- Research article
- Open access
- Published: 20 March 2020

Side effect concerns and their impact on women’s uptake of modern family planning methods in rural Ghana: a mixed methods study
- Leah A. Schrumpf ORCID: orcid.org/0000-0002-9797-4682 1 ,
- Maya J. Stephens 1 ,
- Nathaniel E. Nsarko 2 ,
- Eric Akosah 2 ,
- Joy Noel Baumgartner 1 ,
- Seth Ohemeng-Dapaah 2 &
- Melissa H. Watt 1
BMC Women's Health volume 20 , Article number: 57 ( 2020 ) Cite this article
28k Accesses
16 Citations
17 Altmetric
Metrics details
Despite availability of modern contraceptive methods and documented unmet need for family planning in Ghana, many women still report forgoing modern contraceptive use due to anticipated side effects. The goal of this study was to examine the use of modern family planning, in particular hormonal methods, in one district in rural Ghana, and to understand the role that side effects play in women’s decisions to start or continue use.
This exploratory mixed-methods study included 281 surveys and 33 in-depth interviews of women 18–49 years old in the Amansie West District of Ghana between May and July 2018. The survey assessed contraceptive use and potential predictors of use. In-depth interviews examined the context around uptake and continuation of contraceptive use, with a particular focus on the role of perceived and experienced side effects.
The prevalence of unmet need for modern family planning among sexually active women who wanted to avoid pregnancy ( n = 135) was 68.9%. No factors were found to be significantly different in comparing those with a met need and unmet for modern family planning. Qualitative interviews revealed significant concerns about side effects stemming from previous method experiences and/or rumors regarding short-term impacts and perceived long-term consequences of family planning use. Side effects mentioned include menstrual changes (heavier bleeding, amenorrhea or oligomenorrhea), infertility and childbirth complications.
As programs have improved women’s ability to access modern family planning, it is paramount to address patient-level barriers to uptake, in particular information about side effects and misconceptions about long-term use. Unintended pregnancies can be reduced through comprehensive counseling about contraceptive options including accurate information about side effects, and the development of new contraceptive technologies that meet women’s needs in low-income countries.
Peer Review reports
Modern family planning methods are a cost-effective strategy for reducing high-risk pregnancies, decreasing unsafe abortions, and allowing for birth spacing and limiting [ 1 , 2 , 3 , 4 ]. Despite advances in contraceptive technology and availability, 214 million women had an unmet need for modern family planning in 2017 [ 5 ].
In order to inform the delivery of family planning services, it is important to understand the factors and characteristics that contribute to a woman’s decision to use modern family planning. Demographic factors influencing family planning use may include age, family size, distance from a health care facility and education level [ 6 , 7 ]. Additionally, family planning use is influenced by women’s norms and perceptions. Women may face cultural or religious pressures against using family planning, often rooted in beliefs that family planning leads to unfaithfulness or interferes with goals of procreation [ 7 , 8 ].
Side effects of modern family planning methods, either experienced or anticipated, have been identified as a common reason that women either choose not to start or discontinue contraceptives. Side effects include menstrual changes (heavier bleeding, amenorrhea or oligomenorrhea), changes in weight, headaches, dizziness, nausea, and cardiovascular impacts. In addition, women may harbor fears of long-term effects of contraceptive use, such as infertility and childbirth complications [ 8 , 9 ]. A 2014 systematic review found a significant proportion of women attributed their unmet need for family planning to a fear of side effects: 28% in Africa, 23% in Asia, and 35% in Latin America and the Caribbean [ 10 ]. A fear of side effects may occur when a woman or someone she knows has experienced side effects with a method, or when rumors or overestimations or rare complications are considered factual [ 7 , 8 , 11 , 12 , 13 ].
Ghana has historically had one of the highest rates of unmet need for family planning in Africa, despite having a relatively strong family planning program. Ghana’s rate of unmet need among married women is 32.9 whereas many surrounding countries have a lower rate of unmet need among married women including Senegal (26.2), Nigeria (23.7) and Cote d’Ivoire (30.9) [ 14 ]. Family planning methods are available at both private and public healthcare facilities and offer a diverse contraceptive mix, including injectables, implants and hormonal birth control pills [ 8 ]. The Amansie West district has 22 public health facilities, comprised of 6 health centers and 16 Community-based Health Planning and Services compounds, 5 private health facilities and 1 hospital. Within these various health facilities modern family planning methods (pills, intrauterine devices (IUDs), and implants) can be administered by trained medical doctors, midwives, and trained Community Health Officers. Nurses in health facilities are able to administer pills and condoms. Outside of health facilities condoms, pills, and injectables are available at pharmacies and drug shops [ 15 , 16 ].
Despite efforts to make contraceptives accessible, about one-third of married women have an unmet need for family planning [ 17 ]. Although the use of modern family planning methods has increased from 5 to 22% between 1988 and 2014, one in four contraceptive users discontinued use within the first year. The main reason reported for discontinuing injectables and implants were side effects or other health concerns and health concerns as a reason for non-use of modern methods in Ghana has been growing over time [ 12 , 17 ].
This study was conducted with the goal of understanding modern family planning use in a rural setting of Ghana with three aims. First, we aimed to estimate the prevalence of modern family planning use and the prevalence of unmet need for modern family planning. Second, we identified factors associated with unmet need for modern family planning use, including factors at an individual, household and health care level. Lastly, we sought to qualitatively examine and understand women’s experiences with choices and behaviors related to family planning use, with a focus on the role of side effects. This data can help inform the delivery of modern contraceptives to all women wanting to delay or limit their pregnancies.
This exploratory mixed-methods study was conducted in the Amansie West District, in the Ashanti Region of Ghana. The population of the area is almost entirely rural (95.6%), with an estimated population of 149,437 in 2014 and annual growth of 2.7% [ 18 , 19 ].
The study included 281 household surveys and 33 in-depth interviews of women 18–49 years old from six subdistricts of the Amansie West District. Data were gathered from May to July 2018 as part of a larger study examining the role of community health workers (CHWs) in family planning use. Six of the seven subdistricts within the Amansie West District were selected based on accessibility and penetration of the national CHW program. The six sub-districts were divided into 11 geographical zones containing at least 100 women of reproductive age (18–49) whose household was registered by a CHW. An average of 30 women were recruited from each zone in order to have geographic representation in our sample; the final sample size was informed by the resources available to us in this study. A subset of individuals who completed the household survey were purposively sampled to participate in a separate in-depth interview. Participants for the in-depth interview were selected based on current, past or lack of modern method use.
To collect the survey data, a team of six female research assistants, bilingual in English and Twi, were trained in ethics and research procedures. The research assistants approached women in their homes to tell them about the study and invite them to participate. After written informed consent, the research assistant administered the structured interview using an electronic tablet, which took approximately 45 min. At the end of the interview, participants were asked if they might be interested in taking part in a subsequent in-depth interview; if yes, then their contact information was collected to schedule the interview at a later time.
To conduct in-depth interviews (IDIs), three bilingual nurses from the district were trained on research ethics and qualitative research. IDIs were scheduled in participants’ homes at a time that was convenient and maximized privacy. Participants were provided a separate written informed consent for the IDI, which included consent for audio recording. IDIs were conducted in Twi and lasted on average 30 min. Following each interview, field notes were written and then later reviewed with the full research team.
Instruments
Structured survey.
The structured survey was created based on a review of the literature and consultation with local public health professionals. The survey was locally translated into Twi and reviewed by multiple individuals to confirm accurate translation. The survey was pre-tested in a rural community prior to data collection, which resulted in slight modifications.
The survey included the following constructs: demographics; pregnancy history; knowledge and perceived availability of various forms of contraceptives; use of contraceptives; pregnancy intention and attitudes towards pregnancy (α = 0.81); depression PHQ-9 (α = 0.74); autonomy (α = 0.77); partner communication (α = 0.74); freedom from coercion (α = 0.80); and partner support (α = 0.80) [ 20 , 21 , 22 , 23 , 24 ].
In-depth interviews
The in-depth interviews were conducted using a semi-structured guide that included open-ended questions and probes to explore community and individual perspectives of family planning, barriers to use, experiences with family planning use, and reasons for using or not using family planning. The interview guide developed for this study, available as a supplementary file, was reviewed by local public health professionals and pretested in the community. Research assistants translated the guide into Twi during the interviews to adjust the phrasing for a natural, casual conversation.
Data analysis
Survey data were analyzed using R Studio. In order to define a population that could be in need of community-based contraception, we excluded individuals who were not sexually active (defined as three months since last sex), currently pregnant, wished to become pregnant in the next few months, or reported being infertile (includes hysterectomy) from the analysis. This resulted in a sample for analysis of 135 women. While definitions of unmet need for population level analyses typically include women, who have unwanted/mistimed pregnancies the parent study was particularly interested in community level modern family planning method gaps that might be facilitated by community health workers. We were also most interested in highly effective modern methods and thus current use of natural and barrier methods were also excluded from our main analyses. Individuals were classified as having an unmet need for modern contraception if they met the criteria for inclusion but reported that they were not using a hormonal method (pills, injectables, implants), female sterilization, male sterilization or an IUD. After examining descriptive statistics, bivariate analysis explored whether key factors were significantly associated with unmet need for these highly effective modern family planning methods. Because bivariate statistics were not significant, multivariate statistics were not used.
Qualitative analysis was conducted using applied thematic analysis [ 25 ]. Audio recordings were simultaneously translated and transcribed in English. NVivo 12 was used to facilitate the organization and coding of transcripts. Emergent themes were identified through an iterative process of summary memos and open coding, which led to the development of a structured codebook. Overarching domains were created as parent codes, and child codes were used to organize emerging themes. Coded texts were reviewed and synthesized, and representative quotes were identified to capture meaning and provide context.
Demographics
Table 1 summarizes the demographics of the sub-sample of participants who had a current need for modern family planning ( n = 135). On average, participants were 29.4 years of age. About half (45%, n = 61) were married. In this community couples who have undergone customary marital rights or those that are living together with children were considered to be married. Half of the participants (52%, n = 70) had three or more children. Education was low, with only 15.6% of participants reporting any secondary school education.
Family planning use
Considering the family planning needs of the sample, 31.1% ( n = 42) had a met need, and 68.9% ( n = 93) had an unmet need. More than half ( n = 23) of women with a met need were using the injectable, Depo-Medroxyprogesterone (DMPA) (Table 2 ). In the bivariate analysis of factors potentially associated with family planning use (i.e., pregnancy intentions and attitudes, depression, level of autonomy, communication with their partner, freedom from coercion and levels of partner support), none of the measures were significantly associated (Table 3 ).
Qualitative insights on family planning use
In the qualitative data, two prominent themes emerged to explain unmet need: concerns about side effects and misconceptions about the long-term effects of family planning (Table 4 ).
- Side effects
Side effects were mentioned as a potential concern in all qualitative interviews. For many, the concerns about side effects outweighed the perceived benefits of using family planning. Of the 17 participants who had discontinued family planning use, only 5 reported experiencing side effects themselves, while the majority recited side effects they believed were associated with modern family planning use. The most common concern about hormonal contraceptives was the resultant changes in menstrual patterns. There was a belief that menstruation was a means of cleansing the body, and concerns that a lack of menstruation could lead to sickness, dizziness, bloating, and fainting. Additionally, amenorrhea was concerning for women because they could no longer monitor whether or not they were pregnant.
In addition to changes in menstruation, participants mentioned other side effects they were concerned about, including sickness, dizziness, and changes in weight. Reduction in weight was seen as an undesirable side effect, while weight gain was seen as a desirable side effect. The seven participants currently using DMPA had experienced at least one of these side effects. Even in cases where participants reported support from their partner, family or religious community to use family planning, anxiety about side effects deterred them from using family planning—support was not enough to overcome what the women articulated as unacceptable side effects. Women who had not experienced side effects themselves discussed side effects as the most common reason that other women did not use modern family planning.
Misconceptions about long-term impacts
Participants both using and not using a modern contraceptive method reported misconceptions in the community, particularly about hormonal methods. The most common misconceptions were rumors about the long-term adverse effects caused by modern family planning. Women recited rumors that family planning use led to fibroids, infertility, birth complications, and even premature death. In most cases, these long-term impacts were attributed to changes in menstrual patterns, typically associated with injectables and implants.
Three participants discussed rumors that implants caused fainting and death due to a restriction in blood flow. The rumors and misconceptions that were reported about family planning use spanned all 14 communities that were included in the qualitative portion of the study, illustrating the ubiquitous nature of these concerns.
Knowledge of modern family planning methods is high throughout Ghana; nationwide, 99% of women with an unmet need for family planning identified at least one modern method [ 17 ]. Despite high levels of knowledge, we found that among 135 women who were sexually active and wanting to avoid pregnancy, a majority (68.9%) had an unmet need for a highly effective modern family planning method. When examining factors that might explain unmet need, no significant associations were identified. Our qualitative data suggests that fear of side effects and misconceptions about family planning methods is likely driving the gap between knowledge and behavior in family planning use. This study suggests a need to address accurate information about family planning methods, especially injectables the most common form of modern family planning in African countries [ 26 ]. Addressing structural barriers of access to contraceptives will be insufficient if misinformation about side effects and long-term adverse effects persist.
In order to meet the needs of women who wish to postpone or limit their pregnancies, it is important to have targeted interventions to address the fears and concerns caused by menstrual bleeding changes that frequently occur with hormonal methods such as injectables and implants. This is especially important in low- and middle-income countries (LMICs) where the use of injectables is being prompted due to its higher effectiveness level, as compared to oral hormonal pills, and the ability to use the product discretely [ 27 , 28 ]. The universal concern about menstruation in our sample demonstrates the need for improved counseling, before and during use, to educate women about the role of menstruation in reproduction and how hormones impact menstrual patterns [ 8 , 12 , 13 ]. Both uptake and continuation of reversible contraceptives requires regular counseling, scheduled follow-up, and clinical management of contraceptive side effects [ 29 ]. Health workers, including CHWs, involved in providing family planning education and provision should be equipped to provide reproductive education to help women understand and differentiate between nonharmful and harmful side effects. FHI360 has developed a job aid called “NORMAL” to help health workers counsel clients on expected changes of menstruation on various forms of hormonal contraception [ 9 ]. There is evidence that job aids with accurate injectable information have been shown to increase injectable use in low-resource settings and could be adapted to the Ghanaian context [ 30 ]. CHWs need additional training to help women understand and manage side effects from modern family planning. Job aids such as “NORMAL” could provide CHWs with a tool to better counsel and manage clients regarding uptake and continuation of family planning methods. Comprehensive counseling, including accurate information on side effects, has been shown to increase continuation of modern methods [ 31 , 32 ]. Additional qualitative research among different communities is needed to understand the beliefs that underlie women’s concerns about menstrual changes. Better understanding these beliefs can inform culturally congruent counseling approaches to promote the uptake and sustainability of family planning methods.
Certain side effects will always be considered unacceptable for some women, making their family planning options more limited. A long-term solution for family planning coverage requires investments in new contraceptive technologies that are responsive to women’s preferences and needs. This includes the development of both hormonal and nonhormonal long-acting reversible contraceptives that are accessible and effective in low-income settings. Several new contraceptive technologies under development may hold promise, including biodegradable implants, longer-acting injectables, IUDs that are easier to insert, and non-hormonal vaginal rings [ 33 , 34 ]. Hopefully, these new technologies will address some barriers to family planning use and provide more options for women and couples to limit or space their pregnancies.
The study findings must be interpreted in the context of the study’s limitations. First, social desirability biases may be present in the survey results. The in-depth interviews were conducted by local nurses responsible for administering family planning methods in the clinics; therefore, participants may have been less likely to speak negatively about services or areas in which the nurses work. It is important to note variation among these interviews, as some participants were more willing to discuss and share than others. Second, the in-depth interviews were simultaneously translated and transcribed from the local language, Twi, into English; therefore, some details and phrasing may have been lost in the process. Third, the sample size for the survey was not powered to detect statistically significant differences. Lastly, we did not explore more deeply whether women felt their family planning needs were being met via barrier and/or natural methods—although less effective, some women and couples purposefully choose this option.
Even as modern contraceptives become increasingly accessible, women may perceive potential drawbacks of highly effective family planning methods to outweigh the benefits. The future of family planning research and implementation should focus on developing and implementing evidence-based counseling tools to promote the uptake and continuation of the current method mix and investing in the development of new family planning technologies that fit the lifestyles and needs of women in LMICs.
Availability of data and materials
The data and all related study materials may be requested from the faculty mentor on this study (Dr. Melissa Watt, [email protected] ).
Abbreviations
Community Health Worker
Demographic Health Survey
Depo-Medroxyprogesterone
Estradiol valerate/norethisterone enantate
In-depth interview
Intrauterine device
Low- and middle-income countries
Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet. 2012;380(9837):111–25. https://doi.org/10.1016/S0140-6736(12)60478-4 .
Article PubMed Google Scholar
Beson P, Appiah R, Adomah-Afari A. Modern contraceptive use among reproductive-aged women in Ghana: Prevalence, predictors, and policy implications. BMC Womens Health. 2018;18(1). https://doi.org/10.1186/s12905-018-0649-2 .
Chola L, McGee S, Tugendhaft A, Buchmann E, Hofman K. Scaling Up Family Planning to Reduce Maternal and Child Mortality: The Potential Costs and Benefits of Modern Contraceptive Use in South Africa. PLoS One. 2015;10(6):e0130077. https://doi.org/10.1371/journal.pone.0130077 .
Article CAS PubMed PubMed Central Google Scholar
Starbird E, Norton M, Marcus R. Investing in Family Planning: Key to Achieving the Sustainable Development Goals. Global Health Sci Pract. 2016;4(2):191–210 https://doi.org/10.9745/GHSP-D-15-00374 .
Article Google Scholar
Guttmacher Institute. ADDING IT UP: Investing in Contraception and Maternal and Newborn Health, 2017: Guttmacher Institute; 2017. https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017 Accessed 27 Dec 2018.
Ebrahim NB, Atteraya MS. Structural correlates of modern contraceptive use among Ethiopian women. Health Care Women Int. 2018;39(2):208–19. https://doi.org/10.1080/07399332.2017.1383993 .
Wulifan JK, Brenner S, Jahn A, De Allegri M. A scoping review on determinants of unmet need for family planning among women of reproductive age in low and middle income countries. BMC Womens Health. 2015;16(1). https://doi.org/10.1186/s12905-015-0281-3 .
Staveteig S. Fear, opposition, ambivalence, and omission: Results from a follow-up study on unmet need for family planning in Ghana. PLoS One. 2017;12(7):e0182076. https://doi.org/10.1371/journal.pone.0182076 .
Rademacher KH, Sergison J, Glish L, Maldonado LY, Mackenzie A, Nanda G, Yacobson I. Menstrual Bleeding Changes Are NORMAL: Proposed Counseling Tool to Address Common Reasons for Non-Use and Discontinuation of Contraception. Glob Health. 2018;6(3):8.
Google Scholar
World Health Organization. (2018, February 8). Family planning/Contraception. https://www.who.int/news-room/fact-sheets/detail/family-planning-contraception Accessed 27 Dec 2018.
Casterline JB, Sathar ZA, Haque, M. ul. Obstacles to Contraceptive Use in Pakistan: A Study in Punjab. Stud Fam Plan. 2001;32(2):95–110. https://doi.org/10.1111/j.1728-4465.2001.00095.x .
Article CAS Google Scholar
Machiyama K, Cleland J. Unmet Need for Family Planning in Ghana: The Shifting Contributions of Lack of Access and Attitudinal Resistance. Stud Fam Plan. 2014;45(2):203–26. https://doi.org/10.1111/j.1728-4465.2014.00385.x .
Sedgh G, Hussain R. Reasons for Contraceptive Nonuse among Women Having Unmet Need for Contraception in Developing Countries. Stud Fam Plan. 2014;45(2):151–69. https://doi.org/10.1111/j.1728-4465.2014.00382.x .
Family Planning 2020. (n.d.). Retrieved December 4, 2019, from https://www.familyplanning2020.org/countries .
Lebetkin E, Orr T, Dzasi K, Keyes E, Shelus V, Mensah S, et al. Injectable Contraceptive Sales at Licensed Chemical Seller Shops in Ghana: Access and Reported Use in Rural and Periurban Communities. Int Perspect Sex Reprod Health. 2014;40(01):021–7. https://doi.org/10.1363/4002114 .
Perry R, Sharon Oteng M, Haider S, Geller S. A brief educational intervention changes knowledge and attitudes about long acting reversible contraception for adolescents in rural Ghana. J Pregnancy Reprod. 2017;1(1). https://doi.org/10.15761/JPR.1000106 .
The DHS Program. Demographic and Health Surveys. In: Ghana Demographic and Health Survey 2014. Rockville: GSS, GHS, and ICF International; 2015. http://dhsprogram.com/pubs/pdf/FR307/FR307.pdf . Accessed 11 Dec 2018.
Ghana Statistical Service. 2010 Population and housing census district analytical report: Amansie West. 2014. https://new-ndpc-static1.s3.amazonaws.com/CACHES/PUBLICATIONS/2016/06/06/Amansie+West+2010PHC.pdf Accessed 27 Dec 2018.
Nuamah GB, Agyei-Baffour P, Akohene KM, Boateng D, Dobin D, Addai-Donkor K. Incentives to yield to Obstetric Referrals in deprived areas of Amansie West district in the Ashanti Region, Ghana. Int J Equity Health. 2016;15(1). https://doi.org/10.1186/s12939-016-0408-7 .
Watt HM, Knettel AB, Choi WK, Knippler TE, May AP, Seedat S. Risk for Alcohol-Exposed Pregnancies Among Women at Drinking Venues in Cape Town, South Africa. J Stud Alcohol Drugs. 2017;78(5):795–800. https://doi.org/10.15288/jsad.2017.78.795 .
Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J General Int Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Rominski SD, Gupta M, Aborigo R, Adongo P, Engman C, Hodgson A, Moyer C. Female autonomy and reported abortion-seeking in Ghana, West Africa. Int J Gynecol Obstet. 2014;126(3):217–22. https://doi.org/10.1016/j.ijgo.2014.03.031 .
Upadhyay UD, Dworkin SL, Weitz TA, Foster DG. Development and Validation of a Reproductive Autonomy Scale. Stud Fam Plan. 2014;45(1):19–41. https://doi.org/10.1111/j.1728-4465.2014.00374.x .
Norbeck JS, Lindsey AM, Carrieri VL. Further Development of the Norbeck Social Support Questionnaire: Normative Data and Validity Testing. [Editorial]. Nurs Res. 1983;32(1):4–9.
Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Thousand Oaks: SAGE Publications, Inc.; 2012. https://doi.org/10.4135/9781483384436 .
Book Google Scholar
Bertrand JT, Sullivan TM, Knowles EA, Zeeshan MF, Shelton JD. Contraceptive Method Skew and Shifts in Method Mix in Low- and Middle-Income Countries. Int Perspect Sex Reprod Health. 2014;40(03):144–53. https://doi.org/10.1363/4014414 .
Bigrigg A, Evans M, Gbolade B, Newton J, Pollard L, Szarewski A, et al. Depo Provera. Position paper on clinical use, effectiveness and side effects. Br J Fam Plann. 1999;25(2):69–76.
CAS PubMed Google Scholar
Curry L, Taylor L, Pallas SW, Cherlin E, Pérez-Escamilla R, Bradley EH. Scaling up depot medroxyprogesterone acetate (DMPA): A systematic literature review illustrating the AIDED model. Reprod Health. 2013;10:39.
Ahmed K, Baeten JM, Beksinska M, Bekker L-G, Bukusi EA, Donnell D, et al. HIV incidence among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: A randomised, multicentre, open-label trial. Lancet. 2019;0(0). https://doi.org/10.1016/S0140-6736(19)31288-7 .
Baumgartner JN, Morroni C, Mlobeli R, Otterness, Buga G, Chen M. Impact of a provider job aid intervention on injectable contraceptive continuation in South Africa. Stud Fam Plan. 2012;43(4):305–14. https://doi.org/10.1111/j.1728-4465.2012.00328.x .
Cetina TECD, Canto P, Luna MO. Effect of counseling to improve compliance in Mexican women receiving depot-medroxyprogesterone acetate. Contraception. 2001;63(3):143–6. https://doi.org/10.1016/S0010-7824(01)00181-0 .
Liu J, Shen J, Diamond-Smith N. Predictors of DMPA-SC continuation among urban Nigerian women: The influence of counseling quality and side effects. Contraception. 2018;98(5):430–7. https://doi.org/10.1016/j.contraception.2018.04.015 .
Brunie A, Callahan RL, Godwin CL, Bajpai J, OlaOlorun FM. User preferences for a contraceptive microarray patch in India and Nigeria: Qualitative research on what women want. PLoS One. 2019;14(6). https://doi.org/10.1371/journal.pone.0216797 .
Tolley EE, McKenna K, Mackenzie C, Ngabo F, Munyambanza E, Arcara J, et al. Preferences for a potential longer-acting injectable contraceptive: Perspectives from women, providers, and policy makers in Kenya and Rwanda. Glob Health Sci Pract. 2014;2(2):182–94. https://doi.org/10.9745/GHSP-D-13-00147 .
Article PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors are grateful for the contributions of the data collection team and the local clinic personnel who helped to facilitate study entry. We are grateful to Bright Asare for provided assistance throughout the data collection period. At the Duke Global Health Institute, Mary Story and Randall Kramer were important advocates for the research.
This study was funded by a grant from Duke University’s Global Health Institute. Students of the funding body designed the study based on priorities identified by Ghanaian collaborators. The supplied funds were used to support data collection and management in Ghana. Analysis, interpretation, & writing were completed by the Duke students (LS and MS), in collaboration with the Ghanaian partners (NN, EA and SO), and with support from Duke faculty mentors (JB and MW).
Author information
Authors and affiliations.
Duke Global Health Institute, Duke University, Box 90519, Durham, NC, 27708, USA
Leah A. Schrumpf, Maya J. Stephens, Joy Noel Baumgartner & Melissa H. Watt
Millennium Promise Ghana, 14 Bathur St, East Legon, Accra, Ghana
Nathaniel E. Nsarko, Eric Akosah & Seth Ohemeng-Dapaah
You can also search for this author in PubMed Google Scholar
Contributions
LAS was a co-principal investigator on the study, contributed to the design of the work, analyzed and interpreted data, and was the main contributor in the writing of the manuscript. MJS was a co-principal investigator in this study, contributed to the design of the work, and analyzed and interpreted the data. NEN made substantial contributions to the conception and design of the work. EA made contributions to the design of the work and data interpretation. JNB made contributions in the interpretation of the data and has substantively revised the manuscript. SO-D made contributions to the conception and design of the work. MHW made substantial contributions to the conception and design of the work, as well as data interpretation and revisions to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Leah A. Schrumpf .
Ethics declarations
Ethics approval and consent to participate.
All study procedures and materials were approved by the Duke University Institutional Review Board (2018–0343) and Ghana Health Services Ethical Review Committee. Written consent was obtained from all participants.
Consent for publication
The informed consent form included permission to include de-identified data in publications.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Schrumpf, L.A., Stephens, M.J., Nsarko, N.E. et al. Side effect concerns and their impact on women’s uptake of modern family planning methods in rural Ghana: a mixed methods study. BMC Women's Health 20 , 57 (2020). https://doi.org/10.1186/s12905-020-0885-0
Download citation
Received : 24 August 2019
Accepted : 15 January 2020
Published : 20 March 2020
DOI : https://doi.org/10.1186/s12905-020-0885-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning
- Contraceptives
BMC Women's Health
ISSN: 1472-6874
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Unmet need for family planning in Ghana: the shifting contributions of lack of access and attitudinal resistance
Affiliation.
- 1 Research Fellow, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 7HT, UK. [email protected].
- PMID: 24931076
- DOI: 10.1111/j.1728-4465.2014.00385.x
In Ghana, despite a 38 percent decline in the total fertility rate from 1988 to 2008, unmet need for family planning among married women exposed to pregnancy risk declined only modestly in this period: from 50 percent to 42 percent. Examining data from the five DHS surveys conducted in Ghana during these years, we find that the relative contribution to unmet need of lack of access to contraceptive methods has diminished, whereas attitudinal resistance has grown. In 2008, 45 percent of women with unmet need experienced no apparent obstacles associated with access or attitude, 32 percent had access but an unfavorable attitude, and 23 percent had no access. Concerns regarding health as a reason for nonuse have been reported in greater numbers over these years and are now the dominant reason, followed by infrequent sex. An enduring resistance to hormonal methods, much of it based on prior experience of side effects, may lead many Ghanaian women, particularly the educated in urban areas, to use periodic abstinence or reduced coital frequency as an alternative to modern contraception.
© 2013 The Population Council, Inc.
PubMed Disclaimer
Similar articles
- Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Sedgh G, Hussain R. Sedgh G, et al. Stud Fam Plann. 2014 Jun;45(2):151-69. doi: 10.1111/j.1728-4465.2014.00382.x. Stud Fam Plann. 2014. PMID: 24931073
- Men's unmet need for family planning: implications for African fertility transitions. Ngom P. Ngom P. Stud Fam Plann. 1997 Sep;28(3):192-202. Stud Fam Plann. 1997. PMID: 9322335
- The causes of unmet need for contraception and the social content of services. Bongaarts J, Bruce J. Bongaarts J, et al. Stud Fam Plann. 1995 Mar-Apr;26(2):57-75. Stud Fam Plann. 1995. PMID: 7618196 Review.
- Estimating unmet need for contraception by district within Ghana: an application of small-area estimation techniques. Amoako Johnson F, Padmadas SS, Chandra H, Matthews Z, Madise NJ. Amoako Johnson F, et al. Popul Stud (Camb). 2012 Jul;66(2):105-22. doi: 10.1080/00324728.2012.678585. Epub 2012 May 4. Popul Stud (Camb). 2012. PMID: 22553978
- Meeting unmet need: new strategies. Robey B, Ross J, Bhushan I. Robey B, et al. Popul Rep J. 1996 Sep;(43):1-35. Popul Rep J. 1996. PMID: 8948001 Review.
- The impact of local supply of popular contraceptives on women's use of family planning: findings from performance-monitoring-for-action in seven sub-Saharan African countries. Kristiansen D, Boyle EH, Svec J. Kristiansen D, et al. Reprod Health. 2023 Nov 21;20(1):171. doi: 10.1186/s12978-023-01708-7. Reprod Health. 2023. PMID: 37990268 Free PMC article.
- Dynamic stagnation: reasons for contraceptive non-use in context of fertility stall. Jadhav A, Short Fabic M. Jadhav A, et al. Gates Open Res. 2019 May 7;3:1458. doi: 10.12688/gatesopenres.12990.1. eCollection 2019. Gates Open Res. 2019. PMID: 37795519 Free PMC article.
- Perspectives on the side effects of hormonal contraceptives among women of reproductive age in Kitwe district of Zambia: a qualitative explorative study. Mukanga B, Mwila N, Nyirenda HT, Daka V. Mukanga B, et al. BMC Womens Health. 2023 Aug 18;23(1):436. doi: 10.1186/s12905-023-02561-3. BMC Womens Health. 2023. PMID: 37596577 Free PMC article.
- Assessing the Suitability of Unmet Need as a Proxy for Access to Contraception and Desire to Use It. Senderowicz L, Bullington BW, Sawadogo N, Tumlinson K, Langer A, Soura A, Zabré P, Sié A. Senderowicz L, et al. Stud Fam Plann. 2023 Mar;54(1):231-250. doi: 10.1111/sifp.12233. Epub 2023 Feb 26. Stud Fam Plann. 2023. PMID: 36841972 Free PMC article.
- Measuring Contraceptive Autonomy at Two Sites in Burkina Faso: A First Attempt to Measure a Novel Family Planning Indicator. Senderowicz L, Bullington BW, Sawadogo N, Tumlinson K, Langer A, Soura A, Zabré P, Sié A. Senderowicz L, et al. Stud Fam Plann. 2023 Mar;54(1):201-230. doi: 10.1111/sifp.12224. Epub 2023 Feb 2. Stud Fam Plann. 2023. PMID: 36729070 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources, other literature sources.
- scite Smart Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Fear, opposition, ambivalence, and omission: Results from a follow-up study on unmet need for family planning in Ghana
Roles Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Avenir Health, Glastonbury, Connecticut, United States of America, The Demographic and Health Surveys (DHS) Program, Rockville, Maryland, United States of America
- Sarah Staveteig

- Published: July 31, 2017
- https://doi.org/10.1371/journal.pone.0182076
- Reader Comments
Introduction
Despite a relatively strong family planning program and regionally modest levels of fertility, Ghana recorded one of the highest levels of unmet need for family planning on the African continent in 2008. Unmet need for family planning is a composite measure based on apparent contradictions between women’s reproductive preferences and practices. Women who want to space or limit births but are not using contraception are considered to have an unmet need for family planning. The study sought to understand the reasons behind high levels of unmet need for family planning in Ghana.
A mixed methods follow-up study was embedded within the stratified, two-stage cluster sample of the 2014 Ghana Demographic and Health Survey (GDHS). Women in 13 survey clusters who were identified as having unmet need, along with a reference group of current family planning users, were approached to be reinterviewed within an average of three weeks from their GDHS interview. Follow-up respondents were asked a combination of closed- and open-ended questions about fertility preferences and contraceptive use. Closed-ended responses were compared against the original survey; transcripts were thematically coded and analyzed using qualitative analysis software.
Among fecund women identified by the 2014 GDHS as having unmet need, follow-up interviews revealed substantial underreporting of method use, particularly traditional methods. Complete postpartum abstinence was sometimes the intended method of family planning but was overlooked during questions about method use. Other respondents classified as having unmet need had ambivalent fertility preferences. In several cases, respondents expressed revised fertility preferences upon follow-up that would have made them ineligible for inclusion in the unmet need category. The reference group of family planning users also expressed unstable fertility preferences. Aversion to modern method use was generally more substantial than reported in the GDHS, particularly the risk of menstrual side effects, personal or partner opposition to family planning, and religious opposition to contraception.
Citation: Staveteig S (2017) Fear, opposition, ambivalence, and omission: Results from a follow-up study on unmet need for family planning in Ghana. PLoS ONE 12(7): e0182076. https://doi.org/10.1371/journal.pone.0182076
Editor: Ali Montazeri, Iranian Institute for Health Sciences Research, ISLAMIC REPUBLIC OF IRAN
Received: November 11, 2016; Accepted: July 12, 2017; Published: July 31, 2017
Copyright: © 2017 Sarah Staveteig. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Nationwide Demographic and Health Survey data are available for free upon registration with The Demographic and Health Surveys Program ( www.dhsprogram.com ). Per agreement with the ICF International Institutional Review Board, due to ethical concerns about re-identification of respondents, individual follow-up interview transcripts cannot be made publicly available.
Funding: This study was funded by the United States Agency for International Development (USAID) through The Demographic and Health Surveys (DHS) Program (#AIDOAA-C-13-00095). The funders had no role in data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The author has declared that no competing interests exist.
Unmet need is a central concept in family planning research and a key indicator for gauging the demand for contraception and for measuring the success of programs and policies. At its most basic level, unmet need reflects an apparent discrepancy between women’s stated reproductive preferences and behavior. In surveys some women respond they want to space or limit births, but they are not using any method to prevent pregnancy. These respondents are considered to have unmet need for family planning, and are at risk of unintended pregnancy. Unintended pregnancies frequently lead to unsafe abortions or maternal complications and place the health of mothers and children at risk [ 1 ].
In 2012 there were estimated to be more than 74 million unintended pregnancies in the developing world, including 4.6 million in West Africa [ 2 ]. The global burden of unintended pregnancy includes not only health of mothers and their children, but also costs for health care systems, social costs, and economic well-being of families worldwide. Family planning provides women and families the opportunity to plan and space births in line with their own reproductive preferences, helping to ensure the safety and well-being of both mother and children. Monitoring unmet need has taken on increased emphasis in recent years as policymakers seek to help women and couples achieve their reproductive goals. Reducing unmet need was part of the Millennium Development Goals. An indicator derived from unmet need, demand satisfied for modern contraception—computed as modern contraceptive prevalence divided by the sum of unmet need for modern contraceptive methods and modern contraceptive prevalence—is an indicator for the Sustainable Development Goals and a central part of new efforts by USAID and several donors to scale up family planning for millions of women as part of FP2020 [ 3 ].
The Demographic and Health Surveys (DHS) Program, the largest source of data on contraceptive patterns and unmet need in developing countries, conducts nationally representative surveys during which interviewers ask women questions about sexual activity, fertility preferences, fecundity, contraceptive use, and other topics. DHS and other nationally representative surveys, such as Multiple Indicator Cluster Surveys (MICS) and Performance Monitoring and Accountability 2020 (PMA 2020), compute unmet need for family planning based on a complex algorithm involving women’s responses to 18 questions asked at various points throughout the interview [ 4 ]. Married women, and in some cases sexually active unmarried women, who are fecund and wish to postpone giving birth for two or more years or stop childbearing altogether but who are not using any method of family planning are classified as having unmet need. Additionally, women who are pregnant or postpartum amenorrheic with an unwanted or mistimed pregnancy are considered to have an unmet need for family planning.
Specifically, women are considered to have unmet need if they are in any of the following three categories: (1) at risk of becoming pregnant, not using contraception, and want no more children, or want children but do not want to become pregnant within the next two years, or are unsure if or when they want to become pregnant; (2) pregnant with a mistimed or unwanted pregnancy; or (3) postpartum amenorrheic for up to two years following an unwanted or mistimed birth and not using contraception [ 4 ]. The calculation of unmet need does not involve direct questions about women’s own contraceptive preferences and proclivities; as such, it is described as a measure of latent or potential demand for family planning [ 5 , 6 ].
Relatively few women with an unmet need for family planning in developing countries cite cost or access as reasons for not using a contraceptive method [ 7 ]. Instead, survey respondents tend to cite fear of side effects, abstinence, breastfeeding, and attitudinal factors. The explanations underlying these stated reasons are not well understood.
The mixed methods follow-up study described in the present article leveraged the existing sampling structure and data collection within the 2014 Ghana Demographic and Health Survey (GDHS) to provide additional insights into reproductive preferences and barriers to family planning among women in Ghana with unmet need. The primary objective of the follow-up study was to better understand the lived experience and meanings underlying the apparent contradiction in fertility preferences and reproductive behavior that produce statistical estimates of unmet need in the DHS surveys. Do the survey questions about current family planning use and reproductive preferences retain their intended meaning in the field? How stable and well defined are women’s fertility preferences, and how do women explain their non-use of family planning? The study compares respondents classified as having unmet need with a reference group of respondents who were using family planning at the time of the survey.
Open-ended, qualitative questions can provide substantial insight into ambivalence, perceptions, and attitudes not readily apparent from large-scale survey data. Qualitative and mixed methods studies are well positioned to provide important insights about demographic behaviors [ 8 , 9 ] and are particularly relevant to understanding the meanings that respondents attach to responses in large-scale surveys such as the DHS [ 10 ].
The concept of unmet need
The development of the concept of unmet need is rooted in the KAP (Knowledge, Attitude, and Practice) surveys of the 1960s. Researchers identified married women whose preferences and behavior appeared contradictory—that is, they wanted to limit or space childbearing but were not using a method of family planning [ 11 ]. The KAP surveys gave way to the World Fertility Survey program in the 1970s and 1980s and ultimately evolved into the Demographic and Health Surveys (DHS) Program which covered a wider range of topics, starting in 1984. The algorithm for determining unmet need grew increasingly complex over time as questions on fertility preferences evolved and data from the contraceptive calendar were included when available. In 2012, a simplified, consensus DHS/MICS definition of unmet need was established using a standard algorithm [ 4 ]. A comprehensive history of unmet need and evolution of the classification schema has been detailed by other authors [ 12 – 14 ].
One concern with the concept of unmet need is that the term itself implies a demand for family planning—and, in fact, is summed with contraceptive prevalence to compute an indicator called “demand for family planning”—but the term does not necessarily reflect actual or potential interest in method use. In particular, it does not reflect how women themselves perceive their risk of pregnancy, the strength of their preferences, or their interest in or resistance to family planning. Additional concerns about the measurement of unmet need include the failure to differentiate married women who are sexually active from those who are not, and thus at no risk of pregnancy [ 12 ], the failure to include male partners [ 15 , 16 ], and instability in professed fertility preferences [ 17 – 20 ].
The extent to which survey measures of unmet need gauge latent demand for family planning has been questioned due to the temporal instability of the measure and the number of different groups it encompasses [ 21 ]. Even in the early days of the development of unmet need as a measure of demand for family planning, it was known that in some countries less than half of women with unmet need were currently at risk of pregnancy [ 14 ]; unmet need classification depends on prospective fertility preferences as well as on ex-post facto assessments of the intendedness of pregnancies and recent births. A technical working group for FP2020 opted against using reductions in levels of unmet need as a global goal because it is not a unidirectional measure of programmatic success [ 22 ].
Despite concerns about its measurement and interpretation, unmet need is a powerful concept. Abortions, surreptitious use of family planning, and unwanted pregnancies all attest to an ongoing need for family planning that is unfulfilled [ 23 ]. How to assess women’s ‘need’ or demand for family planning has proven difficult, however. In particular, evidence indicates that—even among survey respondents whose fertility operates within the “calculus of conscious choice”—the answers to prospective fertility preference questions are fraught with ambiguity and uncertainty [ 17 , 19 ]. Measures of unmet need depend on women’s tendency to plan and articulate fertility preferences in a two-year window. Fertility preferences are subject to both social context [ 5 ] and to vital conjunctures in women’s lives [ 24 ], including husband’s desire for children [ 16 , 25 ], future economic well-being, marital stability, and survival of current children. Longitudinal evidence finds substantial instability in individual women’s fertility preferences over time [ 26 – 28 ].
Study context
At the time this study was being designed, Ghana had recorded one of the highest levels of unmet need for family planning among married women on the African continent, at 36 percent in 2008 [ 29 ]. Family planning use had declined slightly among married women, from 25 percent in 2003 to 24 percent in 2008. Meanwhile, Ghana’s Total Fertility Rate (TFR) in 2008 was among the lowest in West Africa, at 4.0 births per woman. Unmet need is typically only measured among currently married women, but the focus of this study is currently married and sexually active women combined, as both groups of women are at risk of unwanted pregnancies. Nationwide, 29 percent of married and sexually active unmarried women in Ghana had an unmet need for family planning as measured by data from the 2014 GDHS.
Ghana’s attainment of regionally low fertility despite modest levels of family planning use has been a demographic puzzle for nearly two decades [ 30 ]. Abortion is legal in Ghana and has been hypothesized as a reason for lower-than-expected fertility [ 31 ]; but evidence has been inconclusive. It may be that high levels of unmet need in Ghana partly reflected women’s growing tendency to articulate a need for spacing or limiting births. During early stages of the demographic transition, the percentage of women with unmet need can increase even as demand for family planning is being satisfied simply due to women’s increased interest in reducing fertility [ 32 ].
Ghana has a relatively strong family planning program. The contraceptive method mix is diverse. Injectables, the pill, and implants are the most common methods, followed by the rhythm method. Women can obtain contraception from public and private sources. Family planning is inexpensive but not free. Ghana does experience occasional contraceptive supply issues and there are some limits to the method mix offered. Social marketing campaigns have proven successful but some very remote areas of the country remain a few hours’ distance from the nearest clinic. Even so, in surveys women rarely cite access and cost as reasons for non-use of family planning [ 33 ].
By 2014 the TFR increased slightly, to 4.2 births per woman [ 34 ]. The 2014 GDHS also found an increase in modern contraceptive prevalence since 2008 (from 17 to 22 percent) and a decline in unmet need (from 36 to 30 percent) among married women ages 15–49. This brings the country on par with levels of unmet need in neighboring West African countries, but still high in a global perspective.
Perceptions about side effects and attitudinal factors pose a challenge to increased family planning use in Ghana. Focus group discussions from a hospital in Ghana found women’s concern with menstrual regularity results in dissatisfaction with family planning methods that prevent menstruation [ 35 ]. Another study found that many Ghanaian women perceive family planning as ineffective or unsafe [ 36 ], and DHS data from 1988 to 2008 show that attitudinal resistance has been an increasing component of unmet need in Ghana [ 33 ]. Male attitudes toward contraception are mixed: in the 2014 GDHS, 73 percent of men age 15–59 rejected the idea that contraception is a woman’s business and men should not have to be involved, but 46 percent supported the statement that women who use contraception may become promiscuous [ 34 ]. Married Ghanaian women’s sexual empowerment is a statistically significant predictor of contraceptive use, even after controlling for other factors [ 37 ].
This study was designed as a data-linked embedded follow-up study, of the type described by Schatz [ 38 , 39 ]. It was independently funded, planned, and fielded, but respondents were systematically selected from among the respondents to the 2014 GDHS. The 2014 GDHS is a nationally representative household survey in which 9,396 women age 15–49 were interviewed [ 34 ]. Fieldwork for the GDHS was conducted by the Ghana Statistical Service (GSS) and the Ghana Health Service (GHS), with technical assistance from ICF International through The DHS Program, which is funded by USAID. At the end of the GDHS, all 9,396 female respondents were asked for consent to be re-contacted for a follow-up study on family planning. Nationwide, 99.6 percent of women agreed to be re-contacted.
The follow-up study selected three of ten regions for follow-up: Greater Accra, the capital, Central Region, and Northern Region. Central Region had the highest level of unmet need in 2008 and Northern Region has typically had higher fertility and low family planning use. In all, 13 survey clusters were selected for follow-up fieldwork five in Northern Region, five in Central Region, and three in Greater Accra, the region with the lowest fertility. It was decided in advance that all three clusters selected in Greater Accra would be urban, and that one of the five clusters in Central Region and in Northern Region would be urban. A completely random selection of clusters from the parent survey would not have been feasible. Fieldwork for the GDHS takes four months, versus one month for the follow-up study, and it was desirable to return within three weeks. Additionally, for a small-scale study the distances might have been prohibitive. Thus cluster selection was based on those available at the time of the study, with an eye toward geographic diversity. However, within a given cluster women were selected systematically, from among those surveyed in a stratified random sample rather than a convenience sample typical for qualitative studies.
Fieldwork for the follow-up study was conducted by the Institute for Statistical, Social, and Economic Research (ISSER) at the University of Ghana, Legon. Preparation for interviews began with an 11-day training and pretest in Accra. Along with a guide from GSS, three field teams each consisting of two interviewers and a field supervisor attempted to relocate the selected DHS respondents within three weeks of the original survey. Interviewers returned up to three times to complete the interview. Interviews were randomly audited to ensure that they were correctly completed. Follow-up interviews were conducted anywhere from 5 to 60 days after the GDHS interview; on average women were reinterviewed 20 days after their GDHS interview. Survey procedures are described in detail elsewhere [ 40 , 41 ].
The overall response rate was 92.3 percent (131 of 142 women selected). Of these 131 respondents, 96 qualified for analysis. Fig 1 shows detailed sample selection criteria. This article analyzes 96 respondents, the 50 women who were classified by the GDHS as having an unmet need for family planning, alongside a reference group of 46 women who were identified as having a met need for family planning.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0182076.g001
Respondents to the follow-up survey were located by address, name of household head, and relationship to the household head; to verify their identity, respondents were asked six additional questions: year of birth, month of birth, marital status, whether ever given birth, number of resident sons, and number of resident daughters. The vast majority of respondents matched on all or all but one characteristic. The 96 cases discussed here reflect confident—but imperfect—identity matching. Prior studies have found inconsistent results on key questions, even with the exact same survey conducted after only a short delay [ 42 , 43 ]. Discrepancies in responses were flagged so that interviewers could inquire further.
Follow-up interviews were conducted using Android tablets to import respondent data and guide questions; audio recorders were used to capture women’s full responses to each question. Questionnaires were translated into three languages—Twi, Ga, and Hausa. The semi-structured questionnaires included a combination of closed and open-ended questions about reproductive preferences, ambivalence, decision-making, and family planning (see S1 File ). Respondents were also asked open-ended questions about fertility desires, family planning use, attitudes toward family planning, role of partner and extended family in decision-making, and barriers to access.
After fieldwork was complete, audio files from the interviews were transcribed into the language of the interview and subsequently translated into English, resulting in over 1,000 single-spaced pages of transcripts. Transcripts were input into ATLAS.ti qualitative analysis software. A number of themes were established and listed at the start, based on the questionnaire, while additional themes were added inductively by iteratively reading transcripts. A list of themes was developed, refined, and independently applied to a set of test transcripts by two raters to compare reliability. After finalizing the schema, the themes were consistently applied to the transcripts in ATLAS.ti. Variables created directly from tablet entry information were reviewed for missing and inconsistent values and, when possible, filled in or manually verified against transcripts. These data were confidentially linked to publicly available GDHS records and analyzed using Stata.
Ethical considerations
The ICF International Institutional Review Board (IRB), which requires compliance with the U.S. Department of Health and Human Services regulations for the protection of human subjects (45 CFR 46), reviewed and approved all study procedures and questionnaires. A waiver of written consent was obtained from the IRB due to minimal risk of harm and a lack of procedures for which written consent is normally required. Respondents were asked for verbal consent to be re-contacted during the main survey and for verbal consent to be interviewed and to be audiotaped at the start of the follow-up interview. Before the interview began interviewers were required to provide their electronic signature attesting that they had received verbal consent from the respondent to be interviewed and that they had correctly indicated whether the respondent consented to be audiotaped.
In keeping with IRB regulations and The DHS Program’s practices, the confidentiality of the respondent’s information was maintained at all stages of the survey. Recordkeeping used anonymous cluster and respondent identifiers. As voluntary HIV serotesting was conducted during the 2014 Ghana DHS, no data entry on names or addresses was done and all cluster and household numbers were scrambled prior to linkage with HIV test results. Similarly, at the conclusion of fieldwork the implementing agency for the follow-up study destroyed all identifying information used to contact respondents, maintaining only an anonymized identification number. A linkage between the anonymized identification number for the follow-up study and the final, publicly available dataset is kept only by The DHS Program.
Sample characteristics
The 96 married and sexually active unmarried women analyzed in this article were systematically selected from among GDHS respondents. The follow-up sample was intended to be diverse, but given the scale of the study, the sample was not designed to be perfectly representative of the three regions. Table 1 indicates how the characteristics of the sample as defined in the GDHS compared with family planning users and with women who had an unmet need in the three selected regions. GDHS sample weights are applied to regional percentages and to the sub-study respondents. Table 1 shows that respondents to the follow-up study were more concentrated in their 30s than their respective regional counterparts. Fewer follow-up respondents were age 15–19. Follow-up respondents were more predominantly rural than both family planning users and women with unmet need in the country as a whole.
https://doi.org/10.1371/journal.pone.0182076.t001
Women who reported using family planning in the GDHS were more highly educated and wealthier than women with unmet need. Both follow-up samples were over-representative of the lowest wealth quintile than the regional averages. The follow-up sample exhibited religious diversity, but was more heavily traditional/spiritualist and no stated religion than women nationwide in both the unmet need and family planning groups. One of the clusters in the North was Konkomba-speaking, and respondents were ethnically Gurma; the follow-up study sample was thus much more heavily comprised of Gurma women than the country as a whole.
Reproductive characteristics of the four groups (regional and follow-up respondents who were family planning users and who had unmet need in the GDHS) are shown in Table 2 . Women’s knowledge of family planning methods is high in Ghana. Nationwide, over 99 percent of women with unmet need know at least one modern method. In the follow-up survey, one respondent was identified by the GDHS as not knowing any method of family planning, another as only knowing traditional methods. The majority of women with unmet need have used a family planning method before.
https://doi.org/10.1371/journal.pone.0182076.t002
Fertility preferences
Fertility preferences are a pivotal component of unmet need. Among fecund women, declared intention to have a/another birth and the preferred timing of the next birth determine unmet need status. The two questions on reproductive preferences used to compute unmet need for this group are: (1) “ Would you like to have (a/another) child , or would you prefer not to have any (more) children ? ” Allowable responses to this question are: (a) want a/another; (b) no more; (c) cannot get pregnant; (d) a special condition, such as ‘after marriage’; or (e) don’t know/undecided. Non-pregnant respondents who want a/another child are then asked: (2) “How long would you like to wait from now before the birth of (a/another) child ? ” Pregnant women are asked: “After the child you are expecting now , would you like to have another child , or would you prefer not to have any more children ? ” The answer must either be a specific number of years and months, a special wait condition, or undecided. While the questions used to ascertain fertility preferences are seemingly straightforward, women’s ability and willingness to articulate a fixed timeline for their preferred time to next birth are culturally and temporally variable.
Non-pregnant respondents who want no more children and meet criteria for fecundity and non-use are considered to have an unmet need for limiting. The consensus definition of unmet need uses a threshold of two or more years to determine whether women have an unmet need for spacing. A comparison between responses to the question from the GDHS and the follow-up survey are shown in Table 3 . As the table indicates, 18 percent of follow-up respondents with unmet need and 13 percent of follow-up family planning users gave inconsistent answers to this question between surveys. The shift in responses occurred largely among women who stated they were undecided in the GDHS but said they wanted another child upon follow-up. There was some additional negligible movement in both directions between wanting no more children and wanting another child during the follow-up.
https://doi.org/10.1371/journal.pone.0182076.t003
The main ambivalence in fertility preferences that emerged through interviews was not whether to have another child, but the timing of that preference. In the GDHS, responses to question about desired timing of the next birth were limited to a single number of months or years, or to a special wait condition. In the follow-up survey women were allowed to specify an open range of desired time until the next birth. Responses to this question, grouped by minimum wait time into one-year intervals, are shown in Table 4 for follow-up respondents with unmet need. Figures include the eight respondents who said in the GDHS that they were undecided or that they wanted no more children but declared in the follow-up survey that they wanted a/another. Twenty of 31 respondents indicated a desire to wait until a single point in time, while the remainder gave a time range, averaging 23 months.
https://doi.org/10.1371/journal.pone.0182076.t004
Of the respondents classified as having unmet need who indicated in the follow-up interview that they wanted a/another birth, 11 declared in follow-up a minimum desired waiting time of less than two years. For seven of these 11 respondents, two years encompassed both the minimum and maximum waiting time, which would have classified them as having no unmet need. The other four respondents gave a range of time that started before two years. If they had been asked to give a fixed number and settled on less than two years, they would also have been excluded from the group defined as having unmet need.
The follow-up survey also asked women the strength of their desire to wait that long for the next birth. Results are shown in Table 4 . Desires to delay were weakest among women who expressed a preference to wait one to three years; they tended to be strongest at the highest and lowest time boundaries.
A main theme that emerged from the discussion of fertility preferences overall was that respondents felt torn between joy versus means—or in many cases torn between the potential future value of a child (who could be the “star of the family”) versus the immediate cost of raising a child. Respondents and their partners valued children highly, but most respondents perceived an inherent trade-off between the value of another child and the financial or health costs of too many or closely spaced births. For example, as a 35-year old woman in urban Central Region (R03.08) described:
Well, it would be good to have another child, and it would be especially good to have a safe delivery. Even the Bible tells us that children are a blessing and a gift from God, so if I have another child and am able to take care of him or her such that he grows to become responsible and respectable person, it would even bring honor to me. People would point at him and say, oh there goes Sister [Name]’s son, and that would bring me fulfillment and joy… I do not know how far the child might go in life; he might even be an important personality and bring honor to our family, so that could be a value that having lots of children might bring us… Even if you look at the Bible, it says to be fruitful and multiply and to replenish the earth, it’s out of many children that some grow to be important personalities of the world but it’s due to economic and financial hardships that people face that’s why they may decide to have fewer children but ideally, you should have more, you never know which of your children would be of significance someday .
Respondents frequently indicated that they would accept an unwanted pregnancy but would not be happy. “ I don’t like it but if it comes I will accept it” or “ I will not be happy but once it has come I will accept it” was how seven respondents (R01.01, R01.03, R01.05, R02.03, R02.07, R04.02, R05.07) described their attitude toward having another child. “I will be disturbed but I will be happy to have a child” said another (R01.07).
For the 11 respondents identified as having an unmet need whose timing shifted below the two-year threshold, including those who had originally said no more, two themes emerged. First was an overall ambivalence toward pregnancy, not simply conflicted feelings but also a sense of fatalism. The majority of women in this category were in rural areas and had parity of four or more. The second theme that emerged was that the respondent had a partner who would be happy or very happy about another birth while the respondent herself did not feel strongly. For example, one 40-year old rural respondent in the Northern Region with seven children (R13.02) who changed from wanting no more children to wanting a child now indicated the decision was her own, but that she was deferential to her husband’s preference.
I know [my husband] likes children even though we have nothing. Take a look at my house, we don’t have strength but we are managing with life… We talk all the time. He said we are going through a tough time but do we still want more children or we should try a method? And I said whatever you decide I have no problem with it… I would like to have another child any moment from now .
In sum, 41 of 50 respondents with unmet need consistently answered the question about desirability of a/another child in the GDHS and the follow-up. The main source of inconsistency was movement from undecided to wanting another child. Including respondents who changed from wanting no more children to wanting a/another child, there were 11 cases where the stated time to next birth moved into the two-year range, seven of which (14% of unmet need sample) would have meant that women were not classified as having unmet need.
Discrepancies in reporting of method use
At the beginning of the follow-up survey, after questions to confirm key identifying characteristics, non-pregnant women were asked if they were currently using family planning. The wording of the question was the same as in the DHS (“Are you currently doing something or using a method to delay or avoid getting pregnant ? ”) . Unlike in the DHS, however, women who responded “no” were prompted about natural methods (“What about the rhythm/calendar method ? What about withdrawal ? ”) .
A comparison of method use reported in the GDHS and the follow-up survey is shown in Table 5 . Out of 44 non-pregnant respondents that the GDHS determined to have unmet need for family planning, 15 (34 percent) reported in the follow-up interview that they actually were using a method of family planning. Five reported using a modern method, nine reported a traditional method, and one reported both. Additionally, three respondents who said they were using a method in the GDHS reported not using a method in the follow-up study.
https://doi.org/10.1371/journal.pone.0182076.t005
Respondents who reported discrepant use of a method in the GDHS and the follow-up survey were closely examined for identity verification questions and checked against other women in the household to see whether the follow-up interview may have been conducted with the wrong household member. None of the GDHS respondents with unmet need who reported using a method at the time of follow-up lived in a household with another woman who used a method. All matched on at least seven of nine pieces of identifying information.
Some of the women may have started or stopped a method in the intervening days between interviews. In cases where women were asked about the discrepancy, none reported starting between interviews. Two users of modern methods said that they were using a method and had told the GDHS interviewers but it was not recorded. The DHS question on method use is specifically intended to be inclusive of traditional methods (“doing something or using a method to prevent pregnancy” ) and in the DHS interview, immediately prior to the question on current method use, respondents are asked whether they have heard of a list of methods, including rhythm or calendar, withdrawal, and lactational amenorrhea. They are read a brief description of each method type. But the main theme that emerged among respondents who reported natural methods was that they misinterpreted the GDHS question about method use as being about modern methods. For example, here is an exchange with a 26-year old woman in an urban part of Central Region (R05.06):
Interviewer: I’d like to begin by confirming the information I received . Are you currently doing something or using any method to delay or avoid getting pregnant ? Respondent: No , I am not on any medication . Interviewer: Yes , I understand you may not be on any medication to prevent pregnancy but there are other ways of preventing pregnancy such as the rhythm or withdrawal methods . Are you currently using any of these to prevent pregnancy ? Respondent: Oh , yes , I didn’t understand at first . I use the withdrawal method . Interviewer: Please according to the information I have from the previous interviewer , you are currently not using any method or means to prevent pregnancy . Is that information correct ? Respondent: Yes , it is . When they came they only asked about the modern methods of family planning . They didn’t ask about the rhythm and the withdrawal like you did . That is why I said no but my husband and I use the withdrawal .
Four other respondents reported similarly that they understood the question as being about modern methods. As a 33-year old woman in a rural part of Central Region (R04.05) stated: “When they asked this question , they asked about the family planning , they didn’t explain that the methods included rhythm and withdrawal , that’s why . ” Overall, of the ten women who had been classified by the GDHS as having unmet need but who reported natural methods, eight initially answered “no” to a repeated GDHS question about method use and only revealed natural method use after they were asked about rhythm and withdrawal.
Unmet need for family planning is designed to be computed among women who are exposed to the risk of unintended pregnancy. Exposure to the risk of pregnancy is assessed in two stages: first through self-reported sexual activity, and second through estimated fecundability. As mentioned, the definition of unmet need can apply to sexually active unmarried women as well as married women. By definition, all women who are currently in union are assumed to be at risk of pregnancy [ 4 ]. The obvious concern about this assumption is that a non-negligible proportion of women who are currently in union report long spells of sexual abstinence, for example, due to spousal migration or postpartum abstinence. A recent analysis finds that, along with fear of side effects, infrequent sexual activity is one of the two most common reasons cited for not using family planning among women with unmet need in Africa, Asia, and Latin America [ 7 ]. If all women who cited infrequent sex or abstinence as a reason for non-use were excluded from the definition of unmet need, the overall level of unmet need would decrease by a country average of 16 percent [ 12 ].
Apart from the underreporting of the rhythm and withdrawal methods, one additional type of omission that emerged from follow-up interviews was the intentional use of prolonged abstinence, particularly during the postpartum period, in order to space births. While the practice of postpartum abstinence has long been known as a dimension of birth spacing in Central and West Africa [ 44 ], and abstinence is the most effective way to prevent pregnancy, prolonged abstinence is not typically considered as a traditional method of family planning by surveys such as DHS. Respondents are asked about the date of last sexual activity separately from questions about methods to prevent pregnancy.
What is missing from DHS assessments of abstinence but emerged from the follow-up interviews is the intentionality behind abstinence. In their follow-up interview, 8 of 44 non-pregnant respondents indicated that abstinence was intentionally ongoing and was designed to prevent pregnancy. For example, one respondent, a 36-year old woman in a rural part of Northern Region (R12.05) said “if he sleeps with me I will be pregnant , and I don’t want to be , and he is okay with the decision [to be abstinent] . ” Others cited lengthy durations of postpartum abstinence for the purposes of birth spacing. “The gods we worship do not allow [family planning] so when you have a small child you avoid sex” was how a 20-year old respondent (R10.03) described it. A 31-year old rural woman in Northern Region (R10.05) responded, “We discussed that the child is small so we should wait for the child to grow first and because of that , I don’t sleep in the same room with my husband again … my husband said he will not touch me until my child grows . ”
Abstinence within marriage is typically considered a temporary state that does not preclude unmet need, as the woman may be at risk of unwanted pregnancy as soon as the abstinence ceases. Indeed, some women indicated that they were abstinent because their husbands were traveling, or that they were withholding sex because of womanizing; such abstinence is involuntary and, based on their fecundability, these respondents will be ‘in need’ of a family planning method as soon as sex resumes. But the most recurrent reason women cited for abstinence was that it was intentionally designed to avoid pregnancy, typically to allow time for their youngest child to grow, and thus unlikely to cease soon: in other words, abstinence was being used as a method of family planning.
The GDHS did not ask about abortion, but follow-up respondents were asked if they had ever had an abortion, and if so how many times. Underreporting of abortion is always a concern in surveys. The follow-up study prefaced the abortion question with phrasing used in prior surveys: ( “Women sometimes take steps to end their pregnancy , for example if they find themselves pregnant when they do not want to be , or when it is difficult for them to continue with their pregnancy because of opposition from their husband , partner , relatives or others . ”) Then, instead of asking whether women had deliberately ended a pregnancy, we asked using local terminology: "Have you ever been in a situation where you or someone else have had to 'put your hand' to your pregnancy ? " If needed, interviewers clarified that they were asking about abortion. The majority of respondents reported never having had an abortion: 10 percent of women with unmet need and 28 percent of GDHS family planning users reported having had an abortion, mostly only once. The pooled result, that 19 percent of all respondents reported having ever had an abortion, is broadly consistent with the 2007 Ghana Maternal Health Survey, which found that 15 percent of all women reported having had an abortion in their lifetime [ 45 ].
Reasons for non-use of family planning
In discussing use and non-use of family planning, five themes emerged: gaps in knowledge, fear of side effects, cost and access, the role of male partners, and religion.
Gaps in knowledge.
Knowledge of contraception is nearly universal in Ghana; in 2014 the GDHS found that 99.5 percent of currently married women know of a method of family planning, and that women know on average nine different methods. Even so, a few interviews revealed gaps in knowledge and education. At the extreme were a small number of respondents who did not know a method or did not know how to access a method, mostly in the rural Northern part of the country. Women’s own perception of their risk of pregnancy occasionally seemed to reflect an opportunity for additional education about fecundity and biological processes.
Interviewer: You have told me you don’t really want to have any child even though your husband wants another baby , please why are you not using any method to delay or prevent getting pregnant ? Respondent (age 40, rural Central Region, R05.04): I won’t get pregnant . I’ve advised my womb not to get pregnant again so I won’t get pregnant … I’ve learnt about family planning . I just don’t want to use any method . My womb is a family planning on its own .
Responses that suggested a lack of knowledge about family planning or biological processes were fairly infrequent, but they do suggest that outreach to rural communities and to men, who hear about side effects mostly from rumors, may be particularly helpful. Additionally, respondents sometimes seemed to have difficulty differentiating the possible side effects of IUDs, implants, and the pill from side effects of injectables.
Fear of side effects.
Among women classified as having unmet need, fear of side effects was by far the most commonly-cited reason for not using modern methods. The theme of side effects arose in 34 of the 50 interviews with follow-up respondents who had unmet need in the GDHS. The side effect mentioned overwhelmingly was menstrual disorders, specifically the absence of menstruation caused by hormonal methods. The second most frequent side effect mentioned was weight gain on injectables. For example, one 38-year old respondent in Greater Accra with four children (R06.05) described:
Respondent: Previously , I use the injection but I stopped when I gave birth to my daughter . Interviewer: So why did you stop ? Respondent: The side effect I had was that anytime I go in for the injection , I grow big and my stomach also grows big; that is why I stopped . With the injection , your menses does not come regularly , but as human beings our menses is supposed to come regularly .
This quote exemplifies an important theme from discussions with respondents: the absence of menstruation was seen as not just as an undesirable trait of modern methods, but also as a marker of disease or even a possible cause of disease in the body. Other side effects, including headaches, dizziness, nausea, heart palpitations, chest pains, and high blood pressure, were mentioned infrequently. Respondents occasionally expressed that they or their partners were also concerned about difficulty conceiving after they ended use. Typically, side effects were something women themselves had experienced or had heard about from a friend or family member’s experience. In a few cases women had tried multiple modern methods without satisfaction. As one respondent explained:
Personally, when I use those modern methods, it does not help me. It has an effect on me. After I removed the IUD, I wanted to try some method but I realized that for exactly a year it was disturbing me. For me to get to the hospital, I was helped by people to sit in a car. My waist, I could not help it at all; that is why I wanted to remove it. As I got to the hospital and told the nurse what I was going through, she said, if that is the case, for me to be free, it has to be removal. Now I am free after it was removed. After that, I went to the doing store to buy another method [pills]; when I take it, I feel a burning sensation in my whole body. I realized that none of the family planning methods are good for me, so I’ve discussed with [my husband] not to use any type of contraceptive. So at least if anything, he will withdraw. I also use my date to calculate . (Age 35, Greater Accra, four children, R06.10)
In addition to side effects, some respondents expressed an overall dislike of chemicals or hormones in their body, even an acceptance of some myths around modern methods. For example:
The clinic and hospital are near us; when you step in you will get it done. The monetary aspect is not expensive, but when you consume it is expensive because it can cost you the future… I don’t want to consume more chemicals into my system… I will rather just abstain from sex . (Age 44, urban part of Northern Region, five children, R11.07)
Some respondents indicated that if not for their bad experience with modern methods they would have wanted years or even decades of protection against pregnancy but now are determined not to use modern methods. In some cases, their experience led them to a preference for a traditional method. For example, a 42-year old respondent in Greater Accra with three children (R05.06) described:
Respondent: I have used the family planning before [injectable] but I developed health issues. As I speak now I have high blood pressure due to the method I used, so now I have to use the withdrawal . Interviewer: So, you are currently using the withdrawal to prevent pregnancy. Why did you choose to use the withdrawal? Was it what you most preferred? Respondent: Well, first of all, I want to avoid getting pregnant and secondly, I do not want to develop any other health conditions due to the side effect of a family planning method. In my case, I have a lot of issues. I do not even menstruate [on injectables]. So I think the withdrawal is better .
Women who expressed a preference for traditional methods were often urban and educated. Although the study sample was too small to draw definitive conclusions about women of a particular educational group and area, this trend is consistent with evidence from Cameroon of a distinct preference for traditional methods among educated, urban women [ 46 ].
Cost and access.
Follow-up respondents were asked about perceived cost and access barriers to obtaining contraception. Table 6 displays the results on cost and access barriers among non-users compared with confirmed users. Here we can see that 15 percent think modern contraceptives are difficult to access and 16 percent think they are expensive, compared to 12 and 10 percent respectively among users. The more important difference is in the don’t know category: an additional 16 percent of non-users don’t know if contraception is difficult to access, most because they have never tried to obtain it, and 38 percent don’t know if it is expensive.
https://doi.org/10.1371/journal.pone.0182076.t006
As indicated in Table 6 , 15 percent of respondents with unmet need perceived access barriers to contraceptives. Access barriers include not only distance to health facility, waiting time, and availability of supplies, but also operating hours: a study in the Nkwanta district of Ghana found that favorable opening hours was the most significant access factor [ 47 ]. Most respondents mentioned that contraception was available in hospitals, clinics, and pharmacies. “Every pharmacy sells some . Immediately you mention what you want , they will give it for you unless they don’t have some , ” said one 35-year old respondent in Greater Accra (R06.02). Another 40-year old respondent in rural Central Region (R02.07) said, “They can easily be accessed from the hospitals and the pharmacy shops at a low cost . ” The only concerns about access tended to be in rural Northern villages. “There is no way you can access the service in this village . We have to travel to the clinic which is far from here , to get the service” (Age 37, rural Northern Region, R13.12).
Family planning is not free in Ghana, but it tends to be offered at very low cost. Among confirmed non-users of modern methods, 38 percent were unaware of cost or had had no opinion on it. Only one respondent explicitly cited a cost barrier. In general, most respondents with unmet need felt that expense did not pose a barrier. As a 41-year old woman in rural Central Region (R02.01) said, “For something that you can use to avoid pregnancy and space your child births , it should have been really expensive , but it has been made in such a way that everyone can afford to use it . ” At the same time, this woman said she preferred traditional methods.
Consistent with the GDHS, in the follow-up study the majority of respondents with unmet need reported knowing a source of family planning. In general, contact with health care facilities had a positive or somewhat neutral influence on non-users. Women reported having been educated through their contact with fieldworkers and health providers. Cost and access emerged in follow-up interviews, but not as a central theme for non-use.
The role of husbands and partners.
In discussing their decisions about family planning, interviewers asked women about the role of their husband, live-in partner, or boyfriend. Transcripts were thematically coded for whether the woman indicated at any point that her husband or partner opposed family planning and for whether he supported or accepted it. Half of the 32 confirmed non-users mentioned at least once that their husband opposed family planning. As one respondent in rural Central Region (R02.01) described, “He always says that if the fish had decided to use family planning , would we have gotten any to eat ? He is against it . ” However, she felt that his opinion was not important to her and she avoided family planning for other reasons. Compared with non-users, only a minority of family planning users indicated that their husband or partner opposed family planning.
In some relationships men acted as gatekeepers, either allowing or refusing family planning. One respondent, a 37-year old woman in rural Northern Region (R13.12), said “I have to get his consent before I go in for the service . ” Other respondents with unmet need said that they did not have permission from their husband to use family planning and so they were not using it. Women’s empowerment within the relationship was an important factor. Some women were willing to use family planning irrespective of their husband’s opinion. For example, a 35-year old married woman in urban Central Region (R03.08) explained:
My husband’s role is very important. You see he opposed it initially because of the rumors about side effects. So when he realized I had been using it for three years and yet had not experienced any of those side effects he had heard about, he realized it was safe after all and gave his consent. He even started encouraging and reminding me to take the pill because he realized I was only helping him and had the family’s best interest at heart .
In other relationships, women referred to a joint discussion about family planning. One respondent who uses the pill recounted her conversation with her husband this way:
My Mom told me that because of the way the world is today, I mean about the hardships, so we should space our births so that we don’t have to have such a hard time. So I went to tell [my husband] what she had said and he said that it doesn’t matter because when it was their turn to have children, nobody stopped them, and they had as many children as they wanted and only stopped when they were much older and couldn’t have any more. Then I told him that the economic conditions of today are not as pertained back in their days so we should try and space our births so that we will be able to cater for our children’s needs in relative comfort. So that when we’re able to, we’ll continue having other children. Then he said that even if I become pregnant now, he will be very happy. I told him that there was no way that would happen because I am using a method to prevent pregnancy. Then he said he’s okay with it . (Age 31, rural Central Region, four children, R04.06)
Overall, husbands and partners were both a positive and a negative influence on women’s decisions about family planning; users and non-users rated the role of their husbands or partners in their decision to use or not use a method equally.
The role of religion.
Respondents came from a diversity of religious backgrounds, including Christian, Muslim, and atheist. In the follow-up survey women were first asked about their religion and how their religion viewed family planning. Women’s interpretation of their religion’s views on family planning varied widely. Some Christian and Muslim women said that it was opposed; others characterized their religion as being tolerant of or even encouraging family planning. Women were then asked whether their religion’s views influenced their decision to use or not use family planning.
Many women indicated that their religion was supportive of family planning or that religion was negative but did not have an influence. For example, here is one exchange with a married respondent, a 35-year old woman in a rural part of Central Region with four children (R04.07):
Interviewer: Please can you tell me a bit about your religion’s views on family planning . Respondent: They say it’s not good. According to them, the Bible says that we should be fruitful and multiply and replenish the earth so if you do that, it’s a sin against God . Interviewer: So is this view the reason why you’re not using family planning? Does this view influence your decision to not use it? Respondent: Oh, no. According to the Bible, God helps those who help themselves. So it may be true that that’s what the Bible says but you also have to help yourself by guarding against difficulties and hardships. So if you have to use it, you must use it. Having lots of children brings nothing but hardship .
In Ghana, some religious practices have made an effort to promote family planning. One current IUD user who was classified as Pentecostal/Charismatic by the GDHS described the positive influence of her church:
There was a lecture / education in our church to the women’s group on what women go through during child birth, caring for the babies, financial problems and how to space the children so that you don’t get pregnant as a Christian and cause abortion which brings problems and sin into our lives. So they have realized that family planning is good for the woman to protect herself and gives you the woman the freedom to do your work to take care of them. I went to church that day and came to inform my husband that this childbearing is something else. I told him that in order for me to not get pregnant and cause several abortions he should allow me to go and fix a family planning method. They were also featuring some advertisements about the family planning on the television, radio and everywhere you go. And he said if that is the case, if [family planning] will not bother me, then I should go for it. He even said that if we decide that we will not have any more children, then it is okay . (Age 42, Greater Accra, five children, R07.04)
While religious support could clearly be helpful or even conducive to initiating use of family planning, religious opposition was also an important reason for non-use. Around half of non-users said that religious opposition to family planning influenced their decision not to use family planning. These respondents tended to cite their traditional, fundamentalist Christian faith or Muslim faith as being opposed to family planning. Respondents whose religion opposed family planning tended explain in simple and absolute terms:
My religion preaches that any means to prevent a pregnancy is equal to committing abortion and this is a sin . (Age 44, urban Central Region, nine children, R03.02) My religion says it is not good for a Muslim to use family planning . (Age 29, rural Northern Region, four children, R13.05)
Overall comparison of reasons for non-use.
The GDHS survey asked most women with unmet need about their reasons for non-use in an open-ended way. (“You have said that you do not want (a/another) child soon [or : You have said that you do not want any (more) children . ] Can you tell me why you are not using a method to prevent pregnancy ? Any other reason ? ” ) Nationwide in 2014, among married and sexually active unmarried women classified as having unmet need who were asked why they were not using a method of family planning, 49 percent stated that fear of side effects or health concerns was a reason for non-use. (Note: Multiple reasons are allowed; women who are pregnant or who have undefined fertility preferences are not asked this question.)
Toward the end of the follow-up survey, women who confirmed that they were not using family planning were asked the same open-ended question. For the 30 women who were asked the GDHS question about non-use, reinterviewed for the follow up survey, and confirmed as non-modern method users, I examined the follow-up transcript for reasons for non-use, including the repeated question when applicable. Table 7 shows the results of this comparison by reason type. Each reason and its count from the GDHS are shown. On the right-hand side, the table shows the percentage of cases where that theme was independently confirmed as a reason for non-use of family planning. I also show the number of respondents who indicated that theme as a reason for non-use in the follow-up survey but had not mentioned it in the GDHS survey. On average, respondents gave 1.1 reasons for their non-use of family planning in the GDHS but 3.0 reasons in the follow-up; the latter estimate would have been higher if respondents who reported actually using a method were excluded.
https://doi.org/10.1371/journal.pone.0182076.t007
The follow-up study was interested in independently understanding unmet need; no attempt was made to quiz respondents on the validity of the reason they gave to the GDHS for non-use. The results shown in Table 7 indicate that fear of side effects, a major theme from the GDHS, was mentioned as a reason for non-use among 23 of 30 respondents. Opposition from husband or partner and religious opposition also appeared to have been underreported in the GDHS. Meanwhile, despite additional prompting on cost and access, no additional cases where cost or access posed a barrier were found.
Some respondents gave reasons not mentioned in the GDHS that are included in Table 7 . Two were explicitly fatalistic about non-use of family planning (“ we are under the care of the gods so am not using anything to protect myself” said a 20-year old respondent in the rural Northern part of Ghana, R09.06). Two said they needed more information; one planned to start family planning soon. Seven of the 30 women interviewed had revised their fertility preferences within the two-year window, and five others (R05.02, R05.04, R06.01, R09.02, R09.06) included a statement along the lines of “I just don’t want it , ” or “My heart does not like it . ” Reliance on abortion did not emerge as a theme for any respondents.
This article endeavored to describe the local meanings and lived experiences behind women’s survey responses that produce measurements of unmet need in surveys such as DHS. A complete picture of unmet need requires examining not just barriers to family planning and resistance to modern contraception but also perceptions of risk of becoming pregnant and fertility preferences that precede interest in the use of family planning. A major finding is the level of discrepancy between interviews in two key pieces of information that determine unmet need status: contraceptive use and fertility preferences. DHS respondents underreported use of family planning, particularly traditional methods. Additional prompting on traditional methods was expected to detect some underreporting of traditional method use, in line with findings from two prior surveys in West Africa that used simulated DHS questions [ 48 , 49 ]. The magnitude of the omission (23 percent) was surprising, however.
An additional theme that emerged was that focusing on periodic abstinence as the only type of abstinence valid for purposes of family planning overlooks the deliberate use of abstinence in the postpartum period to avoid pregnancy. Nationwide in Ghana, nearly one-sixth of married women with unmet need reported having been abstinent since their most recent child was born.
Reproductive preferences are known to be unstable over the long term, but this study finds that for a minority of respondents fertility preferences were revised even in the span of a few weeks. Fertility preferences were also unstable among a reference group of family planning users. The most frequent change to the fertility preference questions between the GDHS and the follow-up study occurred among women who initially reported themselves as undecided on fertility preferences but shifted to wanting another child. The main type of ambivalence was in desired timing of the next birth. In 11 cases, or 25 percent of all non-pregnant women, revised fertility preferences could have affected their unmet need status.
Among women with unmet need who gave consistent information about family planning and reproductive preferences in the GDHS and the follow-up study, the most frequent reason for unmet need was fear of the side effects or health consequences of modern methods. Women frequently have had adverse reactions to hormonal methods of family planning or know someone who has. The overwhelming concern was menstrual irregularities; weight gain, headaches, dizziness, and other side effects were mentioned infrequently. In only a few cases were reports of side effects based on rumors.
In addition to fear of side effects, other reasons for not using contraception were women’s own or husband’s opposition, fatalism, and religious convictions. Earlier studies have found attitudinal resistance to family planning in Ghana and an increasing shift toward concern about side effects [ 33 , 35 ]. This mixed methods study supports and extends the picture of opposition to family planning use. In follow-up discussions with respondents, opposition was more substantial than it appeared from the GDHS: on average, non-users expressed at least three reasons for not using family planning.
Ghana is a religiously diverse country. Religion had both a positive and a negative influence on women’s use of family planning. In some cases, family planning users cited religious educational outreach; other family planning users felt comfortable ignoring religious teachings that were in conflict with their own circumstances or life goals. Half of all non-users said that religion had an important influence on their decision not to use family planning.
Unmet need is measured among women, but it is important to recognize the influence of partners as well. This mixed methods follow-up study shows that the husband’s or partner’s influence appears to be equally important for users and non-users alike. Half of non-users explicitly mentioned that their husband opposed contraceptive use. Consistent with other studies, women’s empowerment appears to be an important dimension of family planning use in Ghana.
Study limitations and strengths
Limitations..
While the sample size interviewed is quite large for a qualitative study, it should not be considered regionally representative. Clusters were selected from among those available for follow-up during the study time period, with some desire for geographic diversity and balance between urban and rural areas. Study clusters overrepresent rural and poorer areas; ambivalent fertility preferences and underreporting of traditional methods may thus be more common among respondents than among the regional population.
Embedding a mixed methods study design within the GDHS survey proved advantageous. First, the follow-up study benefited from the rigorous and standardized sampling and household listing process undertaken by DHS surveys. By definition, the main group of interest for this study was married or sexually active, fecund women who want no more children but who are not using family planning. These women are particularly difficult to locate through facility-based convenience sampling. Current users of family planning in the same clusters could be included as a reference group. Second, the study was aided by a rich array of information already gathered about respondents’ demographic characteristics, reproductive histories, and familial context in the GDHS. Access to GDHS data meant that interviews could be conducted more quickly than otherwise possible; moreover, a small number of identical follow-up questions could provide insight on the quality and consistency of extant data. Third, mixed methods approaches are valuable as they help overcome weaknesses inherent in either a purely quantitative or qualitative approach [ 50 , 51 ]. By including a mixture of closed- and open-ended questions the study was able to help answer key questions about unmet need in Ghana.
The study findings have several major implications. First, although the prevalence of unwanted pregnancies attests to an ongoing need for family planning, Ghanaian women appear to manage their reproductive lives with more agency than may be apparent from survey data. Almost one-third of the respondents identified as having unmet need were either using a traditional method or intentionally abstinent as a method of child spacing. These women would still be defined as having an unmet need for modern contraception, but as previous studies from West Africa have found, women may be knowledgeable about modern methods but prefer traditional methods for a number of reasons [ 46 ]. Unobserved use of traditional and natural methods helps shed light on how Ghanaian women maintain fairly low fertility in regional perspective despite low reported levels of family planning use.
Second, even if we focus only on women with an unmet need for modern methods, the group defined as having an unmet need appears to be somewhat unstable, even in the very short-term. Some women, particularly in the rural Northern part of the country, expressed ambivalence and changing preferences about timing of the next birth even within a week of their original interview. This finding speaks to the importance of recognizing and accounting for women with unstable fertility preferences when designing programmatic interventions.
Third, this study underscores the possibility that opposition to modern methods among non-users is frequently more substantial than what is apparent from survey data. Women who are interested in modern methods but not using them because of lack of knowledge, cost, or access are relatively scarce, even in isolated, rural communities. This is already known from survey data; what this study adds is that opposition to modern methods may be more substantial than generally believed. Many non-users studied cited multiple reasons for non-use: fear of side effects, partner opposition, personal opposition, and religious opposition. Thus while increasing method choice and ensuring safe access to family planning are critically important, the results strongly suggest that additional demand generation and outreach activities appear to be necessary prerequisite to sustained increases in modern contraceptive use.
A previous study found that the most intractable reasons for not using family planning are attitudinal and religious resistance; in contrast, concerns about side effects are more easily overcome with education and information [ 52 ]. The present study confirms that women with attitudinal resistance frequently have multiple layers of resistance to modern methods (religious, partner, personal). Additionally, there appears to be strong opposition to modern methods among women who have themselves experienced negative side effects. Certainly there appear to be opportunities for education about reproductive biology or outreach to dispel myths about modern methods. But ambitious efforts to scale up use of modern methods should continue to guard against any risk of becoming unintentionally coercive at the local level.
Ghana has a relatively strong family planning program. Notably, the reference group of family planning users expressed satisfaction with their methods. There are opportunities for improvement, of course. Ready and safe access to methods should be routine. High-quality care should be standard. The method mix could be expanded: a few non-users expressed a desire for a longer-acting method or even sterilization. Programs providing client-centered or couple-centered counseling about contraception that supports total method choice and discussion about side effects from modern methods should be supported and expanded.
The evidence presented here suggests additional attention should be paid to measurement of traditional and natural methods in contemporary large-scale surveys. To the extent that traditional methods are undercounted, some natural methods considered modern, such as standard days method, lactational amenorrhea, and cycle beads, may also be undercounted as well. Additionally, while current programmatic efforts focus on modern methods, it is still important to understand what proportion of users of non-modern methods already consider themselves protected from the risk of pregnancy. Complete, prolonged abstinence is the most effective way to avoid pregnancy, yet the literature on traditional family planning methods is notably silent about complete abstinence, recognizing only periodic abstinence. This produces a kind of tautology: abstinence as a method of family planning is not measured because it is not recognized, and it remains invisible because its intentional use is not well-measured by contemporary surveys. The present study suggests that some consideration be given to prolonged abstinence as a method of family planning when it is intended to limit or space births.
Apart from complete abstinence, modern contraceptive methods are the most effective form of family planning. They also offer women the opportunity to initiate birth spacing and limitation independently of their male partners and even surreptitiously, thus giving women who may have little voice within their marriage the power to shape their own reproductive lives. Efforts to empower women within marriage would likely have a beneficial spillover effect on the use of family planning; moreover, given the strong influence of male partners, outreach to men should be an important part of efforts to scale-up family planning.
At a macro level, long-acting reversible contraceptive methods are an important source of long-term protection, but women frequently discontinue implants and injectables due to side effects and method-related reasons [ 53 ]. While the absence of menstruation may be seen as an indirect benefit of contraception in some cultures and contexts, non-users in Ghana perceive the absence of menstruation as particularly problematic; in some cases as a sign of disease or a cause of health problems. In the long-term, expanding access to the non-hormonal IUD in Ghana could help meet the needs of women who are opposed to methods that affect their menstrual cycles and who want long-term protection. Access to the IUD in Ghana is low [ 54 ].
A few women also indicated that they would prefer a permanent method. Sterilization is not without controversy and concerns over coercion, but it is a non-hormonal method that could be offered as part of total method choice in Ghana. Additionally, clinical development of contraceptive methods that have fewer side effects—particularly methods that do not affect menstruation—could also be an important strategy to address the unmet contraceptive needs of women and couples in Ghana and other developing countries.
Supporting information
S1 file. study questionnaires..
https://doi.org/10.1371/journal.pone.0182076.s001
Acknowledgments
I thank the women who participated in this study for sharing their perspectives and experiences; Sunita Kishor, Tom Pullum, Jennifer Johnson-Hanks, Enid Schatz, John B. Casterline, Kia Reinis, Madeleine Short Fabic, and Yoonjoung Choi for valuable comments; Clement Ahiadeke, Richmond Aryeetey, Michael Anie-Ansah, Philomena Efua Nyarko, Peter Peprah, and Gulnara Semenov for their contributions to fieldwork; and Kate Gunby, Abena Asamoabea Osei-Akoto, Ladys Ortiz, David Cantor, Mianmian Yu, and Guillermo Rojas for their contributions to data coordination and data processing. The views expressed are those of the author and do not necessarily reflect the views of above-named individuals, USAID, or the United States Government.
- 1. Singh S, Darroch JE. Adding it up: Costs and benefits of contraceptive services. Guttmacher Institute and UNFPA. 2012.
- View Article
- PubMed/NCBI
- Google Scholar
- 4. Bradley SEK, Croft TN, Fishel JD, Westoff CF. Revising unmet need for family planning. Calverton, Maryland, USA: ICF International, 2012.
- 11. Freedman R, Coombs LC. Cross-cultural comparisons. Data on two factors in fertility behavior. 1974.
- 14. Westoff CF, Ochoa LH. Unmet need and the demand for family planning. Columbia, Maryland, USA: Institute for Resource Development, 1991.
- 29. Ghana Statistical Service, Ghana Health Service, ICF International. Ghana Demographic and Health Survey 2008. Calverton, Maryland, USA: Ghana Statistical Service, Ghana Health Service, and ICF International, 2009.
- 34. Ghana Statistical Service, Ghana Health Service, ICF International. Ghana Demographic and Health Survey 2014. Rockville, Maryland, USA: Ghana Statistical Service, Ghana Health Service, and ICF International, 2015.
- 40. Staveteig S. Understanding unmet need in Ghana: Results from a follow-up study to the 2014 Ghana Demographic and Health Survey. Rockville, Maryland, USA: ICF International, 2016.
- 43. Curtis SL, Arnold F. An evaluation of the Pakistan DHS survey based on the reinterview survey. Calverton, Maryland, USA: Macro International, 1994.
- 44. Page HJ, Lesthaeghe R. Child-spacing in tropical Africa: Traditions and change. 1981.
- 45. Ghana Statistical Service—GSS, Ghana Health Service—GHS, Macro International. Ghana maternal health survey 2007. Calverton, Maryland, USA: GSS, GHS, and Macro International, 2009.
- 50. Irwin S. Data analysis and interpretation: Emergent issues in linking qualitative and quantitative evidence. In: Hesse-Biber SN, Leavy P, editors. Handbook of emergent methods: Guilford Press; 2010. p. 427–47.
- 53. Staveteig S, Mallick L, Winter R. Uptake and discontinuation of long-acting reversible contraceptives (LARCs) in low-income countries. Rockville, Maryland, USA: ICF International, 2015.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pan Afr Med J
Factors influencing the uptake of family planning services in the Talensi District, Ghana
Paschal awingura apanga.
1 Ghana Health Service, Talensi district, Upper East Region, Ghana
Matthew Ayamba Adam
Introduction.
Usage of family planning services in developing countries have been found to avert unintended pregnancies, reduce maternal and child mortality, however, it's usage still remains low. Hence, the objective of this study was to investigate the factors that influence the decision of women in fertility age to go for family planning services.
This was a descriptive cross-sectional study conducted in Talensi district in the Upper East Region of Ghana. Systematic random sampling was used to recruit 280 residents aged 15-49 years and data was analysed using SPSS version 21.0.
The study revealed that 89% (249/280), of respondents were aware of family planning services, 18% (50/280) of respondents had used family planning services in the past. Parity and educational level of respondents were positively associated with usage of family planning services (P<0.05). Major motivating factors to the usage of family planning service were to space children, 94% (47/50) and to prevent pregnancy and sexual transmitted infections 84% (42/50). Major reasons for not accessing family planning services were opposition from husbands, 90% (207/230) and misconceptions about family planning, 83% (191/230).
Although most women were aware of family planning services in the Talensi district, the uptake of the service was low. Thus, there is the need for the office of the district health directorate to intensify health education on the benefits of family planning with male involvement. The government should also scale up family planning services in the district to make it more accessible.
Family planning is widely acknowledged as an important intervention towards achieving Millennium Development Goals (MDGs) four (4) and five (5) as it has proven to reduce maternal and child mortality [ 1 – 3 ]. Family planning can prevent unwanted pregnancies and unsafe abortions. Some family planning methods such as condom usage can protect individuals from Sexually Transmitted Infections (STIs) including HIV/AIDS [ 1 – 3 ]. Family planning has also been found to promote gender equality as well as promote educational and economic empowerment for women [ 4 ]. Despite the enormous benefits of family planning services, the uptake of the service still remains low in Sub-Saharan Africa [ 1 ]. This has resulted into high rates of unwanted pregnancies, unplanned deliveries, unsafe abortions and maternal mortalities in Sub-Saharan Africa of which Ghana is no exception [ 1 , 5 ]. The low uptake of family planning is largely blamed on many factors. It has been observed that the awareness of the availability of family planning services has a great influence on the uptake of family planning services [ 6 ]. Additionally, even though some women are aware of the availability of family planning services, they are not properly informed about the various forms of family planning methods and how they work [ 7 ]. Some of the women who went for family planning services were not adequately counselled on the side effects of some of the family planning methods [ 7 ]. For example, in Uganda, some women stopped using contraceptives after they experienced what they perceived were side effects of the contraceptives [ 8 ].
Although most people are aware of the benefits of family planning services, they complained that it was difficult to access family planning services as such services were provided by health facilities that were far from their homes [ 9 ]. In addition, religious inclination has been noted to be a major constrain to the uptake of family planning services in Africa [ 9 , 10 ]. Also, some individuals perceived that family planning services were meant for only married couples whilst others fear that they will become sexually promiscuous if they go for family planning services once they cannot become pregnant [ 1 , 9 , 10 ]. In Ghana, some efforts have been made by the government of Ghana and non-governmental organizations through the implementation of various programmes to improve the coverage of family planning services in the country [ 9 ]. Although some successes have been chucked in the area of awareness of family planning services in the country, the unmet need for family planning still remains high [ 1 , 9 ]. The Ghana Demographic and Health Survey (GDHS) observed that a large number of women have an unmet need for family planning as the acceptor rate for family planning services remains low [ 11 ]. It is on this note the Ghana Health Service argues that the lives of mothers and children will be improved and maternal mortality reduced if family planning acceptor rate is improved [ 1 , 11 ].
Similarly, the Talensi district in Upper East Region (UER) of Ghana is not spared from this predicament as the acceptor rate for family planning services also remains low. The Talensi district offers free family planning services to clients in most of the health facilities in the district [ 12 ]. Despite the provision of free family planning services, the district reported 19% family planning acceptor rate in 2013, which is currently below the Ghana Health Service national family planning acceptor target rate of 23.3% [ 12 ]. The regional annual health report showed an increase in teenage pregnancies as well as unsafe abortions in the Talensi district [ 12 ]. Three maternal deaths were recorded in the Talensi district in 2011 as a result of unsafe abortions [ 12 ]. The increase in teenage pregnancies and unsafe abortions as well as the maternal mortalities that occurred could have been prevented if uptake of family planning services were improved. The decision to investigate the factors that influence the uptake of family planning services in the Talensi district is imperative as very little is known about the factors that influence the decision of people to go for family planning services in the Talensi district.
Settings, population and study design
This was a cross-sectional quantitative survey which was conducted between January and May, 2014. Questionnaires were administered to women aged 15-49years in households in the eight (8) sub-districts of the Talensi district. The Talensi district is one of thirteen districts in the Upper East Region of Ghana. The district has a total of population of 84,712 with a population of 19,738 of the women in fertility age (15-49years) with most inhabitants of the district being peasant farmers [ 12 ]. The district has eighteen (18) health care facilities which comprise of health centres, clinics and Community-based Health Planning and Services (CHPS) compounds of which sixteen (16) of the facilities offer free family planning services. Some of the family planning methods that are currently being offered include; Jadelle, Norplant, Condoms, Depo-provera, combined oral contraceptive pills etc [ 12 ].
Sample size
A sample size of 280 was derived using sample size formula for a single population. The assumptions made were using a 95% confidence interval, 5% margin of error and 23.3% national expected proportion of uptake of family planning service among Women In Fertility Age (WIFA).
n= Z 2 P (1-P)/(d) 2
Where n is the required sample size, P= 23.3% (0.233), Z= 1.96 and d= 5% (0.05). n= (1.96) 2 (0.233 × 0.767)/(0.05) 2 =275 which is 280 (to the nearest tenth).
Sampling method
A total of 280 of women aged 15-49years were recruited for the study using systematic random sampling technique. The 280 participants recruited were from households in the 8 sub-districts that make up the Talensi district (35 households from each sub-district) with one participant from each household. The 280 participants were recruited by the researchers themselves with the help of a community volunteer from each sub-district. The community volunteer helped researchers to approach community leaders to inform them about the purpose of the study and to obtain permission from them to recruit and interview potential participants as this is standard community entry protocol for conducting research within local community context in Ghana [ 13 ]. The presence of community volunteers in the team may have influenced the high response rate of 100% as they are highly respected with good knowledge of local residents. All households were numbered and a sampling interval, n=5 was used to select the first household. Subsequent selection of every 5th household then followed in same direction. Using this technique about 284 households was selected but 4 households were dropped because no one was available at the house to be recruited at the time of the survey.
Measurement
The questionnaires were structured with closed ended pre-coded questions and administered to participants by the Researchers. The questionnaires were divided into four parts. The first part was the socio-demographics whilst the second part was the awareness and usage of family planning services. The third part of the questionnaire provided various reasons that motivated women to access family planning services and the fourth part provided various reasons that discouraged women from using the service. The questionnaires were administered in a language that participants were comfortable to respond. The questionnaires were first piloted on ten (10) participants in the Nabdam district, a neighbouring district which shares border with the Talensi district. Piloting of the questions was done to ensure that the questions were more refined for participants to respond without difficulties [ 14 ].
Data analysis
All data were entered into SPSS version 21.0 and analyzed. The P-value of 0.05 was taken for statistical significance. The association between the binary outcome, usage of family planning services (yes or no) with independent categorical variables such as marital status, age, religion, parity and educational level were investigated using chi-squared test. Binary logistic regression model with the outcome, those who had used family planning services was used to investigate the influence of independent variables such marital status, age, religion, parity and educational level on the uptake of family planning services. Descriptive summary statistics was also used to report various reasons that motivated respondents to go for family planning services as well as reasons why some respondents did not use the service in the district.
Ethics issues
This study was approved by the Ethics committee board of the Catholic University college of Ghana and the Talensi district health directorate. Written consent was obtained from participants and for participants who were within the ages of 15-17years written consent was obtained from their guardians on behalf of them. All participants who consented to take part in the survey were well informed about the purpose of the study and why they were being asked to participate. They were also informed that participation was voluntary and they had the right to withdraw from the study even after they had participated.
Table 1 shows socio-demographic characteristics of 280 participants in relation to utilization of family planning services who were recruited for the survey. Most of the respondents in the study were within the age group of 15-20 years, 25% (70/280). Of the 280 respondents, majority were married, 73% (204/280) and 20% (56/280) of respondents were single. Most of the respondents were Christians, 56% (157/280). With regards to education, most of the respondents in the study had a senior high school level of education, 24 (67/280) and respondents who had four or more children, 55% (154/280) were the majority in the study. Table 1 also shows the results of the association between socio-demographic characteristics and the binary outcome, having used family planning services (yes or no) using chi-squared test. It showed that educational level and parity of respondents were positively associated with usage of family planning services (p<0.05) whereas marital status, age group and religion were not statistically significant.
Utilization of family planning services in relation to socio-demographic characteristics (n=280)
| Variable | Utilization of family planning services | P-value | |||||
|---|---|---|---|---|---|---|---|
| Yes | % | No | % | n | % | ||
| 0.061 | |||||||
| Married | 16 | 8 | 188 | 92 | 204 | 73 | |
| Single | 34 | 61 | 22 | 39 | 56 | 20 | |
| Widowed | 0 | 0 | 20 | 100 | 20 | 7 | |
| Divorced | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total | 50 | 230 | 280 | 100 | |||
| 0.524 | |||||||
| 15-20 | 25 | 36 | 45 | 64 | 70 | 25 | |
| 21-26 | 5 | 7 | 62 | 93 | 67 | 24 | |
| 27-32 | 14 | 21 | 53 | 79 | 67 | 24 | |
| 33-38 | 3 | 7 | 42 | 93 | 45 | 16 | |
| 39-49 | 3 | 10 | 28 | 90 | 31 | 11 | |
| Total | 50 | 230 | 280 | 100 | |||
| 0.624 | |||||||
| Christian | 19 | 138 | 157 | 56 | |||
| Moslem | 14 | 53 | 67 | 24 | |||
| Traditional | 17 | 39 | 56 | 20 | |||
| Total | 50 | 230 | 280 | 100 | |||
| 0.027 | |||||||
| Tertiary | 28 | 4 | 34 | 96 | 64 | 23 | |
| Senior high school | 11 | 16 | 56 | 84 | 67 | 24 | |
| Junior high school | 6 | 11 | 47 | 89 | 53 | 19 | |
| Primary | 3 | 5 | 56 | 95 | 59 | 21 | |
| None | 2 | 3 | 37 | 95 | 39 | 13 | |
| Total | 50 | 230 | 280 | 100 | |||
| 0.012 | |||||||
| 4 or more children | 24 | 16 | 130 | 84 | 154 | 55 | |
| 1 -3 children | 16 | 20 | 64 | 80 | 80 | 29 | |
| No child | 10 | 22 | 36 | 78 | 46 | 16 | |
| Total | 50 | 230 | 280 | 100 | |||
n= frequency %= percentage
Table 2 shows a further logistic regression model that have demonstrated that educated women are more likely to use family planning services as compared their peers who did not receive formal education (P=0.01). Similarly, the higher the parity of women the more likely they are to use the service as compared to people with lower parity (p=0.03). However, the association between age, marital status, religion and usage of family planning services were not statistically significant (P>0.05).
Logistic registration of demographic factors influencing family planning services utilization n=280)
| Variables | OR | 95%CI | P |
|---|---|---|---|
| Age | 0.024 | (0.231;1.658) | 0.21 |
| Marital status | 0.512 | (0.172; 1.342) | 0.12 |
| Religion | 0.493 | (0.169;1.239) | 0.32 |
| Parity | 1.312 | (0.863; 1.785) | 0.03 |
| Education | 1.079 | (0.367; 1.823) | 0.01 |
OR =Odd Ratios, CI =Confident Interval and P=probability value
Table 3 stipulates various responses by study participants towards the usage of family planning services. Of the few respondents who had accessed family planning services in the past, 18% (50/280) provided various reasons that lead to the decision to undertake family planning services. Major reasons that influenced the decision of women to go for family planning services were to space children, 94% (47/50) and to prevent pregnancy and Sexually Transmitted Infections (STIs), 84% (42/50). Majority of survey respondents who had not accessed family planning services, 82% (230/280) also cited various reasons for not using the service. Opposition from husbands for their wives not to access the service, 90% (207/230) as well as misconceptions about family planning methods, 83% (191/230) were reported as major reasons against usage of family services.
Responses to usage of family planning services
| To space children | 47 | 94 |
| To have sex without children | 6 | 12 |
| Fear of pregnancy | 22 | 44 |
| To prevent pregnancy and STIs | 42 | 84 |
| Against my religious faith | 69 | 30 |
| Fear of sexual promiscuity | 14 | 6 |
| Opposition from husbands | 207 | 90 |
| Distance to accessing the service | 28 | 12 |
| Poor health staff attitude | 18 | 8 |
| Side effects | 32 | 14 |
| Misconceptions | 191 | 83 |
n=frequency %=percentage NB: Some respondents gave more than one reason
The study was a cross-sectional study that investigated the factors that influence the utilization of family planning services among women within the age group of 15-49 years in the Talensi district. The findings suggest that although majority of the women were generally aware of family planning services in the district, usage of the service was low. Major reasons cited for not using service included husbands opposition against their wives using family planning services, this argument is in line with the observation made by Allen et al. (2014) in Uganda [ 15 ]. This is a major constrain as women in Ghana cannot take decisions for themselves without the approval of their husbands, who are regarded as the head of the family. Therefore it makes women more unlikely to use contraceptives if their husbands disagree. Another major reason that was reported were some perceived misconceptions about family planning services. Some of these misconceptions included respondents who did not go for family planning services because they perceived that it was meant for only married people whilst others perceived that contraceptives were harmful to the womb. These findings were consistent with studies reported by Meka et al. (2013) in Nigeria and Gebremariam and Addissie (2014) in Ethiopia respectively [ 16 , 17 ]. Other reasons that were reported for using family planning services in the district were; spacing of children and the desire of some women to prevent pregnancy and Sexual Transmitted Infections (STIs). These reasons were also found in similar studies by Abdurahman et al. (2014) and Awusabo-Asare et al. (2006) respectively [ 18 , 19 ].
These current findings have demonstrated that although the government has created an appreciable level of awareness about family planning services through its educational campaign programmes, only 18% of respondents have used the service. Hence, there is the need for the Ghana Health Service to re-visit the methods currently adopted to deliver family planning messages in rural communities in the Talensi district. Family planning messages should be integrated into existing health education programmes as it could help increase awareness, access and utilisation. Also, family planning educational messages should focus on the involvement of male partners in delivering the service as well as the benefits of family planning services as it will help reduce misconceptions about family planning services. On the other hand, the high awareness of family planning services coupled with low usage of the service compares favourably with Hamid and Stephenson (2006) study in Pakistan which observed that despite the high awareness of family planning services in the community, very few people used the service [ 20 ]. However, the high awareness of family planning services in the Talensi district may be attributed to the Community-based health planning and services (CHPS) compounds concept that was introduced to make health care more accessible to the rural communities as well as empowering them to have greater control of their own health [ 21 , 22 ].
In this study, it was found that the educational level of respondents was positively associated with utilization of family planning services. This finding suggests that people with higher education are more likely to go for family planning services than their counterparts with lower education. This agrees with other studies that revealed that women with higher education tends to be better informed about family planning services and are more likely to use the service than their peers with lower education [ 9 , 23 – 25 ]. Parity was also positively associated with usage of family planning services. This conforms to similar studies reported in Nigeria where women are more likely to use family planning service if they have three or more children [ 26 ]. Findings of this study are very useful as it can inform policy and decision making in the Ghana Health Service to help increase the family planning acceptor rate in Talensi district and the Upper East Region as a whole. However, some weakness in the study design limits the generalisation of findings to entire population of Talensi district as participants were conveniently selected from households rather than adopting a random sampling approach, which may not be representative of the general population. However, we ensured that participants were recruited randomly from households to address any problem of selection bias. Also, husbands should be involved in further research to investigate their perceptions about usage of family planning services.
In conclusion, this study has provided evidence to demonstrate that although the awareness of family planning services among community members could be high, it does not necessarily increase the uptake of family planning services if community members are not well informed about the benefits of family planning. It is therefore essential to organise educational campaigns on the awareness of family planning services by emphasising on the benefits of the services as it will help reduce misconceptions, and increase access and utilization of family planning services. Males should also be educated on the benefits of family planning services so as to reduce opposition from husbands. Furthermore, if women have the desire to space their children as well as prevent pregnancy and STIs, they are more likely to use the service.
Acknowledgments
The Authors are indebted to the Faculty of Public Health and Allied Sciences of the Catholic University College of Ghana. We are also grateful to the office of the Talensi District Health Directorate for their immense contribution. Our sincere gratitude also goes to the Community volunteers for their support.
Competing interests
The authors declare no competing interests.
Authors’ contributions
Mathew Ayamba Adam and Paschal Awingura Apanga conceptualized the research idea. The Authors both collected and analysed the data, and wrote the draft of the manuscript. The final manuscript was read, edited and approved by both Authors.
Skip to content. | Skip to navigation
Introduction
Associate Awards
- History and Results
- Work with Us
Capacity Building
- Community-Based Information Systems
Data Demand and Use
Data Quality
Data Science
Economic Evaluation
Family Planning & Reproductive Health
Geographic Information Systems
- Global Health Security
- Health Informatics
Health Information Systems
HIV and AIDS
Key Populations
Learning Agenda
Maternal and Child Health
- Network Analysis
- Organizational Development
Orphans and Vulnerable Children
Pandemic Influenza
- Routine Health Information Systems
Secondary Data Analysis
Systems Thinking
Tuberculosis
Youth and Adolescents
Publications
- Newsroom: News, Blogs, Podcasts, Videos
Presentations
Health Information Systems Strengthening Resource Center
- Results-Based Financing Indicator Compendium
Family Planning and Reproductive Health Indicators Database
Community-Based Indicators for HIV Programs


Improving Family Planning Service Delivery in Ghana

Author(s): Erasmus E.A. Agongo, Kofi Issah, John E. Williams, Francis Ayaba, Beatrice Kunfah, and Windfred Kombla Ofosu

Family planning (FP) is one of the most cost-effective interventions for improving the health of children and women, and the achievement of Millennium Development Goal (MDG) 4 (reducing under-five child mortality by two-thirds) and MDG 5 (reducing maternal mortality by three-fourths) from the 1990 figures by 2015. Despite several national and global initiatives to improve health outcomes, challenges remain in low- and middle-income countries to achieve national and global targets.
Ghana has a long history of population policies and FP programs that have contributed to increased use of contraceptive services and improved maternal and child health. However, the country has not achieved MDGs 4 and 5, particularly in the three northern regions, which are the poorest and most deprived. This study focuses on one of those areas―the Upper East Region (UER). Although the UER has made great strides in improving access to FP services, there is still a huge unmet need.
The objectives of this study were to map out the distribution of all FP service providers in the region and document how the community-based FP information system is linked to the national system as a means to recommend strategies for supporting program planning and implementation and improving FP services.
WORK WITH US
Accomplishments
Evaluate Blog
Results-based Financing Indicator Compendium
Organization Development

- Accessibility
Personal tools
- Open access
- Published: 13 August 2014
Determinants of modern family planning use among women of reproductive age in the Nkwanta district of Ghana: a case–control study
- Sebastian Eliason 1 ,
- John K Awoonor-Williams 2 ,
- Cecilia Eliason 3 ,
- Jacob Novignon 4 ,
- Justice Nonvignon 5 &
- Moses Aikins 5
Reproductive Health volume 11 , Article number: 65 ( 2014 ) Cite this article
21k Accesses
68 Citations
4 Altmetric
Metrics details
Average contraceptive prevalence rate in the Nkwanta district of Ghana was estimated to be 6.2% relative to the national average at the time, of 19%. While several efforts had been made to improve family planning in the country, the district still had very low use of modern family planning methods. This study sought to determine the factors that influenced modern family planning use in general and specifically, the factors that determined the consistently low use of modern family planning methods in the district.
A case–control study was conducted in the Nkwanta district of Ghana to determine socio-economic, socio-cultural and service delivery factors influencing family planning usage. One hundred and thirty cases and 260 controls made up of women aged 15–49 years were interviewed using structured questionnaires. A logistic regression was fitted.
Awareness and knowledge of modern family planning methods were high among cases and controls (over 90%). Lack of formal education among women, socio-cultural beliefs and spousal communication were found to influence modern family planning use. Furthermore, favourable opening hours of the facilities and distance to health facilities influenced the use of modern contraceptives.
While modern family planning seemed to be common knowledge among these women, actual use of such contraceptives was limited. There is need to improve use of modern family planning methods in the district. In addition to providing health facilities and consolidating close-to-client service initiatives in the district, policies directed towards improving modern family planning method use need to consider the influence of formal education. Promoting basic education, especially among females, will be a crucial step as the district is faced with high levels of school dropout and illiteracy rates.
Peer Review reports
Uptake of modern family planning (FP) methods remains low in Sub-Saharan Africa (SSA) including Ghana. This may be associated with high incidence of unintended pregnancies, unsafe abortions, and maternal deaths [ 1 , 2 ]. The United Nation’s Millennium Development Goal (MDG) 5 aims at improving maternal health and reducing maternal mortality by three quarters between 1990 and 2015. An important intervention towards achieving this target is the promotion of modern family planning (FP) among women in Sub- Saharan Africa (SSA) [ 1 , 3 ]. Evidence exists that if couples can space their pregnancies by at least two years apart through the use of family planning, up to 35% of maternal deaths and up to 13% of child mortalities could be averted [ 4 – 6 ], whilst 25% of under – five mortalities could be averted if birth intervals were at least three years [ 5 ].
The cost-effectiveness of family planning in poverty reduction and socio-economic development in the developing world cannot be disputed [ 7 , 8 ]. Evidence from Bangladesh shows that long-term investment in an integrated family planning and maternal and child health (FPMCH) programme contributed to improved economic security for families, households, and communities through larger incomes, greater accumulation of wealth, and higher levels of education [ 8 ]. Further evidence showed that every dollar spent on family planning saved at least US$4 that could have been spent treating complications from unintended pregnancies and saved governments up to US$31 in health care, water, education, housing, sewers, and many more [ 9 , 10 ]. Thus, if individuals and couples, especially in the developing world, planned their pregnancies and families, with improved use of contraception, they are more likely to have fewer and healthier children which will reduce the socio-economic burden on them and allow more investment in each child’s care and education, helping to break the cycle of poverty.
Several studies have been conducted on determinants of family planning use. In some cases strong associations have been established between family planning use and some socio-demographic, socio-cultural and socio-economic characteristics of women and significant others. Depending on the context and setting in which the studies were conducted results were either consistent or contrasting. Studies have revealed that, use of family planning methods was found more in women of higher age group [ 11 , 12 ]. Education has also been observed in many other studies to be associated with contraceptive use [ 11 , 13 – 15 ]. Women with at least primary level of education are 8-10% more likely to be using a modern, or any method of contraception compared to those with no education. Secondary education increases the probability of using contraceptives in the range of 14-17%, and post-secondary education increases the probability to the range 16-20% [ 16 ]. High parity is associated with family planning use [ 11 , 12 , 15 ]. Family planning was more common among women with higher household income and highest wealth quintile [ 11 , 15 ].
In an analysis of 10,204 women from the 2011 demographic and health survey data of Ethiopia, it was reported that, being employed, being in a monogamous relationship, attending community conversation and being visited by a health worker at home increased the likelihood of using modern contraception [ 15 ]. They also observed on the contrary that, living in rural areas, older age, being in polygamous relationship, being Muslim, and witnessing one’s own child’s death were associated with lower odds of adopting modern contraceptive [ 15 ].
Stephenson and Hennink [ 17 ] noted that family planning use and service utilization was associated with socio-economic, demographic, cultural and health experience factors at the individual and household levels. They noted that increasing parity and approval by partner and significant others like mother –in-law were associated with increased family planning service utilization. They also observed that the further away family planning facilities were from women, the lower the tendency to access services [ 17 ]. Those who communicated with their spouses had elevated odds of using family planning. The assumption was that spousal communication was associated with subsequent family planning exposure, which in turn led to family planning use [ 18 ].
Family planning is integrated into the reproductive and child health services at all levels of the health delivery system in Ghana. Health service delivery in Ghana follows a three-tier arrangement: primary, secondary and tertiary levels. The primary level incorporates a Community Based Health Planning and Service (CHPS) system that ensures health provision at the door step of the people. Family planning services are free, but the commodities are not, though they are very highly subsidized. Strong advocacy is however ongoing, to make commodities free in the country. Doctors, midwives and community health nurses are responsible for family planning service provision in the country.
Ghana’s fertility rate was estimated to be at 4 per woman in 2008 which was a reduction from 5.2 in 1993 and 4.4 in 2003 [ 19 ]. About 17% of married women use modern contraceptive methods in Ghana while about 24% use any contraceptives, including traditional contraceptives [ 19 ]. This suggests that the use of contraceptive methods, especially the modern ones, still remain low among women in Ghana. It is estimated that, Ghana’s family planning unmet need increased from 30% in 2003 to 34% in 2008 [ 19 ]. It is therefore imperative to establish and understand the factors that serve as barriers to the use of contraceptives and available family planning services.
The Nkwanta district is located in the Volta region of Ghana and is considered to be one of the poorest and most remote districts in the region. It has a population of 117,878. The district boasts of 13 health facilities including 2 hospitals, health centres, maternity homes and community based health planning and services (CHPS) compounds. The health workforce in the district is inadequate and weak. The Doctor: Patient ratio is 2: 117,878 and the Nurse: Patient ratio also is 1:7,000.
Family planning is integrated into the reproductive and child health programme of the district. Routine service-provision data, as well as survey data from 2000 had consistently indicated low prevalence of modern contraceptive use [ 20 ] compared to all the other districts in the Volta region. According to the annual reports of the District Health Directorate, the average contraceptive prevalence rates computed for the district increased from 3.7% in 1999 to 6.2% in 2004 [ 21 ] relative to the overall national average at the time of 19% and national rural average of 14% [ 22 ]. This trend had become very worrying to the district. The aim of this study was to determine the factors that influenced modern family planning use in general and specifically, the factors that determined the consistently low use of modern family planning methods in the district. This would inform more committed efforts at improving family health and wealth in the region. Field work was undertaken between July and August 2004.
Study methodology
A case control study method was employed because family planning use had been consistently low over a long period compared to the other districts in the region and in the country; funding for study was limited and results of the study were needed quickly by the district to put in necessary interventions. A 2:1 matching was employed in this study, where two control persons were sought for every case person.
Study and target populations
Cases: The study population included all registered modern family planning users aged 15–49 years in the Nkwanta district. The target population included all women aged 15–49 years living in Nkwanta district and currently using any modern contraceptive method, and all women in the specified age group who were not practicing any modern method of contraception, but whose partners were practicing modern male contraception. All women aged 15–49 years who were practicing traditional methods of contraception were excluded because the problem under study was low use of modern family planning.
Controls: Study population included all women aged 15–49 years living in Nkwanta district who had never practiced any modern family planning method. The target population included women aged 15–49 years (matched for age group, marital status, place of residence) living in Nkwanta district who had never used any modern contraceptive method. Women aged 15–49 years who had practiced modern family planning in the past, but who were currently not practicing any modern contraception, were excluded. Women who were currently practicing traditional methods of contraception were also excluded.
Sample size
The sample size, n necessary to estimate the odds ratio (OR) to within Ɛ of OR, with probability 1- α, is given by [ 23 ]:
Where P 1 * and P 2 * are the probabilities of exposure given that a person practices family planning or not, respectively [ 23 ], with
To estimate the population odds ratio (OR) to within Ɛ =25% of its true value, 2, given that the exposure rate computed from a pilot survey was 0.30, the sample size, n was = 408; But in this study, two controls were matched for each case i.e. n control / n case = 2. The exact number of cases and controls were derived as follows: n cases + n controls = 408 ( n controls = 2 n cases ). The number of cases n cases was 136; whilst the number of controls n control was 272.
Identification of cases and controls
Since there was a district register of all women practicing modern family planning, selection of cases, was initially by a stratified sampling procedure as follows:
Stratification of all women aged 15–49 years currently practicing modern family planning, and have their names in the district’s family planning register, into the following age groups- (15-19 yrs), (20-29 yrs), (30-39 yrs) and (40-49 yrs).
Using proportional allocations sample sizes were assigned to each age stratum.
Simple random sampling was used to select the pre-determined number of subjects for each age stratum from the stratified register. Subjects were to be traced to their household using the addresses given in the district family planning register.
At this point, it was realised that most of the addresses provided in the registers were unreliable because of poor household address systems, some evidence of covert use of family planning and culturally sensitive nature of family planning in the district.
The cases were therefore selected through community health officers (CHOs) who were requested to recruit as many women as possible practicing family planning from the various sub-district lists extracted from the district register. This was much easier and suitable because the CHOs knew the clients personally and also knew the households in which they lived. Four (4) out of the five (5) sub-districts were selected (i.e. Kpassa, Brewaniase, Tutukpene, and Nkwanta) because they had CHOs at the health centres or CHPS centres who would help recruit cases. The clients were invited to report at the various health facilities to be screened. Once they fell within the inclusion criteria, they were recruited into the study. Despite the challenges and limitations faced in sampling, a total of 130 cases - Kpassa (30), Brewaniase (23), Tutukpene (32), and Nkwanta (45) - were recruited, giving a response rate of 95.6%.
Control persons were recruited from the same communities where case persons resided, by matching for age, marital status and place of residence. Active search for controls was done starting from the households of the cases. If suitable controls were found for the cases in the households, they were recruited. If controls were not found within the households, they were sought for in the adjacent households till suitable controls were found (two controls per case). A total of 260 controls were recruited.
Data collection
To formalize the data collection process and to ensure reliable responses, consents were sought from the District Chief executive, Chiefs and opinion leaders within the second week. The objectives and likely outcomes were explained to these individuals and culturally sensitive issues in the survey instrument discussed and restructured in a way that would minimize the respondents’ anxiety and at the same time provide the most reliable responses.
Similarly, qualified research assistants were recruited for the purposes of effective data collection. Within the third week, eight (8) research assistants who were fluent in both English language and the local dialects were recruited from the district and trained to do survey data collection using the standardized questionnaire. During the training, the concept of case–control studies, the objectives and methodology of the study were also discussed in detail and explained using the training manual. Each of the Research Assistants was made to translate the questionnaire into local language in the presence of all the others to ensure that he or she understood the questions. Where the translation was not well done, he or she was helped by experts to do them right.
All the questionnaires together with the methodology were pre-tested by the Research Assistants (RAs) at Korantang, a community outside the study area but with similar characteristics like Nkwanta. The necessary corrections and reviews were made before they were finally taken to the field. These activities were carried out in the fourth week.
Interview survey technique using the same structured questionnaires was employed to obtain quantitative data from both cases and controls. Information about the following exposure or explanatory variables was obtained from both cases and controls. The exposure variables were broadly classified into three categories, namely: socio-demographic, socio-economic, socio-cultural and service factors. The socio-demographic characteristics included parity and ethnicity whilst the socio-economic variables included the educational levels and employment status of respondents and their partners, household income, living conditions, and type of employment. The socio-cultural variables included religion, religious approval of FP, discussion with parents and partner about FP, preference for a given number of children, beliefs and myths about side effects of FP, living with significant others and polygamous partner. The service factors included method availability, cost of methods, facility waiting times, facility opening hours, distance of facility from community and time constraints and attitudes of health workers.
The Research Assistants were divided into two (2) groups of four (4). One group was assigned the cases and the other group, the controls. About fifteen (15) to twenty (20) minutes was spent per subject. The interviews were conducted confidentially by the trained assistants at the health facilities and in the communities. Three (3) weeks was assigned for the data collection.
Quality control
Before each interview, the research assistant introduced him/herself to the respondent, and the objectives and the possible outcomes explained to them. It was also explained that the answers that they provided were going to be kept confidential. After each subject was interviewed, the questionnaires were scrutinized for completeness and consistency. Where incompleteness, errors and inconsistencies were observed, the necessary corrections were ensured before the women were allowed to leave.
Ethical considerations
The study was subjected to ethical clearance from the Noguchi Memorial Institute for Medical Research at the University of Ghana. Informed consent was also sought from the subjects involved in the data collection. Further, confidentiality of collected information was ensured by clients not providing names or any identities. Subjects had the right to opt out of the study any time they desired. Subjects were made comfortable and protected from any physical and mental harm in the course of the data collection. Initial findings of the study were presented to the district.
Data analysis
All completed interviews were rechecked for consistency and completeness. Coding and computerisation were done after creation of data analysis fields in Epi Info statistical software package version V3.0. The information was transferred to STATA statistical software version 7.0 for statistical analysis at the time. The data was re-analysed using the STATA version 11.2. Simple frequencies were used to analyse respondents’ background data, whilst logistic regression models (bivariate and multivariate) were employed to test level of significance and association between the dependent and exposure or explanatory variables. The dependent variable used in the logistic regression analyses was “current use of modern family planning methods among respondents”. Modern family planning includes reversible (pills, injectables, condoms, intrauterine device, implants, lactational amenorrhoea) and irreversible (vasectomy and tubal ligation) contraceptive methods. The variable was measured as a dummy binary variable, with 1 representing usage and 0 representing non-usage.
Background characteristics of study women
Most of the cases (63/130) and controls (126/260) were in the 20–29 year group. Most Tawere also from Nkwanta sub-district and were married. Amongst the cases, majority (39.2%) had attained juniour secondary/middle school education, whilst majority of the controls (50.8%) had had no formal education. Majority of the cases (23.8%) belonged to the Ewe ethnic group whilst Konkombas, dominated the control group (23.1%). Christians and farmers dominated the samples of cases and controls Table 1 .
Knowledge and awareness of family planning
A little over 90% of both cases (93.8%) and controls (91.5%) knew at least a method of modern contraceptive. Injectable was the most known modern method of family planning amongst both cases (93.1%) and controls (82.6%), followed by the pill (cases-86.9%; controls-65.9%). The diaphragm was the least known method amongst the cases (3.1%), whilst vasectomy or male sterilization was the least known amongst the controls (0.4%) (Table 2 ). Health workers were the main source of family planning information in the district for both cases and controls, followed by friends and relatives and then by radio. Newspaper sources contributed the least to family planning information in the district (Table 3 ).
Determinants of family planning method use
At the time of the survey, Konkomba women showed significantly less odds of practicing modern family planning compared to women of other ethnic groups (OR = 0.51, 95% C.I.0.29 -0.90) in bivariate analyses. Women with no formal education were significantly less likely to practice modern family planning relative to those with some formal education (OR = 0.57, 95% C.I 0.37- 0.87). Similarly, women whose partners had no formal education were also significantly less likely to practice modern family planning (OR = 0.48, 095% C.I.0.29- 0.80). In multivariate analyses, Konkomba women still showed significantly less odds of practicing modern family planning (AOR = 0.25, 95% CI 0.07 -0.91) (Table 4 ).
As depicted in Table 5 , women who discussed modern family planning with their partners were 4.67 times more likely to use modern family planning methods compared to those who did not discuss with their partners (OR = 4.67, 95% C.I 2.88-7.58) in bivariate analyses. Furthermore, women whose partners approved of modern family planning were 4.33 times more likely to use modern family planning than those whose partners did not approve (OR = 4.33, 95% C.I 2.55-7.36). In multivariate analyses, women who believed that modern family planning use made women promiscuous showed lower odds of practicing modern family planning compared to those without that belief (AOR = 0.06, 95% C.I 0.01- 0.47) Table 5 .
A family planning facility less than 5 km away was more likely to influence modern family planning use compared to if it was located more than 5 km away (OR = 3.63, 95% C.I 1.38- 9.55) (Table 6 ). Also, method availability showed greater odds of influencing modern family planning use compared to method non-availability (OR = 4.98, 95% C.I 2.55- 9.75). Favourable opening hours (five hours or more) of family planning facility significantly increased odds of modern family planning use compared to non-favourable opening hours (OR = 9.25, 95% C.I 4.50 -19.03)). Non- restriction of method use was found to be 1.75 times more likely to influence modern family planning use relative to situations with restrictions to method use (OR = 1.75, 95% C.I 1.03-2.96). In multivariate analyses however, favourable opening hours of family planning facility showed increased odds of influencing modern family planning use compared to non-favourable opening hours (AOR = 5.38, 95% C.I 1.36-21.29) (Table 6 ).
The findings of the study seem to suggest that knowledge of modern family planning methods is very high amongst both cases and controls as a little over 90% of them had knowledge of at least one modern contraceptive method. This result confirms what is reported in the Ghana Demographic and Health Survey (GDHS) [ 19 ] that about 98% of all women aged 15–49 years know at least one modern method of contraception.
Injectables were the most known method of modern contraception amongst both cases (93.1%) and controls (82.6%), followed by the pills and implants. This is contrary to the GDHS [ 19 ] where male condom was the most known method of modern contraception, followed by the pill and injectables. The injectables were well known because it is believed that it was suitable for covert users of modern contraceptives, especially in a community in which women had the belief that practice of modern family planning was associated with promiscuity (finding in this study). It is rather surprising that male condoms were found to be unpopular amongst women in the Nkwanta district. The patriarchal nature of the district [ 20 ] may be promoting the belief that family planning is a ‘woman’s business’ and therefore patronage of the use of male methods may not be prevalent.
The study suggested that the main source of family planning information was health workers in the district. This may be explained by the fact that health workers are accessible to the various communities in the district throughout the day because of the presence of the community based health planning and services (CHPS) system which is widespread in the communities and provide health service at the doorstep of the people. Also, the Nkwanta district generally has very poor radio and television reception hence making it difficult to obtain regular family planning information from such media.
As expected, the study found that partners’ consent to the use of modern family planning methods was very crucial to the success of any family planning intervention. The results showed that women who discussed family planning methods with their partners were more likely to use modern methods of contraception. This finding is consistent with empirical findings from other researchers in other countries [ 18 , 24 – 26 ]. For instance, Mekonnen and Worku [ 27 ] found that women who discussed family planning with their partners were 2.2 times more likely to use family planning.
Moreover, evidence from Nigeria revealed that husband opposition was the major reason for non-use of modern contraceptives [ 28 ]. It is speculated that some partners who do not approve of family planning use feared that their wives use of contraceptives would encourage promiscuity or would undermine their authority as heads of the household [ 29 ]. This belief was confirmed in this study and is a major barrier to modern family planning use in the district. It was revealed that women who had the belief that use of modern family planning promoted promiscuity had significantly lower odds of practicing modern family planning compared to women who did not have that belief (AOR = 0.06, 95% C.I 0.01- 0.47). It may be possible that the partners of these women may have influenced such belief.
The study also found that distance to family planning facilities influenced use of contraceptive methods. Specifically, communities with family planning facilities within a distance of less than 5 km away are more likely to use contraception as opposed to communities with facilities with a distance of more than 5 km. This finding contradicts that of a study in Nigeria in which 40% of women interviewed did not attend the clinic nearest to their homes and 90% of these women said they did so to get better service [ 30 ]. Favourable opening hours of the family planning facilities was also found to be strongly associated with modern family planning use. In the Nkwanta district, the Community Based Health Planning and Services (CHPS) initiative that seeks to bring health services to the doorstep of the people has improved accessibility to family planning services greatly. This was shown by the gradual increase in family planning coverage from 3.7% in 1999 to 6.2% in 2004. The finding in this study reinforces the need to promote and maintain the CHPS initiative in the district.
Educational attainments of both women and their partners were found to be very significant factors in the use of family planning methods. Unlike women with no formal education, women with some formal education were more likely to use modern methods of contraception. A similar relationship was established for their partners. Other researchers also found similar results in their studies [ 31 – 34 ]. Beekle and McCabe [ 31 ] found lack of formal education to strongly reduce modern family planning use. This does not come as much of a surprise as higher education attainment increases female decision making power and awareness of the benefits of good family planning practices [ 17 ]. This study found that, Konkomba women compared to women from the other ethnic groups in the district had lower odds of practicing modern family planning. Lower educational attainment [ 20 ] may explain this finding.
The results show that while family planning knowledge and awareness was widespread in the district, factors such as education, access to facilities and services and partner’s consent were significant determinants of modern family planning method use. Major determinants of low family planning use in the district, are low educational attainment of women in the district especially, the Konkomba women and strong socio-cultural beliefs amongst women, especially the belief that modern family planning use make women promiscuous. In addition to providing health facilities and consolidating the CHPS initiative in the district, policies directed towards improving modern family planning method use need to consider raising the levels of formal education. Promoting basic education, especially among females, will be a crucial step as the district is faced with high levels of school dropout and illiteracy.
The study was limited in the sense that while stratified sampling method was more preferred, the poor nature of household addresses in the district did not make this feasible to its full extent. Furthermore, the extent to which the findings from the study can be generalized is limited due to the various sample size adjustments performed. However, these limitations do not affect the reliability of the findings of the study.
This case–control study sought to determine factors influencing the use of modern family planning in the Nkwanta district of Ghana, especially those that influence low use. The results show that, while family planning knowledge and awareness are wide spread in the district, factors such as low educational attainment of women in the district and widespread socio-cultural beliefs about modern family planning are major barriers to family planning use in the district.
In addition to providing health facilities and consolidating the CHPS initiative in the district, policies directed towards improving modern family planning method use need to consider raising the levels of formal education. Promoting basic education, especially among females, will be a crucial step as the district is faced with high levels school dropout and illiteracy.
Cates W, Abdool Karim Q, El-Sadr W, Haffner DW, Kalema-Zikusoka G, Rogo K, Petruney T, Averill EMD: Global development. Family planning and the millennium development goals. Science. 2010, 329: 1603-10.1126/science.1197080.
Article CAS PubMed Google Scholar
Crossette B: Reproductive health and the millennium development goals: the missing link. Stud Fam Plann. 2005, 36: 71-79. 10.1111/j.1728-4465.2005.00042.x.
Article PubMed Google Scholar
Sachs JD, McArthur JW: The millennium project: a plan for meeting the millennium development goals. Lancet. 2005, 365: 347-353. 10.1016/S0140-6736(05)17791-5.
Cleland J, Bernstein S, Ezeh A, Faundes A, Glasier A, Innis J: Family planning. The unfinished agenda. Lancet. 2006, 368 (9549): 1810-1827. 10.1016/S0140-6736(06)69480-4.
Rutstien SO: Further evidence of the effects of preceding birth intervals on neonatal, infant, and under-five years mortality and nutritional. Calverton, Maryland: Macro International, MEASURE DHS, 2008 Sep. [86] p. (DHS Working Papers No. 41; USAID Contract No. GPO-C-00-03-00002-00), http://www.popline.org/node/209750 ,
Stover J, Ross J: How increased contraceptive use has reduced maternal mortality. Matern Child Health J. 2010, 14 (5): 687-695. 10.1007/s10995-009-0505-y.
Reproductive Health Supplies Coalition: Make a case for supplies, leading voices in securing reproductive health supplies. An Advocacy Guide and Toolkit. 2009, Brussels: Reproductive Health Supplies Coalition
Google Scholar
Population Reference bureau: World population data sheet. Popul Bull. 2009, 2009 (64): 3-
Singh S, Daroch JE, Ashford LS, Vlassoff M: Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. 2009, New York: Guttmacher Institute and United Nations Population Fund
Speidel J, Sinding S, Gillespie D, Maguire E, Neuse M: Making the Case for US. International Family Planning Assistance. 2009, Baltimore, Maryland: Johns Hopkins Bloomberg School of Public Health, Bill and Melinda Gates Institute for Population and Reproductive Health
Jabeen M, Gul F, Wazil F, Javed N: Knowledge, attitudes and practices of contraception in women of reproductive age. Gomal J Med Sci. 2011, 9: 2-
Sharma V, Mohan U, Das V, Awasthi S: Socio demographic determinants and knowledge, attitude, practice: Survey of family planning. J Fam Med Primary Care. 2012, 1: 43-47. 10.4103/2249-4863.94451. Accesed from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893950/ 03/12/13
Article Google Scholar
Arbab A, Bener A, Abdulmalik M: Prevalence, awareness and determinants of contraceptive use in Qatari women. East Mediterr Health J. 2011, 17: 1-
Faisal B, Eria H: Microeffects of women’s education on contraceptive use and fertility: the case of uganda. J Int Develop. 2013, http://onlinelibrary.wiley.com/doi/10.1002/jid.2915/full ,
Yihunie Lakew Y, Reda AA, Tamene H, Benedict S, Deribe K: Geographical variation and factors influencing modern contraceptive use among married women in Ethiopia: evidence from a national population based survey. Reprod Health J. 2013, doi:10.1186/1742-4755-10-52, http://www.reproductive-health-journal.com/content/10/1/52 . accessed 19/12/2013
Bbaale E, Mpuga P: Female education, contraceptive use and fertility: evidence from Uganda: Consilience . J Sustain Develop. 2011, 6 (1): 20-47.
Stephenson R, Hennink M: Barriers to family planning use amongst the urban poor in Pakistan. Southampton, UK: University of Southampton, School of Social Sciences, 34-(Opportunities and Choices, (2); 2004 [ http://eprints.soton.ac.uk/34736/ ]
Sharan M, Valente TW: Spousal communication of family planning adoption. Effects of a radio drama series in Nepal. Int Fam Plan Perspect. 2002, 28 (1): 16-25. 10.2307/3088271.
Ghana Statistical Service: Report of the Ghana Demographic and Health Survey 2008. 2009, Accra, Ghana and Claverton, USA: Ghana Statistical Service
Awoonor-Williams JK, Feinglass FS, Tibey R, Vaughan-Smith MN, Nyonator F, Jones TC, Philips JF: “Bridging the gap between Evidence-based Innovation and National Health Sector Reform in Ghana.”. Population Policy Research Division Working Paper 2004 No. 191.22. 1999
Ghana Health Service: Annual report 1999–2004 Nkwanta district; 1999. 2004
Ghana Statistical Service: Report of the Ghana Demographic and Health Survey 2003. 2004, Accra: Ghana Statistical Service
Lemeshow S, Hosmer DW, Clar J, Lwanga SK: Adequacy of sample size in health studies. 1990, John Wiley and Sons
Mahmood N, Ringheim K: Factors affecting contraceptive use in Pakistan. Pak Dev Rev. 1996, 35 (1): 1-22.
CAS PubMed Google Scholar
Mahmood N, Ringheim K: Knowledge, approval and communication about family planning as correlates of desired fertility among spouses in Pakistan. Int Fam Plan Perspect. 1997, 23 (3): 122-129. 10.2307/2950768.
Pasha O, Fikree FF, Vermund S: Determinants of unmet need for family planning in squatters settlements in Karachi, Pakistan. Asia-Pacific Popul J. 2001, 2 (16): 93-108.
Mekonnen W, Worku A: Determinants of low family planning use and high unmet need in Butajira District, South Central Ethiopia. Reprod Health. 2011, 8: 37-10.1186/1742-4755-8-37. http://www.reproductive-health-journal.com/content/8/1/37 ,
Article PubMed PubMed Central Google Scholar
Ikechebelu JI, Joe-Ikechebelu NN, Obiajulu FN: Knowledge, attitude and practice of family planning among Igbo women of south-eastern Nigeria. J Obstet Gynaecol. 2005, 25 (8): 792-795. 10.1080/01443610500328231. doi:10.1080/01443610500328231
Ghana Statistical Service: Ghana Demographic and Health Survey 1998. 1999, Accra, Ghana and Claverton, USA: Ghana Statistical Service
Mensch B: Using situation analysis data to assess the function of family planning clinics in Nigeria, Tanzania and Zimbabwe. Stud Fam Plann. 1994, 1 (25): 18-31.
Beekle AT, McCabe C: Awareness and determinants of family planning practice in Jimma, Ethiopia. Int Nurs Rev. 2006, 53 (4): 269-276. 10.1111/j.1466-7657.2006.00492.x.
Magadi MK, Madise NJ, Rodrigues RN: Frequency and timing of antenatal care in Kenya: explaining the variations between women of different communities. Soc Sci Med. 2000, 51: 551-561. 10.1016/S0277-9536(99)00495-5.
Addai I: Demographic and socio-cultural factors influencing use of maternal health services in Ghana. Afr J Reprod Health. 1998, 1 (2): 73-80.
Bhatia J, Cleland J: Determinants of maternal care in a region of south India. Health Transit Rev. 1995, 5: 127-142.
Download references
Acknowledgements
We wish to express our great debt of gratitude to all individuals and institutions that supported in diverse ways to the completion of this work. We are particularly grateful to all the staff of Nkwanta District Health Management Team, especially Mr. Nutifafa Glover, Dr. Innocent Adzamli and Ms Gifty Sunu for their support during the data collection, data entry and analysis. Our sincere thanks also go to all the Community Health Officers (CHOs) at the sub-districts in Nkwanta for supporting with the recruitment of clients for the study.
Author information
Authors and affiliations.
Department of Community Medicine, School of Medical Sciences, University of Cape Coast, Cape Coast, Ghana
Sebastian Eliason
Regional Health Directorate, Ghana Health Service, Upper East Region, Bolgatanga, Ghana
John K Awoonor-Williams
Department of Adult Health, School of Nursing, College of Health Sciences, University of Ghana, Legon, Ghana
Cecilia Eliason
Department of Economics, University of Ibadan, Ibadan, Nigeria
Jacob Novignon
Department of Health Policy, Planning and Management, School of Public Health, College of Health Sciences, University of Ghana, Legon, Ghana
Justice Nonvignon & Moses Aikins
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Moses Aikins .
Additional information
Competing interests.
The authors declare they have no competing interests.
Authors’ contributions
SE conceived the study, carried out data collection and participated in analysis and drafting the manuscript. JKAW participated in conceiving the study and reviewing the manuscript. CE participated in conceiving the study, developing data collection tools and reviewing the manuscript. JN(1) participated in analysis, drafting and reviewing the manuscript. JN(2) participated in analysis, drafting and reviewing the manuscript. MA provided general guidance and participated in drafting and reviewing the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Eliason, S., Awoonor-Williams, J.K., Eliason, C. et al. Determinants of modern family planning use among women of reproductive age in the Nkwanta district of Ghana: a case–control study. Reprod Health 11 , 65 (2014). https://doi.org/10.1186/1742-4755-11-65
Download citation
Received : 06 August 2013
Accepted : 28 July 2014
Published : 13 August 2014
DOI : https://doi.org/10.1186/1742-4755-11-65
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning
- Contraception
- Reproductive age
- Case-control study
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
- Open access
- Published: 21 February 2022
Assessment of men involvement in family planning services use and associated factors in rural Ghana
- Senanu Abigail Kpekpo Kwawukume 1 ,
- Alexander Suuk Laar ORCID: orcid.org/0000-0002-0721-4533 2 &
- Tanko Abdulai 3
Archives of Public Health volume 80 , Article number: 63 ( 2022 ) Cite this article
6935 Accesses
7 Citations
Metrics details
In low-and-middle income countries (LMICs) less attention is paid to men’s involvement in Family Planning (FP) programs where public health officials have advocated the involvement of men as a strategy for addressing the dismal performance of FP programs. The study assessed the involvement of men in FP use and the factors which promote or hinder the uptake of FP services among partners in a rural setting of northern Ghana.
A cross-sectional descriptive study was used to collect data from 200 respondents. Study respondents were selected through random cluster sampling.
The findings showed that male partners’ knowledge (95.5%) and approval (72.8%) of FP services were high. About 48% of men were involved in FP service utilization. Having living children (aOR; 1.71(1.27, 2.15)) and being knowledgeable (aOR; 6.14(1.38, 10.90)) about FP were positively associated men’s involvement in FP service utilization. The findings also indicated that men had a higher propensity (X 2 = 4.5534, p = 0.033) of supporting a FP method use. Women who reported that their spouse supported FP method use were more likely to use a contraceptive method (X 2 = 9.5223, P = 0.002) if their spouse supported FP method use (X2 = 9.5223, P = 0.002) and if their partners had some education (X2 = 14.1133, P = 0.000). Reasons for low contraceptive use were health risks, side effects, and socio-cultural norms.
Family planning programs need to include men at all levels of health promotion and education of FP programs to help reduce misconceptions about contraceptive methods to increase acceptance and use among partners in rural settings of Ghana.
Peer Review reports
Worldwide, 12% of married or in-union women are estimated to have had unmet need for contraceptive methods [ 1 ]. In LMICs, 214 million women of reproductive age who want to avoid pregnancy are not using modern contraceptive method [ 1 ]. In Sub-Saharan Africa, the proportion of women who have an unmet need for modern contraception is highest at 21% [ 1 ]. Unmet need for modern contraception and family planning (FP) accounts for 80% of unintended pregnancy in LMICs [ 1 ]. In Ghana, the contraceptive prevalence rate among all women aged 15–49 years is 25%, with 20% using modern methods [ 2 ] with a high unmet need of 45.7% [ 3 ]. Contraceptive use interventions and unmet need for FP are important determinants of fertility decline in LMICs [ 4 ]. Promotion of FP and ensuring access to preferred contraceptive methods for women and couples is essential to securing the well-being and autonomy of women [ 1 ]. Men participation in FP can be either as a user of male contraceptive methods and or encouraging and supporting their partners or wives in contraception [ 5 ]. Family planning services are critical to improving maternal and child health and reducing maternal and infant mortality in LMICs [ 6 ]. Expanding FP services and involving men in LMICs such as Ghana could increase utilization of services in this setting could avert up to 42% of maternal deaths [ 6 , 7 ].
Men are also recognized to be responsible for the large proportion of reproductive ill-health suffered by their partners’ use of FP methods [ 8 ]. Although contraceptive methods and services are frequently geared towards women, men are often the primary decision-makers on family size and their partners’ use of FP methods [ 9 ]. It is well documented that men’s general knowledge and attitude about the ideal family size, gender preference of children, ideal spacing between childbirths, and contraceptive methods use greatly influence women’s preferences and opinions [ 8 , 10 , 11 ].
In Ghana, the focus of this study, knowledge of any contraceptive method is almost universal, with 98% of all women and 99% of all men knowing at least one method of contraception and where 50% of all women reported having used a method of contraception before [ 12 ]. According to the Ghana Demographic and Health Survey (2014), only 27% of married women use FP with 22% using a modern method and 5% using the traditional method [ 13 ]. Family planning programs in Ghana dates as far back as 1956 [ 14 ], however, uptake of FP services has not been encouraging and even worst in rural Ghana including the Sissala East District in Tumu of the Upper West Region where utilization of PF decreased from 71.4% in 2011 to 50.7% in 2012 [ 15 ]. In Ghana, The male partner may have an influence in decision-making regarding contraceptive use and the number of offspring they would like to have. Family planning research in rural Upper West Region has been dominated by findings almost exclusively from women studies.
Men in rural Ghana are seen to be the head of the home and influence the healthcare decisions of the entire household affairs [ 16 ]. Studies have also shown an increase in contraceptive use in cases where men partners have been involved [ 9 , 17 ]. Men’s involvement helps not only in accepting contraceptives uptake but also its effective use and continuation [ 9 , 10 , 17 ]. However, male partners’ role in FP services promotion and uptake has often been overlooked and neglected in rural areas in Africa such as Ghana. To fill this research gap, this study assessed the involvement of men in FP service utilization and the factors that determine their involvement in contraceptive uptake among women in a rural district of the Upper West Region.
Study setting
The study took place in Tumu in the Sissala East District in the north-eastern part of the Upper West Region of Ghana. Tumu, the district capital is predominantly rural by nature, with the majority (85%) living in rural settings [ 18 , 19 ]. A large percentage (84%) of the population lives below the poverty line [ 18 , 19 ]. A greater proportion (76%) of the population are being engaged in agriculture. It is predominantly Islam (88.0%) with Christianity being the largest of the minority (10%) followed by Traditional (1.4%) [ 18 , 19 ]. A greater proportion of the population (52.4%) has Some level of education [ 18 ].
Study design
A cross-sectional descriptive study design was used for this study. An interviewer-administered questionnaire consisting of both open and close-ended questions was administered by experienced research assistants to elicit the necessary information from the study population.
Sampling technique and sample size
The sample size for this study was determined using the Yamane method: \(\mathrm{Sample}\ \mathrm{Size}=\frac{\mathrm{N}}{1+\mathrm{N}{\left(\mathrm{p}\right)}^2}\) where N = Total Population, p = margin of error (5%). A sample size of 386 was derived from the total population of 11,252.
Study population
The study population consisted of adult males and females aged 15 years and above who were either married or cohabitating. For this study, we aimed at recruiting 386 respondents but finally recruited 200 respondents due to logistical constraints.
Data collection method
An interviewer-administered questionnaire consisting of both closed and open-ended questions was used to assess the knowledge and use of FP services among partners and the level of involvement of male partners in FP service utilization. The study questionnaire was developed based on the objective of this study by the principal investigator. The questionnaire was administered by the first author and two experienced research assistants who understand the native dialect. The questionnaire was translated into the local dialect and administered by the two research assistants for participants who could not understand or speak the English language. The questionnaire was administered among households in five communities or clusters out of the ten in Tumu municipality. These communities were chosen using a simple random sampling method. Forty respondents were interviewed from each community. This method gave the individual an equal chance of being selected. Before consent was sought from respondents, the aim of the study was explained to each individual. They were also assured of confidentiality and privacy of the information they will give. The questionnaires were pretested in a similar environment in the district.
Outcome variable
Male participants were asked whether they approved and/or encourage use FP of their partners, ever discussed FP with their partners, provided material support to their partners to access FP services and whether they have used FP themselves in the past. Responses to these questions were them summed to give the level of male partners’ involvement in FP utilization (with no weight given to these variables); the highest possible involvement score was five (indicating a high level of involvement), a zero score indicated no involvement in FP utilization, and score of 3 was considered as sufficient involvement. The involvement of men in FP service utilization for themselves and/or their partners was the main outcome of the study. Female respondents were also asked; if they discuss FP with their male partners, gets approval to use FP from their male partners and whether they receive support from their male partners to access FP services.
The demographic characteristics (age, education, occupation, and religion) and knowledge about FP were the covariates considered for our analyses.
Data management and analysis
To ensure accuracy, the data collected was checked and screened for completeness. The completed copies of the questionnaire were serially numbered and doubly entered and analyzed using Statistical Package for Social Scientists version 20.0. Bivariate and regression analyses were used to determine the associations between the outcome variables and a host of explanatory variables.
Background characteristics of respondents
Two hundred (200) respondents were interviewed for this study. The study involved 107 men representing 53.5% and 93 women representing 46.6%. Respondents’ age ranged between 15 and 54 for men and 15–49 for women. In all, over 70 % (76.5%) had some form of education ranging from primary to tertiary while 23.5% had no education (Table 1 ). All the respondents were involved in some kind of work with over 60 % (66%) being artisans.
Knowledge of family planning
Majority of the male respondents (95.5%) had heard of FP. Almost half of the respondents (48.1%) had information about FP via the mass media (Television, Radio, and Newspaper) followed by friends (27.5%) and the health facility (23.5%) as indicated in Table 2 .
Twenty eight percent (28.0%) of the men interviewed understood FP as avoidance of unintended pregnancy, 25.2% as limiting family size while 19.6% understood it as spacing of childbirth. Others (27.1%) explained it as two or more of the above definitions as shown in Table 3 . The most common method known and used was the condom (42.5%) followed by implants (32.0%) and the least known method being the foaming tablet (7.0%) among male respondents.
Men involvement in FP
Over 50 % (52.2%) of the male respondents reported they or their partner were currently using some form of contraceptives to delay or avoid pregnancy. However, only 36.4% of women reported they or their partners were currently using contraceptives to delay or avoid pregnancy. The majority of the men respondents (72.8%) approved of the use of FP methods by their partners, 75% of the women respondents also indicated their partners had approved of their use of FP. The findings also indicate that men had a higher propensity of reporting FP use (X 2 = 4.5534, p = 0.033). For the couples who did not approve of the FP methods, the reasons included: socio-cultural beliefs (31%), side effects (30.8%) such as delayed or absence of menses, and difficulty of conceiving after terminating use of FP and others (38.5%).
Overall, about 48% of men were sufficiently involved in FP service utilization (see Table 1 ). Involvement of men in FP use was positively associated with knowledge of FP and the number of living children (Table 4 ).
Decision making in FP use
We wanted to know from the women whether their partners support them in their desire to use contraceptives; 67.0% of the women answered in the affirmative and 33.0% answered in a negative. Those who answered in the affirmative said their partners support them by providing money for transport to facility and/or for FP services, encouraging and accompanying them to the health facility. Women who reported that their spouse support FP use were more likely to use a contraceptive method (X 2 = 9.5223, P = 0.002) compared to those who said no. Women who reported their partners had some education were also more likely to use a contraceptive method (X 2 = 14.1133, P = 0.000). In all, female respondents tended to report more favorable attributes for their male partners’ involvement than the male respondents (Fig. 1 ).
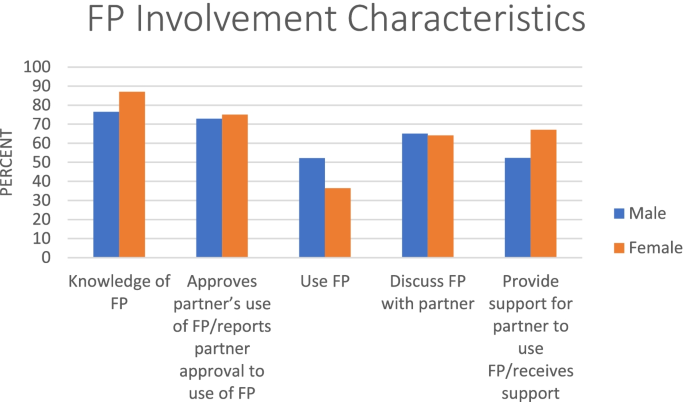
FP involvement characteristics
Generally, a greater proportion of men (77.6%) intend using FP in the future. For those who answered in a negative, 19.1% said most of the contraceptives were designed to suit women and thought it was a woman’s business. Nearly three quarters of women (73.4%) who ever used a FP method indicated their partner had a say in the decision to use. For the women interviewed,70.7% said they would still practice birth control irrespective of their partners’ opinion while 23.9% would not use birth control if their partners were against it, 5.4% were however not certain.
This study assessed male partners’ involvement and factors associated with the use of FP services in Tumu in the Sissala East District of the Upper West Region of Ghana. The study identified several factors that influence FP services use among male partners in this setting. Our study demonstrated that despite the high knowledge of modern contraceptive methods among couples, use was low due to perceived side effects and socio-cultural beliefs. Men’s attitude and social practice towards FP methods also influence the behavior of their partners using contraceptives [ 20 ]. It is found elsewhere that the decision not to practice FP is men-dominated and men are responsible for providing contraceptive decisions when FP is practiced [ 21 ]. A major limitation facing low-and-middle income countries FP promotion programs and population policy development on contraceptive behavior is that men are often not targeted in FP programs [ 22 ].
Our study identified several factors associated with men’s influence in FP service utilization among their partners. Non-approval of FP methods by men in this study was attributed to perceived risks, side effects, and socio-cultural norms. Focus group discussions with men and women in rural Uganda have come out with similar findings [ 9 ]. Contraceptive knowledge and use are shaped by the socio-cultural environment such as personal attitudes and feelings about contraception. In rural settings in low and -middle income countries most men may be unwilling to have their wives adopt FP, which they have little knowledge about. Evidence shows that some men oppose contraceptive use for reasons of tradition and religion which require men to maintain the honor and position of their extended family, village, religious group and social organization [ 23 ]. Studies have shown with similar findings in settings in rural northern Ghana [ 24 , 25 ]. The complex web of social and cultural factors impedes spousal communication regarding reproductive health issues and that discourages them to take their wives to health clinics to discuss FP issues [ 22 ].
Two important factors were identified to be positively associated with men’s involvement in FP use in our study; Knowledge on FP and the number of living children male partners had were positively associated with their involvement in FP use. Knowledge about FP will influence acceptance and therefore impact involvement of men in its utilization. Similar studies by [ 26 , 27 ] have found FP knowledge to be positively linked with its utilization. Our study additionally revealed that men who had greater than two living children were more likely to be involved in FP service utilization. The number of living children have also been shown to be associated with contraceptive use among women in previous studies [ 28 , 29 ]; couples with living children tend to use contraceptives space their births or limit the number of children. Several interventions can be used to address barriers in the uptake of FP services in this setting. Family planning programs need to target men at all levels of health promotion and education with their partners to reduce misconceptions about FP methods to increase acceptance [ 20 ]. Men’s participation is crucial to help reduce misconception about side effects of contraceptive methods [ 20 ]. Therefore, FP family programs need to target men at all levels of the service. Their involvement will also lead to women’s empowerment to increase effective contraceptive use and continuation to improve better health outcomes in reproductive health [ 30 ]. User experiences indicate that text messages provide a novel way to raise awareness, promote behavior change and address myths and socio-cultural norms [ 31 ].
Limitations
This study has some limitations which need to be taken into consideration. The finding of this study cannot be generalized to the entire region of the Upper West region due to the small sample size. Despite the small sample size, views of groups of our respondents which comprised of married partners and those cohabitating, will not differ significantly from the rest of the entire population in the region. Also, this study provides vital insights for policymakers in Ghana and beyond who are working to improve sexual and reproductive health services for men and women. The need for future study to capture the perspectives of men and women on cultural factors influencing PF services for policy.
Conclusions
Our study demonstrated high knowledge of FP among partners. However, the use of modern contraceptives methods was low due to side effects and socio-cultural norms. Involving men partners in FP programs could give them accurate and complete information on contraceptive methods to help reduce misconception and increase uptake. Reproductive health program designers, policymakers, and population researchers, health professionals need to incorporate the findings into reproductive health programs to help address barriers to improve health outcomes among couples.
Availability of data and materials
The dataset for this study is available on request from the corresponding author.
Abbreviations
Family Planning
Low- and Middle-Income Countries
World Health Organization. Contraception: evidence brief. No. WHO/RHR/19.18. Geneva: World Health Organization; 2019.
Ghana Statistical Service (GSS), G.H.S.G., and ICF. Ghana Maternal Health Survey 2017: Key findings. Rockville: GSS, GHS, and ICF; 2018.
Google Scholar
MacQuarrie K. Unmet need for family planning among young women: levels and trends; 2014.
Wulifan JK, et al. A scoping review on determinants of unmet need for family planning among women of reproductive age in low and middle income countries. BMC Womens Health. 2015;16(1):1–15.
Demissie TW, Tegegne EM, Nigatu AM. Involvement in family planning service utilization and associated factors among married men at Debre Tabor town, Northwest Ethiopia, 2017. Pan Afr Med J. 2021;38:211.
Article Google Scholar
Chola L, et al. Scaling up family planning to reduce maternal and child mortality: the potential costs and benefits of modern contraceptive use in South Africa. PLoS One. 2015;10(6):e0130077.
Khan SA, et al. A comparative trial of copper T 380 and cu 375 IUCD. J Ayub Med Coll Abbottabad. 2010;22(3):185–7.
PubMed Google Scholar
Mistik S, et al. Married men’s opinions and involvement regarding family planning in rural areas. Contraception. 2003;67(2):133–7.
Article CAS Google Scholar
Kabagenyi A, et al. Barriers to male involvement in contraceptive uptake and reproductive health services: a qualitative study of men and women’s perceptions in two rural districts in Uganda. Reprod Health. 2014;11(1):21.
Vouking MZ, Evina CD, Tadenfok CN. Male involvement in family planning decision making in sub-Saharan Africa-what the evidence suggests. Pan Afr Med J. 2014;19:349.
Organization, W.H. Programming for male involvement in reproductive health: Report of the meeting of WHO regional advisers in reproductive health, WHO/PAHO, Washington DC, USA 5-7 September 2001. Geneva: World Health Organization; 2002.
GSS, G., Ghana statistical service (GSS), Ghana health service (GHS), and ICF macro. Accra: Ghana Demogr Health Surv, 2009. 2008: p. 79–96.
Staveteig, S., Understanding unmet need in Ghana: Results from a follow-up study to the 2014 Ghana Demographic and Health Survey. 2016: ICF International.
Adanu RM, et al. Contraceptive use by women in Accra, Ghana: results from the 2003 Accra Women’s health survey. Afr J Reprod Health. 2009;13(1):123–33.
Kuganab-Lem RB, Dogudugu R, Kanton L. Birth preparedness and complication readiness: a study of postpartum women in a rural district of Ghana. Public Health Res. 2014;4(6):225–33.
Apusigah AA. The gendered politics of farm household production and the shaping of women’s livelihoods in northern Ghana. Feminist Africa. 2009;12(12):51–67.
Williamson LM, et al. Limits to modern contraceptive use among young women in developing countries: a systematic review of qualitative research. Reprod Health. 2009;6(1):3.
Service, G.S. 2010 Population & Housing Census. Sissala East District: District Analytical Report; 2014.
Report, S.E.D.H.D., Resource endowment, investment opportunities and the attainment of MDGs. 2011.
Bayray A. Assessment of male involvement in family planning use among men in south eastern zone of Tigray, Ethiopia. Scholarly J Med. 2012;2(2):1–10.
Mbizvo MT, Adamchak DJ. Family planning knowledge, attitudes, and practices of men in Zimbabwe. Stud Fam Plan. 1991;22(1):31–8.
Shahjahan M, Kabir M. Why males in Bangladesh do not participate in reproductive health: lessons learned from focus group discussions. Int Q Community Health Educ. 2006;26(1):45–59.
Tuloro T, et al. The role of men in contraceptive use and fertility preference in Hossana town, southern Ethiopia. Ethiop J Health Dev. 2006;20(3).
Apanga PA, Adam MA. Factors influencing the uptake of family planning services in the Talensi District, Ghana. Pan Afr Med J. 2015;20(1):10.
PubMed PubMed Central Google Scholar
Eliason S, et al. Determinants of unintended pregnancies in rural Ghana. BMC Pregnancy Childbirth. 2014;14(1):261.
Manortey S. Determinants of male involvement in family planning services: a case study in the Tema Metropolis, Ghana. Open Access Libr J. 2020;7(01):1.
Kasa AS, Tarekegn M, Embiale N. Knowledge, attitude and practice towards family planning among reproductive age women in a resource limited settings of Northwest Ethiopia. BMC Res Notes. 2018;11(1):1–6.
Haq I, Sakib S, Talukder A. Sociodemographic factors on contraceptive use among ever-married women of reproductive age: evidence from three demographic and health surveys in Bangladesh. Med Sci. 2017;5(4):31.
Islam AZ, et al. Prevalence and determinants of contraceptive use among employed and unemployed women in Bangladesh. Int J MCH AIDS. 2016;5(2):92.
Kassa M, Abajobir AA, Gedefaw M. Level of male involvement and associated factors in family planning services utilization among married men in Debremarkos town, Northwest Ethiopia. BMC Int Health Hum Rights. 2014;14(1):33.
Riley P, et al. Mobiles for quality improvement pilot in Uganda. Bethesda: Abt Associates, Strengthening Health Outcomes through the Private Sector Project; 2011.
Download references
Acknowledgements
The authors wish to acknowledge all study participants for their cooperation in providing the necessary information and the research assistants for data collection.
The authors received no funding for this work.
Author information
Authors and affiliations.
Seventh-Day Adventist Hospital, Koforidua, Eastern Region, Ghana
Senanu Abigail Kpekpo Kwawukume
REJ Institute, Research and ICT Consultancy Services, Tamale, Northern Region, Ghana
Alexander Suuk Laar
Department of Community Health and Family Medicine, SMHS University for Development Studies, Tamale, Northern Region, Ghana
Tanko Abdulai
You can also search for this author in PubMed Google Scholar
Contributions
SAKK conceived the study and conducted the field work. SAKK and TA designed the study and performed the statistical analysis. ASL drafted the manuscript. SAKK and TA reviewed the manuscript. All authors read and approved the final manuscript”.
Corresponding author
Correspondence to Alexander Suuk Laar .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Institutional Review Board of the Community Health Department of the University for Development Studies in Ghana. Informed consent was obtained from the study participants before data collection.
Consent for publication
All authors read the manuscript and approved it for publication.
Competing interests
None to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kwawukume, S.A.K., Laar, A.S. & Abdulai, T. Assessment of men involvement in family planning services use and associated factors in rural Ghana. Arch Public Health 80 , 63 (2022). https://doi.org/10.1186/s13690-022-00822-5
Download citation
Received : 07 April 2021
Accepted : 04 February 2022
Published : 21 February 2022
DOI : https://doi.org/10.1186/s13690-022-00822-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning services
- Upper west region
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
About FP2030
Working together to advance family planning around the world.

Focus Areas
Working towards global reproductive choice; autonomy and empowerment; and gender equality.

Regional Hubs
Supporting country-specific goals with ties to global family planning.

Commitment Makers
Creating a future for women and girls with the freedom and ability to lead healthy lives.

We believe in the power of data to drive results and measure impact.

Empowering accessible rights-based, family planning all over our world.

Knowledge Center
Browse our library for the latest news and resources.
Get Involved
Empowering the voluntary use of modern contraception around the world.

Government Partner
The Republic of Ghana, under the leadership of the Ministry of Health, has developed commitments as part of the FP2030 global movement.
The commitments aim to ensure equitable and timely access to quality family planning information, commodities, and services for all persons of reproductive age in Ghana by the end of 2030.
Commitments made to :
By the end of 2030, all persons of reproductive age in Ghana will have equitable and timely access to quality planning information, commodities, and services.

Ghana Commitment Objectives
- Implement the roll-out of family planning under the National Health Insurance Benefits Package, increasing the number of districts currently providing FP on NHIS to 75% by September 2027 and 100% by 2030.
- Increase government financial commitment to procure 20% of Ghana’s FP commodities needs by 2030, addressing the decline in funding from development partners.
- Increase the modern contraceptive prevalence rate (mCPR) among currently married women or women in a union from 30% in 2020 to 44.4% by the end of 2030, through expanded method choice, improved service delivery, and enhanced data management.
- Reduce unmet need for contraception among sexually active adolescents from 57% to 30% by December 2030, by promoting reproductive health education, strengthening partnerships, and improving access to FP services.
- Develop and implement a targeted social and behavior change communication plan that focuses on rights-based family planning, aiming to provide correct and consistent information to promote family planning adoption.

Become an FP2030 Partner
- IPR Intranet
INSTITUTE FOR POLICY RESEARCH
How immigration laws influence family planning.
New study shows links between immigration policies and how many kids Hispanic adults want
Get all our news
Subscribe to newsletter
Our analyses provide important insights into the unanticipated ways in which immigrant policies impact Hispanics’ reproductive and family life in the context of a rapidly changing U.S. immigrant policy climate.”
Julia Behrman IPR sociologist

Immigration policies may also influence how people think about their ideal family size, especially among groups who see these policies as a threat.
A new study by IPR sociologist Julia Behrman and Abigail Weitzman of the University of Texas at Austin investigates the connection between U.S. immigration policy and Hispanic adults’ ideal family size. They discovered that in states with more punitive immigration policies, Hispanic adults want more children than Hispanic adults do in states without these policies.
“ As someone who studies ideal family size and other childbearing norms, I was particularly interested in exploring how policies affect the childbearing norms of those most affected [by immigration policies],” Behrman explained, noting that the dramatic scale and scope of U.S. immigration policies made them compelling to study.
Since the mid-2000s, states have enacted an unprecedented number of immigration policies. They include restrictive policies such as Secure Communities, which increased data-sharing between federal, state, and local law enforcement, and E-verify mandates, which are used to confirm the work eligibility of employees and restrict undocumented migrants’ jobs. Other states have passed sanctuary policies to protect immigrants from arrest or detention.
Behrman says immigration policies, though targeted at undocumented migrants, can impact the entire Hispanic population because of racial profiling. Others might fear these policies because members of their household are not documented.
To understand how different immigration policies influence the ideal family size of Hispanics, the researchers combined information on state-level immigration policies across time with data from the General Social Survey (GSS). They used GSS data collected between 2006 and 2018 from 3,977 non-Hispanic White and Hispanic adults. The survey included the question: “What do you think is the ideal number of children for a family to have?”
They grouped states into four policy categories: those with multiple restrictive policies called “omnibus immigration policies,” E-verify mandates, sanctuary policies, or no immigration policies. They also estimated which Hispanic survey respondents were unlikely to be documented.
The researchers show that Hispanic adults’ ideal family size was much higher compared to non-Hispanic White adults in states with omnibus immigration policies versus in states without those policies. In states with omnibus policies, Hispanic and White adults’ average ideal number of children was 3.16 and 2.56, respectively. In states without immigration policies, Hispanic adults wanted, on average, 2.62 kids, and White adults wanted 2.49 kids.
“Interestingly, we find that sanctuary policies, which aim to curb federal immigration enforcement, and E-verify mandates, which aim to curb the employment of undocumented immigrants, are not associated with significant differences in ideal family sizes,” Behrman said.
She says the gap in ideal family size between Hispanic and White adults in states with restrictive policies was especially large among Hispanic adults who are likely undocumented.
The researchers speculate that the threat of restrictive policies might make Hispanics look for comfort in having more children and investing in family. These adults might also want larger families to cope with deportations and the loss of family and community members.
This study sheds light on the way immigration policies affect the reproductive lives of the U.S. Hispanic population. It also shows the importance of including social norms about family size in research about the impact of migration policies on fertility.
“Our analyses provide important insights into the unanticipated ways in which immigrant policies impact Hispanics’ reproductive and family life in the context of a rapidly changing U.S. immigrant policy climate,” Behrman said.
Julia Behrman is assistant professor of sociology and an IPR fellow.
Photo credit: iStock
Published: September 3, 2024.
Related Research Stories

Faculty Spotlight: Eli Finkel

The Mental Health Effects of School Shootings
How Do Voters Think About Electability?

IMAGES
VIDEO
COMMENTS
This is in line with national reports on family planning awareness in Ghana and a significant departure from many other studies which tended to focus on awareness alone or translate awareness to knowledge [22, 23]. Understanding the methods and benefits of contraception are critical to having motivated users. ... The research protocol was first ...
Contraceptive Prevalence Rate (CPR) for modern methods has fluctuated from 19% in 2003, decreasing to 17% in 2008 and increasing to 22% in 2014, an indication that even after a decade, still less than a quarter of married women are current users of modern contraception in Ghana. Yet, 30% of married women in Ghana have an unmet need for family ...
Background Unmet need for family planning is high (30%) in Ghana. Reducing unmet need for family planning will reduce the high levels of unintended pregnancies, unsafe abortions, maternal and neonatal morbidity and mortality. The purpose of this study was to examine factors that are associated with unmet need for family planning to help scale up the uptake of family planning services in Ghana ...
Ghana has historically had one of the highest rates of unmet need for family planning in Africa, despite having a relatively strong family planning program. Ghana's rate of unmet need among married women is 32.9 whereas many surrounding countries have a lower rate of unmet need among married women including Senegal (26.2), Nigeria (23.7) and ...
Background Despite availability of modern contraceptive methods and documented unmet need for family planning in Ghana, many women still report forgoing modern contraceptive use due to anticipated side effects. The goal of this study was to examine the use of modern family planning, in particular hormonal methods, in one district in rural Ghana, and to understand the role that side effects ...
This is in line with national reports on family planning awareness in Ghana and a significant departure from many other studies which tended to focus on awareness alone or translate awareness to knowledge [22, 23]. Understanding the methods and benefits of contraception are critical to having motivated users. ... The research protocol was first ...
FAMILY PLANNING HEALTH PROFILE GHANA 2019 Total population (000's) 2019 Total fertility rate (births per women) 2018 Adolescent Birth Rate (births per 1000 adolescent females) 2013 IMR (deaths per 1000 live births)2018 MMR (deaths per 1000 live births)2017 30,418 5 75 35 308 General statistics
In Ghana, despite a 38 percent decline in the total fertility rate from 1988 to 2008, unmet need for family planning among married women exposed to preg nancy risk declined only modestly in this period: from 50 percent to 42 percent. Examining data from the five DHS surveys conducted in Ghana during these
In Ghana, despite a 38 percent decline in the total fertility rate from 1988 to 2008, unmet need for family planning among married women exposed to pregnancy risk declined only modestly in this period: from 50 percent to 42 percent. Examining data from the five DHS surveys conducted in Ghana during …
Introduction Despite a relatively strong family planning program and regionally modest levels of fertility, Ghana recorded one of the highest levels of unmet need for family planning on the African continent in 2008. Unmet need for family planning is a composite measure based on apparent contradictions between women's reproductive preferences and practices. Women who want to space or limit ...
The Ghana Demographic and Health Survey (GDHS) observed that a large number of women have an unmet need for family planning as the acceptor rate for family planning services remains low . It is on this note the Ghana Health Service argues that the lives of mothers and children will be improved and maternal mortality reduced if family planning ...
Year: 2018. Abstract: Family planning (FP) is one of the most cost-effective interventions for improving the health of children and women, and the achievement of Millennium Development Goal (MDG) 4 (reducing under-five child mortality by two-thirds) and MDG 5 (reducing maternal mortality by three-fourths) from the 1990 figures by 2015.
The following sections apply the PH onceptual Framework in describing Ghana's family planning program and its relationship to the PHC system. A. System A1. Governance & Leadership All national and subnational family planning efforts in Ghana operate in a policy and legal environment in which provision of family planning is legal.
This study assesses the long-term fertility impact of the Community Health and Family Planning Project of the Navrongo Health Research Centre in Ghana and addresses policy debates concerning the ...
Ghana's government's efforts were galvanised by preparing and launching the Family Planning Costed Implementation Plan (GFPCIP, 2016-2020), which was launched in September 2015 [12, 13]. The plan ...
Abstract. The purpose of this study was to identify the factors that influence adolescents' knowledge and Family Planning practices in Ghana's Tema Central sub-metropolis. The importance of family ...
Front Matter from Costs and Benefits of Family Planning in Ghana on JSTOR. JSTOR is a digital library of academic journals, books, and primary sources.
The primary goal of the GDHS was to produce reliable and up-to-date data on family planning, fertility, infant and child mortality, maternal and child health, and nutrition. 19 The Multiple Indicator Cluster Survey was developed by the United Nations Children's Fund (UNICEF) as an international multi-purpose household survey project to assist ...
Uptake of modern family planning (FP) methods remains low in Sub-Saharan Africa (SSA) including Ghana. This may be associated with high incidence of unintended pregnancies, unsafe abortions, and maternal deaths [1, 2].The United Nation's Millennium Development Goal (MDG) 5 aims at improving maternal health and reducing maternal mortality by three quarters between 1990 and 2015.
Family planning programs in Ghana dates as far back as 1956 , however, uptake of FP services has not been encouraging and even worst in rural Ghana including the Sissala East District in Tumu of the Upper West Region where utilization of PF decreased from 71.4% in 2011 to 50.7% in 2012 . In Ghana, The male partner may have an influence in ...
The Evolving Landscape of FP in Ghana. Ghana's family planning programme has witnessed remarkable advancements since its inception in 1969. Notably, the year 2022 marked a pivotal juncture with the integration of clinical FP services into the National Health Insurance Scheme, marking a significant step towards wider access to FP services ...
community-based family planning in Ghana: A case study of Community-based Health Planning and Services (CHPS)," Case study report. Washington, DC: Population Council. ... and public health research in 50 countries, we work with our partners to deliver solutions that lead to more effective policies, programs, and technologies that improve lives ...
This Costed Implementation Plan (CIP) is being developed as part of the comprehensive multisectoral strategy to reposition FP programs in Ghana and translate policy intent into realistic actionable programme targets and activities. The CIP calls for a concerted action amongst public, private, civil society, faith-based, and nongovernmental ...
Ghana Commitment Objectives. Implement the roll-out of family planning under the National Health Insurance Benefits Package, increasing the number of districts currently providing FP on NHIS to 75% by September 2027 and 100% by 2030. Increase government financial commitment to procure 20% of Ghana's FP commodities needs by 2030, addressing ...
It also shows the importance of including social norms about family size in research about the impact of migration policies on fertility. "Our analyses provide important insights into the unanticipated ways in which immigrant policies impact Hispanics' reproductive and family life in the context of a rapidly changing U.S. immigrant policy ...
In Ghana's three-tier healthcare system, where preventive care and treatment of minor ailments occur at health centers and Community Health Planning and Services (CHPS) compounds, Citation 39 it would be ideal for healthcare providers in those settings to be involved in providing awareness and education about HPV vaccination, even if not ...