Insight: Indiana University Medical Student Research Journal
Current issue.

Respecting the Limits of Method
Opinion: sleep should be at the forefront of improving wellness in medical students, heart to heart: a journey in cardiovascular research interview with rohan dharmakumar, phd, arts and humanities, voting as a vital sign, blue collar, white coat, the american obsession with interventionism produces global health crises, hummingbird and more, feature: visual art, kathleen ho, feature: visual art, ritu gangadhara, feature: visual art, margaret tharp, feature: visual art, justin yu, feature: visual art, jeffery miller, indiana medical student program for research and scholarship award recipients, brain activation during scene encoding fmri in the alzheimer’s disease continuum: association with amyloid and tau burden in pet, enzyme assay development for hormonally up-regulated neu-associated kinase (hunk) protein: a target in egfr+ (her2+/erbb2+) breast cancers, clinical applications of next-generation sequencing for cancer diagnostics and targeted cancer therapy, decoding the link between xpc and lung cancer susceptibility: a study of cigarette smoke-induced dna damage in the setting of xpc deficiency, silencing coq8b in aortic smooth muscle cells reveals cellular dysfunction related to changes in cell proliferation, importance of per2 in cardiac mitochondrial function during stress, viability of transplanted de novo retinal ganglion cells in human donor eyes maintained under elevated intraocular pressure, investigating the effects of tirzepatide on nafld/nash progression using 3d human liver organoids, improvement in nocturia frequency after holmium laser enucleation of the prostate (holep), reduced endocochlear potential in vivo prevents hair cell degeneration in tmprss3- deficient mice, “there’s healing in music”: veteran perceptions of music interventions for their chronic musculoskeletal pain, indiana medical student program for research and scholarship abstracts, hrsa primary care reaffirmation for indiana medical education abstracts.
Insight: Medical Student Journal ISSN: 2639-1600


Medical Student Research Journals: The International Journal of Medical Students (IJMS) Legacy
- Kiera Liblik BSc. Faculty of Medicine, Queen’s University, Kingston, ON, Canada. Associate Editor, IJMS. https://orcid.org/0000-0003-1385-9298
- Patricio Garcia-Espinosa Social Service Medical Doctor. School of Medicine, Universidad Autónoma de Nuevo León, Monterrey, México and Mexican Institute of Social Security. Palliative Care Unit. High Specialty Medical Unit #25, Monterrey, México. Student Editor, IJMS. https://orcid.org/0000-0002-8139-806X
- Ahmed Nahian BS/DO Medical Student. California Baptist University-Lake Erie College of Osteopathic Medicine, Riverside, CA. United States. Student Editor, IJMS. https://orcid.org/0000-0001-7650-7877
- Surobhi Chatterjee MBBS, Intern Doctor. Department of Medicine, King George's Medical University, Lucknow, Uttar Pradesh, India. Student Editor, IJMS. https://orcid.org/0000-0003-1975-5107
- Mihnea-Alexandru Găman MD, PhD student. Faculty of Medicine, "Carol Davila" University of Medicine and Pharmacy, 050474 Bucharest, Romania & Department of Hematology, Center of Hematology and Bone Marrow Transplantation, Fundeni Clinical Institute, 022328 Bucharest, Romania. Scientific Editor, IJMS. https://orcid.org/0000-0001-7133-8875
- Ciara Egan Medical Student. Humanitas University, Humanitas Research Hospital, Milan, Italy. Deputy Editor, IJMS. https://orcid.org/0000-0001-6662-5167
- Juan C. Puyana MD, FRCSC, FACS, FACCP. School of Medicine, Department of Surgery, Professor of Surgery, Critical Care Medicine, and Clinical Translational Science, Director for Global Health-Surgery, University of Pittsburgh, Pittsburgh, PA, United States. Editorial Board Member, IJMS. https://orcid.org/0000-0003-4284-4693
- Francisco J Bonilla-Escobar MD, MSc, PhD(c). Researcher, Department of Ophthalmology; Institute for Clinical Research Education (ICRE), University of Pittsburgh, Pittsburgh, PA, United States. CEO, Fundación Somos Ciencia al Servicio de la Comunidad, Fundación SCISCO/Science to Serve the Community Foundation, SCISCO Foundation, Cali, Colombia. Grupo de investigación en Visión y Salud Ocular, VISOC, Universidad del Valle, Cali, Colombia. Editor in Chief, IJMS. https://orcid.org/0000-0002-0224-3482
The International Journal of Medical Students (IJMS) has emerged over the past decade as a critical platform for showcasing medical student innovation and experiences. Though the work of trainees has historically been undervalued and over scrutinized, the IJMS is committed to highlighting the immense capacity for novel and robust research in this cohort. Thus, supporting an upcoming generation of leaders in medicine and academia to gain confidence in their work and contribute positively to the scientific community. In this issue of the IJMS, we are proud to present 16 articles from the Americas, Europe, Asia, and Africa. Original research articles cover a breadth of topics, including medical training, impacts of the COVID-19 pandemic on teaching and communication, pediatric respiratory illness, gender equity in medicine, understudied illnesses, and cardiovascular disease. The IJMS is proud to feature first-hand experiences of medical trainees in each issue. Accordingly, in the present issue perspectives of six medical students are outlined following unique and career-altering experiences. From working in palliative care to international outreach program, local vaccination initiatives, and the creation of a student-oriented research and innovation council in India. The IJMs extends our gratitude to our contributors, team, and readers for another remarkable issue.
Bonilla-Escobar FJ, Kumar AA, Farrugia-Bonnici G, Ryan PM, G?man MA. A Grain of Sand in the Ocean: Training New Generations of Editors, Reviewers, and Medical Scientists. Int J Med Stud. 2020 Sep-Dec;8(3):213-6.
Bonilla-Velez J, Peña-Oscuvilca A, Sahin I, Córdoba-Grueso WS, Fernandez-Zapico ME. The International Journal of Medical Students, a Platform for Medical Student Research Worldwide. Int J Med Stud 2013;1(1):6-7.
Verdini N, LeClair J, Quinn E, El-Haddad A. Social Determinants of Health Amplify the Association Between Ethnicity and COVID19: A Retrospective-Cohort study. Int J Med Stud. 2021 Sep-Dec;9(4):282-287.
Abu-Zaid A. A graduate's perspective on medical student journals. J Postgrad Med. 2019 Jul-Sep;65(3):169-170.
Corrales-Reyes I, Fornaris-Cedeño Y. [Latin American scientific student journals: A space for publishing at the undergraduate level]. Educ Medica. 2018 Sep;20(2): 183-185. Spanish.
Al-Busaidi IS, Wells CI, Wilkinson TJ. Publication in a medical student journal predicts short- and long-term academic success: a matched-cohort study. BMC Med Educ. 2019 Jul 19;19(1):271.
Australian Medical Student Journal. History of the AMSJ. Available from: https://www.amsj.org/about/history . Last updated 2022. Cited Mar 23, 2022.
Nguyen, M. Why medical school is depressing and what we should be doing about it. Med Stud J Aust. 2011 March 29;2(1):65-8.
Cureus. The Florida Medical Student Research Publication. About. Available from: https://www.cureus.com/channels/fmsr/about . Last Updated 2022. Cited Mar 23, 2022.
The University of Toronto Medical Journal. About. Available from: https://jps.library.utoronto.ca/index.php/utmj/about . Last Updated 2022. Cited Mar 23, 2022.
Cape JD, Beca JM, Hoch JS. Introduction to cost-effectiveness analysis for clinicians. Univ Tor Med. 2013 March 31;90(3):103-105.
The International Journal of Medical Students. About. Available from: https://www.ijms.info/IJMS/about . Last Updated 2022. Cited Mar 23, 2022.
Rondilla NAO, Rocha ICN, Roque SJR, Lu RMS, Apolinar NLB, Solaiman-Balt AA, et al. Folk Medicine in the Philippines: A Phenomenological Study of Health-Seeking Individuals. Int J Med Stud. 2021 Jan-Apr;9(1):25-32.
Bawazeer NA, Alsobahi N. Prevalence and Side Effects of Energy Drink Consumption among Medical Students at Umm Al-Qura University, Saudi Arabia. Int J Med Stud. 2013;1(3):104-8.
American Medical Student Research Journal. About. Available from: https://www.amsrj.org/index.php?journal=amsrj&page=about&op=editorialPolicies#focusAndScope . Last Updated 2020. Cited Mar 23, 2022.
The Cooper Rowan Medical Journal. About Us. Available from: https://rdw.rowan.edu/crjcsm/about.html . Last Updated 2022. Cited Mar 23, 2022.
Ellis, J. The" M" Word: Accusations of Malingering are Harmful to Patient Care. Cooper Rowan Med J. 2019 May;1(1):33-36.
The New Zealand Medical Student Journal. About Us. Available from: https://www.nzmsj.com/about.html . Last Updated 2022. Cited Mar 23, 2022.
Al-Busaidi, I, Wells, C. Stimulating the clinical academics of tomorrow: a survey of research opportunities for medical students in New Zealand. NZ Med J. 2017 Nov;4(25): 80-88.
Dalhousie Medical Journal. About. Available from: https://ojs.library.dal.ca/DMJ/about . Last Updated 2022. Cited Mar 23, 2022.
The University of British Columbia Medical Journal. About. Available from: https://ubcmj.med.ubc.ca/about/ . Last Updated 2022. Cited Mar 23, 2022.
Corrales-Reyes, I, Fornaris-Cedeño, Y. [Ranking of Latin American scientific student journals according to the h5 index]. Edu Medica. May-June 2019; 20(S2):181-189.
Arman-Pereda D, Gallardo-Madrazo L, Naranjo-Dominguez A, Calzada M, Arman-Alessandrini G. [TYPE 2 DIABETES MELLITUS AND RISK SCORES]. 16 de Abril. 2015 Jan 13; 54 (258): 45-55. Spanish.
García-Rivero, A, González-Argote, J. [Cuban medical student journal in an actual context]. Rev Med Investig. 2017 Jan;5(1):94-98.
The Student’s Journal of Health Research Africa. About the Journal. Available from: http://www.sjhresearchafrica.org/index.php/public-html/about . Last Updated 2022. Cited Mar 23, 2022.
Corrales-Reyes, I, Dorta-Contreras, A. [Scientific production in Latin American student journals: comparative analysis of the period 2013-2016]. Edu Medica. May-June 2019; 20(3):146-154. Spanish.
Alamri Y. How do medical student journals fare? A global survey of journals run by medical students. Educ Health (Abingdon). 2016 May-Aug;29(2):136-41.
Recla, J. [One article, two articles, three articles... one hundred articles; Review of Medical Student Journals in Latin America.] Méd UIS. 2020 Dec;21(3):123-5. Spanish.
Laybourn-Langton L, Smith R. COP26 and Health: Some Progress, But Too Slow and Not Enough. The Health Community Must Step Up Its Efforts to Hold Countries Accountable for Reducing Greenhouse Emissions and Promoting Adaptation. Int J Med Stud. 2021 Oct-Dec;9(4):255-6.
Cox MJ, Shah PC, Komer L, Manan MR, Kutikuppala LVS, Liu B. A Call for Action–Empowering Medical Students to Facilitate Change. Int J Med Stud. 2021 July-Sep;9(3):187-8.
Atwoli L, Baqui AH, Benfield T, Bosurgi R, Godlee F, Hancocks S, et al. Call for Emergency Action to Limit Global Temperature Increases, Restore Biodiversity, and Protect Health. Wealthy Nations Must Do Much More, Much Faster. Int J Med Stud. 2021 Jul-Sep;9(3):189-91.
Srichawla BS, Khazeei Tabari MA, G?man M-A, Munoz-Valencia A, Bonilla-Escobar FJ. War on Ukraine: Impact on Ukrainian Medical Students. Int J Med Stud. 2022 Jan-Mar;10(1):15-17.
Montano, MA, Montano, SA, Harrison, JL, Kivisalu, TM. Reliability Generalization of the Medical Student Stressor Questionnaire. Int J Med Stud. 2022 Jan-Mar;10(1):25-31.
Canton SP, Foley CE, Fulcher I, Newcomb LK, Rindos N, Donnellan NM. Reliability and Discriminant Validity of a Checklist for Surgical Scrubbing, Gowning and Gloving. Int J Med Stud. 2022 Jan-Mar;10(1):18-24.
Johnson JW, Graham L, Williams E, Campbell C, Thomas N, Gossell-Williams M. Clinical Elective Choices and Motivations for Future Career Specialty Selection of Medical School Trainees and Junior Doctors of The University of the West Indies, Jamaica. Int J Med Stud. 2022 Jan-Mar;10(1):49-55.
Huang IA, Dhindsa Y, Chen AJ, Wu J, Wagner JP, Tillou A, et al. Medical Student Teleconferencing Experiences and Financial Status: A Cross-Sectional Survey. Int J Med Stud. 2022 Jan-Mar;10(1):56-62.
Thomas A, Shenoy MT, Kotacherry TS, Kumar SS, Sidheeque A, Khovidh C, et al. Teachers’ View on Online Classes during the COVID-19 Lockdown – A Cross-Sectional Study. Int J Med Stud. 2022 Jan-Mar;10(1):32-37.
Park S-H, Yozbatiran N. A Medical Student’s Perspective on the Growing Importance of Telemedicine/Telerehabilitation. Int J Med Stud. 2022 Jan-Mar;10(1):95-97.
Farley H, Bennett H, Rao S. Rationalizing the Pediatric Emergency Department Workload: An Epidemiological Profile of Presentations Before and During the COVID-19 Pandemic. Int J Med Stud. 2022 Jan-Mar;10(1):69-73.
Murerwa R, Gwala F, Amuti T, Muange M. Childhood effects of prenatal and postnatal exposure to mercurial skin lightening agents. Literature Review. Int J Med Stud. 2022 Jan-Mar;10(1):74-81.
Bonasia, KL, Morgan A, Solomon GC, Damiano EA. Assessing Medical Students’ Self-Perceived Preparedness to Care for Gender Diverse Patients: A Survey Study. Int J Med Stud. 2022 Jan-Mar;10(1):63-68.
Urs GM, R. Doddabele H. Dyke-Davidoff-Masson Syndrome: A Case Report. Int J Med Stud. 2022 Jan-Mar;10(1):82-85.
Cholack G, Garfein J, Krallman R, Feldeisen D, Montgomery D, Kline-Rogers E, et al. Predictors of Early (0-7 Days) and Late (8-30 Days) Readmission in a Cohort of Acute Coronary Syndrome Patients. Int J Med Stud. 2022 Jan-Mar;10(1):38-48.
García-Espinosa, P. Experience in a Palliative Care Unit in a Mexican Tertiary Level Hospital. Int J Med Stud. 2022 Jan-Mar;10(1):92-94.
Waisberg, E. Eye-Opening Medical Missions. Int J Med Stud. 2022 Jan-Mar;10(1):86-88.
Rocha ICN, Ramos KG, Solaiman-Balt AA, Cedeño TDD. Medical Interns as Volunteers in the COVID-19 Vaccination Drives in the Philippines. Int J Med Stud. 2022 Jan-Mar;10(1):89-91.
Patel BM, Humphrey V, James AJ. The Student Dermatology Clinic for the Underserved: A Service-Learning Model to Promote Skin Health Equity. Int J Med Stud. 2022 Jan-Mar;10(1):98-100.
Mulkalwar A. ASPIRE - A Journey from Intuition to Innovation. Int J Med Stud. 2022 Jan-Mar;10(1):101-103.
- 2022-04-12 (2)
- 2022-04-05 (1)
How to Cite
- Endnote/Zotero/Mendeley (RIS)

This work is licensed under a Creative Commons Attribution 4.0 International License .
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to [email protected]
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to [email protected]
Most read articles by the same author(s)
- Surobhi Chatterjee, The COVID-19 Pandemic Through the Lens of a Medical Student in India , International Journal of Medical Students: Vol. 8 No. 1 (2020)
- Bahadar Singh Srichawla, Mohammad Amin Khazeei Tabari, Mihnea-Alexandru Găman, Alejandro Muñoz-Valencia, Francisco J. Bonilla-Escobar, War on Ukraine: Impact on Ukrainian Medical Students , International Journal of Medical Students: Vol. 10 No. 1 (2022)
- Edgar Botello-Hernández, Patricio Garcia-Espinosa, Juan P. Ruiz-Padilla , Gabriela Torres-Hernández, Luis E. Fernandez-Garza , Medical Students’ Perception Towards the COVID-19 Pandemic in Mexico: Distance Learning, Assisting Hospitals, and Vaccination , International Journal of Medical Students: Vol. 9 No. 1 (2021)
- Adnan Mujanovic, Vincent Kipkorir, Cesare Mercalli, Arkadeep Dhali, Purva Shah, Camila Velandia, Ciara Egan, Mihnea-Alexandru Găman, Juan C. Puyana, Francisco J. Bonilla-Escobar, The IJMS World Conference of Medical Student Research and an Overview of the IJMS Volume 10 Issue 2 , International Journal of Medical Students: Vol. 10 No. 2 (2022)
- Francisco J. Bonilla-Escobar, Ciara Egan, Mihnea-Alexandru Găman, Is It Worth Publishing in a Medical Students’ Journal? Insights From a 10-Year Journey , International Journal of Medical Students: Vol. 9 No. 4 (2021)
- Mihnea-Alexandru Găman, Amelia Maria Găman, Pathophysiology, Diagnosis and Treatment of Immune Thrombocytopenia , International Journal of Medical Students: Vol. 5 No. 1 (2017)
- Kelly Rhea MacArthur, Madeleine J. Cox, Ciara Egan, Leah Komer, Pre-Existing Social Conditions: A Call to Prevent the Perpetuation of Gender Inequalities in Research Production during COVID-19 , International Journal of Medical Students: Vol. 8 No. 3 (2020)
- Muhammad Romail Manan, Kiera Liblik, Francisco J. Barrera, Ciara Egan, Juan C. Puyana, Francisco J. Bonilla-Escobar, Thinking Globally in the Pursuit of Individual Identity: Diversity, Equity, and Inclusion in the International Journal of Medical Students (IJMS) , International Journal of Medical Students: Vol. 10 No. 2 (2022)
- Genevieve Dable-Tupas, Victoria Toralba-Lupase, Juan C. Puyana, Mihnea-Alexandru Găman, Research Grant Proposal Writing Course for Students in Higher Institutions , International Journal of Medical Students: Vol. 10 No. 3 (2022)
- Madeleine J. Cox, Leah Komer, Ciara Egan, Purva C. Shah, Nikoleta Tellios, Annora A. Kumar, Back to the Future: Medicine Beyond the COVID-19 Pandemic , International Journal of Medical Students: Vol. 9 No. 1 (2021)
Similar Articles
- Bassam AlRajhi, Ibrahim Omer, Reema Abualnaja, Faisal Alqahtani, Alqassem Y. Hakami, Medical Students’ Attitudes and Influential Factors Towards Conducting Medical Research , International Journal of Medical Students: Vol. 11 No. 1 (2023)
- Juliana Bonilla-Velez, Mariah Small, Raul Urrutia, Gwen Lomberk, The Enduring Value of Research in Medical Education , International Journal of Medical Students: Vol. 5 No. 1 (2017)
- Khalid Osman Mohamed, Ahmed ALemam Ahmed, ElShimaa Ammar Zaki, Sozan Mudather Soumit, Wamda Ahmed Ali, Asmaa Mohamed Abbas, Prevalence of Generalized Anxiety Disorder and Associated Risk Factors Among Medical Students in Sudan: A Cross-Sectional Study at Omdurman Islamic University , International Journal of Medical Students: Vol. 12 No. 1 (2024)
- Alexandra C. Skoczek, Patrick W. Ruane, Cassidy Onley, Torhiana Haydel, Maria Valeria Ortega, H. Dean Sutphin, Alexis M. Stoner, Comparison of Multinational Medical School Students Experiences in the Face of the COVID-19 Pandemic: A Qualitative Analysis , International Journal of Medical Students: Vol. 10 No. 4 (2022)
- Jean Williams Johnson, Leohrandra Graham, Eric Williams, Colleen Campbell, Nidhi Thomas, Maxine Gossell-Williams , Clinical Elective Choices and Motivations for Future Career Specialty Selection of Medical School Trainees and Junior Doctors of the University of the West Indies, Jamaica , International Journal of Medical Students: Vol. 10 No. 1 (2022)
- Maison Evensen-Martinez, Mariangela Santiago, Roger Martinez, Dallin Beck, Ann Trawick, Isain Zapata, Mark Wardle, The Influence of Pre-Trip Medical Spanish Education on a US-Based, Medical Student Service Trip: A Cohort Study , International Journal of Medical Students: Vol. 12 No. 1 (2024)
- Lydia C. Brown, Imran Aziz, Prevalence and Burden of Disorders of Gut-Brain Interaction Among UK Medical Students , International Journal of Medical Students: Vol. 12 No. 1 (2024)
- Nida Gul, Ayaz Ali, Rizwanullah, Khayam, Manahil Saeed Khan, Faiza Gul, Aiysha Gul, Shehriyar, Kashif Ali, Syed Owais Haseeb, Prioritizing Mental Health: A Cross-Sectional Investigation of Depression Prevalence and Risk Factors among Medical Students in Peshawar, Pakistan , International Journal of Medical Students: Vol. 12 No. 1 (2024)
- Supreeth Nekkanti, Sagarika Manjunath, Arun Mahtani, Archana Meka, Tanushree Rao, A Survey Based Feedback Analysis of the Current Medical Teaching Methodology and Trends in Medical Research Practice in a South Indian Medical Institute , International Journal of Medical Students: Vol. 6 No. 1 (2018)
- Hamzah Shahid Rafiq, Erik Blair, Medical Students’ Study Habits Through a Sociocultural Lens: A Systematic Literature Review , International Journal of Medical Students: Vol. 12 No. 1 (2024)
1 2 3 4 5 6 7 8 9 10 > >>
You may also start an advanced similarity search for this article.
Make a Submission
Information.
- For Readers
- For Authors
- For Librarians
Current Issue
Announcements.
Only Two Days Left to Submit Your Abstracts for the IJMS World Conference of Medical Student Research (WCMSR)!
Dear Readers and Researchers,
7-days left: Abstract submission deadline for the 2024 World Conference of Medical Student Research

International Journal of Medical Students

About the Journal
The International Journal of Medical Students ( IJMS ) is an open-access, peer-reviewed scientific journal (ISSN 2076-6327 ) that publishes original research and experiences in all fields of medicine. The IJMS was created in 2009 to share scientific production and experiences where there is at least one author enrolled as a medical student (including MBBS students, MD students, DO students, MD/MSc students, and MD/PhD students) in any medical school in the world or a recently graduated physician. These early-career scientists must be accompanied by a senior researcher that must be also responsible for the research, guaranteeing the quality of the work. The IJMS aims to be the leading publication platform for early-career scientists' medical research. Read more in the About the Journal section .
Current Issue
- Volume 12; Issue 2
Credits & Content
Cover, credits, & content, transforming toxic research cultures: protecting the future of medical students and early career researchers – part i, original article, antibiotic use awareness and practices in the indian community during later stages of covid-19 pandemic: a cross-sectional survey, blindness disparities between racial/ethnic groups in the state of texas, a cross-sectional survey of instagram to assess quality and reliability of information regarding tuberculosis, determining the prevalence and severity of menopausal symptoms in post-menopausal women of eluru, andhra pradesh, india, using the menopause rating scale (mrs), learning of intimate area examination amongst pakistani medical students: knowledge, attitudes, and practices study, leveraging a podcast series for nutrition education in medical curriculum, skipping breakfast is associated with shorter sleep duration in medical students, exploring the impact of covid-19 on the healthcare system and vulnerable populations in the united states, the factors causing stress in medical students and their impact on academic outcomes: a narrative qualitative systematic review, case report, a case report of bardet biedl syndrome in a patient from pakistan who presented with osmotic symptoms associated with diabetes mellitus, disseminated tuberculosis with testes involvement: an intriguing case report, continuous rifampicin therapy induced acute kidney injury in a tuberculous patient: a case report, a medical student experience as an acting intern in colorectal surgery, conducting research as a medical student: a need for change, silent suffering: recognizing and addressing the emotional impact of patient loss on medical students.
If you are experiencing issues logging in, please delete the cache memory of your internet browser and try again.
Make a Submission
Information.
- For Readers
- For Authors
- For Librarians
Announcements
Only Two Days Left to Submit Your Abstracts for the IJMS World Conference of Medical Student Research (WCMSR)!
Dear Readers and Researchers,
7-days left: Abstract submission deadline for the 2024 World Conference of Medical Student Research

Search this website
Florida medical student research journal (fmsrj), mission statement.
FMSRJ is an initiative aimed at providing opportunities for Florida medical students to learn and participate in the peer review process. The FMSRJ is one of eighteen international medical student journals publishing original research, case studies, reviews, and editorials with the help of dedicated faculty advisors.
Editorial Policy
The Florida Medical Student Research Journal is a student-run, refereed journal designed to publish medical research of interest to Florida Medical Students and the greater medical community. The Journal accepts submissions from anyone conducting research in medicine, regardless of their position, field, or location. The Journal bases its policies on the guidelines set forth by the International Committee of Medical Journal Editors .
NOTICE: USF Health Libraries will be closed for the winter break Dec. 21st - Jan.1st, 2024.
- Give to USF Health
- Patient Care
- USF Libraries
- Sarasota-Manatee
Shimberg Health Sciences Library Florida Blue Health Knowledge Exchange
Shimberg health sciences library & florida blue health knowledge exchange, usf health libraries hours of operation, medicine research guide.
- Statistics Resources
- Consumer Health/Patient Education
- Citing Sources
- Journal Evaluation
- Organizing your Paper
- Finding a Journal
- Journal Influence (Impact Factor)
- ORCID & Other Digital Researcher IDs
- Student/Resident Journals
- Resident & Fellow Resources This link opens in a new window
- Biomedical Research
- Innovation, Entrepreneurship & Business in Medicine
- International Medicine
- Law & Medicine
- Medical Education
- Medical Humanities
- Nutritional Research & Health
- Medicine & Gender
- Public Health
FLAGSHIP: Medical Scholarly Proceedings
- FLAGSHIP: Medical Scholarly Proceedings A research journal supported by medical schools across Florida, including USF, to provide another option for peer-reviewed publication created by students, medical residents, and faculty.
Student Journals
This is just a sample of the journals that publish work by Medical Students.
- AMA- Where to publish: Top journals for physicians in training This resource contains links to the Submission Requirements for the linked databases and is the source of the descriptions. There is also additional guidance on publishing as a student.
- Harvard Medical Student Review The Harvard Medical Student Review is student-founded, student-managed and student-administered, under the guidance of faculty and staff. Its mission is to provide a platform for students to contribute to important issues facing health and medicine through a variety of formats, including scholarly articles, editorials and original artwork.
- Harvard Public Health Review This publication seeks diverse research interests that addresses issues of health equity and invites submissions from students and faculty across academic disciplines.
- International Journal of Medical Students The International Journal of Medical Students is a peer-reviewed, open-access scientific journal created to share the research and experiences of medical students worldwide.
- Student BMJ Launched in 1992, this international journal publishes articles that have been commissioned with medical students in mind.
- Medical Student Research Journal A journal authored, reviewed, edited, and published by medical students for medical students. It is dedicated to promoting the scientific achievements of medical students, teaching principles of peer and article review, and providing editorial, publishing and leadership learning experiences.
- Res Medica A peer-reviewed Journal of the Royal Medical Society. They accept articles written by medical students and clinicians covering clinically relevant topics.
Resident & Fellows Journals
This is just a sample of the journals that publish work by Residents & Fellows.
- American Journal of Psychiatry Residents' Journal The American Journal of Psychiatry, serves as a forum for psychiatry residents and fellows to share ideas and experiences in training, clinical practice, research, and careers with colleagues.
- Journal of Graduate Medical Education The Journal of Graduate Medical Education (JGME) disseminates scholarship and promotes critical inquiry to inform and engage the graduate medical education community to improve the quality of graduate medical education. It is a peer-reviewed, editorially independent journal published by the Accreditation Council for Graduate Medical Education.
- Postgraduate Medical Journal (BMJ) A peer-eviewed journal published by BMJ on behalf of the Fellowship of Postgraduate Medicine. PMJ publishes papers that focus on core competencies; describe current practice and new developments in all branches of medicine; describe relevance and impact of translational research on clinical practice; provide background relevant to examinations; as well as papers on medical education and medical education research.
Case Reports
- Case Report Journal List- Excel from Wayne State Complete list of medical journals dedicated to publishing case reports, sortable by medical specialty, author fee requirement, and whether the journal is listed in PubMed. Updated 4/25/2019.
- << Previous: ORCID & Other Digital Researcher IDs
- Next: Resident & Fellow Resources >>
- Last Updated: Jul 16, 2024 3:05 PM
- URL: https://libraries.health.usf.edu/medicine
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Postgrad Med
- v.65(3); Jul-Sep 2019
A graduate's perspective on medical student journals
College of Medicine, Alfaisal University, Riyadh - 11533, Saudi Arabia
Medical student journals (MSJs) refer to a cluster of entirely student-led periodicals that publish student-authored articles. A recent review showed that MSJs characteristically employ a student-friendly and feeble peer review process, which is largely associated with poor quality of published articles. Herein, as a graduate medical student, I call on peer medical students to make an informed decision in refraining from submitting their research work to MSJs for four primary reasons. These reasons, generally, include: 1) opaque peer-review process, 2) lack of MEDLINE® indexing, 3) absence of official journal impact factor scores, and 4) poor article visibility and exposure to scientific community. Furthermore, I encourage students to take advantage of the existing opportunities provided by the professional MEDLINE®-indexed journals in disseminating their research work. These opportunities include: 1) the absolute welcoming calls for student-authored contributions, and 2) the designated 'student contribution corners’. Lastly, I succinctly highlight the joint duties of medical schools, undergraduate research committees, institutional review boards and mentors in publishing the student-authored research work in the professional journals, rather than the MSJs.
Medical student journals (MSJs) refer to a cluster of entirely student-led periodicals that publish student-authored articles.[ 1 ] Their primary aim is to foster scientific research publishing among medical students. They provide a fitting platform for medical students to disseminate their scholarly research work.
Peer review is the practice of appraising manuscripts for quality, legitimacy, and ingenuity. Furthermore, it is the most fundamental vehicle to authenticate and uphold the veracity of the disseminated science.[ 2 ] To that end, the peer review process is always rigorous by the professional journals. Conversely, the “less”-professional MSJs characteristically employ a student-friendly and feeble peer review process, which is largely associated with poor quality of published articles.[ 1 ]
Recently, Al-Busaidi and Alamri adequately scrutinized the peer review practices and policies employed by various English-language peer-reviewed MSJs ( n = 23).[ 3 ] The authors concluded that the peer review process was not largely transparent. I second the authors’ conclusion.
Herein, as a graduate medical student, I call on peer medical students to make an informed decision in refraining from submitting their research work to MSJs for four primary reasons.
First, to date according to Al-Busaidi and Alamri,[ 3 ] the peer review process of MSJs are largely poor and opaque, and this may result in an unfavorable aftermath of disseminating bad and low-quality research.[ 1 ] Thus, medical students should not contribute their research, borne out of hard work, to low-quality MSJs.
Second, only one MSJ (that is, the Yale Journal of Biology and Medicine) is indexed in MEDLINE®—the most trustworthy bibliographic database compiled by the United States National Library of Medicine (NLM). MEDLINE®-indexed journals denote earning a badge of legitimacy in scientific publishing after a thorough examination of predefined critical elements, some of which are the “quality of content” and “quality of editorial work.”[ 3 ] Thus, medical students should strive to publish in professional MEDLINE®-indexed journals which carry higher added value, credit recognition, and scientific reputation than the non-MEDLINE®-indexed MSJs.
Third, none of the MSJs have an official journal impact factor (IF) reported by the Journal Citation Reports® (JCR). Although controversial, the journal IF remains one of the most common and valuable journal-level metrics to evaluate the “reputation” and “ranking” of journals.[ 4 ] Student-authored publications in professional MEDLINE®-indexed journals (with or without journal IF) are always encouraged, and yet possible even from third-world medical schools.[ 5 , 6 ]
Fourth, one of the central goals of conducting research is to disseminate knowledge, preferably through publication in journals, or presentation in scientific meetings.[ 7 ] Unfortunately, the scholarly scientific community is unlikely to be interested in spending time reading research articles published in the “far less professional” journals—the MSJs. Thus, publishing in MSJs is associated with far less visibility and exposure[ 1 ] and student-authors should wisely avoid this publishing pathway.
While all “professional” journals welcome research contributions from all authors including students and junior scholars,[ 1 ] a genuine question arises: why do students decide to publish their research work in MSJs rather than in the “professional” journals? One plausible reason is the challenge put forth by the meticulous scrutiny and critical appraisal (peer review) in professional peer-reviewed journals.[ 2 ] However, as opposed to fearing the comments of reviewers in such high caliber entities, medical students should adopt the demeanor of eminent scholars and develop persistence, confidence, and patience to achieve the highest possible goals in any scholarly driven activity.
Many professional and reputed journals, e.g., Journal of Postgraduate Medicine , encourage research submissions from undergraduate students and junior doctors. Moreover, Journal of Postgraduate Medicine has introduced years ago a “student-friendly contribution corner” to specifically solicit research submissions from young student scholars[ 8 ] and these submissions undergo the mandatory rigorous peer review.
Medical schools, through curricular and extracurricular schemes, play primary instrumental roles in educating students about the discipline of scientific publishing. The central bodies of Undergraduate Research Committees in medical schools should provide counseling to students to publish only in professional MEDLINE®-indexed journals. Furthermore, they should also highlight the academic perils of publishing in dubious journals. Senior medical students and research mentors should offer helping hands in recommending a handful list of suitable journals for the student-authored research work.
Conflicts of interest
There are no conflicts of interest.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis
Affiliations Faculty of Medicine, Cairo University, Cairo, Egypt, Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan
Affiliation Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan
Affiliation European Institute of Oncology (IEO), Milano, Italy
* E-mail: [email protected]
Affiliation National Cancer Institute, Cairo University, Cairo, Egypt
- Mohamed Amgad,
- Marco Man Kin Tsui,
- Sarah J. Liptrott,

- Published: June 18, 2015
- https://doi.org/10.1371/journal.pone.0127470
- Reader Comments
Despite the rapidly declining number of physician-investigators, there is no consistent structure within medical education so far for involving medical students in research.
To conduct an integrated mixed-methods systematic review and meta-analysis of published studies about medical students' participation in research, and to evaluate the evidence in order to guide policy decision-making regarding this issue.
Evidence Review
We followed the PRISMA statement guidelines during the preparation of this review and meta-analysis. We searched various databases as well as the bibliographies of the included studies between March 2012 and September 2013. We identified all relevant quantitative and qualitative studies assessing the effect of medical student participation in research, without restrictions regarding study design or publication date. Prespecified outcome-specific quality criteria were used to judge the admission of each quantitative outcome into the meta-analysis. Initial screening of titles and abstracts resulted in the retrieval of 256 articles for full-text assessment. Eventually, 79 articles were included in our study, including eight qualitative studies. An integrated approach was used to combine quantitative and qualitative studies into a single synthesis. Once all included studies were identified, a data-driven thematic analysis was performed.
Findings and Conclusions
Medical student participation in research is associated with improved short- and long- term scientific productivity, more informed career choices and improved knowledge about-, interest in- and attitudes towards research. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and/or their scientific productivity. Intercalated BSc degrees, mandatory graduation theses and curricular research components may help in standardizing research education during medical school.
Citation: Amgad M, Man Kin Tsui M, Liptrott SJ, Shash E (2015) Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis. PLoS ONE 10(6): e0127470. https://doi.org/10.1371/journal.pone.0127470
Academic Editor: Emmanuel Manalo, Kyoto University, JAPAN
Received: April 1, 2014; Accepted: April 15, 2015; Published: June 18, 2015
Copyright: © 2015 Amgad et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Data Availability: All data are included within the manuscript
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The education of health professionals has seen two revolutions over the past century. The first revolution-marked by what is known as The Flexner Report in 1910- was the effective integration of basic sciences into health education. The second revolution, initiated by the Welch-Rose report in 1915, introduced the concept of problem-based learning into medical education. In 2010, a special report was published by a global commission, The Commission on Education of Health Professionals for the 21 st Century, aimed at updating the standards of an ideal medical curriculum. The committee strongly recommended a new medical educational model that emphasized flexibility and adaptability of traditionally rigid curricula to local and community needs [ 1 ]. Despite these educational advances, there are certain aspects of medical education that remain unstructured and largely variant between medical schools; among these is medical student participation in research. Moreover, there is an alarming decline in the number of physician-scientists in the US, which threatens the progress of translational medicine in the upcoming era [ 2 – 4 ].
In the U.S., outstanding students willing to enter medical school may apply for the National Institute of Health (NIH) funded Medical Scientist Training Program (MSTP) [ 5 ]. This program offers students the opportunity to get a good feel for what a physician-scientist career entails through a funded MD/PhD. The value of those MD/PhD programs is well established; a 2010 study by Brass et al, investigating the outcomes of half of all NIH-funded MD/PhD programs (24 programs in total) found that these programs were very successful at reaching their goals of training future physician-scientists. In fact, 81% of MD/PhD graduates landed academic positions and 82% of them were actively engaged in research [ 6 ]. Nevertheless, due to limited funding, MD/PhD graduates only constitute 3% of the US medical student population, highlighting the value of alternative pipelines for the creation of research-active physicians [ 7 ]. Moreover, organizational and contextual factors might make the support of costly MD/PhD programs difficult to implement in other countries.
Several other programs have also been devised to offer medical and health sciences students the chance to participate in research [ 8 – 13 ]. One of the common forms of medical student research engagement is Intercalated Bachelor of Science (iBSc) degrees. These are particularly common in the UK, and are characterized by research time-out periods between the basic and clinical years of medical school. Students who take intercalated degrees graduate with an extra BSc beside their medical degree. The value of such short-term research placements should not be underestimated. In fact, the benefits of undergraduate research have been discussed richly in the literature, though there were relatively fewer papers focusing primarily on medical student research [ 14 – 16 ]. Unlike many other degrees, a medical degree is at the interface of science and social service. It is therefore expected that the benefits of, and motivations behind, medical student participation in research are different from those of non-medical students [ 17 ].
A 2005 systematic review of the literature by Straus et al investigated the factors that influence career choice in academic medicine among residents, fellows and staff physicians [ 18 ]. Their review found a positive effect of having dual degrees or fellowships beside the medical degree, and of publishing research conducted during medical school. Further, the review highlighted the role of mentorship and desire to teach. Despite the presence of a large body of evidence investigating the impact of, and factors related to, medical student research, a systematic analysis of this evidence is missing. This makes the data seem conflicting and disorganized, and undermines the apparent overall strength of evidence.
This paper is a mixed-methods systematic review and meta-analysis of published studies investigating various aspects of medical student research, including its impact on the development of research-active physicians, difficulties faced by medical students performing research and potential solutions to overcome these difficulties. Our hope is that this work serves to complement the review by Straus et al, and helps provide a thorough overview of the evidence needed for curricular and educational policy reforms [ 18 ].
We aimed to satisfy the following objectives in this review:
Primary Objectives: (a) To examine the short- and long- term influence of curricular and extracurricular undergraduate medical research on the scientific productivity of medical students, measured by the number of published manuscripts, research awards or attainment of faculty rank. (b) To describe the influence of curricular and extracurricular medical student research on the career choice of medical students.
Secondary Objectives: (a) To explore the current forms in which medical students are engaged in research projects, as well as the prevalence of non-mandatory research exposure among medical students. (b) To identify the factors related to medical student engagement in research projects. (c) To investigate miscellaneous issues of relevance, including the pros and cons of research time-out periods (with a focus on Intercalated Bachelor of Science degrees), differences between countries with developing and developed economies and gender equality in medical student research engagement, perceptions and productivity.
Developing economies were identified according to the International Monetary Fund's World Economic Outlook Report [ 19 ]. We counted as a "medical student" anyone who is enrolled in the core medical school program, regardless of program duration, and whose graduation would guarantee the degree Bachelor of Medicine, Bachelor of Surgery (MBBS) or its equivalent (MD, in the US, for example). It should be noted that in the US model of medical education, admission into medical school is on a graduate-entry basis by default, and the first medical degree earned is called the "MD". In the non-graduate entry model, on the on the other hand, the term "MD" is reserved for higher research degrees (postgraduate degrees) in clinical medical and surgical disciplines. Graduate-entry medical students were included, but not MD/PhD students, residents or postgraduate students. The reasons behind excluding studies focusing on MD/PhD students is that this sub-population is considered to be different from the general student population, especially that their enrollment in the medical program was–by definition- meant to prepare them for physician-scientist careers. It may be argued that graduate-entry medical students who had a higher degree (MSc or PhD) at the time of matriculation also constitute a separate sub-population. Hence, we addressed any reported differences between these sub-populations in our results. "Medical student research" was defined as any activity performed by medical students that is driven by inquiry or hypothesis and that legitimately incorporates basic principles of the scientific method. This includes original research, review articles, case reports etc.
We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statement guidelines in this systematic review and meta-analysis, and the relevant checklist can be found as S1 File [ 20 ]. Between March 2012 and September 2013, periodic searches were performed in the following databases for potentially relevant studies: MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews, Cochrane Methodology Register (CMR), Educational Resources Information Center (ERIC), Center for Reviews and Dissemination (CRD), ISI Web of Science and Google Scholar. Further, we searched the bibliographies of the included studies for other potential publications on the subject. Our search strategy included the following keywords in various combinations: medical student; medical students; undergraduate; medical; research; intercalated; bachelor; BSc; iBSc; theses; thesis; developing. The search strategy used for PubMed was as follows: ((((((medical student research) OR undergraduate research) OR medical thesis) OR intercalated bachelor) OR intercalated BSc) OR iBSc) OR undergraduate research developing.
Inclusion criteria: All study designs, including cross-sectional, prospective, retrospective and interventional studies, randomized controlled trials and qualitative studies.
Exclusion criteria: Studies containing inadequate information about the participants and type of study; studies in languages other than English; studies assessing outcomes unrelated to medical student research; theses or commentaries; studies aimed at postgraduates or undergraduates other than medical students; studies whose main population was MD/PhD students. Graduate-entry medical students, nonetheless, were not excluded from this review.
Two of the authors independently reviewed the studies that met these criteria and any disagreements were resolved by consensus. Basic data extraction tables were then used to extract the main finding and characteristics of each of the included studies. Quantitative studies (reporting odds ratios (OR's), p-values, percentages or other statistical measures) were separated from qualitative studies in order to improve the judgment of cumulative evidence.
Qualitative studies were included in order to help contextualize the quantitative outcomes and to provide insights and entry points for future research. Qualitative studies were defined as those studies which satisfied the following criteria: a) Their aims did not include the extraction of quantitative outcomes and thus did not perform any statistical analysis; b) They present original research with clearly-defined study populations; c) They utilize qualitative research methods, including semi-structured and unstructured interviews, open-ended survey questions, focus groups and examination of records and documents.
An integrated methodology was utilized to assimilate quantitative and qualitative outcomes into a single mixed-methods synthesis [ 21 , 22 ]. After relevant studies have been identified, a thematic analysis was performed. The literature search and article inclusion/exclusion strategy was aimed at retrieving all articles relevant to the subject of medical students' research, without prior conceptions or theories about expected outcomes. Hence, our thematic analysis was data-driven (as opposed to being theory-driven) [ 22 ]. Quantitative and qualitative outcomes were discussed together under relevant thematic subject headings.
Two types of quantitative outcomes were used for meta-analysis: percentages (for explorative outcomes) and odds ratios (for interventional/associative outcomes). Whenever relevant or needed, the corresponding authors (or, if unavailable, other authors) of included studies were contacted to get the raw data needed for meta-analysis. In some cases, other outcomes beside the ones mentioned in the original paper were identified in the raw data and used for the meta-analysis.
Further details about the methodology used in this paper, including outcome-specific quality assessment, statistical methods used and the strategy used to tackle study heterogeneity and potential publication bias can be found in our supporting information ( S2 File ).
Results and Discussion
Our search returned 31,367 records in the various databases. After reviewing the abstracts, 31,111 were excluded because they were either duplicates in various databases or satisfied one or more of the exclusion criteria mentioned earlier. 256 articles met (or were suspected to meet) our inclusion criteria upon reviewing their abstract and were thus retrieved for full-text assessment. Eventually 79 articles were found to match the selection criteria and were included in this review. More details about the article selection process can be seen in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0127470.g001
Of the 79 articles retrieved, 71 were of quantitative nature, seven were of qualitative nature and one had both quantitative and qualitative components. Fifty-two articles were self-reported questionnaire studies with response rates ranging from 7.9% to 100%. Ten survey-based articles had response rates less than 60%. Twenty-three studies used a more objective research strategy that relied on searching institutional databases and records, two used both questionnaires and objective database searching and two had an unknown/undisclosed methodology. There were 47 cross-sectional studies, 25 retrospective studies, three prospective studies, three intervention studies and one study with an unknown/undisclosed design. Fifty-seven studies were performed in a single institution (including four qualitative study) and 22 studies involved multiple institutions (including four qualitative studies). Further, there were 14 studies that reported the effects of certain research programs or initiatives, whose study population might or might not be affiliated with multiple institutions. Sixteen studies assessed the value of intercalated BSc's (iBSc's) and 14 studies were carried out in developing countries.
After thematic analysis was performed, the resultant themes and sub-themes, outlined in Fig 2 , also served as the scaffold for writing this paper. The data extraction and quality assessment worksheet and the relevant sensitivity plots can also be found in the supporting information files ( S3 and S4 Files , respectively) [ 7 , 8 , 10 , 11 , 23 – 90 ].
https://doi.org/10.1371/journal.pone.0127470.g002
Assessing the current situation
We assessed the current state of medical student research by focusing on two main outcome measures: interest in- and exposure- to research among the medical student population. Both of these outcomes are explorative in nature (rely on proportions rather than odds ratios) and have been quantitatively pooled to yield a weighed estimate value. The results have been summarized in Fig 3 [ 7 , 10 , 26 , 28 , 32 , 47 – 49 , 52 , 54 , 55 , 58 , 63 , 67 – 69 , 71 – 75 , 80 – 82 , 85 , 90 – 92 ] .
Forest Plot symbols: * The axis, not the data, is shown in logit scale for aesthetic purposes. Table symbols: * Mandatory exposure (in the form of curricular components or graduation theses) was excluded from this analysis. Abbreviations used: D, developing countries; H, higher commitment to a research career; I, intercalated Bachelor of Science degree (iBSc). Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names.
https://doi.org/10.1371/journal.pone.0127470.g003
Interest in research among medical students.
While the only reliable method for probing interest in medical research is assessing actual voluntary research involvement, survey data (self-reported interest) may provide insights into any discrepancies between interest and actual involvement. To avoid pooling survey data that are too heterogeneous, we made a distinction between survey questions that ask about general interest in research and those specifically asking medical students about their interest in making commitments to research during their future careers.
I1a: Interest in performing research: A pooled weighed estimate of 72% of medical students reported having interest in performing research (0.72, 0.57–0.83). One particularly high estimate was that reported by De Olivera and colleagues, which showed that 90% of its 1004 student sample had interest in performing research [ 74 ]. However, even when this study was excluded from the analysis as a possible exception, the pooled weighed estimate remained fairly high (0.67, 0.53–0.79) ( S4 File ).
I1b: Interest in a career involving research: The single best estimator of career intentions of US medical graduates is probably the Graduation Questionnaire (GQ), developed by The Association of American Medical Colleges (AAMC) in 1978 [ 7 ]. In 2013, 63% of the 13,180 respondents indicated intentions to become somewhat-to-exclusively involved in research during their medical careers, including 17% who planned "significant" or "exclusive" future involvement. This huge sample size approaches a true census, with 81.8% of the US fresh medical graduate population being covered.
Upon quantitative pooling of our included studies, we found that about 31% of medical students (0.31, 0.19–0.46) were interested in a career involving research, and 12% (0.12, 0.07–0.21) showed interest in "significant" (higher) commitment to research during their future careers. One particularly important, high-quality study was that of McManus and colleagues, showing that 6.9% of UK medical students planned to pursue academic careers (or found them to be very appealing) [ 85 ]. When we calculated the pooled outcome excluding MacManus et al or the AAMC data, the pooled proportion was not markedly changed ( S4 File ).
It should be noted that there is considerable variation in the proportions reported in our included studies. This may reflect inherent (true) variability in students' research interests due to diversity of settings and study populations (as has been discussed in S2 File ). We also believe that there are other potential contributors to this variability, most notably the ambiguity of wording of survey questions. For example, many studies did not make a clear distinction between interest in an academic (university faculty) medicine career, and interest in a career involving some research outside of academia.
I2. Medical students’ exposure to research.
Even today there is no consistent way in which undergraduate medical students are incorporated into research. For example, students may be engaged in research through summer research electives [ 9 , 45 ], mandatory curricular study modules [ 90 ], extracurricular research activities [ 93 ], or they might decide to intercalate for one or more years to obtain a BSc beside their medical degree. In Germany, it is mandatory for medical students to submit a thesis outlining the results of a research project in order to graduate with the title "Doctor" [ 30 ]. This requirement has also been reported in Peru, Finland, France and some U.S. universities such as Yale [ 24 , 27 , 76 , 94 ]. The AAMC 2013 Graduation Questionnaire shows that 68.2% of US medical graduates participated in a research project with a faculty member on a mandatory or volunteer basis and 41.7% co-authored a research paper [ 7 ].
If we exclude papers describing medical schools asking for mandatory graduation theses or research modules, we find that a little less than one third of medical students participated in research projects (0.31, 0.22–0.41). The proportion exposed to “prolonged” periods of research (>6 weeks) is even less (0.22, 0.16–0.28).
In the U.S., different medical schools have different research expectations, and the exposure of medical students to non-mandatory research seems to be largely dependent on medical school influence. Duke University, for example, incorporates students into summer-long research projects [ 95 ]. On the other hand, Stanford University, the University of Pittsburg and Warren Alpert Medical Schools incorporate students into longitudinal research projects in parallel with their academic studies [ 95 – 97 ]. This longitudinal approach may help in solving some of the reported problems of time-out research, such as the reluctance of medical students towards detachment from their colleagues and financial worries about spending extra time in college. Indeed, the success of Stanford is particularly evident, with 90% of medical students participating in research projects [ 91 ].
We found that the pooled proportion of medical students reporting some interest in research is higher than that of students who were actually involved in research projects. This may be due to: a) self-reported interest may not necessarily reflect serious willingness to pursue research; or b) lack of opportunities to meet students’ interest due to lack of funding, supervision and encouragement or inflexible curricula that leave little or no time for research ( S5 File ) [ 45 , 47 – 50 , 52 , 55 , 57 , 68 , 74 ].
II. Factors related to- or affecting medical student research
We identified four main factors affecting medical student research: previous research experience, academic success, having a higher degree (MSc or PhD) at the time of matriculation and financial factors. The effects of the first three factors were reported using odds ratios due to the presence of untreated groups ( Fig 4 ) [ 32 , 47 , 52 – 55 , 58 , 62 , 63 , 67 , 79 , 81 , 92 , 98 ], while the fourth factor (financial influence) was pooled using proportions from survey studies ( Fig 5 ) [ 55 , 57 , 59 , 67 , 82 ]. Moreover, we discuss the results of various studies reporting other relevant factors that could not be meta-analyzed, including the role of mentorship and competitive residencies in shaping medical students’ perceptions about- and attitudes towards research.
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Abbreviations used: D , developing countries; I , intercalated Bachelor of Science degree (iBSc); M , motivation to perform research; K , research knowledge or skills; C , confidence in research competencies; In , interest in research. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g004
https://doi.org/10.1371/journal.pone.0127470.g005
II1. Effect of previous research experience.
Students who participated in research projects during medical school were over three times as likely to report interest in research involvement during their future careers (OR = 3.55, 1.84–6.83). Two studies [ 92 , 98 ], which were not included in the pooled weighed estimate, reported paired outcomes, with non-significant differences in research career interests after research exposure. Additionally, we found that medical school research involvement has no significant correlation with attitudes or motivation towards research (OR = 2.05, 0.99–4.24).
It is difficult to conclude that self-reported interest is a direct effect of exposure to research, since reverse causality cannot be excluded. That is, it is logical to assume that a fairly large proportion of students who had pre-existing interest in a career in research decide to participate in research projects. As a matter of fact, students in two of the included studies agreed that research participation strengthened pre-existing interest in a research career [ 90 , 91 ]. These findings also make sense in light of the fact that over half of all medical students reported having some interest in a career involving research ( Fig 3 ). Another possible explanation for the above results is that students who have had prior research experience have better research knowledge and skills, and are therefore more confident about their ability to succeed were they to undertake research projects during their future careers. Indeed, in a series of interviews conducted by Jones et al, students who undertook an intercalated BSc in primary healthcare reported a positive influence of the experience on their appreciation of the research process [ 99 ]. Similarly, a thematic analysis of 905 SSC (Student Selected Component) projects by Murdoch-Eaton et al provided by medical students at six UK medical schools revealed gain of various research-related skills [ 90 ]. These results are also supported by eleven quantitative studies, summarized in S5 File [ 11 , 37 , 39 , 40 , 46 , 47 , 55 , 64 , 82 , 89 , 91 ].
II2. Effect of having a higher degree (MSc or PhD) prior to medical school.
II2a: Having a higher degree is associated with involvement in- (or planned involvement in-) research: Siemens et al report that medical students who had a higher degree prior to enrolment in medical school were almost four times more likely to perform research during medical school (OR = 3.95, 2.22–7.01) [ 52 ]. However, data provided by Cruser et al showed no significant difference between the two groups regarding their planned involvement in future research (OR = 1.01, 0.57–1.79) and Gerrard et al actually reported the reverse trend, with higher degree graduate-entry medical students actually being less likely to pursue an iBSc [ 54 , 81 ]. This is consistent with data we obtained from Mahesan et al, which shows that graduate-entry medical students (having any degree prior to matriculation) were almost ten times less likely to pursue an intercalated degree (OR = 0.01, 0.00–0.13) [ 62 ].
Since career progress (especially the pursuit of competitive residency) is a major motive behind medical student research, it may be argued that medical students with a higher degree view this aspect of their Curriculum Vitae (CV) as being “complete enough” and hence devalue the pursuit of another degree. In fact, to the medical student with a prior degree, an iBSc will almost always result in degree duplication, even if the skills and knowledge base of the iBSc course were completely different from those of the other degree already gained by the student.
II2b: Other advantages of having a higher degree (MSc. or PhD.): There is no significant correlation between having a higher degree prior to medical school enrolment and research interest or motivation. However, as might be expected, higher degree graduate-entry medical students were more knowledgeable about research, showed better research skills and had higher confidence in their research competencies ( Fig 4 ). This is expected, given that almost all higher degrees have a compulsory research component.
II3. Effect of academic success.
II3a: Academic success is associated with attitudes towards basic medical sciences or medical research: The data we obtained from Hren et al shows an association between higher Grade Point Average (GPA) and attitudes towards research (OR = 1.83, 1.42–2.36) [ 79 ]. Cruser et al’s data, on the other hand, shows no significant difference between highest MCAT (Medical College Admission Test) scores and attitude scores [ 54 ]. Perhaps GPA during medical school, but not before admission, is a factor that influences attitudes. However, we believe the evidence in favor or against this hypothesis is weak and further investigation is needed in the future.
II3b: Academic success is associated with involvement in- (or planned involvement in-) research: The weighed pooled odds ratio from four included studies shows no association between academic success and involvement (or planned involvement) in research projects (OR = 1.00, 0.62–1.64). The only study showing a significant correlation was Brancati et al, which asserts that students who were academically successful (top third of their class) were more likely to choose an academic career (OR = 2.11, 1.30–3.42) compared to their less successful peers (lower third) [ 32 ]. However, this study investigates choice of an academic career rather than involvement (or planned involvement) in research during or right after medical school. Hence, it may be argued that this study should be excluded from the analysis as it measures a different outcome, in which case the pooled odds ratio remains non-significant (0.82, 0.59–1.15). We suggest further investigation into this issue using studies with more favorable, preferably prospective, designs.
II4. Financial factors affect the appeal of research to medical students.
About half of medical students who chose not to get involved in research reported being deterred by financial factors (0.50, 0.46–0.54) ( Fig 5 ) [ 55 , 57 , 59 , 67 , 82 ]. Nicholson et al and Stubbs et al both show that about half of medical students who choose not to intercalate do so for financial reasons [ 59 , 82 ]. In addition, Galletly et al also reported that about half (48%) of medical students asserted that perceived lower salaries of academicians was an important factor behind their decision not to pursue an academic career [ 55 ]. The consistency of the findings by the former two studies with the latter one suggests that it's not just the short-term financial burden of pursuing an intercalated degree that deters medical students from getting involved in research, but a general long-term financial concern. Financial worries, particularly the fear of running out of grant money and the financial stress of academic careers, were indeed cited by students interviewed by O'Sullivan et al among the deterrents to academic career pursuit [ 100 ].
Similarly, Yamazaki et al and Kumar et al both showed that a considerable fraction of the general medical student population displayed concerns about the financial stability of a research career (45% and 12%, respectively) [ 57 , 67 ].
II5. Career progression is a main motive behind performing research during medical school.
The result from seven included studies indicate that career progression is a main motive (if not the main motive) behind performing research during medical school. These results indicate that in a large fraction of cases, medical students perform research for purely pragmatic reasons (related to their residencies or further post-graduate education), rather than pursuing research for the value it has in and of itself ( Table 1 ) [ 48 , 49 , 52 , 54 , 55 , 82 , 86 ].
https://doi.org/10.1371/journal.pone.0127470.t001
Four studies mentioned the role competitive residencies play in driving medical students to perform research, and in fact students in three of those studies believed that seeking competitive residency was–explicitly- the main motive to perform research during medical school. The results from a qualitative study by Shapiro et al support this conclusion by showing that the motives behind research participation include (but are not limited to) pragmatic targets such as improving the students' relationship with faculty [ 101 ].
These conclusions are consistent with other results reported here showing that: a) there is a discrepancy between interest in clinical practice and interest in a research career ( S5 File ) [ 45 , 51 , 56 , 57 ] and b) there is a correlation between interest in academia or basic medical sciences and interest in research ( S5 File ) [ 55 – 57 ].
Combined, these findings indicate that any policies aimed at boosting medical students’ engagement in research have to align research involvement with the career progress and success of students. In much the same way that peer-reviewed publications are a key competitive edge in academia and in competitive residency applications, it must become clear that research is more than just an accessory when it comes to ordinary clinical practice.
II6. Other factors related- to or affecting medical student research.
As Reynolds has discussed, it is simply not enough to match students with professors in research projects, as good quality research requires real mentorship [ 102 ]. Research instructors also act as role models to encourage students to pursue careers in academic medicine. Further, finding the right mentor is important to ensure that students provide a working and intellectual input into the research projects, rather than simple assistantship in lab work or data collection ( Table 2 ) [ 48 , 52 , 57 , 58 , 82 ].
https://doi.org/10.1371/journal.pone.0127470.t002
This is not always going to be easy; the results from two qualitative studies show that the complexity of ethical approval procedures (whether in terms of time or paperwork) is a major difficulty facing supervisors and students alike [ 90 , 103 ]. Further, the absence of clear, well-structured research governance may result in some aversion to faculty-mentored student research. This was the case in two qualitative studies, where students cited problems with approachability of faculty members and expressed concerns about being used as "free labor" on research projects [ 90 , 101 ].
In fact, Murdoch-Eaton et al's aforementioned project content analysis, while revealing some gain in useful research skills, also highlighted the failed attainment of a balanced skill-set; the majority of student projects involved information gathering and data processing, while fewer projects involved actual student engagement in research methodology development or critical analysis of data [ 90 ].
It may be presumed that the relatively short duration of the undergraduate research experience could limit its publication or citation potential. Indeed, Dyrbye et al found that graduates with a 17–18 week-long research experience published significantly less papers in which they appeared as first authors than their peers who spent 21-weeks doing research [ 29 ]. Further, Fede et al showed that the annual Undergraduate Medical Congress of ABC foundation (COMUABC) had a smaller proportion of abstracts accepted for publication in peer-reviewed journals in comparison to conferences of practicing physicians [ 70 ]. Conversely, Van Eyk et al. reported that the average number of citations of Dutch medical student publications was actually higher than the average citations for papers in the same field. [ 41 ]
A number of studies investigated factors that prevent medical students from being involved in research. Poor mentorship, lack of role models and perceived lower salaries of academic physicians were among the key factors cited ( S5 File ) . The previous findings were also supported by four qualitative studies ( Table 3 ) [ 17 , 45 , 90 , 99 – 101 , 103 , 104 ] .
https://doi.org/10.1371/journal.pone.0127470.t003
In addition, institutional influence as well as the type and length of available research opportunities were found to be relevant factors in determining whether students choose to engage in research [ 51 , 53 ]. McLean and co-authors provided an excellent set of tips to bolster the involvement of students in academic medicine projects and potentially overcome some the aforementioned limitations [ 105 ].
. The importance of psycho-cognitive factors in determining medical students' motivation towards- and engagement in- research was also highlighted in the qualitative literature. One of the most important motives behind performing research is curiosity. Not only is curiosity a main motive behind pursuing research while in medical school (as has been shown by Shapiro et al [ 101 ]), it is one of the very early psycho-cognitive predictors of persistence into scientific or research disciplines even before enrolment into medical school [ 17 , 104 ]. Conversely, perceived lack of competence may deter medical students from pursuing research-active careers [ 45 ].
III) Assessing the impact and effect of medical student research
We assessed three main outcomes that reflect the short- and long- term impact of medical student research: 1) the proportion of research performed during medical school that culminates in a peer-reviewed journal publication, 2) the effect of medical school research on the career choice and future research involvement of medical students, and 3) the effect of medical student research on long- term success in academia. The first outcome has been summarized in Fig 6 [ 10 , 24 , 25 , 27 , 29 – 31 , 37 , 38 , 41 , 49 , 64 , 75 , 76 , 93 , 106 ] and the latter two are shown in Fig 7 [ 8 , 25 , 26 , 31 , 43 , 44 , 66 , 68 , 81 , 83 , 85 , 90 ].
Since the duration of research exposure will almost always affect the publication outcome, it has been shown too. Forest Plot symbols: * The axis, not the data, is shown in logit scale for aesthetic purposes. Table symbols: * The duration is probably prolonged (possibly months long); ** 20–40 European medical school credits; || For published projects, the average duration was 18 months. D , developing countries; I , intercalated Bachelor of Science degree (iBSc); HQ , relatively high quality publication (indexed in Medline, Scopus or Medic), HF , first-author publication in a relatively high quality journal. Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names.
https://doi.org/10.1371/journal.pone.0127470.g006
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Table symbols: * at least one first-author publication; ** at least one citation; || more than 20 citations. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g007
III1. Medical student research results in a publishable product.
Peer-reviewed journal publications are generally considered to be the best indicator of research productivity, and it may be viewed as a major metric (though not the only one) of the “return on investment” in supporting and funding medical student research. An average of 30% (0.30, 0.19–0.44) of research performed by medical students resulted in a peer-reviewed journal publication. When only higher quality publications were included in the analysis (indexed in Medline, Scopus or Medic), the proportion remained more or less the same (0.31, 0.18–0.47). Subgroup analysis of studies investigating the research productivity of graduation theses revealed that 26% (0.26, 0.10–0.52) of graduation theses result in higher quality publications.
As expected, all studies reporting first -authored peer-reviewed publication by medical students described instances of prolonged research exposure. An average of 13% (0.13, 0.06–0.27) of medical student research resulted in a first-authored peer-reviewed publication. The pooled outcome remained the same when only higher quality publications (Medline-, Scopus- or Medic- indexed) were included in the analysis (0.13, 0.05–0.30).
A few initiatives, aimed at propping up medical student publication output, have gained popularity over the last few years. Those initiatives include a number of student-run journals and journal spaces dedicated solely for medical student research publications [ 107 – 110 ]. A subset of these journals is Medline-indexed and some even involve undergraduates in the peer-review process. Similarly, the Yale Journal of Biology and Medicine annually publishes Yale's student thesis abstracts [ 111 ]. These initiatives, we suppose, will help in promoting student participation in research and comfort students about publication issues. To our knowledge, there is no systematic investigation in the literature so far regarding the quality of research published in medical student research journals in comparison to field-specific journals. Hence, we would like to take a conservative stance whenever we see such hierarchical "segmentation" of the scientific enterprise; the stringency of research assessment, in our opinion, should be indiscriminant to the identity of the study authors.
It is important to note that the failure of publication of medical student research may be reflective of other factors beside the success and relative contribution of the student. For example, Weber et al showed that 55% of the papers submitted to a medical specialty conference did not reach the stage of publication five years later [ 112 ]. Similarly, Riveros et al found that half of the clinical trials reporting results in ClinicalTrials.gov had no corresponding journal publication [ 113 ]. Keeping this in mind, the results by Cursiefen et al should not be surprising; showing that medical students were among the authors of 28% of the papers produced by a German medical faculty, even though only 66% of medical student research resulted in a publication [ 30 ].
III2. Research during medical school is associated with later involvement in research projects.
Students who took part in research projects during medical school were more likely to get involved in (or report planned involvement in-) research later in their careers (OR = 3.58, 1.82–7.04). When a subgroup analysis was performed to include only studies that explicitly refer to academic careers (as opposed to brief research encounters), students who performed research during medical school were over six times as likely to pursue academic careers (OR = 6.42, 1.37–29.98) than their “untreated” peers.
With one exception, none of the included studies had a prospective design; hence reverse causality cannot be excluded, and is in fact very likely (students planning academic medicine careers choosing to get involved in research during medical school). Indeed, the only prospective study included (McManus et al [ 85 ]) showed that at the time of application to medical school, students who later chose to take an intercalated degree were already significantly more likely to report definite or highly likely choice of academic medicine careers (OR = 1.37, 1.13–1.66). Just before graduation, however, this likelihood had a substantial increase (OR = 3.45, 2.27–5.24). Together, these results indicate that medical school research strengthens pre-existing interest in an academic career.
A qualitative study by O'sullivan et al emphasized the value of early research exposure in giving medical students the opportunity to entertain the thought of pursuing academic careers [ 114 ]. Such exposure, they concluded, may sometimes even discourage students from pursuing academia, but is necessary nonetheless given the lack of sufficient free time during post-graduation residency to experience research.
III3. Research during medical school is associated with long-term success in academia.
Three studies showed that physicians who performed research during medical school were more likely to attain faculty rank long after graduation [ 8 , 32 , 66 ]. While this has implications on the decision of individual medical students to pursue research, we argue that it has little bearing on policy decision-making, since faculty positions are awarded on a competitive basis. Indeed, Brancati et al showed that this effect was dependent on the publication status of research performed during medical school [ 32 ]. In other words, students who did not publish their research were not significantly more likely to attain higher faculty rank on the long run. Hence, the fact that medical student research is associated with higher likelihood of attaining faculty positions has little implications regarding the systematic incorporation of research into medical curricula.
Students who performed research during medical school were more than twice as likely to author at least one peer-reviewed publication later in their career (OR = 2.31, 1.88–2.83). This remained true after the exclusion of Chusid et al [ 25 ] (which correlates successful publication of graduation theses with long-term publication success) from the analysis (OR = 2.26, 1.83–2.77). They were also twice as likely to acquire first-authorship (OR = 2.21, 1.56–3.13). The total number of publications and ability to secure grants, too, was reported to be significantly higher among students with medical school research experience [ 81 ]. Evered et al, on the other hand, found no significant difference in either of those measures between both groups [ 66 ]. Moreover, students who performed research during medical school were more likely to be cited at least once [ 66 ], had a higher total citation count [ 81 ], were more likely to be cited more than 20 times [ 66 ], and had higher odds of receiving awards [ 8 , 81 ] later in their careers.
While this data provides strong evidence of a correlation between medical school research and long-term success in academia, a causal relationship cannot be established since students who decide to perform research may already have a keen interest in research. Nonetheless, a causal relationship is quite likely since early research experience (especially if it culminates in a first-authored publication) would naturally enhance the career prospects and significantly improve the CV’s of early career medical graduates. Overall, we believe that the long-term impact of medical school research is inadequately assessed, and that further evidence is needed using prospective study designs with proper adjustment for baseline status.
III4. Research during medical school is correlated with career choice of- (or interest in a career in-) the same or related specialty as the research project.
Three of the studies that met the broad inclusion criteria reported results from control or “untreated” groups. Other studies reported results only from treated groups and hence were excluded from the analysis. Overall, students are 2.7 times as likely to be interested in careers in the same (or related) clinical specialty as the research project they got involved in during medical school. As with many other conclusions in this review, a causal relationship cannot be determined from this apparent correlation. This is especially true in the case of competitive residencies (and is particularly relevant to US residencies), where research experience in the same specialty gives recent graduates a competitive edge over their peers without such experience.
The relationship between medical school research and clinical practice was also touched upon in two of the included qualitative studies. Shapiro et al showed that many faculty members mentored student research in family practice in order to attract students to the same specialty [ 101 ]. Indeed, students interviewed by Jones et al believed an iBSc in primary healthcare provided them with deeper insights into patient care and a more thorough understanding of evidence-based clinical practice [ 99 ].
IV) Miscellaneous topics related to medical student research
In the following section of this review we discuss a number of miscellaneous topics relevant to medical student research. Three of these topics were discussed in light of quantitative data, and are summarized in Fig 8 [ 28 , 29 , 47 – 49 , 53 , 54 , 58 , 59 , 62 , 63 , 67 , 71 , 79 , 81 , 83 , 88 , 89 , 92 ] and Fig 9 [ 24 , 27 , 33 , 37 , 38 , 50 , 64 , 70 ]. Though they did not pass our inclusion criteria, four of the citations screened were personal perspectives provided by medical students, and are worth mentioning for enriching the discussion. They discussed the importance of the research experience on their medical career [ 115 , 116 ], the importance of medical students' research in increasing national research output [ 117 ] and the relevance of lab research involving animals to appreciation of human anatomy and physiology [ 118 ].
Forest Plot symbols: * The axis, not the data, is shown in log scale for aesthetic purposes. Abbreviations used: D, developing countries; I, intercalated Bachelor of Science degree (iBSc); FC , studies measuring final year academic performance and controlling for baseline performance. Dates are shown beside studies that may be confused with others referenced in this review having the same similar first-author names. For some studies, odds ratios and 95% confidence interval values were reported, but not the raw numbers.
https://doi.org/10.1371/journal.pone.0127470.g008
https://doi.org/10.1371/journal.pone.0127470.g009
IV1. Effect of prolonged research time-off on subsequent academic performance.
One of the issues discussed in the literature is the effect of prolonged research time-off amid the medical program on subsequent clinical knowledge. This question has been assessed in the context of iBSc degrees in a recent review [ 119 ]. All but one of our included studies investigated the effect of taking an intercalated degree on subsequent academic performance. The results have been conflicting; two studies that either matched groups by previous performance or adjusted for pre-clinical scores found no evidence of improvement in scores [ 88 , 120 ]. All five other studies that met our inclusion criteria reported an improvement in academic performance.
Due to heterogeneity in academic assessment methods and high possibility of confounding, we only pooled the studies for which we could extract odds ratio values that: a) measure final year academic scores and b) control for previous academic performance. Three studies met these two inclusion criteria, all of which reported the effect of iBSc degrees. On average, students who took some time off to perform research were twice as likely to outperform their peers (OR = 1.99, 1.39–2.84), even after adjustment for previous academic performance. It is noteworthy that all pooled studies investigated research time-off that was around one year in duration (iBSc), and that the positive effect of research time-off on subsequent academic performance may actually be reversed if the research delays are prolonged. Dyrbye et al pinned down a critical period of three years, after which medical students start to lose clinical knowledge and skills by the time they return to the core medical program [ 28 ].
IV2. Gender equality in medical student research.
There is no apparent gender difference regarding the following outcomes: Interest in a career in research ; involvement in research during medical school ; attitudes towards research ; interest in- or motivation towards- performing research ; research knowledge or skills. However, on average, males seem to be significantly more likely to publish (or submit for publication) the research they performed during medical school (OR = 1.59, 1.26–2.01). The reasons behind this gender gap in publication are unclear to us, and have been inadequately researched. Since there is no apparent gender difference in research perceptions, attitudes, motivations or knowledge, we suspect that the gender difference in publications is due to factors unrelated to research such as the overall academic environment or psychosocial factors. Indeed, these findings are consistent with a 2006 study by Jagsi et al showing a generalized gender gap in the authorship of academic medical articles in six major medical journals. Whatever the reasons behind gender differences in publication, they underlie a general issue not specific to medical school research [ 121 ].
IV3. Type and field of research performed by medical students.
The majority of medical student research is original in nature (as opposed to literature reviews). We were interested in finding out what percentage of these research projects were in the basic sciences, since this issue is of particular relevance to translational research. We found that the proportion was highly variable between different studies. In four of the five included studies less than half of medical student research was lab-based basic research, and the pooled weighted estimate was 0.32, 0.14–0.49. Given the relevance of research to competitive residency applications, it should not come as a surprise that lab-based projects do not constitute the majority of medical student research. Nonetheless, these results indicate that efforts directed at increasing the number of physician scientists involved in translational research should not only be directed at bolstering research involvement, but also improving the appeal of basic lab-based research to medical students.
IV4. Compulsory vs. elective medical school research.
The question of whether undergraduate medical research should be made compulsory or elective has been discussed in the literature, and is a matter of debate [ 37 , 97 , 122 ]. Arguments in favor of mandatory incorporation revolve around the ever-increasing importance of evidence-based clinical practice, while arguments against it revolve around the importance of focusing on clinical skills education. Diez et al. recommended against Germany's dissertation requirement, due to the steady decline in the number of successful dissertations [ 123 ]. Our results tell a similar story; the fraction of graduation theses resulting in a first-authored higher quality publication was smaller than the overall average (0.07, 0.03–0.14). At first, this may seem counterintuitive, as one may predict that the systematic incorporation of research as a necessary graduation requirement would raise the fraction culminating in a first-authored higher quality publication. However, one needs to bear in mind that since graduation theses are an obligatory requirement, a fraction of those students performing research may not be interested at all in what they are doing. Taking this into consideration, it should not come as a surprise that percentages as high as 34% (Cohen et al [ 38 ]) and 31% (Dyrbye et al [ 29 ]) of voluntary medical student research were reported to result in first-authored Medline-indexed publications. Weihrauch et al and Pabst et al, on the other hand, reported favorable results in terms of the personal and professional value of the German dissertation requirement [ 124 , 125 ].
IV5. The situation in countries with developing economies.
We retrieved studies that were performed in India [ 67 , 72 ], Uganda [ 68 ], China [ 69 ], Brazil [ 70 , 74 ], UAE [ 71 ], Croatia [ 73 , 79 ], Pakistan [ 75 , 77 , 80 , 86 ], Peru [ 76 ], and Turkey [ 78 ].
The number of medical schools and the research budget in developing countries are alarmingly mismatched with their needs [ 1 ]. This disparity, we believe, reflects naturally on the status of medical student research. In fact, medical student research might be even more important in developing countries than in developed countries, due to the pressing need to adapt international standards to local community needs.
Medical students in developing countries arguably face a set of extra challenges and are influenced by a number of different factors in comparison to developed countries [ 126 ]. For example, the high student-to-teacher ratio makes it increasingly difficult for medical students to have mentors and role models. Even research based on statistical analysis of patient records is often difficult to perform in many medical schools, due to suboptimal Information and Communications Technology (ICT) infrastructure in hospitals and in teaching premises in countries with developing economies [ 127 ]. While excellent research may of course be performed in resource-poor countries, it is preferable that any reform in research funding is coupled with a well-developed educational and managerial infrastructure; otherwise the research output may be largely suboptimal [ 128 ]. Worryingly, an essay by Silva et al. reported a decrease in the ratio of Undergraduate Student Research Assistant Programs (USRA's) to the number of undergraduates in Brazil over the past years [ 129 ].
Students’ interest in research was higher in countries with developing economies than in developed countries (0.82, 0.67–0.91 vs. 0.47, 0.26–0.69). One possible explanation for this finding is that the lack of opportunities causes higher eagerness to perform research. Another, possibly more likely, explanation is higher career-related anxiety in lower-income settings, with a resultant boost in research interest. Indeed, students in developing countries were not significantly less exposed to research, a result which may be reflective of the higher interest rates, bolstering research engagement despite inadequacies in resources. These results are supported by the findings of Baig et al, showing that 40% of Pakistani medical students viewed research as a tool to secure competitive residencies in the US [ 86 ].
Conclusions and Future Directions
Overall, our review shows that there’s considerable variability in medical student research exposure, engagement and productivity among different medical schools. A large proportion of the medical student population is interested in research, but is deterred by practical difficulties, including the lack of opportunities and funding. The benefits of research exposure on the short- and long-term scientific productivity is well documented in the literature, and a clear correlation is identified between medical school research engagement and later engagement in research projects (including the choice of an academic career). However, the number of well-controlled, high-quality prospective studies on the topic is limited and it is difficult to exclude reverse-causality. Existing evidence suggests that medical school research does have a positive effect on the choice of an academic career, but it does so through strengthening pre-existing interest. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and their scientific productivity.
Another potential limitation of this review is publication bias. It is conceivable that medical schools where students had a positive experience with research rush to publish their results, whereas others with experiences that were not so positive blamed it on the design of the program without publishing their results. It is also clear that there are plenty of successful undergraduate research programs that do not publish their results.
We suggest that more studies are done to assess the different structural and managerial aspects of standardized undergraduate medical research, as well as the differences between compulsory research components, elective research components, intercalated BSc's and extracurricular research in terms of academic, professional and psycho-cognitive effects. Further, we recommend more investigation into the quality and citation potential of published medical student research in comparison to that of established researchers and physicians.
Supporting Information
S1 file. prisma guidelines checklist..
https://doi.org/10.1371/journal.pone.0127470.s001
S2 File. Supplementary methodology file.
https://doi.org/10.1371/journal.pone.0127470.s002
S3 File. Quality assessment and quantitative data extraction sheet.
Abbreviations used: D, developing countries; I, intercalated Bachelor of Science degree (iBSc); X, Cross-sectional; R, Retrospective; I , Interventional; Pro , Prospective; Q, questionnaire; DS , database search; IN, interview.
https://doi.org/10.1371/journal.pone.0127470.s003
S4 File. Sensitivity plots for the pooled effect size values calculated.
https://doi.org/10.1371/journal.pone.0127470.s004
S5 File. Supplementary tables accompanying the main text.
https://doi.org/10.1371/journal.pone.0127470.s005
Acknowledgments
We would like to acknowledge with gratitude the following authors (and their co-authors) for sending us raw numbers to be used in our meta-analysis: Dr Nishanthan Mahesan, Dr des Anges Cruser, Dr Louise Burgoyne, Dr Neel Halder, Dr Cherrie Galletly, Dr Tracy Air, Dr Anna Chur-Hansen, Dr Craig Ziegler, Dr Ruth B. Greenberg, Dr Darko Hren, Dr Robert Siemens and Dr Matko Marusic.
Author Contributions
Conceived and designed the experiments: MA MMKT SJL ES. Performed the experiments: MA MMKT ES. Analyzed the data: MA MMKT SJL ES. Contributed reagents/materials/analysis tools: MA MMKT SJL ES. Wrote the paper: MA MMKT SJL ES.
- View Article
- PubMed/NCBI
- Google Scholar
- 5. National Institute of General Medical Sciences: Medical Scientist Training Program [Internet]. Available: http://www.nigms.nih.gov/Training/InstPredoc/PredocOverview-MSTP.htm . Accessed 14 April 2015.
- 7. Association of American Medical Colleges. Medical School Graduation Questionnaire—2013 all school summary report [Internet]. Available: https://www.aamc.org/download/350998/data/2013gqallschoolssummaryreport.pdf . Accessed 14 April 2015.
- 19. International Monetary Fund. World Economic Outlook Database [Internet]. 2013. Available: http://www.imf.org/external/pubs/ft/weo/2013/01/weodata/index.aspx . Accessed 14 April 2015.
- 22. Dixon-woods M, Agarwal S, Young B, Jones D, Sutton A. Integrative approaches to qualitative and quantitative evidence. Health Development Agency; 2004. Available: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.96.8783&rep=rep1&type=pdf . Accessed 14 April 2015.
- 107. Journal of Young Investigators [Internet]. Available: http://www.jyi.org/site/ . Accessed 14 April 2015.
- 108. Internationl Medical Journal of Students’ Research [Internet]. Available: http://www.imjsr.org/ . Accessed 14 April 2015.
- 109. McGill Journal of Medicine [Internet]. Available: http://www.med.mcgill.ca/mjm/ . Accessed 14 April 2015.
- 110. American Journal of Undergraduate Research [Internet]. Available: http://www.ajur.uni.edu/index.html . Accessed 14 April 2015.
- Renew Materials
- Pay a Library Fee
- Solutions Hub
- DMU Homepage
- Course Reserves
- Collections A-Z
- How to Find Materials
- Board Review Study Materials
- Bones and Anatomical Models
- Student Checkout Policy
- Pay A Library Fee
- Recommend A Resource
- Apply for a Student Job
- Research Appointment
- Paper Writing and Citation Help
- Information Literacy Program
- Checkout Policy
- Library Liaisons
- Faculty Services Guide
- Textbook Adoption Form
- Request an Instruction Session
- Interlibrary Loan (ILL)
- Search Library FAQs
- Library Guides (LibGuides)
- DMU Historical Archives
- Public Access & Scanning
- Citation Tools
- Coming Soon! Institutional Repository
- Library Consult Reference Service
- About the Library
- Library Mission & Vision
- Library Hours
- Library Location
- Library Staff
- Circulation Policies
- Donation Guidelines
- Ask Us for Help
- Help Finding Resources
- Access to Resources On & Off Campus
- Library Tutorials
- Public Access Computer/Visitor Guide
Find Journals To Publish Your Research: Student Friendly Publishing Options
- Locate Respected Journals
- "Best Match" Services
- Student Friendly Publishing Options
Student Focused Journals
Did you write a case report? DMU can help you get published. See our guide to BMJ Case reports to learn more about this fantastic option!
- BMJ Case Reports
For students interested in getting published, there are a few places that are friendly for student primary authors.
Read more about medical student journals:
- Abu-Zaid A. A graduate's perspective on medical student journals . J Postgrad Med. 2019 Jul-Sep;65(3):169-170. doi: 10.4103/jpgm.JPGM_278_19. PMID: 31267987; PMCID: PMC6659430.
- Abu-Zaid A. Reply to article "Where do medical student authors submit their work?" . Educ Health (Abingdon). 2020 Jan-Apr;33(1):24-25. doi: 10.4103/efh.EfH_189_19. PMID: 32859877.
- Alamri Y. How do medical student journals fare? A global survey of journals run by medical students. Educ Health (Abingdon). 2016 May-Aug;29(2):136-41. doi: 10.4103/1357-6283.188756. PubMed PMID: 27549653.
- Wan JC, McMurran CE, Teo AE. Student-run medical journals: Supporting the future of medical academia. Med Teach. 2016 Oct;38(10):1072. Epub 2016 Aug 30. PubMed PMID: 27573163.
- << Previous: "Best Match" Services
- Last Updated: Aug 11, 2024 1:42 PM
- URL: https://lib.dmu.edu/su/getpublished

Medical Student Research Journal
The Medical Student Research Journal (MSRJ) is a research journal authored, reviewed, edited and published by medical students, for medical students. It is currently the longest running, active medical-student run research journal in the United States. MSRJ is dedicated to promoting scientific achievements of medical students, teaching principles of peer review, and providing editorial, publishing and leadership experiences. Medical students worldwide are invited to submit manuscripts and/or to serve as trained reviewers. The MSRJ publishes original research, case reports, editorials, brief reports, reviews and reflections that meet required standards, are authored by a medical student and advance science. The MSRJ is sponsored by the Michigan State University College of Human Medicine (CHM)
If you are interested in becoming a member of MSRJ as a reviewer, or as part of the journal operations staff, please see our home page ( www.MSRJ.org ). If you are interested in submitting an article to MSRJ.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis
Affiliations.
- 1 Faculty of Medicine, Cairo University, Cairo, Egypt; Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan.
- 2 Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan.
- 3 European Institute of Oncology (IEO), Milano, Italy.
- 4 National Cancer Institute, Cairo University, Cairo, Egypt.
- PMID: 26086391
- PMCID: PMC4472353
- DOI: 10.1371/journal.pone.0127470
Importance: Despite the rapidly declining number of physician-investigators, there is no consistent structure within medical education so far for involving medical students in research.
Objective: To conduct an integrated mixed-methods systematic review and meta-analysis of published studies about medical students' participation in research, and to evaluate the evidence in order to guide policy decision-making regarding this issue.
Evidence review: We followed the PRISMA statement guidelines during the preparation of this review and meta-analysis. We searched various databases as well as the bibliographies of the included studies between March 2012 and September 2013. We identified all relevant quantitative and qualitative studies assessing the effect of medical student participation in research, without restrictions regarding study design or publication date. Prespecified outcome-specific quality criteria were used to judge the admission of each quantitative outcome into the meta-analysis. Initial screening of titles and abstracts resulted in the retrieval of 256 articles for full-text assessment. Eventually, 79 articles were included in our study, including eight qualitative studies. An integrated approach was used to combine quantitative and qualitative studies into a single synthesis. Once all included studies were identified, a data-driven thematic analysis was performed.
Findings and conclusions: Medical student participation in research is associated with improved short- and long- term scientific productivity, more informed career choices and improved knowledge about-, interest in- and attitudes towards research. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and/or their scientific productivity. Intercalated BSc degrees, mandatory graduation theses and curricular research components may help in standardizing research education during medical school.
PubMed Disclaimer
Conflict of interest statement
Competing Interests: The authors have declared that no competing interests exist.
Fig 1. Flow diagram of the citation…
Fig 1. Flow diagram of the citation screening and article selection process followed in this…
Fig 2. Themes and sub-themes resulting from…
Fig 2. Themes and sub-themes resulting from the thematic analysis of included quantitative and qualitative…
Fig 3. Assessing the current situation: Interest…
Fig 3. Assessing the current situation: Interest in- and exposure- to research among medical students.
Fig 4. Factors related to- or affecting…
Fig 4. Factors related to- or affecting medical student research (i)–Effects of previous research experience,…
Fig 5. Factors related to- or affecting…
Fig 5. Factors related to- or affecting medical student research (ii)–The effect of financial factors…
Fig 6. The proportion of medical student…
Fig 6. The proportion of medical student research resulting in a peer-reviewed journal publication.
Fig 7. The impact of medical student…
Fig 7. The impact of medical student research–Impact of medical student research on career choice…
Fig 8. Miscellaneous topics related to medical…
Fig 8. Miscellaneous topics related to medical student research.
Fig 9. Characterizing the research performed by…
Fig 9. Characterizing the research performed by medical students.

Similar articles
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Impact of summer programmes on the outcomes of disadvantaged or 'at risk' young people: A systematic review. Muir D, Orlando C, Newton B. Muir D, et al. Campbell Syst Rev. 2024 Jun 13;20(2):e1406. doi: 10.1002/cl2.1406. eCollection 2024 Jun. Campbell Syst Rev. 2024. PMID: 38873396 Free PMC article. Review.
- Beyond the black stump: rapid reviews of health research issues affecting regional, rural and remote Australia. Osborne SR, Alston LV, Bolton KA, Whelan J, Reeve E, Wong Shee A, Browne J, Walker T, Versace VL, Allender S, Nichols M, Backholer K, Goodwin N, Lewis S, Dalton H, Prael G, Curtin M, Brooks R, Verdon S, Crockett J, Hodgins G, Walsh S, Lyle DM, Thompson SC, Browne LJ, Knight S, Pit SW, Jones M, Gillam MH, Leach MJ, Gonzalez-Chica DA, Muyambi K, Eshetie T, Tran K, May E, Lieschke G, Parker V, Smith A, Hayes C, Dunlop AJ, Rajappa H, White R, Oakley P, Holliday S. Osborne SR, et al. Med J Aust. 2020 Dec;213 Suppl 11:S3-S32.e1. doi: 10.5694/mja2.50881. Med J Aust. 2020. PMID: 33314144
- Recovery schools for improving behavioral and academic outcomes among students in recovery from substance use disorders: a systematic review. Hennessy EA, Tanner-Smith EE, Finch AJ, Sathe N, Kugley S. Hennessy EA, et al. Campbell Syst Rev. 2018 Oct 4;14(1):1-86. doi: 10.4073/csr.2018.9. eCollection 2018. Campbell Syst Rev. 2018. PMID: 37131375 Free PMC article.
- Impact of an intercalated BSc on medical student performance and careers: a BEME systematic review: BEME Guide No. 28. Jones M, Hutt P, Eastwood S, Singh S. Jones M, et al. Med Teach. 2013 Oct;35(10):e1493-510. doi: 10.3109/0142159X.2013.806983. Epub 2013 Aug 20. Med Teach. 2013. PMID: 23962229 Review.
- The impact of a curriculum-based research training program on medical students' research productivity and future research interests: a longitudinal study. Shen J, Qi H, Liu G, Li X, Fang Y. Shen J, et al. BMC Med Educ. 2024 Aug 2;24(1):836. doi: 10.1186/s12909-024-05841-0. BMC Med Educ. 2024. PMID: 39095809 Free PMC article.
- Scientific competence during medical education - insights from a cross-sectional study at a German Medical School. Vogt M, Schuchardt N, Geissler ME, Bereuter JP, Geissler RB, Glauche I, Gerdes S, Deußen A, Günther L. Vogt M, et al. BMC Med Educ. 2024 May 28;24(1):590. doi: 10.1186/s12909-024-05470-7. BMC Med Educ. 2024. PMID: 38807084 Free PMC article.
- Knowledge, Attitudes, and Barriers Toward Research Among Medical Students: A Cross-sectional Study in Turkey. Mokresh ME, Muvaffak E, Kahya M, Torun P; Collaborators. Mokresh ME, et al. Med Sci Educ. 2024 Feb 13;34(2):387-395. doi: 10.1007/s40670-024-01987-0. eCollection 2024 Apr. Med Sci Educ. 2024. PMID: 38686156
- Publication Fate of Research Works Achieved During Master's Degree in Surgical Science in a French Survey. Dhote A, Puygrenier P, Tranchart H, Penna C, Fuks D, Gaillard M. Dhote A, et al. Med Sci Educ. 2024 Jan 19;34(2):363-370. doi: 10.1007/s40670-023-01973-y. eCollection 2024 Apr. Med Sci Educ. 2024. PMID: 38686154
- Do Not Throw Away Your Shot: Pilot Study in Improving Medical School Curricula Through Focused Vaccine Education. Sojati J, Murali A, Rapsinski G, Williams JV. Sojati J, et al. AJPM Focus. 2023 Dec 23;3(2):100178. doi: 10.1016/j.focus.2023.100178. eCollection 2024 Apr. AJPM Focus. 2023. PMID: 38312525 Free PMC article.
- Frenk J, Chen L, Bhutta Z, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–58. 10.1016/S0140-6736(10)61854-5 - DOI - PubMed
- Guelich JM, Singer BH, Castro MC, Rosenberg LE. A gender gap in the next generation of physician-scientists: medical student interest and participation in research. J Investig Med. 2002;50(6):412–8. - PubMed
- Rosenberg LE. Physician-Scientists—Endangered and Essential. Science. 1999;283(5400):331–2. - PubMed
- Mirmira RG. The vulnerable physician-scientist. Mol Endocrinol. 2014;28(5):603–6. 10.1210/me.2014-1085 - DOI - PMC - PubMed
- National Institute of General Medical Sciences: Medical Scientist Training Program [Internet]. Available: http://www.nigms.nih.gov/Training/InstPredoc/PredocOverview-MSTP.htm . Accessed 14 April 2015.
Publication types
- Search in MeSH
Related information
Grants and funding, linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central
- Public Library of Science
Other Literature Sources
- scite Smart Citations

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 30 August 2024
Medical students in distress: a mixed methods approach to understanding the impact of debt on well-being
- Adrienne Yang 1 na1 ,
- Simone Langness 2 na1 ,
- Lara Chehab 1 na1 ,
- Nikhil Rajapuram 3 ,
- Li Zhang 4 &
- Amanda Sammann 1
BMC Medical Education volume 24 , Article number: 947 ( 2024 ) Cite this article
Metrics details
Nearly three in four U.S. medical students graduate with debt in six-figure dollar amounts which impairs students emotionally and academically and impacts their career choices and lives long after graduation. Schools have yet to develop systems-level solutions to address the impact of debt on students’ well-being. The objectives of this study were to identify students at highest risk for debt-related stress, define the impact on medical students’ well-being, and to identify opportunities for intervention.
This was a mixed methods, cross-sectional study that used quantitative survey analysis and human-centered design (HCD). We performed a secondary analysis on a national multi-institutional survey on medical student wellbeing, including univariate and multivariate logistic regression, a comparison of logistic regression models with interaction terms, and analysis of free text responses. We also conducted semi-structured interviews with a sample of medical student respondents and non-student stakeholders to develop insights and design opportunities.
Independent risk factors for high debt-related stress included pre-clinical year (OR 1.75), underrepresented minority (OR 1.40), debt $20–100 K (OR 4.85), debt >$100K (OR 13.22), private school (OR 1.45), West Coast region (OR 1.57), and consideration of a leave of absence for wellbeing (OR 1.48). Mental health resource utilization ( p = 0.968) and counselors ( p = 0.640) were not protective factors against debt-related stress. HCD analysis produced 6 key insights providing additional context to the quantitative findings, and associated opportunities for intervention.
Conclusions
We used an innovative combination of quantitative survey analysis and in-depth HCD exploration to develop a multi-dimensional understanding of debt-related stress among medical students. This approach allowed us to identify significant risk factors impacting medical students experiencing debt-related stress, while providing context through stakeholder voices to identify opportunities for system-level solutions.
Peer Review reports
Introduction
Over the past few decades, it has become increasingly costly for aspiring physicians to attend medical school and pursue a career in medicine. Most recent data shows that 73% of medical students graduate with debt often amounting to six-Fig [ 1 ]. – an amount that is steadily increasing every year [ 2 ]. In 2020, the median cost of a four-year medical education in the United States (U.S.) was $250,222 for public and $330,180 for private school students [ 1 ] – a price that excludes collateral costs such as living, food, and lifestyle expenses. To meet these varied costs, students typically rely on financial support from their families, personal means, scholarships, or loans. Students are thereby graduating with more debt than ever before and staying indebted for longer, taking 10 to 20 years to repay their student loans regardless of specialty choice or residency length [ 1 ].
Unsurprisingly, higher debt burden has been negatively correlated with generalized severe distress among medical students [ 3 , 4 ], in turn jeopardizing their academic performance and potentially impacting their career choices [ 5 ]. Studies have found that medical students with higher debt relative to their peers were more likely to choose a specialty with a higher average annual income [ 5 ], less likely to plan to practice in underserved locations, and less likely to choose primary care specialties [ 4 ]. However, a survey of 2019 graduating medical students from 142 medical schools found that, when asked to rank factors that influenced their specialty choice, students ranked economic factors, including debt and income, at the bottom of the list. With this inconsistency in the literature, authors Youngclaus and Fresne declare that further studies and analysis are required to better understand this important relationship [ 1 ].
Unfortunately, debt and its negative effects disproportionately impact underrepresented minority (URM) students, including African Americans, Hispanic Americans, American Indian, Native Hawaiian, and Alaska Native [ 6 ], who generally have more debt than students who are White or Asian American [ 1 ]. In 2019, among medical school graduates who identified as Black, 91% reported having education debt, in comparison to the 73% reported by all graduates [ 1 ]. Additionally, Black medical school graduates experience a higher median education debt amount relative to other groups of students, with a median debt of $230,000 [ 1 ]. This inequitable distribution of debt disproportionately places financial-related stress on URM students [ 7 ], discouraging students from pursuing a medical education [ 8 ]. These deterring factors can lead to a physician workforce that lacks diversity and compromises health equity outcomes [ 9 ].
Limited literature exists to identify the impact of moderating variables on the relationship between debt and debt-related stress. Financial knowledge is found to be a strong predictor of self-efficacy and confidence in students’ financial management, leading to financial optimism and potentially alleviating debt stress [ 10 , 11 , 12 ]. Numerous studies list mindfulness practices, exercise, and connecting with loved ones as activities that promote well-being and reduce generalized stress among students [ 13 , 14 , 15 ]. However, to date, no studies have examined whether these types of stress-reducing activities, by alleviating generalized stress, reduce debt-related stress. Studies have not examined whether resources such as physician role models may act as a protective factor against debt-related stress.
Despite the growing recognition that debt burdens medical students emotionally and academically, we have yet to develop systemic solutions that target students’ unmet needs in this space. We performed the first multi-institutional national study on generalized stress among medical students, and found that debt burden was one of several risk factors for generalized stress among medical students [ 3 ]. The goal of this study is to build upon our findings by using a mixed methods approach combining rigorous survey analysis and human-centered design to develop an in-depth understanding of the impact that education debt has on medical students’ emotional and academic well-being and to identify opportunities for intervention.
We conducted a mixed methods, cross-sectional study that explored the impact of debt-related stress on US medical students’ well-being and professional development. This study was conducted at the University of California, San Francisco (UCSF). All activities were approved by the UCSF institutional review board, and informed consent was obtained verbally from participants prior to interviews. We performed a secondary analysis of the quantitative and qualitative results of the Medical Student Wellbeing Survey (MSWS), a national multi-institutional survey on medical student wellbeing administered between 2019 and 2020, to determine risk factors and moderating variables of debt-related stress. To further explore these variables, we used human-centered design (HCD), an approach to problem-solving that places users at the center of the research process in order to determine key pain points and unmet needs, and co-design solutions tailored to their unique context [ 16 ]. In this study, we performed in-depth, semi-structured interviews with a purposefully sampled cohort of medical students and a convenience sample of non-student stakeholders to determine key insights representing students’ unmet needs, and identified opportunities to ameliorate the impact of debt-related stress on medical students.
Quantitative data: the medical student wellbeing survey
The MSWS is a survey to assess medical student wellbeing that was administered from September 2019 to February 2020 to medical students actively enrolled in accredited US or Caribbean medical schools [ 3 ]. Respondents of the MSWS represent a national cohort of > 3,000 medical students from > 100 unique medical school programs. The MSWS utilizes a combination of validated survey questions, such as the Medical Student Wellbeing Index (MS-WBI), and questions based on foundations established from previously validated wellbeing survey methods [ 3 ]. Questions generally focused on student demographics, sources of stress during medical school, specialty consideration, and frequency in activities that promote wellbeing. Some questions ask students to rate physical, emotional, and social domains of wellbeing using a five-point Likert scale. Questions of interest from the MSWS included debt-related stress, generalized stress, intended specialty choice, and utilization of well-being resources and counselors. An additional variable investigated was average school tuition, which was determined by a review of publicly available data for each student’s listed medical school [ 17 ]. All data from the MSWS was de-identified for research purposes.
Stress: debt-related and generalized stress
Debt stress was assessed by the question, “How does financial debt affect your stress level?” Students responded using a five-point Likert scale from − 2 to 2: significant increase in stress (-2), mild increase (-1), no change (0), mild decrease (1), or significant decrease (2). Responses for this question were evaluated as a binary index of ‘high debt stress,’ defined as a response of − 2, versus ‘low debt stress,’ defined as a response of − 1 or 0. In addition, generalized stress from the MSWS was assessed by questions from the embedded MS-WBI, which produced a score. Previous studies have shown that the score can be used to create a binary index of distress: a score ≥ 4 has been associated with severe distress, and a score < 4 has been associated with no severe distress [ 18 ].
Intended specialty
We categorized students’ responses to intended specialty choice by competitiveness, using the 2018 National Resident Match Program data [ 19 ]. ‘High’ and ‘low’ competitiveness were defined as an average United States Medical Licensing Examination (USMLE) Step 1 score of > 240 or ≤ 230, respectively, or if > 18% or < 4% of applicants were unmatched, respectively. ‘Moderate’ competition was defined as any specialty not meeting criteria for either ‘high’ or ‘low’ competitiveness.
Resource utilization
The MSWS assessed the utilization of well-being resources by the question, “At your institution, which of the following well-being resources have you utilized? (Select all that apply)” Students responded by selecting each of the resource(s) they used: Mental Health and Counseling Services, Peer Mentorship, Self-Care Education, Mindfulness/Meditation Classes, Community Building Events, and Other. The number of choices that the student selected was calculated, allowing for placement into a category depending on the amount of resource utilization: 0–20%, 20–40%, 40–60%, 60–80%, 80–100%. Responses for this question were evaluated as a binary index of ‘high resource utilization,’ defined as a response of 80–100% resource utilization, versus ‘low resource utilization,’ defined as a response of < 80% resource utilization. The co-authors collaboratively decided upon this “top-box score approach,” [ 20 ] which is the sum of percentages for the most favorable top one, two or three highest categories on a scale, to assess if the most extreme users (80–100%) of these supportive resources experienced a decrease in debt-related stress. Additionally, use of a counselor for mental health support was assessed by the question, “Which of the following activities do you use to cope with difficult situations (or a difficult day on clinical rotation)? (Select all that apply).” Students responded by selecting the activities that they use from a list (e.g., listen to music, mindfulness practice, meet with a counselor, exercise). Responses for this question were evaluated as a binary index of ‘Meeting with a Counselor,’ defined by selection of that option, versus ‘Not Meeting with a Counselor,’ defined as not selecting that option.
Quantitative data analysis
We performed a secondary analysis of quantitative data from the MSWS to calculate frequencies and odds ratios for the five quantitative variables described above (debt-related stress, generalized stress, intended specialty, resource utilization, and school tuition). Tests performed are summarized in Table 1 (“Secondary Analysis Tests Performed”). Univariate analysis and multivariate logistic regression were performed among students in the high debt stress (-2) and low debt stress (0 or − 1) for select variables, such as clinical phase, URM, debt burden, specialty competitiveness, and average school tuition, to identify risk factors for high debt stress. To determine if ‘high resource utilization’ or ‘meeting with a counselor’ were moderating variables on the relationship between debt burden and debt stress, we applied the logistic regression with the interaction terms of ‘debt’ and ‘resource utilization’ (high vs. low). Then, we performed a similar analysis but replaced the interaction term with ‘debt’ and ‘meeting with a counselor’ (yes vs. no). We also performed Chi-squared tests to determine the degree to which severe distress increases as debt burden increases, if specialty competitiveness varied by debt stress, and if the proportion of students who identified as URM, in comparison to non-URM, differed by debt level. All statistical tests were two-sided and p < 0.05 was considered significant. Statistical analyses were performed using SAS version 9.4 and R version 4.0.5.
Qualitative data: interviews and MSWS free text responses
Free-text entries.
At the conclusion of the 2019–2020 MSWS, respondents had unlimited text space to provide comments to two prompts. The first prompt read, “What well-being resource(s), if offered at your school, do you feel would be most useful?” The second prompt read “If you have any further comments to share, please write them below.” Answers to either prompt that pertained to debt, cost of medical school, or finances were extracted for the purpose of this study and analyzed with the other qualitative data subsequently described.
Interview selection & purposive sampling
Interview participants were identified from a repository of respondents to the MSWS who had attached their email address and expressed willingness at the time of the survey to be contacted for an interview [ 3 ]. Our recruitment period was between April 19, 2021 to July 2, 2021. The recruitment process involved sending invitations to all of the email addresses in the list to participate in a 45-minute interview on the topic of student debt and wellbeing. The invitation included a brief screening questionnaire asking students to report updates to questions that were previously asked in the MSWS (i.e.: clinical training year, marital status, dependents). Additional novel questions included primary financial support system, estimate of financial support systems’ household income in the last year, estimate of educational financial debt at conclusion of medical school, student’s plan for paying off debt, and degree of stress (using a Likert scale from 0 to 10) over current and future education debt.
Purposeful sampling of medical student stakeholders for interviews allowed us to maximize heterogeneity. We utilized the students’ responses to the brief screening questionnaire with their corresponding responses to demographic questions from the MSWS to select interviewees that varied by gender, race, presence of severe distress, type of medical school (public vs. private), region of school, and tuition level of school. The sampling ensured a diverse representation, in accordance with HCD methodology [ 21 ]. Brief descriptions of participant experiences are listed in Table 2 (“Interviewee Descriptors”). Students who were selected for interviews were sent a confirmation email to participate. Interviews were to be conducted until thematic saturation was reached. In addition, to include representation from the entire ecosystem, we interviewed a financial aid counselor at a medical school and a pre-medical student, chosen through convenience sampling. We directly contacted those two individuals for interviews.
Semi-structured interviews
All interviews were conducted between April 2021 and July 2021 over Zoom. A single researcher conducted interviews over an average of 45 min. Informed consent was obtained verbally from participants prior to interviews; interviews and their recordings only proceeded following verbal consent. The interview guide (S1 File) included open-ended questions about students’ experience of debt-related stress and their reflections on its consequences. The audio recordings were transcribed using Otter.ai, a secure online transcription service that converts audio files to searchable text files. Interview responses were redacted to preserve anonymity of respondent identity.
Qualitative data analysis
Interview data was analyzed using a general inductive approach to thematic analysis. Specifically, two researchers (SL and AY) independently inductively analyzed transcripts from the first three semi-structured interviews to come up with themes relating to the experiences and consequences of debt-related stress. They reconciled discrepancies in themes through discussion to create the codebook (S2 File), which included 18 themes. SL and AY independently coded each subsequent interview transcript as well as the free text responses from the survey, meeting to reach a consensus on representative quotes for applicable themes.
Following the HCD methodology, two researchers met with the core team to discuss the themes from the interviews and translate them into “insight statements”, which reflect key tensions and challenges experienced by stakeholders. Insight statements carefully articulate stakeholders’ unique perspectives and motivations in a way that is actionable for solution development [ 22 ]. As such, these insight statements are reframed into design opportunities, which suggest that multiple solutions are possible [ 23 , 24 ]. For example, discussion about themes 1a and 1b (“Questionable Job Security” and “Disappointing MD salary and Satisfaction Payoff”) revealed that they were related in the way that they led students to wonder whether the investment in medical school would be offset by the salary payoff. This led to the identification of the tension for low-income students in particular, who have to weigh this tradeoff earlier in their medical school journey than other students who are less financially-constrained (insight: “Medical school is a risky investment for low-income students”.) The design opportunity logically translates into a call to action for brainstorming and solution development: “Support low-income students to make values-based tradeoffs when considering a career in medicine.”
MSWS respondents and quantitative analysis
A total of 3,162 students responded to the MSWS and their sociodemographic characteristics have been described previously [ 3 ]. A total of 2,771 respondents (87.6%) responded to our study’s variables of interest, including a response for ‘high debt stress’ (–2) or ‘low debt stress’ (–1 or 0). Table 3 lists the distribution of debt-related stress across different variables for all respondents.
Risk factors for debt-related stress
Factors that were independently associated with higher debt-related stress included being in pre-clinical year (OR 1.75, 95% CI 1.30–2.36, p < 0.001), identifying as URM (OR 1.40, 95% CI 1.03–1.88), p = 0.029), having debt $20–100 K (OR 4.85, 95% CI 3.32–7.30, p < 0.001), debt > 100 K (OR 13.22, 95% CI 9.05–19.90, p < 0.001), attending a private medical school (OR 1.45, 95% CI 1.06–1.98, p = 0.019), attending medical school on the West Coast (OR 1.57, 95% CI 1.17–2.13, p = 0.003), and having considered taking a leave of absence for wellbeing (OR 1.48, 95% CI 1.13–1.93, p = 0.004) (Table 4 , S1 Table).
Severe distress by debt amount
Levels of generalized severe distress differed across debt burden groups. As debt level increased, the percentage of individuals with “severe” distress increased ( p < 0.001).
Debt and career decisions
There were significant differences between the high debt stress versus low debt stress groups and plans to pursue highly vs. moderately vs. minimally competitive specialties ( p = 0.027) (Fig. 1 ) A greater percentage of low debt stress students were pursuing a highly competitive specialty or a minimally competitive specialty. A greater percentage of high debt stress students were pursuing a moderately competitive specialty. As shown in Table 4 , there were no differences in debt-associated stress between students who choose different specialties, such as medical versus surgical versus mixed (medical/surgical).
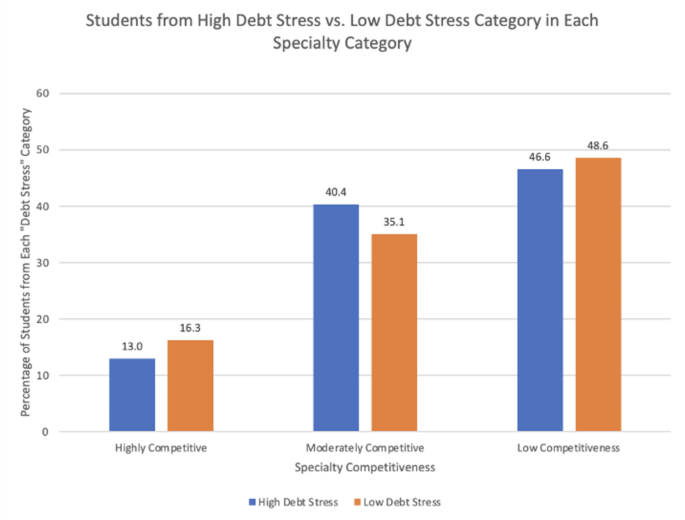
Debt stress by specialty competitiveness
URM students’ experience of debt
URM identity was an independent risk factor for higher debt-related stress (Table 4 ) In addition, debt levels varied between those who identify as URM versus non-URM ( p < 0.001). Students identifying as URM tended to have higher debt than those who did not. Although the percentage of non-URM students was higher than that of URM students within the lowest debt burden category (<$20k), among all higher debt burden categories, including $20–100 K, $100–300 K, and >$300K, the percentage of URM students was higher than the percentage of non-URM students.
Moderating factors on the relationship between debt and debt stress
Protective factors such as high degree of mental health resource utilization and meeting with a counselor did not reduce the impact of debt burden on debt stress. Among students who reported a high degree of mental health resource utilization, there was no impact on the relationship between debt and debt stress ( p = 0.968). Similarly, meeting with a counselor had no impact on the relationship between debt and debt stress ( p = 0.640).
Interview respondents and qualitative analysis
We conducted in-depth, semi-structured interviews with 11 medical students, who are briefly described in Table 2 . We reached thematic saturation with 11 interviews, a point at which we found recurring themes. Therefore, no further interviews were needed. Among the medical student interviewees, there was representation from all regions, including the Northeast ( n = 3), West Coast ( n = 5), Midwest ( n = 2), and South ( n = 1). Students were also from all clinical phases, including pre-clinical ( n = 3), clinical ( n = 4), gap year/other ( n = 2), and post-clinical ( n = 2). Most interviewees were female ( n = 8) and 5 of the interviewees identified as URM. Financial support systems were diverse, including self ( n = 3), spouse/partner ( n = 3), and parents/other ( n = 5). Most interviewees reported low debt stress ( n = 8), as opposed to high debt stress ( n = 3). 55% of interviewees planned to pursue specialties that pay <$300K ( n = 6), with some pursuing specialties that pay $300–400 K ( n = 2) and >$400K ( n = 3).
Among the MSWS free-text responses, to the prompt, “What well-being resource(s), if offered at your school, do you feel would be most useful?” 20 of 118 respondents (16.9%) provided free-text responses that pertained to debt, cost of medical school, or finances. To the prompt “If you have any further comments to share, please write them below” 11 of 342 students (3.2%) provided relevant free-text responses. Analysis of the free-text responses and semi-structured interviews revealed 6 distinct insights (Table 5 ), with each insight translated into an actionable design opportunity.
Medical school is a risky investment for low-income students.
Description
The personal and financial sacrifices required for low-income students to attend medical school and pursue a career in medicine outweigh the benefits of becoming a physician. When considering a career in medicine, students feel discouraged by questionable job security (theme 1a) and reduced financial compensation (theme 1b) – a combination that jeopardizes immediate and long-term job satisfaction. Some students feel hopeful that their decision to pursue medicine will be personally rewarding (1b.6) and their salaries will stabilize (1a.1, 1a.5), but many low-income students experience doubt about whether they made the right career choice (1b.2, 1b.4, 1b.6), and feel stressed that they will be in debt for longer than they expected (1a.3, 1a.4, 1b.1, 1b.5). Support low-income students to make values-based tradeoffs when considering a career in medicine.
Design opportunity
Support low-income students to make values-based tradeoffs when considering a career in medicine.
Medical schools lack the adaptive infrastructure to be welcoming to low-income students.
Students face financial challenges from the moment they apply to medical school (theme 2a), a costly process that limits admissions options for low-income students due to their inability to pay for numerous application fees (2a.1) and expensive test preparation courses (2a.2, 2a.3). Once students begin medical school, they feel unsupported in their varied responsibilities towards their families (theme 2b) and additional financial needs (theme 2c), requiring them to make tradeoffs with their education and personal lives (2b.2, 2c.1).
Design opportunity 2
Develop flexible systems that can recognize and accommodate students’ complex financial needs during medical school.
Students worry about the impact that their medical school debt has on their present and future families, which compounds feelings of guilt and anxiety.
For students who need to take loans, the decision to pursue a career in medicine is a collective investment with their families. Students feel guilty about the sacrifices their families have to make for the sake of their career (theme 3a) and feel pressure to continue to provide financially for their family while having debt (theme 3b). Students are stressed about acquiring more debt throughout their training (3a.1) and the impact that has on loved ones who are dependent on them (3a.4, 3a.5, 3b.2), especially with respect to ensuring their financial security in the future (3b.4).
Design opportunity 3
Create an environment that acknowledges and accounts for the burden of responsibility that students face towards their families.
Without the appropriate education about loans, the stress of debt is exponentially worse.
Students feel the greatest fear around loans when they do not understand them, including the process of securing loans and paying off debt (theme 4a). Students are overwhelmed by their loan amounts (4a.5) and lack the knowledge or resources to manage their debt (4a.1, 4a.2), making them uncertain about how they will become debt-free in the future (4a.3, 4a.4). Students reported that various resources helped to alleviate those burgeoning fears (theme 4b), including financial aid counselors (4b.2, 4b.3) and physician role models (4b.5, 4b.6) that generally increase knowledge and skills related to debt management (4b.1).
Design opportunity 4
Empower students to become experts in managing their debt by making loan-related resources more available and accessible.
The small, daily expenses are the most burdensome and cause the greatest amount of stress.
Students with educational debt are mentally unprepared for the burden of managing their daily living expenses (theme 5a), causing them to make significant lifestyle adjustments in the hopes to ease their resulting anxiety (theme 5b). These costs are immediate and tangible, compared to tuition costs which are more distant and require less frequent management (5a.3) Students learn to temper their expectations for living beyond a bare minimum during medical school (5a.1, 5b.2, 5b.4) and develop strategies to ensure that their necessary expenses are as low as possible (5b.1, 5b.2, 5b.3, 5b.4).
Design opportunity 5
Develop and distribute resources to support both short- and long-term financial costs for medical students.
Students view debt as a dark cloud that constrains their mental health and dictates their career trajectory.
The constant burden of educational debt constrains students’ abilities to control their mental health (theme 6a) and pursue their desired career path in medicine (themes 6b & 6c). Students feel controlled by their debt (6a.3) and concerned that it will impact their [ability] to live a personally fulfilling life (6a.1, 6a.2, 6c.6), especially with respect to pursuing their desired medical specialties (6b.1, 6c.3, 6c.5, 6c.6). Students with scholarships, as opposed to loans, felt more able to choose specialties that prioritized their values rather than their finances (6c.1, 6c.2), an affordance that impacts long-term career growth and satisfaction.
Design opportunity 6
Create a culture of confidence for managing debt and debt-stress among medical students.
This is the first multi-institutional national study to explore the impact of debt-related stress on medical students’ well-being in the United States. We used an innovative, mixed methods approach to better understand the factors that significantly affect debt-related stress, and propose opportunities for improving medical student well-being.
URM students
Analysis of survey results found that students who identify as URM are more likely to experience higher levels of debt-related stress than non-URM students. Our study also found that among all higher debt burden categories, debt levels were higher for URM students, findings consistent with studies that have shown the disproportionate burden of debt among URM students [ 1 ]. Our semi-structured interviews illuminated that students from low-income backgrounds feel unsupported by their medical schools in these varied financial stressors that extend beyond tuition costs (insight 2), leaving their needs unmet and increasing financial stress over time: “We don’t have different socio-economic classes in medicine because there’s constantly a cost that [isn’t] even factored into tuition cost [and] that we can’t take student loans for.” Many URM students feel especially stressed by their financial obligations towards their families (insight 3), and describe the decision to enter into medicine as one that is collective ( “the family’s going to school” ) rather than individual, placing additional pressure on themselves to succeed in their career: “ Being of low SES , the most significant stressor for me is the financing of medical school and the pull of responsibility for my family.” Several other studies from the literature confirm that students who identify as URM and first generation college or medical students are at higher risk for financial stress compared to their counterparts [ 7 ], and report that they feel as though it is their responsibility to honor their families through their educational and career pursuits [ 25 ]. Our study demonstrates and describes how low-income and URM students face numerous financial barriers in medical school, resulting in medical trainees that are less diverse than the patient populations they are serving [ 1 , 8 ].
Debt amount
Our quantitative analysis found that students with debt amounts over $100,000 are at much higher risk for experiencing severe stress than students with debt less than that amount. Although this finding may seem intuitive, it is important to highlight the degree to which this risk differs between these two cohorts. Students with debt amounts between $20,000 and $100,000 are approximately 5 times more likely to experience high stress than students with debt less than $20,000, while students with debt amounts over $100,000 are approximately 13 times more likely to experience severe stress when compared to the same cohort. Interview participants describe that the more debt they have, the less hopeful they feel towards achieving financial security (insight 1): “There are other healthcare professionals that will not accrue the same amount of loans that we will , and then may or may not have the same salary or privileges […] makes me question , did I do the right thing?” Students internalize this rising stress so as not to shift the feelings of guilt onto their families (insight 3), thereby compounding the psychological burden associated with large amounts of debt (insight 6): “As long as you’re in debt , you’re owned by someone or something and the sooner you can get out of it , the better; the sooner I can get started with my life.”
Pre-clinical students
According to our survey analysis, students who are in their pre-clinical years are at higher risk for stress than students in their clinical years. Our interview findings from insight 4 suggest that students feel initially overwhelmed and unsure about what questions to ask ( “One of my fears is that I don’t know what I don’t know”) or how to manage their loans so that it doesn’t have a permanent impact on their lives: “The biggest worry is , what if [the debt] becomes so large that I am never able to pay it off and it ends up ruining me financially.” Pre-clinical students may therefore feel unsure or ill-equipped to manage their loans, making them feel overwhelmed by the initial stimulus of debt. By the time students reach their clinical years, they may have had time to develop strategies for managing stress, acquire more financial knowledge, and/or normalize the idea of having debt.
Medical school characteristics
Our survey analysis found several risk factors related to medical school characteristics. First, we found that students who attended a private school were at higher risk for debt-related stress than students who attended a public school. Not only is the median 4-year cost of attendance in 2023 almost $100,000 higher in private compared to public medical schools [ 26 ], but it is also the case that financial aid packages are more liberally available for public schools due to state government funding [ 27 ]. This not only relieves students from having higher amounts of debt, but it also creates a more inclusive cohort of medical students. Insight 2 from our interviews suggests that private medical schools without the infrastructure to meet students’ varying financial needs force low-income students to make tradeoffs between their education and personal lives.
Another characteristic that was found to be a risk factor for debt stress was attending a medical school on the West Coast (compared to a non-coastal school.) This was a surprising finding given that tuition rates for both private and public schools on the West Coast are no higher than those in other regions [ 17 ]. The distribution of survey respondents did not vary significantly across regional categories, so no bias in sample size is suspected. While these interviews were not designed to address the reasoning behind students’ choice of medical school matriculation, there is a potential explanation for this finding. Historically, students match for residency programs that are in their home state or not far from their home state; [ 28 , 29 ] therefore, we speculate that students may prefer to settle on the West Coast, and may be willing to take on more financial debt in pursuit of their long-term practice and lifestyle goals.
Our quantitative analysis found that students who reported having considered taking a leave of absence for well-being purposes were at higher risk for debt-related stress. This cohort of students likely experience higher levels of stress as they are conscious of the negative impact it has on their life, and have already ruminated on leaving medical school. A study by Fallar et al. found that the period leading up to a leave of absence is particularly stressful for students because they are unfamiliar with the logistics of taking time off, and don’t feel as though leaving medical school is encouraged or normalized for students [ 30 ]. An interview with a student who did a joint MD and PhD program expressed having more time for herself during her PhD program, and described using money for activities that could alleviate stress (“I took figure skating during my PhD”) rather than create more stress by compromising on their lifestyle during medical school (insight 5). More research may be needed to better understand and support students considering taking a leave of absence from medical school.
- Specialty choice
Our study found that students with high debt stress pursue moderately competitive specialties compared to students with low debt stress. This may be explained by the fact that low debt stress gives students the freedom to pursue minimally competitive specialties, which may be more fulfilling to them but typically have lower salaries. Insight 6 further elaborates upon this finding that students with high debt stress deprioritize specialties for which they are passionate in favor of higher paying specialties that might alleviate their debt: “I love working with kids…but being an outpatient pediatrician just wasn’t going to be enough to justify the [private school] price tag.” Students with lower debt stress describe having the freedom to choose specialties that align with their values, regardless of anticipated salary: “Scholarships give me the freedom to do [specialties] that maybe are a little bit less well-paying in medicine.” Interestingly, certain studies examining the relationship between specialty choice and debt stress have found that high debt stress is associated with a higher likelihood of pursuing a more competitive, and presumably higher paying, specialty [ 5 ]. More research investigating the relationship between debt stress and specialty choice could illuminate opportunities for increasing a sense of agency and overall satisfaction among students for their career choices.
In our exploration of potential protective factors against the effects of debt-related stress, our survey analysis found that the two variables measured (high mental health resource utilization and meeting with a counselor) did not have any impact on reducing debt-related stress. This finding is inconsistent with the literature, which considers these activities to promote general well-being among students but has never been studied in the context of debt-related stress [ 13 , 14 , 15 ]. A potential explanation is that the survey questions that assessed these activities were imperfect. For example, the question of meeting with a counselor was not a standalone question, but instead, was at the bottom of a list of other wellbeing activities; therefore, students may have been fatigued by the time they got to the bottom of the list and not selected it. Additionally, our definition of “high” mental health resource utilization may have been perceived as too strict (i.e.: 80–100%) and perhaps we would have seen effects at lower percentages of utilization (i.e.: 40–60%). Despite this finding, students describe in their interviews that having access to certain resources such as financial knowledge and physician role models can help to alleviate stress by helping them feel confident in managing their loans in the immediate and more distant future (insight 4): “I’ve had explicit discussions with physicians who went to med school , had debt , paid it off [.] the debt hasn’t hindered their life in any way. I think that just makes me feel a lot calmer.” This finding aligns with previous studies that suggest that financial knowledge, such as knowledge about loans and a payoff plan, confers confidence in students’ financial management [ 11 , 12 ]. These factors are also aligned with previous studies that suggest financial optimism, such as with a physician role model who successfully paid off loans, is associated with less financial stress [ 10 ].
Our quantitative analysis of risk factors helped us to identify which areas might significantly impact debt-related stress among medical students, while our qualitative analysis provided more in-depth insight into those risk factors for more human-centered intervention design. The HCD process not only provides additional context from the perspective of medical students, but also proposes distinct design opportunities upon which interventions may be designed and tested. Drawing from the six design opportunities outlined in this paper, we propose a solution on a national scale: lowering the cost of the MCAT and medical school applications to reduce the financial barrier to applying to medical school [ 31 ]. We also propose the following solutions that can be implemented at the level of medical schools to better support medical students facing debt-related stress: (1) providing adequate financial aid that prevents low-income students from needing to work while being in medical school [ 32 ], (2) providing targeted financial planning classes and counseling for first-year medical students who have taken loans [ 33 ], and (3) creating mentorship programs that pair medical students with debt with physician role models who had also had debt but successfully paid it off [ 34 ]. We encourage medical schools to consider these suggestions, choosing the ideas from the list that make sense and tailoring them as necessary for their students and their unique needs. Additionally, given that our quantitative portion of the study was a secondary analysis of a survey focused on general medical student well-being, a nationwide study is needed that is specifically designed to explore the topic of debt-related stress among medical students. Furthermore, more research is needed that assesses the impact of activities that promote well-being (e.g., access to therapy, mindfulness practices, exercise) on debt-related stress among medical students.
Limitations
Our study had some notable limitations. One potential limitation is that our data collection occurred between 2019 and 2021 for this publication in 2023. Additionally, as described in the original study [ 3 ], a limitation of the MSWS is the inability to determine a response rate of students due to the survey distribution by medical student liaisons from each medical school; under the reasonable assumption that the survey was distributed to every US allopathic medical student, the response rate was estimated to have been 8.7%. 3 An additional limitation is the potential for response bias [ 3 ]. A limitation of the qualitative interviews is the potential for response bias among the interviewees. Although we purposely sampled, the students who accepted the invitation to interview may have been students with extreme views, either very negative views of debt or very neutral views of debt. Additionally, the interviewees were not representative of all possible financial situations, given that most students were from private schools, which typically have higher tuition rates. Also, all students had debt amounts in the middle and high categories, with none in the low category. Finally, our model of risk factors for debt-related stress suggested the presence of negative confounding factors, which exerted effects on specific variables (i.e.: pre-clinical year, West Coast) for which univariate analysis found no significant associations but multivariate analysis did. We did not perform further analysis to identify which variables served as the negative confounding variables.
In conclusion, our mixed methods, cross-sectional study exploring debt-related stress and its impact on US medical students’ wellbeing and professional development revealed a set of risk factors and design opportunities for intervention. By using a combined quantitative and qualitative HCD approach, we were able to develop a broad, in-depth understanding of the challenges and opportunities facing medical students with education debt. With these efforts to support the well-being and academic success of students at higher risk of debt-related stress, medical education institutions can develop and nurture a more diverse medical field that can best support the needs of future patients.
Data availability
Data is provided within the supplementary information files.
Youngclaus J, Julie Fresne. Physician education debt and the cost to attend medical school: 2020 update. Association of American Medical Colleges; 2020.
Association of American Medical Colleges. Medical school graduation questionnaire: 2020 all schools summary report. 2020 [cited 2023 Sep 7]. https://www.aamc.org/data-reports/students-residents/report/graduation-questionnaire-gq
Rajapuram N, Langness S, Marshall MR, Sammann A. Medical students in distress: the impact of gender, race, debt, and disability. PLoS ONE. 2020;15(12):e0243250.
Article Google Scholar
Rohlfing J, Navarro R, Maniya OZ, Hughes BD, Rogalsky DK. Medical student debt and major life choices other than specialty. Med Educ Online. 2014;19. https://doi.org/10.3402/meo.v19.25603
Pisaniello MS, Asahina AT, Bacchi S, Wagner M, Perry SW, Wong ML, et al. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. BMJ Open. 2019;9(7):e029980.
AAMC. [cited 2023 Oct 18]. Unique populations. https://www.aamc.org/professional-development/affinity-groups/gfa/unique-populations
McMichael B, Lee IVA, Fallon B, Matusko N, Sandhu G. Racial and socioeconomic inequity in the financial stress of medical school. MedEdPublish (2016). 2022;12:3.
Mclnturff B. E. Frontczak. Medical school applicant survey. 2004.
Morrison E, Grbic D. Dimensions of diversity and perception of having learned from individuals from different backgrounds: the particular importance of racial diversity. Acad Med. 2015;90(7):937.
Heckman S, Lim H, Montalto C. Factors related to financial stress among college students. J Financial Therapy. 2014;5(1):19–39.
Heckman SJ, Grable JE. Testing the role of parental debt attitudes, student income, dependency status, and financial knowledge have in shaping financial self-efficacy among college students. Coll Student J. 2011;45(1):51–64.
Google Scholar
Gillen M, Loeffler DN. Financial literacy and social work students: knowledge is power. Journal of Financial Therapy. 2012 [cited 2023 Sep 13];3(2). https://newprairiepress.org/jft/vol3/iss2/4
Conley CS, Durlak JA, Dickson DA. An evaluative review of outcome research on universal mental health promotion and prevention programs for higher education students. J Am Coll Health. 2013;61(5):286–301.
Luken M, Sammons A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther. 2016;70(2):p70022500201–10.
Weight CJ, Sellon JL, Lessard-Anderson CR, Shanafelt TD, Olsen KD, Laskowski ER. Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clin Proc. 2013;88(12):1435–42.
Design. Kit. [cited 2023 Oct 2]. What is human-centered design? https://www.designkit.org/human-centered-design.html
AAMC. Tuition and student, fees reports. 2006–2013 tuition and student fees report. https://www.aamc.org/data-reports/reporting-tools/report/tuition-and-student-fees-reports
Dyrbye LN, Schwartz A, Downing SM, Szydlo DW, Sloan JA, Shanafelt TD. Efficacy of a brief screening tool to identify medical students in distress. Acad Med. 2011;86(7):907–14.
Charting outcomes in the match. U.S. allopathic seniors (Characteristics of U.S. allopathic seniors who matched to their preferred specialty in the 2018 main residency match). [cited 2023 Sep 18]. https://www.nrmp.org/wp-content/uploads/2021/07/Charting-Outcomes-in-the-Match-2018_Seniors-1.pdf
Greg Timpany. Top-box score – deriving a new measure. QuestionPro. https://www.questionpro.com/blog/creating-a-top-box-score/
Design. Kit. [cited 2023 Oct 9]. Extremes and mainstreams. https://www.designkit.org/methods/extremes-and-mainstreams.html
Design Kit. [cited 2023 Sep 18]. Create insight statements. https://www.designkit.org/methods/create-insight-statements.html
Designing an information and communications technology tool with and for victims of violence and their case managers in San Francisco. Human-centered design study. [cited 2024 Aug 12]. https://mhealth.jmir.org/2020/8/e15866
Bridge Innovate ® . 2017 [cited 2024 Aug 12]. Turning insights into opportunities. https://www.bridgeinnovate.com/blog/2017/12/19/turning-insights-into-opportunities
Van T, Bui K. First-generation college students at a four-year university: background characteristics, reasons for pursuing higher education, and first-year experiences. Coll Student J. 2002;36(1):3.
Students. & Residents. [cited 2023 Oct 18]. You can afford medical school. https://students-residents.aamc.org/financial-aid-resources/you-can-afford-medical-school
Medical schools with best financial aid. in 2023 | BeMo ® . [cited 2023 Oct 18]. https://bemoacademicconsulting.com/blog/medical-schools-with-best-financial-aid
Hasnie A, Hasnie U, Nelson B, Aldana I, Estrada C, Williams W. Relationship between residency match distance from medical school and virtual application, school characteristics, and specialty competitiveness. Cureus. 15(5):e38782.
Dorner FH, Burr RM, Tucker SL. The geographic relationships between physicians’ residency sites and the locations of their first practices. Acad Med. 1991;66(9):540.
Fallar R, Leikauf J, Dokun O, Anand S, Gliatto P, Mellman L, et al. Medical students’ experiences of unplanned leaves of absence. Med Sci Educ. 2019;29(4):1003–11.
Millo L, Ho N, Ubel PA. The cost of applying to medical school — a barrier to diversifying the profession. N Engl J Med. 2019;381(16):1505–8.
Should you work during medical school? | Medical School Admissions Doctor | U.S. News. [cited 2024 Jul 27]. https://www.usnews.com/education/blogs/medical-school-admissions-doctor/articles/should-you-work-during-medical-school
First year in medical school?. Here’s your financial checklist | American Medical Association. [cited 2024 Jul 27]. https://www.ama-assn.org/medical-students/medical-student-finance/first-year-medical-school-heres-your-financial-checklist
The White Coat Investor - Investing. & Personal Finance for Doctors. [cited 2024 Jul 27]. Physician Personal Finance | White Coat Investor. https://www.whitecoatinvestor.com/personal-finance-for-doctors/
Download references
Acknowledgements
We thank the members of The Better Lab, including Devika Patel, Christiana Von Hippel, and Marianna Salvatori, for their support. We appreciate Pamela Derish (UCSF) for assistance in manuscript editing and the UCSF Clinical and Translational Science Institute (CTSI) for assistance in statistical analysis. This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 TR001872. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Funding was not obtained for this project.
Author information
Adrienne Yang, Simone Langness and Lara Chehab contributed equally to this work.
Authors and Affiliations
Department of Surgery, University of California, San Francisco, CA, USA
Adrienne Yang, Lara Chehab & Amanda Sammann
Department of Trauma Surgery, Sharp HealthCare, San Diego, CA, USA
Simone Langness
Department of Pediatrics, Stanford University, Stanford, CA, USA
Nikhil Rajapuram
Department of Epidemiology and Biostatistics, University of California, San Francisco, CA, USA
You can also search for this author in PubMed Google Scholar
Contributions
A.Y. and L.C. wrote the main manuscript text and prepared the figures. S.L. created the study design. All authors reviewed the manuscript.
Corresponding author
Correspondence to Adrienne Yang .
Ethics declarations
Ethics approval and consent to participate.
All activities conducted as part of this study were approved by the UCSF Institutional Review Board. Informed consent was obtained verbally from all participants prior to conducting interviews.
Consent for publication
We, the authors, consent to the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Yang, A., Langness, S., Chehab, L. et al. Medical students in distress: a mixed methods approach to understanding the impact of debt on well-being. BMC Med Educ 24 , 947 (2024). https://doi.org/10.1186/s12909-024-05927-9
Download citation
Received : 12 April 2024
Accepted : 19 August 2024
Published : 30 August 2024
DOI : https://doi.org/10.1186/s12909-024-05927-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 28.8.2024 in Vol 26 (2024)
Current Status of ChatGPT Use in Medical Education: Potentials, Challenges, and Strategies
Authors of this article:

Tianhui Xu 1, 2 , MSN, RN ; Huiting Weng 1 , MSN, RN ; Fang Liu 1 , MSN, RN, PhD ; Li Yang 1 , MSN, RN ; Yuanyuan Luo 2 , MSN, RN ; Ziwei Ding 2 , MSN, RN ; Qin Wang 1, 2 , MSN, RN
1 Clinical Nursing Teaching and Research Section, The Second Xiangya Hospital of Central South University, Changsha, China
2 Xiangya School of Nursing, Central South University, Changsha, China
Corresponding Author:
- Qin Wang , MSN, RN
- Clinical Nursing Teaching and Research Section
- The Second Xiangya Hospital of Central South University
- 139 Middle Renmin Road
- Changsha , 410011
- Phone: 86 18774806226
- Email: [email protected]
Medical Student Research Journal
Michigan state university college of human medicine.

Questions not answered here or on other pages can be directed to our contact page .
- How does the submission or review process work?
- What is the timeline of submission to publication?
- What are the outcomes of the review process?
- What types of articles do you accept?
- Who is eligible to submit an article?
- Can I get a physical copy of my article?
- How much does it cost to publish with MSRJ?
- When are issues published and when do I have to submit?
- How can I become a reviewer?
- What is your journal’s ISSN number?
- How do you cite an article from the Medical Student Research Journal?
- How do you subscribe to issues from MSRJ?
1. How does the submission or review process work?
For more details, review our MSRJ Review Process page.
2. What is the timeline of submission to publication?
Generally, it should take about 3-6 months from initial receipt of the manuscript to publication (E-publication or printed journal). See our MSRJ Review Process page for more specific details.
3. What are the outcomes of the review process?
- Accept without revisions
- Accept with revisions
This is detailed more specifically in our MSRJ Review Process page.
4. What types of articles do you accept? (Follow links for more detailed descriptions of each type) :
- Case Studies
- Original Research
- Reflections
- Brief Report
5. Who is eligible to submit an article?
There are few criteria required to be eligible for submitting to MSRJ , described in the general guidelines , but briefly:
The submission has not been previously published, nor is it currently submitted to another journal for consideration, and the first author is a medical student enrolled in an accredited medical college. A copy of a letter of current enrollment or letter of good standing that is signed by appropriate faculty on school letterhead must be submitted, including year of anticipated graduation.
6. Can I get a physical copy of my article?
Yes! However, we do only produce limited quantities of the journal in booklet format, so if you would like a copy, please let us know. Full color, or color cover-only copies are available. Each issue of the journal is published online for public access because this is an open-access journal.
7. How much does it cost to publish with MSRJ?
The Medical Student Research Journal (MSRJ) is a non-profit organization that does not charge its authors or readers as we aim to promote medical student learning and publication abilities.
8. When are issues published and when do I have to submit?
The publishing timeline of the MSRJ is given in the table below. In order to be published in a specific issue of the journal, articles must be submitted by the given submission deadline for that issue. The editors work hard to ensure articles will make it into a specified issue. Revisions that are not returned in a timely fashion may create a delay, leading to article being published in the next issue. Articles that are asked to be resubmitted may not follow this timeline, but every effort will be made to publish as soon as possible.
| Issue | Submission Deadline | Publication Date |
|---|---|---|
| Winter Issue | October 1st | December 31st |
| Spring Issue | February 15th | May 31st |
| Fall Issue | July 15th | September 30th |
9. How can I become a reviewer?
Students enrolled in an accredited medical college (verified by letter from dean’s department) may apply to become a reviewer for the journal. The prospective reviewers will complete a concise training, including lectures and modules on the process and background of article review. After finishing the MSRJ training, the students will then be a reviewer for the journal.
If you would like to become a reviewer, please visit our reviewer training page .
10. What is your journal’s ISSN number?
The Medical Student Research Journal is catalogued with an ISSN: 2159-3647
11. How do you cite an article from the Medical Student Research Journal?
Kabadi CJ, Smith III CR, Gomez F. Potential Pathogen Transmission on Medical Student Anatomy Laboratory Clothing. Medical Student Research Journal . 2013;2(Spring):30-35.
Kabadi CJ, Smith III CR, Gomez F. Potential Pathogen Transmission on Medical Student Anatomy Laboratory Clothing [Abstract]. Medical Student Research Journal . 2013;2(Spring):30-35.
12. How do you subscribe to issues from MSRJ?
Contact us here and in the subject line include “Please add me to the subscription list”. Please make sure your email address is included. We’ll send you updates about MSRJ its issues!

IMAGES
VIDEO
COMMENTS
Methods: An online, cross-sectional survey was distributed in October 2022 to medical students at Michigan State University College of Human Medicine (n = 806) to explore demographics, bias, family planning, and available resources. Descriptive analyses, a two- tailed t-test comparing female and male responses, and a one-way analysis of ...
The Medical Student Research Journal (MSRJ) is a research journal authored, reviewed, edited and published by medical students, for medical students. It is currently the longest running, active medical-student run research journal in the United States. MSRJ is dedicated to promoting scientific achievements of medical students, teaching ...
These journals specifically seek submissions from physicians in training and are accessible for newcomers in publishing. The Harvard Medical Student Review - The Harvard Medical Student Review is student-founded, student-managed and student-administered, under the guidance of faculty and staff. Its mission is to provide a platform for students to contribute to important issues facing health ...
Insight: Indiana University Medical Student Research Journal. Current Archives Announcements About About the Journal Submissions Editorial Team Contact Search Register Login Current Issue Vol. 6 No. 1 (2024) Published: 2024-05-15 Full Issue PDF Respecting the Limits of Method ...
This piece of work strives to piece together and serve as a reminder of the elements that make for a successful and impactful relationship. Published on date: September 31, 2014 Senior Editor: N/A Junior Editor: N/A DOI: pending Citation: DeKoninck T. Broken. Medical Student Research Journal. 2014;4(Fall):2-3. References: N/A
Vol. 2: Winter, 2013 February 27, 2013. We are pleased to release the Volume 2, Winter 2013 issue of the Medical Student Research Journal. This is our second issue and contains articles from authors at the Liverpool University, the University of Dundee and our home institution, Michigan State University's College of Human Medicine.
As the longest-standing, non-interrupted, International Journal for Medical Students with a high impact, visibility, and an international inclusive editorial board, the objective of the International Journal of Medical Students (IJMS) is to be the primary diffusion platform for early-career scientists in medicine, using evidence-based standards in the process of scientific publication. 1 It is ...
The Harvard Medical Student Review (HMSR) is a student-run medical journal publishing scholarly articles, reviews, editorials, and original artwork. The Harvard Medical Student Review (HMSR) is a student-run medical journal publishing scholarly articles, reviews, editorials, and original artwork. ... Research. Jul 29, 2024. Assessing the Oral ...
The International Journal of Medical Students (IJMS) has emerged over the past decade as a critical platform for showcasing medical student innovation and experiences. Though the work of trainees has historically been undervalued and over scrutinized, the IJMS is committed to highlighting the immense capacity for novel and robust research in this cohort.
The International Journal of Medical Students ( IJMS) is an open-access, peer-reviewed scientific journal (ISSN 2076-6327) that publishes original research and experiences in all fields of medicine. The IJMS was created in 2009 to share scientific production and experiences where there is at least one author enrolled as a medical student ...
Editorial Policy. The Florida Medical Student Research Journal is a student-run, refereed journal designed to publish medical research of interest to Florida Medical Students and the greater medical community. The Journal accepts submissions from anyone conducting research in medicine, regardless of their position, field, or location.
The International Journal of Medical Students is a peer-reviewed, open-access scientific journal created to share the research and experiences of medical students worldwide. Student BMJ Launched in 1992, this international journal publishes articles that have been commissioned with medical students in mind.
The American Medical Student Research Journal: Created by medical students, this journal gives future physician-scientists the opportunity to develop the critical thinking skills needed to succeed in academia and clinical practice. The journal is written, reviewed and edited by medical students working under the guidance of faculty mentors.
Medical student journals (MSJs) refer to a cluster of entirely student-led periodicals that publish student-authored articles. [ 1] Their primary aim is to foster scientific research publishing among medical students. They provide a fitting platform for medical students to disseminate their scholarly research work.
The Medical Student Research Journal (MSRJ) is the longest-running international academic journal in the United States authored, reviewed, edited, and published by medical students for medical students. It is dedicated to promoting the scientific achievements of medical students, teaching principles of peer and article review, and providing ...
An average of 30% (0.30, 0.19-0.44) of research performed by medical students resulted in a peer-reviewed journal publication. When only higher quality publications were included in the analysis (indexed in Medline, Scopus or Medic), the proportion remained more or less the same (0.31, 0.18-0.47).
Student Editor, IJMS. 5 MD, PhD student. Faculty of Medicine, "Carol Davila" University of Medicine and Pharmacy, 050474 Bucharest, Romania & Department of Hematology, Center of Hematology and Bone Marrow Transplantation, Fundeni Clinical Institute, 022328 Bucharest, Romania. Scientific Editor, IJMS.
Medical Student Research Journal (MSRJ) (MSRJ) is the longest-running international academic journal in the United States authored, reviewed, edited, and published by medical students for medical students. It is dedicated to promoting the scientific achievements of medical students, teaching principles of peer and article review, and providing editorial, publishing and leadership learning ...
The Medical Student Research Journal (MSRJ) is a research journal authored, reviewed, edited and published by medical students, for medical students. It is currently the longest running, active medical-student run research journal in the United States. MSRJ is dedicated to promoting scientific achievements of medical students, teaching ...
Medical student participation in research is associated with improved short- and long- term scientific productivity, more informed career choices and improved knowledge about-, interest in- and attitudes towards research. ... 2015 Jun 18;10(6):e0127470. doi: 10.1371/journal.pone.0127470. eCollection 2015. Authors Mohamed Amgad 1 , Marco Man Kin ...
Similar findings from additional research with medical students indicated that they did not comprehend AI or machine language. (Jha et al., Citation 2022 ; Jindal & Bansal, Citation 2020 ) In a study it was seen that the level of knowledge was good since 'virtual patient learning', and 'virtual reality simulation', have been ...
The submission file must be in Microsoft Word (either .doc or .docx). Measurements of length, height, weight, and volume should be reported in metric units (meters, kilograms, or liters); if information is better conveyed using U.S. standards of measurement, such as height or weight of a patient, those should be in parentheses in addition to ...
Medical Student Research Journal, Grand Rapids, Michigan. 3,178 likes. The Medical Student Research Journal (MSRJ) is the longest-run academic journal in the United States
Medical students' knowledge about antibiotic use and AMR varies based on school type, major, and clinical experience, with positive associations observed between enhanced knowledge and classroom instruction as well as the time dedicated to learning about these issues. 27 To identify the factors that influence the prescribing behavior of ...
Background Nearly three in four U.S. medical students graduate with debt in six-figure dollar amounts which impairs students emotionally and academically and impacts their career choices and lives long after graduation. Schools have yet to develop systems-level solutions to address the impact of debt on students' well-being. The objectives of this study were to identify students at highest ...
With your submission, please include: 1. Letter of good standing or letter of current enrollment from medical school, on school letterhead, signed by appropriate faculty. 2. Original manuscript that has NOT been previously published or submitted to another journal for review. 3.
ChatGPT, a generative pretrained transformer, has garnered global attention and sparked discussions since its introduction on November 30, 2022. However, it has generated controversy within the realms of medical education and scientific research. This paper examines the potential applications, limitations, and strategies for using ChatGPT.
The Medical Student Research Journal is catalogued with an ISSN: 2159-3647. 11. How do you cite an article from the Medical Student Research Journal? Kabadi CJ, Smith III CR, Gomez F. Potential Pathogen Transmission on Medical Student Anatomy Laboratory Clothing. Medical Student Research Journal. 2013;2(Spring):30-35.