- OJIN Homepage
- Table of Contents
- Volume 23 - 2018
- Number 2: May 2018
- Evidence Psychiatric Mental Health Interventions

Evidence for Psychiatric and Mental Health Nursing Interventions: An Update (2011 through 2015)
Dr. Bekhet is an Associate Professor at Marquette University College of Nursing in Milwaukee, WI. She received aBSN and MSN from Alexandria University in Alexandria, Egypt. She received a PhD from Case Western Reserve University (CWRU) in Cleveland, OH. Her clinical experience in psychiatric nursing is with persons having schizophrenia, bipolar disorders, obsessive-compulsive disorders, and depressive disorders. She has taught psychiatric mental health nursing to undergraduate and direct entry students. She has also advised PhD students. Dr. Bekhet’s program of research focuses on the effects of positive cognitions and resourcefulness in overcoming adversity in vulnerable populations. Her research has been funded by Sigma Theta Tau International; American Psychiatric Nursing Foundation; International Society of Psychiatric Mental Health Nurses; and Marquette University. She is a past recipient of a Midwest Nursing Research Society Mentorship Grant Award, and has received the Award for Excellence from the CWRU Nursing Alumni Association in 2011 and the Way-Klinger Young Scholar Award from Marquette University in 2012. More recently, she was awarded the 2014 research award from the International Society of Psychiatric Mental Health Nurses. Dr. Bekhet has published numerous articles and presented numerous papers and posters at regional, national, and international conferences.
Dr. Zauszniewski is the Kate Hanna Harvey Professor in Community Health Nursing, and Director of the PhD in Nursing Program at the Case Western Reserve University (CWRU), Cleveland, OH. She received a PhD and MSN from CWRU, Cleveland, OH; a MA in Counseling and Human Services from John Carroll University, Cleveland, OH; a BA in psychology from Cleveland State University, Cleveland, OH; and a diploma in nursing from St. Alexis Hospital School of Nursing, Cleveland, OH. She has practiced nursing for 42 years, including 33 years in the field of psychiatric-mental health nursing; she has experience as a staff nurse, clinical preceptor, head nurse, supervisor, patient care coordinator, nurse educator, and nurse researcher, and is board certified by the American Nurses Credentialing Center (ANCC). Her program of research focuses on the identification of factors and strategies to prevent depression and to preserve healthy functioning across the lifespan. She is best known for her research examining the development and testing of nursing interventions to teach resourcefulness skills to family caregivers. She has received research funding from the National Institutes of Nursing Research and Aging; the National Institutes of Health; Sigma Theta Tau International; the American Nurses Foundation; Midwest Nursing Research Society; and the State of Ohio Board of Regents.
Denise Matel-Anderson is a doctoral student at Marquette University College of Nursing in Milwaukee, WI. She holds an Advanced Practice Nurse Prescriber license, and is currently working on a PhD in nursing with a focus on mental health. She has three publications in mental health nursing journals. Ms. Matel-Anderson currently lectures at Carroll University, Waukesha, WI, in the undergraduate mental health nursing theory course, and serves as a nurse practitioner on the medical team at an acute mental health facility.
Jane Suresky is an Adjunct Assistant Professor at the Frances Payne Bolton School of Nursing of Case Western Reserve University (CWRU) in Cleveland, OH. She has received DNP and MSN degrees from CWRU, and a BSN degree from Cleveland State University, Cleveland, OH. Her clinical experience in psychiatric nursing covers the areas of psychobiological research, adolescent dual diagnosis, and mood disorders. She has taught psychiatric mental health nursing to undergraduate and graduate students. In addition, she has been involved in nursing research that focuses on the stress of the female family members of the severely mentally ill.
Mallory Stonehouse recently graduated with a Master of Science in Nursing degree from Marquette University in Milwaukee, WI, where she completed the adult-older adult, primary care, nurse practitioner program. She is a registered nurse at Froedtert Community Memorial Hospital in Wisconsin, where she works on the Behavioral Health Unit. Ms. Stonehouse holds a Bachelor of Arts degree in psychology.
- Figures/Tables
This state-of-the-evidence review summarizes characteristics of intervention studies published from January 2011 through December 2015, in five psychiatric nursing journals. Of the 115 intervention studies, 23 tested interventions for mental health staff, while 92 focused on interventions to promote the well-being of clients. Analysis of published intervention studies revealed 92 intervention studies from 2011 through 2015, compared with 71 from 2006 through 2010, and 77 from 2000 through 2005. This systematic review identified a somewhat lower number of studies from outside the United States; a slightly greater focus on studies of mental health professionals compared with clients; and a continued trend for testing interventions capturing more than one dimension. Though substantial progress has been made through these years, room to grow remains. In this article, the authors discuss the background and significance of tracking the progress of intervention research disseminated within the specialty journals, present the study methods used , share their findings , describe the intervention domains and nature of the studies , discuss their findings , consider the implications of these studies , and conclude that continued track of psychiatric and mental health nursing intervention research is essential.
Key Words: best practices, evidence-based practice, psychiatric nursing journals, psychiatric nursing research, published research, research dissemination, research utilization, systematic review, tradition, intervention research
Implementation science is concerned with the translation of research into practice... The past five years have seen a rapidly growing interest in the field of implementation science ( Sorensen & Kosten, 2011 ). Implementation science is concerned with the translation of research into practice; it involves the examination of the challenges and the opportunities for successful, evidence-based changes in practice ( Nilsen, 2015 ). Translating research into practice depends heavily on the dissemination of findings from intervention research to those most likely to use those findings in clinical or community settings. In contrast to implementation, dissemination involves the spread of information about an intervention, for example, through publication of the intervention in professional journals. Dissemination strategies that are actively targeted toward spreading evidence-based findings concerning an intervention may prompt future implementation in clinical practice ( Proctor et al., 2009 ).
Translating research into practice depends heavily on the dissemination of findings from intervention research... Important for psychiatric and mental health nurses, it is critical that implementation of evidence-based findings occurs across multiple settings (i.e., beyond specialty mental healthcare units) to medical settings, such as primary care areas in which mental health services are provided, and to non-specialized settings, such as criminal justice and school systems and community social service agencies, where mental healthcare is delivered (Proctor et al., 2009). However, before implementation can happen, dissemination of findings from well-designed intervention studies that can inform psychiatric and mental health nursing practice is needed.
One of the best mediums for disseminating evidence-based findings in psychiatric and mental health nursing is the professional nursing journals that are most available to practicing psychiatric and mental health nurses. Nursing journals that are specifically designed a specialty are more likely to be read by persons in the given specialty area than are other nursing research journals. Nurses in practice settings, including those at an advanced practice level, may not have access to scientific research journals or may choose not to read them if the research does not appear meaningful for their practice. The goal of this review was to describe the findings from intervention studies disseminated through publication in one of the five psychiatric and mental health nursing specialty journals published from 2011 through 2015.
Background and Significance
Through the years, more psychiatric and mental health nurse researchers have been targeting specialty journals for disseminating findings from intervention research. For example, in previous reviews of intervention studies published in the five major psychiatric and mental health specialty journals, there was a higher percentage of quantitative intervention studies conducted from 2006 through 2010 (84%) than in a similar review conducted from 2000-2005 (64%) ( Zauszniewski, Suresky, Bekhet, & Kidd, 2007 ; Zauszniewski, Bekhet, & Haberlein, 2012 ), indicating increased use of more rigorous, statistical analytic methods in published intervention research over time ( Zauszniewski et al., 2007 ; Zauszniewski et al., 2012 ).
Tracking the progress of intervention research disseminated within the specialty journals in psychiatric and mental health nursing is important for two reasons. First, it provides data to show improvements in dissemination efforts of psychiatric and mental health nurse researchers. Second, it calls attention to the importance for continued dissemination of intervention research to practicing psychiatric and mental health nurses who are in the best positions to implement the findings in practice. Therefore, the purpose of this review of the same, five, peer-reviewed psychiatric and mental health nursing journals, covering 2011 through 2015, was to determine the number and types of intervention studies within the specified review period. For consistency, the same criteria for selecting the intervention studies that were described in the previous review ( Zauszniewski et al., 2012 ) were applied: A study was determined to be an intervention study if nursing strategies, procedures, or practices were examined for effectiveness in enhancing or promoting health or preventing disability or dysfunction ( Kane, 2015 ).
Five peer-reviewed nursing journals, regarded as the most frequently read in the mental health nursing profession, were analyzed for the years 2011 through 2015. The journals included in the analysis were Archives of Psychiatric Nursing ; Issues in Mental Health Nursing ; Journal of the American Psychiatric Nurses Associatio n; Journal of Psychosocial and Mental Health Services; and Perspectives in Psychiatric Care .
Journals were reviewed for the type of intervention study (qualitative or quantitative); the study domain (biological, psychological, or social); and the number of intervention studies found within the journals. After review, the agreed upon intervention studies were extracted and individually analyzed by the co-authors.
There were 832 databased articles published from January 2011 through December 2015. However, only 115 (14%) evaluated or tested psychiatric nursing interventions. Of these 115 intervention studies, 14 tested interventions with nursing students, nine involved nurses and mental health professionals, while 92 focused on interventions to promote mental health in clients of care.
This section describes the findings from the 115 intervention studies included in the review. The 23 studies that included nursing students, nurses, and mental health professional, and the 92 that involved recipients of mental health services or care are presented in this section. First, the research settings in which the 115 studies were conducted, and descriptions of the targeted populations are described. Next, the 23 studies’ designs, purposes, and findings are discussed in detail. Third, the 92 studies that involved recipients of mental health services or care are presented using the categories of the bio-psycho-social framework. Finally, the type of data (quantitative, qualitative, or mixed) are discussed and presented in the table.
Research Settings Sixty-six of the 115 intervention studies were completed in the United States. Five studies each were done in Australia and United Kingdom. Four each were completed in Korea, China, and Turkey; three each in Norway, Canada, and Iran; and two each in Taiwan, Mexico, Sweden, France, and Netherlands. One study each was conducted in Jordan, Europe, Iceland, Pacific Islands, Thailand, Spain, Greece, and Singapore
Targeted Populations Fourteen of the 115 intervention studies involved interventions with nursing students, while nine studies focused on nurses and mental health professionals. Ninety-two of the studies examined the effect of the intervention on the client. Examples of the studies describing each of these groups are described below.
Fourteen of the 23 nursing intervention studies involved undergraduate nursing students. Nursing students . Fourteen of the 23 nursing intervention studies involved undergraduate nursing students. One study was conducted in Australia regarding consumer participation ( Happell, Moxham, & Plantain-Phung, 2011 ). In this study, researchers investigated whether education programs introducing nursing students to mental health nursing lead to more favorable attitudes towards consumer participation in the mental health setting after completing the mental health component of the nursing program. Study participants were in the first semester of the final year of the Bachelor of Nursing program. The study used a within-subject design using two points (pre-and post-educational program implementation). Results indicated that students demonstrated positive attitudes toward consumer participation even before completing the mental health component. Only marginal and non-significant changes were noted at the post-test stage. The authors concluded that the findings were not surprising given the positive scores recorded at baseline (ceiling effect) ( Happell et al., 2011 ). Another study investigated the effect of pedagogy of curriculum infusion on nursing students’ well-being and the improvement of quality of patients’ care ( Riley & Yearwood, 2012 ).
Pedagogy of curriculum infusion involves instilling the university values and mission with a focus on educating the whole person, and encouraging faculty to translate the core mission of the university into practice in the classroom. this can be accomplished through a variety of courses that provide students with opportunities for contemplation, reflective engagement, and also action through volunteerism, service, and study abroad. The ultimate goal of the study was to encourage critical thinking through reflective exercises and group discussion. Results indicated that students who have experienced the curriculum infusion showed an ability to be self-advocates when discussing their work challenges. Also, they were able to identify specific nursing actions for patient safety; to recognize the patient as a partner in care; and to demonstrate respect for patients' uniqueness, values, and desires as evidenced by case analysis and personal reflections ( Riley & Yearwood, 2012 ).
Three intervention studies explored simulation to see its impact on improving the learning experiences of the nursing students. Three intervention studies explored simulation to see its impact on improving the learning experiences of the nursing students ( Kameg, Englert, Howard, & Perozzi, 2013 ; Kidd, Knisley & Morgan, 2012 ; Masters, Kane, & Pike, 2014 ). Different simulations were used in the three studies; all of them were deemed effective. For example, the results of the study conducted by Kidd and colleagues indicated that undergraduate, mental health nursing students perceived that Second Life® virtual simulation was moderately effective as an educational strategy and slightly difficult as a technical program ( Kidd et al., 2012 ). Also, second degree and traditional BSN students found that a tabletop simulation, which was developed as a patient safety activity and involved checking-in a patient admitted to a psychiatric care unit, was a good learning experience and helpful to prepare students for situations they may experience in the workplace ( Masters et al., 2014 ). The third study used a high-fidelity, patient simulation (HFPS) to assess senior level nursing student knowledge and retention of knowledge utilizing three parallel, 30-item Elsevier Health Education Systems, Inc. (HESITM) Custom Exams. Although students’ knowledge did not improve following the HFPS experiences, the findings provided evidence that HFPS may improve knowledge in students who are at risk (defined as those earning less than 850 on HESI exam). Students reported that they viewed this simulation as a positive learning experience ( Kameg et al., 2013 ).
An additional intervention study used a quasi-experimental design to explore perceptions of student nurses toward nurses who are chemically dependent, using a two-group, pretest–posttest design (prior to formal education and after receiving substance abuse education). Results indicated that the student nurses in this study had positive perceptions about nurses who are chemically dependent before the intervention; and the education program appeared to reinforce their existing attitudes. ( Boulton & Nosek, 2014 ).
Mitchell et al. ( 2013 ) investigated the impact of an addiction training program for nurses consisting of Screening, Brief Intervention, and Referral to Treatment (SBIRT), and embedded within an undergraduate nursing curriculum, on students’ abilities to apply an evidence-based screening and brief intervention approach for risky alcohol and drug use in their nursing practice. Results indicated that the SBIRT program was effective in changing the undergraduate nursing students’ self-perceptions of their knowledge, skills, and effectiveness in screening and intervening for hazardous alcohol and drug use. Furthermore, this positive perception was maintained at 30-day follow-up ( Mitchell et al., 2013 ).
Luebbert and Popkess ( 2015 ) investigated the impact of an innovative, active-learning strategy using simulated, standardized patients on suicide assessment skills in a sample of 34 junior and senior baccalaureate nursing students. Additionally, Schwindt, McNelis, and Sharp ( 2014 ) evaluated a theory-based educational program to motivate nursing students to intervene with persons having serious mental illness. Other intervention studies among nursing students focused on improving students' interpersonal relationships; communication competence; empathetic skills; and confidence in performing mental health nursing skills among nursing students ( Choi, Song, & Oh, 2015 ; Choi & Won, 2013 ; Fiedler, Breitenstein, & Delaney 2012 ; Ozcan, Bilgin, & Eracar, 2011 ; Stiberg, Holand, Ostad, & Lorem, 2012 ).
Nursing staff and mental health professionals . Interventions among the nursing staff and mental health professionals accounted for nine of the nursing intervention studies. The majority of these studies were nursing interventions to educate the nursing staff. Educational interventions included: training videos ( Irvine et al., 2012 ); a continuing education course on suicide awareness ( Tsai, Lin, Chang, Yu,& Chou, 2011 ); an education program using simulation ( Usher et al., 2014 ; Wynn, 2011 ); an educational workshop ( White, Hemingway, & Stephenson, 2014 ); training on family-centered care ( Wong, 2014 ); and the impact of the completion of a 26-week trial on nursing staff’s experience for working as a cardio-metabolic health nurse ( Happell et al., 2014 ).
Terry and Cutter ( 2013 ) used a mixed methods pilot study to evaluate the effect of education on confidence in assessing and addressing physical health needs following attendance at a module titled “Physical Health Issues in Adult Mental Health Practice.” The majority of the participants had studied at the university during the previous five years, at either the diploma or the degree level. Results showed improvement in confidence scores for all study participants following the module; participants were able to identify new knowledge and perspectives for practice change.
Results indicated that care zoning increased the nursing team’s capacity to share information and to communicate patients’ clinical needs... Finally, the study conducted by Taylor and colleagues ( 2011 ) used a pragmatic approach to increase understanding of the clinical-risks needs in acute in-patient unit settings. Each patient was classified according to three zoning levels using a traffic light system: red (high level of risk), amber (medium/moderate level of risk), and green (low level of risk). The level of risk was based on multiple factors including clinical judgment and team discussion ( Taylor et al., 2011 ). Results indicated that care zoning increased the nursing team’s capacity to share information and to communicate patients’ clinical needs, as well as to enhance their abilities to address complex clinical presentation and to seek support when needed.
Intervention Domains
Ninety-two of the studies examined the effect of an intervention for the client. In the following section, we will describe the intervention domains of these 92 articles and provided examples. Additional detail is included in the Table .
Interventions in the Biological Domain Eight interventions were in the biological domain. Study interventions included yoga, dancing, diet, medication, electroconvulsive therapy (ECT), exercise, walking, and educational intervention on metabolic syndrome. Four interventions used various kinds of exercises, including walking ( Beebe, Smith, Davis, Roman, & Burke, 2012 ); dancing ( Emory, Silva, Christopher, Edwards, & Wahl, 2011 ); yoga ( Kinser, Bourguigion, Whaley, Hauenstein, & Taylor, 2013 ); and group exercise program ( Stanton, Donohue, Garnon, & Happell, 2015 ). Diet was also used as an intervention. For example, Lindseth, Helland, and Caspers ( 2015 ) used dietary intake of a high or low tryptophan diet as an intervention. Results indicated improvement in patients’ mood, depression, and anxiety for those consuming a high tryptophan diet as compared to those who consumed a low tryptophan diet ( Lindseth et al. 2015 ). A third category within the biological domain was the use of medications as an intervention. One study tested the use of different psychotropic medications for patients diagnosed with schizophrenia ( Zhou et al., 2014 ). A second used ECT as a treatment modality and measured scores on the Montgomery Asberg (MA) Depression Rating Scale before and after the course of treatment ( Pulia, Vaidya, Jayaram, Hayat, & Reti, 2013 ). A final category was an educational program on metabolic syndrome provided to mental health counselors who performed intake assessments on patients newly admitted to two outpatient mental health facilities. ( Arms, Bostic, & Cunningham, 2014 ). Prior to the intervention, neither facility screened for metabolic syndrome at intake or referred patients with a body mass index (BMI) >25 for medical evaluation. Following the intervention, 53 of 132 patients had a documented BMI >25, and 47 of 53 patients were referred to a primary care provider for evaluation. These findings suggested that screening for metabolic syndrome and associated illnesses will increase the rate of detection of chronic conditions ( Arms et al., 2014 ).
Interventions in the Psychological Domain ...the psychological domain had the largest number of intervention studies. Compared to the other domains, the psychological domain had the largest number of intervention studies. Twenty-four of the 92 total intervention studies extracted were in the psychological domain. The intervention studies in the psychological domain included emotion, behavior, and cognition (e.g., counseling) in addition to studies that focused on behavior therapy and psychoeducational programs. Examples of psychological domains studies included: counseling regarding tobacco cessation treatment ( Battaglia, Benson, Cook, & Prochazka, 2013 ); counseling regarding sexual assault ( Lawson, Munoz-Rojas, Gutman, & Siman, 2012 ); resourcefulness training intervention for relocated older adults ( Bekhet, Zauszniewski, & Matel-Anderson, 2012 ); and resilience training and cognitive therapy in women with symptoms of depression aged 18-22 years of age ( Zamirinejad, Hojjat, Golzari, Borjali, & Akaberi, 2014 ) Please see the Table for further details.
One study utilizing an intervention from the psychological domain examined a brief, six- session, cognitive-behavioral intervention among patients with alcohol dependence and depression. The researchers used a quasi-experimental design with a control group and pretest, posttest, and follow-up assessments. Results indicated that the mean depression scores decreased significantly in both the experimental (n = 33) and control groups (n = 27) at the one-month follow-up (Week 7). However, only the experimental group showed significant differences in their mean depression scores between pre- and posttest. At Week 7, the experimental group showed significantly lower mean depression scores than the control group ( Thapinta, Skulphan, & Kittrattanapaiboon, 2014 ).
Interventions in the Social Domain The social domain considers the patients’ environment and its impact on patients’ adjustment and responses to stress. Nine studies involved use of the social domain in their interventions. The social domain considers the patients’ environment and its impact on patients’ adjustment and responses to stress. Interventions in this domain included family, friends, and social support, as well as community interactions ( Zauszniewski et al., 2012 ). One example of an intervention in the social domain involved studying the long-term impact of safe shelter and justice services on abused women’s ability to function after receiving services ( Koci, 2014 ). Another example of an intervention study in the social domain was a pilot, randomized, controlled trial study by Simpson, Quigley, Henry, and Hall ( 2014 ). In this study, the researchers evaluated the selection, training, and support of a group of peer workers recruited to provide support to service users discharged from acute psychiatric unites in London, comparing peer support with usual care ( Simpson et al., 2014 ) (see Table ). A third example in the social domain was designed to help participants successfully transfer from hospitals to the community by enhancing staff participation, creating/maintaining supportive ward milieus, and supporting managers throughout the implementation process ( Forchuk et al., 2012 ).
The study conducted by Horgan, McCarthy, and Sweeny ( 2013 ) was another example of research in the social domain. This study included designing a website for people ages 18-24 who were experiencing depressive symptoms. The website provided a forum to allow participants to offer peer support to each other; it also provided information on depression and links to other supports ( Horgan et al., 2013 ).
Combinations of the Domains Many studies used more than one domain as interventions. Many studies used more than one domain as interventions (see Figure ). Almost half (49%) of the 92 reviewed studies (n = 45) tested an intervention that included two domains. Thirty studies were psychosocial, twelve were biopsychological, and three were biosocial. In addition, six studies (7%) tested intervention with all three domains (biopsychosocial). In the following section, one study from each combination will be described. Again, additional information is provided in the Table .
Figure. Psychiatric Nursing Interventions: Examples of Domains and Their Total Numbers

Iskhandar Shah and colleagues ( 2015 ) studied and tested an intervention from the biopsychological domain using a single-group, pretest–posttest, quasi-experimental research design. Their intervention program included three daily, one-hour sessions incorporating psychoeducation and virtual-reality-based relaxation practice in a convenience sample of twenty-two people with mental disorders. Results indicated that those who completed the program had significantly lowered subjective stress, depression, and anxiety, along with increased skin temperature, perceived relaxation, and knowledge ( Iskhandar Shah et al., 2015 ).
Pedersen, Nordaunet, Martinsen, Berget, and Braastad ( 2011 ) studied an intervention from the biosocial domain. Their intervention program tested the impact of a 12-week, farm-animal-assisted intervention consisting of work and contact with dairy cattle, on levels of anxiety and depression in a sample of fourteen adults diagnosed with clinical depression. The twice-a-week program involved video recording each participant twice during the intervention. Participants were given the choice of either choosing their work tasks with animals (e.g., milking, feeding, hand feeding, moving animals) or the choice of spending their time in contact with farm animals (e.g., patting, stroking, and other non-work-related physical contact). Results indicated that levels of anxiety and depression decreased, and self-efficacy increased during the intervention. Interaction with farm animals (social) via work tasks showed a greater potential for improved mental health than merely animal contact, but only when progress in working skills (biological aspect) was achieved, indicating the role of coping experiences for a successful intervention. ( Pedersen et al., 2011 ).
The NP often accompanied the participant to medical and mental health appointments... Chandler, Roberts, and Chiodo ( 2015 ) conducted a study in the psychosocial domain that examined the feasibility and potential efficacy of implementing a four-week, empower-resilience intervention (ERI) to build resilience capacity with young adults who have identified adverse childhood experiences. The intervention included using mindfulness-based stress reduction (psychological domain) and social support with guided peer and facilitator interaction (social domain). The study randomly assigned a purposive sample of female undergraduate students between the ages of 18 and 24 years of age into two groups: intervention (n = 17) and control (n = 11), and used a pretest–posttest design to compare symptoms, health behaviors, and resilience before and after the intervention program. Results indicated that subjects in the intervention group reported greater building of strengths, reframing resilience, and creating support connections as compared with the control group ( Chandler et al., 2015 ).
Interventions in the biopsychosocial domain include all three components (biological, psychological, and social). There were six studies that included all three domains in their interventions. Hanrahan, Solomon, and Hurford ( 2014 ) used a randomized controlled design to deliver a transitional care model (TCM) intervention to patients with serious mental illness who were transferring from hospital care to home. The intervention group (n = 20) received the TCM intervention delivered by a psychiatric nurse practitioner (NP) for 90 days post hospitalization and the control group (n = 20) received the usual care. The intervention by the nurse practitioner included helping the patients adapt to the home by focusing on managing problem behaviors and physical problems, managing risk factors to prevent further cognitive or emotional decline, promoting adherence to therapies, and integrating physical and mental care approaches. The NP often accompanied the participant to medical and mental health appointments to facilitate communication, translate information to specialty providers, and advocate for the participant ( Hanrahan et al., 2014 ).
Table. Research Classifications by Domains, Design, and Type of Data Used
|
|
|
|
|
|
|
| Beebe et al. ( ) | Walking program | Self-efficacy for exercise was significantly higher in experimental participants than in controls after intervention. | Random assignment, researchers blinded, pre-/ posttest | Quantitative | Biological |
| Emory et al. ( ) | Line dancing program | The fall rate post intervention was 2.8% compared with 3.2% before intervention. | Pretest-posttest | Quantitative | Biological |
| Kinser, Bourguignon, Taylor, & Steeves ( ) | 8-week yoga intervention | Yoga served as a self-care technique for the stress and ruminative aspects of depression. Yoga facilitated connectedness and helped in sharing experiences in a safe environment. | Qualitative data through daily logs in which participants documented their feelings before and after daily home yoga practice. | Qualitative | Biological |
| Stanton et al. ( ) | Evaluate satisfaction with inpatient group activities designed to assist with recovery, including cognitive behavioral therapy, creative expression, relaxation, reflection/ discussion, and exercise. | More inpatients (50%) rated exercise as “excellent” compared with all other activities. Nonattendance rates were lowest for cognitive behavioral therapy (6.3%), highest for the relaxation group (18.8%), and for the group exercise program (12.5%). | Site evaluation upon discharge; evaluation survey was completed anonymously. | Quantitative | Biological |
| Lindseth et al. ( ) | Dietary intake of high or low tryptophan diet. | Improvement in patients’ mood, depression, and anxiety for those consuming a high tryptophan diet as compared to those who consumed a low Tryptophan. | Within-subjects crossover-designed study, random assignment to control /experimental | Quantitative | Biological |
| Zhou et al. ( ) | Examine the predictive value of time-based prospective memory (TBPM) and other cognitive components for remission of positive symptoms in first episode of schizophrenia. | Higher scores, reflecting better TBPM, at baseline were more likely to achieve remission after 8 weeks of optimized antipsychotic treatment. | Random assignment, pretest-posttest | Quantitative | Biological |
| Pulia et al. ( ) | ECT technique. Two changes were introduced: (a) switching the anesthetic agent from propofol to methohexital, and (b) using a more aggressive ECT charge dosing regimen for right unilateral (RUL) electrode placement. | Compared with patients receiving ECT with RUL placement prior to the changes, patients who received RUL ECT after the changes had a significantly shorter inpatient Length of stay (27.4 versus 18 days, p = 0.028). | A retrospective analysis was performed on two inpatient groups treated on Mood Disorders Unit. | Quantitative | Biological |
| Arms et al. ( ) | Education session about metabolic syndrome for clinicians. | No difference in educational pre-posttest scores. Clinicians increased referral to Primary Care Provider for BMI >25. | Pretest/posttest, chart audit | Quantitative | Biological |
| Battaglia et al. ( ) | Counseling regarding tobacco cessation treatment designed to increase patient engagement while hospitalized. | The intervention had minimal impacts on internalized stigma and personal recovery. Peer support demonstrated positive effects on internalized stigma and personal recovery. | Pilot study, single group, unblinded intervention trial | Quantitative and Qualitative | Psychological |
| Lawson et al. ( ) | “Men's Program”- rape prevention intervention. | Promising change in attitudes about rape beliefs and bystander behaviors in Hispanic males exposed to the educational intervention. | Exploratory study, mixed methods design, pre- and post-test, focus group transcription thematic coding | Quantitative and Qualitative | Psychological |
| Bekhet, Zauszniewski, & Matel-Anderson ( ) | Resourcefulness training (RT) for relocated older adults assessing necessity, acceptability, feasibility, safety and effectiveness of RT. | 76.3% of the older adults scoring below 120, indicating a strong need for RT. Participants indicated acceptability, feasibility, safety, and effectiveness with recommendations for intervention improvement. | Pilot study, random assignment, convenience sample | Quantitative and Qualitative | Psychological |
| Zamirinejad, Hojjat, Golzari, Borjali, & Akaberi ( ) | Resilience training and cognitive therapy for young women with depression | The resilience training group and cognitive therapy group showed a signiï¬cant decrease in the average depression score from pretest to posttest and from pretest to follow-up. There was no signiï¬cant difference between effectiveness of resilience training and cognitive therapy on depression but there was a signiï¬cant difference between these two treatment groups and the control group. | Three-group design with control, pretest- posttest | Quantitative | Psychological |
| Thapinta, Skulphan, & Kittrattanapaiboon ( ) | Brief Cognitive Behavioral Therapy intervention to reduce depression among alcohol-dependent individuals | The mean depression scores decreased signiï¬cantly in both the experimental and control groups at the one-month follow-up. However, only the experimental group showed signiï¬cant differences in their mean depression scores between pre-and posttest. At Week 7, the experimental group showed signiï¬cantly lower mean depression scores than the control group. | Quasi-experimental, control group, pretest/ posttest design | Quantitative | Psychological |
| Koci et al. ( ) | shelter and justice services for abused women | At 4 months following a shelter stay or justice services, improvement in all mental health measures; however, improvement was the lowest for PTSD. minimum further improvement at 12 months. | Prospective study | Quantitative | Social |
| Simpson et al. ( ) | peer support workers for inpatient aftercare | Participants indicated that the training was valuable, challenging, yet positive experience that provided them with a good preparation for the role. | Pilot randomized controlled trial (RCT), focus groups | Quantitative and Qualitative | Social |
| Forchuk et al. ( ) | Transitional Relational Model (TRM) was used to help mental health clients transitioning from a psychiatric hospital setting to the community. Strategies included enhancing staff participation, creating/ maintaining supportive ward milieus. | Group C implemented the TRM model significantly quicker than the other groups. | Randomized controlled trial; compared three groups of hospital wards; Group A wards had already adopted the TRM, Group B wards implemented the TRM in Year 1, and Group C wards implemented the TRM in Year 2. | Quantitative | Social |
| Horgan, McCarthy, & Sweeney ( ) | online peer support for young adults experiencing depressive symptoms | No statistical significance difference pre- and post-test. The forum posts revealed that the participants' main difficulties were loneliness and perceived lack of socialization skills. The website provided a place for emotional support. | Mixed method, involving quantitative descriptive, pre- and post-test and qualitative descriptive designs | Quantitative and Qualitative | Social |
| Iskhandar Shah et al. ( ) | Virtual reality (VR)-based stress management (VR DE-STRESS) program for people with mood disorders | Those who completed the program had significantly lowered stress, depression, anxiety. | Single-group, pretest–posttest, quasi-experimental research design and convenience sample | Quantitative and Qualitative | Bio-psychological |
| Pedersen et al. ( ) | Farm animal-assisted intervention consisting of work and contact with dairy cattle | Levels of anxiety and depression decreased, and self-efficacy increased during the intervention. | Pretest-posttest, video recording thematic coding | Quantitative and Qualitative | Bio-Social |
| Chandler et al ( ) | Empower resilience intervention (ERI) to build resilience | Subjects in the intervention group reported building strengths, reframing resilience, and creating support connections. | Purposive sampling, random assignment, intervention and control, pretest-posttest design | Quantitative and Qualitative | Psychosocial |
| Hanrahan et al. ( ) | Transitional care model (TCM) intervention to patients with serious mental illness transferring from hospital care to home | Emergency room use was lower for intervention group but not statistically significant. Continuity of care with primary care appointments were significantly higher for the intervention group. The intervention group's general health improved but was not statistically significant compared with controls. | Randomized controlled trial | Quantitative | Bio-psychosocial |
Discussion
Although substantial progress is being made to develop and test interventions for persons with psychiatric and mental health challenges and their families, there remains much work to be done. Nurse scientists and practitioners share a professional obligation to persons entrusted to their care, which includes providing the highest quality care grounded in solid empirical evidence ( Willis, Beeber, Mahoney, & Sharp, 2010 ). This review yields evidence for the continued dissemination of findings from intervention studies from 2011 through 2015. To perform the analysis reported here, we employed methods that were similar to those used for amassing information from the intervention studies in two previous reviews ( Zauszniewski et al., 2007 ; Zauszniewski et al., 2012 ) in order to facilitate comparisons over time.
... the continued publication of evidence from countries outside the United States remains important... During the review period (2011-2015), 57% of the published intervention studies took place in the United States (U.S.) while 43% were conducted outside the U.S. (i.e., internationally). These percentages compare with 72% and 54% of published U.S. intervention studies and 28% and 46% published international intervention studies in the 2000-2005 and 2006-2010 reviews, respectively. The somewhat lower percentages (28% and 46%) of international intervention studies within the current time frame (2011-2015) may indicate a need for more descriptive research to identify distinguishing characteristics of international populations and important phenomena that may be amenable to intervention prior to the systematic testing of interventions. However, the continued publication of evidence from countries outside the United States remains important for developing globally relevant interventions for psychiatric nursing practice.
...there have been dramatic increases through the years in the overall number of studies that have tested interventions that tap more than one domain. Of the 115 intervention studies from 2011 through 2015 found in the five journals, nurses, student nurses, nursing staff, or other mental health professionals were the intervention recipients in 23, representing 20% of the intervention studies. This percent is higher than the 14% reported in the previous review conducted from 2006 through 2010, indicating a slightly greater focus on testing interventions in mental health care professionals in recent years. Although the interventions tested in these populations are not focused directly on outcomes for clients with mental health issues, promoting or preserving the mental health of professional caregivers most certainly affects those for whom they provide care.
Analysis of published intervention studies in the 5-year interval from 2011 through 2015 revealed an increase in the number of studies of psychiatric patients or clients in the five selected journals. For this time frame, we found 92 intervention studies in comparison with 71 from 2006 through 2010 and 77 from 2000 through 2005, which reflect 5 and 6-year intervals respectively.
We also noted fewer intervention studies where all three domains were integrated within the intervention... Moreover, there have been dramatic increases through the years in the overall number of studies that have tested interventions that tap more than one domain. For example, 33% of intervention studies from 2011 through 2015 tested psychosocial interventions, compared to 17% in the previous review (2006-2010) and 12% in the one prior to that (2000-2005). In addition, 13% of the studies from 2011 through 2015 tested biopsychological interventions compared with 4% and 5% in the previous two reviews. However, there was a slightly lower percent of biosocial intervention studies, specifically 3% in comparison with 4% from 2000-2005 and 6% from 2006-2010. We also noted fewer intervention studies where all three domains were integrated within the intervention, specifically only 6% in comparison with 17% in the previous time frame (2006-2010). Yet, our review revealed a larger percent of biopsychosocial intervention studies than from the review conducted from 2000-2005 (1%). Despite the lower number of studies that integrated all three intervention domains, there was an overall trend toward testing interventions that were not restricted only to one domain, indicating increased attention toward more holistic interventions.
... the overall trend shows a lesser focus on testing interventions within a single domain over time... There were 41 intervention studies between 2011 and 2015 that focused solely on one domain. With the exception of the biological domain (9%), interventions within the psychological (26%) and social (10%) domains were fewer than in previous reviews. For example, there has been a clear downward trend in the percent of psychological intervention studies over time with 57% from 2000-2005 to 38% from 2006-2010 and 26% in this current review. Intervention studies within the social domain decreased from 17% in 2006-2010 to 10% in this review. Studies of interventions in the biological domain have fluctuated over time from 11% in 2000-2005 down to 1% from 2005-2010 and up to 9% in the review reported here. However, the overall trend shows a lesser focus on testing interventions within a single domain over time, pointing perhaps to a growing interest in determining effective interventions that are multifaceted and target multiple factors that affect a person’s health.
Implications: Research Needed
The mind and body do not function independently of each other; therefore, when considering the focus of nursing research, we need to target both systems. Nursing has as its foundation a holistic approach to patient care. At this point in our history as we build a knowledge base, a multifaceted approach is needed when planning nursing research. This study of nursing interventions in our research has explored the biological, psychological, and social domains. Studies in the biopsychosocial domain would benefit our knowledge base and improve the criteria for more accurate, evidence-based nursing interventions.
Medicine has increasingly focused on the mental health component of medical illnesses. Nursing research would be strengthened by focusing on the possibility of medical illness and its relationship to mental illness. This nursing research approach'‹ would support our holistic philosophy of care and increase our knowledge of the whole person. It would provide the best evidence-based approach to planning treatment. In addition, it would serve to increase the sphere of psychiatric nursing beyond the psychiatric unit in health care settings.
...an increase in multicultural studies is needed to further strengthen our evidenced based practice. Finally, an increase in multicultural studies is needed to further strengthen our evidenced based practice. The individual person is complex. Identified culture provides important information as to how patients view health and illness. This information is an important component when planning our evidenced based care and should not be isolated from the patient presentation.
Tracking the progress in intervention research relevant for psychiatric and mental health nursing practice is essential to identify evidence gaps. This current, systematic review of intervention studies published in the most accessible psychiatric and mental health nursing journals for practicing nurses, educators, and researchers in the United States has revealed a somewhat lower number of studies from outside the United States; a slightly greater focus on studies of nurses, nursing students, or other mental health professionals as compared with clients who receive their care or services; and a continued trend for testing interventions that captured more than one dimension. Tracking the progress in intervention research relevant for psychiatric and mental health nursing practice is essential to identify evidence gaps. Though substantial progress has been made through the years, there is still room to grow.
Abir K. Bekhet, PhD, RN, HSMI Email: [email protected]
Jaclene A. Zauszniewski, PhD, RN-BC, FAAN Email: [email protected]
Denise M. Matel-Anderson, APNP, RN Email: [email protected]
Jane Suresky, DNP, MSN Email: [email protected]
Mallory Stonehouse, MSN, RN Email: [email protected]
Arms, T., Bostic, T., & Cunningham, P. (2014). Educational intervention to increase detection of metabolic syndrome in patients at community mental health centers. Journal of Psychosocial Nursing & Mental Health Services, 52 (9), 32-36. doi:10.3928/02793695-20140703-01
Battaglia, C., Benson, S.L., Cook, P.F., & Prochazka, A. (2013). Building a tobacco cessation telehealth care management for veterans with posttraumatic stress disorder. Journal of the American Psychiatric Nurses Association , 19 (2), 78-91. doi:10.1177/1078390313483314
Beebe, L.H., Smith, K., Davis, J., Roman, M., & Burke, R. (2012). Meet me at the crossroads: Clinical research engages practitioners, educators, students, and patients. Perspectives in Psychiatric Care, 48 (2), 76-82. doi: 10.1111%2Fj.1744-6163.2011.00306.x
Bekhet, A.K., Zauszniewski, J.A., & Matel-Anderson, D.M. (2012). Resourcefulness training intervention: Assessing critical parameters from relocated older adults’ perspectives. Issues in Mental Health Nursing, 33 (7), 430-435. doi:10.3109/01612840.2012.664802
Boulton, M.A., & Nosek, L. (2014). How do nursing students perceive substance abusing nurses? Archives of Psychiatric Nursing, 28 (1), 29-34. doi:10.1016/j.apnu.2013.10.005
Chandler, G.E., Roberts, S.J., & Chiodo, L. (2015). Resilience intervention for young adults with adverse childhood experiences. The Journal of Psychiatric Nurses Association, 21 (6), 406-416. doi:10.1177/1078390315620609
Choi, Y., Song, E., & Oh, E. (2015). Effects of teaching communication skills using a video clip on a smart phone on communication competence and emotional intelligence in nursing students. Archives of Psychiatric Nursing, 29 (2), 90-95. doi:10.1016/j.apnu.2014.11.003
Choi, Y-J., & Won, M-R. (2013). A pilot study on effects of a group program using recreational therapy to improve interpersonal relationships for undergraduate nursing students. Archives of Psychiatric Nursing, 27 (1), 54-55. doi:10.1016/j.apnu.2012.08.002
Emory, S.L., Silva, S.G., Edwards, P.B., & Wahl, L.E. (2011). Stepping to stability and fall prevention in adult psychiatric patients. Issues in Mental Health Nursing, 49 (12), 30-36 doi:10.3928/02793695-20111102-01
Fiedler, R.A., Breitenstein, S., & Delaney, K. (2012). An assessment of students’ confidence in performing psychiatric mental health nursing skills: The impact of the clinical practicum experience. Journal of the American Psychiatric Nurses Association, 18 (4), 244-250. doi:10.1177/1078390312455218
Forchuk, C., Martin, M-L., Jensen, E., Ouseley, S., Sealy, P., Beal, G., … Sharkey, S. (2012). Integrating the transitional relationship model into clinical practice. Archives in Psychiatric Nursing, 26 (5), 374-381. doi:10.1111/j.1365-2850.2012.01956.x
Hanrahan, N.P., Solomon, P., & Hurford, M.O. (2014). A pilot randomized control trial: Testing a transitional care model for acute psychiatric conditions. Journal of the American Psychiatric Nurses Association , 20 (5), 315-327. doi:10.1177/1078390314552190
Happell, B., Hodgetts, D., Stanton, R., Millar, F., Phung, C.P., & Scott, D. (2014). Lessons learned from the trial of a cardiometabolic health nurse. Perspectives in Psychiatric Care, 50 (4), 1-9. doi:10.1111/ppc.12091
Happell, B., Moxham, L., &Platania-Phung, C. (2011). The impact of mental health nursing education on undergraduate nursing students’ attitudes to consumer participation. Issues in Mental Health Nursing, 32 (2), 108-113. doi:10.3109/01612840.2010.531519
Horgan, A., McCarthy, G., & Sweeny, J. (2013). An evaluation of an online peer support forum for university students with depressive symptoms. Archives of Psychiatric Nursing, 27 (2), 54-55. doi:10.1016/j.apnu.2012.12.00
Irvine, A.B., Billow, M.B., Eberhage, M.G., Seeley, J.R., McMahon, E., & Bourgeois, M. (2012). Mental illness training for licensed staff in long-term care. Issues in Mental Health Nursing, 33 (3), 181-194. doi: 10.3109/01612840.2011.639482
Iskhandar Shah, L.B., Torres, S., Kannusamy, P., Lee Chng, C.M., He, H-G., Klainin-Yobas, P. (2015). Efficacy of the virtual reality-based stress management program on stree-related variables in people with mood disorders: The feasibility of the study. Archives of Psychiatric Nursing, 29 (1), 6-13. doi:10.1016/j.apnu.2014.09.003
Kameg, K.M., Englert, N.C., Howard, V.M., & Perozzi, K.J. (2013). Fusion of psychiatric and medical high-fidelity patient simulation scenarios: Effect on nursing student knowledge, retention of knowledge, and perception. Issues in Mental Health Nursing, 34 (12), 892-900. doi:10.3109/01612840.2013.854543
Kane, C. (2015). The 2014 Scope and Standards of Practice for psychiatric mental health nursing: Key Updates. OJIN: The Online Journal of Issues in Nursing, 20 (1), Manuscript 1. doi:10.3912/OJIN.Vol20No01Man01
Kidd, L.I., Knisley, S.J. & Morgan, K.I. (2012). Effectiveness of a Second Life® simulation as a teaching strategy for undergraduate mental health nursing students. Journal of Psychosocial & Mental Health Services, 50 (7), 3-5. doi:10.3928/02793695-20120605-04
Kinser, P.A., Bourgugnon, C. Taylor, A.G., Steeves, R. (2013). "A feeling of connectedness": Perspectives on a gentle yoga interenvention for women with major depression. Issues in Mental Health Nursing, 34 (6), 402-211. doi:10.3109/01612840.2012.762959
Kinser, P.A., Bourguigion, C., Whaley, D., Hauenstein, E., & Taylor, A.G. (2013). Feasibility, acceptability, and effects of gentle Hatha yoga for women with major depression: Findings from a randomized controlled mixed-methods study. Archives of Psychiatric Nursing, 27 (3), 137-147. doi:10.1016/j.apnu.2013.01.003
Koci, A.F., Cesario, S., Nava, A., Liu, F., Montalvo-Liendo, N., & Zahed, H. (2014). Women’s functioning following an intervention for partner violence: New knowledge for clinical practice from a 7-year study. Issues in Mental Health Nursing, 35 (10), 745-755. doi:10.3109/01612840.2014.901450
Lawson, S.L., Munoz-Rojas, D., & Siman, M.N. (2012). Changing attitudes and perceptions of Hispanic men ages 18-25 about rape and rape prevention. Issues in Mental Health Nursing, 22 (12), 864-70. doi:10.3109/01612840.2012.728279
Lindseth, G., Helland, B., & Caspers, J. (2015). The effects of dietary tryptophan on affective disorders. Archives of Psychiatric Nursing, 29 (3), 102-107. doi:10.1016/j.apnu.2014.11.008
Luebbert, R., & Popkess, A. (2015). The influence of teaching method on performance of suicide assessment in baccalaureate nursing students. The Journal of American Psychiatric Nurses Association, 21 (2), 126-133. doi:10.1177/1078390315580096
Masters, J.C., Kane, M.G., & Pike, M.E. (2014). The suitcase simulation: An effective and inexpensive psychiatric nursing teaching activity. Journal of Psychosocial Nursing, 52 (8), 39-44. doi:10.3928/02793695-20140619-01
Mitchell, A.M., Puskar, K., Hagle, H., Gotham, H.J., Talcott, K.S., Terhorst, L., … Burns, H.K. (2013). Screening, brief intervention, and referral to treatment: Overview of and student satisfaction with an undergraduate addiction training program for nurses. Journal of Psychosocial Nursing & Mental Health Services, 51 (10), 29-37. doi:10.3928/02793695-20130628-01
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science : IS , 10 , 53. doi:10.1186/s13012-015-0242-0
Ozcan, N.D., Bilgin, H., & Eracar, N. (2011). The use of expressive methods for developing empathetic skills. Issues in Mental Health Nursing, 32 (2), 131-136. doi:10.3109/01612840.2010.534575
Pedersen, I., Nordaunet, T., Martinsen, E.W., Berget, B., & Braastad, B.O. (2011). Farm animal-assisted intervention: Relationship between work and contact with farm animals and change in depression, anxiety, and self-efficacy among persons with clinical depression. Issues in Mental Health Nursing, 32 (8), 493-500. doi:10.3109/01612840.2011.566982
Proctor, E.K., Landsverk, J., Aarons, G., Chambers, D., Glisson, C., & Mittman, B. (2009). Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health, 36 (1), 24-34 doi:10.1007/s10488-008-0197-4
Pulia, K., Vaidya, P., Jayaram, G., Hayat, M., & Reti, I.M. (2013). ECT treatment outcomes following performance improvement changes. Journal of Psychosocial and Mental Health Services, 51 (11), 20-25. doi:10.3928/02793695-20130628-02
Riley, J.B., & Yearwood, E.L. (2012). The effect of a pedagogy of curriculum infusion on nursing student well-being and intent to improve the quality of nursing care. Achieves in Psychiatric Nursing, 26 (5), 364-63. doi:10.1016/j.apnu.2012.06.004
Schwindt, R.G., McNelis, A.M., & Sharp, D. (2014). Evaluation of a theory-based educational program to motivate nursing students to intervene with their seriously mentally ill clients who use tobacco. Archives of Psychiatric Nursing, 28 (4), 277-283. doi:10.1016/j.apnu.2014.04.003
Simpson, A., Quigley, J., Henry, S.J., & Hall, C. (2014). Evaluating the selection, training, and support of peer support workers in the United Kingdom. Journal of Psychosocial Nursing and Mental Health Services, 52 (1), 31-40. doi:10.3928/02793695-20131126-03
Sorensen, J. L., & Kosten, T. (2011). Developing the tools of implementation science in substance use disorders treatment: applications of the consolidated framework for implementation research. Psychology of Addictive Behaviors, 25 (2), 262-268. doi:10.1037/a0022765
Stanton, R., Donohue, T., Garnon, M., & Happell, B. (2015). Participation in and satisfaction with an exercise program for inpatient mental health consumers. Perspectives in Psychiatric Care, 52 (1), 62-67. doi:10.1111/ppc.12108
Stiberg, E., Holand, U., Olstad, R., & Lorem, G. (2012). Teaching care and cooperation with relatives: Video as a learning tool in mental health work . Issues in Mental Health Nursing, 33 (8). doi:10.3109/01612840.2012.687804
Taylor. K., Guy, S., Stewart, L., Ayling, M., Miller, G., Anthony, A., … Thomas, M. (2011). Care zoning a pragmatic approach to enhance the understanding of clinical needs as it relates to clinical risks in acute in-patient unit settings. Issues in Mental Health Nursing, 32 (5), 318-326. doi:10.3109/01612840.2011.559570
Terry, J. & Cutter, J. (2013). Does education improve mental health practitioners’ confidence in meeting the physical health needs of mental health service users? A mixed method pilot study. Issues in Mental Health , 34(4), 249-255. doi:10.3109/01612840.2012.740768
Thapinta, D., Skulphan, S., & Kittrattanapaiboon, P. (2014). Brief cognitive behavioral therapy for depression among patients with alcohol dependence in Thailand. Issues in Mental Health Nursing, 35( 9), 689-693. doi:10.3109/01612840.2014.917751
Tsai, W-P., Lin, L-Y., Chang, H-C., Yu, L-S., & Chou, M-C. (2011). The effects of the gatekeeper suicide-awareness program for nursing personnel. Perspectives in Psychiatric Care, 47 (3), 117-125. doi:10.1111/j.1744-6163.2010.00278
Usher, K., Park, T., Trueman, S., Redman-MacLaren, M., Casella, E., & Woods, C. (2014). An educational program for mental health nurses and community health workers from Pacific Island countries: Results from a pilot study . Issues in Mental Health Nursing, 35 (5), 337-343. doi:10.3109%2F01612840.2013.868963
White, J., Hemingway, S., & Stephenson, J. (2014). Training mental health nurses to assess the physical health needs of mental health service users: A pre- and post-test analysis. Perspectives in Psychiatric Care, 50( 4), 243-250. doi:10.1111/ppc.12048
Willis, D.G., Beeber, L., Mahoney, J., & Sharp, D. (2010). Strategies for advancing psychiatric-mental health nursing science relevant to practice. Perspectives from the American Psychiatric Nurses Association research council co-chairs. Contemporary Nurse, 34 (2), 135-139
Wong, O.L. (2014). Contextual barriers to the successful implementation of family-centered practice in mental health care: A Hong Kong study. Archives of Psychiatric Nursing, 28 (3), 197-199. doi:10.1016/j.apnu.2014.02.001
Wynn, S.D. (2011). Improving the quality of care of veterans with diabetes. Journal of Psychosocial Nursing & Mental Health Services, 49 (2), 38-43. doi:10.3928/02793695-20110111-01
Zamirinejad, S., Hojjat, SK., Golzari, M., Borjali, A., &Akaberi, A. (2014). Effectiveness of resilience training versus cognitive therapy on reduction of depression in female Iranian college students. Issues in Mental Health Nursing, 36 (6), 480-488. doi:10.3109/01612840.2013.879628
Zauszniewski, J.A, Bekhet, A., &Haberlein, S. (2012). A decade of published evidence for psychiatric and mental health nursing interventions. OJIN: The Online Journal of Issues in Nursing, 17 (3), doi:10.3912/OJIN.Vol17No03HirshPsy01
Zauszniewski, J., Suresky M.J., Bekhet, A., & Kidd, L. (May 14, 2007). Moving from Tradition to Evidence: A Review of Psychiatric Nursing Intervention Studies . Online Journal of Issues in Nursing 12 (2) doi:10.3912/OJIN.Vol12No02HirshPsy01
Zhou, F-C., Xiang, Y-T., Wang, C-Y., Dickerson, F., Kryenbuhl, J., Ungari, G.S., … Chiu, H.F.K. (2014). Predictive value of prospective memory for remission in first-episode schizophrenia. Perspectives in Psychiatric Care, 50 (2), 102-110. doi:10.1111/ppc.12027
May 31, 2018
DOI : 10.3912/OJIN.Vol23No02Man04
https://doi.org/10.3912/OJIN.Vol23No02Man04
Citation: Bekhet, A.K., Zauszniewski, J.A., Matel-Anderson, D.M., Suresky, M.J., Stonehouse, M., (May 31, 2018) "Evidence for Psychiatric and Mental Health Nursing Interventions: An Update (2011 through 2015)" OJIN: The Online Journal of Issues in Nursing Vol. 23, No. 2, Manuscript 4.
- Article May 31, 2018 Advancing Scholarship through Translational Research: The Role of PhD and DNP Prepared Nurses Deborah E. Trautman, PhD, RN, FAAN; Shannon Idzik, DNP, CRNP, FAANP, FAAN; Margaret Hammersla, PhD, CRNP-A; Robert Rosseter, MBA, MS
- Article May 31, 2018 Connecting Translational Nurse Scientists Across the Nation—The Nurse Scientist-Translational Research Interest Group Elizabeth Gross Cohn, RN, NP, PhD, FAAN; Donna Jo McCloskey, RN, PhD, FAAN; Christine Tassone Kovner, PhD, RN, FAAN; Rachel Schiffman, RN, PhD, FAAN; Pamela H. Mitchell, RN, PhD, FAAN
- Article May 31, 2018 Translation Research in Practice: An Introduction Marita G. Titler, PhD, RN, FAAN
- Research article
- Open access
- Published: 26 April 2019
Mental health nurses’ attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings
- Geoffrey L. Dickens ORCID: orcid.org/0000-0002-8862-1527 1 , 2 ,
- Robin Ion 3 ,
- Cheryl Waters 1 ,
- Evan Atlantis 1 &
- Bronwyn Everett 1
BMC Nursing volume 18 , Article number: 16 ( 2019 ) Cite this article
59k Accesses
19 Citations
20 Altmetric
Metrics details
There has been a recent growth in research addressing mental health nurses’ routine physical healthcare knowledge and attitudes. We aimed to systematically review the empirical evidence about i) mental health nurses’ knowledge, attitudes, and experiences of physical healthcare for mental health patients, and ii) the effectiveness of any interventions to improve these aspects of their work.
Systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Multiple electronic databases were searched using comprehensive terms. Inclusion criteria: English language papers recounting empirical studies about: i) mental health nurses’ routine physical healthcare-related knowledge, skills, experience, attitudes, or training needs; and ii) the effectiveness of interventions to improve any outcome related to mental health nurses’ delivery of routine physical health care for mental health patients. Effect sizes from intervention studies were extracted or calculated where there was sufficient information. An integrative, narrative synthesis of study findings was conducted.
Fifty-one papers covering studies from 41 unique samples including 7549 mental health nurses in 14 countries met inclusion criteria. Forty-two (82.4%) papers were published since 2010. Eleven were intervention studies; 40 were cross-sectional. Observational and qualitative studies were generally of good quality and establish a baseline picture of the issue. Intervention studies were prone to bias due to lack of randomisation and control groups but produced some large effect sizes for targeted education innovations. Comparisons of international data from studies using the Physical Health Attitudes Scale for Mental Health Nursing revealed differences across the world which may have implications for different models of student nurse preparation.
Conclusions
Mental health nurses’ ability and increasing enthusiasm for routine physical healthcare has been highlighted in recent years. Contemporary literature provides a base for future research which must now concentrate on determining the effectiveness of nurse preparation for providing physical health care for people with mental disorder, determining the appropriate content for such preparation, and evaluating the effectiveness both in terms of nurse and patient- related outcomes. At the same time, developments are needed which are congruent with the needs and wants of patients.
Peer Review reports
People with a mental disorder diagnosis are at more than double the risk of all-cause mortality than the general population. Most at risk are those with psychosis, mood disorder and anxiety diagnoses. Median length of life lost by this group is 10.1 years greater for people with a diagnosis of mental disorder than for general population controls, but mortality rates are significantly higher in studies which include inpatients [ 1 ]. While risk of unnatural causes of death, notably suicide, are greatly increased in this group, it is death from natural causes that remains responsible for the vast majority of mortality. In people with schizophrenia, for example, cardiovascular disease accounts for about one third of all deaths and cancer for one in six, while other common causes are diabetes mellitus, COPD, influenza, and pneumonia [ 2 ]. A relatively high rate of tobacco smoking in this group is implicated in significant increased mortality [ 3 ], as is obesity [ 4 ], exposure to high levels of antipsychotic pharmacological treatment [ 5 ], and mental disorder itself [ 1 ].
Accordingly, the physical health of patients with mental disorder has been prioritised, becoming the focus of guidelines for practitioners in general [ 6 ] and for mental health nurses and other clinical professionals specifically [ 7 , 8 , 9 ]. However, while policies and guidelines are necessary prerequisites of change they must also be implemented in practice if they are to have a positive effect; one of the key barriers to change implementation for mental health nurses has been identified as lack of confidence, skills, and knowledge [ 10 ]. Robson and Haddad ([ 11 ]: p.74) identified that surprisingly ‘modest attention’ had been paid to the issue of such attitudes and knowledge among nurses related to their role in physical health care provision, and developed the Physical Health Assessment Scale for mental health nurses (PHASe) in order to further investigate the phenomenon. Since then, there has been a tangible and growing response among mental health nursing academics and practitioners. In recent years, published literature reviews have covered a decade of UK-only research on the role of mental health nurses in physical health care [ 12 ], patients’ and professionals’ perceptions of barriers to physical health care for people with serious mental illness [ 13 ], the focus and content of nurse-provided physical healthcare for mental health patients [ 14 ], and the physical health of people with severe mental illness [ 15 ]. There has also been an upsurge in the amount of related empirical research. However, to date, no one has systematically reviewed this growing literature about mental health nurses’ attitudes towards, or their related knowledge and experience about providing routine physical healthcare. Further, studies about the effectiveness of interventions designed to improve their delivery of or attitudes to routine physical healthcare have not been systematically appraised. This is surprising given the known links between nurses’ attitudes and their implementation of evidence-based practice [ 16 , 17 , 18 ] and the centrality of measuring nurses’ attitudes to physical health care delivery in recent mental health nursing research on the topic [ 11 , 19 , 20 ].
In this context we have conducted a systematic review to identify, appraise, and synthesise existing evidence from empirical research literature about i) mental health nurses’ experience of providing physical healthcare for patients and about their related knowledge, skills, educational preparation, and attitudes; ii) the effectiveness of any interventions aimed at improving or changing mental health nurse-related outcomes; and iii) to identify implications for the future provision of relevant training and education, for policy, research, and practice. The specific review question being addressed therefore is: what is known from the international, English language, empirical literature about mental health nurses’ skills, knowledge, attitudes, and experiences regarding provision of physical healthcare.
A systematic review of the literature following the relevant points of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [ 21 ].
Search strategy
Since the review scope encompassed questions about experience and effectiveness a dual literature search strategy was developed. For studies about mental health nurses’ experience of delivering physical healthcare a Population Exposure Outcome (PEO) format review question was developed (Population: mental health nurses; Exposure: physical healthcare provision for patients or related training; Outcomes: experiential, social, educational, knowledge, or attitudinal terms, see Additional file 1 : Table S1). For studies of the effectiveness of interventions to improve or change mental health nurse-related outcomes a Population Intervention Comparator Outcome (PICO) structure was implemented (Population: mental health nurses; Intervention: any intervention including physical health-related education, policy or guideline change; Comparator: any or none; Outcome: any) [ 22 ]. We searched five electronic databases: i) CINAHL, ii) PubMed, iii) MedLine, iv) Scopus, and v) ProQuest Dissertations and Theses using text words and MeSH terms. The references list of all included studies, together with those of relevant literature reviews, and the tables of contents of selected mental health nursing journals were hand searched. The search terms were informed by previous literature reviews on the subject of physical healthcare in mental health. The initial search was conducted in April 2018 and re-run in September 2018.
Inclusion and exclusion criteria
Inclusion criteria for studies were English language accounts of empirical research which investigated mental health nurses’ experience of providing physical health care or examined the effectiveness of any intervention that aimed to improve outcomes related to the provision of physical healthcare. Thus, studies of interventions aimed at changing nursing practice, behaviour, knowledge, attitudes, or experiences were eligible, but not those which solely attempted to determine the effect of an intervention on nurses in terms of patient outcomes. While improvement in patient care and outcomes is clearly the desirable endpoint of any intervention on nurses, previous reviews have indicated that no good quality studies exist [ 23 ]. Additionally, studies were only eligible for inclusion where the practitioners involved comprised or included mental health or psychiatric nurses or mental health nursing students, or registered nurses whose practice was within mental health services. Included studies could have used any design or methodological approach. As in previous reviews, studies solely about mental health nurses providing care for people with alcohol/ drug misuse, or mental disorder/substance misuse dual diagnosis were not eligible. Studies about mental health nurses and the provision of emergency physical care or of their experience of providing care for the seriously deteriorating physical health of a patient were omitted as this is the subject of a separate review (Dickens et al. submitted).
Data extraction
Information about the study title, author, publication year, data collection years, location (country), research objectives, aims or hypotheses, design, population, sample details and size, data sources, study variables (i.e. details of intervention) or other exposure, unit of analysis, and study findings were extracted from full text papers. Corresponding authors of included studies were contacted regarding any issues where clarification or additional data could aid the review.
Studies were categorised as interventional or observational. Intervention studies investigated the impact of an educational, policy, or practice intervention in terms of any mental health nurse- or nursing- related outcome, e.g., knowledge, attitudes, behaviour. Intervention studies were further sub-classified as simulation studies (as defined by Bland et al. ([ 24 ]: p.668) “a dynamic process involving the creation of a hypothetical opportunity that incorporates an authentic representation of reality, facilitates active student engagement and integrates the complexities of practical and theoretical learning with opportunity for repetition, feedback, evaluation and reflection”), traditional educational interventions (e.g., lectures, workshops, workbooks), or policy-level interventions (e.g., requiring nurses to follow some new policy or implement some new practice). Observational studies either described mental health nurse- or nursing- related outcomes and/or utilised case control designs to compare them with those of other occupational or professional groups and/or used qualitative methods.
Study quality appraisal
The likelihood of bias in intervention studies was assessed against criteria described by Thomas et al. [ 25 ] and encompassed assessment of the likelihood of selection bias in the obtained sample, study design, potential confounders, blinding, potential for bias in data collection from invalid instrumentation, and participant retention (see Additional file 2 : Table S2). Relevant items from the US Department of Health & Human Sciences NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [ 26 ] were used to assess cross-sectional observational studies (see Additional file 3 : Table S3). Qualitative descriptive studies were assessed using the Critical Appraisal Skills Programme [ 27 ] tool (See Additional file 4 : Table S4). Multiple papers arising from single studies were quality assessed as a single entity. Study quality was initially undertaken independently by at least two of the team. A good level of inter-rater agreement was achieved (Cohen’s Kappa = 0.742 between pairs of raters). Disputed items were discussed by GD and CW and consensus achieved.
Study synthesis
The available total and subscale data from those studies that conducted data collection via the Physical Healthcare Attitude Scale for mental health nurses (PHASe [ 11 ]), the only scale used across more than two studies, was tabulated and compared across studies using unpaired t-tests in QuickCalcs GraphPad software. Where individual item mean and dispersion scores were unavailable estimates were calculated as follows: the mean mean (i.e., Σ means / n means) and the estimated standard deviation (the square root of the average of the variances [ 28 ]). Also, and where available, dichotomised data (‘Strongly agree’ or ‘agree’ responses versus all other responses) from the multiple studies using the 14-item PHASe scale investigating self-reported current involvement in aspects of physical healthcare was tabulated and subjected to Chi-squared analysis. Significant cross-study differences of means and proportions involved all subscale or item data for each study being compared with the corresponding subscale or item from the original study development sample, ‘the reference group’ [ 11 ].
Where available, effect sizes for correlational, interventional, or difference-related outcomes from studies were extracted or, where sufficient information presented, calculated. Where sufficient information was not presented we attempted to contact the corresponding author for clarification. Appropriate effect size statistics were calculated using an online resource [ 29 ]. All other information from study results was subject to a qualitative synthesis conducted by author 1 and subsequently refined and agreed by all of the authors.
Study settings and participants
The search strategy resulted in the inclusion of 41 study samples published in 51 papers (see Fig. 1 ) involving 7549 ( M [ SD ] = 200.5[374.1], Mdn = 47, range 2 to 1899) mental health nurses and n = 213 mental health nursing students ( Mdn = 33). Thirty-three samples included only nurses, of which 20 drew specifically on mental health nurses or nurses working in mental health settings only; eight samples were multidisciplinary. Four papers drew on two samples (i.e., two papers per study) while one sample featured in nine separate papers [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. Studies were conducted in the UK ( k = 17), Australia ( k = 9), US ( k = 4), Canada ( k = 2), Qatar, Hong Kong, Japan, Jordan, Belgium, Norway, Israel, Turkey, India, and Taiwan (all k = 1); two studies were conducted internationally; first, in Qatar, Hong Kong, and Japan [ 19 ], and the US and Canada [ 39 ]. Studies were published between 1994 and 2018 ( Mdn year of publication 2016, only n = 9 before 2010 and n = 1 before 2000).
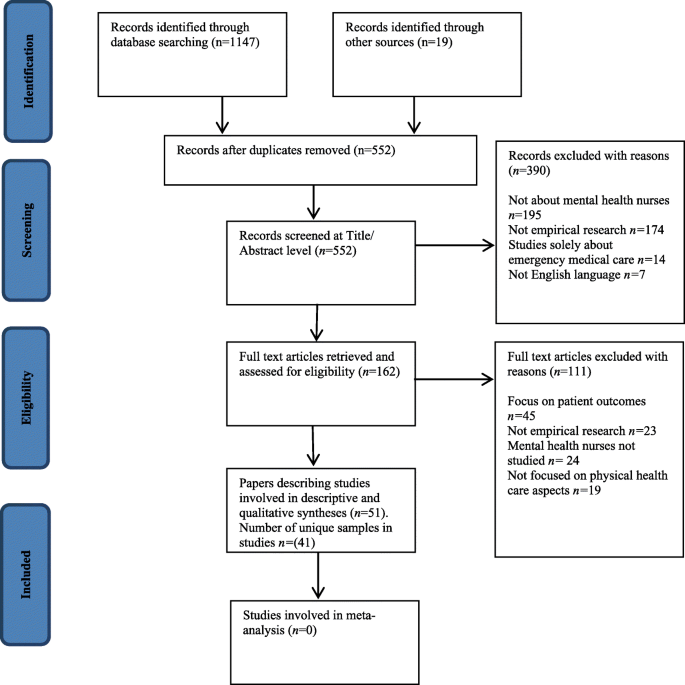
PRISMA study inclusion flowchart
Study design
Eleven studies evaluated an intervention; of these, 10 utilised pre- post AB designs and one adopted a randomised controlled trial design. Other studies used cross-sectional survey or qualitative designs. Intervention studies sometimes incorporated additional qualitative or descriptive elements.
Outcome measures
The most commonly used measure employed was the PHASe or some adaptation of it [ 11 ] in seven studies reported across eight papers [ 11 , 19 , 20 , 40 , 41 , 42 , 43 , 44 ]. The PHASe comprises four factors: 1. Nurses’ attitudes to physical health care; 2. Nurses’ confidence to provide physical health care; 3. Nurses’ perceived barriers in providing physical health care; and 4. Nurses’ attitude towards smoking. Contact with study corresponding authors (Bressington, Chee, Haddad) resulted in acquisition of additional PHASe total and subscale information that was not included in the respective published study papers. Two other outcomes tools were used in two studies each, these being the purpose-designed survey measure of Howard and Gamble [ 45 ] subsequently used by Terry and Cutter [ 46 ], and Happell’s [ 33 ] own questionnaire adapted for use by Clancy et al. [ 40 ]. Most studies used purpose-designed tools. Many reported sufficient information to allow confidence about their internal reliability and face/content validity but there was little information about their measurement reliability, criterion validity, or sensitivity to change (see Additional file 5 : Table S5). A small number of papers used existing validated measures [ 47 , 48 , 49 , 50 , 51 , 52 ] and these were generally the most robust tools (see Additional file 6 : Table S6).
Study quality
All K = 7 qualitative studies were rated very highly in terms of their quality on a 10-point assessment ( Mdn = 9, range 9–10). Cross-sectional observational studies met a median of four of seven quality criteria (range two to six; mean[SD] 4.43[1.33]). Four of these provided an a priori sample size calculation and there was a lack of valid outcome measures in nine of the 21 studies. Overall risk of bias for cross-sectional studies was judged to be low for nine studies, unclear for six and high for six. The quality of interventional studies was generally the poorest ( Mdn = 5, range 2 to 7 of 10 indicators). Only two were judged to be at low risk of bias (see Additional file 2 : Tables S2, Additional file 3 : Table S3, Additional file 4 : Table S4, Additional file 5 : Table S5 and Additional file 6 : Table S6 for further details). Common omissions were, again, sample size justification, lack of repeat pre-baseline and follow up measures, and information about the representativeness of included samples.
Non-intervention studies
Studies examined physical healthcare in general ( k = 24), sexual health ( k = 4), smoking ( k = 6), physical activity and healthy eating, nutrition - in particular the role of Omega-3 in diet, mild brain injury, and breastfeeding (all k = 1; see Table 1 ).
With regards to studies using the PHASe, of all possible comparisons across studies (see Tables 2 and 3 ), the mean score of the study sample differed significantly from the reference sample [ 11 ] on 13 out of 21 (61.9%) subscale and three of four total score combinations (75.0%). Analysis revealed poorer attitudes compared to the reference sample on all three of the significantly poorer attitude scores on 10/17 (58.9%) subscale comparisons, and better attitudes on three (14.3%). However, the reference group only outperformed the other studies on two of the eight possible comparisons on the subscales ‘Physical Healthcare’ and ‘Confidence in Providing Physical Healthcare’ and was poorer for three comparisons. The PHASe total score difference was greatest (large effect size) between the reference sample and Chee et al’s [ 41 ] Australian sample (Cohens d = 1.13) followed by Bressington et al’s [ 19 ] Japanese mental health nurse sub-sample ( d = 0.72). For subscale scores, effect sizes for differences were also largest between the reference sample and that of Chee et al. [ 41 ]. Effect sizes were in favour of the reference sample on the attitudes to smoking and barriers to physical healthcare subscales ( d = 1.48 and 1.78 respectively). Next largest were differences between Haddad et al’s [ 43 ] sample also on the barriers to healthcare ( d = 0.93) and attitudes to smoking subscales ( d = 1.01). On this occasion differences were in favour of Haddad et al’s [ 43 ] sample. Attitudes to smoking were more favourable than the reference sample in two studies, comparable in one and poorer in two.
Regarding the level of self-reported involvement in aspects of physical healthcare the proportion of respondents in PHASe-studies answering ‘strongly agree’ or ‘agree’ to 14 items revealed considerable cross-sample differences. Of 95 possible comparisons between the reference study and others, 70 (73.7%) differed significantly. Of these, 86.7% compared unfavourably with the UK reference study, 13.3% favourably). The number of items per sample differing from the reference sample ranged from 7 to 13 ( Mdn = 10). Japan [ 19 ] provided the only sample of mental health nurses whose responses compared favourably with the reference sample (7/10 significantly differing responses being more favourable in the Japanese sub-sample), while Ganiah et al’s [ 42 ] sample (0/11 favourable comparisons among significantly differing responses), Happell et al’s [ 30 ] (0/14 favourable comparisons), Chee et al’s [ 41 ] Australian sample (1/11 favourable comparisons), Haddad et al’s [ 43 ] UK sample (1/10 favourable comparisons) and Bressington et al’s [ 19 ] Hong Kong sample (2/12 favourable comparisons) all fared poorly. Items relating to checking GP-status, advising on exercise, weight management, healthy eating, contraception, and eyesight checks were all rated less favourably by at least two other samples (range 2 to 6, Mdn = 4) and more favourably by none compared with the reference sample. Only the item about ensuring patients have had their general physical health assessed on first contact with mental health services was rated more favourably by two samples and less favourably by none compared with the reference sample. For all other items there were item-level variations with no clear pattern.
The remaining non-intervention studies provide a mixed and sometimes contradictory picture. First, in terms of reported use of physical health care skills, Osborn et al’s [ 47 ] study revealed that nurses working in mental health settings in one large hospital were less likely to use physical healthcare skills than colleagues in medical, oncology, maternity and surgical settings. Further, they reported using a smaller range of relevant skills. In Howard and Gamble’s [ 45 ] survey, nurses’ responses indicated a gap between their perceived responsibilities for physical healthcare and their practice. Elsewhere, compared with those responding on behalf of healthcare and educational organisations, nurses were less likely to endorse their role in physical healthcare provision [ 53 ] and they reported very low levels of endorsement of related skills training need [ 54 ]. However, for others in more recent studies, they displayed a clear commitment to the physical healthcare role [ 55 ], and said they want more training [ 31 , 56 ]. Further, nurses strongly endorsed their own role in physical health, sexual health, and substance abuse related care and were supported strongly by other healthcare professionals [ 40 ]. Across a series of linked surveys and qualitative studies, Happell et al. [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 57 ] reported associations between nurses’ positive evaluation of the physical healthcare role and practicing aspects of it more commonly. In studies of nurses and specific physical healthcare-related activities there was a suggestion that respondents’ own values or beliefs might be more influential in determining their health-giving or advising behaviour in relation to smoking cessation [ 50 , 58 ]. In relation to sexual health, both Dorsay and Forchuk [ 59 ] and Quinn et al. [ 60 ] have reported that nurses cite patient embarrassment as a reason for not asking patients about sexual side effects of antipsychotic medications. Lack of time, resources and knowledge were reported as barriers to providing advice and interventions regarding exercise and physical activity [ 61 ], Omega-3 [ 62 ]. Knowledge and attitudes to HIV/AIDS were generally good [ 63 ]. Finally, smoking-cessation training was associated with more smoking-cessation helping behaviour [ 64 ] though, counter-inuitively, training was negatively associated with attitudes to smoking cessation in a single study [ 65 ]. Further, Sharma et al’s [ 64 ] study compared the attitudes of mental health trained nurses and comprehensive/ generalist trained nurses working in mental health services: the most marked differences between the groups were on the smoking-related items with the former group expressing significantly more liberal views about smoking restrictions, more worrying attitudes about the benefits and utility of cigarette use as a therapeutic tool, and less confidence in the ability of mental health patients to quit smoking. This was particularly concerning in the study context which was about attitudes to physical healthcare with younger, first episode psychosis patients.
Intervention studies
Five studies focused on physical healthcare in general and six on specific issues (diabetes n = 3; sexual health, cardiometabolic health, obesity all n = 1). Ten evaluated an educational innovation, the exception being Happell et al. [ 35 ], who examined attitudes among nurses to the introduction of a specialist cardiometabolic health nurse role. Haddad et al. [ 43 ] examined the impact of the introduction of personal physical health care plans for patients on nurses’ physical healthcare attitudes alongside the delivery of a single educational session on physical healthcare assessment. The remaining nine studies evaluated educational interventions including three involving simulation and six involving didactic teaching, workshop-format or blended-learning approaches.
Simulation studies
Duration of interventions was 30 min [ 49 ] and1-day [ 66 ], while information was not provided by Wynn [ 52 ]. The mode of simulation delivery involved manikins [ 66 ], human actor as patient [ 66 ], software-based Human Person Simulator [ 52 ], and participant as ‘patient’ in which student participants wore a 15 kg bariatric empathy suit while undertaking everyday tasks in order to help them appreciate the experience of obesity [ 49 ]. Other simulations involved diabetes care [ 52 ], fractured leg in the context of a jump or fall in a patient with first episode psychosis, medical deterioration in the same patient following transfer to a psychiatric ward, and delirium [ 66 ]. Results indicated improved clinical judgement and reduced diabetes-related medical emergency reports [ 52 ], improved knowledge, attitudes, and confidence about physical healthcare [ 66 ], improved response to obese patients, characteristics of obese patients and supportive roles in caring for obese patients [ 49 ].
Non-simulation studie
Study duration ranged from a 2.5-h workshop on physical health [ 67 ] to a 20-credit bachelor’s degree level (equivalent to 200-h of taught and self-directed study and assessment completion) module on physical healthcare in mental health [ 46 ]. Non-simulation studies evaluated the introduction of personal health plans for patients in a low secure forensic unit together with a single educational session on physical health care for nursing staff [ 43 ]. Specific topics addressed included diabetes [ 68 , 69 ], health assessment [ 46 , 67 ], oral health, IM injectables [ 68 ], vital signs, blood readings, BMI measurement [ 46 ], and cardio-metabolic health [ 35 , 57 ].
In Sung et al’s [ 51 ] RCT, nurses were allocated in a random stratified design to attend 8 × 2-h session about sexual healthcare over a period of 4-w or no intervention. Significant effects were detected in the experimental group relative to the control group for improvements in related knowledge and in attitudes, but not in self-efficacy. The study involved nurses employed both in medical and psychiatric wards (stratified allocation from both) and there was no reported effect of ward-type on outcomes. Pretest- posttest design intervention studies targeted at diabetes found greatly improved clinical judgment in relation to diabetes care and reduced diabetes-related emergency referrals [ 52 ] and similarly impressive improved diabetes-related knowledge [ 69 , 70 ]. Improved attitudes to obesity, obese patients, and supportive roles in caring for obese individuals have been reported across a mixed group of participants and did not differ between mental health and other nurses [ 49 ]. and physical healthcare in general. Happell et al. [ 57 ] reported improved support for a specialist cardiometabolic nurse role following its introduction, however we find this conclusion is unwarranted since it is derived from statistical testing of 14-questionnaire items only one of which was found significant. Interventions aimed at physical healthcare in general found some impressive post- group improvements in knowledge [ 66 , 67 , 68 ], attitudes [ 66 ], and confidence [ 46 , 66 ].
We have conducted a systematic review of the empirical literature about mental health nurses and their attitudes towards, knowledge about, and experiences of physical health care for patients. We took a broad approach to searching the literature and included interventional and observational studies involving real or simulated situations. We included studies involving mental health nursing students and multidisciplinary professional groups in addition to those including only mental health nurses. We contacted study authors to gain additional information and, for the studies using the PHASe [ 11 ] and this elicited significant, previously unpublished information. While we applied no time limits to our comprehensive search we found studies only from as early as 1994, only nine from before 2000, and the median year of publication was 2016. This means that there has been a welcome increase, which we described as a ‘mini-explosion’ in the Introduction, in related empirical work in recent years. The total number of nurses involved in studies, 7549, makes this to our knowledge one of the largest amalgamations of evidence gathered directly from mental health nurses.
However, the overall methodological quality of studies was somewhat limited, particularly interventional studies to improve mental health nurses’ physical healthcare assessment practices and skills. Nevertheless, while many of the included studies examine mental health nurses, and nurses working in mental health settings, this group comprises a heterogeneous collection of individuals of vastly differing experience, preparation, knowledge, and roles. As a result, it is not too surprising that some less well-researched areas have thrown up starkly different results. However, there is consistent evidence that there is a strong association between mental health nurses’ reported attitudes and their reported involvement in physical health care [ 19 , 20 , 42 ]. Similarly, that the nurses who value physical health care also report that they deliver more of it [ 30 ] and those who talk to at least one other discipline about their patients’ physical health do so with multiple professional groups [ 33 ]. Accordingly, fewer resources could be expended on answering these sorts of associational questions in the future.
Our conclusion is that it is now time for a new phase for mental health nursing research related to physical healthcare: efforts must be redoubled to focus on developing and testing interventions to improve nurses’ attitudes, knowledge, and skills. We must ensure that new studies are well-designed and rigorously conducted. More specifically, further research is required to build knowledge about whether the supposed benefits arising from this relationship translate into objectively better practice and indeed better patient outcomes. This would strengthen the case for training to improve attitudes and provide some urgency to better understand what interventions might deliver that outcome. Further, it appears that mental health nurses well-recognise that they require further skills and knowledge related to physical health care across a wide range of areas [ 19 , 30 , 31 , 57 , 71 ]. However, ambivalence and reluctance remains about embracing the change needed to achieve this [ 61 ].
The PHASe was used across multiple studies which allowed for some international and setting-specific comparison of nurses’ attitudes. We found that nurses’ self-perceived practices and attitudes differed significantly between samples from across the world. This, of course, may well reflect different approaches to mental health nurse preparation; for example, in Australia, all pre-registration nurses undergo the same core programme whereas in the UK mental health nursing is a specialist branch of pre-registration training. Therefore, results from Chee et al’s [ 41 ] recent study are enlightening since they reveal equivalent attitudes to physical healthcare specifically, more confidence in delivering physical healthcare but poorer scores in relation to barriers to physical healthcare delivery and smoking cessation. Given the non-equivalence of results on the attitudes to smoking subscale between Chee et al. [ 41 ] and Wynaden et al. [ 44 ], both conducted in Western Australia by related research teams, there are questions about the extent to which results are sample specific. Larger scale, representative data collection in Australia and New Zealand could therefore add significantly to the debate about nurses’ preparation for physical healthcare skills under different preparation regimes. As the PHASe authors’ note, the tool has not been subjected to tests of its stability or criterion validity and improvements in evidence for this would add significantly to the ability to draw sound conclusions from research using the tool. Findings from Osborne et al’s [ 47 ] large hospital-wide survey indicate that the gap in the physical health-related skills addressed by the PHASe is real and of concern.
Apart from the PHASe the literature is peppered with outcomes tools designed for single studies and with little evidence of anything other than face validity and internal consistency. Is it possible, we must ask, that this reflects that researchers are asking the wrong questions i.e., focusing overly on mental health nurses’ attitudes and self-proclaimed knowledge and efficacy when what is now required is a more robust approach to examining their actual knowledge and performance and, crucially, their impact on patient outcomes. Little seems to have been added to the literature on this since Hardy et al. [ 23 ] found no studies to include in their systematic review. Further, Haddad et al’s [ 43 ] study in a low secure forensic setting found nurses scoring favourably on PHASe subscales about attitudes to physical healthcare and to smoking compared with non-forensic nurses in the reference sample, suggesting perhaps that in a setting where length of stay is considerably longer then nurses have more opportunity to engage with patients in this aspect of care. Notably, however, nurses in the same sample compared unfavourably with the reference sample in terms of perceived involvement in actual physical healthcare, a somewhat contradictory finding.
For intervention studies, effect sizes were generally largest, and were in fact sometimes startlingly large, where interventions were targeted and outcomes were knowledge based (e.g., educational studies). This is unsurprising since educational interventions are generally evaluated against criteria that are specifically and directly addressed in the intervention. Outcomes tended to be measured immediately following the training [ 46 , 52 ], but their long term retention is generally not known and neither is any practical beneficial change to practice. The apparent potency of these interventions requires further testing in randomized designs with appropriate follow-up periods.
Some study samples in the current review included non-nursing staff; though their occurrence and representativeness was too limited to allow robust conclusions to be drawn about the relative state of nurses’ knowledge and attitudes within the multidisciplinary team context. Given the current review explicitly focused on mental health nurses then further research exploring the multidisciplinary aspects of physical health care provision is warranted.
Mental health nurses’ ability to provide routine physical healthcare has been highlighted in recent years. Recent literature provides a starting point for future research which must now concentrate on determining the effectiveness of nurse preparation for providing physical health care for people with mental disorder, determining the appropriate content for such preparation, and evaluating the effectiveness both in terms of nurse and patient- related outcomes. At the same time, developments are needed which are congruent with the needs and wants of patients. Perhaps what the included studies best demonstrate is that mental health nurses seem to realise that physical health care is part of their role.
Abbreviations
Medical Subject Headings
Physical Health Attitudes Scale for mental health nurses
Population Intervention Comparator Outcome
Preferred Reporting Items for Systematic Reviews and Meta Analyses
Walker ER, McGee E, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–41. https://doi.org/10.1001/jamapsychiatry.2014.2502 .
Article Google Scholar
Olfson M, Gerhard T, Huang C. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiat. 2015;72(12):1172–81. https://doi.org/10.1001/jamapsychiatry.2015.1737 .
Drope J, Liber AC, Cahn Z, Stoklosa M, Kennedy R, Douglas CE, Henson R, Drope J. Who's still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68(2):106–15. https://doi.org/10.3322/caac.21444 .
Article PubMed Google Scholar
Annamalai A, Kosir U, Tek C. Prevalence of obesity and diabetes in patients with schizophrenia. World J Diabetes. 2017;8(8):390–6. https://doi.org/10.4239/wjd.v8.i8.390 .
Article PubMed PubMed Central Google Scholar
Tomiainen M, Mittendorfer-Rutz E, Bjӧrkenstam C, Suvisaari J, Alexanderson K, Tiihonen J. Antipsychotic treatment and mortality in schizophrenia. Schizophr Bull. 2016;41(3):656–63. https://doi.org/10.1093/schbul/sbu164 .
World Health Organisation. Guidelines for the management of physical health conditions in adults with severe mental disorders. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO
Google Scholar
New South Wales Government. Physical Health Care of Mental Health Consumers. North Sydney: NSW Ministry of Health; 2017. Accessed 29 Jan 2019: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2017_019.pdf
Nursing, Midwifery and Allied Health Professions Policy Unit. Improving the physical health of people with mental health problems: Actions for mental health nurses. London: Department of Health; 2016. Accessed 4 Jan 2019 at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/532253/JRA_Physical_Health_revised.pdf
Royal Australian and New Zealand College of Psychiatrists. Keeping Body and Mind Together: Improving the physical health and life expectancy of people with serious mental illness. Melbourne: Victoria; 2015. Accessed 29 Jan 2019 at: https://www.ranzcp.org/files/resources/reports/ranzcp-keeping-body-and-mind-together.aspx
Department of Health. From values to action: the chief nursing Officer’s review of mental health nursing. London: DOH; 2006.
Robson D, Haddad M. Mental health nurses' attitudes towards the physical health care of people with severe and enduring mental illness: the development of a measurement tool. Int J Nurs Stud. 2012;49(1):72–83. https://doi.org/10.1016/j.ijnurstu.2011.07.011 .
Blythe J, White J. Role of the mental health nurse towards physical health care in serious mental illness: an integrative review of 10 years of UK literature. Int J Ment Health Nurs. 2012;21(3):193–201. https://doi.org/10.1111/j.1447-0349.2011.00792.x .
Happell B, Scott D, Platania-Phung C. Perceptions of barriers to physical health care for people with serious mental illness: a review of the international literature. Issues Ment Health Nurs. 2012;33(11):752–61. https://doi.org/10.3109/01612840.2012.708099 .
Happell B, Platania-Phung C, Scott D. A systematic review of nurse physical healthcare for consumers utilizing mental health services. J Psychiatr Ment Health Nurs. 2014;21(1):11–22. https://doi.org/10.1111/jpm.12041 .
Article CAS PubMed Google Scholar
Collins E, Tranter S, Irvine F. The physical health of the seriously mentally ill: an overview of the literature. J Psychiatr Ment Health Nurs. 2012;19(7):638–46. https://doi.org/10.1111/j.1365-2850.2011.01831.x .
Estabrooks CA, Floyd JA, Scott-Findlay S, O’Leary KA, Gushta M. Individual determinants of research utilization: a systematic review. J Adv Nurs. 2003;43(5):506–20. https://doi.org/10.1046/j.1365-2648.2003.02748.x .
Melnyk BM, Fineout-Overholt E, Feinstein NF, Li H, Wilcox L, Kraus R. Nurses’ perceived knowledge, beliefs, skills and needs regarding evidence-based practice: implications for accelerating the paradigm shift. Worldviews Evid-Based Nurs. 2004;1(4):185193. https://doi.org/10.1111/j.1524-475X.2004.04024.x .
Varnell G, Haas B, Duke G, Hudson K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid-Based Nurs. 2008;5(4):172–81. https://doi.org/10.1111/j.1741-6787.2008.00124.x .
Bressington D, Badnapurkar A, Inoue S, Ma HY, Chien WT, Nelson D, Gray R. Physical health care for people with severe mental illness. Int J Environ Res Public Health. 2018;15(343). https://doi.org/10.3390/ijerph15020343 .
Robson D, Haddad M, Gray R, Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses' attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. 2013;22(5):409–17. https://doi.org/10.1111/j.1447-0349.2012.00883.x .
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097 .
Munn Z, Srtern C, Aromataris E, Lockwood C, Jordan Z. What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol. 2018;18(5):1–9. https://doi.org/10.1186/s12874-017-0468-4 .
Hardy S, White J, Deane K, Gray R. Educating healthcare professionals to act on the physical health needs of people with serious mental illness: a systematic search for evidence. J Psychiatr Ment Health Nurs. 2011;18(8):721–7. https://doi.org/10.1111/j.13652850.2011.01722.x .
Bland AJ, Topping A, Wood B. A concept analysis of simulation as a learning strategy in the education of undergraduate nursing students. Nurse Educ Today. 2011;31:664–70. https://doi.org/10.1016/j.nedt.2010.10.013 .
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid-Based Nurs. 2004;1(3):176–84. https://doi.org/10.1111/j.1524-475X.2004.04006.x .
NIH National Heart, Lung and Blood Institute (n.d.). Study Quality Assessment Tools: Quality Assessment Tool for Observational Cohort and Cross Sectional Studies. Accessed 28 Apr 2018: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools
Critical Appraisal Skills Programme (n.d.). CASP checklist: 10 questions to help you make sense of qualitative research. Oxford: CASP. Available at: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf . Accessed 16 Apr 2019.
Campbell MJ. Statistics at square one (9th edition) T.D.V. Swinscow [revised by M.J. Campbell]: University of Southampton: BMJ publishing group; 1997. Accessed 14 Jun 2018: https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/
Wilson, D.B. (n.d.). Practical meta-analysis effect size calculator. Accessed 11 Mar 2019 https://campbellcollaboration.org/escalc/html/EffectSizeCalculator-SMD-main.php .
Happell B, Platania-Phung C, Scott D. Are nurses in mental health services providing physical health care for people with serious mental illness? An Australian perspective. Issues Ment Health Nurs. 2013;34(3):198–207. https://doi.org/10.3109/01612840.2012.733907 .
Happell B, Platania-Phung C, Scott D. Physical health care for people with mental illness: training needs for nurses. Nurse Educ Today. 2013;33:396–401. https://doi.org/10.1016/j.nedt.2013.01.015 .
Happell B, Platania-Phung C, Scott D. Proposed nurse-led initiatives in improving physical health of people with serious mental illness: a survey of nurses in mental health. J Clin Nurs. 2013;23:1018–29. https://doi.org/10.1111/jocn.12371 .
Happell B, Platania-Phung C, Scott D, Nankivell J. Communication with colleagues: frequency of collaboration regarding physical health of consumers with mental illness. Perspect Psychiatr Care. 2014;50(1):33–43. https://doi.org/10.1111/ppc.12021 .
Happell B, Platania-Phung C, Scott D. What determines whether nurses provide physical health care to consumers with serious mental illness? Arch Psychiatr Nurs. 2014;28:87–93. https://doi.org/10.1016/j.apnu.2013.11.001 .
Happell B, Platania-Phung C, Scott D, Stanton R. Predictors of nurse support for the introduction of the cardiometabolic health nurse in the Australian mental health sector. Perspect Psychiatr Care. 2015;51(3):162–70. https://doi.org/10.1111/ppc.12077 .
Happell B, Platania-Phung C. Cardiovascular health promotion and consumers with mental illness in Australia. Issues Ment Health Nurs. 2015;36:286–93. https://doi.org/10.3109/01612840.2014.981770 .
Happell B, Platania-Phung C, Stanton R, Millar F. Exploring the views of nurses on the cardiometabolic health nurse in mental health services in Australia. Issues Ment Health Nurs. 2015;36:135–44. https://doi.org/10.3109/01612840.2014.901449 .
Happell B, Platania-Phung C, Scott D, Hanley C. Access to dental care and dental ill-health of people with serious mental illness: views of nurses working in mental health settings in Australia. Aust J Prim Health. 2015;21(1):32–7. https://doi.org/10.1071/PY13044 .
Klein TA, Graves JM. A comparison of psychiatric and non-psychiatric nurse practitioner knowledge and management recommendations regarding adolescent mild traumatic brain injury. J Am Psychiatr Nurses Assoc. 2017;23(1):37–49. https://doi.org/10.1177/1078390316668992 .
Clancy R, Lewin TJ, Bowman JA, Kelly BJ, Mullen AD, Flanagan K, Hazelton MJ. Providing physical health care for people accessing mental health services: clinicians’ perceptions of their role. Int J Ment Health Nurs. 2018;28(1):256–67. https://doi.org/10.1111/inm.12529 .
Chee G, Wynaden D, Heslop K. The provision of physical health care by nurses to young people with first episode psychosis: a cross-sectional study. J Psychiatr Ment Health Nurs. 2018;25(7):411–22.
Ganiah AN, Al-Hussami M, Alhadidi M. Mental health nurses’ attitudes and practice toward physical health care in Jordan. Community Ment Health J. 2017;53(6):725–35. https://doi.org/10.1007/s10597-017-0143-6 .
Haddad M, Llewellyn-Jones S, Yarnold S, Simpson A. Improving the physical health of people with severe mental illness in a low secure forensic unit: an uncontrolled evaluation study of staff training and physical health care plans. Int J Ment Health Nurs. 2016;25(6):554–65. https://doi.org/10.1111/inm.12246 .
Wynaden D, Heslop B, Heslop K, Barr L, Lim E, Chee GL, Murdock J. The chasm of care: where does the mental health nursing responsibility lie for the physical health care of people with severe mental illness? Int J Ment Health Nurs. 2016;25(6):516–25. https://doi.org/10.1111/inm.12242 .
Howard L, Gamble C. Supporting mental health nurses to address the physical health needs of people with serious mental illness in acute inpatient care settings. J Psychiatr Ment Health Nurs. 2010;18(2):105112. https://doi.org/10.1111/j.1365-2850.2010.01642.x .
Terry J, Cutter J. Does education improve mental health practitioners' confidence in meeting the physical health needs of mental health service users? A mixed methods pilot study. Issues Ment Health Nurs. 2013;34(4):249–55. https://doi.org/10.3109/01612840.2012.740768 .
Osborn S, Douglas C, Reid C, Jones L, Gardner G. The primacy of vital signs – acute care nurses’ and midwives’ use of physical assessment skills: a cross sectional study. Int J Nurs Stud. 2015;52:952–62 https://doi.org/10.1016/j.ijnurstu.2015.01.014 .
Artzi-Medvedik R, Chertok IRA, Romem Y. Nurses' attitudes towards breastfeeding among women with schizophrenia in southern Israel. J Psychiatr Ment Health Nurs. 19(8):702–8. https://doi.org/10.1111/j.1365-2850.2011.01846.x .
Hunter J, Rawlings-Anderson K, Lindsay T, Bowden T, Aitken LM. Exploring student nurses' attitudes towards those who are obese and whether these attitudes change following a simulated activity. Nurse Educ Today. 2018;65:225–31. https://doi.org/10.1016/j.nedt.2018.03.013 .
Magor-Blatch LE, Rugendyke AR. Going smoke-free: attitudes of mental health professionals to policy change. J Psychiatr Ment Health Nurs. 2016;23(5):290–302. https://doi.org/10.1111/jpm.12309 .
Sung SC, Jiang HH, Chen RR, Chao JK. Bridging the gap in sexual healthcare in nursing practice: implementing a sexual healthcare training programme to improve outcomes. J Clin Nurs. 2016;25:19–20. https://doi.org/10.1111/jocn.13441 2989-3000.
Wynn SD. Improving the quality of care of veterans with diabetes: a simulation intervention for psychiatric nurses. J Psychosoc Nurs Ment Health Serv. 2011;49(2):38–45. https://doi.org/10.3928/02793695-20110111-01 .
Brimblecombe N, Tingle A, Tunmore R, Murrells T. Implementing holistic practices in mental health nursing: a national consultation. Int J Nurs Stud. 2007;44(3):339–48. https://doi.org/10.1016/j.ijnurstu.2006.07.021 .
Delaney KR, Hamera E, Drew BL. Health advanced practice nursing: the adequacy of educational preparation: voices of our graduates. J Am Psychiatr Nurses Assoc. 2009;15(6):383–92. https://doi.org/10.1177/1078390309353070 .
Mwebe H. Physical health monitoring in mental health settings: a study exploring mental health nurses' views of their role. J Clin Nurs. 2017;26(19/20):3067–78. https://doi.org/10.1111/jocn.13653 .
Çelik Ince S, Partlak Günüşen N, Serçe Ö. The opinions of Turkish mental health nurses on physical health care for individuals with mental illness: a qualitative study. J Psychiatr Ment Health Nurs. 2018;25(4):245–57.
Happell B, Stanton R, Hoey W, Scott D. Reduced ambivalence to the role of the cardiometabolic health nurse following a 6-month trial. Perspect Psychiatr Care. 2015;51(2):80–5. https://doi.org/10.1111/ppc.12066 .
Sharp DL, Blaakman SW, Cole RE, Evinger JS. Report from a national tobacco dependence survey of psychiatric nurses. J Am Psychiatr Nurses Assoc. 2009;15(3):172–81. https://doi.org/10.1177/1078390309336746 .
Dorsay JP, Forchuk C. Assessment of the sexuality needs of individuals with psychiatric disability. J Psychiatr Ment Health Nurs. 2009;1(2):93–7. https://doi.org/10.1111/j.1365-2850.1994.tb00025.x .
Quinn C, Platania-Phung C, Bale C, Happell B, Hughes E. Understanding the current sexual health service provision for mental health consumers by nurses in mental health settings: findings from a survey in Australia and England. Int J Ment Health Nurs. 2018;27(5):1522–34. https://doi.org/10.1111/inm.12452 .
Verhaege N, De Maeseneer J, Maes L, Van Heeringen C, Annemans L. Health promotion in mental health care: perceptions from patients and mental health nurses. J Clin Nurs. 2013;22(11–12):1569–78. https://doi.org/10.1111/jocn.12076 .
Johannessen B, Skagestad I, Bergkaasa AM. Food as medicine in psychiatric care: which profession should be responsible for imparting knowledge and use of omega-3 fatty acids in psychiatry. Complement Ther Clin Pract. 2011;17(2):107–12. https://doi.org/10.1016/j.ctcp.2010.08.001 .
Hughes E, Gray R. HIV prevention for people with serious mental illness: a survey of mental health workers' attitudes, knowledge and practice. J Clin Nurs. 2009;18(4):591–600. https://doi.org/10.1111/j.1365-2702.2007.02227.x .
Sharma R, Meurk C, Bell S, Ford P, Gartner C. Australian mental health care practitioners’ practices and attitudes for encouraging smoking cessation and tobacco harm reduction in smokers with severe mental illness. Int J Ment Health Nurs. 2018;27:247–57. https://doi.org/10.1111/inm.12314 .
Parel JT, Khakha DC, Balhara YPS. Do psychiatric nurses have favourable knowledge and attitude towards tobacco prevention among their patients? A cross-sectional study from national capital of India. Asian J Nurs Educ Res. 2018;8(1):01–4. https://doi.org/10.5958/2349-2996.2018.00001.0 .
Fernando A, Attoe C, Jaye P, Cross S, Pathan J, Wessely S. Improving interprofessional approaches to physical and psychiatric comorbidities through simulation. Clin Simul Nurs. 2017;13(4):186193. https://doi.org/10.1016/j.ecns.2016.12.004 .
White J, Hemingway S, Stephenson J. Training mental health nurses to assess the physical health needs of mental health service users: a pre- and post-test analysis. Perspect Psychiatr Care. 2014;50(4):243–50. https://doi.org/10.1111/ppc.12048 .
Hemingway S, Clifton A, Stephenson J, Edward KL. Facilitating knowledge of mental health nurses to undertake physical health interventions: a pre-test/post-test evaluation. J Nurs Manag. 2014;22(3):383–93. https://doi.org/10.1111/jonm.12220 .
Hemingway S, Stephenson J, Trotter F, Clifton A, Holdich P. Increasing the health literacy of learning disability and mental health nurses in physical care skills: a pre and post-test evaluation of a workshop on diabetes care. Nurse Educ Pract. 2015;15(1):30–7. https://doi.org/10.1016/j.nepr.2014.08.003 .
Hemingway S, Trotter F, Stephenson J, Holdich P. Diabetes: Increasing the knowledge base of mental health nurses. Br J Nurs. 2013;22(17):991–5. https://doi.org/10.12968/bjon.2013.22.17.991 .
Nash M. Physical care skills: a training needs analysis of inpatient and community mental health nurses. Ment Health Pract. 2005;9(4):20–3. https://doi.org/10.7748/mhp2005.12.9.4.20.c1896 .
Happell B, Scott D, Nankivell J, Platania-Phung C. Nurses’ views on training needs to increase provision of primary care for consumers with serious mental illness. Perspect Psychiatr Care. 2013;49:210–7. https://doi.org/10.1111/j.1744-6163.2012.00351.x .
Happell B, Scott D, Nankivell J, Platania-Phung C. Screening physical health? Yes! But…: nurses’ views on physical health screening in mental health care. J Clin Nurs. 2013;22:2286–97. https://doi.org/10.1111/j.1365-2702.2012.04325.x .
Birks M, Cant R, James A, Chung C, Davis J. The use of physical assessment skills by registered nurses in Australia: issues for nursing education. Collegian. 2012;20:27–33. https://doi.org/10.1016/j.colegn.2012.02.004 .
Giddens JF. A survey of physical assessment techniques performed by RNs: lessons for nursing education. J Nurs Educ. 2007;46:83–7.
PubMed Google Scholar
Douglas C, Osborne S, Reid C, Batch M, Hollingdrake O, Gardner G. What factors influence nurses’ assessment practices? Development of the barriers to nurses’ use of physical assessment scale. J Adv Nurs. 2014;70:2683–94. https://doi.org/10.1111/jan.12408 .
Phelan M, Stradins L, Amin D, Isadore R, Hitrov C, Doyle A, Inglis R. The physical health check: a tool for mental health workers. J Ment Health. 2004;13(3):277–85. https://doi.org/10.1080/09638230410001700907 .
Shuel F, White J, Jones M, Gray R. Using the serious mental illness health improvement profile [HIP] to identify physical problems in a cohort of community patients: a pragmatic case series evaluation. Int J Nurs Stud. 2010;47(2):136–45. https://doi.org/10.1016/j.ijnurstu.2009.06.003 .
Freed GL, Clark SJ, Sorensen J, Lohr JA, Cefalo R, Curtis P. National assessment of physicians’ breastfeeding knowledge, attitudes, training, and experience. JAMA. 1995;273:472–6.
Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44(2):162–79.
Shore TH, Tashchian A, Adams JS. Development and validation of a scale measuring attitudes toward smoking. J Soc Psychol. 2000;140(5):615–23.
Nash M. Mental health nurses' diabetes care skills - a training needs analysis. Br J Nurs. 2009;18(10):626–30. https://doi.org/10.12968/bjon.2009.18.10.42472 .
Quinn C, Happell B, Browne G. Opportunity lost? Psychiatric medications and problems with sexual function: a role for nurses in mental health. J Clin Nurs. 2011;21:415–23. https://doi.org/10.1111/j.1365-2702.2011.03908.x .
Ford P, Tran P, Keen B, Gartner C. Survey of Australian oral health practitioners and their smoking cessation practices. Aust Dent J. 2015;60:43–51.
Morris C, Waxmonsky J, May M, Giese A, Martin L. Smoking cessation for persons with mental illness: a toolkit for mental health providers: University pf Colorado Denver, CO; 2009. Accessed 19 Mar 2019: https://www.integration.samhsa.gov/Smoking_Cessation_for_Persons_with_MI.pdf
Watson L, Oberle K, Deutscher D. Development and psychometric testing of the Nurses' attitudes toward obesity and obese patients scale (NATOOPS). Res Nurs Health. 2008;31(6):586–93. https://doi.org/10.1002/nur.20292 .
Lasater K. Clinical judgment development: using simulation to create an assessment rubric. J Nurs Educ. 2007;46(11):496–503. https://doi.org/10.1097/NND.0000000000000209 .
Download references
Acknowledgements
The study was partly funded as part of the CUBIC Capability, Capacity and Cultural Change project funded by Nursing and Midwifery Office (NaMO) New South Wales
‘The funding body played no part in the in the design of the study, collection, analysis, interpretation of data, and in writing the manuscript.’
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files] and, where applicable data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and affiliations.
Professor Mental Health Nursing, Centre for Applied Nursing Research (CANR), Western Sydney University, Sydney, Australia
Geoffrey L. Dickens, Cheryl Waters, Evan Atlantis & Bronwyn Everett
South West Sydney Local Health District, Sydney, Australia
Geoffrey L. Dickens
Division of Mental Health Nursing and Counselling, Abertay University, Dundee, Scotland
You can also search for this author in PubMed Google Scholar
Contributions
GLD conceived of and designed the study. GLD, RI, CW, EA, BE contributed to acquisition of data, analysis and interpretation of data. GLD, RI, CW, EA, BE contributed to drafting the manuscript or revising it critically for important intellectual content. GLD, RI, CW, EA, BE gave final approval of the version to be published. GLD, RI, CW, EA, BE agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Geoffrey L. Dickens .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Table S1. Example PICO-style electronic literature search. Example literature search (DOCX 13 kb)
Additional file 2:
Table S2. Controlled intervention evaluation study quality assessment. Study Quality Assessment (controlled intervention study) (DOCX 13 kb)
Additional file 3:
Table S3. Cross-sectional, observational studies quality assessment (adapted from National Heart, Lung, and Blood Institute [ 26 ]. Study Quality Assessment (Cross-sectional and observational studies) (DOCX 16 kb)
Additional file 4:
Table S4. Longitudinal uncontrolled intervention study quality assessment. Study Quality Assessment (uncontrolled intervention studies) (DOCX 14 kb)
Additional file 5:
Table S5. Qualitative study quality assessment. Study Quality Assessment. (Qualitative studies) (DOCX 14 kb)
Additional file 6:
Table S6. Outcome measure content and quality assessment. Quality assessment of outcomes measures used in studies. (DOCX 25 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Dickens, G.L., Ion, R., Waters, C. et al. Mental health nurses’ attitudes, experience, and knowledge regarding routine physical healthcare: systematic, integrative review of studies involving 7,549 nurses working in mental health settings. BMC Nurs 18 , 16 (2019). https://doi.org/10.1186/s12912-019-0339-x
Download citation
Received : 30 October 2018
Accepted : 01 April 2019
Published : 26 April 2019
DOI : https://doi.org/10.1186/s12912-019-0339-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health nurses
- Emergency medicine
- Deteriorating patient
- Educational interventions
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Applied Ethics
- Medical Ethics
- Professional-Patient Relations
- Nurse-Patient Relations
Therapeutic Nurse-Patient Relationship with Individuals Living with A Mental Illness
- December 2021

- Western Michigan University

- Bethel University, Indiana
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Idode Mercy

- Okakwu-Okwuobi Ehaiorimen Emarehi
- Atuba Patricia

- Issues Ment Health Nurs
- Mehrnoosh Pazargadi

- INT J OFFENDER THER

- Gina Panozzo
- Barbara Harris
- Christopher Gordon
- Eugene V. Beresin
- J CLIN NURS

- PERSPECT PSYCHIATR C

- Int J Ment Health Nurs

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Search Close search
- Find a journal
- Search calls for papers
- Journal Suggester
- Open access publishing
We’re here to help
Find guidance on Author Services
Free access
Perspectives and Predictions on the Future of Psychiatric-Mental Health Nursing
- Cite this article
- https://doi.org/10.1080/01612840.2023.2264164
Perspectives and predictions for the future
Challenges of mental health care delivery, innovative technologies for care delivery and pedagogy, disclosure statement, additional information.
- Full Article
- Figures & data
- Reprints & Permissions
- View PDF PDF View EPUB EPUB
In January, the history of mental health care/mental health nursing was reviewed in a special issue of this journal edited by Toby Raeburn, Julie Bradshaw, and Michelle Cleary. In a troubled world with heightened needs for mental health care by victims of violence, disruptive climate change, and pandemic sequelae, where are we going in the future? This special issue on the future of psychiatric-mental health nursing, featuring the voices of many world-renowned nurse clinicians and researchers, offers diverse perspectives and visionary predictions. Mental health nurses are educated differently in different countries, choosing the specialty as undergraduates in some countries (e.g. UK) versus specializing at the masters or doctoral level in others (e.g. USA). Care delivery systems and resources also vastly differ. Yet commonalities can be found among the challenges facing mental health nurses in the twenty first century. For example, countries as diverse as the USA and India struggle with integration of behavioral services and primary health care. Despite a vigorous recovery movement, therapeutic nihilism still abounds regarding conditions such as schizophrenia, borderline personality disorder, and substance use disorders (Thomas, Citation 2018 ).
This special issue includes a variety of conceptual, empirical, and review articles as well as reflective comments by two seasoned psychiatric-mental health nurses (Bonham and Ward-Miller), both of whom have practiced for decades. Manuscripts were received from North America, Australia, Scandinavia, Qatar, and India. Some of the review articles also included research that was conducted in other European and Asian countries. Papers addressed care of children and adolescents as well as adults, and a range of care delivery settings from psychiatric intensive care to community clinics. Altogether, the issue provides an impressive collection of ideas on the future of psychiatric-mental health nursing, although I would have welcomed more submissions from low-income countries. Circumstances are very different in low-income countries with a severe shortage of mental health nurses and an affluent country such as the USA, where the size of the mental health nursing work force is an asset. As Kathy Delaney ( Citation 2023 , this issue) points out, advanced practice registered nurses (APRNs) are one of the largest provider groups of psychiatric services in the USA, and RNs comprise a large majority of the inpatient psychiatric workforce. It is my hope that readers from less advantaged parts of our global village will respond to these articles, adding to the collegial conversation.
The articles in this issue can be organized into 3 themes: (1) perspectives and predictions for the future; (2) challenges of mental health care delivery; and (3) innovative technologies for care delivery and pedagogy. Woven all through the issue are foundational tenets of the philosophical and theoretical stance of psychiatric nursing. Especially prominent were references to the foundational scholarly work of Hildegard Peplau ( Citation 1952 ), who so beautifully elucidated the transformational power of the therapeutic nurse-patient relationship. Principles of her theory of Interpersonal Relations are explicit in the theoretical framework for virtual care offered by Brooke Finley et al. ( Citation 2023 , this issue).
Victoria Soltis-Jarrett ( Citation 2023 , this issue) recalls a number of oppressive societal conditions that were prevalent in the history of mental health nursing (drawing from the January issue of IMHN) and then directs reader attention to specific actions that must be taken now. Her energetic agenda includes reclaiming community mental health nursing and achieving more enlightened public policy (including full practice authority for nurse practitioners, who are still restricted in many American states by the requirement of physician oversight of their practice). She presents a successful federally funded model of educating primary care nurse practitioner students with psychiatric-mental health practitioner students, in which they learn to collaborate during graduate school (e.g. “curbside consults” and “warm handoffs”) (Soltis-Jarrett, Citation 2023 , p. 1073). She also calls for change in undergraduate nursing education, to expose students in the psychiatric nursing course to community treatment settings, not just hospitals and long-term care settings.
Kathy Delaney’s paper ( Citation 2023 , this issue) not only highlights underserved populations in the USA (uninsured, unstably housed, incarcerated), but also offers specific recommendations for better collaboration among RNs, advanced practice nurse practitioners (APRNs) and psychiatric-mental health nurse practitioners (PMHNPs) to meet the needs of these populations. She recommends reform of outpatient delivery systems and processes, such as providing services beyond standard times of 9-5, and in places other than mental health clinician offices, such as schools and community settings. Inpatient settings should return to a focus on “restoring engagement” rather than a “surveillance approach” (McAllister et al. 2021, cited in Delaney, Citation 2023 , this issue).
After reviewing worldwide adversity facing psychiatric-mental health nursing (difficulty recruiting nurses to the specialty, low job satisfaction in the workforce, deficit of mental health nurses involved in policymaking), Australian authors Cleary et al. ( Citation 2023a , this issue) summarized factors that can enable our specialty to overcome adversity. They emphasize our skills in relationship-building, collaboration, resilience, and innovation. They advocate increased international networking. Additionally, they recommend drawing on the wisdom of mental health nurses with decades of experience. In a separate commentary, Cleary et al. ( Citation 2023b , this issue) offer lessons for mental health nurses about toxic leadership.
In accord with the recommendation by Cleary et al. this issue includes commentary by Beth Bonham ( Citation 2023 , this issue) and Sharon Ward-Miller ( Citation 2023 , this issue), both “wise women” with extensive psychiatric experience. Dr. Bonham is a child and adolescent specialist and a founding member of the International Society of Psychiatric-Mental Health Nurses. Dr. Ward-Miller studied at Rutgers when Peplau was there, at NYU when Suzanne Lego was there (and Martha Rogers was the dean), and at Case Western, where she received her Doctor of Nursing Practice under the mentorship of Joyce Fitzpatrick at age 70. She continues to practice and contribute to the literature (e.g. Ward-Miller et al. Citation 2021 , an account of the psychiatric nursing response to COVID-19 at New York-Presbyterian Westchester Behavioral Health Center, during those terrifying early days when the pandemic created a global existential crisis).
Care of patients in psychiatric intensive care (PICU), a challenging environment for humanistic psychiatric nursing practice, was the topic of an integrative review article by Swedish author Martin Salzmann-Erikson ( Citation 2023 , this issue). The author sought to synthesize research conducted within the past 5 years. Included were 47 articles about intensive psychiatric care being delivered to children and adolescents as well as adults. Most commonly, the patients had been involuntarily hospitalized, and most had engaged in assaultive behaviors prior to hospitalization. Discouraging descriptions by patients of sensory deprivation and restrictive practices were reminiscent of a long line of previous research in nursing and other mental health disciplines. However, Salzmann-Erikson concluded that there is some movement toward patient-empowering models of care. He called for multidisciplinary collaboration in the future, pointing out that most of the studies are conducted in disciplinary silos (physicians examining medically-focused interventions and nurse researchers studying nurses).
Australian author Lisa Wright et al. ( Citation 2023 , this issue) explored barriers influencing the use of sensory approaches in acute psychiatric units, despite studies demonstrating their efficacy. Sensory approaches include a variety of therapeutic interventions involving equipment and environmental modifications to create sensory experiences (e.g. weighted blankets, aromatherapy, stress balls, fidget items). This paper depicts a multidisciplinary team co-designing a theory-informed strategy to increase the use of sensory approaches in one acute psychiatric unit.
The provision of physical health care for individuals with severe mental illness in India was the focus of a survey in India. Jothamani Gurusamy et al. ( Citation 2023 , this issue) surveyed nurses who provided direct care in a tertiary-level psychiatric center serving 1,000 outpatients and 550 inpatients. Not all of the survey respondents were mental health specialists, but 77% had a Bachelor’s degree in nursing. Although study participants exhibited positive attitudes toward providing physical care for individuals with severe mental illness, some lacked confidence in offering exercise advice, cancer screening, and several other important aspects of comprehensive care. As shown frequently in previous research, barriers to provision of physical care included nurse workload.
A focused ethnography conducted within the cultural context of an Australian state was conducted by Sharon Picot et al. ( Citation 2023 , this issue) to explore provision of spiritual care by mental health nurses to people with enduring mental illness who were now facing death from a life-limiting illness. The nurses described a dominant biomedical culture in which they were reluctant to bring up spiritual care interventions to the treatment team. They deplored the lack of end-of-life plans. However, they described “pockets of spiritual care” happening, permitting the voices of patients facing death to be heard. Nurses were skillful in assessing spiritual needs even when patients were psychotic. Furthermore, they had the expertise & willingness to provide spiritual care, which they viewed as integral to the culture of nursing.
We turn now to the topic of innovative technologies, which are creating widespread enthusiasm– along with some caution regarding risk of cyber attacks and data breaches. In the article by Brooke Finley et al. ( Citation 2023 , this issue), virtual care (VC) is illustrated by a case example. Virtual care, also called telehealth care, enables many patients to receive care who would not have the opportunity otherwise, as in the case of the client V.M. in this paper. In fact, VC became essential for many isolated psychiatric patients during the COVID-19 pandemic. Many intriguing issues have arisen, however, such as the added intimacy during a Zoom session of the psychiatric nurse seeing the patient’s home environment and the patient likewise seeing the nurse’s personal spaces. Delivery of care via distance technologies has rapidly expanded without a theoretical framework. The nurse-patient relationship could be hindered by inappropriate media usage. Therefore, Finley and colleagues suggest a blend of Peplau’s Interpersonal Relations Theory (IRT) and Media Richness Theory (MRT) to guide modern psychiatric-mental health nursing virtual care practice and research in the twenty first century.
In a narrative review paper, Nashwan et al. ( Citation 2023 , this issue) describe the potential of artificial intelligence (AI) in early detection of mental health problems and in clinical decision-making. This body of literature, although small, also suggests the promise of AI regarding tracking of patients’ medication adherence and improving detection of risk for post-traumatic stress disorder and suicide. Chatbots and virtual health assistants are already being used to provide therapeutic interventions, although they should complement rather than replace humanistic care by psychiatric-mental health nurses. Limitations of AI, such as AI algorithms that may discriminate against patients, are acknowledged.
Although it may seem “low-tech,” the telephone is still a valuable technological tool. In Anne-Marie Wangel’s ( Citation 2023 ) paper, we learn of nurses skillfully performing telephone triage in a child and adolescent service facility in Sweden. As noted by authors of other papers in this special issue, the higher incidence of children and adolescents with depression is a global concern. Wangel et al. studied nurses performing triage by phone, prior to a physical clinic visit, using a standardized screening tool. A typical call was about 45 min, and the nurse always aimed to speak directly to the child or adolescent, not just to the parent/guardian. Critical incident technique was used by the researchers to elicit examples of triage where the nurses found it easy (or difficult) to assess the child’s status and level of need for mental health services. Interestingly, an increasing number of adolescents are self-initiating telephone contact, with or without their guardians’ awareness. Swedish law permits this, and the nurses welcomed it.
Our attention turns to pedagogy in the article by Jennifer Moyer ( Citation 2023 , this issue). She provides an integrative review of virtual reality (VR) simulation in teaching undergraduate students psychiatric nursing. VR uses 3-dimensional characteristics to present students with realistic clinical scenarios via a computer, smartphone, or other device. Research reviewed in this article was conducted in Israel, Korea, China, Sweden, Canada, and the USA. Moyer concluded that VR simulation is equivalent to (or superior to) traditional pedagogical methods, producing gains in both knowledge and skills of the students. An unanticipated problem was motion sickness, suggesting that screening students for this is necessary. Further VR research would be useful, especially regarding medication administration.
Creating a positive learning culture is imperative for encouraging undergraduate nursing students to consider a career in psychiatric-mental health nursing. Roach and Tadesse ( Citation 2023 , this issue) describe a qualitative study involving 60 students who were asked to write reflections on their backgrounds and perceptions of mental health stigma. Although the students’ backgrounds differed, mental illness had often been stigmatized or not discussed in their families. They reported that stigma decreased through clinical and personal experiences, especially sharing their own stories of mental health issues (“it is OK not to be OK”). Although the course assignment did not ask for students to reveal personal experiences, many of them did so, leading Roach and Tadesse to suggest trauma-informed pedagogy. Students must be able to manage their own mental health issues in order to provide empathic and compassionate care of others, as Peplau ( Citation 1952 ) emphasized long ago.
This special issue on the future or psychiatric-mental health nursing provides rich food for thought. I know Peplau would be pleased by the spirit of innovation exhibited by the authors of these papers on delivery of care via distance technologies. She would echo Soltis-Jarrett’s call for nurses to join their professional organizations, as she herself served as a distinguished president of the American Nurses Association. Undoubtedly, Peplau would also be pleased that psychiatric-mental health specialty still preserves the optimism that she displayed toward the abiding potential for patients to heal, and nurses themselves to grow, as they partner together in the healing process.
No potential conflict of interest was reported by the authors.
- Bonham, B. (2023). The future of psychiatric-mental health nursing. Issues in Mental Health Nursing , 44 (10), 1064–1067. PubMed Web of Science ® Google Scholar
- Cleary, M., West, S., & Hungerford, C. (2023a). Mental health nurses overcoming adversity: A discursive review. Issues in Mental Health Nursing , 44 ( 10 ), 944–950. https://doi.org/10.1080/01612840.2023.2236698 PubMed Web of Science ® Google Scholar
- Cleary, M., West, S., & Hungerford, C. (2023b). Toxic leadership: Lessons for mental health nurses. Issues in Mental Health Nursing , 44 ( 10 ), 1059–1063. https://doi.org/10.1080/01612840.2023.2193629 PubMed Web of Science ® Google Scholar
- Delaney, K. (2023). The future of the psychiatric mental health work force: Using our skill set to address incongruities in mental health care delivery. Issues in Mental Health Nursing , 44 ( 10 ), 933–943. https://doi.org/10.1080/01612840.2023.2252498 PubMed Web of Science ® Google Scholar
- Finley, B., Shea, K., Gallagher, S., Palitsky, R., & Gauvin, J. (2023). A theoretical framework for conducting psychiatric mental health nursing virtual care and research. Issues in Mental Health Nursing , 44 (10), 1002–1008. PubMed Web of Science ® Google Scholar
- Green, S., Sjostrum, K., & Wangel, A.-M. (2023). Nurses’ perceptions of telephone triage in child and adolescent mental health services: An enhanced critical incident technique study. Issues in Mental Health Nursing , 44 (10), 974–983. PubMed Web of Science ® Google Scholar
- Gurusamy, J., Amudhan, S., Menen, M., Veerabhadraih, K., & Damodharan, D. (2023). Barriers and needs of mental health nursing practitioners towards provision of physical healthcare for individuals with severe mental illness: Findings from a cross-sectional survey in India. Issues in Mental Health Nursing , 44 (10), 1009–1019. PubMed Web of Science ® Google Scholar
- Moyer, J. (2023). Virtual reality simulation applications in prelicensure psychiatric nursing curricula: An integrative review. Issues in Mental Health Nursing , 44 ( 10 ), 984–1001. https://doi.org/10.1080/01612840.2023.2243330 PubMed Web of Science ® Google Scholar
- Nashwan, A., Gharib, S., Alhadidi, M., El-Ashry, A., Alamgir, A., Al-Hassan, M., Khedr, M., Dawood, S., & Abufarsakh, B. (2023). Harnessing artificial intelligence: Strategies for mental health nurses in optimizing psychiatric patient care. Issues in Mental Health Nursing , 44 (10), 1020–1034. PubMed Web of Science ® Google Scholar
- Peplau, H. (1952). Interpersonal relations in nursing . G. P. Putnam’s Sons. Google Scholar
- Picot, S., Harrington, S., & Fuller, J. (2023). Finding the hidden professional culture of mental health nursing: Spiritual care for individuals with a co-morbid life-limiting illness. Issues in Mental Health Nursing , 44 ( 10 ), 951–959. https://doi.org/10.1080/01612840.2023.2246064 PubMed Web of Science ® Google Scholar
- Roach, A., & Tadesse, R. (2023). “It is OK not to be OK”: Nursing students’ backgrounds and perceptions of mental health stigma and implications for future mental health nursing education. Issues in Mental Health Nursing , 44 (10), 1050–1058. PubMed Web of Science ® Google Scholar
- Salzmann-Erikson, M. (2023). An integrative review on psychiatric intensive care. Issues in Mental Health Nursing , 44 (10), 1035–1049. PubMed Web of Science ® Google Scholar
- Soltis-Jarrett, V. (2023). The future of psychiatric-mental health nursing: Observe, reflect, and take action to empower knowledge and practice for the greater good. Issues in Mental Health Nursing , 44 (10), 1071–1079. PubMed Web of Science ® Google Scholar
- Thomas, S. P. (2018). Finding inspiration from the philosophy of Maurice Merleau-Ponty for the practice of psychiatric-mental health nursing. Archives of Psychiatric Nursing , 32 ( 3 ), 373–378. https://doi.org/10.1016/j.apnu.2017.11.029 PubMed Web of Science ® Google Scholar
- Ward-Miller, S. (2023). The future of psychiatric-mental health nursing: Reflections on my 50 years as a psychiatric mental health clinical specialist. Issues in Mental Health Nursing , 44 (10), 1068–1070. PubMed Web of Science ® Google Scholar
- Ward-Miller, S., Farley, E., Espinosa, L., Brous, M., Giorgi-Cipriano, J., & Ferguson, J. (2021). Psychiatric-mental health nursing in the international year of the nurse and COVID-19: One hospital’s perspective on resilience and innovation- past, present and future. Archives of Psychiatric Nursing , 35 ( 3 ), 303–310. https://doi.org/10.1016/j.apnu.2020.11.002 PubMed Web of Science ® Google Scholar
- Wright, L., Bennett, S., Meredith, P., & Doig, E. (2023). Planning for change: Co-designing implementation strategies to improve the use of sensory approaches in an acute psychiatric unit. Issues in Mental Health Nursing , 44 ( 10 ), 960–973. https://doi.org/10.1080/01612840.2023.2236712 PubMed Web of Science ® Google Scholar
Reprints and Corporate Permissions
Please note: Selecting permissions does not provide access to the full text of the article, please see our help page How do I view content?
To request a reprint or corporate permissions for this article, please click on the relevant link below:
Academic Permissions
Obtain permissions instantly via Rightslink by clicking on the button below:
If you are unable to obtain permissions via Rightslink, please complete and submit this Permissions form . For more information, please visit our Permissions help page .
- Back to Top
Related research
People also read lists articles that other readers of this article have read.
Recommended articles lists articles that we recommend and is powered by our AI driven recommendation engine.
Cited by lists all citing articles based on Crossref citations. Articles with the Crossref icon will open in a new tab.
- People also read
- Recommended articles
To cite this article:
Download citation, your download is now in progress and you may close this window.
- Choose new content alerts to be informed about new research of interest to you
- Easy remote access to your institution's subscriptions on any device, from any location
- Save your searches and schedule alerts to send you new results
- Export your search results into a .csv file to support your research
Login or register to access this feature
Register now or learn more
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Mental health in nursing
A student's perspective.
Halsted, Candis DNP-PMHNP, RN; Hart, Virginia T. DNP, RN, PMHNP-BC
At Radford University School of Nursing in Radford, Va., Candis Halsted recently earned her DNP and Virginia T. Hart is an assistant professor and interim psychiatric mental health NP program coordinator.
The authors have disclosed no financial relationships related to this article.
A stigma around mental health issues within healthcare and nursing itself has created a culture of perfectionism in the workplace, and nurses struggle to live up to the expectations while pushing aside their feelings, thoughts, and needs. Inspired by one author's personal experiences, this article explores mental health issues many nurses confront today.
Inspired by one author's personal experiences, this article explores mental health issues many nurses confront today.

I DECIDED TO RETURN to school in 2015 after practicing as a nurse in various settings for 7 years. I subscribe to the adage that knowledge is power. My drive for additional education and experience was based on my desire to achieve a higher status, assume more control over my practice, and to garner more respect from other healthcare professionals. As I immersed myself in my graduate studies, however, I found my desires, self-image, and professional viewpoint had changed.
I have always endeavored to be the best student, greatest employee, and most dependable teammate. Those efforts took on a feverish intensity during periods of transition—student to nurse, nurse to working mother, mother and nurse to professional student. Good was not good enough, and my drive to be the best and greatest was an integral part of my self-worth. Unfortunately, it led to anxiety, depression, hopelessness, and isolation that negatively impacted my education, practice, and personal life.
It was not until my clinical rotations as a psychiatric-mental health NP student that I came to realize the magnitude of the situation. There I was, taking courses on trauma-informed care and giving my patients tools for building self-efficacy, self-compassion, and coping skills while simultaneously ignoring my own needs.
Having left the workplace to focus on my online studies, I was isolated, lacking confidence, feeling overwhelmed, and overcompensating for some perceived shortcoming that I could not even define. I felt hopeless and defeated. I experienced bouts of anxiety and depression so intense I lost my sense of purpose. I considered dropping out of school many times, but I gave in to the expectations of others. I forced myself to continue pushing aside my own needs, persisting despite my growing depression and anxiety.
Looking back, I had so many chances to speak up and reach out for help. I could have spoken with nurse managers, coworkers, fellow students, and faculty a hundred different ways on so many occasions. Instead, I allowed the culture of silence and my own perfectionism to rule.
At my lowest point, I made the life-altering decision to reach out for help—first to my husband, then a therapist, a fellow student, and finally my school faculty. With their assistance, some serious self-reflection, and a lot of self-help reading, I am working to address my mental illness and establish a sense of well-being.
That is not to say that I have it all figured out. I still struggle many days to keep faith in my strengths and abilities. The things I have learned and witnessed, the obstacles I have encountered and overcome, whether academic, professional, or personal, have humbled me and restored my desire to return to the love, service, and justice at the core of my professional drive and practice. I am once again prioritizing my values and making sure my actions reflect them. Among those values is the desire to work toward the unification of our profession and to advocate for policy changes that support the mental health of all nurses. Inspired by my personal experiences, this article explores mental health issues many nurses confront today.
A pervasive problem
Although mental health and suicide among nurses have emerged as areas of professional concern in recent years, little research or literature exists regarding profession-specific risk factors, prevalence of mental illness, and suicide rates. With little to no concrete statistics to draw from, the true incidence of mental illness within the nursing profession is unknown. Furthermore, little has been done to bring these problems to the attention of the general public or to acquire the recognition and support of the professional community. 1-3
What can be found are decades of research stating that nursing is psychologically demanding and can contribute to poor mental health in a variety of ways, such as depression, anxiety, secondary trauma, compassion fatigue, and burnout. 1-7 The occupational hazards of nursing can also compromise work-life balance. Add to this various individual risk factors such as genetic predisposition or history of personal trauma, as well as the fact that academic standards for the profession favor those who are exacting and high-performing. It stands to reason that nurses are in jeopardy of significantly elevated levels of stress and maladaptive coping. 5,8 When ongoing, this can lead to impaired functioning. In the professional setting, impairment has been correlated with increased risk for errors, patient harm, and clinical ineffectiveness. 9
Mental illness can be defined as clinically significant impairment in social, conceptual, and practical functioning. 9,10 Although very common, mental illness is often untreated. 11 One in five adults will have some experience with mental illness each year, but less than half will receive treatment. 11
Nursing has a hidden culture of stigma and silence regarding mental illness, which serves to minimize and overshadow those experiencing clinically significant distress. 6,12 Competition, intimidation, and bullying among nurses are pervasive across practice and in academic settings. 13,14 These behaviors can breed psychologically hazardous and hostile environments. Fear of becoming a target may result in blame, shame, self-stigmatization, isolation, and suffering in any individual with potentially undesirable characteristics in such settings, regardless of his or her mental health status. Such abuses and fear can promote conformity and negatively impact disclosure and help-seeking behaviors in stressed, distressed, and impaired individuals. 1,2,5,13
The issue is exacerbated by a lack of respect and recognition for nursing that is still present within the healthcare culture at large. The traditional hierarchy holds physicians as experts, not nurses. Even advanced practice nurses are diminished, often referred to as “mid-level providers” and “physician extenders.” 15 These attitudes undermine the autonomy and dignity of nurses, especially when they collaborate with other healthcare disciplines. 14
In addition, while healthcare entities and societies champion the rights of the patient, the need to protect the basic human dignity and professional image of nurses is often overlooked. 14 Fundamental protections and rights for nurses are being compromised every day when we are expected to tolerate long hours, interrupted (or nonexistent) breaks, heavy patient caseloads, incivility, and even violence in the workplace. Nurse unions across the country are threatening walkouts and going on strike because of the failure of hospitals to address these issues. 16,17 The situation is not helped by the fact that guiding and governing bodies for nursing practice are numerous yet, in my opinion, self-segregated.
Systemic change
Although some organizations have created emotional wellness programs, a cohesive or public effort to address systemic problems is lacking. 1-3 Until employers, boards of nursing, and nursing organizations place the same importance on the well-being of nurses and risk mitigation, nurses may continue to suffer in silence. Within the currently disjointed system, we cannot hope to make substantive changes without offering our passion and expertise as well as identifying and supporting means for promoting self-care and wellness among the thousands of practicing nurses and preprofessionals experiencing distress or symptoms of mental illness.
Pressures and barriers to mental health and help-seeking extend to the academic setting. 4-5 For professional nurses returning to school, the pressure associated with practice and professional expectations may be exacerbated by their increased need to balance a variety of personal and/or family responsibilities, deadlines, financial obligations, leisure time, and peer competitiveness. Despite these contributory risk factors, I have seen few—if any—educational programs for health and helping disciplines, such as nursing, medicine, and social work, place value on assessing students' stress and distress. In commiserative discussions with others doing graduate work in nursing, social work, occupational therapy, and physical therapy, I have yet to meet anyone who felt the faculty took action to address the genuine difficulties many of them faced in balancing their lives. In short, students (myself included) feel devalued by the lack of respect, holistic consideration, and mentorship they encounter. Academic learning environments have a great need to support improvement of the emotional well-being and psychological resiliency of students and for improving the accessibility of support, counseling, and mental health resources. 4,5
I encourage you to take a long, hard look at yourself and those around you. If you are struggling, please reach out to someone you trust and let them know you are not okay. If you are not sure that what you are experiencing is normal or cause for concern, there are many websites that provide education and information on how to identify mental health problems, as well as hotline crisis intervention services and referrals to local counseling. These websites often have articles and tips on how to improve your mental health through physical, spiritual, and psychological self-care. (See Mental health resources .)
No mental health concern is too big or too small. If you are not well, talk to a friend, family member, professional, or help hotline. If you suspect a coworker, colleague, or student needs help, please reach out. Something as simple as asking if they are okay and giving them the space and time to express their feelings can make all the difference. As Edward Everett Hale once said, “I am only one, but still I am one. I cannot do everything, but still I can do something. And because I cannot do everything, I will not refuse to do the something that I can do.” 18 We owe it to ourselves, our profession, our patients, and their families to seek help and to offer help to our fellow nurses in need.
For anyone requiring immediate crisis intervention or assistance finding a local mental health provider, the following resources are available:
- Mental Health America: 1-866-400-6428 for referrals, 1-800-273-8255 for crisis
- National Alliance on Mental Illness HelpLine 1-800-950-6264
- National Suicide Prevention Helpline 1-800-273-8255
Crisis Text Line available 24 hours a day, text “HOME” to 741741
Mental health resources
- American Psychological Association
- www.apa.org
- American Psychiatric Nurses Association (APNA)
- www.apna.org
- MentalHealth.gov
- www.mentalhealth.gov
- National Alliance on Mental Illness
- www.nami.org
- National Suicide Prevention Lifeline
- https://suicidepreventionlifeline.org
- Crisis Text Line
- www.crisistextline.org
- Cited Here |
- View Full Text | PubMed | CrossRef
- PubMed | CrossRef
anxiety; compassion fatigue; depression; emotional wellness; mental health; nursing; suicide prevention
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Assessing mental health in vulnerable adolescents, anorexia nervosa in adolescents: an overview, focus on pharmacotherapy for depression, managing loneliness and chronic illness in older adults, improving mental health education in nursing school.
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
| Property | Value |
|---|---|
| Status | |
| Version | |
| Ad File | |
| Disable Ads Flag | |
| Environment | |
| Moat Init | |
| Moat Ready | |
| Contextual Ready | |
| Contextual URL | |
| Contextual Initial Segments | |
| Contextual Used Segments | |
| AdUnit | |
| SubAdUnit | |
| Custom Targeting | |
| Ad Events | |
| Invalid Ad Sizes |
Access provided by
Violence toward staff in the inpatient psychiatric setting: Nurses' perspectives: A qualitative study
Download started
- Add to Mendeley

Participants
Conclusions.
- Workplace violence
- Psychiatric nurses
- Mental health nurses
- Impact of workplace violence
- Qualitative research

Get full text access
Log in, subscribe or purchase for full access.
Article metrics
Related articles.
- Download Hi-res image
- Download .PPT
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- Current Issue
- List of Issues
- Special Issues
- For Authors
- About Open Access
- Author Information
- Author Services
- Permissions
- Researcher Academy
- Submit a Manuscript
- Journal Info
- Aims and Scope
- Activate Online Access
- Contact Information
- Editorial Board
- Information for Advertisers
- New Content Alerts
- Nursepoint by Elsevier Australia
- More Periodicals
- Find a Periodical
- Go to Product Catalog
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

- Institutional Access: Log in to ScienceDirect
- New Subscriber: Claim access with activation code. New subscribers select Claim to enter your activation code.
Academic & Personal
Corporate r&d professionals.
- Full online access to your subscription and archive of back issues
- Table of Contents alerts
- Access to all multimedia content, e.g. podcasts, videos, slides
- Open access
- Published: 24 September 2024
Influence of self-compassion on fatigue and psychological wellbeing among psychiatric nurses
- Sahar Behilak 1 , 2 ,
- Saleh Abdullah 3 ,
- Gellan K. Ahmed ORCID: orcid.org/0000-0002-5830-4117 4 &
- Ola Ali Abd El-Fatah Ali Saraya 5
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery volume 60 , Article number: 113 ( 2024 ) Cite this article
Metrics details
Psychiatric mental health nurses often work in highly demanding environments and situations and are exposed to multiple work-based stressors simultaneously. We aimed to explore the influence of self-compassion on fatigue and psychological wellbeing, and to evaluate the possible contributing factors for self-compassion, fatigue, and psychological wellbeing among psychiatric nurses. A descriptive correlational study using a convenience sample was used to employ 50 psychiatric nurses. Participants categorized into three groups based on their scores on The Self-Compassion Scale (SCS-SF): Group 1: low self-compassion, Group 2: moderate self-compassion, and Group 3: high self-compassion. All participants were assessed by socio-demographic data questionnaire, Fatigue Assessment Scale (FAS), and Psychological Wellbeing Scale.
Regarding FAS and wellbeing, group 1 had the highest mean of both scores, whereas group 3 had the lowest mean of both scores. Psychiatric nurses with high self-compassion were significantly more likely to be male, have a lower overall fatigue score, and have better psychological wellbeing. Psychiatric nurses with high fatigue scores were more likely to be female, married, have diploma, have less self-compassion, and have poorer psychological wellbeing.
Conclusions
Psychiatry nurses with higher self-compassion had lower fatigue score and better psychological wellbeing. Gender and education level were significant factors for self-compassion and fatigue.
Self-compassion is the capacity to exhibit empathy or compassion for oneself when faced with failure, insufficiency, or suffering [ 1 , 2 ]. Several studies have indicated that self-compassion can assist individuals in coping with adverse life situations and minimizing their harmful outcomes, such as burnout and fatigue [ 3 , 4 ].
Three interrelated elements have been identified to determine self-compassionate responses to personal negative feelings and events [ 5 ]: self-kindness as opposed to self-judgment, a sense of common humanity as opposed to isolation, and mindfulness as opposed to over-identification. Self-kindness is a compassionate attitude toward oneself in the presence of pain. Common humanity refers to the understanding that life’s stressors and experiences are shared human experiences, as opposed to a perception that they are unique. Mindfulness is a kind of balanced awareness that neither minimizes nor magnifies the discomfort of our current experience [ 6 ] as we cannot demonstrate self-compassion without recognizing that we are experiencing suffering [ 7 ]. It has been claimed that self-compassion can improve the mental health of healthcare providers by encouraging optimism, happiness, and a broader perspective on challenges [ 8 ].
An issue that nursing staff face at work is fatigue, which inhibits them from functioning properly. Fatigue is a critical challenge and a significant problem among nurses who experience higher workloads, which further causes various issues, such as distress and burnout. Fatigue has an adverse influence on nurses and causes physical, cognitive, and emotional issues that may affect their quality of life. In contrast, self-compassion helps nurses enhance their ability to manage emotions and prevent some negative outcomes of nursing, such as burnout and fatigue [ 9 ].
Psychiatric mental health nurses frequently work in extremely demanding settings and circumstances and are exposed to various stressors instantly. Stressors, including work pressure, excessive complexity, skipping breaks, longer work hours than agreed upon, lack of resources and staff, and unsatisfactory patient outcomes, can make psychiatric nurses feel psychologically depleted and put them at risk of mental illness. Self-compassion improves an individual’s overall wellbeing and health [ 10 ]. Self-compassion may serve as a protective factor and help psychiatric nurses maintain psychological wellness [ 11 , 12 , 13 ]. Unfortunately, the impact of self-compassion on the health and wellbeing of psychiatric nurses is less understood. Moreover, studies examining the relationship between fatigue and self-compassion and psychological wellbeing among nurses are limited [ 14 ], particularly psychiatric nurses, worldwide and in Egypt [ 15 , 16 , 17 ].
Individuals with a high degree of self-compassion hardly ever adopt maladaptive coping strategies, such as self-criticism, contemplation, thought suppression, and avoidance, when confronting their own experiences. Improving one’s own self-compassion can also effectively reduce fatigue [ 5 ]. Consequently, identifying the relationship between self-compassion, fatigue, and psychological wellbeing might enhance our understanding of how self-compassion may translate into reduced fatigue and increased psychological wellbeing among psychiatric nurses.
Although self-compassion can promote positive wellbeing among adults, there is a lack of research in this area that should be addressed. This study was designed to explore the influence of self-compassion on fatigue and psychological wellbeing among psychiatric nurses.
This study was designed to assess the influence of self-compassion on fatigue and psychological wellbeing among psychiatric nurses. Also, to evaluate the possible contributing factors for self-compassion, fatigue, and psychological wellbeing among psychiatric nurses.
A cross-sectional study was conducted with convenience sample of 50 registered nurses working in the Psychiatric Department of the Psychiatry and Neurology Hospital of [Assiut University] between October 2023 and February 2024. The questionnaire was distributed 3 days each week throughout three work shifts (morning shift from 10 a.m. to 12 p.m., afternoon shift from 4 p.m. to 6 p.m., and night shift from 9 p.m. to 11 p.m.). A pilot study was conducted involving 10 nurses working at the Psychiatric Department of the Psychiatry and Neurology Hospital of Assiut University to evaluate the questionnaire’s clarity, feasibility, and applicability. Modifications were made to evaluate any additional problems or difficulties, such as question sequencing and clarity. The nurses included in this pilot study were excluded from the overall sample.
Tools of the study: This study used a specially structured assessment questionnaire that was designed by the researchers after reviewing the different related studies and literature to collect the required data; the assessment questionnaire was categorized as follows:
Sociodemographic data: This was developed by researchers based on previous literature. It included age, sex, residence, educational level (diploma (2 years) or Bachelor (4 years), marital status, years of experience, the number of working hours per week, working shifts per month, the number of nurses caring for patients during a shift, and previous training about self-compassion.
The Self-Compassion Scale—Short Form (SCS-SF): It is a widely recognized tool for assessing self-compassion. It is a condensed version of the original Self-Compassion Scale (SCS), developed by Kristin Neff, which includes 26 items. The short form contains 12 items that cover the same six components: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. This scale provides a quick yet effective way to measure self-compassion, maintaining strong psychometric properties similar to the full version. This scale consists of 12 items scored on a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always) [ 18 ]. Cronbach’s alpha for the scale is 0.86 [ 19 ]. The total self-compassion is the sum of all items divided by the number of items. The mean and standard deviation of the total scores for the studied sample were calculated. Individuals with scores greater than one standard deviation above the mean were classified as belonging to the high self-compassion, while those with scores lower than one standard deviation below the mean were categorized as belonging to low self-compassion. Individuals with scores falling between these two ranges were classified as moderate self-compassion. An overall score of 1–2.5 denotes low self-compassion, 2.5–3.5 denotes moderate self-compassion, and 3.5–5.0 denotes high self-compassion.
The fatigue assessment scale (FAS): The FAS consists of 10 items: five questions measure physical fatigue, and five questions measure mental fatigue. The scale’s internal consistency was 0.90. Each question is answered using a 5-point Likert-type scale ranging from 1 (“never”) to 5 (“always”). The total score can range from 10 to 50; those < 22 indicate “normal” (healthy) levels of fatigue, those between 22 and 34 indicate mild-to-moderate fatigue, and those > 35 indicate severe fatigue [ 20 ]. In this study, we used Arabic version [ 21 ].
Psychological wellbeing scale: It was formerly used to measure six aspects of wellbeing and happiness: autonomy, environmental mastery, personal growth, positive relationships with others, life purpose, and self-acceptance. To determine subscale scores for each participant, the responses to each subscale item are added. Higher scores indicate greater psychological wellbeing [ 22 ].
Validation and reliability of tools
In translating the SCS-SF and Psychological wellbeing scale: into Arabic, we followed a structured process to ensure the translation maintained its validity and reliability. This involved both forward and backward translation, ensuring that the meaning of each item was preserved in the Arabic context. The translated Arabic version of the SCS [ 23 ] was used as a guide to support our further work in translating SCS-SF. Validity of all tools was evaluated by five experts from the Faculty of Nursing, Assuit University. They were from different academic categories, that is, professor and assistant professor, to confirm the accuracy and relevance of the data and tools.
Reliability of the study tools: The reliability was evaluated using the Cronbach alpha coefficient test for the SCS-SF, FAS, and psychological wellbeing scale ( r = 0.855, 0.880, and 0.861, respectively).
Statistical analysis: Statistical Package for the Social Sciences, version 26, was used for data entry and statistical analysis. Qualitative data were represented as numbers and percentages; the Chi-square (χ 2 ) test or Fisher’s exact test was used to compare categorical variables, as appropriate. Quantitative data were described as means and standard deviations and after testing for normality using the Kolmogorov–Smirnov test; analysis of variance was used to compare more than two groups of normally distributed variables, and the nonparametric Kruskal–Wallis test was used to compare more than two groups of not normally distributed data. The Spearman correlation coefficient is used to evaluate the relationship between continuous variables. Using a point-biserial correlation coefficient, a correlation between a dichotomous categorical variable and a continuous variable was determined. The researchers used univariate linear regression to identify potential risk factors for self-compassion, fatigue, and psychological wellbeing in the groups under study. A two-tailed p ≤ 0.05 was used to denote statistical significance.
Sociodemographic data: Table 1 displays the socio-demographic characteristics of the psychiatric nurses in this study. Fifty psychiatric nurses were recruited and categorized into three groups based on their scores on SCS-SF: Group 1: low self-compassion ( n = 13), Group 2: moderate self-compassion ( n = 27), and Group 3: high self-compassion ( n = 10).
A statistically significant difference in years of experience was observed between the three groups. Group 1 was significantly younger (mean age, 37.15 ± 7.49 years), had significantly lower years of experience (15.69 ± 8.57 years), and had a lower number of nurses caring for patients during a shif t ( 7.31 ± 4.38) than other groups. Group 3 had a higher proportion of nurses aged ≥ 45 (30%), nurses from urban areas (80%), nurses with a bachelor’s degree in nursing (50%), nurses working < 45 h per week (100%), and nurses caring for ≥ 10 patients per shift (50%).
FAS and psychological wellbeing scale results: No significant difference in FAS scores was observed among the groups. Meanwhile, Group 1 had the highest mean FAS score (29.69 ± 7.59), whereas Group 3 had the lowest mean FAS score (23.50 ± 5.23). Severe fatigue was observed in Group 1 and 2 only, whereas normal fatigue was more prevalent in Group 3(60%) than in other groups (Table 2 ).
Statistically significant differences in the total and subscale scores of the Psychological Wellbeing Scale were observed between the groups. Group 1 had the lowest mean total and subscale scores, whereas Group 3 had the highest mean total and subscale scores.
Relational studies: Correlation between the total scores in SCS-SF, the FAS, and the Psychological Wellbeing Scale and other parameters (Table 3 ) found that the total FAS score had a negative correlation with age ( r = − 0.28; p = 0.042) and a positive correlation with being married ( r = 0.28; p = 0.044). The total score on SCS-SF had a strong positive correlation with the total score on the Psychological Wellbeing Scale ( r = 0.72; p < 0.0001).
Univariate linear regression between self-compassion and other parameters (Table 4 ) reported psychiatric nurses with high self-compassion were significantly more likely to be male ( p = 0.04), have a lower overall fatigue score ( p = 0.028), and have better psychological wellbeing ( p = 0.0001).
Univariate linear regression between fatigue and other parameters and univariate linear regression between psychological wellbeing and other parameters (Tables 5 and 6 ) shows psychiatric nurses with high fatigue scores were more likely to be female ( p = 0.047), married ( p = 0.042), have diploma ( p = 0.04), have less self-compassion ( p = 0.028), and have poorer psychological wellbeing ( p = 0.04).
Mental health nurses must deal with patients at many levels, ranging from patients with psychological issues to those with physical disorders, from children to adults, and from inpatients to those in critical situations [ 24 ]. They face many challenges and experience several negative events. Self-compassion appears to be an important tool for dealing with unpleasant events [ 25 ]. Individuals with high self-compassion respond less emotionally to unfavorable events, produce more reasonable and less harsh perceptions of their experiences, and do not develop bad feelings when thinking of stressful or bad situations [ 4 ]. Therefore, we evaluated the relationships between self-compassion and fatigue and psychological wellbeing among psychiatric nurses and determined its possible risk factors.
In this study, psychiatric nurses with lower self-compassion were younger, had fewer years of experience, and cared for fewer patients during a shif t . In contrast, nurses with high self-compassion were aged ≥ 45 years, were from urban areas, had a bachelor’s degree in nursing (high academic degree), were working < 45 h per week, and were caring for ≥ 10 patients per shift. Two studies found that increased age and having longer clinical experience are related to low compassion fatigue [ 26 ] and high compassion satisfaction [ 27 ] as experienced nurses may have higher professional performance and coping methods to care for psychiatric patients and they are confident in their ability to respond effectively to situations [ 27 ].
Regarding high education, a study found that students who practice high levels of self-compassion are less likely to suffer from anxiety or procrastination, both of which can impair academic progress [ 28 ].
Regarding working hours, higher self-compassion ratings were correlated with decreased working hours, as working few hours help reduce the negative effects associated with stressful situations at work [ 29 ]. In contrast, living in urban areas helps reduce traffic time and stress to get in work as this study was conducted at an urban hospital.
This study found no significant difference in FAS scores among the groups. The low self-compassion group had the highest mean FAS scale score (worst score), whereas the high self-compassion group had the lowest mean FAS scale score (better score). Additionally, statistically significant differences in the total and subscale scores on the Psychological Wellbeing Scale were observed among the groups. The lowest mean total and subscale scores on the Psychological Wellbeing Scale were observed in the low self-compassion group, whereas the high self-compassion group had the highest mean total and subscale scores.
In a previous study, nurses working in special care departments, such as the emergency room, intensive care unit, and operating room, reported higher levels of fatigue, which could be because these nurses must care for patients who have more severe diseases or injuries and are more physically dependent [ 30 ]. Furthermore, the role of a mental health nurse is significantly different from that of a general nurse, although both nurses are responsible for patient care. Even so, the care demanded by psychiatric patients is significantly different from that required by a patient with physical diseases [ 24 ].
It has been demonstrated that individuals with high self-compassion are more likely to have good psychological wellbeing and have a stronger sense of satisfaction than those with low self-compassion [ 31 ]. In contrast, individuals who lack self-compassion are more likely to have psychological issues and fatigue [ 10 ].
This finding is consistent with those of Durkin and colleagues, who investigated the relationship between self-compassion and wellbeing among community nurses and discovered that community nurses who reported high levels of self-compassion also reported less burnout and more compassion for others [ 32 ].
Moreover, the total FAS score was associated with younger age and being married. Additionally, univariate linear regression studies found that psychiatric nurses with high self-compassion were significantly more likely to be male, have a low fatigue, and have high psychological wellbeing. Psychiatric nurses with high fatigue scores were more likely to be female, be married, have a diploma, have less self-compassion, and have less psychological wellbeing. Similarly, fatigue was associated with female sex [ 33 ], lower education level [ 34 ], being divorced or married [ 35 ], and poor psychological wellbeing [ 36 ].
This study established the influence of self-compassion on fatigue and psychological wellbeing among psychiatric nurses by providing important insights and substantial proof. As a result, we hope that the findings of this study will be applicable not only to mental nursing but to all nursing disciplines.
We recommend creating an educational intervention program about self-compassion that can reduce fatigue and improve the psychological wellbeing of psychiatric hospital nurses. An intervention program for all psychiatric nurses should be established to increase self-compassion knowledge, attitudes, and abilities to protect them from fatigue and psychological distress. Also, a self-compassion training program should be addressed at various population levels, such as schools, jobs, or public service. To attract participants, it must be free or low-cost.
This study has some limitations: (a) first, the convenience sample limits the generalization of the findings; (b) second, the study was limited to Assiut University’s Psychiatry and Neurology Hospital; (c) third, we did not exclude nurses with psychiatric disorders or medical conditions that might have affected their levels of compassion and psychological wellbeing.
Psychiatry nurses with higher self-compassion had lower fatigue score and better psychological wellbeing. Gender and education level were significant factors for self-compassion and fatigue. Future studies should evaluate therapies and techniques for improving self-compassion among psychiatric nurses to reduce fatigue and increase psychological wellbeing.
Availability of data and materials
All data generated or analyzed during this study are available from corresponded on request.
Abbreviations
Fatigue Assessment Scale
The Self-Compassion Scale
Thompson BL, Waltz J. Self-compassion and PTSD symptom severity. J Trauma Stress. 2008;21(6):556–8.
Article PubMed Google Scholar
Bluth K, Eisenlohr-Moul TA. Response to a mindful self-compassion intervention in teens: a within-person association of mindfulness, self-compassion, and emotional well-being outcomes. J Adolesc. 2017;57:108–18.
Article PubMed PubMed Central Google Scholar
Neely ME, Schallert DL, Mohammed SS, Roberts RM, Chen Y-J. Self-kindness when facing stress: the role of self-compassion, goal regulation, and support in college students’ well-being. Motiv Emotion. 2009;33(1):88–97.
Article Google Scholar
Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904.
Neff KD. The development and validation of a scale to measure self-compassion. Self and identity. 2003;2(3):223–50.
Kabat-Zinn J. Wherever you go, there you are: mindfulness meditation in everyday life. New York: Hyperion; 1994.
Google Scholar
Kabat-Zinn J. Wherever you go, there you are: mindfulness meditation in everyday life. Paris: Hachette; 2023.
Pauley G, McPherson S. The experience and meaning of compassion and self-compassion for individuals with depression or anxiety. Psychol Psychother. 2010;83(2):129–43.
Bhat SA, Shah SA. Self compassion and mental health: a study on young adults. IJRANSS. 2015;3(4):2347–4580.
Dev V, Fernando AT 3rd, Consedine NS. Self-compassion as a stress moderator: a cross-sectional study of 1700 doctors, nurses, and medical students. Mindfulness. 2020;11(5):1170–81.
Andrews H, Tierney S, Seers K. Needing permission: the experience of self-care and self-compassion in nursing: a constructivist grounded theory study. Int J Nurs Stud. 2020;101:103436.
Beaumont E, Durkin M, Hollins Martin CJ, Carson J. Compassion for others, self-compassion, quality of life and mental well-being measures and their association with compassion fatigue and burnout in student midwives: a quantitative survey. Midwifery. 2016;34:239–44.
Shapira LB, Mongrain M. The benefits of self-compassion and optimism exercises for individuals vulnerable to depression. J Posit Psychol. 2010;5(5):377–89.
Vaillancourt ES, Wasylkiw L. The intermediary role of burnout in the relationship between self-compassion and job satisfaction among nurses. Can J Nurs Res. 2020;52(4):246–54.
Jones G, Hocine M, Salomon J, Dab W, Temime L. Demographic and occupational predictors of stress and fatigue in French intensive-care registered nurses and nurses’ aides: a cross-sectional study. Int J Nurs Stud. 2015;52(1):250–9.
Vasconcelos S, Marqueze E, Gonçalves L, Lemos L, Araújo L, Fischer FM, et al. Morbidity among nursing personnel and its association with working conditions and work organization. Work. 2012;41(Suppl 1):3732–7.
Laschinger HKS, Fida R. New nurses burnout and workplace wellbeing: the influence of authentic leadership and psychological capital. Burn research. 2014;1(1):19–28.
Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the self-compassion scale. Clin Psychol Psychother. 2011;18(3):250–5.
Neff KD, Tóth-Király I. Self-Compassion Scale (SCS). In: Medvedev ON, Krägeloh CU, Siegert RJ, Singh NN, editors. Handbook of assessment in mindfulness research. Cham: Springer International Publishing; 2022. p. 1–22.
Hendriks C, Drent M, Elfferich M, De Vries J. The fatigue assessment Scale: quality and availability in sarcoidosis and other diseases. Curr Opin Pulm Med. 2018;24(5):495–503.
Alhanbali S, AlJasser A, Aboudi O, Alaqrabawi W, Munro KJ. Establishing the reliability and the validity of the Arabic translated versions of the effort assessment scale and the fatigue assessment scale. Int J Audiol. 2023;62(9):853–8.
Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69(4):719–27.
Alabdulaziz H, Alquwez N, Almazan JU, Albougami A, Alshammari F, Cruz JP. The self-compassion scale Arabic version for baccalaureate nursing students: a validation study. Nurse Educ Today. 2020;89:104420.
Levert T, Lucas M, Ortlepp K. Burnout in psychiatric nurses: contributions of the work environment and a sense of coherence. S Afr J Psychol. 2000;30:36–43.
MacBeth A, Gumley A. Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clin Psychol Rev. 2012;32(6):545–52.
Stacey W, Kramer M, Gunnarsdottir K, Gonzalez-Martinez J, Zaghloul K, Inati S, et al. Emerging roles of network analysis for epilepsy. Epilepsy Res. 2020;159:106255.
Xie W, Wang J, Okoli CTC, He H, Feng F, Zhuang L, et al. Prevalence and factors of compassion fatigue among Chinese psychiatric nurses: a cross-sectional study. Medicine (Baltimore). 2020;99(29):e21083.
Williams JG, Stark SK, Foster EE. Start today or the very last day?. The relationships among self-compassion, motivation, and procrastination. Am J Psychol Res. 2008;4(1):37-44.
Cotterill M, Kotera Y, Garip G. The effect of self-compassion on job burnout and hours worked in employees’ working from home. J Concurr Disord. 2021. https://doi.org/10.54127/GRNJ6778 .
Lee E-Y, Kim J-S. Relationships among Emotional Labor, Fatigue, and Musculoskeletal Pain in Nurses [Internet]. Vol. 18, Journal of the Korea Academia-Industrial cooperation Society. The Korea Academia-Industrial Cooperation Society; 2017. p. 351–9. Available from: https://doi.org/10.5762/KAIS.2017.18.1.351
Benzo R, Kirsch JL, Nelson C. Compassion, mindfulness, and the happiness of healthcare workers. Explore. 2017;13:201–6.
Durkin M, Beaumont E, Hollins Martin CJ, Carson J. A pilot study exploring the relationship between self-compassion, self-judgement, self-kindness, compassion, professional quality of life and wellbeing among UK community nurses. Nurse Educ Today. 2016;46:109–14.
Cullen W, Kearney Y, Bury G. Prevalence of fatigue in general practice. Ir J Med Sci. 2002;171:10–2.
Lee K-J, Kim J. Related factors on fatigue symptom in married working women. J Epidemiol. 2008;30:82.
Baye M, Fisseha B, Bayisa M, Abebe SM, Janakiraman B. Experience of fatigue and associated factors among adult people living with HIV attending ART clinic: a hospital-based cross-sectional study in Ethiopia. BMJ Open. 2020;10(10):e042029.
Sagherian K, Cho H, Steege LM. The insomnia, fatigue, and psychological well-being of hospital nurses 18 months after the COVID-19 pandemic began: a cross-sectional study. J Clin Nurs. 2022. https://doi.org/10.1111/jocn.16451 .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Psychiatric and Mental Health Nursing, Faculty of Nursing, Mansoura University, Mansoura, Dakahlia Governorate, Egypt
Sahar Behilak
Department of Nursing, College of Applied Medical Sciences, University of Jeddah, Jeddah, Saudi Arabia
Department of Psychiatric and Mental Health Nursing, Faculty of Medicine & Health Science, Hodeidah University, Al Hudaydah, Yemen
Saleh Abdullah
Department of Neurology and Psychiatry, Faculty of Medicine, Assiut University, Assiut, Egypt
Gellan K. Ahmed
Department of Psychiatric Mental Health Nursing, Faculty of Nursing, Suez Canal University, Ismailia, Egypt
Ola Ali Abd El-Fatah Ali Saraya
You can also search for this author in PubMed Google Scholar
Contributions
SB contributed to the study conception, design of the work, statistical analysis, and critical revision of the manuscript. SA and GKA contributed to data interpretation, statistical analysis, and critical revision of the manuscript. OAAS contributed to the study conception, design of the work, data recruitment, and drafted the manuscript. All authors gave final approval of the version to be published.
Corresponding author
Correspondence to Gellan K. Ahmed .
Ethics declarations
Ethics approval and consent to participate.
The institutional review board of the Faculty of Medicine, Assiut University, granted ethical approval for the investigation (IRB: 17300900). In addition to the questionnaire, the nurses received a cover letter with a written explanation of the purpose and nature of the study. Before the request for participation, the anonymity and confidentiality of the nurses were assured. Informed written consent was obtained from the participants. Additionally, the nurses were reassured that their participation in this study was voluntary.
Consent for publication
Competing interests.
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Behilak, S., Abdullah, S., Ahmed, G.K. et al. Influence of self-compassion on fatigue and psychological wellbeing among psychiatric nurses. Egypt J Neurol Psychiatry Neurosurg 60 , 113 (2024). https://doi.org/10.1186/s41983-024-00891-z
Download citation
Received : 05 April 2024
Accepted : 15 September 2024
Published : 24 September 2024
DOI : https://doi.org/10.1186/s41983-024-00891-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Self-compassion
- Psychological wellbeing
- Psychiatric nursing
Mental Health and Psychiatric Nursing
The field of mental health often seems a little unfamiliar or mysterious, making it hard to imagine what the experience will be like or what nurses do in this area. This is an overview of the history of mental illness, advances in treatment, current issues in mental health, and the role of the psychiatric nurse .
Table of Contents
Mental health, mental illness, diagnostic and statistical manual of mental disorders, ancient times, period of enlightenment and creation of mental institutions, sigmund freud and treatment of mental disorders, development of psychopharmacology, mental illness in the 21st century, psychiatric nursing practice, mental health and mental illness.
Mental health and mental illness are difficult to define precisely. The culture of any society strongly influences its beliefs and values, and this in turn affects how that society defines health and illness.
No single universal definition of mental health exists. Generally, a person’s behavior can provide clues to his or her mental health.
- In most cases, mental health is a state of emotional, psychological, and social wellness evidenced by satisfying interpersonal relationships , effective behavior and coping, positive self-concept, and emotional stability.
- Factors influencing a person’s mental health can be categorized as individual, interpersonal, and social/cultural.
- Individual , or personal, factors include a person’s biologic make up, autonomy and independence, self-esteem , capacity for growth, vitality, ability to find meaning in life, emotional resilience or hardiness, sense of belonging, reality orientation, and coping or stress management abilities.
- Interpersonal , or relationship, factors include effective communication , ability to help others, intimacy, and a balance of separateness and connectedness.
- Social/cultural , or environmental, factors include a sense of community, access to adequate resources, intolerance of violence, support of diversity among people, mastery of the environment, and a positive, yet realistic, view of one’s world.
The American Psychiatric Association (APA, 2000) defines a mental disorder as “a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and is associated with present distress or with a significantly increased risk of suffering death , pain , disability, or an important loss of freedom.
- General criteria to diagnose mental disorders include dissatisfaction with one’s characteristics, abilities, and accomplishments; ineffective or unsatisfying relationships; dissatisfaction with one’s place in the world; ineffective coping with life events; and lack of personal growth.
- Factors contributing to mental illness also can be viewed within individual, interpersonal, and social/cultural categories.
- Individual factors include biologic make up, intolerable or unrealistic worries or fears, inability to distinguish reality from fantasy, intolerance of life’s uncertainties, a sense of disharmony in life, and a loss of meaning in one’s life.
- Interpersonal factors include ineffective communication , excessive dependency on or withdrawal from relationships, no sense of belonging, inadequate social support, and loss of emotional control.
- Social/cultural factors include lack of resources, violence, homelessness, poverty, an unwarranted negative view of the world, and discrimination.
The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR) is a taxonomy published by the APA.
- The DSM-IV-TR describes all mental disorders, outlining specific diagnostic criteria for each based on clinical experience and research.
- The DSM-IV-TR has three purposes:
- To provide a standardized nomenclature and language for all mental health professionals.
- To present defining characteristics or symptoms that differentiate specific diagnoses.
- To assist in identifying the underlying causes of disorders.
- The multiaxial classification system that involves assessment on several axes, or domains of information, allows the practitioner to identify all the factors that relate to a person’s condition.
- Axis I is for identifying all major psychiatric disorders except mental retardation and personality disorders .
- Axis II is for reporting mental retardation and personality disorders as well as prominent maladaptive personality features and defense mechanisms .
- Axis III is for reporting current medical conditions that are potentially relevant to understanding or managing the person’s mental disorder as well as medical conditions that might contribute to understanding the person.
- Axis IV for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders.
- Axis V presents a Global Assessment of Functioning, which rates the person’s overall psychological functioning on a scale of 0 to 100; this represents the clinician’s assessment of the person’s current level of functioning.
Historical Perspectives of the Treatment of Mental Illness
- People of ancient times believed that any sickness indicated displeasure of the gods and in fact was punishment for sins and wrongdoing.
- Those with mental disorders were viewed as either divine or demonic, depending on their behavior.
- Later, Aristotle attempted to relate mental disorders to physical disorders and developed his theory that the amounts of blood , water, and yellow and black bile in the body controlled the emotions.
- These four substances, or humors, corresponded with happiness, calmness, anger, and sadness; imbalances of the four humors were believed to cause mental disorders, so treatment was aimed at restoring balance through bloodletting, starving, and purging.
- In early Christian times, all diseases were again blamed on demons, and the mentally ill were viewed as possessed; priests perform exorcism to to rid evil spirits.
- During the Renaissance, people with mental illness were distinguished from criminals in England; those considered harmless were allowed to wander the countryside and or live in rural communities, but the more “dangerous lunatics” were thrown in prison, chained, and starved.
- In 1547, the Hospital of St. Mary of Bethlehem was officially declared a hospital for the insane, the first of its kind; by 1775, visitors at the institution were charged a fee for the privilege of viewing and ridiculing the intimates, who were seen as animals, less than human.
- In the 1790s, a period of enlightenment concerning persons with mental illness began.
- Phillipe Pinel in France and William Tukes in England formulated the concept of asylum as a safe refuge or haven offering protection at institutions where people had been whipped, beaten, or starved just because they were mentally ill (Gollaher, 1995).
- In the United States, Dorothea Dix (1802-1887) began a crusade to reform the treatment of mental illness after a visit to Tukes’ institution in England; she was instrumental in opening 32 state hospitals that offered asylum to the suffering.
- The period of scientific study and treatment of mental disorders began with Sigmund Freud (1856-1939) and others, such as Emil Kraeplin (1856-1926) and Eugene Bleuler (1857-1939).
- With these men, the study of psychiatry and the diagnosis and treatment of mental illness started in earnest.
- Freud challenged society to view human beings objectively; he studied the mind, its disorders, and their treatment as no one had before.
- Kraeplin began classifying mental disorders according to their symptoms, and Bleuler coined the term schizophrenia .
- A great leap in the treatment of mental illness began in about 1950 with the development of psychotropic drugs, or drugs used to treat mental illness.
- Chlorpromazine ( Thorazine ) an antipsychotic drug, and lithium, an antimanic agent, were the first drugs to be developed.
- Over the following 10 years, monoamine oxidase inhibitor antidepressants , haloperidol ( Haldol ), an antipsychotic; tricyclic antidepressants ; and antianxiety agents, called benzodiazepines , were introduced.
The National Institute of Mental Health (NIMH) estimates that more than 26% of Americans aged 18 years and older have a diagnosable mental disorder- approximately 57.7 million persons each year (2006).
- Furthermore, mental illness or serious emotional disturbances impair daily activities for an estimated 10 million adults and 4 million children and adolescents.
- Mental disorders are the leading cause of disability in the United States and Canada for persons 15 to 44 years of age.
- Homelessness is a major problem in the United States today; the National Resource and Training Center on Homelessness and Mental Illness (2006) estimates that one-third of adult homeless persons have a serious mental illness and that more than one half also have substance abuse problems.
- In 1993, the federal government created and funded Access to Community Care and Effective Services and Support (ACCESS) to begin to address the needs of people with mental illness who were homeless either all or part of the time.
- In 1873, Linda Richards graduated from the New England Hospital for Women and Children in Boston; she went on to improve nursing care in psychiatric hospitals and organized educational programs in state mental hospitals in Illinois.
- Richards is called the first American psychiatric nurse; she believed that “the mentally sick should be at least as well cared for as the physically sick” (Doona, 1984).
- The first training of nurses to work with persons with mental illness was in 1882 at McLean Hospital in Belmont, Massachusetts.
- The care was primarily custodial and focused on nutrition , hygiene , and activity.
- The role of psychiatric nurses expanded as somatic therapies for the treatment of mental disorders were developed.
- Treatments such as insulin shock therapy (1935), psychosurgery (1936), and electroconvulsive therapy (1937) required nurses to use their medical- surgical skills more extensively.
- The first psychiatric nursing textbook, Nursing Mental Diseases by Harriet Bailey was published in 1920; in 1913, John Hopkins was the first school of nursing to include a course in psychiatric nursing in its curriculum.
- In 1973, the division of psychiatric and mental health practice of the American Nurses Association (ANA) developed standards of care, which it revised in 1982, 1994, and 2000.
- Standards of care are authoritative statements by professional organizations that describe the responsibilities for which nurses are accountable.
- The goal of self-awareness is to know oneself so that ones’ values, attitudes, and beliefs are not projected to the client, interfering with nursing care; self-awareness does not mean having to change one’s values and beliefs unless one desires to do so.
1 thought on “Mental Health and Psychiatric Nursing”
Such a useful information in brief, really appreciate the efforts of writer Marianne
Leave a Comment Cancel reply
- View PDF

International Journal of Nursing Studies Advances
Nurses’ experiences and sense making of covid-19 redeployment and the impact on well-being, performance, and turnover intentions: a longitudinal multimethod study., participants, conclusions, cited by (0).
Search Utah State University:
Teaching & Learning
A Soldier's Resolve: Jacob Hunsaker's Dedication to Nursing, Mental Health
By Maren Aller | September 25, 2024

Jacob Hunsaker

Planes filled the air, carrying young soldiers from the United States into the heart of Afghanistan's treacherous terrain. With each step onto foreign soil, soldiers, like Utah State University alum Jacob Hunsaker ’13 BA, ’15 MMFT, ’21 BSN, a member of the U.S. Army Reserve, braced for the battles ahead, knowing they would test their resolve and change them forever.
It was late 2010, and the United States had intensified its military efforts in Afghanistan, deploying an additional 30,000 troops to combat the Taliban insurgency. Jacob, serving as a combat engineer, took his job of searching for IEDs and roadside bombs very seriously. His dedication earned him promotions to team leader and later squad leader. Understanding the wellbeing of his team was paramount, he realized that being in good physical shape was crucial, but maintaining mental health was equally important.
“I began doing talk therapy techniques with my team members,” Jacob recalled of his service during late 2010 and throughout 2011. “I realized what a difference it made under the heavy circumstances we were placed in, and, when I returned to Logan, I knew I had to continue my USU studies to become a licensed marriage and family therapist.”
After earning a bachelor's degree in Spanish from the College of Humanities and Social Sciences in 2013, Jacob immediately enrolled in the master's program for marriage and family therapy at the Emma Eccles Jones College of Education and Human Services , graduating in 2015. He began his career at a community health center, which sparked his interest in the medical side of therapy.
“I recognized in graduate school that I was not only interested in therapy, but also in the medical aspects of the field,” Jacob said. “I wanted to help families navigate therapy in stressful medical situations through an integrated health care approach, where patients, providers and therapists work together. So, I enrolled in USU’s Registered Nurse, baccalaureate of science in nursing program.”
USU’s Department of Nursing , housed in the Emma Eccles Jones College of Education and Human Services, was established in 2017 and has quickly garnered an excellent reputation. Impressively, the 2021-22 and 2022-23 graduating cohorts both achieved a 100 percent first-time pass rate on the NCLEX exam, a crucial step in becoming a registered nurse. Most USU nursing students secure job offers even before graduation.
However, the program is rigorous, particularly in the final semester when students must complete a 144-hour preceptored capstone experience, where they shadow and work alongside a registered nurse for twelve 12-hour shifts. Students in USU’s nursing program complete their preceptorships at institutions such as Logan Regional Hospital, Primary Children’s Hospital, Huntsman Cancer Institute, and McKay Dee Hospital.
“Our students typically complete their preceptorships during the latter half of their final semester, mirroring whenever possible the exact schedule of their assigned registered nurse,” said Dr. Carma Miller, department head and professional practice associate professor for the Department of Nursing. “If the nurse has two 12-hour shifts at Primary Children’s Hospital, our students are expected to be there — on top of their regular class load. The students do not get paid for their preceptorship, and, as you can imagine, they are practically running on fumes. It's a valuable reality check that demonstrates the dedication required for the profession.”
Jacob recalls his last semester and the immense strain it put on him and his family. Married with three children at the time, a fourth would come later, Jacob juggled completing his labs and clinicals during the day while working full-time as a therapist. The day he learned he had received a scholarship, he walked out of the building and called his wife, and together they shared a joyful, tearful moment.
“The final year of nursing school is, by far, the busiest,” Jacob said. “You are financially the most vulnerable you will ever be as a student, and receiving a scholarship was a huge deal for me and my family. We were barely scraping by, and the money helped lessen some of the financial strain so we could purchase groceries and gas. It meant so much to us.”
Since he was slightly older than his fellow nursing cohorts, Jacob, who graduated with his bachelor’s of nursing in 2021, was seen as a type of father figure and mentor to those who studied alongside him.
“Jacob’s decision to pursue a second bachelor’s degree in nursing is a testament to his dedication to his clients,” Miller said. “By doing so, he aims to provide both psychological and medical care, eliminating the need for his clients to see multiple professionals for their treatment. This choice is remarkable, given the financial hardship and time away from his family that pursuing a second-degree can entail. Everyone in his graduating class looked up to him.”
Nursing education can be financially challenging for many students, particularly those from low-income and first-generation college student backgrounds. At Utah State, nursing education is not only provided at the main campus in Logan, but is a vital part of the statewide campus system as well. The nursing program is one of the most popular majors in Blanding and Moab, and, in Blanding, the nursing cohort is largely made up of Navajo students. This diversity enriches the program and ensures that USU is training nurses who can provide culturally competent care across different communities right here in Utah.
“Financial support can make nursing education more accessible to a wider range of students,” Miller said. “It can also help attract high-potential students who might otherwise be discouraged by the cost of education. Overall, financial support, combined with our excellent facilities and dedicated faculty, will increase the number of qualified nurses entering the workforce.”
USU’s nursing program offers individuals an emotionally fulfilling and rewarding career with the flexibility to choose a specialty they are passionate about in a setting of their choice. With degrees ranging from a practical nursing certificate and an associate of applied science in nursing to a bachelor of science in nursing and an online-only registered nurse to bachelor of science in nursing , there is truly something for everyone.
Dr. Miller notes that “When you ask someone why they want to become a nurse, the majority will say it’s because they want to help people.”
Jacob Hunsaker Hardship Nursing Fund
Helping people is exactly what Chloe Richmond, the 2023-24 Emma Eccles Jones College of Education and Human Services student senator, aimed to do when she started as a pre-nursing student at USU. Although she later switched her major to kinesiology, Chloe witnessed the challenges her peers faced in the nursing program.
“I saw many peers drop out of nursing because of the long hours, extensive clinical shifts, and lack of compensation,” Chloe said. “I wanted to address this during my time as senator, so I discussed creating a hardship fund for nursing students with Dean Al Smith and Dr. Miller.”
For Chloe, it became clear that supporting nursing students is crucial to their success. She recognized that nurses do more than provide medical care; they work on the front lines, administering treatments, offering comfort, and advocating for their patients. With a diverse skill set, nurses act as caregivers, innovators, and critical thinkers. In every hospital, clinic, and healthcare facility, they ensure that patients receive comprehensive and compassionate care. This dedication to local service is especially vital in today’s healthcare landscape.
“When Chloe proposed the idea of creating a hardship fund to help nursing students, we immediately thought of Jacob because his story perfectly embodies the spirit of compassion and service essential to the nursing profession,” Dr. Miller said.
The Jacob Hunsaker Hardship Nursing Fund is now part of the AggieFunded program , thanks to Chloe’s dedication and efforts. AggieFunded is a platform that enables student organizations and affinity groups to raise funds for innovative projects, programs, and initiatives, allowing them to make a significant impact on campus and beyond. The ultimate goal is growing the fund into an endowment, which requires reaching a minimum of $25,000.
“Donating to USU’s Jacob Hunsaker Hardship Nursing Fund is truly an investment in the future and we have a lot of money to raise to reach the endowment level,” Miller said. “Donations help attract and retain students, expand program capacity, and advance nursing science. The best part is that supporting nursing education ensures more highly-skilled and compassionate nurses will be available to provide care for us or our loved ones in the future as so many of our graduates stay to serve right here in Utah.”
Jacob, honored and humbled by the nursing students’ decision to name the fund after him, remains proud of his Aggie heritage. He has remained in Logan, running a successful practice, River Hollow Mental Health, because he wanted to give back to the community that gave him so much.
“Our practice mentors nursing and therapy students, and we hire USU graduates,” Jacob said. “We pride ourselves on giving back by hosting free seminars at the university, other schools, hospitals, and churches, and we provide a free mental health support group every Wednesday for adults. We try to give back as much as we can.”
Today, Jacob is pursuing a doctorate degree of nursing practice in psychiatric and mental health to further his goal of providing a full range of services for those dealing with stressful situations throughout their lifespan, thus embodying the true spirit of caring.
Create Your Aggie Impact by giving to an AggieFunded program and support the student-focused area that most inspires you to make a difference through the power of philanthropy.
Maren Aller Senior Writer Advancement (435) 797-1355 [email protected]
Comments and questions regarding this article may be directed to the contact person listed on this page.
Next Story in Teaching & Learning
September 25, 2024 129
CEHS Undergrads Receive Robust Opportunities to Thrive in Research
Creating undergraduate research opportunities has been a priority for both Utah State University and the Emma Eccles Jones College of Education for the past 50 years.

September 25, 2024 185
Nursing Students Receive Training in New State-of-the-Art Advanced Nursing Education Suite
Utah State University formally opened its Emma Eccles Jones Advanced Nursing Education Suite this summer.
Trending on Utah State Today

UNIVERSITY AFFAIRS
September 10, 2024 2725
Utah State Responds to Notice of Noncompliance From Department of Justice

SCIENCE & TECHNOLOGY
September 03, 2024 2171
USU's Science Unwrapped STEM Outreach Program Launches 'Joining Forces' Series

CAMPUS LIFE
August 29, 2024 2105
Welcome Message From Student Affairs: Explore Your Campus Resources

August 29, 2024 1862
USU Hosts Info Meeting on New Threat Assessment Management Team on Sept. 4
Study funded by NIHR highlights inequalities in access to green spaces and mental health
- 10 October 2023
On World Mental Health Day (Tuesday 10 October), a newly-published study has highlighted how access to green or blue spaces boosts mental health.
The study, funded by the NIHR, saw researchers examining data covering a 10-year period. This made it the largest, most comprehensive evaluation of differences in exposure to green and blue spaces on mental health.
The study team’s findings highlighted the beneficial role of greenness and access to green or blue spaces in reducing socioeconomic-related inequalities in mental health. They also discovered every additional 360m to the nearest green or blue space was associated with higher odds of anxiety and depression.
The study was led by researchers from the University of Liverpool. They worked with researchers internationally to anonymously link three groups of records:
- household greenness
- access to green and blue space
- GP records of anxiety and depression for over 2 million adults in Wales
The effects of green spaces on mental health are well documented. However, using the medical records of an entire adult population over such a length of time gives a new level of understanding to this work.
Huge potential
Richard Mitchell, Professor of Health and Environment at the University of Glasgow, said: “This brilliant study gives us three reasons to be cheerful. First, it confirms that natural environments around us really do benefit our mental health. Second, the benefits seem strongest for those most at risk, so there’s huge potential for tackling the gulf in health between richer and poorer people. Third, the study shows what great science we can do in the UK using our world-leading health datasets safely and securely.”
The researchers stressed investing in improved public green spaces might bring mental health benefits to everyone. But this would be particularly beneficial for those living in more deprived areas. Their findings can support organisations and authorities responsible for green and blue spaces. It can help them to engage planners and policymakers to ensure that local green and blue spaces meet residents’ health needs.
Professor Sarah Rodgers, Professor of Health Informatics at the University of Liverpool, said: “Our study has shown that green and blue spaces are likely to protect people from needing to see their GP for anxiety or depression, and in places where people have fewer resources overall, living near these spaces seems to have a bigger protective effect than for people living in areas with more resources.”
Need for more research
The researchers also called for further related studies to be undertaken in future. They say a greater understanding is needed of why those living in lower-income and higher-income areas are affected differently by access and exposure to green and blue spaces. They argue this will ensure those in most need have access to free green and blue spaces. They believe it will also help to protect the health of our population.
Dr Rebecca Geary, Lecturer in Epidemiology and Public Health at The University of Liverpool, said: “Our environmental health equity evidence shows the importance of enhancing our built environments by including appropriate green and blue spaces to improve the health and wellbeing of all adults, especially those living in the most deprived areas.
“Providing urban green and blue spaces may also give additional co-benefits of job or food creation, biodiversity promotion, flood prevention and carbon sequestration, so are both a public health and social investment.”
The full study has been published in The Lancet Planetary Health . It has been funded by our Public Health Research (PHR) Programme . For more information, please visit the Funding and Awards page on our website.
Share this page
Latest news.

NIHR takes on management of Better Methods for Better Research Programme

New findings on the use of molnupiravir to treat COVID-19

New funding opportunities for novel brain tumour research launched
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Community Based Nurs Midwifery
- v.8(1); 2020 Jan
Nursing Students’ Perceptions of Effective Factors on Mental Health: A Qualitative Content Analysis
Roghieh sodeify, phd.
1 Department of Medical-Surgical Nursing, School of Nursing, Khoy University of Medical Sciences, Khoy, Iran
Fatemah Moghaddam Tabrizi, PhD
2 Reproductive Health Research Center, School of Nursing and Midwifery, Urmia University of Medical Sciences, Urmia, Iran
Background:
Mental health is a fundamental and widespread concept with individual meanings. The purpose of this study is to perceive and clarify the factors influencing mental health from the perspectives of nursing students
The present qualitative study was conducted in Khoy, Iran from July-December 2018. Twenty nursing students were selected as the research participants through purposeful sampling method and interviewed using semi-structured in-depth interviews. All interviews were recorded, transcribed, and then analyzed with Graneheim and Lundman’s approach of conventional content analysis. The Trail version of the MAXQDA 10 software was applied to conduct the coding process
Data analysis revealed four themes and 12 sub-themes. The themes included feeling of self-worth, religious beliefs, socio-economic factors, and behavioral factors.
Conclusion:
The results showed that mental health in nursing students is a multidimensional phenomenon and is influenced by various factors. The current results could help the nurse educators to intervene and provide suitable, effective, practicable, and culture based mental health services and also help the nursing students achieve mental stability. Therefore, it is suggested that further qualitative and interventional studies should be conducted in this area
I NTRODUCTION
Mental health is one of the most important requirements of man and an important aspect of health. As defined by the World Health Organization (WHO), health means full physical, mental and social well-being, and it doesn’t refer to the lack of illness or infirmity. 1 The central part of health is mental health because all health-related interactions are carried out mentally. 2 Health is a perceptual concept based on learning, values and beliefs of each individual who is influenced by the environment, family, and community. If the concept of health is understood abstractly, its effects in life will not be clear. 3
Several definitions of mental health have been made: lack of mental illness, emotional balance, social harmony, feeling of comfort, integrity of personality, self and environmental awareness, ability to play a social, physical and emotional role, ability to co-ordinate with others, modification and improvement of the individual and social environment, resolution of conflicts and personal preferences logically, fairly and appropriately, the ability to adapt to the normal stresses of life, and finally self management. The concept of mental health, according to the WHO, refers to a status beyond the absence of mental disorders and it includes mental well-being, self-efficacy, autonomy, competence, social relations, social communication, prosperity, and intellectual and emotional potentialities. 4 , 5
Many factors affect mental health. Researchers consider reasons such as personality structures and cognitive and attitudinal components such as hope, optimism, empathy, affiliation, forgiveness, religion and spirituality in the stability of a sense of well-being and health. 6 , 7 Studies have shown that those with a high psychological well-being also have a better physical health. These people are generally happy, optimistic, and positive, and have emotional stability, self-esteem, and high self-efficacy. High mental health is positively associated with the logical perception of others and negatively associated with suicidal ideation, unprofessional behavior and burnout. 8
The results of many studies in and out the country (IRAN) show that nursing students have lower general and mental health than other health related disciplines and non-medical students. 9 , 10 In fact, nursing education does not create a suitable environment for nursing students. According to the nursing education curriculum, nursing students, in addition to learning theoretical courses, are placed in various clinical settings to acquire knowledge, skills and clinical judgment to achieve professional competence. 9 During this period, they experience stressful events that affect their personal and professionals life. 11 Some previous researches in this area also revealed that stressors which affected the students’ mental health were related to academic training. The most common stressors included ‘stress experience in the educational environment’, ‘relationships at work’, ‘issues of death and suffering, ‘inadequate knowledge and training’, ‘insufficient hospital resources’, and ‘communication and procedural aspects of client care’. 12
The consequences of a meta-analysis study in Iran during a 23-year period between 1991 and 2015 showed that the prevalence of mental disorders among students in Iran using random models was 33%. Unfortunately, the prevalence rate showed an increasing rate over time while in other countries this rate was below 20%. 13 Previous studies conducted in United States, Iran, Singapour, India, and Malaysia showed that mental health issues are a growing concern among college student 14 , 15 and depression, alcohol use, stress, low sleep quality, excessive daytime sleepiness, and anxiety are major mental health problems among nursing students. 8 , 16 The results of another study which assessed the general health of nursing and other health related disciplines students indicated that mental disorders were observed 19.5%. 17 Findings of some studies showed that a very small percentage of nursing students had a good status of happiness as an indicator of the mental health. Happiness was claimed to be essential in developing nursing students as future nurses since happy nurses are more energetic, creative, successful, sociable, and more interested in caring. 18 , 19 In general, the results of most empirical research indicate that nursing students are at a relatively poor level of mental health which could have undesirable personal and professional consequences. 4 , 8 , 9 In fact, major changes in the social, family, and personal life of the nursing students and experience of traumatic events in various clinical setting can lead to some psychological problems. Considering the fact that young people and university students include more than one third of the whole population of Iran, it is important to be aware of their perceptions of the factors affecting mental health. Nursing educators are always concerned about the knowledge and skills of nursing students. One of the obstacles in this regard is mental health problems. Therefore, the researchers tried to get deeper understanding about the factors affecting nursing students’ mental health. Regarding the fact that mental health is formed in the socio-cultural context and due to low knowledge about the mental health of nursing students, the researchers decided to use nursing students’ own experiences to discover and deeply understand this phenomenon. Thus, they chose the qualitative content analysis method to perceive and clarify the factors influencing mental health from the perspectives of nursing students.
M ATERIAL AND M ETHODS
The present qualitative study using content analysis approach was conducted in Khoy, Iran during July-December 2018. In accordance with qualitative research, sampling was started with purposeful method and done with theoretical sampling with maximum variation. In the purposeful sampling, the researcher is looking for those who have a rich experience of the phenomena under the study and have the ability and desire to express it. 20
The participants in this study were 20 nursing students who were studying at Khoy Medical Science University, Iran. The inclusion criteria for the study were having at least one semester of university experience and willingness to express their own experiences. Exclusion criteria for the study were having a mental or physical illness during the previous year based on the participants’ own self report.
Data collection was done through in-depth semi-structured interviews. The time and place of the interviews were agreed upon by the parties and they were conducted in a private class at the university by the first author. In the first instance, the researcher initially referred to the participants and presented the purpose of the research and if they were willing to participate in the research, an interview was scheduled. The open questions were designed as an interview guide to provide an open and interpretative response and follow-up questions were asked after the interviewees’ responses. The general question in all interviews was: When do you feel you have mental health and when not? Which factors increase or decrease your mental health? As the interview went on, more detailed questions were asked about the influential factors (inhibitors or facilitators) expressed by the participants. The duration of interviews varied from 30-50 minutes. The guiding principle in the sampling of qualitative research is the saturation of the data to the extent that no new data is obtained. 20 In general, 20 interviews were conducted with 20 students to achieve theoretical saturation. No new data or concept was obtained after analyzing the last (18th) interviews. However, two more interviews were conducted to ensure data saturation. Data analysis process was carried out continuously and concurrently with data collection.
Interviews were analyzed using Graneheim and Lundman’s (2004) conventional content analysis guidelines. 21 (i) The recorded interviews were transcribed (ii) The researchers listened to the recordings and reviewed the transcripts several times to find the meaning units. (iii) The meaning units from the statements of the participants were extracted in the form of initial codes. (iv) Codes were categorized according to the conceptual similarities to be minimized. (v) This trend continued across all the analysis units until themes and subthemes emerged. Each interview was recorded and typed in MAXQDA software, version 10.
Guba and Lincoln’s criteria were used to assure the trustworthiness and rigor of the data. Credibility was achieved by reviewing the transcripts by participants themselves and using their complementary ideas as well as the prolonged engagement of the researchers with the data. For conformability, peer examination was done on the process of the work and research findings. For transferability, an extensive description of details regarding the methodology and context was included and sampling was done purposively. And finally for dependability, all accomplished activities were recorded precisely from the first step of the study. 22
This study was approved by the research ethic committee of Khoy Medical University (IR.KHOY.REC.1398.005). Written informed consent was signed by all participants. They were made aware of ethical, confidentiality (anonymity in publishing) and voluntary participation principles and recording of their interviews.
The participants in the study were in the age range of 20-24 years. They were 12 female and 8 male undergraduate nursing students from different semesters ( Table 1 ). The analysis of the findings from the interview resulted in the extraction of four themes. They were classified as: feeling of self-worth, religious beliefs, socio-economic factors, and behavioral factors. ( Table 2 ).
Demographic characteristics of the participants
| Participants | Sex | Age (years) | Semester |
|---|---|---|---|
| Participant 1 | Female | 21 | 4 |
| Participant 2 | Male | 20 | 4 |
| Participant 3 | Female | 22 | 6 |
| Participant 4 | Female | 20 | 2 |
| Participant 5 | Female | 24 | 8 |
| Participant 6 | Female | 23 | 6 |
| Participant 7 | Female | 22 | 6 |
| Participant 8 | Male | 20 | 4 |
| Participant 9 | Male | 20 | 6 |
| Participant 10 | Female | 22 | 4 |
| Participant 11 | Male | 20 | 2 |
| Participant 12 | Female | 22 | 4 |
| Participant 13 | Male | 20 | 2 |
| Participant 14 | Female | 24 | 8 |
| Participant 15 | Female | 24 | 6 |
| Participant 16 | Male | 24 | 8 |
| Participant 17 | Female | 22 | 6 |
| Participant 18 | Male | 20 | 4 |
| Participant 19 | Male | 22 | 8 |
| Participant 20 | Female | 20 | 2 |
Themes and sub-themes extracted from the interviews
| Sub-theme | Themes |
|---|---|
| ● Confirmation | Feeling of self-worth |
| ● Success | |
| ● Autonomy | |
| ● Self-acceptance | |
| ● Hope | |
| ● Participating in religious ceremonies | Religious beliefs |
| ● Reciting the holy Quran and other religious books | |
| ● Social Support | Socio-economic factors |
| ● Economical support | |
| ● Disengagement | Behavioral factors |
| ● Physical Exercise | |
| ● Balanced use of social networks |
Theme 1: Feeling of Self-Worth
Throughout the interviews, nursing students with various statements tried to express this important theme that their mental health is influenced by factors affecting their feeling of self- worth, and as long as students have a positive perception of themselves, their mental well-being will increase. The components of the feeling of self-worth in this study include: ‘confirmation’, ‘success’, ‘autonomy’, ‘self-acceptance’, and ‘hope’ that are discussed in detail below. In fact, students described in a variety of ways how to gain feeling of self-worth for mental health.
1.a. Confirmation
Participants believed that when they received positive feedback from others and were confirmed, they were both satisfied and mentally health.
“People around you have a lot of influence. For example, when your parents accept, care about, and listen to you well, you feel quite well off, but when they say come on, forget it, and she’s really young, you feel worthless and upset” .(p.4)
1.b. Success
Most participants say that they feel relaxed when they feel successful or have a successful experience of overcoming problems.
“I think mental health is a sense of success. When your work is done successfully, it has a good effect on your minds. Imagine you are in charge of a task and you are just cutting the mustard” .(p.18)
“When you fulfill your colleagues’ expectations and reach the required standard, you feel relaxed” .(p.10)
1.c. Autonomy
Participants said that they had psychologically good feelings when parents or relatives did not create a constraint for them, or when they felt independent and were able to manage their own affairs a and make decisions or once others respected their decisions, they were emotionally well-off. But when faced with resistance, they did not experience a good psychological feeling.
“I feel psychologically healthy when I am independent in my own work and decide for myself. We youth need to be free, we need to think independently” .(p.10)
“When my friends and acquaintance give me power and freedom and respect my decision, I feel psychologically healthy” .(p.5)
1.d. Self-acceptance
Participants thought someone as a healthy person if s/he values himself and accepts him/herself with all the weaknesses and abilities.
“To have mental health, first of all, one needs to accept herself/himself, I value my own self. I accept myself as I am” . (p.15)
Participants believed that having hope for the future was also the key to health. They expressed hope as a driving force behind the development of mental health.
“When you have the hope of life, you are healthy; that is, there is something that pushes you forward” .(p.8)
Theme 2: Religious Beliefs
Another extracted theme of the study was religious beliefs. This theme consisted of ‘participating in religious ceremonies’ and ‘reciting the holy Quran and other religious books’.
2. A. Participating in religious ceremonies
Students asserted that participating in religious ceremonies, praying and asking God to provide help to meet their needs, help them overcome the problems and make them feel calm and relaxed.
“When I attend religious ceremonies, I feel well at the time” . (p. 3)
2.b. Reciting the holy Quran and other religious books
Students stated that they were turning to religious books when they felt lonely, depressed and troubled, and thus became mentally relaxed.
“Whenever I feel depressed or bored, either physically or mentally, I prefer to recite the holy Quran or pray. It helps me feel calm” .(p.5)
“I don’t feel lonely by reciting the holy Quran and thinking about God” .(p.7)
Theme 3: Socio-Economic Factors
Socio-economic factors were one of the most important and influential experiences in the mental health. This theme consisted of ‘social support’ and ‘economical support’.
3. a. Social Support
Students expressed that when they had a sense of family support and had suitable social relationships, such as the ability to communicate with parents, family, friends or university teachers, they felt mentally relaxed, and vice versa. This information empowered them.
“When your family understands you, you feel happy, but sometimes they cause you feel disappointed and depressed. Sometimes, they don’t live up to your expectations” .(p.6)
“My parents always remind me to inform them if any problem occurs, and I always do it. When I keep them posted on how my works go on, I feel mentally relaxed” .(p.17)
“When I’m getting along with my friends well, I feel mentally relaxed but when it is hard to get along with them or dispute a problem with them, I feel bored and tired” .(p.5)
“When I don’t behave like my friends, they often reject me or taunt me. They are the reasons to drive me up the wall” .(p.15)
“When you are in an environment where you feel you have a supporter, for example, a professor who can help you solve your problems, you can tolerate everything and you feel mentally sound” .(p.10)
3. b. Economical support
Students expressed that having at least the financial resources and having fun with their friends made them feel happy and ultimately mentally healthy. But they did not feel happy when they themselves had to work to meet their own education costs and when there was no possibility of having fun because of financial problems.
“Nowadays, being well off can calm you down mentally. When you have some money to have fun with, then you’re happy” .(p.13)
“It makes you upset when the prospects for the job are unclear or when you’re not sure what the future holds” .(p.18)
“When you have to work hard to help fund your studies, when you cannot go out and have fun with your friends, when you cannot dip into your own pocket, it is then that you feel small and humiliated” .(p.20)
Theme 4: Behavioral Factors
This theme includes the following sub-themes of disengagement, exercise, and balanced use of social networks. During the interviews, students often pointed to the role of these factors in mental health. According to the expressed experiences, nursing students described some behavioral factors in maintaining mental health and reducing their stress. They struggled to gain psychological stability by refraining from encounter with problems, physical and sports activities, which were often irregular, and also having self-control over the use of cyberspace.
4.a. Disengagement
Most participants stated that they were not involved in problems to maintain mental peace. They used ineffective mechanisms to solve problems such as avoidance and escape from problems.
“There are so many problems to which I do not want to think about. I try to avoid problems myself” .(p.15)
4.b. Physical exercise
Participants expressed that by exercising; they reduced their mental conflicts and experienced a sense of mental relaxation.
“The days I exercise myself or go to the gym, I feel happier. It makes me get rid of some intrusive thoughts. It helps you forget your daily problems for a few hours” .(p.13)
4. c. Balanced use of social networks
Another factor that participants felt to be effective in the sense of mental health was the balanced use of social networks and believed that excessive use of it caused anger and nervousness.
“I have a roommate who is always head over heels for social media. When you talk to her, she starts shouting and fighting. It has made her very nervous” .(p.7)
D ISCUSSION
The results of this study showed that there are many factors influencing the students’ perceptions of mental health. Data analysis revealed four themes and twelve sub-themes. The four themes were classified as: Feeling of self-worth, religious beliefs, socio-economic factors, and behavioral factors.
The feeling of self-worth theme included the five sub-themes of ‘confirmation’, ‘success’, ‘autonomy’, ‘self-acceptance’, and ‘hope’. Participants believed that when they received positive feedback from others and were confirmed, or when they were trying to succeed, or when they felt more autonomous, highly self-confident, ‘self-acceptance’, and hopeful, they found a positive perception of themselves, and this contributed to their mental well-being. Findings of some studies showed that there was a significant reverse correlation between self-reported stress and self-acceptance. This finding emphasized the importance of creating a sense of positive self-perception and self-confidence among nursing students to improve their mental health. Indeed, self-confidence in nursing students was considered as a buffer and protective shield in the face of stress and prevented mental disorder. Thus, the nursing students who have a sense of self-esteem have a high ability to communicate and can play an effective role in the development of the profession, handle fatigue and pressure, and positively impact the interpersonal relationships, quality of care, and job satisfaction. 23 , 24
The participants in the present study considered autonomy as an effective factor in creating positive sense of self-worth and in achieving mental well-being. The findings of this study are in line with those of a research done in Iranian context in which the researchers studied the concept of health in adolescents’ point of views. They expressed that autonomy and sense of independence is another key factor affecting health. They also continued that preventing adolescents and young people’s access to independence and posing unfair and undeserved restrictions for them can lead to some unsatisfactory consequences such as depression, hiding, urging, recklessness and immorality (night party, runaway, cigarette smoking, and addiction) and double dealing. 25
Another key sub-theme of the study was ‘hope’. The findings of the present study showed that those nursing students who had hope for the future had a better psychological feeling. Findings of a study conducted in Turkey reveled that university students have some negative mental states such as hopelessness and suicidal behavior. Their findings suggest that there are significant correlations among life satisfaction, hope, and mental health. 26 In fact, having self acceptance and positive self-image can act as a social protection factor against stress and anxiety. Those who feel good about themselves and are more confident also have a good sense of life and can successfully face problems and are able to handle them easily. Hope also makes life meaningful. It prevents us from mental breakdown and protects us from harmful situations. 6 In sum, it is argued that self-acceptance has been inversely associated with depressive symptoms, anxious symptomatology, and disruptive behaviors.
Another important theme of the research was religious beliefs. Participants stated that they felt mentally healthy when they participated in religious ceremonies. We know different religions have different beliefs. Several studies have shown a reciprocal relationship between different religious beliefs and mental health. The findings of research in Hindu system of beliefs showed that there was a significant negative correlation between the components of religious commitment, beliefs, and emotions, and components of general health (physical complaints, anxiety, depression and social dysfunction). They also proved that religion had a protective and supportive role for teenagers. 27 Another study conducted in Iranian context revealed that religiosity attitude was considered as a main factor affecting self-esteem and psychological hardiness and could promote psychological well-being. 28 Hence, institutionalizing of this religious teaching, trust in God, by health service developers and planners seems to be necessary in confronting the disruptive factors in mental health.
Another theme was socio-economic factors Participants in the present study described their mental health with various statements. Receiving emotional and spiritual support from family, friends, and university professors and their proper relationships, their empathy and verbal attention helped the students’ mental health. Indeed social support gives students a perception of being loved, cared, respected, and belonging to communication network. The results of the present study are in line with those reported in other studies. 29 , 30 In the present study, poor economic conditions had negative effects on the students’ perception of mental health. Economic deprivation, lack of a bright futures, and unemployment were regarded as mental and annoying concern which was affecting the mental health of the majority of participants. Generally, poor mental health is related to poor economic conditions. WHO states that mental health is determined by socio-economic and environmental factors, and economic crisis is likely to negatively affect the mental health. 31 Another study also mentioned that economic crisis can be associated with a higher use of prescription medications and an increase in hospitalization for mental disorders. 32
The last theme extracted from the study was behavioral factors. Participants stated that they do some behaviors such as disengagement, physical exercise, and use of social networks to relive stress.
Disengagement from problems is an avoiding and ineffective strategy to deal with stress. Therefore, it is necessary to provide students with the necessary training on effective coping strategies. Some studies have reported adverse coping strategies such as drinking alcohol, smoking, and waterpipe. 33 , 34 Participants in this study did not state the use of these materials perhaps because of the embarrassment and unfavorable views toward those who consume these materials in Iranian Islamic culture. In a qualitative study conducted in Malaysia, students showed that they used effective adaptive strategies and did not use undesirable behaviors. 35
In this study, nursing students expressed exercise and physical activities as another type of solution or strategy to achieve mental health. Although these activities were carried out irregularly and restrictively, they were described as useful in reducing daily stress. The results of a study in this area showed that increased physical activity which has been associated with life satisfaction, happiness, and positive attitude toward life can lead to the promotion of physical and mental health. 36
The balanced use of social networks was another subtheme of the study. Students argued that the high use of cyberspace or social networks has harmful effects on the nerves .Internet addiction and its association with mental distress can impact their academic achievement and long term career goals among medical students. Internet addiction would also indirectly impact the community of health care professionals and the society. There was a significant relationship between the student internet addiction and anxiety symptoms. 37 The results of another study showed that severe prevalence of internet addiction among nursing students was associated with poor mental health and depression without any impact on academic performance. 38
The strength of this study is that it increases our knowledge of the factors affecting the mental health of nursing students as a qualitative study conducted for the first time in Iran. However, as it is common for all qualitative studies, the results of the study cannot be generalized to other contexts and disciplines. Future qualitative and interventional studies are also suggested to be carried out in other contexts and on the students of other disciplines.
C ONCLUSION
The results showed that mental health in nursing students is a multidimensional phenomenon and is influenced by various factors. The current results could help the nurse educators to intervene and provide suitable, effective, practical, and culture based mental health services and help the nursing students achieve mental stability. Promoting physical activities among nursing students, training problem-solving skills and activating the student counseling centers at universities are suggested. Nurse educators and clinical psychologist can provide opportunities for nursing students to express their own concerns and learn the strategies to cope with crises. Finally, deep religious and moral beliefs can be effective in providing mental health to students.
A CKNOWLEDGEMENT
First, the researchers express thanks to the University of Medical Sciences, Khoy, Iran, for its support in carrying out this study. (Grant no. 1018). Our special thanks go to the nursing students who were voluntarily interviewed. Without them, this study would not have been possible. Their honesty and commitment were essential in carrying out this study.
Conflict of Interest: None declared.

- Undergraduate
- Postgraduate
Quick Access
- Find Your Programmes
- Our Faculties and Schools
- Programme A-Z
- Non-JUPAS Year 1
- Non-JUPAS Senior Year
- International / Other Qualifications
- Undergraduate Entry Scholarships
- Current Undergraduate Students
- A Unique Learning Experience
- University Ranking
- PolyU in Figures
- Student Stories
- A Day in PolyU
- Campus Life
- Virtual Campus Tour
- Campus Visit and School Talk
- International / Other Qualification
Sept 2025 Entry
116 (plus 41 clinical/field credits)
- Applicants should check with the professional bodies in their own countries for licensing requirements.
- BSc (Hons) in Mental Health Nursing

Programme Aims & Learning Outcomes
Our mission is to equip young people to take up professional careers in mental health nursing, one of the world’s most “caring” professions. This innovative academic programme develops students’ competence in delivering high-quality care, carrying out relevant research and making significant contributions to mental healthcare services.
Students develop skills in clinical reasoning, critical thinking, problem-solving, therapeutic communication and the management of change in mental health nursing. They also learn how to work both independently and with other healthcare professionals to provide high-quality mental healthcare in a range of contexts, from psychiatric clinical settings to community mental health services.
Programme Characteristics
PolyU was the first university in Hong Kong to provide a pre-registration degree programme in nursing. Our innovative approaches to learning and teaching enhance our students’ critical thinking and clinical decision making. This programme builds on our successful experience of conducting the psychiatric stream of the part-time Bachelor of Science (Honours) in Nursing programme, which is accredited by the Nursing Council of Hong Kong.
Our modern facilities include nursing therapeutics laboratories, mental health nursing laboratories, the Yuen Yuen Institute Chinese Medicinal Nursing Laboratory, the Dorothy Wong Intensive Care Laboratory, the Centre for Smart Health, the Herbal Medicine Learning Centre, the World Health Organization Collaborating Centre for Community Health Services, and the Yuen Yuen Institute Learning Resources Centre.
In this programme, field practice is arranged in a variety of healthcare settings, including general hospitals, psychiatric hospitals, psychiatric rehabilitation units, community psychiatric nursing services, mental health out-reaching services and other community settings. We also offer a wide range of overseas student exchange opportunities.
Professional Recognition
The programme is accredited by the Nursing Council of Hong Kong, and graduates are eligible to apply for registration as Registered Nurses (Psychiatric).
Career Prospects
Graduates are eligible to become Registered Nurses (Psychiatric) in Hong Kong. They can find employment in the Hospital Authority, government departments and non-government organisations.
Graduates can also find employment opportunities in various mental health settings, such as major psychiatric hospitals in Hong Kong, psychiatric units of general hospitals, and various rehabilitation sectors run by non-government organisations.
Graduates may also pursue further studies. They can pursue the Master of Science in Nursing programme or other postgraduate programmes offered by the School.
Graduates may also undertake research work or work overseas.
This is a 5-year full-time programme leading to registration with the Nursing Council of Hong Kong as a Registered Nurse (Psychiatric). The programme aims to equip students to become competent, creative, and caring practitioners of psychiatric/mental health nursing and to apply their creativity and critical thinking skills in the care of their clients.
The programme equips students to provide holistic care that encompasses safe, ethical, legal, and culturally sensitive nursing therapeutics provided to clients of all ages and their families in various mental healthcare settings, recognising their central role in managing mental healthcare. Students have opportunities to develop sensitivity through interactions with individuals, families, groups, communities, and other healthcare providers. Through their participation in the healthcare system, they are prepared to become key players in health promotion and care for psychiatric patients.
The programme curriculum is based on the Bio–Psycho–Social Model of Psychiatric Nursing Care and includes the following major content:
In junior years, studies include health foundation subjects to enhance students’ understanding of the factors predisposing and precipitating stresses. Applied sciences and nursing arts subjects such as Public Health and Infection Control, Human Physiology, Sociology of Health, Introduction to Psychology, Human Anatomy, Fundamentals of Mental Health Nursing, Pathophysiology and Pharmacology, Medical and Surgical Nursing I, Communication Skills and Group Dynamics, Fundamentals of Nursing Therapeutics I & II, Abnormal Psychology and Mental Health Nursing Therapeutics I & II, Clinical Microbiology, and Fundamentals of Nursing Therapeutics in Chinese Medicine and Chinese Communication for Nursing are introduced in the first two years of study.
In senior years, the programme broadens the focus from illness to health to develop nurses’ understanding of people and their experiences with health and recovery. Inherent in this orientation is the use of blended teaching methodologies, which encourage students to develop their critical thinking, enhance their self-awareness, and discover the world around them. Subjects such as Medical and Surgical Nursing II, Psychotherapeutic Practice, Quality and Patient Safety, Mental Health Nursing Therapeutics III & IV, Mental Health Education and Promotion, Neurobiological Basis in Mental Health, Ethical and Legal Aspects in Health Care, Mental Health Nursing Therapeutics in Community, Nursing Research and the Honours Project are introduced.
In Year 5, the programme focuses on preparing students to take up the role of Registered Nurse. Subjects such as Psychotherapeutic Practice II and Leadership Roles and Management Functions in Health Care are offered.
There is an emphasis throughout the programme on practical experience as the foundation for integrating psychiatric nursing theory into practice. Students are encouraged to be thoughtful and reflective in their nursing practice. Psychiatric/mental health nursing practice experience is essential. Students are directly involved with clients in their homes and in hospitals and community settings. This may involve working in shifts.
A specific set of General University Requirement subjects, such as Artificial Intelligence and Data Analytics, Innovation and Entrepreneurship, Leadership Education and Development, Healthy Lifestyle, Language and Communication, Service Learning, and broader subjects provide students with a comprehensive knowledge base for holistic professional learning.
Information on the subjects offered can be found here .
Dr Sau Fong LEUNG
PhD (Syd.); MSc (HC) [PolyU (HK)]; BN (Syd.); Dip(PN) (H.K.G.H.S.P.N.); PRegDip(N) (HKPoly); RN (HK); RN (NSW); RN (UKCC); RNT (HK)
Please click here to view the entrance requirements for international applicants.
Other Information
- Preference is given to those who are competent in written English and Chinese, and in oral English and Cantonese. (Applicants for clinical placements are expected to communicate in Cantonese, including speaking and listening.)
- Students must pass a health check before clinical training.
For further programme information, please contact:
The General Office (tel: 2766 4369; fax: 2364 9663; email: [email protected] ; website: sn.polyu.edu.hk ).
Studying Mental Health Nursing in PolyU’s School of Nursing is a wonderful experience. The programme has given me many opportunities to learn, develop nursing competency, and explore career pathways as well as lifelong goals.
The five-year programme equips students with fundamental nursing and mental health knowledge. It covers areas such as psychology, human anatomy, physiology, public health, and infection control. The teaching of ethics, care-related concepts and communication skills prepares us to participate in healthcare communication and decision making with an empathetic heart and a caring disposition. In the senior years of my studies, I have learned more about mental illnesses, the progression of mental disorders, and the needs of patients, from the acute stage to the rehabilitation stage. The more I learn about the needs of patients on their journeys towards recovery, the more I want to use my knowledge and skills to help establish a therapeutic alliance to support patients in their recovery.
The School also offers us overseas learning opportunities. The overseas exchange programmes that I joined have broadened my horizon, prepared me to meet new challenges, increased my confidence, and developed my nursing competency for serving people with mental health needs from all walks of life.

Studying at PolyU is about more than getting the qualifications needed to become a registered nurse. It is about having a wonderful university life and personal growth. For those interested in biology and psychology, this five-year BSc (Honours) in Mental Health Nursing programme offers the chance to gain theoretical knowledge and practical skills related to health and mental care, and insights into nursing practice and mental health issues. The clinical placements give students opportunities to deepen their understanding of mental health illnesses, from minor mood disorders to severe psychiatric illnesses for children and the elderly, and to apply their communication skills while working with a multi-disciplinary healthcare team to provide nursing care in various settings.
During my studies, I joined various student societies and participated in some voluntary work. These activities enriched my knowledge and prepared me well to give care and support to others. Finally, I am grateful to my teachers and student academic advisors for giving me lots of support throughout the years of my study.

Please input your public examination results, such as HKDSE, HKCEE, HKAL, IGCSE, GCEAL, etc., by subject under the "Public Examination" section to your online application.
To evaluate the potential and interest of applicants, and to assess their language, communication skills and understanding of the nursing discipline.
About 1 hour
Shortlisted applicants will be invited to interviews.

- PolyU Main Site
- Academic Registry (AR)
- Global Engagement Office (GEO)
- Graduate School (GS)
- Office of Undergraduate Studies (OUS)
- Student Affairs Office (SAO)
- Hong Kong Community College (HKCC)
- School of Professional Education and Executive Development (SPEED)
- School Nominations Direct Admission Scheme (SNDAS)

COMMENTS
Psychiatric nurses face additional challenges due to negative perceptions, workplace violence, and a lack of respect, impacting their well-being and job satisfaction, which are crucial for improving psychiatric care and patient outcomes. This study aims to examine the relationship between effort-reward imbalance, well-being, burnout, and decent work among psychiatric nurses.
This state-of-the-evidence review summarizes characteristics of intervention studies published from January 2011 through December 2015, in five psychiatric nursing journals. Of the 115 intervention studies, 23 tested interventions for mental health staff, while 92 focused on interventions to promote the well-being of clients.
A qualitative study of mental health nurse identities: Many roles, one profession. International Journal of Mental Health Nursing, 18 (6), 383-390. [Google Scholar] Hurley, J. (2012). Perceptual shifts of priority: a qualitative study bringing emotional intelligence to the foreground for nurses in talk‐based therapy roles.
85 baseline (42% mental health nurses), 74 at follow up. 24 1 h sessions per unit over six months. Facilitated by clinical psychologist. Formulation-based with written report and care planning. WAI- short form (staff and patient report), completed in relation to key worker: Intention to treat analysis controlling for clustering.
International Journal of Mental Health Nursing is a mental health journal examining trends and developments in mental health practice and research. ... although 18.7% had sample sizes below 1000. In terms of study duration, 66 studies spanned <5 years, 44 studies lasted between 5 and 10 years, and 30 studies extended for 10-20 years. Mental ...
The Journal of the American Psychiatric Nurses Association (JAPNA) is a peer-reviewed bi-monthly journal publishing up-to-date information to promote psychiatric nursing, improve mental health care for culturally diverse individuals, families, groups, and communities, as well as shape health care policy for the delivery of mental health services. ...
Inclusion criteria for studies were English language accounts of empirical research which investigated mental health nurses' experience of providing physical health care or examined the effectiveness of any intervention that aimed to improve outcomes related to the provision of physical healthcare. Thus, studies of interventions aimed at changing nursing practice, behaviour, knowledge ...
The Journal of Psychiatric & Mental Health Nursing is pleased to present this very special Virtual Issue. This is a collection of people's mental health and mental illness narratives from this section's inception, in one place. This collection is free to access and all lived experience narratives are free to view.
Current State of the Future of Nursing Recommendations. Experts have described the arena of children's mental health as a "labyrinth of systems" (Miles, Espiritu, Horen, Sebian, & Waetzig, 2010), reflecting its complex nature and characterized as multiple silos of influence where children receive care.These silos include public health systems, schools, communities, faith organizations ...
One study acknowledged there is a lack of an agreed definition of resilience in mental health nursing (Delgado et al., 2020), and two others noted that the primary focus of resilience research in mental health nursing has been on individual resilience rather than inclusive of its complex and multidimensional nature (Dahan et al., 2022; Delgado ...
The future of nursing: A guide for advancement in the US. Two publications, The Future of Nursing: Leading Change, Advancing Health (IOM, Citation 2011) and The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (NASEM, Citation 2021) have focused on how the discipline of nursing can engage with individuals, families, and communities in the US.
The therapeutic. relationship is considered the fundamental core of care in psychiatric and mental health nursing. [2]. The nurse must utilize their communication skills, understanding of human ...
Challenges of mental health care delivery. Care of patients in psychiatric intensive care (PICU), a challenging environment for humanistic psychiatric nursing practice, was the topic of an integrative review article by Swedish author Martin Salzmann-Erikson (Citation 2023, this issue).The author sought to synthesize research conducted within the past 5 years.
The nursing care of individuals with mental illness in the ED is complex. A scoping review is undertaken to contextualize knowledge on the nursing care of psychiatric patients in the ED, determine the current understanding, and identify gaps in the literature. A scoping review is a study that allows for the mapping of key concepts and relevant ...
The same study found that patients and nurses were equally satisfied with the quality of psychiatric nursing care, but patients scored lower than nurses . According to Zhao et al. [ 7 ], because nurses and patients use distinct criteria and methods to describe and assess the nursing care given, they have diverse perspectives on the quality of ...
For anyone requiring immediate crisis intervention or assistance finding a local mental health provider, the following resources are available: Mental Health America: 1-866-400-6428 for referrals, 1-800-273-8255 for crisis. National Alliance on Mental Illness HelpLine 1-800-950-6264.
Design: This is a cross-sectional and correlational study. Method: All participants were recruited from psychiatric wards of six hospitals in Taiwan. The data were collected through structured questionnaires from October 2013-March 2014 and a total of 278 psychiatric wards nurses participated in this study and completed all questionnaires.
This study aims to explore nurses' experiences with workplace violence and the impact of violence on nurses. Whereas the objectives of this study are to explore and analyze mental health nurses' experiences with workplace violence in Brunei Darussalam, identify and explore the impact of violence on mental health nurses, and discuss nurses' coping mechanisms following a workplace violence ...
International Journal of Mental Health Nursing is a mental health journal examining trends and developments in mental health practice and research. ... Correspondence: Kim Foster, Mental Health Nursing Research Unit, Australian Catholic University & North Western ... In-depth qualitative studies exploring nurses' experiences of challenging ...
their clinical experience. A number of recommendations were proposed in order to support the psychiatric nursing clinical practice. Keywords: Clinical practice , Nursing student, Psychiatry, Qualitative study, Saudi Arabia I. Introduction Psychiatric mental health nursing is a specialized area of nursing practice, education, and research that
Some studies focused on examining nurses when they encounter violence and suicidal patients [16,17]. However, there are few studies examining emergency department nursing care of psychiatric patients, particularly the experiences and thoughts of emergency department nurses when they care for psychiatric patients [18,19]. These studies ...
In this study, psychiatric nurses with lower self-compassion were younger, had fewer years of experience, and cared for fewer patients during a shift. In contrast, nurses with high self-compassion were aged ≥ 45 years, were from urban areas, had a bachelor's degree in nursing (high academic degree), were working < 45 h per week, and were ...
The period of scientific study and treatment of mental disorders began with Sigmund Freud (1856-1939) and others, such as Emil Kraeplin (1856-1926) and Eugene Bleuler ... In 1973, the division of psychiatric and mental health practice of the American Nurses Association (ANA) developed standards of care, which it revised in 1982, 1994, and 2000. ...
The COVID-19 pandemic imposed unprecedented demands on health services (Maben & Bridges, 2020) and, as part of the response, nurses were redeployed to support patient care (Dunn et al., 2020).Redeployment - reassigning employees to new places or functions - is used to manage staffing numbers and patient safety by covering areas where the number and acuity of patients requires a greater ...
Around 50,000 people leave mental healthcare hospitals every year. However, a national survey from the mental health charity Mind, found that 40 per cent of those have no plan in place to support them after they leave. Sarah Rae, a mental health service user, experienced difficulties when discharged from mental health wards in the past.
Planes filled the air, carrying young soldiers from the United States into the heart of Afghanistan's treacherous terrain. With each step onto foreign soil, soldiers, like Utah State University alum Jacob Hunsaker '13 BA, '15 MMFT, '21 BSN, a member of the U.S. Army Reserve, braced for the battles ahead, knowing they would test their resolve and change them forever.
We are interested in funding high quality applied health and social care research to increase and improve the evidence base about mental health nursing and the mental health nursing workforce. Our Health Technology Assessment (HTA) Programme is accepting Stage 1 applications to this funding opportunity.
The study was led by researchers from the University of Liverpool. They worked with researchers internationally to anonymously link three groups of records: household greenness; access to green and blue space; GP records of anxiety and depression for over 2 million adults in Wales; The effects of green spaces on mental health are well documented.
The results of the present study are in line with those reported in other studies. 29, 30 In the present study, poor economic conditions had negative effects on the students' perception of mental health. Economic deprivation, lack of a bright futures, and unemployment were regarded as mental and annoying concern which was affecting the mental ...
This is a 5-year full-time programme leading to registration with the Nursing Council of Hong Kong as a Registered Nurse (Psychiatric). The programme aims to equip students to become competent, creative, and caring practitioners of psychiatric/mental health nursing and to apply their creativity and critical thinking skills in the care of their clients.