
- Bachelor’s Degrees
- Master’s Degrees
- Doctorate Degrees
- Certificate Programs
- Nursing Degrees
- Cybersecurity
- Human Services
- Science & Mathematics
- Communication
- Liberal Arts
- Social Sciences
- Computer Science
- Admissions Overview
- Tuition and Financial Aid
- Incoming Freshman and Graduate Students
- Transfer Students
- Military Students
- International Students
- Early Access Program
- About Maryville
- Our Faculty
- Our Approach
- Our History
- Accreditation
- Tales of the Brave
- Student Support Overview
- Online Learning Tools
- Infographics
Home / Blog

Speech Impediment Guide: Definition, Causes, and Resources
December 8, 2020

Tables of Contents
What Is a Speech Impediment?
Types of speech disorders, speech impediment causes, how to fix a speech impediment, making a difference in speech disorders.
Communication is a cornerstone of human relationships. When an individual struggles to verbalize information, thoughts, and feelings, it can cause major barriers in personal, learning, and business interactions.
Speech impediments, or speech disorders, can lead to feelings of insecurity and frustration. They can also cause worry for family members and friends who don’t know how to help their loved ones express themselves.
Fortunately, there are a number of ways that speech disorders can be treated, and in many cases, cured. Health professionals in fields including speech-language pathology and audiology can work with patients to overcome communication disorders, and individuals and families can learn techniques to help.

Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual’s ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
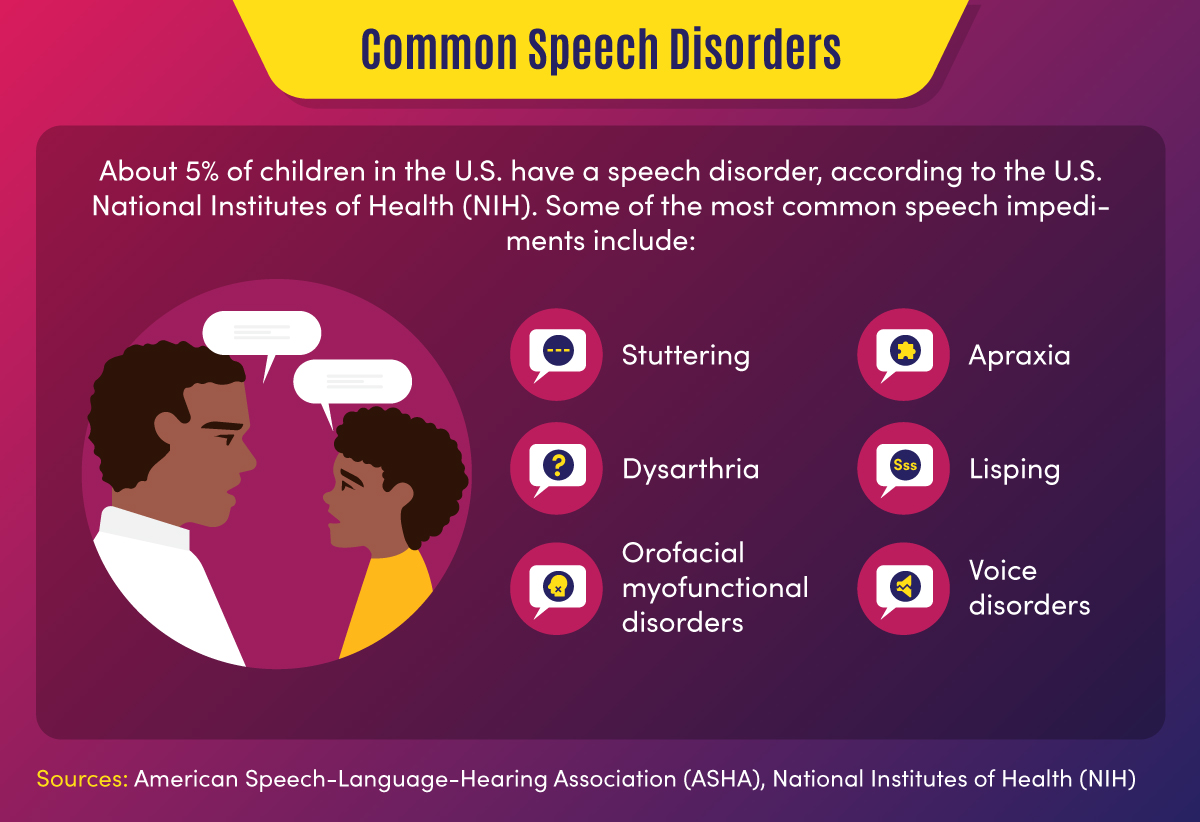
Some 7.7% of U.S. children — or 1 in 12 youths between the ages of 3 and 17 — have speech, voice, language, or swallowing disorders, according to the National Institute on Deafness and Other Communication Disorders (NIDCD). About 70 million people worldwide, including some 3 million Americans, experience stuttering difficulties, according to the Stuttering Foundation.
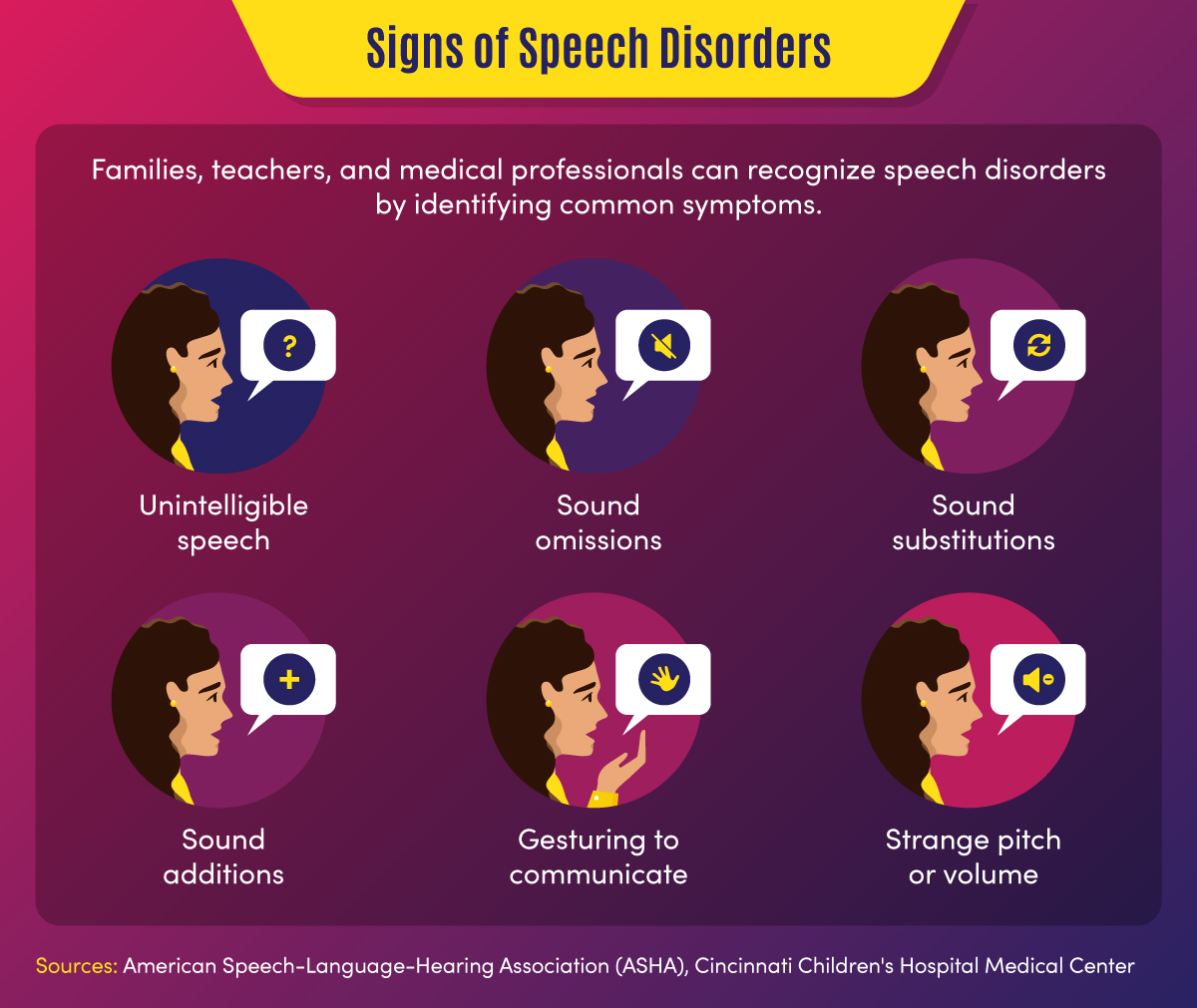
Common signs of a speech disorder
There are several symptoms and indicators that can point to a speech disorder.
- Unintelligible speech — A speech disorder may be present when others have difficulty understanding a person’s verbalizations.
- Omitted sounds — This symptom can include the omission of part of a word, such as saying “bo” instead of “boat,” and may include omission of consonants or syllables.
- Added sounds — This can involve adding extra sounds in a word, such as “buhlack” instead of “black,” or repeating sounds like “b-b-b-ball.”
- Substituted sounds — When sounds are substituted or distorted, such as saying “wabbit” instead of “rabbit,” it may indicate a speech disorder.
- Use of gestures — When individuals use gestures to communicate instead of words, a speech impediment may be the cause.
- Inappropriate pitch — This symptom is characterized by speaking with a strange pitch or volume.
In children, signs might also include a lack of babbling or making limited sounds. Symptoms may also include the incorrect use of specific sounds in words, according to the American Speech-Language-Hearing Association (ASHA). This may include the sounds p, m, b, w, and h among children aged 1-2, and k, f, g, d, n, and t for children aged 2-3.
Back To Top
Categories of Speech Impediments
Speech impediments can range from speech sound disorders (articulation and phonological disorders) to voice disorders. Speech sound disorders may be organic — resulting from a motor or sensory cause — or may be functional with no known cause. Voice disorders deal with physical problems that limit speech. The main categories of speech impediments include the following:
Fluency disorders occur when a patient has trouble with speech timing or rhythms. This can lead to hesitations, repetitions, or prolonged sounds. Fluency disorders include stuttering (repetition of sounds) or (rapid or irregular rate of speech).
Resonance disorders are related to voice quality that is impacted by the shape of the nose, throat, and/or mouth. Examples of resonance disorders include hyponasality and cul-de-sac resonance.
Articulation disorders occur when a patient has difficulty producing speech sounds. These disorders may stem from physical or anatomical limitations such as muscular, neuromuscular, or skeletal support. Examples of articulation speech impairments include sound omissions, substitutions, and distortions.
Phonological disorders result in the misuse of certain speech sounds to form words. Conditions include fronting, stopping, and the omission of final consonants.
Voice disorders are the result of problems in the larynx that harm the quality or use of an individual’s voice. This can impact pitch, resonance, and loudness.
Impact of Speech Disorders
Some speech disorders have little impact on socialization and daily activities, but other conditions can make some tasks difficult for individuals. Following are a few of the impacts of speech impediments.
- Poor communication — Children may be unable to participate in certain learning activities, such as answering questions or reading out loud, due to communication difficulties. Adults may avoid work or social activities such as giving speeches or attending parties.
- Mental health and confidence — Speech disorders may cause children or adults to feel different from peers, leading to a lack of self-confidence and, potentially, self-isolation.
Resources on Speech Disorders
The following resources may help those who are seeking more information about speech impediments.
Health Information : Information and statistics on common voice and speech disorders from the NIDCD
Speech Disorders : Information on childhood speech disorders from Cincinnati Children’s Hospital Medical Center
Speech, Language, and Swallowing : Resources about speech and language development from the ASHA
Children and adults can suffer from a variety of speech impairments that may have mild to severe impacts on their ability to communicate. The following 10 conditions are examples of specific types of speech disorders and voice disorders.
1. Stuttering
This condition is one of the most common speech disorders. Stuttering is the repetition of syllables or words, interruptions in speech, or prolonged use of a sound.
This organic speech disorder is a result of damage to the neural pathways that connect the brain to speech-producing muscles. This results in a person knowing what they want to say, but being unable to speak the words.
This consists of the lost ability to speak, understand, or write languages. It is common in stroke, brain tumor, or traumatic brain injury patients.
4. Dysarthria
This condition is an organic speech sound disorder that involves difficulty expressing certain noises. This may involve slurring, or poor pronunciation, and rhythm differences related to nerve or brain disorders.
The condition of lisping is the replacing of sounds in words, including “th” for “s.” Lisping is a functional speech impediment.
6. Hyponasality
This condition is a resonance disorder related to limited sound coming through the nose, causing a “stopped up” quality to speech.
7. Cul-de-sac resonance
This speech disorder is the result of blockage in the mouth, throat, or nose that results in quiet or muffled speech.
8. Orofacial myofunctional disorders
These conditions involve abnormal patterns of mouth and face movement. Conditions include tongue thrusting (fronting), where individuals push out their tongue while eating or talking.
9. Spasmodic Dysphonia
This condition is a voice disorder in which spasms in the vocal cords produce speech that is hoarse, strained, or jittery.
10. Other voice disorders
These conditions can include having a voice that sounds breathy, hoarse, or scratchy. Some disorders deal with vocal folds closing when they should open (paradoxical vocal fold movement) or the presence of polyps or nodules in the vocal folds.
Speech Disorders vs. Language Disorders
Speech disorders deal with difficulty in creating sounds due to articulation, fluency, phonology, and voice problems. These problems are typically related to physical, motor, sensory, neurological, or mental health issues.
Language disorders, on the other hand, occur when individuals have difficulty communicating the meaning of what they want to express. Common in children, these disorders may result in low vocabulary and difficulty saying complex sentences. Such a disorder may reflect difficulty in comprehending school lessons or adopting new words, or it may be related to a learning disability such as dyslexia. Language disorders can also involve receptive language difficulties, where individuals have trouble understanding the messages that others are trying to convey.
Resources on Types of Speech Disorders
The following resources may provide additional information on the types of speech impediments.
Common Speech Disorders: A guide to the most common speech impediments from GreatSpeech
Speech impairment in adults: Descriptions of common adult speech issues from MedlinePlus
Stuttering Facts: Information on stuttering indications and causes from the Stuttering Foundation
Speech disorders may be caused by a variety of factors related to physical features, neurological ailments, or mental health conditions. In children, they may be related to developmental issues or unknown causes and may go away naturally over time.
Physical and neurological issues. Speech impediment causes related to physical characteristics may include:
- Brain damage
- Nervous system damage
- Respiratory system damage
- Hearing difficulties
- Cancerous or noncancerous growths
- Muscle and bone problems such as dental issues or cleft palate
Mental health issues. Some speech disorders are related to clinical conditions such as:
- Autism spectrum disorder
- Down syndrome or other genetic syndromes
- Cerebral palsy or other neurological disorders
- Multiple sclerosis
Some speech impairments may also have to do with family history, such as when parents or siblings have experienced language or speech difficulties. Other causes may include premature birth, pregnancy complications, or delivery difficulties. Voice overuse and chronic coughs can also cause speech issues.
The most common way that speech disorders are treated involves seeking professional help. If patients and families feel that symptoms warrant therapy, health professionals can help determine how to fix a speech impediment. Early treatment is best to curb speech disorders, but impairments can also be treated later in life.
Professionals in the speech therapy field include speech-language pathologists (SLPs) . These practitioners assess, diagnose, and treat communication disorders including speech, language, social, cognitive, and swallowing disorders in both adults and children. They may have an SLP assistant to help with diagnostic and therapy activities.
Speech-language pathologists may also share a practice with audiologists and audiology assistants. Audiologists help identify and treat hearing, balance, and other auditory disorders.
How Are Speech Disorders Diagnosed?
Typically, a pediatrician, social worker, teacher, or other concerned party will recognize the symptoms of a speech disorder in children. These individuals, who frequently deal with speech and language conditions and are more familiar with symptoms, will recommend that parents have their child evaluated. Adults who struggle with speech problems may seek direct guidance from a physician or speech evaluation specialist.
When evaluating a patient for a potential speech impediment, a physician will:
- Conduct hearing and vision tests
- Evaluate patient records
- Observe patient symptoms
A speech-language pathologist will conduct an initial screening that might include:
- An evaluation of speech sounds in words and sentences
- An evaluation of oral motor function
- An orofacial examination
- An assessment of language comprehension
The initial screening might result in no action if speech symptoms are determined to be developmentally appropriate. If a disorder is suspected, the initial screening might result in a referral for a comprehensive speech sound assessment, comprehensive language assessment, audiology evaluation, or other medical services.
Initial assessments and more in-depth screenings might occur in a private speech therapy practice, rehabilitation center, school, childcare program, or early intervention center. For older adults, skilled nursing centers and nursing homes may assess patients for speech, hearing, and language disorders.
How Are Speech Impediments Treated?
Once an evaluation determines precisely what type of speech sound disorder is present, patients can begin treatment. Speech-language pathologists use a combination of therapy, exercise, and assistive devices to treat speech disorders.
Speech therapy might focus on motor production (articulation) or linguistic (phonological or language-based) elements of speech, according to ASHA. There are various types of speech therapy available to patients.
Contextual Utilization — This therapeutic approach teaches methods for producing sounds consistently in different syllable-based contexts, such as phonemic or phonetic contexts. These methods are helpful for patients who produce sounds inconsistently.
Phonological Contrast — This approach focuses on improving speech through emphasis of phonemic contrasts that serve to differentiate words. Examples might include minimal opposition words (pot vs. spot) or maximal oppositions (mall vs. call). These therapy methods can help patients who use phonological error patterns.
Distinctive Feature — In this category of therapy, SLPs focus on elements that are missing in speech, such as articulation or nasality. This helps patients who substitute sounds by teaching them to distinguish target sounds from substituted sounds.
Core Vocabulary — This therapeutic approach involves practicing whole words that are commonly used in a specific patient’s communications. It is effective for patients with inconsistent sound production.
Metaphon — In this type of therapy, patients are taught to identify phonological language structures. The technique focuses on contrasting sound elements, such as loud vs. quiet, and helps patients with unintelligible speech issues.
Oral-Motor — This approach uses non-speech exercises to supplement sound therapies. This helps patients gain oral-motor strength and control to improve articulation.
Other methods professionals may use to help fix speech impediments include relaxation, breathing, muscle strengthening, and voice exercises. They may also recommend assistive devices, which may include:
- Radio transmission systems
- Personal amplifiers
- Picture boards
- Touch screens
- Text displays
- Speech-generating devices
- Hearing aids
- Cochlear implants
Resources for Professionals on How to Fix a Speech Impediment
The following resources provide information for speech therapists and other health professionals.
Assistive Devices: Information on hearing and speech aids from the NIDCD
Information for Audiologists: Publications, news, and practice aids for audiologists from ASHA
Information for Speech-Language Pathologists: Publications, news, and practice aids for SLPs from ASHA
Speech Disorder Tips for Families
For parents who are concerned that their child might have a speech disorder — or who want to prevent the development of a disorder — there are a number of activities that can help. The following are tasks that parents can engage in on a regular basis to develop literacy and speech skills.
- Introducing new vocabulary words
- Reading picture and story books with various sounds and patterns
- Talking to children about objects and events
- Answering children’s questions during routine activities
- Encouraging drawing and scribbling
- Pointing to words while reading books
- Pointing out words and sentences in objects and signs
Parents can take the following steps to make sure that potential speech impediments are identified early on.
- Discussing concerns with physicians
- Asking for hearing, vision, and speech screenings from doctors
- Requesting special education assessments from school officials
- Requesting a referral to a speech-language pathologist, audiologist, or other specialist
When a child is engaged in speech therapy, speech-language pathologists will typically establish collaborative relationships with families, sharing information and encouraging parents to participate in therapy decisions and practices.
SLPs will work with patients and their families to set goals for therapy outcomes. In addition to therapy sessions, they may develop activities and exercises for families to work on at home. It is important that caregivers are encouraging and patient with children during therapy.
Resources for Parents on How to Fix a Speech Impediment
The following resources provide additional information on treatment options for speech disorders.
Speech, Language, and Swallowing Disorders Groups: Listing of self-help groups from ASHA
ProFind: Search tool for finding certified SLPs and audiologists from ASHA
Baby’s Hearing and Communication Development Checklist: Listing of milestones that children should meet by certain ages from the NIDCD
If identified during childhood, speech disorders can be corrected efficiently, giving children greater communication opportunities. If left untreated, speech impediments can cause a variety of problems in adulthood, and may be more difficult to diagnose and treat.
Parents, teachers, doctors, speech and language professionals, and other concerned parties all have unique responsibilities in recognizing and treating speech disorders. Through professional therapy, family engagement, positive encouragement and a strong support network, individuals with speech impediments can overcome their challenges and develop essential communication skills.
Additional Sources
American Speech-Language-Hearing Association, Speech Sound Disorders
Identify the Signs, Signs of Speech and Language Disorders
Intermountain Healthcare, Phonological Disorders
MedlinePlus, Speech disorders – children
National Institutes of Health, National Institutes on Deafness and Other Communication Disorders, “Quick Statistics About Voice, Speech, Language”
Bring us your ambition and we’ll guide you along a personalized path to a quality education that’s designed to change your life.
Take Your Next Brave Step
Receive information about the benefits of our programs, the courses you'll take, and what you need to apply.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Overcoming Speech Impediment: Symptoms to Treatment
There are many causes and solutions for impaired speech
- Types and Symptoms
- Speech Therapy
- Building Confidence
Speech impediments are conditions that can cause a variety of symptoms, such as an inability to understand language or speak with a stable sense of tone, speed, or fluidity. There are many different types of speech impediments, and they can begin during childhood or develop during adulthood.
Common causes include physical trauma, neurological disorders, or anxiety. If you or your child is experiencing signs of a speech impediment, you need to know that these conditions can be diagnosed and treated with professional speech therapy.
This article will discuss what you can do if you are concerned about a speech impediment and what you can expect during your diagnostic process and therapy.
FG Trade / Getty Images
Types and Symptoms of Speech Impediment
People can have speech problems due to developmental conditions that begin to show symptoms during early childhood or as a result of conditions that may occur during adulthood.
The main classifications of speech impairment are aphasia (difficulty understanding or producing the correct words or phrases) or dysarthria (difficulty enunciating words).
Often, speech problems can be part of neurological or neurodevelopmental disorders that also cause other symptoms, such as multiple sclerosis (MS) or autism spectrum disorder .
There are several different symptoms of speech impediments, and you may experience one or more.
Can Symptoms Worsen?
Most speech disorders cause persistent symptoms and can temporarily get worse when you are tired, anxious, or sick.
Symptoms of dysarthria can include:
- Slurred speech
- Slow speech
- Choppy speech
- Hesitant speech
- Inability to control the volume of your speech
- Shaking or tremulous speech pattern
- Inability to pronounce certain sounds
Symptoms of aphasia may involve:
- Speech apraxia (difficulty coordinating speech)
- Difficulty understanding the meaning of what other people are saying
- Inability to use the correct words
- Inability to repeat words or phases
- Speech that has an irregular rhythm
You can have one or more of these speech patterns as part of your speech impediment, and their combination and frequency will help determine the type and cause of your speech problem.
Causes of Speech Impediment
The conditions that cause speech impediments can include developmental problems that are present from birth, neurological diseases such as Parkinson’s disease , or sudden neurological events, such as a stroke .
Some people can also experience temporary speech impairment due to anxiety, intoxication, medication side effects, postictal state (the time immediately after a seizure), or a change of consciousness.
Speech Impairment in Children
Children can have speech disorders associated with neurodevelopmental problems, which can interfere with speech development. Some childhood neurological or neurodevelopmental disorders may cause a regression (backsliding) of speech skills.
Common causes of childhood speech impediments include:
- Autism spectrum disorder : A neurodevelopmental disorder that affects social and interactive development
- Cerebral palsy : A congenital (from birth) disorder that affects learning and control of physical movement
- Hearing loss : Can affect the way children hear and imitate speech
- Rett syndrome : A genetic neurodevelopmental condition that causes regression of physical and social skills beginning during the early school-age years.
- Adrenoleukodystrophy : A genetic disorder that causes a decline in motor and cognitive skills beginning during early childhood
- Childhood metabolic disorders : A group of conditions that affects the way children break down nutrients, often resulting in toxic damage to organs
- Brain tumor : A growth that may damage areas of the brain, including those that control speech or language
- Encephalitis : Brain inflammation or infection that may affect the way regions in the brain function
- Hydrocephalus : Excess fluid within the skull, which may develop after brain surgery and can cause brain damage
Do Childhood Speech Disorders Persist?
Speech disorders during childhood can have persistent effects throughout life. Therapy can often help improve speech skills.
Speech Impairment in Adulthood
Adult speech disorders develop due to conditions that damage the speech areas of the brain.
Common causes of adult speech impairment include:
- Head trauma
- Nerve injury
- Throat tumor
- Stroke
- Parkinson’s disease
- Essential tremor
- Brain tumor
- Brain infection
Additionally, people may develop changes in speech with advancing age, even without a specific neurological cause. This can happen due to presbyphonia , which is a change in the volume and control of speech due to declining hormone levels and reduced elasticity and movement of the vocal cords.
Do Speech Disorders Resolve on Their Own?
Children and adults who have persistent speech disorders are unlikely to experience spontaneous improvement without therapy and should seek professional attention.
Steps to Treating Speech Impediment
If you or your child has a speech impediment, your healthcare providers will work to diagnose the type of speech impediment as well as the underlying condition that caused it. Defining the cause and type of speech impediment will help determine your prognosis and treatment plan.
Sometimes the cause is known before symptoms begin, as is the case with trauma or MS. Impaired speech may first be a symptom of a condition, such as a stroke that causes aphasia as the primary symptom.
The diagnosis will include a comprehensive medical history, physical examination, and a thorough evaluation of speech and language. Diagnostic testing is directed by the medical history and clinical evaluation.
Diagnostic testing may include:
- Brain imaging , such as brain computerized tomography (CT) or magnetic residence imaging (MRI), if there’s concern about a disease process in the brain
- Swallowing evaluation if there’s concern about dysfunction of the muscles in the throat
- Electromyography (EMG) and nerve conduction studies (aka nerve conduction velocity, or NCV) if there’s concern about nerve and muscle damage
- Blood tests, which can help in diagnosing inflammatory disorders or infections
Your diagnostic tests will help pinpoint the cause of your speech problem. Your treatment will include specific therapy to help improve your speech, as well as medication or other interventions to treat the underlying disorder.
For example, if you are diagnosed with MS, you would likely receive disease-modifying therapy to help prevent MS progression. And if you are diagnosed with a brain tumor, you may need surgery, chemotherapy, or radiation to treat the tumor.
Therapy to Address Speech Impediment
Therapy for speech impairment is interactive and directed by a specialist who is experienced in treating speech problems . Sometimes, children receive speech therapy as part of a specialized learning program at school.
The duration and frequency of your speech therapy program depend on the underlying cause of your impediment, your improvement, and approval from your health insurance.
If you or your child has a serious speech problem, you may qualify for speech therapy. Working with your therapist can help you build confidence, particularly as you begin to see improvement.
Exercises during speech therapy may include:
- Pronouncing individual sounds, such as la la la or da da da
- Practicing pronunciation of words that you have trouble pronouncing
- Adjusting the rate or volume of your speech
- Mouth exercises
- Practicing language skills by naming objects or repeating what the therapist is saying
These therapies are meant to help achieve more fluent and understandable speech as well as an increased comfort level with speech and language.
Building Confidence With Speech Problems
Some types of speech impairment might not qualify for therapy. If you have speech difficulties due to anxiety or a social phobia or if you don’t have access to therapy, you might benefit from activities that can help you practice your speech.
You might consider one or more of the following for you or your child:
- Joining a local theater group
- Volunteering in a school or community activity that involves interaction with the public
- Signing up for a class that requires a significant amount of class participation
- Joining a support group for people who have problems with speech
Activities that you do on your own to improve your confidence with speaking can be most beneficial when you are in a non-judgmental and safe space.
Many different types of speech problems can affect children and adults. Some of these are congenital (present from birth), while others are acquired due to health conditions, medication side effects, substances, or mood and anxiety disorders. Because there are so many different types of speech problems, seeking a medical diagnosis so you can get the right therapy for your specific disorder is crucial.
Centers for Disease Control and Prevention. Language and speech disorders in children .
Han C, Tang J, Tang B, et al. The effectiveness and safety of noninvasive brain stimulation technology combined with speech training on aphasia after stroke: a systematic review and meta-analysis . Medicine (Baltimore). 2024;103(2):e36880. doi:10.1097/MD.0000000000036880
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, language .
Mackey J, McCulloch H, Scheiner G, et al. Speech pathologists' perspectives on the use of augmentative and alternative communication devices with people with acquired brain injury and reflections from lived experience . Brain Impair. 2023;24(2):168-184. doi:10.1017/BrImp.2023.9
Allison KM, Doherty KM. Relation of speech-language profile and communication modality to participation of children with cerebral palsy . Am J Speech Lang Pathol . 2024:1-11. doi:10.1044/2023_AJSLP-23-00267
Saccente-Kennedy B, Gillies F, Desjardins M, et al. A systematic review of speech-language pathology interventions for presbyphonia using the rehabilitation treatment specification system . J Voice. 2024:S0892-1997(23)00396-X. doi:10.1016/j.jvoice.2023.12.010
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
- Children's Health
- Common Symptoms
- Common Conditions
- Chronic Conditions
- View Full Guide
Common Speech and Language Disorders

Speech and language problems may make it hard for your child to understand and speak with others, or make the sounds of speech. They're common, affecting as many as one in 12 kids and teens in the U.S.
Kids with these disorders often have trouble when they learn to read and write, or when they try to be social and make friends. But treatment helps most children improve, especially if they start it early.
Adults can also have these disorders. It may have started in childhood, or they may have them because of other problems such as brain injuries, stroke , cancer , or dementia .
Speech Disorders
For children with speech disorders, it can be tough forming the sounds that make up speech or putting sentences together. Signs of a speech disorder include:
- Trouble with p, b, m, h, and w sounds at 1 to 2 years of age
- Problems with k, g, f, t, d, and n sounds between the ages of 2 and 3
- When people who know the child well find it hard to understand them
The causes of most speech disorders are unknown.
There are three major types:
Articulation: It’s hard for your child to pronounce words. They may drop sounds or use the wrong sounds and say things like “wabbit” instead of “rabbit.” Letters such as p, b, and m are easier to learn. Most kids can master those sounds by age 2. But r, l, and th sounds take longer to get right.
Fluency: Your child may have problems with how their words and sentences flow. Stuttering is a fluency disorder. That’s when your child repeats words, parts of words, or uses odd pauses. It’s common as kids approach 3 years of age. That’s when a child thinks faster than they can speak. If it lasts longer than 6 months, or if your child is more than 3.5 years old, get help.
Voice: If your child speaks too loudly, too softly, or is often hoarse, they may have a voice disorder. This can happen if your child speaks loudly and with too much force. Another cause is small growths on the vocal cords called nodules or polyps. They’re also due to too much voice stress.
Language Disorders
Does your child use fewer words and simpler sentences than their friends? These issues may be signs of a language disorder. For kids with this disorder, it’s hard to find the right words or speak in complete sentences. It may be tough for them to make sense of what others say. Your child may have this disorder if they:
- Don’t babble by 7 months
- Only speak a few words by 17 months
- Can’t put two words together by 2 years
- Have problems when they play and talk with other kids from the ages of 2 to 3
There are two major types of language disorders. It’s possible for a child to have both.
Receptive: This is when your child finds it hard to understand speech. They may find it hard to:
- Follow directions
- Answer questions
- Point to objects when asked
Expressive : If your child has trouble finding the right words to express themselves, they may have this type of language disorder. Kids with an expressive disorder may find it tough to:
- Ask questions
- String words into sentences
- Start and continue a conversation
It’s not always possible to trace the cause of language disorders. Physical causes of this type of disorder can include head injuries , illness, or ear infections . These are sometimes called acquired language disorders.
Other things that make it more likely include:
- A family history of language problems
- Being born early
- Down syndrome
- Poor nutrition
Doctors don’t always know what causes your child’s condition. Remember, these kinds of disorders have nothing to do with how smart your child is. Often, kids with language disorders are smarter than average.
Diagnosis and Treatment
Speech and language disorders are legally defined disabilities. Your child may get testing and treatment through your state’s early intervention program or local public schools. Some services are free.
Your child may see a speech language pathologist, or SLP. The SLP may try to find out if your child:
- Can follow directions
- Is able to name common objects
- Knows how to play with toys
- Can hold books the right way
The SLP will first check your child’s hearing. If that’s OK, the SLP will do tests to find out what kind of disorder may be present, if it’s a short-term problem or one that needs treatment, and what treatment plan to recommend.
How to Help Your Child
Children learn and grow at their own pace. The younger they are, the more likely they are to make mistakes. So you’ll want to learn the milestones. Know what skills your child should be able to master at a given age.
To help your child with their speech and language skills:
- Talk to your child, even as a newborn .
- Point to objects and name them.
- When your child is ready, ask them questions.
- Respond to what they say, but don’t correct mistakes.
- Read to your child at least 15 minutes a day.
If your child has one of these disorders, don’t assume they’ll outgrow it. But treatment does help most kids get better. The sooner they get it, the better the results.
Top doctors in ,
Find more top doctors on, related links.
- Children's Health News
- Children's Health Reference
- Children's Health Slideshows
- Children's Health Quizzes
- Children's Health Videos
- Find a Pediatrician
- ADHD in Children
- Baby Development
- BMI Calculator for Parents
- Children's Vaccines
- Kids' Dental Care
- Newborn & Baby
- Teen Health
- More Related Topics

10 Most Common Speech-Language Disorders & Impediments
As you get to know more about the field of speech-language pathology you’ll increasingly realize why SLPs are required to earn at least a master’s degree . This stuff is serious – and there’s nothing easy about it.
In 2016 the National Institute on Deafness and Other Communication Disorders reported that 7.7% of American children have been diagnosed with a speech or swallowing disorder. That comes out to nearly one in 12 children, and gets even bigger if you factor in adults.
Whether rooted in psycho-speech behavioral issues, muscular disorders, or brain damage, nearly all the diagnoses SLPs make fall within just 10 common categories…
Types of Speech Disorders & Impediments
Apraxia of speech (aos).
Apraxia of Speech (AOS) happens when the neural pathway between the brain and a person’s speech function (speech muscles) is lost or obscured. The person knows what they want to say – they can even write what they want to say on paper – however the brain is unable to send the correct messages so that speech muscles can articulate what they want to say, even though the speech muscles themselves work just fine. Many SLPs specialize in the treatment of Apraxia .
There are different levels of severity of AOS, ranging from mostly functional, to speech that is incoherent. And right now we know for certain it can be caused by brain damage, such as in an adult who has a stroke. This is called Acquired AOS.
However the scientific and medical community has been unable to detect brain damage – or even differences – in children who are born with this disorder, making the causes of Childhood AOS somewhat of a mystery. There is often a correlation present, with close family members suffering from learning or communication disorders, suggesting there may be a genetic link.
Mild cases might be harder to diagnose, especially in children where multiple unknown speech disorders may be present. Symptoms of mild forms of AOS are shared by a range of different speech disorders, and include mispronunciation of words and irregularities in tone, rhythm, or emphasis (prosody).
Stuttering – Stammering
Stuttering, also referred to as stammering, is so common that everyone knows what it sounds like and can easily recognize it. Everyone has probably had moments of stuttering at least once in their life. The National Institute on Deafness and Other Communication Disorders estimates that three million Americans stutter, and reports that of the up-to-10-percent of children who do stutter, three-quarters of them will outgrow it. It should not be confused with cluttering.
Most people don’t know that stuttering can also include non-verbal involuntary or semi-voluntary actions like blinking or abdominal tensing (tics). Speech language pathologists are trained to look for all the symptoms of stuttering , especially the non-verbal ones, and that is why an SLP is qualified to make a stuttering diagnosis.
The earliest this fluency disorder can become apparent is when a child is learning to talk. It may also surface later during childhood. Rarely if ever has it developed in adults, although many adults have kept a stutter from childhood.
Stuttering only becomes a problem when it has an impact on daily activities, or when it causes concern to parents or the child suffering from it. In some people, a stutter is triggered by certain events like talking on the phone. When people start to avoid specific activities so as not to trigger their stutter, this is a sure sign that the stutter has reached the level of a speech disorder.
The causes of stuttering are mostly a mystery. There is a correlation with family history indicating a genetic link. Another theory is that a stutter is a form of involuntary or semi-voluntary tic. Most studies of stuttering agree there are many factors involved.
Dysarthria is a symptom of nerve or muscle damage. It manifests itself as slurred speech, slowed speech, limited tongue, jaw, or lip movement, abnormal rhythm and pitch when speaking, changes in voice quality, difficulty articulating, labored speech, and other related symptoms.
It is caused by muscle damage, or nerve damage to the muscles involved in the process of speaking such as the diaphragm, lips, tongue, and vocal chords.
Because it is a symptom of nerve and/or muscle damage it can be caused by a wide range of phenomena that affect people of all ages. This can start during development in the womb or shortly after birth as a result of conditions like muscular dystrophy and cerebral palsy. In adults some of the most common causes of dysarthria are stroke, tumors, and MS.
A lay term, lisping can be recognized by anyone and is very common.
Speech language pathologists provide an extra level of expertise when treating patients with lisping disorders . They can make sure that a lisp is not being confused with another type of disorder such as apraxia, aphasia, impaired development of expressive language, or a speech impediment caused by hearing loss.
SLPs are also important in distinguishing between the five different types of lisps. Most laypersons can usually pick out the most common type, the interdental/dentalised lisp. This is when a speaker makes a “th” sound when trying to make the “s” sound. It is caused by the tongue reaching past or touching the front teeth.
Because lisps are functional speech disorders, SLPs can play a huge role in correcting these with results often being a complete elimination of the lisp. Treatment is particularly effective when implemented early, although adults can also benefit.
Experts recommend professional SLP intervention if a child has reached the age of four and still has an interdental/dentalised lisp. SLP intervention is recommended as soon as possible for all other types of lisps. Treatment includes pronunciation and annunciation coaching, re-teaching how a sound or word is supposed to be pronounced, practice in front of a mirror, and speech-muscle strengthening that can be as simple as drinking out of a straw.
Spasmodic Dysphonia
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably. Many SLPs specialize in the treatment of Spasmodic Dysphonia .
SLPs will most often encounter this disorder in adults, with the first symptoms usually occurring between the ages of 30 and 50. It can be caused by a range of things mostly related to aging, such as nervous system changes and muscle tone disorders.
It’s difficult to isolate vocal chord spasms as being responsible for a shaky or trembly voice, so diagnosing SD is a team effort for SLPs that also involves an ear, nose, and throat doctor (otolaryngologist) and a neurologist.
Have you ever heard people talking about how they are smart but also nervous in large groups of people, and then self-diagnose themselves as having Asperger’s? You might have heard a similar lay diagnosis for cluttering. This is an indication of how common this disorder is as well as how crucial SLPs are in making a proper cluttering diagnosis .
A fluency disorder, cluttering is characterized by a person’s speech being too rapid, too jerky, or both. To qualify as cluttering, the person’s speech must also have excessive amounts of “well,” “um,” “like,” “hmm,” or “so,” (speech disfluencies), an excessive exclusion or collapsing of syllables, or abnormal syllable stresses or rhythms.
The first symptoms of this disorder appear in childhood. Like other fluency disorders, SLPs can have a huge impact on improving or eliminating cluttering. Intervention is most effective early on in life, however adults can also benefit from working with an SLP.
Muteness – Selective Mutism
There are different kinds of mutism, and here we are talking about selective mutism. This used to be called elective mutism to emphasize its difference from disorders that caused mutism through damage to, or irregularities in, the speech process.
Selective mutism is when a person does not speak in some or most situations, however that person is physically capable of speaking. It most often occurs in children, and is commonly exemplified by a child speaking at home but not at school.
Selective mutism is related to psychology. It appears in children who are very shy, who have an anxiety disorder, or who are going through a period of social withdrawal or isolation. These psychological factors have their own origins and should be dealt with through counseling or another type of psychological intervention.
Diagnosing selective mutism involves a team of professionals including SLPs, pediatricians, psychologists, and psychiatrists. SLPs play an important role in this process because there are speech language disorders that can have the same effect as selective muteness – stuttering, aphasia, apraxia of speech, or dysarthria – and it’s important to eliminate these as possibilities.
And just because selective mutism is primarily a psychological phenomenon, that doesn’t mean SLPs can’t do anything. Quite the contrary.
The National Institute on Neurological Disorders and Stroke estimates that one million Americans have some form of aphasia.
Aphasia is a communication disorder caused by damage to the brain’s language capabilities. Aphasia differs from apraxia of speech and dysarthria in that it solely pertains to the brain’s speech and language center.
As such anyone can suffer from aphasia because brain damage can be caused by a number of factors. However SLPs are most likely to encounter aphasia in adults, especially those who have had a stroke. Other common causes of aphasia are brain tumors, traumatic brain injuries, and degenerative brain diseases.
In addition to neurologists, speech language pathologists have an important role in diagnosing aphasia. As an SLP you’ll assess factors such as a person’s reading and writing, functional communication, auditory comprehension, and verbal expression.
Speech Delay – Alalia
A speech delay, known to professionals as alalia, refers to the phenomenon when a child is not making normal attempts to verbally communicate. There can be a number of factors causing this to happen, and that’s why it’s critical for a speech language pathologist to be involved.
The are many potential reasons why a child would not be using age-appropriate communication. These can range anywhere from the child being a “late bloomer” – the child just takes a bit longer than average to speak – to the child having brain damage. It is the role of an SLP to go through a process of elimination, evaluating each possibility that could cause a speech delay, until an explanation is found.
Approaching a child with a speech delay starts by distinguishing among the two main categories an SLP will evaluate: speech and language.
Speech has a lot to do with the organs of speech – the tongue, mouth, and vocal chords – as well as the muscles and nerves that connect them with the brain. Disorders like apraxia of speech and dysarthria are two examples that affect the nerve connections and organs of speech. Other examples in this category could include a cleft palette or even hearing loss.
The other major category SLPs will evaluate is language. This relates more to the brain and can be affected by brain damage or developmental disorders like autism. There are many different types of brain damage that each manifest themselves differently, as well as developmental disorders, and the SLP will make evaluations for everything.
Issues Related to Autism
While the autism spectrum itself isn’t a speech disorder, it makes this list because the two go hand-in-hand more often than not.
The Centers for Disease Control and Prevention (CDC) reports that one out of every 68 children in our country have an autism spectrum disorder. And by definition, all children who have autism also have social communication problems.
Speech-language pathologists are often a critical voice on a team of professionals – also including pediatricians, occupational therapists, neurologists, developmental specialists, and physical therapists – who make an autism spectrum diagnosis .
In fact, the American Speech-Language Hearing Association reports that problems with communication are the first detectable signs of autism. That is why language disorders – specifically disordered verbal and nonverbal communication – are one of the primary diagnostic criteria for autism.
So what kinds of SLP disorders are you likely to encounter with someone on the autism spectrum?
A big one is apraxia of speech. A study that came out of Penn State in 2015 found that 64 percent of children who were diagnosed with autism also had childhood apraxia of speech.
This basic primer on the most common speech disorders offers little more than an interesting glimpse into the kind of issues that SLPs work with patients to resolve. But even knowing everything there is to know about communication science and speech disorders doesn’t tell the whole story of what this profession is all about. With every client in every therapy session, the goal is always to have the folks that come to you for help leave with a little more confidence than when they walked in the door that day. As a trusted SLP, you will build on those gains with every session, helping clients experience the joy and freedom that comes with the ability to express themselves freely. At the end of the day, this is what being an SLP is all about.
Ready to make a difference in speech pathology? Learn how to become a Speech-Language Pathologist today
- Emerson College - Master's in Speech-Language Pathology online - Prepare to become an SLP in as few as 20 months. No GRE required. Scholarships available.
- Arizona State University - Online - Online Bachelor of Science in Speech and Hearing Science - Designed to prepare graduates to work in behavioral health settings or transition to graduate programs in speech-language pathology and audiology.
- NYU Steinhardt - NYU Steinhardt's Master of Science in Communicative Sciences and Disorders online - ASHA-accredited. Bachelor's degree required. Graduate prepared to pursue licensure.
- Calvin University - Calvin University's Online Speech and Hearing Foundations Certificate - Helps You Gain a Strong Foundation for Your Speech-Language Pathology Career.
American Speech-Language-Hearing Association
- Certification
- Publications
- Continuing Education
- Practice Management
- Audiologists
- Speech-Language Pathologists
- Academic & Faculty
- Audiology & SLP Assistants
Speech Sound Disorders-Articulation and Phonology
View All Portal Topics
See the Speech Sound Disorders Evidence Map for summaries of the available research on this topic.
The scope of this page is speech sound disorders with no known cause—historically called articulation and phonological disorders —in preschool and school-age children (ages 3–21).
Information about speech sound problems related to motor/neurological disorders, structural abnormalities, and sensory/perceptual disorders (e.g., hearing loss) is not addressed in this page.
See ASHA's Practice Portal pages on Childhood Apraxia of Speech and Cleft Lip and Palate for information about speech sound problems associated with these two disorders. A Practice Portal page on dysarthria in children will be developed in the future.
Speech Sound Disorders
Speech sound disorders is an umbrella term referring to any difficulty or combination of difficulties with perception, motor production, or phonological representation of speech sounds and speech segments—including phonotactic rules governing permissible speech sound sequences in a language.
Speech sound disorders can be organic or functional in nature. Organic speech sound disorders result from an underlying motor/neurological, structural, or sensory/perceptual cause. Functional speech sound disorders are idiopathic—they have no known cause. See figure below.
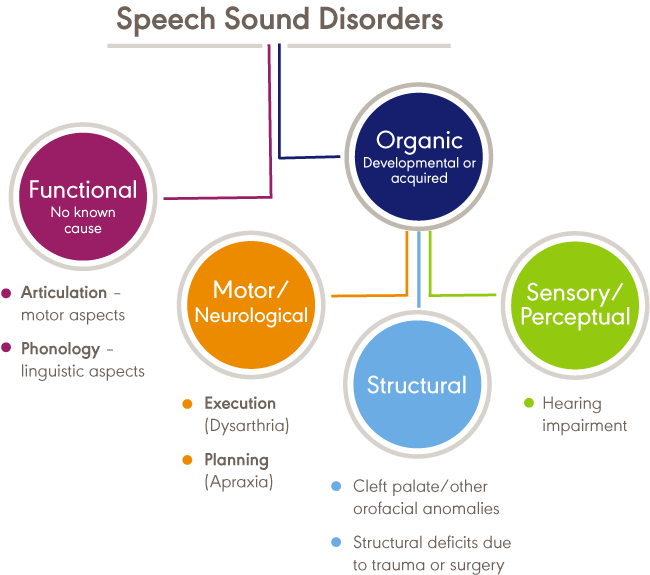
Organic Speech Sound Disorders
Organic speech sound disorders include those resulting from motor/neurological disorders (e.g., childhood apraxia of speech and dysarthria), structural abnormalities (e.g., cleft lip/palate and other structural deficits or anomalies), and sensory/perceptual disorders (e.g., hearing loss).
Functional Speech Sound Disorders
Functional speech sound disorders include those related to the motor production of speech sounds and those related to the linguistic aspects of speech production. Historically, these disorders are referred to as articulation disorders and phonological disorders , respectively. Articulation disorders focus on errors (e.g., distortions and substitutions) in production of individual speech sounds. Phonological disorders focus on predictable, rule-based errors (e.g., fronting, stopping, and final consonant deletion) that affect more than one sound. It is often difficult to cleanly differentiate between articulation and phonological disorders; therefore, many researchers and clinicians prefer to use the broader term, "speech sound disorder," when referring to speech errors of unknown cause. See Bernthal, Bankson, and Flipsen (2017) and Peña-Brooks and Hegde (2015) for relevant discussions.
This Practice Portal page focuses on functional speech sound disorders. The broad term, "speech sound disorder(s)," is used throughout; articulation error types and phonological error patterns within this diagnostic category are described as needed for clarity.
Procedures and approaches detailed in this page may also be appropriate for assessing and treating organic speech sound disorders. See Speech Characteristics: Selected Populations [PDF] for a brief summary of selected populations and characteristic speech problems.
Incidence and Prevalence
The incidence of speech sound disorders refers to the number of new cases identified in a specified period. The prevalence of speech sound disorders refers to the number of children who are living with speech problems in a given time period.
Estimated prevalence rates of speech sound disorders vary greatly due to the inconsistent classifications of the disorders and the variance of ages studied. The following data reflect the variability:
- Overall, 2.3% to 24.6% of school-aged children were estimated to have speech delay or speech sound disorders (Black, Vahratian, & Hoffman, 2015; Law, Boyle, Harris, Harkness, & Nye, 2000; Shriberg, Tomblin, & McSweeny, 1999; Wren, Miller, Peters, Emond, & Roulstone, 2016).
- A 2012 survey from the National Center for Health Statistics estimated that, among children with a communication disorder, 48.1% of 3- to 10-year old children and 24.4% of 11- to 17-year old children had speech sound problems only. Parents reported that 67.6% of children with speech problems received speech intervention services (Black et al., 2015).
- Residual or persistent speech errors were estimated to occur in 1% to 2% of older children and adults (Flipsen, 2015).
- Reports estimated that speech sound disorders are more prevalent in boys than in girls, with a ratio ranging from 1.5:1.0 to 1.8:1.0 (Shriberg et al., 1999; Wren et al., 2016).
- Prevalence rates were estimated to be 5.3% in African American children and 3.8% in White children (Shriberg et al., 1999).
- Reports estimated that 11% to 40% of children with speech sound disorders had concomitant language impairment (Eadie et al., 2015; Shriberg et al., 1999).
- Poor speech sound production skills in kindergarten children have been associated with lower literacy outcomes (Overby, Trainin, Smit, Bernthal, & Nelson, 2012). Estimates reported a greater likelihood of reading disorders (relative risk: 2.5) in children with a preschool history of speech sound disorders (Peterson, Pennington, Shriberg, & Boada, 2009).
Signs and Symptoms
Signs and symptoms of functional speech sound disorders include the following:
- omissions/deletions —certain sounds are omitted or deleted (e.g., "cu" for "cup" and "poon" for "spoon")
- substitutions —one or more sounds are substituted, which may result in loss of phonemic contrast (e.g., "thing" for "sing" and "wabbit" for "rabbit")
- additions —one or more extra sounds are added or inserted into a word (e.g., "buhlack" for "black")
- distortions —sounds are altered or changed (e.g., a lateral "s")
- syllable-level errors —weak syllables are deleted (e.g., "tephone" for "telephone")
Signs and symptoms may occur as independent articulation errors or as phonological rule-based error patterns (see ASHA's resource on selected phonological processes [patterns] for examples). In addition to these common rule-based error patterns, idiosyncratic error patterns can also occur. For example, a child might substitute many sounds with a favorite or default sound, resulting in a considerable number of homonyms (e.g., shore, sore, chore, and tore might all be pronounced as door ; Grunwell, 1987; Williams, 2003a).
Influence of Accent
An accent is the unique way that speech is pronounced by a group of people speaking the same language and is a natural part of spoken language. Accents may be regional; for example, someone from New York may sound different than someone from South Carolina. Foreign accents occur when a set of phonetic traits of one language are carried over when a person learns a new language. The first language acquired by a bilingual or multilingual individual can influence the pronunciation of speech sounds and the acquisition of phonotactic rules in subsequently acquired languages. No accent is "better" than another. Accents, like dialects, are not speech or language disorders but, rather, only reflect differences. See ASHA's Practice Portal pages on Multilingual Service Delivery in Audiology and Speech-Language Pathology and Cultural Responsiveness .
Influence of Dialect
Not all sound substitutions and omissions are speech errors. Instead, they may be related to a feature of a speaker's dialect (a rule-governed language system that reflects the regional and social background of its speakers). Dialectal variations of a language may cross all linguistic parameters, including phonology, morphology, syntax, semantics, and pragmatics. An example of a dialectal variation in phonology occurs with speakers of African American English (AAE) when a "d" sound is used for a "th" sound (e.g., "dis" for "this"). This variation is not evidence of a speech sound disorder but, rather, one of the phonological features of AAE.
Speech-language pathologists (SLPs) must distinguish between dialectal differences and communicative disorders and must
- recognize all dialects as being rule-governed linguistic systems;
- understand the rules and linguistic features of dialects represented by their clientele; and
- be familiar with nondiscriminatory testing and dynamic assessment procedures, such as identifying potential sources of test bias, administering and scoring standardized tests using alternative methods, and analyzing test results in light of existing information regarding dialect use (see, e.g., McLeod, Verdon, & The International Expert Panel on Multilingual Children's Speech, 2017).
See ASHA's Practice Portal pages on Multilingual Service Delivery in Audiology and Speech-Language Pathology and Cultural Responsiveness .
The cause of functional speech sound disorders is not known; however, some risk factors have been investigated.
Frequently reported risk factors include the following:
- Gender —the incidence of speech sound disorders is higher in males than in females (e.g., Everhart, 1960; Morley, 1952; Shriberg et al., 1999).
- Pre- and perinatal problems —factors such as maternal stress or infections during pregnancy, complications during delivery, preterm delivery, and low birthweight were found to be associated with delay in speech sound acquisition and with speech sound disorders (e.g., Byers Brown, Bendersky, & Chapman, 1986; Fox, Dodd, & Howard, 2002).
- Family history —children who have family members (parents or siblings) with speech and/or language difficulties were more likely to have a speech disorder (e.g., Campbell et al., 2003; Felsenfeld, McGue, & Broen, 1995; Fox et al., 2002; Shriberg & Kwiatkowski, 1994).
- Persistent otitis media with effusion —persistent otitis media with effusion (often associated with hearing loss) has been associated with impaired speech development (Fox et al., 2002; Silva, Chalmers, & Stewart, 1986; Teele, Klein, Chase, Menyuk, & Rosner, 1990).
Roles and Responsibilities
Speech-language pathologists (SLPs) play a central role in the screening, assessment, diagnosis, and treatment of persons with speech sound disorders. The professional roles and activities in speech-language pathology include clinical/educational services (diagnosis, assessment, planning, and treatment); prevention and advocacy; and education, administration, and research. See ASHA's Scope of Practice in Speech-Language Pathology (ASHA, 2016).
Appropriate roles for SLPs include the following:
- Providing prevention information to individuals and groups known to be at risk for speech sound disorders, as well as to individuals working with those at risk
- Educating other professionals on the needs of persons with speech sound disorders and the role of SLPs in diagnosing and managing speech sound disorders
- Screening individuals who present with speech sound difficulties and determining the need for further assessment and/or referral for other services
- Recognizing that students with speech sound disorders have heightened risks for later language and literacy problems
- Conducting a culturally and linguistically relevant comprehensive assessment of speech, language, and communication
- Taking into consideration the rules of a spoken accent or dialect, typical dual-language acquisition from birth, and sequential second-language acquisition to distinguish difference from disorder
- Diagnosing the presence or absence of a speech sound disorder
- Referring to and collaborating with other professionals to rule out other conditions, determine etiology, and facilitate access to comprehensive services
- Making decisions about the management of speech sound disorders
- Making decisions about eligibility for services, based on the presence of a speech sound disorder
- Developing treatment plans, providing intervention and support services, documenting progress, and determining appropriate service delivery approaches and dismissal criteria
- Counseling persons with speech sound disorders and their families/caregivers regarding communication-related issues and providing education aimed at preventing further complications related to speech sound disorders
- Serving as an integral member of an interdisciplinary team working with individuals with speech sound disorders and their families/caregivers (see ASHA's resource on interprofessional education/interprofessional practice [IPE/IPP] )
- Consulting and collaborating with professionals, family members, caregivers, and others to facilitate program development and to provide supervision, evaluation, and/or expert testimony (see ASHA's resource on person- and family-centered care )
- Remaining informed of research in the area of speech sound disorders, helping advance the knowledge base related to the nature and treatment of these disorders, and using evidence-based research to guide intervention
- Advocating for individuals with speech sound disorders and their families at the local, state, and national levels
As indicated in the Code of Ethics (ASHA, 2023), SLPs who serve this population should be specifically educated and appropriately trained to do so.
See the Assessment section of the Speech Sound Disorders Evidence Map for pertinent scientific evidence, expert opinion, and client/caregiver perspective.
Screening is conducted whenever a speech sound disorder is suspected or as part of a comprehensive speech and language evaluation for a child with communication concerns. The purpose of the screening is to identify individuals who require further speech-language assessment and/or referral for other professional services.
Screening typically includes
- screening of individual speech sounds in single words and in connected speech (using formal and or informal screening measures);
- screening of oral motor functioning (e.g., strength and range of motion of oral musculature);
- orofacial examination to assess facial symmetry and identify possible structural bases for speech sound disorders (e.g., submucous cleft palate, malocclusion, ankyloglossia); and
- informal assessment of language comprehension and production.
See ASHA's resource on assessment tools, techniques, and data sources .
Screening may result in
- recommendation to monitor speech and rescreen;
- referral for multi-tiered systems of support such as response to intervention (RTI) ;
- referral for a comprehensive speech sound assessment;
- recommendation for a comprehensive language assessment, if language delay or disorder is suspected;
- referral to an audiologist for a hearing evaluation, if hearing loss is suspected; and
- referral for medical or other professional services, as appropriate.
Comprehensive Assessment
The acquisition of speech sounds is a developmental process, and children often demonstrate "typical" errors and phonological patterns during this acquisition period. Developmentally appropriate errors and patterns are taken into consideration during assessment for speech sound disorders in order to differentiate typical errors from those that are unusual or not age appropriate.
The comprehensive assessment protocol for speech sound disorders may include an evaluation of spoken and written language skills, if indicated. See ASHA's Practice Portal pages on Spoken Language Disorders and Written Language Disorders .
Assessment is accomplished using a variety of measures and activities, including both standardized and nonstandardized measures, as well as formal and informal assessment tools. See ASHA's resource on assessment tools, techniques, and data sources .
SLPs select assessments that are culturally and linguistically sensitive, taking into consideration current research and best practice in assessing speech sound disorders in the languages and/or dialect used by the individual (see, e.g., McLeod et al., 2017). Standard scores cannot be reported for assessments that are not normed on a group that is representative of the individual being assessed.
SLPs take into account cultural and linguistic speech differences across communities, including
- phonemic and allophonic variations of the language(s) and/or dialect(s) used in the community and how those variations affect determination of a disorder or a difference and
- differences among speech sound disorders, accents, dialects, and patterns of transfer from one language to another. See phonemic inventories and cultural and linguistic information across languages .
Consistent with the World Health Organization's (WHO) International Classification of Functioning, Disability and Health (ICF) framework (ASHA, 2016a; WHO, 2001), a comprehensive assessment is conducted to identify and describe
- impairments in body structure and function, including underlying strengths and weaknesses in speech sound production and verbal/nonverbal communication;
- co-morbid deficits or conditions, such as developmental disabilities, medical conditions, or syndromes;
- limitations in activity and participation, including functional communication, interpersonal interactions with family and peers, and learning;
- contextual (environmental and personal) factors that serve as barriers to or facilitators of successful communication and life participation; and
- the impact of communication impairments on quality of life of the child and family.
See ASHA's Person-Centered Focus on Function: Speech Sound Disorder [PDF] for an example of assessment data consistent with ICF.
Assessment may result in
- diagnosis of a speech sound disorder;
- description of the characteristics and severity of the disorder;
- recommendations for intervention targets;
- identification of factors that might contribute to the speech sound disorder;
- diagnosis of a spoken language (listening and speaking) disorder;
- identification of written language (reading and writing) problems;
- recommendation to monitor reading and writing progress in students with identified speech sound disorders by SLPs and other professionals in the school setting;
- referral for multi-tiered systems of support such as response to intervention (RTI) to support speech and language development; and
- referral to other professionals as needed.
Case History
The case history typically includes gathering information about
- the family's concerns about the child's speech;
- history of middle ear infections;
- family history of speech and language difficulties (including reading and writing);
- languages used in the home;
- primary language spoken by the child;
- the family's and other communication partners' perceptions of intelligibility; and
- the teacher's perception of the child's intelligibility and participation in the school setting and how the child's speech compares with that of peers in the classroom.
See ASHA's Practice Portal page on Cultural Responsiveness for guidance on taking a case history with all clients.
Oral Mechanism Examination
The oral mechanism examination evaluates the structure and function of the speech mechanism to assess whether the system is adequate for speech production. This examination typically includes assessment of
- dental occlusion and specific tooth deviations;
- structure of hard and soft palate (clefts, fistulas, bifid uvula); and
- function (strength and range of motion) of the lips, jaw, tongue, and velum.
Hearing Screening
A hearing screening is conducted during the comprehensive speech sound assessment, if one was not completed during the screening.
Hearing screening typically includes
- otoscopic inspection of the ear canal and tympanic membrane;
- pure-tone audiometry; and
- immittance testing to assess middle ear function.
Speech Sound Assessment
The speech sound assessment uses both standardized assessment instruments and other sampling procedures to evaluate production in single words and connected speech.
Single-word testing provides identifiable units of production and allows most consonants in the language to be elicited in a number of phonetic contexts; however, it may or may not accurately reflect production of the same sounds in connected speech.
Connected speech sampling provides information about production of sounds in connected speech using a variety of talking tasks (e.g., storytelling or retelling, describing pictures, normal conversation about a topic of interest) and with a variety of communication partners (e.g., peers, siblings, parents, and clinician).
Assessment of speech includes evaluation of the following:
- Accurate productions
- sounds in various word positions (e.g., initial, within word, and final word position) and in different phonetic contexts;
- sound combinations such as vowel combinations, consonant clusters, and blends; and
- syllable shapes —simple CV to complex CCVCC.
- Speech sound errors
- consistent sound errors;
- error types (e.g., deletions, omissions, substitutions, distortions, additions); and
- error distribution (e.g., position of sound in word).
- Error patterns (i.e., phonological patterns)—systematic sound changes or simplifications that affect a class of sounds (e.g., fricatives), sound combinations (e.g., consonant clusters), or syllable structures (e.g., complex syllables or multisyllabic words).
See Age of Acquisition of English Consonants (Crowe & McLeaod, 2020) [PDF] and ASHA's resource on selected phonological processes (patterns) .
Severity Assessment
Severity is a qualitative judgment made by the clinician indicating the impact of the child's speech sound disorder on functional communication. It is typically defined along a continuum from mild to severe or profound. There is no clear consensus regarding the best way to determine severity of a speech sound disorder—rating scales and quantitative measures have been used.
A numerical scale or continuum of disability is often used because it is time-efficient. Prezas and Hodson (2010) use a continuum of severity from mild (omissions are rare; few substitutions) to profound (extensive omissions and many substitutions; extremely limited phonemic and phonotactic repertoires). Distortions and assimilations occur in varying degrees at all levels of the continuum.
A quantitative approach (Shriberg & Kwiatkowski, 1982a, 1982b) uses the percentage of consonants correct (PCC) to determine severity on a continuum from mild to severe.
To determine PCC, collect and phonetically transcribe a speech sample. Then count the total number of consonants in the sample and the total number of correct consonants. Use the following formula:
PCC = (correct consonants/total consonants) × 100
A PCC of 85–100 is considered mild, whereas a PCC of less than 50 is considered severe. This approach has been modified to include a total of 10 such indices, including percent vowels correct (PVC; Shriberg, Austin, Lewis, McSweeny, & Wilson, 1997).
Intelligibility Assessment
Intelligibility is a perceptual judgment that is based on how much of the child's spontaneous speech the listener understands. Intelligibility can vary along a continuum ranging from intelligible (message is completely understood) to unintelligible (message is not understood; Bernthal et al., 2017). Intelligibility is frequently used when judging the severity of the child's speech problem (Kent, Miolo, & Bloedel, 1994; Shriberg & Kwiatkowski, 1982b) and can be used to determine the need for intervention.
Intelligibility can vary depending on a number of factors, including
- the number, type, and frequency of speech sound errors (when present);
- the speaker's rate, inflection, stress patterns, pauses, voice quality, loudness, and fluency;
- linguistic factors (e.g., word choice and grammar);
- complexity of utterance (e.g., single words vs. conversational or connected speech);
- the listener's familiarity with the speaker's speech pattern;
- communication environment (e.g., familiar vs. unfamiliar communication partners, one-on-one vs. group conversation);
- communication cues for listener (e.g., nonverbal cues from the speaker, including gestures and facial expressions); and
- signal-to-noise ratio (i.e., amount of background noise).
Rating scales and other estimates that are based on perceptual judgments are commonly used to assess intelligibility. For example, rating scales sometimes use numerical ratings like 1 for totally intelligible and 10 for unintelligible, or they use descriptors like not at all, seldom, sometimes, most of the time, or always to indicated how well speech is understood (Ertmer, 2010).
A number of quantitative measures also have been proposed, including calculating the percentage of words understood in conversational speech (e.g., Flipsen, 2006; Shriberg & Kwiatkowski, 1980). See also Kent et al. (1994) for a comprehensive review of procedures for assessing intelligibility.
Coplan and Gleason (1988) developed a standardized intelligibility screener using parent estimates of how intelligible their child sounded to others. On the basis of the data, expected intelligibility cutoff values for typically developing children were as follows:
22 months—50%
37 months—75%
47 months—100%
See the Resources section for resources related to assessing intelligibility and life participation in monolingual children who speak English and in monolingual children who speak languages other than English.
Stimulability Testing
Stimulability is the child's ability to accurately imitate a misarticulated sound when the clinician provides a model. There are few standardized procedures for testing stimulability (Glaspey & Stoel-Gammon, 2007; Powell & Miccio, 1996), although some test batteries include stimulability subtests.
Stimulability testing helps determine
- how well the child imitates the sound in one or more contexts (e.g., isolation, syllable, word, phrase);
- the level of cueing necessary to achieve the best production (e.g., auditory model; auditory and visual model; auditory, visual, and verbal model; tactile cues);
- whether the sound is likely to be acquired without intervention; and
- which targets are appropriate for therapy (Tyler & Tolbert, 2002).
Speech Perception Testing
Speech perception is the ability to perceive differences between speech sounds. In children with speech sound disorders, speech perception is the child's ability to perceive the difference between the standard production of a sound and his or her own error production—or to perceive the contrast between two phonetically similar sounds (e.g., r/w, s/ʃ, f/θ).
Speech perception abilities can be tested using the following paradigms:
- Auditory Discrimination —syllable pairs containing a single phoneme contrast are presented, and the child is instructed to say "same" if the paired items sound the same and "different" if they sound different.
- Picture Identification —the child is shown two to four pictures representing words with minimal phonetic differences. The clinician says one of these words, and the child is asked to point to the correct picture.
- Speech production–perception task —using sounds that the child is suspected of having difficulty perceiving, picture targets containing these sounds are used as visual cues. The child is asked to judge whether the speaker says the item correctly (e.g., picture of a ship is shown; speaker says, "ship" or "sip"; Locke, 1980).
- Mispronunciation detection task —using computer-presented picture stimuli and recorded stimulus names (either correct or with a single phoneme error), the child is asked to detect mispronunciations by pointing to a green tick for "correct" or a red cross for "incorrect" (McNeill & Hesketh, 2010).
- Lexical decision/judgment task —using target pictures and single-word recordings, this task assesses the child's ability to identify words that are pronounced correctly or incorrectly. A picture of the target word (e.g., "lake") is shown, along with a recorded word—either "lake" or a word with a contrasting phoneme (e.g., "wake"). The child points to the picture of the target word if it was pronounced correctly or to an "X" if it was pronounced incorrectly (Rvachew, Nowak, & Cloutier, 2004).
Considerations For Assessing Young Children and/or Children Who Are Reluctant or Have Less Intelligible Speech
Young children might not be able to follow directions for standardized tests, might have limited expressive vocabulary, and might produce words that are unintelligible. Other children, regardless of age, may produce less intelligible speech or be reluctant to speak in an assessment setting.
Strategies for collecting an adequate speech sample with these populations include
- obtaining a speech sample during the assessment session using play activities;
- using pictures or toys to elicit a range of consonant sounds;
- involving parents/caregivers in the session to encourage talking;
- asking parents/caregivers to supplement data from the assessment session by recording the child's speech at home during spontaneous conversation; and
- asking parents/caregivers to keep a log of the child's intended words and how these words are pronounced.
Sometimes, the speech sound disorder is so severe that the child's intended message cannot be understood. However, even when a child's speech is unintelligible, it is usually possible to obtain information about his or her speech sound production.
For example:
- A single-word articulation test provides opportunities for production of identifiable units of sound, and these productions can usually be transcribed.
- It may be possible to understand and transcribe a spontaneous speech sample by (a) using a structured situation to provide context when obtaining the sample and (b) annotating the recorded sample by repeating the child's utterances, when possible, to facilitate later transcription.
Considerations For Assessing Bilingual/Multilingual Populations
Assessment of a bilingual individual requires an understanding of both linguistic systems because the sound system of one language can influence the sound system of another language. The assessment process must identify whether differences are truly related to a speech sound disorder or are normal variations of speech caused by the first language.
When assessing a bilingual or multilingual individual, clinicians typically
- gather information, including
- language history and language use to determine which language(s) should be assessed,
- phonemic inventory, phonological structure, and syllable structure of the non-English language, and
- dialect of the individual;
- assess phonological skills in both languages in single words as well as in connected speech;
- account for dialectal differences, when present; and
- identify and assess the child's
- common substitution patterns (those seen in typically developing children),
- uncommon substitution patterns (those often seen in individuals with a speech sound disorder), and
- cross-linguistic effects (the phonological system of one's native language influencing the production of sounds in English, resulting in an accent—that is, phonetic traits from a person's original language (L1) that are carried over to a second language (L2; Fabiano-Smith & Goldstein, 2010).
See phonemic inventories and cultural and linguistic information across languages and ASHA's Practice Portal page on Multilingual Service Delivery in Audiology and Speech-Language Pathology . See the Resources section for information related to assessing intelligibility and life participation in monolingual children who speak English and in monolingual children who speak languages other than English.
Phonological Processing Assessment
Phonological processing is the use of the sounds of one's language (i.e., phonemes) to process spoken and written language (Wagner & Torgesen, 1987). The broad category of phonological processing includes phonological awareness , phonological working memory , and phonological retrieval .
All three components of phonological processing (see definitions below) are important for speech production and for the development of spoken and written language skills. Therefore, it is important to assess phonological processing skills and to monitor the spoken and written language development of children with phonological processing difficulties.
- Phonological Awareness is the awareness of the sound structure of a language and the ability to consciously analyze and manipulate this structure via a range of tasks, such as speech sound segmentation and blending at the word, onset-rime, syllable, and phonemic levels.
- Phonological Working Memory involves storing phoneme information in a temporary, short-term memory store (Wagner & Torgesen, 1987). This phonemic information is then readily available for manipulation during phonological awareness tasks. Nonword repetition (e.g., repeat "/pæɡ/") is one example of a phonological working memory task.
- Phonological Retrieval is the ability to retrieve phonological information from long-term memory. It is typically assessed using rapid naming tasks (e.g., rapid naming of objects, colors, letters, or numbers). This ability to retrieve the phonological information of one's language is integral to phonological awareness.
Language Assessments
Language testing is included in a comprehensive speech sound assessment because of the high incidence of co-occurring language problems in children with speech sound disorders (Shriberg & Austin, 1998).
Spoken Language Assessment (Listening and Speaking)
Typically, the assessment of spoken language begins with a screening of expressive and receptive skills; a full battery is performed if indicated by screening results. See ASHA's Practice Portal page on Spoken Language Disorders for more details.
Written Language Assessment (Reading and Writing)
Difficulties with the speech processing system (e.g., listening, discriminating speech sounds, remembering speech sounds, producing speech sounds) can lead to speech production and phonological awareness difficulties. These difficulties can have a negative impact on the development of reading and writing skills (Anthony et al., 2011; Catts, McIlraith, Bridges, & Nielsen, 2017; Leitão & Fletcher, 2004; Lewis et al., 2011).
For typically developing children, speech production and phonological awareness develop in a mutually supportive way (Carroll, Snowling, Stevenson, & Hulme, 2003; National Institute for Literacy, 2009). As children playfully engage in sound play, they eventually learn to segment words into separate sounds and to "map" sounds onto printed letters.
The understanding that sounds are represented by symbolic code (e.g., letters and letter combinations) is essential for reading and spelling. When reading, children have to be able to segment a written word into individual sounds, based on their knowledge of the code and then blend those sounds together to form a word. When spelling, children have to be able to segment a spoken word into individual sounds and then choose the correct code to represent these sounds (National Institute of Child Health and Human Development, 2000; Pascoe, Stackhouse, & Wells, 2006).
Components of the written language assessment include the following, depending on the child's age and expected stage of written language development:
- Print Awareness —recognizing that books have a front and back, recognizing that the direction of words is from left to right, and recognizing where words on the page start and stop.
- Alphabet Knowledge —including naming/printing alphabet letters from A to Z.
- Sound–Symbol Correspondence —knowing that letters have sounds and knowing the sounds for corresponding letters and letter combinations.
- Reading Decoding —using sound–symbol knowledge to segment and blend sounds in grade-level words.
- Spelling —using sound–symbol knowledge to spell grade-level words.
- Reading Fluency —reading smoothly without frequent or significant pausing.
- Reading Comprehension —understanding grade-level text, including the ability to make inferences.
See ASHA's Practice Portal page on Written Language Disorders for more details.
See the Treatment section of the Speech Sound Disorders Evidence Map for pertinent scientific evidence, expert opinion, and client/caregiver perspective.
The broad term "speech sound disorder(s)" is used in this Portal page to refer to functional speech sound disorders, including those related to the motor production of speech sounds (articulation) and those related to the linguistic aspects of speech production (phonological).
It is often difficult to cleanly differentiate between articulation and phonological errors or to differentially diagnose these two separate disorders. Nevertheless, we often talk about articulation error types and phonological error types within the broad diagnostic category of speech sound disorder(s). A single child might show both error types, and those specific errors might need different treatment approaches.
Historically, treatments that focus on motor production of speech sounds are called articulation approaches; treatments that focus on the linguistic aspects of speech production are called phonological/language-based approaches.
Articulation approaches target each sound deviation and are often selected by the clinician when the child's errors are assumed to be motor based; the aim is correct production of the target sound(s).
Phonological/language-based approaches target a group of sounds with similar error patterns, although the actual treatment of exemplars of the error pattern may target individual sounds. Phonological approaches are often selected in an effort to help the child internalize phonological rules and generalize these rules to other sounds within the pattern (e.g., final consonant deletion, cluster reduction).
Articulation and phonological/language-based approaches might both be used in therapy with the same individual at different times or for different reasons.
Both approaches for the treatment of speech sound disorders typically involve the following sequence of steps:
- Establishment —eliciting target sounds and stabilizing production on a voluntary level.
- Generalization —facilitating carry-over of sound productions at increasingly challenging levels (e.g., syllables, words, phrases/sentences, conversational speaking).
- Maintenance —stabilizing target sound production and making it more automatic; encouraging self-monitoring of speech and self-correction of errors.

Target Selection
Approaches for selecting initial therapy targets for children with articulation and/or phonological disorders include the following:
- Developmental —target sounds are selected on the basis of order of acquisition in typically developing children.
- Complexity —focuses on more complex, linguistically marked phonological elements not in the child's phonological system to encourage cascading, generalized learning of sounds (Gierut, 2007; Storkel, 2018).
- Dynamic systems —focuses on teaching and stabilizing simple target phonemes that do not introduce new feature contrasts in the child's phonological system to assist in the acquisition of target sounds and more complex targets and features (Rvachew & Bernhardt, 2010).
- Systemic —focuses on the function of the sound in the child's phonological organization to achieve maximum phonological reorganization with the least amount of intervention. Target selection is based on a distance metric. Targets can be maximally distinct from the child's error in terms of place, voice, and manner and can also be maximally different in terms of manner, place of production, and voicing (Williams, 2003b). See Place, Manner and Voicing Chart for English Consonants (Roth & Worthington, 2018) .
- Client-specific —selects targets based on factors such as relevance to the child and his or her family (e.g., sound is in child's name), stimulability, and/or visibility when produced (e.g., /f/ vs. /k/).
- Degree of deviance and impact on intelligibility —selects targets on the basis of errors (e.g., errors of omission; error patterns such as initial consonant deletion) that most effect intelligibility.
See ASHA's Person-Centered Focus on Function: Speech Sound Disorder [PDF] for an example of goal setting consistent with ICF.
Treatment Strategies
In addition to selecting appropriate targets for therapy, SLPs select treatment strategies based on the number of intervention goals to be addressed in each session and the manner in which these goals are implemented. A particular strategy may not be appropriate for all children, and strategies may change throughout the course of intervention as the child's needs change.
"Target attack" strategies include the following:
- Vertical —intense practice on one or two targets until the child reaches a specific criterion level (usually conversational level) before proceeding to the next target or targets (see, e.g., Fey, 1986).
- Horizontal —less intense practice on a few targets; multiple targets are addressed individually or interactively in the same session, thus providing exposure to more aspects of the sounds system (see, e.g., Fey, 1986).
- Cyclical —incorporating elements of both horizontal and vertical structures; the child is provided with practice on a given target or targets for some predetermined period of time before moving on to another target or targets for a predetermined period of time. Practice then cycles through all targets again (see, e.g., Hodson, 2010).
Treatment Options
The following are brief descriptions of both general and specific treatments for children with speech sound disorders. These approaches can be used to treat speech sound problems in a variety of populations. See Speech Characteristics: Selected Populations [PDF] for a brief summary of selected populations and characteristic speech problems.
Treatment selection will depend on a number of factors, including the child's age, the type of speech sound errors, the severity of the disorder, and the degree to which the disorder affects overall intelligibility (Williams, McLeod, & McCauley, 2010). This list is not exhaustive, and inclusion does not imply an endorsement from ASHA.
Contextual Utilization Approaches
Contextual utilization approaches recognize that speech sounds are produced in syllable-based contexts in connected speech and that some (phonemic/phonetic) contexts can facilitate correct production of a particular sound.
Contextual utilization approaches may be helpful for children who use a sound inconsistently and need a method to facilitate consistent production of that sound in other contexts. Instruction for a particular sound is initiated in the syllable context(s) where the sound can be produced correctly (McDonald, 1974). The syllable is used as the building block for practice at more complex levels.
For example, production of a "t" may be facilitated in the context of a high front vowel, as in "tea" (Bernthal et al., 2017). Facilitative contexts or "likely best bets" for production can be identified for voiced, velar, alveolar, and nasal consonants. For example, a "best bet" for nasal consonants is before a low vowel, as in "mad" (Bleile, 2002).
Phonological Contrast Approaches
Phonological contrast approaches are frequently used to address phonological error patterns. They focus on improving phonemic contrasts in the child's speech by emphasizing sound contrasts necessary to differentiate one word from another. Contrast approaches use contrasting word pairs as targets instead of individual sounds.
There are four different contrastive approaches— minimal oppositions, maximal oppositions , treatment of the empty set, and multiple oppositions.
- Minimal Oppositions (also known as "minimal pairs" therapy)—uses pairs of words that differ by only one phoneme or single feature signaling a change in meaning. Minimal pairs are used to help establish contrasts not present in the child's phonological system (e.g., "door" vs. "sore," "pot" vs. "spot," "key" vs. "tea"; Blache, Parsons, & Humphreys, 1981; Weiner, 1981).
- Maximal Oppositions —uses pairs of words containing a contrastive sound that is maximally distinct and varies on multiple dimensions (e.g., voice, place, and manner) to teach an unknown sound. For example, "mall" and "call" are maximal pairs because /m/ and /k/ vary on more than one dimension—/m/ is a bilabial voiced nasal, whereas /k/ is a velar voiceless stop (Gierut, 1989, 1990, 1992). See Place, Manner and Voicing Chart for English Consonants (Roth & Worthington, 2018) .
- Treatment of the Empty Set —similar to the maximal oppositions approach but uses pairs of words containing two maximally opposing sounds (e.g., /r/ and /d/) that are unknown to the child (e.g., "row" vs. "doe" or "ray" vs. "day"; Gierut, 1992).
- Multiple Oppositions —a variation of the minimal oppositions approach but uses pairs of words contrasting a child's error sound with three or four strategically selected sounds that reflect both maximal classification and maximal distinction (e.g., "door," "four," "chore," and "store," to reduce backing of /d/ to /g/; Williams, 2000a, 2000b).
Complexity Approach
The complexity approach is a speech production approach based on data supporting the view that the use of more complex linguistic stimuli helps promote generalization to untreated but related targets.
The complexity approach grew primarily from the maximal oppositions approach. However, it differs from the maximal oppositions approach in a number of ways. Rather than selecting targets on the basis of features such as voice, place, and manner, the complexity of targets is determined in other ways. These include hierarchies of complexity (e.g., clusters, fricatives, and affricates are more complex than other sound classes) and stimulability (i.e., sounds with the lowest levels of stimulability are most complex). In addition, although the maximal oppositions approach trains targets in contrasting word pairs, the complexity approach does not. See Baker and Williams (2010) and Peña-Brooks and Hegde (2015) for detailed descriptions of the complexity approach.
Core Vocabulary Approach
A core vocabulary approach focuses on whole-word production and is used for children with inconsistent speech sound production who may be resistant to more traditional therapy approaches.
Words selected for practice are those used frequently in the child's functional communication. A list of frequently used words is developed (e.g., based on observation, parent report, and/or teacher report), and a number of words from this list are selected each week for treatment. The child is taught his or her "best" word production, and the words are practiced until consistently produced (Dodd, Holm, Crosbie, & McIntosh, 2006).
Cycles Approach
The cycles approach targets phonological pattern errors and is designed for children with highly unintelligible speech who have extensive omissions, some substitutions, and a restricted use of consonants.
Treatment is scheduled in cycles ranging from 5 to 16 weeks. During each cycle, one or more phonological patterns are targeted. After each cycle has been completed, another cycle begins, targeting one or more different phonological patterns. Recycling of phonological patterns continues until the targeted patterns are present in the child's spontaneous speech (Hodson, 2010; Prezas & Hodson, 2010).
The goal is to approximate the gradual typical phonological development process. There is no predetermined level of mastery of phonemes or phoneme patterns within each cycle; cycles are used to stimulate the emergence of a specific sound or pattern—not to produce mastery of it.
Distinctive Feature Therapy
Distinctive feature therapy focuses on elements of phonemes that are lacking in a child's repertoire (e.g., frication, nasality, voicing, and place of articulation) and is typically used for children who primarily substitute one sound for another. See Place, Manner and Voicing Chart for English Consonants (Roth & Worthington, 2018) .
Distinctive feature therapy uses targets (e.g., minimal pairs) that compare the phonetic elements/features of the target sound with those of its substitution or some other sound contrast. Patterns of features can be identified and targeted; producing one target sound often generalizes to other sounds that share the targeted feature (Blache & Parsons, 1980; Blache et al., 1981; Elbert & McReynolds, 1978; McReynolds & Bennett, 1972; Ruder & Bunce, 1981).
Metaphon Therapy
Metaphon therapy is designed to teach metaphonological awareness —that is, the awareness of the phonological structure of language. This approach assumes that children with phonological disorders have failed to acquire the rules of the phonological system.
The focus is on sound properties that need to be contrasted. For example, for problems with voicing, the concept of "noisy" (voiced) versus "quiet" (voiceless) is taught. Targets typically include processes that affect intelligibility, can be imitated, or are not seen in typically developing children of the same age (Dean, Howell, Waters, & Reid, 1995; Howell & Dean, 1994).
Naturalistic Speech Intelligibility Intervention
Naturalist speech intelligibility intervention addresses the targeted sound in naturalistic activities that provide the child with frequent opportunities for the sound to occur. For example, using a McDonald's menu, signs at the grocery store, or favorite books, the child can be asked questions about words that contain the targeted sound(s). The child's error productions are recast without the use of imitative prompts or direct motor training. This approach is used with children who are able to use the recasts effectively (Camarata, 2010).
Nonspeech Oral–Motor Therapy
Nonspeech oral–motor therapy involves the use of oral-motor training prior to teaching sounds or as a supplement to speech sound instruction. The rationale behind this approach is that (a) immature or deficient oral-motor control or strength may be causing poor articulation and (b) it is necessary to teach control of the articulators before working on correct production of sounds. Consult systematic reviews of this treatment to help guide clinical decision making (see, e.g., Lee & Gibbon, 2015 [PDF]; McCauley, Strand, Lof, Schooling, & Frymark, 2009 ). See also the Treatment section of the Speech Sound Disorders Evidence Map filtered for Oral–Motor Exercises .
Speech Sound Perception Training
Speech sound perception training is used to help a child acquire a stable perceptual representation for the target phoneme or phonological structure. The goal is to ensure that the child is attending to the appropriate acoustic cues and weighting them according to a language-specific strategy (i.e., one that ensures reliable perception of the target in a variety of listening contexts).
Recommended procedures include (a) auditory bombardment in which many and varied target exemplars are presented to the child, sometimes in a meaningful context such as a story and often with amplification, and (b) identification tasks in which the child identifies correct and incorrect versions of the target (e.g., "rat" is a correct exemplar of the word corresponding to a rodent, whereas "wat" is not).
Tasks typically progress from the child judging speech produced by others to the child judging the accuracy of his or her own speech. Speech sound perception training is often used before and/or in conjunction with speech production training approaches. See Rvachew, 1994; Rvachew et al., 2004; Rvachew, Rafaat, & Martin, 1999; Wolfe, Presley, & Mesaris, 2003.
Traditionally, the speech stimuli used in these tasks are presented via live voice by the SLP. More recently, computer technology has been used—an advantage of this approach is that it allows for the presentation of more varied stimuli representing, for example, multiple voices and a range of error types.
Treatment Techniques and Technologies
Techniques used in therapy to increase awareness of the target sound and/or provide feedback about placement and movement of the articulators include the following:
- Using a mirror for visual feedback of place and movement of articulators
- Using gestural cueing for place or manner of production (e.g., using a long, sweeping hand gesture for fricatives vs. a short, "chopping" gesture for stops)
- Using ultrasound imaging (placement of an ultrasound transducer under the chin) as a biofeedback technique to visualize tongue position and configuration (Adler-Bock, Bernhardt, Gick, & Bacsfalvi, 2007; Lee, Wrench, & Sancibrian, 2015; Preston, Brick, & Landi, 2013; Preston et al., 2014)
- Using palatography (various coloring agents or a palatal device with electrodes) to record and visualize contact of the tongue on the palate while the child makes different speech sounds (Dagenais, 1995; Gibbon, Stewart, Hardcastle, & Crampin, 1999; Hitchcock, McAllister Byun, Swartz, & Lazarus, 2017)
- Amplifying target sounds to improve attention, reduce distractibility, and increase sound awareness and discrimination—for example, auditory bombardment with low-level amplification is used with the cycles approach at the beginning and end of each session to help children perceive differences between errors and target sounds (Hodson, 2010)
- Providing spectral biofeedback through a visual representation of the acoustic signal of speech (McAllister Byun & Hitchcock, 2012)
- Providing tactile biofeedback using tools, devices, or substances placed within the mouth (e.g., tongue depressors, peanut butter) to provide feedback on correct tongue placement and coordination (Altshuler, 1961; Leonti, Blakeley, & Louis, 1975; Shriberg, 1980)
Considerations for Treating Bilingual/Multilingual Populations
When treating a bilingual or multilingual individual with a speech sound disorder, the clinician is working with two or more different sound systems. Although there may be some overlap in the phonemic inventories of each language, there will be some sounds unique to each language and different phonemic rules for each language.
One linguistic sound system may influence production of the other sound system. It is the role of the SLP to determine whether any observed differences are due to a true communication disorder or whether these differences represent variations of speech associated with another language that a child speaks.
Strategies used when designing a treatment protocol include
- determining whether to use a bilingual or cross-linguistic approach (see ASHA's Practice Portal page on Multilingual Service Delivery in Audiology and Speech-Language Pathology );
- determining the language in which to provide services, on the basis of factors such as language history, language use, and communicative needs;
- identifying alternative means of providing accurate models for target phonemes that are unique to the child's language, when the clinician is unable to do so; and
- noting if success generalizes across languages throughout the treatment process (Goldstein & Fabiano, 2007).
Considerations for Treatment in Schools
Criteria for determining eligibility for services in a school setting are detailed in the Individuals with Disabilities Education Improvement Act of 2004 (IDEA). In accordance with these criteria, the SLP needs to determine
- if the child has a speech sound disorder;
- if there is an adverse effect on educational performance resulting from the disability; and
- if specially designed instruction and/or related services and supports are needed to help the student make progress in the general education curriculum.
Examples of the adverse effect on educational performance include the following:
- The speech sound disorder affects the child's ability or willingness to communicate in the classroom (e.g., when responding to teachers' questions; during classroom discussions or oral presentations) and in social settings with peers (e.g., interactions during lunch, recess, physical education, and extracurricular activities).
- The speech sound disorder signals problems with phonological skills that affect spelling, reading, and writing. For example, the way a child spells a word reflects the errors made when the word is spoken. See ASHA's resource language in brief and ASHA's Practice Portal pages on Spoken Language Disorders and Written Language Disorders for more information about the relationship between spoken and written language
Eligibility for speech-language pathology services is documented in the child's individualized education program, and the child's goals and the dismissal process are explained to parents and teachers. For more information about eligibility for services in the schools, see ASHA's resources on eligibility and dismissal in schools , IDEA Part B Issue Brief: Individualized Education Programs and Eligibility for Services , and 2011 IDEA Part C Final Regulations .
If a child is not eligible for services under IDEA, they may still be eligible to receive services under the Rehabilitation Act of 1973, Section 504. 29 U.S.C. § 701 (1973) . See ASHA's Practice Portal page on Documentation in Schools for more information about Section 504 of the Rehabilitation Act of 1973.
Dismissal from speech-language pathology services occurs once eligibility criteria are no longer met—that is, when the child's communication problem no longer adversely affects academic achievement and functional performance.
Children With Persisting Speech Difficulties
Speech difficulties sometimes persist throughout the school years and into adulthood. Pascoe et al. (2006) define persisting speech difficulties as "difficulties in the normal development of speech that do not resolve as the child matures or even after they receive specific help for these problems" (p. 2). The population of children with persistent speech difficulties is heterogeneous, varying in etiology, severity, and nature of speech difficulties (Dodd, 2005; Shriberg et al., 2010; Stackhouse, 2006; Wren, Roulstone, & Miller, 2012).
A child with persisting speech difficulties (functional speech sound disorders) may be at risk for
- difficulty communicating effectively when speaking;
- difficulty acquiring reading and writing skills; and
- psychosocial problems (e.g., low self-esteem, increased risk of bullying; see, e.g., McCormack, McAllister, McLeod, & Harrison, 2012).
Intervention approaches vary and may depend on the child's area(s) of difficulty (e.g., spoken language, written language, and/or psychosocial issues).
In designing an effective treatment protocol, the SLP considers
- teaching and encouraging the use of self-monitoring strategies to facilitate consistent use of learned skills;
- collaborating with teachers and other school personnel to support the child and to facilitate his or her access to the academic curriculum; and
- managing psychosocial factors, including self-esteem issues and bullying (Pascoe et al., 2006).
Transition Planning
Children with persisting speech difficulties may continue to have problems with oral communication, reading and writing, and social aspects of life as they transition to post-secondary education and vocational settings (see, e.g., Carrigg, Baker, Parry, & Ballard, 2015). The potential impact of persisting speech difficulties highlights the need for continued support to facilitate a successful transition to young adulthood. These supports include the following:
- Transition Planning —the development of a formal transition plan in middle or high school that includes discussion of the need for continued therapy, if appropriate, and supports that might be needed in postsecondary educational and/or vocational settings (IDEA, 2004).
- Disability Support Services —individualized support for postsecondary students that may include extended time for tests, accommodations for oral speaking assignments, the use of assistive technology (e.g., to help with reading and writing tasks), and the use of methods and devices to augment oral communication, if necessary.
The Americans with Disabilities Act of 1990 (ADA) and Section 504 of the Rehabilitation Act of 1973 provide protections for students with disabilities who are transitioning to postsecondary education. The protections provided by these acts (a) ensure that programs are accessible to these students and (b) provide aids and services necessary for effective communication (U.S. Department of Education, Office for Civil Rights, 2011).
For more information about transition planning, see ASHA's resource on Postsecondary Transition Planning .
Service Delivery
See the Service Delivery section of the Speech Sound Disorders Evidence Map for pertinent scientific evidence, expert opinion, and client/caregiver perspective.
In addition to determining the type of speech and language treatment that is optimal for children with speech sound disorders, SLPs consider the following other service delivery variables that may have an impact on treatment outcomes:
- Dosage —the frequency, intensity, and duration of service
- Format —whether a person is seen for treatment one-on-one (i.e., individual) or as part of a group
- Provider —the person administering the treatment (e.g., SLP, trained volunteer, caregiver)
- Setting —the location of treatment (e.g. home, community-based, school [pull-out or within the classroom])
- Timing —when intervention occurs relative to the diagnosis.
Technology can be incorporated into the delivery of services for speech sound disorders, including the use of telepractice as a format for delivering face-to-face services remotely. See ASHA's Practice Portal page on Telepractice .
The combination of service delivery factors is important to consider so that children receive optimal intervention intensity to ensure that efficient, effective change occurs (Baker, 2012; Williams, 2012).
ASHA Resources
- Consumer Information: Speech Sound Disorders
- Interprofessional Education/Interprofessional Practice (IPE/IPP)
- Let's Talk: For People With Special Communication Needs
- Person- and Family-Centered Care
- Person-Centered Focus on Function: Speech Sound Disorder [PDF]
- Phonemic Inventories and Cultural and Linguistic Information Across Languages
- Postsecondary Transition Planning
- Selected Phonological Processes (Patterns)
Other Resources
- Age of Acquisition of English Consonants (Crowe & McLeod, 2020) [PDF]
- American Cleft Palate–Craniofacial Association
- English Consonant and Vowel Charts (University of Arizona)
- Everyone Has an Accent
- Free Resources for the Multiple Oppositions approach - Adventures in Speech Pathology
- Multilingual Children's Speech: Overview
- Multilingual Children's Speech: Intelligibility in Context Scale
- Multilingual Children's Speech: Speech Participation and Activity Assessment of Children (SPAA-C)
- Phonetics: The Sounds of American English (University of Iowa)
- Phonological and Phonemic Awareness
- Place, Manner and Voicing Chart for English Consonants (Roth & Worthington, 2018)
- RCSLT: New Long COVID Guidance and Patient Handbook
- The Development of Phonological Skills (WETA Educational Website)
- The Speech Accent Archive (George Mason University)
Adler-Bock, M., Bernhardt, B. M., Gick, B., & Bacsfalvi, P. (2007). The use of ultrasound in remediation of North American English /r/ in 2 adolescents. American Journal of Speech-Language Pathology, 16, 128–139.
Altshuler, M. W. (1961). A therapeutic oral device for lateral emission. Journal of Speech and Hearing Disorders, 26, 179–181.
American Speech-Language-Hearing Association. (2016a). Code of ethics [Ethics]. Available from www.asha.org/policy/
American Speech-Language-Hearing Association. (20016b). Scope of practice in speech-language-pathology [Scope of Practice]. Available from www.asha.org/policy/
Americans with Disabilities Act of 1990, P.L. 101-336, 42 U.S.C. §§ 12101 et seq.
Anthony, J. L., Aghara, R. G., Dunkelberger, M. J., Anthony, T. I., Williams, J. M., & Zhang, Z. (2011). What factors place children with speech sound disorders at risk for reading problems? American Journal of Speech-Language Pathology, 20, 146–160.
Baker, E. (2012). Optimal intervention intensity. International Journal of Speech-Language Pathology, 14, 401–409.
Baker, E., & Williams, A. L. (2010). Complexity approaches to intervention. In S. F. Warren & M. E. Fey (Series Eds.). & A. L. Williams, S. McLeod, & R. J. McCauley (Volume Eds.), Intervention for speech sound disorders in children (pp. 95–115). Baltimore, MD: Brookes.
Bernthal, J., Bankson, N. W., & Flipsen, P., Jr. (2017). Articulation and phonological disorders: Speech sound disorders in children . New York, NY: Pearson.
Blache, S., & Parsons, C. (1980). A linguistic approach to distinctive feature training. Language, Speech, and Hearing Services in Schools, 11, 203–207.
Blache, S. E., Parsons, C. L., & Humphreys, J. M. (1981). A minimal-word-pair model for teaching the linguistic significant difference of distinctive feature properties. Journal of Speech and Hearing Disorders, 46, 291–296.
Black, L. I., Vahratian, A., & Hoffman, H. J. (2015). Communication disorders and use of intervention services among children aged 3–17 years; United States, 2012 (NHS Data Brief No. 205). Hyattsville, MD: National Center for Health Statistics.
Bleile, K. (2002). Evaluating articulation and phonological disorders when the clock is running. American Journal of Speech-Language Pathology, 11, 243–249.
Byers Brown, B., Bendersky, M., & Chapman, T. (1986). The early utterances of preterm infants. British Journal of Communication Disorders, 21, 307–320.
Camarata, S. (2010). Naturalistic intervention for speech intelligibility and speech accuracy. In A. L. Williams, S. McLeod, & R. J. McCauley (Eds.), Interventions for speech sound disorders in children (pp. 381–406). Baltimore, MD: Brookes.
Campbell, T. F., Dollaghan, C. A., Rockette, H. E., Paradise, J. L., Feldman, H. M., Shriberg, L. D., . . . Kurs-Lasky, M. (2003). Risk factors for speech delay of unknown origin in 3-year-old children. Child Development, 74, 346–357.
Carrigg, B., Baker, E., Parry, L., & Ballard, K. J. (2015). Persistent speech sound disorder in a 22-year-old male: Communication, educational, socio-emotional, and vocational outcomes. Perspectives on School-Based Issues, 16, 37–49.
Carroll, J. M., Snowling, M. J., Stevenson, J., & Hulme, C. (2003). The development of phonological awareness in preschool children. Developmental Psychology, 39, 913–923.
Catts, H. W., McIlraith, A., Bridges, M. S., & Nielsen, D. C. (2017). Viewing a phonological deficit within a multifactorial model of dyslexia. Reading and Writing, 30, 613–629.
Coplan, J., & Gleason, J. R. (1988). Unclear speech: Recognition and significance of unintelligible speech in preschool children. Pediatrics, 82, 447–452.
Crowe, K., & McLeod, S. (2020). Children’s English consonant acquisition in the United States: A review. American Journal of Speech-Language Pathology, 29 (4), 2155-2169. https://doi.org/10.1044/2020_AJSLP-19-00168.
Dagenais, P. A. (1995). Electropalatography in the treatment of articulation/phonological disorders. Journal of Communication Disorders, 28, 303–329.
Dean, E., Howell, J., Waters, D., & Reid, J. (1995). Metaphon: A metalinguistic approach to the treatment of phonological disorder in children. Clinical Linguistics & Phonetics, 9, 1–19.
Dodd, B. (2005). Differential diagnosis and treatment of children with speech disorder . London, England: Whurr.
Dodd, B., Holm, A., Crosbie, S., & McIntosh, B. (2006). A core vocabulary approach for management of inconsistent speech disorder. International Journal of Speech-Language Pathology, 8, 220–230.
Eadie, P., Morgan, A., Ukoumunne, O. C., Eecen, K. T., Wake, M., & Reilly, S. (2015). Speech sound disorder at 4 years: Prevalence, comorbidities, and predictors in a community cohort of children. Developmental Medicine & Child Neurology, 57, 578–584.
Elbert, M., & McReynolds, L. V. (1978). An experimental analysis of misarticulating children's generalization. Journal of Speech and Hearing Research, 21, 136–149.
Ertmer, D. J. (2010). Relationship between speech intelligibility and word articulation scores in children with hearing loss. Journal of Speech, Language, and Hearing Research, 53, 1075–1086.
Everhart, R. (1960). Literature survey of growth and developmental factors in articulation maturation. Journal of Speech and Hearing Disorders, 25, 59–69.
Fabiano-Smith, L., & Goldstein, B. A. (2010). Phonological acquisition in bilingual Spanish–English speaking children. Journal of Speech, Language, and Hearing Research, 53, 1 60–178.
Felsenfeld, S., McGue, M., & Broen, P. A. (1995). Familial aggregation of phonological disorders: Results from a 28-year follow-up. Journal of Speech, Language, and Hearing Research, 38, 1091–1107.
Fey, M. (1986). Language intervention with young children . Boston, MA: Allyn & Bacon.
Flipsen, P. (2006). Measuring the intelligibility of conversational speech in children. Clinical Linguistics & Phonetics, 20, 202–312.
Flipsen, P. (2015). Emergence and prevalence of persistent and residual speech errors. Seminars in Speech Language, 36, 217–223.
Fox, A. V., Dodd, B., & Howard, D. (2002). Risk factors for speech disorders in children. International Journal of Language and Communication Disorders, 37, 117–132.
Gibbon, F., Stewart, F., Hardcastle, W. J., & Crampin, L. (1999). Widening access to electropalatography for children with persistent sound system disorders. American Journal of Speech-Language Pathology, 8, 319–333.
Gierut, J. A. (1989). Maximal opposition approach to phonological treatment. Journal of Speech and Hearing Research, 54, 9–19.
Gierut, J. A. (1990). Differential learning of phonological oppositions. Journal of Speech and Hearing Research, 33, 540–549.
Gierut, J. A. (1992). The conditions and course of clinically induced phonological change. Journal of Speech and Hearing Research, 35, 1049–1063.
Gierut, J. A. (2007). Phonological complexity and language learnability. American Journal of Speech-Language Pathology, 16, 6–17.
Glaspey, A. M., & Stoel-Gammon, C. (2007). A dynamic approach to phonological assessment. Advances in Speech-Language Pathology, 9, 286–296.
Goldstein, B. A., & Fabiano, L. (2007, February 13). Assessment and intervention for bilingual children with phonological disorders. The ASHA Leader, 12, 6–7, 26–27, 31.
Grunwell, P. (1987). Clinical phonology (2nd ed.). London, England: Chapman and Hall.
Hitchcock, E. R., McAllister Byun, T., Swartz, M., & Lazarus, R. (2017). Efficacy of electropalatography for treating misarticulations of /r/. American Journal of Speech-Language Pathology, 26, 1141–1158.
Hodson, B. (2010). Evaluating and enhancing children's phonological systems: Research and theory to practice. Wichita, KS: PhonoComp.
Howell, J., & Dean, E. (1994). Treating phonological disorders in children: Metaphon—Theory to practice (2nd ed.). London, England: Whurr.
Individuals with Disabilities Education Improvement Act of 2004, P. L. 108-446, 20 U.S.C. §§ 1400 et seq. Retrieved from http://idea.ed.gov/
Kent, R. D., Miolo, G., & Bloedel, S. (1994). The intelligibility of children's speech: A review of evaluation procedures. American Journal of Speech-Language Pathology, 3, 81–95.
Law, J., Boyle, J., Harris, F., Harkness, A., & Nye, C. (2000). Prevalence and natural history of primary speech and language delay: Findings from a systematic review of the literature. International Journal of Language and Communication Disorders, 35, 165–188.
Lee, A. S. Y., & Gibbon, F. E. (2015). Non-speech oral motor treatment for children with developmental speech sound disorders. Cochrane Database of Systematic Reviews, 2015 (3), 1–42.
Lee, S. A. S., Wrench, A., & Sancibrian, S. (2015). How to get started with ultrasound technology for treatment of speech sound disorders. Perspectives on Speech Science and Orofacial Disorders, 25, 66–80.
Leitão, S., & Fletcher, J. (2004). Literacy outcomes for students with speech impairment: Long-term follow-up. International Journal of Language and Communication Disorders, 39, 245–256.
Leonti, S., Blakeley, R., & Louis, H. (1975, November). Spontaneous correction of resistant /ɚ/ and /r/ using an oral prosthesis. Paper presented at the annual convention of the American Speech and Hearing Association, Washington, DC.
Lewis, B. A., Avrich, A. A., Freebairn, L. A., Hansen, A. J., Sucheston, L. E., Kuo, I., . . . Stein, C. M. (2011). Literacy outcomes of children with early childhood speech sound disorders: Impact of endophenotypes. Journal of Speech, Language, and Hearing Research, 54, 1628–1643.
Locke, J. (1980). The inference of speech perception in the phonologically disordered child. Part I: A rationale, some criteria, the conventional tests. Journal of Speech and Hearing Disorders, 45, 431–444.
McAllister Byun, T., & Hitchcock, E. R. (2012). Investigating the use of traditional and spectral biofeedback approaches to intervention for /r/ misarticulation. American Journal of Speech-Language Pathology, 21, 207–221.
McCauley, R. J., Strand, E., Lof, G. L., Schooling, T., & Frymark, T. (2009). Evidence-based systematic review: Effects of nonspeech oral motor exercises on speech. American Journal of Speech-Language Pathology, 18, 343–360.
McCormack, J., McAllister, L., McLeod, S., & Harrison, L. (2012). Knowing, having, doing: The battles of childhood speech impairment. Child Language Teaching and Therapy, 28, 141–157.
McDonald, E. T. (1974). Articulation testing and treatment: A sensory motor approach. Pittsburgh, PA: Stanwix House.
McLeod, S., & Crowe, K. (2018). Children's consonant acquisition in 27 languages: A cross-linguistic review. American Journal of Speech-Language Pathology, 27, 1546–1571.
McLeod, S., Verdon, S., & The International Expert Panel on Multilingual Children's Speech. (2017). Tutorial: Speech assessment for multilingual children who do not speak the same language(s) as the speech-language pathologist. American Journal of Speech-Language Pathology, 26, 691–708.
McNeill, B. C., & Hesketh, A. (2010). Developmental complexity of the stimuli included in mispronunciation detection tasks. International Journal of Language & Communication Disorders, 45, 72–82.
McReynolds, L. V., & Bennett, S. (1972). Distinctive feature generalization in articulation training. Journal of Speech and Hearing Disorders, 37, 462–470.
Morley, D. (1952). A ten-year survey of speech disorders among university students. Journal of Speech and Hearing Disorders, 17, 25–31.
National Institute for Literacy. (2009). Developing early literacy: Report of the National Early Literacy Panel. A scientific synthesis of early literacy development and implications for intervention. Washington, DC: U.S. Department of Education.
National Institute of Child Health and Human Development. (2000). Teaching children to read: An evidence-based assessment of the scientific research literature on reading and its implications for reading instruction [Report of the National Reading Panel]. Washington, DC: Author.
Overby, M.S., Trainin, G., Smit, A. B., Bernthal, J. E., & Nelson, R. (2012). Preliteracy speech sound production skill and later literacy outcomes: A study using the Templin Archive. Language, Speech, and Hearing Services in Schools, 43, 97–115.
Pascoe, M., Stackhouse, J., & Wells, B. (2006). Persisting speech difficulties in children: Children's speech and literacy difficulties, Book 3. West Sussex, England: Whurr.
Peña-Brooks, A., & Hegde, M. N. (2015). Assessment and treatment of articulation and phonological disorders in children . Austin, TX: Pro-Ed.
Peterson, R. L., Pennington, B. F., Shriberg, L. D., & Boada, R. (2009). What influences literacy outcome in children with speech sound disorder? Journal of Speech, Language, and Hearing Research, 52, 1175-1188.
Powell, T. W., & Miccio, A. W. (1996). Stimulability: A useful clinical tool. Journal of Communication Disorders, 29, 237–253.
Preston, J. L., Brick, N., & Landi, N. (2013). Ultrasound biofeedback treatment for persisting childhood apraxia of speech. American Journal of Speech-Language Pathology, 22, 627–643.
Preston, J. L., McCabe, P., Rivera-Campos, A., Whittle, J. L., Landry, E., & Maas, E. (2014). Ultrasound visual feedback treatment and practice variability for residual speech sound errors. Journal of Speech, Language, and Hearing Research, 57, 2102–2115.
Prezas, R. F., & Hodson, B. W. (2010). The cycles phonological remediation approach. In A. L. Williams, S. McLeod, & R. J. McCauley (Eds.), Interventions for speech sound disorders in children (pp. 137–158). Baltimore, MD: Brookes.
Section 504 of the Rehabilitation Act of 1973, P.L. No. 93-112, 29 U.S.C. § 794.
Roth, F. P., & Worthington, C. K. (2018). Treatment resource manual for speech-language pathology . San Diego, CA: Plural Publishing.
Ruder, K. F., & Bunce, B. H. (1981). Articulation therapy using distinctive feature analysis to structure the training program: Two case studies. Journal of Speech and Hearing Disorders, 46, 59–65.
Rvachew, S. (1994). Speech perception training can facilitate sound production learning. Journal of Speech, Language, and Hearing Research, 37, 347–357.
Rvachew, S., & Bernhardt, B. M. (2010). Clinical implications of dynamic systems theory for phonological development. American Journal of Speech-Language Pathology, 19, 34–50.
Rvachew, S., Nowak, M., & Cloutier, G. (2004). Effect of phonemic perception training on the speech production and phonological awareness skills of children with expressive phonological delay. American Journal of Speech-Language Pathology, 13, 250–263.
Rvachew, S., Rafaat, S., & Martin, M. (1999). Stimulability, speech perception skills, and treatment of phonological disorders. American Journal of Speech-Language Pathology, 8, 33–43.
Shriberg, L. D. (1980). An intervention procedure for children with persistent /r/ errors. Language, Speech, and Hearing Services in Schools, 11, 102–110.
Shriberg, L. D., & Austin, D. (1998). Comorbidity of speech-language disorders: Implications for a phenotype marker for speech delay. In R. Paul (Ed.), The speech-language connection (pp. 73–117). Baltimore, MD: Brookes.
Shriberg, L. D., Austin, D., Lewis, B., McSweeny, J. L., & Wilson, D. L. (1997). The percentage of consonants correct (PCC) metric: Extensions and reliability data. Journal of Speech, Language, and Hearing Research, 40, 708–722.
Shriberg, L. D., Fourakis, M., Hall, S. D., Karlsson, H. B., Lohmeier, H. L., McSweeny, J. L., . . . Wilson, D. L. (2010). Extensions to the speech disorders classification system (SDCS). Clinical Linguistics & Phonetics, 24, 795–824.
Shriberg, L. D., & Kwiatkowski, J. (1980). Natural Process Analysis (NPA): A procedure for phonological analysis of continuous speech samples. New York, NY: Macmillan.
Shriberg, L. D., & Kwiatkowski, J. (1982a). Phonological disorders II: A conceptual framework for management. Journal of Speech and Hearing Disorders, 47, 242–256.
Shriberg, L. D., & Kwiatkowski, J. (1982b). Phonological disorders III: A procedure for assessing severity of involvement. Journal of Speech and Hearing Disorders, 47, 256–270.
Shriberg, L. D., & Kwiatkowski, J. (1994). Developmental phonological disorders I: A clinical profile. Journal of Speech and Hearing Research, 37, 1100–1126.
Shriberg, L. D., Tomblin, J. B., & McSweeny, J. L. (1999). Prevalence of speech delay in 6-year-old children and comorbidity with language impairment. Journal of Speech, Language, and Hearing Research, 42, 1461–1481.
Silva, P. A., Chalmers, D., & Stewart, I. (1986). Some audiological, psychological, educational and behavioral characteristics of children with bilateral otitis media with effusion. Journal of Learning Disabilities, 19, 165–169.
Stackhouse, J. (2006). Speech and spelling difficulties: Who is at risk and why? In M. Snowling & J. Stackhouse (Eds.), Dyslexia speech and language: A practitioner's handbook (pp. 15–35). West Sussex, England: Whurr.
Storkel, H. L. (2018). The complexity approach to phonological treatment: How to select treatment targets. Language, Speech, and Hearing Sciences in Schools, 49, 463–481.
Storkel, Holly. (2019). Using Developmental Norms for Speech Sounds as a Means of Determining Treatment Eligibility in Schools. Perspectives of the ASHA Special Interest Groups, 4, 67-75.
Teele, D. W., Klein, J. O., Chase, C., Menyuk, P., & Rosner, B. A. (1990). Otitis media in infancy and intellectual ability, school achievement, speech, and language at 7 years. Journal of Infectious Disease, 162, 685–694.
Tyler, A. A., & Tolbert, L. C. (2002). Speech-language assessment in the clinical setting. American Journal of Speech-Language Pathology, 11, 215–220.
U.S. Department of Education, Office for Civil Rights. (2011). Transition of students with disabilities to postsecondary education: A guide for high school educators . Washington, DC: Author. Retrieved from http://www2.ed.gov/about/offices/list/ocr/transitionguide.html
Wagner, R. K., & Torgesen, J. K. (1987). The nature of phonological processing and its causal role in the acquisition of reading skills. Psychological Bulletin, 101, 192–212.
Weiner, F. (1981). Treatment of phonological disability using the method of meaningful minimal contrast: Two case studies. Journal of Speech and Hearing Disorders, 46, 97–103.
Williams, A. L. (2000a). Multiple oppositions: Case studies of variables in phonological intervention. American Journal of Speech-Language Pathology, 9, 289–299.
Williams, A. L. (2000b). Multiple oppositions: Theoretical foundations for an alternative contrastive intervention approach. American Journal of Speech-Language Pathology, 9, 282–288.
Williams, A. L. (2003a). Speech disorders resource guide for preschool children. Clifton Park, NY: Delmar Learning.
Williams, A. L. (2003b). Target selection and treatment outcomes. Perspectives on Language Learning and Education, 10, 12–16.
Williams, A. L. (2012). Intensity in phonological intervention: Is there a prescribed amount? International Journal of Speech-Language Pathology, 14, 456–461.
Williams, A. L., McLeod, S., & McCauley, R. J. (2010). Direct speech production intervention. In A. L. Williams, S. McLeod, & R. J. McCauley (Eds.), Interventions for speech sound disorders in children (pp. 27–39). Baltimore, MD: Brookes.
Wolfe, V., Presley, C., & Mesaris, J. (2003). The importance of sound identification training in phonological intervention. American Journal of Speech-Language Pathology, 12, 282–288.
World Health Organization. (2001). International classification of functioning, disability and health. Geneva, Switzerland: Author.
Wren, Y., Miller, L. L., Peters, T. J., Emond, A., & Roulstone, S. (2016). Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. Journal of Speech, Language, and Hearing Research , 59, 647–673.
Wren, Y. E., Roulstone, S. E., & Miller, L. L. (2012). Distinguishing groups of children with persistent speech disorder: Findings from a prospective population study. Logopedics Phoniatrics Vocology, 37, 1–10.
About This Content
Acknowledgements .
Content for ASHA's Practice Portal is developed through a comprehensive process that includes multiple rounds of subject matter expert input and review. ASHA extends its gratitude to the following subject matter experts who were involved in the development of the Speech Sound Disorders: Articulation and Phonology page:
- Elise M. Baker, PhD
- John E. Bernthal, PhD, CCC-A/SLP
- Caroline Bowen, PhD
- Cynthia W. Core, PhD, CCC-SLP
- Sharon B. Hart, PhD, CCC-SLP
- Barbara W. Hodson, PhD, CCC-SLP
- Sharynne McLeod, PhD
- Susan Rvachew, PhD, S-LP(C)
- Cheryl C. Sancibrian, MS, CCC-SLP
- Holly L. Storkel, PhD, CCC-SLP
- Judith E. Trost-Cardamone, PhD, CCC-SLP
- Lynn Williams, PhD, CCC-SLP
Citing Practice Portal Pages
The recommended citation for this Practice Portal page is:
American Speech-Language-Hearing Association (n.d.) Speech Sound Disorders: Articulation and Phonology. (Practice Portal). Retrieved month, day, year, from www.asha.org/Practice-Portal/Clinical-Topics/Articulation-and-Phonology/ .

In This Section
- Practice Portal Home
- Clinical Topics
- Professional Issues
- Advertising Disclaimer
- Advertise with us
Evidence Maps
- ASHA Evidence Maps
Peer Connections
- Connect with your colleagues in the ASHA Community
- ASHA Special Interest Groups
ASHA Related Content
- Find related products in ASHA's Store
- Search for articles on ASHAWire
- ASHA Stream
Content Disclaimer: The Practice Portal, ASHA policy documents, and guidelines contain information for use in all settings; however, members must consider all applicable local, state and federal requirements when applying the information in their specific work setting.
ASHA Corporate Partners
- Become A Corporate Partner

The American Speech-Language-Hearing Association (ASHA) is the national professional, scientific, and credentialing association for 234,000 members, certificate holders, and affiliates who are audiologists; speech-language pathologists; speech, language, and hearing scientists; audiology and speech-language pathology assistants; and students.
- All ASHA Websites
- Work at ASHA
- Marketing Solutions
Information For
Get involved.
- ASHA Community
- Become a Mentor
- Become a Volunteer
- Special Interest Groups (SIGs)
Connect With ASHA
American Speech-Language-Hearing Association 2200 Research Blvd., Rockville, MD 20850 Members: 800-498-2071 Non-Member: 800-638-8255
MORE WAYS TO CONNECT
Media Resources
- Press Queries
Site Help | A–Z Topic Index | Privacy Statement | Terms of Use © 1997- American Speech-Language-Hearing Association
- Slurred Speech
6 Causes of Slurred Speech

- Most common questions
What is slurred speech?
Slurred speech quiz.
Take a quiz to find out what's causing your slurred speech.
6 most common cause(s)
Slurred speech is when you have trouble speaking, your words are slow or garbled, or your words run together. When you talk, many components of your nervous system work together to form words. When these parts don’t work correctly, your speech can become distorted, or “slurred.” The medical term for slurred speech is dysarthria.
Slurred speech includes problems pronouncing words and regulating the speed or pace of your speech. It can range from a barely noticeable problem to one that’s so severe that others can’t understand what you’re saying.
People often describe slurred speech as feeling like you’re trying to talk with your mouth full of marbles.
Common causes of slurred or slow speech include drinking too much alcohol and not getting enough sleep. In these cases, the slurring will stop once you’re sober again and have gotten rest, respectively.
There are also other causes of slurred speech such as a stroke (a medical emergency), brain tumor, Bell’s palsy, or a serious migraine.
Does slurred speech always need to be treated?
"People often think slurred speech is a minor symptom that does not need a medical evaluation. As our speech and ability to speak is our main form of communication, it is important to look for correctable causes." — Dr. Karen Hoerst
Should I go to the ER for slurred speech?
You should call 911 if:
- Your slurred speech starts suddenly.
- You have other symptoms, such as a sudden or severe headache and weakness or numbness of one side of your body.
- Your tongue, face, or lips are swelling, which could mean you’re having an allergic reaction.
Slurred speech emergency quiz
Take a quiz to find out if your symptoms are an emergency.
Take emergency quiz
1. Stroke or TIA (transient ischemic attack)
- Slurred speech
- Drooping of one side of the face
- Weakness or trouble controlling one side of the body
- Numbness in the face , arm , or leg
- Difficulty walking
- Sudden loss of vision or double vision
- Sudden, severe headache
A stroke occurs in the brain because the blow flow in a blood vessel is blocked. It can also happen when a blood vessel ruptures or leaks. This affects the blood supply to parts of the brain, which leads long-term damage. If it affects the area of the brain responsible for speech, it can cause slurred speech.
A transient ischemic attack , or TIA, is sometimes called a "mini stroke." A TIA is a temporary interruption of blood flow that causes the same symptoms as a stroke, but improves without any permanent damage to the brain or symptoms.
For example, if you have slurred speech because of a TIA, once the blood flow is restored to that area of the brain, the slurred speech goes away. But people who have a TIA are at a high risk of having a stroke in the future, especially if their risk factors are not treated. Risk factors are the same for stroke and TIA and include smoking, obesity, and cardiovascular disease.
It’s extremely important to call 911 right away if you suddenly have slurred speech. Getting immediate treatment is critical to minimizing permanent damage. Paramedics can begin treating you in the ambulance on the way to the hospital, so it’s better to call 911 than go to the ER yourself.
Treatments for strokes and TIAs include medications to break up blood clots and surgery to remove blood clots from the vessels. If your stroke is from bleeding in the brain, you may need surgery to repair a blood vessel.
Following treatment, your doctor will recommend medications to prevent another TIA or stroke. These typically include drugs that prevent clots from forming in the blood (like aspirin or other blood thinners) and cholesterol medication to prevent plaque from building up on the walls of the blood vessels. You may also need to take medication to control your blood pressure.
Speech therapy is recommended to help treat problems with speech.
It may not be a stroke
"There are so many possible causes of slurred speech. Most of the time we need a detailed history and physical exam to guide the diagnosis and treatment." — Dr. Hoerst
Take symptoms quiz
2. Bell’s palsy
- Drooping of the face
- Drooping of the eye
- Changes in taste or hearing
Bell’s palsy is a relatively common condition that affects the facial nerve, which is responsible for movement of your face.
In Bell’s palsy, the nerve gets inflamed typically because of a recent viral infection. This inflammation can cause the facial nerve to not work as well, leading to drooping and slurred speech.
Bell’s palsy usually improves in a few months, but medications such as steroids and antiviral drugs are typically given to help speed the process. If nerve problems continue, physical therapy is recommended. In rare instances, surgery may be needed to help improve facial muscle function.
3. Brain tumor
- Slurred speech or speech difficulties
- New or changing headaches
- Weakness or coordination and balance problems
- Abnormal vision
A brain tumor is an abnormal growth of cells in the brain. A brain tumor may be cancerous (malignant) or noncancerous (benign). Both types can cause symptoms including slurred speech.
The diagnosis of a tumor in the brain or spinal cord is based on an exam and imaging of the brain, such as an MRI or CT scan. A biopsy (tissue sample) may be needed to determine what type of tumor it is.
Some tumors, such as a small noncancerous tumor, do not need treatment, though your doctor will recommend periodic MRI scans to make sure it hasn’t changed.
Most larger or cancerous tumors do require treatment, which may consist of chemotherapy, radiation, or surgery. If you develop physical or cognitive (mental) problems from the tumor, rehabilitation such as physical therapy, occupational therapy, or speech therapy may be needed.
4. Multiple sclerosis
- Blurred vision or decreased vision, typically in one eye
- Weakness or trouble walking
- Numbness or pins-and-needles sensation on your face, arm, or leg (typically on one side)
- A band-like squeezing sensation around the chest or abdomen
- Difficulty focusing
Multiple sclerosis, or MS, is a central-nervous system disease that affects the cells of the brain and spinal cord. In MS, a fatty tissue that surrounds nerve fibers (myelin) is attacked. Myelin helps to insulate the electrical signals sent through the nerves. When there is a problem with this fatty tissue, information sent to and from the brain can be disrupted.
MS is most common in young adults between the ages of 20 and 50, according to the National MS Society .
MS is not curable , but treatments have dramatically improved the ability to control MS, so people usually have fewer symptoms and less disability.
Treatment includes medications that may be taken orally or injected or infused through an IV line. Physical therapy and speech therapy are commonly used to help in physical recovery, and medications can be used to treat other symptoms, such as depression, pain, and fatigue.
5. Amyotrophic lateral sclerosis (ALS)
- Difficulty with speech, including slurred speech
- Progressive weakness and difficulty balancing
- Muscle cramps, twitching, and stiffness
- Difficulty swallowing
Amyotrophic lateral sclerosis (ALS) is also known as Lou Gehrig’s disease. It affects nerve cells called motor neurons that control your movement.
The disease primarily causes a loss of strength, impaired swallowing and speech, and in most cases, difficulty breathing because of impaired respiratory muscles. It is a progressive disease, meaning that symptoms are mild at first and worsen over time.
Previously, it was thought that ALS doesn’t affect a person’s mental ability. But it’s now known that people with ALS can get a specific type of dementia called frontotemporal dementia (FTD). That condition can affect behavior, mood, and speech.
Symptoms of ALS can develop in adults of any age, but it’s most commonly diagnosed in people who are between the ages of 40 and 70, according to the ALS Association .
While there are some medications that can be used to delay the progression of the disease, there is currently no cure for ALS. Treatment includes rehabilitation with physical therapy, occupational therapy, speech therapy, and respiratory therapy.
6. Migraine
- Sensitivity to light and sound
- Visual disturbances
A migraine causes a severe headache that is often accompanied by nausea and sensitivity to light or sound. But some migraines don’t cause head pain.
Other symptoms that involve the nervous system can occur. Some of these sensory symptoms are called “auras.” These distortions can cause visual changes , including flashing lights or distorted vision. People may feel tingling or numbness of their face, arm, or leg.
In some types of migraine, people may even develop slurred speech and weakness of the face, arm, or leg. These are also symptoms of a stroke, so it may be hard to figure out which condition you have. If you develop sudden slurred speech or weakness, go to the ER immediately.
In an acute migraine attack, medications can be used to stop a migraine that has already started, such as triptans or newer medications called CGRP inhibitors. These medications can be in pill form, inhaled form, or injectable medications.
Migraine prevention can include taking medications for blood pressure, anticonvulsants, or even antidepressants. In some instances, Botox treatments are used to prevent migraine.
Behavior and lifestyle changes such as exercise, improved sleep, and healthy diet or weight loss are also often recommended to help decrease the number of migraine headaches you experience.
Other possible causes
Slurred speech may occur from alcohol intoxication or tiredness. It can also be a side effect of medications like high dose pain medications, antipsychotic medications or even some allergy medications like antihistamines. Other causes include:
- Infections such as urinary tract infections or electrolyte imbalances (particularly in elderly people).
- Brain infections such as meningitis or encephalitis.
- Problems that affect your mouth or throat, such as poorly fitting dentures, dental infections, dental numbing medications, swelling in your throat, or muscle or nerve problems.
- An allergic reaction , especially if you notice slurred speech along with tongue swelling , lip swelling, or shortness of breath.
"Early speech therapy can not only help with early improvement but also with diagnosis. Speech-language pathologists have special training in detecting the various types of slurred speech, which helps to determine the possible causes."— Dr. Hoerst
Specialty treatment options
- Speech therapy is the most common treatment for slurred speech.
- Injected medications such as Botox are sometimes used, depending on the cause of slurred speech.
- Medications to improve nerve and muscle function.
While it's important to follow your healthcare provider's guidance, here are some over-the-counter (OTC) options that might provide extra support.
- Proper nutrition supports overall health, including nerve function. Supplements like B vitamins may support neurological health.
- Staying hydrated is key, especially if speech difficulties make it hard to drink. Consider a no-spill, easy-sip water bottle designed for easy grip.
- Engaging in exercises to improve speech clarity can be helpful. Explore speech therapy tools and resources that you can use at home.
Slurred speech treatment quiz
Take a quiz to find out how to treat your symptoms.
Take treatment quiz
Required field
Was this article helpful?
Learn About the 50 Essential Biomakers that Determine Your Health, Energy, and Lifespan
How Google's huge defeat in antitrust case could change how you search the internet

In the most significant legal ruling against a major technology giant in more than two decades, a federal judge says Google illegally monopolized online search and advertising by paying companies like Apple and Samsung billions of dollars a year to install Google as the default search engine on smartphones and web browsers.
By monopolizing search queries on smartphones and browsers, Google abused its dominance in the search market, throttling competition and harming consumers, U.S. District Judge Amit P. Mehta said in his 286-page decision. Google owes much of its more than $300 billion in annual revenue to search ads.
“ Google is a monopolist , and it has acted as one to maintain its monopoly,” Mehta wrote.
The massive win for the Department of Justice could fundamentally reshape how Google does business . It also could change how we use the internet and search for information.
The DOJ filed antitrust charges during the final weeks of the Trump administration, making good on Donald Trump’s pledge to challenge the runaway power of Big Tech. That mission continued during the Biden administration, which has been aggressive in pursuing antitrust cases.
“This victory against Google is an historic win for the American people,” Attorney General Merrick Garland said in a statement. “No company – no matter how large or influential – is above the law.”
The case is the most significant victory for the DOJ in a monopoly case in decades, said Notre Dame Law School professor Roger Alford, who served in the DOJ’s antitrust division. “Not since Microsoft lost in the 1990s have we seen a case of this magnitude.”
Google said it would appeal the decision. “This decision recognizes that Google offers the best search engine, but concludes that we shouldn’t be allowed to make it easily available,” Kent Walker, president of global affairs, said in a statement.
Shares in Google's parent company Alphabet slipped following the judge's ruling. They closed down nearly 5% Monday, part of a broader tech stock selloff .
If upheld, the decision will be a “major boost” for other antitrust cases pending against Google as well as other major tech players like Amazon, Apple and Meta, said Loyola University Chicago School of Law professor Spencer Weber Waller.
Monday’s ruling did not include remedies. Remedies will be decided separately, likely after an appeal. One remedy could see Google losing its ability to strike device deals that have helped make its search engine so ubiquitous.
Devising the right remedy is critical to restoring competition to the marketplace, Waller said.
“There are no fines or monetary penalties in these types of cases, but the court will have to decide whether Google should be broken up in some way. More likely, it will order Google to eliminate the exclusive contracts and licensing restrictions that have reinforced its monopoly position for years,” he said.
Google has argued that its distribution deals are common in the business world. It pays for its search engine to be on phones the way a food manufacturer pays to promote its products at eye level in a grocery store aisle.
The way Google sees it, if you don’t like Google, you can switch the default search engine on your device. But people don’t switch, Google says, because they prefer Google.
If Google was not the default search engine on so many devices, would consumers still use it for 90% of web searches?
During the 10-week trial, Microsoft CEO Satya Nadella testified that Google’s unchallenged dominance created a “Google web.”
“You get up in the morning, you brush your teeth and you search on Google,” Nadella said at one point in his testimony. “Everybody talks about the open web, but there is really the Google web.”
Nadella has expressed concern that Microsoft’s disadvantage would increase as artificial intelligence becomes a major component of search.
In a research note Monday, Baird Equity Research senior analyst Colin Sebastian pointed to a range of tactics Google's arch-competitor Microsoft has used to grow the market share of its Bing search engine over the years, from paying users to use its search engine to embedding it in Office.
“People clearly prefer Google to Bing,” Sebastian said.
Chamber of Progress CEO Adam Kovacevich said Monday's ruling hands Microsoft an unearned boost.
“The biggest winner from today's ruling isn't consumers or little tech, it’s Microsoft,” Kovacevich said in a statement. “Microsoft has underinvested in search for decades, but today’s ruling opens the door to a court mandate of default deals for Bing. That’s a slap in the face to consumers who chose Google because they think it’s the best.”
What Kamala Harris has said so far on key issues in her campaign
As she ramps up her nascent presidential campaign, Vice President Kamala Harris is revealing how she will address the key issues facing the nation.
In speeches and rallies, she has voiced support for continuing many of President Joe Biden’s measures, such as lowering drug costs , forgiving student loan debt and eliminating so-called junk fees. But Harris has made it clear that she has her own views on some key matters, particularly Israel’s treatment of Gazans in its war with Hamas.
In a departure from her presidential run in 2020, the Harris campaign has confirmed that she’s moved away from many of her more progressive stances, such as her interest in a single-payer health insurance system and a ban on fracking.
Harris is also expected to put her own stamp and style on matters ranging from abortion to the economy to immigration, as she aims to walk a fine line of taking credit for the administration’s accomplishments while not being jointly blamed by voters for its shortcomings.
Her early presidential campaign speeches have offered insights into her priorities, though she’s mainly voiced general talking points and has yet to release more nuanced plans. Like Biden, she intends to contrast her vision for America with that of former President Donald Trump. ( See Trump’s campaign promises here .)
“In this moment, I believe we face a choice between two different visions for our nation: one focused on the future, the other focused on the past,” she told members of the historically Black sorority Zeta Phi Beta at an event in Indianapolis in late July. “And with your support, I am fighting for our nation’s future.”
Here’s what we know about Harris’ views:
Harris took on the lead role of championing abortion rights for the administration after Roe v. Wade was overturned in June 2022. This past January, she started a “ reproductive freedoms tour ” to multiple states, including a stop in Minnesota thought to be the first by a sitting US president or vice president at an abortion clinic .
On abortion access, Harris embraced more progressive policies than Biden in the 2020 campaign, as a candidate criticizing his previous support for the Hyde Amendment , a measure that blocks federal funds from being used for most abortions.
Policy experts suggested that although Harris’ current policies on abortion and reproductive rights may not differ significantly from Biden’s, as a result of her national tour and her own focus on maternal health , she may be a stronger messenger.
High prices are a top concern for many Americans who are struggling to afford the cost of living after a spell of steep inflation. Many voters give Biden poor marks for his handling of the economy, and Harris may also face their wrath.
In her early campaign speeches, Harris has echoed many of the same themes as Biden, saying she wants to give Americans more opportunities to get ahead. She’s particularly concerned about making care – health care, child care, elder care and family leave – more affordable and available.
Harris promised at a late July rally to continue the Biden administration’s drive to eliminate so-called “junk fees” and to fully disclose all charges, such as for events, lodging and car rentals. In early August, the administration proposed a rule that would ban airlines from charging parents extra fees to have their kids sit next to them.
On day one, I will take on price gouging and bring down costs. We will ban more of those hidden fees and surprise late charges that banks and other companies use to pad their profits.”
Since becoming vice president, Harris has taken more moderate positions, but a look at her 2020 campaign promises reveals a more progressive bent than Biden.
As a senator and 2020 presidential candidate, Harris proposed providing middle-class and working families with a refundable tax credit of up to $6,000 a year (per couple) to help keep up with living expenses. Titled the LIFT the Middle Class Act, or Livable Incomes for Families Today, the measure would have cost at the time an estimated $3 trillion over 10 years.
Unlike a typical tax credit, the bill would allow taxpayers to receive the benefit – up to $500 – on a monthly basis so families don’t have to turn to payday loans with very high interest rates.
As a presidential candidate, Harris also advocated for raising the corporate income tax rate to 35%, where it was before the 2017 Tax Cuts and Jobs Act that Trump and congressional Republicans pushed through Congress reduced the rate to 21%. That’s higher than the 28% Biden has proposed.
Affordable housing was also on Harris’ radar. As a senator, she introduced the Rent Relief Act, which would establish a refundable tax credit for renters who annually spend more than 30% of their gross income on rent and utilities. The amount of the credit would range from 25% to 100% of the excess rent, depending on the renter’s income.
Harris called housing a human right and said in a 2019 news release on the bill that every American deserves to have basic security and dignity in their own home.
Consumer debt
Hefty debt loads, which weigh on people’s finances and hurt their ability to buy homes, get car loans or start small businesses, are also an area of interest to Harris.
As vice president, she has promoted the Biden administration’s initiatives on student debt, which have so far forgiven more than $168 billion for nearly 4.8 million borrowers . In mid-July, Harris said in a post on X that “nearly 950,000 public servants have benefitted” from student debt forgiveness, compared with only 7,000 when Biden was inaugurated.
A potential Harris administration could keep that momentum going – though some of Biden’s efforts have gotten tangled up in litigation, such as a program aimed at cutting monthly student loan payments for roughly 3 million borrowers enrolled in a repayment plan the administration implemented last year.
The vice president has also been a leader in the White House efforts to ban medical debt from credit reports, noting that those with medical debt are no less likely to repay a loan than those who don’t have unpaid medical bills.
In a late July statement praising North Carolina’s move to relieve the medical debt of about 2 million residents, Harris said that she is “committed to continuing to relieve the burden of medical debt and creating a future where every person has the opportunity to build wealth and thrive.”
Health care
Harris, who has had shifting stances on health care in the past, confirmed in late July through her campaign that she no longer supports a single-payer health care system .
During her 2020 campaign, Harris advocated for shifting the US to a government-backed health insurance system but stopped short of wanting to completely eliminate private insurance.
The measure called for transitioning to a Medicare-for-All-type system over 10 years but continuing to allow private insurance companies to offer Medicare plans.
The proposal would not have raised taxes on the middle class to pay for the coverage expansion. Instead, it would raise the needed funds by taxing Wall Street trades and transactions and changing the taxation of offshore corporate income.
When it comes to reducing drug costs, Harris previously proposed allowing the federal government to set “a fair price” for any drug sold at a cheaper price in any economically comparable country, including Canada, the United Kingdom, France, Japan or Australia. If manufacturers were found to be price gouging, the government could import their drugs from abroad or, in egregious cases, use its existing but never-used “march-in” authority to license a drug company’s patent to a rival that would produce the medication at a lower cost.
Harris has been a champion on climate and environmental justice for decades. As California’s attorney general, Harris sued big oil companies like BP and ConocoPhillips, and investigated Exxon Mobil for its role in climate change disinformation. While in the Senate, she sponsored the Green New Deal resolution.
During her 2020 campaign, she enthusiastically supported a ban on fracking — but a Harris campaign official said in late July that she no longer supports such a ban.
Fracking is the process of using liquid to free natural gas from rock formations – and the primary mode for extracting gas for energy in battleground Pennsylvania. During a September 2019 climate crisis town hall hosted by CNN, she said she would start “with what we can do on Day 1 around public lands.” She walked that back later when she became Biden’s running mate.
Biden has been the most pro-climate president in history, and climate advocates find Harris to be an exciting candidate in her own right. Democrats and climate activists are planning to campaign on the stark contrasts between Harris and Trump , who vowed to push America decisively back to fossil fuels, promising to unwind Biden’s climate and clean energy legacy and pull America out of its global climate commitments.
If elected, one of the biggest climate goals Harris would have to craft early in her administration is how much the US would reduce its climate pollution by 2035 – a requirement of the Paris climate agreement .
Immigration
Harris has quickly started trying to counter Trump’s attacks on her immigration record.
Her campaign released a video in late July citing Harris’ support for increasing the number of Border Patrol agents and Trump’s successful push to scuttle a bipartisan immigration deal that included some of the toughest border security measures in recent memory.
The vice president has changed her position on border control since her 2020 campaign, when she suggested that Democrats needed to “critically examine” the role of Immigration and Customs Enforcement, or ICE, after being asked whether she sided with those in the party arguing to abolish the department.
In June of this year, the White House announced a crackdown on asylum claims meant to continue reducing crossings at the US-Mexico border – a policy that Harris’ campaign manager, Julie Chavez Rodriguez, indicated in late July to CBS News would continue under a Harris administration.
Trump’s attacks stem from Biden having tasked Harris with overseeing diplomatic efforts in Central America in March 2021. While Harris focused on long-term fixes, the Department of Homeland Security remained responsible for overseeing border security.
She has only occasionally talked about her efforts as the situation along the US-Mexico border became a political vulnerability for Biden. But she put her own stamp on the administration’s efforts, engaging the private sector.
Harris pulled together the Partnership for Central America, which has acted as a liaison between companies and the US government. Her team and the partnership are closely coordinating on initiatives that have led to job creation in the region. Harris has also engaged directly with foreign leaders in the region.
Experts credit Harris’ ability to secure private-sector investments as her most visible action in the region to date but have cautioned about the long-term durability of those investments.
Israel-Hamas
The Israel-Hamas war is the most fraught foreign policy issue facing the country and has spurred a multitude of protests around the US since it began in October.
After meeting with Israeli Prime Minister Benjamin Netanyahu in late July, Harris gave a forceful and notable speech about the situation in Gaza.
We cannot look away in the face of these tragedies. We cannot allow ourselves to become numb to the suffering. And I will not be silent.”
Harris echoed Biden’s repeated comments about the “ironclad support” and “unwavering commitment” to Israel. The country has a right to defend itself, she said, while noting, “how it does so, matters.”
However, the empathy she expressed regarding the Palestinian plight and suffering was far more forceful than what Biden has said on the matter in recent months. Harris mentioned twice the “serious concern” she expressed to Netanyahu about the civilian deaths in Gaza, the humanitarian situation and destruction she called “catastrophic” and “devastating.”
She went on to describe “the images of dead children and desperate hungry people fleeing for safety, sometimes displaced for the second, third or fourth time.”
Harris emphasized the need to get the Israeli hostages back from Hamas captivity, naming the eight Israeli-American hostages – three of whom have been killed.
But when describing the ceasefire deal in the works, she didn’t highlight the hostage for prisoner exchange or aid to be let into Gaza. Instead, she singled out the fact that the deal stipulates the withdrawal by the Israeli military from populated areas in the first phase before withdrawing “entirely” from Gaza before “a permanent end to the hostilities.”
Harris didn’t preside over Netanyahu’s speech to Congress in late July, instead choosing to stick with a prescheduled trip to a sorority event in Indiana.
Harris is committed to supporting Ukraine in its fight against Russian aggression, having met with Ukrainian President Volodymyr Zelensky at least six times and announcing last month $1.5 billion for energy assistance, humanitarian needs and other aid for the war-torn country.
At the Munich Security Conference earlier this year, Harris said: “I will make clear President Joe Biden and I stand with Ukraine. In partnership with supportive, bipartisan majorities in both houses of the United States Congress, we will work to secure critical weapons and resources that Ukraine so badly needs. And let me be clear: The failure to do so would be a gift to Vladimir Putin.”
More broadly, NATO is central to our approach to global security. For President Biden and me, our sacred commitment to NATO remains ironclad. And I do believe, as I have said before, NATO is the greatest military alliance the world has ever known.”
Police funding
The Harris campaign has also walked back the “defund the police” sentiment that Harris voiced in 2020. What she meant is she supports being “tough and smart on crime,” Mitch Landrieu, national co-chair for the Harris campaign and former mayor of New Orleans, told CNN’s Pamela Brown in late July.
In the midst of nationwide 2020 protests sparked by George Floyd’s murder by a Minneapolis police officer, Harris voiced support for the “defund the police” movement, which argues for redirecting funds from law enforcement to social services. Throughout that summer, Harris supported the movement and called for demilitarizing police departments.
Democrats largely backed away from calls to defund the police after Republicans attempted to tie the movement to increases in crime during the 2022 midterm elections.
Related links

Additional credits
What Is Price Gouging? Here’s What To Know About Kamala Harris’ Core Economic Policy
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Central to Vice President Kamala Harris’ economic agenda is a proposal to combat “price gouging” on food products, an initiative aimed at tackling voters’ top priority in inflation, though the benefits of the bold plan are not immediately clear, and it faces a wall of criticism from industry groups and some economists.
US Vice President Kamala Harris on Friday.
Price gouging can broadly be defined as when sellers charge more for a product than the fair market dictates based on supply and demand in order to make a higher profit, typically taking advantage of an adverse situation—think ballpark vendors charging twice the normal gameday price for a bottle of water when it’s 100 degrees.
But price gouging is not a “technical term in economics,” according to the Federal Reserve Bank of Richmond, meaning the concept is far from agreed upon like other economic effects such as supply and demand or the inverse relationship between inflation and unemployment, and it’s less clear what the effects of efforts to limit price gouging would look like or their efficacy.
The Harris campaign said Friday it plans to ban price gouging to combat “the excessive prices unrelated to the costs of doing business that Americans have seen in the food and grocery industry,” as well as crack down on mergers and acquisitions in the food industry to keep competition robust.
Yet it remains unclear that restrictions on grocery price increases will have the intended effect of helping the American consumer, as food prices are historically fickle as they can go up or down based on a variety of factors, like less rain in Western Africa causing cocoa prices to skyrocket or an American avian flu outbreak causing egg prices to spike, in addition to the alleged corporate greed.
And it’s hardly a consensus view that corporate profit taking was the sole driver of soaring food prices: A Federal Reserve Bank of San Francisco study published in May found “rising markups have not been a main driver” of inflation over the last three years.
“Price regulation can be beneficial, but it's tricky,” Carnegie Mellon University economics professor Felix Koenig explained to Forbes.
Would A Price Gouging Ban Work?
“The kind of logic that Kamala Harris and others are proposing is that these markets aren't really competitive,” said Koenig, adding the “key question” is whether or not they are regulating an “imperfect” market. That’s a critical distinction considering price caps in an already competitive market can have the unintended effect of discouraging new companies from entering a market, making an industry less competitive over the long run. “Economists generally oppose most price controls, believing that they produce costly shortages and gluts,” wrote Federal Reserve Bank of St. Louis economist Christopher J. Neely in a 2022 article .
27%. That’s how much more expensive groceries were last month than they were in July 2019, according to the consumer price index’s food at home subcategory. That equates to 5.4% annualized grocery inflation over the last five years, a reflection of the continued strain on Americans to put food on their tables even as price increases moderate, with year-over-year grocery inflation coming in at 1.1% in July.
Chief Critics
Harris’ proposal to curb price gouging inspired a litany of pushback from economic policy experts from both sides of the aisle, unsurprising considering it goes against the basic economic principle of potentially undue intervention. Brian Riedl, senior fellow of the right-leaning Manhattan Institute, told The Washington Post it “represents a return to the lazy, failed economic policies of the 1970s, when price controls proved to be a disaster for the economy,” and Jason Furman, an economist at Harvard University and a Biden administration official, told The New York Times : “This is not sensible policy, and I think the biggest hope is that it ends up being a lot of rhetoric and no reality.”
Further Reading

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.
Advertisement
Supported by
Harris Plans to Ban Grocery ‘Price Gouging.’ What Does the Evidence Say?
Price increases when demand exceeds supply are textbook economics. The question is whether, and how much, the pandemic yielded an excess take.
- Share full article

By Jim Tankersley and Jeanna Smialek
Reporting from Washington
Vice President Kamala Harris’s economic agenda for her presidential campaign features an argument that blames corporate price gouging for high grocery prices.
That message polls well with swing voters. It has been embraced by progressive groups , which regularly point to price gouging as a driver of rapid inflation, or at least something that contributes to rapid price increases. Those groups cheered the announcement late Wednesday that Ms. Harris would call for a federal ban on corporate price gouging on groceries in an economic policy speech on Friday.
But the economic argument over the issue is complicated.
Economists have cited a range of forces for pushing up prices in the recovery from the pandemic recession, including snarled supply chains, a sudden shift in consumer buying patterns , and the increased customer demand fueled by stimulus from the government and low rates from the Federal Reserve. Most economists say those forces are far more responsible than corporate behavior for the rise in prices in that period.
Biden administration economists have found that corporate behavior has played a role in pushing up grocery costs in recent years — but that other factors have played a much larger one.
The Harris campaign announcement on Wednesday cited meat industry consolidation as a driver of excessive grocery prices, but officials did not respond on Thursday to questions about the evidence Ms. Harris would cite or how her proposal would work.
There are examples of companies telling investors in recent years that they have been able to raise prices to increase profits. But even the term “price gouging” means different things to different people.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Watch CBS News
President Biden speaks on the stakes of the 2024 election, and on his place in history
By Robert Costa
Updated on: August 12, 2024 / 2:07 PM EDT / CBS News
In his first interview since withdrawing from his re-election bid last month , President Biden told "CBS Sunday Morning" that he made his decision, in part, so that the Democratic Party could fully concentrate on what he believes is an urgent task at hand: preventing former President Donald Trump from regaining the White House.
Speaking with CBS News chief election & campaign correspondent Robert Costa, Mr. Biden said that he made his historic decision at his family home in Rehoboth Beach, Delaware, in late July, just weeks after his debate with Trump, which caused concern in some Democratic circles.
"The polls we had showed that it was a neck-and-neck race, would have been down to the wire," Mr. Biden said. "But what happened was, a number of my Democratic colleagues in the House and Senate thought that I was gonna hurt them in the races. And I was concerned if I stayed in the race, that would be the topic. You'd be interviewing me about 'Why did Nancy Pelosi say…' 'Why did so-and-so…' And I thought it'd be a real distraction, number one.
"Number two, when I ran the first time, I thought of myself as being a transition President. I can't even say how old I am; it's hard for me to get it outta my mouth. But things got moving so quickly, it didn't happen."
Added to that combination, he said, was "the critical issue for me still – it's not a joke – maintaining this democracy. I thought it was important. Because, although it's a great honor being president, I think I have an obligation to the country to do what [is] the most important thing you can do, and that is, we must, we must, we must defeat Trump."

President Biden announced his decision on Sunday, July 21, and addressed the nation from the Oval Office three days later, saying that he would not let anything, even "personal ambition," get in the way of "saving our democracy."
- Read President Biden's letter announcing his withdrawal from the 2024 presidential race
Following his speech, he was joined by members of his family. Asked what he told them after his historic address, Mr. Biden replied, "It's what they said to me. They said – my grandchildren call me Pop, my children call me Dad. And they said they were proud, and it mattered to me a lot."
Costa then asked about the president's late son, Beau Biden, who died in 2015. "When I saw you with your family in the Oval, I wondered, is he thinking of Beau, too?"
Mr. Biden paused. "Look, I can honestly say that I think of him all the time. Whenever I have a decision that's really hard to make, I literally ask myself, 'What would Beau do?' He should be sitting here being interviewed, not me. He was really a fine man. You know, Beau was committed to my staying committed. We had a conversation toward the end when he was … we, everybody, we knew he wasn't going to live. And he said, 'Dad, I know, we know what's gonna happen. I'm gonna be okay, Dad. I'm all right. I'm not afraid. But Dad, you gotta make me a promise.' I said, 'What's that, Beau?' He said, 'I know when it happens, you're gonna want to quit. You're not gonna stay engaged …. Look at me. Look at me, Dad. Give me your word as a Biden. When I go, you'll stay engaged. Give me your word. Give me your word.' And I did.
"And that's why – I had not planned on running after he died, and then Charlottesville happened."
On August 12, 2017, white supremacist demonstrations in Charlottesville, Virginia turned deadly when Heather Heyer, a civil rights activist, was murdered in what the Justice Department called a "hate-inspired act of domestic terrorism."
Mr. Biden has long traced his decision to run in 2020 to that moment – the beginning of his journey to the presidency.
Costa asked, "As you look at American democracy seven years later, how do you see it?"
"When I spoke to the mom who lost her daughter as a consequence of neo-Nazis and right [wing], white supremacists coming out of fields in America with torches, carrying Nazi banners, singing the same, sick antisemitic bile that was sung in Germany in the '30s, and when her daughter was killed, the press went to then-President Trump and said, 'What do you think?' He said, 'There are very fine people on both sides.' I knew then, I knew I had to do something. And that's why I decided to run, because democracy was literally at stake."
Mr. Biden explained that the Republican nominee's talk underscores his concerns that a second Trump term would undermine democracy.
"He evidenced everything that we thought," Mr. Biden said. "Now, January 6th, attack on the Capitol, he talks about now, because he now talks about making sure they're all, you know, let out of prison. He's gonna pardon them. Think of this. Every other time the Ku Klux Klan has been involved they wore hoods so they're not identified. Under his presidency, they came out of those woods with no hoods, knowing they had an ally. That's how I read it. They knew they had an ally in the White House. And he stepped up for them."
Mr. Biden said he is not confident that there would be a peaceful transfer of power should Trump [who refused to acknowledge his election loss in 2020] lose in November to Vice President Kamala Harris.
"If Trump wins ... I mean, if Trump loses, I'm not confident at all," Mr. Biden said. "He means what he says. We don't take him seriously. He means it. All the stuff about, 'If we lose, it'll be a bloodbath …' Look what they're trying to do now in the local election districts where people count the votes. They're putting people in place in states that they're gonna 'count the votes,' right?"
Repeating his familiar maxim about politics in a democracy, President Biden said, "You can't love your country only when you win."
Trump has said his remarks on Charlottesville were not intended to praise white nationalists, and that he was warning of economic carnage when he said "bloodbath."
But Trump isn't the only thing on Mr. Biden's mind, with five months left in his presidency.
Asked if he believes a ceasefire is possible in Israel's war with Hamas before he leaves office, Mr. Biden replied, "Yes. It's still possible. The plan I put together, endorsed by the G7, endorsed by the U.N. Security Council, et cetera, is still viable. And I'm working literally every single day – and my whole team – to see to it that it doesn't escalate into a regional war. But it easily can."

When Mr. Biden entered office in early 2021, he had an ambitious agenda. Costa said, "Some Senators told me, in March of 2021, you took them into the Oval Office and pointed up at FDR's portrait and said, 'We're going big. We're going in that direction.'"
"I did," Mr. Biden said. "And we have, with the great help of so many people. Look, democracy works. And it was very important to prove that it worked, prove that it worked. I mean, look at what we've been able to do: We created 16 million jobs, I mean, real new jobs. We've gotten around a brink of having the private sector invest over a trillion dollars – a trillion dollars – in the American economy. One of the things I fought for as a Senator for a long time was to change the dynamic of how we grow the economy, not from the top down, but from the bottom up. The idea of trickle-down economics doesn't work, in my view."
Asked if he would project that pride in his administration's record by going on the campaign trail with Harris, Mr. Biden said yes. "I talk to her frequently, and by the way, I've known her running mate is a great guy. As we say, if we grew up in the same neighborhood, we'd have been friends. He's my kind of guy. He's real, he's smart. I've known him for several decades. I think it's a hell of a team."
"To those who have expressed skepticism about how much you'll be on the trail, or about the rest of your term, raised questions about your health, what do you say to them?" asked Costa.
"All I can say is, 'Watch.' That's all," Mr. Biden replied. "Look, I had a really, really bad day in that debate because I was sick. But I have no serious problem.
"I was talking to Governor Shapiro, who's a friend. We have got to win Pennsylvania, my original home state. He and I are putting together a campaign tour in Pennsylvania. I'm going to be campaigning in other states as well. And I'm going to do whatever Kamala thinks I can do to help most."
Mr. Biden talked with "CBS Sunday Morning" in the president's private residence, in the White House Treaty Room, where historic peace agreements have been signed, beneath a portrait of Ulysses S. Grant, the general-turned-president who labored to restore the Union after the Civil War.
Asked how he wishes history to remember him, President Biden replied, "That he proved democracy can work. It got us out of a pandemic. It produced the single greatest economic recovery in American history. We're the most powerful economy in the world. We have more to do. And it demonstrated that we can pull the nation together.
"Look, I've always believed, and I still do, the American people are good and decent, honorable people," he said. "When I announced my candidacy to run way back for President, I said, 'We've got to do three things: Restore the soul of America; build the economy from the middle out and the bottom up, not the top down; and bring the country together.' No one thought we could get done – including some of my own people – what we got done.
"One of the problems is, I knew all the things we did were going to take a little time to work their way through," he continued. "So now, people are realizing, 'Oh, that highway, oh, that …' The biggest mistake we made, we didn't put up signs saying, 'Joe did it'!"
Four years ago, what "Joe" did was defeat Donald Trump. Now, with Trump attempting to return to the White House, the president is sounding the alarm in a way sitting presidents rarely, if ever, do.
"The stakes are that high to you?" asked Costa.
"I give you my word, I think they're that high," Mr. Biden said. "Mark my words: If he wins this nomination, I mean, excuse me, this election, watch what happens. It's a danger. He's a genuine danger to American security.
"Look, we're at an inflection point in world history, we really are," the president said. "The decisions we make in the last three, four years, and the next three or four years are going to determine what the next six decades look like. And democracy is the key. And that's why I went down and made that speech in Johnson Center about the Supreme Court. Supreme Court is so out of whack, so out of whack. And so, I proposed that we limit terms to 18 years .
"There's little regard by the MAGA Republicans for the political institutions," he said. "That's what holds this country together. That's what democracy's about. That's who we are as a nation."
Story produced by Ed Forgotson. Editor: Carol A. Ross.
WEB EXTRA: President Biden on uniting Europe, making NATO stronger (Video)

Robert Costa is the Chief Election & Campaign correspondent for CBS News, where he covers national politics and American democracy.
More from CBS News

Willie Brown threatens to sue Trump over helicopter ride story
RFK Jr. attempted to arrange meeting with Harris, sources say

Biden praises Harris in first joint event, saying she will make "one hell of a president"

3 vulnerable Senate Democrats to skip DNC
- Patient Care & Health Information
- Diseases & Conditions
- Primary progressive aphasia
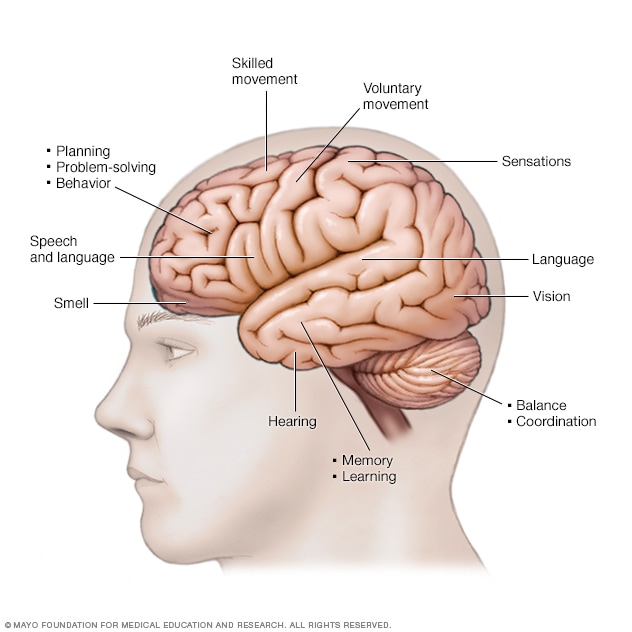
Functions of the brain
Different areas of the brain are responsible for different vital functions.
Primary progressive aphasia (uh-FAY-zhuh) is a rare nervous system syndrome that affects the ability to communicate. People who have it can have trouble expressing their thoughts and understanding or finding words.
Symptoms begin gradually, often before age 65. They get worse over time. People with primary progressive aphasia can lose the ability to speak and write. Eventually they're not able to understand written or spoken language.
This condition progresses slowly. People who have primary progressive aphasia may continue caring for themselves and participating in daily activities for several years.
Primary progressive aphasia is a type of frontotemporal dementia. Frontotemporal dementia is a cluster of disorders that results from the degeneration of the frontal or temporal lobes of the brain. These areas include brain tissue involved in speech and language.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Primary progressive aphasia symptoms vary based on which part of the brain's language areas are involved. The condition has three types. Each type causes different symptoms. Symptoms develop over time and gradually get worse.
Semantic variant primary progressive aphasia
Symptoms include:
- Trouble understanding spoken or written language, particularly single words.
- Trouble understanding the meaning of words.
- Not being able to name objects.
- Trouble formulating sentences.
Logopenic variant primary progressive aphasia
- Trouble understanding spoken language, particularly long sentences.
- Pausing and hesitancy during speech while searching for words.
- Not being able to repeat phrases or sentences.
Nonfluent-agrammatic variant primary progressive aphasia
- Poor grammar in written and spoken language.
- Trouble understanding complex sentences.
- Using grammar incorrectly.
- May have problems speaking. This includes making errors in speech sounds, known as apraxia of speech.
Primary progressive apraxia of speech is related to primary progressive aphasia, but people with this disorder don't have trouble with language. They have problems speaking. This includes making errors in speech sound or having trouble saying words quickly.
When to see a doctor
See your health care provider if you have concerns about your ability to communicate. If you have a family member or friend who has symptoms of primary progressive aphasia, talk to the person about your concerns. Offer to go with the person to see a health care provider.
If changes in speech or communication come on suddenly, call 911 or your local emergency number.
Primary progressive aphasia is caused by a shrinking of certain areas of the brain, known as lobes. In this case, the frontal, temporal or parietal lobes are affected. When areas of the brain shrink, it's called atrophy. The atrophy caused by primary progressive aphasia mainly occurs on the left side of the brain. The areas affected are responsible for speech and language.
Atrophy is associated with the presence of certain proteins in the brain. The proteins may reduce brain activity or function.
Risk factors
Risk factors for primary progressive aphasia include:
- Learning disabilities. People who had a childhood learning disability such as dyslexia might be at somewhat higher risk of primary progressive aphasia.
- Certain gene changes. Rare gene changes have been linked to primary progressive aphasia. If other members of your family have had it, you might be more likely to develop it.
Complications
People with primary progressive aphasia eventually lose the ability to speak and write. This may take anywhere from 3 to 15 years. They also have trouble understanding written and spoken language. Some people are not able to form sounds to speak, even when they still have the ability to write and comprehend language. This is called apraxia of speech.
As the disease progresses, other mental skills such as memory, planning and organizing can be affected. Some people develop other symptoms such as problems with movement, balance and swallowing. With these complications, people with the disease eventually will need help with day-to-day care.
People with primary progressive aphasia also can develop depression as the disease progresses. Other problems might include blunted emotions such as not showing concern, poor judgment or inappropriate social behavior.
Primary progressive aphasia care at Mayo Clinic
- Primary progressive aphasia. National Aphasia Association. http://www.aphasia.org/aphasia-resources/primary-progressive-aphasia/. Accessed Feb. 20, 2023.
- Lee SE, et al. Frontotemporal dementia: Clinical features and diagnosis. https://www.uptodate.com/contents/search. Accessed Feb. 20, 2023.
- Jankovic J, et al., eds. Alzheimer disease and other dementias. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Feb. 20, 2023.
- Budson AE, et al. Primary progressive aphasia and apraxia of speech. In: Memory Loss, Alzheimer's Disease, and Dementia. 3rd ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Feb. 20, 2023.
- Baratono S, et al. What are the key diagnostic cognitive impairment and dementia subtypes and how to integrate all of the diagnostic data to establish a diagnosis? Clinics in Geriatric Medicine. 2023; doi:10.1016/j.cger.2022.08.002.
- Coemans S, et al. Executive functions in primary progressive aphasia: A meta-analysis. Cortex. 2022; doi:10.1016/j.cortex.2022.
- Nicolo Aiello E, et al. Primary progressive aphasia and motor neuron disease: A review. Frontiers in Aging Neuroscience. 2022; doi:10.3389/fnagi.2022.1003792.
- Aphasia. American Speech-Language-Hearing Association. https://www.asha.org/public/speech/disorders/aphasia/. Accessed Feb. 20, 2023.
- A diagnosis of primary progressive aphasia? What to expect. National Aphasia Association. https://www.aphasia.org/stories/ppa-what-to-expect/. Accessed Feb. 21, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. Jan. 10, 2023.
- Srinivasan J, et al., eds. Dementia: Mild cognitive impairment, Alzheimer disease, Lewy Body Dementia, Frontotemporal Lobar Dementia, Vascular Dementia. In: Netter's Neurology. 3rd ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Feb. 21, 2023.
- Tippett DC, et al. Clinical and neuroimaging characteristics of primary progressive aphasia. Handbook of Clinical Neurology. 2022; doi:10.1016/B978-0-12-823384-9.00016-5.
- Tartaglia MC, et al. Recent advances in frontotemporal dementia. Canadian Journal of Neurological Sciences. 2022; doi:10.1017/cjn.2022.69.
- Providing care for a person with a frontotemporal disorder. National Institute on Aging. https://www.nia.nih.gov/health/providing-care-person-frontotemporal-disorder. Accessed Feb. 21, 2023.
- Support for people with FTD. Association for Frontotemporal Degeneration. https://www.theaftd.org/living-with-ftd/support-for-people-with-ftd/. Accessed Feb. 21, 2023.
- Alzheimer's disease research centers. National Institute on Aging. https://www.nia.nih.gov/health/alzheimers-disease-research-centers. Accessed Feb. 20, 2023.
- Arizona Alzheimer's Consortium. http://azalz.org/about-us/. Accessed Feb. 20, 2023.
- Botha H, et al. Primary progressive aphasia and apraxia of speech. Continuum. 2019; doi:10.1212/CON.0000000000000699.
- Utianski RL (expert opinion). Mayo Clinic. Feb. 22, 2023.
Associated Procedures
- Genetic testing
- Positron emission tomography scan
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
- Environment
- National Politics
- Transportation
- Coronavirus
Tim Walz couch joke explained; what he said about JD Vance

Minnesota governor and Democratic VP pick Tim Walz waded into internet meme territory Tuesday with a snappy one-liner about JD Vance.
During the Harris-Walz rally in Philadelphia , Walz delivered a couch-related zinger to Republican VP nominee Vance .
Here's what Tim Walz said about JD Vance and the much-discussed couch .
Tim Walz tells JD Vance to 'get off the couch' and agree to debate
During his speech at the Harris-Walz rally at Temple University in Philadelphia on Tuesday, Walz set up the zinger by telling the crowd that JD Vance doesn't represent the midwesterners Walz grew up with.
"JD studied at Yale, had his career funded by Silicon Valley millionaires, and then wrote a bestseller trashing that community," Walz said. "C'mon; that's not what middle America is."
Then came the zinger.
"And I gotta tell ya; I can't wait to debate this guy," Walz continued, before pausing for dramatic effect. "That's if he's willing to get off the couch and show up.
"See what I did there?"
The joke appeared to be off-script, given the facial reaction of running mate Vice President Kamala Harris, which sent the partisan crowd at the Liacouras Center into a frenzy.
@meidastouch Gov. Tim Walz obliterates JD Vance: I can't wait to debate the guy — that is if he's willing to get off the couch and show up. #timwalz #jdvance #couch #meidastouch ♬ original sound - MeidasTouch
JD Vance couch joke explained
Tim Walz' jab at JD Vance has many levels, and grew out of the false allegations that JD Vance had sex with his couch .
That many respected news outlets ran with it as fact only fueled the joke, which lead to the creation of several JD Vance couch sex-related memes and spawned dozens of related social media accounts.
JD Vance couch story
Social media then amplified the JD Vance couch sex rumor even further by tying it to Vance's book, " Hillbilly Elegy ," a best-selling memoir written by Vance in 2016 and made into a film in 2020 .
Many JD couch-meme creators have identified themselves and seem to enjoy that these memes generated so much traction that well-known publications had to issue corrections and retract stories that stated it as fact that JD Vance had intercourse with his couch.
Damon C. Williams is a Philadelphia-based journalist reporting on trending topics across the Mid-Atlantic Region.
- Election 2024
- Entertainment
- Newsletters
- Photography
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Delegate Tracker
- AP & Elections
- 2024 Paris Olympic Games
- Auto Racing
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Trump’s vow to only be a dictator on ‘day one’ follows growing worry over his authoritarian rhetoric
Former President Donald Trump speaks during a Commit to Caucus rally, Saturday, Dec. 2, 2023, in Ankeny, Iowa. (AP Photo/Matthew Putney)
Former President Donald Trump sits at the defense table while waiting for proceedings to begin in his civil business fraud trial at New York Supreme Court, Thursday, Dec. 7, 2023, in New York. (Mike Segar/Pool via AP)
Former President Donald Trump speaks after exiting the courtroom for a break at New York Supreme Court, Thursday, Dec. 7, 2023, in New York. (AP Photo/Eduardo Munoz Alvarez)
Former President Donald Trump talks to supporters during a stop at the Front Street Pub & Eatery, Tuesday, Dec. 5, 2023, in Davenport, Iowa. (AP Photo/Charlie Neibergall)
- Copy Link copied
TUSCALOOSA, Ala. (AP) — As Donald Trump faces growing scrutiny over his increasingly authoritarian and violent rhetoric , Fox News host Sean Hannity gave his longtime friend a chance to assure the American people that he wouldn’t abuse power or seek retribution if he wins a second term.
But instead of offering a perfunctory answer brushing off the warnings, Trump stoked the fire.
“Except for day one,” the GOP front-runner said Tuesday night before a live audience in Davenport, Iowa. “I want to close the border, and I want to drill, drill, drill.”
And in case anyone missed it, he reenacted the exchange.
“We love this guy,” Trump said of Hannity. “He says, ‘You’re not going to be a dictator, are you?’ I said: ‘No, no, no, other than day one. We’re closing the border, and we’re drilling, drilling, drilling. After that, I’m not a dictator.’”
Trump has a long history of making inflammatory proclamations that spark outrage from detractors and generate a stream of headlines, without ever coming to fruition. Often they are made in a tongue-in-cheek manner that allows Trump’s allies to claim he was joking and cite the backlash as another example of a candidate skilled at baiting an out-of-touch press that takes him far too literally.
Trump campaign aides said Thursday that the former president was simply trying to trigger the left and the media with his dictator comment, while also seeking to focus attention on the influx of migrants at the border and stubborn inflation, two vulnerabilities for President Joe Biden heading into the 2024 general election.
But the consequences of Trump’s rhetoric have been made all too clear, after he refused to accept the results of the 2020 election and a mob of his supporters violently stormed the U.S. Capitol to stop the certification of Biden’s victory.
The former president, who has long expressed regard for authoritarian leaders and the power they wield, is now vowing vengeance and retribution as he outlines a second-term agenda marked by an unprecedented expansion of executive power, unparalleled interference in the justice system, and a massive purge of civil servants.
Indeed, hours before his remarks were aired, a longtime ally who is widely expected to serve in a top national security role if Trump returns to the White House vowed to target journalists in a second Trump term.
“We’re going to come after the people in the media who lied about American citizens, who helped Joe Biden rig presidential elections,” said Kash Patel, even though numerous federal and local officials, a long list of courts, top former campaign staffers and even Trump’s own attorney general have all said there is no evidence of the fraud he alleges .
Biden and other critics have seized on Trump’s comments, painting him as a threat to democracy as they seek to turn the 2024 election into another referendum on the former president instead of Biden. Cognizant of the risks, Trump’s campaign has tried to distance itself from Patel’s statement as well as headline-grabbing policy plans proposed by several outside groups staffed by longtime Trump allies, with top aides issuing a statement last month saying the groups did not speak for the campaign.
Trump, too, has tried to turn the tables on Biden, who has increasingly argued the former president poses a fundamental danger to the country. In a speech in Iowa this month, Trump insisted it is really Biden who is the true “destroyer” of democracy, citing the four criminal indictments he is facing as politically motivated efforts to damage his campaign.
What to know about the 2024 Election
- Today’s news: Follow live updates from the campaign trail from the AP.
- Ground Game: Sign up for AP’s weekly politics newsletter to get it in your inbox every Monday.
- AP’s Role: The Associated Press is the most trusted source of information on election night, with a history of accuracy dating to 1848. Learn more.
It’s an argument Trump and his campaign plan to continue to make heading into the 2024 general election.
The Biden campaign’s attack, said Trump senior adviser Jason Miller, “is a clear sign that the Democrats believe their only possible pathway to victory is to go scorched earth on President Trump.”
Despite Democrats’ attempts “to make outlandish statements about what a future Trump term could look like,” Miller said, there is now a reference point: “Four years of President Trump in the White House, and he never did any of the types of things that Joe Biden is currently doing to him.”
But Trump’s own words are clear.
“In 2016, I declared I am your voice. Today, I add, I am your warrior. I am your justice. And for those who have been wronged and betrayed, I am your retribution,” he said in March 2023.
In the months since, Trump has repeatedly and explicitly vowed to use the Justice Department to target his enemies in a dramatic break from the long-standing, post-Watergate tradition of independence.
“I will appoint a real special prosecutor to go after the most corrupt president in the history of the United States of America, Joe Biden, the entire Biden crime family, and all others involved with the destruction of our elections, borders and our country itself,” he said in a June video.
In an interview with Univision, he went even further. “If I happen to be president and I see somebody who’s doing well and beating me very badly, I say, ‘Go down and indict them,’” he said.
Last December, he mused about circumventing the Constitution, arguing that the election fraud he alleges “allows for the termination of all rules, regulations, and articles, even those found in the Constitution.”
He has taken an especially hostile approach to the press, vowing to “rout the fake news media,” calling reporters “THE ENEMY OF THE PEOPLE!” and saying outlets like NBC News and MSNBC should be investigated for treason.
Trump’s extensive policy plans also rely on a dramatic expansion of executive power. He wants to strip tens of thousands of career federal workers of their civil service protections, has vowed new ideological tests for those entering the country and has talked about increasing the military’s role on domestic soil , including sending the National Guard to the border and to cities like Chicago to tackle crime.
He has warned that the gravest threats to the nation come “not from abroad, but from within,” has called for expanded use of the death penalty while praising countries that rely on “quick” trials and extrajudicial killings , and has said looters should be shot.
He has continued to praise authoritarian leaders like China’s Xi Jinping, Hungary’s Viktor Orbán and Russia’s Vladimir Putin, while dehumanizing his enemies as “scum” and “thugs” who “live like vermin.”
Aides argue the former president did not enact some of his most extreme campaign promises, like jailing his then-rival Hillary Clinton or enacting “a total and complete shutdown of Muslims entering the United States,” though he did try to ban foreign nationals from a handful of Muslim-majority countries. They note his campaign operation this time around has been widely praised as more disciplined and professional than his previous efforts — a sign of what could be to come.
But if he wins again, Trump is expected to face far fewer guardrails, including an administration filled with loyalists now experienced in wielding federal power, fewer rivals in Congress and more appointees across the courts.
Quentin Fulks, the No. 2 official on Biden’s reelection campaign, pushed back at Trump’s attempts to turn the issue back on Biden and said there is no comparison between the men. Biden, he said, is not standing at the presidential podium “saying that he’s going to round up his political enemies or use the government to go after his political enemies.”
He said it was imperative for Democrats to “call out this rhetoric when we see it and make sure the American people really know what’s at stake.”
Meanwhile, Ken Cuccinelli, a top immigration official in Trump’s administration who now leads a super PAC supporting Florida Gov. Ron DeSantis for president, called the former president’s dictator remarks “provocative” and vintage Trump.
“Do I think he’s trying to needle everybody? Yes, I do. He enjoys doing that,” Cuccinelli said. “Does it help improve America? No, it doesn’t. And he doesn’t care about that because his first concern is Donald Trump.”
Colvin reported from New York.


IMAGES
COMMENTS
Speech and language impairments are two words that are often used interchangeably, but they are two very different types of problems. Speech means talking. It uses the jaw muscles, tongue, lips ...
stroke. traumatic brain injury. degenerative neurological or motor disorder. injury or illness that affects your vocal cords. dementia. Depending on the cause and type of speech impairment, it may ...
Speech disorders affect the vocal cords, muscles, nerves, and other structures within the throat. Causes may include: vocal cord damage. brain damage. muscle weakness. respiratory weakness ...
Definition. A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the child's speech difficult to understand. Common speech disorders are: Articulation disorders; Phonological disorders; Disfluency Voice disorders or resonance disorders
People develop a voice disorder for many reasons. A voice disorder is a change in how the voice sounds. Health care providers trained in ear, nose and throat illnesses and speech-language pathologists diagnose and treat voice issues. Treatment depends on what's causing the voice change. Treatment can include voice therapy, drugs, shots or surgery.
Speech disorders, impairments, or impediments, are a type of communication disorder in which normal speech is disrupted. [1] This can mean fluency disorders like stuttering, cluttering or lisps.Someone who is unable to speak due to a speech disorder is considered mute. [2] Speech skills are vital to social relationships and learning, and delays or disorders that relate to developing these ...
Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual's ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
Speech and Language Disorders. Speech is how we say sounds and words. People with speech problems may: not say sounds clearly. have a hoarse or raspy voice. repeat sounds or pause when speaking, called stuttering. Language is the words we use to share ideas and get what we want. A person with a language disorder may have problems:
Speech apraxia (difficulty coordinating speech) Difficulty understanding the meaning of what other people are saying; Inability to use the correct words; ... Many different types of speech problems can affect children and adults. Some of these are congenital (present from birth), while others are acquired due to health conditions, medication ...
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Fluency: Your child may have problems with how their words and sentences flow. Stuttering is a fluency disorder. That's when your child repeats words, parts of words, or uses odd pauses. It's ...
And by definition, all children who have autism also have social communication problems. Speech-language pathologists are often a critical voice on a team of professionals - also including pediatricians, occupational therapists, neurologists, developmental specialists, and physical therapists - who make an autism spectrum diagnosis.
Symptoms of dysarthria depend on the underlying cause and the type of dysarthria. Symptoms may include: Slurred speech. Slow speech. Not being able to speak louder than a whisper or speaking too loudly. Rapid speech that is difficult to understand. Nasal, raspy or strained voice. Uneven speech rhythm. Uneven speech volume.
Symptoms vary depending on a child's age and the severity of the speech problems. CAS can result in: Babbling less or making fewer vocal sounds than is typical between the ages of 7 to 12 months. Speaking first words late, typically after ages 12 to 18 months old. Using a limited number of consonants and vowels.
See the Speech Sound Disorders Evidence Map for summaries of the available research on this topic.. The scope of this page is speech sound disorders with no known cause—historically called articulation and phonological disorders—in preschool and school-age children (ages 3-21).. Information about speech sound problems related to motor/neurological disorders, structural abnormalities, and ...
Weakness or coordination and balance problems. Abnormal vision. Confusion. Seizures. A brain tumor is an abnormal growth of cells in the brain. A brain tumor may be cancerous (malignant) or noncancerous (benign). Both types can cause symptoms including slurred speech.
Contamination: fusing ideas into one another. Accelerated thinking: rapid flow and increased volume of speech. Flight of ideas: losing track of where a thought is going. Inhibited thinking: slow ...
Speech problems after stroke are often diagnosed as aphasia, dysarthria, or apraxia of speech. These conditions affect a number of different speech and language functions, making it difficult for survivors to communicate effectively. It is best to work with a speech-language pathologist to discover which exercises and techniques may be most ...
The case is the most significant victory for the DOJ in a monopoly case in decades, said Notre Dame Law School professor Roger Alford, who served in the DOJ's antitrust division.
Causes. The most common cause of aphasia is brain damage resulting from a stroke — the blockage or rupture of a blood vessel in the brain. Loss of blood to the brain leads to brain cell death or damage in areas that control language. Brain damage caused by a severe head injury, a tumor, an infection or a degenerative process also can cause ...
As she ramps up her nascent presidential campaign, Vice President Kamala Harris is revealing how she will address the key issues facing the nation.. In speeches and rallies, she has voiced support ...
Central to Vice President Kamala Harris' economic agenda is a proposal to combat "price gouging" on food products, an initiative aimed at tackling voters' top priority in inflation, though ...
Price increases when demand exceeds supply are textbook economics. The question is whether, and how much, the pandemic yielded an excess take.
In his first interview since withdrawing from the race, the president reflects on his decision to end his bid for reelection and what he says is the importance of defeating Trump to protect democracy.
Trouble understanding the meaning of words. Not being able to name objects. Trouble formulating sentences. Logopenic variant primary progressive aphasia. Symptoms include: Trouble understanding spoken language, particularly long sentences. Pausing and hesitancy during speech while searching for words. Not being able to repeat phrases or sentences.
During his speech at the Harris-Walz rally at Temple University in Philadelphia on Tuesday, Walz set up the zinger by telling the crowd that JD Vance doesn't represent the midwesterners Walz grew ...
In a speech in Iowa this month, Trump insisted it is really Biden who is the true "destroyer" of democracy, ... Quentin Fulks, the No. 2 official on Biden's reelection campaign, pushed back at Trump's attempts to turn the issue back on Biden and said there is no comparison between the men. Biden, he said, is not standing at the ...