REVIEW article
Obesity: epidemiology, pathophysiology, and therapeutics.

- Department of Endocrinology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
Obesity is a complex multifactorial disease that accumulated excess body fat leads to negative effects on health. Obesity continues to accelerate resulting in an unprecedented epidemic that shows no significant signs of slowing down any time soon. Raised body mass index (BMI) is a risk factor for noncommunicable diseases such as diabetes, cardiovascular diseases, and musculoskeletal disorders, resulting in dramatic decrease of life quality and expectancy. The main cause of obesity is long-term energy imbalance between consumed calories and expended calories. Here, we explore the biological mechanisms of obesity with the aim of providing actionable treatment strategies to achieve a healthy body weight from nature to nurture. This review summarizes the global trends in obesity with a special focus on the pathogenesis of obesity from genetic factors to epigenetic factors, from social environmental factors to microenvironment factors. Against this background, we discuss several possible intervention strategies to minimize BMI.
There has been a significant global increase in obesity rate during the last 50 years. Obesity is defined as when a person has a body mass index [BMI (kg/m 2 ), dividing a person’s weight by the square of their height] greater than or equal to 30, overweight is defined as a BMI of 25.0-29.9. Being overweight or obesity is linked with more deaths than being underweight and is a more common global occurrence than being underweight. This is a global phenomenon occurring in every region except parts of sub-Saharan Asia and Africa ( 1 ), and also countries with low obesity rates (i.e., Sri Lanka, Indonesia, Sudan, Singapore, Djibouti, etc.) ( 2 ).
Obesity increases the likelihood of various diseases and conditions which are linked to increased mortality. These include Type 2 diabetes mellitus (T2DM), cardiovascular diseases (CVD), metabolic syndrome (MetS), chronic kidney disease (CKD), hyperlipidemia, hypertension, nonalcoholic fatty liver disease (NAFLD), certain types of cancer, obstructive sleep apnea, osteoarthritis, and depression ( 3 ).Treating these conditions can place an additional load on healthcare systems: for example, it is estimated that obese have a 30% higher medical cost than those with a normal BMI ( 4 ). As related total health-care costs double every decade, treating the consequences of obesity poses an expensive challenge for patients ( 5 ).
There are several possible mechanisms leading to obesity. Actually, the traditional view is usually that the main cause is the significantly more excess energy stored than the energy the body used. The excess energy is stored in fat cells, thereby developing the characteristic obesity pathology. The pathologic enlargement of fat cells will alter the nutrient signals responsible for obesity ( 6 ).However, the latest research showed that the food sources and quality of nutrients matter more than their quantities in the diet for weight control, and also for disease prevention ( 7 ). More and more etiologies or defects that lead to obesity can be identified under the background of struggle between nurture and nature, genetic and epigenetic, environmental and microenvironment. We are increasingly understanding how food cravings are upregulated in obesity individuals’ brains, how gut hormones, adipose tissue, or gut microbiota regulate appetite and satiety in the hypothalamus, as well as the roles of gut dysbiosis played in obesity development and how dysfunction of glucose and lipids metabolism causes secondary health problems ( 8 ). In addition, genetic factors are known to play critical roles in determining an individual’s predisposition to weight gain ( 9 ). Recent epigenetic studies have provided very useful tools for understanding the worldwide increase in obesity ( 10 ). Studies have discussed the relationships between genetics, epigenetics, and environment in obesity and explored the roles of epigenetic factors in metabolism regulation and obesity risk as well as its complications ( 11 ).
The field of obesity is rapidly evolving as an abundance of new scientific data continue to emerge. Herein, we discuss the epidemiology of obesity, covering the pathophysiology, pathogenesis, genetics, epigenetics, and environmental (macro and micro) causes that result in obesity. We end by summarizing possible management and prevention strategies.

Epidemiology of Obesity
BMI is used to define and diagnose obesity according to World Health Organization (WHO) guidelines ( 4 ). In adults, WHO defines ‘overweight’ as a BMI of 25.0 to 29.9 and ‘obese’ as a BMI ≥ 30.0. Obesity is further classified into three severity levels: class I (BMI 30.0-34.9), class II (BMI 35.0-39.9) and class III (BMI ≥ 40.0) ( 12 ).However, large individual differences exist in the percent body fat for the given BMI value, which can be attributed to sex, ethnicity and age ( 13 ).Excess fat deposition in the abdominal region is termed ‘abdominal obesity’ and is associated with greater health risks ( 14 ).The definition and measurement guidelines of abdominal obesity differed from WHO, IDF (International Diabetes Federation) to AHA (American Heart Association) ( 15 ). However, there is no international standard suitable for all countries or regions.
The prevalence of excessive weight gain has doubled worldwide since 1980, and about a third of the global population has been determined to be obese or overweight ( 16 ). Obesity rate has dramatically enhanced in both male and female, and across all ages, with proportionally higher prevalence in older persons and women ( 4 ). While this trend is present globally, absolute prevalence rates vary across regions, countries, and ethnicities. The prevalence of obesity also varies with socioeconomic status, with slower rates of BMI increase in high-income and some middle-income countries. While obesity was once considered a problem of high-income countries, the incidence rates of obese or overweight children in high-income countries, including the United States, Sweden, Denmark, Norway, France, Australia and Japan, have decreased or plateaued since the early 2000s ( 17 ).
In low- and middle-income countries, rates of overweight and obesity are rising especially in urban areas. In China, one study based on 12,543 participants monitored over 22 years revealed that the prevalence of age-adjusted obesity rose from 2.15% to 13.99% in both sexes, going from 2.78 to 13.22% in female and from 1.46 to 14.99% in male, respectively ( 18 , 19 ). The overweight rate of African children under 5 years old has increased by 24% since 2000. As of 2019, almost half of the Asian children under 5 years old were obese or overweight ( 20 ). WHO datasets from sub-Sarahan Africa reveal that prevalence of overweight and obese in adults and stunting, underweight, and wasting in children are inversely associated ( 21 ).
Pathogenesis of Obesity
The pathogenesis of obesity involves regulation of calorie utilization, appetite, and physical activity, but have complex interactions with availability of health-care systems, the role of socio-economic status, and underlying hereditary and environmental factors.
Food Intake and Energy Balance
The essential causes of obesity remain somewhat controversial. Current health recommendations to manage obesity are based on the underlying physiological property that fat accumulation is driven by an energy imbalance between consumed and expended calories. The obesity epidemic has been fueled in large part by increased energy from greater availability of highly rewarding and energy-dense food. Diet and various social, economic, and environmental factors related to food supply have a significant effect on patient’s ability to achieve the balance ( 22 ). In a 13-year follow-up study on 3,000 young, those who consumed much more fast-food were found to weigh an average of ~6kg more and have larger waist circumferences than those with the lowest fast-food-intake. They were also found to have higher incidences of negative weight-related health issues, such as elevated triglycerides and twice the odds of developing MetS ( 23 ). These issues are compounded in certain individuals that possess a genetic susceptibility to fat accumulation, which may be caused by significant interactions between homeostatic circuits and brain reward. Accumulation of lipid metabolites, inflammatory signaling, or other hypothalamic neuron impairing mechanisms may also lead to obesity, which might explain the biological defense of elevated body fat mass ( 24 ).
Obesogenic marketing to promote beverages or foods that are high in sugar and fat negatively modulates human behavior. Such advertisements may increase preference for energy-dense foods and beverages ( 25 ). Analysis showed that African American programs had more food advertisements than other general market programs. More food advertisements were for meat, candy, soda, and fast food than for grains, pasta, cereals, vegetables, and fruits. Advertised products were designed to be cheap, have a long shelf-life, and taste ‘irresistible’. This applies particularly to high-fat, high-sugar junk foods that can stimulate the brain reward centers, the same part of the brain that’s stimulated by cocaine, heroin, and other addictive drugs, that is, these products are specifically engineered to be addictive ( 25 ). The brain reward offers a plausible mechanism to explain the elevated body fat mass, however, it seems that only certain individuals present this characteristic according to this theory.
For clinicians, a systematic evaluation of patient health factors affecting energy intake, metabolism, and expenditure is required for effective management of obesity. However, attempting to manage obesity through behavioral alterations aiming at addressing these three factors is more often than not unsuccessful. This suggests that our understanding of energy management and the interactions between intake, metabolism, and expenditure are not yet fully understood ( 26 ).
Family History and Lifestyle
Family history, lifestyle, and psychological factors all function in propensity for obesity. The likelihood of becoming obese can be affected by nature and nurture, enhanced by family genetics (propensity to accumulate fat) ( 27 ) or life style (poor dietary or exercise habits) ( 28 ). A child with one obese parent has a three-time risk to become obese as an adult, while when a child’s parents are both obese, this child has a 10-fold risk of future obesity. A cross-sectional observational study of 260 children (139 female, 121 male, aged 2.4 and 17.2 years) demonstrated that the family history of cardiometabolic diseases and obesity are critical risk factors for severity of obesity in childhood ( 29 ).
A prospective survey of 3148 school boys (aged six to ten years) in Ariana highlighted several child obesity risk factors, including parental obesity of parents, the snacks between meals especially after the dinner, lack of sleep (< 8 hours), and daily consumption of juice, sparkling drink, sweets, and sugary foods ( 30 ). Two studies of mother-child pairs in the United States found that the healthy lifestyle of mothers during the childhood and adolescence of their offspring was closely associated with a significantly reduced risk of obesity in their children ( 31 ). These results underscore the benefits of intervening at the family- or parental-level to reduce the risk of obesity in children ( 31 ).
However, parents are not the sole instigators of childhood obesity. For example, in the United States, physical education was used as a regular part of a public education curriculum ( 32 ). Starting 2011 physical education programs were curtailed such that 25 percent of students could achieve four out of five the national standards of at least 225 minutes weekly at the senior school levels and at least 150 minutes weekly at the primary level ( 33 ). Other factors that may have resulted in the decline of physical activity in children include increasing time spent on video game consoles and mobile devices at a reduction of time spent actively or outdoors. It is hard to argue against technological progress, but based on these studies, such innovations may be taking a toll on children’s health ( 34 ).
Microenvironment and Gut Microbiome
Our knowledge of the intestinal microbiome has grown substantially over recent years, as has our understanding of its intricate relationship to disease. For example, obesity is involved in an altered gut microenvironment that supports more diverse viral species than found in leaner hosts ( 35 ). This environment is more susceptible to the generation of pathogenic variants that can induce more serious disease ( 36 ). Increasing evidence shows that variations of gut microbiome cause alterations in host weight and metabolism. For example, compared with those with normal gut microbiota, germ-free male mice (without gut microflora) had 42% less total body fat, even while consuming 29% more food a day. However, after cecal microbe colonization, the total body fat of these mice increased 57%in, lean body mass decreased 7%, and daily food intake decreased 27% ( 35 ). A follow-up study suggested that these alterations resulted from decreased metabolic rates, with concomitant increased adipose tissue deposition, as capillary density in distal small intestinal villi increased 25% after microflora colonization. Similar results were also observed from female mice ( 37 ).
The human body contains around 3.8 × 10 13 microorganisms and the majority of them occupy the gastrointestinal tract. Over half of the microbial population are bacteria, followed by Archaea and Eukarya ( 38 ). The diversity of healthy gut microbiome allows for functional redundancy, in which multiple microbes can perform similar functions. Normally, gut microbiota have substantial beneficial roles in the host, including involvement in metabolism of carbohydrate and lipid, synthesis of vitamins and amino acids, epithelial cell proliferation, protection against pathogens, and hormone modulation. Gut bacteria can also break down indigestible molecules such as human milk oligosaccharides and plant polysaccharides ( 39 ). Imbalance of microbial populations (‘dysbiosis’) has been show to associate with a wide range of diseases including neurological disorders, inflammatory bowel disease, malnutrition, cancer, diabetes, and obesity ( 40 ). Recent research suggests that caloric restriction can beneficially reshape the gut microbiome and that antibiotic use can negatively harm gut microflora in ways that result in diabetes and obesity. Human studies support findings that microbiome alterations are associated with obesity; however, the exact mechanisms (i.e., ratios and amounts of microflora diversity) are still unknown ( 41 ).
Gut microbiota are central players in the host immune system. Disturbances in gut microflora can lead to inflammation of the intestinal lining ( 42 ). This response has been demonstrated to be mediated by TLRs (toll-like receptors), which identify and attack host microbes. For example, TLR4 recognizes the bacterial LPS (lipopolysaccharides) in the cell walls of Gram-negative bacteria while TLR5 recognizes bacterial flagellin. The body mass of TLR5-knockout mice increased 20% and their epididymal fat pad size increased 100% when compared to the wild-type controls ( 43 ). The dietary fiber and starch fermentation in lower gastrointestinal tract induced by microbiome can also produce SCFAs (Short-chain fatty acids), which can regulate production of gut hormone such as peptide YY (PYY) in the intestinal epithelium and GLP-1, GLP-2 (glucagon-like peptides), and the secretion of gastric inhibitory peptides by K cells ( 44 ). In obese patients, enzymes participated in or glucose signaling pathways are downregulated. It may be that alterations in specific microbial populations are more important than overall phylogenetic ratios, resulting in alterations in enzymes and SCFAs production, which further influence regulation of insulin and glucose, ultimately leading to development of obesity ( 41 ).
Genetic Factors and Causes
The studies from family and twin studies showed that around 40-70% of the obesity variation in human are resulted from genetic factors ( 45 ). While during the last 20 years, environmental alterations have increased obesity rates, the genetic factors play key roles in development of obesity ( 46 ). GWAS (Genome-wide association scans) approaches have identified over 400 genes associated with T2DM ( 47 , 48 ), however, these genes only predict 5% of obesity risk ( 49 ). The low predictive power may be due to the situation that gene-gene, gene-environment, and epigenetic interactions have not been thoroughly identified using the current methods based on population genetics ( 50 ). Many obesity -associated genes have been identified to be involved in energy homeostasis regulating pathways.
Genetic causes of obesity can be broadly classified as: 1) monogenic causes that result from a single gene mutation, primarily located in the leptin- melanocortin pathway. Many of the genes, such as AgRP (Agouti-related peptide), PYY (orexogenic), or MC4R (the melanocortin-4 receptor), were identified for monogenic obesity disrupt the regulatory system of appetite and weight, hormonal signals (ghrelin, leptin, insulin) are sensed by the receptors located in the arcuate nucleus of the hypothalamus ( 51 ). 2) Syndromic obesity were severe obesity results from neurodevelopmental abnormalities and other organ/system malformations. This may be caused by alterations in a single gene or a larger chromosomal region encompassing several genes ( 52 ). 3) Polygenic obesity is caused by cumulative contribution of many genes. Further, some people with obesity gain excess weight due to the multiple genes they have ( 53 ), and these genes make them to favor food and thereby have a higher caloric intake. The presence of these types of genes can cause increased caloric intake, increased hunger levels, reduced control overeating, reduced satiety, increased tendency to store body fat, and increased tendency to be sedentary ( 54 ).
Rare single-gene defects are associated with high level of hunger and can cause dramatic obesity in young children. Those individuals with severe obesity developed before two years old should consult obesity medicine specialists and consider to be involved in screening for MC4R Deficiency, leptin deficiency, and POMC deficiency ( 55 ). Leptin deficiency can cause diet-induced obesity and metabolic dysregulation. About 50% of female with polymorphism came up with binge eating ( 56 ). The MC4R polymorphism influences the release of ghrelin ( 57 ). The chromosome 2p22 (a region encompassing the POMC gene) has been identified as the site of gene(s) affecting obesity and obesity-related traits ( 58 ). These studies suggest that childhood obesity should be considered in the light of both environmental context and genetic heritage ( 59 ).
There are several genetic, neuroendocrine, and chromosomal precursors that can result in obesity. PWS (Prader-Willi Syndrome) is a neurodevelopmental disorder with hypothalamic dysfunction, due to the deficiency of imprinted genes ( 60 ). Endocrine disorders such as PCOS (Polycystic Ovary Syndrome) can also lead to increased body fat ( 61 ). Chromosomal defects can lead to obesity, including deletion of 16p11.2, 2q37 (brachydactyly mental retardation syndrome; BDMR), 1p36 (monosomy 1p36 syndrome), 9q34 (Kleefstra syndrome), 6q16 (PWS-like syndrome), 17p11.2 (Smith Magenis syndrome; SMS), and 11p13 (WAGR syndrome) ( 62 ). These conditions rely on the conventional current health recommendations that energy imbalance between calories consumed and expended is the key cause of obesity and present circumstances under which traditional weight management methods may not help.
Epigenetic Modification
We have been able to identify some of the genes that contribute to monogenic forms of obesity, but the human genome alterations on timescales that are too long for the genome to be a major player in the current obesity pandemic. Epigenetics, however, may offer a logical explanation for increasing obesity prevalence over the past few decades without necessitating a radical change in the genome ( 63 ). In multicellular organisms, the genetic code is homogenous throughout the body, but the expression of code can vary across cell types. Epigenetics studies showed that the heritable regulatory alterations in the genetic expression do not require alterations in the nucleotide sequence ( 64 ). Epigenetic modifications can be thought of as the differential packaging of the DNA that either allows or silences the expression of certain genes across tissues. Environmental and gut microbiota can influence the epigenetic programming of parental gametes, or programming in later stages of life ( 10 ).
The known epigenetic mechanisms include DNA methylation, histone modifications, and miRNA-mediated regulation. These can be passed from one generation to another meiotically or mitotically. There is evidence showing that the perinatal and embryo-fetal development period plays a critical role in human tissues and organs programming ( 65 ). DNA methylation appears to be the most important epigenetic mechanism for regulating gene expression. Alterations in DNA methylation can be a hallmark of many diseases such as cancers ( 66 ). LEP (Leptin) plays critical roles in adipose tissue regulation. The maternal metabolic status can affect DNA methylation of LEP profile at birth, affecting metabolic remodeling of obesity ( 67 ). The Adiponectin (ADIPOQ) epigenetic status also has relationship with obesity, and association has been reported between LDL-cholesterol levels and DNA methylation of both LEP and ADIPOQ ( 68 ). Paternal obesity has also been associated with inhibited methylation levels in IGF2 (insulin-like growth factor 2) regions, which promote the division and growth of various types of cells ( 69 ). Other genes investigated in the context of metabolism and obesity include: tumor necrosis factor (TNF), hypoxia-inducible factor 3a (HIF3A), neuropeptide Y (NPY), insulin receptor substrate 1 (IRS1), mitochondrial transcription factor A (TFAM), interleukin 6 (IL6), lymphocyte antigen 86 (LY86) and glucose transport 4 (GLUT4) ( 10 , 63 ).
Histones are proteins function in DNA packaging and modifications to histones are associated with epigenetic regulation of adipogenesis and obesity development ( 70 ). Five key regulatory genes in adipogenesis, CCAAT-enhancer-binding protein β (C/EBP β), pre-adipocyte factor-1 (Pref-1), adipocyte protein 2 (aP2), PPARγ, and C/EBPα, are modulated by histone modifications during adipocyte differentiation ( 71 ). The enzymes play roles in histone modification also function in obesity. They also regulate the expression of HDACs (histone deacetylases), which participated in the epigenetic control of gene expression involved in a large amount of environmental factors ( 72 ).
MicroRNAs (miRNAs) are 18 to 25 nucleotides long short noncoding RNA sequences that can regulate gene expression by gene silencing and post-transcriptional alterations. MicroRNAs function in a variety of biological processes, including adipocyte differentiation and proliferation, and are associated with low-grade inflammation and insulin resistance displayed in obese individuals ( 73 ). Increased levels of miRNAs including miR-486-3p, miR-142-3p, miR-486-5p, miR-423-5p and miR-130b were seen in children with high BMI values, among which 10 miRNAs exhibited significant alterations with increasing body weight ( 74 ). Zhao et al. identified miRNA as a signature for weight gain and showed that the individuals with a high-risk score for 8 of these miRNAs had over 3-fold higher odds of weight gain ( 75 ). Alterations in adipocyte-derived exosomal miRNAs is also seen following weight loss and decrease in insulin resistance after gastric bypass ( 76 ). miRNAs have been shown to play a key role in obesity and that the associated metabolic alterations can serve as biomarkers, or potentially therapeutic targets for intervention. Consideration of genetic and epigenetic causes of obesity provide valuable tools for the clinical treatment of obesity.
Therapeutics of Obesity
Lifestyle modifications.
Given the lack of specific pharmacological interventions, ‘lifestyle modification’ remains the cornerstone of obesity management ( 4 ). Individuals with obesity are suggested to lose at least 10% body weight via combination of diet, physical activity, and behavior therapy (or lifestyle modification) ( 77 ). Significant short-term weight loss can be achieved by consumption of portion-controlled diets ( 78 ). Long-term weight control can be achieved via high levels of physical activity and continued patient–practitioner contact. In many cases, lifestyle modification results in dramatic loss of body weight, leading to significant reduction of cardiovascular risk ( 79 ).
Since food choices are mainly determined by peoples’ surroundings, it is imperative that governments improve policies and environment to reduce the availability of unhealthful foods and make healthy foods more accessible. Policies should be changed to increase development of foods with reduced sugar, fat, and salt and decrease availability of obesogenic foods aimed at children ( 80 ). Policy makers and Practitioners must be made aware of the potential impact of food advertisements on human health and behavior and should encourage food manufacturers to create and promote weight-friendly foods. Nutrition educators should help teach how to evaluate food advertisements ( 81 ). Interventions aimed at motivating behavioral alterations (e.g., health promotion, nutrition education, incentives for healthy living, sugar-sweetened beverage tax, and social marketing) and enforcing actions that reduce causes of obesity (e.g., policy changes, regulations and laws) are likely to have strong impacts on reducing the obesity crisis ( 82 ).
Anti-Obesity Medications
Pharmacotherapy is recommended for those whose BMI ≥30 (or a BMI ≥27 with comorbid conditions) and are unable to lose weight using lifestyle modification alone ( 83 ). The U.S. FDA (Food and Drug Administration) approved some new pharmacotherapy drugs for short-term obesity treatment ( Table 1 ) and since Lorcaserin was withdrawn, there are only four [Naltrexone-Bupropion (Contrave), Orlistat (Xenical, Alli), Liraglutide (Saxenda) and Phentermine-Topiramate (Qsymia)] approved in addition to Gelesis which is now the fifth, have been approved for long-term use ( 84 , 86 , 87 ). The FDA also approved the MC4R agonist-Setmelanotide for use in individuals with severe obesity due to either POMC, PCSK1 (proprotein convertase subtilisin/kexin type 1), or LEPR (leptin receptor) deficiency at the end of 2020 ( 85 ).
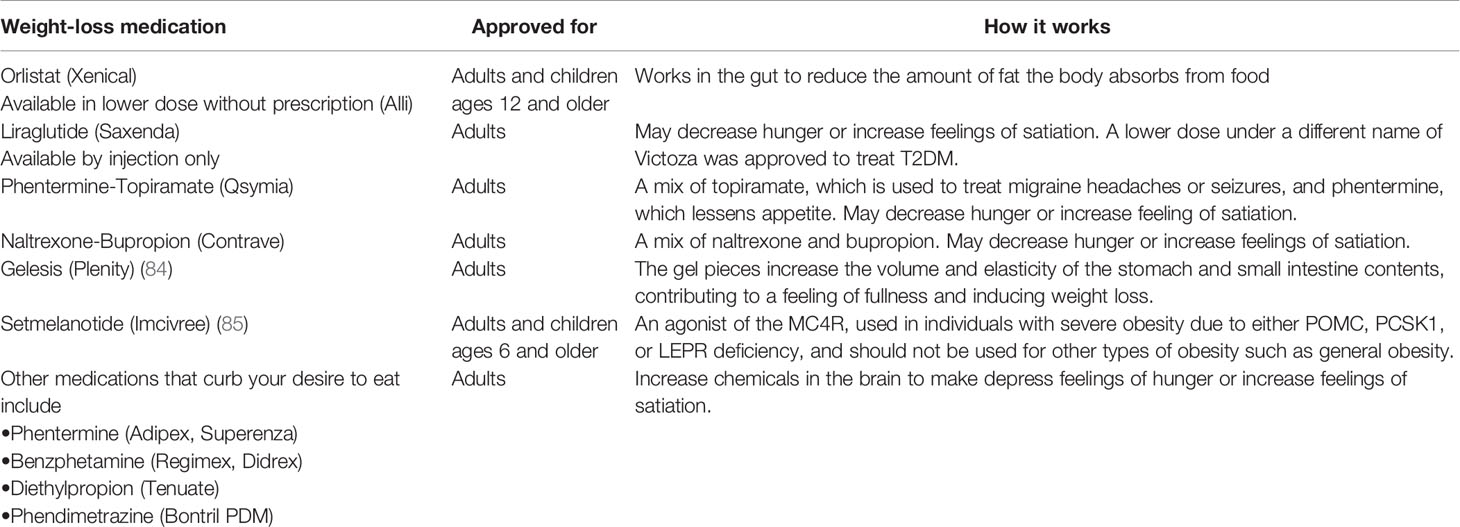
Table 1 Prescription medications approved for obesity treatment.
In addition, 11 different components have been identified from 54 families of the plants to have anti-obesity potential. These families include Celastraceae, Zingiberaceae, Theaceae, Magnoliaceae, and Solanaceae ( 88 ). Traditional Chinese medicine delivers unique solutions to treat obesity, such as regulating fat metabolism, enhancing hormone level, regulating intestinal microflora, among other pathways ( 89 ). These findings are helpful for selection of herbal medicine or traditional Chinese medicine for further research.
Bariatric Surgery
For individuals with a BMI > 40 or BMI > 35 with comorbidities who are unable to lose weight by lifestyle modifications or pharmacotherapy bariatric surgery or weight loss surgery is another option ( 83 ). Standard bariatric operations, including BPD (Bilio-pancreatic diversion), SG (sleeve gastrectomy), RYGB (Roux-en-Y gastric bypass), and AGB (adjustable gastric banding), benefits individuals׳ metabolic profiles to varying degrees ( 90 ). Studies reported that the benefits of bariatric surgery go beyond just losing weight. Bariatric surgery reduces chronic inflammation involved in obesity and alters biomarkers, the gut microbiota, and long-term remission for T2DM ( 91 – 93 ). Take RYGB for example, in human subjects, overall gut microbial richness increased after RYGB surgery ( 94 ). Further analysis revealed RYGB contributed to increase of expression of some specific white adipose tissue genes, upregulation of genes central to the transforming growth factor-β signaling pathway, and remarkable downregulation of genes involved in metabolic pathways and inflammatory responses ( 95 ). Decrease of serum leptin levels, which are associated with leaned BMI, typically results from bariatric surgery. Interestingly, those women who had a higher presurgical baseline leptin level were easier to remain the post-procedure weight loss, while those with a lower presurgical baseline level were easier to regain the weight. There is a correlation between the baseline leptin level and alterations in body mass, BMI, as well as total weight loss although the success degree of surgery cannot be predicted by a patient’s serum leptin level ( 96 ).
Fecal Microbiota Transplantation
FMT has attracted considerable research interest recently in the treatment of obesity ( 97 ). There are promising indications that FMT of microbes from healthy individuals into patients with obesity may be affected in weight loss and maintenance. In a groundbreaking key study, Ridaura et al. transplanted fecal slurries from human twins discordant for obesity into germ-free mice ( 98 ). The mice with obese individuals’ microbiota successfully developed obesity, while those with healthy individuals’ microbiota remained lean. The sequencing results of mice post-procedure stool samples showed that the human microbiomes were successfully infused, indicative of the transfer of functions related to the obese or lean microbial communities, respectively ( 98 ). Promising studies in humans are also being attempted: Vrieze et al. were able to improve microbial diversity and insulin sensitivity in obese, diabetic adult males after the transplantation with the taxa from lean donors ( 99 ). An increase was observed in butyrate-producing bacteria and Bacteroidetes, indicative of a shift toward a leaner phenotype related microbial community. While in early stages, FMT may be an option for replacing obesogenic microbial communities ( 100 ).
Summary and Conclusions
The global prevalence of obesity has nearly tripled since 1975 and continues to grow at an exponential rate. Obesity has become the number one lifestyle-related risk factor for premature death. As such, public health policies focused on reducing and treating obesity must be developed ( 17 ). The WHO “Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013-2020” defines strategies to prevent further increase in obesity prevalence, but progress so far has been slow ( 101 ). However, with the identification of the main obesity causes the modulating factors, the challenge remains is to translate them into effective actions.
Epigenetic modifications and interactions between our genes and environment have strong influences on human health and disease. Increasing evidence is revealing the involvement of epigenetics in obesity prevalence ( 9 ). Propensity for obesity can result from the effects of environmental factors, such as nutrition and lifestyle to the epigenetic remodeling of the early postnatal development, and parental gametes. Epigenetic marks could also significantly affect the obesity risk of the child and thus be transmitted trans-generationally ( 11 ). This epigenetic ‘memory’ may help explain our lack of evidence for genetic heritability in obesity and other diseases. A foundational knowledge of the mechanisms of epigenetic inheritance is of great importance for treating and preventing obesity. Exploration of epigenetic changes is a key for predicting disease trajectories and choosing effective treatment. The reversible characteristic of these modifications makes them ideal targets for epigenetic treatment, and promising “epigenetic drugs” for therapies of obesity are already in the marketplace or in various stages of development ( 102 ). These types of therapies include DNA methyltransferase inhibitors (DNMTis), protein arginine methyltransferase inhibitors (PRMTis), histone acetyltransferase inhibitors (HATi), histone deacetylase inhibitors (HDACi), sirtuin-activating compounds (STACs) and histone demethylating inhibitors (HDMis) ( 103 ).
Microbiome research holds much promise for treating pandemics such as obesity and diabetes. On-going developments in technology and bioinformatics of microbiology are increasingly allowing for the development of a microbiome-manipulating capsule to favor a healthy, lean, and insulin-sensitive profile, but this is still an area of active research ( 8 , 104 ). More targeted therapies will also become possible as we increase our understanding of microbial metabolites, allowing for clinal treatment of inflammation, weight gain and insulin resistance, and ultimately preventing the progression to obesity.
In conclusion, improved understanding of the various dimension of obesity, including propensity to regain lost weight, interindividual differences in pathogenesis, and response to therapy, is needed for developing effective as well as cost-effective interventions. The insights will in turn benefit the related health complications such as incidence of diabetes. More research is required to identify behavioral modification that are effective and available to people from diverse backgrounds. More studies were performed to develop more effective and safer medications to help obese people lose body weight and maintain a healthy weight for long term. Moreover, we must devote greater efforts and resources to the prevention of obesity in children as well as adults. Prevention is a key as treatment alone is not very effective and cannot well reverse the epidemic of obesity for long term.
Author Contributions
HL and XL conceived and wrote the manuscript. All authors contributed to the article and approved the submitted version.
This project was funded by grants from the Zhejiang Provincial Medical Science and Technology Program (2020KY166).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Al Kibria GM. Prevalence and Factors Affecting Underweight, Overweight and Obesity Using Asian and World Health Organization Cutoffs Among Adults in Nepal: Analysis of the Demographic and Health Survey 2016. Obes Res Clin Pract (2019) 13(2):129–36. doi: 10.1016/j.orcp.2019.01.006
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Mbogori T, Kimmel K, Zhang M, Kandiah J, Wang Y. Nutrition Transition and Double Burden of Malnutrition in Africa: A Case Study of Four Selected Countries With Different Social Economic Development. AIMS Public Health (2020) 7:425–39. doi: 10.3934/publichealth.2020035
3. Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The Global Obesity Pandemic: Shaped by Global Drivers and Local Environments. Lancet (2011) 378(9793):804–14. doi: 10.1016/S0140-6736(11)60813-1
4. WHO Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. World Health Organ Tech Rep Ser (2000) 894:i–xii, 1-253.
PubMed Abstract | Google Scholar
5. Bray GA, Kim KK, Wilding J, World Obesity Federation. Obesity: A Chronic Relapsing Progressive Disease Process. A Position Statement of the World Obesity Federation. Obes Rev (2017) 18(7):715–23.doi: 10.1111/obr.12551
6. Lee SJ, Shin SW. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med (2017) 376(15):1491–2. doi: 10.1056/NEJMc1701944
7. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of Weight-Loss Diets With Different Compositions of Fat, Protein, and Carbohydrates. N Engl J Med (2009) 360(9):859–73. doi: 10.1056/NEJMoa0804748
8. Singer-Englar T, Barlow G, Mathur R. Obesity, Diabetes, and the Gut Microbiome: An Updated Review. Expert Rev Gastroenterol Hepatol (2019) 13(1):3–15. doi: 10.1080/17474124.2019.1543023
9. Singh RK, Kumar P, Mahalingam K. Molecular Genetics of Human Obesity: A Comprehensive Review. C R Biol (2017) 340(2):87–108. doi: 10.1016/j.crvi.2016.11.007
10. Lopomo A, Burgio E, Migliore L. Epigenetics of Obesity. Prog Mol Biol Transl Sci (2016) 140:151–84. doi: 10.1016/bs.pmbts.2016.02.002
11. Dubern B. Genetics and Epigenetics of Obesity: Keys to Understand. Rev Prat (2019) 69(9):1016–9.
12. Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss. Arterioscler Thromb Vasc Biol (2006) 26(5):968–76. doi: 10.1161/01.ATV.0000216787.85457.f3
13. Kok P, Seidell JC, Meinders AE. [The Value and Limitations of the Body Mass Index (BMI) in the Assessment of the Health Risks of Overweight and Obesity]. Ned Tijdschr Geneeskd (2004) 148(48):2379–82.
14. Løvsletten O, Jacobsen BK, Grimsgaard S, Njølstad I, Wilsgaard T, Løchen ML, et al. Prevalence of General and Abdominal Obesity in 2015-2016 and 8-Year Longitudinal Weight and Waist Circumference Changes in Adults and Elderly: The Tromsø Study. BMJ Open (2020) 10(11):e038465. doi: 10.1136/bmjopen-2020-038465
15. Paley CA, Johnson MI. Abdominal Obesity and Metabolic Syndrome: Exercise as Medicine. BMC Sports Sci Med Rehabil (2018) 10:7. doi: 10.1186/s13102-018-0097-1
16. Ataey A, Jafarvand E, Adham D, Moradi-Asl E. The Relationship Between Obesity, Overweight, and the Human Development Index in World Health Organization Eastern Mediterranean Region Countries. J Prev Med Public Health (2020) 53(2):98–105. doi: 10.3961/jpmph.19.100
17. NCD Risk Factor Collaboration (NCD-RisC). Worldwide Trends in Body-Mass Index, Underweight, Overweight, and Obesity From 1975 to 2016: A Pooled Analysis of 2416 Population-Based Measurement Studies in 128·9 Million Children, Adolescents, and Adults. Lancet (2017) 390(10113):2627–42. doi: 10.1016/S0140-6736(17)32129-3
18. Chen Y, Peng Q, Yang Y, Zheng S, Wang Y, Lu W. The Prevalence and Increasing Trends of Overweight, General Obesity, and Abdominal Obesity Among Chinese Adults: A Repeated Cross-Sectional Study. BMC Public Health (2019) 19(1):1293. doi: 10.1186/s12889-019-7633-0
19. Jia W. Obesity in China: Its Characteristics, Diagnostic Criteria, and Implications. Front Med (2015) 9(2):129–33. doi: 10.1007/s11684-015-0387-x
20. Wariri O, Alhassan J, Mark G, Adesiyan O, Hanson L. Trends in Obesity by Socioeconomic Status Among non-Pregnant Women Aged 15-49 Y: A Cross-Sectional, Multi-Dimensional Equity Analysis of Demographic and Health Surveys in 11 Sub-Saharan Africa Countries, 1994-2015. Int Health (2020) 0:1–10. doi: 10.1093/inthealth/ihaa093
CrossRef Full Text | Google Scholar
21. Tydeman-Edwards R, Van Rooyen FC, Walsh CM. Obesity, Undernutrition and the Double Burden of Malnutrition in the Urban and Rural Southern Free State, South Africa. Heliyon (2018) 4(12):e00983. doi: 10.1016/j.heliyon.2018.e00983
22. Yoo S. Dynamic Energy Balance and Obesity Prevention. J Obes Metab Syndr (2018) 27(4):203–12. doi: 10.7570/jomes.2018.27.4.203
23. Duffey KJ, Gordon-Larsen P, Jacobs DR Jr, Williams OD, Popkin BM. Differential Associations of Fast Food and Restaurant Food Consumption With 3-Y Change in Body Mass Index: The Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr (2007) 85(1):201–8. doi: 10.1093/ajcn/85.1.201
24. Obri A, Claret M. The Role of Epigenetics in Hypothalamic Energy Balance Control: Implications for Obesity. Cell Stress (2019) 3(7):208–20. doi: 10.15698/cst2019.07.191
25. Sadeghirad B, Duhaney T, Motaghipisheh S, Campbell NR, Johnston BC. Influence of Unhealthy Food and Beverage Marketing on Children's Dietary Intake and Preference: A Systematic Review and Meta-Analysis of Randomized Trials. Obes Rev (2016) 17(10):945–59. doi: 10.1111/obr.12445
26. Willett WC, Leibel RL. Dietary Fat Is Not a Major Determinant of Body Fat. Am J Med (2002) 113(Suppl 9B):47S–59S. doi: 10.1016/S0002-9343(01)00992-5
27. Fitzgerald MP, Hennigan K, O'Gorman CS, McCarron L. Obesity, Diet and Lifestyle in 9-Year-Old Children With Parentally Reported Chronic Diseases: Findings From the Growing Up in Ireland Longitudinal Child Cohort Study. Ir J Med Sci (2019) 188(1):29–34. doi: 10.1007/s11845-018-1814-1
28. Romero-Ibarguengoitia ME, Vadillo-Ortega F, Caballero AE, Ibarra-González I, Herrera-Rosas A, Serratos-Canales MF, et al. Family History and Obesity in Youth, Their Effect on Acylcarnitine/Aminoacids Metabolomics and Non-Alcoholic Fatty Liver Disease (NAFLD). Structural Equation Modeling Approach. PloS One (2018) 13(2):e0193138. doi: 10.1371/journal.pone.0193138
29. Corica D, Aversa T, Valenzise M, Messina MF, Alibrandi A, De Luca F, et al. Does Family History of Obesity, Cardiovascular, and Metabolic Diseases Influence Onset and Severity of Childhood Obesity. Front Endocrinol (Lausanne) (2018) 9:187. doi: 10.3389/fendo.2018.00187
30. Ben Slama F, Achour A, Belhadj O, Hsairi M, Oueslati M, Achour N. [Obesity and Life Style in a Population of Male School Children Aged 6 to 10 Years in Ariana (Tunisia)]. Tunis Med (2002) 80(9):542–7.
31. Dhana K, Haines J, Liu G, Zhang C, Wang X, Field AE, et al. Association Between Maternal Adherence to Healthy Lifestyle Practices and Risk of Obesity in Offspring: Results From Two Prospective Cohort Studies of Mother-Child Pairs in the United States. BMJ (2018) 362:k2486. doi: 10.1136/bmj.k2486
32. Mulligan EP, Rauh MJ, Heiderscheit B, Jenkins WL. Sports Physical Therapy Education in the United States: Where Do We Go From Here? A Survey of American Academy of Sports Physical Therapy Members. J Allied Health (2020) 49:e79–79e87.
33. Beets MW, Wallner M, Beighle A. Defining Standards and Policies for Promoting Physical Activity in Afterschool Programs. J Sch Health (2010) 80:411–7. doi: 10.1111/j.1746-1561.2010.00521.x
34. Salam RA, Padhani ZA, Das JK, Shaikh AY, Hoodbhoy Z, Jeelani S, et al. Effects of Lifestyle Modification Interventions to Prevent and Manage Child and Adolescent Obesity: A Systematic Review and Meta-Analysis. Nutrients (2020) 12(8):2208. doi: 10.3390/nu12082208
35. Bäckhed F, Ding H, Wang T, Hooper LV, Koh GY, Nagy A, et al. The Gut Microbiota as an Environmental Factor That Regulates Fat Storage. Proc Natl Acad Sci USA (2004) 101(44):15718–23. doi: 10.1073/pnas.0407076101
36. Honce R, Karlsson EA, Wohlgemuth N, Estrada LD, Meliopoulos VA, Yao J, et al. Obesity-Related Microenvironment Promotes Emergence of Virulent Influenza Virus Strains. mBio (2020) 11(2):e03341–19. doi: 10.1128/mBio.03341-19
37. Stappenbeck TS, Hooper LV, Gordon JI. Developmental Regulation of Intestinal Angiogenesis by Indigenous Microbes via Paneth Cells. Proc Natl Acad Sci USA (2002) 99(24):15451–5. doi: 10.1073/pnas.202604299
38. Sender R, Fuchs S, Milo R. Revised Estimates for the Number of Human and Bacteria Cells in the Body. PloS Biol (2016) 14(8):e1002533. doi: 10.1371/journal.pbio.1002533
39. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D. Role of the Normal Gut Microbiota. World J Gastroenterol (2015) 21(29):8787–803. doi: 10.3748/wjg.v21.i29.8787
40. DeGruttola AK, Low D, Mizoguchi A, Mizoguchi E. Current Understanding of Dysbiosis in Disease in Human and Animal Models. Inflammation Bowel Dis (2016) 22(5):1137–50. doi: 10.1097/MIB.0000000000000750
41. Gao R, Zhu C, Li H, Yin M, Pan C, Huang L, et al. Dysbiosis Signatures of Gut Microbiota Along the Sequence From Healthy, Young Patients to Those With Overweight and Obesity. Obes (Silver Spring) (2018) 26(2):351–61. doi: 10.1002/oby.22088
42. Chassaing B, Raja SM, Lewis JD, Srinivasan S, Gewirtz AT. Colonic Microbiota Encroachment Correlates With Dysglycemia in Humans. Cell Mol Gastroenterol Hepatol (2017) 4(2):205–21. doi: 10.1016/j.jcmgh.2017.04.001
43. Vijay-Kumar M, Aitken JD, Carvalho FA, Cullender TC, Mwangi S, Srinivasan S, et al. Metabolic Syndrome and Altered Gut Microbiota in Mice Lacking Toll-Like Receptor 5. Science (2010) 328(5975):228–31. doi: 10.1126/science.1179721
44. Gill PA, van Zelm MC, Muir JG, Gibson PR. Review Article: Short Chain Fatty Acids as Potential Therapeutic Agents in Human Gastrointestinal and Inflammatory Disorders. Aliment Pharmacol Ther (2018) 48(1):15–34. doi: 10.1111/apt.14689
45. Wu Y, Duan H, Tian X, Xu C, Wang W, Jiang W, et al. Genetics of Obesity Traits: A Bivariate Genome-Wide Association Analysis. Front Genet (2018) 9:179. doi: 10.3389/fgene.2018.00179
46. Kasuga M. [Genetic Factor for Diabetes and Obesity]. Nihon Rinsho (2010) 68(Suppl 8):359–63.
47. Srinivasan S, Chen L, Todd J, Divers J, Gidding S, Chernausek S, et al. The First Genome-Wide Association Study for Type 2 Diabetes in Youth: The Progress in Diabetes Genetics in Youth (ProDiGY) Consortium. Diabetes (2021) 70:996–1005. doi: 10.2337/db20-0443
48. Chen J, Sun M, Adeyemo A, Pirie F, Carstensen T, Pomilla C, et al. Genome-Wide Association Study of Type 2 Diabetes in Africa. Diabetologia (2019) 62:1204–11. doi: 10.1007/s00125-019-4880-7
49. Bogardus C. Missing Heritability and GWAS Utility. Obes (Silver Spring) (2009) 17(2):209–10. doi: 10.1038/oby.2008.613
50. Wang T, Xu M, Bi Y, Ning G. Interplay Between Diet and Genetic Susceptibility in Obesity and Related Traits. Front Med (2018) 12(6):601–7. doi: 10.1007/s11684-018-0648-6
51. Thaker VV. Genetic And Epigenetic Causes Of Obesity. Adolesc Med State Art Rev (2017) 28(2):379–405.
52. Huvenne H, Dubern B, Clément K, Poitou C. Rare Genetic Forms of Obesity: Clinical Approach and Current Treatments in 2016. Obes Facts (2016) 9(3):158–73. doi: 10.1159/000445061
53. Czajkowski P, Adamska-Patruno E, Bauer W, Fiedorczuk J, Krasowska U, Moroz M, et al. The Impact of FTO Genetic Variants on Obesity and Its Metabolic Consequences Is Dependent on Daily Macronutrient Intake. Nutrients (2020) 12(11):3255. doi: 10.3390/nu12113255
54. Koochakpour G, Esfandiar Z, Hosseini-Esfahani F, Mirmiran P, Daneshpour MS, Sedaghati-Khayat B, et al. Evaluating the Interaction of Common FTO Genetic Variants, Added Sugar, and Trans-Fatty Acid Intakes in Altering Obesity Phenotypes. Nutr Metab Cardiovasc Dis (2019) 29(5):474–80. doi: 10.1016/j.numecd.2019.01.005
55. Martins MC, Trujillo J, Freitas-Vilela AA, Farias DR, Rosado EL, Struchiner CJ, et al. Associations Between Obesity Candidate Gene Polymorphisms (Fat Mass and Obesity-Associated (FTO), Melanocortin-4 Receptor (MC4R), Leptin (LEP) and Leptin Receptor (LEPR)) and Dietary Intake in Pregnant Women. Br J Nutr (2018) 120(4):454–63. doi: 10.1017/S0007114518001423
56. Yupanqui-Lozno H, Bastarrachea RA, Yupanqui-Velazco ME, Alvarez-Jaramillo M, Medina-Méndez E, Giraldo-Peña AP, et al. Congenital Leptin Deficiency and Leptin Gene Missense Mutation Found in Two Colombian Sisters With Severe Obesity. Genes (Basel) (2019) 10(5):342. doi: 10.3390/genes10050342
57. Magno F, Guaraná HC, da Fonseca A, Pedrosa AP, Zembrzuski VM, Cabello PH, et al. Association of the MC4R Rs17782313 Polymorphism With Plasma Ghrelin, Leptin, IL6 and Tnfα Concentrations, Food Intake and Eating Behaviors in Morbidly Obese Women. Eat Weight Disord (2020) 26(4):1079–87. doi: 10.1007/s40519-020-01003-5
58. Yu H, Chhabra KH, Thompson Z, Jones GL, Kiran S, Shangguan G, et al. Hypothalamic POMC Deficiency Increases Circulating Adiponectin Despite Obesity. Mol Metab (2020) 35:100957. doi: 10.1016/j.molmet.2020.01.021
59. Cunha M, Aparício G, Duarte J, Pereira A, Albuquerque C, Oliveira A. Genetic Heritage as a Risk Factor Enabling Chilhood Obesity. Aten Primaria (2013) 45(Suppl 2):201–7. doi: 10.1016/S0212-6567(13)70023-4
60. Gupta N, Jain V. Prader Willi Syndrome - A Common Epigenetic Cause of Syndromic Obesity. Indian J Pediatr (2017) 84:809–10. doi: 10.1007/s12098-017-2512-0
61. Cena H, Chiovato L, Nappi RE. Obesity, Polycystic Ovary Syndrome, and Infertility: A New Avenue for GLP-1 Receptor Agonists. J Clin Endocrinol Metab (2020) 105(8):e2695–709. doi: 10.1210/clinem/dgaa285
62. D'Angelo CS, Koiffmann CP. Copy Number Variants in Obesity-Related Syndromes: Review and Perspectives on Novel Molecular Approaches. J Obes (2012) 2012:845480. doi: 10.1155/2012/845480
63. Rosen ED, Kaestner KH, Natarajan R, Patti ME, Sallari R, Sander M, et al. Epigenetics and Epigenomics: Implications for Diabetes and Obesity. Diabetes (2018) 67(10):1923–31. doi: 10.2337/db18-0537
64. Jaenisch R, Bird A. Epigenetic Regulation of Gene Expression: How the Genome Integrates Intrinsic and Environmental Signals. Nat Genet (2003) 33(Suppl):245–54. doi: 10.1038/ng1089
65. Holmes D. Epigenetics: On-Off Switch for Obesity. Nat Rev Endocrinol (2016) 12(3):125. doi: 10.1038/nrendo.2016.18
66. Burgio E, Lopomo A, Migliore L. Obesity and Diabetes: From Genetics to Epigenetics. Mol Biol Rep (2015) 42(4):799–818. doi: 10.1007/s11033-014-3751-z
67. Sherwood WB, Bion V, Lockett GA, Ziyab AH, Soto-Ramírez N, Mukherjee N, et al. Duration of Breastfeeding Is Associated With Leptin (LEP) DNA Methylation Profiles and BMI in 10-Year-Old Children. Clin Epigenet (2019) 11(1):128. doi: 10.1186/s13148-019-0727-9
68. Houde AA, Légaré C, Biron S, Lescelleur O, Biertho L, Marceau S, et al. Leptin and Adiponectin DNA Methylation Levels in Adipose Tissues and Blood Cells are Associated With BMI, Waist Girth and LDL-Cholesterol Levels in Severely Obese Men and Women. BMC Med Genet (2015) 16:29. doi: 10.1186/s12881-015-0174-1
69. Soubry A, Schildkraut JM, Murtha A, Wang F, Huang Z, Bernal A, et al. Paternal Obesity is Associated With IGF2 Hypomethylation in Newborns: Results From a Newborn Epigenetics Study (NEST) Cohort. BMC Med (2013) 11:29. doi: 10.1186/1741-7015-11-29
70. Bannister AJ, Kouzarides T. Regulation of Chromatin by Histone Modifications. Cell Res (2011) 21(3):381–95. doi: 10.1038/cr.2011.22
71. Zhang Q, Ramlee MK, Brunmeir R, Villanueva CJ, Halperin D, Xu F. Dynamic and Distinct Histone Modifications Modulate the Expression of Key Adipogenesis Regulatory Genes. Cell Cycle (2012) 11(23):4310–22. doi: 10.4161/cc.22224
72. Funato H, Oda S, Yokofujita J, Igarashi H, Kuroda M. Fasting and High-Fat Diet Alter Histone Deacetylase Expression in the Medial Hypothalamus. PloS One (2011) 6(4):e18950. doi: 10.1371/journal.pone.0018950
73. Pasquinelli AE. MicroRNAs and Their Targets: Recognition, Regulation and an Emerging Reciprocal Relationship. Nat Rev Genet (2012) 13(4):271–82. doi: 10.1038/nrg3162
74. Cruz K, de Oliveira A, Morais J, Severo JS, Marreiro D. Role of microRNAs on Adipogenesis, Chronic Low-Grade Inflammation, and Insulin Resistance in Obesity. Nutrition (2017) 35:28–35. doi: 10.1016/j.nut.2016.10.003
75. Zhao H, Shen J, Daniel-MacDougall C, Wu X, Chow WH. Plasma MicroRNA Signature Predicting Weight Gain Among Mexican-American Women. Obes (Silver Spring) (2017) 25(5):958–64. doi: 10.1002/oby.21824
76. Hubal MJ, Nadler EP, Ferrante SC, Barberio MD, Suh JH, Wang J, et al. Circulating Adipocyte-Derived Exosomal MicroRNAs Associated With Decreased Insulin Resistance After Gastric Bypass. Obes (Silver Spring) (2017) 25(1):102–10. doi: 10.1002/oby.21709
77. Guidelines (2013) for Managing Overweight and Obesity in Adults. Preface to the Expert Panel Report (Comprehensive Version Which Includes Systematic Evidence Review, Evidence Statements, and Recommendations). Obes (Silver Spring) (2014) 22 Suppl 2:S40. doi: 10.1002/oby.20822
78. Lee EY, Yoon KH. Epidemic Obesity in Children and Adolescents: Risk Factors and Prevention. Front Med (2018) 12(6):658–66. doi: 10.1007/s11684-018-0640-1
79. Nguyen B, Clements J. Obesity Management Among Patients With Type 2 Diabetes and Prediabetes: A Focus on Lifestyle Modifications and Evidence of Antiobesity Medications. Expert Rev Endocrinol Metab (2017) 12(5):303–13. doi: 10.1080/17446651.2017.1367285
80. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in Diet and Lifestyle and Long-Term Weight Gain in Women and Men. N Engl J Med (2011) 364(25):2392–404. doi: 10.1056/NEJMoa1014296
81. Struben J, Chan D, Dubé L. Policy Insights From the Nutritional Food Market Transformation Model: The Case of Obesity Prevention. Ann N Y Acad Sci (2014) 1331:57–75. doi: 10.1111/nyas.12381
82. Lal A, Mantilla-Herrera AM, Veerman L, Backholer K, Sacks G, Moodie M, et al. Correction: Modelled Health Benefits of a Sugar-Sweetened Beverage Tax Across Different Socioeconomic Groups in Australia: A Cost-Effectiveness and Equity Analysis. PloS Med (2020) 17(7):e1003310. doi: 10.1371/journal.pmed.1003310
83. Telles S, Gangadhar BN, Chandwani KD. Lifestyle Modification in the Prevention and Management of Obesity. J Obes (2016) 2016:5818601. doi: 10.1155/2016/5818601
84. Greenway FL, Aronne LJ, Raben A, Astrup A, Apovian CM, Hill JO, et al. A Randomized, Double-Blind, Placebo-Controlled Study of Gelesis100: A Novel Nonsystemic Oral Hydrogel for Weight Loss. Obes (Silver Spring) (2019) 27:205–16. doi: 10.1002/oby.22347
85. Yeo G, Chao D, Siegert AM, Koerperich ZM, Ericson MD, Simonds SE, et al. The Melanocortin Pathway and Energy Homeostasis: From Discovery to Obesity Therapy. Mol Metab (2021) 48:101206. doi: 10.1016/j.molmet.2021.101206
86. Gomez G, Stanford FC. US Health Policy and Prescription Drug Coverage of FDA-Approved Medications for the Treatment of Obesity. Int J Obes (Lond) (2018) 42(3):495–500. doi: 10.1038/ijo.2017.287
87. Rebello CJ, Greenway FL. Obesity Medications in Development. Expert Opin Investig Drugs (2020) 29:63–71. doi: 10.1080/13543784.2020.1705277
88. Karri S, Sharma S, Hatware K, Patil K. Natural Anti-Obesity Agents and Their Therapeutic Role in Management of Obesity: A Future Trend Perspective. BioMed Pharmacother (2019) 110:224–38. doi: 10.1016/j.biopha.2018.11.076
89. Gong S, Ye T, Wang M, Wang M, Li Y, Ma L, et al. Traditional Chinese Medicine Formula Kang Shuai Lao Pian Improves Obesity, Gut Dysbiosis, and Fecal Metabolic Disorders in High-Fat Diet-Fed Mice. Front Pharmacol (2020) 11:297. doi: 10.3389/fphar.2020.00297
90. Aminian A, Zelisko A, Kirwan JP, Brethauer SA, Schauer PR. Exploring the Impact of Bariatric Surgery on High Density Lipoprotein. Surg Obes Relat Dis (2015) 11:238–47. doi: 10.1016/j.soard.2014.07.017
91. Osto M, Abegg K, Bueter M, le Roux CW, Cani PD, Lutz TA. Roux-En-Y Gastric Bypass Surgery in Rats Alters Gut Microbiota Profile Along the Intestine. Physiol Behav (2013) 119:92–6. doi: 10.1016/j.physbeh.2013.06.008
92. Al-Rubaye H, McGlone ER, Farzaneh B, Mustafa L, Johnson M, Kayal A, et al. Roux-En-Y Gastric Bypass or Sleeve Gastrectomy for Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Laparoscopic Endoscopic Robotic Surg (2019) 2(3):53–8. doi: 10.1016/j.lers.2019.05.002
93. Kops NL, Vivan MA, Fülber ER, Fleuri M, Fagundes J, Friedman R. Preoperative Binge Eating and Weight Loss After Bariatric Surgery: A Systematic Review and Meta-Analysis. Obes Surg (2020) 31(3):1239–48. doi: 10.1007/s11695-020-05124-9
94. Kong LC, Tap J, Aron-Wisnewsky J, Pelloux V, Basdevant A, Bouillot JL, et al. Gut Microbiota After Gastric Bypass in Human Obesity: Increased Richness and Associations of Bacterial Genera With Adipose Tissue Genes. Am J Clin Nutr (2013) 98(1):16–24. doi: 10.3945/ajcn.113.058743
95. Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y, et al. Human Gut Microbiota in Obesity and After Gastric Bypass. Proc Natl Acad Sci USA (2009) 106(7):2365–70. doi: 10.1073/pnas.0812600106
96. van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter LM, et al. Blood Pressure, Lipids, and Obesity are Associated With Retinopathy: The Hoorn Study. Diabetes Care (2002) 25(8):1320–5. doi: 10.2337/diacare.25.8.1320
97. Yu EW, Gao L, Stastka P, Cheney MC, Mahabamunuge J, Torres Soto M, et al. Fecal Microbiota Transplantation for the Improvement of Metabolism in Obesity: The FMT-TRIM Double-Blind Placebo-Controlled Pilot Trial. PloS Med (2020) 17(3):e1003051. doi: 10.1371/journal.pmed.1003051
98. Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, et al. Gut Microbiota From Twins Discordant for Obesity Modulate Metabolism in Mice. Science (2013) 341(6150):1241214. doi: 10.1126/science.1241214
99. Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JF, et al. Transfer of Intestinal Microbiota From Lean Donors Increases Insulin Sensitivity in Individuals With Metabolic Syndrome. Gastroenterology (2012) 143(4):913–6.e7. doi: 10.1053/j.gastro.2012.06.031
100. Zhang Z, Mocanu V, Cai C, Dang J, Slater L, Deehan EC, et al. Impact of Fecal Microbiota Transplantation on Obesity and Metabolic Syndrome-A Systematic Review. Nutrients (2019) 11(10):2291. doi: 10.3390/nu11102291
101. Phan HD, Nguyen T, Bui PL, Pham TT, Doan TV, Nguyen, et al. Overweight and Obesity Among Vietnamese School-Aged Children: National Prevalence Estimates Based on the World Health Organization and International Obesity Task Force Definition. PloS One (2020) 15(10):e0240459. doi: 10.1371/journal.pone.0240459
102. Epigenetic Drugs. Nat Biotechnol (2020) 38(5):558. doi: 10.1038/s41587-020-0523-2
103. Arguelles AO, Meruvu S, Bowman JD, Choudhury M. Are Epigenetic Drugs for Diabetes and Obesity at Our Door Step. Drug Discov Today (2016) 21(3):499–509. doi: 10.1016/j.drudis.2015.12.001
104. Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial Ecology: Human Gut Microbes Associated With Obesity. Nature (2006) 444(7122):1022–3. doi: 10.1038/4441022a
Keywords: obesity, epidemiology, pathophysiology, genetics, epigenetics, microenvironment
Citation: Lin X and Li H (2021) Obesity: Epidemiology, Pathophysiology, and Therapeutics. Front. Endocrinol. 12:706978. doi: 10.3389/fendo.2021.706978
Received: 08 May 2021; Accepted: 10 August 2021; Published: 06 September 2021.
Reviewed by:
Copyright © 2021 Lin and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Li, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Loading metrics
Open Access
Perspective
The Perspective section provides experts with a forum to comment on topical or controversial issues of broad interest.
See all article types »
Obesity research: Moving from bench to bedside to population
* E-mail: [email protected]
Affiliation Diabetes Research Program, Department of Medicine, New York University Grossman School of Medicine, New York, New York, United States of America
- Ann Marie Schmidt

Published: December 4, 2023
- https://doi.org/10.1371/journal.pbio.3002448
- Reader Comments
Globally, obesity is on the rise. Research over the past 20 years has highlighted the far-reaching multisystem complications of obesity, but a better understanding of its complex pathogenesis is needed to identify safe and lasting solutions.
Citation: Schmidt AM (2023) Obesity research: Moving from bench to bedside to population. PLoS Biol 21(12): e3002448. https://doi.org/10.1371/journal.pbio.3002448
Copyright: © 2023 Ann Marie Schmidt. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: AMS received funding from U.S. Public Health Service (grants 2P01HL131481 and P01HL146367). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The author has declared that no competing interests exist.
Abbreviations: EDC, endocrine disruptor chemical; GIP, gastric inhibitory polypeptide; GLP1, glucagon-like peptide 1; HFCS, high-fructose corn syrup
This article is part of the PLOS Biology 20th anniversary collection.
Obesity is a multifaceted disorder, affecting individuals across their life span, with increased prevalence in persons from underrepresented groups. The complexity of obesity is underscored by the multiple hypotheses proposed to pinpoint its seminal mechanisms, such as the “energy balance” hypothesis and the “carbohydrate–insulin” model. It is generally accepted that host (including genetic factors)–environment interactions have critical roles in this disease. The recently framed “fructose survival hypothesis” proposes that high-fructose corn syrup (HFCS), through reduction in the cellular content of ATP, stimulates glycolysis and reduces mitochondrial oxidative phosphorylation, processes that stimulate hunger, foraging, weight gain, and fat accumulation [ 1 ]. The marked upswing in the use of HFCS in beverages and foods, beginning in the 1980s, has coincided with the rising prevalence of obesity.
The past few decades of scientific progress have dramatically transformed our understanding of pathogenic mechanisms of obesity ( Fig 1 ). Fundamental roles for inflammation were unveiled by the discovery that tumor necrosis factor-α contributed to insulin resistance and the risk for type 2 diabetes in obesity [ 2 ]. Recent work has ascribed contributory roles for multiple immune cell types, such as monocytes/macrophages, neutrophils, T cells, B cells, dendritic cells, and mast cells, in disturbances in glucose and insulin homeostasis in obesity. In the central nervous system, microglia and their interactions with hypothalamic neurons affect food intake, energy expenditure, and insulin sensitivity. In addition to cell-specific contributions of central and peripheral immune cells in obesity, roles for interorgan communication have been described. Extracellular vesicles emitted from immune cells and from adipocytes, as examples, are potent transmitters of obesogenic species that transfer diverse cargo, including microRNAs, proteins, metabolites, lipids, and organelles (such as mitochondria) to distant organs, affecting functions such as insulin sensitivity and, strikingly, cognition, through connections to the brain [ 3 ].
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
Basic, clinical/translational, and epidemiological research has made great strides in the past few decades in uncovering novel components of cell-intrinsic, intercellular, and interorgan communications that contribute to the pathogenesis of obesity. Both endogenous and exogenous (environmental) stressors contribute to the myriad of metabolic perturbations that impact energy intake and expenditure; mediate innate disturbances in the multiple cell types affected in obesity in metabolic organelles and organs, including in immune cells; and impair beneficial interkingdom interactions of the mammalian host with the gut microbiome. The past few decades have also witnessed remarkable efforts to successfully treat obesity, such as the use of the incretin agonists and bariatric surgery. Yet, these and other strategies may be accompanied by resistance to weight loss, weight regain, adverse effects of interventions, and the challenges of lifelong implementation. Hence, through leveraging novel discoveries from the bench to the bedside to the population, additional strategies to prevent obesity and weight regain post-weight loss, such as the use of “wearables,” with potential for implementation of immediate and personalized behavior modifications, may hold great promise as complementary strategies to prevent and identify lasting treatments for obesity. Figure created with BioRender.
https://doi.org/10.1371/journal.pbio.3002448.g001
Beyond intercellular communication mediated by extracellular vesicles, the discovery of interactions between the host and the gut microbiome has suggested important roles for this interkingdom axis in obesity. Although disturbances in commensal gut microbiota species and their causal links to obesity are still debated, transplantation studies have demonstrated relationships between Firmicutes/Bacteroidetes ratios and obesity [ 4 ]. Evidence supports the concept that modulation of gut microbiota phyla modulates fundamental activities, such as thermogenesis and bile acid and lipid metabolism. Furthermore, compelling discoveries during the past few decades have illustrated specific mechanisms within adipocytes that exert profound effects on organismal homeostasis, such as adipose creatine metabolism, transforming growth factor/SMAD signaling, fibrosis [ 5 ], hypoxia and angiogenesis, mitochondrial dysfunction, cellular senescence, impairments in autophagy, and modulation of the circadian rhythm. Collectively, these recent discoveries set the stage for the identification of potential new therapeutic approaches in obesity.
Although the above discoveries focus largely on perturbations in energy metabolism (energy intake and expenditure) as drivers of obesity, a recently published study suggests that revisiting the timeline of obesogenic forces in 20th and 21st century society may be required. The authors tracked 320,962 Danish schoolchildren (born during 1930 to 1976) and 205,153 Danish male military conscripts (born during 1939 to 1959). Although the overall trend of the percentiles of the distributions of body mass index were linear across the years of birth, with percentiles below the 75th being nearly stable, those above the 75th percentile demonstrated a steadily steeper rise the more extreme the percentile; this was noted in the schoolchildren and the military conscripts [ 6 ]. The authors concluded that the emergence of the obesity epidemic might have preceded the appearance of the factors typically ascribed to mediating the obesogenic transformation of society by several decades. What are these underlying factors and their yet-to-be-discovered mechanisms?
First, in terms of endogenous factors relevant to individuals, stressors such as insufficient sleep and psychosocial stress may impact substrate metabolism, circulating appetite hormones, hunger, satiety, and weight gain [ 7 ]. Reduced access to healthy foods rich in vegetables and fruits but easy access to ultraprocessed ingredients in “food deserts” and “food swamps” caused excessive caloric intake and weight gain in clinical studies [ 8 ]. Second, exogenous environmental stresses have been associated with obesity. For example, air pollution has been directly linked to adipose tissue dysfunction [ 9 ], and ubiquitous endocrine disruptor chemicals (EDCs) such as bisphenols and phthalates (found in many items of daily life including plastics, food, clothing, cosmetics, and paper) are linked to metabolic dysfunction and the development of obesity [ 10 ]. Hence, factors specific to individuals and their environment may exacerbate their predisposition to obesity.
In addition to the effects of exposure to endogenous and exogenous stressors on the risk of obesity, transgenerational (passed through generations without direct exposure of stimulant) and intergenerational (direct exposure across generations) transmission of these stressors has also been demonstrated. A leading proposed mechanism is through epigenetic modulation of the genome, which then predisposes affected offspring to exacerbated responses to obesogenic conditions such as diet. A recent study suggested that transmission of disease risk might be mediated through transfer of maternal oocyte-derived dysfunctional mitochondria from mothers with obesity [ 11 ]. Additional mechanisms imparting obesogenic “memory” may be evoked through “trained immunity.”
Strikingly, the work of the past few decades has resulted in profound triumphs in the treatment of obesity. Multiple approved glucagon-like peptide 1 (GLP1) and gastric inhibitory polypeptide (GIP) agonists [ 12 ] (alone or in combinations) induce highly significant weight loss in persons with obesity [ 13 ]. However, adverse effects of these agents, such as pancreatitis and biliary disorders, have been reported [ 14 ]. Therefore, the long-term safety and tolerability of these drugs is yet to be determined. In addition to pharmacological agents, bariatric surgery has led to significant weight loss as well. However, efforts to induce weight loss through reduction in caloric intake and increased physical activity, pharmacological approaches, and bariatric surgery may not mediate long-term cures in obesity on account of resistance to weight loss, weight regain, adverse effects of interventions, and the challenges of lifelong implementation of these measures.
Where might efforts in combating obesity lie in the next decades? At the level of basic and translational science, the heterogeneity of metabolic organs could be uncovered through state-of-the-art spatial “omics” and single-cell RNA sequencing approaches. For example, analogous to the deepening understanding of the great diversity in immune cell subsets in homeostasis and disease, adipocyte heterogeneity has also been suggested, which may reflect nuances in pathogenesis and treatment approaches. Further, approaches to bolster brown fat and thermogenesis may offer promise to combat evolutionary forces to hoard and store fat. A better understanding of which interorgan communications may drive obesity will require intensive profiling of extracellular vesicles shed from multiple metabolic organs to identify their cargo and, critically, their destinations. In the three-dimensional space, the generation of organs-on-a-chip may facilitate the discovery of intermetabolic organ communications and their perturbations in the pathogenesis of obesity and the screening of new therapies.
Looking to prevention, recent epidemiological studies suggest that efforts to tackle obesity require intervention at multiple levels. The institution of public health policies to reduce air pollution and the vast employment of EDCs in common household products could impact the obesity epidemic. Where possible, the availability of fresh, healthy foods in lieu of highly processed foods may be of benefit. At the individual level, focused attention on day-to-day behaviors may yield long-term benefit in stemming the tide of obesity. “Wearable” devices that continuously monitor the quantity, timing, and patterns of food intake, physical activity, sleep duration and quality, and glycemic variability might stimulate on-the-spot and personalized behavior modulation to contribute to the prevention of obesity or of maintenance of the weight-reduced state.
Given the involvement of experts with wide-ranging expertise in the science of obesity, from basic science, through clinical/translational research to epidemiology and public health, it is reasonable to anticipate that the work of the next 2 decades will integrate burgeoning multidisciplinary discoveries to drive improved efforts to treat and prevent obesity.
Acknowledgments
The author is grateful to Ms. Latoya Woods of the Diabetes Research Program for assistance with the preparation of the manuscript and to Ms. Kristen Dancel-Manning for preparation of the Figure accompanying the manuscript.
- View Article
- PubMed/NCBI
- Google Scholar

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases & Disorders Education Program
- Publications and Resources
- Clinical Trials
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Ask a Scientist
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Obesity Research
Language switcher.
Over the years, NHLBI-supported research on overweight and obesity has led to the development of evidence-based prevention and treatment guidelines for healthcare providers. NHLBI research has also led to guidance on how to choose a behavioral weight loss program.
Studies show that the skills learned and support offered by these programs can help most people make the necessary lifestyle changes for weight loss and reduce their risk of serious health conditions such as heart disease and diabetes.
Our research has also evaluated new community-based programs for various demographics, addressing the health disparities in overweight and obesity.
NHLBI research that really made a difference
- In 1991, the NHLBI developed an Obesity Education Initiative to educate the public and health professionals about obesity as an independent risk factor for cardiovascular disease and its relationship to other risk factors, such as high blood pressure and high blood cholesterol. The initiative led to the development of clinical guidelines for treating overweight and obesity.
- The NHLBI and other NIH Institutes funded the Obesity-Related Behavioral Intervention Trials (ORBIT) projects , which led to the ORBIT model for developing behavioral treatments to prevent or manage chronic diseases. These studies included families and a variety of demographic groups. A key finding from one study focuses on the importance of targeting psychological factors in obesity treatment.
Current research funded by the NHLBI
The Division of Cardiovascular Sciences , which includes the Clinical Applications and Prevention Branch, funds research to understand how obesity relates to heart disease. The Center for Translation Research and Implementation Science supports the translation and implementation of research, including obesity research, into clinical practice. The Division of Lung Diseases and its National Center on Sleep Disorders Research fund research on the impact of obesity on sleep-disordered breathing.
Find funding opportunities and program contacts for research related to obesity and its complications.
Current research on obesity and health disparities
Health disparities happen when members of a group experience negative impacts on their health because of where they live, their racial or ethnic background, how much money they make, or how much education they received. NHLBI-supported research aims to discover the factors that contribute to health disparities and test ways to eliminate them.
- NHLBI-funded researchers behind the RURAL: Risk Underlying Rural Areas Longitudinal Cohort Study want to discover why people in poor rural communities in the South have shorter, unhealthier lives on average. The study includes 4,000 diverse participants (ages 35–64 years, 50% women, 44% whites, 45% Blacks, 10% Hispanic) from 10 of the poorest rural counties in Kentucky, Alabama, Mississippi, and Louisiana. Their results will support future interventions and disease prevention efforts.
- The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) is looking at what factors contribute to the higher-than-expected numbers of Hispanics/Latinos who suffer from metabolic diseases such as obesity and diabetes. The study includes more than 16,000 Hispanic/Latino adults across the nation.
Find more NHLBI-funded studies on obesity and health disparities at NIH RePORTER.

Read how African Americans are learning to transform soul food into healthy, delicious meals to prevent cardiovascular disease: Vegan soul food: Will it help fight heart disease, obesity?
Current research on obesity in pregnancy and childhood
- The NHLBI-supported Fragile Families Cardiovascular Health Follow-Up Study continues a study that began in 2000 with 5,000 American children born in large cities. The cohort was racially and ethnically diverse, with approximately 40% of the children living in poverty. Researchers collected socioeconomic, demographic, neighborhood, genetic, and developmental data from the participants. In this next phase, researchers will continue to collect similar data from the participants, who are now young adults.
- The NHLBI is supporting national adoption of the Bright Bodies program through Dissemination and Implementation of the Bright Bodies Intervention for Childhood Obesity . Bright Bodies is a high-intensity, family-based intervention for childhood obesity. In 2017, a U.S. Preventive Services Task Force found that Bright Bodies lowered children’s body mass index (BMI) more than other interventions did.
- The NHLBI supports the continuation of the nuMoM2b Heart Health Study , which has followed a diverse cohort of 4,475 women during their first pregnancy. The women provided data and specimens for up to 7 years after the birth of their children. Researchers are now conducting a follow-up study on the relationship between problems during pregnancy and future cardiovascular disease. Women who are pregnant and have obesity are at greater risk than other pregnant women for health problems that can affect mother and baby during pregnancy, at birth, and later in life.
Find more NHLBI-funded studies on obesity in pregnancy and childhood at NIH RePORTER.
Learn about the largest public health nonprofit for Black and African American women and girls in the United States: Empowering Women to Get Healthy, One Step at a Time .
Current research on obesity and sleep
- An NHLBI-funded study is looking at whether energy balance and obesity affect sleep in the same way that a lack of good-quality sleep affects obesity. The researchers are recruiting equal numbers of men and women to include sex differences in their study of how obesity affects sleep quality and circadian rhythms.
- NHLBI-funded researchers are studying metabolism and obstructive sleep apnea . Many people with obesity have sleep apnea. The researchers will look at the measurable metabolic changes in participants from a previous study. These participants were randomized to one of three treatments for sleep apnea: weight loss alone, positive airway pressure (PAP) alone, or combined weight loss and PAP. Researchers hope that the results of the study will allow a more personalized approach to diagnosing and treating sleep apnea.
- The NHLBI-funded Lipidomics Biomarkers Link Sleep Restriction to Adiposity Phenotype, Diabetes, and Cardiovascular Risk study explores the relationship between disrupted sleep patterns and diabetes. It uses data from the long-running Multiethnic Cohort Study, which has recruited more than 210,000 participants from five ethnic groups. Researchers are searching for a cellular-level change that can be measured and can predict the onset of diabetes in people who are chronically sleep deprived. Obesity is a common symptom that people with sleep issues have during the onset of diabetes.
Find more NHLBI-funded studies on obesity and sleep at NIH RePORTER.

Learn about a recent study that supports the need for healthy sleep habits from birth: Study finds link between sleep habits and weight gain in newborns .
Obesity research labs at the NHLBI
The Cardiovascular Branch and its Laboratory of Inflammation and Cardiometabolic Diseases conducts studies to understand the links between inflammation, atherosclerosis, and metabolic diseases.
NHLBI’s Division of Intramural Research , including its Laboratory of Obesity and Aging Research , seeks to understand how obesity induces metabolic disorders. The lab studies the “obesity-aging” paradox: how the average American gains more weight as they get older, even when food intake decreases.
Related obesity programs and guidelines
- Aim for a Healthy Weight is a self-guided weight-loss program led by the NHLBI that is based on the psychology of change. It includes tested strategies for eating right and moving more.
- The NHLBI developed the We Can! ® (Ways to Enhance Children’s Activity & Nutrition) program to help support parents in developing healthy habits for their children.
- The Accumulating Data to Optimally Predict obesity Treatment (ADOPT) Core Measures Project standardizes data collected from the various studies of obesity treatments so the data can be analyzed together. The bigger the dataset, the more confidence can be placed in the conclusions. The main goal of this project is to understand the individual differences between people who experience the same treatment.
- The NHLBI Director co-chairs the NIH Nutrition Research Task Force, which guided the development of the first NIH-wide strategic plan for nutrition research being conducted over the next 10 years. See the 2020–2030 Strategic Plan for NIH Nutrition Research .
- The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) , which is a public–private partnership to accelerate progress in reducing childhood obesity.
- The NHLBI has been providing guidance to physicians on the diagnosis, prevention, and treatment of obesity since 1977. In 2017, the NHLBI convened a panel of experts to take on some of the pressing questions facing the obesity research community. See their responses: Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents (PDF, 3.69 MB).
- In 2021, the NHLBI held a Long Non-coding (lnc) RNAs Symposium to discuss research opportunities on lnc RNAs, which appear to play a role in the development of metabolic diseases such as obesity.
- The Muscatine Heart Study began enrolling children in 1970. By 1981, more than 11,000 students from Muscatine, Iowa, had taken surveys twice a year. The study is the longest-running study of cardiovascular risk factors in children in the United States. Today, many of the earliest participants and their children are still involved in the study, which has already shown that early habits affect cardiovascular health later in life.
- The Jackson Heart Study is a unique partnership of the NHLBI, three colleges and universities, and the Jackson, Miss., community. Its mission is to discover what factors contribute to the high prevalence of cardiovascular disease among African Americans. Researchers aim to test new approaches for reducing this health disparity. The study incudes more than 5,000 individuals. Among the study’s findings to date is a gene variant in African Americans that doubles the risk of heart disease.
Explore more NHLBI research on overweight and obesity
The sections above provide you with the highlights of NHLBI-supported research on overweight and obesity . You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.

Access Obesity and Affiliated Journals
As the leading scientific membership organization dedicated to the study of obesity, The Obesity Society connects you to indispensable scientific, educational and clinical information from an array of perspectives.
Obesity is the Official Journal of The Obesity Society

Information About Obesity
Editor-in-Chief : Michael Jensen, MD Associate Editor-In-Chief : Leanne Redman, PhD
Available in print and online, Obesity publishes vital, peer-reviewed studies and leads the field in exploring scientific developments in all areas of research, including clinical investigations, obesity biology and integrated physiology, pediatric obesity, epidemiology and genetics.
Connect with Obesity
You can access Obesity online any time. To view the journal’s current content, members can log in using the “Access Obesity ” link at the top of the TOS home page .
Non-members can view abstracts of recent articles and full text of articles older than 12 months.
Having Obesity login issues? Please call 301-563-6526 or email [email protected] .
Submit your research to Obesity today!
Submit your best research and join the community of thought leaders in the fight against obesity. For submission instructions, read our author guidelines . Then submit your paper here .
Authors benefit from:
- 2022 Impact Factor – 6.9
- Nearly 2 million article downloads per year
- Quick and easy online submission
- Fast first decision: The average time from submission to first decision is 13 days (median 5 days)
- Rapid publication: 6–8 weeks from acceptance to publication
- Extensive exposure across the scientific and academic communities
- Promotion to media outlets by the TOS Communications Department and our publisher, Wiley
- Open Access: You can choose to make your article freely available immediately upon publication
Obesity Journal Symposium
Papers from the annual Obesity symposium will be presented during ObesityWeek each November. The papers will also be published online during ObesityWeek and in a special section of an issue of Obesity that follows the meeting.
Keep an eye on the ObesityWeek website for complete details and read the ObesityWeek selections from previous competitions.
TOS/AHA/ACC Obesity Guidelines
Obesity has published the full report of the Obesity Treatment Guidelines online. You can also order a print version of the guidelines.
Note: When referring to the Obesity Treatment Guidelines in your work, don’t forget to use this citation: Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, Hu FB, Hubbard VS, Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM, Yanovski SZ. Guidelines (2013) for managing overweight and obesity in adults. Obesity 2014;22(S2):S1-S410.
Affiliated Journals
As a TOS member, you automatically receive membership in the World Obesity Federation (WOF). We are proud to partner with WOF by co-publishing the open access journal Obesity Science & Practice , as well as providing access and discounted subscriptions to other noteworthy journals published by the Federation.
To receive a discounted journal subscription as a WOF member, visit the WOF journals page and follow one of the “subscribe as a member” links.
Obesity Science & Practice
Obesity reviews, clinical obesity, pediatric obesity.

- Discusses new medical, behavioral, dietary, pharmalogic and surgical approaches to obesity treatment
- Publishes research papers designed to engage both healthcare professionals and other individuals

- Genetic, molecular, biochemical and physiological aspects of obesity—basic, applied and clinical studies
- Metabolic consequences of child and adolescent obesity
- Epidemiological and public health-related studies of child and adolescent overweight and obesity
- Clinical management of children and adolescents who have overweight or obesity
- Comorbidities linked to child and adolescent obesity—mechanisms, assessment and treatment
- Life-cycle factors (e.g., familial, intrauterine and developmental aspects of child and adolescent obesity)
- Nutrition security and the “double burden” of obesity and malnutrition
- Health promotion strategies around the issues of obesity, nutrition, and physical activity in children and adolescents
Thank you for your interest in joining a TOS Committee.
Your request has been sent..
Cookies on Obesity.org
By using Obesity.org, you agree to our use of cookies. We use cookies to provide you with a great experience and to help our website run effectively.
Your payment has been processed successfully!
We’re sorry. we could not process your payment..
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Author Biographies
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Nurses’ role in obesity management in adults in primary healthcare settings worldwide: a scoping review.

1. Introduction
Significance, 2.1. protocol, 2.2. eligibility criteria, 2.3. information sources, 2.4. search strategy, 2.5. selection of sources of evidence, 2.6. process of data extraction, 2.7. thematic analysis, 3.1. characteristics of the studies, 3.2. synthesis of results, 3.2.1. patient-centred care, 3.2.2. patient assessments, 3.2.3. therapeutic nursing interventions, 3.2.4. patient education, 3.2.5. care management, 3.2.6. professional development, 4. discussion, limitations, supplementary materials, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. Can. Med. Assoc. J. 2020 , 192 , E875–E891. [ Google Scholar ] [ CrossRef ]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 April 2024).
- Pray, R.; Riskin, S. The history and faults of the body mass index and where to look next: A literature review. Cureus 2023 , 15 , e48230. [ Google Scholar ] [ CrossRef ]
- Chen, X.; Zhou, C.W.; Fu, Y.Y.; Li, Y.Z.; Chen, L.; Zhang, Q.W.; Chen, Y.F. Global, regional, and national burden of chronic respiratory diseases and associated risk factors, 1990-2019: Results from the Global Burden of Disease Study 2019. Front. Med. 2023 , 10 , 1066804. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- The British Heart Foundation. Global Heart & Circulatory Diseases Factsheet. Available online: https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-global-factsheet.pdf (accessed on 10 March 2024).
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020 , 10 , 14790. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet 2023 , 402 , 203–234. [ Google Scholar ] [ CrossRef ]
- World Obesity Federation. World Obesity Atlas 2024. Available online: https://data.worldobesity.org/publications/?cat=22 (accessed on 10 April 2024).
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Grosse, Y.; Bianchini, F.; Straif, K. Body Fatness and Cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016 , 375 , 794–798. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Obesity Canada. Health Impacts of Obesity. Available online: https://obesitycanada.ca/understanding-obesity/health-impacts-obesity/ (accessed on 20 November 2023).
- Recalde, M.; Pistillo, A.; Viallon, V.; Fontvieille, E.; Duarte-Salles, T.; Freisling, H. Body mass index and incident cardiometabolic conditions in relation to obesity-related cancer risk: A population-based cohort study in Catalonia, Spain. Cancer Med. 2023 , 12 , 20188–20200. [ Google Scholar ] [ CrossRef ]
- Rueda-Clausen, C.F.; Poddar, M.; Lear, S.A.; Poirier, P.; Sharma, A.M. Canadian Adult Obesity Clinical Practice Guidelines: Assessment of People Living with Obesity. Available online: https://obesitycanada.ca/guidelines/assessment (accessed on 20 November 2023).
- World Cancer Research Fund/American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: A Global Perspective ; Continuous Update Project Expert Report; World Cancer Research Fund International: London, UK, 2018. [ Google Scholar ]
- Puhl, R.M.; Lessard, L.M.; Himmelstein, M.S.; Foster, G.D. The roles of experienced and internalized weight stigma in healthcare experiences: Perspectives of adults engaged in weight management across six countries. PLoS ONE 2021 , 16 , e0251566. [ Google Scholar ] [ CrossRef ]
- Wu, Y.K.; Berry, D.C. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: A systematic review. J. Adv. Nurs. 2018 , 74 , 1030–1042. [ Google Scholar ] [ CrossRef ]
- World Health Organization. WHO Acceleration Plan to Stop Obesity. Available online: https://www.who.int/publications/i/item/9789240075634 (accessed on 21 November 2023).
- World Health Organization. Declaration of Alma Ata. International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978. Available online: https://www.who.int/docs/default-source/documents/almaata-declaration-en.pdf (accessed on 12 April 2024).
- World Health Organization. WHO Package of Essential Noncommunicable (WHO PEN) Disease Interventions for Primary Health Care. Available online: https://www.who.int/publications/i/item/9789240009226 (accessed on 21 September 2023).
- Tandan, M.; Dunlea, S.; Cullen, W.; Bury, G. Teamwork and its impact on chronic disease clinical outcomes in primary care: A systematic review and meta-analysis. Public Health 2024 , 229 , 88–115. [ Google Scholar ] [ CrossRef ]
- Semlitsch, T.; Stigler, F.L.; Jeitler, K.; Horvath, K.; Siebenhofer, A. Management of overweight and obesity in primary care-A systematic overview of international evidence-based guidelines. Obes. Rev. 2019 , 20 , 1218–1230. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Griffin, C.D. A Primary Care Nursing Perspective on Chronic Disease Prevention and Management. Del. J. Public Health 2017 , 3 , 78–83. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- World Health Organization (WHO). Regional Office for Europe. Competencies for Nurses Working in Primary Health Care. Available online: https://iris.who.int/handle/10665/365607 (accessed on 20 March 2024).
- Wilkes, L.; Cioffi, J.; Cummings, J.; Warne, B.; Harrison, K. Clients with chronic conditions: Community nurse role in a multidisciplinary team. J. Clin. Nurs. 2014 , 23 , 844–855. [ Google Scholar ] [ CrossRef ]
- World Health Organization. Nursing and Midwifery. Available online: https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery (accessed on 21 September 2023).
- Jackson, S.E.; Wardle, J.; Johnson, F.; Finer, N.; Beeken, R.J. The impact of a health professional recommendation on weight loss attempts in overweight and obese British adults: A cross-sectional analysis. BMJ Open 2013 , 3 , e003693. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bright, D.; Gray, B.J.; Kyle, R.G.; Bolton, S.; Davies, A.R. Factors influencing initiation of health behaviour conversations with patients: Cross-sectional study of nurses, midwives, and healthcare support workers in Wales. J. Adv. Nurs. 2021 , 77 , 4427–4438. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Walsh, K.; Grech, C.; Hill, K. Health advice and education given to overweight patients by primary care doctors and nurses: A scoping literature review. Prev. Med. Rep. 2019 , 14 , 100812. [ Google Scholar ] [ CrossRef ]
- Warr, W.; Aveyard, P.; Albury, C.; Nicholson, B.; Tudor, K.; Hobbs, R.; Roberts, N.; Ziebland, S. A systematic review and thematic synthesis of qualitative studies exploring GPs’ and nurses’ perspectives on discussing weight with patients with overweight and obesity in primary care. Obes. Rev. 2021 , 22 , e13151. [ Google Scholar ] [ CrossRef ]
- Rust, C.; Prior, R.M.; Stec, M. Implementation of a clinical practice guideline in a primary care setting for the prevention and management of obesity in adults. Nurs. Forum 2020 , 55 , 485–490. [ Google Scholar ] [ CrossRef ]
- Peters, M.; Godfrey, C.; McInerney, P.; Munn, Z.; Trico, A.; Khalil, H. Chapter 11: Scoping Reviews. JBI Man. Evid. Synth. 2020 , 169 , 467–473. [ Google Scholar ]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018 , 169 , 467–473. [ Google Scholar ] [ CrossRef ]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006 , 3 , 77–101. [ Google Scholar ] [ CrossRef ]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021 , 372 , n71. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barrea, L.; Framondi, L.; Di Matteo, R.; Verde, L.; Vetrani, C.; Graziadio, C.; Pugliese, G.; Laudisio, D.; Vitale, G.; Iannicelli, A.; et al. The role of the nurse in the Obesity Clinic: A practical guideline. Panminerva Medica 2021 , 63 , 539–546. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Braga, V.A.S.; Jesus, M.C.P.; Conz, C.A.; Silva, M.H.D.; Tavares, R.E.; Merighi, M.A.B. Actions of nurses toward obesity in primary health care units. Rev. Bras. Enferm. 2020 , 73 , e20180404. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brewah, H.; Todhunter, J.; Bades, A.; Colyer, S. Can community nurses take on obesity? J. Community Nurs. 2018 , 32 , 8–11. [ Google Scholar ]
- Campbell-Scherer, D.L.; Asselin, J.; Osunlana, A.M.; Ogunleye, A.A.; Fielding, S.; Anderson, R.; Cave, A.; Johnson, J.A.; Sharma, A.M. Changing provider behaviour to increase nurse visits for obesity in family practice: The 5As Team randomized controlled trial. CMAJ Open 2019 , 7 , E371–E378. [ Google Scholar ] [ CrossRef ]
- Fernández-Ruiz, V.E.; Armero-Barranco, D.; Paniagua-Urbano, J.A.; Sole-Agusti, M.; Ruiz-Sánchez, A.; Gómez-Marín, J. Short-medium-long-term efficacy of interdisciplinary intervention against overweight and obesity: Randomized controlled clinical trial. Int. J. Nurs. Pract. 2018 , 24 , e12690. [ Google Scholar ] [ CrossRef ]
- Fernández-Ruiz, V.E.; Paniagua-Urbano, J.A.; Solé-Agustí, M.; Ruiz-Sánchez, A.; Gómez-Marín, J.; Armero-Barranco, D. Impact of the I 2 AO 2 interdisciplinary program led by nursing on psychological comorbidity and quality of life: Randomized controlled clinical trial. Arch. Psychiatr. Nurs. 2018 , 32 , 268–277. [ Google Scholar ] [ CrossRef ]
- Govindasamy, S.; Beek, K.; Yates, K.; Jayasuriya, R.; Reynolds, R.; de Wit, J.B.F.; Harris, M. Experiences of overweight and obese patients with diabetes and practice nurses during implementation of a brief weight management intervention in general practice settings serving Culturally and Linguistically Diverse disadvantaged populations. Aust. J. Prim. Health 2023 , 29 , 358–364. [ Google Scholar ] [ CrossRef ]
- Hinks, S.R. Exploring community nurses’ views on the implementation of a local Weight Management Pathway. Br. J. Community Nurs. 2022 , 27 , 612–618. [ Google Scholar ] [ CrossRef ]
- Kelley, S. The Role of the Faith Community Nurse in Weight Management. J. Christ. Nurs. 2018 , 35 , 53–59. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Palmeira, C.S.; Mussi, F.C.; Santos, C.A.S.d.T.; Lima, M.L.; Ladeia, A.M.T.; Silva, L.C.d.J. Effect of remote nursing monitoring on overweight in women: Clinical trial. Rev. Lat.-Am. De Enferm. 2019 , 27 , e3129. [ Google Scholar ] [ CrossRef ]
- Parker, S.; Tran, A.; Saito, S.; McNamara, C.; Denney-Wilson, E.; Nutbeam, D.; Harris, M.F. Exploring organisational readiness to implement a preventive intervention in Australian general practice for overweight and obese patients: Key learnings from the HeLP-GP trial. Aust. J. Prim. Health 2024 , 30 , PY23085. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Parker, S.M.; Barr, M.; Stocks, N.; Denney-Wilson, E.; Zwar, N.; Karnon, J.; Kabir, A.; Nutbeam, D.; Roseleur, J.; Liaw, S.-T.; et al. Preventing chronic disease in overweight and obese patients with low health literacy using eHealth and teamwork in primary healthcare (HeLP-GP): A cluster randomised controlled trial. BMJ Open 2022 , 12 , e060393. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Parker, S.M.; Stocks, N.; Nutbeam, D.; Thomas, L.; Denney-Wilson, E.; Zwar, N.; Karnon, J.; Lloyd, J.; Noakes, M.; Liaw, S.-T.; et al. Preventing chronic disease in patients with low health literacy using eHealth and teamwork in primary healthcare: Protocol for a cluster randomised controlled trial. BMJ Open 2018 , 8 , e023239. [ Google Scholar ] [ CrossRef ]
- Shaji, P.; Singh, M.; Sahu, B.; Arulappan, J. Effectiveness of Nurse-led Lifestyle Modification Intervention on Obesity Among Young Women in India. SAGE Open Nurs. 2023 , 9 , 23779608231186705. [ Google Scholar ] [ CrossRef ]
- Virtanen, J.; Penttinen, M.; Kautiainen, H.; Korhonen, P. The impact of lifestyle counselling on weight management and quality of life among working-age females. Scand. J. Prim. Health Care 2021 , 39 , 382–388. [ Google Scholar ] [ CrossRef ]
- Alexander, S.C.; Cox, M.E.; Boling Turer, C.L.; Lyna, P.; Østbye, T.; Tulsky, J.A.; Dolor, R.J.; Pollak, K.I. Do the five A’s work when physicians counsel about weight loss? Fam. Med. 2011 , 43 , 179–184. [ Google Scholar ]
- Braga, V.A.S.; Jesus, M.C.P.; Conz, C.A.; Tavares, R.E.; Silva, M.H.D.; Merighi, M.A.B. Nursing interventions with people with obesity in Primary Health Care: An integrative review. Rev. Esc. Enferm. USP 2017 , 51 , e03293. [ Google Scholar ] [ CrossRef ]
- Jay, M.; Gillespie, C.; Schlair, S.; Sherman, S.; Kalet, A. Physicians’ use of the 5As in counseling obese patients: Is the quality of counseling associated with patients’ motivation and intention to lose weight? BMC Health Serv. Res. 2010 , 10 , 159. [ Google Scholar ] [ CrossRef ]
- Ogunleye, A.; Osunlana, A.; Asselin, J.; Cave, A.; Sharma, A.M.; Campbell-Scherer, D.L. The 5As team intervention: Bridging the knowledge gap in obesity management among primary care practitioners. BMC Res. Notes 2015 , 8 , 810. [ Google Scholar ] [ CrossRef ]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic ; Report of a WHO Consultation on Obesity; World Health Organization: Geneva, Switzerland, 1998. [ Google Scholar ]
- European Association for the Study of Obesity. Environmental Scan of Obesity Care Policies and Strategies for Adults in Europe 2020 ; European Association for the Study of Obesity: London, UK, 2020. [ Google Scholar ]
- Luli, M.; Yeo, G.; Farrell, E.; Ogden, J.; Parretti, H.; Frew, E.; Bevan, S.; Brown, A.; Logue, J.; Menon, V.; et al. The implications of defining obesity as a disease: A report from the Association for the Study of Obesity 2021 annual conference. EClinicalMedicine 2023 , 58 , 101962. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Executive Summary. NHLBI Obesity Education Initiative Expert Panel. Available online: https://www.ncbi.nlm.nih.gov/books/NBK2008/ (accessed on 17 July 2024).
- Allison, D.B.; Downey, M.; Atkinson, R.L.; Billington, C.J.; Bray, G.A.; Eckel, R.H.; Finkelstein, E.A.; Jensen, M.D.; Tremblay, A. Obesity as a disease: A white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obesity 2008 , 16 , 1161–1177. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- American Medical Association. Proceedings of the 2013 Annual Meeting of the House of Delegates. 162nd Annual Meeting; AMA: Chicago, IL, USA, 2013. Available online: https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/hod/a13-resolutions_0.pdf (accessed on 12 July 2024).
- Bray, G.A.; Kim, K.K.; Wilding, J.P.H. Obesity: A chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 2017 , 18 , 715–723. [ Google Scholar ] [ CrossRef ]
- Burki, T. European Commission classifies obesity as a chronic disease. Lancet Diabetes Endocrinol. 2021 , 9 , 418. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tham, K.W.; Abdul Ghani, R.; Cua, S.C.; Deerochanawong, C.; Fojas, M.; Hocking, S.; Lee, J.; Nam, T.Q.; Pathan, F.; Saboo, B.; et al. Obesity in South and Southeast Asia-A new consensus on care and management. Obes. Rev. 2023 , 24 , e13520. [ Google Scholar ] [ CrossRef ]
- De Lorenzo, A.; Gratteri, S.; Gualtieri, P.; Cammarano, A.; Bertucci, P.; Di Renzo, L. Why primary obesity is a disease? J. Transl. Med. 2019 , 17 , 169. [ Google Scholar ] [ CrossRef ]
- Heshka, S.; Allison, D.B. Is obesity a disease? Int. J. Obes. 2001 , 25 , 1401–1404. [ Google Scholar ] [ CrossRef ]
- Stunkard, A.J. Current views on obesity. Am. J. Med. 1996 , 100 , 230–236. [ Google Scholar ] [ CrossRef ]
- Vallgårda, S.; Nielsen, M.E.J.; Hansen, A.K.K.; Cathaoir, K.Ó.; Hartlev, M.; Holm, L.; Christensen, B.J.; Jensen, J.D.; Sørensen, T.I.A.; Sandøe, P. Should Europe follow the US and declare obesity a disease?: A discussion of the so-called utilitarian argument. Eur. J. Clin. Nutr. 2017 , 71 , 1263–1267. [ Google Scholar ] [ CrossRef ]
- Aboueid, S.; Ahmed, R.; Jasinska, M.; Pouliot, C.; Hermosura, B.J.; Bourgeault, I.; Giroux, I. Weight Communication: How Do Health Professionals Communicate about Weight with Their Patients in Primary Care Settings? Health Commun. 2022 , 37 , 561–567. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Smolowitz, J.; Speakman, E.; Wojnar, D.; Whelan, E.M.; Ulrich, S.; Hayes, C.; Wood, L. Role of the registered nurse in primary health care: Meeting health care needs in the 21st century. Nurs. Outlook 2015 , 63 , 130–136. [ Google Scholar ] [ CrossRef ]
- Davis, K.M.; Eckert, M.C.; Hutchinson, A.; Harmon, J.; Sharplin, G.; Shakib, S.; Caughey, G.E. Effectiveness of nurse–led services for people with chronic disease in achieving an outcome of continuity of care at the primary-secondary healthcare interface: A quantitative systematic review. Int. J. Nurs. Stud. 2021 , 121 , 103986. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Holloway, D.; James, S.; Ekinci, E.; Craft, J. Systematic review of the effectiveness of nurse-led care in reducing glycated haemoglobin in adults with Type 1 or 2 diabetes. Int. J. Nurs. Pract. 2023 , 29 , e13135. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Miao, J.-H.; Wang, H.-S.; Liu, N. The evaluation of a nurse-led hypertension management model in an urban community healthcare: A randomized controlled trial. Medicine 2020 , 99 , e20967. [ Google Scholar ] [ CrossRef ]
- Herrmann-Werner, A.; Loda, T.; Wiesner, L.M.; Erschens, R.S.; Junne, F.; Zipfel, S. Is an obesity simulation suit in an undergraduate medical communication class a valuable teaching tool? A cross-sectional proof of concept study. BMJ Open 2019 , 9 , e029738. [ Google Scholar ] [ CrossRef ]
- Mayer-Brown, S.; Basch, M.C.; Robinson, M.E.; Janicke, D.M. Impact of child and maternal weight on healthcare trainee clinical assessment decision making: A virtual human study. Child. Obes. 2019 , 15 , 63–70. [ Google Scholar ] [ CrossRef ]
- Tanneberger, A.; Ciupitu-Plath, C. Nurses’ Weight Bias in Caring for Obese Patients: Do Weight Controllability Beliefs Influence the Provision of Care to Obese Patients? Clin. Nurs. Res. 2018 , 27 , 414–432. [ Google Scholar ] [ CrossRef ]
- Ryan, L.; Coyne, R.; Heary, C.; Birney, S.; Crotty, M.; Dunne, R.; Conlan, O.; Walsh, J.C. Weight stigma experienced by patients with obesity in healthcare settings: A qualitative evidence synthesis. Obes. Rev. 2023 , 24 , e13606. [ Google Scholar ] [ CrossRef ]
- Telo, G.H.; Friedrich Fontoura, L.; Avila, G.O.; Gheno, V.; Bertuzzo Brum, M.A.; Teixeira, J.B.; Erthal, I.N.; Alessi, J.; Telo, G.H. Obesity bias: How can this underestimated problem affect medical decisions in healthcare? A systematic review. Obes. Rev. 2024 , 25 , e13696. [ Google Scholar ] [ CrossRef ]
- Garcia, J.T.; Amankwah, E.K.; Hernandez, R.G. Assessment of Weight Bias Among Pediatric Nurses and Clinical Support Staff Toward Obese Patients and Their Caregivers. J. Pediatr. Nurs. 2016 , 31 , e244–e251. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McHale, C.T.; Laidlaw, A.H.; Cecil, J.E. Primary care patient and practitioner views of weight and weight-related discussion: A mixed-methods study. BMJ Open 2020 , 10 , e034023. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ringel, M.M.; Ditto, P.H. The moralization of obesity. Soc. Sci. Med. 2019 , 237 , 112399. [ Google Scholar ] [ CrossRef ]
- Torres-Carot, V.; Suárez-González, A.; Lobato-Foulques, C. The energy balance hypothesis of obesity: Do the laws of thermodynamics explain excessive adiposity? Eur. J. Clin. Nutr. 2022 , 76 , 1374–1379. [ Google Scholar ] [ CrossRef ]
- Masood, B.; Moorthy, M. Causes of obesity: A review. Clin. Med. 2023 , 23 , 284–291. [ Google Scholar ] [ CrossRef ]
- Sternson, S.M.; Eiselt, A.K. Three Pillars for the Neural Control of Appetite. Annu. Rev. Physiol. 2017 , 79 , 401–423. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kanmiki, E.W.; Fatima, Y.; Mamun, A.A. Multigenerational transmission of obesity: A systematic review and meta-analysis. Obes. Rev. 2022 , 23 , e13405. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gupta, R.; Kumar, P.; Fahmi, N.; Garg, B.; Dutta, S.; Sachar, S.; Matharu, A.S.; Vimaleswaran, K.S. Endocrine disruption and obesity: A current review on environmental obesogens. Curr. Res. Green Sustain. Chem. 2020 , 3 , 100009. [ Google Scholar ] [ CrossRef ]
- Safaei, M.; Sundararajan, E.A.; Driss, M.; Boulila, W.; Shapi’i, A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput. Biol. Med. 2021 , 136 , 104754. [ Google Scholar ] [ CrossRef ]
- Mojkowska, A.; Sobczak, K.; Leoniuk, K.; Henzler, M.; Jackowski, M. Medical or Common Knowledge? Knowledge of Medical Professionals on Obesity Diagnosis Criteria and Treatment. Obes. Facts 2023 , 16 , 216–223. [ Google Scholar ] [ CrossRef ]
- Vallis, M.; Piccinini-Vallis, H.; Sharma, A.M.; Freedhoff, Y. Clinical review: Modified 5 As: Minimal intervention for obesity counseling in primary care. Can. Fam. Physician 2013 , 59 , 27–31. [ Google Scholar ] [ PubMed ]
- Rueda-Clausen, C.F.; Benterud, E.; Bond, T.; Olszowka, R.; Vallis, M.T.; Sharma, A.M. Effect of implementing the 5As of obesity management framework on provider-patient interactions in primary care. Clin. Obes. 2014 , 4 , 39–44. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sharma, A.M. M, M, M & M: A mnemonic for assessing obesity. Obes. Rev. 2010 , 11 , 808–809. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Berring, L.L.; Holm, T.; Hansen, J.P.; Delcomyn, C.L.; Søndergaard, R.; Hvidhjelm, J. Implementing Trauma-Informed Care—Settings, Definitions, Interventions, Measures, and Implementation across Settings: A Scoping Review. Healthcare 2024 , 12 , 908. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Inclusion | Exclusion | |
|---|---|---|
| Population | Registered nurses Case management nurses General practice nurses | Student nurses Advanced practice nurses Nurse practitioner (NP) Clinical nurse specialist (CNS) Certified Registered Nurse Anesthetist (CRNA) Certified Nurse Midwife (CNM) |
| Concept | Individuals with obesity Adults (19–64 years old) Nurses’ role or intervention | RN’s role indecipherable from other disciplines Primary focus on other disease (e.g., cancer, serious mental illness, NAFLD, T2DM, etc.) Bariatric and pharmaceutical related interventions Population who requires expertise beyond scope of this paper (i.e., perinatal, postnatal, prenatal, and parenting and people with developmental, and intellectual disabilities) |
| Context | Worldwide Primary healthcare setting District nursing General practice Community settings (home care, occupational health, or faith-based) | Any setting outside inclusion criteria |
| Medical Subject Headings (MeSHs) and Descriptors | String/ Boolean | Keywords (Title or Abstract) | |
|---|---|---|---|
| Population | “nurses” OR “nursing” OR “Public Health Service Nurses” | Or | nurs* |
| And | |||
| Concept | “role” OR “Nursing Role” OR “Nursing Interventions” OR “Professional Role” OR “Delivery of Health Care” OR “Practice Patterns, Nurses” OR | Or | role* or “nurs* intervention*” OR “nurs* strateg*” OR “nurs* role” OR “nurs* guided” OR “nurse-directed” OR “nurse-led” OR “nurse-managed” OR “nurs* function*” |
| And | |||
| “obesity” OR “Obesity, Morbid” OR “weight control” OR “Weight Reduction Programs” OR “weight management” OR “obesity management” OR “Body Weight Maintenance” OR “Body Weight Changes” OR “weight loss+” OR “Weight Reduction Programs+” OR “Body Weight” OR “overweight” OR “body mass index” OR “Obesity (Attitudes Toward)” | Or | obes* OR “high BMI” OR “high body mass index” OR “weight control” OR “weight reduction” OR “weight management” OR “overweight” | |
| Context | Omitted (too restrictive) | Omitted (too restrictive) | |
| Frist Author/Year/Citation | Title | Study Design | Population | Setting | Country | |
|---|---|---|---|---|---|---|
| Barrea (2021) [ ] | The role of the nurse in the obesity clinic: a practical guideline. | Review | RNs caring for people living with obesity (PwO) | Outpatient obesity clinics | Italy | |
| Braga (2020) [ ] | Actions of nurses toward obesity in primary health care units. | Qualitative | Primary healthcare nurses (PHNs) | Primary healthcare Units | Brazil | |
| Brewah (2018) [ ] | Can community nurses take on obesity? | Commentary | District/ community RNs caring for homebound PwO | Home care | U.K. | |
| Campbell- Scherer (2019) [ ] | Changing provider behaviour to increase nurse visits for obesity in family practice: the 5As Team randomized controlled trial (RCT). | Mixed-methods, RCT, and qualitative | Chronic disease RNs in a primary care clinic providing care for PwO | Primary care network clinics | Canada | |
| Fernández- Ruiz (2018) [ ] | Short-medium-long-term efficacy of interdisciplinary intervention against overweight and obesity: randomized controlled clinical trial. | RCT | Multidisciplinary program for PwO led and coordinated by RNs | Community care centre | Spain | |
| Fernández- Ruiz (2018) [ ] | Impact of the I(2)AO(2) interdisciplinary program led by nursing on psychological comorbidity and quality of life: randomized controlled clinical trial. | RCT | Multidisciplinary program for PwO led and coordinated by RNs | Community care centre | Spain | |
| Govindasamy (2023) [ ] | Experiences of overweight and obese patients with diabetes and practice nurses during implementation of a brief weight management intervention in general practice settings serving culturally and linguistically diverse disadvantaged populations. | Qualitative | RNs PwO who are culturally and linguistically diverse with socioeconomic disadvantage | General practice office | Australia | |
| Hinks (2022) [ ] | Exploring community nurses’ views on the implementation of a local weight management pathway. | Qualitative | District and community RNs | Community care | Isle of Man | |
| Kelley (2018) [ ] | The role of the faith community nurse in weight management. | Opinion | Faith community RNs providing care for PwO | Faith community setting (church) | USA | |
| Palmeira (2019) [ ] | Effect of remote nursing monitoring on overweight in women: clinical trial. | RCT | RNs providing remote weight monitoring for PwO | Primary care Remote nursing | Brazil | |
| Parker | 2018 [ ] | Preventing chronic disease in patients with low health literacy using eHealth and teamwork in primary healthcare: protocol for a cluster randomised controlled trial. | Protocol | RNs caring for PwO | General practice | Australia |
| 2022 [ ] | Preventing chronic disease in overweight and obese patients with low health literacy using eHealth and teamwork in primary healthcare (HeLP-GP): a cluster randomised controlled trial. | RCT | RNs caring for PwO | General practice | Australia | |
| 2024 [ ] | Exploring organisational readiness to implement a preventive intervention in Australian general practice for overweight and obese patients: key learnings from the HeLP-GP trial. | Qualitative | RNs caring for PwO | General practice | Australia | |
| Shaji et al. (2023) [ ] | Effectiveness of nurse-led lifestyle modification intervention on obesity among young women in India. | Quantitative | RN caring for PwO | General practice office and telehealth | India | |
| Virtanen (2021) [ ] | The impact of lifestyle counselling on weight management and quality of life among working-age females. | Quantitative cohort study | RNs caring for PwO | Primary healthcare | Finland | |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Piwowarczyk, E.; MacPhee, M.; Howe, J. Nurses’ Role in Obesity Management in Adults in Primary Healthcare Settings Worldwide: A Scoping Review. Healthcare 2024 , 12 , 1700. https://doi.org/10.3390/healthcare12171700
Piwowarczyk E, MacPhee M, Howe J. Nurses’ Role in Obesity Management in Adults in Primary Healthcare Settings Worldwide: A Scoping Review. Healthcare . 2024; 12(17):1700. https://doi.org/10.3390/healthcare12171700
Piwowarczyk, Emilia, Maura MacPhee, and Jo Howe. 2024. "Nurses’ Role in Obesity Management in Adults in Primary Healthcare Settings Worldwide: A Scoping Review" Healthcare 12, no. 17: 1700. https://doi.org/10.3390/healthcare12171700
Article Metrics
Article access statistics, supplementary material.
ZIP-Document (ZIP, 296 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Rising incidence of obesity-related cancers among younger adults in China: A population-based analysis (2007-2021)
Affiliations.
- 1 Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University, Beijing 100730, China; Beijing Diabetes Institute, Beijing 100730, China; Beijing Key Laboratory of Diabetes Research and Care, Laboratory for Clinical Medicine, Capital Medical University, Beijing 100069, China.
- 2 Beijing Municipal Health Big Data and Policy Research Center, Beijing 100034, China.
- 3 The Center for Research on Genomics and Global Health, National Human Genome Research Institute, National Institutes of Health, Bethesda, MD 20892, USA.
- 4 Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University, Beijing 100730, China; Beijing Diabetes Institute, Beijing 100730, China; Beijing Key Laboratory of Diabetes Research and Care, Laboratory for Clinical Medicine, Capital Medical University, Beijing 100069, China. Electronic address: [email protected].
- PMID: 39181132
- DOI: 10.1016/j.medj.2024.07.012
Background: Developing countries face an "obesity epidemic," particularly affecting children and younger adults. While obesity is a known risk factor for 12 types of cancer, primarily affecting older populations, its impact on younger generations is understudied.
Methods: This study analyzed data from a population-based cancer registry covering 14.14 million individuals in China (2007-2021). We compared the incidence of obesity- and non-obesity-related cancers and applied an age-period-cohort model to estimate their impacts.
Findings: Among 651,342 cancer cases, 48.47% were obesity related. The age-standardized incidence rates (ASRs) of the 12 obesity-related cancers increased annually by 3.6% (p < 0.001), while ASRs for non-obesity-related cancers remained stable. Obesity-related cancers surged among younger adults, with rates rising across successive generations. The annual percentage of change decreased with age, from 15.28% for ages 25-29 years to 1.55% for ages 60-64 years. The incidence rate ratio for obesity-related cancer was higher in younger generations compared to those born in 1962-1966. We predict that the ASR for obesity-related cancers will nearly double in the next decade.
Conclusions: The rising incidence of obesity-related cancers among young adults poses a significant public health concern. The increasing cancer burden underscores the need for targeted interventions to address the obesity epidemic.
Funding: This work was supported by the National Natural Science Foundation of China (81930019, 82341076) to J.-K.Y.
Keywords: Translation to population health.
Copyright © 2024 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of interests The authors declare no competing interests.
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals
You are here
- Volume 14, Issue 8
- Comparing long-term prognosis following different surgical methods in patients with early stage breast cancer and obesity: a retrospective cohort study in China
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Lun Li 1 , 2 , 3 ,
- http://orcid.org/0000-0002-8343-065X Jian Pang 1 , 3 ,
- Yiqing Yan 1 , 3 ,
- Qi Zhang 2 ,
- Shuyue Zheng 2 ,
- Ming Chen 2 ,
- Wenjun Yi 1 , 3 ,
- http://orcid.org/0000-0002-8103-0505 Jiong Wu 2 , 4
- 1 Department of General Surgery , The Second Xiangya Hospital, Central South University , Changsha , China
- 2 Department of Breast Surgery , Fudan University Shanghai Cancer Center , Shanghai , China
- 3 Clinical Research Center for Breast Disease in Hunan Province , Changsha , China
- 4 Collaborative Innovation Center for Cancer Medicine , Shanghai , China
- Correspondence to Professor Jiong Wu; wujiong1122{at}vip.sina.com ; Professor Wenjun Yi; yiwenjun{at}csu.edu.cn
Objective Breast-conserving therapy (BCT) includes breast-conserving surgery (BCS) combined with radiation therapy (RT). RT plays a crucial role in improving the prognosis of patients who undergo BCS. However, obesity is a potential risk factor for resistance to radiation. The aim of this study was to evaluate any difference in the long-term prognosis of patients with early stage breast cancer and obesity treated with BCT or total mastectomy (TM).
Design, setting and participants This was a retrospective cohort study involving 1125 patients diagnosed with early stage breast cancer and obesity at the Shanghai Cancer Center of Fudan University from 2013 to 2016.
Outcome measures Obesity in the Chinese population was defined as a body mass index ≥28 kg/m 2 . Surgical options included BCT and TM. The primary survival outcomes were overall survival (OS), disease-free survival (DFS) and recurrence-free survival (RFS). Inverse probability of treatment weighting (IPTW) was used to control for the impact of confounding factors on prognosis.
Results The median follow-up times in the BCT group and TM group without postoperative RT were 51.1 months (IQR of 40.6–68.1 months) and 61.8 months (IQR of 46.5–76.7 months), respectively. After IPTW, the baseline data were balanced. Compared with those in the TM cohort, patients in the whole IPTW cohort in the BCT cohort had worse DFS (HR 4.280, 95% CI 2.180 to 8.400; p<0.001), RFS (HR 4.380, 95% CI 2.370 to 8.120; p<0.001) and OS (HR 3.590, 95% CI 1.620 to 7.950; p=0.002).
Conclusion In patients with early stage breast cancer and obesity, TM is associated with better survival outcomes than BCT.
- Breast tumours
- Breast surgery
- Retrospective Studies
Data availability statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author, JW, upon reasonable request. The data are not publicly available since this could compromise the privacy of the research participants.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-078816
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This was a large cohort study on the surgical approach and survival duration of patients with early stage breast cancer and obesity.
This study was based on a retrospective cohort study of Chinese patients.
It is necessary to further investigate the robustness and generalisability of the findings by conducting prospective studies and including other populations.
Introduction
In recent years, the global prevalence of obesity has rapidly increased, leading to a global epidemic. 1 Over the past three decades, the number of individuals with obesity worldwide has more than doubled, with an estimated 1.9 billion overweight or obese adults. 2 3 Obesity is among the top five causes of global mortality and accounts for 5% of all deaths. 4 Furthermore, it is recognised as a risk factor for various malignancies, including breast cancer. 5 Obesity, as measured by body mass index (BMI), is associated with poorer disease-specific survival, disease-free survival (DFS) and overall survival (OS) in patients with breast cancer. 6–9 It increases the risk of local or regional breast cancer recurrence and may influence prognosis through its effects on systemic and local therapy. In patients with obesity, systemic treatment can improve local control of breast cancer, whereas ineffective systemic treatment may increase the risk of local recurrence. 10 The detrimental effects of obesity on local control may lead to worse breast cancer-specific survival and/or DFS, as improved local control after radiation therapy (RT) has been shown to increase breast cancer-specific survival. 10
Breast-conserving therapy (BCT), consisting of breast tumour excision and local RT, is employed for invasive breast cancer and ductal carcinoma in situ. Previous studies have shown no difference in long-term prognosis between BCT and total mastectomy (TM). 11 12 Additionally, RT reduces the long-term risk of local recurrence. 13 Indeed, RT has long been used to treat various malignancies, including breast cancer, and has been shown to significantly improve patient survival. 14 However, resistance to RT, which is characterised by the absence of a response of some cancer cells to radiation, remains a major challenge. 14 Obesity is considered a risk factor for radiation resistance and metastasis, and overall poor prognosis in patients with breast cancer. 15–17 If women receiving whole-breast RT have two or more breast cancer risk factors, including obesity, the likelihood of developing regional recurrence increases by 12.6% after 5 years. 18 Obesity-induced radiation resistance may arise through mechanisms involving DNA repair and adipose-derived stem cells. 11 19
Therefore, RT plays a critical role in breast-conserving surgery (BCS), with obesity being a risk factor for radiation resistance. The choice between BCT and TM in patients with obesity and early stage breast cancer still needs further clarification. Accordingly, we conducted a retrospective analysis of 1125 patients with early stage breast cancer and obesity who received treatment at the Shanghai Cancer Center of Fudan University from 2013 to 2016 to compare long-term prognoses following different surgical methods.
Data sources and study design
In this study, which was conducted at the Shanghai Cancer Center of Fudan University, a total of 18 700 patients were recruited between 2013 and 2016. The patient population had a BMI ranging from 12.9 kg/m 2 to 39.13 kg/m 2 . Of the entire cohort, 1125 patients were early stage breast cancer with obesity, accounting for 6% of the overall population. To be included in this study, the patients met specific inclusion criteria, including primary breast cancer without metastasis, clinical stage T 1–2 N 0 M 0 , and no prior neoadjuvant therapy, such as chemotherapy, RT, or endocrine therapy. Furthermore, they did not have serious complications arising from conditions such as hypertension, diabetes mellitus or other underlying diseases.
All patients underwent diagnostic mammography and ultrasonography to identify any additional calcifications or masses. To be eligible for BCS, the surgical margins had to be negative. In cases in which positive margins were observed, wider resection ensured that the distance between the margin and the lesion was ≥5 mm. Patients eligible for BCS had singular or limited localised lesions that could be completely excised according to predetermined criteria. In addition, all patients who underwent BCS expressed a strong desire to preserve their breasts and agreed to postoperative RT. Patients with multicentric lesions, nipple involvement (such as Paget’s disease of the nipple), active connective tissue disease with poor radiotherapy tolerance, or unwillingness to receive RT for personal or economic reasons are typically recommended to undergo TM.
Laboratory data
Immunohistochemistry (IHC) was performed on tumour samples using an IHC staining module that specifically targeted oestrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2). The IHC results were evaluated by a breast pathologist and further reviewed by senior experts. Clinical and pathological staging was performed according to the guidelines outlined in the American Joint Committee on Cancer Staging Manual, eighth edition. 20 HER2 positivity was determined based on IHC or fluorescence in situ hybridisation positivity. oestrogen receptor and PR were considered positive when expressed in 1% or more of the cells of a section; Ki67 was classified as high if 14% or more of the cells of a section stained positive.
Ethics and consent
This research complied with the Declaration of Helsinki. All patients provided informed consent when the database was constructed.
Definition of patients with obesity
According to the WHO, BMI for adults is 18.5 kg/m 2 <BMI≤24.9 kg/m 2 for normal weight, 25 kg/m 2 ≤BMI≤29.9 kg/m 2 for overweight, and≥30 kg/m 2 for obese. The standard was based on data from European and American populations. 21 Due to the differences in skeletal, height and muscle development between Asians and Europeans and Americans, reference standards for overweight and obesity boundary values suitable for the Chinese population have been proposed as follows: 18.5 kg/m 2 ≤BMI<24 kg/m 2 for normal weight, 24 kg/m 2 ≤BMI<28 kg/m 2 for overweight, and a BMI≥28 kg/m 2 for obese. In this study, with reference to the Chinese BMI obese population standard, BMI≥28 kg/m 2 was defined as obese. 22
Study endpoints
OS, DFS and recurrence-free survival (RFS) were the endpoints of this study. OS was defined as the time from the end of the diagnosis process to death from any cause. RFS was defined as the time from the end of the diagnosis process to tumour recurrence or the development of a new primary breast tumour. Finally, DFS was defined as the time from end of the diagnosis process to the time of tumour recurrence, metastasis or death from any cause.
Data integration and statistical methods
Descriptive statistics or columns are used to summarise patient demographic and baseline characteristics. Differences in clinicopathological characteristics between groups were assessed using the χ 2 test or Fisher’s exact test.
To account for selection bias and potential confounding factors between groups, a propensity model was constructed using the inverse probability of treatment weighting (IPTW) approach. The weight of each patient was determined based on the inverse probability of belonging to the TM group compared with the BCS group, aiming to achieve a balance in observed characteristics, such as menopausal status, tumour grade, pathological T stage, pathological N stage and PR status.
Survival curves were constructed using the Kaplan‒Meier (KM) method, and the log-rank test was used to compare survival between groups. HRs with 95% CIs were estimated using Cox proportional hazards regression analysis.
The R programming language (V.4.1.3) was employed for data analysis and graphical plotting. A value of p<0.05 was considered to indicate statistical significance for all statistical analyses.

Patient and public involvement
Clinical baseline information of patients with obesity in the tm and bcs groups.
The study flow chart of our investigation is presented in online supplemental figure 1 . Patients were divided into two groups according to the surgical intervention they received: the TM group and the BCS group. In the TM group, 885 patients had a median BMI of 29.0 (IQR 28.0–30.0) kg/m 2 and a median follow-up time of 61.1 (IQR 46.2–77.7) months. In the BCS group, 240 patients had a median BMI of 29.0 (IQR 28.0–30.3) kg/m 2 and a median follow-up time of 50.7 (IQR 40.9–66.9) months. Among the patients who underwent TM treatment, 185 received RT. A total of 176 patients who underwent BCS completed postoperative RT. The specific indications for radiotherapy and the corresponding strategies were evaluated by a radiation oncologist for a more standardised approach. However, 35 patients refused RT due to external or uncontrollable factors, and no records were available for 34 patients.
Supplemental material
Online supplemental table 1 displays the clinical and pathological characteristics of the patients with obesity before and after IPTW. Before IPTW, a greater percentage of premenopausal patients were in the BCS group (36.2% vs 29.5%, p=0.045), had a grade 1 tumour (54.6% vs 53.9%, p<0.001), had a pathological T 1 stage (67.1% vs 52.8%, p<0.001), had a pathological N 0 stage (82.1% vs 69.3%, p<0.001), and were PR positive (73.8% vs 66.9%, p=0.043) than in the TM group. After IPTW, menopausal status, tumour grade, pathological T stage, pathological N stage and PR status were balanced between the groups (all p>0.050) ( online supplemental table 1 ).
Survival analyses of patients with obesity in the TM and BCS groups
In the TM group, there were 34 deaths (4.0%) and 36 cases of local recurrence or distant metastasis (4.2%). In the BCS group, 15 patients died (6.3%), and 21 patients experienced local recurrence or distant metastasis (8.8%). The 3-year, 5-year and 7-year DFS rates of the TM group were 98.3%, 95.5 and 91.7%, respectively, and 96.9%, 88.8% and 79.4% in the BCS group, respectively ( figure 1A ). The 3-year, 5-year and 7-year RFS rates in the TM group were 99.2%, 97.5% and 94.0%, respectively; in the BCS group, they were 97.8%, 91.3% and 81.7%, respectively ( figure 1B ). The 3-year, 5-year and 7-year OS rates of the TM group were 98.4%, 96.9% and 95.4%, respectively; they were 97.4%, 93.0% and 88.6% in the BCS group, respectively ( figure 1C ). Therefore, patients in the TM group had superior outcomes to those in the BCS group in terms of DFS, RFS and OS.
- Download figure
- Open in new tab
- Download powerpoint
Kaplan‒Meier (KM) curves of (A) DFS, (B) RFS and (C) OS in patients with obesity who underwent different surgical approaches before and after IPTW. BCS, breast-conserving surgery; DFS, disease-free survival; IPTW, inverse probability of treatment weighting; OS, overall survival; RFS, relapse-free survival; TM, total mastectomy.
After IPTW, the TM group still exhibited significantly better DFS, RFS and OS than did the BCS group (p<0.001, p<0.001 and p=0.009, respectively) ( figure 1A–1C ).
Factors affecting the prognosis of the population with obesity
After IPTW, the results of multivariate analysis showed that HER2 status (positive vs negative: HR 0.350, 95% CI 0.150 to 0.820, p=0.015) and surgical procedure (BCS vs TM: HR 3.390, 95% CI 2.090 to 5.520, p<0.001) were independent predictive factors for DFS ( online supplemental table 2 ). As indicated in online supplemental table 3 , HER2 status (positive vs negative: HR 0.270, 95% CI 0.120 to 0.590, p=0.001), adjuvant hormonal therapy (yes vs no: HR=0.290, 95% CI 0.180 to 0.490, p<0.001) and surgical procedure (BCS vs TM: HR=4.440, 95% CI 2.630 to 7.520, p<0.001) were independent predictive factors for RFS. Furthermore, as shown in online supplemental table 4 , menopausal status (postmenopausal vs premenopausal: HR 4.400, 95% CI 1.730 to 11.200, p=0.002), pathological T stage (T 2 vs T 1 : HR 3.090, 95% CI 1.520 to 6.270, p=0.002) and surgical procedure (BCS vs TM: HR 2.860, 95% CI 1.410 to 5.790, p=0.004) were independent predictive factors for OS.
Survival analyses of patients with obesity in the BCS group, BCS+RT group, and TM group without postoperative RT
To explore prognostic differences between patients with obesity treated with BCS or TM, we further performed survival prognostic analyses on three groups of 700 patients treated with TM without postoperative RT, 35 patients treated with BCS but not receiving RT due to external factors, and 176 treated with BCS and receiving postoperative RT. In the TM group, 700 patients had a median BMI of 29.0 (IQR 28.0–30.0) kg/m 2 and a median follow-up time of 61.8 (IQR 46.5–76.7) months. In the BCS group, 35 patients had a median BMI of 29.0 (IQR 28.0–31.0) kg/m 2 and a median follow-up time of 52.1 (IQR 45.1–61.9) months. In the BCS+RT group, 176 patients had a median BMI of 29.0 (IQR 28.0–30.0) kg/m 2 and a median follow-up time of 51.1 (IQR 40.6–68.1) months.
Online supplemental table 5 lists the baseline characteristics of these patients. Compared with those in the TM group and the BCS group without postoperative RT, a greater percentage of patients in the BCS+RT group were under 60 years old, were premenopausal, had a tumour grade of 1 and received adjuvant chemotherapy.
In the TM group, there were 20 deaths (2.9%) and 21 cases of local recurrence or distant metastasis (3.0%). In the BCS group, three patients died (8.6%), and four experienced local recurrence or distant metastasis (11.4%). In the BCS+RT group, there were 11 deaths (6.3%) and 15 cases of local recurrence or distant metastasis (8.5%). Survival analysis demonstrated that the TM group had better 3-year, 5-year and 7-year DFS rates (98.7%, 96.3% and 93.0%, respectively) than the BCS without RT group (97.1%, 76.1%, 76.1%) and the BCS with RT group (96.4%, 92.0%, 79.7%) ( figure 2A ). Moreover, the TM group had higher 3-year, 5-year and 7-year RFS rates (99.4%, 98.2% and 94.8%, respectively) than the BCS without RT group (97.1%, 79.2%, 79.2%) and the BCS with RT group (97.6%, 94.0%, 81.4%) ( figure 2B ). Additionally, the 3-year, 5-year and 7-year OS rates were higher (98.7%, 97.5% and 96.8%, respectively) than those of the BCS without RT group (97.1%, 86.5%, 86.5%) and the BCS with RT group (97.0%, 93.9%, 88.2%) ( figure 2C ). These findings suggest that adding adjuvant RT in combination with BCS can improve DFS, RFS and OS. Furthermore, the prognosis of BCS patients with obesity, even after the addition of postoperative RT, remains lower than that of patients who undergo TM without postoperative RT.
Kaplan‒Meier (KM) curves of (A) DFS, (B) RFS and (C) OS in patients with obesity who underwent different surgical approaches BCS, breast-conserving surgery; DFS, disease-free survival; OS, overall survival; RT, radiation therapy; RFS, relapse-free survival; TM, total mastectomy.
Survival analyses of patients with obesity in the BCS+RT group and TM group without postoperative RT
We performed subgroup analysis to further explore the value of BCS with RT versus TM for determining the prognosis of patients with obesity. Table 1 describes differences in baseline characteristics between the BCS+RT group and TM group without postoperative RT. Before IPTW, we observed that among patients undergoing BCS treatment, there were higher proportions of individuals younger than 60 years old, premenopausal status, tumour grade 1, pathological stage T 1 , ER−/PR−/HER2− subtype, and ER+ or PR+/HER2+ subtype compared with the TM group. However, the effect of these potential confounders was neutralised after IPTW (all p>0.05), suggesting that the groups were balanced in terms of these characteristics.
- View inline
Clinical and pathological characteristics of patients with obesity in the BCS+RT group and TM group without postoperative RT
Survival analysis revealed that the 3-year, 5-year and 7-year DFS rates in the TM group were 98.7%, 96.3% and 93.0%, respectively, which were better than those in the BCS+RT group (96.4%, 92.0% and 79.7%, respectively) ( figure 3A ). The 3-year, 5-year and 7-year RFS rates in the TM group were also greater than those in the BCS+RT group (99.4%, 98.2% and 94.8%, respectively) (97.6%, 94.0%, 81.4%) ( figure 3B ). Furthermore, the 3-year, 5-year and 7-year OS rates in the TM group were 98.7%, 97.5% and 96.8%, respectively, which were superior to those in the BCS+RT group (97.0%, 93.9%, 88.2%) ( figure 3C ).
Kaplan‒Meier (KM) curves of (A) DFS, (B) RFS and (C) OS in the BCS+RT group and TM group without postoperative RT before and after IPTW. BCS, breast-conserving surgery; DFS, disease-free survival; IPTW, inverse probability of treatment weighting; OS, overall survival; RFS, relapse-free survival; RT, radiation therapy; TM, total mastectomy.
Prognostic factors of patients with obesity in the BCS+RT group and TM group without postoperative RT
After IPTW, multivariate analysis revealed several key factors that predicted different outcomes.
For DFS, pathological T stage (T 2 vs T 1 : HR 2.520, 95% CI 1.200 to 5.280, p=0.014), Ki67% (>14 vs ≤14: HR 3.420, 95% CI 1.270 to 9.250, p=0.015) and surgery (BCS with RT vs TM: HR 4.280, 95% CI 2.180 to 8.400, p<0.001) were identified as independent predictors ( table 2 ).
IPTW-adjusted univariate and multivariate analyses of the association between the DFS rate and clinical factors of patients with obesity in the BCS+RT group and TM group without postoperative RT
In addition, Ki67% (>14 vs ≤14: HR 2.960, 95% CI 1.010 to 8.730, p=0.049) and surgery type (BCS with RT vs TM: HR 4.380, 95% CI 2.370 to 8.120; p<0.001) were found to be independent factors for predicting RFS ( online supplemental table 6 ).
Furthermore, menopausal status (postmenopausal vs premenopausal: HR 7.790, 95% CI 2.420 to 25.080, p=0.001), tumour grade (2–3 vs 1: HR 3.360, 95% CI 1.030 to 10.990, p=0.045), pathological T stage (T 2 vs T 1 : HR 2.990, 95% CI 1.130 to 7.920, p=0.028), and surgery type (BCS with RT vs TM: HR 3.590, 95% CI 1.620 to 7.950, p=0.002) were independent predictors of OS ( online supplemental table 7 ).
Prognostic factors in patients without obesity
We further selected the overweight population (24 kg/m 2 ≤BMI<28 kg/m 2 ) and the population with normal weight (18.5 kg/m 2 ≤BMI<24 kg/m 2 ) from the patients with early stage breast cancer for analysis, in order to investigate the relationships between surgical methods, clinical pathological factors and prognosis. The baseline data for the population with normal weight and the population with overweight can be found in online supplemental tables 8 and 9 . After IPTW, the results of the multivariate analysis show that the surgical method is not an independent factor influencing DFS ( online supplemental tables 10 and 11 ), RFS ( online supplemental tables 12 and 13 ) or OS ( online supplemental tables 14 and 15 ), regardless of whether it is in the population with normal weight or the overweight population.
Survival analyses of the BCS+RT group and TM group in the total population
We finally plotted KM curves for patients undergoing BCS+RT and TM in different BMI populations, as shown in figure 4 . The results showed that patients with obesity who underwent BCS+RT treatment had the lowest prognostic outcomes, regardless of whether it was in terms of OS, DFS or RFS. In addition, ignoring the BMI factor, we further compared the survival benefits of BCS+RT treatment and TM treatment in the overall population. The results showed that there was no significant difference in the long-term survival benefits of patients between the two surgical methods ( online supplemental figure 2 ).
Kaplan‒Meier (KM) curves of (A) DFS, (B) RFS and (C) OS in the BCS+RT group and TM group among patients with different BMI levels. BCS, breast-conserving surgery; BMI, body mass index; DFS, disease-free survival; OS, overall survival; RFS, relapse-free survival; RT, radiation therapy; TM, total mastectomy.
Our study revealed that patients with early stage breast cancer and obesity who underwent TM achieved better DFS, RFS and OS than those who underwent BCS. Further analyses showed that BCS combined with RT was superior to BCS alone, but its prognosis was still inferior to that of TM. Furthermore, when comparing the prognostic differences between different surgical methods in the overall population, the results found no significant difference in long-term prognosis between TM and BCS plus RT if the distribution of BMI in the overall population is not considered. Additionally, when comparing the effects of different surgical methods on prognosis in the normal BMI and overweight populations, the results also found no significant prognostic difference between the different surgical approaches.
Current research concludes that there are no significant differences in long-term survival outcomes between the BCS+RT and TM treatment methods in early stage breast cancer. For instance, the results of two meta-analyses on the prognostic differences between the BCS+RT and TM treatment methods in early stage breast cancer showed no statistically significant differences in long-term prognostic outcomes such as OS, local recurrence rate and DFS rate between the BCS+RT and TM groups. 23 24 This is consistent with our research conclusions in the overall population.
However, to date, there has been little research focusing on obese patients with breast cancer, especially the long-term prognostic differences between the BCS+RT and TM treatment methods in the Chinese population. Our study found that in obese patients with breast cancer in China, the prognosis of the BCS+RT group is worse than that of the TM group. Further subgroup analysis found that radiotherapy resistance may be the reason why the treatment outcomes for patients with obesity undergoing BCS surgery are worse than those undergoing TM.
Rapiti et al reported that BCS is associated with worse prognosis than TM in patients with breast cancer but that BCS+RT is associated with better prognosis than TM. 25 Similar conclusions were reached by Guidolin et al , suggesting that adjuvant RT has a protective effect on recurrence and survival in patients with early stage breast cancer. 26 These findings suggest that RT may be a key factor influencing the long-term prognosis of patients treated with both surgical modalities. Moreover, obesity itself is a definitive adverse prognostic factor for early stage breast cancer. 27–29 Numerous studies have shown that obesity often leads to resistance to chemotherapy, endocrine therapy and RT. 30–35 Additionally, the influence of obesity on the pharmacokinetics and pharmacodynamics of anticancer drugs is multifaceted and variable. First, obesity can directly or indirectly affect the pharmacokinetics of small molecules and complex drugs (such as antibodies and antibody–drug conjugates) and alter metabolism of drugs in the liver and their elimination through the kidneys, thereby changing drug exposure in the blood, tissues and particularly in tumours. 36 Furthermore, obesity potentially impacts drug exposure by modifying the function and phenotype of the innate immune system. 37 Previous studies have found that BMI is a significant factor affecting the pharmacokinetics of drugs such as doxorubicin, cyclophosphamide, trastuzumab, tamoxifen and anastrozole. 38–42 As a result, the effects of obesity on pharmacokinetics might alter the efficacy and toxicity of anticancer drugs, making it a critical factor in determining prognosis. Although the causal mechanism by which obesity affects prognosis has yet to be determined, it is believed to be related to the biology of the disease or to poorer treatment outcomes in patients with obesity. 30 While RT reduces the risk of recurrence after BCS for breast cancer, its potential protective effects may diminish in patients with obesity. RT resistance significantly increases the risk of local recurrence, thus affecting the long-term survival of patients. However, the specific mechanisms of RT resistance in breast cancer remain unclear. Sabol et al discovered that adipose-derived stem cells altered by obesity promote radiation resistance in oestrogen receptor-positive breast cancer through paracrine signalling. 11 Su et al reported that ionising radiation induces DNA double-strand breaks (DSBs) and enhances Serpin Family E Member 1 (SERPINE1) expression in cancer cells in an Ataxia Telangiectasia Mutated/Ataxia Telangiectasia and Rad3-Related (ATM/ATR)-dependent manner, which promotes nuclear localisation of SERPINE1 and facilitates DSB repair. The link between obesity and RT resistance in triple-negative breast cancer has been revealed, with SERPINE1 identified as a key factor mediating RT resistance in obesity-associated tumours. 19
Therefore, the superior prognosis of patients who undergo TM compared with BCT is likely attributed to differences in RT resistance among patients with obesity. Considering the above conclusions, patients with early stage breast cancer and obesity who show RT resistance may benefit more from TM or breast reconstruction surgery. Nevertheless, clinical application of these findings requires validation through large-scale randomised experiments.
One of the strengths of this study is that we adopted measures to balance potential confounding factors. The baseline characteristics of patients in subgroups, such as age, pT stage, pN stage and PR status, were somewhat heterogeneous. Regardless, we confirmed the prognostic differences between different surgical methods using IPTW without compromising the sample size. This approach helps to reduce confounding bias or covariate imbalance.
Our study has several limitations. First, this was a retrospective study with a relatively small sample size and was conducted at a single centre. Second, our data lacked information on obesity-related complications such as diabetes and hypertension. We did not conduct subgroup analysis on additional dimensions, such as cholesterol level, which may provide a more refined definition of obesity. Patients with obesity often have comorbidities such as diabetes and hypertension, which may influence treatment choices and prognoses. Additionally, patients with diabetes prefer TM to BCS, but diabetes itself does not seem to influence the choice of RT among patients who undergo BCS. 43 Third, whether the impact of obesity on the pharmacokinetics of drugs will affect the conclusions of this study is still worth further exploration. Finally, this study used BMI standards for the Asian population to define obesity, which may limit the generalisability of the results. No similar studies have been performed in Asia, and further exploration through randomised experiments or retrospective analyses in other regions is needed.
In patients with early stage breast cancer and obesity, TM is associated with better survival outcomes than BCT.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This research was granted approval by the Ethics Committee of Shanghai Cancer Center, Fudan University (Shanghai, China; ID: 050432-4-1911D, 1905202–7), and complied with the Declaration of Helsinki.
- Mao B , et al
- Tremmel M ,
- Gerdtham UG ,
- Nilsson PM , et al
- Moccaldi M , et al
- Jiralerspong S ,
- Patterson RE ,
- Marinac CR ,
- Natarajan L , et al
- Guldberg TL ,
- Christensen S ,
- Zachariae R , et al
- Bedi M , et al
- Buchholz TA ,
- Tucker SL ,
- Erwin J , et al
- Villela VA ,
- Denys A , et al
- Zou Y , et al
- Sjöström M ,
- Fishbane N , et al
- McCall NS ,
- Simone BA ,
- Mehta M , et al
- Ahearn TU , et al
- Dibaba DT ,
- Ogunsina K ,
- Braithwaite D , et al
- Oh YT , et al
- Ann DK , et al
- Chmielik E ,
- Cserni B , et al
- De Jong A ,
- Deane AM , et al
- Wang H-J , et al
- Gao B , et al
- Li YP , et al
- Fioretta G ,
- Vlastos G , et al
- Guidolin K ,
- Vogt K , et al
- Trestini I ,
- Carbognin L ,
- Monteverdi S , et al
- Carroll J ,
- Protani M ,
- Walpole E , et al
- Dieras V , et al
- Kim S , et al
- Park SK , et al
- Shastri AA ,
- Lombardo J ,
- Okere SC , et al
- Feng LR , et al
- Ruffolo C ,
- Erroi F , et al
- Xu Y , et al
- Zamboni WC ,
- Charlab R ,
- Burckart GJ , et al
- Hendrikx JJMA ,
- Haanen JBAG ,
- Voest EE , et al
- Dilli Batcha JS ,
- Matcha S , et al
- Makonnen E ,
- Bisaso RK , et al
- Froehlich PE
- González García J ,
- Gutiérrez Nicolás F ,
- Nazco Casariego GJ , et al
- Hubalek M ,
- Oberguggenberger A ,
- Beer B , et al
- Lawrenson R ,
- Stanley J , et al
LL and JP contributed equally.
Contributors LL and JP: Conceptualisation, data curation, formal analysis, methodology, validation, writing—original draft. YY, QZ, SZ and MC: Investigation, resources, writing—review and editing. JW and WY: Conceptualisation, funding acquisition, investigation, resources, supervision, writing—original draft. The work reported in the article has been performed by the authors, unless clearly specified in the text. LL and JP contributed equally. JW is the guarantor.
Funding This study was funded by the Academic Leaders of Shanghai Science and Technology Commission (18XD1401300) and the Youth Program of the National Natural Science Foundation of China (82002797), the Changsha Natural Science Fundation (kq2208336), the Hunan Provincial Natural Science Fundation (2023JJ40831; 2023JJ60441), and the Scientific ResearchLaunch Project for new employees of the Second Xiangya Hospital of Central South University (2022- 086).
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Constance and Martin Silver Endowed Professor in Data Science and Prevention; Director, Constance and Martin Silver Center on Data Science and Social Equity
Areas of Expertise: Environmental influences and population-level interventions on obesity, weight-related behaviors and outcomes across the life course; Social and economic determinants and policies affecting physical, mental, and cognitive health in children, adults of all ages, and individuals with disabilities; Applications of artificial intelligence and data analytics for public health and social equity; Using data and statistical research methods to evaluate the effects of policies; Systematic review and meta-analysis to identify and appraise existing research.

Dr. Ruopeng An is a leading expert in obesity epidemiology and policy evaluation, a noted interdisciplinary data scientist, and an internationally recognized scholar in applying artificial intelligence to address public health disparities and social inequities.
He currently holds the Constance and Martin Silver Endowed Professorship in Data Science and Prevention and serves as the Director of the Constance and Martin Silver Center on Data Science and Social Equity. Dr. An is also an elected Fellow of the American Academy of Health Behavior and the American College of Epidemiology.
His research has been funded by various federal agencies and public/private organizations, including OpenAI, Abbott, and Amgen. Recognized as one of Elsevier’s top 2% most cited scientists, his work has been featured by major media outlets such as TIME , The New York Times , The Los Angeles Times , The Washington Post , Reuters , USA Today , Bloomberg , Forbes , The Atlantic , The Guardian , FOX, NPR , and CNN . He also serves on research grants and expert panels for the NIH, CDC, NSF, HHS, USDA, and the French National Research Agency.
Before joining NYU, Dr. An was the Faculty Lead in Public Health Sciences and Faculty Fellow for AI Innovations in Education at Washington University in St. Louis, where he also founded two certificate programs focused on artificial intelligence and data science.
Dr. An holds a PhD in Policy Analysis from the Pardee RAND Graduate School, a Master of Public Policy from the National Graduate Institute for Policy Studies, and a BA in Political Science and Public Administration from Peking University.
Recent Publications
An, R ., & Ji, M. (2023). Building Machine Learning Models to Correct Self-Reported Anthropometric Measures. Journal of Public Health Management and Practice , 29 (5), 671-674.
An, R ., Perez-Cruet, J., & Wang, J. (2024). We got nuts! use deep neural networks to classify images of common edible nuts. Nutrition and Health , 30 (2), 301-307.
An, R. , Perez-Cruet, J. M., Wang, X., & Yang, Y. (2024). Build Deep Neural Network Models to Detect Common Edible Nuts from Photos and Estimate Nutrient Portfolio. Nutrients , 16 (9), 1294.
An, R ., Yang, Y., Batcheller, Q., & Zhou, Q. (2023). Sentiment analysis of tweets on soda taxes. Journal of Public Health Management and Practice , 29 (5), 633-639.
Yang, Y., Lin, N., Batcheller, Q., Zhou, Q., Anderson, J., & An, R. (2023). Sentiment Analysis of Tweets on Menu Labeling Regulations in the US. Nutrients , 15 (19), 4269.
Huang, J., Guo, P., Zhang, S., Ji, M., & An, R. (2024). Use of Deep Neural Networks to Predict Obesity With Short Audio Recordings: Development and Usability Study. JMIR Artificial Intelligence , 3 , e54885.
An, R. , Batcheller, Q., Wang, J., & Yang, Y. (2023). Build neural network models to identify and correct news headlines exaggerating obesity-related scientific findings. Journal of Data and Information Science , 8 (3), 88-97.
An, R ., Byron Jr, C. W., Chen, C., & Xiang, X. (2023). A Field Test of Popular Chatbots’ Responses To Questions Concerning Negative Body Image. Health Behavior Research , 6 (1), 3.
An, R. , Yang, Y., Yang, F., & Wang, S. (2023). Use prompt to differentiate text generated by ChatGPT and humans. Machine Learning with Applications , 14 , 100497.
An, R. , Zheng, J., & Xiang, X. (2022). Projecting the influence of sugar-sweetened beverage warning labels and restaurant menu labeling regulations on energy intake, weight status, and health care expenditures in US adults: a microsimulation. Journal of the Academy of Nutrition and Dietetics , 122 (2), 334-344.
An, R. (2020). Projecting the impact of COVID-19 pandemic on childhood obesity in the US: A microsimulation model. Journal of Sport and Health Science, 9 (4): 302-312.
Tainio, M., Andersen, Z. J., Nieuwenhuijsen, M. J., Hu, L., De Nazelle, A., An, R. , ... & de Sá, T. H. (2021). Air pollution, physical activity and health: A mapping review of the evidence. Environment international , 147 , 105954.
An, R. , Kang, H., Cao, L., & Xiang, X. (2022). Engagement in outdoor physical activity under ambient fine particulate matter pollution: A risk-benefit analysis. Journal of Sport and Health Science , 11 (4), 537-544.
Si, Y., Yang, Y., Wang, X., An, R. , Zu, J., Chen, X., ... & Gong, S. (2024). Quality and Accountability of Large Language Models (LLMs) in Healthcare in Low-and Middle-Income Countries (LMIC): A Simulated Patient Study using ChatGPT (No. 1472). GLO Discussion Paper.
- Article Information
Data Sharing Statement
- As Ozempic’s Popularity Soars, Here’s What to Know About Semaglutide and Weight Loss JAMA Medical News & Perspectives May 16, 2023 This Medical News article discusses chronic weight management with semaglutide, sold under the brand names Ozempic and Wegovy. Melissa Suran, PhD, MSJ
- Patents and Regulatory Exclusivities on GLP-1 Receptor Agonists JAMA Special Communication August 15, 2023 This Special Communication used data from the US Food and Drug Administration to analyze how manufacturers of brand-name glucagon-like peptide 1 (GLP-1) receptor agonists have used patent and regulatory systems to extend periods of market exclusivity. Rasha Alhiary, PharmD; Aaron S. Kesselheim, MD, JD, MPH; Sarah Gabriele, LLM, MBE; Reed F. Beall, PhD; S. Sean Tu, JD, PhD; William B. Feldman, MD, DPhil, MPH
- What to Know About Wegovy’s Rare but Serious Adverse Effects JAMA Medical News & Perspectives December 12, 2023 This Medical News article discusses Wegovy, Ozempic, and other GLP-1 receptor agonists used for weight management and type 2 diabetes. Kate Ruder, MSJ
- GLP-1 Receptor Agonists and Gastrointestinal Adverse Events—Reply JAMA Comment & Response March 12, 2024 Ramin Rezaeianzadeh, BSc; Mohit Sodhi, MSc; Mahyar Etminan, PharmD, MSc
- GLP-1 Receptor Agonists and Gastrointestinal Adverse Events JAMA Comment & Response March 12, 2024 Karine Suissa, PhD; Sara J. Cromer, MD; Elisabetta Patorno, MD, DrPH
- GLP-1 Receptor Agonist Use and Risk of Postoperative Complications JAMA Research Letter May 21, 2024 This cohort study evaluates the risk of postoperative respiratory complications among patients with diabetes undergoing surgery who had vs those who had not a prescription fill for glucagon-like peptide 1 receptor agonists. Anjali A. Dixit, MD, MPH; Brian T. Bateman, MD, MS; Mary T. Hawn, MD, MPH; Michelle C. Odden, PhD; Eric C. Sun, MD, PhD
- Glucagon-Like Peptide-1 Receptor Agonist Use and Risk of Gallbladder and Biliary Diseases JAMA Internal Medicine Original Investigation May 1, 2022 This systematic review and meta-analysis of 76 randomized clinical trials examines the effects of glucagon-like peptide-1 receptor agonist use on the risk of gallbladder and biliary diseases. Liyun He, MM; Jialu Wang, MM; Fan Ping, MD; Na Yang, MM; Jingyue Huang, MM; Yuxiu Li, MD; Lingling Xu, MD; Wei Li, MD; Huabing Zhang, MD
- Cholecystitis Associated With the Use of Glucagon-Like Peptide-1 Receptor Agonists JAMA Internal Medicine Research Letter October 1, 2022 This case series identifies cases reported in the US Food and Drug Administration Adverse Event Reporting System of acute cholecystitis associated with use of glucagon-like peptide-1 receptor agonists that did not have gallbladder disease warnings in their labeling. Daniel Woronow, MD; Christine Chamberlain, PharmD; Ali Niak, MD; Mark Avigan, MDCM; Monika Houstoun, PharmD, MPH; Cindy Kortepeter, PharmD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Sodhi M , Rezaeianzadeh R , Kezouh A , Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023;330(18):1795–1797. doi:10.1001/jama.2023.19574
Manage citations:
© 2024
- Permissions
Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss
- 1 Faculty of Medicine, University of British Columbia, Vancouver, British Columbia, Canada
- 2 StatExpert Ltd, Laval, Quebec, Canada
- 3 Department of Ophthalmology and Visual Sciences and Medicine, University of British Columbia, Vancouver, Canada
- Medical News & Perspectives As Ozempic’s Popularity Soars, Here’s What to Know About Semaglutide and Weight Loss Melissa Suran, PhD, MSJ JAMA
- Special Communication Patents and Regulatory Exclusivities on GLP-1 Receptor Agonists Rasha Alhiary, PharmD; Aaron S. Kesselheim, MD, JD, MPH; Sarah Gabriele, LLM, MBE; Reed F. Beall, PhD; S. Sean Tu, JD, PhD; William B. Feldman, MD, DPhil, MPH JAMA
- Medical News & Perspectives What to Know About Wegovy’s Rare but Serious Adverse Effects Kate Ruder, MSJ JAMA
- Comment & Response GLP-1 Receptor Agonists and Gastrointestinal Adverse Events—Reply Ramin Rezaeianzadeh, BSc; Mohit Sodhi, MSc; Mahyar Etminan, PharmD, MSc JAMA
- Comment & Response GLP-1 Receptor Agonists and Gastrointestinal Adverse Events Karine Suissa, PhD; Sara J. Cromer, MD; Elisabetta Patorno, MD, DrPH JAMA
- Research Letter GLP-1 Receptor Agonist Use and Risk of Postoperative Complications Anjali A. Dixit, MD, MPH; Brian T. Bateman, MD, MS; Mary T. Hawn, MD, MPH; Michelle C. Odden, PhD; Eric C. Sun, MD, PhD JAMA
- Original Investigation Glucagon-Like Peptide-1 Receptor Agonist Use and Risk of Gallbladder and Biliary Diseases Liyun He, MM; Jialu Wang, MM; Fan Ping, MD; Na Yang, MM; Jingyue Huang, MM; Yuxiu Li, MD; Lingling Xu, MD; Wei Li, MD; Huabing Zhang, MD JAMA Internal Medicine
- Research Letter Cholecystitis Associated With the Use of Glucagon-Like Peptide-1 Receptor Agonists Daniel Woronow, MD; Christine Chamberlain, PharmD; Ali Niak, MD; Mark Avigan, MDCM; Monika Houstoun, PharmD, MPH; Cindy Kortepeter, PharmD JAMA Internal Medicine
Glucagon-like peptide 1 (GLP-1) agonists are medications approved for treatment of diabetes that recently have also been used off label for weight loss. 1 Studies have found increased risks of gastrointestinal adverse events (biliary disease, 2 pancreatitis, 3 bowel obstruction, 4 and gastroparesis 5 ) in patients with diabetes. 2 - 5 Because such patients have higher baseline risk for gastrointestinal adverse events, risk in patients taking these drugs for other indications may differ. Randomized trials examining efficacy of GLP-1 agonists for weight loss were not designed to capture these events 2 due to small sample sizes and short follow-up. We examined gastrointestinal adverse events associated with GLP-1 agonists used for weight loss in a clinical setting.
We used a random sample of 16 million patients (2006-2020) from the PharMetrics Plus for Academics database (IQVIA), a large health claims database that captures 93% of all outpatient prescriptions and physician diagnoses in the US through the International Classification of Diseases, Ninth Revision (ICD-9) or ICD-10. In our cohort study, we included new users of semaglutide or liraglutide, 2 main GLP-1 agonists, and the active comparator bupropion-naltrexone, a weight loss agent unrelated to GLP-1 agonists. Because semaglutide was marketed for weight loss after the study period (2021), we ensured all GLP-1 agonist and bupropion-naltrexone users had an obesity code in the 90 days prior or up to 30 days after cohort entry, excluding those with a diabetes or antidiabetic drug code.
Patients were observed from first prescription of a study drug to first mutually exclusive incidence (defined as first ICD-9 or ICD-10 code) of biliary disease (including cholecystitis, cholelithiasis, and choledocholithiasis), pancreatitis (including gallstone pancreatitis), bowel obstruction, or gastroparesis (defined as use of a code or a promotility agent). They were followed up to the end of the study period (June 2020) or censored during a switch. Hazard ratios (HRs) from a Cox model were adjusted for age, sex, alcohol use, smoking, hyperlipidemia, abdominal surgery in the previous 30 days, and geographic location, which were identified as common cause variables or risk factors. 6 Two sensitivity analyses were undertaken, one excluding hyperlipidemia (because more semaglutide users had hyperlipidemia) and another including patients without diabetes regardless of having an obesity code. Due to absence of data on body mass index (BMI), the E-value was used to examine how strong unmeasured confounding would need to be to negate observed results, with E-value HRs of at least 2 indicating BMI is unlikely to change study results. Statistical significance was defined as 2-sided 95% CI that did not cross 1. Analyses were performed using SAS version 9.4. Ethics approval was obtained by the University of British Columbia’s clinical research ethics board with a waiver of informed consent.
Our cohort included 4144 liraglutide, 613 semaglutide, and 654 bupropion-naltrexone users. Incidence rates for the 4 outcomes were elevated among GLP-1 agonists compared with bupropion-naltrexone users ( Table 1 ). For example, incidence of biliary disease (per 1000 person-years) was 11.7 for semaglutide, 18.6 for liraglutide, and 12.6 for bupropion-naltrexone and 4.6, 7.9, and 1.0, respectively, for pancreatitis.
Use of GLP-1 agonists compared with bupropion-naltrexone was associated with increased risk of pancreatitis (adjusted HR, 9.09 [95% CI, 1.25-66.00]), bowel obstruction (HR, 4.22 [95% CI, 1.02-17.40]), and gastroparesis (HR, 3.67 [95% CI, 1.15-11.90) but not biliary disease (HR, 1.50 [95% CI, 0.89-2.53]). Exclusion of hyperlipidemia from the analysis did not change the results ( Table 2 ). Inclusion of GLP-1 agonists regardless of history of obesity reduced HRs and narrowed CIs but did not change the significance of the results ( Table 2 ). E-value HRs did not suggest potential confounding by BMI.
This study found that use of GLP-1 agonists for weight loss compared with use of bupropion-naltrexone was associated with increased risk of pancreatitis, gastroparesis, and bowel obstruction but not biliary disease.
Given the wide use of these drugs, these adverse events, although rare, must be considered by patients who are contemplating using the drugs for weight loss because the risk-benefit calculus for this group might differ from that of those who use them for diabetes. Limitations include that although all GLP-1 agonist users had a record for obesity without diabetes, whether GLP-1 agonists were all used for weight loss is uncertain.
Accepted for Publication: September 11, 2023.
Published Online: October 5, 2023. doi:10.1001/jama.2023.19574
Correction: This article was corrected on December 21, 2023, to update the full name of the database used.
Corresponding Author: Mahyar Etminan, PharmD, MSc, Faculty of Medicine, Departments of Ophthalmology and Visual Sciences and Medicine, The Eye Care Center, University of British Columbia, 2550 Willow St, Room 323, Vancouver, BC V5Z 3N9, Canada ( [email protected] ).
Author Contributions: Dr Etminan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Sodhi, Rezaeianzadeh, Etminan.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Sodhi, Rezaeianzadeh, Etminan.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Kezouh.
Obtained funding: Etminan.
Administrative, technical, or material support: Sodhi.
Supervision: Etminan.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was funded by internal research funds from the Department of Ophthalmology and Visual Sciences, University of British Columbia.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Weird But True
- Sex & Relationships
- Viral Trends
- Human Interest
- Fashion & Beauty
- Food & Drink
- Health Care
- Men’s Health
- Women’s Health
- Mental Health
- Health & Wellness Products
- Personal Care Products
trending now in Lifestyle

Tourist spot is 'total chaos' with cars stuck in 4-hour traffic...

Impacted wisdom tooth led to deadly illness in 23-year-old -- and...

I signed up for a three-year, $90K cruise but never left dry land...

Dear Abby: My husband's personality changed for the worst when he...

I'm a doctor — here's how to keep your bones strong for a...

Rare coin from 1776 found in bottom of toffee tin to sell at...

Dear Abby: My stepmom encourages my disabled elderly dad to drive...

What is 'rucking'? Low-impact exercise trend has a wild military...
Breaking news, ozempic not linked to suicidal behavior, new research says, as safety debate continues.

Two new studies find that the popular weight loss and diabetes drug semaglutide , sold under the brand names Ozempic and Wegovy, does not increase the risk of depression and suicide .
But while two medical doctors who examined the research call the results “reassuring,” they say that neither study “fully answers the question of whether these drugs are safe in those with preexisting mental health problems.”
In the first study , researchers from the Perelman School of Medicine at the University of Pennsylvania analyzed data from over 3,500 people who participated in one of four semaglutide clinical trials and who did not have a major mental health condition.

The study authors found that 1% or fewer participants reported suicidal ideation or behavior during treatment, with no differences between 2.4 milligrams of semaglutide — the dosage for Wegovy — and a placebo.
“The STEP trials provide strong evidence that semaglutide 2.4 mg reduces body weight and improves numerous health complications associated with obesity,” said Thomas Wadden , a professor of psychology in psychiatry and the former director of Penn’s Center for Weight and Eating Disorders.
“Our new analyses provide assurance that the medication, when taken by individuals who are free of significant mental health concerns, does not increase the risk of depression, suicidal thoughts, or suicidal behavior,” added Wadden, who has received grants and consulting fees from Novo Nordisk.
The Danish pharmaceutical giant, which manufactures Wegovy and Ozempic, funded the study.
The US Food and Drug Administration (FDA) approved Ozempic in 2017 to treat Type 2 diabetes in adults and Wegovy in 2021 for adult weight loss.
They are part of a class of drugs that mimic the GLP-1 hormone to make people feel full and eat less.

The FDA and European Medicines Agency (EMA) recently investigated reports of suicidal thoughts or behavior by GLP-1 users, finding no evidence that these medicines cause either.
Novo Nordisk referenced the FDA and EMA findings in a statement to The Post about the new research — both studies were published Tuesday in JAMA Internal Medicine.
The second study found that GLP-1 drugs did not increase the risk of death by suicide among nearly 125,000 adults in Denmark and Sweden.
“These findings align with data collected from our comprehensive clinical trials, including large-scale outcomes trials and observational studies,” Novo Nordisk told The Post.
However, a study published last month found that semaglutide users may face a higher risk of suicidal thoughts.
Get the latest breakthroughs in medicine, diet & nutrition tips and more.
Subscribe to our weekly Post Care newsletter!
Thanks for signing up!
Please provide a valid email address.
By clicking above you agree to the Terms of Use and Privacy Policy .
Never miss a story.

In an editorial accompanying Tuesday’s research, two doctors raised concern about the exclusion of people with preexisting mental health problems, such as moderate or severe depression, in the Penn study.
Though more than one-third of patients had a history of psychiatric disorders in the other study, researchers only analyzed two types of GLP-1 drugs — semaglutide and liraglutide (brand name: Victoza). There are others on the market .
JAMA Internal Medicine Associate Editor Timothy S. Anderson and Deputy Editor Deborah Grady also pointed out that participants “may have stopped GLP-1 medications at the onset of worsening depressive symptoms prior to the development of suicidal ideation.”
As interest grows to see what else GLP-1 drugs can treat , like substance abuse , Anderson and Grady say “continued vigilance in monitoring mental health symptoms is essential.”
This story discusses suicide. If you or someone you know is having thoughts of suicide, please contact the Suicide & Crisis Lifeline at 988 or 1-800-273-TALK (8255).

Advertisement
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Obesity articles from across Nature Portfolio
Obesity is a condition in which excess fat has accumulated in the body, such that it can have an adverse effect on health. Obesity is defined as a body mass index (BMI) of greater than 30 kg/m2.
New insights into the regulation of GIPR signalling
Two recent studies have unravelled novel modes of glucose-dependent insulinotropic polypeptide receptor (GIPR) signalling regulation. Kizilkaya et al. characterized the effect of changes in β-arrestin 2 coupling with naturally occurring GIPR coding variants, whereas Regmi et al. investigated GIPR expression profiles and functional regulation in adipocytes.
- Yusman Manchanda
- Alejandra Tomas

Insights into optimal BMI from the GlasVEGAS study
A human experiment confirms the higher susceptibility of South Asians to adverse metabolic consequences with weight gain compared with white Europeans, which is attributed to underlying differences in muscle and adipose biology.
- Chun-Kwan O
- Juliana C. N. Chan
Latest Research and Reviews
Metabolic adaptation following gastric bypass surgery: results from a 2-year observational study
- Fathimath Naseer
- Shu-Dong Zhang
- Ruth K. Price

Triiodothyronine (T3) promotes browning of white adipose through inhibition of the PI3K/AKT signalling pathway
- LingHong Huang
- ZhiFeng Guo
- HuiBin Huang

G-quadruplex forming regions in GCK and TM6SF2 are targets for differential DNA methylation in metabolic disease and hepatocellular carcinoma patients
- Angelika Lahnsteiner
- Victoria Ellmer
- Angela Risch

Acute elevated dietary fat alone is not sufficient to decrease AgRP projections in the paraventricular nucleus of the hypothalamus in mice
- Selma Yagoub
- Robert A. Chesters
- Rachel N. Lippert
Polypeptide N -acetylgalactosaminyltransferase-15 regulates adipogenesis in human SGBS cells
- Asuka Takahashi
- Takeo Iwata
Exposure to gestational diabetes mellitus in utero impacts hippocampal functional connectivity in response to food cues in children
- Lorenzo Semeia
- Stephanie Kullmann
News and Comment
Neurons in the diagonal band of Broca moderate food intake
- Senegal Carty
The complexity of adipocyte heterogeneity
- Claire Greenhill
Inulin supplementation in pediatric obesity management: a critical appraisal of efficacy and limitations
- Yanggang Hong
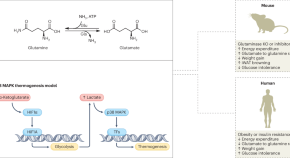
Adipose glutaminolysis resurfaces in metabolic disease
Analysis of glutamine metabolism in white adipose tissue (WAT) uncovers a novel role in metabolic disease that could be leveraged in therapies to combat disease.
- John A. Haley
- David A. Guertin
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Epidemiology of Obesity in Adults: Latest Trends
Inoue yosuke.
1 Carolina Population Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27516
2 Department of Population Science, Rutgers Cancer Institute of New Jersey, New Brunswick, NJ 08903
Poti Jennifer
3 Department of Nutrition, Gillings School of Global Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27516
Sokol Rebeccah
4 Department of Health Behavior, Gillings School of Global Public Health, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27516
Gordon-Larsen Penny
Associated data, purpose of review:.
An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe. We conducted a systematic review for studies using measured anthropometry to examine trends in obesity in the US published from 2012 to 2018 and for systematic reviews to document trends in obesity across the globe published from 2014 to 2018.
Recent findings:
For the US, the only nationally representative data source capturing trends in obesity in this period was the National Health and Nutrition Examination Survey, which uses repeated cross-sectional data to document national trends in obesity in the US.. For global trends, the only systematic reviews of obesity across the globe were the Global Burden of Disease Obesity study and the Non-communicable Disease Risk Factor Collaboration study. In general, the population distribution of Body Mass Index (BMI) in the US has shifted towards the upper end of its distribution over the past three decades. The global distribution has similarly increased, albeit with large regional differences.
US and global studies suggest an increasing trend in obesity since the 1980s, and there is a dearth of nationally representative longitudinal studies using measured anthropometry to capture trends in adult obesity in the US for the same individuals over time. Greater efforts are needed to identify factors contributing to the continued increases in obesity.
Introduction
Obesity is linked with elevated risk of non-communicable diseases (NCDs) [ 1 ]. An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe [ 2 ] while obesity prevalence varies by region and country [ 1 , 3 ].
Country-specific trends in obesity are generally tracked using longitudinal panel or repeated cross-sectional data, with the highest quality studies using measured anthropometry. In the US, the National Health and Nutrition Examination Survey (NHANES), which is a nationally representative, repeated cross-sectional survey of the civilian, noninstitutionalized US population [ 4 ], is the predominant dataset used to track changes in obesity over time. There are a set of national- or population-representative longitudinal studies following the same individuals over time or repeated cross-sections, some of which use self-reported height and weight (e.g., National Longitudinal Survey of Youth [ 5 ]; Health Information National Trends Survey [ 6 ]; California Health Interview Survey [ 7 ]; Medical Expenditure Panel Survey-Household Component [ 8 ]; Panel Study of Income Dynamics [ 9 ]; Behavioral Risk Factor Surveillance System [ 10 ]; and National Health Interview Survey [ 11 ]) while others capture specific subpopulations or portions of the lifecycle (e.g, Early Childhood Longitudinal Study [ 12 ]; National Longitudinal Study of Adolescent to Adult Health (Add Health) [ 13 ]; National Hospital Ambulatory Medical Care Survey [ 14 ]). For global studies, the predominant data sources include the Global Burden of Disease (GBD) study [ 2 , 3 , 15 ] and the Non-communicable Disease Risk Factor Collaboration (NCD-RisC) [ 16 , 17 ], both of which include approximately 200 countries, allowing comparisons over time, across age groups, and among populations [ 2 , 15 – 17 ].
We conducted a systematic review to examine trends in obesity in the US for studies providing nationally or sub-nationally representative estimates of body mass index (BMI), obesity, or abdominal obesity using measured anthropometry and published from 2012 to 2018. In addition, we reviewed the literature on global trends in obesity, restricting our search to systematic reviews or meta-analyses of global obesity in adults. In this review, we present findings on trends in obesity in the US and across the globe and discuss future research directions.
Search strategy
We used the following cut-off values to define overweight/obesity: overweight (BMI: 25–29.9), class I obesity (BMI: 30–34.9), class II obesity (BMI: 35–39.9) and class III obesity (BMI: ≥ 40) [ 18 ]. We defined abdominal obesity (i.e., cut-off values of waist circumference (WC) ≥ 102 cm (40 in) for men and WC ≥ 88 cm (35 in) for women) [ 19 ]. In addition, we considered the non-Hispanic Asian cut-points of WC ≥ 90 cm for men and WC ≥ 80 cm for women [ 20 ].
We systematically reviewed the literature using a protocol informed by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. We searched for articles published in English, peer-reviewed journals in PubMed. For the global study, we further restricted studies to systematic reviews or meta-analyses. We developed the search syntax in collaboration with a reference librarian ( Supplementary Tables 1 and 2 ). Our query included the following terms, their cognates, and synonyms: obesity AND trend AND United States AND adults AND nationally representative (US studies); obesity AND trend AND global AND adults (global studies).
Inclusion/exclusion criteria
For the search of domestic studies, articles had to fit the following inclusion criteria: 1) estimates of obesity following our criteria above; 2) sampling to be nationally representative or sub-nationally representative of the US; 3) include adults over the age of 18 years; 4) measured (rather than self-report) anthropometry; 5) repeated cross-sectional or longitudinal study design; 6) peer-reviewed; 7) available in English; and 8) published between January 1, 2012 and July 1, 2018 ( Supplementary table 1 ).
For the search of global studies, we restricted studies to systematic reviews and began with the seminal GBD paper [ 2 ] as a model and searched for studies that evaluated the prevalence or incidence of obesity using measured height and weight in countries outside the United States. To be included, articles had to fit the following inclusion criteria: 1) estimates of obesity following our criteria above; 2) estimates for areas outside the US; 3) adults over the age of 18 years; 4) measured (rather than self-report) anthropometry; 5) systematic review or meta-analysis; 6) peer-reviewed; 7) available in English; and 8) published between January 1, 2014 and July 1, 2018 ( Supplementary table 2 ).
Study selection and data extraction
We used Covidence, an online platform, to manage screening and selection of studies. A single reviewer completed an initial independent screen of all titles and abstracts retrieved from the database searches. A second reviewer checked a random sampling of titles to guarantee no articles were falsely excluded at this stage, and the second reviewer found no such discrepancies. Three separate reviewers independently reviewed the full texts of studies, whereby each study was dually screened, to determine final study inclusion. All conflicts in the full text review were resolved via discussion with the authorship team.
In our electronic search for the domestic studies, we found 695 references, two of which were duplicates, resulting in a total of 693 studies. In the initial title and abstract screen, the research team deemed 620 studies irrelevant, leaving 73 full-texts to review. We retained and extracted data from 18 studies that met inclusion criteria ( Figure 1 ). Our search for the global studies returned 141 references, of which we deemed 120 studies irrelevant on the basis of initial title and abstract screen, leaving 21 full-texts to review of which one fit inclusion criteria. In addition, we included the GBD study published in July 2017 [ 2 ] and used the reference lists of the papers captured in our search to add one NCD-RisC paper [ 17 ] ( Figure 2 ).

PRISMA diagram for US studies that used nationally representative adult samples with measured anthropometry, published between Jan 2012 and July 2018.

PRISMA diagram for global studies that were systematic review published between Jan 2014 and July 2018.
We identified 18 US studies and three global studies that fit search criteria ( Table 1 ). All the US studies used information collected in the NHANES and one also used information collected in the National Health Examination Survey (predecessor to the NHANES) [ 21 ]. Periods of time covered in each study differed; Hales et al. [ 38 ] provided the most updated information covering the period between 2013 and 2016 while Ljungvall et al. [ 21 ] presented data across the longest timespan (i.e., 1959 – 2008) among the studies extracted in our search. Three studies examined abdominal obesity, one of which used different cut-off points as their study participants were confined to non-Hispanic Asian Americans [ 36 ]. In relation to the global obesity trends, the GBD study used information obtained from 1514 sources [ 2 ] while the NCD RisC studies used information collected in 1698 population-based studies [ 16 ] and 1820 studies [ 17 ].
Eighteen US studies reviewing obesity prevalence in the US published from January 2012 to July 2018 and three studies of global obesity published from January 2014 to July 2018
| Authors | Data source | Study period | Age range | BMI cut-off points | Waist circumference cut-off points |
|---|---|---|---|---|---|
| Ljungvall et al., 2012 [ ] | NHANES | 1959-2008 | 20-74 | ≥ 30 and ≥ 35 | |
| Romero et al., 2012 [ ] | NHANES | 1988-2004 | 25-84 | ≥ 30 | |
| Yu, 2012 [ ] | NHANES | 1971-2006 | 25-64 | ≥ 30 | |
| Huffman et al., 2012 [ ] | NHANES | 1988-2008 | 20+ | ≥ 30 | |
| Robinson et al., 2013 [ ] | NHANES | 1971-2008 | 2-74 | ≥ 30 for respondents aged 20-74 years ≥ the 95th percentile values of the sex- and age-specific CDC standards or BMI ≥ 30 for respondents aged 2-19 years | |
| Robinson et al., 2013 [ ] | NHANES | 1988-2008 | 20-74 | ≥ 102 cm (40 in) for men ≥ 88 cm (35 in) for women | |
| Saydah et al., 2014 [ ] | NHANES | 1999-2010 | 18+ | BMI ≥ 30 and BMI ≥ 35 | |
| Ladabaum et al., 2014 [ ] | NHANES | 1988-2010 | 18+ | BMI ≥ 30 | |
| Cohen et al., 2015 [ ] | NHANES | 1965-2011 | 18-64 | ≥ 102 cm (40 in) for men ≥ 88 cm (35 in) for women | |
| Flegal et al., 2016 [ ] | NHANES | 2005-2014 | 20+ | ≥ 30 and ≥ 40 | |
| Mehta et al., 2016 [ ] | NHANES | 1971-1994 | 25-60 | ≥ 30 and ≥ 35 | |
| Kranjac et al. 2016 [ ] | NHANES | 1971-2012 | 20+ | 30 to < 40 and ≥ 40 | |
| Yu, 2016 [ ] | NHANES | 1971-2012 | 25-74 | ≥ 30 | |
| Yu, 2016 [ ] | NHANES | 1971-2006 | 25-74 | 30 to < 35 and ≥ 35 | |
| Casagrande et al., 2016 [ ] | NHANES | 1971-2012 | 20-49 | ≥ 30 | |
| Liu et al., 2017 [ ] | NHANES | 2011-2014 | 20+ | ≥ 90 cm for men ≥ 80 cm for women | |
| Ogden et al. 2017 [ ] | NHANES | 2011-2014 | 20+ | ≥ 30 | |
| Hales et al., 2018 [ ] | NHENES | 2013-2016 | 20+ | ≥ 30 and ≥ 40 | |
| GBD 2015 Obesity Collaborators, 2017 [ ] | 1514 studies | 1980-2015 | 20+ | ≥ 30 | |
| NCD RisC, 2016 [ ] | 1698 studies | 1975-2014 | 18+ | 30 to < 35; 35 to < 40; ≥ 40 | |
| NCD RisC, 2017 [ ] | 1820 studies | 1975-2016 | 20+ | 30 to < 35; 35 to < 40; ≥ 40 (online) |
BMI: Body Mass Index; GBD: Global Burden of Disease; NCD RisC: NCD Risk Factor Collaboration; NHANES: National Health and Nutrition Survey.
Overall obesity trends in the US
Flegal et al. [ 30 ] estimated obesity prevalence to be 34.6% (men: 33.5%; women: 35.7%) in 2005–2006, which decreased in 2007–2008 to 33.9% (men: 32.2%; women: 35.5%) but then increased to 37.9% (men: 35.2%; women: 40.5%) in 2013–2014 ( Table 2 ). Hales et al. [ 38 ], including the most recent cycle of the NHANES, reported that obesity prevalence in 2013–2016 to be 36.5% for men and 40.8% for women.
Summary of findings reported in the Eighteen US studies reviewing obesity prevalence in the US published from January 2012 to July 2018 and three studies of global obesity published from January 2014 to July 2018.
| Authors | Study objectives | Statistical analysis | Selected findings / conclusions (related to obesity) |
|---|---|---|---|
| Ljungvall et al., 2012 [ ] | • To analyze how obesity prevalence and the adjusted distribution of BMI have changed over time while paying attention to differences among population subgroups (i.e., race/ethnicity, education attainment and income). | • Probability linear models using obesity and BMI ≥ 35 as the outcomes. • Quantile regression models using BMI as the outcome. • Models were stratified by gender. | • Increases in obesity, BMI ≥ 35 and BMI were similar across the different population subgroups while the additional increases among Blacks merit further investigation. • The obesity epidemic is not limited to low socioeconomic and minority groups. |
| Romero et al., 2012 [ ] | • To examine trends in the prevalence of obesity and other CVD risk factors by race/ethnic groups. • To test whether the prevalence and trends differ according to race/ethnicity. | • Absolute changes in the prevalence estimates within each race/ethnic group were calculated for each period (1988-1994 and 1999-2004) and over time (1988-1994 vs. 1999-2004). | • The prevalence of obesity increased significantly in non-Hispanic white and non-Hispanic black, both in men and women. • Among Mexican American, the prevalence of obesity increased only among men. • There existed persistent race/ethnic differences for all CVD risk factors, with non-Hispanic black and Mexican American generally having worse profiles than non-Hispanic white. |
| Yu, 2012 [ ] | • To examine the time trends in educational differences in obesity by gender and race (non-Hispanic white and non-Hispanic black). | • The prevalence model; interaction terms between time (1971-1980 vs. 1999-2006) and education categories (< high school; high school degree; some college; at least 4-year college) were incorporated to indicate the change in the education-obesity association. • The analysis is done separately for each of the four gender-race groups. | • The increase in obesity was similar for most educational groups, but significantly greater for younger women with some college and smaller for younger white men without a high-school degree. |
| Huffman et al., 2012 [ ] | • To evaluate recent trends in composite cardiovascular health metrics • To estimate future levels of cardiovascular health behaviors and factors among adults in the US to determine whether the American Heart Association 2020 goals will be met if current trends continue. | • Weighted linear regression using prevalence as the dependent variables and survey time as independent variables. • The coefficient based on the regression (i.e., the average annual change in the prevalence) was used to project the obesity prevalence and trends of other components for 2020 by assuming that trends would be the same. | • Prevalence of obesity and dysglycemia increase as opposed to prevalence of smoking, hypercholesterolemia and hypertension that declined over the study periods. • The obesity prevalence was projected to increase up to 43.4% among men and 42.2% among women in 2020. |
| Robinson et al., 2013 [ ] | • To estimate cohort-specific propensity to obesity for those born in the US in the 1980s. | • Age-period-cohort analysis | • Cohorts born in the 1980s had increased propensity to obesity versus those born in the late 1960s. |
| Robinson et al., 2013 [ ] | • To estimate cohort-specific risks for abdominal obesity. | • Age-period-cohort effect | • The birth cohorts of the post-World War II Baby Boom appeared to have low cohort-specific risks of abdominal obesity. • The cohorts preceding and succeeding the Baby Boom showed evidence of birth cohort effects that increased prevalence of abdominal obesity. • These generational differences were more pronounced in women than in men. |
| Saydah et al., 2014 [ ] | • To assess whether trends in CVD risk factors have improved by weight status (normal, overweight and obese). | • Data was grouped into 4-year periods (1999-2002, 2003-2006 and 2007-2010). • Prevalence of risk factors (total and undiagnosed diabetes, total and untreated hypertension, total and untreated dyslipidemia, self-reported smoking and moderate to heavy smoking exposure (cotinine levels ≥ 10ng/ml)) was calculated overall and for each BMI group. • Absolute change in prevalence was calculated as the percent estimate for 2007-2010 minus the percent estimate for 1999-2002. | • The prevalence of cardiovascular risk factors increases as people become overweight and obese. • The prevalence of CVD risk factors has remained the same or declined over time. • From 1999-2002 to 2007-2010, untreated hypertension decreased among obese and overweight adults and untreated dyslipidemia decreased for all weight groups. • The proportion of those with 3 or more CVD risk factors increased over time among the obese population. |
| Ladabaum et al., 2014 [ ] | • To characterize trends in and associations among overweight and obesity, abdominal obesity, physical activity and caloric intake in the US adults in the last 2 decades. | • Linear regression to assess trends in log-transformed BMI, WC and daily energy intake. • Logistic regression to assess the trends in the prevalence of obesity and abdominal obesity. | • The prevalence of obesity and abdominal obesity increased substantially during the period between 1988 and 2010. • The proportion of people who reported no leisure time physical activity increased while average daily caloric intake did not change significantly. |
| Cohen et al., 2015 [ ] | • To determine how macronutrient consumption patterns and body mass index in the US adult population have changed since the 1960s. | • Descriptive. | • Americans in general have been following the official nutrition advice for more than 40 years. • General adherence to recommendations to reduce fat consumption has coincided with a substantial increase in obesity. |
| Flegal et al., 2016 [ ] | • To examine prevalence of obesity and Class 3 obesity (BMI ≥ 40) in 2013-2014. • To examine trends over the decade from 2005 through 2014. | • Sex-stratified logistic regression models to assess the associations of age group, race/Hispanic origin, smoking status, and education with obesity prevalence. • When examining the trends, 5 cycles of the NHANES survey (2005-2014) were treated as a categorical variable. • Predicted margins are calculated. | • The age-adjusted prevalence of obesity in 2013-2014 was 35.0% among men and 40.4% among women. • The prevalence of overall and class 3 obesity both showed a significant linear trend between 2005 and 2014, while there were no significant trends for men. |
| Mehta et al., 2016 [ ] | • To test the hypothesis that even if the true effect of BMI as a continuous variable on mortality has not changed, changes in the BMI distribution could affect the calculated estimates of the effects for specific BMI categories. | • The NHANES I dataset (1971-1975) linked with mortality data was used to fit a Cox proportional hazards model incorporating BMI as a continuous variable. • Coefficients obtained from this model were used to simulate mortality for participants in the NHANES III (1988-1994). • Hazard ratios of mortality by BMI categories were compared between the NHANES I and the NHANES III with simulated mortality data. | • Some of the diminution of the association between obesity and mortality may be an artifact of treating BMI as a categorical variable. |
| Kranjac et al. 2016 [ ] | • To decompose change in body mass index, obesity and severe obesity from 1971 through 2012 into parts attributable to (1) older, fitter cohorts in the population being replaced by newer, less fit cohorts (between-cohort change) and cohort members becoming less fit over time (within-cohort change). | • Glenn Firebaugh’s linear decomposition technique and Kitagawa’s algebraic decomposition method to decompose aggregate change into two components (i.e., intracohort change and cohort replacement [i.e., intercohort change]). | • The rise in mean BMI and rates of obesity and severe obesity was primarily a consequence of intracohort change driven by variation in the demographic and socioeconomic composition and in the diet of the population overtime. • Obesity and BMI in the population rose largely because of individual increases in weight status that were broadly distributed across age and cohort groups. |
| Yu, 2016 [ ] | • To analyze the influences of educational attainment on obesity trends. | • The linear probability model that included education (< high school; high school degree; some college; at least 4-year college), survey year, and interactions between education and survey year. • Obesity prevalence was simulated under several scenarios (different age distribution, educational distribution or educational inequality in obesity prevalence.) | • Educational inequality in obesity was generally larger for women than men and for non-Hispanic white than non-Hispanic black. No difference was observed among non-Hispanic black men. • Obesity prevalence among some college group experienced the largest increase compared to other groups, except for non-Hispanic black men. |
| Yu, 2016 [ ] | • To estimate model for year-of-birth (cohort) and year-of-observation (period) trends in how age-specific mortality rates differ across BMI categories. | • Logistic regression model • Models were compared to determine which temporal patterns provided a better fit to the data (age, period and /or cohort) • The final model includes interactions between birth cohort and BMI categories. | • Among women, those who were born later were more likely to die when they were overweight, obese and severe obese (BMI ≥ 35) compared to normal weight. • Among men, those who were born later were less likely to die when they were overweight and were more likely to die when they were severely obese, compared to those with normal weight. |
| Casagrande et al., 2016 [ ] | • To examine generational differences in cardiovascular risk factors of younger adults over the past 40 years. | • Logistic regression was used to calculate the odds of health conditions among adults aged 20-49 years. | • Cardiovascular risk factors in younger adults have worsened over the past 40 years. • Participants in 2009-2012 were more likely to be obese than those in 1971-1975 (OR = 4.98) |
| Liu et al., 2017 [ ] | • To examine the prevalence of central obesity and the difference in the prevalence across demographic and socioeconomic groups were examined among US non-Hispanic Asian adults. | • Chi-squared tests were used to examine the difference in the prevalence of central obesity over time (2011-2012 vs. 2013-2014). | • Overall prevalence of central obesity (2011-2014) was 58.1%, with higher prevalence observed in women than in men. • Significant increases in central obesity were observed in younger adults (20-39 years), men, those with higher education and non-poor population. |
| Ogden et al., 2017 [ ] | • To analyze trends in obesity prevalence by household income levels and individual education level during 1999-2002 to 2011-2014, | • No information on models provided. • Household income level was defined based on percentage of the federal poverty level (≤130%; >130 to 350%; and >350%) and education level was categorized into high school graduate or less; some college; and college graduate. | • The prevalence of obesity increased among women in the two lower income groups. Among men, obesity prevalence increased among men in all three income groups. • Obesity prevalence increased among both sexes in all education groups except for men who were college graduates. |
| Hales et al., 2018 [ ] | • To estimate obesity prevalence and examine trends in the prevalence by urbanization level. | • Logistic regression models were used to calculate obesity prevalence by urbanization level and 4-year period (2001-2004, 2005-2008, 2009-2012, 2013-2016). • Urbanization level was based on the National Center for Health Statistics classification schemes (large metropolitan statistical areas [MSAs]; medium or small MSAs; and non-MSAs). | • Men living in medium or small MSAs had a higher obesity prevalence compared to those living in large MSAs. Women living in medium or smalle MSAs and non-MSAs had a higher prevalence compared to women living in large MSAs. • Obesity prevalence increased across all the urbanization level between 2001-2004 and 2013-2016. |
| GBD 2015 Obesity Collaboration, 2017 [ ] | • To assess the trends in the obesity and overweight prevalence during the period between 1980 and 2015. • To quantify the burden of disease related to high BMI (1990 – 2015). | • Mixed-effects linear regression models (Bayesian meta-regression model and spatiotemporal Gaussian process regression model) | • In 2015, overall obesity prevalence was 12.0%. • Since 1980, obesity prevalence has doubled in more than 70 countries. |
| NCD RisC, 2016 [ ] | • To estimate trends in adult body mass index and trends in the prevalence of underweight, overweight and obesity from 1975 to 2014 in the world | • Bayesian hierarchical model | • During the period between 1975 and 2014, age-adjusted obesity prevalence increased from 3.2% to 10.8% in men and from 6.4% to 14.9 in women. |
| NCD RisC, 2017 [ ] | • To estimates trends in mean BMI and the prevalence of underweight, overweight and obesity from 1975 to 2016 in children, adolescents and adults in the world. | • Bayesian hierarchical model | • Adult results were not presented in the manuscript while the updated results are available on the NCD-RisC website. |
BMI: Body mass index; CVD: cardiovascular disease; GBD: Global Burden of Disease; NCD-RisC: NCD Risk Factor Collaboration; WC: waist circumference
Ljungvall et al. [ 21 ] reported an obesity prevalence of 10% for men and 16% for women in 1959–1962, which increased to 18% for men and 23% for women in 1988–91, 27% for men and 34% for women in 1999–2000, and again to 32% for men and 36% for women in NHANES 2007 – 2008. The increasing trend in obesity prevalence was featured in the other studies in our search as well [ 22 – 24 , 33 , 35 ].
Several studies that used BMI cut-offs higher than 30 suggest a shift in population distribution for BMI towards the upper end of the BMI distribution. [ 21 , 27 , 30 , 32 ]. For example, Ljungvall et al. [ 21 ] reported that prevalence of BMI ≥ 35, which was 1% and 5% for men and women, respectively in 1959, increased to 5% and 9% in 1988–1991 and finally to 11% and 19% in 2007–2008. Kranjac et al. [ 32 ] reported that the prevalence of BMI ≥ 40 was 1% in 1971, rising to 6% in 2012, with higher prevalence reported in women than in men. The prevalence of BMI ≥ 40 for men and women was 5.5% and 9.9% in 2013–2014 [ 30 ] and 5.5% and 9.8% in 2013–2016 [ 38 ].
Between 1988–1994 and 2009–2010, abdominal obesity prevalence increased from 29.1% to 42.0% among men and from 46.0% to 61.5% among women [ 28 ]. Robinson et al. [ 26 ] reported that in 1986–1990 abdominal obesity prevalence was 36.0% (27.5% for men and 44.3% for women) increasing to 52.5% (43.1% for men and 61.5% for women) in 2006–2010. Liu et al. [ 36 ] reported that central obesity among US non-Hispanic Asian adults in 2011–2014 was 55.3% and 60.9% for men and women, respectively.
Sociodemographic disparities
Several of the US studies examined differences in obesity prevalence by race/ethnicity, educational attainment, income and urbanization level. For example, Ljungvall et al. [ 21 ] reported that probability of obesity in 1960 was higher in non-Hispanic black women than non-Hispanic white women by 10 percentage points and that total increase during the study period (1960 – 2008) was also larger in non-Hispanic black women than non-Hispanic white women (by 5 – 10 percentage points). Romero et al. [ 22 ] studied a shorter period of time (1988 – 2004) and showed that a baseline difference observed between non-Hispanic white and non-Hispanic black did not change over time, while a difference between non-Hispanic black and Hispanic increased over time.
Yu et al [ 33 ] concluded that educational inequalities in relation to obesity prevalence from 1971 to 2012 were generally larger in women than men and larger in non-Hispanic white than non-Hispanic black and that obesity prevalence did not differ by educational attainment among non-Hispanic black men. In addition, individuals with some college education (i.e., 13 – 15 years of school or associate’s degree) experienced the most rapid increase in obesity prevalence among the four educational attainment categories in non-Hispanic white men, non-Hispanic white women and non-Hispanic black women. Ogden et al. [ 37 ], which also examined the trends by educational attainment (high school graduates or less; some college; and college graduates) between 1999–2002 and 2011–2014, showed that obesity prevalence among men with some college tended to increase at a faster pace than other two groups. On the other hand, such difference was not observed among women.
Ljungvall et al. [ 21 ] found an initial disparity by income, with higher prevalence observed among women in the lower (versus higher) income groups in 1959; this difference did not diverge over the full period captured (1959–2008). The initial income disparity for men in 1960 disappeared by the 1970s. When Ogden et al. [ 37 ] examined trends in obesity prevalence by three categories of household income from 1999–2002 to 2011–2014, obesity prevalence increased among women in the bottom two income groups, but it did not among women in the highest income group. Among men, obesity prevalence in the three income groups increased during the same period.
Hales et al. [ 38 ] examined if obesity prevalence differed by urbanization level (large metropolitan statistical areas [MSAs]; medium or small MSAs; and non-MSAs), showing that in 2013–2016, participants living in medium or small MSAs had a higher obesity prevalence compared to those living in large MSAs in both sexes. In addition, women living in non-MSAs also had a higher prevalence compared to women living in large MSAs.
Given less change in obesity prevalence in the first decade of the 2000s compared to previous years, several authors suggested that the increase in obesity prevalence among US adults may be leveling off [ 39 , 40 ]. Robinson et al. examined differences in obesity prevalence [ 25 ] and abdominal obesity prevalence [ 26 ] by birth cohort using an age-period-cohort analysis. Robinson et al. [ 25 ] found that cohorts born in the 1980s had increased propensity to obesity compared to previous generations, suggesting obesity prevalence may continue to increase as this younger generation reaches the ages of peak prevalence of obesity. Robinson et al. [ 26 ] reported that the baby boomers (those born in 1946–1964) seemed to have low cohort effects on abdominal obesity.
Differences in obesity and abdominal obesity patterns
The authors of two studies reported trends in obesity defined using BMI and abdominal obesity (per waist circumference). Robinson et al. [ 26 ] reported that in 1986–1990 abdominal obesity prevalence was 27.5% for men and 44.3% for women and increased up to 43.1% for men and 61.5% for women in 2006–2010. During the same period, obesity defined with BMI increased from 18.5% to 32.6% and from 23.6% to 36.0% among men and women, respectively. Ladabaum et al. [ 28 ] reported that between 1988–1994 and 2009–2010, obesity prevalence increased from 19.9% to 34.6% among men and 24.9% to 35.4% among women while abdominal obesity prevalence increased from 29.1% to 42.0% among men and 46.0% to 61.5% among women.
Global trends in adult obesity prevalence
The GBD 2015 Obesity Collaborators based their study on a systematic literature search in Medline for studies providing nationally or sub-nationally representative estimates of BMI, overweight, or obesity among children or adults. Information came from 1514 data sources from 174 countries (713 measured and 801 self-report data) between 1980 and 2015. On the other hand, the NCD-RisC estimated global trends of BMI and obesity prevalence between 1975 and 2014 using data collected from 1698 population-based studies (e.g., nationally or sub-nationally representative studies and community-based studies) that used measured height and weight [ 16 ]. Following this initial paper, they expanded their study period to 2016 using data collected from 1820 population-based studies [ 17 ].
Both research groups described how obesity prevalence has increased in the last few decades. The GBD study showed that between 1980 and 2015 obesity prevalence doubled in 73 countries and showed an increase in most of the other countries as well. The NCD-RisC [ 16 , 17 ] found that between 1975 and 2014, age-standardized prevalence of obesity increased from 3.2% to 10.8% in men and from 6.4% to 14.9% in women. In 2014, 2.3% and 5.0% of men and women from these 200 countries had BMI ≥35 and 0.64% and 1.6% had BMI ≥ 40.
The GBD study also showed trends in adult obesity prevalence by country’s sociodemographic development quintiles (categorized into quintiles: low, low-middle, middle, high-middle, and high). The GBD study showed that between 1980 and 2015, men aged 25 to 29 and living in countries with a low-middle degree of development experienced the largest relative increase in obesity prevalence (1.1% in 1980 to 3.8% in 2015) among population subgroups stratified by sex, age and country’s level of sociodemographic level.
The NCD RisC [ 16 , 17 ] emphasized large regional differences in obesity prevalence. Areas with obesity prevalence of ≥25% or higher in 2016 included High-income Western countries (men: 29.6%; women: 29.6%), Central and Eastern Europe (women: 26.1%), Central Asia, Middle East and North Africa (women: 35.2%), Latin America and Caribbean (women: 29.2%), and Oceania (women: 30.0%), while several areas had obesity prevalence of <10%, i.e., East and South East Asia (men: 5.9%; women: 7.4%), High-income Asia Pacific (men: 4.9%; women: 4.3%), South Asia (men: 3.2%; women: 6.0%); and Sub-Saharan Africa (men: 4.8%).
Synthesis of findings
We extracted 18 US studies from the NHANES in our search, which indicate an increase in obesity prevalence over the past 40 years, with the latest prevalence estimates from the NHANES 2013–2016 at 36.6% (men) and 41.0% (women) [ 38 ]. In addition, Hales et al. [ 41 ], which was published as a letter and thus not included in our search, reported obesity prevalence in 2015–2016 to be 37.9% (men) and 41.1% (women).
Several papers by Flegal and her colleagues published outside of our inclusion window, and thus not included in our search, reported obesity prevalence during the periods between 1960 and 1988–1994 [ 42 ], 1988–1994 to 1999–2000 [ 43 ], and 1999–2000 and 2007–2008 [ 39 , 44 – 47 ]. The earlier two studies showed that obesity prevalence increased significantly from 14.5% to 22.5% to 30.5% between NHANES II (1976–1980), NHANES III (1988–1994), and the first cycle of the continuous NHANES (1999–2000), while the more recent studies suggested a stabilized trend in obesity prevalence in the early 2000s. Whereas some authors report that the increase in adult obesity prevalence may be slowing over time [ 39 , 40 ], the 18 more recent studies included in our review do not support such trend. In particular, Flegal et al. [ 30 ] found a significant increasing linear trend in the prevalence between 2005–2006 and 2013–2014 among women. Significant increases were reported between 2001–2004 and 2013–2016 [ 38 ] and between 2007–2008 and 2015–2016 [ 41 ]. In addition, US-specific estimates provided by the GBD [ 2 ] and the NCD-RisC [ 17 ] also suggest an increase in US obesity prevalence ( Figure 3 ).

Trends in US adult obesity prevalence based on data from the National Health and Nutrition Survey (NHANES), and US data included in the Global Burden of Disease (GBD), the NCD Risk Factor Collaborations (NCD-RisC).
The studies that examined obesity trends suggest particularly high risk among non-Hispanic black women [ 21 , 22 ], individuals with some college education versus the other educational attainment categories [ 33 ], those whose communities were classified as the intermediate category of urbanization [ 38 ] and cohort differences in obesity prevalence. [ 25 , 26 ].
Our findings for global obesity trends indicate that obesity prevalence has increased in the last few decades across the world. The GBD study showed that between 1980 and 2015 obesity prevalence doubled in 73 countries and the NCD-RisC [ 16 , 17 ] found that age-standardized prevalence of obesity increased from 3.2% to 10.8% in men and from 6.4% to 14.9% in women across 200 countries between 1975 and 2014 [ 16 ].
Differences in surveillance
The NHANES is a repeated cross-sectional survey, in which different participants were randomly sampled from population at several time points. Thus, unlike in longitudinal studies, it is not possible to track within-person changes in weight over time. While there are several representative longitudinal cohort studies in the US that collect measured height and weight (e.g., Add Health [ 13 ], the Longitudinal Health and Retirement Study [ 48 ], the National Social Life, Health, and Aging Project [ 49 ] and the Wisconsin Longitudinal Study [ 50 ]), none had data published in the date range that fit our inclusion criteria.
The GBD study and the NCD-RisC study based their estimates on many population-based studies, some of which were cross-sectional and the others were longitudinal follow-up. Rather than looking at the longitudinal association, the GBD and NCD-RisC studies estimated obesity prevalence for each country and year using data collected in each given country and the year of data collection, but allowed for inclusion of data from other years in the same country or from data in other countries across similar time periods within regions.
Analytical issues
Several aspects of the analysis of obesity prevalence trends can impact the magnitude and direction of estimated effects, potentially resulting in inconsistent conclusions across studies. Conclusions in relation to the trends in obesity prevalence differed by time periods covered by each study. Studies that covered a longer period (e.g., 1959–2008 [ 21 ]; 1988–2008 [ 28 ]) documented increases in obesity prevalence, while Flegal et al. [ 43 ] suggested that obesity prevalence from 1999 to 2008 did not continue to increase at the same rate as that observed in the prior 10 years. Another example is a difference between Ljungvall et al. [ 21 ] that covered the period between 1959–2008 and Romero et al. [ 22 ] that used information collected in 1988–2004. While the former described that the increases in obesity prevalence during the study periods (1960–2008) were similar across the racial/ethnic subgroups (or, at least, smaller than the increase experienced by the whole population), the latter emphasized that non-Hispanic black were at higher risk of obesity compared to non-Hispanic white.
The time point used as baseline for evaluating obesity prevalence trends can also have an important impact on findings [ 47 ]. A notable example comes from studies of recent childhood obesity trends; evaluations using 2003–2004 as the baseline time point reported decreases in the prevalence of obesity among 2–5 year old children through 2011–2014 [ 47 , 51 ], while studies using 1999–2000 as baseline reported no evidence of a decline in obesity prevalence in this or any age group through 2011–2014 [ 52 – 54 ]. Because prevalence estimates can fluctuate substantially between study waves, inclusion of data from several prior years and subsequent years can aid in determining whether prevalence changes at any given time point reflect a transient anomalous dip or a true downward trend [ 53 ]. The need to place data in context and see the bigger picture underscores the need for ongoing, consistent monitoring of obesity prevalence and trends in the US and worldwide.
One must consider exclusion criteria for each specific study, even when based on the same study source. For example, in the 18 studies we reviewed, three studies explicitly excluded BMI < 18.5 [ 23 , 27 , 34 ]. Studies also varied greatly in the exclusion of older adults, with some studies excluding adults in their late 60s or 70s while others making no exclusions of older adults, and also varied in exclusion of younger adults aged 18–24 years old. Because obesity prevalence varies across the lifespan and some evidence suggests that obesity trends differ by age [ 30 , 47 ], the age range of included participants could potentially impact estimated trends or limit comparability across studies. The analytical approaches used to evaluate obesity trends also varied, with methods including pairwise difference testing, linear trend tests, regression modeling to evaluate linear and quadratic trends, and age-period-cohort analysis. Studies using multivariable regression modeling to evaluate changes over time also differed in the selection of covariates used for adjustment in regression models. However, regardless of these differences, studies of US trends included in our review consistently found significant long-term increases in the prevalence of obesity.
There are also analytical issues related to future obesity projections. Flegal et al. [ 30 ] cautioned that several previous attempts to use past data to extrapolate to future trends in obesity prevalence may not have provided valid estimates [ 55 – 57 ]. Mehta et al. [ 31 ] conducted simulations using NHANES I to simulate mortality for NHANES III participants to test whether a decline in association between BMI and mortality related to statistical nuisance issues, finding that these nuisance contributors, such as the usage of categorical BMI variable (vs. continuous variable) and changes in population distribution altered findings.
Limitations
There are several limitations that should be addressed. First, only studies based on the NHANES data were captured with our inclusion criteria. While the NHANES is nationally representative sample and designed to estimate obesity prevalence in the US, it is a repeated cross sectional, which precludes within-individual change in BMI/obesity. Second, although NHANES is nationally representative, the subpopulation groups can get quite small by sex, race/ethnicity and socioeconomic groups. Third, we only included systematic reviews and meta analyses for our global search. Thus, some smaller within country studies that were not a part of GBD and NCD RisC might have been missed. Fourth, the GBD study and the NCD-RisC studies estimated obesity prevalence in each country as a whole, thus ignoring within-country heterogeneity by region, SES, or other subpopulations.
Conclusions and Future directions
It would be ideal to use longitudinal studies that allow intra-individual changes between study waves for surveillance. Surveillance that can fully address age-period-cohort differences are needed to identify whether obesity trajectories by age are different by cohort. For example, the Global Burden of Disease Study [ 3 ] presented obesity prevalence by age across birth cohorts, suggesting that obesity prevalence tended to increase at a faster pace among those who were born in later cohorts than in earlier cohorts (e.g., those born in 1985 vs. those born in 1960). Age-period-cohort analyses might be particularly relevant in countries undergoing dramatic changes in social and economic environment. There remains a need for studies that allow within-country differences in obesity prevalence.
Although significant increases in the prevalence of obesity since the 1980s are well-documented, relatively little is known about the causes for these population-level trends [ 30 ]. Future studies are needed to identify the factors contributing to the continued increases in obesity. Moreover, there is a need for evaluation of the effectiveness of programs and policies to prevent obesity, as well as to understand the reasons for limited progress in reversing obesity trends [ 58 – 61 ]. Because of the large inter-individual heterogeneity in the efficacy of obesity intervention and treatment approaches, further studies are warranted to identify individual factors that predict response and to evaluate personalized precision approaches based on genetic and phenotypic characterization [ 62 ]. In addition, given the established relations between central obesity and cardiometabolic risk, a close monitoring of trends in central obesity prevalence may be necessary.
Supplementary Material
Conflict of Interest
Yosuke Inoue declares that he has no conflict of interest.
Bo Qin declares that she has no conflict of interest.
Jennifer Poti declares that she has no conflict of interest.
Rebeccah Sokol declares that she has no conflict of interest.
Penny Gordon-Larsen is supported by grants from the National Institutes of Health (NIH) and the Office of the Vice Chancellor for Research at the University of North Carolina at Chapel Hill.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.

IMAGES
VIDEO
COMMENTS
In the United States, overweight and obesity are chronic diseases that contribute to excess morbidity and mortality. Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the ...
The 2013 White Paper from the American Nurse Practitioners Foundation on the Prevention and Treatment of Obesity considers a food diary as an important evidence‐based nutritional intervention in aiding weight loss (ANPF). ... Obesity Research & Clinical Practice, 9 (5), 435-447. [Google Scholar] Musunuru, K. (2010).
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Obesity, mortality and BMI. Obesity, as defined by BMI (Table 1), is associated with an increased risk of all-cause mortality, with CVD and malignancy being the most common causes of death. 5 -8 A meta-analysis of 239 prospective studies involving 10.6 million individuals from Asia, Australia, New Zealand, Europe and North America found that all-cause mortality was lowest between a BMI of 20 ...
The findings from our approach suggest with high predictive accuracy that by 2030 nearly 1 in 2 adults will have obesity (48.9%; 95% confidence interval [CI], 47.7 to 50.1), and the prevalence ...
Obesity prevalence among children is >30% in the Cook Islands, Nauru and Palau, with a notable increase over the past few decades. Worldwide prevalence of obesity increased at an alarming rate in ...
Welcome to the. International Journal of Obesity. Publishing the latest research and reviews on biochemical, physiological, genetic, molecular, metabolic, nutritional, psychological and ...
Background. There has been a significant global increase in obesity rate during the last 50 years. Obesity is defined as when a person has a body mass index [BMI (kg/m 2), dividing a person's weight by the square of their height] greater than or equal to 30, overweight is defined as a BMI of 25.0-29.9.Being overweight or obesity is linked with more deaths than being underweight and is a more ...
The research highlighted the multifaceted aetiology of obesity, which extends beyond personal lifestyle choices to encompass genetic, physiological, socioeconomic and environmental factors.
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity. Consequently, this ...
Obesity is the official journal of The Obesity Society and is the premier source of information for increasing knowledge, fostering translational research from basic to population science, and promoting better treatment for people with obesity.Obesity publishes important peer-reviewed research and cutting-edge reviews.
Globally, obesity is on the rise. Research over the past 20 years has highlighted the far-reaching multisystem complications of obesity, but a better understanding of its complex pathogenesis is needed to identify safe and lasting solutions. ... (found in many items of daily life including plastics, food, clothing, cosmetics, and paper) are ...
The Obesity Society (TOS) first published a position statement on obe-sity as a disease in 2008 (1). This statement reflected the thoughtful deliberations and consensus of Society members that was published in the same year (2). In 2016, an updated in-house position paper affirmed the 2008 declaration, stating, "TOS recommits to its position ...
See the 2020-2030 Strategic Plan for NIH Nutrition Research. The NHLBI is an active member of the National Collaborative on Childhood Obesity (NCCOR) external link. , which is a public-private partnership to accelerate progress in reducing childhood obesity. The NHLBI has been providing guidance to physicians on the diagnosis, prevention ...
Future childhood obesity research should evaluate the best methods for educating primary care providers in providing family-centered care and the optimal approaches to delivering this care. ... and was drafter of the manuscript. Dr Brian A. Lynch and Dr. John M. Wilkinson contributed equally to work on paper by critically reviewing literature ...
Obesity is a multi-factorial disorder, which is often associated with many other significant diseases such as diabetes, hypertension and other cardiovascular diseases, osteoarthritis and certain cancers. The management of obesity will therefore require a comprehensive range of strategies focussing on those with existing weight problems and also on those at high risk of developing obesity ...
1. Introduction. Obesity is a chronic disease that is increasing in prevalence and is now considered to be a global epidemic. Epidemiologic studies have revealed an association between high body mass index (BMI) and an extensive range of chronic diseases such as Non Alcoholic Fatty Liver (NAFL), cardiovascular disease , , diabetes mellitus , several malignancies , , musculoskeletal diseases ...
Pediatric Obesity. is a leading journal presenting high-quality papers that contain the latest research on obesity during childhood and adolescence.. Topics include: Genetic, molecular, biochemical and physiological aspects of obesity—basic, applied and clinical studies; Metabolic consequences of child and adolescent obesity
Obesity is a chronic, prevalent, and complex health condition that adversely impairs physical and mental health. The World Health Organization calls for integrating obesity care into existing chronic disease management programs within primary healthcare services. This scoping review aimed to examine registered nurses' roles in the primary healthcare management of individuals with obesity.
This paper, together with Yeo et al. (1998), shows that heterozygous mutations in MC4R result in severe human obesity, establishing the role of the central melanocortin pathway in regulating human ...
The incidence rate ratio for obesity-related cancer was higher in younger generations compared to those born in 1962-1966. We predict that the ASR for obesity-related cancers will nearly double in the next decade. Conclusions: The rising incidence of obesity-related cancers among young adults poses a significant public health concern. The ...
Objective Breast-conserving therapy (BCT) includes breast-conserving surgery (BCS) combined with radiation therapy (RT). RT plays a crucial role in improving the prognosis of patients who undergo BCS. However, obesity is a potential risk factor for resistance to radiation. The aim of this study was to evaluate any difference in the long-term prognosis of patients with early stage breast cancer ...
Areas of Expertise: Environmental influences and population-level interventions on obesity, weight-related behaviors and outcomes across the life course; Social and economic determinants and policies affecting physical, mental, and cognitive health in children, adults of all ages, and individuals with disabilities; Applications of artificial intelligence and data analytics for public health ...
Glucagon-like peptide 1 (GLP-1) agonists are medications approved for treatment of diabetes that recently have also been used off label for weight loss. 1 Studies have found increased risks of gastrointestinal adverse events (biliary disease, 2 pancreatitis, 3 bowel obstruction, 4 and gastroparesis 5) in patients with diabetes. 2-5 Because such patients have higher baseline risk for ...
Two new studies find that the popular weight loss and diabetes drug semaglutide, sold under the brand names Ozempic and Wegovy, does not increase the risk of depression and suicide. millaf - stock ...
Jeff Shander, Research Associate in Professor Alan Kay's lab in the Department of Biology, contributed to a decade-long research project that culminated in the publication of the article "The human cell count and size distribution" in the Proceedings of the National Academy of Science journal! Shander's dedication to studying human proteins and their relationship to disease, combined ...
Obesity is a condition in which excess fat has accumulated in the body, such that it can have an adverse effect on health. Obesity is defined as a body mass index (BMI) of greater than 30 kg/m2.
Two graduate students in Melkani's lab, Chris Livelo and Yiming Guo, are co-first authors of the paper. "Obesity is a global health concern associated with various health issues and economic challenges," said Melkani, researcher in the Division of Molecular and Cellular Pathology.
Both research groups described how obesity prevalence has increased in the last few decades. The GBD study showed that between 1980 and 2015 obesity prevalence doubled in 73 countries and showed an increase in most of the other countries as well. ... This study is one of this group's most recent papers to document US obesity prevalence during ...