

Understanding psychotherapy and how it works
Learn how to choose a psychologist, how therapy works, how long it lasts, and what should and shouldn’t happen during psychotherapy
- Psychotherapy

Do you ever feel too overwhelmed to deal with your problems? If so, you’re not alone.
According to the National Institute of Mental Health , more than a quarter of American adults experience depression, anxiety, or another mental disorder in any given year. Others need help coping with a serious illness, losing weight, or stopping smoking. Still others struggle to cope with relationship troubles, job loss, the death of a loved one, stress, substance abuse, or other issues. And these problems can often become debilitating.
What is psychotherapy?
A psychologist can help you work through such problems. Through psychotherapy, psychologists help people of all ages live happier, healthier, and more productive lives.
In psychotherapy, psychologists apply scientifically validated procedures to help people develop healthier, more effective habits. There are several approaches to psychotherapy—including cognitive-behavioral, interpersonal, and other kinds of talk therapy—that help individuals work through their problems.
Psychotherapy is a collaborative treatment based on the relationship between an individual and a psychologist. Grounded in dialogue, it provides a supportive environment that allows you to talk openly with someone who’s objective, neutral, and nonjudgmental. You and your psychologist will work together to identify and change the thought and behavior patterns that are keeping you from feeling your best.
By the time you’re done, you will not only have solved the problem that brought you in, but you will have learned new skills so you can better cope with whatever challenges arise in the future.
When should you consider psychotherapy?
Because of the many misconceptions about psychotherapy , you may be reluctant to try it out. Even if you know the realities instead of the myths, you may feel nervous about trying it yourself.
Some people seek psychotherapy because they have felt depressed, anxious, or angry for a long time. Others may want help for a chronic illness that is interfering with their emotional or physical well-being. Still others may have short-term problems they need help navigating. They may be going through a divorce, facing an empty nest, feeling overwhelmed by a new job, or grieving a family member’s death, for example.
Signs that you could benefit from therapy include:
- You feel an overwhelming, prolonged sense of helplessness and sadness
- Your problems don’t seem to get better despite your efforts and help from family and friends
- You find it difficult to concentrate on work assignments or to carry out other everyday activities
- You worry excessively, expect the worst, or are constantly on edge
- Your actions, such as drinking too much alcohol, using drugs, or being aggressive, are harming you or others
What are the different kinds of psychotherapy?
There are many different approaches to psychotherapy. Psychologists generally draw on one or more of these. Each theoretical perspective acts as a roadmap to help the psychologist understand their patients and their problems and develop solutions.
The kind of treatment you receive will depend on a variety of factors: current psychological research, your psychologist’s theoretical orientation, and what works best for your situation.
Your psychologist’s theoretical perspective will affect what goes on in his or her office. Psychologists who use cognitive-behavioral therapy, for example, have a practical approach to treatment. Your psychologist might ask you to tackle certain tasks designed to help you develop more effective coping skills. This approach often involves homework assignments.
Your psychologist might ask you to gather more information, such as logging your reactions to a particular situation as they occur. Or your psychologist might want you to practice new skills between sessions, such as asking someone with an elevator phobia to practice pushing elevator buttons. You might also have reading assignments so you can learn more about a particular topic.
In contrast, psychoanalytic and humanistic approaches typically focus more on talking than doing. You might spend your sessions discussing your early experiences to help you and your psychologist better understand the root causes of your current problems.
Your psychologist may combine elements from several styles of psychotherapy. In fact, most therapists don’t tie themselves to any one approach. Instead, they blend elements from different approaches and tailor their treatment according to each patient’s needs.
The main thing to know is whether your psychologist has expertise in the area you need help with and whether your psychologist feels he or she can help you.
Finding a psychologist
Once you’ve decided to try psychotherapy, you need to find a psychologist.
Why choose a psychologist for psychotherapy?
Psychologists who specialize in psychotherapy and other forms of psychological treatment are highly trained professionals with expertise in mental health assessment, diagnosis, and treatment, and behavior change.
After graduating from a four-year undergraduate college or university, psychologists spend an average of seven years in graduate education and training to earn a doctoral degree. That degree may be a PhD, PsyD or EdD.
Psychologists pass a national examination and must be licensed by the state or jurisdiction in which they practice. Licensure laws are intended to protect the public by limiting licensure to those who are qualified to practice psychology as defined by state law. Most states also require psychologists to stay up-to-date by earning several hours of continuing education credits annually.
In addition, APA members adhere to a strict code of professional ethics.
How do I find a psychologist?
If you plan to use your insurance or employee assistance program to pay for psychotherapy, you may need to select a psychologist who is part of your insurance plan or employee assistance program. But if you’re free to choose, there are many ways to find a psychologist:
- Ask trusted family members and friends.
- Ask your primary care physician, obstetrician/gynecologist, pediatrician, or another health professional. If you’re involved in a divorce or other legal matters, your attorney may also be able to provide referrals.
- Search online for psychologists’ websites.
- Contact your area community mental health center.
- Consult a local university or college department of psychology.
- Call your local or state psychological association , which may have a list of practicing psychologists organized by geographic area or specialty.
Or use a trusted online directory, such as APA’s Psychologist Locator service . This service makes it easy for you to find practicing psychologists in your area.
Psychologists may work in their own private practice or with a group of other psychologists or health care professionals. Practicing psychologists also work in schools, colleges and universities, hospitals, health systems and health management organizations, veterans’ medical centers, community health and mental health clinics, businesses and industry, and rehabilitation and long-term care centers.
Selecting a psychologist
APA estimates that there are about 85,000 licensed psychologists in the United States. How can you find the one who’s right for you?
Psychologists and patients work together, so the right match is important. Good “chemistry” with your psychologist is critical, so don’t be afraid to interview potential candidates about their training, clinical expertise, and experience treating problems like yours. Whether you interview a psychologist by phone, during a special 15-minute consultation, or at your first session, look for someone who makes you feel comfortable and inspires confidence.
But it’s also important to check more practical matters, too.
What should you ask yourself?
When you’re ready to select a psychologist, think about the following points:
- Do you want to do psychotherapy by yourself, with your partner or spouse, or with your children?
- What are your main goals for psychotherapy?
- Will you use your health insurance or employee assistance program to pay for psychotherapy?
- If you’ll be paying out of pocket, how much can you afford?
- How far are you willing to drive?
- What days and times would be convenient?
What should you ask a psychologist?
You’ll need to gather some information from the psychologists whose names you have gathered.
The best way to make initial contact with a psychologist is by phone. While you may be tempted to use email, it’s less secure than the telephone when it comes to confidentiality. A psychologist will probably call you back anyway. And it’s faster for everyone to talk rather than have to write everything down.
Psychologists are often with patients and don’t always answer their phones right away. Just leave a message with your name, phone number, and brief description of your situation.
Once you connect, some questions you can ask a psychologist are:
- Are you accepting new patients?
- Do you work with men, women, children, teens, couples, or families? (Whatever group you are looking for.)
- Are you a licensed psychologist in the state where I live?
- How many years have you been practicing?
- What are your areas of expertise?
- Do you have experience helping people with symptoms or problems like mine?
- What is your approach to treatment? Have the treatments you use been proven effective for dealing with my problem?
- What are your fees? Do you have a sliding-scale policy if I can’t afford your regular fees? Do you accept credit cards or personal checks? Do you expect payment at the time of service?
- Do you accept my insurance? Are you affiliated with any managed care organizations? Do you accept Medicare or Medicaid?
- Will you accept direct billing to or payment from my insurance company?
- What are your policies concerning things like missed appointments?
If you have particular concerns that are deal-breakers for you, ask the psychologist about them. You might want to work with a psychologist who shares your religious views or cultural background, for example. While some psychologists are more open to disclosing personal information than others, the response will give you important information about whether you’ll work well together.
While you’re assessing a psychologist, he or she will also be assessing you. To ensure that psychotherapy is successful, the psychologist must determine whether there’s a good match when it comes to personality as well as professional expertise. If the psychologist feels the fit isn’t right—perhaps because you need someone with a different specialty area—he or she will refer you to another psychologist who can help.
Getting started
How can i pay for psychotherapy.
If you have private health insurance or are enrolled in a health maintenance organization or other type of managed care plan, it may cover mental health services such as psychotherapy. Before you start psychotherapy, you should check with your insurance plan to see what is covered.
Thanks to the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 , group insurers of more than 50 employees that offer mental health and substance use services must cover both mental and physical health equally. That means insurers are no longer allowed to charge higher copays or deductibles for psychological services or arbitrarily limit the number of psychotherapy sessions you can receive.
However, insurance companies vary in terms of which mental health conditions they cover. That means some insurance policies may not cover certain mental health disorders.
Government-sponsored health care programs are another potential source of mental health services. These include Medicare for people age 65 and older and people with disabilities, as well as health insurance plans for military personnel and their dependents. In some states, Medicaid programs may also cover mental health services provided by psychologists.
Other options include community mental health centers, free clinics, religious organizations, and university and medical center training programs. These groups often offer high-quality services at low cost.
What should I ask my insurance company?
Look on the back of your insurance card for a phone number for mental or behavioral health or call your insurance company’s customer service number. Before your first psychotherapy appointment, ask your insurer the following questions:
- Does my plan cover mental health services?
- Do I have a choice about what kind of mental health professionals I can see? Ask whether your plan covers psychologists and what kinds of treatments are covered and excluded.
- Is there a deductible? In some plans, you have to pay a certain amount yourself before your benefits start paying. Also ask how much the deductible is, what services count toward your deductible and when your deductible amount starts over again. Some deductibles re-set at the first of the year, for example, while others re-set at the beginning of your employer’s fiscal year.
- What is my copayment? Your plan probably requires you to pay for part of treatment yourself by paying either a set amount or a percentage of the fee directly to your psychologist for each treatment session.
- Is there a limit to the number of sessions? Unlike group or employer-based insurance that must provide mental health parity, private insurance does not. It may only be willing to pay for a certain number of sessions.
Making your first appointment
You may feel nervous about contacting a psychologist. That anxiety is perfectly normal. But having the courage to overcome that anxiety and make a call is the first step in the process of empowering yourself to feel better. Just making a plan to call and sticking to it can bring a sense of relief and put you on a more positive path.
Psychologists understand how difficult it can be to make initial contact. The first call is something new for you, but it’s something they handle regularly. Leave a message with your name, your contact number, and why you are calling. It’s enough to just say that you are interested in knowing more about psychotherapy. Once your call is returned, they’ll lead a brief conversation to get a better sense of what you need, whether they are able to help, and when you can make an appointment.
You might be tempted to take the first available appointment slot. Take a few minutes to stop and think before you do. If it does not fit with your schedule, you can ask if there are other times available that might fit better for you.
What factors should you consider?
You’ll need to think about the best time of day and week to see your psychologist. Factors to consider include:
- Your best time of day. Whether you’re a morning person or a night owl, know when you’re at your best and schedule your appointment accordingly.
- Work. If you have to take time off from work, ask your human resources department if you can use sick leave for your psychotherapy sessions. You might also want to schedule your first appointment later in the day so you don’t have to go back to work afterward. If you have an upsetting topic to discuss, you may be tired, emotionally spent, puffy-eyed, or distracted after your first session.
- Family responsibilities. Unless your children are participating in treatment, it’s usually not a good idea to bring them along. Choose a time when you will have child care available.
- Other commitments. A psychotherapy session typically lasts 45 to 50 minutes. Try to schedule your session at a time when you won’t have to rush to your next appointment afterward. Worrying about being late to your next commitment will distract you from your psychotherapy session.
How should I prepare for the appointment?
Once you’ve made an appointment, ask your psychologist how you should prepare. A psychologist might ask you to:
- Call your insurer to find out what your outpatient mental health benefits cover, what your copay is, and whether you have a deductible. If you don’t get this information ahead of time, your psychologist may ask you to come to your appointment a little early so he or she can help you verify your benefits.
- Fill out new patient paperwork for your psychologist. Your psychologist may have a website with forms you can download and fill out before you arrive at your appointment. If not, you can ask your psychologist to get you the forms and fill them out at home rather than while sitting in the psychologist’s waiting room. Your psychologist may also provide a packet of materials covering logistical issues, such as cancellation fees and confidentiality.
- Get records from other psychologists or health care providers you’ve seen.
- You may also want to prepare a list of questions, such as the average treatment duration, the psychologist’s feelings about medication, or good books on your issue.
- Learn about therapy. If any of your friends have done psychotherapy, ask them what it was like. Or read up on the subject. If you’ve had psychotherapy before, think about what you liked and didn’t like about your former psychologist’s approach.
- Keep an open mind. Even if you’re skeptical about psychotherapy or are just going because someone told you to, be willing to give it a try. Be willing to be open and honest so you can take advantage of this opportunity to learn more about yourself.
- Make sure you know where you’re going. Check the psychologist’s website or do a map search for directions to the psychologist’s office.
Going to your first appointment
It’s normal to feel nervous when you head off to your first psychotherapy appointment. But preparing ahead of time and knowing what to expect can help calm your nerves.
What should I bring?
A typical psychotherapy session lasts 45 to 50 minutes. To make the most of your time, make a list of the points you want to cover in your first session and what you want to work on in psychotherapy. Be prepared to share information about what’s bringing you to the psychologist. Even a vague idea of what you want to accomplish can help you and your psychologist proceed efficiently and effectively.
If you’re on any medications, jot down which medications and what dosage so your psychologist can have that information.
It can be difficult to remember everything that happens during a psychotherapy session. A notebook can help you capture your psychologist’s questions or suggestions and your own questions and ideas. Jotting a few things down during your session can help you stay engaged in the process.
Most people have more than a single session of psychotherapy. Bring your calendar so you can schedule your next appointment before you leave your psychologist’s office.
You’ll also need to bring some form of payment. If you’ll be using your health insurance to cover your psychotherapy, bring along your insurance card so your psychologist will be able to bill your insurer. (Some insurers require psychologists to check photo IDs, so bring that along, too.) If you’ll be paying for psychotherapy out of pocket, bring along a credit card, checkbook, or cash.
What should I expect?
For your first session, your psychologist may ask you to come in a little early to fill out paperwork if you haven’t already done so.
Don’t worry that you won’t know what to do once the session actually begins. It’s normal to feel a little anxious in the first few sessions. Psychologists have experience setting the tone and getting things started. They are trained to guide each session in effective ways to help you get closer to your goals. In fact, the first session might seem like a game of 20 questions.
Sitting face to face with you, your psychologist could start off by acknowledging the courage it takes to start psychotherapy. He or she may also go over logistical matters, such as fees, how to make or cancel an appointment, and confidentiality, if he or she hasn’t already done so by phone.
Your psychologist will also want to know about your own and your family’s history of psychological problems such as depression, anxiety, or similar issues. You’ll also explore how your problem is affecting your everyday life. Your psychologist will ask questions like whether you’ve noticed any changes in your sleeping habits, appetite or other behaviors. A psychologist will also want to know what kind of social support you have, so he or she will also ask about your family, friends and coworkers.
It’s important not to rush this process, which may take more than one session. While guiding you through the process, your psychologist will let you set the pace when it comes to telling your story. As you gain trust in your psychologist and the process, you may be willing to share things you didn’t feel comfortable answering at first.
Once your psychologist has a full history, the two of you will work together to create a treatment plan. This collaborative goal-setting is important, because both of you need to be invested in achieving your goals. Your psychologist may write down the goals and read them back to you so you’re both clear about what you’ll be working on. Some psychologists even create a treatment contract that lays out the purpose of treatment, its expected duration, and goals, with both the individual’s and psychologist’s responsibilities outlined.
At the end of your first session, the psychologist may also have suggestions for immediate action. If you’re depressed, for example, the psychologist might suggest seeing a physician to rule out any underlying medical conditions, such as a thyroid disorder. If you have chronic pain, you may need physical therapy, medication, and help for insomnia as well as psychotherapy.
By the end of the first few sessions, you should have a new understanding of your problem, a game plan, and a new sense of hope.
Undergoing psychotherapy
Psychotherapy is often referred to as talk therapy, and that’s what you’ll be doing as your treatment continues. You and your psychologist will engage in a dialogue about your problems and how to fix them.
What should I expect as I continue psychotherapy?
As your psychotherapy goes on, you’ll continue the process of building a trusting, therapeutic relationship with your psychologist.
As part of the ongoing getting-to-know-you process, your psychologist may want to do some assessment. Psychologists are trained to administer and interpret tests that can help to determine the depth of your depression, identify important personality characteristics, uncover unhealthy coping strategies such as drinking problems, or identify learning disabilities.
If parents have brought in a bright child who’s nonetheless struggling academically, for example, a psychologist might assess whether the child has attention problems or an undetected learning disability. Test results can help your psychologist diagnose a condition or provide more information about the way you think, feel and behave.
You and your psychologist will also keep exploring your problems through talking. For some people, just being able to talk freely about a problem brings relief. In the early stages, your psychologist will help you clarify what’s troubling you. You’ll then move into a problem-solving phase, working together to find alternative ways of thinking, behaving, and managing your feelings.
You might role-play new behaviors during your sessions and do homework to practice new skills in between. As you go along, you and your psychologist will assess your progress and determine whether your original goals need to be reformulated or expanded.
In some cases, your psychologist may suggest involving others. If you’re having relationship problems, for instance, having a spouse or partner join you in a session can be helpful. Similarly, an individual having parenting problems might want to bring his or her child in. And someone who has trouble interacting with others may benefit from group psychotherapy.
As you begin to resolve the problem that brought you to psychotherapy, you’ll also be learning new skills that will help you see yourself and the world differently. You’ll learn how to distinguish between situations you can change and those you can’t and how to focus on improving the things within your control.
You’ll also learn resilience, which will help you better cope with future challenges. A 2006 study of treatment for depression and anxiety , for example, found that the cognitive and behavioral approaches used in psychotherapy have an enduring effect that reduces the risk of symptoms returning even after treatment ends. Another study found a similar result when evaluating the long-term effects of psychodynamic psychotherapy .
Soon you’ll have a new perspective and new ways of thinking and behaving.
How can I make the most of psychotherapy?
Psychotherapy is different from medical or dental treatments, where patients typically sit passively while professionals work on them and tell them their diagnosis and treatment plans. Psychotherapy isn’t about a psychologist telling you what to do. It’s an active collaboration between you and the psychologist.
So be an active, engaged participant in psychotherapy. Help set goals for treatment. Work with your psychologist to come up with a timeline. Ask questions about your treatment plan. If you don’t think a session went well, share that feedback and have a dialogue so that the psychologist can respond and tailor your treatment more effectively. Ask your psychologist for suggestions about books or websites with useful information about your problems.
And because behavior change is difficult, practice is also key. It’s easy to fall back into old patterns of thought and behavior, so stay mindful between sessions. Notice how you’re reacting to things and take what you learn in sessions with your psychologist and apply it to real-life situations. When you bring what you’ve learned between sessions back to your psychologist, that information can inform what happens in his or her office to further help you.
Through regular practice, you’ll consolidate the gains you’ve made, get through psychotherapy quicker, and maintain your progress after you’re done.
Should I worry about confidentiality?
Psychologists consider maintaining your privacy extremely important. It is a part of their professional code of ethics. More importantly, it is a condition of their professional license. Psychologists who violate patient confidentiality risk losing their ability to practice psychology in the future.
To make your psychotherapy as effective as possible, you need to be open and honest about your most private thoughts and behaviors. That can be nerve-wracking, but you don’t have to worry about your psychologist sharing your secrets with anyone except in the most extreme situations.
If you reveal that you plan to hurt yourself or others, for example, your psychologist is duty-bound to report that to authorities for your own protection and the safety of others. Psychologists must also report abuse, exploitation, or neglect of children, the elderly, or people with disabilities. Your psychologist may also have to provide some information in court cases.
Of course, you can always give your psychologist written permission to share all or part of your discussions with your physician, teachers, or anyone else if you desire.
Psychologists take confidentiality so seriously that they may not even acknowledge that they know you if they bump into you at the supermarket or anywhere else. And it’s OK for you to not say hello either. Your psychologist won’t feel bad; he or she will understand that you’re protecting your privacy.
Understanding medication
In our quick-fix culture, people often hope a pill will offer fast relief from such problems as depression or anxiety. And primary care physicians or nurse practitioners—most people’s first contact when they have a psychological problem—are typically trained to prescribe medication. They don’t have the extensive training or the time to provide psychotherapy.
Is medication effective?
There are some psychological conditions, such as severe depression, bipolar disorder, or schizophrenia, where medication is clearly warranted. But many other cases are less clear-cut.
Evidence suggests that in many cases, medication doesn’t always work. In a 2010 study in the Journal of the American Medical Association , for instance, researchers reviewed previous research on the effectiveness of antidepressants . They found that antidepressants did help people with severe cases of depression. For mild to moderate depression, however, the medication wasn’t any more effective than a placebo.
What’s more, medications don’t help you develop the skills you need to deal with life’s problems. Once you stop taking medication, your problems often remain or come back. In contrast, psychotherapy will teach you new problem-solving strategies that will also help you cope with future problems.
Do I need medication?
If you can function relatively well—meaning you can function well at work or school and have healthy relationships with family and friends—the answer is probably no. Psychotherapy alone can be very effective. Or you might just need a more balanced lifestyle—one that combines work, exercise, and social interactions.
Medication can be useful in some situations, however. Sometimes, people need medication to get to a point where they’re able to engage in psychotherapy. Medication can also help those with serious mental health disorders. For some conditions, combining psychotherapy and medication works best.
How can I get medication if I need it?
If you need medication, your psychologist will work with your primary care provider or a psychiatrist to ensure a coordinated approach to treatment that is in your best interest.
Five states, Idaho, Illinois, Iowa, Louisiana, and New Mexico, have laws allowing licensed psychologists with advanced training to prescribe certain medications to treat emotional and mental health problems. In those states, the psychologists must have completed a specialized training program (often earning a master’s degree in psychopharmacology), passed an examination for prescribing, and be additionally licensed as prescribing psychologists.
Assessing psychotherapy’s effectiveness
Some people wonder why they can’t just talk about their problems with family members or friends. Psychologists offer more than someplace to vent. Psychologists have years of training and experience that help people improve their lives. And there is significant evidence showing that psychotherapy is a very effective treatment.
How does psychotherapy work?
Successful treatment is the result of three factors working together:
- Evidence-based treatment that is appropriate for your problem
- The psychologist’s clinical expertise
- Your characteristics, values, culture, and preferences
When people begin psychotherapy, they often feel that their distress is never going to end. Psychotherapy helps people understand that they can do something to improve their situation. That leads to changes that enhance healthy behavior, whether it’s improving relationships, expressing emotions better, doing better at work or school, or thinking more positively.
While some issues and problems respond best to a particular style of therapy, what remains critical and important is the therapeutic alliance and relationship with your psychologist.
What if psychotherapy doesn’t seem to be working?
When you began psychotherapy, your psychologist probably worked with you to develop goals and a rough timeline for treatment. As you go along, you should be asking yourself whether the psychologist seems to understand you, whether the treatment plan makes sense, and whether you feel like you’re making progress.
Keep in mind that as psychotherapy progresses, you may feel overwhelmed. You may feel more angry, sad, or confused than you did at the beginning of the process. That doesn’t mean psychotherapy isn’t working. Instead, it can be a sign that your psychologist is pushing you to confront difficult truths or do the hard work of making changes. In such cases, these strong emotions are a sign of growth rather than evidence of a standstill. Remember, sometimes things may feel worse before they get better.
In some cases, of course, the relationship between a patient and the psychologist isn’t as good as it should be. The psychologist should be willing to address those kinds of issues, too. If you’re worried about your psychologist’s diagnosis of your problems, it might be helpful to get a second opinion from another psychologist, as long as you let your original psychologist know you’re doing so.
If the situation doesn’t improve, you and your psychologist may decide it’s time for you to start working with a new psychologist. Don’t take it personally. It’s not you; it’s just a bad fit. And because the therapeutic alliance is so crucial to the effectiveness of psychotherapy, you need a good fit.
If you do decide to move on, don’t just stop coming to your first psychologist. Instead, tell him or her that you’re leaving and why you’re doing so. A good psychologist will refer you to someone else, wish you lucky, and urge you not to give up on psychotherapy just because your first attempt didn’t go well. Tell your next psychologist what didn’t work to help ensure a better fit.
Knowing when you’re done
You might think that undergoing psychotherapy means committing to years of weekly treatment. Not so.
How long should psychotherapy take?
How long psychotherapy takes depends on several factors: the type of problem or disorder, the patient’s characteristics and history, the patient’s goals, what’s going on in the patient’s life outside psychotherapy, and how fast the patient is able to make progress.
Some people feel relief after only a single session of psychotherapy. Meeting with a psychologist can give a new perspective, help them see situations differently, and offer relief from pain. Most people find some benefit after a few sessions, especially if they’re working on a single, well-defined problem and didn’t wait too long before seeking help.
Other people and situations take longer—maybe a year or two—to benefit from psychotherapy. They may have experienced serious traumas, have multiple problems, or just be unclear about what’s making them unhappy. It’s important to stick with psychotherapy long enough to give it a chance to work.
People with serious mental illness or other significant life changes may need ongoing psychotherapy. Regular sessions can provide the support they need to maintain their day-to-day functioning.
Others continue psychotherapy even after they solve the problems that brought them there initially. That’s because they continue to experience new insights, improved well-being, and better functioning.
How do I know when I’m ready to stop?
Psychotherapy isn’t a lifetime commitment.
In one classic study, half of psychotherapy patients improved after eight sessions. And 75% improved after six months.
You and your psychologist will decide together when you are ready to end psychotherapy. One day, you’ll realize you’re no longer going to bed and waking up worrying about the problem that brought you to psychotherapy. Or you will get positive feedback from others. For a child who was having trouble in school, a teacher might report that the child is no longer disruptive and is making progress both academically and socially. Together you and your psychologist will assess whether you’ve achieved the goals you established at the beginning of the process.
What happens after psychotherapy ends?
You probably visit your physician for periodic check-ups. You can do the same with your psychologist.
And don’t think of psychotherapy as having a beginning, middle and end. You can solve one problem, then face a new situation in your life and feel the skills you learned during your last course of treatment need a little tweaking. Just contact your psychologist again. After all, he or she already knows your story.
Of course, you don’t have to wait for a crisis to see your psychologist again. You might just need a “booster” session to reinforce what you learned last time. Think of it as a mental health tune-up.
The American Psychological Association gratefully acknowledges the assistance of June Ching, PhD; Angela Londoño-McConnell, PhD; Elaine Ducharme, PhD; Terry Gock, PhD; Bethe Lonning, PsyD; Nancy Molitor, PhD; Dianne Polowczyk, PhD; and Michael Ritz, PhD, in developing this material.

Related Reading
- Protecting your privacy: Understanding confidentiality
You may also like
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol
Psychotherapy: A World of Meanings
Despite a wealth of findings that psychotherapy is an effective psychological intervention, the principal mechanisms of psychotherapy change are still in debate. It has been suggested that all forms of psychotherapy provide a context which enables clients to transform the meaning of their experiences and symptoms in such a way as to help clients feel better, and function more adaptively. However, psychotherapy is not the only health care intervention that has been associated with “meaning”: the reason why placebo has effects has also been proposed to be a “meaning response.” Thus, it has been argued that the meaning of treatments has a central impact on beneficial (and by extension, negative) health-related responses. In light of the strong empirical support of a contextual understanding of psychotherapy and its effects, the aim of this conceptual analysis is to examine the role of meaning and its transformation in psychotherapy—in general—and within three different, commonly used psychotherapy modalities.
Introduction
Psychotherapy is an effective psychological intervention for a multitude of psychological, behavioral, and somatic problems, symptoms, and disorders and thus rightfully considered as a main approach in mental and somatic health care management ( Prince et al., 2007 ; Goldfried, 2013 ). But despite the wealth of empirical findings, the principal mechanisms of psychotherapy change are still in debate ( Wampold and Imel, 2015 ). Two rival models have been contested ever since the very beginning of psychotherapy research, when some 80 years ago Saul Rosenzweig wondered, “whether the factors alleged to be operating in a given therapy are identical with the factors that actually are operating and whether the factors that actually are operating in several different therapies may not have much more in common than have the factors alleged to be operating.” ( Rosenzweig, 1936 , p. 412). Rosenzweig questioned the common understanding of psychotherapy, in which it is assumed that specific techniques have specific effects. This proposition was later elaborated through the work of Jerome Frank who argued that all forms of psychotherapy provide a context which enables patients to transform the meaning of their experiences and symptoms in such a way as to help them to feel better, function more favorably, and think more adaptively ( Frank, 1986 ).
Interestingly and central to this paper, psychotherapy is not the only psychological intervention which has been associated with meaning. Following the assumption that “meaning responses are always there” ( Moerman, 2006 , p. 234)—i.e., in any medical and psychological treatment—the attribution of meaning has also been considered as an overarching mechanism for those treatment effects which placebo controls for in clinical trials. Thus, the attribution of a therapeutic meaning to a given intervention has a central impact on health-related responses ( Barrett et al., 2006 ).
The contextual model of psychotherapy remains topical ( Kirsch et al., 2016 ), and also controversial ( Marcus et al., 2014 ). The model has been developed to propose that it is the “common factors” (e.g., client-therapist relationship, clients’ expectations, trust, understanding, and expertise) across different versions of psychotherapy that explain their effectiveness (for details, see Wampold et al. (2011) ). The hypothesis for the general equivalence of various forms of psychotherapies is usually referred to as the dodo bird conjecture ( Rosenzweig, 1936 ). Hence, the contextual model of psychotherapy is markedly in contrast with the long-held assumption that specific methods are at the root of psychotherapy’s effects. The assumption that psychotherapy’s effects can be reduced to incidental—or contextual—constituents, which are typically called common or unspecific factors, has been a constant in psychotherapy research ( Luborsky et al., 2002 ; Gaab et al., 2016 ) but at least in terms of empirical evidence, there is sound reason and accumulating empirical support for a contextual understanding of psychotherapy ( Wampold and Imel, 2015 ). For example, a number of meta-analyses showed that various bona fide psychotherapies, i.e., therapies with a clear treatment rationale but with very different underlying theories, aims, and methods appear to be equally effective ( Spielmans et al., 2007 ; Cuijpers et al., 2008 ; Barth et al., 2013 ; Frost et al., 2014 ). In addition, opposing treatment approaches with the same treatment rationale have shown to be equally effective in a trial on clients with panic disorder ( Kim et al., 2012 ) as much as similar treatments provided with opposing treatment rationales have shown to differ in their effects ( Tondorf et al., 2017 ).
Building on the strong empirical support for a contextual understanding of psychotherapy ( Wampold and Imel, 2015 ), which proposes the transformation of meaning as its central mechanisms, the aim of this conceptual analysis is to examine the role of meaning and its transformation in psychotherapy in general and in three different and commonly used psychotherapy approaches.
In Search of a New Meaning
The main incentive to undergo a psychotherapy treatment is to change the general level of functioning, as well as to reduce the symptoms of suffering ( Strong and Matross, 1973 ). Clients’ belief that they are unable or incapable of solving disturbing problems contributes to demoralization and feelings of confusion, despair, and incompetence ( Vissers et al., 2010 ) or as Frank (1986) put it: “Often an important feature of demoralization is a sense of confusion resulting from the client’s inability to make sense out of his experiences or to control them, leading to the commonly expressed fear of going insane” (p. 341). This demoralization is not only a shared aspect of various psychological disorders, but can also be considered as a starting point for change in psychotherapy. Therapeutic change is thereby accompanied by clients “working through” their problems, gaining insight, achieving personal fulfillment, and becoming self-actualized, eventually transforming their problems and symptoms, self-perception, and experiences with their social environment ( Evans, 2013 ; Krause et al., 2015 ).
Frank (1986) stated that psychotherapy seeks to help clients to transform the meanings of their problems and symptoms and to overcome confusion with newly acquired clarity, i.e., by offering a narrative that links symptoms with hypothesized causes and providing a collaborative procedure for overcoming the suffering. Likewise, Wampold (2007) defined the core of psychotherapy in the transformation of non-adaptive explanations for their problems into new and more adaptive ones. Also, Dan Moerman ( Moerman, 2002 ) stated that “it sounds reasonable to me to say that psychotherapy evokes meaning responses” (p. 94) and that psychotherapy supports clients to create their stories and myths, although therapists are not considered a mandatory requirement for this ( Moerman, 2002 ). It should be noted that other mechanisms underlying positive response to psychotherapy have been proposed, e.g., reward mechanisms in psychotherapy ( Northoff and Boeker, 2006 ; Panksepp and Solms, 2012 ).
Considering processes of change in diverse interventions, narratives are thought to be created in order to render the demoralization less painful and promote remoralization ( Moerman, 2002 ). In this perspective, the therapists help their clients to give new meanings to their experiences or stories they tell, the language they use, and the beliefs they have ( Shaw, 2010 ).
Similar processes have been proposed to underlie placebo responses, which are “most likely to occur when the meaning of the illness experience is altered in a positive direction” ( Brody, 2000 ). These beneficial changes in meaning occur when three core conditions are present, which again resemble those proposed in the context of psychotherapy: (1) the clients feel listened to and receive a satisfactory, coherent explanation of their mental suffering and demoralization; (2) the client feels care and concern from the therapist; and (3) the clients feel an enhanced sense of mastery and control over their mental suffering (i.e., remoralization). A direct implementation can be seen in so-called narrative therapies, which are defined as “an approach that focuses on client stories with the goal of challenging existing meaning systems and creating more functional ones” ( Kropf and Tandy, 1998 ). Narrative approaches have come to a central role in systemic family therapy ( Carr, 1998 ; Wallis et al., 2011 ), emphasizing the role of language and how it affects the way clients frame their ideas of self and identity, while the therapist directly deals with clients’ concerns and the meaning of the worlds they live in ( Besley, 2002 ). Furthermore, it has been assumed that relying on the clients’ individual narratives is more significant than focusing on a pathological psychiatric diagnosis ( Gysin-Maillart et al., 2016 ). Of course, narrative therapies should not be mistaken as the exception of (dodo) rule, i.e., to be instances of “specific” therapies, but rather as possibilities to operationalize the rule in real life, i.e., to employ meaning processes in psychotherapy. Accordingly, it has been shown that meaning-making through language enhances clients’ well-being after a traumatic experience—which mainly stems from the connection, abstraction, and reflection of the whole experience ( Freda and Martino, 2015 ; Park et al., 2016 ).
Co-Construction of Narratives
To bring about these meaning transformations, psychotherapists mostly rely “on the use of words to form attitudes or induce actions” ( Frank, 1986 ). The overarching definition of a narrative is as a sequence of actions and events that involves a certain number of human beings as characters or actors ( Bruner, 1990 ). However, narratives differ from conventional discourse forms in variety of ways as narratives have an inherent sequentiality which is more than a just chronological sequence of lived experiences as it links the past to the present and future ( Bruner, 1990 ). A narrative creates a coherent whole out of a sequence of events ( Mattingly, 1994 ). In order to report an experience in a meaningful way, the protagonists not only focus on overt characteristics, but also reflect on their beliefs and feelings and how these are connected to their personal life in general ( Ochs and Capps, 1996 ). In regard to a broader social context, Justman (2011) argues that any information about a given intervention has an influence on the experience of clients receiving the intervention, which of course is particularly applicable for any form of psychotherapy.
In this understanding, any psychotherapy alleviates the symptoms of a target illness through meaning transformation. Thus, the relationship between narrative and illness—understood as the subjective experience of a given pathological process and their embedment in social context ( Engel, 1977 )—should briefly be exemplified. An illness narrative is defined as the important channel through which the meaning of an illness is created ( Kleinman, 1988 ). Thus, illness narratives do not merely reflect an illness experience, but they have been shown to be clinically relevant as they significantly impact on health behaviors and coping strategies as well as treatment outcomes ( Broadbent et al., 2004 ; Horne et al., 2007 ; Frenkel, 2008 ; Galli et al., 2010 ).
Furthermore, narratives are interdependent with the social context, so that therapists should use “images from the same sensory modality as that of the patient’s own imagery” ( Frank, 1986 ). The alternative narratives which are provided to the client in order to offer new and adaptive perspectives should be different but not too far off the client’s general beliefs ( Wampold, 2007 ) as much as exploring the clients’ narrative through attentive listening—both considered as key factors of healing processes ( Egnew, 2005 ; Mauksch et al., 2008 )—as they allow the therapist to reformulate and interpret the perceived meanings in a way that the clients can connect them with their personal conception of the world on the background of their beliefs and culture ( Strupp, 1986 ). Considering narratives in the psychotherapeutic encounter, the importance of the therapist’s and client’s co-construction of the narrative has been considered as a significant element of psychotherapy ( Brody, 1994 ) as jointly developed narratives significantly contribute to new forms of self-understanding and of being in the world ( Levitt et al., 2016 ). According to Brody (1994) , a shorter form of the client’s possible plea to the psychotherapist might be, “My story is broken; can you help me fix it?” (p. 85). Recovery in this understanding includes a deepening of a client’s experience and the development of a more comprehensive and coherent personal narrative ( Lysaker et al., 2011 ).
Truth Matters?
As outlined, the transformation of non-adaptive narratives into more adaptive ones is central to the contextual understanding of psychotherapy. This raises the question of the relationship between the narratives, i.e., their quality to induce subjective understanding, and the “real world,” i.e., the actual facts of a client’s life and actual causes of symptoms ( Kendler et al., 2011 ). Importantly, two kinds of narratives should be distinguished. First is the narrative behind the therapeutic approach, i.e., the healing narrative. Frank reasoned “that the chief criterion of the truth of any psychotherapeutic formulation is its plausibility” ( Frank, 1986 ). Hence, the explanation for why the treatment works should be plausible for both the therapist and the client. When the healing narrative is credible for the clients, they will discern and pick up on the aims and goals of therapy. Common factors associated with the healing narrative are for example the provision of an explanation for the client’s problems, therapeutic actions that are consistent with the explanation, as well as education ( Kirsch et al., 2016 ).
A second narrative is the client narrative that may emerge from therapy. This kind of narrative amounts to the actual change in the personal story, i.e., explanations that clients in therapy come to acquire about their own personality and reasons for their suffering. Common factors related with the client narrative are insight, corrective emotional experience, emotion regulation, and mindfulness among others ( Kirsch et al., 2016 ). Forming personal experiences into a narrative has further been associated with both physical and mental well-being and, accordingly, “psychotherapy is a more formal venue that often involves putting together a story” ( Pennebaker and Seagal, 1999 ). While this concept resonates with the now sadly predominant concept of “truthiness” (i.e., the quality of stating concepts or facts one wishes or believes to be true, rather than concepts or facts known to be true) in everyday life ( Metcalf, 2005 ), the understanding of plausibility in the context of a narrative is basically subjunctive or put otherwise: something is subjectively perceived to be possible ( Kleinman, 1988 ; Bruner, 1990 ). Further, this subjunctivity emphasizes that the anticipated future course is indispensably reported with some level of uncertainty, thus “to make a story good, it would seem, you must make it somewhat uncertain, somehow open to variant readings, rather subject to the vagaries of intentional states, undermined” ( Bruner, 1990 ). Likewise, Frank (1986) pointed out that “life histories do not provide adequate causal explanations of clients’ symptoms” (p. 343) and Jopling notes that “insights such as these may strike clients as entirely plausible and coherent, but neither plausibility nor coherence are, in themselves, a guarantee that the insights are true and that they fit the facts” ( Jopling, 2011 ). This corresponds with the idea that a client narrative emphasizes possibilities rather than predefined certainties ( Bruner, 2004 ) and that it not only copies reality as it is, but gives meaning to it through language ( Bruner, 1990 ). In turn, constructing the reality according to own beliefs and experiences affects as well as constitutes one’s self-perception. Accordingly, a client narrative is not only considered a personal report, but it also creates the identity of the story-teller ( Ricoeur, 1991 ). The self is reformed, which means that narrative and self are actually inseparable ( Ochs and Capps, 1996 ).
With these considerations in mind, the necessity of truth of an adaptive explanation for the client’s healing process comes into question. In this regard, it has been assumed that it might not be the truth itself that makes a narrative meaningful, yet rather its plausibility and “the extent to which a client is convinced by it” ( Frank, 1986 ). A plausible narrative for a mental disorder or a therapeutic change, respectively, invokes new information and is related to previous explanatory structures and networks of a client, when the new explanation is not too divergent from the previous one and takes a client’s perception of the world into account ( Wampold, 2007 ). Likewise, for clients who accept the treatment rationale, psychotherapeutic success occurs more quickly and psychotherapy outcomes are significantly better than for those who do not agree with the treatment rationale ( Addis and Jacobson, 2000 ; Overholser et al., 2010 ). However, the position that truth of a narrative is not the prerequisite for its meaningfulness does of course and in no way preclude psychotherapy and psychotherapists from the ethical obligations to respect clients’ autonomy. First, clients should not be deceived by providing false, but plausible narratives under any circumstances. Second, therapists should be aware to not withhold proven but possible implausible evidence about psychotherapy and psychotherapy change ( Blease et al., 2016 ; Gaab et al., 2016 ; Trachsel and Gaab, 2016 ).
Meaning Transformation in Psychotherapeutic Schools
Each psychotherapeutic school relies on a specific treatment theory, which addresses the connection between symptoms and hypothesized causes, as well as the process of therapeutic change. This treatment theory defines which treatment constituents are to be considered characteristic and which incidental ( Grünbaum, 1981 ). Although the various therapy approaches not only differ substantially in their operationalization of their constituents, but also in assignment to be either characteristic or incidental (e.g., the therapeutic alliance, Flückiger et al. (2012) ), they explicitly or implicitly promote a meaningful transformation regarding how clients understand and cope with their problems and symptoms, which in turn affects their self-perception and the interaction with their social environment. In the following, this shall be exemplified on three psychotherapeutic approaches. We decided to focus on three prominent psychotherapeutic approaches, with no claim to be complete in terms of therapeutic theories and methods. The following arguments guided our decision: first, the chosen psychotherapy approaches differ substantially in their underlying treatment theory; second, we decided to not focus on the link between psychodynamic psychotherapy with the “narrative feature of psychotherapy ‘which may be’ its main therapeutic engine” (cited from Blease, 2015 , p. 178) since this has been discussed elsewhere ( Jopling, 2011 ; Blease, 2015 ); third, popular third wave approaches (e.g., dialectical behavior therapy or acceptance and commitment therapy) conceptualize cognitions and cognitive thought processes as a way of “private behavior” ( Hayes et al., 2006 ), focusing primarily on the function of cognitions ( Churchill et al., 2010 ). We assume that the reflections on cognitive therapies will exhibit at least some comparable inferences.
Cognitive Therapies
The cognitive approach is based on the assumptions that the cognitive representation of clients’ experiences influences how they respond, act, and feel and that humans have the potential to metacognitize, thus to observe and change their thoughts and beliefs through reflection and practice, resulting in a different perception of one’s symptoms, self, and social environment ( Beck, 1996 ). The process of transformation through metacognition is embedded in a caring, collaborative, and respectful therapeutic relationship ( Alford et al., 1998 ; DeRubeis et al., 2001 ; Dobson and Dozois, 2001 ; Beck, 2005 ) and therapists should be competent not only in technical but also in interpersonal skills ( Beck and Padesky, 1989 ; Gaston et al., 1998 ).
The cognitive approach was initially formulated as a treatment for depression; later, it became very popular as an approach for treating a multitude of other mental disorders including anxiety disorders and posttraumatic stress disorders. However, even from its early days, reception to cognitive therapy included the criticisms that the approach faced “formidable conceptual, methodological, and empirical difficulties” ( Coyne and Gotlib, 1983 ) and that “it has the force of a good story, and does not ask us to believe in any cognitive mechanism beyond those that have been familiar to playwrights and novelists for centuries.” ( Lang, 1988 ).
Interestingly, the conceptualization of clients’ cognitions soon developed from being a merely covert behavior or the result of erroneous information-processing to the notion that clients are constructors of their own representation of the world and that the reality is “a product of personal meanings that individuals create” ( Meichenbaum, 1993 ). As such the cognitive therapist “helps clients to construct narratives that fit their particular present circumstances, that are coherent, and that are adequate in capturing, and explaining their difficulties” ( Meichenbaum, 1993 ). Besides this kind of meaning, where the cognitive therapist and the client create meaningful narratives, there is also another kind: the meaningfulness or plausibility of the therapy itself. In an earlier publication, Don Meichenbaum—a major proponent of cognitive therapies—also addressed the supremacy of plausibility over validity stating that “although the theory (i.e., Schachter’s model of emotional arousal) and research upon which it is based have been criticized (…), the theory has an aura of plausibility that the clients tend to accept. The logic of the treatment plan is clear to clients in light of this conceptualization” ( Wampold and Imel, 2015 ).
Addressing the lack of differences in efficacy between cognitive and clearly non-cognitive treatments for panic disorder and the lack of a clear confirmation of the validity of underlying cognitive theories, Roth (2010) noted that “there is little doubt that therapists have been able to greatly help clients in spite of giving rationales that have turned out to be questionable or demonstrably false” ( Roth, 2010 ). In the same vein, it is interesting to note that although the hyperventilation theory (i.e., clients are instructed to counteract hyperventilation by breathing slowly and abdominally, which is expected to increase Pco₂) has been falsified as well as the suffocation false alarm theory (i.e., clients are thought to lower their Pco₂) is difficult to falsify ( Roth et al., 2005 ), treatments on the basis of these—interestingly opposing!—theories have been shown to be equally effective in the treatment of panic disorder ( Kim et al., 2012 ). As a solution of the ethical conundrum to provide effective therapies despite them being false or questionable, Roth (2010) referred to Williams James’ pragmatic approach ( James, 1896 ) and to “simply teach clients a practice that has prevented attacks in others (such as breathing control) but without its pseudoscientific rationale, asking clients to test whether that practice helps them as individuals.”
Systemic Therapy
Systemic therapy is based on the assumption that a system is constructed by shared representations of realities, building a consensus on how to interpret the internal and external environment ( Reiss and Olivieri, 1980 ) and that this collective perception is largely determined by the emotional experiences of the members of the given system. The pattern of meaning within a system is mediated by its use of language and its narrative tradition. Behaviors, symptoms, and expression of emotions are thus not considered as objective and independent entities, but rather as functional to the mutual relationships within a system and as constructed through the actions and communications of and between its members. Therefore, systemic therapy intends to change the shared patterns of meaning and definitions of realities in the context of the particular system, i.e., therapists aim to understand and accept the individual pattern of meaning as much as the systems’ narrative about their reality. Neutrality and unconditional therapeutic curiosity ( Cecchin, 1987 ), i.e., the therapist does not side or support individual members of a given system, are thought to encourage all involved members of a system to share ideas and problem perceptions, while subjective truths are appreciated in the same way. This attitude of neutrality is contrary to the idea that a system could be understood entirely, i.e., that “truth” exists, and thus attempts to explore the systems’ narratives ( Selvini et al., 1980 ).
The meaning-changing nature of systemic therapy shall be exemplified on the basis of a commonly used method in systematic therapy, the “genogram”, which consists of a structural diagram of a family’s generational relationship system using specific symbols for illustration ( Guerin and Pendagast, 1976 ). The “genogram” aims to unravel idiosyncratic perceptions, trigger the unfolding of shared narratives with a given system, and capture the communicative meaning of behavior, symptoms, or expression of emotions ( McGoldrick and Gerson, 1985 ). When relationship patterns become apparent and members of a given system are challenged to perceive reality by another perspective, this can result in new illness narratives and eventually new meanings ( Satir et al., 1991 ). Another approach in systemic therapy to change meaning is to reframe communication without changing its content ( Watzlawick et al., 2011 ). For example, the otherwise negatively and non-adaptive connoted behavior of acting-out is reframed as functional to make yourself heard in the context of a demanding and bullying school environment, thus transforming a formerly non-adaptive meaning of symptom into a new and more adaptive justification. Also, systemic therapy makes use of externalizing, i.e., to differentiate a problem and the identity of the client in order to enable a new context of meaning and to change the assumptions of what is driving and maintaining the problem ( White et al., 1990 ). According to De Shazer’ (1985) solution-focused approach, a system is viewed as having all resources that it needs for solving the problem but it is not using them currently. Thus, idiosyncratic meanings of a problem on the one hand are thought to underlie the presenting problems and on the other hand are also considered as the starting point for change: building new shared narratives involve all relevant members of the system and activate individual processes.
Person-Centered Therapy
The subjective experience of a person, i.e., the self-concept, is both the starting point as much as the therapeutic focus of the person-centered approach which is based on the principles of humanistic psychology. The person-centered approach originated in the works of Carl Rogers, who defined the necessary and sufficient condition for personality change ( Rogers, 1957 ). The self-concept is viewed as fluid and associated with changing idiosyncratic interpretations and attributions of subjective meanings. The driving force behind any change is the self-actualizing tendency for development, enhancement, and growth ( Rogers and Carmichael, 1951 ). Accordingly, a discrepancy between self-concept and the actual experience leads to incongruence, i.e., a state of tension and internal confusion, resembling Frank’s term demoralization ( Frank, 1986 ). This incongruence can either be the starting point for personality change and development or—in case of too large a discrepancy—be distorted, i.e., denied, biased, and not fully represented in experience.
The aim of person-centered therapy is congruence, i.e., to enable the clients to understand their own experiences and to be able to integrate them with their self-concept ( Rogers and Carmichael, 1951 ). A meaning transformation is understood as the clients revising their self-concept in a way to allow congruence with their experience ( Rogers, 1957 ). In this therapeutic process, the therapist is central and thus acknowledges the subjective experience of the client as much as specific techniques are only advocated when they “become a channel for communicating the essential conditions” (i.e., empathy, congruence and unconditional positive regard) (cited from Rogers, 1957 , p. 247). Thus, in person-centered therapy, the therapist and client construct a shared narrative as the therapist empathically understands the client’s inner representation of its experience and to carefully offer meanings to the client’s experience of which the client is scarcely aware ( Rogers, 1957 ).
Based on the contextual understanding of psychotherapy, we set out to examine the role and construction of meaning as a means to induce change in general and in three different psychotherapy approaches. The described psychotherapeutic approaches differ in their etiological assumptions and their therapeutic implications, but clearly all share the aim to promote a meaningful transformation in order to generate convincing narratives that “persuasively influence clients to accept more adaptive explanations for their disorders and take ameliorative actions” ( Wampold, 2007 ).
However, the exemplified approaches differ with regard to the extent this is communicated in both the treatment rationale and to the clients. Therefore, different kinds of psychotherapy can be distinguished by the way in which they explicitly engage and lead to transform clients’ meaning in more adaptive ways. Considering the importance of the transformation of meaning through narratives in psychotherapy and the varying degree this is openly defined as a characteristic constituent of the given approach and communicated to clients, we believe that psychotherapy would benefit from acknowledging this within education and training, and (arguably) in communicating this to clients.
The described therapeutic schools are all placed in an interpersonal context marked by empathy, warmth, cooperation, and transparency ( Langhoff et al., 2008 ). However, different emphases of the therapist’s and client’s roles are apparent. In cognitive therapies, the therapists assist their clients in constructing narratives that fit their perception of the world and their particular present challenges ( Meichenbaum, 1993 ). In systemic therapy, therapists aim to understand and accept how each member of a system understands reality and which unique narratives describe the current problem ( Selvini et al., 1980 ), while person-centered therapists promote a shared and empathetic understanding of clients’ narratives ( Rogers, 1957 ).
The current conceptual analysis has the limitation to focus only on a selective choice of therapeutic approaches, with no claim to be complete regarding therapeutic theories, rationales, techniques, and strategies ( Blease, 2015 ). However, the chosen psychotherapy approaches are illustrative as they differ significantly in focus, underlying treatment theory and paradigmatic orientation.
To conclude, the meaning and their underlying narratives matter—regardless of the specific psychotherapy approach. However, this importance is not equally well acknowledged by the examined approaches or to rephrase this observation in the terms of Grünbaum’s ( Grünbaum, 1981 ; Howick, 2017 ) definition of intervention constituents and with regard to Rosenzweig’s (1936) early and seminar observation: The characteristic factors that actually are operating in several different therapies—the transformation of meaning—may not have much more in common than have the factors alleged to be operating. The ethical obligation at hand is to make these characteristic elements of psychotherapy, which promote the change from non-adaptive into adaptive explanations, allowing the client to feel better, function more favorably, and think more adaptively, transparent in both, therapeutic manuals and the informed consent of clients ( Blease et al., 2016 ; Gaab et al., 2016 ; Trachsel and Gaab, 2016 ).
Author Contributions
CL, SM, and JG conceived and designed the conceptual analysis. CL drafted the paper. CL, SM, and JG wrote the final paper, critically revised the manuscript and gave important intellectual contribution to it.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to thank Deborah Meier, Cora Wagner, Sarah Bürgler, and Linda Kost for their assistance with editing the manuscript. Further, we would like to thank Süheyla Seker for her conceptual contribution.
Funding. CL, PhD, received funding from the Swiss National Science Foundation (SNSF): P400PS_180730.
- Addis M. E., Jacobson N. S. (2000). A closer look at the treatment rationale and homework compliance in cognitive-behavioral therapy for depression . Cognit. Ther. Res. 24 , 313–326. 10.1023/A:1005563304265 [ CrossRef ] [ Google Scholar ]
- Alford B. A., Beck A. T., Jones J. V., Jr. (1998). The integrative power of cognitive therapy. New York: Guilford Press. [ Google Scholar ]
- Barrett B., Muller D., Rakel D., Rabago D., Marchand L., Scheder J. (2006). Placebo, meaning, and health . Perspect. Biol. Med. 49 , 178–198. 10.1353/pbm.2006.0019, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barth J., Munder T., Gerger H., Nuesch E., Trelle S., Znoj H., et al.. (2013). Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis . PLoS Med. 10 :e1001454. 10.1371/journal.pmed.1001454, PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beck A. T. (1996). “ Beyond belief: a theory of modes, personality, and psychopathology ” in Frontiers of cognitive therapy. ed. Salkovskis P. M. (New York: Guilford Press; ), 1–25. [ Google Scholar ]
- Beck A. T. (2005). The current state of cognitive therapy: a 40-year retrospective . Arch. Gen. Psychiatry 62 , 953–959. 10.1001/archpsyc.62.9.953, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beck A. T., Padesky C. A. (1989). Love is never enough. London: Penguin. [ Google Scholar ]
- Besley A. C. T. (2002). Foucault and the turn to narrative therapy . Br. J. Guid. Counc. 30 , 125–143. 10.1080/03069880220128010 [ CrossRef ] [ Google Scholar ]
- Blease C. R. (2015). “ Informed consent, the placebo effect and psychodynamic psychotherapy ” in New perspectives on paternalism and health care. ed. Schramme T. (Switzerland: Springer International Publishing; ), 163–181. [ Google Scholar ]
- Blease C. R., Lilienfeld S. O., Kelley J. M. (2016). Evidence-based practice and psychological treatments: the imperatives of informed consent . Front. Psychol. 7 :1170. 10.3389/fpsyg.2016.01170 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blease C. R., Trachsel M., Holtforth M. G. (2016). Paternalism and placebos: the challenge of ethical disclosure in psychotherapy . Verhaltenstherapie 26 , 22–30. 10.1159/000442928 [ CrossRef ] [ Google Scholar ]
- Broadbent E., Petrie K. J., Ellis C. J., Ying J., Gamble G. (2004). A picture of health - myocardial infarction patients’ drawings of their hearts and subsequent disability- a longitudinal study . J. Psychosom. Res. 57 , 583–587. 10.1016/j.jpsychores.2004.03.014, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brody H. (1994). “My story is broken, can you help me fix it?”: medical ethics and the joint construction of narrative . Lit. Med. 13 , 79–92. 10.1353/lm.2011.0169, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brody H. (2000). The placebo response - recent research and implications for family medicine . J. Fam. Pract. 49 , 649–654. PMID: . [ PubMed ] [ Google Scholar ]
- Bruner J. (1990). Acts of meaning. Cambridge: Harvard University Press. [ Google Scholar ]
- Bruner J. (2004). Life as narrative . Soc. Res. 71 , 691–710. [ Google Scholar ]
- Carr A. (1998). Michael White’s narrative therapy . Contemp. Fam. Ther. 20 , 485–503. 10.1023/A:1021680116584 [ CrossRef ] [ Google Scholar ]
- Cecchin G. (1987). Hypothesizing, circularity, and neutrality revisited - an invitation to curiosity . Fam. Process 26 , 405–413. 10.1111/j.1545-5300.1987.00405.x, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Churchill R., Moore T. H., Davies P., Caldwell D., Jones H., Lewis G., et al. (2010). Mindfulness-based ‘third wave’ cognitive and behavioural therapies versus treatment as usual for depression . The Cochrane Database of Systematic Reviews. 9 :CD008705. 10.1002/14651858.CD008705 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coyne J. C., Gotlib I. H. (1983). The role of cognition in depression - a critical appraisal . Psychol. Bull. 94 , 472–505. 10.1037/0033-2909.94.3.472, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cuijpers P., van Straten A., Andersson G., van Oppen P. (2008). Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies . J. Consult. Clin. Psychol. 76 , 909–922. 10.1037/a0013075, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Shazer S. (1985). Keys to solution in brief therapy. New York: Ww Norton. [ Google Scholar ]
- DeRubeis R. J., Tang T. Z., Beck A. T. (2001). Cognitive therapy. New York: Guilford Press. [ Google Scholar ]
- Dobson K., Dozois D. J. (2001). Historical and philosophical bases of the cognitive behavioral therapies. New York: Guilford Press. [ Google Scholar ]
- Egnew T. R. (2005). The meaning of healing: transcending suffering . Ann. Fam. Med. 3 , 255–262. 10.1370/afm.313, PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Engel G. L. (1977). The need for a new medical model: a challenge for biomedicine . Science 196 , 129–136. 10.1126/science.847460, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans I. M. (2013). How and why people change: Foundations of psychological therapy. New York: Oxford University Press. [ Google Scholar ]
- Flückiger C., Del Re A. C., Wampold B. E., Symonds D., Horvath A. O. (2012). How central is the alliance in psychotherapy? A multilevel longitudinal meta-analysis . J. Couns. Psychol. 59 , 10–17. 10.1037/a0025749, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frank J. D. (1986). Psychotherapy - the transformation of meanings: discussion paper . J. R. Soc. Med. 79 , 341–346. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Freda M. F., Martino M. L. (2015). Health and writing: meaning-making processes in the narratives of parents of children with leukemia . Qual. Health Res. 25 , 348–359. 10.1177/1049732314551059 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frenkel O. (2008). A phenomenology of the ‘placebo effect’: taking meaning from the mind to the body . J. Med. Philos. 33 , 58–79. 10.1093/jmp/jhm005, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frost N. D., Laska K. M., Wampold B. E. (2014). The evidence for present-centered therapy as a treatment for posttraumatic stress disorder . J. Trauma. Stress 27 , 1–8. 10.1002/jts.21881, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gaab J., Blease C., Locher C., Gerger H. (2016). Go open: a plea for transparency in psychotherapy . Psychol. Conscious 3 , 175–198. 10.1037/cns0000063 [ CrossRef ] [ Google Scholar ]
- Galli U., Ettlin D. A., Palla S., Ehlert U., Gaab J. (2010). Do illness perceptions predict pain-related disability and mood in chronic orofacial pain patients? A 6-month follow-up study . Eur. J. Pain 14 , 550–558. 10.1016/j.ejpain.2009.08.011, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gaston L., Thompson L., Gallagher D., Cournoyer L. G., Gagnon R. (1998). Alliance, technique, and their interactions in predicting outcome of behavioral, cognitive, and brief dynamic therapy . Psychother. Res. 8 , 190–209. [ Google Scholar ]
- Goldfried M. R. (2013). What should we expect from psychotherapy? Clin. Psychol. Rev. 33 , 862–869. 10.1016/j.cpr.2013.05.003, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grünbaum A. (1981). The placebo concept . Behav. Res. Ther. 19 , 157–167. 10.1016/0005-7967(81)90040-1, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guerin P. J., Pendagast E. G. (1976). “ Evaluation of family system and genogram ” in Family therapy: Theory and practice. ed. Guerin P. J. (New York: Gardner; ), 450–464. [ Google Scholar ]
- Gysin-Maillart A., Schwab S., Soravia L., Megert M., Michel K. (2016). A movel brief therapy for patients who attempt suicide: a 24-months follow-up randomized controlled study of the attempted suicide short intervention program (ASSIP) . PLoS Med. 13 :e1001968. 10.1371/journal.pmed.1001968, PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hayes S. C., Luoma J. B., Bond F. W., Masuda A., Lillis J. (2006). Acceptance and commitment therapy: Model, processes and outcomes . Behav. Res. Ther. 44 , 1–25. 10.1016/j.brat.2005.06.006, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Horne R., Cooper V., Gellaitry G., Date H. L., Fisher M. (2007). Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence - the utility of the necessity-concerns framework . J. Acquir. Immune Defic. Syndr. 45 , 334–341. 10.1097/QAI.0b013e31806910e3, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Howick J. (2017). The relativity of ‘placebos’: defending a modified version of Grünbaum’s definition . Synthese 194 , 1363–1396. 10.1007/s11229-015-1001-0 [ CrossRef ] [ Google Scholar ]
- James W. (1896). The will to believe: And other essays in popular philosophy. New York and London: Longmans, Green, and Co. [ Google Scholar ]
- Jopling D. A. (2011). “Much ado to know myself … ”: Insight in the talking cures . Ann. N. Y. Acad. Sci. 1234 , 158–167. 10.1111/j.1749-6632.2011.06189.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Justman S. (2011). The power of rhetoric: two healing movements . Yale J. Biol. Med. 84 , 15–25., PMID: [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kendler K. S., Myers J., Halberstadt L. J. (2011). Do reasons for major depression act as causes? Mol. Psychiatry 16 , 626–633. 10.1038/mp.2011.22, PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kim S. Y., Wollburg E., Roth W. T. (2012). Opposing breathing therapies for panic disorder: a randomized controlled trial of lowering vs raising end-tidal Pco₂ . J. Clin. Psychiatry 73 , 931–939. 10.4088/JCP.11m07068, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirsch I., Wampold B., Kelley J. M. (2016). Controlling for the placebo effect in psychotherapy: noble quest or tilting at windmills? Psychol. Conscious. 3 , 121–131. 10.1037/cns0000065 [ CrossRef ] [ Google Scholar ]
- Kleinman A. (1988). The illness narratives: Suffering, healing, and the human condition. New York: Basic books. [ PubMed ] [ Google Scholar ]
- Krause M., Altimir C., Pérez J. C., De la Parra G. (2015). Generic change indicators in therapeutic processes with different outcomes . Psychother. Res. 25 , 533–545. 10.1080/10503307.2014.935516 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kropf N. P., Tandy C. (1998). Narrative therapy with older clients: the use of a “meaning-making” approach . Clin. Gerontol. 18 , 3–16. [ Google Scholar ]
- Lang P. J. (1988). Fear, anxiety, and panic: Context, cognition, and visceral arousal. Hillsdale: Lawrence Erlbaum Associates, Inc. [ Google Scholar ]
- Langhoff C., Baer T., Zubraegel D., Linden M. (2008). Therapist–patient alliance, patient–therapist alliance, mutual therapeutic alliance, therapist–patient concordance, and outcome of CBT in GAD . J. Cogn. Psychother. 22 , 68–79. 10.1891/0889.8391.22.1.68 [ CrossRef ] [ Google Scholar ]
- Levitt H. M., Pomerville A., Surace F. I. (2016). A qualitative meta-analysis examining clients’ experiences of psychotherapy: a new agenda . Psychol. Bull. 142 , 801–830. 10.1037/bul0000057, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Luborsky L., Rosenthal R., Diguer L., Andrusyna T. P., Berman J. S., Levitt J. T., et al. (2002). The dodo bird verdict is alive and well—mostly . Clin. Psychol. Sci. Pract. 9 , 2–12. 10.1093/clipsy/9.1.2 [ CrossRef ] [ Google Scholar ]
- Lysaker P. H., Buck K. D., Carcione A., Procacci M., Salvatore G., Nicolò G., et al. (2011). Addressing metacognitive capacity for self reflection in the psychotherapy for schizophrenia: a conceptual model of the key tasks and processes . Psychol. Psychother. Theory Res. Pract. 84 , 58–69. 10.1348/147608310X520436 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Marcus D. K., O’Connell D., Norris A. L., Sawaqdeh A. (2014). Is the Dodo bird endangered in the 21st century? A meta-analysis of treatment comparison studies . Clin. Psychol. Rev. 34 , 519–530. 10.1016/j.cpr.2014.08.001, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mattingly C. (1994). The concept of therapeutic emplotment . Soc. Sci. Med. 38 , 811–822. 10.1016/0277-9536(94)90153-8, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mauksch L. B., Dugdale D. C., Dodson S., Epstein R. (2008). Relationship, communication, and efficiency in the medical encounter: creating a clinical model from a literature review . Arch. Intern. Med. 168 , 1387–1395. 10.1001/archinte.168.13.1387, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McGoldrick M., Gerson R. (1985). Genograms in family assessment. New York: Norton. [ Google Scholar ]
- Meichenbaum D. (1993). Changing conceptions of cognitive behavior-modification - retrospect and prospect . J. Consult. Clin. Psychol. 61 , 202–204. 10.1037/0022-006X.61.2.202, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Metcalf A. (2005). Truthiness voted 2005 word of the year by American dialect society . Am. Dialect Soc. 2005 , 1–7. [ Google Scholar ]
- Moerman D. E. (2002). Meaning, medicine, and the “placebo effect”. Cambridge: University Press Cambridge. [ Google Scholar ]
- Moerman D. E. (2006). The meaning response: thinking about placebos . Pain Pract. 6 , 233–236. 10.1111/j.1533-2500.2006.00091.x, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Northoff G., Boeker H. (2006). Principles of neuronal integration and defense mechanisms: neuropsychoanalytic hypothesis . Neuropsychoanalysis 8 , 69–84. 10.1080/15294145.2006.10773514 [ CrossRef ] [ Google Scholar ]
- Ochs E., Capps L. (1996). Narrating the self . Annu. Rev. Anthropol. 25 , 19–43. 10.1146/annurev.anthro.25.1.19 [ CrossRef ] [ Google Scholar ]
- Overholser J. C., Braden A., Fisher L. (2010). You’ve got to believe: core beliefs that underlie effective psychotherapy . J. Contemp. Psychother. 40 , 185–194. 10.1007/s10879-010-9151-3 [ CrossRef ] [ Google Scholar ]
- Panksepp J., Solms M. (2012). What is neuropsychoanalysis? Clinically relevant studies of the minded brain . Trends Cogn. Sci. 16 , 6–8. 10.1016/j.tics.2011.11.005, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Park J., Ayduk O., Kross E. (2016). Stepping back to move forward: expressive writing promotes self-distancing . Emotion 16 , 349–364. 10.1037/emo0000121, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pennebaker J. W., Seagal J. D. (1999). Forming a story: the health benefits of narrative . J. Clin. Psychol. 55 , 1243–1254. 10.1002/(SICI)1097-4679(199910)55:10<1243::AID-JCLP6>3.0.CO;2-N, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prince M., Patel V., Saxena S., Maj M., Maselko J., Phillips M. R., et al.. (2007). No health without mental health . Lancet 370 , 859–877. 10.1016/S0140-6736(07)61238-0, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reiss D., Olivieri M. (1980). Family paradigm and family coping: a proposal for linking the family’s intrinsic adaptive capacities to its responses to stress . Fam. Relat. 29 , 431–444. 10.2307/584456 [ CrossRef ] [ Google Scholar ]
- Ricoeur P. (1991). Narrative identity . Philos. Today 35 , 73–81. 10.5840/philtoday199135136 [ CrossRef ] [ Google Scholar ]
- Rogers C. R. (1957). The necessary and sufficient conditions of therapeutic personality-change . J. Consult. Psychol. 21 , 95–103. 10.1037/h0045357, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rogers C. R., Carmichael L. (1951). Client-centered therapy: Its current practice, implications, and theory. London: Constable and Co. [ Google Scholar ]
- Rosenzweig S. (1936). Some implicit common factors in diverse methods of psychotherapy . Am. J. Orthopsychiatry 6 , 412–415. 10.1111/j.1939-0025.1936.tb05248.x [ CrossRef ] [ Google Scholar ]
- Roth W. T. (2010). Diversity of effective treatments of panic attacks: what do they have in common? Depress. Anxiety 27 , 5–11. 10.1002/da.20601, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roth W. T., Wilhelm F. H., Pettit D. (2005). Are current theories of panic falsifiable? Psychol. Bull. 131 , 171–192. 10.1037/0033-2909.131.2.171, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Satir V., Banmen J., Gerber J., Gomori M. (1991). The satir model: Family therapy and beyond. Palo Alto: Science and Behavior Books. [ Google Scholar ]
- Selvini M. P., Boscolo L., Cecchin G., Prata G. (1980). Hypothesizing—circularity—neutrality: three guidelines for the conductor of the session . Fam. Process 19 , 3–12. 10.1111/j.1545-5300.1980.00003.x, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shaw J. (2010). A review of “Maps of Narrative Practice” by Michael White . J. Sex Marital Ther. 36 , 385–387. 10.1080/0092623X.2010.491354 [ CrossRef ] [ Google Scholar ]
- Spielmans G. I., Pasek L. F., McFall J. P. (2007). What are the active ingredients in cognitive and behavioral psychotherapy for anxious and depressed children? A meta-analytic review . Clin. Psychol. Rev. 27 , 642–654. 10.1016/j.cpr.2006.06.001, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strong S. R., Matross R. P. (1973). Change processes in counseling and psychotherapy . J. Couns. Psychol. 20 , 25–37. 10.1037/h0034055 [ CrossRef ] [ Google Scholar ]
- Strupp H. H. (1986). The nonspecific hypothesis of therapeutic effectiveness - a current assessment . Am. J. Orthopsychiatry 56 , 513–520. 10.1111/j.1939-0025.1986.tb03484.x, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tondorf T., Kaufmann L. K., Degel A., Locher C., Birkhauer J., Gerger H., et al.. (2017). Employing open/hidden administration in psychotherapy research: a randomized-controlled trial of expressive writing . PLoS One 12 :e0187400. 10.1371/journal.pone.0187400, PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Trachsel M., Gaab J. (2016). Disclosure of incidental constituents of psychotherapy as a moral obligation for psychiatrists and psychotherapists . J. Med. Ethics 42 , 493–495. 10.1136/medethics-2015-102986, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vissers W., Hutschemaekers G., Keijsers G., Van der Veld W., Hendriks G. J. (2010). Utility of measuring remoralization in addition to symptoms in efficacy research: a preliminary study . Psychother. Res. 20 , 611–618. 10.1080/10503307.2010.496469, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wallis J., Burns J., Capdevila R. (2011). What is narrative therapy and what is it not? The usefulness of Q methodology to explore accounts of White and Epston’s (1990) approach to narrative therapy . Clin. Psychol. Psychother. 18 , 486–497. 10.1002/cpp.723, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wampold B. E. (2007). Psychotherapy: the humanistic (and effective) treatment . Am. Psychol. 62 , 857–873. 10.1037/0003-066X.62.8.857, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wampold B. E., Budge S. L., Laska K. M., Del Re A. C., Baardseth T. P., Fluckiger C., et al.. (2011). Evidence-based treatments for depression and anxiety versus treatment-as-usual: a meta-analysis of direct comparisons . Clin. Psychol. Rev. 31 , 1304–1312. 10.1016/j.cpr.2011.07.012, PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wampold B. E., Imel Z. E. (2015). Great psychotherapy debate: The evidence for what makes psychotherapy work. 2nd edn. New York: Routledge. [ Google Scholar ]
- Watzlawick P., Weakland J. H., Fisch R. (2011). Change: Principles of problem formation and problem resolution. New York: WW Norton & Company. [ Google Scholar ]
- White M., White M. K., Wijaya M., Epston D. (1990). Narrative means to therapeutic ends. New York: WW Norton & Company. [ Google Scholar ]

- About Northwestern
- Student Stories
- Application Requirements
- How to Apply
- Standard Program
- Course Descriptions
- Bridge to Counseling Program
- Continuing Education
- Child and Adolescent Specialization
- Clinical Training and Placement
- In-Person Immersion Experiences
- What Is Counseling?
- Counseling versus Psychology
- The Differences between Clinical Mental Health Counseling and Social Work
- Careers in Mental Health Counseling
- Leadership & Faculty
- Program Data
Five Counseling Theories and Approaches
- Inclusive Language Guide
- Holiday Survival Guide Toolkit
- Building and Maintaining Wellness
- Apply External link: open_in_new
Counseling@Northwestern / Blog
June 1, 2015
Psychotherapy theories provide a framework for therapists and counselors to interpret a client’s behavior, thoughts, and feelings and help them navigate a client’s journey from diagnosis to post-treatment. Theoretical approaches are an understandably integral part of the therapeutic process. But with so many different methods out there, how do you know which counseling approach works best for you? Whether you’re a student learning about counseling theories or a client looking for the right therapist, the following detailed descriptions will give you a deeper understanding of each counseling method. These theories are integrated throughout the curriculum of Counseling@Northwestern and are built into a foundation grounded in the psychodynamic perspective.
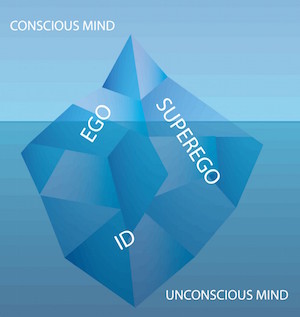
Psychoanalysis/Psychodynamic Theory
Psychoanalysis or psychodynamic theory, also known as the “historical perspective,” has its roots with Sigmund Freud, who believed there were unconscious forces that drive behavior. The techniques he developed, such as free association (freely talking to the therapist about whatever comes up without censoring), dream analysis (examining dreams for important information about the unconscious), and transference (redirecting feelings about certain people in one’s life onto the therapist) are still used by psychoanalysts today.
Counseling@Northwestern uses this theory to train counselors, and it is embedded throughout the counselor training process. In general, psychotherapists and counselors who use this approach direct much of their focus and energy on analyzing past relationships and, in particular, traumatic childhood experiences in relation to an individual’s current life. The belief is that by revealing and bringing these issues to the surface, treatment and healing can occur. This theory is highly researched, and as the field of neuroscience advances, counselors are finding how psychodynamic theory can actually positively affect a client’s brain. Psychodynamic theory can be more time intensive in comparison to some short-term theories because it involves changing deeply ingrained behaviors and requires significant work on understanding one’s self.
Behavioral Theory
Behavioral theory is based on the belief that behavior is learned. Classic conditioning is one type of behavioral therapy that stems from early theorist Ivan Pavlov’s research. Pavlov executed a famous study using dogs, which focused on the effects of a learned response (e.g., a dog salivating when hearing a bell) through a stimulus (e.g., pairing the sound of a bell with food).
B. F. Skinner developed another behavioral therapy approach, called operant conditioning. He believed in the power of rewards to increase the likelihood of a behavior and punishments to decrease the occurrence of a behavior. Behavioral therapists work on changing unwanted and destructive behaviors through behavior modification techniques such as positive or negative reinforcement.
Cognitive Theory
In the 1960s, psychotherapist Aaron Beck developed cognitive theory . This counseling theory focuses on how people’s thinking can change feelings and behaviors. Unlike psychodynamic theory, therapy based on cognitive theory is brief in nature and oriented toward problem solving. Cognitive therapists focus more on their client’s present situation and distorted thinking than on their past. Cognitive and behavioral therapy are often combined as one form of theory practiced by counselors and therapists. Cognitive behavioral therapy, or CBT, has been found in research to help with a number of mental illnesses including anxiety, personality, eating, and substance abuse disorders.
Humanistic Approach
Humanistic therapists care most about the present and helping their clients achieve their highest potential. Instead of energy spent on the past or on negative behaviors, humanists believe in the goodness of all people and emphasize a person’s self-growth and self-actualization.
Humanistic theories include client-centered, gestalt, and existential therapies. Carl Rogers developed client-centered therapy, which focuses on the belief that clients control their own destinies. He believed that all therapists need to do is show their genuine care and interest. Gestalt therapists’ work focuses more on what’s going on in the moment versus what is being said in therapy. Existential therapists help clients find meaning in their lives by focusing on free will, self-determination, and responsibility.
Holistic/Integrative Therapy
Holistic and integrative therapy involves integrating various elements of different theories to the practice. In addition to traditional talk therapy, holistic therapy may include nontraditional therapies such as hypnotherapy or guided imagery. The key is to use the techniques and psychotherapy tools best suited for a particular client and problem.
There are various therapies that counselors can choose to study, but the type of theory matters less than the success of the relationship between client and therapist. In the Counseling@Northwestern online Master of Arts in Counseling Program, students are prepared to become self-reflective practitioners and learn to examine the factors that influence the client-therapist relationship to become successful counselors.
Request More Information
Complete the form to receive information about the online graduate counseling and therapy programs offered by the Family Institute at Northwestern University.
Logotherapy: Viktor Frankl’s Theory of Meaning

When we bask in the glory of a sunset and reflect on creation or enjoy the embrace of a loved one, it provides meaning.
As we engage with our community, participate in creative endeavors, and support a cause greater than ourselves, we experience the value of life.
What is it then that brings meaning to life? What is it that makes those hard moments, the dark nights, and endless struggles worth the fight?
The quest to answer “what is the meaning of life?” has been around since the beginning of time. To find meaning in life can be seen as the primary motivation of each person, and the concept of logotherapy is based on that proposition.
In the following article, we will take a deep dive into the creation of logotherapy, research, techniques, and worksheets.
Before you read on, we thought you might like to download our three Meaning & Valued Living Exercises for free . These creative, science-based exercises will help you learn more about your values, motivations, and goals and will give you the tools to inspire a sense of meaning in the lives of your clients, students, or employees.
This Article Contains:
Logotherapy: a definition, who was viktor frankl, viktor frankl’s theory, research and empirical results, 3 techniques of logotherapy, 4 activities and worksheets, 6 famous quotes on life and meaning, 5 books on the topic, our meaning & valued living masterclass, a take-home message.
Logotherapy is often referred to as the “ third Viennese school of psychotherapy ,” and it originated in the 1930s as a response to both Freud’s psychoanalysis and Adler’s emphasis on power within society. It is more than just “therapy.” It is a philosophy for the spiritually lost and an education for those who are confused. It offers support in the face of suffering and healing for the sick (Guttmann, 2008).
Logotherapy examines the physical, psychological, and spiritual (noological) aspects of a human being, and it can be seen through the expression of an individual’s functioning. It is often regarded as a humanistic–existential school of thought but can also be used in conjunction with contemporary therapies (McMullin, 2000).
In contrast to Freud’s “ will to pleasure ” and Adler’s “ will to power ,” logotherapy is based on the idea that we are driven by a “ will to meaning ” or an inner desire to find purpose and meaning in life (Amelis & Dattilio, 2013).
As humans, we often respond to situations in the first two dimensions of functioning (physical/psychological) with conditioned and automatic reactions. Examples of these reactions include negative self-talk, irrational actions, outbursts, and negative emotions.
Animals also respond in the first two dimensions. It is the third dimension of functioning that separates humans from other species. This is the unique beauty of logotherapy.
While humans can survive just like animals living within the first two dimensions (satisfying physical needs and thinking), logotherapy offers a deeper connection to the soul and an opportunity to explore that which makes us uniquely human.
The spiritual dimension is one of meaning. The basic tenets of logotherapy are that
- human life has meaning,
- human beings long to experience their own sense of life meaning, and
- humans have the potential to experience meaning under any and every circumstance (Schulenberg, 2003).
The Austrian psychiatrist and neurologist was born March 26, 1905, and is best known for his psychological memoir Man’s Search for Meaning (2006) and as the father of logotherapy.
He published 40 books that have been translated into 50 languages, demonstrating that love, freedom, meaning, and responsibility transcend race, culture, religion, and continents.
His most famous memoir begins by outlining a personal experience through the gruesome Auschwitz concentration camps. The three years he spent in concentration camps became more than a story of survival. Frankl embodies the modern-day definition of resilience.
Download 3 Meaning & Valued Living Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to find meaning in life help and pursue directions that are in alignment with values.
Download 3 Free Meaning Tools Pack (PDF)
By filling out your name and email address below.
Frankl viewed logotherapy as a way to enhance existing therapies by emphasizing the “meaning-dimension” or spiritual dimension of human beings. Three philosophical and psychological concepts make up Frankl’s logotherapy: freedom of will, will to meaning, and meaning of life (Batthyany, 2019).
Freedom of will asserts that humans are free to decide and can take a stance toward both internal and external conditions. Freedom in this context is defined as a space to shape one’s own life within limits of specific possibilities. It provides the client with room for autonomy in the face of somatic or psychological illness. In essence, we are free to choose our responses no matter our circumstances.
Will to meaning states that humans are free to achieve goals and purposes in life. Frustration, aggression, addiction, depression, and suicidality arise when individuals cannot realize their “will to meaning.” As humans, our primary motive is to search for meaning or purpose in our lives. We are capable of surpassing pleasure and supporting pain for a meaningful cause.
Meaning in life is based on the idea that meaning is an objective reality rather than merely an illusion or personal perception. Humans have both freedom and responsibility to bring forth their best possible selves by realizing the meaning of the moment in every situation.
Can we find meaning under all circumstances, even unavoidable suffering? We can discover meaning in life through creative clues, experiential values, and attitudinal values (Lewis, 2011).
Viktor Frankl: Logotherapy and man’s search for meaning
Logotherapy has significant application to every dimension of an individual (the tri-dimensional ontology). Psychologically, logotherapy uses the specific techniques of paradoxical intention and dereflection to deal with problems of anxiety, compulsive disorders, obsessions, and phobias. These will be discussed in further detail in the next section.
Physiologically, logotherapy is an effective way to cope with suffering and physical pain or loss. Spiritually, logotherapy demonstrates that life has meaning or purpose when people suffer from the “existential vacuum” that we experience as boredom, apathy, emptiness, and depression (Frankl, 2006).
1. PTSD and acute stress
One of the most effective things about logotherapy is its ability to empower individuals, allowing them to be freed from their symptoms and increase their capacity to be proactive.
Since logotherapy was founded on a preface of suffering, it is a natural therapy for treating traumatic experiences. Logotherapy is a useful treatment for individuals with acute stress disorder or post-traumatic stress disorder (PTSD).
In numerous case studies of clients with combat-related PTSD, logotherapy exercises that highlight the construct of meaning led to a significant decrease in symptoms of stress, anxiety, and depression (Schiraldi, 2000). Research on logotherapy’s effectiveness for treating PTSD has mostly been established through qualitative research and case studies.
2. Alcohol and drug treatment
There are obvious parallels between the spiritual elements of Alcoholics Anonymous and the concepts of discovering personal meaning found in logotherapy.
Frankl (2006) discussed a “mass neurotic triad” of aggression, depression, and addiction that occurs when individuals experience an existential vacuum. This vacuum leads to violations of social norms, symptoms of stress, and addiction.
The treatment for this existential vacuum is, of course, to guide the client into discovering the freedom to choose, the will to find meaning, and the responsibility of living a purposeful life (Hutzell, 1990).
Logotherapy has been effective in reducing cravings and participation in drinking among alcoholics. Additionally, logotherapy groups successfully improved the meaning of life and mental health among wives of alcoholics (Cho, 2008).
Frankl would argue that when individuals can tap into their freedom, responsibility, and life purpose, there is no longer a need or desire for mind-altering substances like alcohol or drugs.
3. Anxiety and depression
Logotherapy has successfully been used to treat depression and anxiety. One study looked specifically at depression and stress among cervical cancer patients (Soetrisno & Moewardi, 2017).
Researchers measured cortisol levels (stress hormone) and scores from the Beck Depression Inventory (BDI) among two groups of 15 patients. One group received logotherapy treatment for a total of six weeks (45-minute sessions once per week), and the control group received standard cancer treatment.
After six weeks, there was a significant decrease in BDI scores and levels of cortisol for the treatment group, while the control group had no change (Soetrisno & Moewardi, 2017). It makes sense that improving the meaning of life for cancer patients decreased their levels of stress and depression.
Logotherapy also successfully decreased measurable levels of suffering and increased the meaning of life in a group of adolescent cancer patients when compared with a matched control group (Kang et al., 2009).
Similarly, two-hour sessions of logotherapy among a group of 22 breast cancer patients significantly decreased BDI scores (Hagighi, Khodaei, and Sharifzadeh, 2012). This research demonstrated that logotherapy can be a beneficial treatment for individuals struggling through cancer or other major illnesses.
4. Group logotherapy
There is also significant research to support the use of logotherapy in group settings. Instructing both individuals and groups on the dimensions of responsibility, freedom, and values can help decrease suffering and increase various measures of psychological wellbeing.
When comparing the effectiveness of gestalt and logotherapy in a group setting of divorced women, logotherapy provided a more substantial decrease in depression, anxiety, and aggression (Yousefi, 2006).
Group logotherapy also led to increased psychological wellbeing, positive relationships, autonomy, personal growth, and mastery among mothers of children with intellectual disabilities (Faramarzi & Bavali, 2017).

There are similarities between the therapeutic techniques of logotherapy and both Cognitive Behavioral Therapy (CBT) and Acceptance and Commitment Therapy (ACT).
1. Dereflection
The first technique is dereflection, which is aimed at helping clients focus attention away from problems and complaints and toward something positive. It is based on the concept of self-distancing and self-transcendence .
Practically speaking, it involves asking questions like “ What would your life be like without X problem? ”; “ If everything went perfectly in your life, what would that look like? ”; and “ Is there anything in your life you would die for? ”
2. Paradoxical intention
Paradoxical intention is an effective technique to use with phobias, fear, and anxiety.
The basis of this technique is that humor and ridicule can be useful when fear is paralyzing. Fear is removed when action/intention focuses on what is feared the most. For example, if a person struggles with a fear of rejection, they would purposely put themselves in positions where they would be rejected or told “no.”
An apt illustration is in Harry Potter and the Prisoner of Azkaban (Rowling, 1999), where young students had to face their worst fears. To conquer their fear, they had to turn the terrifying thought into something laughable, such as a big spider on roller skates, thereby ridiculing and overcoming the paralyzing fear.
3. Socratic dialogue
Socratic dialogue is a tool in logotherapy that walks a client through a process of self-discovery in their own words.
It is different from Socratic questioning , which is often used in CBT. Socratic questioning breaks down anxious or negative thoughts, while Socratic dialogue is used to find meaning within a conversation. It allows the client to realize they already have the answers to their purpose, meaning, and freedom.
World’s Largest Positive Psychology Resource
The Positive Psychology Toolkit© is a groundbreaking practitioner resource containing over 500 science-based exercises , activities, interventions, questionnaires, and assessments created by experts using the latest positive psychology research.
Updated monthly. 100% Science-based.
“The best positive psychology resource out there!” — Emiliya Zhivotovskaya , Flourishing Center CEO
Our Positive Psychology Toolkit© contains over 400 tools, exercises and questionnaires to assist therapists, coaches and educators, to name a few. Some of these worksheets are described below.
1. Valued Living During Challenging Times
A perfect fit for Frankl’s logotherapy, the Valued Living During Challenging Times worksheet has clients reflect on a challenging circumstance and reconnect with personal values. Through this process, clients can find meaning in their suffering and become more resilient and tolerant of stress.
2. Passengers on the Bus group activity
The empirically tested metaphor “passengers on the bus” has been effectively used in ACT interventions. The Passengers on the Bus group activity uses role-play and debriefing to help clients learn to react to distressing situations in line with their values rather than choosing to avoid painful situations or act on their emotions.
3. A Value Tattoo
While logotherapy uses Socratic dialogue to find meaning, the Value Tattoo worksheet is helpful for clients who might find questions difficult or confronting. Instead of asking, “ What is most important in life? ” the client is encouraged to use creativity and imagine a tattoo that would be meaningful to them.
4. Find Your Purpose worksheet
This Find Your Purpose worksheet asks a series of basic questions designed to identify gifts, talents, skills, and abilities, which can ultimately reflect finding purpose in life. By finding your purpose and using your strengths in a positive way, you can create a lasting impact on the world around you and ultimately find meaning in life.
While finding the meaning of life seems to be at the forefront of logotherapy, Frankl argued that instead of asking this question, an individual should realize that they are the one being questioned.
He stated, “ It doesn’t really matter what we expected from life, but what life expected from us ” (Frankl, 1986).
Other notable quotes from Frankl’s Man’s Search for Meaning (2006) include:
When we are no longer able to change a situation, we are challenged to change ourselves.
Suffering is an ineradicable part of life, even as fate and death. Without suffering and death human life cannot be complete. For success, like happiness, cannot be pursued; it must ensue, and it only does so as the unintended side-effect of one’s personal dedication to a cause greater than oneself or as the by-product of one’s surrender to a person other than oneself.
Related famous quotes include:
He who has a why to live for can bear with almost any how.
- Man’s Search for Meaning (2006) is the best place to start for a brief background on Viktor Frankl and a great introduction to logotherapy. ( Amazon )
- The Will to Meaning (Frankl, 2014) dives a bit deeper into the application of logotherapy ( Amazon )
- Frankl’s The Doctor and the Soul: From Psychotherapy to Logotherapy (1986) is the first book published after his release from Nazi concentration camps. He discusses that the fundamental human drive is not sex (Freud’s view) or the need for approval (Adler’s perspective) but the drive to have a meaningful life . ( Amazon )
- In the book Viktor Frankl’s Logotherapy , author Ann Graber (2019) focuses on the practical application of logotherapy and the effectiveness of using the spiritual dimension in existential therapy to find healing. ( Amazon )
- Joseph Fabry compiles work on logotherapy in the text Finding Meaning in Life: Logotherapy (1995) , which can specifically help clients with drug, alcohol, or life adjustment issues. ( Amazon )
For more reading, visit our post listing the 7 Best Books to Help You Find the Meaning of Life .
17 Tools To Encourage Meaningful, Value-Aligned Living
This 17 Meaning & Valued Living Exercises [PDF] pack contains our best exercises for helping others discover their purpose and live more fulfilling, value-aligned lives.
Created by Experts. 100% Science-based.
The apparent parallels between positive psychology and Viktor Frankl’s logotherapy are endless.
While there are also notable differences, there is no denying that finding value and meaning in this journey of life leads to an array of positive outcomes.
The Meaning & Valued Living Masterclass provides an excellent background of positive psychology. It builds on the sailboat metaphor by emphasizing the types and paradox of meaning. By introducing practical exercises to find meaning and values, professionals can immediately apply techniques to address a wide range of issues.
One of the best things about positive psychology and the practicality of this masterclass is that it can improve life and wellbeing for those who are struggling, those who are suffering, and those who are looking to thrive.
If you’re looking for more science-based ways to help others discover meaning, this collection contains 17 validated meaning tools for practitioners. Use them to help others choose directions for their lives in alignment with what is truly important to them.
Perhaps the question, “ what is the meaning of life? ” is not the right question for us.
Asking this question is like addressing the symptom rather than the actual problem.
If we worked on finding sources of meaning within our lives through both the good and bad experiences, then we could gain relief from existential issues and increase our resilience and wellbeing.
Once we find these potential sources of meaning and align them with our personal values and strengths, that will ultimately result in the most profound sense of joy and meaning possible.
We hope you enjoyed reading this article. Don’t forget to download our three Meaning & Valued Living Exercises for free .
- Amelis, M., & Dattilio, F. M. (2013). Enhancing cognitive behavior therapy with logotherapy: Techniques for clinical practice. Psychotherapy , 50 (3), 387–391.
- Batthyany, A. (2019). What is logotherapy/existential analysis? Logotherapy and existential analysis. Viktor Frankl Institut . Retrieved from https://www.viktorfrankl.org/logotherapy.html
- Cho, S. (2008). Effects of logo-autobiography program on meaning in life and mental health in the wives of alcoholics. Journal of Asian Nursing Research , 2 (2), 129–139.
- Fabry, J. B. (1995). Finding meaning in life: Logotherapy . Jason Aronson.
- Faramarzi, S., & Bavali, F. (2017). The effectiveness of group logotherapy to improve psychological wellbeing of mothers with intellectually disabled children. International Journal of Developmental Disabilities , 63 (1), 45–51.
- Frankl, V. E. (1986). The doctor and the soul. Penguin Random House.
- Frankl, V. E. (2006). Man’s search for meaning. Beacon Press.
- Frankl, V. E. (2014). The will to meaning: Foundations and applications of logotherapy (Expanded ed.). Plume.
- Graber, A. V. (2019). Viktor Frankl’s logotherapy: Method of choice in ecumenical pastoral psychology (2nd ed.). Wyndham Hall Press.
- Guttmann, D. (2008). Finding meaning in life, at midlife and beyond: Wisdom and spirit from logotherapy. Praege Inc.
- Hagighi, F., Khodaei, S., & Sharifzadeh, G. R. (2012). Effect of logotherapy group counseling on depression in breast cancer patients. Modern Care Journal , 9 (3), 165–172.
- Hutzell, R. R. (1990). An introduction to logotherapy. In P. A. Keller & S. R. Heyman (Eds.) Innovations in clinical practice: A source book. Professional Resource Exchange.
- Kang, K. A., Im, J. I., Kim, H. S., Kim, S. J., Song, M. K., & Songyong, S. (2009). The effect of logotherapy on the suffering, finding meaning, and spiritual wellbeing of adolescents with terminal cancer. Journal of Korean Academy of Child Health Nursing , 15 (2), 136–144.
- Lewis, M. H. (2011). Defiant power: An overview of Viktor Frankl’s logotherapy and existential analysis. Retrieved June 19, 2020, from www.defiantpower.com.
- McMullin, R. E. (2000). The new handbook of cognitive therapy techniques. Norton Press.
- Rowling, J. K. (1999). Harry Potter and the Prisoner of Azkaban. Bloomsbury Publishing.
- Schulenberg, S. E. (2003). Empirical research and logotherapy. Psychological Reports , 93 , 307–319.
- Schiraldi, G. R. (2000). Post traumatic stress disorder sourcebook: A guide to healing, recovery and growth. Lowell House.
- Soetrisno, S., & Moewardi. (2017). The effect of logotherapy on the expressions of cortisol, HSP70, Beck Depression Inventory (BDI), and pain scales in advanced cervical cancer patients. Health Care for Women International , 38( 2), 91–99.
- Yousefi, N. (2006). Comparing the effectiveness of two counseling approaches of gestalt therapy and logotherapy on decrease of depression symptoms, anxiety and aggression among women divorce applicants. Cross-Country Congress of Family Pathology , 10 (3), 658–663.
Share this article:
Article feedback
What our readers think.
I am a trauma survivor, I didn’t even realize, what I was dealing with for such a long time was PTSD, Disassociation, Depression, Grief and Anxiety. I found a lot of relief when I discovered that I have the power, in how I perceive my past. I listen more than I speak, unless someone wants to hear what I have to say. During COVID-19 I was deemed an essential worker, I am an Auto Technician, before and during COVID-19 I was Shop Manager, I had never felt such extreme pressure knowing that the safety of the people I work with was in my hands. I drove to work everyday with no other car in sight, until I got to work. The atmosphere was so tense, I felt where I cut into it, as I walked from my car to the building I work in, I could not understand other managers attitudes and why I questioned mine. Like a wise Philosopher once said in a moment of chaos, normal behavior seems abnormal. I encouraged everyone everyday, letting them know, this wasn’t the first time in history this has happened, just like the Philosopher King Marcus Aurelius. Everyday I had something humors to say. I am used to pressure, being I grew up around violence and witnessed a kid get shot and killed by drive a by. This wasn’t my first Rodeo. What was going on in the moment, did not phase me. I would find justification in my own way, why things happen. I continued until my back eventually gave out from so much stress. I felt guilt that I had never felt before, I kept giving happiness and hope until I lost my own, and gave into the excruciating pain that bulging disc in my lower back produce. This was the life changing moment in my life. COVID-19 in full bloom and running rampant, I did not turn to traditional medicine. Instead I found a Phycologist and Therapist that helped me get past my own internal struggles, as I have come together with myself and countless hours of reading, exercising, meditation, yoga, and Philosophy. I have come to this website. After reading your article, and understanding my own struggles, I am a firm believer Logotherapy can help so many people.
Dr. Melissa Madeson, Thank you for your well defined points about V Frankle and logotherapy. I once led a group of seniors at a convalescent center. We discussed the meaningful moments they recalled in their lives. I encouraged the participants to write their short and focused memoirs. These writings were subsequently published in a small volume. The writers and participants took part in a public reading, with family, friends, facility staff , and public in attendance. Overall, the lectures, writing, and readings were meaningful to all involved.
Finding meaning in trauma patients’ stories help them heal. Their traumas don’t define them, they’re just facts when their stories make sense. I am a trauma therapist and I love Viktor Frankl. This article actually helped me realize that how I work with trauma patients is actually how logotherapy help patients. Thank you.
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

How to Keep a Healthy Mind While Aging: 8 Easy Strategies
With 1 in 5 people likely to be over 60 by 2050 (Ballesteros, 2022), it is becoming increasingly essential to understand why our cognitive powers [...]

Existential Crisis: How to Cope With Meaninglessness
Recent statistics suggest that over a quarter of UK nationals feel a deep sense of meaninglessness (Dinic, 2021). In the wake of multiple global economic, [...]

9 Powerful Existential Therapy Techniques for Your Sessions
While not easily defined, existential therapy builds on ideas taken from philosophy, helping clients to understand and clarify the life they would like to lead [...]
Read other articles by their category
- Body & Brain (52)
- Coaching & Application (39)
- Compassion (23)
- Counseling (40)
- Emotional Intelligence (22)
- Gratitude (18)
- Grief & Bereavement (18)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (16)
- Mindfulness (40)
- Motivation & Goals (41)
- Optimism & Mindset (29)
- Positive CBT (28)
- Positive Communication (23)
- Positive Education (37)
- Positive Emotions (32)
- Positive Leadership (16)
- Positive Parenting (14)
- Positive Psychology (21)
- Positive Workplace (35)
- Productivity (16)
- Relationships (46)
- Resilience & Coping (39)
- Self Awareness (20)
- Self Esteem (37)
- Strengths & Virtues (29)
- Stress & Burnout Prevention (33)
- Theory & Books (42)
- Therapy Exercises (37)
- Types of Therapy (54)
3 Meaning Exercises Pack (PDF)
- What is Psychotherapy?
Psychotherapy is a type of treatment that can help individuals experiencing a wide array of mental health conditions and emotional challenges. Psychotherapy can help not only alleviate symptoms, but also, certain types of psychotherapies can help identify the psychological root causes of one’s condition so a person can function better and have enhanced emotional well-being and healing.
Conditions that can be helped by psychotherapy include coping with stressful life events, the impact of trauma, medical illness or loss such as the death of a loved one; and specific mental health conditions such as depression or anxiety. There are several different types of psychotherapy and some types may work better with certain clinical situations. Psychotherapy may be used in combination with medication or other therapies.
Therapy Sessions
Therapy may be conducted in an individual, family, couple, or group setting, and can help both children and adults. Sessions are typically held once a week for about 45 to 50 minutes. Both patient and therapist need to be actively involved in psychotherapy. The trust and relationship between a person and his/her therapist is important for working together effectively and making gains from psychotherapy.
Psychotherapy can be short-term (a few weeks to months), dealing with more immediate challenges, or long-term (months to years), dealing with longstanding and complex issues. The goals of treatment and duration and frequency of treatment are discussed by the patient and therapist together.
Confidentiality is a basic requirement of psychotherapy. Also, although patients share personal feelings and thoughts, intimate physical contact with a therapist is never appropriate, acceptable.
Psychotherapy and Medication
Psychotherapy is often used in combination with medication to treat mental health conditions. In some circumstances medication may be clearly indicated and in others psychotherapy may be the best option. For many people combined medication and psychotherapy treatment can be more beneficial than either alone. Healthy lifestyle improvements, such as healthy nutrition, regular exercise and adequate sleep, can also be valuable in supporting recovery and overall wellness.
Does Psychotherapy Work?
Research shows that most people who receive psychotherapy experience symptom relief and are better able to function in their lives. About 75 percent of people who enter psychotherapy show some benefit from it. 1 Psychotherapy has been shown to improve emotional and psychological well-being and is linked with positive changes in the brain and body. The benefits also include fewer sick days, less disability, fewer medical problems, and increased work satisfaction.
With the use of brain imaging techniques researchers have been able to see changes in the brain after a person has undergone psychotherapy. Numerous studies have identified brain changes in people with mental illness (including depression, panic disorder, PTSD and other conditions) as a result of undergoing psychotherapy. In most cases the brain changes resulting from psychotherapy were similar to changes resulting from medication. 2
To help get the most out of psychotherapy, approach the therapy as a collaborative effort, be open and honest, and follow your agreed upon plan for treatment. Follow through with any assignments between sessions, such as writing in a journal or practicing what you’ve talked about.
Types of Psychotherapy
Psychiatrists and other mental health professionals use several types of therapy. The choice of therapy type depends on the patient’s particular illness and circumstances and his/her preference. Psychiatrists and other clinicians may combine elements from different approaches to best meet the needs of the person receiving treatment.
- Cognitive behavioral therapy (CBT) helps people identify and change thinking and behavior patterns that are unhealthy or ineffective, replacing them with more accurate thoughts and functional behaviors. It can help a person focus better on current problems and how to solve them. It often involves practicing new skills in the “real world.” CBT can be helpful in treating a variety of disorders, including depression, anxiety, trauma related disorders, and eating disorders. For example, CBT can help a person with depression recognize and change unhelpful or maladaptive thought patterns or behaviors that are contributing to the depression.
- Interpersonal therapy (IPT) is a short-term form of treatment. It helps patients understand underlying interpersonal issues that are troublesome, like unresolved grief, changes in social or work roles, conflicts with significant others, and problems relating to others. It can help people learn healthy ways to express emotions and ways to improve communication and how they relate to others. It is most often used to treat depression.
- Dialectical behavior therapy is a specific type of CBT that helps more effectively regulate emotions. It is often used to treat people with chronic suicidal thoughts and people with borderline personality disorder, eating disorders and PTSD. It teaches new skills to help people take personal responsibility to change unhealthy or disruptive behavior. It involves both individual and group therapy.
- Psychodynamic therapy is based on the idea that behavior and mental well-being are rooted in childhood and past experiences and involves bringing to conscious awareness feelings that might be unconscious (outside a person's awareness). A person works with the therapist to improve self-awareness and to change deep-seated patterns so that they can more fully take charge of their life.
- Psychoanalysis is a more intensive form of psychodynamic therapy. Sessions are typically conducted three or more times a week.
- Supportive therapy uses guidance and encouragement to help patients develop their own resources. It helps build self-esteem, reduce anxiety, strengthen coping mechanisms, and improve social and community functioning. Supportive psychotherapy helps patients deal with issues related to their mental health conditions which in turn affect the rest of their lives.
Additional therapies sometimes used in combination with psychotherapy include:
- Animal-assisted therapy – working with dogs, horses or other animals to bring comfort, help with communication and help cope with trauma.
- Creative arts therapy – use of art, dance, drama, music and poetry therapies.
- Play therapy – to help children identify and talk about their emotions and feelings.
Finding and Choosing a Psychotherapist
How is depression treated.
Psychotherapy can be provided by a number of different types of professionals including psychiatrists, psychologists, licensed social workers, licensed marriage and family therapists, and others with specialized training in psychotherapy. Psychiatrists are also trained medical doctors and are able to prescribe medication as well as help with ruling out any underlying medical condition (or medication) that may be causing one's condition. For example, untreated thyroid conditions or use of certain medications can cause depressive symptoms.
Finding a psychiatrist or other therapist with whom an individual can work well is important. Sources of referrals include primary care physicians, local psychiatric societies, medical schools, community health centers, workplace Employee Assistance Programs (EAP), and online resources (see links to online locators below).
Federal law requires that in most cases mental health services, including psychotherapy, be covered by health insurance similar to other medical care costs. ( Read more about insurance coverage of mental health care )
Physician Review
Richa Bhatia, M.D.
References
- American Psychological Association. Understanding psychotherapy and how it works. 2016.
- Karlsson, H. How Psychotherapy changes the Brain. Psychiatric Times . 2011.
- Wiswede D, et al. 2014. Tracking Functional Brain Changes in Patients with Depression under Psychodynamic Psychotherapy Using Individualized Stimuli. PLoS ONE . 2014. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0109037
Medical leadership for mind, brain and body.
Mobile menu.
- Psychiatrists
- Residents & Medical Students
- Patients and Families
- Advocacy & APAPAC
- Diversity & Health Equity
- Research & Registry
- Meetings & Events
- Search Directories & Databases
- International
- Medical Students
- What is Psychiatry?
- Find a Psychiatrist
- Addiction and Substance Use Disorders
- Dementia and Alzheimer's Disease
- Alcohol Use Disorder
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder
- Bipolar Disorders
- Climate Change and Mental Health Connections
- Coping After Disaster
- Disruptive, Impulse-Control and Conduct Disorders
- Dissociative Disorders
- Domestic Violence
- Eating Disorders
- E-Cigarettes and Vaping
- Gambling Disorder
- Gender Dysphoria
- Helping a Loved One Cope with Mental Illness
- Hoarding Disorder
- Integrated Behavioral Healthcare
- Intellectual Disability
- Internet Gaming
- Obsessive-Compulsive Disorder
- Opioid Use Disorder
- Perinatal Depression (formerly Postpartum)
- Personality Disorders
- Posttraumatic Stress Disorder (PTSD)
- Prolonged Grief Disorder
- Schizophrenia
- Seasonal Affective Disorder (SAD)
- Sleep Disorders
- Somatic Symptom Disorder
- Specific Learning Disorders
- Stigma, Prejudice and Discrimination Against People with Mental Illness
- Suicide Prevention
- Technology Addictions: Social Media, Online Gaming, and More
- Warning Signs of Mental Illness
- Electroconvulsive Therapy (ECT)
- What is Mental Illness?
- What is Telepsychiatry?
- La Salud Mental
- Childhood Disorders: Medication Guides for Parents
- Lifestyle to Support Mental Health
- Member Benefits
- Honorary Fellowship (FAPA & DFAPA)
- Awards & Leadership Opportunities
- Get Involved
- Directories, Contact Info & FAQs
- District Branches
- APA's Vision, Mission, Values, and Goals
- Meet Our Organization
- Read APA Organization Documents and Policies
- Work At APA
- About APA's Headquarters
- Policy Finder
- News Releases
- Messages from the APA President
- Reporting on Mental Health Conditions
- Goldwater Rule
- Annual Meeting Press Registration + Guidelines
- APA Public Opinion Polls
- Reporter Toolkit: Recommendations on Covering the AAPI Community
- Comunicados de prensa en español
- APA Annual Meeting
- APA Communities
- APA Foundation
- APA JobCentral
- APA Learning Center
- APA Publishing
- Center for Workplace Mental Health
- Melvin Sabshin, M.D. Library & Archives
- Psychiatric News
- Psychiatry Online
- Annual Meeting
- APA On Demand
- At the APA Educational Series
- Books and Journals
- Certification and Licensure
- Diversity and Health Equity Education Resources
- Meeting Submission and Guidelines
- Mental Health Innovation Zone
- The Mental Health Services Conference
- The Virtual Immersive
- Virtual Paid Courses
- Clinical Practice Guidelines
- Covid-19 / Coronavirus
- Digital Mental Health
- Helping Patients Access Care
- Media and Communications
- Mental Health Apps
- Mental Health Parity
- Practice Management
- Professional Interests
- Quality Improvement
- Risk Management
- Social Media
- Sunshine Act
- Telepsychiatry
- The Clozapine Risk Evaluation and Mitigation Strategy (REMS) Program
- Transition to Practice and Early Career Resources
- Well-being and Burnout
- Mental Health and Faith Community Partnership
- Mental Health Equity Looking Beyond Series
- Minority and Underrepresented (M/UR) Caucuses
- Moore Equity in Mental Health Initiative
- News and Updates
- Striving for Excellence Series
- SAMHSA Minority Fellowship Program
- AMNet: Addiction Medicine Practice Based Research Network
- PsychPRO: APA's Mental Health Registry
- Research Colloquium for Junior Psychiatrist Investigators
- Perinatal Mental Health Toolkit
- Psychiatric Bed Crisis Report
- Advocacy Action Center
- Congressional Advocacy Network
- Election Resource Center
- Federal Affairs
- State Affairs
- Implementing 9-8-8
- Advocacy Update Webinars
- 2025 Annual Meeting
- The 2024 Mental Health Services Conference
- Addressing Structural Racism Town Hall Series
- APA Meetings App
- Governance Meetings
- Mental Health Equity Fireside Chat Series
- Moore Equity in Mental Health 5K
- Policy & Practice Insights Series
- September Component Meetings
- Social Determinants of Mental Health Town Hall Series
- Amicus Briefs
- Assembly Directory
- Component Directory
- Conference Publications
- Library and Archive
- Member Directory
- Member Obituaries
- Practice Guidelines
- Resource Documents
- International Trainees
- International Humanitarian Opportunities
- Global Mental Health
- International Medical Graduates Resources
- Residents' Journal
- Featured Publications
- APAF Fellowships
- External Fellowships and Awards
- Helping Residents Cope with a Patient Suicide
- Vacant Resident Positions
- Leadership Positions
- SET for Success
- Apply for Psychiatric Residency
- Choosing a Career in Psychiatry
- Building a Career in Psychiatry
- Medical Student Programs
- Resident-Fellow Census
- Transitioning to Residency During COVID-19
- What Is a Substance Use Disorder?
- Expert Q&A: Addiction and Substance Use Disorders
- What Are Dementia and Alzheimer’s Disease?
- Expert Q&A: Dementia and Alzheimer's Disease
- What are Anxiety Disorders?
- Expert Q&A: Anxiety Disorders
- What is ADHD?
- Expert Q&A: ADHD
- What Is Autism Spectrum Disorder?
- Expert Q&A: Autism Spectrum Disorder
- What Are Bipolar Disorders?
- Expert Q&A: Bipolar Disorder
- How Extreme Weather Events Affect Mental Health
- Who Is Affected by Climate Change?
- What Is Depression?
- Expert Q&A: Depression
- What are Disruptive, Impulse Control and Conduct Disorders?
- Expert Q&A: Disruptive, Impulse Control and Conduct Disorders
- What Are Dissociative Disorders?
- Expert Q&A: Dissociative Disorders
- What are Eating Disorders?
- Expert Q&A: Eating Disorders
- What is Gambling Disorder?
- Expert Q&A: Gambling Disorder
- What is Gender Dysphoria?
- Expert Q&A: Gender Dysphoria
- What is Hoarding Disorder?
- Expert Q&A: Hoarding Disorder
- What is Intellectual Disability?
- Expert Q&A: Intellectual Disability
- What Is Obsessive-Compulsive Disorder?
- Expert Q&A: Obsessive-Compulsive Disorder
- What is Perinatal Depression (formerly Postpartum)?
- Expert Q&A: Perinatal Depression
- What are Personality Disorders?
- Expert Q&A: Personality Disorders
- What is Posttraumatic Stress Disorder (PTSD)?
- Expert Q&A: Posttraumatic Stress Disorder (PTSD)
- What is Schizophrenia?
- Expert Q&A: Schizophrenia
- What are Sleep Disorders?
- Expert Q&A: Sleep Disorders
- What is Somatic Symptom Disorder?
- Expert Q&A: Somatic Symptom Disorder
- What Are Specific Learning Disorders?
- Expert Q&A: Specific Learning Disorders
- What is Technology Addiction?
- Expert Q&A: Technology Addiction
- Cigarrillos electrónicos y vapeo
- Trastorno del espectro autista
- Trastorno por consumo de alcohol
- Trastorno por consumo de opioides
- Trastorno de estrés postraumático (TEPT)
- Adicción a la tecnología: redes sociales, juegos en línea, y más
- ¿Qué es la psiquiatría?
- Conexiones entre el cambio climático y la salud mental
- Más temas de salud mental
- General Members
- Early Career Psychiatrists
- Residents and Fellows
- International Resident-Fellows
- Semi-Retired and Retired
- View Your Profile
- Resident-Fellow Members
- Fellow of the APA
- Distinguished Fellow of the APA
- International Fellow of the APA
- International Distinguished Fellow of the APA
- 2024 Class of Honorary Fellows
- 2025 APA National Elections
- Councils, Committees and Components
- Resident-Fellow Leadership Opportunities
- Volunteer Leadership Opportunities
- Advocacy and APAPAC
- APA/APAF Fellowships
- APA Insider Sessions
- APA Specialty Interest Caucuses, Listservs & Communities
- Leadership, Equity and Diversity Institute
- Mentorship Program for APA/APAF Fellows
- Research Colloquium
- Contact Your Membership Specialist
- Contact Your District Branch
- Membership FAQs
- Semi-Retired and Retired FAQs
- Lump Sum Dues
- 2025 APA Dues Rate Changes FAQs
- District Branch Resources
- District Branch Dues for General Members
- District Branch Dues for Residents and Fellows
- Craft and Criticism
- Fiction and Poetry
- News and Culture
- Lit Hub Radio
- Reading Lists

- Literary Criticism
- Craft and Advice
- In Conversation
- On Translation
- Short Story
- From the Novel
- Bookstores and Libraries
- Film and TV
- Art and Photography
- Freeman’s
- The Virtual Book Channel
- Behind the Mic
- Beyond the Page
- The Cosmic Library
- The Critic and Her Publics
- Emergence Magazine
- Fiction/Non/Fiction
- First Draft: A Dialogue on Writing
- The History of Literature
- I’m a Writer But
- Lit Century
- The Lit Hub Podcast
- Tor Presents: Voyage Into Genre
- Windham-Campbell Prizes Podcast
- Write-minded
- The Best of the Decade
- Best Reviewed Books
- BookMarks Daily Giveaway
- The Daily Thrill
- CrimeReads Daily Giveaway


On the Uncertain Border Between Writing and Therapy
Veronica esposito explores the intersection of creativity and trauma.
Years ago, I entered the world of mental health by getting myself a therapist. Little did I know that this small but decisive step would lead me deeper and deeper into the world of mental health, until I eventually found myself practicing therapy.
Every now and then I take a moment to look back on things, and I’m always kind of amazed: the changes the mental health world has made on me have been so great that it’s hard to imagine how the person I am today can actually occupy the same timeline as that of my pre-therapy self.
On a micro level, therapy has changed the very texture of the language that I use to speak and think my way through life; and on a macro level, it has transformed the basics of how I conceptualize myself and my world. To put it into literary terms, it’s a little like I switched the genre of my life—from say the claustrophobic modernism of a Franz Kafka to the truth-seeking comedy of a Lorrie Moore.
Going from Franz Kafka to Lorrie Moore is a pretty stunning change, and I think it shows the depth of what therapy can achieve. At its deepest, therapy seeks to make foundational change in who a person is. The various philosophies, approaches, techniques, laws, and ethics that collectively form the knowledge that therapy means to offer to the world is, at root, an attempt to imagine nothing less than how to live a good life and be a good person.
I’ve often reflected that such a transformative experience as that which I’ve had in the world of mental health must have made a sizable impact on who I am as a writer—and, in fact, many people have told me that they have seen the difference. I absolutely believe it’s there. Not just in how my writing looks and feels but in the very basis of what animates me to write, and basic assumptions I bring to my writing practice, how I envision and pursue the whole venture. My experiences have filled me with an interest in knowing exactly what therapy does for a writer’s work, which is why I set out to create this essay.
In researching this piece, I found something interesting: many creative writers and scientific researchers have explored the question of how creative writing may or may not be therapy, but I could not find anyone who had posed the question in the other direction: what impact therapy may have on one’s creative writing.
The research that I found on the matter tended—as research does—to focus on what effects specific applications of creative writing had on various mental health outcomes, like depression, dysfunction, and quality of life. There was an emphasis on trauma-processing and exploration, and the verdict was clear: writing can be an effective therapeutic tool.
By contrast, many of the creative writers who I read on the matter were much more leery of the prospect of writing being therapy. This is epitomized by memorist T Kira Madden’s Literary Hub essay “Against Catharsis: Writing is Not Therapy,” the jist of which states that artistic writing is much too prosaic and difficult to involve the “bleeding into the typewriter” that she equates with true “healing.” That is, when you’re laboring over every last word, there’s no room for catharsis—the very craftiness of creative labor precludes it, with Madden styling her writing self as just an actor working to create a product for an audience.
There were other voices, like that of Tara DaPra in Creative Nonfiction , who saw the writing process as more emotionally engaged and thus more therapeutic. In her essay “Writing Memoir and Writing for Therapy” she argues that “writing emotionally driven memoir is, in fact, cathartic, at least initially.” She see hammering out that messy first draft as akin to what one does in a therapy room, and she offers that this drafting can have further therapeutic benefits: you can let that draft sit for a while and return to your problems with fresh eyes, or the braver can show it to their friends and ask for input. In contrast to Madden’s boring workmanship, DaPra sees the writing process as driven by “emotion and instinct.”
Whether or not a writer was pro or con regarding creative writing being therapeutic, they tended toward an overly simplistic equation of therapy with the raw emotionality of catharsis. Certainly, therapy can provide individuals with space to fall to pieces and gush in a way that most daren’t do with friends, family, or partners, but it is much more than that. On its deepest and most powerful level, therapy attempts to change the basic assumptions and beliefs that one operates with as a human being: the story you tell yourself about who you are and what kind of a world you live in.
This is the most powerful kind of trauma-processing: to ask your brain to let go of the lessons that trauma has taught you and to instead believe in something different. Not all clients, of course, will reach that stage—for many, therapy may just be a space for emotional catharsis, working out day-to-day questions, and attaining better coping mechanisms—and that of course is fine and can still offer substantial benefit.
But I do think that, for writers, the opportunity to drill down to the most deeply held beliefs about who we are and what world we live in offers an amazing chance to examine the very stuff of one’s writing and to transform a writing practice. It is authors who had precisely these sorts of experiences in therapy whom I turn toward now.
Writer Isle McElroy, author of The Atmospherians , initially struck a note similar to Madden and DaPra, beginning our conversation by telling me that therapy has let them better “engage with traumatic events because I can see them differently because of the processing that I’ve done. It’s a thing that I can carry, not a thing that I have stepped inside of.” In our conversation, McElroy noted that they had to get through stages of processing their trauma; in these initial stages their writing tended to come out more like a journal-y first draft than a polished essay—therapy helped them do that work and move on to a different sort of writing.
Accordingly, McElroy explained that subsequent experiences in therapy went beyond just finding it useful as a tool for catharsis. They told me that therapy has helped them “connect with my curiosity. I’m being asked to have curiosity about myself that I didn’t previously. It’s the curiosity of discovery. Once I’ve become more settled, having an opportunity to explore has been really good. It drives me deeper into my own understanding of myself.” They added that “the relationship puts the onus on me, which has been especially helpful for the writing process. I’m digging deeper toward my actual thoughts.”
Ultimately, therapy lead McElroy to re-conceptualize the very purpose and goal of their writing: “a lot of the therapeutic process was finding self-worth outside of the entertainment that I can give to people. Previously my writing had been a desire to entertain others by revealing my own personal pain.”
McElroy’s remarks resemble my own experience of therapy and my aims as a therapist. Whereas the initial stages of therapy often involve lots of catharsis—letting go of all this painful emotional stuff that you’ve been holding on to—it usually moves on to a less emotionally flooded opportunity to re-envision yourself.
I very much relate to that deeper understanding of self that McElroy mentioned; for me personally, in drilling past the layers of trauma, I was able to see how so much of my relationship with the world was a product of that trauma mindset. I got down to a deeper stratum of self that felt more authentically me, and that I more and more let loose on the page. I also discovered, as McElroy mentioned, ways to be curious about myself, to in fact adopt curiosity as a stance.
I found my conversation with poet Kim Koga very stimulating in that she opened new ways for me to understand therapy itself as a creative process. Koga shared her experiences with EMDR—an acronym that stands for eye movement desensitization and reprocessing, an increasingly popular method for processing heavy trauma—telling me that EMDR felt like a creative process for her. “I like EMDR because it’s very experiential and creative,” she told me. “I use a lot of my creativity in my healing.” I liked Koga’s remarks because they troubled Madden’s binary of catharsis versus creativity: for Koga, catharsis itself involved using her creativity.
Koga was kind enough to share some of her experiences with EMDR with me, discussing it in terms very different from what many would consider therapy: she told me about magnificent, dreamlike journeys through her mind’s eye that she undertakes in the trance-like state created by EMDR. Part of Koga’s purpose in taking these inner journeys is to “make safe spaces inside my body and brain, where me and my child self can go. I put a door on it, where I can go when I need to.”
That is, when Koga has used therapy to build safe refuges where she can ride out the storm when she feels the trauma of past experiences manifesting in her brain and body. This process involves creativity that Koga has found transferable to her work as a poet.
In our conversation Koga also spoke of therapy in the more familiar terms of helping her get past creative blocks. “There’s a part of me that feels like I can’t stop writing the same poem that I’ve been writing since I was 20. I feel like so much of my poetry has been around trauma, death sex, violence. Therapy really helped me get unstuck. It’s helped me become more aware of things that I’m feeling, to move out of trauma in a way that can open my brain up more creatively.”
Koga also talked about therapy in terms of opening up her sensitivity: she shared how, before therapy, she used to be able to watch the extremely violent drama The Wire and not feel anything, but now she is so emotionally attuned that she finds it difficult to get through an episode.
Much of what Koga shared with me resonated with my own journey through therapy. Like Koga, it helped me to realign my sense of purpose and values so that I became interested in writing about different things than the trauma that had formerly drawn my writerly attention with a laser-focus.
Also like Koga, I found my senses opening back up, letting me connect with the world more thoroughly—this reconnection has had profound impacts on how I write. And even though I have not, like Koga, undertaken surreal journeys via EMDR, I have found that a lot of the creativity I’m pushed to use in therapy has also found applications in my writing process.
In writing this essay, I’ve come to see what a big, big topic this is, and I want to conclude here by stating my belief that this is a much larger story than I can hope to tell right here. Any sort of conclusion I can make right now is going to feel a little like a Band Aid. But, hoping to find somewhere to land for the time being, I’ll say the following: as writers, our inspiration and trauma often go hand in hand—they can often be difficult to distinguish, and they can feed off one another.
At this moment it feels right to hypothesize that my experiences in the world of mental health have left me better able to understand the inter-relationships between the two and to be in greater control of both. I’ll give the final word to Koga, whom I believe well embodies what I’m trying to say:
Post-therapy, the texture of my poems is now lighter and more introspective in an exploratory way, rather than focusing on the brutality that I felt. The textures have gotten more varied. It’s like when I walk into a fabric store and I can see everything, whereas I used to walk into a fabric store and feel like the black crepe was all there was. I feel like my poems are more nuanced than they used to be, and I’m more able to explore that darkness in a nuanced way.
- Share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Google+ (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Pocket (Opens in new window)

Veronica Esposito
Previous article, next article, support lit hub..
Join our community of readers.
to the Lithub Daily
Popular posts.

The Lives of the Wives : Carmela Ciuraru on Marriage, Writing, and Equity
- RSS - Posts
Literary Hub
Created by Grove Atlantic and Electric Literature
Sign Up For Our Newsletters
How to Pitch Lit Hub
Advertisers: Contact Us
Privacy Policy
Support Lit Hub - Become A Member
Become a Lit Hub Supporting Member : Because Books Matter
For the past decade, Literary Hub has brought you the best of the book world for free—no paywall. But our future relies on you. In return for a donation, you’ll get an ad-free reading experience , exclusive editors’ picks, book giveaways, and our coveted Joan Didion Lit Hub tote bag . Most importantly, you’ll keep independent book coverage alive and thriving on the internet.

Become a member for as low as $5/month
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Types of Mental Health Therapy
Overview of Approaches, Types, and How They're Used
- Psychoanalysis
Behavior Therapy
Cognitive therapy, humanistic therapy.
- Integrative Therapy
Deciding to start therapy is a big, personal step toward prioritizing mental health and improving overall well-being. There are differing types of mental health therapy, from cognitive behavior therapy to play therapy.
It can be overwhelming to determine which type is the best fit. At its core, therapy provides a safe and nonjudgmental environment where patients can identify problems and work collaboratively with a therapist to achieve goals.
This article discusses the five major approaches to therapy, their subtypes, and how they work.
Verywell / Theresa Chiechi
A counselor or therapist is a professional with training in treating mental health conditions and concerns. This can include various mental health diagnoses, including but not limited to:
- Bipolar disorder
- Post-traumatic stress disorder (PTSD)
- Personality disorders
- Eating disorders
- Substance use disorders
Psychoanalysis and Psychodynamic Therapies
Psychoanalysis , developed by Sigmund Freud, is one of the oldest treatment methods. In this approach, the primary focus is on uncovering and examining meaningful events or patterns from the past that may be influencing a person’s current state.
Freud believed that incidents from childhood, or thoughts and feelings lying below the surface, are the root of current unhealthy behaviors. Once unearthed, the priority becomes working to process the unconscious thoughts and feelings to change behavior. There have been many developments and advancements in psychoanalytical approaches since Freud.
While some may find this form of therapy beneficial due to deep exploration, psychoanalysis can be a significant time investment for patients.
Interpersonal Therapy
In an interpersonal therapeutic approach, the patient and therapist work together to identify the patient's diagnosis and examine it within the context of their lives and experiences. Through conducting an inventory of experiences, the patient can begin to understand patterns and significant events in their lives and relationships.
Strengthening relationships and establishing and deepening support systems are essential in this type of therapy.
Interpersonal therapy can be effective for individuals living with mood disorders, such as depression.
Mentalization Therapy
Mentalizing refers to a person’s capacity to distinguish between their emotions and the feelings of others. This process can also help patients understand how their emotions are connected to their actions.
Mentalization therapy is most commonly implemented with patients who are diagnosed with borderline personality disorder , as a way to increase awareness of thoughts and emotions, and improve interpersonal functioning.
Family Therapy
Family counseling tackles problems that occur within the family system. This therapy can help family members give voice to issues, understand each other and how the issue impacts them as a unit, and create plans to resolve issues.
This method of therapy can help families learn to communicate and support each other, improve day-to-day interactions, and manage issues by taking action.
When to Seek Family Therapy
A family might want to reach out to a family counselor if:
- A child is having a behavioral health issue.
- A family member is managing a mental or physical health condition, like a drug addiction or eating disorder.
- The family is going through a divorce.
- The family is grieving the loss of a loved one.
Group Therapy
One or two clinicians typically facilitate group therapy which may have up to 15 participating patients. This format is excellent for support groups, developing skills, or education about specific topics (e.g., substance use, grief, stress management).
Group therapy provides an atmosphere of emotional safety and connects people experiencing similar challenges. Group members can often learn and receive support from both the therapist and each other.
Group therapy can be advantageous for people who need a more cost-effective way to get treatment.
Play Therapy
Play therapy can be a directive or non-directive expressive form of therapy that helps children cultivate communication and interpersonal skills. This can be helpful as children may not be able to express their emotional concerns directly through words.
In play therapy, children work closely with a therapist—who may be an active participant or an observer—to examine how a child expresses and manages themselves. This approach can enhance a child’s social skills and communication skills.
Eye movement desensitization and reprocessing (EMDR) is a form of therapy that can help people heal after distressing or traumatic events. A therapist who utilizes EMDR will help the patient access stressful or difficult memories by pairing them with external stimuli, such as eye movement or EFT tapping .
EMDR incorporates aspects of cognitive-behavioral therapy. Research demonstrates that patients can create new associations during this process, which can help decrease psychological distress and improve functioning.
EDMR for Trauma
EMDR has been effective in helping veterans reduce PTSD symptoms, as well as demonstrating improvement in symptoms with people who have experienced other kinds of trauma. EMDR should only be performed with a licensed and certified professional due to the sensitive nature of revisiting trauma.
Behaviorism suggests that people can change their behavior by focusing on what can be observed and using proper reinforcements. Therapists can help patients evaluate behaviors that are not serving them but have been reinforced by factors throughout their lives.
By naming a target behavior and exploring how they would like the behavior to change, patients and clinicians can develop a plan that allows the patient to improve negative or unhelpful behaviors while picking up new techniques to support them in creating sustainable change.
Classical Conditioning
In a famous experiment conducted by Ivan Pavlov, dogs were conditioned to associate the sound of a bell with food. This demonstrates the essence of classical conditioning.
Human beings can also make associations between two stimuli when paired, leading to a learned response. These responses can be adaptive (positive) or maladaptive (negative).
Because the association between stimuli can change, therapists can work with patients to form different mental relationships with the stimuli, such as ones that elicit a relaxation response instead of a fear-based response. This type of learning association can be applied to phobias, anxiety, and fear.
Operant Conditioning
This behavioral approach is centered around the notion of reinforcement. A person’s behavior can be influenced one way or another by the resulting consequences.
For instance, if a child is rewarded every time they clean their room, they may repeat the behavior because they have learned that positive reinforcement will follow the activity. Alternatively, a lack of reinforcement or an unwanted consequence can cause a decrease in a specific behavior.
A therapist can apply these principles when working with a child to reinforce wanted behaviors and extinguish unwanted behaviors.
Desensitizing
People who experience fear-based responses to a trigger may engage in avoidant behavior because they have learned that they are unsafe in certain situations or events.
Desensitizing is a technique for a person to change their relationship with fear, anxiety, and safety about a situation or event.
Eventually, patients recognize that they are safe and can manage strong emotions. Desensitizing can be especially effective with anxiety and phobias.
Desensitizing Strategies
When drawing on this approach, a therapist can teach relaxation strategies like deep breathing, grounding, body scanning, and progressive muscle relaxation to decrease tension. Gradual exposure to a distressing situation or event through imagery changes the association between the trigger and the response.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy (CBT) is a popular form of psychotherapy that combines cognitive therapy and behavioral therapy to form a more holistic approach.
CBT teaches patients to recognize and challenge unhelpful or irrational thoughts that may influence their emotions and behaviors. The emphasis is on understanding the connection between thoughts, emotions, and actions and developing a more balanced perspective and response.
During sessions, patients can practice and hone new skills, as well as apply them outside of sessions through tracking or monitoring their thoughts and behaviors.
Disorders Treated With CBT
CBT is an evidence-based treatment that is effective with a variety of diagnoses, including anxiety disorders, mood disorders, stress management, interpersonal issues, and more.
There are few subtypes of CBT, which include dialectical behavioral therapy, rational emotive therapy, exposure therapy, and mindfulness-based therapy.
Dialectical Behavioral Therapy
Developed in the 1980s, this type of therapy teaches skills that improve emotional regulation, interpersonal effectiveness, and distress tolerance. It also incorporates mindfulness.
As the standard treatment for people with borderline personality disorder, patients are taught how to identify and accept their emotions and behaviors, self-validate, distinguish themselves and their experiences from others, and manage emotional distress or discomfort.
This treatment approach emphasizes expanding the skills in a person’s toolbox to help them navigate their thoughts, emotions, and relationships.
Rational Emotive Therapy
Rational emotive therapy prioritizes recognizing and challenging dysfunctional thought patterns. A principle of this treatment is that how a person views and interprets events can shape their emotions and behavior.
Therapists utilizing this approach aim to help patients replace irrational thoughts with rational thoughts, which can help them better evaluate their thoughts, feelings, and behaviors.
Exposure Therapy
Exposure therapy is an evidence-based treatment geared toward showing patients that their fears can be managed. Upon identifying situations or events that cause psychological distress, the therapist and patient work together to prioritize coping skills patients can use as needed, as well as create a plan to slowly begin exposing the patient to different levels or aspects of the trigger.
Implemented with individuals grappling with anxiety, phobias, trauma, panic attacks, or obsessive-compulsive symptoms, patients practice restructuring their thoughts about the situation or events, managing feelings of fear, anxiety, or panic, all while seeing that they are safe and can cope with distress as it arises.
Mindfulness-Based Therapy
This method is rooted in meditative practices and may incorporate cognitive behavioral therapy. It emphasizes mindfulness, or the ability to be aware and in the present.
Therapists can teach patients to tap into thoughts and feelings as they arise. Patients can gain perspective and put space between themselves and negative thoughts. Research demonstrates that mindfulness-based techniques are instrumental in decreasing symptoms of depression and anxiety.
Mindfulness Techniques
Mindfulness-based therapy techniques may include:
- Deep breathing exercises
- Visualization
- Guided imagery
This type of therapy stems from behavioral therapy. It focuses on the relationship between thoughts and feelings. When patients are able to detect dysfunctional or irrational thoughts and transform them into balanced thoughts, there is a significant emotional impact that can lead to healthier responses.
Adopting strategies to change thinking patterns is the focus here. This treatment approach is effective and can be used with patients who experience depression, anxiety, or phobias . Cognitive therapy may be combined with behavior therapy, which can provide a more comprehensive experience for patients.
In this approach to therapy, the patient is viewed as a whole and individual person. In examining their choices and behavior, therapists can aid patients in recognizing their strengths and capacity to take responsibility for themselves and their lives, and work toward evolving into a fuller version of themselves.
Part of this process is investigating how patients view the world and themselves within the world. Examining these connections keeps patients focused on the here and now and allows them to become active participants.
Existential Therapy
Through exploring a patient's personal experiences, therapists can help patients identify and create meaning in their lives. Awareness and personal responsibility are emphasized in an existential approach.
In existential therapy, pain, suffering, anxiety, and free will are all recognized as aspects of life. Patients are encouraged to be flexible in their thinking and adaptive in how they meet what life throws their way. Ultimately, patients learn acceptance and to be accountable for themselves.
Person-Centered Therapy
Also referred to as client-centered therapy, this approach prioritizes helping patients achieve personal growth and create change in their lives. Patients are viewed as the experts on themselves, and therapists empower patients to make choices that align with their goals.
The therapist uses non-directive techniques to meet the patient where they are in their journey with authenticity, empathy, and unconditional positive regard. This therapy aims to support patients in harnessing their inner strength and reaching the best possible version of themselves.
Gestalt Therapy
This therapeutic approach encourages patients to be present and evaluate the here and now. Gestalt therapy is not concerned with the past but more about how patients are impacted presently.
A therapist utilizing this approach may work with patients on cultivating a sense of acceptance, awareness, and responsibility for where they are in their lives. How a person perceives and understands themselves and their life is valuable in this form of therapy, as it can shape how humans view and interact with the world.
Emotion-Focused Therapy (EFT)
Emotion-focused therapy (EFT) is a brief therapy that helps people better identify, experience, and manage their emotions more flexibly. Centered in the here and now, EFT works to pinpoint problems, identify changes that can occur in the present, and help individuals learn to have healthier interactions in the future.
EFT for Individuals
In addition to being beneficial for couples and families, EFT is effective in the treatment of depression and trauma for individuals. One study indicated that EFT decreased symptoms of depression in couples where one member of the couple was struggling with depression.
Integrative or Holistic Therapy
Instead of utilizing one treatment method, some therapists will tailor their therapeutic approach to the patient's needs by introducing strategies and methods from two or more types of therapy.
In this approach, the patient and their concerns are viewed through a holistic lens, and interventions are selected to help patients achieve more meaningful results in therapy.
For instance, a therapist may utilize cognitive behavioral therapy to help patients identify, challenge, and develop healthier thinking patterns while also applying techniques from a mindfulness-based approach to assist patients with managing stress or emotional discomfort.
Holistic therapy can be supportive to patients managing anxiety, depression, trauma, or stress.
Animal-Assisted Therapy
The connection between animals and humans can create a sense of calm and safety. Exposure to animals can enhance psychological well-being, specifically decreasing anger and stress, improving social interactions, or helping soothe people affected by trauma.
Animal-assisted therapy has been shown to help individuals develop and strengthen their social skills, as animal-assisted therapy teaches people about empathy and bonding.
Different kinds of animals, including dogs and horses, may be used in animal-assisted therapy.
Art Therapy
Art therapy is an integrative form of therapy that involves working with different artistic mediums to facilitate self-expression.
Art therapy employs creative activities such as:
This self-expression can be significant when helping patients cultivate a more profound sense of self or heal from life events. It can also enhance cognitive and motor skills.
Art therapy can be applied to a variety of populations, including children, adults, and group settings.
Many forms of therapy can treat specific mental health diagnoses and symptoms. You might consider going to therapy if you are looking to navigate daily stressors, work through a problem, improve your relationships, cope with a traumatic event, or notice new or worsening symptoms of a mental health disorder. Having a sense of your needs, personal goals, and what you hope to get out of therapy is essential as you explore options.
Rajhans P, Hans G, Kumar V, Chadda RK. Interpersonal psychotherapy for patients with mental disorder s. Indian J Psychiatry . 2020;62(Suppl 2):S201-S212. doi:10.4103/psychiatry.IndianJPsychiatry_771_19
Søndergaard AA, Juul S, Poulsen S, Simonsen S. Mentalizing the therapist – Therapist experiences with short-term mentalization-based therapy for borderline personality disorder: A qualitative study . Front Psychiatry . 2023;14:1088865. doi:10.3389/fpsyt.2023.1088865
American Psychological Association. Understanding group therapy .
Senko K, Bethany H. Play therapy: an illustrative case . Innovations in Clinical Neuroscience . 2019;16(5-6):38.
Landin-Romero R, Moreno-Alcazar A, Pagani M, Amann BL. How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action . Front Psychol . 2018;9:1395. doi:10.3389/fpsyg.2018.01395
Lee IS, Jung WM, Lee YS, Wallraven C, Chae Y. Operant and classical learning principles underlying mind–body interaction in pain modulation: a pilot fMRI study . Sci Rep . 2021;11:1663. doi:10.1038/s41598-021-81134-6
American Psychological Association. What is cognitive behavioral therapy?
Nakao M, Shirotsuki K, Sugaya N. Cognitive–behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies . Biopsychosoc Med . 2021;15:16. doi:10.1186/s13030-021-00219-w
Gillespie C, Murphy M, Kells M, Flynn D. Individuals who report having benefitted from dialectical behaviour therapy (Dbt): a qualitative exploration of processes and experiences at long-term follow-up . Bord personal disord emot dysregul . 2022;9(1):8. doi:10.1186/s40479-022-00179-9
Huang T, Li H, Tan S, et al. The efficacy and acceptability of exposure therapy for the treatment of post-traumatic stress disorder in children and adolescents: a systematic review and meta-analysis . BMC Psychiatry . 2022;22:259. doi:10.1186/s12888-022-03867-6
Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression . Psychiatr Clin North Am . 2017;40(4):739-749. doi:10.1016/j.psc.2017.08.008
Heidari S, Shahbakhsh B, Janjoo M. The effectiveness of Gestalt therapy on depressed women in comparison with the drug therapy . Journal of Applied Psychology & Behavioral Science . 2(1):14-18.
Alder MC, Dyer WJ, Sandberg JG, Davis SY, Holt-Lunstad J. Emotionally-focused therapy and treatment as usual comparison groups in decreasing depression: A clinical pilot study . The American Journal of Family Therapy . 2018;46(5):541-555. doi:10.1080/01926187.2019.1572478
American Psychological Association. Different approaches to psychotherapy .
American Art Therapy Association. About art therapy .
By Geralyn Dexter, PhD, LMHC Dexter has a doctorate in psychology and is a licensed mental health counselor with a focus on suicidal ideation, self-harm, and mood disorders.

- Rehabilitation
- Nursing Services
- Medical Services
- Respite Care
- Personalized Plan of Care
- Attending Physicians
- Alzheimer's Care
- Accommodations
A Comprehensive Guide to 250 Essay Topics in Therapy: Exploring CBT, Psychoanalysis, Family Therapy, and More
Welcome to our comprehensive guide on therapeutic approaches and interventions. In this blog article, we will explore a wide range of essay topics related to various therapeutic modalities. Whether you're a student, professional, or someone interested in learning more about different types of therapy, this article is designed to provide you with a wealth of ideas and insights.
We will delve into 25 essay topics for each of the following therapeutic approaches: Cognitive Behavioral Therapy (CBT), Psychoanalysis, Family Therapy, Group Therapy, Art Therapy, Mindfulness-Based Therapy, Gestalt Therapy, Solution-Focused Brief Therapy (SFBT), Trauma-Informed Therapy, and Dialectical Behavior Therapy (DBT). Each section will present thought-provoking essay topics that cover various aspects of these approaches, ranging from theoretical foundations and techniques to practical applications and research.
By exploring these essay topics, you will gain a deeper understanding of the principles, interventions, and unique features of each therapeutic modality. Whether you're looking for inspiration for your next essay or simply want to broaden your knowledge in the field of psychotherapy, this article aims to provide you with valuable insights and ideas.
So, let's dive into the fascinating world of therapeutic approaches and discover the wide range of topics awaiting exploration!
Cognitive Behavioral Therapy (CBT)
CBT is a widely used therapy that focuses on identifying and changing negative thought patterns and behaviors. It aims to help individuals develop healthier coping strategies and improve their overall well-being.
Cognitive Behavioral Therapy (CBT) Essay Topics
- The principles and foundations of Cognitive Behavioral Therapy (CBT)
- The effectiveness of CBT in treating anxiety disorders
- Applying CBT techniques in managing depression
- The role of CBT in addressing phobias and specific fears
- CBT interventions for managing stress and improving resilience
- CBT for children and adolescents: Challenges and benefits
- Integrating mindfulness practices into CBT for enhanced outcomes
- The application of CBT in treating post-traumatic stress disorder (PTSD)
- CBT techniques for addressing obsessive-compulsive disorder (OCD)
- CBT in the treatment of eating disorders: An evidence-based approach
- The role of CBT in managing chronic pain and physical health conditions
- CBT for insomnia: A cognitive-behavioral approach to improving sleep
- Addressing anger management through CBT strategies
- CBT for substance abuse and addiction: A comprehensive approach
- The impact of CBT on self-esteem and self-worth
- CBT interventions for improving body image and reducing body dissatisfaction
- CBT in the workplace: Enhancing employee well-being and productivity
- The use of technology and online platforms in delivering CBT
- CBT for couples: Strengthening relationships and improving communication
- Cultural considerations in the application of CBT across diverse populations
- CBT as a complementary therapy for chronic medical conditions
- CBT for social anxiety: Overcoming social fears and improving social skills
- The role of CBT in managing borderline personality disorder (BPD)
- CBT techniques for managing procrastination and improving time management
- CBT and resilience-building in the face of adversity and trauma
Psychoanalysis
Psychoanalysis is a therapeutic approach developed by Sigmund Freud. It involves exploring the unconscious mind and the influence of early childhood experiences on a person's current thoughts, emotions, and behaviors.
Psychoanalysis Essay Topics
- The foundational principles of psychoanalysis: Freud's contributions and the development of the psychoanalytic approach.
- The role of the unconscious mind in psychoanalysis: Exploring the hidden motivations and desires that shape human behavior.
- The psychoanalytic concept of the Oedipus complex and its influence on individuals' relationships and development.
- The significance of dreams in psychoanalysis: Understanding the symbolic meaning and interpretation of dreams.
- Psychoanalysis and the concept of transference: Analyzing the dynamics between therapist and client.
- Freud's stages of psychosexual development and their implications for personality formation.
- The psychoanalytic perspective on defense mechanisms: Exploring how individuals protect themselves from anxiety and emotional distress.
- Critiques and controversies surrounding psychoanalysis: Evaluating the scientific validity and criticisms of the psychoanalytic approach.
- Psychoanalysis and its impact on mental health treatment: Historical context and contemporary relevance.
- The application of psychoanalysis beyond therapy: Analyzing its influence on literature, art, and culture.
- Psychoanalysis and trauma: Examining the role of repressed memories and unresolved trauma in psychological well-being.
- The relationship between psychoanalysis and sexuality: Freud's theories on human sexuality and their implications.
- Analyzing the effectiveness of psychoanalysis in treating personality disorders.
- Psychoanalysis and gender: Exploring the psychoanalytic perspective on gender identity and gender roles.
- The integration of psychoanalysis with other therapeutic approaches: Examining the compatibility and benefits of combining psychoanalysis with other modalities.
- The impact of psychoanalysis on psychotherapy: Tracing the historical evolution of psychotherapy influenced by psychoanalytic principles.
- Psychoanalysis and the nature-nurture debate: Examining the interplay between innate drives and external influences in shaping human behavior.
- The relevance of psychoanalysis in contemporary psychology: Assessing its ongoing influence in the field.
- Psychoanalysis and the interpretation of literature: Applying psychoanalytic concepts to analyze literary works.
- The role of psychoanalysis in understanding psychopathology: Exploring its contributions to diagnostic frameworks and classification systems.
- Freud's concept of the ego, superego, and id: Analyzing the interplay between these components of the psyche.
- The psychoanalytic perspective on creativity: Exploring the connection between unconscious processes and artistic expression.
- Psychoanalysis and attachment theory: Examining the influence of early childhood experiences on adult relationships.
- The limitations and challenges of practicing psychoanalysis in contemporary society.
- The influence of psychoanalysis on the field of psychology: Tracing its impact on research, theory, and clinical practice.
Family Therapy
Family therapy involves working with families as a whole to improve communication, resolve conflicts, and strengthen relationships. It recognizes the interconnectedness of family members and seeks to address issues within the family system.
Family Therapy Essay Topics
- The foundations and principles of family therapy: Exploring the theoretical underpinnings and key concepts.
- The evolution of family therapy: Tracing its historical development and major contributors.
- The role of the family therapist: Examining the skills, qualities, and ethical considerations involved in working with families.
- Family systems theory: Understanding the interconnectedness of family members and its implications for therapy.
- The use of genograms in family therapy: Analyzing family patterns and dynamics through the visual representation of family history.
- Structural family therapy: Exploring the techniques and interventions used to restructure family interactions and hierarchies.
- Narrative therapy in family settings: Examining the use of storytelling and reauthoring techniques to empower families.
- The impact of cultural diversity on family therapy: Addressing the importance of cultural competence and understanding in working with diverse families.
- Collaborative and solution-focused approaches in family therapy: Examining techniques that focus on strengths and problem-solving.
- Attachment theory and its application in family therapy: Analyzing how attachment dynamics shape family relationships and interventions.
- The role of family therapy in treating adolescent behavioral issues: Exploring interventions and strategies for working with troubled teens and their families.
- The impact of divorce and separation on family dynamics: Examining the role of family therapy in supporting families through transitions.
- Family therapy for eating disorders: Addressing the role of family systems in the development and recovery of eating disorders.
- The effectiveness of family therapy in the treatment of substance abuse and addiction.
- The use of play therapy techniques in family therapy: Analyzing the benefits of incorporating play and expressive modalities in working with families.
- Systemic family constellations: Examining the use of experiential techniques to explore family dynamics and unresolved issues.
- The integration of mindfulness in family therapy: Exploring how mindfulness practices can enhance family communication and well-being.
- Emotionally focused family therapy (EFFT): Analyzing interventions that focus on creating secure emotional bonds within families.
- LGBTQ+ families and affirmative family therapy: Addressing the unique needs and challenges faced by LGBTQ+ families in therapy.
- Multicultural considerations in family therapy: Examining how culture, race, and ethnicity influence family dynamics and therapeutic interventions.
- Collaborative therapy approaches with external systems: Exploring how family therapy can collaborate with schools, communities, and other institutions.
- Systemic family therapy for trauma: Analyzing interventions that address the impact of trauma on the entire family system.
- Family therapy in the context of blended families and step-parenting: Exploring interventions that support the integration of family members from different households.
- The impact of technology on family dynamics: Examining the role of family therapy in addressing challenges posed by digital communication and screen time.
- Ethical considerations in family therapy: Addressing issues of confidentiality, dual relationships, and informed consent in working with families.
Group Therapy
Group therapy brings together a small group of individuals who share similar concerns or challenges. It provides a supportive environment where participants can share their experiences, learn from one another, and gain insight and perspective.
Group Therapy Essay Topics
- The foundations and principles of group therapy: Exploring the theoretical underpinnings and key concepts.
- The evolution of group therapy: Tracing its historical development and major contributors.
- The role of the group therapist: Examining the skills, qualities, and ethical considerations involved in leading therapeutic groups.
- Group dynamics in therapy: Understanding the interpersonal processes and interactions that occur within therapy groups.
- The therapeutic factors and mechanisms of change in group therapy: Analyzing the specific elements that contribute to positive outcomes.
- Group therapy for specific populations: Examining the application of group therapy in diverse settings, such as substance abuse, trauma, or eating disorders.
- The use of expressive arts in group therapy: Exploring the benefits and techniques of incorporating creative modalities.
- Process-oriented versus structured group therapy: Comparing and contrasting different approaches and their effectiveness.
- The impact of cultural diversity in group therapy: Addressing the importance of cultural competence and understanding in working with diverse groups.
- Group therapy for children and adolescents: Examining age-appropriate interventions and strategies for promoting growth and development.
- The use of mindfulness in group therapy: Analyzing how mindfulness practices can enhance group cohesion and individual well-being.
- Group therapy for couples: Exploring interventions and techniques for improving communication and relational dynamics.
- Online group therapy: Examining the benefits, challenges, and ethical considerations of delivering therapy in a virtual group setting.
- Group therapy for grief and loss: Analyzing the unique benefits of sharing and processing grief within a supportive group environment.
- The impact of group therapy on self-esteem and social skills: Exploring how group interactions can facilitate personal growth and improve interpersonal relationships.
- The integration of cognitive-behavioral techniques in group therapy: Examining how cognitive restructuring and behavioral interventions are applied in a group context.
- The use of group therapy in the treatment of personality disorders: Analyzing specific techniques and interventions for addressing maladaptive patterns.
- Group therapy for anxiety and stress management: Exploring interventions and coping strategies taught within a group setting.
- LGBTQ+ affirming group therapy: Addressing the unique needs and challenges faced by LGBTQ+ individuals in therapy groups.
- Multicultural considerations in group therapy: Examining how culture, race, and ethnicity influence group dynamics and therapeutic interventions.
- Process groups versus psychoeducation groups: Comparing different types of therapeutic groups and their purposes.
- Group therapy in inpatient and outpatient settings: Examining the different contexts and applications of group therapy within a treatment continuum.
- The impact of leadership styles on group therapy outcomes: Analyzing the role of the group therapist's style and approach in facilitating change.
- Ethical considerations in group therapy: Addressing issues of confidentiality, group norms, and informed consent in the context of group therapy.
- Research and evidence-based practice in group therapy: Examining the empirical support for group therapy and identifying areas for further research.
Art Therapy
Art therapy utilizes the creative process of art-making to improve mental, emotional, and physical well-being. It allows individuals to express themselves visually, explore their emotions, and gain self-awareness and personal insight.
Art Therapy Essay Topics
- The therapeutic power of art: Exploring the psychological and emotional benefits of engaging in art-making.
- The history and evolution of art therapy as a recognized therapeutic modality.
- The role of the art therapist: Examining the skills, qualities, and ethical considerations involved in practicing art therapy.
- Art therapy with children: Analyzing the use of art as a means of communication and expression in working with young clients.
- The application of art therapy in trauma-informed care: Exploring the use of art to facilitate healing and recovery from traumatic experiences.
- Art therapy and self-discovery: Examining how art-making can enhance self-awareness and personal insight.
- The use of art therapy in addressing anxiety and stress: Analyzing how art-based interventions can reduce symptoms and promote relaxation.
- Art therapy in the treatment of eating disorders: Exploring the unique benefits of art therapy in addressing body image and self-esteem issues.
- The integration of mindfulness and art therapy: Examining the combination of mindfulness practices with art-making for enhanced therapeutic outcomes.
- Art therapy and grief: Analyzing the role of art in the process of mourning and facilitating emotional expression.
- The use of art therapy in addiction treatment: Exploring how art-making can support individuals in exploring and processing underlying emotions.
- Art therapy and cultural diversity: Addressing the importance of cultural sensitivity and inclusivity in art therapy practice.
- The role of art therapy in promoting positive mental health and well-being: Examining its preventative and wellness-focused applications.
- Art therapy in group settings: Analyzing the benefits and dynamics of art therapy groups and their impact on participants.
- The role of art therapy in supporting individuals with autism spectrum disorder: Exploring art-based interventions for communication and emotional regulation.
- Art therapy in hospital settings: Examining the use of art as a tool for coping, expression, and healing in medical environments.
- The use of digital and technology-based art therapy: Analyzing the benefits and limitations of incorporating digital platforms and tools in art therapy practice.
- Art therapy and body image: Exploring art-based interventions for cultivating self-acceptance and positive body image.
- Art therapy and cognitive enhancement: Examining the potential benefits of art-making on cognitive functions such as memory, attention, and problem-solving.
- The impact of art therapy on individuals with developmental disabilities: Analyzing how art-making can support personal growth and skill development.
- Art therapy and self-care: Exploring how engaging in art can promote self-nurturance and self-expression.
- The role of art therapy in palliative care and end-of-life settings: Examining the use of art as a means of emotional support and legacy-building.
- Art therapy and community engagement: Analyzing the use of art-making to promote social connection and empowerment within communities.
- The intersection of art therapy and neuroscience: Exploring how art-making influences brain activity and emotional processing.
- Research and evidence-based practice in art therapy: Examining the empirical support for the effectiveness of art therapy interventions and identifying areas for further research.
Mindfulness-Based Therapy
Mindfulness-based therapies, such as mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), incorporate mindfulness practices to help individuals cultivate present-moment awareness, reduce stress, and manage difficult emotions.
Mindfulness-Based Therapy Essay Topics
- The foundations and principles of Mindfulness-Based Therapy: Exploring the origins and key concepts.
- The application of mindfulness in psychotherapy: Examining the integration of mindfulness practices into therapeutic approaches.
- Mindfulness-Based Stress Reduction (MBSR): Analyzing the use of mindfulness techniques in reducing stress and promoting well-being.
- The role of mindfulness in the treatment of anxiety disorders: Examining the effectiveness of mindfulness-based interventions.
- Mindfulness-Based Cognitive Therapy (MBCT): Exploring the use of mindfulness in preventing relapse of depression.
- The impact of mindfulness on emotional regulation: Analyzing the role of mindfulness in enhancing emotional awareness and regulation.
- Mindfulness-based interventions for chronic pain management: Examining the use of mindfulness techniques in reducing pain and improving quality of life.
- The role of mindfulness in addiction recovery: Exploring mindfulness-based approaches in substance abuse treatment.
- Mindfulness and self-compassion: Analyzing the benefits of cultivating self-compassion through mindfulness practice.
- Mindfulness in the workplace: Examining the application of mindfulness-based interventions for stress reduction and improving work performance.
- Mindfulness-based interventions for children and adolescents: Exploring the use of mindfulness techniques in promoting emotional well-being and resilience.
- The impact of mindfulness on sleep quality and insomnia: Analyzing the benefits of mindfulness practices in improving sleep.
- Mindfulness and relationship satisfaction: Examining the role of mindfulness in enhancing interpersonal connections and communication.
- Mindfulness-based interventions for eating disorders: Analyzing the use of mindfulness techniques in promoting mindful eating and body acceptance.
- Mindfulness in the treatment of post-traumatic stress disorder (PTSD): Exploring mindfulness-based approaches in trauma therapy.
- The impact of mindfulness on cognitive functioning: Analyzing the effects of mindfulness practice on attention, memory, and cognitive flexibility.
- Mindfulness-based interventions for older adults: Examining the benefits of mindfulness in promoting well-being and quality of life in the aging population.
- Mindfulness and resilience: Analyzing the role of mindfulness in building psychological resilience and coping with adversity.
- Mindfulness and creativity: Exploring the relationship between mindfulness practice and creative expression.
- Mindfulness-based interventions in schools and education: Examining the benefits of mindfulness in promoting emotional well-being and academic performance.
- The impact of mindfulness on self-esteem and self-acceptance: Analyzing how mindfulness practice can enhance self-worth and self-compassion.
- Mindfulness and body-mind connection: Exploring the role of mindfulness in cultivating awareness of bodily sensations and promoting holistic well-being.
- Mindfulness and chronic illness management: Analyzing the benefits of mindfulness-based interventions for individuals with chronic health conditions.
- The integration of technology and mindfulness: Examining the use of digital platforms and applications in delivering mindfulness-based interventions.
- Research and evidence-based practice in mindfulness-based therapy: Examining the empirical support for the effectiveness of mindfulness-based interventions and identifying areas for further research.
Gestalt Therapy
Gestalt therapy focuses on promoting self-awareness and personal growth through the integration of mind, body, and emotions. It emphasizes the importance of the present moment and encourages individuals to take responsibility for their thoughts, feelings, and actions.
Gestalt Therapy Essay Topics
- The foundations and principles of Gestalt Therapy: Exploring the theoretical underpinnings and key concepts.
- The role of the Gestalt therapist: Examining the skills, qualities, and ethical considerations involved in practicing Gestalt Therapy.
- Gestalt therapy techniques and interventions: Analyzing the specific methods used to facilitate self-awareness and personal growth.
- The concept of awareness in Gestalt therapy: Exploring the importance of present moment awareness and its role in therapeutic change.
- The use of the empty chair technique in Gestalt therapy: Analyzing its application and effectiveness in working with unresolved emotions and conflicts.
- The emphasis on personal responsibility in Gestalt therapy: Examining how individuals are encouraged to take ownership of their thoughts, feelings, and behaviors.
- Gestalt therapy and the exploration of unfinished business: Analyzing the significance of unresolved past experiences and their impact on present functioning.
- The role of contact in Gestalt therapy: Examining how individuals engage in authentic and meaningful interactions with others and their environment.
- Gestalt therapy and the integration of body and mind: Exploring the importance of somatic experiences and bodily awareness in the therapeutic process.
- The holistic approach of Gestalt therapy: Analyzing how therapy addresses the individual as a whole, considering their thoughts, emotions, sensations, and behaviors.
- The use of experiments in Gestalt therapy: Examining the creative techniques and interventions used to explore and resolve personal conflicts.
- Gestalt therapy for individuals with trauma: Analyzing the application of Gestalt principles and techniques in trauma therapy.
- The role of dreams in Gestalt therapy: Exploring the symbolic and experiential aspects of dream work in therapy.
- Gestalt therapy in couples and relationship counseling: Analyzing how Gestalt principles are applied to address relational dynamics and enhance communication.
- The integration of mindfulness and Gestalt therapy: Examining the use of mindfulness practices to deepen self-awareness and support the therapeutic process.
- Gestalt therapy and creativity: Exploring how the therapeutic process can facilitate creative expression and personal growth.
- The role of dialogue and authentic communication in Gestalt therapy: Analyzing the importance of open and honest communication in therapy.
- Gestalt therapy and the exploration of polarities: Examining how individuals can integrate conflicting aspects of themselves to achieve wholeness.
- The impact of culture and diversity on Gestalt therapy: Addressing the importance of cultural sensitivity and inclusivity in Gestalt therapy practice.
- Gestalt therapy and the exploration of resistance: Analyzing how therapy addresses defense mechanisms and facilitates acceptance and change.
- Gestalt therapy and group dynamics: Examining the unique benefits and challenges of using Gestalt principles in group therapy.
- The integration of Gestalt therapy with other therapeutic modalities: Exploring the compatibility and benefits of combining Gestalt therapy with other approaches.
- Gestalt therapy and personal growth: Analyzing how Gestalt principles can be applied to support individuals in achieving their full potential.
- The impact of therapist-client relationship in Gestalt therapy: Examining the importance of the therapeutic relationship and the role of the therapist.
- Research and evidence-based practice in Gestalt therapy: Examining the empirical support for the effectiveness of Gestalt therapy interventions and identifying areas for further research.
Solution-Focused Brief Therapy (SFBT)
SFBT is a goal-oriented therapy that focuses on identifying and building upon an individual's existing strengths and resources. It emphasizes finding practical solutions to problems rather than dwelling on the issues themselves.
Solution-Focused Brief Therapy (SFBT) Essay Topics
- The foundations and principles of Solution-Focused Brief Therapy (SFBT): Exploring the theoretical underpinnings and key concepts.
- The role of the SFBT therapist: Examining the skills, qualities, and ethical considerations involved in practicing SFBT.
- The focus on strengths and resources in SFBT: Analyzing how SFBT emphasizes clients' existing strengths and abilities to facilitate change.
- Solution-focused questions and techniques in SFBT: Exploring specific questioning techniques and interventions used to explore solutions and goals.
- The future-oriented approach of SFBT: Examining how SFBT focuses on envisioning and working towards a desired future rather than dwelling on problems.
- The use of scaling and goal setting in SFBT: Analyzing how SFBT utilizes scaling questions and goal setting to facilitate progress and measurement of change.
- SFBT with children and adolescents: Exploring the adaptation and application of SFBT techniques for younger populations.
- The brief nature of SFBT: Examining the effectiveness of short-term therapy and its implications for clients and therapists.
- SFBT and cultural diversity: Addressing the importance of cultural sensitivity and inclusivity in SFBT practice.
- The application of SFBT in organizational settings: Analyzing how SFBT principles can be used to address challenges and promote positive change in workplaces.
- SFBT and trauma-informed care: Exploring the use of SFBT techniques in supporting individuals who have experienced trauma.
- The integration of SFBT with other therapeutic modalities: Examining the compatibility and benefits of combining SFBT with other approaches.
- SFBT and addiction treatment: Analyzing the application of SFBT techniques in addressing substance abuse and addictive behaviors.
- SFBT in couples and family therapy: Exploring how SFBT can be applied to enhance communication, problem-solving, and relationship dynamics.
- The use of exceptions and miracle questions in SFBT: Analyzing the effectiveness of these techniques in shifting perspectives and generating solutions.
- SFBT and resilience: Examining how SFBT can promote and enhance individuals' resilience in the face of challenges.
- The impact of therapist-client collaboration in SFBT: Analyzing the importance of a collaborative partnership between the therapist and client in the therapeutic process.
- SFBT and school counseling: Exploring the use of SFBT techniques in supporting students' academic, social, and emotional well-being.
- The role of feedback and outcome measures in SFBT: Examining how feedback and measurement tools are utilized to monitor progress and evaluate outcomes.
- SFBT in crisis intervention: Analyzing how SFBT can be applied effectively in time-limited and high-stress situations.
- SFBT and self-efficacy: Exploring how SFBT can empower individuals by fostering a sense of competence and self-belief.
- The impact of cultural narratives and storytelling in SFBT: Examining the role of storytelling and cultural narratives in shaping clients' perceptions and desired outcomes.
- SFBT and post-traumatic growth: Analyzing how SFBT principles can support individuals in finding meaning and growth following trauma.
- The use of SFBT in community settings: Exploring how SFBT can be utilized to promote well-being and positive change in communities.
- Research and evidence-based practice in SFBT: Examining the empirical support for the effectiveness of SFBT interventions and identifying areas for further research.
Trauma-Informed Therapy
Trauma-informed therapy acknowledges the impact of past traumatic experiences on an individual's mental health and well-being. It provides a safe and supportive environment where trauma survivors can process their emotions, develop coping skills, and work towards healing.
Trauma-Informed Therapy Essay Topics
- The foundations and principles of trauma-informed therapy: Exploring the theoretical underpinnings and key concepts.
- The impact of trauma on individuals: Examining the psychological, emotional, and physical effects of trauma.
- Trauma-informed assessment and diagnosis: Analyzing the considerations and approaches in assessing trauma and its effects.
- The role of the therapist in trauma-informed therapy: Examining the skills, qualities, and ethical considerations involved in working with trauma survivors.
- Trauma-focused interventions: Exploring evidence-based approaches used in trauma-informed therapy, such as Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) or Eye Movement Desensitization and Reprocessing (EMDR).
- Understanding complex trauma: Analyzing the unique challenges and treatment considerations for individuals who have experienced chronic and multiple traumas.
- The use of psychoeducation in trauma-informed therapy: Examining the importance of providing information and education to empower trauma survivors.
- Trauma-informed care in diverse populations: Addressing the importance of cultural sensitivity and inclusivity in trauma therapy practice.
- The impact of trauma on attachment and relationships: Exploring the effects of trauma on interpersonal connections and strategies for healing relational wounds.
- The role of safety and stabilization in trauma-informed therapy: Analyzing the importance of creating a safe and supportive therapeutic environment.
- Trauma and somatic experiencing: Examining the integration of body-oriented approaches in trauma therapy to address trauma held in the body.
- Trauma-informed approaches in substance abuse treatment: Analyzing the intersection of trauma and addiction and the integration of trauma-informed care in recovery.
- Secondary trauma and vicarious resilience: Exploring the effects of working with trauma survivors on therapists and strategies for self-care and resilience.
- Trauma-informed interventions for children and adolescents: Analyzing developmentally appropriate approaches in trauma therapy for younger populations.
- The use of narrative therapy in trauma-informed care: Examining the power of storytelling and narrative reconstruction in healing from trauma.
- Trauma-informed therapy in the criminal justice system: Exploring the importance of trauma-informed approaches in supporting individuals who have experienced trauma within the legal system.
- The impact of adverse childhood experiences (ACEs) on long-term health outcomes: Analyzing the connection between childhood trauma and physical and mental health conditions.
- Trauma-informed therapy and resilience: Examining how trauma-informed approaches can support the development of resilience in trauma survivors.
- The role of trauma-informed therapy in post-disaster and emergency response: Exploring the application of trauma-informed care in crisis situations.
- Trauma-informed care in educational settings: Analyzing the importance of trauma-informed approaches in supporting students who have experienced trauma.
- The use of mindfulness in trauma-informed therapy: Examining the integration of mindfulness practices to enhance self-regulation and promote healing.
- Trauma-informed therapy and cultural humility: Addressing the importance of understanding and honoring diverse cultural perspectives and experiences in trauma treatment.
- Trauma-informed therapy and the neurobiology of trauma: Exploring the impact of trauma on the brain and the role of trauma-informed approaches in promoting neurobiological healing.
- The use of expressive arts in trauma-informed therapy: Analyzing the benefits of utilizing creative modalities, such as art, music, and dance, in trauma treatment.
- Research and evidence-based practice in trauma-informed therapy: Examining the empirical support for trauma-informed interventions and identifying areas for further research.
Dialectical Behavior Therapy (DBT)
DBT combines elements of cognitive-behavioral therapy with mindfulness practices. It is particularly effective for individuals who struggle with regulating emotions and engaging in self-destructive behaviors. DBT focuses on developing skills for emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness.
Dialectical Behavior Therapy (DBT) Essay Topics
- The foundations and principles of Dialectical Behavior Therapy (DBT): Exploring the theoretical underpinnings and key concepts.
- The role of the DBT therapist: Examining the skills, qualities, and ethical considerations involved in practicing DBT.
- Dialectics in DBT: Analyzing the importance of finding balance and synthesizing seemingly contradictory ideas in therapy.
- The four modules of DBT: Exploring the components of DBT, including mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Mindfulness in DBT: Examining the role of mindfulness practice in cultivating present moment awareness and non-judgmental acceptance.
- Distress tolerance in DBT: Analyzing the strategies and skills used to cope with distressing situations and emotions.
- Emotion regulation in DBT: Exploring the techniques and interventions used to identify, understand, and regulate intense emotions.
- Interpersonal effectiveness in DBT: Examining the skills and strategies for enhancing communication, setting boundaries, and building healthy relationships.
- DBT with borderline personality disorder: Analyzing the effectiveness of DBT in treating individuals with borderline personality disorder and related difficulties.
- DBT for self-harm and suicidal behaviors: Exploring the application of DBT techniques in addressing self-destructive behaviors.
- DBT and substance use disorders: Examining the integration of DBT principles and strategies in the treatment of substance abuse and addiction.
- DBT and trauma: Analyzing how DBT can be adapted to address the impact of trauma and promote healing.
- The use of diary cards and behavioral tracking in DBT: Examining the importance of self-monitoring and tracking progress in DBT.
- DBT skills groups: Exploring the benefits and structure of DBT skills groups in promoting skill acquisition and peer support.
- The role of validation in DBT: Analyzing the importance of validating experiences and emotions in fostering therapeutic rapport and change.
- DBT in forensic settings: Examining the application of DBT principles and techniques in working with individuals involved in the criminal justice system.
- Cultural considerations in DBT: Addressing the importance of cultural sensitivity and inclusivity in DBT practice.
- DBT in schools and educational settings: Exploring the use of DBT skills in supporting students' emotional well-being and academic success.
- The impact of the therapeutic relationship in DBT: Analyzing the role of the therapeutic alliance and the dynamics between therapist and client in DBT.
- The use of coaching calls and phone consultations in DBT: Examining the benefits and effectiveness of remote support between therapy sessions.
- DBT and emotion dysregulation: Exploring how DBT addresses difficulties in emotional regulation and promotes adaptive coping strategies.
- The integration of DBT with other therapeutic modalities: Examining the compatibility and benefits of combining DBT with other approaches.
- DBT and self-compassion: Analyzing the role of self-compassion practices in DBT and their impact on well-being and change.
- The application of DBT in community settings: Exploring how DBT principles can be utilized to support individuals in diverse community settings.
- Research and evidence-based practice in DBT: Examining the empirical support for the effectiveness of DBT interventions and identifying areas for further research.
We have reached the end of our exploration into the world of therapeutic approaches and interventions. Throughout this blog article, we have examined 25 essay topics for each of the following therapeutic modalities: Cognitive Behavioral Therapy (CBT), Psychoanalysis, Family Therapy, Group Therapy, Art Therapy, Mindfulness-Based Therapy, Gestalt Therapy, Solution-Focused Brief Therapy (SFBT), Trauma-Informed Therapy, and Dialectical Behavior Therapy (DBT).
By delving into these diverse essay topics, we have gained valuable insights into the theoretical foundations, interventions, and practical applications of each therapeutic modality. From exploring the cognitive restructuring techniques in CBT to understanding the role of the therapeutic relationship in psychoanalysis, and from examining the dynamics of family systems in Family Therapy to unraveling the creative potential of Art Therapy, each therapeutic approach offers its unique perspective on supporting individuals and facilitating personal growth.
We have explored the wide range of topics related to group dynamics in Group Therapy, the cultivation of mindfulness in Mindfulness-Based Therapy, the holistic approach of Gestalt Therapy, the goal-oriented interventions of Solution-Focused Brief Therapy (SFBT), the trauma-informed care in Trauma-Informed Therapy, and the integration of acceptance and change in Dialectical Behavior Therapy (DBT).
By engaging with these essay topics, we have deepened our understanding of the multifaceted field of psychotherapy, its diverse approaches, and the array of issues that can be explored within each modality. Whether you are a student, a professional, or simply curious about therapy, we hope that these essay topics have sparked your interest and provided you with inspiration for further exploration and research.
Remember, the field of therapy is ever-evolving, and there is always more to learn and discover. So, continue your journey of knowledge and exploration, and may these essay topics serve as a stepping stone toward a deeper understanding of the transformative power of therapy in the lives of individuals and communities.
Our Services

Find anything you save across the site in your account
The Rise of Therapy-Speak

First, let’s survey the situation. It’s as though the haze of our inner lives were being filtered through a screen of therapy work sheets. If we are especially online, or roaming the worlds of friendship, wellness, activism, or romance, we must consider when we are centering ourselves or setting boundaries, sitting with our discomfort or being present. We “just want to name” a dynamic. We joke about our coping mechanisms, codependent relationships, and avoidant attachment styles. We practice self-care and shun “toxic” acquaintances. We project and decathect; we are triggered, we say wryly, adding that we dislike the word; we catastrophize, ruminate, press on the wound, process. We feel seen and we feel heard, or we feel unseen and we feel unheard, or we feel heard but not listened to , not actively. We diagnose and receive diagnoses: O.C.D., A.D.H.D., generalized anxiety disorder, depression. We’re enmeshed, fragile. Our emotional labor is grinding us down. We’re doing the work. We need to do the work .
Around every corner, trauma, like the unwanted prize at the bottom of a cereal box. The trauma of puberty, of difference, of academia, of women’s clothing. When I asked Twitter whether the word’s mainstreaming was productive, I was struck by two replies. First, overapplying the term might dilute its meaning, robbing “people who have experienced legitimate trauma of language that is already oftentimes too thin.” And, second, invoking “trauma” where “harm” might suffice could play into the hands of “people who despise and fear vulnerability.” During this exchange, Twitter served me an advertisement that urged me to “understand my trauma” by purchasing a yoga membership. Ridiculous, I thought. I’m not a sexual-assault survivor. I’ve never been to a war zone. But, countered my brain, after four years of Trump and four seasons of COVID , are you not hurting? The earth is dying. Your mother issues! Your daddy issues! A clammy wave engulfed me. My cursor hovered over the banner.
Perhaps the language of mental health is burgeoning because actual mental health is declining. According to one report , nineteen per cent of adults experienced a mental illness between 2017 and 2018, an increase of 1.5 million people from the previous year. COVID -19 has correlated with soaring rates of depression and anxiety, especially among young people. (In one study, conducted last September, more than half of eleven-to-seventeen-year-olds in a screening of 1.5 million said that they’d thought about suicide or self-harm “nearly every day” for the past two weeks.) A growing awareness of mental illness may be prodding these numbers even higher, although our everyday lexicon still lags behind the science. “We live in a lonely country,” Darby Saxbe , an associate professor of psychology at the University of Southern California, told me. “There’s a lot of genuine distress.”
Yet that may not be the full story. As Saxbe pointed out, the language of the therapist’s office has long flooded popular culture: terms like “hysteria,” “shell shock,” and one’s “inner child” all reflected the psychoanalytic approaches of their day. Freud, in particular, showered Western letters with now common phrases: repression, death wish, slip of the tongue, denial, transference. And the new stuff, too, is still pretty Freudian. It conjures not so much behavioral or cognitive modes of counselling—which might, for instance, inspire influencers to post about the interplay of their thoughts, feelings, environments, and actions—as it does a “kind of modern confessional,” Saxbe said. This language, with its sensitivity to trauma and abuse, seems aimed at “revealing the truth of a difficult experience.” It refreshes Freud’s emphasis on self-disclosure—itself a refreshment of an older religious impulse, a hunger for connection and absolution.
But if the make of the therapeutic chassis hasn’t changed, the past few years have driven it somewhere new. Therapy-speak’s expressive and confessional qualities implicate Freud, and yet its aim, its attention to grounding behavior in care and respect, suggests a rival influence: the psychoanalyst D. W. Winnicott, who was known for his gentle portraits of early childhood. Consider “holding space,” a standout in the new vernacular. The words often appear as a verb phrase, which the Gender and Sexuality Therapy Center defines as “putting your focus on someone to support them as they feel their feelings.” (This, in turn, can be tweaked to “holding” or “holding feelings.”) But the concept of the holding space, or the holding “environment,” grew out of Winnicott’s writings in the nineteen-fifties and sixties, when he broke from his peers at the British Psychoanalytical Society. While his colleagues were bent on studying the fallout of repressed yearning, Winnicott cast back to his patients’ pre-Oedipal beginnings, training his eye on the elemental processes that buttress the self.
In the holding space, the “good enough mother” interacts with her baby, mirroring and sheltering its tender sense of identity. Revealingly, contemporary therapy-speak imagines this dynamic everywhere. Winnicott argued that our ego is shaped in a web of met and unmet needs. The infant discovers that he is a self, an I, when his ordinary devoted mother, over the course of responding to his cries, cannot satisfy every yearning. The ensuing frustration drives home for the child that he and his parent are two, not one—and yet, in a healthy environment, the child figures out how to “go on being.” Therapy-speak, with its first-person narratives of pain, assumes a similar link between vulnerability and identity. Its confessional aspect doubles as an affirmation of humanness, which is always both empowered and frail.
But confession can also become a class performance. (Think of Woody Allen’s Manhattanites, talking endlessly about their shrinks.) In the United States, basic mental-health care remains a luxury item; there’s a reason that the most fluent speakers of the trending argot tend to be wealthy and white. This may explain some of the irritation that therapy-speak occasionally provokes: the words suggest a sort of woke posturing, a theatrical deference to norms of kindness, and they also show how the language of suffering often finds its way into the mouths of those who suffer least. In 2019, for instance, a much-mocked Twitter thread offered a template for turning down a friend’s request for help. “Hey! I’m so glad you reached out,” it read . “I’m actually at capacity/helping someone else who’s in crisis/dealing with some personal stuff right now, and I don’t think I can hold appropriate space for you. Could we connect [later date or time] instead/Do you have someone else you could reach out to?” The technical vocabulary, the holding (or not) of appropriate space, did read as slightly unfeeling, but people seemed more annoyed at such a strenuous attempt to avoid a sad pal.
For Lori Gottlieb, the author of the book “ Maybe You Should Talk to Someone ,” the downsides of casual therapy-speak are more straightforward. “I want to be clear that there’s no reason why people who are not professional psychologists should be expected to use these terms correctly,” she told me. “But there’s a lot of inaccuracy.” Error can be introduced via colloquialism—“O.C.D.” for “organized”—or the actual misconstrual of a word’s meaning. (Someone mistaking “conflict” for “abuse” or labelling you a “gaslighter” because you’ve expressed an opinion that they don’t agree with.) As philosophers from Michel Foucault to Peter Conrad have observed, medical vocabulary lifts up the speaker—claiming that your intrusive neighbor has “borderline personality disorder” cloaks you in authority while pathologizing him. Using these words as bludgeons strips them of complexity; the problem with armchair therapy, or what we now might call “Instagram therapy,” is that it can transform a “deeply relational, nuanced, contextual process,” Gottlieb said, into something “ego-directed, as if the point were always, ‘I’m the most important person and I need to take care of myself.’ ”
Consider boundaries. (Seriously, always do this.) Online and in the letters sent to many a relationship-advice column or podcast, boundary drawing is often invoked to mean cutting people off. “But when we talk about boundaries in therapy,” Gottlieb explained, “it’s something that is really reflected upon and not extreme, and it’s all about interrelationality.” That crude/subtle contrast, Gottlieb said, plays out more broadly between the “idiot compassion” of social media—blind agreement with whatever your friend does—and the “wise compassion” of the psychologist’s office, the effort to help a patient see herself anew. Unquestioning validation “can feel wonderful in the moment,” Gottlieb added, “but it’s not useful to you in the long term.”
Saxbe voiced a similar concern about the appropriation of “triggers,” a concept that is intertwined with the clinical treatment for P.T.S.D., and “spoons,” which arises from the disability-advocacy community. (A spoon is like a unit of energy that you can spend on routine tasks; once you’ve used up your daily allotment, it’s hard to function.) “The most empirically validated approaches would have the patient slowly gaining mastery over her discomfort through exposure, whereas the popular understanding is much more about avoidance,” Saxbe said. In a clinical setting, in other words, the focus falls on interacting with the world—on “developing approach behaviors,” or building routines that pair challenging activities with rewards. But, online, protesting that you’re out of spoons can give you permission to hide from the world, and a trigger warning can seem less an opportunity than a hazard sign: keep away .
One concern that I expected to hear was that the mass adoption of psychological speech might disserve people with severe mental illness. Wasn’t it disrespectful to toss around terms—trauma, depression—that can imply so much suffering? Where was the line between unravelling a taboo and draining a word of its value? The psychologists I spoke to surprised me: steeped in a counter-history of silence about and vilification of mental illness, they could not bring themselves, it seemed, to worry about this particular aspect of therapy-speak’s rise. Gottlieb, pointing to a cottage industry of drinking memes on social media, noted that most of us are still more likely to minimize mental-health challenges (including addiction) than to exaggerate them. And although Saxbe allowed that “there’s a danger of pathologizing and over-treating,” she found both modes preferable to fear and shame. Nor is the seam between “real” conditions and invented ones as conspicuous as some might believe. For more than a century, American culture has embraced a biomedical model of misery; we source bad feelings to chemical imbalances in the brain. But that emphasis “hasn’t actually been well supported by the data,” Saxbe told me. “There’s a lot of evidence that mental health is also related to social connection and having a sense of purpose.”
It only makes sense, then, that the language of psychology has seeped into the rest of our lives; psychology itself is entwined with the rest of our lives. Our emotions are social as well as neural phenomena—their expression can be gendered, racialized—and how we talk about them prefigures both what we want for ourselves and for others. (Hurt people hurt people, as a cohort of psychoanalysts would have it.) If I was once suspicious of the language budding across my social-media feeds, lamenting its expansion now feels like making a claim about who, exactly, “mental health” is for and what we’d like it to do. We could say that it’s for individuals who struggle with its opposite—but, in that case, the language of healing will always be a language of difference. And if we say that it’s for those who have traditionally spoken of such things, we restrict well-being to a milieu that can afford it.
Such border patrolling may be obsolete, anyway. Therapy seems to have absorbed not just our language but our idea of the good life; its framework of fulfillment and reciprocity, compassion and care, increasingly drives our vision for society. Writing this piece, I thought especially of the Greek concept of eudaimonia, or human flourishing. Some might call it blessedness. In any case, it seems worth talking about.

- Counselor Resources
- Benefits of National Certification
- Earn Continuing Education
- Certification Management
- Credentialing Gateway
- Marketing Yourself
- Therapy Directory
- Digital Badges
- The Professional Counselor
- Liability Insurance
- CCE Academy
- CE Credit Verification PDF
Essays on the Importance of . . . in Psychotherapy and Counseling
- essays-on-the-importance-of-in-psychotherapy-and-counseling
Article Published: 11/11/2020
The following is a series of three short essays on the importance of various aspects of doing psychotherapy and counseling. I received my counseling degree in 1978, and I have a small private practice specializing in very brief therapy (mostly single-session), generally using hypnosis based on the work of Milton H. Erickson. I have published 11 books in this field and written many articles, and I have provided workshops, trainings, and presentations in the United States and abroad.
On the Importance of Inclusivity
Clients come to see us because they are stuck; that is, they know only one interpretation for a particular stimulus in their life and that interpretation leads to one response. Although this is a rather simplistic model of psychotherapy, it seems to fit the facts. This means that our main task as therapists is to help clients discover choices in interpretation and choices in responses. Then, they are not stuck!
Also, both we and our clients tend to think about what is troubling them in an either/or fashion. They are depressed, panicked, anxious, obsessive, sad, grieving, unhappy, desperate, blocked, and limited OR they are not. O’Hanlon (2003) found a fascinating way to deal with this stuck state of affairs. He calls it inclusivity , which gets into the realm of both/and . This is oxymoronic technique, using confusion or scrambling of meaning, and is best illustrated by the following statements, generally prefaced by “I wonder how it would feel to be . . .”
- happily depressed/depressedly happy
- compulsively spontaneous/spontaneously compulsive
- obsessively casual/casually obsessive
- sadly delighted/delightedly or happily sad
- desperately free/freely desperate
- actively blocked/blocked actively
- grievingly full of warm memories/warmly grieving
- calmly panicked/panicky calm
- anxiously at peace/ peacefully or calmly anxious
- stressedly calm/calmly stressed
- openly protective/protectively open
- freely dependent/dependently free
Please note that these are all oxymorons, like a “down escalator” or “jumbo shrimp.”
Recently, in the support group I facilitate, one of the members was talking about being depressed. This was first normalized by another group member talking about how depressed she had been and how she is still occasionally depressed about having cancer. I pointed out that almost everyone I know who has been diagnosed with a life-challenging disease goes through depression at one time or another. Then, I said, “I wonder what it would be like to be happily depressed?” The confusion that appeared in his face was a wonder to behold. Others in the group got the idea and added many both/and comments. (I leave this to your imagination.) He began to smile with the novelty of these new ideas. How could he be depressedly alive and active? What would it be like to be energetically slothful?
Inclusive statements scramble thinking and provide interesting choices for what had hitherto been restricted. I hope thinking more about the transformation involved in going from either/or to both/and will provide you with choices in your own life and also choices for your clients. You might even become effectively ineffective, for example! On the Importance of Expectation in Hypnosis and Psychotherapy
Expectation is considered the basis of the placebo effect in both medicine and psychotherapy. Expectation involves hope and anticipation and wishing.
In the beginning, psychoanalysis and psychodynamic approaches were structured for long-term involvement with a client, frequently going on for many years. As psychotherapy developed, the expectation was for fewer and fewer sessions. We now have brief therapy and very brief therapy and single-session therapy. Hoyt (2009) gives an excellent history of brief therapy, along with a scholarly based introduction to the subject. In my practice, I function as a very brief therapist, rarely seeing clients more than one or two times (more if they request). Let me relate how I arrived at this way of working.
I heard the late Steve de Shazer describe a research project carried out at the Brief Family Therapy Center in Milwaukee. Clients were randomly told at intake that their particular presenting problem usually took five or 10 sessions with a therapist. The therapists did not know about this. At follow-up, it was found that the clients who were told 10 sessions began to do “serious” work in their eighth or ninth session, and the clients who were told five sessions did this generally in the fourth session. Having spent most of my life as an academic scientist, I did a simple extrapolation and wondered what would happen if a client were told that their concerns could be resolved to their satisfaction in one session (two if really needed). So I began telling clients that I worked as a very brief therapist who rarely saw clients more than one or two times. My expectation was one or two sessions, and this turned out to be the case with most of my clients. The late Kay Thompson (2004), one of Erickson’s best students, was fond of saying something like, “If you do not believe in what you are doing, then why should the client?” I believe. It also undoubtedly helps that my sessions are always open-ended with respect to time. (I believe that the record for this is Erickson’s 17-hour session—my record is about three hours.)
Because I have written a book about how I work in this mode (Battino, 2006), I will just mention a few of the things that I do here.
- Solution-Focused Brief Therapy (SFBT) – A session frequently involves some use of the SFBT m iracle question , with its expectation that the client will create in their post-miracle thinking such realistic and appealing life changes that they cannot help but incorporate these changes into their lives. The trick, if you will, is to get the client to provide as much detail as you can elicit for their post-miracle life. Connected with this is suggesting a number of ways they can act as if their life has changed in a particularly desirable way.
- Narrative Therapy – When a client is stuck (why they come to see you), they feel as if they cannot act differently (i.e., they are being controlled in some way by internal forces). Externalization is then used to suggest to the client that the controlling power/entity can be resisted and overcome and even “exorcized.” Although describing the externalization process as an exorcism may appear to be strange, my clients liked this description, and we then work out ways for this to happen. When and how have they successfully resisted or overcome this internal demon? Usually, this work is done in the hypnosis segment of the session, but it can be done directly.
- Gestalt Therapy, Two-Chair Technique – With a surprising number of clients, the Gestalt therapy two-chair procedure is just the correct thing to do. This is the case with polarities within the client and with conflicts with parents or other relatives or people. When a client really gets into switching roles, they are usually in some level of trance.
- Reframing – Suggesting a different meaning to an event, feeling, or experience can be revolutionary. Being stuck means interpreting what is happening in one’s life in only one way. Reframing provides alternate meanings and allows the client to view their life from a changed perspective. Thinking of behaviors in different contexts is also a reframing. To perceive one’s self differently is change that is lasting.
- Stories – Telling stories and building metaphors that contain alternative ways of being and thinking allow the client to discover new ways of living and acting. I tell lots of stories, many of them personal.
- Hypnosis for Consolidation – It is generally accepted that people are more receptive to suggestions while they are in a trance state. The hypnosis segment of a session usually occurs at the end and is used to consolidate and repeat the various themes that have emerged during the session. New suggestions are introduced and woven into the tapestry of the session. The client’s inner mind can then pick and choose what makes the most sense for them. Many relevant possibilities are introduced here.
Milton H. Erickson was an artist in structuring a session with a client so that various expectations were “seeded” at the beginning of the session and then utilized at later, appropriate times. People anticipate change in various ways. Anticipating going to a hospital for surgery can be scary in terms of the procedure or it can be hopeful in terms of the expected outcome. When I got a full knee replacement, I did not look forward to the surgery or the long rehab period, but I certainly looked forward to being able to walk and hike comfortably. Which aspect do you focus on? When you focus on the hopeful and positive aspects of change, the negative aspects dim and blur and can be quickly forgotten or overlooked. When hoped-for change is seeded, then it is more likely to occur. The placebo effect is about anticipating positive change, healing, and health. The literature shows it to be remarkably effective. That is why my expectation is that therapy will proceed rapidly and effectively.
Expect happiness, health, joy, and the probability of rapid change. On the Importance of Concerns (vs. Problems) in Hypnosis and Psychotherapy
The development of solution-focused brief therapy (SFBT) by Steve de Shazer and colleagues was a paradigmatic 180-degree shift from the problem-focused therapy that was based initially on the medical model. Yet even with SFBT, the work is still about the “problems” that the clients present. The conversation with the client is about the solutions they have attempted and the solutions that they can attempt. If you ask clients to tell you about their problems, they will do so, and almost ad infinitum . If you ask them what has changed in their life recently that they would like to continue, what has worked for them, and what works for them from time to time, they will tell you that. The emphasis is on solution talk and not problem talk. Stating this another way, the emphasis is not on the organic medical “disease” model but a mental model in which the client has gotten stuck in ways of thinking and behaving that they would like to change.
I have a problem with clients having problems that need solutions. (This is too mathematical!) I prefer thinking about clients being concerned about their thoughts and behaviors (i.e., there are things in their lives that bother them). A concern is of a lesser magnitude than a problem. Problems are serious, and concerns are troubling. Concerns are more easily remedied. I like to think of my clients (and this is my personal belief) as being temporarily troubled . In fact, that is the only diagnosis I am willing to give: being temporarily troubled.
You may think that I am playing games with words here, and I am. Yet in talk therapy, the words we use are the essence of the treatment, the nature of the interaction, and the change agent. Going from a problem to a concern to being temporarily troubled is a major reframe. And reframing is the linguistic mind-changing mechanism of choice for second-order change. Watzlawick et al. (1974) wrote about reframing as the central approach to second-order change, or really changing the system. The goal of therapy is to get the client to do something different, and this occurs via thinking and believing differently about their life and circumstance. They are stuck because they typically have only one way of interpreting or viewing their lives, and this typically leads to only one response. Change comes from changing perspective.
I am simply urging a small change from problem to concern and suggesting that you think about using the diagnosis (if needed) of temporarily troubled .
Battino, R. (2006). Expectation: The very brief therapy book . Crown House Publishing Ltd.
Hoyt, M. F. (2009). Brief psychotherapies. Principles & practices . Zeig, Tucker & Theisen Inc.
O’Hanlon. B. (2003). A guide to inclusive therapy: 26 methods of respectful resistance-dissolving therapy . W.W. Norton and Company.
Thompson, K. F. (2004). The art of therapeutic communication. The collected works of Kay F. Thompson . Crown House Publishing Ltd.
Watzlawick, P., Weakland, J., & Fisch, R. (1974). Change: Principles of problem formation and problem resolution . W.W. Norton & Company.
For more information about my work, please visit rubinbattino.com .
**Opinions and thoughts expressed in our Counseling Confab articles belong to the authors and do not necessarily reflect the opinions or practices of NBCC and Affiliates.
Share On Social Media:
Copyright ©2024 National Board for Certified Counselors, Inc. and Affiliates | All rights reserved.
Existential Therapy Meaning and Principles Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Despite its long history, existential psychotherapy has remained on the fringes of mainstream practice. This is unfortunate because the therapy could be useful in a society that, some argue, is becoming more existentially minded. One reason for its limited acceptance is that the literature to date has tended to be quite convoluted, and the existential psychotherapists’ ideas heterogeneous. Another reason for its limited acceptance is the dearth of empirical validation studies. Again, I think the lack of clear definition and cohesiveness makes it difficult to evaluate the therapy quantitatively (Cooper, 2003).
The type of existential psychotherapy to be developed revolves around the issue of purposelessness. The concept is more tangible and amenable to quantitative evaluation than other existential foci (e.g. scales are available to evaluate purpose in life). As a result, it is more feasible to develop this existential domain into a manualized model that can be rigorously evaluated. One argument against focusing on purpose-centered existential psychotherapy is that historically it has tended to impose value judgments on its clients. Purpose-centered existential psychotherapists may, for example, suggest to clients that there is one ultimate meaning or that only certain types of “higher” activities are legitimate sources of purpose.
Experiential therapy seems to be relatively free of the common problems associated with differences between the client and the therapist. These include such dimensions as gender, age, body size, skin color, physical state, sexual preferences, religious beliefs, and cultural background. “Physical state” may include health conditions such as paraplegia, being blind, being in a wheelchair, or having cancer. (Mahrer, 1997)
The Existential Psychotherapy theory is most appropriately narrated as a “movement wanting to know to the best level probable the survival of the patient in the world in which he lives, moves, and experiences” (May, R. 1983). According to May, the purpose of this approach is to understand human existence, not a system of “how-to” (p.43) and his objective “to understand the life history of a patient as modifications if his being-in-the-world, not as the idiosyncratic pathology of specific theory” (May, R. 1983, p.40, 151).
The ability of the therapist to be aware and knowledgeable to incorporate the right elements of the patient’s ethnic and cultural background will improve therapeutic results and will make possible a more appropriate intervention strategy that will match with the patient’s cultural values.
But it does not matter how our therapy techniques evolve, the important thing we should remember is that as therapists we need to focus on how our patient’s process, store, and use the information and how this information influences what they attend to, perceive, learn, remember, believe and feel and how those feeling are then decoded based on their ethnic and cultural background, their age, gender, and past experiences so we can attempt to understand the cultural influences on identity development, the barriers that affect multicultural counseling and develop culturally appropriate intervention strategies for our patients.
The goal of therapy is to allow the patient to experience his way of life as real while becoming aware of his potentialities and becoming able to act on the basis of his own discoveries (May, R.2005). “As the patient gains insight and knowledge about himself he will then make appropriate decisions.” (May, R.2005) One thing is certain, ethnic background combined with culture will have an intense effect on attitudes, emotions; behaviors, and that failure to consider ethnicity can be an obstacle to an effective treatment. Related concepts that will also have an effect include multicultural therapy and culturally competent psychotherapy (Pope-Davis, 1997). Ethnicity and culture will “influence in the therapeutic relationship and will shape the nature of the interaction between the therapist and patient” (Wong, 2005).
In Viktor Frankl’s existential psychotherapy, the therapist is not a co-creator of reality. The therapist is, instead, a co-explorer who helps the client discover the reality of the meanings and meaning potentials that call to the client for their discovery, actualization, and re-collection as a way to “shrink” the existential-meaning vacuum (Frankl, 1955; Lantz and Gregoire, 2000). Frankl’s ideas about time and reality suggest that the function of the therapist is to induce a phenomenological struggle in the life of the client that will help the client “notice” the meaning potentials in the future, “actualize” such meaning potentials in the “here and now” and remember, re-collect and “honor” those meaning potentials previously actualized and deposited into the forever of the past
Rogers would describe his kind of therapy as a process of freeing a person and removing any obstacles that would inhibit them, in hopes that normal growth and development can advance and the client can become independent and self-sufficient. (Richard, 1975) Certain conditions are necessary for this process to become successful. A growth-promoting environment requires the therapist to be congruent, have unconditional positive regard for the client, as well as show empathic understanding. It is necessary during therapy for the therapist to try to be completely congruent, meaning absolutely genuine no matter neither what their own beliefs are nor what the client’s case is at hand.
Another condition that is necessary is having accurate empathy, which refers to understanding the client’s feelings and personal meanings as they are experienced and communicated back and forth. Most importantly, as Rogers sees it is having unconditional positive regard at all times. This “unconditional positive regard involves relating from therapist to client, not as a scientist to an object of study, but as a person to a person. He feels this client be a person of self-worth; of value no matter what his condition, his behavior, or his feelings. He respects him for what he is and accepts him as he is, with his potentialities (Rogers, 1965, Pescitelli, 1996).
The client can then feel accepted, not feel judged, whereas this tends to reduce the need to defend his self-concept and begin to accept and value himself. In order for the client to be able to accept experiences that have been distorted or denied to their own awareness, there must be a decrease in the client’s conditions of worth and an increase in the client’s unconditional self-regard. If the therapist can demonstrate unconditional positive regard for the client, then the client can begin to become accurately aware of experiences that had been previously distorted or denied because they experienced a loss of positive regard from significant others.
These “significant others” most times are the client’s parents, teachers, bosses, someone that is seen to have some control over the client. When a client perceives unconditional positive regard, their existing conditions of low worth are weakened and are soon replaced by a stronger unconditional positive self-regard. Existential Psychotherapy is a form that aims to enhance self-knowledge in the client and allows them to be the sole person responsible for their own lives and choices.
Cardemil, E. & Battle, C. L., 2003. (Brown University and Butler Hospital) Professional Psychology: Research and Practice American Psychological Association, Inc. Vol. 34, No. 3.
Carl Rogers. On Becoming a Person: A Therapist’s View of Psychotherapy: Boston: Houghton Mifflin, 1965.
Cooper, M. (2003). Existential Therapies: London: Sage Publications.
Frankl, V. (1955). The doctor and the soul. New York: Vintage.
Lantz, J., & Gregoire, T. (2000). Existential psychotherapy with Vietnam veteran couples: A twenty-five year report. Contemporary Family Therapy, 22, 19-37.
Mahrer, A. R. (1997). Experiential psychotherapy: An unabashedly biased comparison with some other psychotherapies. In C. Feltham (Ed.), Which psychotherapy? Leading exponents explain their differences (pp. 119–148). London: Sage.
May, Rollo. (1983). The discovery of being: Writings in existential psychology. New York: Norton.
May, Rollo: The Meaning of Anxiety: 2005: W. W. Norton & Company; Revised edition.
Pope-Davis, D. B. & Coleman, H. L. K., 1997: Multicultural counseling competencies: Thousand Oaks, CA.
Richard I. Evans. Carl Rogers: The Man and His Ideas. Vol. 8 of Notable Contributors to Personality Theory: New York: E. P. Dutton, 1975.
Schaeffer, F., 1968: The God Who is There. Published by Inter Varsity Press (U.S.A. and Canada).
Wong, P.S., 2005. The inscrutable Dr.Wu. In C. Muran (Ed.) Dialogues in Difference: Diversity Studies of the Therapeutic Relationship. APA Books.
- The Techniques of Psychodrama
- Stress: Causes, Sources and Symptoms
- Existential Theory and Therapy
- Psychology. Existential and Person-Centered Theories
- Rural Community Development and its Potentials
- Organizational Psychology: Communities of Commitment
- Stress of Police Officers and How They Cope With It
- The Scholastic Aptitude Test Assessment and Test
- Teamwork, Team Dynamics and Communication
- Depression: Risk Factors, Incidence, Preventive Measures & Prognostic Factors
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, October 13). Existential Therapy Meaning and Principles. https://ivypanda.com/essays/existential-psychotherapy/
"Existential Therapy Meaning and Principles." IvyPanda , 13 Oct. 2021, ivypanda.com/essays/existential-psychotherapy/.
IvyPanda . (2021) 'Existential Therapy Meaning and Principles'. 13 October.
IvyPanda . 2021. "Existential Therapy Meaning and Principles." October 13, 2021. https://ivypanda.com/essays/existential-psychotherapy/.
1. IvyPanda . "Existential Therapy Meaning and Principles." October 13, 2021. https://ivypanda.com/essays/existential-psychotherapy/.
Bibliography
IvyPanda . "Existential Therapy Meaning and Principles." October 13, 2021. https://ivypanda.com/essays/existential-psychotherapy/.
IvyPanda uses cookies and similar technologies to enhance your experience, enabling functionalities such as:
- Basic site functions
- Ensuring secure, safe transactions
- Secure account login
- Remembering account, browser, and regional preferences
- Remembering privacy and security settings
- Analyzing site traffic and usage
- Personalized search, content, and recommendations
- Displaying relevant, targeted ads on and off IvyPanda
Please refer to IvyPanda's Cookies Policy and Privacy Policy for detailed information.
Certain technologies we use are essential for critical functions such as security and site integrity, account authentication, security and privacy preferences, internal site usage and maintenance data, and ensuring the site operates correctly for browsing and transactions.
Cookies and similar technologies are used to enhance your experience by:
- Remembering general and regional preferences
- Personalizing content, search, recommendations, and offers
Some functions, such as personalized recommendations, account preferences, or localization, may not work correctly without these technologies. For more details, please refer to IvyPanda's Cookies Policy .
To enable personalized advertising (such as interest-based ads), we may share your data with our marketing and advertising partners using cookies and other technologies. These partners may have their own information collected about you. Turning off the personalized advertising setting won't stop you from seeing IvyPanda ads, but it may make the ads you see less relevant or more repetitive.
Personalized advertising may be considered a "sale" or "sharing" of the information under California and other state privacy laws, and you may have the right to opt out. Turning off personalized advertising allows you to exercise your right to opt out. Learn more in IvyPanda's Cookies Policy and Privacy Policy .
Home — Essay Samples — Psychology — Cognitive Behavioral Therapy — Cognitive-Behavioral Therapy: Its Meaning, Purpose and Benefits
Cognitive-behavioral Therapy: Its Meaning, Purpose and Benefits
- Categories: Cognitive Behavioral Therapy
About this sample

Words: 1259 |
Published: Jan 4, 2019
Words: 1259 | Pages: 3 | 7 min read

Cite this Essay
To export a reference to this article please select a referencing style below:
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Prof Ernest (PhD)
Verified writer
- Expert in: Psychology

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 1085 words
5 pages / 2423 words
1 pages / 450 words
1 pages / 473 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Cognitive Behavioral Therapy
Alderson P. The importance of theories in health care. Br Med J. 1998; 317(7164):1007-10Alice Theadom, Mark Cropley, Kristy-Louise Humphrey: Journal of Pscyho-somatic Research 62 (2007) 145-151Braun, V. and Clarke, V. (2013) [...]
Religion has been intertwined with therapy for centuries, influencing the way individuals seek treatment and the approach therapists take in addressing their clients' needs. This essay aims to explore the ethical considerations [...]
Overthinking, the art of dwelling on thoughts to the point of obsession, is a mental state that plagues individuals across the globe. In this essay, we embark on a journey to explore the intricacies of overthinking—what it [...]
Effortful processing refers to the cognitive process that requires deliberate, conscious attention and effort to encode information. Unlike automatic processing, which happens subconsciously and without much thought, effortful [...]
There are many people who continue to suffer depression, fear, anger and aggression but are unaware of the simple remedy in Cognitive behavioural therapy (CBT) to the seemingly complicated problems. Cognitive behavioural therapy [...]
Cognitive behavioral therapy relies on the notion that as humans, our thoughts, emotions and behaviors are linked to one another. The aim of cognitive behavioral therapy is to identify the linkages between emotions, thoughts and [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is Group Therapy?
- Effectiveness
- Making the Decision
How to Get Started
Group therapy is a form of psychotherapy that involves one or more therapists working with several people at the same time. This type of therapy is widely available at a variety of locations including private therapeutic practices, hospitals, mental health clinics, and community centers.
Group therapy is sometimes used alone, but it is also commonly integrated into a comprehensive treatment plan that also includes individual therapy.
Types of Group Therapy
Group therapy can be categorized into different types depending on the mental health condition it is intended to treat as well as the clinical method used during the therapy. The most common types of group therapy include:
- Cognitive behavioral groups , which center on identifying and changing inaccurate or distorted thinking patterns , emotional responses, and behaviors
- Interpersonal groups , which focus on interpersonal relationships and social interactions, including how much support you have from others and the impact these relationships have on mental health
- Psychoeducational groups , which focus on educating clients about their disorders and ways of coping; often based on the principles of cognitive behavior therapy (CBT)
- Skills development groups , which focus on improving social skills in people with mental disorders or developmental disabilities
- Support groups , which provide a wide range of benefits for people with a variety of mental health conditions as well as their loved ones
Groups can be as small as three or four, but group therapy sessions often involve around eight to 12 people (although it is possible to have more participants). The group typically meets once or twice each week, or more, for an hour or two.
Group therapy meetings may either be open or closed. New participants are welcome to join open sessions at any time. Only a core group of members are invited to participate in closed sessions.
Group Therapy Techniques
What does a typical group therapy session look like? In many cases, the group will meet in a room where the chairs are arranged in a large circle so that members can see every other person in the group.
A session might begin with members of the group introducing themselves and sharing why they are in group therapy. Members might also share their experiences and progress since the last meeting.
The precise manner in which the session is conducted, and any group therapy activities, depend largely on the goals of the group and the therapist's style.
Some therapists might encourage a more free-form style of dialogue, where each member participates as they see fit. Other therapists have a specific plan for each session that might include having participants practice new skills with other members of the group.
Group Therapy Activities
Common group therapy activities can include:
- Icebreaker activities that help group members get to know one another
- Gratitude activities, such as mapping different aspects of their life that they are thankful for
- Sharing activities, where group members ask one another questions
- Expressive writing activities to explore experiences and emotions connected to those events
- Goal visualization activities to help people set goals and make a plan to accomplish them
What Group Therapy Can Help With
Group therapy is used to treat a wide variety of conditions, including:
- Attention-deficit/hyperactivity disorder (ADHD)
- Eating disorders
- Generalized anxiety disorder
- Panic disorder
- Post-traumatic stress disorder (PTSD)
- Substance use disorder
In addition to mental health conditions, CBT-based group therapy has been found to help people cope with:
- Anger management
- Chronic pain
- Chronic illness
- Chronic stress
- Domestic violence
- Grief and loss
- Weight management
After analyzing self-reports from people who have been involved in the process, Irvin D. Yalom outlines the key therapeutic principles of group therapy in "The Theory and Practice of Group Psychotherapy."
- Altruism : Group members can share their strengths and help others in the group, which can boost self-esteem and confidence.
- Catharsis : Sharing feelings and experiences with a group of people can help relieve pain, guilt, or stress.
- The corrective recapitulation of the primary family group : The therapy group is much like a family in some ways. Within the group, each member can explore how childhood experiences contributed to personality and behaviors. They can also learn to avoid behaviors that are destructive or unhelpful in real life.
- Development of socialization techniques : The group setting is a great place to practice new behaviors. The setting is safe and supportive, allowing group members to experiment without the fear of failure.
- Existential factors : While working within a group offers support and guidance, group therapy helps members realize that they are responsible for their own lives, actions, and choices.
- Group cohesiveness : Because the group is united in a common goal, members gain a sense of belonging and acceptance.
- Imparting information : Group members can help each other by sharing information.
- Imitative behavior : Individuals can model the behavior of other members of the group or observe and imitate the behavior of the therapist.
- Instills hope : The group contains members at different stages of the treatment process. Seeing people who are coping or recovering gives hope to those at the beginning of the process.
- Interpersonal learning : By interacting with other people and receiving feedback from the group and the therapist, members of the group can gain a greater understanding of themselves.
- Universality : Being part of a group of people who have the same experiences helps people see that what they are going through is universal and that they are not alone.
Benefits of Group Therapy
There are several advantages of group therapy.
Support, Safety and Encouragement
Group therapy allows people to receive the support and encouragement of the other members of the group. People participating in the group can see that others are going through the same thing, which can help them feel less alone. The setting allows people to practice behaviors and actions within the safety and security of the group.
Role Modeling
Group members can serve as role models for other members of the group. By observing someone successfully coping with a problem, other members of the group can see that there is hope for recovery. As each person progresses, they can, in turn, serve as a role model and support figure for others. This can help foster feelings of success and accomplishment.
Insight on Social Skills
By working with a group, the therapist can see first-hand how each person responds to other people and behaves in social situations. Using this information, the therapist can provide valuable feedback to each client.
Affordability
Group therapy is often very affordable. Instead of focusing on just one client at a time, the therapist can devote their time to a much larger group of people, which reduces the cost for participants.
While costs vary depending on a variety of factors, estimates suggest that group therapy costs, on average, one-half to one-third less than individual therapy.
Effectiveness of Group Therapy
Group therapy can be effective for depression. In a study published in 2014, researchers analyzed what happened when individuals with depression received group cognitive behavioral therapy (CBT). They found that 44% of the patients reported significant improvements. The dropout rate for group treatment was high, however, as almost one in five patients quit treatment.
An article published in the American Psychological Association's Monitor on Psychology suggests that group therapy also meets efficacy standards established by the Society of Clinical Psychology (Division 12 of the APA) for the following conditions:
- Bipolar disorder
- Obsessive-compulsive disorder (OCD)
- Social phobia
Is Group Therapy for You?
If you or someone you love is thinking about group therapy, there are several things you should consider.
You Need to Be Willing to Share
Especially if you struggle with social anxiety or phobias, sharing in a group might not be right for you. In addition, some types of group therapy involve exercises like role-playing and intense personal discussion, which can be overwhelming for people who are extremely private or uncomfortable around strangers.
You May Need to Try a Few Groups
Just like you might need to shop around to find the right therapist, you may also need to try a few groups before you find the one that fits you best. Think a little about what you want and need, and consider what might be most comfortable or the best match for you.
It’s Not Meant for Crisis
There are limitations to group therapy and not all people are good candidates. If you or someone you love is in crisis or having suicidal thoughts, individual therapy is a better choice than group therapy. In general, group settings are best for individuals who are not currently in crisis.
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
If you feel that you or someone you love might benefit from group therapy, begin with the following steps:
- Consult with a physician for a recommendation of the best type of group therapy for your condition.
- Consider your personal preferences , including whether an open or closed group therapy session is right for you. You may also choose to explore group therapy online .
- Contact your health insurance to see if they cover group therapy, and if so, how many sessions they cover per year.
Before joining, think about whether you want to participate in an open or closed group. If you would prefer an open group, you can likely join in at any time. For closed groups, you will likely have to wait until a new session begins.
It is also important to consider whether group therapy will be sufficient on its own or if you need additional assistance in the form of individual and/or medication. Talk to your doctor or therapist to decide what treatment approach is right for your needs.
Ezhumalai S, Muralidhar D, Dhanasekarapandian R, Nikketha BS. Group interventions . Indian J Psychiatry . 2018;60(Suppl 4):S514–S521. doi:10.4103/psychiatry.IndianJPsychiatry_42_18
McDermut W, Miller IW, Brown RA. The efficacy of group psychotherapy for depression: A meta-analysis and review of the empirical research . Clin Psychol Sci Pract . 2001;8(1):98-116. doi:10.1093/clipsy.8.1.98
Castillo DT, C’de Baca J, Qualls C, Bornovalova MA. Group exposure therapy treatment for post-traumatic stress disorder in female veterans . Mil Med . 2012;177(12):1486-1491. doi:10.7205/milmed-d-12-00186
Lo Coco G, Melchiori F, Oieni V, et al. Group treatment for substance use disorder in adults: A systematic review and meta-analysis of randomized-controlled trials . J Substance Abuse Treat . 2019;99:104-116. doi:10.1016/j.jsat.2019.01.016
Kanas N. Group therapy for patients with chronic trauma–related stress disorders . Int J Group Psychother . 2005;55(1):161-165. doi:10.1521/ijgp.55.1.161.56551
Yalom ID, Leszcz M. Inpatient Group Psychotherapy . Basic Books.
Hartgrove Behavioral Health System. When should you consider group therapy? The answer might surprise you .
Thimm JC, Antonsen L. Effectiveness of cognitive behavioral group therapy for depression in routine practice . BMC Psychiatry . 2014;14:292. doi:10.1186/s12888-014-0292-x
Paturel A. Power in numbers . Monitor on Psychology. American Psychological Association.
American Psychological Association. Psychotherapy: Understanding group therapy .
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Defining Lives: Occupation as Identity: An Essay on Competence, Coherence, and the Creation of Meaning
- November 1999
- American Journal of Occupational Therapy 53(6):547-558
- 53(6):547-558
- This person is not on ResearchGate, or hasn't claimed this research yet.
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Aaron Eakman

- Dakota Handzlik

- Steven Skiena

- Javiera Fredes
- Francisca Rantul
- Anu Raudasoja

- Sanna Heino

- Igor Zavgorodnii
- O. Litovchenko

- Adrienne R. Brown
- SOC SCI MED
- Dana A. Glei
- Casey L. Brown
- Maxine Weinstein
- RES AUTISM SPECT DIS

- Kristin L. Sommer

- T.F. Stillman
- Robert K Bing
- David D. Franks

- Jean Piaget
- Erving E. Goffman

- Kenneth J. Gergen
- Tech Disabil

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Lucy May Need Therapy
Lucy’s obsession with Faith borders on stalking. There’s some underlying issues that makes her want to drink and misbehave. I can see if her parents were still separated, but they’re not. Also, there was a time when Y&R had more cast members who were Lucy’s age. There were even s/l’s that involved their lives at Walnut Grove. Lucy could and should make friends at her school.
Ya think? She’s going to turn out to be just as looney as her bio-Mom.
I’m not too thrilled with yet another mental illness storyline. Lucy has a behavioural problem and shouldn’t have to see a therapist at this point in time. That stigma could make matters worse for her and make her feel abnormal. Kids can be cruel.
Not all obsessive types or mentally ill. I am wondering if they will go with a lesbian storyline. Her fixation on faith doesn’t seem straight.
That’s totally how it feels, but I think the producers won’t ever actually come out and say it onscreen.
Look at how they handle Mariah and Tessa.
Nah, i think its more that Lucy would like to be like Faith who she admires and looks up to. I dont see any sexual attraction there.
Sharon needs therapy… a grown adult who is a therapist yelling and screaming at a child… for something her daughter did… Cassie died because of her stalking Daniel… and now Sharon is blaming everyone else… she is unhinged.
If they took the word “unhinged” out of the English language, we would actually have to come up with another similar word to describe faux-polar Sharon. lol. Unhinged makes me think of a door that gets ripped violently off in a tornado.
Unbalanced? disturbed? off her rocker??
I do think that Lucy needs therapy. She has the genes of Sheila, Daisy, & Phyllis & it is starting to get bad.
I agree. I think that Lucy looks up to Faith and as you said, admires her. Faith is older than Lucy so I think that’s why she is going overboard.
Well, it’s a healthy variety. Unhinged was becoming a cliche. lol
I wish SOMEONE, ANYONE, would take a deep breath after Lucy says “what’s the big deal?!” and simply ask her…“What’s the big deal about being Faith’s friend?! What exactly is so great about Faith? Where is this huge connection you feel you share with her?” Just to make her think for a minute how desperate she comes across.
Yes! I’m also waiting for Daniel & Heather to ask her what exactly is going on as far as getting along with her peers. Is she being bullied? Shunned? Rejected by boys she likes? Hit on too aggressively by boys? Is she dealing with mean/abusive teachers?
The main problem here is that Daniel and Heather are somewhat out of touch with their daughter. She needs discipline and it’s the parents’ responsibility to provide it. They are simply too permissive and dismissive. (And this is totally off-topic but everytime I see your username I want to start singing, “Soft kitty, warm kitty little ball of fur. Happy kitty sleepy kitty, purr purr purr.” lol)
Yes!! Something to get to the root of the issue!!
I love TBBT!!
Plus unmedicated…
It’s a great show. And no mental illnesses, self-harming children or recurring cancer.

IMAGES
VIDEO
COMMENTS
For five to 10 minutes just start writing in a "stream of consciousness.". Start a dialogue with your inner child by writing in your nondominant hand. Cultivate an attitude of gratitude by maintaining a daily list of things you appreciate, including uplifting quotes. Start a journal of self-portraits.
Through psychotherapy, psychologists help people of all ages live happier, healthier, and more productive lives. In psychotherapy, psychologists apply scientifically validated procedures to help people develop healthier, more effective habits. There are several approaches to psychotherapy—including cognitive-behavioral, interpersonal, and ...
The meaning-changing nature of systemic therapy shall be exemplified on the basis of a commonly used method in systematic therapy, the "genogram", ... The will to believe: And other essays in popular philosophy. New York and London: Longmans, Green, and Co. [Google Scholar]
Psychotherapy, also known as talk therapy, refers to techniques that help people change behaviors, thoughts, and emotions that cause problems or distress. It is an umbrella term that describes treating psychological disorders and mental distress through verbal and psychological techniques. During this process, a trained psychotherapist helps ...
Logotherapy is a therapeutic approach that helps people find personal meaning in life. It's a form of psychotherapy that is focused on the future and on our ability to endure hardship and suffering through a search for purpose. Psychiatrist and psychotherapist Viktor Frankl developed logotherapy prior to his deportation to a concentration ...
Psychotherapy is a space for you to talk about how you feel, act, and think with a professionally trained individual who can guide you. Psychotherapy can be a one-on-one experience or one for the ...
Holistic and integrative therapy involves integrating various elements of different theories to the practice. In addition to traditional talk therapy, holistic therapy may include nontraditional therapies such as hypnotherapy or guided imagery. The key is to use the techniques and psychotherapy tools best suited for a particular client and problem.
Logotherapy: A Definition. Logotherapy is often referred to as the "third Viennese school of psychotherapy," and it originated in the 1930s as a response to both Freud's psychoanalysis and Adler's emphasis on power within society.It is more than just "therapy." It is a philosophy for the spiritually lost and an education for those who are confused.
Psychoanalysis is a more intensive form of psychodynamic therapy. Sessions are typically conducted three or more times a week. Supportive therapy uses guidance and encouragement to help patients develop their own resources. It helps build self-esteem, reduce anxiety, strengthen coping mechanisms, and improve social and community functioning.
By contrast, many of the creative writers who I read on the matter were much more leery of the prospect of writing being therapy. This is epitomized by memorist T Kira Madden's Literary Hub essay "Against Catharsis: Writing is Not Therapy," the jist of which states that artistic writing is much too prosaic and difficult to involve the ...
Abstract. Cognitive behavioural therapy (CBT) explores the links between thoughts, emotions and behaviour. It is a directive, time-limited, structured approach used to treat a variety of mental health disorders. It aims to alleviate distress by helping patients to develop more adaptive cognitions and behaviours.
Behavior Therapy. Cognitive Therapy. Humanistic Therapy. Integrative Therapy. Deciding to start therapy is a big, personal step toward prioritizing mental health and improving overall well-being. There are differing types of mental health therapy, from cognitive behavior therapy to play therapy. It can be overwhelming to determine which type is ...
Dialectical behavioral therapy (DBT) is a form of CBT that utilizes both behavioral and cognitive techniques to help people learn to manage their emotions, cope with distress, and improve interpersonal relationships. Exposure therapy utilizes behavioral techniques to help people overcome their fears of situations or objects.
Logotherapy is a form of existential therapy developed by neurologist and psychiatrist Viktor Frankl [1].It is founded on the premise that the primary motivational force of individuals is to find meaning in life. [2] Frankl describes it as "the Third Viennese School of Psychotherapy" [3] [4] along with Freud's psychoanalysis and Alfred Adler's individual psychology.
However, group therapy helps an individual to comprehend their emotions and transform problem behaviours with the help of others (Seikkula, 2019). This essay about counseling can help reveal and understand the prospects for using various techniques in the process of helping clients.
Art Therapy Essay Topics. The therapeutic power of art: Exploring the psychological and emotional benefits of engaging in art-making. The history and evolution of art therapy as a recognized therapeutic modality. The role of the art therapist: Examining the skills, qualities, and ethical considerations involved in practicing art therapy.
Revealingly, contemporary therapy-speak imagines this dynamic everywhere. Winnicott argued that our ego is shaped in a web of met and unmet needs. The infant discovers that he is a self, an I ...
Article Published: 11/11/2020. The following is a series of three short essays on the importance of various aspects of doing psychotherapy and counseling. I received my counseling degree in 1978, and I have a small private practice specializing in very brief therapy (mostly single-session), generally using hypnosis based on the work of Milton H ...
Get a custom essay on Existential Therapy Meaning and Principles. The type of existential psychotherapy to be developed revolves around the issue of purposelessness. The concept is more tangible and amenable to quantitative evaluation than other existential foci (e.g. scales are available to evaluate purpose in life).
There are a few studies that are mentioned within this paper that outline the benefits of cognitive-behavioral therapy. Each study focuses on a group of individuals that greatly benefit from therapy, as well as highlighting the differences between clinicians that are cognitive-behavioral therapists and those who only use cognitive-behavioral techniques.
Group therapy is a form of psychotherapy that involves one or more therapists working with several people at the same time. This type of therapy is widely available at a variety of locations including private therapeutic practices, hospitals, mental health clinics, and community centers. Group therapy is sometimes used alone, but it is also ...
This article presents a view of occupation as the principal means through which people develop and express their personal identities. Based on a review of theory and research, it proposes that identity is instrumental to social life because it provides a context for deriving meaning from daily experiences and interpreting lives over time. The article proposes that identity also provides a ...
Within this framework, it is postulated that performance limitations and disfigurement that sometimes result from illness or injury have identity implications that should be recognized by ...
Lucy's obsession with Faith borders on stalking. There's some underlying issues that makes her want to drink and misbehave. I can see if her parents were still separated, but they're not. Also, there was a time when Y&R had more cast members who were Lucy's age. There were even s/l's that involved their lives at Walnut Grove. Lucy could and should make friends at her school.