies, other antibodies Magnetic resonance cholangiography | |
| Viral hepatitis B (chronic) | Born in endemic country | Hepatitis B surface antigen |
| Hepatitis B core antibody | ||
| If either is positive, order hepatitis B virus DNA | ||
| Viral hepatitis C (chronic) | Born 1945 to 1965 | Anti–hepatitis C virus antibody |
| Specific risk factors for hepatitis C virus | If positive, order hepatitis C virus RNA | |
| Wilson disease | Autosomal recessive trait | Low serum ceruloplasmin |
| Age younger than 40 years with chronic liver disease or fatty liver and negative workup for the above | If abnormal, serum copper, urinary copper excretion, liver biopsy, hepatic tissue copper measurement, and genetic marker testing can be considered | |
| Kayser-Fleischer rings |
Staging Fibrosis and Diagnosing Cirrhosis
Liver fibrosis is scored on a scale from F0 to F4 ( Table 4 ) . 23 Differentiating between significant (F2 or greater) and advanced (F3 or greater) fibrosis and cirrhosis (F4) is difficult even with complete clinical, laboratory, and imaging data because findings are often nonspecific or insensitive. 24 Liver biopsy remains the reference standard for assessing liver fibrosis; however, use of noninvasive methods has become increasingly common in clinical practice. 18
| No fibrosis | F0 |
| Minimal scarring | F1 |
| Positive scarring with extension beyond area containing blood vessels | F2 |
| Bridging fibrosis with connection to other areas of fibrosis | F3 |
| Cirrhosis or advanced liver scarring | F4 |
Noninvasive testing includes serum-based and imaging modalities ( Table 5 25 – 37 ) . Generally, noninvasive tests are most useful in identifying patients with no to minimal fibrosis (F0) or advanced fibrosis (F3 to F4) and are less accurate at distinguishing early or intermediate stages of liver disease (F1 to F2). 24 , 38 They are most beneficial when combined with all available data, accounting for the pretest probability of fibrosis. 24 , 38
| AST to platelet ratio index score | AST, platelets | < 0.5: good NPV (80% in HCV) for significant fibrosis |
| > 2.0: high specificity for cirrhosis in HCV (46% sensitivity, 91% specificity) ; the World Health Organization recommended cutoff for HBV-related cirrhosis in low-resource settings (28% sensitivity, 87% specificity) , | ||
| Fibrosis 4 score | Age, platelets, AST, ALT | < 1.45: good NPV (95% in HCV) for advanced fibrosis |
| > 3.25 (range: 2.67 to 3.60): good PPV for advanced fibrosis/cirrhosis in HCV, HBV, and NAFLD , , | ||
| In HCV with ≥ 3.25, PPV for advanced fibrosis = 82% | ||
| In NAFLD with ≥ 2.67, PPV for advanced fibrosis = 80% | ||
| FibroTest/FibroSure | Alpha -macroglobulin, gamma-glutamyl transferase, haptoglobin, apolipoprotein A-I, bilirubin | < 0.30: good NPV (90%) for advanced fibrosis in NAFLD |
| > 0.48: high specificity for significant fibrosis in HCV (specificity = 85%) and HBV (specificity = 80%) | ||
| > 0.70: high specificity for advanced fibrosis or cirrhosis | ||
| In NAFLD with > 0.70, PPV for advanced fibrosis = 73% | ||
| In HBV with > 0.74, specificity for cirrhosis = 91% | ||
| NAFLD fibrosis score | Age, body mass index, AST, ALT, glucose, platelets, albumin | < −1.455: good NPV (88%) for advanced fibrosis in NAFLD |
| > 0.676: good PPV (82%) for advanced fibrosis in NAFLD | ||
| Transient elastography | Liver stiffness measured in kPa | HCV (> 12.5 kPa): high sensitivity (87%) and specificity (91%) for cirrhosis; very accurate for F2 to F4 when combined with FibroTest |
| HBV (> 9.0 to 12.0 kPa): good sensitivity (83%) and specificity (87%) but may be falsely elevated during flare-up | ||
| NAFLD (> 10.3 kPa): good NPV (98.5%) but lower PPV (56%) | ||
| Ultrasonography | Standard ultrasonography | Hepatic nodularity specific for severe fibrosis or cirrhosis in all forms of liver disease (sensitivity = 54%, specificity = 95%) |
| Evidence of portal hypertension (splenomegaly, portosystemic collaterals) |
Most serum tests show indirect markers of liver damage, except hyaluronic acid (found in the liver's extracellular matrix), which is included in biomarker panels such as FibroMeter or Hepascore. 24 The AST to platelet ratio index (APRI; https://www.mdcalc.com/ast-platelet-ratio-index-apri ), Fibrosis 4 score ( http://gihep.com/calculators/hepatology/fibrosis-4-score/ ), and NAFLD fibrosis score ( http://nafldscore.com/ ) are accessible, serum-based, nonproprietary calculations. 18 , 39 FibroTest (FibroSure in the United States), FibroMeter, and Hepascore are patented calculations using several serum biomarkers, with FibroTest being the most validated. 24
Biomarkers are most validated in chronic HCV, 40 with the exception of the NAFLD fibrosis score for non-alcoholic steatohepatitis. 33 For other etiologies of liver disease, including alcoholic liver disease, few studies of noninvasive methods exist.
STANDARD ULTRASONOGRAPHY
Given its relatively low cost, accessibility, and lack of radiation, ultrasonography is useful for diagnosing cirrhosis, cirrhosis complications (e.g., splenomegaly, portal hypertension, ascites, hepatocellular carcinoma), and comorbid liver diseases (e.g., extrahepatic cholestasis). 24 Ultrasonography is good at detecting steatosis (94% sensitivity, 84% specificity), but it may frequently miss fibrosis or cirrhosis (for which it is 40% to 57% sensitive). 41 , 42 Characteristics of cirrhosis include hepatic nodularity, coarseness, and echogenicity, 24 with hepatic nodularity being the most specific. 36 Additionally, features consistent with portal hypertension, such as splenomegaly and portosystemic collaterals, are suggestive of cirrhosis. 37 Patients with cirrhosis and some with chronic HBV should undergo right upper quadrant ultrasonography every six months to screen for hepatocellular carcinoma. 43
TRANSIENT ELASTOGRAPHY
Transient elastography, which has become more widely available, is rapidly replacing biopsy as the preferred method for fibrosis staging. Transient elastography, an ultrasound technique performed with a specialized machine (Fibro-Scan), determines liver stiffness in kilopascals (kPa) by measuring the velocity of low-frequency elastic shear waves propagating through the liver. It is a five-minute procedure performed in an outpatient setting and provides point-of-care results. In a meta-analysis of more than 10,000 patients spanning multiple etiologies of liver disease, transient elastography was sensitive (81%) and specific (88%) for detecting liver fibrosis and cirrhosis 40 (see Table 5 25 – 37 for cutoff values). Transient elastography performs better than the biomarker-based tools in detecting cirrhosis and is accurate at excluding cirrhosis (negative predictive value greater than 90%). 38 Similar to serum tests, however, transient elastography is less accurate at distinguishing between intermediate stages of liver disease, and cutoff values vary depending on the etiology of liver disease and population studied. 24 , 38
LIMITATIONS
Abnormal serum results may be seen from non–liver-related causes, including bone marrow disease, hemolysis, and medications. Transient elastography is less reliable in patients with obesity (though an extra-large probe has been developed), ascites, excessive alcohol intake, and extrahepatic cholestasis. If performed during an episode of acute hepatic inflammation, these tests can also lead to falsely elevated results. 38
LIVER BIOPSY
Liver biopsy remains the reference standard in diagnosing cirrhosis; however, a 20% error rate still occurs in fibrosis staging. 44 Pathologic changes may be heterogeneous; therefore, sampling error is common, and interpretation should be made by an experienced pathologist using validated scoring systems. 38 Liver biopsy is recommended when concern for fibrosis remains after indeterminate or conflicting clinical, laboratory, and imaging results; in those for whom transient elastography is not suitable; or to clarify etiology of disease after inconclusive noninvasive evaluation. 9 Liver biopsy may be indicated to diagnose necroinflammation (in HBV) and steatohepatitis (nonalcoholic steatohepatitis) because they are not easily distinguished by noninvasive methods.
Staging Cirrhosis
After the diagnosis of cirrhosis is established, Child-Pugh ( https://www.mdcalc.com/child-pugh-score-cirrhosis-mortality ) and Model for End-Stage Liver Disease ( https://www.mdcalc.com/meld-score-model-end-stage-liver-disease-12-older ) scores should be used to identify the stage of cirrhosis and mortality risk, respectively. 9 , 45 A Child-Pugh grade B classification (seven to nine points) is consistent with early hepatic decompensation, 46 whereas a Model for End-Stage Liver Disease score of 12 or more is predictive of increased risk for cirrhosis complications. 9
Cirrhosis Management
The primary goals of liver disease management are to prevent cirrhosis complications, liver decompensation, and death. These goals are accomplished with rigorous prevention counseling, monitoring, and management by primary care physicians, in consultation with subspecialists as needed.
PREVENTION COUNSELING
For all patients with liver disease, counseling points should be discussed, including avoidance of alcohol; maintenance of a healthy weight; nutrition; medication and supplement review; prevention of infections (including receiving vaccinations); screening and treatment of causative factors; and avoidance of unnecessary surgical procedures. Table 6 provides more details on counseling for patients with chronic liver disease. 7 , 9 , 18 , 21 , 45 , 47 – 52
| Alcohol use | Brief physician counseling, behavioral counseling, and group support |
| Complete alcohol abstinence in cirrhosis | |
| Medication-assisted treatment for alcohol use disorder | |
| Avoid naltrexone and acamprosate in patients with Child-Pugh grade C cirrhosis , | |
| Baclofen (Lioresal), 5 mg three times daily for three days, then 10 mg three times daily can be used, even with ascites , | |
| Avoidance of unnecessary surgical procedures | Cirrhosis, especially if decompensated or with Model for End-Stage Liver Disease score ≥ 14, increases perioperative mortality risk ; an online calculator has been developed to help guide decision-making ( ) |
| Coffee consumption | Three to four cups of coffee per day may reduce the risk of hepatocellular carcinoma and fibrosis progression in patients with nonalcoholic fatty liver disease and hepatitis C virus infection |
| Infection prevention: bacterial exposures | Avoid exposure to brackish/salt water and consumption of raw seafood ( can be fatal in patients with cirrhosis, iron overload, or immunocompromise) |
| Avoid unpasteurized dairy (risk of serious infections in patients with cirrhosis) | |
| Infection prevention: vaccinations | All patients with liver disease should receive yearly influenza vaccinations and hepatitis A and B vaccinations if not known to be immune |
| In patients with cirrhosis and chronic hepatitis B virus infection, 23-valent pneumococcal polysaccharide vaccine (Pneumovax 23) is recommended | |
| Medication and supplement review | For patients with cirrhosis |
| Analgesics: acetaminophen preferred, limit to 2 g per day 7; nonsteroidal anti-inflammatory drugs contraindicated , ; low-dose tramadol may be used for severe symptoms of pain | |
| Antihypertensives: discontinue if patient has hypotension or ascites (linked to hepatorenal syndrome and mortality) | |
| Aspirin: low-dose aspirin may be continued if cardiovascular disease severity exceeds the severity of cirrhosis | |
| Metformin: should be continued for patients with diabetes mellitus | |
| Proton pump inhibitors: avoid unnecessary use (linked to increased risk of spontaneous bacterial peritonitis) | |
| Sedating medications: avoid benzodiazepines and opiates, especially in hepatic encephalopathy; hydroxyzine or trazodone may be considered for severe insomnia | |
| Statins: may be safely used | |
| Supplements: avoid daily dosage of vitamin A > 5,000 IU (may increase fibrosis production); avoid multivitamins with iron | |
| Obesity and diabetes management | Maximize obesity and diabetes management because they increase the risk of cirrhosis , |
| Weight loss of 10% improves histopathologic features of nonalcoholic steatohepatitis, including fibrosis | |
| Screening for and treatment of underlying causative factors of liver disease | Treatment of alcohol use disorder, chronic hepatitis B or C virus infection, and nonalcoholic fatty liver disease can prevent progression and complications of liver disease and can improve fibrosis levels, even in patients with cirrhosis |
MONITORING OF PATIENTS WITH CIRRHOSIS
For patients with cirrhosis, a basic metabolic panel, liver function tests, complete blood count, and PT/INR should be completed every six months to recalculate Child-Pugh and Model for End-Stage Liver Disease scores. Patients with a Model for End-Stage Liver Disease score of 15 or higher should be referred for liver transplantation evaluation 37 , 45 ; patients with ascites, hepatic encephalopathy, or variceal hemorrhage should also be referred. 37 , 53
Screening and Management for Specific Complications
Patients with cirrhosis are at risk of multiple complications, including hepatic decompensation, hepatocellular carcinoma, and other more common conditions (e.g., malnutrition, leg cramps, umbilical hernias). Table 7 includes specific recommendations for the screening and management of select complications of cirrhosis. 7 , 9 , 43 , 45 , 46 , 49 , 53 – 55
| Abdominal hernia | Clinical | Defer surgery until medically optimized and ascites controlled | High perioperative risk and hernia recurrence in presence of ascites |
| Increased risk with ascites | Consult with multidisciplinary team | ||
| Surgeon with experience in the care of patients with cirrhosis is best | |||
| Ascites | Clinical Paracentesis if new-onset moderate to severe ascites or if concern for spontaneous bacterial peritonitis | Moderate (grade 2) and severe (grade 3) ascites: Diuresis with mineralocorticoids for treatment and prophylaxis Salt restriction < 2 g per day 7; no added salt; avoid preprepared meals , Fluid restriction usually not helpful Large (grade 3) ascites: Paracentesis: large-volume paracentesis with albumin infusion | Spironolactone, 100 mg per day Titrate every three days to maximum of 400 mg daily Goal of no more than 1.1 to 2.2 lb (0.5 to 1 kg) daily of weight loss Add furosemide (Lasix; or torsemide [Demadex]) if not responsive to spironolactone alone or if limiting adverse effects occur (e.g., hyperkalemia , ) Decrease to lowest effective dosage |
| Esophageal varices | EGD at diagnosis of cirrhosis May defer EGD if compensated, transient elastography with liver stiffness < 20 kPa, and platelets > 150,000 per mm (< 5% probability of high-risk varices) Repeat EGD if decompensation develops; if no varices (every two to three years ); if small varices (every one to two years ); or if medium or large varices or high-risk timing of repeat EGD varies | Medium, large, or high-risk varices (red wale markings): Endoscopic band ligation or nonselective beta blocker for prophylaxis , , , Prophylaxis with nonselective beta blocker should be indefinite | Propranolol, 20 to 40 mg twice daily; maximum: 160 to 320 mg per day Nadolol (Corgard), 20 to 40 mg daily; maximum: 80 to 160 mg per day Carvedilol (Coreg), 6.25 mg daily; maximum: 12.5 mg per day Titrate every two to three days; goal 25% heart rate reduction, keep heart rate > 55 beats per minute , , Discontinue if hemodynamic instability: sepsis, spontaneous bacterial peritonitis, acute gastrointestinal bleeding, refractory ascites, systolic blood pressure < 90 mm Hg, sodium concentration < 120 to 130 mEq per L (120 to 130 mmol per L), or acute kidney injury , |
| Hepatic encephalopathy | Clinical | Reverse precipitants | Lactulose syrup, 25 mL every one to two hours until two soft bowel movements per day Titrate to two to three soft bowel movements per day Rifaximin, 550 mg orally twice per day , |
| Exclude other causes | Nutritional support | ||
| Ammonia levels should not be used for diagnosis or monitoring , | Medications First episode: lactulose for treatment and prophylaxis Second episode: add rifaximin (Xifaxan) for prophylaxis | ||
| Hepatocellular carcinoma | Right upper quadrant ultrasonography every six months for all patients with cirrhosis and in certain patients with chronic hepatitis B virus infection without cirrhosis , | Treat obesity, nonalcoholic steatohepatitis, nonalcoholic fatty liver disease, diabetes mellitus, and hepatitis B virus infection | Refer to hepatologist for suspicious findings |
| Leg cramps | Clinical | Manage electrolytes | Baclofen, 10 mg per day, titrate weekly up to 30 mg per day |
| Especially if taking diuretics | Baclofen (Lioresal) as needed and tolerated | ||
| Malnutrition | Clinical | Multivitamin | Avoid protein restriction, even during hepatic encephalopathy Because of the increased risk of osteoporosis in chronic cholestasis and cirrhosis, performing a bone mineral density scan at the time of liver disease diagnosis or liver transplantation evaluation should be considered |
| Especially if new hepatic encephalopathy | Small frequent meals and late-night snack | ||
| Protein intake of 1 to 1.5 g per kg per day, with supplementation as needed , | |||
| Consider bone mineral density scan | |||
| Spontaneous bacterial peritonitis | Clinical Paracentesis if suspicion of disease (new or worsening ascites, gastrointestinal bleeding, hemodynamic instability, fever or signs of systemic inflammation, gastrointestinal symptoms, worsening liver or kidney function, new or worsening hepatic encephalopathy) Diagnosis Ascitic fluid neutrophil count > 250 per mm | Treatment (empiric, IV antibiotics): Community-acquired bacterial peritonitis: third-generation cephalosporin or piperacillin/tazobactam (Zosyn) Prophylaxis per criteria: Ceftriaxone IV if acute gastrointestinal bleeding and Child-Pugh grade B/C Trimethoprim/sulfamethoxazole or ciprofloxacin oral if acute gastrointestinal bleeding and Child-Pugh grade A [corrected] History of spontaneous bacterial peritonitis, ascitic protein < 1.5 g per dL and advanced liver disease (Child-Pugh score ≥ 9 or bilirubin ≥ 3 mg per dL) or kidney disease (creatinine ≥ 1.2 mg per dL, sodium ≤ 130 mmol per L) , , , | Treatment dosing: Cefotaxime, 2 g IV every eight to 12 hours Ceftriaxone, 2 g IV every 24 hours Piperacillin/tazobactam, 3.375 g IV every six hours Prophylactic dosing: Ceftriaxone, 1 g IV per day for seven days Trimethoprim/sulfamethoxazole, one 800-mg/160-mg tablet per day Ciprofloxacin, 500 mg per day Norfloxacin, 400 mg per day (not available in United States) Routine use of antibiotic prophylaxis in ascites without spontaneous bacterial peritonitis or acute gastrointestinal bleeding is not recommended |
COMMON COMPLICATIONS IN DECOMPENSATED CIRRHOSIS
Ascites, which develops in 5% to 10% of patients with cirrhosis per year, leads to decreased quality of life, frequent hospitalizations, and directly increases risk of further complications such as spontaneous bacterial peritonitis, umbilical hernias, and respiratory compromise. It also portends a poor prognosis, with a 30% five-year survival. 53 Hepatic encephalopathy, which occurs in 5% to 25% of patients within five years of a cirrhosis diagnosis, is likewise associated with increased medical cost and mortality, with a reported 15% inpatient mortality rate. 54
SCREENING FOR VARICES
Portal hypertension predisposes patients with cirrhosis to develop esophageal varices. Patients with varices have a one in three chance of developing a variceal bleed in the two years after diagnosis, with a 20% to 40% mortality rate per episode. 45 Endoscopy is the preferred screening method for esophageal varices. Many experts and guidelines recommend screening all patients with cirrhosis 9 ; however, newer recommendations suggest targeted screening of patients with clinically significant portal hypertension. 46 A liver stiffness greater than 20 kPa, alone or combined with a low platelet count (less than 150,000 per mm 3 ) and increased spleen size, and/or the presence of portosystemic collaterals on imaging may be sufficient to diagnose clinically significant portal hypertension and warrant endoscopic screening for varices. Repeat endoscopy should be performed every one to two years if small varices are found and every two to three years if no varices are found. 46
Consultation
Varices, hepatic encephalopathy, and ascites herald hepatic decompensation; these conditions warrant referral for subspecialist evaluation. The management of acute or refractory complications of cirrhosis (e.g., spontaneous bacterial peritonitis, acute gastrointestinal bleeding, hepatorenal syndrome, unresponsive portal hypertension, hepatic encephalopathy, ascites) is best addressed in the inpatient or referral setting.
This article updates previous articles on this topic by Starr and Raines , 56 Heidelbaugh and Bruderly , 57 and Riley and Bhatti . 58
Data Sources: A literature search was completed in Medline via Ovid, EBSCOhost, DynaMed, and the Cochrane Database of Systematic Reviews using the keywords cirrhosis, end stage liver disease, management of liver disease, and liver fibrosis staging. Additionally, the EE+Evidence Summary literature search sent by the AFP medical editors was reviewed. Search dates: November 26, 2018; December 27, 2018; and August 7, 2019.
Kochanek KD, Murphy S, Xu J, et al. Mortality in the United States, 2016. NCHS Data Brief. 2017(293):1-8.
Best AF, Haozous EA, Berrington de Gonzalez A, et al. Premature mortality projections in the USA through 2030: a modelling study [published correction appears in Lancet Public Health . 2018;3(8):e364]. Lancet Public Health. 2018;3(8):e374-e384.
Scaglione S, Kliethermes S, Cao G, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015;49(8):690-696.
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018 [published correction appears in Gastroenterology . 2019;156(6):1936]. Gastroenterology. 2019;156(1):254-272.e11.
National Institute of Diabetes and Digestive and Kidney Diseases. The burden of digestive diseases in the United States. January 2008. Accessed January 4, 2019. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/burden-of-digestive-diseases-in-united-states
Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
Ge PS, Runyon BA. Treatment of patients with cirrhosis. N Engl J Med. 2016;375(8):767-777.
Wiegand J, Berg T. The etiology, diagnosis and prevention of liver cirrhosis: part 1 of a series on liver cirrhosis. Dtsch Arztebl Int. 2013;110(6):85-91.
National Institute for Health and Care Excellence. Cirrhosis in over 16s: assessment and management. NICE guideline [NG50]. July 2016. Accessed May 28, 2019. https://www.nice.org.uk/guidance/ng50
Poynard T, Mathurin P, Lai CL, et al.; PANFIBROSIS Group. A comparison of fibrosis progression in chronic liver diseases. J Hepatol. 2003;38(3):257-265.
Bonis PA, Friedman SL, Kaplan MM. Is liver fibrosis reversible?. N Engl JMed. 2001;344(6):452-454.
Jung YK, Yim HJ. Reversal of liver cirrhosis: current evidence and expectations. Korean J Intern Med. 2017;32(2):213-228.
Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149(2):379-388.
Asrani SK, Kamath PS. Natural history of cirrhosis. Curr Gastroenterol Rep. 2013;15(2):308.
D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217-231.
Stanford Medicine. Liver disease, head to foot. Accessed January 4, 2019. http://stanfordmedicine25.stanford.edu/the25/liverdisease.html
Reuben A. The liver has a body—a Cook's tour. Hepatology. 2005;41(2):408-415.
Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis?. JAMA. 2012;307(8):832-842.
Oh RC, Hustead TR, Ali SM, et al. Mildly elevated liver transaminase levels: causes and evaluation. Am Fam Physician. 2017;96(11):709-715. Accessed August 28, 2019. https://www.aafp.org/afp/2017/1201/p709.html
Newsome PN, Cramb R, Davison SM, et al. Guidelines on the management of abnormal liver blood tests. Gut. 2018;67(1):6-19.
O'Shea RS, Dasarathy S, McCullough AJ Practice Guideline Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51(1):307-328.
Bacon BR, Adams PC, Kowdley KV, et al.; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54(1):328-343.
Wilkins T, Akhtar M, Gititu E, et al. Diagnosis and management of hepatitis C. Am Fam Physician. 2015;91(12):835-842. Accessed August 28, 2019. https://www.aafp.org/afp/2015/0615/p835.html
Lurie Y, Webb M, Cytter-Kuint R, et al. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J Gastroenterol. 2015;21(41):11567-11583.
Lin ZH, Xin YN, Dong QJ, et al. Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology. 2011;53(3):726-736.
Parikh P, Ryan JD, Tsochatzis EA. Fibrosis assessment in patients with chronic hepatitis B virus (HBV) infection. Ann Transl Med. 2017;5(3):40.
World Health Organization. Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. March 2015. Accessed January 4, 2019. https://www.who.int/hiv/pub/hepatitis/hepatitis-b-guidelines/en/
Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and Fibrotest. Hepatology. 2007;46(1):32-36.
Shah AG, Lydecker A, Murray K, et al.; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with non-alcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7(10):1104-1112.
Ratziu V, Massard J, Charlotte F, et al.; LIDO Study Group; CYTOL Study Group. Diagnostic value of biochemical markers (FibroTest-FibroSURE) for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease. BMC Gastroenterol. 2006;6:6.
Imbert-Bismut F, Ratziu V, Pieroni L, et al.; MULTIVIRC Group. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet. 2001;357(9262):1069-1075.
Salkic NN, Jovanovic P, Hauser G, et al. FibroTest/Fibrosure for significant liver fibrosis and cirrhosis in chronic hepatitis B: a meta-analysis. Am J Gastroenterol. 2014;109(6):796-809.
Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846-854.
Castéra L, Vergniol J, Foucher J, et al. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005;128(2):343-350.
Hashemi SA, Alavian SM, Gholami-Fesharaki M. Assessment of transient elastography (FibroScan) for diagnosis of fibrosis in non-alcoholic fatty liver disease: a systematic review and meta-analysis. Caspian J Intern Med. 2016;7(4):242-252.
Colli A, Fraquelli M, Andreoletti M, et al. Severe liver fibrosis or cirrhosis: accuracy of US for detection—analysis of 300 cases. Radiology. 2003;227(1):89-94.
Martin P, DiMartini A, Feng S, et al. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59(3):1144-1165.
European Association for Study of Liver; Asociacion Latinoamericana para el Estudio del Higado. EASL-ALEH Clinical Practice Guidelines: non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63(1):237-264.
Noureddin M, Loomba R. Nonalcoholic fatty liver disease: indications for liver biopsy and noninvasive biomarkers. Clin Liver Dis (Hoboken). 2012;1(4):104-107.
Geng XX, Huang RG, Lin JM, et al. Transient elastography in clinical detection of liver cirrhosis: a systematic review and meta-analysis. Saudi J Gastroenterol. 2016;22(4):294-303.
Bonekamp S, Kamel I, Solga S, et al. Can imaging modalities diagnose and stage hepatic fibrosis and cirrhosis accurately?. J Hepatol. 2009;50(1):17-35.
Saverymuttu SH, Joseph AE, Maxwell JD. Ultrasound scanning in the detection of hepatic fibrosis and steatosis. Br Med J (Clin Res Ed). 1986;292(6512):13-15.
Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018;68(2):723-750.
Afdhal NH. Diagnosing fibrosis in hepatitis C: is the pendulum swinging from biopsy to blood tests?. Hepatology. 2003;37(5):972-974.
Herrera JL, Rodríguez R. Medical care of the patient with compensated cirrhosis. Gastroenterol Hepatol (N Y). 2006;2(2):124-133.
Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases [published correction appears in Hepatology . 2017;66(1):304]. Hepatology. 2017;65(1):310-335.
Addolorato G, Mirijello A, Leggio L, et al. Management of alcohol dependence in patients with liver disease. CNS Drugs. 2013;27(4):287-299.
Addolorato G, Leggio L, Ferrulli A, et al. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007;370(9603):1915-1922.
Runyon BA. Management of adult patients with ascites due to cirrhosis: update 2012. Accessed August 20, 2019. https://www.aasld.org/sites/default/files/2019-06/141020_Guideline_Ascites_4UFb_2015.pdf
Wadhawan M, Anand AC. Coffee and liver disease. J Clin Exp Hepatol. 2016;6(1):40-46.
Zhang X, Harmsen WS, Mettler TA, et al. Continuation of metformin use after a diagnosis of cirrhosis significantly improves survival of patients with diabetes. Hepatology. 2014;60(6):2008-2016.
Glass LM, Dickson RC, Anderson JC, et al. Total body weight loss of ≥ 10% is associated with improved hepatic fibrosis in patients with non-alcoholic steatohepatitis. Dig Dis Sci. 2015;60(4):1024-1030.
European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol . 2018;69(5):1207]. J Hepatol. 2018;69(2):406-460.
Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715-735.
Terrault NA, Lok AS, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560-1599.
Starr SP, Raines D. Cirrhosis: diagnosis, management, and prevention. Am Fam Physician. 2011;84(12):1353-1359. Accessed August 28, 2019. https://www.aafp.org/afp/2011/1215/p1353.html
Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74(5):756-762. Accessed August 28, 2019. https://www.aafp.org/afp/2006/0901/p756.html
Riley TR, Bhatti AM. Preventive strategies in chronic liver disease: part II. Cirrhosis. Am Fam Physician. 2001;64(10):1735-1740. Accessed August 28, 2019. https://www.aafp.org/afp/2001/1115/p1735.html
Continue Reading
More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Evaluation of meld scores and thyroid hormones as prognostic factors of liver cirrhosis.

1. Introduction
2. materials and methods, 2.1. samples, 2.2. inclusion criteria, 2.3. exclusion criteria, 2.4. participants, 2.5. data analysis methods, 3.1. socio-demographic data, 3.2. univariate descriptive analysis, 3.3. bivariate correlation analysis, 3.4. data analysis, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- WHO. The Global Health Observatory. Global Health Estimates: Leading Causes of Death. Available online: https://Www.Who.Int/Data/Gho/Data/Themes/Mortality-and-Global-Health-Estimates/Ghe-Leading-Causes-of-Death (accessed on 20 May 2023).
- Huang, D.Q.; Terrault, N.A.; Tacke, F.; Gluud, L.L.; Arrese, M.; Bugianesi, E.; Loomba, R. Global Epidemiology of Cirrhosis—Aetiology, Trends and Predictions. Nat. Rev. Gastroenterol. Hepatol. 2023 , 20 , 388–398. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moon, A.M.; Singal, A.G.; Tapper, E.B. Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2020 , 18 , 2650–2666. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jalilova, A.S. The spread of cirrhosis of the liver by etiological factors. Orient. Renaiss. Innov. Educ. Nat. Soc. Sci. 2022 , 2 , 253–257. [ Google Scholar ]
- Patel, R.; Mueller, M. Alcoholic Liver Disease. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. [ Google Scholar ]
- Llamosas-Falcón, L.; Probst, C.; Buckley, C.; Jiang, H.; Lasserre, A.M.; Puka, K.; Tran, A.; Zhu, Y.; Rehm, J. How Does Alcohol Use Impact Morbidity and Mortality of Liver Cirrhosis? A Systematic Review and Dose–Response Meta-Analysis. Hepatol. Int. 2024 , 18 , 216–224. [ Google Scholar ] [ CrossRef ]
- GinËs, P.; Krag, A.; Abraldes, J.G. Liver Cirrhosis. Lancet 2021 , 398 , 1359–1376. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cheemerla, S.; Balakrishnan, M. Epidemiologia Globală a Bolii Hepatice Cronice. Boală Hepatică Clin. 2021 , 17 , 365–370. [ Google Scholar ]
- Devarbhavi, H.; Asrani, S.K.; Arab, J.P.; Nartey, Y.A.; Pose, E.; Kamath, P.S. Global Burden of Liver Disease: 2023 Update. J. Hepatol. 2023 , 79 , 516–537. [ Google Scholar ] [ CrossRef ]
- Aguirre-Villarreal, D.; Servin-Rojas, M.; Sánchez-Cedillo, A.; Chávez-Villa, M.; Hernandez-Alejandro, R.; Arab, J.P.; Ruiz, I.; Avendaño-Castro, K.P.; Matamoros, M.A.; Adames-Almengor, E.; et al. Liver Transplantation in Latin America: Reality and Challenges. Lancet Reg. Health–Am. 2023 , 28 , 100633. [ Google Scholar ] [ CrossRef ]
- Punekar, P.; Sharma, A.K.; Jain, A. A Study of Thyroid Dysfunction in Cirrhosis of Liver and Correlation with Severity of Liver Disease. Indian J. Endocrinol. Metab. 2018 , 22 , 645–650. [ Google Scholar ] [ CrossRef ]
- Gangadharam, D.Y.; Veeranarayana, D.G.; Kanha, D.M.M. A Study on Thyroid Function Tests as a Biomarker to Differentiate Acute from Chronic Liver Disease. J. Cardiovasc. Dis. Res. 2023 , 14 , 1–11. [ Google Scholar ]
- Nardin, G.D.; Colombo, B.d.S.; Ronsoni, M.F.; Silva, P.E.S.e; Fayad, L.; Wildner, L.M.; Bazzo, M.L.; Dantas-Correa, E.B.; Narciso-Schiavon, J.L.; Schiavon, L.d.L. Thyroid Hormone Profile Is Related to Prognosis in Acute Decompensation of Cirrhosis. Arch. Endocrinol. Metab. 2024 , 68 , e230249. [ Google Scholar ] [ CrossRef ]
- Kasper, D.L.; Fauci, A.S.; Hauser, S.L.; Longo, D.L.; Jameson, J.L.; Loscalzo, J. Thyroid Gland Disorders. In Harrison’s Manual of Medicine ; McGraw-Hill Education: New York, NY, USA, 2016. [ Google Scholar ]
- Kharb, S.; Garg, M.K.; Puri, P.; Brar, K.S.; Pandit, A.; Srivastava, S. Assessment of Thyroid and Gonadal Function in Liver Diseases. Indian J. Endocrinol. Metab. 2015 , 19 , 89–94. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ritter, M.J.; Amano, I.; Hollenberg, A.N. Thyroid Hormone Signaling and the Liver. Hepatology 2020 , 72 , 742. [ Google Scholar ] [ CrossRef ]
- Kim, H.J. Importance of Thyroid-Stimulating Hormone Levels in Liver Disease. J. Pediatr. Endocrinol. Metab. JPEM 2020 , 33 , 1133–1137. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gionfra, F.; De Vito, P.; Pallottini, V.; Lin, H.-Y.; Davis, P.J.; Pedersen, J.Z.; Incerpi, S. The Role of Thyroid Hormones in Hepatocyte Proliferation and Liver Cancer. Front. Endocrinol. 2019 , 10 , 532. [ Google Scholar ] [ CrossRef ]
- Sinha, R.A.; Singh, B.K.; Yen, P.M. Direct Effects of Thyroid Hormones on Hepatic Lipid Metabolism. Nat. Rev. Endocrinol. 2018 , 14 , 259–269. [ Google Scholar ] [ CrossRef ]
- Piantanida, E.; Ippolito, S.; Gallo, D.; Masiello, E.; Premoli, P.; Cusini, C.; Rosetti, S.; Sabatino, J.; Segato, S.; Trimarchi, F.; et al. The Interplay between Thyroid and Liver: Implications for Clinical Practice. J. Endocrinol. Investig. 2020 , 43 , 885–899. [ Google Scholar ] [ CrossRef ]
- Mullur, R.; Liu, Y.-Y.; Brent, G.A. Thyroid Hormone Regulation of Metabolism. Physiol. Rev. 2014 , 94 , 355–382. [ Google Scholar ] [ CrossRef ]
- Marino, L.; Kim, A.; Ni, B.; Celi, F.S. Thyroid Hormone Action and Liver Disease, a Complex Interplay. Hepatology 2023 , 10-1097. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Verma, S.; Kumar, V.; Tiwari, P.; Joge, N.; Misra, R. Thyroid Profile in Patients of Cirrhosis of Liver: A Cross-Sectional Study. J. Clin. Diagn. Res. 2017 , 11 , 6. [ Google Scholar ] [ CrossRef ]
- Ruf, A.; Dirchwolf, M.; Freeman, R.B. From Child-Pugh to MELD Score and beyond: Taking a Walk down Memory Lane. Ann. Hepatol. 2022 , 27 , 100535. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, W.R.; Mannalithara, A.; Heimbach, J.K.; Kamath, P.S.; Asrani, S.K.; Biggins, S.W.; Wood, N.L.; Gentry, S.E.; Kwong, A.J. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology 2021 , 161 , 1887–1895.e4. [ Google Scholar ] [ CrossRef ]
- Nallagangula, K.S.; Nagaraj, S.K.; Venkataswamy, L.; Chandrappa, M. Liver Fibrosis: A Compilation on the Biomarkers Status and Their Significance During Disease Progression. Future Sci. OA 2018 , 4 , FSO250. [ Google Scholar ] [ CrossRef ]
- Kumar, A.; Ahuja, V.; Kaur, I.; Pandov, V.; Singh, A.; Sibia, R.P. Prevalence of Thyroid Dysfunction in Patients of Cirrhosis of Liver and Its Correlation with Severity of Cirrhosis. Int. J. Adv. Res. 2020 , 8 , 91–95. [ Google Scholar ] [ CrossRef ]
- Zucchi, R. Thyroid Hormone Analogues: An Update. Thyroid 2020 , 30 , 1099–1105. [ Google Scholar ] [ CrossRef ]
- R Core Team. R: A Language and Environment for Statistical Computing ; R Foundation for Statistical Computing: Vienna, Austria, 2024. [ Google Scholar ]
- Royston, J.P. An Extension of Shapiro and Wilk’s W Test for Normality to Large Samples. J. R. Stat. Soc. Ser. C Appl. Stat. 1982 , 31 , 115–124. [ Google Scholar ] [ CrossRef ]
- Royston, P. Remark AS R94: A Remark on Algorithm AS 181: The W-Test for Normality. J. R. Stat. Soc. Ser. C Appl. Stat. 1995 , 44 , 547–551. [ Google Scholar ] [ CrossRef ]
- Templ, M.; Kowarik, A.; Alfons, A.; de Cillia, G.; Prantner, B.; Rannetbauer, W. VIM: Visualization and Imputation of Missing Values. R Package Version 2022 , 2 , 2. [ Google Scholar ]
- West Haven Criteria for Hepatic Encephalopathy—GPnotebook. Available online: https://gpnotebook.com/pages/surgery/west-haven-criteria-for-hepatic-encephalopathy (accessed on 26 August 2024).
- Mandiga, P.; Kommu, S.; Bollu, P.C. Hepatic Encephalopathy. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2024. [ Google Scholar ]
- Vincken, S.; Reynaert, H.; Schiettecatte, J.; Kaufman, L.; Velkeniers, B. Liver Cirrhosis and Thyroid Function: Friend or Foe? Acta Clin. Belg. 2017 , 72 , 85–90. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ye, F.; Zhai, M.; Long, J.; Gong, Y.; Ren, C.; Zhang, D.; Lin, X.; Liu, S. The Burden of Liver Cirrhosis in Mortality: Results from the Global Burden of Disease Study. Front. Public Health 2022 , 10 , 909455. [ Google Scholar ] [ CrossRef ]
- Trajkovic, M.; Visser, T.J.; Mittag, J.; Horn, S.; Lukas, J.; Darras, V.M.; Raivich, G.; Bauer, K.; Heuer, H. Abnormal Thyroid Hormone Metabolism in Mice Lacking the Monocarboxylate Transporter 8. J. Clin. Investig. 2007 , 117 , 627–635. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
Click here to enlarge figure
| Variable | N | Mean | Ab. Std | Median | Min | Max | Skew (ES) | Kurt (ES) | Normal |
|---|---|---|---|---|---|---|---|---|---|
| MELD Score | 419 | 14.08 | 4.32 | 14 | 5 | 31 | 0.72 (0.12) | 0.92 (0.24) | |
| TSH (mUI/L) | 419 | 5.89 | 1.92 | 5.7 | 2.4 | 14.4 | 0.70 (0.12) | 1.03 (0.24) | 0.4–4.0 |
| T3 (pmol/L) | 419 | 0.84 | 0.50 | 0.77 | 0.05 | 2.5 | 0.51 (0.12) | −0.24 (0.24) | 1.2–3.0 |
| fT4 (pmol/L) | 419 | 14.13 | 2.62 | 13.5 | 8.8 | 23 | 0.83 (0.12) | 0.43 (0.24) | 12.0–22.0 |
| Variable | N | Mean | Ab. Std | Median | Min | Max | Skew (ES) | Kurt (ES) | Normal |
|---|---|---|---|---|---|---|---|---|---|
| TSH (mUI/L) | 419 | 3.89 | 1.26 | 3.55 | 1.35 | 8.15 | 0.68 (0.12) | 0.04 (0.24) | 0.4–4.0 |
| T3 (pmol/L) | 419 | 0.78 | 0.52 | 0.65 | 0.00 | 2.25 | 0.64 (0.12) | −0.64 (0.24) | 1.2–3.0 |
| fT4 (pmol/L) | 419 | 12.76 | 3.04 | 12.4 | 8.8 | 23.4 | 0.86 (0.12) | 0.26 (0.24) | 12.0–22.0 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| (1) MELD | - | ||||||||
| (2) Non-surviving patients | −0.09 | - | |||||||
| (3) Hospitalization (days) | −0.03 | −0.02 | - | ||||||
| (4) TSH—Admission | 0.27 *** | −0.19 *** | 0.03 | - | |||||
| (5) TSH—Discharge | 0.21 *** | −0.14 ** | 0.00 | 0.75 *** | - | ||||
| (6) T3—Admission | −0.10 | 0.04 | 0.01 | −0.35 *** | −0.28 *** | - | |||
| (7) T3—Discharge | −0.17 *** | −0.02 | −0.01 | −0.23 *** | −0.14 ** | 0.46 *** | - | ||
| (8) fT4—Admission | −0.02 | 0.01 | 0.06 | −0.18 *** | −0.07 | 0.23 *** | 0.13 ** | - | |
| (9) fT4—Discharge | 0.08 | 0.02 | 0.07 | 0.05 | 0.20 *** | 0.09 | 0.51 *** | 0.42 *** | - |
| Media | 14.08 | 1.92 | 7.21 | 5.89 | 3.89 | 0.84 | 0.78 | 14.13 | 12.76 |
| Standard deviations | 4.32 | 0.27 | 6.73 | 1.92 | 1.26 | 0.50 | 0.52 | 2.62 | 3.04 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |

Share and Cite
Belu, A.M.; Nicoara, A.D.; Belu, D.M.; Circo, E. Evaluation of MELD Scores and Thyroid Hormones as Prognostic Factors of Liver Cirrhosis. Medicina 2024 , 60 , 1474. https://doi.org/10.3390/medicina60091474
Belu AM, Nicoara AD, Belu DM, Circo E. Evaluation of MELD Scores and Thyroid Hormones as Prognostic Factors of Liver Cirrhosis. Medicina . 2024; 60(9):1474. https://doi.org/10.3390/medicina60091474
Belu, Anca M., Alina D. Nicoara, Daniela M. Belu, and Eduard Circo. 2024. "Evaluation of MELD Scores and Thyroid Hormones as Prognostic Factors of Liver Cirrhosis" Medicina 60, no. 9: 1474. https://doi.org/10.3390/medicina60091474
Article Metrics
Further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Research Highlight
- Open access
- Published: 09 September 2024
Metabolic inflexibility of mitochondria: beneficial for the fitness of regenerating liver cells
- Josef Ecker ORCID: orcid.org/0000-0003-4799-0788 1 ,
- Sarah Brunner 1 &
- Klaus-Peter Janssen ORCID: orcid.org/0000-0002-4707-7887 2
Signal Transduction and Targeted Therapy volume 9 , Article number: 233 ( 2024 ) Cite this article
Metrics details
- Gastrointestinal diseases
- Metabolic disorders
- Transdifferentiation
In a recent manuscript in Science , Wang and coworkers discovered that metabolic inflexibility is required for proper mitochondrial function during liver regeneration. 1 This study deepens our understanding of liver metabolism, stem cell biology and adult tissue renewal, suggesting that metabolic flexibility, generally assumed to be a selective advantage, may actually be detrimental for mitochondrial function in the regenerating liver.
Whereas these findings appear surprising in the light of traditional metabolic concepts, they offer a detailed view into the regulatory networks that ensure that only healthy liver cells with functional mitochondria contribute to regeneration. The study has considerable relevance for human health, since primary or metastatic cancer often affects the liver. Moreover, chronic hepatitis, toxins, or metabolic stress can lead to the development of fibrosis, cirrhosis, and chronic conditions like alcoholic steatohepatitis (ASH) and metabolic dysfunction-associated steatohepatitis. 2 Thus, liver diseases rank among the global health burdens, and research efforts are needed to better understand the processes that govern the self-renewal capacity of the adult liver (Fig. 1 ).
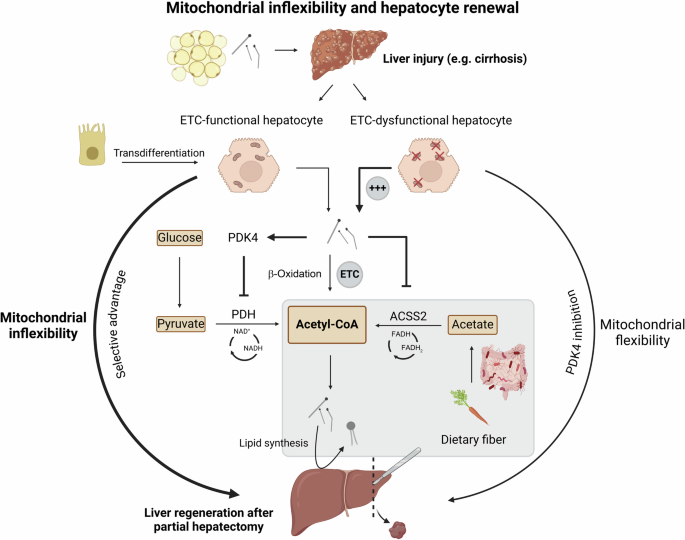
Mitochondrial inflexibility and hepatocyte renewal. During liver injury and regeneration, fatty acids released from adipose tissue fuel liver mitochondria to maintain acetyl-CoA levels. Cholangiocytes (upper left) have the capacity to undergo transdifferentiation into hepatocytes, and phospholipids are generated in the liver from acetate (Short chain fatty acids derived from microbiota-metabolized dietary fiber), both of which further promote liver regeneration. Mitochondria with ETC dysfunction upregulate PDK4 and inhibit ACSS2 expression, ultimately blocking acetyl-CoA generation and stopping proliferation of dysfunctional hepatocytes. Mitochondrial inflexibility therefore selects for ETC-functional healthy mitochondria and promotes liver recovery after partial hepatectomy. Conversely, PDK4 inhibition (mitochondrial flexibility) increases the proliferation of ETC-dysfunctional mitochondria. Created with BioRender
As a radical yet potentially curative treatment option, it would appear logical to replace non-functional livers by transplantation. However, the continuing shortage of donor organs for liver transplantation has often been acknowledged. In the clinical context, a major treatment option therefore is partial hepatectomy (PHx), based on surgical removal of cancerous tissue with the objective of sparing as much of functional liver parenchyma as possible to allow for its self-renewal. Up to 75% of healthy liver tissue can be safely removed, indicative of the stunning regenerative capacity of the liver in adults. 2 The outcome of this procedure is confounded by diverse pathologies and by the type of intervention itself, but five-year survival rates of around 50% can be obtained. 2
The processes underlying liver regeneration are not fully understood, and regenerative capacities are drastically limited under disease conditions, such as metabolic dysfunction-associated fatty liver disease (MAFLD). In order to follow these processes in depth, the authors have tackled mitochondria, the central regulators of bioenergetics and metabolic powerhouses of eukaryotic cells. They focused on the crucial components in mitochondria, the electron transport chain (ETC). This complex multi-protein machinery is composed of four inner mitochondrial membrane complexes and two electron carriers, coenzyme Q and cytochrome c, which oxidize reducing equivalents (e.g., NADH). The resulting electrochemical proton gradient enables ATP-synthase to generate energy within cells. Of note, ETC dysfunction has been involved previously in liver pathologies by the same working group. 3
By default, the regenerating liver can be repopulated from preexisting hepatocytes that enter the cell cycle and proliferate. As a backup mechanism to compensate for a lack of proliferating hepatocytes, the epithelia lining intrahepatic biliary ducts (cholangiocytes or biliary epithelial cells) can transdifferentiate into hepatocytes via transitional liver progenitor states, and thus help to regenerate the liver parenchyma. However, how is it ensured that only metabolically healthy liver cells with fully functional mitochondria contribute to regeneration? Moreover, how are cells with defective ETC excluded from this process, to avoid clonal expansion of “unfit” hepatocytes?
The Mishra lab has revealed in an elegant and compelling set of experiments, based on a series of genetic mouse models, a selective mechanism that prevents hepatocytes containing defective ETC to propagate. This process selects for healthy mitochondria, which finally leads to successful and effective liver regeneration.
The beneficial mechanism uncovered in this study has been termed “metabolic inflexibility”. This may appear counterintuitive since the flexibility of the mitochondrial metabolism is essential for mammalian organisms to adapt to different food sources or to survive fasting periods. Moreover, obesity and type 2 diabetes are commonly associated with “metabolic inflexibility”. However, the “inflexibility” of mitochondria actually helps to maintain hepatocytes healthy and ultimately boosts liver regeneration. Under physiological conditions, acetyl-CoA can be generated either from glycolytic breakdown of carbohydrates, or via β-oxidation from fatty acids, and enters the citric cycle in healthy mitochondria to generate energy in the form of ATP and GTP.
Applying stable isotope labeling of different metabolic pathways in mice, the authors identified a metabolic quality control mechanism that promotes mitochondrial health and liver regeneration. In healthy hepatocytes, fatty acids from adipose tissue reach the liver to fuel β-oxidation upon liver injury, thereby displacing cells with ETC-dysfunctional mitochondria. In these “malfunctioning” mitochondria, generation of acetyl-CoA through β-oxidation is inhibited, because the ETC is essential for this process. This leads to the accumulation of longer-chain fatty acids, blocking the breakdown of carbohydrates and eventually inhibiting the synthesis of acetyl-Coa from pyruvate Importantly, acetyl-CoA is not only used for energy production but also for epigenetic chromatin acetylation and as a precursor for cell membrane lipids, like phosphatidylcholine and phosphatidylethanolamine. The importance of cellular phospholipid synthesis in proliferating hepatocytes for liver regeneration has been recently demonstrated and was found to be influenced by the gut microbiota, which degrades and ferments complex carbohydrates, i.e. dietary fiber, to acetate. 3 , 4 , 5
Mechanistically, the accumulation of excess lipids caused by dysfunctional ETC induces mitochondrial kinase PDK4 ( pyruvate dehydrogenase kinase 4 ), negatively regulating the pyruvate dehydrogenase complex that generates acetyl-CoA from pyruvate. In parallel, excess lipids suppress the cytosolic enzyme ACSS2 ( Acyl-coenzyme A synthetase short-chain family member 2 ), which converts acetate to acetyl-CoA. 1 Wang and colleagues report that PDK4 inhibition actually increases the mitochondrial flexibility, allowing liver cells with dysfunctional ETC to use carbohydrates as an energy source, and, ultimately, to proliferate in the context of liver regeneration, with detrimental consequences.
The inability of “unfit” hepatocytes with a perturbed ETC to metabolize acetyl-CoA from pyruvate or acetate results in the privileged selection of hepatocytes with healthy mitochondria for proliferation, as acetyl-CoA production is prevented.
The authors further provide compelling evidence for the importance of transdifferentiation of cholangiocytes to hepatocytes during liver regeneration and convincingly show that a functional ETC is crucial during this process as well. By applying state-of-the-art methods like single nucleus RNAseq, the authors were able to further characterize TLPCs (transitional liver progenitor cells), the intermediate progenitor cell populations, and found an increasing expression of genes related to lipid metabolism along the transdifferentiation process. Moreover, cholangiocytes may have a profound impact on liver composition and zonation even under homeostatic conditions. Even though these findings are thoroughly controlled, the study is strongly based on preclinical animal models. This creates an inherent methodological bias, due to obvious species-specific differences between mice and men.
However, several questions remain to be answered, such as the role of this metabolic “quality control” mechanism in other cell and tissue types. Obviously, mitochondrial inflexibility is a double-edged sword, since it clearly is associated with obesity and other unfavorable conditions. Therefore, it would appear necessary to induce metabolic inflexibility exclusively in liver cells, if one aims at a direct therapeutical application. Of note, it is currently not clear how hepatic PDK4, the main beneficial factor for liver regeneration identified in this study, could be safely activated or how its expression could be increased in a tissue-specific manner. This could make a direct translational application based on PDK4 challenging, especially in patients with chronic liver damage. From a clinical perspective, it is noteworthy that insulin is well known to directly inhibit the transcription of PDK4. Therefore, measures to restore insulin responsiveness by exercise and dietary interventions could have beneficial side effects for mitochondrial health in the context of liver regeneration. Taken together, clinical data would be essential to determine the relevance of these processes for human liver disease, and it is currently unclear how new therapeutic interventions could be derived from the study.
Wang, X. et al. Metabolic inflexibility promotes mitochondrial health during liver regeneration. Science 384 , 1189 (2024).
Article Google Scholar
Asrani, S. K., Devarbhavi, H., Eaton, J. & Kamath, P. S. Burden of liver diseases in the world. J. Hepatol. 70 , 151–171 (2019).
Article PubMed Google Scholar
Lesner, N. P. et al. Differential requirements for mitochondrial electron transport chain components in the adult murine liver. eLife 11 , e80919 (2022).
Article CAS PubMed PubMed Central Google Scholar
Yin, Y. et al. Gut microbiota promote liver regeneration through hepatic membrane phospholipid biosynthesis. J. Hepatol. 78 , 820–835 (2023).
Article CAS PubMed Google Scholar
Kindt, A. et al. The gut microbiota promotes hepatic fatty acid desaturation and elongation in mice. Nat. Commun. 9 , 3760 (2018).
Article PubMed PubMed Central Google Scholar
Download references
Acknowledgements
K.P.J. and J.E. acknowledge support from the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) project no 395357507 – SFB 1371. The project DEAL between Springer Nature and German Universities covers the publication costs.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Institute of Clinical Chemistry and Laboratory Medicine, Functional Lipidomics and Metabolism Research, University Hospital Regensburg, Regensburg, Germany
Josef Ecker & Sarah Brunner
Department of Surgery, School of Medicine and Health, Technical University of Munich, 81675, Munich, Germany
Klaus-Peter Janssen
You can also search for this author in PubMed Google Scholar
Contributions
J.E., S.B., and K.P.J. conceived and drafted the manuscript, S.B. prepared the figure. All authors critically revised the manuscript. All authors have read and approved the article.
Corresponding author
Correspondence to Klaus-Peter Janssen .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ecker, J., Brunner, S. & Janssen, KP. Metabolic inflexibility of mitochondria: beneficial for the fitness of regenerating liver cells. Sig Transduct Target Ther 9 , 233 (2024). https://doi.org/10.1038/s41392-024-01959-1
Download citation
Received : 23 July 2024
Revised : 19 August 2024
Accepted : 24 August 2024
Published : 09 September 2024
DOI : https://doi.org/10.1038/s41392-024-01959-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
iCliniq Cope
For doctors and hospitals
Ask a Doctor Online Now
Management of Liver Cirrhosis: An Overview of Surgical Approaches
Liver transplants, shunt operations, and minimally invasive methods are surgical approaches to manage liver cirrhosis.
Dr. Tadimeti Sravya
Medically reviewed by
Dr. Pandian. P
By subscribing, I agree to iCliniq's Terms & Privacy Policy.
Introduction
Liver cirrhosis is a serious, advancing condition in which normal tissue in the liver gets replaced by scar tissue, resulting in impaired liver function and complications. It may arise from prolonged alcohol abuse and non-alcoholic fatty liver, among other causes. Although medical treatments emphasize dealing with symptoms and decreasing disease progression, surgical procedures are essential for handling complications and improving patient survival. Liver transplantation, Transjugular Intrahepatic Portosystemic Shunt (TIPS) procedures, and minimally invasive procedures are the surgical procedures used to treat liver cirrhosis. By recognizing the function and efficiency of those surgical interventions, healthcare professionals can more effectively customize treatments to meet the unique needs of individuals with liver cirrhosis, subsequently enhancing quality of life and long-term prognosis.
What Are the Indications, Benefits, and Long-Term Outcomes of Liver Transplantation for Patients With End-Stage Liver Cirrhosis?
Technique Overview: Liver transplantation is the only effective treatment for end-stage liver disease caused by liver cirrhosis. In this procedure, a healthy donor liver replaces the diseased liver. Either a full or partial liver transplant (live donor liver transplant) can be performed.
Benefits and Indications: Patients with acute liver failure, hepatocellular cancer, and decompensated liver cirrhosis should consider liver transplantation. The complete replacement of the damaged liver, which can greatly enhance liver function and patient survival, is the key benefit of this surgery.
Surgical Outcomes: Liver transplant surgery results are usually good, with survival rates exceeding 70 percent after five years. However, the surgery is complicated and needs careful selection of patients and management of complications following surgery. Immunosuppression must be maintained for a long time to avoid transplant rejection.
What Are the Tips Procedure's Indications, Benefits, and Potential Complications in Liver Cirrhosis Patients?
Technique Overview: By directing blood flow away from the liver, the TIPS surgery produces a shunt between the portal and hepatic veins with a stent, which helps lower portal hypertension. This minimally invasive operation is carried out under fluoroscopic supervision.
Benefits and Indications: TIPS might benefit patients with portal hypertensive gastropathy (damage of the stomach lining), recurrent variceal hemorrhage (repeated bleeding from enlarged veins (varices) in the esophagus or stomach), and refractory ascites (excess fluid in the abdomen that does not respond to standard medical treatments). The primary benefits involve decreased portal pressure, reduced ascites, and prevention of variceal bleeding. It is especially beneficial for patients who are not candidates for liver transplantation.
Surgical Outcomes: TIPS surgery usually produces favorable outcomes, with significant improvements in problems associated with portal hypertension. Careful monitoring and management are necessary due to the possibility of hepatic encephalopathy and shunt malfunction.
What Are the Surgical Options for Managing Portal Hypertension in Liver Cirrhosis Patients?
Shunt Procedures: Shunt surgeries, which include portocaval, mesocaval, and splenorenal shunts, treat portal hypertension by redirecting blood flow away from the liver. The goals of these treatments are to lower portal pressure and prevent complications like variceal hemorrhage.
Benefits and Indications: Patients with portal hypertension who are not suitable candidates for TIPS or liver transplants might consider shunt operations. The main advantages are the prevention of potentially fatal variceal hemorrhage and a rapid lowering of portal pressure.
Surgical Outcomes: Although shunt surgeries can be successful, they have been linked to significant risks, such as hepatic encephalopathy and shunt occlusion. Choosing appropriate patients and managing them after surgery is crucial for obtaining favorable outcomes.
What Are the Surgical Approaches for Managing Hepatocellular Carcinoma (HCC) in Patients With Liver Cirrhosis?
Hepatic Resection: Hepatic resection includes the surgical excision of a portion of the liver affected by hepatocellular carcinoma . Patients with early-stage HCC and retained liver function are usually the ones who undergo this surgery.
Benefits and Indications: Hepatic resection is indicated for resectable HCC patients with normal liver function. The main advantage is the possibility of complete tumor removal, which increases the possibility of survival.
Surgical Outcomes: Hepatic resection for HCC has good surgical results; five-year survival rates vary from 40 percent to 70 percent based on the liver's number, size, and function. However, the possibility of recurrence continues to be a serious obstacle.
What Are the Surgical Approaches for Managing Ascites in Patients With Liver Cirrhosis?
Paracentesis: Paracentesis is done to drain ascitic fluid from the abdominal cavity for individuals with refractory ascites. It relieves symptoms and is frequently used in conjunction with other therapies to address ascites .
Benefits and Indications: Patients with large-volume or resistant ascites should consider paracentesis. The main advantages are immediate relief from symptoms, improved breathing, and less discomfort in the abdomen.
Surgical Outcomes: Paracentesis results are usually favorable and offer quick symptom reduction. Infection and protein depletion are possible, and repeated treatments could be required.
What Are the Surgical Approaches for Managing Variceal Bleeding?
Endoscopic Methods: Acute variceal hemorrhage can be treated with endoscopic methods such as band ligation (the base of a hemorrhoid or varix is wrapped with a rubber band to cut off its blood supply, causing the growth to fall off gradually) and sclerotherapy (a technique that involves injecting a chemical solution that shrinks the size of blood or lymph vessels). These operations can be performed during an endoscopic examination and are less invasive.
Benefits and Indications: Patients with active variceal hemorrhage or those who are at high risk of bleeding may consider endoscopic procedures. The main advantages include immediate management of bleeding and decreased likelihood of recurrent bleeding.
Surgical Outcomes: Endoscopic surgical procedures have positive results, with high success rates in controlling acute bleeding. However, these procedures do not treat the underlying portal hypertension, so bleeding is still a possibility.
What Are the Minimally Invasive Surgical Approaches for Managing Liver Cirrhosis?
Minimally Invasive Surgery
Advances in Surgical Techniques: Minimally invasive surgery, such as robotically assisted and laparoscopic procedures, has transformed the treatment of liver cirrhosis. These methods have a lower incidence of complications, shorter recovery periods, and less surgical stress.
Benefits and Indications: Minimally invasive methods are recommended for a range of surgical procedures in liver cirrhosis, such as splenectomy, shunt, and hepatic resection. The main advantages are less postoperative discomfort, faster recovery, and better cosmetic results.
Surgical Outcomes: Minimally invasive surgical procedures have favorable surgical outcomes, including lower incidence of complications and shorter hospital stays. These developments have made the surgical treatment for liver cirrhosis more secure and accessible to a larger range of patients.
The management of cirrhosis of the liver includes a range of surgical approaches to deal with specific complications and improve patient outcomes. Every approach has advantages and disadvantages of its own, ranging from minimally invasive operations and endoscopic methods to liver transplants and TIPS procedures. Patients suffering from this painful condition now have hope because of considerable improvements in the safety and effectiveness of these procedures due to advancements in surgical methods and preoperative evaluation. The treatment of liver cirrhosis has a bright future as long as research and surgical techniques advance. Recent advances can significantly enhance patient outcomes and quality of life.
Surgical Risk Assessment in Patients with Chronic Liver Diseases
https://pubmed.ncbi.nlm.nih.gov/35814505/
Surgery in the Patient with Liver Disease
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2917124/
Treatment for Cirrhosis
https://www.niddk.nih.gov/health-information/liver-disease/cirrhosis/treatment

General Surgery
Rate this article
Source Article Arrow Most popular articles

Ovulation and Safe Period: What is the Safe Period to Have Sex?

Dr. Sabita Laskar

Unwanted 72 - Uses, Dosage, Side Effects, Drug Warnings, and Precautions

Dr. Divya Banu M

Jelqing - Penis Enlargement Exercise

Dr. Ramchandra Lamba

Dolo 650 MG Tablet

Dr. Anshul Varshney

I-Pill - Uses, Dosage, Side Effects, Drug Warnings, and Precautions

Dr. Vasantha. K. S
Ask your health query to a doctor online
*guaranteed answer within 4 hours
Disclaimer: No content published on this website is intended to be a substitute for professional medical diagnosis, advice or treatment by a trained physician. Seek advice from your physician or other qualified healthcare providers with questions you may have regarding your symptoms and medical condition for a complete medical diagnosis. Do not delay or disregard seeking professional medical advice because of something you have read on this website. Read our Editorial Process to know how we create content for health articles and queries.
This website uses cookies to ensure you get the best experience on our website. iCliniq privacy policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Dietary Approaches to Stop Hypertension (DASH) and mortality risk among patients with liver cirrhosis: a prospective cohort study
Affiliations.
- 1 School of Nutrition and Food Sciences, Shiraz University of Medical Sciences, Shiraz, Iran.
- 2 Student Research Committee, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
- 3 Basic and Molecular Epidemiology of Gastrointestinal Disorders Research Center, Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 4 Clinical Nutrition and dietetics Department, Faculty of Nutrition Sciences and Food Technology, National Nutrition and Food Technology Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 5 Liver and Pancreatobiliary Research Center, Digestive Disease Research Institute, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran.
- 6 Gastroenterology and Liver Diseases Research Center, Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 7 Department of Nutrition Research, National Nutrition and Food Technology Research Institute, Faculty of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran. [email protected].
- PMID: 39232774
- PMCID: PMC11376012
- DOI: 10.1186/s13104-024-06928-z
Background and purpose: The relationship between dietary patterns and cirrhosis is undeniable. The present study aimed to investigate the association between the Dietary Approaches to Stop Hypertension (DASH) diet and the risk of mortality in patients with cirrhosis prospectively.
Methods: In this cohort study, 121 cirrhotic patients were enrolled and followed up annually for four years. Nutritional status and dietary intakes were assessed initially, and the DASH score was calculated accordingly. Crude and multivariable-adjusted hazard ratios (HR) with 95% confidence intervals (CI) were estimated using Cox proportional hazard analyses.
Results: DASH components including fruits, vegetables, legumes, nuts and seeds, and low-fat dairy products were significantly associated with lower mortality risk in cirrhotic patients. Also, a higher DASH score was significantly associated with a reduction in the risk of mortality in patients with cirrhosis, so that after adjusting for all confounders, the risk of mortality in the upper tertile was 89% lower than the first tertile (HR = 0.11, 95% CI: 0.03-0.42, P trend < 0.001). The 4-year survival rate among patients across tertiles of DASH was 32%, 37%, and 46%, respectively (P = 0.005).
Conclusion: It can be concluded that a higher DASH diet score may be associated with a reduced risk of mortality in cirrhotic patients. However, larger studies are needed to confirm the findings and determine their potential mechanisms.
Keywords: Cirrhosis; DASH; Mortality; Survival.
© 2024. The Author(s).
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
Multivariate hazard ratios of DASH…
Multivariate hazard ratios of DASH tertiles for mortality in patients with cirrhosis according…
Kaplan-Meier survival curve for death…
Kaplan-Meier survival curve for death among cirrhotic patients stratified by tertiles of DASH…
- Yao CK, Fung J, Chu NHS, Tan VPY. Dietary interventions in liver cirrhosis. J Clin Gastroenterol. 2018;52(8):663–73. 10.1097/MCG.0000000000001071 - DOI - PubMed
- Ginès P, Krag A, Abraldes JG, Solà E, Fabrellas N, Kamath PS. Liver cirrhosis. Lancet. 2021;398(10308):1359–76. 10.1016/S0140-6736(21)01374-X - DOI - PubMed
- Pashayee-khamene F, Hatami B, Cheraghpour M, Yari Z. Keeping an eye on the nutrition: the importance of nutrition management on cardiometabolic risk factors in cirrhotic patients. Clin Nutr ESPEN. 2023. - PubMed
- GinËs P, Krag A, Abraldes J, Sol‡ E, Fabrellas N, Kamath PS. Liver Cirrhosis Lancet. 2021;398(10308):1359–76. - PubMed
- Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–71. 10.1016/j.jhep.2018.09.014 - DOI - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Search the site GO Please fill out this field.
- Newsletters
- Vitamins and Supplements
Can Supplements Boost Liver Health?
:max_bytes(150000):strip_icc():format(webp)/SuzanneFisher-9cf2794cb7e14044ae6aafcb78c59f19.png)
Why Liver Function Is Important
- Supplements
What To Consider
Liver health support.
nomadnes / Getty Images
Your liver is responsible for many bodily functions, including detoxification, balancing your metabolism, and helping your body digest food.
Complications with your liver can lead to chronic liver diseases and, in severe cases, liver cancer. Many supplements on the market promise to help protect your liver, reduce inflammation, and improve liver function. However, there is not enough research on many supplements to determine their effectiveness for your long-term health.
More human studies are needed to verify the effects of supplements on liver health.
Your liver is responsible for removing waste from your blood and storing energy. This helps with other processes like producing cholesterol, regulating amino acids (the building blocks of protein), and storing glucose in your body.
Other liver functions include:
- Storing vitamins A, D, C, and vitamin B12
- Producing bile to help ease digestion and absorb fats
- Breaking down hemoglobin (a protein that delivers oxygen throughout your body)
Viral infections, like hepatitis B and C, can weaken your liver. Visible symptoms include jaundice , a health condition where the eyes and skin have a yellowish hue because of a lack of or overproduction of bilirubin. Other common causes of liver dysfunction include alcoholic liver disease, genetics, and non-alcoholic fatty liver disease.
Popular Supplements for Liver Health
Though more research is needed, research suggests that certain supplements may support liver health.
Milk Thistle
Milk thistle ( Silybum marianum ) is a flowering herb native to Europe with liver-protecting properties.
As an antioxidant, silymarin (a flavonoid in milk thistle seeds) helps prevent inflammation that can lead to liver disorders. Silymarin also combats cell-damaging free radicals, prevents fibrosis (scarring) in your liver, and increases enzymes needed for detoxification.
A few studies of people with fatty liver disease, viral hepatitis, and cirrhosis support these findings. Still, more research is needed to confirm if milk thistle affects your liver enough to produce long-term results.
Artichoke Leaf
Artichoke ( Cynara scolymus ), an edible plant from the Mediterranean region, is a common ingredient in most liver supplements. The leaves are rich in antioxidants that help prevent certain compounds from damaging your liver.
Antioxidants like cynarin and chlorogenic acids reduce elevated levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT), which can cause liver damage . Larger studies and additional research are needed to confirm these findings.
Dandelion Root
Dandelion ( Taraxacum officinale ) is a medicinal herb with several beneficial compounds that may improve liver function. Dandelion roots and leaves contain active compounds, such as phenolic acids, flavonoids, and polysaccharides, that act as anti-inflammatory and antioxidant agents. Dandelions can protect the body from free radicals that may damage healthy cells.
Oligofructans in dandelions may help reduce lipid (fat) and inflammation in your liver. Many of these findings are connected to animal studies. More human studies are needed to know how much dandelion extract in supplements benefits your liver.
Jujube ( Ziziphus jujuba ), also known as red date or Chinese date, is a small oval-shaped fruit. Its seed is rich in antioxidants that protect the body against free radicals. Studies on jujube syrup found that it may help prevent liver toxicity in people receiving treatment for tuberculosis. However, more research is needed on jujube as a supplement ingredient.
A selenium deficiency may increase your risk for chronic liver conditions like hepatitis, liver cirrhosis, and liver cancer.
Selenium is involved with several processes in your body, including helping with thyroid function and protecting your body from infection. Antioxidant enzymes like glutathione peroxidase in selenium help protect liver cells from damage by reducing unstable oxygen molecules.
Choline is a nutrient essential for transporting fats out of your liver. Choline supplements can help increase low choline levels, which can cause too much fat to be stored in your liver. Too much fat in your liver can cause non-alcoholic fatty liver disease (NAFLD). More research is needed to verify the effect of choline on reducing your risk of NAFLD.
Dietary and herbal supplements have not yet been evaluated for safety or approved by the U.S. Food and Drug Administration (FDA). This means there is currently no way to verify if the ingredients listed on the label are consistent with each supply of supplements. If you choose to add supplements to your routine, try to stick to those that have completed third-party testing to ensure they are free of harmful contaminants.
Always consult your healthcare provider before purchasing a supplement. Some supplements may negatively interact with certain medications.
While evidence on the effects of supplements in protecting your liver is limited, there are several lifestyle changes you can make to prevent chronic liver diseases.
Strategies to support your liver include the following:
- Bee mindful of your intake of saturated and trans fats, especially in processed foods
- Eat more fiber-rich, low-glycemic foods like fruits, vegetables, and whole grains
- Reduce your intake of added sugars
- Keep your alcohol consumption low
- Get at least 30 minutes of physical activity into your daily schedule
- Stick to a consistent diet
- Make sure you get at least 7-9 hours of sleep each night
During routine doctor visits, you can request that your healthcare provider perform a liver function test to know the status of your liver health. Although these tests cannot predict diseases, they can indicate to your healthcare provider if there is any unusual activity in your liver. Your healthcare provider may suggest a follow-up visit if anything looks out of the ordinary.
A Quick Review
The liver is among the hardest-working organs in the human body. It is responsible for detoxification, proper digestion, and nutrient storage.
Certain dietary supplements like milk thistle, artichoke leaf, and dandelion may help improve your liver function by reducing inflammation and harmful cells in your body. However, more research is needed to verify the effects these supplements have on your liver health.
The FDA does not have guidelines for dietary or herbal supplements. It is important to check with your healthcare provider before adding any supplements to your routine, especially if you also take other medications.
:max_bytes(150000):strip_icc():format(webp)/DSC00324.01-3-47d3d32d4c4d466b92a3a66bc24756c6.jpg)
Kalra A, Yetiskul E, Wehrle CJ, Tuma F. Physiology, liver . In: StatPearls . StatPearls Publishing; 2024
National Institute of Diabetes and Digestive and Kidney Diseases. Liver disease .
Trefts E, Gannon M, Wasserman DH. The liver . Curr Biol . 2017;27(21):R1147-R1151. doi:10.1016/j.cub.2017.09.019
Sharma A, Nagalli S. Chronic Liver Disease . In: StatPearls . StatPearls Publishing; 2024
National Center for Complementary and Integrative Health. Milk Thistle .
Achufusi TGO, Pellegrini MV, Patel RK. Milk Thistle . In: StatPearls . StatPearls Publishing; 2024
Gillessen A, Schmidt HH. Silymarin as supportive treatment in liver diseases: A narrative review . Adv Ther . 2020;37(4):1279-1301. doi:10.1007/s12325-020-01251-y
de Avelar CR, Pereira EM, de Farias Costa PR, de Jesus RP, de Oliveira LPM. Effect of silymarin on biochemical indicators in patients with liver disease: Systematic review with meta-analysis . World J Gastroenterol . 2017;23(27):5004-5017. doi:10.3748/wjg.v23.i27.5004
Amini MR, Sheikhhossein F, Talebyan A, Bazshahi E, Djafari F, Hekmatdoost A. Effects of artichoke supplementation on liver enzymes: A systematic review and meta-analysis of randomized controlled trials . Clin Nutr Res . 2022;11(3):228-239. Published 2022. doi:10.7762/cnr.2022.11.3.228
Mahboubi, Mohaddese; Mahboubi, Mona. Hepatoprotection by dandelion (Taraxacum officinale) and mechanisms . Asian Pacific Journal of Tropical Biomedicine 10(1):2020. doi:10.4103/2221-1691.273081
Lu Y, Bao T, Mo J, Ni J, Chen W. Research advances in bioactive components and health benefits of jujube ( Ziziphus jujuba Mill.) fruit . J Zhejiang Univ Sci B . 2021;22(6):431-449. doi:10.1631/jzus.B2000594
Lin Y, He F, Lian S, et al. Selenium status in patients with chronic liver disease: A systematic review and meta-analysis . Nutrients . 2022;14(5):952. Published 2022. doi:10.3390/nu14050952
Xu L, Lu Y, Wang N, Feng Y. The role and mechanisms of selenium supplementation on fatty liver-associated disorder . Antioxidants (Basel) . 2022;11(5):922. Published 2022. doi:10.3390/antiox11050922
National Institutes of Health Office of Dietary Supplements. Choline .
Food and Drug Administration. Facts about Dietary Supplements .
National Institutes of Health. Dietary Supplements: What You Need to Know .
Philip Esteban J, Dinani A. Lifestyle interventions beyond diet and exercise for patients with nonalcoholic fatty liver disease . Gastroenterol Hepatol (N Y) . 2020;16(3):119-130.
Medline Plus. Liver Function Tests .
Related Articles
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Alcohol consumption and risk of liver cirrhosis: a systematic review and meta-analysis
Michael Roerecke, Afshin Vafaei, Omer SM Hasan, Bethany R Chrystoja, Jürgen Rehm
Centre for Addiction and Mental Health, Institute for Mental Health Policy Research, 33 Russell Street, Toronto, Ontario, Canada M5S 2S1
Marcus Cruz, Roy Lee, Manuela G Neuman
In Vitro Drug and Biotechnology, Banting Institute, lab. 217, 100 College St., Toronto, Ontario, M5G 1L5, Canada
Authors’ contributions
Associated Data
To systematically summarize the risk relationship between different levels of alcohol consumption and incidence of liver cirrhosis.
Medline and Embase were searched up to March 6 th , 2019 to identify case-control and cohort studies with sex-specific results and more than two categories of drinking in relation to incidence of liver cirrhosis. Study characteristics were extracted and random-effects meta-analyses and meta-regressions were conducted.
A total of seven cohort studies and two case-control studies met the inclusion criteria, providing data from 2,629,272 participants with 5,505 cases of liver cirrhosis. There was no increased risk for occasional drinkers. Consumption of 1 drink per day in comparison to long-term abstainers showed an increased risk for liver cirrhosis in women, but not in men. The risk for women was consistently higher compared to men. Drinking ≥5 drinks per day was associated with a substantially increased risk in both women (RR = 12.44, 95% CI: 6.65 – 23.27 for 5–6 drinks, and RR = 24.58, 95% CI: 14.77 – 40.90 for ≥7 drinks) and men (RR = 3.80, 95% CI: 0.85 – 17.02, and RR = 6.93, 95% CI: 1.07 – 44.99, respectively). Heterogeneity across studies indicated the additional impact of other risk factors.
Conclusions
Alcohol is a major risk factor for liver cirrhosis with risk increasing exponentially. Women may be at higher risk compared to men even with little alcohol consumption. More high-quality research is necessary to elucidate the role of other risk factors, such as genetic vulnerability, body weight, metabolic risk factors, and drinking patterns over the life course. High alcohol consumption should be avoided, and people drinking at high levels should receive interventions to reduce their intake.
INTRODUCTION
Alcohol is a major risk factor for liver disease in general, and for liver cirrhosis in particular.( 1 – 3 ) In fact, about half of the liver cirrhosis burden of morbidity and mortality would disappear in a world without alcohol.( 4 ) Mortality from liver cirrhosis has been on the rise in the US( 5 ) and Europe,( 6 ) more so in women than in men. Alcohol consumption is partly responsible, but liver disease is increasingly recognized as a multifactorial disease process.( 6 )
The importance of alcohol in the etiology of liver disease has led to establishing different codes for categories of liver diseases, which are considered to be primarily caused by alcohol. Thus, the International Classification of Diseases (ICD-10( 7 )) recognizes several forms of alcoholic liver disease (ICD-10, K70), sometimes considered stages( 8 ) that range from relatively mild and reversible alcoholic hepatic steatosis (fatty liver) (K70.0) and alcoholic hepatitis (K70.1), to alcoholic fibrosis and sclerosis of the liver (K70.2), and further to severe and irreversible stages such as alcoholic liver cirrhosis (K70.3) and alcoholic hepatic failure (K70.4). Alcohol consumption, in particular heavy use over time, has been found crucial in the etiology and progression of these diseases.( 1 , 9 , 10 ) However, liver diseases are multifactorial, and alcohol use may play a role in the progression of all types of cirrhosis,( 11 ) and even one drink per day may have an effect on the incidence of liver cirrhosis, ( 12 ). For scientific review of all liver cirrhosis, it is therefore crucial to include both alcoholic and non-alcoholic liver cirrhosis when examining the impact of alcohol use.
Most of the epidemiological literature to date has dealt with the level of drinking and incidence or mortality of liver cirrhosis.( 13 ) It followed the epidemiological tradition of the early studies of Lelbach and others,( 14 , 15 ) who, based on studies in people with alcohol use disorders, postulated a clear association between volume of alcohol use and liver cirrhosis.( 1 ) This association was corroborated in more rigorous studies.( 1 , 13 , 16 ) It remains to be determined, however, if a threshold for alcohol-related damage to the liver exists, or whether any amount of alcohol increases the risk for liver cirrhosis, which has been discussed recently.( 17 – 19 ) In fact, the last meta-analysis on the topic is now more than 10 years old and found some evidence for a protective association at low levels of alcohol intake in men.( 13 ) Furthermore, several large-scale studies have been published since then.( 20 – 22 )
The present review provides an overview of the current knowledge on the dose-response relationship between alcohol consumption and risk of liver cirrhosis in comparison to abstainers, with particular consideration given to the effects of study design and sex, and other subgroups where data were available. As noted above, our review was not restricted to alcoholic liver cirrhosis.
Search strategy and selection criteria
Following the MOOSE guidelines,( 23 ) we conducted a systematic electronic literature search using Medline and Embase from inception to March 6 th , 2019 for keywords and MeSH terms relating to alcohol consumption, liver cirrhosis, and observational studies ( Supplementary Table 1 ). Additionally, we searched reference lists of identified articles and published meta-analyses and reviews. Inclusion criteria were as follows:
- cohort and case-control studies examining the sex-specific association between average alcohol consumption and liver cirrhosis,
- analyses were adjusted for age at baseline,
- data for at least two quantitatively defined categories of average alcohol consumption in relation to non-drinkers, or data for former drinkers in relation to long-term abstainers were reported,
- more than 50 cases of liver cirrhosis occurred.
We did not apply language restrictions. At least two reviewers independently excluded articles based on title and abstract or full-text and abstracted the data. Any discrepancies were resolved in consultation with a third reviewer.
Data extraction
From all relevant articles we extracted authors’ names, year of publication, country, year(s) of baseline examination, follow-up period, setting of the study, study design, assessment of liver cirrhosis, age (range, mean or median) at baseline, sex, number of observed liver cirrhosis cases among participants by drinking group, number of total participants by drinking group, specific adjustment or stratification for potential confounders, and adjusted relative risks (RRs) and their confidence intervals (CIs) or standard errors. Risk estimates by sex were treated as independent samples. Where necessary, RRs within studies were re-calculated to contrast alcohol consumption categories against non-drinkers.( 24 )
Exposure and outcome assessment
Consolidating exposure measures across primary studies involved a two-step process. First, among drinkers, we converted reported alcohol intake categories in primary studies into an average of pure alcohol in grams per day (g/day) using the midpoints (mean or median) of reported drinking group categories. For open-ended categories, we added three quarters of the second highest category’s range to the lower limit of the open-ended category of alcohol intake if the mean was not reported. Standard drinks vary by country, with one standard drink containing approximately 8–14 g of pure alcohol.( 25 ) We used reported conversion factors when standard drinks were the unit of measurement to convert all measures to grams per day. Then, for reporting of our analyses, we considered categories with a mean of up to 12 grams pure ethanol as one standard drink for a global representation. Qualitative descriptions, such as ‘social’ or ‘frequent’ drinkers with no clear total alcohol intake in g/day were excluded. When current non-drinkers were the reference group (i.e., including both long-term abstainers and former drinkers), we adjusted risk estimates for the effect of former drinking compared to long-term abstention, based on the pooled risk for former drinking from two studies included in this review to avoid the sick-quitter effect. Long-term abstainers were defined as people who stated that they never consumed alcohol,( 20 ) people who stated that they never, or almost never, drank alcohol in the past,( 26 ) and when people who had greatly decreased their consumption in the last 10 years were excluded from non-drinkers.( 27 ) The logRR for former drinkers in comparison to long-term abstainers (RR former drinkers = 2.52) was multiplied by the mean fraction of former drinkers among current non-drinkers (0.23) and added to the respective logRRs of current drinking groups from primary studies used in our analysis when current non-drinkers was the reference group.
Liver cirrhosis due to known aetiology such as alcohol, and unspecified liver cirrhosis was defined as in the primary studies, which included ICD codes for liver cirrhosis (ICD-7: 581; ICD-8: 571; ICD-10: K70, K73, K74) and unspecified liver cirrhosis (ICD-8: 571.9, 456.0, 785.3; ICD-10: I85.0, I85.9, K74.6, R18.9). Because we aimed to estimate the relative risk in comparison to abstainers, we excluded several studies (e.g., ( 28 , 29 )) which focused only on alcoholic liver cirrhosis (or included alcoholism in addition to liver cirrhosis in the outcome),( 30 ) which, by definition, cannot occur in lifetime abstainers.
Quality assessment
Most quality scores are tailored for meta-analyses of randomized trials of interventions( 31 – 33 ) and many criteria do not apply to epidemiological studies examined in this study. Additionally, quality score use in meta-analyses remains controversial.( 34 – 36 ) As a result, study quality was enhanced by including quality components, such as study design, measurement of alcohol consumption and liver cirrhosis, adjustment for age in our inclusion and exclusion criteria, and further by investigating potential heterogeneity in several sensitivity analyses. We used the most adjusted RR reported and the most comprehensive data available for each analysis and gave priority to estimates where lifetime or long-term abstainers were used as the risk reference group.
In a formal risk of bias analysis, we used the Cochrane Risk of Bias Tool for Non-Randomized Studies (ROBINS-I( 37 )) to assess risk of bias in primary studies. We rated the evidence for the association between alcohol consumption and incidence of liver cirrhosis based on the Grades of Recommendation, Assessment, Development and Evaluation system (GRADE).( 38 )
Statistical analyses
In categorical analyses using standard drinks (12 grams pure alcohol) as the exposure measure, RRs were pooled with inverse-variance weighting using DerSimonian-Laird random-effect models to allow for between-study heterogeneity.( 39 ) Small-study bias was examined using Egger’s regression-based test.( 40 ) Variation in the effect size because of heterogeneity between studies was quantified using the I 2 statistic.( 41 )
Using studies that reported data for four or more alcohol intake groups, we conducted two-stage restricted cubic spline regression analysis in multivariate meta-regression models, taking into account the variance-covariance matrix for risk estimates derived from one reference group( 42 , 43 ) to test for non-linear dose-response relationships in relation to long-term abstainers. All meta-analytical analyses were conducted on the natural log scale in Stata Statistical Software, Version 14.2.
Role of funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
In total, out of 2,977 identified references, 385 articles were retrieved in full-text. Of these, seven cohort and two case-control studies fulfilled our inclusion criteria ( Figure 1 ). Four studies were conducted in the US,( 26 , 27 , 44 , 45 ), two in Italy,( 46 , 47 ) and one each in China,( 22 ) the UK,( 21 ) and Denmark.( 20 ) In total, data from 2,629,272 participants (579,592 men, 2,049,680 women) and 5,505 cases of liver cirrhosis (2,196 men, 3,309 women) were used in the analyses. All cohort studies included liver cirrhosis mortality as the outcome. The two case-control studies investigated first-time diagnosis of symptomatic liver cirrhosis in comparison to lifetime abstainers ( Table 1 ). The study by Liu et al contributed 2,078 liver cirrhosis cases from the National Health Service Million Women Study linked to death and morbidity registries.( 21 ) The proportion of non-drinkers varied widely, from 0.002% (lifetime abstainers) among men in the Danish study by Askgaard et al. ( 20 ) to 80% (current abstainers) in the study of women from the American Cancer Society I cohort by Garfinkel et al .( 44 ) All cohort studies used a one-time measurement of alcohol consumption as the baseline alcohol intake, while the three case-control studies from Italy assessed lifetime alcohol consumption retrospectively. All but one cohort study were rated to be of moderate quality mainly because of the one-time measurement of alcohol consumption at baseline (cohort studies), and the observational study design ( Supplementary Table 2 ). One cohort study( 44 ) had potential serious bias because the results were adjusted only for age.

Flowchart of study selection
Characteristics of 7 cohort and 2 case-control studies investigating risk of liver cirrhosis by alcohol intake, 1988–2017.
| Reference | Baseline years, setting | Sex, age (years), country, cases (no.), participants (no.), follow-up time (years) | Exposure assessment | Outcome assessment | Adjustments |
|---|---|---|---|---|---|
| Askgaard et al, 2015( ) | 1993–1997, Danish men and women aged 50 to 64 participating in the Diet, Cancer, and Health study Exclusions: Previously diagnosed with cancer or alcoholic cirrhosis, missing or conflicting information on alcohol, smoking, education, and waist circumference. | M, W 55.9 Denmark Women: 229 cases 29,221 participants Men: 393 cases 26,696 participants 14.9 | Lifetime abstainers, former drinkers, current drinkers: (<14, 14–28, >28) d/week | Mortality from liver cirrhosis (obtained from the National Patient Register and the Danish Register of Causes of Death. ICD-8: 571.0 and ICD-10: K70.3, and codes for unspecified cirrhosis, ICD-8: 571.9, 456.0, 785.3 and ICD-10: I85.0, I85.9, K74.6, R18.9) | Age (underlying time axis), smoking, education, waist circumference. Subgroups: by drinking frequency. |
| Bofetta et al, 1990( ) | 1959, American Cancer Society volunteers (White men aged 40–59) from 25 states in the United States. | M, 49.5 (40–59), USA 732 276,802 12 | Current abstainers, occasional drinkers, irregular drinkers, current drinkers: (1, 2, 3, 4, 5, ≥6) d/day | Mortality from liver cirrhosis. ICD-7 code: 581 | Age (5-year groups), smoking (non-smoker, 1–20 cigarettes per day, 21+ cigarettes per day) |
| Corrao et al, 1993( ) | 1986–1990, Consecutive admissions from the emergency ward to the Division of Gastroenterology in Turin. Exclusion: Hepatocellular carcinoma, primary biliary cirrhosis. | M, W 58.7 Italy Men: 207 cases, 207 controls Women: 113 cases, 113 controls N/A | Lifetime abstainers, average lifetime intake: <50, 50–100, 100–150, 150–200, 200–250, >250) g/day | First-time diagnosis of liver cirrhosis based on signs of liver failure (ascites and/or encephalopathy and/or jaundice, or bleeding from ruptured oesophageal varices) | Matched on age (±5 years), sex. Subgroups: Stratified by duration of drinking (10, 20, ≥30 years); by age group (≤60 years, >60 years). |
| Corrao et al, 1997( ) | 1986–1990, Patients admitted to a) medical departments of 6 district hospitals (L’Aquila, 1989–1990), b) gastroenterology unit of a district hospital (Turin, 1993), c) medical departments of 16 hospitals nationwide (SIDECAR project, 1994–1996). Exclusion: Hepatic encephalopathy, hepatocellular carcinoma, primary biliary cirrhosis, Wilson’s disease, haemochromatosis, or acute causes of liver damage. Controls: Selected from the same hospitals for diseases unrelated to alcohol consumption (excluded were: orthopaedic and infectious diseases, patients from the psychiatry, gynaecology, obstetric departments, and gastroenterologic, metabolic, neoplastic, and cardiovascular diseases). | M, W 57 Italy Men: 300 cases, 355 controls Women: 162 cases, 296 controls N/A | Lifetime abstainers, average lifetime intake: <50, 50–100, >100) g/day | First-time diagnosis of liver cirrhosis based on signs of liver decompensation (ascites, jaundice, oedema, or bleeding from ruptured oesophageal varices), confirmed by liver biopsy in 319 cases. | Age (3 categories), area of residence, HCV status, HBsAg status Subgroups( ): HBsAg and/or anti-HCV positive participants were excluded. |
| Fuchs et al, 1995( ) | 1980, The Nurses’ Health Study (female registered nurses). Exclusion: ≥10 or more food items left blank, implausibly high or low scores for total food intake, history of cancer, angina, myocardial infarction, or stroke, women who reported no alcohol intake at baseline in 1980 but had greatly decreased their alcohol intake in the previous 10 years. | W, 42.5 (30–55), USA 52 85,709 12 | Long-term abstainers, current drinkers: (0.1–1.4, 1.5–4.9, 5–14.9, 15–29.2, ≥30) g/day | Mortality from liver cirrhosis. ICD-8 code: 571 | Age (5-year groups), smoking (never, <15, 15–24, >24 cigarettes per day), BMI, aspirin use, regular cholesterol level, diabetes, hypertension, myocardial infarction in a parent at 60 years of age, past or present oral-contraceptive use’ menopausal status, past or present postmenopausal hormone use, and energy-adjusted intake of dietary fiber and saturated fat |
| Garfinkel et al, 1988( ) | 1959–1960, American Cancer Society’s study (A prospective study of 581 321 women) Exclusion: Women with breast cancer | W, 45, USA 589 581,321 12 | Current abstainers, current drinkers: (occasional, 1, 2, 3, 4, 5, ≥6) d/day | Mortality from liver cirrhosis | Age (standardized mortality ratio stratified into 5-year age groups) |
| Klatsky et al, 2003( ) | 1978–1998, Kaiser Permanente Medical Care Program | M, W, 40.6 USA Men: 146 cases 56,836 participants Women: 86 cases 72,008 participants 20 | Lifetime abstainers, ex-drinkers, current drinkers: (<1 drink/month, >1 drink/month but <1 drink/day, 1–2, 3–5, ≥6) d/day | Mortality from liver cirrhosis ascertained by using an automated matching system to ascertain death in California | Age (undefined), race, BMI, education, marital status, smoking (never, ex, <1 pack, >=1 pack a day), coronary disease risk/symptoms |
| Liu et al, 2009( ) | 1996–2005, Women who were recruited through the United Kingdom National Health Service (NHS) Breast Screening Service (The Million Women Study). Exclusion: Hospital admission for or reported a history of either of the diagnoses of interest (liver cirrhosis or gallbladder disease) before recruitment, a diagnosis of cancer (except nonmelanomatous skin cancer (ICD-10 code C44)), self-reported hepatitis or had a record of viral hepatitis (ICD-10 codes B15–B19) at recruitment or during follow-up. | W, 56, UK 2078 1,280,737 6.1 | Current abstainers, current drinkers: (1–2, 3–6, 7–14, > 15) units/week | Mortality and incidence of liver cirrhosis with record linkage to the NHS central registries for deaths, cancers, and emigrations, and to the Hospital Episode Statistics for England, and Scottish Morbidity Records for hospital admission data: ICD-10 codes: K70, K73, K74 | Age (underlying time axis), region of recruitment, SES, BMI, smoking (never, past, current: 1–9, 10–19, >=20 cigarettes per day). Subgroups: by smoking status. Subgroups among drinkers by drinking frequency, drinking with or without meals, and type of beverage.( ) |
| Yang et al, 2012( ) | 1990–1991, Men randomly selected from China’s National Disease Surveillance Points (23 urban and 22 rural areas). Exclusion: A prior disease, deaths within the first 3 years of follow-up, missing values. | M, 54.3, China 418 218,189 15 | Current abstainers, current drinkers: (<140, 140–279, 280–419, 420–699, ≥700) g/week | Mortality due to liver cirrhosis, obtained from official death certificates using ICD-9 | Age (stratified by 5-year groups), area, smoking, education |
Abbreviations: BMI, body mass index; M, men; W, women; M, W, men and women stratified; M/W, men and women combined; SES, socioeconomic status; NHS, National Health System.
The pooled proportion of former drinkers among current abstainers( 20 , 26 ) was 23%, and the pooled RR for liver cirrhosis in comparison to long-term abstainers was 2.56 (95% CI: 0.93 – 6.79). Figure 2 displays the RRs for liver cirrhosis in cohort studies by alcohol intake in reference to long-term abstainers after current abstention at baseline was adjusted for the proportion and risk in former drinkers. Alcohol consumption beyond occasional drinking, which showed a similar risk compared to long-term abstainers, was associated with increasing risk for liver cirrhosis ( Figure 2 ) with a pooled RR of 10.70 (95% CI: 2.95–38.78) for consumption of 7 drinks or more per day. However, all drinking categories showed substantial heterogeneity across studies (I 2 between 70 and 98%, all P-values <0.001), resulting in large confidence intervals. We restricted analyses of small-study effects and influential studies to drinkers of 1 or 2 drinks per day for both sexes because of the small number of studies identified. We found no statistical evidence for small study bias for drinkers of 1 or 2 drinks per day (P = 0.94), the funnel plot showed similar results ( Supplementary Figure 1 ). None of the studies had an overly large impact on the pooled estimates ( Supplementary Figure 2 ).

Relative risk on the log scale. 1 standard drink = 12 grams pure ethanol per day. RR = relative risk.
Results for men and women are shown separately in Figures 3 and and4, 4 , respectively. Across all consumption levels, RRs in women were higher, reaching RR = 24.58 (95% CI: 14.77–40.90) for ≥7 drinks. While consumption of 1–2 drinks was associated with a substantially elevated risk for liver cirrhosis in women, this was not the case in men. However, these results need to be interpreted with caution because of the small number of studies available. Four cohort studies( 20 , 21 , 26 , 27 ) in women were adjusted for age, BMI or waist circumference, and smoking. The relationship was similar to the main analysis with an elevated and linearly increasing risk for consumption of 1 drink and beyond ( Supplementary Figure 3 ).

In both men and women, there was no evidence for a non-linear dose-response relationship on the log scale (P=0.24 and 0.27, respectively, Supplementary Figures 4 and 5 ). However, the number of studies available was low, resulting in little power to detect non-linearity.
The two case-control studies with liver cirrhosis morbidity as the outcome yielded smaller risks associated with alcohol consumption, with 1–4 drinks showing no risk increase compared to lifetime abstainers (pooled RR=1.19, 95% CI: 0.58–2.43, Figure 5 ). Risks for consumption of 5–8 and 9–13 drinks were associated with large heterogeneity with one study( 47 ) showing substantial risk increases for both men and women, while the other study( 46 ) showed no or marginally statistically significant risk increases for either men or women (see also Supplementary Figures 6 and 7 ).

Subgroup analyses
One cohort study( 21 ) showed that while the risk in smokers was higher than in never-smokers, the risk of liver cirrhosis by alcohol intake increased in never-smokers similar to current smokers, indicating that smoking is a confounder but not an effect modifier. In another report( 48 ) from the case-control studies by Corrao et al , it was shown that the relationship between alcohol and liver cirrhosis in all participants was similar to participants without serum HBsAg and/or positive anti-HCV status. One of the case-control studies( 46 ) included in our main analysis also showed that the risk for liver cirrhosis was greatest in drinkers who drank heavily for 10 or 20 years, but not for 30 years, indicating potentially a survivor bias. Similarly, the same study( 46 ) reported risk by age (≤60 years and > 60 years), showing that the risk increase was stronger in younger participants for both sexes. The cohort study by Askgaard et al. ( 20 ) reported results by frequency of drinking days adjusted for weekly alcohol intake. In men, there was an increased risk for daily drinking in comparison to drinking on 2–4 days per week (RR = 2.25, 95% CI: 1.68–3.00). In women, the RR was 1.28 (95% CI: 0.82–2.02). Results from the UK Million Women study( 49 ) showed that among drinkers daily drinking in comparison to non-daily drinking (RR = 1.61, 95% CI: 1.40–1.85) and drinking with meals in comparison to drinking outside of meals (RR = 0.69, 95% CI: 0.62–0.77) were associated with incidence of liver cirrhosis. These associations were similar in strata of BMI, smoking status, and type of alcoholic beverage. Women who both drank daily and outside of meals had a 2.47 (95% CI: 1.96–3.11) increased risk for liver cirrhosis with adjustment for amount and type of beverage.( 49 )
Given the observational nature of the studies included in this report, we rate the evidence for a causal effect of alcohol consumption and risk for liver cirrhosis as moderate. However, the dose-response relationship in addition to established biological pathways confirmed in randomized controlled trials( 50 ) give rise to high confidence in a causal dose-response relationship. There was no clear indication for a threshold effect, but we rate the quality of the evidence as low because of imprecision and the small number of studies reporting sex-specific RRs for low levels of drinking.
We conducted a systematic review and various meta-analyses on alcohol consumption and risk of liver cirrhosis. Contrary to prior analyses,( 13 ) we found overall no protective effects at any level of drinking when compared to long-term abstainers, and a steadily increasing dose-response relationship in women, and some evidence for a threshold effect in men. However, risks varied widely and the analysis of case-control studies showed no risk increase for consumption of 1–4 drinks per day. The high risk for heavy drinkers found in our meta-analysis of cohort studies is in line with prior research on risk for liver cirrhosis in people with alcohol use disorders.( 11 , 51 , 52 ) The pooled RRs from case-control studies were much smaller; however, the more recent case-control study( 47 ) corresponds with the risks found in people with alcohol use disorder. One of the cohort studies and one of the case-control studies reported very small RRs compared to the other studies. The reasons for this are unclear, although some outliers are to be expected in any statistical analysis.
Additionally, many studies were not well adjusted and of generally moderate methodological quality, mostly related to potential bias due to confounding and selection bias. While the increase in risk was stronger in women, confidence intervals were large and overlapped with those for men. Stronger effects in women are supported by studies in people with alcohol use disorder with or without liver cirrhosis( 53 , 54 ), and higher hepatotoxicity. While there is no doubt that heavy alcohol consumption is one of the main risk factors for liver cirrhosis, the large heterogeneity observed indicates that the multifactorial nature of development of liver cirrhosis has not been reflected in the epidemiological literature. Liver cirrhosis has a complex and not fully understood etiology, and the contributory role of other risk factors for liver cirrhosis, such as BMI, metabolic syndrome, diabetes, drinking frequency and outside of meals, and others, at any given level of alcohol intake over the life course, need more attention in both research and prevention efforts.
While several important confounders have been identified and should be adjusted for in epidemiological studies, it is likely that some of them are in fact effect modifiers that impact the risk associated with alcohol consumption. Most important here is genetic vulnerability. Twin studies have shown a three-fold higher disease concordance between monozygotic twins and dizygotic twins, but the genetic case-control studies have not yet led to conclusive results.( 55 ) Genetic vulnerability is seen as the major reason why only a minority of very heavy drinkers develop liver problems. With respect to other potential effect modifiers, it seems that the drinking frequency modifies the risk for liver cirrhosis associated with a given total weekly alcohol intake with fewer drinking days being associated with lower risk supporting the notion of a ‘liver holiday’.( 56 – 58 ) A report from the Singapore Chinese Health Study( 59 ) showed that among daily drinkers, consumption of even one drink a day was associated with a RR = 2.72 (95% CI: 0.98–7.50) for liver cirrhosis in comparison to non-drinkers. In more recent years, patterns of drinking, especially binge drinking, were introduced as potentially important for the etiology and progression of liver cirrhosis.( 60 , 61 ) However, evidence is limited and inconclusive at this point.( 62 , 63 ) Future research should include standard measures on patterns of drinking, such as measures of irregular heavy drinking in addition to average volume of drinking and drinking frequency, to test hypotheses about such patterns, and to determine whether there is a positive effect of abstinence days.( 64 ) The consumption of mostly wine, as opposed to beer or liquor, has been shown to modify the risk for alcoholic liver cirrhosis in some studies;( 29 , 58 ) however, as the UK Million Women study showed,( 49 ) this may be explained by the consumption of alcohol with meals, which is more common in wine drinkers than consumers of other types of alcohol.
An investigation of Midspan cohorts( 65 ) in Scotland indicated that BMI modifies the effect of alcohol consumption on liver disease, with obese participants being more susceptible to the harms from alcohol consumption than participants with lower BMI. An analysis of the Million Women Study( 66 ) confirmed that BMI and alcohol consumption interact in development of liver cirrhosis, in particular at alcohol intake of more than 150 g/week and BMI above 30. Potential interaction with drinking patterns seem possible.( 62 ) The effect of smoking in relation to alcohol consumption on liver cirrhosis is not clear. Several studies have reported an effect independent of alcohol consumption( 21 , 67 ), and no clear effect.( 68 , 69 ) Meta-analyses of the association of coffee consumption and risk for liver disease consistently show a decreased risk.( 70 , 71 ) Potential interaction with alcohol consumption should be explored. Liver cirrhosis severity may also play a role. Another analysis from the series of case-control studies from Italy showed the risk increase from alcohol consumption was characterized by a threshold effect at approximately 150 g/day, and a smaller risk at higher consumption for asymptomatic liver cirrhosis than for symptomatic liver cirrhosis. In other reports including the same participants,( 69 , 72 ) it was shown that HBV and HCV infection were risk factors independent from alcohol consumption. The role of nutrient intake is unclear. Several nutrients were investigated in reports from the Italian case-control studies. Possible interaction effects were observed for dietary intake of lipids,( 73 ) vitamin A,( 74 ) and iron.( 74 ) However, larger sample sizes are required to detect an effect with sufficient power. More and higher quality epidemiological studies are needed to reach firm conclusions about confounding and interaction effects of these risk and protective factors in men and women.( 51 )
Other limitations of this review are based on the underlying literature. First, the number of original articles was limited. This is surprising given the fact that the majority of liver cirrhosis cases would not exist in a counterfactual scenario without alcohol. Second, the quality of the contributions was limited. Because of the small number of studies published, we were unable to investigate in detail the role of many study design characteristics, such as adjustment for potential confounders, follow-up length, race/ethnicity, and others that may play a role in the development of liver cirrhosis. Low response rates and inclusion criteria in primary studies, such as participants in screening programs, may limit the generalizability of our findings. Although self-reported alcohol consumption is generally reliable,( 75 ) it may result in underestimation of the real consumption. No cohort study measured alcohol consumption more than once, thus opening the research to measurement and regression dilution bias, and underestimation of the real effect.( 76 ) While the two case-control studies from Italy were able to assess lifetime drinking retrospectively, these types of studies are prone to recall bias, and categories of alcohol consumption were large, and adjustments for other risk factors for liver cirrhosis were minimal. Again, even with similar methodology in the same country, the two studies observed large differences in risk for liver cirrhosis for a given total alcohol intake. One possibility for the difference in risk observed between cohort and case-control studies is because of the difference in outcome assessment (mortality vs morbidity).
In comparison to our earlier meta-analysis,( 13 ) the strengths of this meta-analysis lie in its clear definition of the outcome, and its methodological rigour. For example, we excluded studies with insufficient number of cases or adjustment,( 77 ) and provide an examination of age, drinking patterns, and type of beverage where data were available. This strength came at a cost - some of the most well-known studies in the field, which were limited to subcategories of liver cirrhosis, had to be excluded.( 28 , 29 ), which was crucial to quantify the risk of liver cirrhosis in comparison to abstainers, which by definition cannot develop alcoholic liver cirrhosis.
What are the clinical conclusions of this study? The exponential dose-response curve on the relative risk level indicates that the highest levels of average volume of alcohol consumption confer exponentially higher risks and should be avoided.( 78 ) For people at the high end of this trajectory, the risk for liver cirrhosis is very high,( 16 ) and reductions of the highest levels are associated with the highest health gains.( 79 ) This can be achieved on the individual level in two ways: first, the trajectory towards these levels should be interrupted early, and more than once. This should best be done at the general practitioner level with screening and brief interventions or treatment;( 80 ) however, screening for unhealthy alcohol use is still not conducted routinely.( 81 , 82 )` Second, ( 79 )to prevent liver cirrhosis and subsequent complications including death in people with continued high consumption, it is most important to reduce high levels, even if the new drinking level are still high, and even if the patients still qualify for alcohol use disorders. Of course, the larger the reduction from a given level, the larger the reduction of relative risk, but it should be taken into consideration that any reduction of high volume drinking will be beneficial.( 83 ) Finally, there are alcohol control policy measures. Measures like increase in price via taxation( 84 ) or restrictions in availability have historically shown to impact on liver cirrhosis deaths.( 85 ) Thus, the current high impact of alcohol consumption on liver cirrhosis is avoidable, and both individual interventions in the health care sector and alcohol control policies can contribute to reduce this impact.
Study Highlights
What is the current knowledge.
- Alcohol is involved in all types of liver disease, and high alcohol consumption is associated with high disease risk.
- Prior systematic evidence syntheses have included inconsistent definitions of alcohol exposure and liver cirrhosis.
What is new here
- The risk for incidence of liver cirrhosis for former drinkers in comparison to long-term abstainers was three-fold.
- With any alcohol consumption, the risk for liver cirrhosis increased exponentially among women; among men, the risk increased beyond consumption of 1 drink or more per day.
- Drinking daily and outside of meals increases the risk for liver cirrhosis at any given level of overall alcohol intake. Several other risk factors for liver cirrhosis may modify the association of alcohol with liver cirrhosis, such as genetics, age, BMI, metabolic risk factors, and others.
Supplementary Material
Supplementary file, financial support.
Research reported in this publication was supported by the National Institute On Alcohol Abuse And Alcoholism (NIAAA) of the National Institutes of Health under Award Number R21AA023521 to MR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsor of the study (NIAAA) had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The authors collected the data, and had full access to all of the data in the study. The authors also had final responsibility for the decision to submit the study results for publication.
Declaration of interests
MR and JR report grants from National Institutes of Health (NIH), National Institute on Alcohol Abuse and Alcoholism (NIAAA), during the conduct of the study. JR reports grants and personal fees from Lundbeck and D&A Pharma outside of this work. AV, OSMH, BRC, MGN, RL, MC report no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Evidence-based clinical practice guidelines for Liver ...
1. Introduction. Cirrhosis is a major cause of morbimortality, constituting around 2.4% of global deaths ().The natural history of cirrhosis has a progressive and dynamic course transitioning from a relatively stable state of compensated cirrhosis to an advanced stage of decompensated cirrhosis ().Central to the dynamics of the transition is the degree of portal hypertension (PH) which serves ...
Diagnosis and Management of Cirrhosis and Its ...
Cirrhosis is widely prevalent worldwide and can be a consequence of different causes, such as obesity, non-alcoholic fatty liver disease, high alcohol consumption, hepatitis B or C infection, autoimmune diseases, cholestatic diseases, and iron or copper overload. Cirrhosis develops after a long period of inflammation that results in replacement of the healthy liver parenchyma with fibrotic ...
Liver cirrhosis - Latest research and news
Hepatic Cirrhosis - StatPearls
Treatment of Patients with Cirrhosis
In addition to the clinical questions (CQs), background questions (BQs) are new items for basic clinical knowledge, and future research questions (FRQs) are newly added clinically important items. Concerning the clinical treatment of liver cirrhosis, new findings have been reported over the past 5 years since the second edition.
Chemokines have an important role in liver diseases such as alcohol-associated liver disease, nonalcoholic fatty liver disease, cirrhosis and hepatocellular carcinoma. This Review describes the ...
Global epidemiology of cirrhosis — aetiology, trends and ...
Liver cirrhosis - PubMed ... Liver cirrhosis
MeSH terms. Liver cirrhosis is a frequent consequence of the long clinical course of all chronic liver diseases and is characterized by tissue fibrosis and the conversion of normal liver architecture into structurally abnormal nodules. Portal hypertension is the earliest and most important consequence of cirrho ….
However, liver transplant has been traditionally thought of as the only cure once cirrhosis develops. 7 But new research is exploring the reversibility of liver cirrhosis. 8,9 Because progression toward cirrhosis is slow, taking 2 to 3 decades, cirrhosis is most often diagnosed in patients' fourth or fifth decade of life.
Liver cirrhosis (LC) is a worldwide health problem that is associated with various complications and high mortality. Although, in the past four decades, the incidence of hepatitis B continuously decreased and a promising cure for hepatitis C was developed, LC remains a formidable challenge in clinical practice due to the ever-increasing incidences of alcoholic and non-alcoholic fatty liver ...
Cirrhosis is widely prevalent worldwide and can be a consequence of different causes, such as obesity, non-alcoholic fatty liver disease, high alcohol consumption, hepatitis B or C infection, autoimmune diseases, cholestatic diseases, and iron or copper overload. Cirrhosis develops after a long period of inflammation that results in replacement of the healthy liver parenchyma with fibrotic ...
Since there are several cases in which portal pressure gets worse after HCV eradication, the research on "point of no return" still remains a major issue in clinical practice. In addition to HCV, many new findings have been reported in the last 5 years regarding the treatment of hepatitis B liver cirrhosis with newly developed nucleic acid ...
INTRODUCTION. Liver cirrhosis is a common clinical chronic progressive disease with high mortality caused by one or more factors. It is the fifth leading cause of adult deaths, the top cause of liver-related death worldwide[], and the eighth of the primary diseases in economic cost[].Cirrhosis is a heterogeneous disease classified into two prognosis stages: compensated cirrhosis and ...
However, liver transplant has been traditionally thought of as the only cure once cirrhosis develops. 7 But new research is exploring the reversibility of liver cirrhosis. 8,9 Since progression toward cirrhosis is slow, taking 2 to 3 decades, cirrhosis is most often diagnosed in the fourth or fifth decade of life.
Cirrhosis transcends various progressive stages from compensation to decompensation driven by the severity of portal hypertension. The downstream effect of increasing portal hypertension severity ...
Cirrhosis: Diagnosis and Management
Introduction. Cirrhosis is defined as the histological development of regenerative nodules surrounded by fibrous bands in response to chronic liver injury, that leads to portal hypertension and end stage liver disease. Recent advances in the understanding of the natural history and pathophysiology of cirrhosis, and in treatment of its complications, resulting in improved management, quality of ...
Background and Objectives: Hepatic cirrhosis is a disease with an increasing frequency globally, but its mechanisms of disease development are not yet completely known. The aim of this study was to evaluate the relationship between thyroid hormone levels (T3, fT4, and TSH) and survival in patients with chronic liver disease. Materials and Methods: A total of 419 patients diagnosed with liver ...
Moreover, chronic hepatitis, toxins, or metabolic stress can lead to the development of fibrosis, cirrhosis, and chronic conditions like alcoholic steatohepatitis (ASH) and metabolic dysfunction ...
Liver cirrhosis is a serious, advancing condition in which normal tissue in the liver gets replaced by scar tissue, resulting in impaired liver function and complications. ... The treatment of liver cirrhosis has a bright future as long as research and surgical techniques advance. Recent advances can significantly enhance patient outcomes and ...
Dietary Approaches to Stop Hypertension (DASH) and mortality risk among patients with liver cirrhosis: a prospective cohort study BMC Res Notes. 2024 Sep 4 ... 6 Gastroenterology and Liver Diseases Research Center, Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Reversal of liver cirrhosis: current evidence and expectations
A few studies of people with fatty liver disease, viral hepatitis, and cirrhosis support these findings. Still, more research is needed to confirm if milk thistle affects your liver enough to ...
Alcohol consumption and risk of liver cirrhosis - NCBI