Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Universality of universal health coverage: A scoping review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations School of Public Health, The University of Queensland, Brisbane, Australia, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Roles Conceptualization, Supervision
Affiliation College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Affiliation School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Roles Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
- Aklilu Endalamaw,
- Charles F. Gilks,
- Fentie Ambaw,
- Yibeltal Assefa

- Published: August 22, 2022
- https://doi.org/10.1371/journal.pone.0269507
- Reader Comments
16 May 2024: Endalamaw A, Gilks CF, Ambaw F, Assefa Y (2024) Correction: Universality of universal health coverage: A scoping review. PLOS ONE 19(5): e0304023. https://doi.org/10.1371/journal.pone.0304023 View correction
The progress of Universal health coverage (UHC) is measured using tracer indicators of key interventions, which have been implemented in healthcare system. UHC is about population, comprehensive health services and financial coverage for equitable quality services and health outcome. There is dearth of evidence about the extent of the universality of UHC in terms of types of health services, its integrated definition (dimensions) and tracer indicators utilized in the measurement of UHC. Therefore, we mapped the existing literature to assess universality of UHC and summarize the challenges towards UHC.
The checklist Preferred Reporting Items for Systematic reviews and Meta-analysis extension for Scoping Reviews was used. A systematic search was carried out in the Web of Science and PubMed databases. Hand searches were also conducted to find articles from Google Scholar, the World Bank Library, the World Health Organization Library, the United Nations Digital Library Collections, and Google. Article search date was between 20 October 2021 and 12 November 2021 and the most recent update was done on 03 March 2022. Articles on UHC coverage, financial risk protection, quality of care, and inequity were included. The Population, Concept, and Context framework was used to determine the eligibility of research questions. A stepwise approach was used to identify and select relevant studies, conduct data charting, collation and summarization, as well as report results. Simple descriptive statistics and narrative synthesis were used to present the findings.
Forty-seven papers were included in the final review. One-fourth of the articles (25.5%) were from the African region and 29.8% were from lower-middle-income countries. More than half of the articles (54.1%) followed a quantitative research approach. Of included articles, coverage was assessed by 53.2% of articles; financial risk protection by 27.7%, inequity by 25.5% and quality by 6.4% of the articles as the main research objectives or mentioned in result section. Most (42.5%) of articles investigated health promotion and 2.1% palliation and rehabilitation services. Policy and healthcare level and cross-cutting barriers of UHC were identified. Financing, leadership/governance, inequity, weak regulation and supervision mechanism, and poverty were most repeated policy level barriers. Poor quality health services and inadequate health workforce were the common barriers from health sector challenges. Lack of common understanding on UHC was frequently mentioned as a cross-cutting barrier.
Conclusions
The review showed that majority of the articles were from the African region. Methodologically, quantitative research design was more frequently used to investigate UHC. Palliation and rehabilitation health care services need attention in the monitoring and evaluation of UHC progress. It is also noteworthy to focus on quality and inequity of health services. The study implies that urgent action on the identified policy, health system and cross-cutting barriers is required to achieve UHC.
Citation: Endalamaw A, Gilks CF, Ambaw F, Assefa Y (2022) Universality of universal health coverage: A scoping review. PLoS ONE 17(8): e0269507. https://doi.org/10.1371/journal.pone.0269507
Editor: Wen-Wei Sung, Chung Shan Medical University, TAIWAN
Received: May 27, 2022; Accepted: August 9, 2022; Published: August 22, 2022
Copyright: © 2022 Endalamaw et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its supporting information files.
Funding: The authors received no specific funding for this work.
Competing interests: Authors declared no conflict of interest.
Abbreviations: ANC, Antenatal Care; AR, Antiretroviral Therapy; CHI, Catastrophic Health Expenditure; FP, Family Planning; GBD2019, Global Burden Disease 2019; HIV/AIDS, Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome; IDs, Infectious diseases; NCDs, Non-communicable diseases; RMNC, Reproductive, Maternal, Neonatal and Child; SCA, Service Capacity and Access; SDGs, Sustainable Development Goals; UN, United Nations; UHC, Universal Health Coverage; WB, World Bank; WHO, World Health Organization
Introduction
Universal health coverage (UHC) is a multi-dimensional concept that includes population coverage, services coverage and financial protection as its building blocks, as well as equity and quality in its integrated definition [ 1 ]. Health policy and decision makers believe UHC as a foundation to improve population’s health, facilitate economic progress, and achieve social justice [ 2 , 3 ]. It is also essential to minimize disparities, promote effective and comprehensive health governance, and build resilient health systems [ 4 ].
The United Nation’s (UN) post-2015 goals described UHC as the predominant approach to realize the 2030’s sustainable health goals [ 5 ]. It is also taken as an urgent priority in 2020 UHC high-level meeting to address global health crises, through delivering affordable essential quality healthcare services, including the pandemic COVID-19 [ 6 ]. The UN General Assembly further declared, at its 73 rd session, that global institutions and countries make healthcare accessible to one billion more people by 2023 [ 7 ] and 80 percent of the population by 2030 with no catastrophic health expenditures [ 5 ].
WHO and the WB established core tracers of health service coverage to monitor UHC [ 8 ]. These tracers are categorized under the main theme reproductive, maternal, neonatal, and child health (RMNC), infectious diseases (IDs), non-communicable diseases (NCDs), and service capacity and access (SCA). Another dimension of UHC in SDG 3.8.2 is financial risk protection, which is typically measured by catastrophic health expenditure (CHE) and impoverishment due to healthcare costs [ 8 ].
While no prior studies have been conducted to identify and map the available evidence on UHC, other related studies such as “a synthesis of conceptual literature and global debates” [ 1 ] and a scoping review of “implementation research approaches of UHC” [ 9 ] are available. In addition to these literature, another study assessed the hegemonic nature of UHC in health policy described historical background of how UHC emerged, and frequency of UHC mentioned in all fields of articles available in PubMed database [ 10 ]. None of those previous studies addressed the universality of UHC in terms of its building blocks and service types and summarized the findings from each study included in the review.
A scoping review of the studies on UHC and its dimensions is crucial to map and characterize the existing studies towards UHC. This will help to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research [ 11 ]. The goals of this scoping review towards universality of UHC were, first, to determine the distribution of articles across WHO and WB regions, health service types, and dimensions including major components and tracer indicators, and second, to synthesize barriers of UHC. This review provides insight that is useful in setting strategies, evaluating health service performance, and advancing knowledge on priority research questions for future studies.
Identifying a research question
The protocol of this scoping review is available elsewhere https://doi.org/10.21203/rs.3.rs-1082468/v1 . The overall activities adhered to the Arksey and O’Malley’s (2005) scoping review framework [ 12 ], which was expanded with a methodological enhancement for scoping review projects [ 13 ], and the Joanna Briggs Institute framework [ 14 ]. The review followed five steps: (1) identifying research questions, (2) identifying relevant studies, (3) study selection, (4) data charting, and (5) collation, summarization, and reporting of results. The checklist Preferred Reporting Items for Systematic reviews and Meta-analysis extension for Scoping Reviews were used ( S1 Checklist ) [ 15 ].
The research questions were developed by AE in collaboration with YA. The Population, Concept, and Context framework was used to determine the eligibility of research questions [ 16 ]. According to the framework, the population represented study participants to whom findings infer which includes people at any age or other important characteristics of study participants. Not all UHC expected to have population component, which is non-applicable in some research. The concept was overall UHC or financial risk protection, equity, quality, and coverage. Context includes the study settings or countries and, in this review, the global context.
Identifying relevant studies
Web of Science, PubMed and Google Scholar were used to find literature in the field. Hand search was also used to find articles from WB Library, WHO Library, UN Digital Library Collections, and Google. Using the relevant keywords and/or phrases, a comprehensive search strategy was established. Universal, health, "health care", healthcare, "health service”, quality, access, coverage, equity, disparity, inequity, equality, inequality, expenditure, and cost were search words and/or phrases. “AND” or “OR” Boolean operators were used to broaden and narrow the specific search results. Search strings were formed in accordance with the need for databases ( S1 Table ). Article search date was between 20 October 2021 and 12 November 2021, with the most recent update on 03 March 2022. The articles were imported into EndNote desktop version x7, which was used to perform an automatic duplication check. Manual duplication removal was also performed. The database search strategies are shown in the ( S1 Table ).
Study selection
In consultation with YA, AE developed and tested study selection forms (inclusion and exclusion criteria) using a random sample from collected references, which were found using search strategy. A second meeting was held to approve the study screening form and process. Then, inclusion and exclusion criteria were applied during the article screening process for all articles. Studies conducted using the English language were included. Articles on overall UHC (UHC effective service coverage and FRP), UHC effective service coverage, UHC without specification with service coverage and FRP, and which reported coverage, quality, inequity, FRP in the outcome of the study or explored UHC research objectives were included. Types of study design included were quantitative, qualitative, mixed-research, and review types. The search was narrowed to include only literature published since 2015 to find studies which addressed the SDG target 3.8 and proceeding years. Non-English language literature, abstracts only, comments or letters to the editor, erratum, corrections, and brief communications were all excluded.
Articles’ titles, abstracts, and full texts were reviewed in stages. After duplicates were removed using EndNote desktop x7 software and manual duplication removal, titles were screened. After that, abstracts were used to screen the literature. Those who passed abstract review were eligible for full-text review. Full-text articles were also screened for data charting purposes. For articles with only an abstract, contact was made with the study’s corresponding authors.
Data charting
A piloted and refined data extraction tool was initially developed to chart the results of the review from full-text literature. Data was examined, charted, and sorted according to key issues and themes. Author(s), publication year, WHO geographic category, WB group, study approach, studied domain or topic, UHC themes, and health care service types were all extracted.
Collation, summarization, and report of results
Based on years of publication, studied dimensions (interrelated objectives), WHO region, WB group, study approach, and health care service types, available articles were compiled and summarized with frequency and percentage.
A simple descriptive analysis was performed, and the results were presented in the form of tables and figure. The data reporting scheme was adjusted as needed based on the findings.
Search results
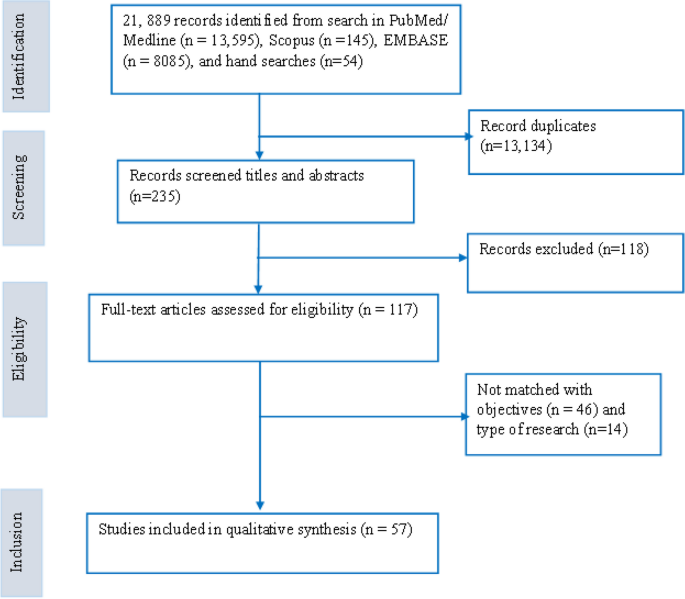
PubMed (n = 6,230) and Web of Science (n = 832) databases were searched. Google Scholar (n = 21), WB Library (n = 5), WHO Library (n = 7), UN Digital Library Collections (n = 13), and Google (n = 63) were also manually searched. A total of 7,171 records were discovered. Following title and abstract screening, 65 articles were chosen for full-text review. Finally, 47 articles were selected for scoping review ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0269507.g001
Articles characteristics
Almost one-fourth of articles were from WHO Africa region and another 25.5% were across two or more WHO regions. According to income category, 42.5% were from lower-middle-income countries followed by 29.8% across two or more WB economy groups. More than half of the articles (54.1%) followed a quantitative research approach ( Table 1 ). The countries where each article conducted are available in S2 Table .
https://doi.org/10.1371/journal.pone.0269507.t001
Health service types
Twenty articles [ 17 – 36 ] are categorized under health promotion. These articles were focused on pathways and efforts, program evaluation and change, opportunities and challenges, barriers/factors/enablers, community-based health planning and service initiative, perceived effect of health reform on UHC, health-seeking behaviour and knowledge, health security and health promotion activities, the impact of insurance on coverage, and SCA dimensions of UHC. Health promotion encompasses funding and infrastructure, health literacy, the development of healthy public policies, the creation of supportive environments, and the strengthening of community actions and skills, as well as any activities that assist governments, communities, and individuals in dealing with and addressing health challenges.
Six articles discussed treatment aspects of health services, which were access to care for illness, access to treatment for rheumatic heart diseases, neglected tropical diseases (NTDs), mental disorders and hypertension [ 37 – 42 ].
According to GBD-2019, WHO and WB tracers, FP and/or SCA components for promotion, immunization for prevention and other diseases in RMNC, IDs, NCDs for treatment aspects, nineteen articles were a combination of promotion, prevention, and treatment aspects [ 43 – 61 ].
One study looked at both the promotion and treatment of health services [ 62 ].
One study done on the quality of health care for disabled people [ 63 ] was classified as a palliative and rehabilitative care service type despite it did not adhere to palliative care assessment guidelines.
Components and dimensions of UHC
The main four components of UHC are RMNC, IDs, NCDs and SCA. Of included articles, RMNC was reported by 19 articles, 17 assessed NCDs were reported by 17 articles, CDs was assessed by 13 articles, and SCA was assessed by 9 articles. Regarding dimensions, coverage was assessed by 25 of articles; FRP by 13 articles, inequity by 10 articles and quality by 3 articles ( S2 Table ).
Tracer indicators for summary measure of UHC
Of 25 quantitative articles, 19 articles used various tracer indicators to assess UHC quantitatively; the remaining six quantitative articles assessed each empirical analysis of the potential impact of importing health services, access and financial protection of emergency cares, perceived availability and quality of care, the performance of district health systems, crude coverage and financial protection, health-seeking behaviour and OOP health expenditures, and the performance of health system.
Accessibility and affordability in China [ 64 ], as well as curative care and quality of care components in India [ 48 ] were developed as new tracers.
Ten tracers were used in RMNC component of UHC. Five tracers in IDs, seven tracers in SCA and 18 tracers were used NCDs component of UHC. Three tracers were used for FRP estimation. The iteration of tracers under four components of UHC effective service coverage and FRP is shown in Table 2 .
https://doi.org/10.1371/journal.pone.0269507.t002
Barriers/challenges of UHC
Policy, health sector and cross-cutting barriers of UHC were identified. Financing, leadership/governance, inequity, regulation and supervision mechanism, and poverty were most repeated policy level barriers. Poor quality health services and inadequate health workforce were the common barriers from health sector challenges. Lack of common understanding on UHC was frequently mentioned cross-cutting barriers ( Table 3 ).
https://doi.org/10.1371/journal.pone.0269507.t003
The purpose of this scoping review was to map existing research, and the most researched UHC dimensions, components and summarized main findings. Many articles were found in the African region and in countries with middle-income (lower and upper). Many of the studies followed a quantitative research approach. Palliative and rehabilitative health care types did not be well address in UHC research. The service coverage and financial protection dimensions were most frequently studied, followed by inequity and quality of health care services.
The current evidence found a greater number of articles than a scoping review of African implementation research of UHC [ 65 ]. This is because the former was conducted on a single continent and concentrated on UHC research approaches. Another bibliometric analysis, on the other hand, discovered a greater number of available evidence than the current scoping review [ 66 ]. Because it includes all available evidence as terminology, title, phrases, or words in policy documents, commentaries, editorials, and all frequency counts found in databases by the first search without the conditions of pre-established exclusion criteria. Aside from that, the bibliometric analysis included articles dating back to 1990. UHC is a global agenda that has improved the health of the global population through political support, funding, and active national and international collaborations [ 67 , 68 ]. The number of research output is likely increasing over time though current evidence shows that comparable numbers of articles are available in each year. An earlier bibliometric analysis discovered an increasing trend of UHC research outputs [ 66 ].
Many of the studies in this review used a quantitative approach. A prior scoping review conducted in Africa discovered that qualitative and mixed-methods studies were the commonest method to investigate UHC [ 10 ]. The former study did not consider financial protection research, UHC effective service and crude coverage, service capacity and access. UHC is intended to be quantified numerically as a summary index to track the progress of health care performance. Given the nature of UHC, fewer articles used qualitative research design to investigate its challenges, opportunities, and success of UHC. Various health systems and policies in low, middle, and high-income countries may present different barriers and facilitators to achieve UHC [ 69 – 71 ]. The current review has also identified policy, health system and cross-cutting barriers of UHC that were frequently explored by qualitative research.
Many number of countries are available in the European region and the high-income category [ 72 , 73 ]. In contrast, a substantial amount of UHC research was produced in middle-income countries, most were from African region. Trend analysis in health policy and systems research conducted on the overall research progress discovered that an increasing trend of publications in low-and middle-income countries between 2003 and 2009 [ 74 ]. This could be attributed to the nature of the health problems and the health policy in place regarding health research. Furthermore, health research budgets and clinical trial infrastructures may determine health research activities in each continent. Health budget might not always true in its effect of high research publication. For instance, evidence from a review finding indicated that nations with significant donor investment in health research may not necessarily produce a large number of research [ 75 ]. Articles available across WHO regions were comparable to frequency of articles in WHO African region. This might be due to UHC is a global strategy in monitoring the global process towards universal access to health care. The availability of UHC monitoring framework helps to conduct to conduct research at the multicounty level.
In 2019, the burden of NCDs was 63.8 percent worldwide, followed by IDs, RMNC, and nutritional disease (26.4 percent) [ 76 ]. In the summary measure of the UHC index, RMNC was the most frequently studied component followed by NCDs. This could be because many of the articles in the current review came from Africa and lower-and middle-income countries. In these countries, maternal and child morbidity and mortality were extremely high [ 77 ], making RMNC more likely to be investigated in UHC context. Similarly, a scoping review study on maternal, neonatal, and child health realized a high rate of publication in the most recent period [ 78 ].
This review provides an answer to the question of how much UHC is universal and how much UHC is covered in the current health systems and policy research. UHC tracer indicators are focused on health promotion, disease prevention, treatment, palliative, and rehabilitative health care services at the individual and population level. Promotion aspects of health services were more frequently investigated in the current review. This could be because those articles non-specific to either component of UHC were classified as health promotion. A single study was conducted on disabled population, close to palliative and rehabilitative health care types. Palliative care focuses on the physical, social, psychological, spiritual, and other issues confronting adults and children living with and dying from life-limiting conditions, as well as their families [ 79 ]. Assessment of pain and symptom management, functional status, psychosocial care, caregiver assessment, and quality of life are all part of a palliative care measurement and evaluation domains [ 80 ]. The Worldwide Hospice Palliative Care Alliance recommended research to improve palliative care coverage [ 81 ] in order to ensure equitable health care access for more than 40 million people who require palliative care each year worldwide [ 82 ]. However, UHC effective service coverage measurement indicators are appropriate only for assessing the promotion, prevention and treatment aspects of health care, even though all health care services are theoretically expected to be covered [ 54 ].
In terms of dimensions, coverage was more commonly studied. The framework for monitoring and tracking was initially established for effective service coverage and FRP. UHC’s service coverage is a collection of many individual disease indicators used to assess the performance of the health care system. Therefore, it is not surprising that many articles have been written about the coverage dimension. Aside from the usual trend of calculating the service coverage summary index, a few articles estimated UHC by combining effective service coverage and FRP indicators. In the current review, a few studies assessed the quality of care as a dimension of UHC; a single study developed a distinct quality of care measurement that integrated into the UHC matrix. Effective service coverage is predicated on the assumption that those in need receive high-quality health care services. Effective services coverage and quality are theoretically integrated. However, having a high UHC index value does not imply that high-quality care is provided for each specific disease. For example, in countries with high UHC index value [ 54 ], quality medical care services were found to be inadequate for patients with chronic diseases [ 83 ]. Quality of health care can be assessed using structure, process, and outcome indicators in the healthcare system [ 84 ].Therefore, generally, measuring the quality of care for specific disease is helpful for stakeholders, clinicians, and health policymakers working on specific health problems [ 85 ].
The UHC summary index is also useful in comparing the national and subnational progress of health system performance between countries and within a specific country. One of UHC’s primary functions is to promote health equity [ 3 ], and equity has been identified as a measurable component of UHC [ 86 ]. It is linked to social determinants that should be monitored over time, across or within different settings and populations [ 87 ]. Inequity in UHC service coverage studies was reported broadly. None of the UHC articles examined health disparities based on age, gender, race or ethnicity, residence, education level, or socioeconomic status. Moreover, range, absolute or relative difference, concentration index, and Gini coefficient were not used as equity measurement techniques in the included articles.
As implication to policy/program manager and researcher, more research is needed in settings where UHC has not been thoroughly investigated qualitatively. Future research better focus on the quality and equity dimension of UHC health care services. Given that the distinct nature of UHC tracers may limit UHC’s articles on health promotion, prevention, and treatment aspects, palliative and rehabilitative care services require attention in the future research environment. For specific health problems, additional review may be required to identify research gaps in specific tracer.
Strength and limitation
This is the first scoping review of UHC, and it is accompanied by the most recent articles. Our review identified UHC literature in each category of health service type.
In terms of limitations, this review included only articles conducted in English; articles conducted in other languages may have been missed, and geographical representation of UHC articles may have been over or underestimated for regions. When considering UHC dimensions, they may have a different level of research articles discovered if another mapping review is done for specific disease types.
Most articles were from Africa, across WHO regions and middle-income countries. Quantitative research approach has been frequently used. Equity and quality of services have got little attention in UHC research. Palliation and rehabilitation health services have also got little attention in the UHC research. Tracer indicators other than WHO and WB were developed and utilized in different countries. Policy, health sector and cross-cutting barriers of UHC were identified. Financing, leadership/governance, inequity, regulation and supervision mechanism, and poverty were most repeated policy level barriers. Poor quality health services and inadequate health workforce were the common challenges of the health sector towards UHC. Lack of common understanding on UHC was frequently mentioned as cross-cutting barrier.
Supporting information
S1 checklist. items followed in conducting this review..
https://doi.org/10.1371/journal.pone.0269507.s001
S1 Table. Search strategy.
https://doi.org/10.1371/journal.pone.0269507.s002
S2 Table. Articles’ country and main findings.
https://doi.org/10.1371/journal.pone.0269507.s003
- View Article
- PubMed/NCBI
- Google Scholar
- 6. uhc 2030. State of commitment to universal health coverage: synthesis, 2020 2020 Available from: https://www.uhc2030.org/blog-news-events/uhc2030-news/state-of-commitment-to-universal-health-coverage-synthesis-2020-555434/ .
- 16. The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual: 2014 edition/supplement. Australia: The Joanna Briggs Institute.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Universal healthcare in the united states of america: a healthy debate.

1. Introduction
2. argument against universal healthcare, 3. argument for universal healthcare, preventive initiatives within a universal healthcare model, 4. conclusions, author contributions, conflicts of interest.
- NBC News/Wall Street Journal Survey ; Study #19175; Hart Research Associates/Public Opinion Strategies: New York, NY, USA, 2019.
- WHO. Universal Health Coverage. Available online: https://www.who.int/healthsystems/universal_health_coverage/en/ (accessed on 2 October 2020).
- Light, D.W. Universal health care: Lessons from the British experience. Am. J. Public Health 2003 , 93 , 25–30. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chernichovsky, D.; Leibowitz, A.A. Integrating public health and personal care in a reformed US health care system. Am. J. Public Health 2010 , 100 , 205–211. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Unger, J.P.; De Paepe, P. Commercial Health Care Financing: The Cause of U.S., Dutch, and Swiss Health Systems Inefficiency? Int. J. Health Serv. 2019 , 49 , 431–456. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Country Rankings: World & Global Economy Rankings on Economic Freedom. Available online: https://www.heritage.org/index/ranking (accessed on 29 September 2020).
- Economic Freedom of the World. Cato Institute. Available online: https://www.cato.org/economic-freedom-world (accessed on 29 September 2020).
- Disparities|Healthy People 2020. Available online: https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities (accessed on 17 January 2020).
- Fuchs, V.R. How and why US health care differs from that in other OECD countries. JAMA J. Am. Med. Assoc. 2013 , 309 , 33–34. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Blahous, C.; Fish, J.; Smith, L.F.; Strategist, S.R. The Costs of a National Single-Payer Healthcare System. 2018. Available online: https://www.mercatus.org/publications/federal-fiscal-policy/costs (accessed on 8 January 2020).
- Daniels, M.; Panetta, L.; Penny, T. Primary Care: Estimating Democratic Candidates’ Health Plans ; Committee for a Responsible Federal Budget: Washington, DC, USA, 2020. [ Google Scholar ]
- Sessions, S.Y.; Lee, P.R. A road map for universal coverage: Finding a pass through the financial mountains. J. Health Polit. Policy Law 2008 , 33 , 155–197. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sanders, B. Options to Finance Medicare for All. 2020. Available online: https://www.sanders.senate.gov/download/options-to-finance-medicare-for-all?inline=file (accessed on 8 January 2020).
- Thorpe, K.E. An Analysis of Senator Sanders Single Payer Plan. 2016. Available online: https://berniesanders.com/issues/ (accessed on 8 January 2020).
- Skocpol, T. Boomerang: Health Care Reform and the Turn Against Government ; Norton: New York, NY, USA, 1997; pp. 133–143. [ Google Scholar ]
- Podemska-Mikluch, M. Understanding Medicare’s Impact on Innovation: A Framework for Policy Reform. 2018. Available online: https://www.mercatus.org/publications (accessed on 2 October 2020).
- Barua, B. Waiting Your Turn: Wait Times for Health Care in Canada, 2017 Report ; Fraser Institute: Vancouver, CO, Canada, 2016. [ Google Scholar ]
- Arguing for Universal HealtH Coverage ; World Health Organization: Geneva, Switzerland, 2013.
- A Vision for Primary Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals ; UNICEF, World Health Organization: Geneva, Switzerland, 2020.
- Crowley, R.; Daniel, H.; Cooney, T.G.; Engel, L.S. Envisioning a better U.S. health care system for all: Coverage and cost of care. Ann. Intern. Med. 2020 , 172 , S7–S32. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Doherty, R.; Cooney, T.G.; Mire, R.D.; Engel, L.S.; Goldman, J.M. Envisioning a Better U.S. Health Care System for All: A Call to Action by the American College of Physicians. Ann. Intern. Med. 2020 , 172 , S3. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ward, B.W.; Schiller, J.S.; Goodman, R.A. Multiple chronic conditions among US adults: A 2012 update. Prev. Chronic Dis. 2014 , 11 , E62. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Fryar, C.D.; Chen, T.-C.; Li, X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief 2012 , 1–8. Available online: http://www.ncbi.nlm.nih.gov/pubmed/23101933 (accessed on 13 March 2020).
- Pampel, F.C.; Krueger, P.M.; Denney, J.T. Socioeconomic Disparities in Health Behaviors. Annu. Rev. Sociol. 2010 , 36 , 349–370. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- U.S. Department of Health & Human Services. Office of the Assistant Secretary for Planning and Evaluation Value of Health Insurance: Few of the Uninsured Have Adequate Resources to Pay Potential Hospital Bills|ASPE . Available online: https://aspe.hhs.gov/basic-report/value-health-insurance-few-uninsured-have-adequate-resources-pay-potential-hospital-bills (accessed on 13 March 2020).
- McBride, T.D. Uninsured spells of the poor: Prevalence and duration. Health Care Financ. Rev. 1997 , 19 , 145–160. [ Google Scholar ]
- Saydah, S.H.; Imperatore, G.; Beckles, G.L. Socioeconomic status and mortality: Contribution of health care access and psychological distress among U.S. adults with diagnosed diabetes. Diabetes Care 2013 , 36 , 49–55. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2012. Diabetes Care 2013 , 36 , 1033–1046. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012 , 380 , 2224–2260. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension: A meta-analysis. J. Hypertens. 2015 . [ Google Scholar ] [ CrossRef ]
- Kirkland, E.B.; Heincelman, M.; Bishu, K.G.; Schumann, S.O.; Schreiner, A.; Axon, R.N.; Mauldin, P.D.; Moran, W.P. Trends in healthcare expenditures among US adults with hypertension: National estimates, 2003–2014. J. Am. Heart Assoc. 2018 . [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Bhurosy, T.; Jeewon, R. Overweight and obesity epidemic in developing countries: A problem with diet, physical activity, or socioeconomic status? Sci. World J. 2014 , 2014 , 964236. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Hammond, R.A.; Levine, R. The economic impact of obesity in the United States. Diabetes Metab. Syndr. Obes. 2010 , 3 , 285–295. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Clark, G.; O’Dwyer, M.; Chapman, Y.; Rolfe, B. An Ounce of Prevention is Worth a Pound of Cure-Universal Health Coverage to Strengthen Health Security. Asia Pac. Policy Stud. 2018 , 5 , 155–164. [ Google Scholar ] [ CrossRef ]
- A Better-Quality Alternative: Single-Payer National Health System Reform|Physicians for a National Health Program. Available online: https://www.pnhp.org/publications/a_better_quality_alternative.php?page=all (accessed on 7 October 2020).
- Fielding, J.E.; Teutsch, S.; Koh, H. Health reform and healthy people initiative. Am. J. Public Health 2012 , 102 , 30–33. [ Google Scholar ] [ CrossRef ]
- CDC The Power of Prevention. 2009. Available online: https://www.cdc.gov/chronicdisease/pdf/2009-power-of-prevention.pdf (accessed on 11 May 2020).
- Levi, J.; Segal, L.; Juliano, C. Issue Report: Prevention for a Healthier America: Investments in Disease Prevention Yield Significant Savings, Stronger Communities ; Trust for America’s Health: Washington, DC, USA, 2009. [ Google Scholar ]
- Lee, B.Y.; Adam, A.; Zenkov, E.; Hertenstein, D.; Ferguson, M.C.; Wang, P.I.; Wong, M.S.; Wedlock, P.; Nyathi, S.; Gittelsohn, J.; et al. Modeling the economic and health impact of increasing children’s physical activity in the United States. Health Aff. 2017 . [ Google Scholar ] [ CrossRef ]
- Hamasaki, H. Daily physical activity and type 2 diabetes: A review. World J. Diabetes 2016 . [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Magnussen, J.; Vrangbaek, K.; Saltman, R.B. Nordic Health Care Systems Recent Reforms and Current Policy Challenges Nordic Health Care Systems. Eur. Obs. Heal. Syst. Policies Ser. 2009 . [ Google Scholar ] [ CrossRef ]
- Fullman, N.; Yearwood, J.; Abay, S.M.; Abbafati, C.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; Abebe, Z.; Abebo, T.A.; Aboyans, V.; et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: A systematic analysis from the Global Burden of Disease Study 2016. Lancet 2018 . [ Google Scholar ] [ CrossRef ]
- Blumenthal, D.; Abrams, M.; Nuzum, R. The Affordable Care Act at 5 Years. N. Engl. J. Med. 2015 , 372 , 2451–2458. [ Google Scholar ] [ CrossRef ] [ Green Version ]
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Zieff, G.; Kerr, Z.Y.; Moore, J.B.; Stoner, L. Universal Healthcare in the United States of America: A Healthy Debate. Medicina 2020 , 56 , 580. https://doi.org/10.3390/medicina56110580
Zieff G, Kerr ZY, Moore JB, Stoner L. Universal Healthcare in the United States of America: A Healthy Debate. Medicina . 2020; 56(11):580. https://doi.org/10.3390/medicina56110580
Zieff, Gabriel, Zachary Y. Kerr, Justin B. Moore, and Lee Stoner. 2020. "Universal Healthcare in the United States of America: A Healthy Debate" Medicina 56, no. 11: 580. https://doi.org/10.3390/medicina56110580
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 04 January 2024
Building a resilient health system for universal health coverage and health security: a systematic review
- Ayal Debie ORCID: orcid.org/0000-0002-5596-8401 1 , 4 ,
- Adane Nigusie 2 ,
- Dereje Gedle 3 ,
- Resham B. Khatri 3 &
- Yibeltal Assefa 3
Global Health Research and Policy volume 9 , Article number: 2 ( 2024 ) Cite this article
3652 Accesses
3 Citations
5 Altmetric
Metrics details
Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security.
A systematic search was conducted including studies published from 01 January 2000 to 31 December 2021. Studies were searched in three databases (PubMed, Embase, and Scopus) using search terms under four domains: resilience, health system, universal health coverage, and health security. We critically appraised articles using Rees and colleagues’ quality appraisal checklist to assess the quality of papers. A systematic narrative synthesis was conducted to analyse and synthesise the data using the World Health Organization’s health systems building block framework.
A total of 57 articles were included in the final review. Context-based redistribution of health workers, task-shifting policy, and results-based health financing policy helped to build RHS. High political commitment, community-based response planning, and multi-sectorial collaboration were critical to realising UHC and health security. On the contrary, lack of access, non-responsive, inequitable healthcare services, poor surveillance, weak leadership, and income inequalities were the constraints to achieving UHC and health security. In addition, the lack of basic healthcare infrastructures, inadequately skilled health workforces, absence of clear government policy, lack of clarity of stakeholder roles, and uneven distribution of health facilities and health workers were the challenges to achieving UHC and health security.
Conclusions
Advanced healthcare infrastructures and adequate number of healthcare workers are essential to achieving UHC and health security. However, they are not alone adequate to protect the health system from potential failure. Context-specific redistribution of health workers, task-shifting, result-based health financing policies, and integrated and multi-sectoral approaches, based on the principles of primary health care, are necessary for building RHS toward UHC and health security.
Resilient health system (RHS) is essential to ensure universal health coverage (UHC) and health security. It is about the health system’s preparedness and response to severe and acute shocks, and how the system can absorb, adapt and transform to cope with such changes [ 1 , 2 ]. Resilient health system reflects the ability to continue service delivery despite extraordinary shocks to achieving UHC [ 3 ]. A study in Nepal showed that adoption of coexistence strategy on the continuation of the international community on strengthening the health sector with the principle of “do-no-harm” and impartiality at the time of conflicts improve the health outcomes [ 4 ].
In 2015, the United Nations (UN) General Assembly adopted a new development agenda aiming to transform the world by achieving the Sustainable Development Goals (SDGs) by 2030 [ 5 ], based on the lessons from the Millennium Development Goals (MDGs) [ 6 ]. The SDGs seek to tackle the “unfinished business” of the MDGs era and recognise that health is a major contributor and beneficiary of sustainable development policies [ 7 ]. One of the 17 goals has been devoted specifically to health: “ensure healthy lives and promote well-being for all ages” [ 6 ]. All UN Member States have agreed to achieve UHC (target 3.8) by 2030, as part of the SDGs [ 8 ]. The 2030 UHC target was intended to reach at least 80% for the UHC service coverage index and 100% for financial protection [ 9 ]. Universal health coverage is achieved when everyone has access to essential healthcare services without financial hardship associated with paying for care [ 10 ].
Universal health coverage and health security are two sides of the same coin. They are interconnected and complementary goals that require strong health systems and public health infrastructure to ensure that everyone has access to essential health services [ 11 ]. Universal health coverage and health security require an integrated and multi-sectorial system strengthening to provide quality and equitable healthcare services across populations [ 12 ].
A resilient health system provides the foundation for both [ 11 ]. Strengthening the World Health Organisation’s (WHO’s) six health system building blocks, including service delivery, health workforce, health information systems, health financing, leadership and governance, and access to essential medicines and infrastructures are essential to achieve UHC and health security [ 13 ]. The 13th WHO programme is structured in three interconnected strategic priorities to ensure SDG-3 including: achieving UHC, addressing health emergencies, and promoting healthier populations [ 14 ].
In the World Health Organisation (WHO) European Region, health security emphasises on the analysis of infectious diseases, natural and human-made disasters, conflicts and complex emergencies, and potential future challenges from global changes, particularly climate change [ 15 ]. Health security is also considered as the activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries [ 16 ]. The links between health system and health security have started to emerge in several national strategic plans and global initiatives, such as the Global Health Security Agenda (GHSA) and One Health, which aim to better facilitate the implementation of the International Health Regulations (IHR) [ 17 ]. The aim of IHR is to prevent, detect, and respond to the international spread of disease in effective and efficient manner [ 18 ]. The GHSA also help countries to build their capacity to prevent, detect, and respond to infectious disease threats [ 19 ].
Although almost all nations are progressing towards UHC, the advancement in low and low-middle income countries (LLMICs) is slow [ 20 ]. This is because the ethos and organisations of many health systems are more suitable for yesterday’s disease burden than tomorrow [ 21 , 22 ]. Health systems of various nations faced numerous shocks, including public health, social, economic and political crises associated with COVID-19 [ 23 ]. The COVID -19 pandemic has made an unprecedented impact on the international community and exposed the vulnerabilities of the present global health architecture [ 24 ]. The COVID-19 pandemic is a perfect reminder that countries, individually and collectively, require a strong RHS now more than ever; however, there was no adequate evidence on the strategies toward RHS to improving UHC and health security. Thus, this study can inform the global health community on the lessons of RHS and its applications to UHC in pandemic and beyond. This review generally aimed to address the following research questions: 1) What are the existing evidence on the impact of RHS for UHC and health security? 2) What are the essential elements and characteristics of RHS for UHC and health security as per the WHO building blocks? and 3) What examples exist to demonstrate on how to build RHS core components for UHC and health security?
Registration and search strategy
This review was conducted and reported following enhancing transparency in reporting the synthesis of qualitative research (ENTERQ). Following ENTERQ guidelines, the systematic review was registered with the international prospective register of systematic reviews (PROSPERO) on 02 January 2022 with registration: CRD42020210471. Studies were searched in three databases (PubMed, Embase and Scopus) using search terms of under four broader domains, including resilience, health system, universal health coverage, and health security. Additional literatures were identified by searching in Google and Google Scholar. The search strategies were built using the four domains of search terms, and “Title/Abstract” by linking “AND” and “OR” Boolean operator terms as appropriate (Additional file 1 ). We also used the ENTERQ checklist for reporting the articles (Additional file 2 ).
Inclusion and exclusion criteria
All articles in relation to RHS towards UHC and health security were included in the review. Inclusion criteria were articles written in the English language published from 01 January 2000 to 31 December 2021. Qualitative, quantitative, and mixed methods studies were eligible for inclusion. Exclusion criteria were perspectives, commentary, expert’s opinion, conference papers, debates, conference reports, letters to the editor, and editorials. We presented this paper as a narrative review, following some components of the preferred reporting of systematic review and meta-analysis (PRISMA) guideline for scoping review (Additional file 3 ).
Selection process
The primary author (AD) imported all retrieved articles into the Endnote library to remove duplicates. After removing the duplicates, three authors (AD, AN and DG) independently screened the articles by title and abstract based on inclusion criteria. The senior authors (RBK and YA) mediated the discrepancies between the three reviewers through discussion. Finally, we retained and reviewed the full texts of all relevant studies for final data synthesis.
Data extraction and framework for synthesis
We used the Rees and colleagues’ appraisal instrument as a guiding tool to appraise the quality of included articles in the review [ 25 ]. The quality appraisal instrument is a comprehensive tool designed to assess the quality, rigor of research studies, covers key aspects of research design, data collection, analysis, and reporting. This includes rigour in sampling, rigour in data collection, rigour in data analysis, findings supported by the data, breadth and depth of findings, extent of the study privilege perspectives, reliability or trustworthiness, and usefulness[ 25 ]. A template was developed to extract relevant data from each eligible study. After reading the selected studies, key findings were extracted into the template, including information about the first author, year of publication, type of article, study design, and key summary findings. Three independent reviewers (AD, AN and DG) extracted the data. The senior authors (RBK and YA) verified the extracted information. The successes and challenges of RHS for UHC and health security were extracted using health system building blocks.
We analysed the findings using the WHO health system building blocks, including service delivery, health workforce, health information systems, medicines and infrastructures, healthcare financing, and leadership and governance [ 13 ]. We analysed the key challenges and successes of RHS for UHC and health security using the WHO health system frameworks. Framework analysis provides a systematic approach to analysing large amounts of textual data using pre-determined framework components. This allows the analyst and those commissioning the research to move between multiple layers of abstraction without losing sight of raw data [ 26 ].
Search results
A total of 21,889 records were identified in the initial literature search. After removing 13,134 duplicates, 235 articles were screened by titles and abstracts, and 118 were excluded. Next, 117 studies were reviewed using the full texts, and finally, 57 articles met the inclusion criteria and were analyzed in the systematic review (Fig. 1 ). Of these, 32 articles were primary studies, and 25 articles investigated the application of RHS on UHC. In addition, nine articles explained RHS's implications on UHC and health security. Of these, approximately one-third (19 articles) were conducted in various African nations, while 19 articles were from Asian countries. The remaining articles were from other parts of the world. The study also reviewed articles on various aspects of health system building blocks, including health service delivery, health workforce, health information systems, health financing, leadership/governance, and medicines and infrastructure. The number of articles reviewed for each aspect were 17, 9, 10, 13, 22, and 10, respectively.
ENTREQ flow diagram for the articles included in the review
Successes and challenges of RHS
This review used the six-health system building blocks to achieve UHC and health security. These include service delivery, health workforce, health information system, health financing, medicines, diagnostics and infrastructures, and leadership and governance (Table 1 ).
Service delivery
Of the total reviewed articles, 17 described their healthcare service delivery findings. Good service delivery provides comprehensive and person-centered healthcare services with full accountability [ 27 ]. Continuation of healthcare service delivery in the face of extraordinary shocks facilitated UHC progress [ 3 ]. Studies reported that health service inputs, access to transportation, communication infrastructures, capacity building, referral systems, intersectoral actions, and electronic healthcare platforms could facilitate service delivery and improve access to health services [ 13 , 28 ]. Operational integration between health service continuity and emergency response through proactive planning across all income nations reduced health services disruptions during emergencies [ 29 ]. Community resources, cohesion, and physical accesses were significant assets to improve service utilisation and quality [ 30 ].
An inward migration or mass casualty incidents compromised the quality of services and increased deaths attributed to delays in treatment [ 30 ]. In the Ebola crisis, the long-standing lack of access to basic primary health care to isolate and treat infected people fueled the epidemic’s spread resulting in a death toll [ 31 ]. Uneven health facilities distribution and lack of well-trained personnel and supplies led to geographical inequities and poor healthcare access [ 32 , 33 ]. A combination of public health security threats, both new and reemerging infectious diseases, challenged ensuring health security [ 34 ]. For example, the health service delivery, mainly the lives of many children, was at risk associated with the lack of treatment for common childhood illnesses in Liberia during the Ebola outbreak [ 35 , 36 ]. Exclusion from work due to health problems can easily result in economic impoverishment and inequitable healthcare access, which will undoubtedly worsen health status [ 37 ]. For instance, socially excluded population groups received health services from a dysfunctional publicly provided health system marked by gaps and often invisible barriers in Guatemala and Peru, which undermines the progress towards UHC [ 38 ]. The changes in frequency, intensity, spatial extent, duration, and timing of extreme weather and climate events were also exposed to health threats [ 39 ]. For example, extreme weather events caused an increase in disease prevalence, such as malaria and other vector-borne diseases, malnutrition, food insecurity and food-borne diseases [ 40 ]. Inadequate primary health care system capacity to provide responsive health services to storm and flood-related health problems was another challenge [ 41 ].
Health workforce
In our review, nine articles reported their findings on the successes and challenges of health workforces towards UHC and health security. A well-performing health workforce provides responsive, fair and efficient health services to achieve the best health outcomes [ 27 ]. Task-shifting policy, ensuring accountability and ad hoc redistribution of health workers had a knock-on effect on health services delivery and building RHS [ 42 , 43 , 44 ]. Training on disaster preparedness and management, and rewarding packages, such as incentives and hazard allowance, facilitated healthcare workers willing to participate in disaster management [ 45 ]. Monitoring and evaluating frontline health workers levels of preparedness against public health emergency threats periodically by their higher-level hierarchy was crucial for early detection and control of health threats [ 46 ].
Lack of skilled and inadequate health workforce distribution was the major obstacle to containing an outbreak, and deaths were attributed to treatment delays [ 35 , 43 ]. Low perception of risks by tourists/ pilgrims, ineffective training, poor control of risk factors, and shortages of infrastructures were the challenges in combating contagious diseases [ 47 ]. Healthcare workers’ practices on effective pandemic management, including corona-virus disease (COVID)-19 were constrained by individual factors, such as education, residence, work station location, hygiene promotion, and social distance management [ 42 ]. Patient assessments by non-indigenous health workers during an emergency were also barriers to early identification and management of acute health events [ 30 ].
Health information system
In this review, ten articles described the contributions and challenges of health information on RHS to realise UHC and health security. A well-functioning HIS ensures the production, analysis, dissemination and use of reliable information for policy decisions [ 27 ]. Building accountability, knowledge culture management, and evidence through regular data quality audit strengthened health management information systems (HMIS) [ 44 ]. Integrated disease surveillance, flexible automation and data processing improved clinical care and health system preparedness to tackle health threats [ 48 , 49 , 50 ]. Strengthening the health system’s capacity was another key measure to rapidly process and communicate test results for pandemic responses [ 51 ].
Poor surveillance, late timing of responses and lack of triggers weakened the functionality of plans and exposed to a high burden of diseases [ 52 ]. Poor data management, misinformation on the risk and transmission, lack of awareness, resources and insufficient electronic reporting system were responsible for the spread of diseases [ 51 , 53 , 54 ]. For instance, misinformation during the Ebola outbreak affected most communities in putting measures in place to stop the spread of the virus [ 54 ]. People approached traditional healers who lacked knowledge on treating certain health shocks in modern medicine was the major problems in early responses [ 35 ].
Medical products, diagnostics, and infrastructures
Of the reviewed articles, 10 reported their findings on the successes and constraints of medical products, diagnostics, and infrastructures to realise UHC and health security. Equitable access to essential medical products, vaccines and technologies to assure quality, safety, efficacy and cost-effective healthcare services to users was the attribute of a well-functioning health system [ 27 ]. To attain UHC, strengthening local preparedness, planning, manufacturing, and coordinating public–private initiatives and training in LMICs was important [ 55 ]. The key factors to facilitate early detection were the provision of rapid, cost-effective, sensitive, and specific diagnostic centers through the inauguration of national centers [ 53 , 56 ]. Identifying emergency medicines, adaptable mobile health care units and systems for mobilisation of health professionals contributed to successful interventions to curb health emergencies [ 57 ].
High patient load, lack of diagnostics, destruction of health facilities and lack of specific funds for medicine procurement may compromise the health system’s hardware (health facilities and supplies) and contained public health threats [ 3 , 30 , 32 , 57 ]. For instance, inadequate essential logistics such as blood, oxygen cylinders, ergometrine and sulphadoxine paramita mine in Ghana was the causes for low level of preparedness to control maternal mortality [ 58 ]. Shortages of medical supplies, personal protective equipment (PPE), and electricity increased the rate of Ebola infections during the outbreak [ 35 ]. Most medicine outlets experienced longer lead times associated with the poor inter-country transportation and limited manufacturing capacity, which were also Namibia's main challenges [ 55 ].
Health financing
In this study, 13 articles described their findings on the contributions and limitations of healthcare financing to realise UHC and health security. A good health financing system raised adequate funds for health to ensure people can use needed services and be protected from financial catastrophes [ 27 ]. Under a publicly funded health financing system that fits well with values and population preferences improved compliance, sustainability, and equity [ 59 ]. An integrated financing mechanism through high income and risk cross-subsidies reduced reliance on OOP payments, maximises risk pools and resource allocation mechanisms facilitated to achieve UHC [ 60 ]. Universal health coverage can substantially improve human security through securing finances [ 61 ]. Universal health coverage indicators were also positively associated with the gross domestic product (GDP) per capita and the share of health spending channels [ 62 ]. Income redistribution improved equity in health care service delivery [ 63 ].
Lack of adequate funds and non-affordable medical costs were the main barriers to universal financial protection and poor management of an outbreak [ 33 , 35 ]. In Burundi, for example, performance-based financing without accompanying access to incentives for the poor was the critical challenge to improve equity in health [ 64 ]. Health equity advancement challenges secured dedicated funds to support transformative learning opportunities and build infrastructures [ 65 ]. Because of causalities, the health sector requires additional financial support to address the increased demand for health services; however, movement restrictions limit people’s access to participate in gainful activities [ 30 ]. Low funds from international donors were erratic and far below the amounts required to meet the health needs at crisis time [ 66 ]. People could not trade their commodities because of the fear of attacks exposing service users to lack finances [ 30 ]. Falling in financial access to health services has resulted in political demonstrations and violent unrest [ 67 ].
Leadership and governance
Our review found that 22 articles reported their findings on health system governance (HSG) to realise UHC and health security. Good HSG ensured strategic policy frameworks combined with effective oversight, coalition, appropriate regulations, system design and accountability [ 27 ]. Building strong partnerships, ensuring accountability, coordination, rationalisation, and connection of pandemic planning across sectors and jurisdictions resulted in better preparedness [ 48 , 68 ]. Clear communication channels, multisectoral, and multilevel controls were essential to translate policy into actions [ 52 , 56 ]. Vertical and horizontal integration, centralised governance, responsible leadership, and social capital at community level were needed to address health shocks and homogenous implementation of health interventions [ 54 , 69 , 70 ]. Fueling high-performing teams and increasing investment in early warning and detection systems required leadership resilience to enable action at all levels [ 71 , 72 ].
Working alone the state had proven only partially effective, a situation exacerbated by the natural tendency within the public to ignore as irrelevant to themselves [ 73 ]. In addition, lack of clarity of stakeholder roles, poor leadership and absence of clear government policy for the delivery channels and financial coverage led to fragmentation and poor health system response [ 35 , 52 , 66 ]. For instance, weak governance and decision-making processes, such as high bureaucracy, low prevention culture, and lack of coordination between primary, social and hospital care providers, indicated virus’s rapid spread in the French population in the first wave of COVID-19 [ 74 ].
Moving away from a one-size fits-to all approach in guiding pandemic response, service delivery, political commitment, fair contribution and distribution of resources are helpful to speed up the path towards UHC [ 75 ]. For example, village health volunteers in Thailand, Zanmi Lazante’s Community Health Program in Haiti, Agentes Polivalentes Elementares in Mozambique, Village Health Teams in Uganda, lady health workers in Pakistan, BRAC in Bangladesh, Family Health Program in Brazil, and Health Extension Program in Ethiopia are successful community-based models contributed immensely to achieve health development goals [ 76 ]. In addition, community participation and coordination between different stakeholders significantly impact the prevention of encephalitis in Japan [ 77 ], and early detection of cases and collection of mortality data in Cambodia [ 78 ]. On the contrary, it was difficult for the system to automatically adjust its structure to reduce uncertainty and ascertain complex adaptive behaviour when facing public health emergencies [ 79 ].
With an overarching political will, well-integrated and locally grounded health system can be more resilient to external shocks [ 80 ]. Political leadership was critical during the crisis, which helped the government to develop a response strategy and effective implementation [ 81 ]. For instance, Singapore’s dexterous political environment allowed the government to institute measures to control COVID-19 swiftly [ 56 ]. On the other hand, political instability or war in Syria affected healthcare services by destroying physical health care infrastructures [ 3 ].
In this review, we developed a resilient health system framework that could assist countries in their endeavor toward universal health coverage and health security. The framework involves an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The input components of the framework include health financing, health workforce, and infrastructure, while service delivery is the process component, and UHC and health security are the impact program components. The framework also considers health system performance attributes, such as access, equity, quality, safety, efficiency, sustainability, responsiveness, and financial risk protection. Additionally, the cross-cutting components of the framework are leadership and governance, health information systems (HIS), and contextual factors (e.g., political, environmental/climate, socioeconomic, and community engagement) that can affect the health system at any stage of the program components (Fig. 2 ).

Resilient health system framework for UHC and health security
We also indicated that RHS is critical to achieving UHC because it enables the provision of accessible, quality, and equitable health services, while also protecting people from financial risks associated with illness or injury. Such systems are built on strong primary healthcare services, effective governance and leadership, adequate financing, reliable health information systems, and a well-trained and motivated health workforce [ 42 , 43 , 44 ]. Resilient health systems are better equipped to deliver high-quality healthcare services to all people, including those who are marginalised or living in poverty. This, in turn, investing in RHS is essential for achieving UHC, promoting health equity, and building more sustainable and equitable societies. On the contrary, lack of healthcare access, skilled health workforces, and uneven distribution of health facilities and health workers [ 32 , 33 , 35 , 43 ] were the challenges to achieving health sector goals.
Lack of access, non-responsive and inequitable healthcare services were the challenges to achieve UHC and health security [ 31 , 32 , 33 ]. Such challenges can be solved by primary health care approach which is an effective strategy to provide accessible, acceptable, equitable and affordable health services to achieve UHC [ 82 , 83 ]. Community-based and differentiated service delivery models are also important platforms for improving healthcare delivery, access, outcomes, and to meet the specific needs and preferences of different groups of patients [ 84 , 85 ]. Community-based service delivery model can bring healthcare services closer to where people live and work, and overcome barriers to healthcare access such as transportation, distance, and cost [ 84 ]. This service delivery model has also the potential to facilitate a more effective response during healthcare crises by minimising top-down approaches and maximising bottom-up strategies through empowering local communities to take ownership of their health and wellbeing [ 86 ]. Additionally, differentiated service delivery model can meet the specific needs and preferences of different groups of patients. For example, providing family planning services within HIV clinics helps women living with HIV to access both services at the same time [ 85 ]. Similarly, considering a health system away from a one-size-fits-all approach to healthcare delivery is essential in meeting the needs of diverse patient populations [ 87 ].
Lack of skilled and inadequate distribution of health workforces were another major obstacle to contain an outbreak and deaths attributed to delays in treatment [ 35 , 43 ]. Conducting integrated supportive supervision, maintenance of human resource information systems, and national task shifting policy are important strategies that can help to address critical health workforce gaps and maldistribution [ 42 , 44 ]. Healthcare workers' pre-service and in-service training opportunities are indeed key to providing quality care. Healthcare workers who receive adequate pre-service and in-service training are better equipped to provide quality care to patients, and also to adapt to new challenges and changing healthcare needs over time [ 88 ]. Training in disaster preparedness and offering rewarding packages can also play an essential role in enhancing the willingness of healthcare workers to participate in disaster management [ 45 ]. For instance, Kenya's Field Epidemiology and Laboratory Training Program (FELTP) has played a significant role in strengthening the capacity of healthcare workers to detect, document, respond, and report unusual health events [ 89 ]. In addition, monitoring frontline health levels is an essential part of preparedness against public health emergencies. This can involve monitoring healthcare facility capacities and the overall preparedness of the healthcare system to respond to an emergency [ 46 ].
Poor infrastructure, absence of emergency stockpiles, inadequate logistics, and shortages of medical supplies can be potential obstacles to achieving UHC during health emergencies [ 30 , 35 , 57 , 58 ]. A strong public health infrastructure can help to ensure that healthcare resources are distributed equitably, based on need rather than ability to pay. This is particularly important during a pandemic, when resources may be scarce and demand for healthcare services is high [ 90 ]. Integrating pharmaceutical supply chain activities with modern technologies and establishing strong relationships between manufacturers, distributors, prescribers, and insurance organizations can help ensure that essential supplies and logistics are available promptly [ 91 ]. Efficient procurement and an effective supply chain management system are essential components of a well-functioning healthcare system. They can help ensure that essential medicines, medical supplies, and equipment are available where and when they are needed, which is critical to achieving UHC and providing quality healthcare services to all individuals, regardless of their ability to pay [ 92 ].
The main challenges for universal financial protection were inadequate healthcare funds [ 35 ]. Context specific health financing mechanisms are essential to provide strong and sustainable health financing and move towards UHC [ 44 , 93 ]. Additionally, cross-subsidisation from rich to poor and low-risk to high-risk groups provide universal access for the entire population [ 94 ]. Similarly, reducing of health systems reliance on OOP payments and maximising risk pools were supportive to achieving UHC [ 60 ]. Universal health coverage can play a significant role in improving human security by providing financial protection against the cost of healthcare. In many countries, people face significant financial barriers to accessing healthcare services, and as a result, they may be forced to forgo necessary care or incur significant debt to pay for it. The example of Thailand is a good illustration of the potential benefits of UHC. Thailand implemented a comprehensive UHC program in the early 2000s, which provided coverage for all citizens and legal residents. Over the course of a decade, this program helped to reduce the annual impoverishment rate due to medical costs from 2.71% to 0.49% [ 61 ].
Poor leadership and absence of clear government policy led to fragmentation and poor health system response [ 35 , 66 ]. It is essential to involve a diverse range of stakeholders in pandemic preparedness and response efforts to ensure that a comprehensive and effective response is implemented. Collaborative efforts that include input from various stakeholders are more likely to lead to successful outcomes in mitigating the impact of a pandemic [ 73 , 95 ]. Good leadership is essential for effective outbreak response because it helps to coordinate and guide the efforts of different stakeholders, including health workers, community leaders, and government officials. A strong leader can help to build trust and confidence among the community, mobilise resources, and ensure that everyone is working together towards a common goal [ 54 ]. Health systems governance is essential for creating RHS that can respond to emerging health challenges, such as pandemics, as well as ongoing health concerns. By building strong partnerships and accountability mechanisms, health systems can better address the needs of individuals and communities, and improve overall health outcomes [ 48 ]. Cultivating bottom-up and top-down forms of accountability is also important to improve the quality and coverage of health services [ 96 ].
This study will provide an insight on RHS framework for achieving UHC and health security with an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The limitations of this review include that the study did not quantitatively estimate the extent of resilient health system for UHC and health security. This is because we used articles based on various quantitative, qualitative, and mixed methods. In addition, we used the Rees et al. appraisal instrument as a guiding framework for the eligibility criteria [ 25 ]. The Rees specifies some methodological criteria for diverse types of studies but does not have a cut-off point for excluding studies.
This review provides evidence of the successes and challenges of RHS and its impact on achieving UHC globally. The review will also give an insight into the key determinants of RHS to achieve long term health sector goals. It will raise health programmers’ awareness of the importance of RHS and initiate an idea for future discussion and arguments on the subject. The review will also help policymakers and government officials to revise and update their strategic plans and policy directions. This review will also assist policy makers in introducing accountability within public institutions to provide more inclusive and equitable health services without excluding any population groups to achieve UHC. This review will help policymakers to formulate an agreed core set of global and national indicators to improve their health systems performance. This review will also help future researchers as baseline information.
The aspiration for UHC and health security will be realised only through a RHS. Advanced healthcare infrastructures and adequate number of health care workers are essential to build a RHS; however, they are not adequate to protect the health systems from potential failures. The health system’s ideology, traditions in policymaking and management, orientation of service delivery, capacities, motivation, and morale of healthcare workers can affect the nation’s health system. Context-specific redistribution of health workers, task-shifting policy, and result-based health financing policy are helpful in building RHS. It is high time that countries transform their health systems through an integrated and multi-sectoral approach to serve as a road map to realise UHC and health security. We are also recommending for future research studies to focus on building a RHS that can support UHC and ensure health security. Such future studies shall be conducted at the national, regional and sub-regional levels to provide context-specific guidance.
Availability of data and materials
Not applicable.
Acknowledgements
The first author would like to acknowledge other authors for their contribution in searching, extracting, and writing this article. The first author would also extend his gratitude, particularly for the last two senior authors (RBK and YA), for their exceptional dedication in shaping this review.
Author information
Authors and affiliations.
Departement of Health Systems and Policy, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Departement of Health Education and Behavioral Sciences, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Adane Nigusie
School of Public Health, The University of Queensland, Brisbane, Australia
Dereje Gedle, Resham B. Khatri & Yibeltal Assefa
College of Medicine and Public Health, Flinders University, Adelaide, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation: AD and YA. Data curation: AD, AN and DG. Formal analysis: AD, AN, DG, RBK and YA. Methodology: AD, AN, DG, RBK and YA. Supervision: RBK and YA. Writing – original draft: AD. Writing – review & editing: AD, AN, DG, RBK and YA.
Corresponding author
Correspondence to Ayal Debie .
Ethics declarations
Ethics approval and consent to participate.
Ethical approvals were not required as the study was a systematic review of articles. The study was registered with PROSPERO number CRD42020210471.
Consent for publication
Competing interests.
All authors declared that they have no competing interest.
Supplementary Information
Additional file 1..
Search strategy.
Additional file 2.
ENTREQ checklist.
Additional file 3.
PRISMA-ScR checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Debie, A., Nigusie, A., Gedle, D. et al. Building a resilient health system for universal health coverage and health security: a systematic review. glob health res policy 9 , 2 (2024). https://doi.org/10.1186/s41256-023-00340-z
Download citation
Received : 31 March 2022
Accepted : 05 December 2023
Published : 04 January 2024
DOI : https://doi.org/10.1186/s41256-023-00340-z

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health security
Global Health Research and Policy
ISSN: 2397-0642
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 23 March 2023
Quality of care in the context of universal health coverage: a scoping review
- Bernice Yanful ORCID: orcid.org/0000-0002-6824-6694 1 ,
- Abirami Kirubarajan 2 ,
- Dominika Bhatia 2 ,
- Sujata Mishra 2 ,
- Sara Allin 2 &
- Erica Di Ruggiero 1 , 2 , 3
Health Research Policy and Systems volume 21 , Article number: 21 ( 2023 ) Cite this article
9118 Accesses
4 Citations
7 Altmetric
Metrics details
Introduction
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize the existing conceptual and empirical literature on quality of care within the context of UHC and identify knowledge gaps.
We conducted a scoping review using the Arksey and O’Malley framework and further elaborated by Levac et al. and applied the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines. We systematically searched MEDLINE, EMBASE, CINAHL-Plus, PAIS Index, ProQuest and PsycINFO for reviews published between 1 January 1995 and 27 September 2021. Reviews were eligible for inclusion if the article had a central focus on UHC and discussed quality of care. We did not apply any country-based restrictions. All screening, data extraction and analyses were completed by two reviewers.
Of the 4128 database results, we included 45 studies that met the eligibility criteria, spanning multiple geographic regions. We synthesized and analysed our findings according to Kruk et al.’s conceptual framework for high-quality systems, including foundations, processes of care and quality impacts. Discussions of governance in relation to quality of care were discussed in a high number of studies. Studies that explored the efficiency of health systems and services were also highly represented in the included reviews. In contrast, we found that limited information was reported on health outcomes in relation to quality of care within the context of UHC. In addition, there was a global lack of evidence on measures of quality of care related to UHC, particularly country-specific measures and measures related to equity.
There is growing evidence on the relationship between quality of care and UHC, especially related to the governance and efficiency of healthcare services and systems. However, several knowledge gaps remain, particularly related to monitoring and evaluation, including of equity. Further research, evaluation and monitoring frameworks are required to strengthen the existing evidence base to improve UHC.
Peer Review reports
According to the World Health Organization, universal health coverage (UHC) is achieved when ‘all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship’ [ 1 ]. UHC has gained renewed attention from researchers and policymakers following its inclusion in the 2030 Agenda for Sustainable Development (SDGs). SDG target 3.8 calls for achieving ‘universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all’ [ 2 ].
While there is growing evidence linking UHC to different health, economic and social outcomes, recent estimates suggest that about 800 million people globally still do not have access to full financial coverage of essential health services, including but not limited to high-income countries [ 3 ]. The WHO’s well-established UHC cube identifies three dimensions of UHC: (1) population (who is covered); (2) services (services that are covered); (3) direct costs (the proportion of the costs that are covered) [ 4 ]. Absent from the cube is the explicit inclusion of quality of care. However, without attention to the quality of care provided, increasing service coverage alone is unlikely to produce better health outcomes. As such, quality of care is critical to the achievement of UHC. A high-quality health system has been defined as one ‘that optimises health care in a given context by consistently delivering care that improves or maintains health outcomes, by being valued and trusted by all people, and by responding to changing population needs’ [ 5 , p. e1200].
Current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries (LMICs) [ 6 ]. While the era of the Millennium Development Goals (MDGs) expanded access to essential health services in LMICs, poor quality of care remains a significant problem, and explains persistently high levels of maternal and child mortality [ 6 ]. In addition, poor quality of care is estimated to cause between 5.7 and 8.4 million deaths yearly in LMICs [ 7 ]. Low-quality services are also an issue in high-income countries (HICs), particularly for disadvantaged populations such as immigrant and Indigenous groups [ 6 , 8 ].
As such, efforts to achieve UHC focused solely on expanding access to care are insufficient. Achieving UHC will require a more deliberate focus on quality of care across its various dimensions including effectiveness, safety, people-centredness, timeliness, equity, integration of care and efficiency [ 6 ]. However, existing literature synthesizing evidence on the quality of care within the context of UHC is more limited.
The primary objective of this scoping review is to synthesize and analyse the existing conceptual and empirical literature on quality of care within the context of UHC. The secondary objective is to identify knowledge gaps on quality of care within the context of advancing UHC and highlight areas for further inquiry.
We conducted a scoping review using the five-stage scoping review framework proposed by Arksey and O’Malley [ 9 ] and further elaborated by Levac et al. with the following stages [ 10 ]: (1) formulating the research question; (2) searching for relevant studies; (3) selection of eligible studies; (4) data extraction and (5) analysing and describing the results. In addition, we followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews reporting guidelines [ 11 ]. In accordance with the guidelines, our protocol is publicly available through Open Science Forum [ 12 ]. The scoping review methodology was selected due to its relevance to both identifying emerging and established content areas, and integration of diverse study methodologies [ 13 ]. As such, our methodology was well-aligned with the exploratory aims of our study.
To synthesize the existing knowledge on quality of care within the context of UHC, we focused on retrieving and analysing relevant reviews (as opposed to primary research studies). Bennett et al. [ 14 ] applied this overview of reviews approach in identifying health policy and system research priorities for the SDGs.
Information sources and search strategy
We developed the search strategy in consultation with a research librarian with expertise in public health and health systems. After finalizing our search in MEDLINE (Ovid) through an iterative process involving pilot tests, we completed a systematic search of MEDLINE (Ovid), EMBASE (Ovid), CINAHL-Plus (EBSCO), PAIS Index, ProQuest and PsycINFO (Ovid) for articles published from 1 January 1995 to 27 September 2021. The date cut-off of 1995 was selected to capture articles published during the period leading up to the adoption of the MDGs. We applied adapted search filters from the InterTASC Information Specialists’ Subgroup Search Filter Resource for each database [ 15 ].
Our searches combined terms related to the concepts of (1) UHC (e.g. universal health insurance, universal coverage) and (2) quality of care and its seven dimensions (e.g. equity, safety, people-centredness). Our search strategy is available in Appendix A. Figure 1 outlines the eligibility criteria we used to assess studies for inclusion in the review.
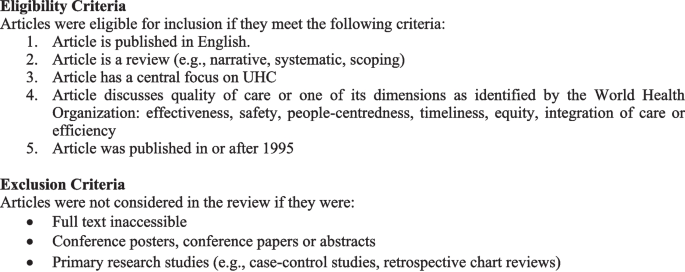
Eligibility and exclusion criteria
Data management
Results from database searches were managed through Covidence ( www.covidence.org ) for deduplication and screening.
Study selection
Two reviewers (BY&AK) independently assessed studies against the eligibility criteria in two phases: (1) titles and abstracts and (2) full-text articles. A pilot test of the title and abstract screening was completed for approximately the first 100 search results. The two reviewers discussed disagreements to revise eligibility criteria as required. Any disagreements were resolved via consensus and in consultation with senior co-authors.
Data extraction
BY & AK independently completed data extraction for the first 10 articles using a standardized form. Following the pilot, the full data extraction was completed by the two reviewers in parallel. We extracted data on key study characteristics and according to each domain and subcomponent identified in Kruk et al.’s [ 5 ] framework described in the following section. The process of data extraction was iterative, with the form subject to revisions. Geographic regions were classified either by WHO regions [ 16 ] or through self-identification by the articles, such as a global focus, LMICs, HICs, ‘developing’ or ‘developed’.
Data synthesis
We synthesized the results through both a descriptive summary and a qualitative, narrative synthesis. We anchored our narrative synthesis in Kruk et al.’s [ 5 ] conceptual framework for high-quality health systems. The framework draws from Donabedian’s well-known conceptual model of quality of care, which was first developed in the 1960s and identifies structures, processes and outcomes as three components of quality of care. Kruk et al. [ 5 ] offer a new evidence-based framework relevant to present-day health systems, recognizing the heterogeneity of health systems across HIC and LMIC contexts.
They define three key domains of a high-quality health system, which they argue should be at the core of implementing and advancing UHC: foundations, processes of care and quality impacts. Foundations refer to the context and resources required to lead a high-quality health system. Processes of care include competent care and systems, relating to evidence-based effective care and health systems’ ability to respond to patient needs. Quality impacts include both patient and provider-reported health outcomes and client confidence in the health system, as well as economic benefits such as a reduction of resource waste and financial risk protection. The Kruk et al. [ 5 ] framework does not explicitly address equity; however, the authors state that equity in the quality of healthcare is critical, which they define as ‘the absence of disparities in the quality of health services between individuals and groups with different levels of underlying social disadvantage [p. e1214].’ When compared with Donabedian’s model for evaluating the quality of care [ 17 ], Kruk et al. [ 5 ] offer a much more elaborated framework that explicitly names a range of subcomponents to guide quality measurement and improvement (e.g. governance, positive user experience, etc.).
As our scoping review examines the existing literature on quality of care within the context of UHC and identifies knowledge gaps, Kruk et al.’s [ 5 ] framework provided a useful analytic tool by which to organize and interpret our findings.
We organized the results from our narrative synthesis according to each component of the framework (foundations, processes of care and quality impacts), addressing equity as a cross-cutting theme across these components. Table 1 summarizes the components and subcomponents of the framework.
Description of included reviews
The database searches yielded 4128 results after deduplication. Following screening, 45 articles that met eligibility criteria were included in the review. The search results are shown in Appendix A and a summary of each article is presented in Table 2 . Narrative reviews comprised 40.0% of the studies ( n = 18), 35.6% were systematic reviews (n = 16), while 20.0% were scoping reviews ( n = 9), and 4.4% were overviews of systematic reviews ( n = 2). Of the 45 reviews, 28 covered multiple WHO regions (62.2%). This included reviews with a broad global focus, reviews focused on LMICs, ‘developing’ or ‘developed’ countries, as well as reviews with an explicit focus on more than one of six WHO regions. Regarding the dimensions of quality of care, equity was the most well represented, examined by 40 of the studies (88.9%). Integration of care and safety were the least represented across the studies, each examined by 11 of the reviews (24.4%). We did not formally appraise the quality of studies included in our review, which is not required for a scoping review given its overarching aim to map the scope and size of the available literature on a given topic.
Narrative synthesis of results
Conceptualizing universal healthcare/coverage and quality of care.
The included studies highlighted varying definitions of UHC and quality of care. A common definition of UHC was that all people who require any essential healthcare services, including but not limited to promotion, prevention and treatment, are able to access services without financial stress [ 18 , 19 , 20 ]. One study further expanded this definition to include that UHC was the desired outcome of health system performance [ 18 ]. Some studies specified the definition was outlined in the Alma Ata declaration [ 21 , 22 ].
Definitions of quality of care also varied. One study distinguished between service quality (e.g. patient satisfaction, responsiveness) and technical quality (e.g. adherence to clinical guidelines) [ 23 ]. Another study defined high-quality healthcare as ‘providing the highest possible level of health with the available resources’ [ 24 , p. 142]. However, most studies did not provide a working definition of quality of care, and instead used proxy indicators such as infant mortality [ 25 ] to highlight quality-related outcomes.
Synthesis according to Kruk et al. Conceptual framework
Below, we synthesize findings from the studies according to the components of Kruk et al.’s [ 5 ] conceptual framework (foundations, processes of care and impacts). We highlight the most common themes that we identified in the literature for each domain and provide illustrative examples. Unless specified, findings were not specific to LMIC or HIC contexts.
Foundations
Governance: leaders, policies, processes and procedures providing direction and oversight of health system(s).
A common theme across the literature was health system governance at local, regional and national scales, and its relationship to quality of care within the context of UHC. Naher et al. [ 26 ] identified transparency, accountability, laws and regulations, and citizen engagement as critical components of governance. The articles discussed both poor and good governance, their underlying determinants and drivers, as well as interventions to improve governance and thus quality of care [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ].
The literature suggests that poor governance is a common issue across health systems, and is both a cause and indicator of poor-quality care. Causes and forms of poor governance include weak supervision of, and inadequate incentives and remuneration for healthcare providers; lack of transparency and accountability in decision-making; and insufficient financial capacity; in addition to fragmented regulations and policies. Poor governance has also been found to result in low patient trust and confidence in the health system, wasted resources and poor patient outcomes [ 26 , 40 , 44 ]. In contrast, the reviewed literature described strong governance as critical to effective healthcare services [ 26 ] and the basis for achieving UHC [ 32 ].
Interventions to improve governance described by the reviewed literature include decentralization, social accountability mechanisms, such as social audits, and policy reforms to strengthen provider incentives and service integration [ 26 , 28 , 31 , 45 , 47 , 53 ]. However, the evidence regarding the effectiveness of these interventions on governance and quality of care was largely inconclusive. Regarding integration, White [ 45 ] noted the need to ensure adequate leadership and organizational capacity before integrating services, as a key determinant of success.
Quality of care measures
Six studies identified measures and/or measurement instruments to assess quality of care or its various dimensions within the context of UHC [ 19 , 22 , 27 , 30 , 42 , 51 ]. These measures differed based on their service areas of focus (e.g. family planning, primary care), the geographic contexts for which they are intended and whether they assessed foundations, processes of care or quality impacts. The reviewed literature identified a lack of standardized quality assessment tools as a significant barrier to the realization of UHC [ 22 , 42 ]. However, researchers also noted the need for country-specific indicators reflective of a country’s unique social, political and economic circumstances, and population needs and expectations [ 18 , 22 , 30 , 39 , 51 ]. Studies also emphasized the importance of integrating equity as an explicit component in the measurement and monitoring of UHC through for example, disaggregation of data by key socioeconomic and demographic variables including place of residence, occupation, religion, ethnicity and migration status [ 18 , 27 , 30 , 35 ]. Table 3 maps the measures identified in the studies according to the domains and subdomains of Kruk et al.’s framework.
Skills and availability of health system workers
Several studies also identified critical health workforce shortages and inequities in the distribution of appropriately qualified staff between urban and rural areas as significant constraints to the provision of high-quality, equitable care within the context of UHC, particularly in LMIC contexts [ 21 , 23 , 25 , 29 , 31 , 38 , 40 , 43 , 44 , 46 , 47 , 48 , 49 , 50 , 53 ]. Strategies discussed to address these concerns included (i) improving recruitment and retention of health system staff for rural and remote areas [ 21 , 46 , 47 , 50 ]; (ii) recruiting and training community health workers, while increasing the skills of lay health workers [ 21 ]; (iii) training traditional medicine practitioners in conventional medicine and utilizing them as community health workers [ 49 ]; and (iv) increasing task shifting, through delegating tasks to less specialized health workers [ 21 , 31 ], for which supportive supervision and adequate training is required [ 21 ].
Processes of care
Access to competent care and systems, incentives to improve quality of care delivery.
Evidence from the reviewed studies suggests that poor provider competence across a range of health services remains an ongoing issue, particularly in LMICs, posing a considerable barrier to the provision of timely, safe and effective quality of care [ 22 , 23 , 29 , 31 , 33 , 39 , 40 , 46 , 47 , 49 ]. For example, in China, a study with standardized patients found that providers in village hospitals provided correct treatment for tuberculosis only 28% of the time [ 47 ].
Within health systems seeking to provide UHC, significant inequities remain in both LMICs and HICs regarding the quality of care received by different populations. Vulnerable populations, who are more likely to receive care from lower-level health facilities, such as health centres, are disproportionately impacted by incompetent care and systems, having already constrained access to care [ 26 ], fewer options regarding providers and being more likely to receive inappropriate referrals [ 40 ], all indicators of lower-quality care.
Four studies described organizational factors influencing provider competence, including performance appraisal, continuing education, incentives, and remuneration and payment mechanisms [ 27 , 31 , 40 , 46 ]. For example, Sanogo et al. [ 40 ] discussed how delays in provider reimbursement as observed in Ghana, can demotivate healthcare providers, which Agarwal et al. [ 27 ] noted may decrease providers’ willingness to exert maximum effort on assigned tasks, compromising the quality of care.
Regarding incentives to improve motivation and quality of care delivery, Yip et al. [ 47 ] suggested a pay-for-performance system in China, as physicians are traditionally incentivized for treatment-based care through fee-for-service. However, the systematic review from Wiysonge et al. [ 46 ] noted a lack of evidence to support whether financial incentives for healthcare providers would improve quality of care in low-income countries.
User experience: wait times and people centredness
Wait times, a core component of quality of care, were noted as ongoing concerns in HICs and LMICs [ 21 , 23 , 33 , 39 , 40 , 47 , 48 , 55 , 56 ]. In HICs such as Norway and the United Kingdom, long wait times have been found to increase the demand for duplicative voluntary private health insurance, which Kiil argues may threaten the overall quality of public-sector driven UHC and exacerbate inequities [ 56 ]. In LMICs, evidence has shown that service quality is often superior in the private sector compared with the public sector, defined in relation to shorter wait times, better hospitality and increased time spent with providers [ 23 ].
Several studies described the relationship between positive user experience and people-centred care, which focuses on the needs and preferences of populations served while engaging them in shaping health policies and services. In addition, people centredness has been linked to improved mental and physical health, and reduced health inequities among other outcomes [ 20 , 22 , 31 , 35 , 57 ].
One study presented a people-centred care partnership model intended to support the work of advanced practice nurses in sustaining UHC, identifying nine attributes of people centredness including mutual trust and shared decision-making [ 20 ].
Several studies also discussed strategies aimed at increasing patient/community voice and engagement and the people centredness of health systems. These strategies included citizenship endorsement groups in Mexico [ 34 ] and various public forums to foster accountability and transparency [ 26 ]. However, McMichael et al. [ 35 ] cautioned that approaches to increase the voice of patients and communities risk excluding the most vulnerable, as those facing the greatest barriers to participation in such initiatives are often the most disadvantaged in their access and use of health services.
Quality impacts
Quality of care outcomes.
A few of the reviewed articles reported on empirical studies that analyzed patient and population health outcomes in relation to quality of care in the context of UHC. Where reported, these outcomes were discussed in reference to (i) specific programmes intended to improve quality of care and advance UHC, (ii) the impacts of health insurance schemes or health system reforms, (iii) private versus public sector provision of healthcare and/or (iv) the effects of specific service delivery models.
Regarding programmes intended to improve the quality of care, a community health extension programme in Ethiopia was associated with increased perinatal survival and decreased prevalence of communicable diseases. Though resource constraints such as inadequate medical supplies and limited supervision of health extension workers were noted as challenges, a key success factor included strong community engagement [ 29 ].
Another six studies examined health outcomes in relation to health insurance schemes or health system reforms [ 25 , 40 , 46 , 47 , 48 , 55 ]. Some improvements in health outcomes were noted. For example, in China, health system reforms aimed at achieving UHC have been associated with decreased maternal mortality rates [ 25 ]. However, the burden of noncommunicable diseases such as diabetes is rising amid significant gaps in their detection and treatment [ 47 ].
Studies also compared patient outcomes in relation to private versus public sector healthcare provision [ 24 , 56 , 58 ]. How the private sector was conceptualized varied across the studies, both in terms of how it was categorized (e.g. for-profit versus not-for-profit), as well as its role in healthcare financing and delivery. Given this heterogeneity, whether the public or private sector leads to higher-quality care and consequently, better health outcomes, is unclear in the reviewed literature. However, the private sector, when financed through out-of-pocket payments, is more likely to exacerbate inequities in access to healthcare.
Finally, two studies examined integrated models of care and their relationship to health outcomes [ 52 , 54 ]. According to these studies, different forms of service integration may positively impact health, for example, through slowed disease progression [ 54 ] and decreased preterm births [ 52 ].
Patient-reported satisfaction and trust in health system
Reports of poor perceived quality of care and low patient satisfaction as barriers to healthcare uptake and enrollment in health insurance schemes were common across the reviewed studies [ 26 , 28 , 36 , 40 , 44 , 47 , 55 , 56 ]. For instance, Alhassan et al. [ 28 ] found that perceived low quality of care, long wait times and poor treatment by healthcare providers reduced clients’ trust in Ghana’s National Health Insurance Scheme, reducing subsequent re-enrollment rates. In Ghana, perceived quality of care was found to exert a greater influence on men’s decisions regarding care uptake than on women’s decisions [ 36 , 44 ]. O’Connell et al. [ 36 ] suggested this gendered difference may be due to men’s care being more likely to be prioritized within household financial decisions, affording them the opportunity to be more discerning regarding the quality of care.
Several studies also discussed the effects of health system reforms and different service delivery models on patient satisfaction and trust in healthcare systems [ 23 , 28 , 29 , 31 , 38 , 43 , 47 , 54 , 57 ]. Yip et al. noted that despite reforms aimed at expanding access to care across China, many patients have chosen to forgo care at primary healthcare facilities altogether due to a lack of trust and dissatisfaction with quality of care [ 47 ]. Similarly, Ravaghi et al. identified contradictory results regarding the effects of hospital autonomy reforms on patient satisfaction. Two studies in Indonesia cited in Ravaghi’s review reported improvements, while others noted decreased or no change in patient satisfaction [ 38 ]. In contrast, four reviews found that integrated, people-centred health services may positively impact patient satisfaction [ 29 , 31 , 54 , 57 ].
Efficiency of healthcare services and systems
Twenty-seven studies addressed the efficiency of healthcare systems and services, which the review by Morgan et al., defined as ‘the extent to which resources are used effectively or are wasted’ [ 23 , p. 608]. These studies discussed inefficiencies in health systems [ 22 , 26 , 28 , 29 , 44 , 48 ], the possible effects of health reforms and other interventions on efficiency [ 21 , 25 , 31 , 37 , 38 , 41 , 44 , 45 , 46 , 47 , 50 , 53 , 54 , 55 , 58 , 59 ], efficiency as a criterion in health policymaking [ 32 ], and the measurement of efficiency [ 22 , 30 , 42 , 51 ], an example of which, as cited in Rezapour et al.’s study, was the percentage of prescriptions including antibiotics in health centres and health posts [ 51 ].
Additionally, some studies compared the efficiency of public and private sector healthcare provision, reporting mixed results [ 23 , 24 , 48 , 58 , 61 ]. For example, higher overhead costs and lower quality of care outcomes, including higher death rates, have been observed in private hospitals compared with public hospitals in the United States [ 24 ]. In contrast, research on the National Health Service in England has suggested that privatization and market-oriented reforms have improved the efficiency of hospital care through cost cutting without evidence of reduced quality [ 58 ].
In LMICs, the private sector has been linked to increased service costs related to overprescribing and use of unnecessary and expensive procedures [ 23 ]. However, Morgan et al. noted that studies assessing private sector performance in LMICs have often focused on unqualified or informal small private providers, such as small drug shops, operating amid weak public health systems and poor regulation, providing an incomplete picture of the role of the private sector in progress towards UHC [ 23 ]. Table 4 captures a high-level overview of the key highlights related to each domain and subdomain of Kruk et al.’s [ 5 ] framework discussed in the studies.
Identified evidence gaps and priorities for future research
Substantial evidence gaps that were identified in the reviewed literature are grouped thematically below. Themes are ordered by how frequently they were discussed by the reviewed studies.
Gap 1: How to measure and monitor UHC, with particular attention to quality of care and equity
Several studies identified the need for additional research to inform the development, selection and use of monitoring and evaluation frameworks and measures to assess quality of care and equity in relation to UHC in various geographic contexts at multiple levels of the health system, including facility and institutional levels [ 22 , 30 , 31 , 34 , 39 , 42 ]. For example, Rodney et al. stressed that countries should select contextually relevant indicators, and pay particular attention to the measurement of equity within UHC, cautioning that measuring equity based solely on wealth quintiles may mask inequities related to other factors such as race or disability [ 39 ]. In addition, two studies discussed the lack of client-reported measurements and advocated for further research to integrate data from household surveys and user-experience surveys [ 22 , 30 ].
Gap 2: Comparative information on the efficiency and effectiveness of public and private health provision and appropriate mix of public and private healthcare
Researchers noted the need for more conclusive evidence comparing the efficiency and effectiveness of public and private health sector provision, and the role of the private sector in contributing to UHC [ 21 , 23 , 56 , 57 , 62 ]. For example, Morgan et al. highlighted the need for greater evidence on how system-level influences such as regulations, may be used to create a public–private healthcare mix that promotes high-quality care and supports the achievement of UHC [ 23 ].
Gap 3: Effects of financial and insurance schemes on quality-of-care delivery and patient outcomes
The reviewed literature identified a lack of evidence regarding the impacts of different financial and insurance schemes on quality-of-care delivery and patient outcomes, particularly for vulnerable groups including women-headed households, children with special needs and migrants [ 34 , 46 , 55 , 62 ]. For example, van Hees et al. noted a lack of evidence regarding the impacts of financial schemes, such as pooling of funds and cost sharing, on equity [ 55 ].
Gap 4: Effects of integrated service delivery models
Studies identified the need for more robust evidence related to the effects of integrated service delivery models on access to quality care, as well as patient and population health outcomes [ 22 , 37 , 52 , 54 ]. Lê et al. specifically highlighted the lack of evidence on equity outcomes related to service integration, suggesting the need for further research in this area [ 54 ].
Gap 5: Mechanisms and contexts that enable and hinder implementation of quality-related interventions
Finally, researchers called for additional evidence regarding the mechanisms and contextual factors such as societal stigma that influence the effectiveness of interventions related to quality of care in the context of UHC [ 34 , 37 , 55 ]. To this aim, van Hees et al. recommended realist evaluations to surface what works, for whom, and in what contextual circumstances [ 55 ]. For example, Palagyi et al. identified a need for further research on task shifting, particularly how the skills gained by health workers can be maintained, and its implications for team dynamics and the delivery of existing programmes [ 37 ].
This scoping review aimed to characterize the existing conceptual and empirical literature on quality of care within the context of UHC. As noted in our results, in the reviewed literature, quality of care was often ill defined or defined inconsistently. A lack of conceptual clarity compromises the development of a robust evidence base able to inform the design and implementation of effective quality-related policies and interventions.
The 45 articles we reviewed for our study reveal a heterogeneous body of literature when compared with Kruk et al.’s quality of care framework. While some framework components including governance and the efficiency of healthcare services and systems were highly represented in the included literature, others were less represented such as physical and technological resources and tools, and patient and population health outcomes.
We also noted in the reviewed literature a lack of clarity regarding how the studies distinguished between private sector involvement in financing and/or delivery of care. This lack of clarity limits our understanding of the implications of private sector engagement for the quality of care and the achievement of UHC in various geographical contexts. Research is required to provide greater clarity of the role and impacts of private sector involvement in financing and/or delivery of health services, to help inform countries’ decision-making regarding private sector engagement. In addition, further research is needed regarding the interactions between the public and private sector and their effects on the sustainability of UHC. For example, studies have noted a concern that the availability of concierge services can create downstream implications for people who cannot afford private insurance, such as an imbalance in resource distribution [ 57 ].
Overall, the identified evidence gaps pointed to the need to build a stronger evidence base about what works, for whom, and under what contextual circumstances, and with what effects on equity to improve quality of care in LMICs and HICs. This includes a need for further evidence on the effects of integrated service delivery models, as well as how regulation can be used to create a public–private healthcare mix promoting high-quality and equitable care. The literature further highlighted the urgent need for additional research to inform the creation of robust monitoring and evaluation frameworks prioritizing equity that could support improvements to quality of care. This includes further research to help support the inclusion and use of disaggregated data, such as by wealth, sex and ethnicity to monitor and inform efforts to increase equity in access, utilization and outcomes for vulnerable populations. Beyond the above-noted research priorities, we also recommend additional research comparing quality related outcomes before and after UHC implementation, and how they intersect with health equity.
Strengths of our scoping review include the use of a broad search methodology and validated search filters in consultation with an expert librarian, and the use of a conceptual framework to guide analysis of findings. Further, our search was not constrained based on country of origin. In our search of the literature, we did not find other published reviews of similar scope about quality of care within the context of UHC.
The primary limitation of our review is the small number of included studies that met our eligibility criteria. This highlights that quality-related research in UHC remains an emerging field. In addition, many of the included studies were narrative reviews, which may not have captured the full breadth of the literature. Another limitation of our review is that we included only English-language studies. Future reviews should attempt to search and synthesize evidence in additional languages to provide more global relevance. Further, the conceptual framework we applied to the analysis of findings does not consider various factors that render health systems more fragile such as pandemics, disasters and conflicts, which may compromise the quality of care and realization of UHC. As our study did not include search terms for specific vulnerable populations such as Indigenous or racialized groups, there is also need for future research related to LMICs and communities experiencing marginalization and discrimination within HICs.
In addition, there may be limited applicability of findings across studies to different geographic regions. Finally, due to the heterogeneity and qualitative nature of the included studies, meta-analysis and synthesis beyond thematic analysis were not feasible.
This review summarized the existence of available evidence on quality of care within the context of UHC, identifying strategies aimed at improving quality of care as well as diverse knowledge gaps. Further research, evaluation and monitoring frameworks including those that attend to equity are required to strengthen the existing evidence base.
Availability of data and materials
This work analyzed secondary sources, which are cited and are publicly accessible or with academic institutional credentials. Authors can confirm that all other relevant data are included in the article and/or its additional files.
Abbreviations
African Region
Region of the Americas
Community Health Worker
Eastern Mediterranean Region
European Region
High-Income Countries
Low- and Middle-Income Countries
Millennium Development Goals
National Health Insurance Scheme
National Health Service
Primary Healthcare
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Sustainable Development Goals
South-East Asian Region
Universal Health Coverage
Western Pacific Region
World Health Organization. Regional Office for the Eastern Mediterranean. Universal health coverage. WHO; 2023. Available from: https://www.emro.who.int/health-topics/uhc/index.html .
United Nations. SDG indicators. Metadata repository. UN; 2023. Available from: https://unstats.un.org/sdgs/metadata/?Text=&Goal=3&Target=3.8SDG .
World Health Organization. Primary health care on the road to universal health coverage. WHO; 2019. Available from: https://www.who.int/docs/default-source/documents/2019-uhc-report-executive-summary .
World Health Organization. The world health report: health systems financing: the path to universal coverage. WHO; 2010. Available from: https://apps.who.int/iris/handle/10665/44371 .
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018;6(11):e1196–252. https://doi.org/10.1016/S2214-109X(18)30386-3 .
Article PubMed PubMed Central Google Scholar
World Health Organization, OECD, International Bank for Reconstruction and Development/The World Bank. Delivering quality health services: a global imperative for universal health coverage. WHO, OECD, World Bank Group; 2018. Available from: https://www.worldbank.org/en/topic/universalhealthcoverage/publication/delivering-quality-health-services-a-global-imperative-for-universal-health-coverage .
National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, Board on Global Health, Committee on Improving the Quality of Health Care Globally. Crossing the global quality chasm: improving health care worldwide. National Academies Press; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535653/ .
Canadian Institute for Health Information. Hospital care for heart attacks among First Nations, Inuit and Métis. CIHI; 2013. Available from: https://publications.gc.ca/site/eng/439389/publication.html .
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616 .
Article Google Scholar
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. https://doi.org/10.1186/1748-5908-5-69 .
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7);467–73. https://doi.org/10.7326/M18-0850 .
Yanful B, Kirubarajan A, Mishra S, Bhatia D, Allin S, Di Ruggiero E. Quality in universal health coverage: protocol for a scoping review. Open Science Framework; 2020. Available from: https://osf.io/f8vb6/ .
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4. https://doi.org/10.1016/j.jclinepi.2014.03.013 .
Article PubMed Google Scholar
Bennett S, Jessani N, Glandon D, Qiu M, Scott K, Meghani A, et al. Understanding the implications of the Sustainable Development Goals for health policy and systems research: results of a research priority setting exercise. Global Health. 2020;16(1):5. https://doi.org/10.1186/s12992-019-0534-2 .
The InterTASC Information Specialists’ Sub-Group. The ISSG search filter resource. ISSG; 2022. Available from: https://sites.google.com/a/york.ac.uk/issg-search-filters-resource/home .
World Health Organization. WHO regional offices. WHO; 2023. Available from: https://www.who.int/about/who-we-are/regional-offices .
Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3):166. https://doi.org/10.1111/j.1468-0009.2005.00397.x .
Boerma T, Eozenou P, Evans D, Evans T, Kieny MP, Wagstaff A. Monitoring progress towards universal health coverage at country and global levels. PLoS Med. 2014;11(9):e1001731. https://doi.org/10.1371/journal.pmed.1001731 .
Gupta RD, Shahabuddin A. Measuring progress toward universal health coverage: does the monitoring framework of Bangladesh need further improvement? Cureus. 2018; 10(1):e2041. https://doi.org/10.7759/cureus.2041 .
Kamei T, Takahashi K, Omori J, Arimori N, Hishinuma M, Asahara K, et al. Toward advanced nursing practice along with people-centered care partnership model for sustainable universal health coverage and universal access to health. Rev Lat Am Enfermagem. 2017; 25:1–10. https://doi.org/10.1590/1518-8345.1657.2839 .
Blanchet K, Gordon I, Gilbert CE, Wormald R, Awan H. How to achieve universal coverage of cataract surgical services in developing countries: lessons from systematic reviews of other services. Ophthalmic Epidemiol. 2012;19(6):329–39. https://doi.org/10.3109/09286586.2012.717674 .
Bresick G, Christians F, Makwero M, Besigye I, Malope S, Dullie L. Primary health care performance: a scoping review of the current state of measurement in Africa. BMJ Glob Health. 2019;4(Suppl 8):e001496. https://doi.org/10.1136/bmjgh-2019-001496 .
Morgan R, Ensor T, Waters H. Performance of private sector health care: implications for universal health coverage. Lancet. 2016;388(10044):606–12. https://doi.org/10.1016/s0140-6736(16)00343-3 .
Petrou P, Samoutis G, Lionis C. Single-payer or a multipayer health system: a systematic literature review. Public Health. 2018;163:141–52. https://doi.org/10.1016/j.puhe.2018.07.006 .
Article CAS PubMed Google Scholar
Li H, Liu K, Gu J, Zhang Y, Qiao Y, Sun X. The development and impact of primary health care in China from 1949 to 2015: a focused review. Int J Health Plann Manage. 2017;32(3):339–50. https://doi.org/10.1002/hpm.2435 .
Naher N, Hoque R, Hassan MS, Balabanova D, Adams AM, Ahmed SM. The influence of corruption and governance in the delivery of frontline health care services in the public sector: a scoping review of current and future prospects in low and middle-income countries of south and south-east Asia. BMC Public Health. 2020;20(1), 880. https://doi.org/10.1186/s12889-020-08975-0 .
Agarwal S, Sripad P, Johnson C, Kirk K, Bellows B, Ana J, et al. A conceptual framework for measuring community health workforce performance within primary health care systems. Hum Resour Health. 2019;17(1):86. https://doi.org/10.1186/s12960-019-0422-0 .
Alhassan RK, Nketiah-Amponsah E, Arhinful DK. A review of the national health insurance scheme in Ghana: what are the sustainability threats and prospects? PLoS ONE. 2016;11(11):e0165151. https://doi.org/10.1371/journal.pone.0165151 .
Article CAS PubMed PubMed Central Google Scholar
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):24. https://doi.org/10.1186/s12992-019-0470-1 .
Báscolo E, Houghton N, del Riego A. Construcción de un marco de monitoreo para la salud universal. Rev Panam Salud Pública. 2018. https://doi.org/10.26633/rpsp.2018.81 .
Bitton A, Fifield J, Ratcliffe H, Karlage A, Wang H, Veillard JH, et al. Primary healthcare system performance in low-income and middle-income countries: a scoping review of the evidence from 2010 to 2017. BMJ Glob Health. 2019;4(Suppl 8):e001551. https://doi.org/10.1136/bmjgh-2019-001551 .
Farzaneh A, Ravaghi H. Fanaei A. The ethical framework for policy-making of universal health coverage: a systematic review. J Clin Diagn Res. 2020;14(3):IE01–6. https://doi.org/10.7860/jcdr/2019/43038.13589 .
Ansu-Mensah M, Danquah FI, Bawontuo V, Ansu-Mensah P, Kuupiel D. Maternal perceptions of the quality of care in the free maternal care policy in sub-Sahara Africa: a systematic scoping review. BMC Health Serv Res. 2020;20(1):911. https://doi.org/10.1186/s12913-020-05755-9 .
Mate KS, Sifrim ZK, Chalkidou K, Cluzeau F, Cutler D, Kimball M, et al. Improving health system quality in low- and middle-income countries that are expanding health coverage: a framework for insurance. Int J Qual Health Care. 2013;25(5):497–504. https://doi.org/10.1093/intqhc/mzt053 .
McMichael C, Healy J. Health equity and migrants in the Greater Mekong Subregion. Glob Health Action. 2017;10(1):1271594. https://doi.org/10.1080/16549716.2017.1271594 .
O’Connell TS, Bedford KJA, Thiede M, McIntyre D. Synthesizing qualitative and quantitative evidence on non-financial access barriers: implications for assessment at the district level. Int J Equity Health. 2015;14(1):54. https://doi.org/10.1186/s12939-015-0181-z .
Palagyi A, Dodd R, Jan S, Nambiar D, Joshi R, Tian M, et al. Organisation of primary health care in the Asia-Pacific region: developing a prioritised research agenda. BMJ Glob Health. 2019;4(Suppl 8):e001467. https://doi.org/10.1136/bmjgh-2019-001467 .
Ravaghi H, Foroughi Z, Nemati A, Bélorgeot VD. A holistic view on implementing hospital autonomy reforms in developing countries: a systematic review. Health Policy Plan. 2018;33(10):1118–27. https://doi.org/10.1093/heapol/czy095 .
Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13(1):72. https://doi.org/10.1186/s12939-014-0072-8 .
Sanogo NA, Fantaye AW, Yaya S. Universal health coverage and facilitation of equitable access to care in Africa. Front Public Health. 2019;26(7):102. https://doi.org/10.3389/fpubh.2019.00102 .
Sehngelia L, Pavlova M, Groot W. Impact of healthcare reform on universal coverage in Georgia: a systematic review. Divers Equal Health Care. 2016;13:5. https://doi.org/10.21767/2049-5471.100074 .
Sprockett A. Review of quality assessment tools for family planning programmes in low- and middle-income countries. Health Policy Plan. 2017;32(2):292-302. https://doi.org/10.1093/heapol/czw123 .
Teerawattananon Y, Luz A, Pilasant S, Tangsathitkulchai S, Chootipongchaivat S, Tritasavit N, et al. How to meet the demand for good quality renal dialysis as part of universal health coverage in resource-limited settings? Health Res Policy Syst. 2016;14(1):21. https://doi.org/10.1186/s12961-016-0090-7 .
Umeh CA. Challenges toward achieving universal health coverage in Ghana, Kenya, Nigeria, and Tanzania. Int J Health Plann Manage. 2018;33(4):794–805. https://doi.org/10.1002/hpm.2610 .
White F. Primary health care and public health: foundations of universal health system. Med Princ Pract. 2015;24(2):103–16. https://doi.org/10.1159/000370197 .
Wiysonge CS, Paulsen E, Lewin S, Ciapponi A, Herrera CA, Opiyo N, et al. Financial arrangements for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011084.pub2 .
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet. 2019;394(10204):1192–204. https://doi.org/10.1016/s0140-6736(19)32136-1 .
Christmals CD, Aidam K. Implementation of the National Health Insurance Scheme (NHIS) in Ghana: lessons for South Africa and low- and middle-income countries. Risk Manag Healthc Policy. 2020;13:1879–904. https://doi.org/10.2147/rmhp.s245615 .
Kim JK, Kim KH, Shin YC, Jang BH, Ko SG. Utilization of traditional medicine in primary health care in low- and middle-income countries: a systematic review. Health Policy Plan. 2020; 35(8):1070–83. https://doi.org/10.1093/heapol/czaa022 .
Mumghamba EG, Joury E, Fatusi O, Ober-Oluoch J, Onigbanjo RJ, Honkala S. Capacity building and financing oral health in the African and Middle East Region. Adv Dent Res. 2015;27(1):32–42. https://doi.org/10.1177/0022034515578909 .
Rezapour R, Tabrizi JS, Farahbakhsh M, Saadati M, Abdolahi HM. Developing Iranian primary health care quality framework: a national study. BMC Public Health. 2019;19(1):911. https://doi.org/10.1186/s12889-019-7237-8 .
Schmied V, Mills A, Kruske S, Kemp L, Fowler C, Homer C. The nature and impact of collaboration and integrated service delivery for pregnant women, children and families: collaboration in universal child and family health services. J Clin Nurs. 2010;19(23–24):3516–26. https://doi.org/10.1111/j.1365-2702.2010.03321.x .
Victora CG, Hanson K, Bryce J, Vaughan JP. Achieving universal coverage with health interventions. Lancet. 2004;364(9444):1541–8. https://doi.org/10.1016/s0140-6736(04)17279-6 .
Lê G, Morgan R, Bestall J, Featherstone I, Veale T, Ensor T. Can service integration work for universal health coverage? Evidence from around the globe. Health Policy. 2016;120(4):406–19. https://doi.org/10.1016/j.healthpol.2016.02.007 .
van Hees SGM, O’Fallon T, Hofker M, Dekker M, Polack S, Banks LM, et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health. 2019;18(1):134. https://doi.org/10.1186/s12939-019-1040-0 .
Kiil A. What characterises the privately insured in universal health care systems? A review of the empirical evidence. Health Policy. 2012;106(1):60–75. https://doi.org/10.1016/j.healthpol.2012.02.019 .
Palumbo R. Keeping candles lit: the role of concierge medicine in the future of primary care. Health Serv Manage Res. 2017;30(2):121–8. https://doi.org/10.1177/0951484816682397 .
Almeida ÁS. The role of private non-profit healthcare organizations in NHS systems: implications for the Portuguese hospital devolution program. Health Policy. 2017;121(6):699–707. https://doi.org/10.1016/j.healthpol.2017.03.016 .
Hayati R, Bastani P, Kabir MJ, Kavosi Z, Sobhani G. Scoping literature review on the basic health benefit package and its determinant criteria. Glob Health. 2018;14(1):26. https://doi.org/10.1186/s12992-018-0345-x .
Schveitzer MC, Zoboli ELCP, Vieira MM da S. Nursing challenges for universal health coverage: a systematic review. Rev Lat Am Enfermagem. 2016(24):e2676. https://doi.org/10.1590/1518-8345.0933.2676 .
Fallah R, Bazrafshan A. Participation of delivering private hospital services in universal health coverage: a systematic scoping review of the developing countries’ evidence. J Educ Health Promot. 2021;31(10):113. https://doi.org/10.4103/jehp.jehp_957_20 .
Nandi S, Schneider H. Using an equity-based framework for evaluating publicly funded health insurance programmes as an instrument of UHC in Chhattisgarh State, India. Health Res Policy Syst. 2020;18(1):50. https://doi.org/10.1186/s12961-020-00555-3 .
Download references
Acknowledgements
Thank you to Vincci Lui from Gerstein Science Information Centre at the University of Toronto for her guidance and advice regarding the search strategy. We also would like to acknowledge Garry Aslanyan, Beverley Essue, Miguel Ángel González Block, Greg Marchildon and Jeremy Veillard, for their guidance.
This research was funded by the Canadian Institutes of Health Research (CIHR) (#407149) for the project titled ‘Towards Equitable Universal Health Coverage in a Globalized Era: A Research Agenda-Setting Workshop’.
Author information
Authors and affiliations.
Division of Social and Behavioural Health Sciences, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Bernice Yanful & Erica Di Ruggiero
Institute of Health Policy, Management and Evaluation, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Abirami Kirubarajan, Dominika Bhatia, Sujata Mishra, Sara Allin & Erica Di Ruggiero
Centre for Global Health, Dalla Lana School of Public Health, University of Toronto, Toronto, Canada
Erica Di Ruggiero
You can also search for this author in PubMed Google Scholar
Contributions
All listed authors were involved in the study design. BY and AK performed title/abstract and full-text screening, data extraction, and data synthesis, as well as drafting the manuscript. All authors contributed to subsequent revisions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Bernice Yanful .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sara Allin and Erica Di Ruggiero are co-senior authors.
APPENDIX A: Appendix: Search Strategy
Database: ovid medline: epub ahead of print, in-process & other non-indexed citations, ovid medline® daily and ovid medline®, 1946: september 27, 2021.
# | Searches | Results |
|---|---|---|
1 | Universal health insurance.mp or exp Universal Health Insurance/ | 4022 |
2 | (UHC or (universal adj2 (coverage or care or healthcare or healthcare or health-care)) or ((universal or population or public) adj2 (healthcare or health care or health-care or health coverage or healthcare coverage or health care coverage or health-care coverage or access to care or access to health or access to healthcare or access to health care or access to health-care or access to health service* or access to medicine* or health access or healthcare access or health care access or health-care access or health service* access or medicine* access or health insurance or healthcare insurance or health care insurance or health-care insurance))).mp | 34,774 |
3 | exp Quality Improvement/ or exp Quality Indicators, Health Care/ | 43,714 |
4 | quality.mp | 1,170,848 |
5 | ((integrat* adj2 care) or (consult* or participat* or collab* or partner*) or ((people or person) adj2 cent*) or effective* or timel* or safe* or efficien*).mp | 4,263,417 |
6 | (((systematic OR state-of-the-art OR scoping OR literature OR umbrella) ADJ (review* OR overview* OR assessment*)) OR "review* of reviews" OR meta-analy* OR metaanaly* OR ((systematic OR evidence) ADJ1 assess*) OR "research evidence" OR metasynthe* OR meta-synthe*).tw. OR exp Review Literature as Topic/ OR exp Review/ OR Meta-Analysis as Topic/ OR Meta-Analysis/ OR "systematic review"/ | 2,838,112 |
7 | 1 OR 2 | 34,774 |
8 | 3 OR 4 OR 5 | 5,042,750 |
9 | 6 AND 7 AND 8 | 1799 |
10 | limit 9 to yr = "1995 -Current" | 1612 |
Appendix B: Study Selection
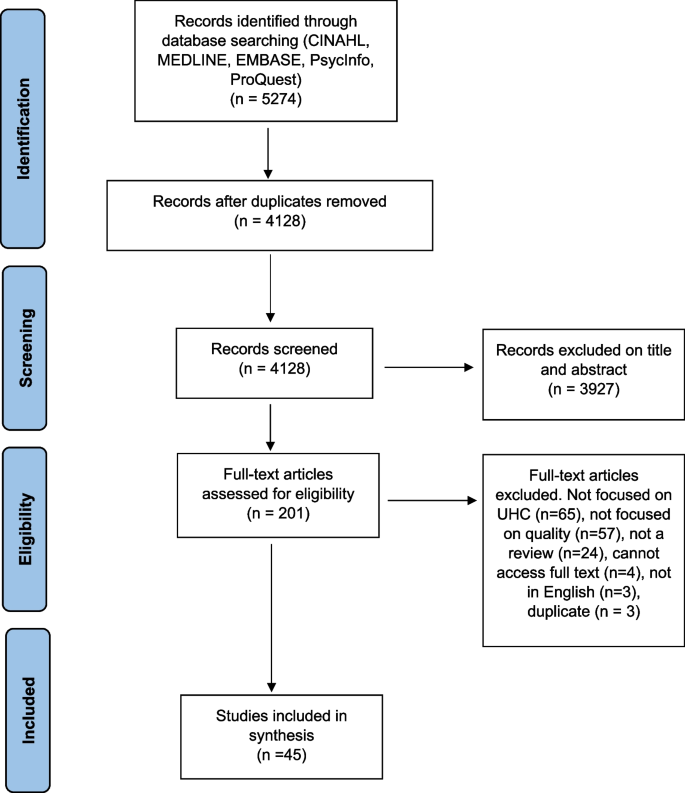
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yanful, B., Kirubarajan, A., Bhatia, D. et al. Quality of care in the context of universal health coverage: a scoping review. Health Res Policy Sys 21 , 21 (2023). https://doi.org/10.1186/s12961-022-00957-5
Download citation
Received : 21 June 2022
Accepted : 28 December 2022
Published : 23 March 2023
DOI : https://doi.org/10.1186/s12961-022-00957-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of care
- Universal health coverage
- Health systems
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The political economy of universal health coverage: a systematic narrative review
Affiliations.
- 1 Faculty of Medicine, The University of Queensland, Herston Road, Herston, QLD 4006, Australia.
- 2 Milken Institute School of Public Health, The George Washington University, 950 New Hampshire Ave NW, Washington, DC 20052, USA.
- 3 School of Public Health, Faculty of Medicine, The University of Queensland, Herston Road, Herston, QLD 4006, Australia.
- PMID: 31904858
- DOI: 10.1093/heapol/czz171
The uptake and implementation of universal health coverage (UHC) is primarily a political, rather than a technical, exercise, with contested ideas and diverse stakeholders capable of facilitation or resistance-even veto-of the policy uptake. This narrative systematic review, undertaken in 2018, sought to identify all peer-reviewed publications dealing with concepts relating to UHC through a political economy framing. Of the 627 papers originally identified, 55 papers were directly relevant, with an additional eight papers added manually on referral from colleagues. The thematic analysis adapted Fox and Reich's framework of ideas and ideologies, interests and institutions to organize the analysis. The results identified a literature strong in its exploration of the ideologies and ideas that underpin UHC, but with an apparent bias in authorship towards more rights-based, left-leaning perspectives. Despite this, political economy analyses of country case studies suggested a more diverse political framing for UHC, with the interests and institutions engaged in implementation drawing on pragmatic and market-based mechanisms to achieve outcomes. Case studies offered limited detail on the role played by specific interests, though the influence of global development trends was evident, as was the role of donor organizations. Most country case studies, however, framed the development of UHC within a narrative of national ownership, with steps in implementation often critical political milestones. The development of institutions for UHC implementation was predicated largely on available infrastructure, with elements of that infrastructure-federal systems, user fees, pre-existing insurance schemes-needing to be accommodated in the incremental progress towards UHC. The need for technical competence to deliver ideological promises was underlined. The review concludes that, despite the disparate sources for the analyses, there is an emerging shared narrative in the growing literature around the political economy of UHC that offers an increasing awareness of the political dimensions to UHC uptake and implementation.
Keywords: Political economy; ideology; policy analysis; policy process; stakeholder analysis.
© The Author(s) 2020. Published by Oxford University Press in association with The London School of Hygiene and Tropical Medicine. All rights reserved. For permissions, please e-mail: [email protected].
PubMed Disclaimer
Similar articles
- The political economy of health financing reforms in Zimbabwe: a scoping review. Mhazo AT, Maponga CC. Mhazo AT, et al. Int J Equity Health. 2022 Mar 27;21(1):42. doi: 10.1186/s12939-022-01646-z. Int J Equity Health. 2022. PMID: 35346208 Free PMC article. Review.
- The genesis of the PM-JAY health insurance scheme in India: technical and political elements influencing a national reform towards universal health coverage. Srivastava S, Bertone MP, Parmar D, Walsh C, De Allegri M. Srivastava S, et al. Health Policy Plan. 2023 Aug 2;38(7):862-875. doi: 10.1093/heapol/czad045. Health Policy Plan. 2023. PMID: 37436821
- The Political Economy of UHC Reform in Thailand: Lessons for Low- and Middle-Income Countries. Tangcharoensathien V, Patcharanarumol W, Kulthanmanusorn A, Saengruang N, Kosiyaporn H. Tangcharoensathien V, et al. Health Syst Reform. 2019;5(3):195-208. doi: 10.1080/23288604.2019.1630595. Epub 2019 Aug 13. Health Syst Reform. 2019. PMID: 31407962
- Political economy analysis of universal health coverage and health financing reforms in low- and middle-income countries: the role of stakeholder engagement in the research process. Loffreda G, Bello K, Kiendrébéogo JA, Selenou I, Ahmed MAA, Dossou JP, Witter S, Bertone MP. Loffreda G, et al. Health Res Policy Syst. 2021 Dec 11;19(1):143. doi: 10.1186/s12961-021-00788-w. Health Res Policy Syst. 2021. PMID: 34895251 Free PMC article. Review.
- Moving towards universal health coverage: lessons from 11 country studies. Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, Takemi K, Evans TG. Reich MR, et al. Lancet. 2016 Feb 20;387(10020):811-6. doi: 10.1016/S0140-6736(15)60002-2. Epub 2015 Aug 21. Lancet. 2016. PMID: 26299185
- Advancing Empirics and Theory for a Deeper Political Economy Analysis Comment on "Health Coverage and Financial Protection in Uganda: A Political Economy Perspective". Fox AM. Fox AM. Int J Health Policy Manag. 2023;12:7537. doi: 10.34172/ijhpm.2023.7537. Epub 2023 Sep 10. Int J Health Policy Manag. 2023. PMID: 38618806 Free PMC article.
- Mapping health service coverage inequalities in Africa: a scoping review protocol. Karamagi HC, Ben Charif A, Afriyie DO, Sy S, Kipruto H, Oyelade T, Droti B. Karamagi HC, et al. BMJ Open. 2023 May 30;13(5):e068903. doi: 10.1136/bmjopen-2022-068903. BMJ Open. 2023. PMID: 37253504 Free PMC article.
- Developing technical support and strategic dialogue at the country level to achieve Primary Health Care-based health systems beyond the COVID-19 era. Cheong Chi Mo J, Shah A, Downey C, Genay-Diliautas S, Saikat S, Mustafa S, Meru N, Dalil S, Schmets G, Porignon D. Cheong Chi Mo J, et al. Front Public Health. 2023 Apr 11;11:1102325. doi: 10.3389/fpubh.2023.1102325. eCollection 2023. Front Public Health. 2023. PMID: 37113176 Free PMC article.
- Political economy analysis of subnational health management in Kenya, Malawi and Uganda. Rodríguez DC, Balaji LN, Chamdimba E, Kafumba J, Koon AD, Mazalale J, Mkombe D, Munywoki J, Mwase-Vuma T, Namakula J, Nambiar B, Neel AH, Nsabagasani X, Paina L, Rogers B, Tsoka M, Waweru E, Munthali A, Ssengooba F, Tsofa B. Rodríguez DC, et al. Health Policy Plan. 2023 May 17;38(5):631-647. doi: 10.1093/heapol/czad021. Health Policy Plan. 2023. PMID: 37084282 Free PMC article.
- Evaluation of the National Health Insurance Program of Nepal: are political promises translated into actions? Khanal GN, Bharadwaj B, Upadhyay N, Bhattarai T, Dahal M, Khatri RB. Khanal GN, et al. Health Res Policy Syst. 2023 Jan 20;21(1):7. doi: 10.1186/s12961-022-00952-w. Health Res Policy Syst. 2023. PMID: 36670433 Free PMC article. Review.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Public Health
- v.105(Suppl 5); Nov 2015
Universal Health Coverage: A Political Struggle and Governance Challenge
S. L. Greer led the development and writing of the article, including preparation of the initial outline. C. A. Méndez contributed to the conceptualization of the article and reviewed the drafts.
Universal health coverage has become a rallying cry in health policy, but it is often presented as a consensual, technical project. It is not.
A review of the broader international literature on the origins of universal coverage shows that it is intrinsically political and cannot be achieved without recognition of its dependence on, and consequences for, both governance and politics.
On one hand, a variety of comparative research has shown that health coverage is associated with democratic political accountability. Democratization, and in particular left-wing parties, gives governments particular cause to expand health coverage. On the other hand, governance, the ways states make and implement decisions, shapes any decision to strive for universal health coverage and the shape of its implementation.
Universal health coverage (UHC) has become a focal point in global health conversations. In the spirit of previous unifying concepts such as Health for All, basic health needs, and the Alma-Ata declaration, it presents a vision in which all citizens will enjoy (1) a strong and efficient health system that spans preventive and curative medicine, (2) affordable access to that health system, (3) access to relevant medicines, and (4) sufficient human resources for the health system. The 2010 World Health Report presented UHC as an objective and a strategy for its member states to reform, or design, their health systems. 1 UHC has been the focus of much research and policy prescription since then. Various authors have shown its implications for the health workforce and its governance, 2,3 health financing, 4 and management. 5
But is UHC likely to be attained? We draw on political science and public health literature to argue that politics and governance have been undervalued as key drivers for universal health coverage.
UNIVERSAL HEALTH COVERAGE IS POLITICAL
It is a political victory that UHC is discussed at all, and still more so that it has any veneer of consensus. UHC is a highly political concept. In the world of global health governance, it is part of an ongoing debate about the relative importance of “vertical” priorities such as disease eradication and broader “horizontal” system-strengthening proposals. 6,7 Given the momentum behind disease-specific interventions and the appeal of solving particular problems (e.g., antiretrovirals or polio eradication), it is always difficult to argue for more amorphous health system goals that are part of UHC or predecessor agendas. 8
The contentiousness of global health politics is nothing like the domestic politics of UHC or universal health care access by any other name. The US State Department has even objected to a World Health Organization fact sheet on the right to health. 9 Observation of politics in the United States, 10,11 or reading about the history of health politics anywhere, supports this point. UHC is expensive and redistributive; that is enough to make it contentious. 12,13 As if that were not enough, UHC also builds in additional contentious goals such as efficiency or access and medicines. 14–16 It is unwise to assume that UHC goals are entrenched in the countries that have broadly achieved them, to overstate the influence of health ministries or advocates committed to UHC, or to overstate the degree of consensus among governments that have adopted them on paper. 17,18
If any generalization about UHC holds, it is that democratization promotes it. Middle-income countries can broadly afford to aim for UHC, but they are most likely to enact access expansions when they have governments that are accountable to the population. 19–21 The effects of widespread democratization from the 1970s to the late 1990s help to explain the expansion of UHC in middle-income countries today. 22–25 Authoritarian regimes, by contrast, are less responsive to the broad population, can discourage or repress organized challenges, and therefore often focus benefits on a narrower set of people who are part of the regime or who can threaten it (e.g., by striking or staging a military coup). The result has been the historical pattern of segmentation that southern Europe and Latin America have had to confront, in which a few crucial sets of workers (especially the public sector and key strategic industries) enjoy extensive health and other benefits and groups without the capacity to threaten the regime receive less. 19,26–28
Partisan politics are one of the most promising avenues for explaining UHC. In particular, left-wing parties are more likely to enact redistributive policies such as UHC. 27,29–31 Socialist parties enacted universal health care across southern Europe when they came to power after democratization, 32 despite major recessions that might be expected to block health access expansion, and later it was the left that universalized health care in Latin American countries such as Brazil and Chile. 33,34 Conservative parties have also at times expanded health coverage for their own political purposes. 20,35 Otto von Bismarck created the first social health insurance in response to socialist challenges, Japan’s health insurance expansion came about as a response to a left labor challenge to the dominant conservative Liberal Democratic Party, and the expansion of health care access in Mexico was partly a strategy to maintain the popularity of its once-dominant Party of the Institutional Revolution. 36,37
Democracy and partisanship do not automatically produce UHC; UHC still needs organized support and faces organized opposition. 38–40 Unorganized voters are unlikely to have their preferences reflected in any political system. The complexities of organization, political coalitions, and parties, a long-standing issue in comparative politics, therefore demand attention; the relationship between left-party success and UHC policies is not simple, 31 and part of the reason is the interaction between politics and governance.
“Good governance” is a widely supported goal, but there is great disagreement about what it is and how it is to be attained. 41,42 Governance discussion often mixes governance as a phenomenon (how decisions are made) with normative policy advice (how decisions should be made and implemented, i.e., good governance). Governance as a phenomenon is the institutional framework of the decisions and policy implementation. 43 A review of components of governance in the health and broader policy literatures by authors associated with the European Observatory on Health Systems and Policies found that diverse authors focused on the same five areas in which governance can affect health systems: transparency, participation, accountability, integrity (management and anticorruption measures), and policymaking capacity. 44
Governance shapes the likelihood that UHC will be adopted and actually implemented for three reasons. First, it is a prerequisite for some policies. Just as policies for UHC can cost too much for a given state, they can also demand a level of expertise, accountability, and good public administration that is not always available. In particular, elaborate public–private, market-based, and personal insurance schemes can overwhelm the capacity to design, regulate, and operate them. 44
Second, governance, particularly political institutions, can shape the likelihood of pro-UHC forces winning in politics. Veto points at which a policy can be blocked include bicameralism, referenda, strong supreme courts, and some forms of federalism; they are correlated with slower increases of expenditure, less redistribution, and less programmatic coherence, although they also slow retrenchment. 29 Among the rich countries, the United States and Switzerland stand out for the expense, slow development, and inegalitarianism of their health systems and for their particularly high number of veto points. Their many veto points make opposition easier, demand larger political coalitions, and allow interest groups to extract a higher price for their support. 45–48
Third, governance affects the likelihood that programs will be entrenched by affording programs greater or lesser real effectiveness and greater or lesser political defenses. Although the post-Communist states have shown that it is politically very difficult to take away UHC, 19 their experiences also show that a system that only formally delivers UHC can engender effective privatization through exit from the system (into private provision) or informal payments. Ineffective programs engender less loyalty. Alternatively, governments can lock in UHC achievements by making the systems transparent and accountable to affected groups who will in the future be able to ward off efforts to reduce government commitments or undermine achievements. 49 A well-crafted policy includes governance changes that promote its own political survival by biasing policymaking toward groups who defend UHC. Just as Latin American's military regimes left institutional safeguards for their interests, 50 UHC advocates should pay attention to ways they can create institutional safeguards for a right to health. “Policies create politics,” after all. 51
CONCLUSIONS
There is a strong tendency to discuss UHC as though it were a settled goal that only requires technical follow-up. This approach contradicts or at least underplays a large body of evidence suggesting that UHC is potentially transformative and intensely political, and depends on the features of a country’s governance. Without support in domestic politics, a redistributive policy such as UHC is unlikely to happen. Without political support in the international arena, it can be undermined by advocates of other attractive goals such as programs focused on single diseases. Decision-making and implementation—governance—can support or hinder UHC advocates and deserve attention for the ways in which they can bias decisions and improve or hinder implementation.
For researchers, this means that we need to apply ourselves to better understanding the mechanisms connecting governance, political forces, and UHC decisions; although studies have pointed to the interplay of parties and institutions under democratization, much still remains to be understood about the coalitions and political strategies that shape UHC politics. For UHC advocates, this means that technical skills and advice should be regarded as resources to be used in what are ultimately political fights within countries, that the commitment to UHC by member states is a resource for political argument rather than a binding obligation, and that attention to health governance should come with an explicit objective of strengthening those who seek UHC.
Human Participant Protection
No protocol approval was necessary because this work was not considered human participant research.

IMAGES
VIDEO
COMMENTS
Ssengooba F, Ssennyonjo A. Research for universal health coverage: ... Universal Health Care. (2022). Available online at: https: ... Paper Presented World Health Forum. (1994) 15:323-3281994. [Google Scholar] 54. Wallace LS. A view of health care around the world.
2. Argument against Universal Healthcare. Though the majority of post-industrial Westernized nations employ a universal healthcare model, few—if any—of these nations are as geographically large, populous, or ethnically/racially diverse as the U.S. Different regions in the U.S. are defined by distinct cultural identities, citizens have unique religious and political values, and the populace ...
Abstract. Universal health care (UHC) is garnering growing support throughout the world, a reflection of social and economic progress and of the recognition that population health is both an indicator and an instrument of national development. Substantial human and financial resources will be required to achieve UHC in any of the various ways ...
Increasing the coverage of public health services will also involve allocating resources beyond the remit of the traditional health sector. Good examples of the need for increased upstream investment in public health are diseases associated with smoking—eg, 80% of tobacco-attributable deaths will occur in low-income countries 5 —with similar inequities associated with air pollution in ...
Universal health coverage is sometimes misunderstood as a goal to provide all available health services and products free to every person through national health insurance schemes. 9 In reality, universal health coverage means that all people can access the health services they need without suffering financial hardship. As the health needs across income groups, ages, and health status vary, it ...
Background The progress of Universal health coverage (UHC) is measured using tracer indicators of key interventions, which have been implemented in healthcare system. UHC is about population, comprehensive health services and financial coverage for equitable quality services and health outcome. There is dearth of evidence about the extent of the universality of UHC in terms of types of health ...
Universal healthcare will better facilitate and encourage sustainable, preventive health practices and be more advantageous for the long-term public health and economy of the United States. ... Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial ...
Conclusions: research needed for universal health coverage 21 2. The growth of research for universal health coverage 31 Creativity everywhere 35 Research ascending 35 Growing unevenly 42 The value of health research 46 Conclusions: building on the foundations 47 3. How research contributes to universal health coverage 57 Case-study 1 61
Background Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security. Methods A systematic search was conducted including studies ...
Universal health care, a term for various models of health care systems that provide care for every resident of a given country, will help move the United States toward higher quality, more affordable, and more equitable care. This article defines a reproductive justice and human rights foundation for universal health care, explores how health ...
Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries.
Universal health care, a term for various models of health care systems that provide care for every resident of a given country, will help move the United States toward higher quality, more affordable, and more equitable care. This article defines a reproductive justice and human rights foundation for universal health care, explores how health ...
Abstract. This commentary offers discussion on the pros and cons of universal healthcare in the United States. Disadvantages of universal healthcare include significant upfront costs and logistical challenges. On the other hand, universal healthcare may lead to a healthier populace, and thus, in the long-term, help to mitigate the economic ...
The UN has declared universal health coverage an urgent global goal. Efforts to achieve this goal have been supported by rigorous research on the scientific, technical, and administrative aspects of health systems design. Yet a substantial portion of the world's population does not have access to essential health services. There is growing recognition that achieving universal health coverage ...
There is growing recognition that achieving universal health coverage is a political challenge. However, fundamental concepts from the political science discipline are often overlooked in the health literature. This Series paper draws on political science research to highlight the ways in which politics can facilitate, or stymie, policy reform.
Introduction Universal health coverage (UHC) is an emerging priority of health systems worldwide and central to Sustainable Development Goal 3 (target 3.8). Critical to the achievement of UHC, is quality of care. However, current evidence suggests that quality of care is suboptimal, particularly in low- and middle-income countries. The primary objective of this scoping review was to summarize ...
The financial cost of massively expanding access to health care globally is a formidable barrier to achieving UHC. For example, the Disease Control Priorities Network estimates that low- and lower-middle-income countries would, on average, need to raise their respective annual per capita health expenditures by U.S.$53 and U.S.$61 per person to achieve coverage with the essential UHC package of ...
Berg S. Primary healthcare policy research: including variables associated with the social determinants of health matters; Comment on "Universal health coverage for non-communicable diseases and health equity: lessons from Australian primary healthcare. " Int J Health Policy Manag. 2022; 11 (5):717-719. doi: 10.34172/ijhpm.2021.102.
Abstract. The uptake and implementation of universal health coverage (UHC) is primarily a political, rather than a technical, exercise, with contested ideas and diverse stakeholders capable of facilitation or resistance-even veto-of the policy uptake. This narrative systematic review, undertaken in 2018, sought to identify all peer-reviewed ...
Universal health care would ensure access to health care services for the entire population, improving health outcomes regardless of gender, race, age, employment status, geographic location, or other factors. The economic benefits of universal health care are widely shared and support growth. Universal health care would reduce health care ...
The present study demonstrates the utility of measuring effective coverage and its role in supporting improved health outcomes for all people—the ultimate goal of UHC and its achievement. Global ambitions to accelerate progress on UHC service coverage are increasingly unlikely unless concerted action on non-communicable diseases occurs and countries can better translate health spending into ...
A scoping review of the studies on UHC and its dimensions is crucial to map and characterize the existing studies towards UHC. This will help to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and research [11]. The goals of this scoping review towards universality of UHC were ...
UNIVERSAL HEALTH COVERAGE IS POLITICAL. It is a political victory that UHC is discussed at all, and still more so that it has any veneer of consensus. UHC is a highly political concept. In the world of global health governance, it is part of an ongoing debate about the relative importance of "vertical" priorities such as disease eradication ...