An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Prev Med

Qualitative Methods in Health Care Research
Vishnu renjith.
School of Nursing and Midwifery, Royal College of Surgeons Ireland - Bahrain (RCSI Bahrain), Al Sayh Muharraq Governorate, Bahrain
Renjulal Yesodharan
1 Department of Mental Health Nursing, Manipal College of Nursing Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India
Judith A. Noronha
2 Department of OBG Nursing, Manipal College of Nursing Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India
Elissa Ladd
3 School of Nursing, MGH Institute of Health Professions, Boston, USA
Anice George
4 Department of Child Health Nursing, Manipal College of Nursing Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India
Healthcare research is a systematic inquiry intended to generate robust evidence about important issues in the fields of medicine and healthcare. Qualitative research has ample possibilities within the arena of healthcare research. This article aims to inform healthcare professionals regarding qualitative research, its significance, and applicability in the field of healthcare. A wide variety of phenomena that cannot be explained using the quantitative approach can be explored and conveyed using a qualitative method. The major types of qualitative research designs are narrative research, phenomenological research, grounded theory research, ethnographic research, historical research, and case study research. The greatest strength of the qualitative research approach lies in the richness and depth of the healthcare exploration and description it makes. In health research, these methods are considered as the most humanistic and person-centered way of discovering and uncovering thoughts and actions of human beings.
Introduction
Healthcare research is a systematic inquiry intended to generate trustworthy evidence about issues in the field of medicine and healthcare. The three principal approaches to health research are the quantitative, the qualitative, and the mixed methods approach. The quantitative research method uses data, which are measures of values and counts and are often described using statistical methods which in turn aids the researcher to draw inferences. Qualitative research incorporates the recording, interpreting, and analyzing of non-numeric data with an attempt to uncover the deeper meanings of human experiences and behaviors. Mixed methods research, the third methodological approach, involves collection and analysis of both qualitative and quantitative information with an objective to solve different but related questions, or at times the same questions.[ 1 , 2 ]
In healthcare, qualitative research is widely used to understand patterns of health behaviors, describe lived experiences, develop behavioral theories, explore healthcare needs, and design interventions.[ 1 , 2 , 3 ] Because of its ample applications in healthcare, there has been a tremendous increase in the number of health research studies undertaken using qualitative methodology.[ 4 , 5 ] This article discusses qualitative research methods, their significance, and applicability in the arena of healthcare.
Qualitative Research
Diverse academic and non-academic disciplines utilize qualitative research as a method of inquiry to understand human behavior and experiences.[ 6 , 7 ] According to Munhall, “Qualitative research involves broadly stated questions about human experiences and realities, studied through sustained contact with the individual in their natural environments and producing rich, descriptive data that will help us to understand those individual's experiences.”[ 8 ]
Significance of Qualitative Research
The qualitative method of inquiry examines the 'how' and 'why' of decision making, rather than the 'when,' 'what,' and 'where.'[ 7 ] Unlike quantitative methods, the objective of qualitative inquiry is to explore, narrate, and explain the phenomena and make sense of the complex reality. Health interventions, explanatory health models, and medical-social theories could be developed as an outcome of qualitative research.[ 9 ] Understanding the richness and complexity of human behavior is the crux of qualitative research.
Differences between Quantitative and Qualitative Research
The quantitative and qualitative forms of inquiry vary based on their underlying objectives. They are in no way opposed to each other; instead, these two methods are like two sides of a coin. The critical differences between quantitative and qualitative research are summarized in Table 1 .[ 1 , 10 , 11 ]
Differences between quantitative and qualitative research
| Areas | Quantitative Research | Qualitative Research |
|---|---|---|
| Nature of reality | Assumes there is a single reality. | Assumes existence of dynamic and multiple reality. |
| Goal | Test and confirm hypotheses. | Explore and understand phenomena. |
| Data collection methods | Highly structured methods like questionnaires, inventories and scales. | Semi structured like in-depth interviews, observations and focus group discussions. |
| Design | Predetermined and rigid design. | Flexible and emergent design. |
| Reasoning | Deductive process to test the hypothesis. | Primarily inductive to develop the theory or hypothesis. |
| Focus | Concerned with the outcomes and prediction of the causal relationships. | Concerned primarily with process, rather than outcomes or products. |
| Sampling | Rely largely on random sampling methods. | Based on purposive sampling methods. |
| Sample size determination | Involves a-priori sample size calculation. | Collect data until data saturation is achieved. |
| Sample size | Relatively large. | Small sample size but studied in-depth. |
| Data analysis | Variable based and use of statistical or mathematical methods. | Case based and use non statistical descriptive or interpretive methods. |
Qualitative Research Questions and Purpose Statements
Qualitative questions are exploratory and are open-ended. A well-formulated study question forms the basis for developing a protocol, guides the selection of design, and data collection methods. Qualitative research questions generally involve two parts, a central question and related subquestions. The central question is directed towards the primary phenomenon under study, whereas the subquestions explore the subareas of focus. It is advised not to have more than five to seven subquestions. A commonly used framework for designing a qualitative research question is the 'PCO framework' wherein, P stands for the population under study, C stands for the context of exploration, and O stands for the outcome/s of interest.[ 12 ] The PCO framework guides researchers in crafting a focused study question.
Example: In the question, “What are the experiences of mothers on parenting children with Thalassemia?”, the population is “mothers of children with Thalassemia,” the context is “parenting children with Thalassemia,” and the outcome of interest is “experiences.”
The purpose statement specifies the broad focus of the study, identifies the approach, and provides direction for the overall goal of the study. The major components of a purpose statement include the central phenomenon under investigation, the study design and the population of interest. Qualitative research does not require a-priori hypothesis.[ 13 , 14 , 15 ]
Example: Borimnejad et al . undertook a qualitative research on the lived experiences of women suffering from vitiligo. The purpose of this study was, “to explore lived experiences of women suffering from vitiligo using a hermeneutic phenomenological approach.” [ 16 ]
Review of the Literature
In quantitative research, the researchers do an extensive review of scientific literature prior to the commencement of the study. However, in qualitative research, only a minimal literature search is conducted at the beginning of the study. This is to ensure that the researcher is not influenced by the existing understanding of the phenomenon under the study. The minimal literature review will help the researchers to avoid the conceptual pollution of the phenomenon being studied. Nonetheless, an extensive review of the literature is conducted after data collection and analysis.[ 15 ]
Reflexivity
Reflexivity refers to critical self-appraisal about one's own biases, values, preferences, and preconceptions about the phenomenon under investigation. Maintaining a reflexive diary/journal is a widely recognized way to foster reflexivity. According to Creswell, “Reflexivity increases the credibility of the study by enhancing more neutral interpretations.”[ 7 ]
Types of Qualitative Research Designs
The qualitative research approach encompasses a wide array of research designs. The words such as types, traditions, designs, strategies of inquiry, varieties, and methods are used interchangeably. The major types of qualitative research designs are narrative research, phenomenological research, grounded theory research, ethnographic research, historical research, and case study research.[ 1 , 7 , 10 ]
Narrative research
Narrative research focuses on exploring the life of an individual and is ideally suited to tell the stories of individual experiences.[ 17 ] The purpose of narrative research is to utilize 'story telling' as a method in communicating an individual's experience to a larger audience.[ 18 ] The roots of narrative inquiry extend to humanities including anthropology, literature, psychology, education, history, and sociology. Narrative research encompasses the study of individual experiences and learning the significance of those experiences. The data collection procedures include mainly interviews, field notes, letters, photographs, diaries, and documents collected from one or more individuals. Data analysis involves the analysis of the stories or experiences through “re-storying of stories” and developing themes usually in chronological order of events. Rolls and Payne argued that narrative research is a valuable approach in health care research, to gain deeper insight into patient's experiences.[ 19 ]
Example: Karlsson et al . undertook a narrative inquiry to “explore how people with Alzheimer's disease present their life story.” Data were collected from nine participants. They were asked to describe about their life experiences from childhood to adulthood, then to current life and their views about the future life. [ 20 ]
Phenomenological research
Phenomenology is a philosophical tradition developed by German philosopher Edmond Husserl. His student Martin Heidegger did further developments in this methodology. It defines the 'essence' of individual's experiences regarding a certain phenomenon.[ 1 ] The methodology has its origin from philosophy, psychology, and education. The purpose of qualitative research is to understand the people's everyday life experiences and reduce it into the central meaning or the 'essence of the experience'.[ 21 , 22 ] The unit of analysis of phenomenology is the individuals who have had similar experiences of the phenomenon. Interviews with individuals are mainly considered for the data collection, though, documents and observations are also useful. Data analysis includes identification of significant meaning elements, textural description (what was experienced), structural description (how was it experienced), and description of 'essence' of experience.[ 1 , 7 , 21 ] The phenomenological approach is further divided into descriptive and interpretive phenomenology. Descriptive phenomenology focuses on the understanding of the essence of experiences and is best suited in situations that need to describe the lived phenomenon. Hermeneutic phenomenology or Interpretive phenomenology moves beyond the description to uncover the meanings that are not explicitly evident. The researcher tries to interpret the phenomenon, based on their judgment rather than just describing it.[ 7 , 21 , 22 , 23 , 24 ]
Example: A phenomenological study conducted by Cornelio et al . aimed at describing the lived experiences of mothers in parenting children with leukemia. Data from ten mothers were collected using in-depth semi-structured interviews and were analyzed using Husserl's method of phenomenology. Themes such as “pivotal moment in life”, “the experience of being with a seriously ill child”, “having to keep distance with the relatives”, “overcoming the financial and social commitments”, “responding to challenges”, “experience of faith as being key to survival”, “health concerns of the present and future”, and “optimism” were derived. The researchers reported the essence of the study as “chronic illness such as leukemia in children results in a negative impact on the child and on the mother.” [ 25 ]
Grounded Theory Research
Grounded theory has its base in sociology and propagated by two sociologists, Barney Glaser, and Anselm Strauss.[ 26 ] The primary purpose of grounded theory is to discover or generate theory in the context of the social process being studied. The major difference between grounded theory and other approaches lies in its emphasis on theory generation and development. The name grounded theory comes from its ability to induce a theory grounded in the reality of study participants.[ 7 , 27 ] Data collection in grounded theory research involves recording interviews from many individuals until data saturation. Constant comparative analysis, theoretical sampling, theoretical coding, and theoretical saturation are unique features of grounded theory research.[ 26 , 27 , 28 ] Data analysis includes analyzing data through 'open coding,' 'axial coding,' and 'selective coding.'[ 1 , 7 ] Open coding is the first level of abstraction, and it refers to the creation of a broad initial range of categories, axial coding is the procedure of understanding connections between the open codes, whereas selective coding relates to the process of connecting the axial codes to formulate a theory.[ 1 , 7 ] Results of the grounded theory analysis are supplemented with a visual representation of major constructs usually in the form of flow charts or framework diagrams. Quotations from the participants are used in a supportive capacity to substantiate the findings. Strauss and Corbin highlights that “the value of the grounded theory lies not only in its ability to generate a theory but also to ground that theory in the data.”[ 27 ]
Example: Williams et al . conducted a grounded theory research to explore the nature of relationship between the sense of self and the eating disorders. Data were collected form 11 women with a lifetime history of Anorexia Nervosa and were analyzed using the grounded theory methodology. Analysis led to the development of a theoretical framework on the nature of the relationship between the self and Anorexia Nervosa. [ 29 ]
Ethnographic research
Ethnography has its base in anthropology, where the anthropologists used it for understanding the culture-specific knowledge and behaviors. In health sciences research, ethnography focuses on narrating and interpreting the health behaviors of a culture-sharing group. 'Culture-sharing group' in an ethnography represents any 'group of people who share common meanings, customs or experiences.' In health research, it could be a group of physicians working in rural care, a group of medical students, or it could be a group of patients who receive home-based rehabilitation. To understand the cultural patterns, researchers primarily observe the individuals or group of individuals for a prolonged period of time.[ 1 , 7 , 30 ] The scope of ethnography can be broad or narrow depending on the aim. The study of more general cultural groups is termed as macro-ethnography, whereas micro-ethnography focuses on more narrowly defined cultures. Ethnography is usually conducted in a single setting. Ethnographers collect data using a variety of methods such as observation, interviews, audio-video records, and document reviews. A written report includes a detailed description of the culture sharing group with emic and etic perspectives. When the researcher reports the views of the participants it is called emic perspectives and when the researcher reports his or her views about the culture, the term is called etic.[ 7 ]
Example: The aim of the ethnographic study by LeBaron et al . was to explore the barriers to opioid availability and cancer pain management in India. The researchers collected data from fifty-nine participants using in-depth semi-structured interviews, participant observation, and document review. The researchers identified significant barriers by open coding and thematic analysis of the formal interview. [ 31 ]
Historical research
Historical research is the “systematic collection, critical evaluation, and interpretation of historical evidence”.[ 1 ] The purpose of historical research is to gain insights from the past and involves interpreting past events in the light of the present. The data for historical research are usually collected from primary and secondary sources. The primary source mainly includes diaries, first hand information, and writings. The secondary sources are textbooks, newspapers, second or third-hand accounts of historical events and medical/legal documents. The data gathered from these various sources are synthesized and reported as biographical narratives or developmental perspectives in chronological order. The ideas are interpreted in terms of the historical context and significance. The written report describes 'what happened', 'how it happened', 'why it happened', and its significance and implications to current clinical practice.[ 1 , 10 ]
Example: Lubold (2019) analyzed the breastfeeding trends in three countries (Sweden, Ireland, and the United States) using a historical qualitative method. Through analysis of historical data, the researcher found that strong family policies, adherence to international recommendations and adoption of baby-friendly hospital initiative could greatly enhance the breastfeeding rates. [ 32 ]
Case study research
Case study research focuses on the description and in-depth analysis of the case(s) or issues illustrated by the case(s). The design has its origin from psychology, law, and medicine. Case studies are best suited for the understanding of case(s), thus reducing the unit of analysis into studying an event, a program, an activity or an illness. Observations, one to one interviews, artifacts, and documents are used for collecting the data, and the analysis is done through the description of the case. From this, themes and cross-case themes are derived. A written case study report includes a detailed description of one or more cases.[ 7 , 10 ]
Example: Perceptions of poststroke sexuality in a woman of childbearing age was explored using a qualitative case study approach by Beal and Millenbrunch. Semi structured interview was conducted with a 36- year mother of two children with a history of Acute ischemic stroke. The data were analyzed using an inductive approach. The authors concluded that “stroke during childbearing years may affect a woman's perception of herself as a sexual being and her ability to carry out gender roles”. [ 33 ]
Sampling in Qualitative Research
Qualitative researchers widely use non-probability sampling techniques such as purposive sampling, convenience sampling, quota sampling, snowball sampling, homogeneous sampling, maximum variation sampling, extreme (deviant) case sampling, typical case sampling, and intensity sampling. The selection of a sampling technique depends on the nature and needs of the study.[ 34 , 35 , 36 , 37 , 38 , 39 , 40 ] The four widely used sampling techniques are convenience sampling, purposive sampling, snowball sampling, and intensity sampling.
Convenience sampling
It is otherwise called accidental sampling, where the researchers collect data from the subjects who are selected based on accessibility, geographical proximity, ease, speed, and or low cost.[ 34 ] Convenience sampling offers a significant benefit of convenience but often accompanies the issues of sample representation.
Purposive sampling
Purposive or purposeful sampling is a widely used sampling technique.[ 35 ] It involves identifying a population based on already established sampling criteria and then selecting subjects who fulfill that criteria to increase the credibility. However, choosing information-rich cases is the key to determine the power and logic of purposive sampling in a qualitative study.[ 1 ]
Snowball sampling
The method is also known as 'chain referral sampling' or 'network sampling.' The sampling starts by having a few initial participants, and the researcher relies on these early participants to identify additional study participants. It is best adopted when the researcher wishes to study the stigmatized group, or in cases, where findings of participants are likely to be difficult by ordinary means. Respondent ridden sampling is an improvised version of snowball sampling used to find out the participant from a hard-to-find or hard-to-study population.[ 37 , 38 ]
Intensity sampling
The process of identifying information-rich cases that manifest the phenomenon of interest is referred to as intensity sampling. It requires prior information, and considerable judgment about the phenomenon of interest and the researcher should do some preliminary investigations to determine the nature of the variation. Intensity sampling will be done once the researcher identifies the variation across the cases (extreme, average and intense) and picks the intense cases from them.[ 40 ]
Deciding the Sample Size
A-priori sample size calculation is not undertaken in the case of qualitative research. Researchers collect the data from as many participants as possible until they reach the point of data saturation. Data saturation or the point of redundancy is the stage where the researcher no longer sees or hears any new information. Data saturation gives the idea that the researcher has captured all possible information about the phenomenon of interest. Since no further information is being uncovered as redundancy is achieved, at this point the data collection can be stopped. The objective here is to get an overall picture of the chronicle of the phenomenon under the study rather than generalization.[ 1 , 7 , 41 ]
Data Collection in Qualitative Research
The various strategies used for data collection in qualitative research includes in-depth interviews (individual or group), focus group discussions (FGDs), participant observation, narrative life history, document analysis, audio materials, videos or video footage, text analysis, and simple observation. Among all these, the three popular methods are the FGDs, one to one in-depth interviews and the participant observation.
FGDs are useful in eliciting data from a group of individuals. They are normally built around a specific topic and are considered as the best approach to gather data on an entire range of responses to a topic.[ 42 Group size in an FGD ranges from 6 to 12. Depending upon the nature of participants, FGDs could be homogeneous or heterogeneous.[ 1 , 14 ] One to one in-depth interviews are best suited to obtain individuals' life histories, lived experiences, perceptions, and views, particularly while exporting topics of sensitive nature. In-depth interviews can be structured, unstructured, or semi-structured. However, semi-structured interviews are widely used in qualitative research. Participant observations are suitable for gathering data regarding naturally occurring behaviors.[ 1 ]
Data Analysis in Qualitative Research
Various strategies are employed by researchers to analyze data in qualitative research. Data analytic strategies differ according to the type of inquiry. A general content analysis approach is described herewith. Data analysis begins by transcription of the interview data. The researcher carefully reads data and gets a sense of the whole. Once the researcher is familiarized with the data, the researcher strives to identify small meaning units called the 'codes.' The codes are then grouped based on their shared concepts to form the primary categories. Based on the relationship between the primary categories, they are then clustered into secondary categories. The next step involves the identification of themes and interpretation to make meaning out of data. In the results section of the manuscript, the researcher describes the key findings/themes that emerged. The themes can be supported by participants' quotes. The analytical framework used should be explained in sufficient detail, and the analytic framework must be well referenced. The study findings are usually represented in a schematic form for better conceptualization.[ 1 , 7 ] Even though the overall analytical process remains the same across different qualitative designs, each design such as phenomenology, ethnography, and grounded theory has design specific analytical procedures, the details of which are out of the scope of this article.
Computer-Assisted Qualitative Data Analysis Software (CAQDAS)
Until recently, qualitative analysis was done either manually or with the help of a spreadsheet application. Currently, there are various software programs available which aid researchers to manage qualitative data. CAQDAS is basically data management tools and cannot analyze the qualitative data as it lacks the ability to think, reflect, and conceptualize. Nonetheless, CAQDAS helps researchers to manage, shape, and make sense of unstructured information. Open Code, MAXQDA, NVivo, Atlas.ti, and Hyper Research are some of the widely used qualitative data analysis software.[ 14 , 43 ]
Reporting Guidelines
Consolidated Criteria for Reporting Qualitative Research (COREQ) is the widely used reporting guideline for qualitative research. This 32-item checklist assists researchers in reporting all the major aspects related to the study. The three major domains of COREQ are the 'research team and reflexivity', 'study design', and 'analysis and findings'.[ 44 , 45 ]
Critical Appraisal of Qualitative Research
Various scales are available to critical appraisal of qualitative research. The widely used one is the Critical Appraisal Skills Program (CASP) Qualitative Checklist developed by CASP network, UK. This 10-item checklist evaluates the quality of the study under areas such as aims, methodology, research design, ethical considerations, data collection, data analysis, and findings.[ 46 ]
Ethical Issues in Qualitative Research
A qualitative study must be undertaken by grounding it in the principles of bioethics such as beneficence, non-maleficence, autonomy, and justice. Protecting the participants is of utmost importance, and the greatest care has to be taken while collecting data from a vulnerable research population. The researcher must respect individuals, families, and communities and must make sure that the participants are not identifiable by their quotations that the researchers include when publishing the data. Consent for audio/video recordings must be obtained. Approval to be in FGDs must be obtained from the participants. Researchers must ensure the confidentiality and anonymity of the transcripts/audio-video records/photographs/other data collected as a part of the study. The researchers must confirm their role as advocates and proceed in the best interest of all participants.[ 42 , 47 , 48 ]
Rigor in Qualitative Research
The demonstration of rigor or quality in the conduct of the study is essential for every research method. However, the criteria used to evaluate the rigor of quantitative studies are not be appropriate for qualitative methods. Lincoln and Guba (1985) first outlined the criteria for evaluating the qualitative research often referred to as “standards of trustworthiness of qualitative research”.[ 49 ] The four components of the criteria are credibility, transferability, dependability, and confirmability.
Credibility refers to confidence in the 'truth value' of the data and its interpretation. It is used to establish that the findings are true, credible and believable. Credibility is similar to the internal validity in quantitative research.[ 1 , 50 , 51 ] The second criterion to establish the trustworthiness of the qualitative research is transferability, Transferability refers to the degree to which the qualitative results are applicability to other settings, population or contexts. This is analogous to the external validity in quantitative research.[ 1 , 50 , 51 ] Lincoln and Guba recommend authors provide enough details so that the users will be able to evaluate the applicability of data in other contexts.[ 49 ] The criterion of dependability refers to the assumption of repeatability or replicability of the study findings and is similar to that of reliability in quantitative research. The dependability question is 'Whether the study findings be repeated of the study is replicated with the same (similar) cohort of participants, data coders, and context?'[ 1 , 50 , 51 ] Confirmability, the fourth criteria is analogous to the objectivity of the study and refers the degree to which the study findings could be confirmed or corroborated by others. To ensure confirmability the data should directly reflect the participants' experiences and not the bias, motivations, or imaginations of the inquirer.[ 1 , 50 , 51 ] Qualitative researchers should ensure that the study is conducted with enough rigor and should report the measures undertaken to enhance the trustworthiness of the study.
Conclusions
Qualitative research studies are being widely acknowledged and recognized in health care practice. This overview illustrates various qualitative methods and shows how these methods can be used to generate evidence that informs clinical practice. Qualitative research helps to understand the patterns of health behaviors, describe illness experiences, design health interventions, and develop healthcare theories. The ultimate strength of the qualitative research approach lies in the richness of the data and the descriptions and depth of exploration it makes. Hence, qualitative methods are considered as the most humanistic and person-centered way of discovering and uncovering thoughts and actions of human beings.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
- Systematic review
- Open access
- Published: 10 October 2019
An integrative review on methodological considerations in mental health research – design, sampling, data collection procedure and quality assurance
- Eric Badu ORCID: orcid.org/0000-0002-0593-3550 1 ,
- Anthony Paul O’Brien 2 &
- Rebecca Mitchell 3
Archives of Public Health volume 77 , Article number: 37 ( 2019 ) Cite this article
23k Accesses
20 Citations
1 Altmetric
Metrics details
Several typologies and guidelines are available to address the methodological and practical considerations required in mental health research. However, few studies have actually attempted to systematically identify and synthesise these considerations. This paper provides an integrative review that identifies and synthesises the available research evidence on mental health research methodological considerations.
A search of the published literature was conducted using EMBASE, Medline, PsycINFO, CINAHL, Web of Science, and Scopus. The search was limited to papers published in English for the timeframe 2000–2018. Using pre-defined inclusion and exclusion criteria, three reviewers independently screened the retrieved papers. A data extraction form was used to extract data from the included papers.
Of 27 papers meeting the inclusion criteria, 13 focused on qualitative research, 8 mixed methods and 6 papers focused on quantitative methodology. A total of 14 papers targeted global mental health research, with 2 papers each describing studies in Germany, Sweden and China. The review identified several methodological considerations relating to study design, methods, data collection, and quality assurance. Methodological issues regarding the study design included assembling team members, familiarisation and sharing information on the topic, and seeking the contribution of team members. Methodological considerations to facilitate data collection involved adequate preparation prior to fieldwork, appropriateness and adequacy of the sampling and data collection approach, selection of consumers, the social or cultural context, practical and organisational skills; and ethical and sensitivity issues.
The evidence confirms that studies on methodological considerations in conducting mental health research largely focus on qualitative studies in a transcultural setting, as well as recommendations derived from multi-site surveys. Mental health research should adequately consider the methodological issues around study design, sampling, data collection procedures and quality assurance in order to maintain the quality of data collection.
Peer Review reports
In the past decades there has been considerable attention on research methods to facilitate studies in various academic fields, such as public health, education, humanities, behavioural and social sciences [ 1 , 2 , 3 , 4 ]. These research methodologies have generally focused on the two major research pillars known as quantitative or qualitative research. In recent years, researchers conducting mental health research appear to be either employing both qualitative and quantitative research methods separately, or mixed methods approaches to triangulate and validate findings [ 5 , 6 ].
A combination of study designs has been utilised to answer research questions associated with mental health services and consumer outcomes [ 7 , 8 ]. Study designs in the public health and clinical domains, for example, have largely focused on observational studies (non-interventional) and experimental research (interventional) [ 1 , 3 , 9 ]. Observational design in non-interventional research requires the investigator to simply observe, record, classify, count and analyse the data [ 1 , 2 , 10 ]. This design is different from the observational approaches used in social science research, which may involve observing (participant and non- participant) phenomena in the fieldwork [ 1 ]. Furthermore, the observational study has been categorized into five types, namely cross-sectional design, case-control studies, cohort studies, case report and case series studies [ 1 , 2 , 3 , 9 , 10 , 11 ]. The cross-sectional design is used to measure the occurrence of a condition at a one-time point, sometimes referred to as a prevalence study. This approach of conducting research is relatively quick and easy but does not permit a distinction between cause and effect [ 1 ]. Conversely, the case-control is a design that examines the relationship between an attribute and a disease by comparing those with and without the disease [ 1 , 2 , 12 ]. In addition, the case-control design is usually retrospective and aims to identify predictors of a particular outcome. This type of design is relevant when investigating rare or chronic diseases which may result from long-term exposure to particular risk factors [ 10 ]. Cohort studies measure the relationship between exposure to a factor and the probability of the occurrence of a disease [ 1 , 10 ]. In a case series design, medical records are reviewed for exposure to determinants of disease and outcomes. More importantly, case series and case reports are often used as preliminary research to provide information on key clinical issues [ 12 ].
The interventional study design describes a research approach that applies clinical care to evaluate treatment effects on outcomes [ 13 ]. Several previous studies have explained the various forms of experimental study design used in public health and clinical research [ 14 , 15 ]. In particular, experimental studies have been categorized into randomized controlled trials (RCTs), non-randomized controlled trials, and quasi-experimental designs [ 14 ]. The randomized trial is a comparative study where participants are randomly assigned to one of two groups. This research examines a comparison between a group receiving treatment and a control group receiving treatment as usual or receiving a placebo. Herein, the exposure to the intervention is determined by random allocation [ 16 , 17 ].
Recently, research methodologists have given considerable attention to the development of methodologies to conduct research in vulnerable populations. Vulnerable population research, such as with mental health consumers often involves considering the challenges associated with sampling (selecting marginalized participants), collecting data and analysing it, as well as research engagement. Consequently, several empirical studies have been undertaken to document the methodological issues and challenges in research involving marginalized populations. In particular, these studies largely addresses the typologies and practical guidelines for conducting empirical studies in mental health. Despite the increasing evidence, however, only a few studies have yet attempted to systematically identify and synthesise the methodological considerations in conducting mental health research from the perspective of consumers.
A preliminary search using the search engines Medline, Web of Science, Google Scholar, and Scopus Index and EMBASE identified only two reviews of mental health based research. Among these two papers, one focused on the various types of mixed methods used in mental health research [ 18 ], whilst the other paper, focused on the role of qualitative studies in mental health research involving mixed methods [ 19 ]. Even though the latter two studies attempted to systematically review mixed methods mental health research, this integrative review is unique, as it collectively synthesises the design, data collection, sampling, and quality assurance issues together, which has not been previously attempted.
This paper provides an integrative review addressing the available evidence on mental health research methodological considerations. The paper also synthesises evidence on the methods, study designs, data collection procedures, analyses and quality assurance measures. Identifying and synthesising evidence on the conduct of mental health research has relevance to clinicians and academic researchers where the evidence provides a guide regarding the methodological issues involved when conducting research in the mental health domain. Additionally, the synthesis can inform clinicians and academia about the gaps in the literature related to methodological considerations.
Methodology
An integrative review was conducted to synthesise the available evidence on mental health research methodological considerations. To guide the review, the World Health Organization (WHO) definition of mental health has been utilised. The WHO defines mental health as: “a state of well-being, in which the individual realises his or her own potentials, ability to cope with the normal stresses of life, functionality and work productivity, as well as the ability to contribute effectively in community life” [ 20 ]. The integrative review enabled the simultaneous inclusion of diverse methodologies (i.e., experimental and non-experimental research) and varied perspectives to fully understand a phenomenon of concern [ 21 , 22 ]. The review also uses diverse data sources to develop a holistic understanding of methodological considerations in mental health research. The methodology employed involves five stages: 1) problem identification (ensuring that the research question and purpose are clearly defined); 2) literature search (incorporating a comprehensive search strategy); 3) data evaluation; 4) data analysis (data reduction, display, comparison and conclusions) and; 5) presentation (synthesising findings in a model or theory and describing the implications for practice, policy and further research) [ 21 ].
Inclusion criteria
The integrative review focused on methodological issues in mental health research. This included core areas such as study design and methods, particularly qualitative, quantitative or both. The review targeted papers that addressed study design, sampling, data collection procedures, quality assurance and the data analysis process. More specifically, the included papers addressed methodological issues on empirical studies in mental health research. The methodological issues in this context are not limited to a particular mental illness. Studies that met the inclusion criteria were peer-reviewed articles published in the English Language, from January 2000 to July 2018.
Exclusion criteria
Articles that were excluded were based purely on general health services or clinical effectiveness of a particular intervention with no connection to mental health research. Articles were also excluded when it addresses non-methodological issues. Other general exclusion criteria were book chapters, conference abstracts, papers that present opinion, editorials, commentaries and clinical case reviews.
Search strategy and selection procedure
The search of published articles was conducted from six electronic databases, namely EMBASE, CINAHL (EBSCO), Web of Science, Scopus, PsycINFO and Medline. We developed a search strategy based on the recommended guidelines by the Joanna Briggs Institute (JBI) [ 23 ]. Specifically, a three-step search strategy was utilised to conduct the search for information (see Table 1 ). An initial limited search was conducted in Medline and Embase (see Table 1 ). We analysed the text words contained in the title and abstract and of the index terms from the initial search results [ 23 ]. A second search using all identified keywords and index terms was then repeated across all remaining five databases (see Table 1 ). Finally, the reference lists of all eligible studies were manually hand searched [ 23 ].
The selection of eligible articles adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 24 ] (see Fig. 1 ). Firstly, three authors independently screened the titles of articles that were retrieved and then approved those meeting the selection criteria. The authors reviewed all the titles and abstracts and agreed on those needing full-text screening. E.B (Eric Badu) conducted the initial screening of titles and abstracts. A.P.O’B (Anthony Paul O’Brien) and R.M (Rebecca Mitchell) conducted the second screening of titles and abstracts of all the identified papers. The authors (E.B, A.P.O’B and R.M) conducted full-text screening according to the inclusion and exclusion criteria.
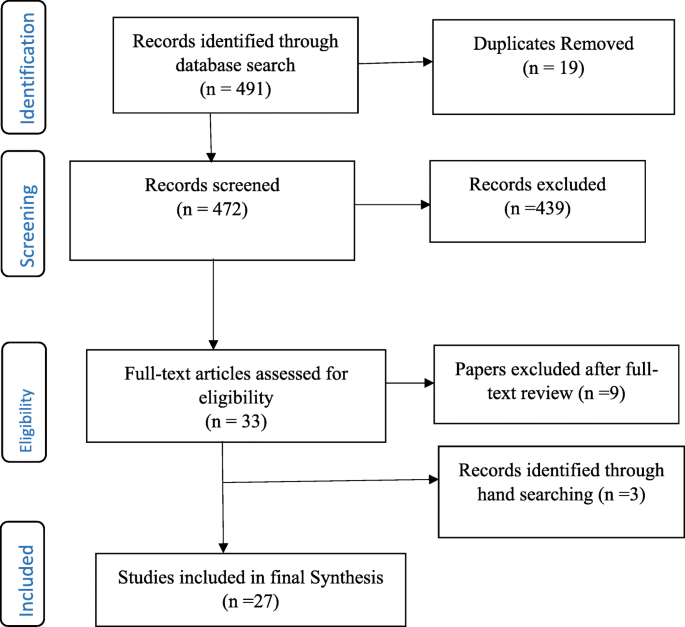
Flow Chart of studies included in the review
Data management and extraction
The integrative review used Endnote ×8 to screen and handle duplicate references. A predefined data extraction form was developed to extract data from all included articles (see Additional file 1 ). The data extraction form was developed according to Joanna Briggs Institute (JBI) [ 23 ] and Cochrane [ 24 ] manuals, as well as the literature associated with concepts and methods in mental health research. The data extraction form was categorised into sub-sections, such as study details (citation, year of publication, author, contact details of lead author, and funder/sponsoring organisation, publication type), objective of the paper, primary subject area of the paper (study design, methods, sampling, data collection, data analysis, quality assurance). The data extraction form also had a section on additional information on methodological consideration, recommendations and other potential references. The authors extracted results of the included papers in numerical and textual format [ 23 ]. EB (Eric Badu) conducted the data extraction, A.P.O’B (Anthony Paul O’Brien) and R.M (Rebecca Mitchell), conducted the second review of the extracted data.
Data synthesis
Content analysis was used to synthesise the extracted data. The content analysis process involved several stages which involved noting patterns and themes, seeing plausibility, clustering, counting, making contrasts and comparisons, discerning common and unusual patterns, subsuming particulars into general, noting relations between variability, finding intervening factors and building a logical chain of evidence [ 21 ] (see Table 2 ).
Study characteristics
The integrative review identified a total of 491 records from all databases, after which 19 duplicates were removed. Out of this, 472 titles and abstracts were assessed for eligibility, after which 439 articles were excluded. Articles not meeting the inclusion criteria were excluded. Specifically, papers excluded were those that did not address methodological issues as well as papers addressing methodological consideration in other disciplines. A total of 33 full-text articles were assessed – 9 articles were further excluded, whilst an additional 3 articles were identified from reference lists. Overall, 27 articles were included in the final synthesis (see Fig. 1 ). Of the total included papers, 12 contained qualitative research, 9 were mixed methods (both qualitative and quantitative) and 6 papers focused on quantitative data. Conversely, a total of 14 papers targeted global mental health research and 2 papers each describing studies in Germany, Sweden and China. The papers addressed different methodological issues, such as study design, methods, data collection, and analysis as well as quality assurance (see Table 3 ).
Mixed methods design in mental health research
Mixed methods research is defined as a research process where the elements of qualitative and quantitative research are combined in the design, data collection, and its triangulation and validation [ 48 ]. The integrative review identified four sub-themes that describe mixed methods design in the context of mental health research. The sub-themes include the categories of mixed methods, their function, structure, process and further methodological considerations for mixed methods design. These sub-themes are explained as follows:
Categorizing mixed methods in mental health research
Four studies highlighted the categories of mixed methods design applicable to mental health research [ 18 , 19 , 43 , 48 ]. Generally, there are differences in the categories of mixed methods design, however, three distinct categories predominantly appear to cross cut in all studies. These categories are function, structure and process. Some studies further categorised mixed method design to include rationale, objectives, or purpose. For instance, Schoonenboom and Johnson [ 48 ] categorised mixed methods design into primary and secondary dimensions.
The function of mixed methods in mental health research
Six studies explain the function of conducting mixed methods design in mental health research. Two studies specifically recommended that mixed methods have the ability to provide a more robust understanding of services by expanding and strengthening the conclusions from the study [ 42 , 45 ]. More importantly, the use of both qualitative and quantitative methods have the ability to provide innovative solutions to important and complex problems, especially by addressing diversity and divergence [ 48 ]. The review identified five underlying functions of a mixed method design in mental health research which include achieving convergence, complementarity, expansion, development and sampling [ 18 , 19 , 43 ].
The use of mixed methods to achieve convergence aims to employ both qualitative and quantitative data to answer the same question, either through triangulation (to confirm the conclusions from each of the methods) or transformation (using qualitative techniques to transform quantitative data). Similarly, complementarity in mixed methods integrates both qualitative and quantitative methods to answer questions for the purpose of evaluation or elaboration [ 18 , 19 , 43 ]. Two papers recommend that qualitative methods are used to provide the depth of understanding, whilst the quantitative methods provide a breadth of understanding [ 18 , 43 ]. In mental health research, the qualitative data is often used to examine treatment processes, whilst the quantitative methods are used to examine treatment outcomes against quality care key performance targets.
Additionally, three papers indicated that expansion as a function of mixed methods uses one type of method to answer questions raised by the other type of method [ 18 , 19 , 43 ]. For instance, qualitative data is used to explain findings from quantitative analysis. Also, some studies highlight that development as a function of mixed methods aims to use one method to answer research questions, and use the findings to inform other methods to answer different research questions. A qualitative method, for example, is used to identify the content of items to be used in a quantitative study. This approach aims to use qualitative methods to create a conceptual framework for generating hypotheses to be tested by using a quantitative method [ 18 , 19 , 43 ]. Three papers suggested that using mixed methods for the purpose of sampling utilize one method (eg. quantitative) to identify a sample of participants to conduct research using other methods (eg. qualitative) [ 18 , 19 , 43 ]. For instance, quantitative data is sequentially utilized to identify potential participants to participate in a qualitative study and the vice versa.
Structure of mixed methods in mental health research
Five studies categorised the structure of conducting mixed methods in mental health research, into two broader concepts including simultaneous (concurrent) and sequential (see Table 3 ). In both categories, one method is regarded as primary and the other as secondary, although equal weight can be given to both methods [ 18 , 19 , 42 , 43 , 48 ]. Two studies suggested that the sequential design is a process where the data collection and analysis of one component (eg. quantitative) takes place after the data collection and analysis of the other component (eg qualitative). Herein, the data collection and analysis of one component (e.g. qualitative) may depend on the outcomes of the other component (e.g. quantitative) [ 43 , 48 ]. An earlier review suggested that the majority of contemporary studies in mental health research use a sequential design, with qualitative methods, more often preceding quantitative methods [ 18 ].
Alternatively, the concurrent design collects and analyses data of both components (e.g. quantitative and qualitative) simultaneously and independently. Palinkas, Horwitz [ 42 ] recommend that one component is used as secondary to the other component, or that both components are assigned equal priority. Such a mixed methods approach aims to provide a depth of understanding afforded by qualitative methods, with the breadth of understanding offered by the quantitative data to elaborate on the findings of one component or seek convergence through triangulation of the results. Schoonenboom and Johnson [ 48 ] recommended the use of capital letters for one component and lower case letters for another component in the same design to indicate that one component is primary and the other is secondary or supplemental.
Process of mixed methods in mental health research
Five papers highlighted the process for the use of mixed methods in mental health research [ 18 , 19 , 42 , 43 , 48 ]. The papers suggested three distinct processes or strategies for combining qualitative and quantitative data. These include merging or converging the two data sets, connecting the two datasets by having one build upon the other; and embedding one data set within the other [ 19 , 43 ]. The process of connecting occurs when the analysis of one dataset leads to the need for the other data set. For instance, in the situation where quantitative results lead to the subsequent collection and analysis of qualitative data [ 18 , 43 ]. A previous study suggested that most studies in mental health sought to connect the data sets. Similarly, the process of merging the datasets brings together two sets of data during the interpretation, or transforms one type of data into the other type, by combining the data into new variables [ 18 ]. The process of embedding data into mixed method designs in mental health uses one dataset to provide a supportive role to the other dataset [ 43 ].
Consideration for using mixed methods in mental health research
Three studies highlighted several factors that need to be considered when conducting mixed methods design in mental health research [ 18 , 19 , 45 ]. Accordingly, these factors include developing familiarity with the topic under investigation based on experience, willingness to share information on the topic [ 19 ], establishing early collaboration, willingness to negotiate emerging problems, seeking the contribution of team members, and soliciting third-party assistance to resolve any emerging problems [ 45 ]. Additionally, Palinkas, Horwitz [ 18 ] recommended that mixed methods in the context of mental health research are mostly applied in studies that assess needs of services, examine existing services, developing new or adapting existing services, evaluating services in randomised control trials, and examining service implementation.
Qualitative study in mental health research
This theme describes the various qualitative methods used in mental health research. The theme also addresses methodological considerations for using qualitative methods in mental health research. The key emerging issues are discussed below:
Considering qualitative components in conducting mental health research
Six studies recommended the use of qualitative methods in mental health research [ 19 , 26 , 28 , 32 , 36 , 44 ]. Two qualitative research paradigms were identified, including the interpretive and critical approach [ 32 ]. The interpretive methodologies predominantly explore the meaning of human experiences and actions, whilst the critical approach emphasises the social and historical origins and contexts of meaning [ 32 ]. Two studies suggested that the interpretive qualitative methods used in mental health research are ethnography, phenomenology and narrative approaches [ 32 , 36 ].
The ethnographic approach describes the everyday meaning of the phenomena within a societal and cultural context, for instance, the way phenomena or experience is contrasted within a community, or by collective members over time [ 32 ]. Alternatively, the phenomenological approach explores the claims and concerns of a subject with a speculative development of an interpretative account within their cultural and physical environments focusing on the lived experience [ 32 , 36 ].
Moreover, the critical qualitative approaches used in mental health research are predominantly emancipatory (for instance, socio-political traditions) and participatory action-based research. The emancipatory traditions recognise that knowledge is acquired through critical discourse and debate but are not seen as discovered by objective inquiry [ 32 ]. Alternatively, the participatory action based approach uses critical perspectives to engage key stakeholders as participants in the design and conduct of the research [ 32 ].
Some studies highlighted several reasons why qualitative methods are relevant to mental health research. In particular, qualitative methods are significant as they emphasise naturalistic inquiry and have a discovery-oriented approach [ 19 , 26 ]. Two studies suggested that qualitative methods are often relevant in the initial stages of research studies to understand specific issues such as behaviour, or symptoms of consumers of mental services [ 19 ]. Specifically, Palinkas [ 19 ] suggests that qualitative methods help to obtain initial pilot data, or when there is too little previous research or in the absence of a theory, such as provided in exploratory studies, or previously under-researched phenomena.
Three studies stressed that qualitative methods can help to better understand socially sensitive issues, such as exploring the solutions to overcome challenges in mental health clinical policies [ 19 , 28 , 44 ]. Consequently, Razafsha, Behforuzi [ 44 ] recommended that the natural holistic view of qualitative methods can help to understand the more recovery-oriented policy of mental health, rather than simply the treatment of symptoms. Similarly, the subjective experiences of consumers using qualitative approaches have been found useful to inform clinical policy development [ 28 ].
Sampling in mental health research
The theme explains the sampling approaches used in mental health research. The section also describes the methodological considerations when sampling participants for mental health research. The sub-themes emerging are explained in the following sections:
Sampling approaches (quantitative)
Some studies reviewed highlighted the sampling approaches previously used in mental health research [ 25 , 34 , 35 ]. Generally, all quantitative studies tend to use several probability sampling approaches, whilst qualitative studies used non-probability techniques. The quantitative mental health studies conducted at community and population level employ multi-stage sampling techniques usually involving systematic sampling, stratified and random sampling [ 25 , 34 ]. Similarly, quantitative studies that recruit consumers in the hospital setting employ consecutive sampling [ 35 ]. Two studies reviewed highlighted that the identification of consumers of mental health services for research is usually conducted by service providers. For instance, Korver, Quee [ 35 ] research used a consecutive sampling approach by identifying consumers through clinicians working in regional psychosis departments, or academic centres.
Sampling approaches (qualitative)
Seven studies suggested that the sampling procedures widely used in mental health research involving qualitative methods are non-probability techniques, which include purposive [ 19 , 28 , 32 , 42 , 46 ], snowballing [ 30 , 32 , 46 ] and theoretical sampling [ 31 , 32 ]. The purposive sampling identifies participants that possess relevant characteristics to answer a research question [ 28 ]. Purposive sampling can be used in a single case study, or for multiple cases. The purposive sampling used in mental health research is usually extreme, or deviant case sampling, criterion sampling, and maximum variation sampling [ 19 ]. Furthermore, it is advised when using purposive sampling in a multistage level study, that it should aim to begin with the broader picture to achieve variation, or dispersion, before moving to the more focused view that considers similarity, or central tendencies [ 42 ].
Two studies added that theoretical sampling involved sampling participants, situations and processes based on concepts on theoretical grounds and then using the findings to build theory, such as in a Grounded Theory study [ 31 , 32 ]. Some studies highlighted that snowball sampling is another strategy widely used in mental health research [ 30 , 32 , 46 ]. This is ascribed to the fact that people with mental illness are perceived as marginalised in research and practically hard-to-reach using conventional sampling [ 30 , 32 ]. Snowballing sampling involves asking the marginalised participants to recommend individuals who might have direct knowledge relevant to the study [ 30 , 32 , 46 ]. Although this approach is relevant, some studies advise the limited possibility of generalising the sample, because of the likelihood of selection bias [ 30 ].
Sampling consideration
Four studies in this section highlighted some of the sampling considerations in mental health research [ 30 , 31 , 32 , 46 ]. Generally, mental health research should consider the appropriateness and adequacy of sampling approach by applying attributes such as shared social, or cultural experiences, or shared concern related to the study [ 32 ], diversity and variety of participants [ 31 ], practical and organisational skills, as well as ethical and sensitivity issues [ 46 ]. Robinson [ 46 ] further suggested that sampling can be homogenous or heterogeneous depending on the research questions for the study. Achieving homogeneity in sampling should employ a variety of parameters, which include demographic, graphical, physical, psychological, or life history homogeneity [ 46 ]. Additionally, applying homogeneity in sampling can be influenced by theoretical and practical factors. Alternatively, some samples are intentionally selected based on heterogeneous factors [ 46 ].
Data collection in mental health research
This theme highlights the data collection methods used in mental health research. The theme is explained according to three sub-themes, which include approaches for collecting qualitative data, methodological considerations, as well as preparations for data collection. The sub-themes are as follows:
Approaches for collecting qualitative data
The studies reviewed recommended the approaches that are widely applied in collecting data in mental health research. The widely used qualitative data collection approaches in mental health research are focus group discussions (FGDs) [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ], extended in-depth interviews [ 19 , 30 , 34 ], participant and non-participant observation [ 19 ], Delphi data collection, quasi-statistical techniques [ 19 ] and field notes [ 31 , 40 ]. Seven studies suggest that FGDs are widely used data collection approaches [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ] because they are valuable in gathering information on consumers’ perspectives of services, especially regarding satisfaction, unmet/met service needs and the perceived impact of services [ 47 ]. Conversely, Ekblad and Baarnhielm [ 31 ] recommended that this approach is relevant to improve clinical understanding of the thoughts, emotions, meanings and attitudes towards mental health services.
Such data collection approaches are particularly relevant to consumers of mental health services, due to their low self-confidence and self-esteem [ 41 ]. The approach can help to understand specific terms, vocabulary, opinions and attitudes of consumers of mental health services, as well as their reasoning about personal distress and healing [ 31 ]. Similarly, the reliance on verbal rather than written communication helps to promote the participation of participants with serious and enduring mental health problems [ 31 , 41 ]. Although FGD has several important outcomes, there are some limitations that need critical consideration. Ekblad and Baarnhielm [ 31 ] for example suggest, that marginalised participants may not always feel free to talk about private issues regarding their condition at the group level mostly due to perceived stigma and group confidentiality.
Some studies reviewed recommended that attempting to capture comprehensive information and analysing group interactions in mental health research requires the research method to use field notes as a supplementary data source to help validate the FGDs [ 31 , 40 , 41 ]. The use of field notes in addition to FGDs essentially provides greater detail in the accounts of consumers’ subjective experiences. Furthermore, Montgomery and Bailey [ 40 ] suggest that field notes require observational sensitivity, and also require having specific content such as descriptive and interpretive data.
Three studies in this section suggested that in-depth interviews are used to collect data from consumers of mental health services [ 19 , 30 , 34 ]. This approach is particularly important to explore the behaviour, subjective experiences and psychological processes; opinions, and perceptions of mental health services. de Jong and Van Ommeren [ 30 ] recommend that in-depth interviews help to collect data on culturally marked disorders, their personal and interpersonal significance, patient and family explanatory models, individual and family coping styles, symptom symbols and protective mediators. Palinkas [ 19 ] also highlights that the structured narrative form of extended interviewing is the type of in-depth interview used in mental health research. This approach provides participants with the opportunity to describe the experience of living with an illness and seeking services that assist them.
Consideration for data collection
Six studies recommended consideration required in the data collection process [ 31 , 32 , 37 , 41 , 47 , 49 ]. Some studies highlighted that consumers of mental health services might refuse to participate in research due to several factors [ 37 ] like the severity of their illness, stigma and discrimination [ 41 ]. Subsequently, such issues are recommended to be addressed by building confidence and trust between the researcher and consumers [ 31 , 37 ]. This is a significant prerequisite, as it can sensitise and normalise the research process and aims with the participants prior to discussing their personal mental health issues. Similarly, some studies added that the researcher can gain the confidence of service providers who manage consumers of mental health services [ 41 , 47 ], seek ethical approval from the relevant committee(s) [ 41 , 47 ], meet and greet the consumers of mental health services before data collection, and arrange a mutually acceptable venue for the groups and possibly supply transport [ 41 ].
Two studies further suggested that the cultural and social differences of the participants need consideration [ 26 , 31 ]. These factors could influence the perception and interpretation of ethical issues in the research situation.
Additionally, two studies recommended the use of standardised assessment instruments for mental health research that involve quantitative data collection [ 33 , 49 ]. A recent survey suggested that measures to standardise the data collection approach can convert self-completion instruments to interviewer-completion instruments [ 49 ]. The interviewer can then read the items of the instruments to respondents and record their responses. The study further suggested the need to collect demographic and behavioural information about the participant(s).
Preparing for data collection
Eight studies highlighted the procedures involved in preparing for data collection in mental health research [ 25 , 30 , 33 , 34 , 35 , 39 , 41 , 49 ]. These studies suggest that the preparation process involve organising meetings of researchers, colleagues and representatives of the research population. The meeting of researchers generally involves training of interviewers about the overall design, objectives and research questions associated with the study. de Jong and Van Ommeren [ 30 ] recommended that preparation for the use of quantitative data encompasses translating and adapting instruments with the aim of achieving content, semantic, concept, criterion and technical equivalence.
Quality assurance procedures in mental health research
This section describes the quality assurance procedures used in mental health research. Quality assurance is explained according to three sub-themes: 1) seeking informed consent, 2) the procedure for ensuring quality assurance in a quantitative study and 3) the procedure for ensuring quality control in a qualitative study. The sub-themes are explained in the following content.
Seeking informed consent
The papers analysed for the integrative review suggested that the rights of participants to safeguard their integrity must always be respected, and so each potential subject must be adequately informed of the aims, methods, anticipated benefits and potential hazards of the study and any potential discomforts (see Table 3 ). Seven studies highlight that potential participants of mental health research must be consented to the study prior to data collection [ 25 , 26 , 33 , 35 , 37 , 39 , 47 ]. The consent process helps to assure participants of anonymity and confidentiality and further explain the research procedure to them. Baarnhielm and Ekblad [ 26 ] argue that the research should be guided by four basic moral values for medical ethics, autonomy, non-maleficence, beneficence, and justice. In particular, potential consumers of mental health services who may have severe conditions and unable to consent themselves are expected to have their consent signed by a respective family caregiver [ 37 ]. Latvala, Vuokila-Oikkonen [ 37 ] further suggested that researchers are responsible to agree on the criteria to determine the competency of potential participants in mental health research. The criteria are particularly relevant when potential participants have difficulties in understanding information due to their mental illness.
Procedure for ensuring quality control (quantitative)
Several studies highlighted procedures for ensuring quality control in mental health research (see Table 3 ). The quality control measures are used to achieve the highest reliability, validity and timeliness. Some studies demonstrate that ensuring quality control should consider factors such as pre-testing tools [ 25 , 49 ], minimising non-response rates [ 25 , 39 ] and monitoring of data collection processes [ 25 , 33 , 49 ].
Accordingly, two studies suggested that efforts should be made to re-approach participants who initially refuse to participate in the study. For instance, Liu, Huang [ 39 ] recommended that when a consumer of mental health services refuse to participate in a study (due to low self-esteem) when approached for the first time, a different interviewer can re-approach the same participant to see if they are more comfortable to participate after the first invitation. Three studies further recommend that monitoring data quality can be accomplished through “checks across individuals, completion status and checks across variables” [ 25 , 33 , 49 ]. For example, Alonso, Angermeyer [ 25 ] advocate that various checks are used to verify completion of the interview, and consistency across instruments against the standard procedure.
Procedure for ensuring quality control (qualitative)
Four studies highlighted the procedures for ensuring quality control of qualitative data in mental health research [ 19 , 32 , 37 , 46 ]. A further two studies suggested that the quality of qualitative research is governed by the principles of credibility, dependability, transferability, reflexivity, confirmability [ 19 , 32 ]. Some studies explain that the credibility or trustworthiness of qualitative research in mental health is determined by methodological and interpretive rigour of the phenomenon being investigated [ 32 , 37 ]. Consequently, Fossey, Harvey [ 32 ] propose that the methodological rigour for assessing the credibility of qualitative research are congruence, responsiveness or sensitivity to social context, appropriateness (importance and impact), adequacy and transparency. Similarly, interpretive rigour is classified as authenticity, coherence, reciprocity, typicality and permeability of the researcher’s intentions; including engagement and interpretation [ 32 ].
Robinson [ 46 ] explained that transparency (openness and honesty) is achieved if the research report explicitly addresses how the sampling, data collection, analysis, and presentation are met. In particular, efforts to address these methodological issues highlight the extent to which the criteria for quality profoundly interacts with standards for ethics. Similarly, responsiveness, or sensitivity, helps to situate or locate the study within a place, a time and a meaningful group [ 46 ]. The study should also consider the researcher’s background, location and connection to the study setting, particularly in the recruitment process. This is often described as role conflict or research bias.
In the interpretive phenomenon, coherence highlights the ability to select an appropriate sampling procedure that mutually matches the research aims, questions, data collection, analysis, as well as any theoretical concepts or frameworks [ 32 , 46 ]. Similarly, authenticity explains the appropriate representation of participants’ perspectives in the research process and the interpretation of results. Authenticity is maximised by providing evidence that participants are adequately represented in the interpretive process, or provided an opportunity to give feedback on the researcher’s interpretation [ 32 ]. Again, the contribution of the researcher’s perspective to the interpretation enhances permeability. Fossey, Harvey [ 32 ] further suggest that reflexive reporting, which distinguishes the participants’ voices from that of the researcher in the report, enhances the permeability of the researcher’s role and perspective.
One study highlighted the approaches used to ensure validity in qualitative research, which includes saturation, identification of deviant or non-confirmatory cases, member checking and coding by consensus. Saturation involves completeness in the research process, where all relevant data collection, codes and themes required to answer the phenomenon of inquiry are achieved; and no new data emerges [ 19 ]. Similarly, member checking is the process whereby participants or others who share similar characteristics review study findings to elaborate on confirming them [ 19 ]. The coding by consensus involves a collaborative approach to analysing the data. Ensuring regular meetings among coders to discuss procedures for assigning codes to segments of data and resolve differences in coding procedures, and by comparison of codes assigned on selected transcripts to calculate a percentage agreement or kappa measure of interrater reliability, are commonly applied [ 19 ].
Two studies recommend the need to acknowledge the importance of generalisability (transferability). This concept aims to provide sufficient information about the research setting, findings and interpretations for readers to appropriately determine the replicability of the findings from one context, or population to another, otherwise known as reliability in quantitative research [ 19 , 32 ]. Similarly, the researchers should employ reflexivity as a means of identifying and addressing potential biases in data collection and interpretation. Palinkas [ 19 ] suggests that such bias is associated with theoretical orientations; pre-conceived beliefs, assumptions, and demographic characteristics; and familiarity and experience with the methods and phenomenon. Another approach to enhance the rigour of analysis involves peer debriefing and support meetings held among team members which facilitate detailed auditing during data analysis [ 19 ].
The integrative review was conducted to synthesise evidence into recommended methodological considerations when conducting mental health research. The evidence from the review has been discussed according to five major themes: 1) mixed methods study in mental health research; 2) qualitative study in mental health research; 3) sampling in mental health research; 4) data collection in mental health research; and 5) quality assurance procedures in mental health research.
Mixed methods study in mental health research
The evidence suggests that mixed methods approach in mental health are generally categorised according to their function (rationale, objectives or purpose), structure and process [ 18 , 19 , 43 , 48 ]. The mixed methods study can be conducted for the purpose of achieving convergence, complementarity, expansion, development and sampling [ 18 , 19 , 43 ]. Researchers conducting mental health studies should understand the underlying functions or purpose of mixed methods. Similarly, mixed methods in mental health studies can be structured simultaneously (concurrent) and sequential [ 18 , 19 , 42 , 43 , 48 ]. More importantly, the process of combining qualitative and quantitative data can be achieved through merging or converging, connecting and embedding one data set within the other [ 18 , 19 , 42 , 43 , 48 ]. The evidence further recommends that researchers need to understand the stage of integrating the two sets of data and the rationale for doing so. This can inform researchers regarding the best stage and appropriate ways of combining the two components of data to adequately address the research question(s).
The evidence recommended some methodological consideration in the design of mixed methods projects in mental health [ 18 , 19 , 45 ]. These issues include establishing early collaboration, becoming familiar with the topic, sharing information on the topic, negotiating any emerging problems and seeking contributions from team members. The involvement of various expertise could ensure that methodological issues are clearly identified. However, addressing such issues midway, or late through the design can negatively affect the implementation [ 45 ]. Any robust discoveries can rarely be accommodated under the existing design. Therefore, the inclusion of various methodological expertise during inception can lead to a more robust mixed-methods design which maximises the contributions of team members. Whilst fundamental and philosophical differences in qualitative and quantitative methods may not be resolved, some workable solutions can be employed, particularly if challenges are viewed as philosophical rather than personal [ 45 ]. The cultural issues can be alleviated by understanding the concepts, norms and values of the setting, further to respecting and including perspectives of the various stakeholders.
The review findings suggest that qualitative methods are relevant when conducting mental health research. The qualitative methods are mostly used where there has been limited previous research and an absence of theoretical perspectives. The approach is also used to gather initial pilot data. More importantly, the qualitative methods are relevant when we want to understand sensitive issues, especially from consumers of mental health services, where the ‘lived experience is paramount [ 19 , 28 , 44 ]. Qualitative methods can help understand the experiences of consumers in the process of treatment, as well as their therapeutic relationship with mental health professionals. The experiences of consumers from qualitative data are particularly important in developing clinical policy [ 28 ]. The review findings find two paradigms of qualitative methods are used in mental health research. These paradigms are the interpretive and critical approach [ 32 ]. The interpretive qualitative method(s) include phenomenology, ethnography and narrative approaches [ 32 , 36 ]. Conversely, critical qualitative approaches are participatory action research and emancipatory approach. The review findings suggest that these approaches to qualitative methods need critical considerations, particularly when dealing with consumers of mental health services.
The review findings identified several sampling techniques used in mental health research. Quantitative studies, usually employ probability sampling, whilst qualitative studies use non-probability sampling [ 25 , 34 ]. The most common sampling techniques for quantitative studies are multi-stage sampling, which involves systematic, stratified, random sampling and consecutive sampling. In contrast, the predominant sampling approaches for qualitative studies are purposive [ 19 , 28 , 32 , 42 , 46 ], snowballing [ 30 , 32 , 46 ] and theoretical sampling [ 31 , 32 ].
The sampling of consumers of mental health services requires some important considerations. The sampling should consider the appropriateness and adequacy of the sampling approach, diversity and variety of consumers of services, attributes such as social, or cultural experiences, shared concerns related to the study, practical and organisational skills, as well as ethical and sensitivity issues are all relevant [ 31 , 32 , 46 ]. Sampling consumers of mental health services should also consider the homogeneity and heterogeneity of consumers. However, failure to address these considerations can present difficulty in sampling and subsequently result in selection and reporting bias in mental health research.
The evidence recommends several data collection approaches in collecting data in mental health research, including focus group discussion, extended in-depth interviews, observations, field notes, Delphi data collection and quasi-statistical techniques. The focus group discussions appear as an approach widely used to collect data from consumers of mental health services [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ]. The focus group discussion appears to be a significant source of obtaining information. This approach promotes the participation of consumers with severe conditions, particularly at the group level interaction. Mental health researchers are encouraged to use this approach to collect data from consumers, in order to promote group level interaction. Additionally, field notes can be used to supplement information and to more deeply analyse the interactions of consumers of mental health services. Field notes are significant when wanting to gather detailed accounts about the subjective experiences of consumers of mental health services [ 40 ]. Field notes can help researchers to capture the gestures and opinions of consumers of mental health services which cannot be covered in the audio-tape recording. Particularly, the field note is relevant to complement the richness of information collected through focus group discussion from consumers of mental health services.
Furthermore, it was found that in-depth interviews can be used to explore specific mental health issues, particularly culturally marked disorders, their personal and interpersonal significance, patient and family explanatory models, individual and family coping styles, as well as symptom symbols and protective mediators [ 19 , 30 , 34 ]. The in-depth interviews are particularly relevant if the study is interested in the lived experiences of consumers without the contamination of others in a group situation. The in-depth interviews are relevant when consumers of mental health services are uncomfortable in disclosing their confidential information in front of others [ 31 ]. The lived experience in a phenomenological context preferably allows the consumer the opportunity to express themselves anonymously without any tacit coercion created by a group context.
The review findings recommend significant factors requiring consideration when collecting data in mental health research. These considerations include building confidence and trust between the researcher and consumers [ 31 , 37 ], gaining confidence of mental health professionals who manage consumers of mental health services, seeking ethical approval from the relevant committees, meeting consumers of services before data collection as well as arranging a mutually acceptable venue for the groups and providing transport services [ 41 , 47 ]. The evidence confirms that the identification of consumers of mental health services to participate in research can be facilitated by mental health professionals. Similarly, the cultural and social differences of the consumers of mental health services need consideration when collecting data from them [ 26 , 31 ].
Moreover, our review advocates that standardised assessment instruments can be used to collect data from consumers of mental health services, particularly in quantitative data. The self-completion instruments for collecting such information can be converted to interviewer-completion instruments [ 33 , 49 ]. The interviewer can read the questions to consumers of mental health services and record their responses. It is recommended that collecting data from consumers of mental health services requires significant preparation, such as training with co-investigators and representatives from consumers of mental health services [ 25 , 30 , 33 , 34 , 35 , 39 , 49 ]. The training helps interviewers and other investigators to understand the research project, particularly translating and adapting an instrument for the study setting with the aim to achieve content, semantic, concept, criteria and technical equivalence [ 30 ]. The evidence indicates that there is a need to adequately train interviewers when preparing for fieldwork to collect data from consumers of mental health services.
The evidence provides several approaches that can be employed to ensure quality assurance in mental health research involving quantitative methods. The quality assurance approach encompasses seeking informed consent from consumers of mental health services [ 26 , 37 ], pre-testing of tools [ 25 , 49 ], minimising non-response rates and monitoring of the data collection process [ 25 , 33 , 49 ]. The quality assurance process in mental health research primarily aims to achieve the highest reliability, validity and timeliness, to improve the quality of care provided. For instance, the informed consent exposes consumers of mental health services to the aim(s), methods, anticipated benefits and potential hazards and discomforts of participating in the study. Herein, consumers of mental health services who cannot respond to the inform consent process because of the severity of their illness can have it signed by their family caregivers. The implication is that researchers should determine which category of consumers of mental health services need family caregivers involved in the consent process [ 37 ].
The review findings advises that researchers should use pre-testing to evaluate the data collection procedure on a small scale and then to subsequently make any necessary changes [ 25 ]. The pre-testing aims to help the interviewers get acquainted with the procedures and to detect any potential problems [ 49 ]. The researchers can discuss the findings of the pre-testing and then further resolve any challenges that may arise prior to the actual field work being commenced. The non-response rates in mental health research can be minimised by re-approaching consumers of mental health services who initially refuse to participate in the study.
In addition, quality assurance for qualitative data can be ensured by applying the principles of credibility, dependability, transferability, reflexivity, confirmability [ 19 , 32 ]. It was found that the credibility of qualitative research in mental health is achieved through methodological and interpretive rigour [ 32 , 37 ]. The methodological rigour for assessing credibility relates to congruence, responsiveness or sensitivity to a social context, appropriateness, adequacy and transparency. By contrast, ensuring interpretive rigour is achieved through authenticity, coherence, reciprocity, typicality and permeability of researchers’ intentions, engagement and interpretation [ 32 , 46 ].
Strengths and limitations
The evidence has several strengths and limitations that require interpretation and explanation. Firstly, we employed a systematic approach involving five stages of problem identification, literature search, data evaluation, data synthesis and presentation of results [ 21 ]. Similarly, we searched six databases and developed a data extraction form to extract information. The rigorous process employed in this study, for instance, searching databases and data extraction forms, helped to capture comprehensive information on the subject.
The integrative review has several limitations largely related to the search words, language limitations, time period and appraisal of methodological quality of included papers. In particular, the differences in key terms and words concerning methodological issues in the context of mental health research across cultures and organisational contexts may possibly have missed some relevant articles pertaining to the study. Similarly, limiting included studies to only English language articles and those published from January 2000 to July 2018 could have missed useful articles published in other languages and those published prior to 2000. The review did not assess the methodological quality of included papers using a critical appraisal tool, however, the combination of clearly articulated search methods, consultation with the research librarian, and reviewing articles with methodological experts in mental health research helped to address the limitations.
The review identified several methodological issues that need critical attention when conducting mental health research. The evidence confirms that studies that addressed methodological considerations in conducting mental health research largely focuses on qualitative studies in a transcultural setting, in addition to lessons from multi-site surveys in mental health research. Specifically, the methodological issues related to the study design, sampling, data collection processes and quality assurance are critical to the research design chosen for any particular study. The review highlighted that researchers conducting mental health research can establish early collaboration, familiarise themselves with the topic, share information on the topic, negotiate to resolve any emerging problems and seek the contribution of clinical (or researcher) team members on the ground. In addition, the recruitment of consumers of mental health services should consider the appropriateness and adequacy of sampling approaches, diversity and variety of consumers of services, their social or cultural experiences, practical and organisational skills, as well as ethical and sensitivity issues.
The evidence confirms that in an attempt to effectively recruit and collect data from consumers of mental health services, there is the need to build confidence and trust between the researcher and consumers; and to gain the confidence of mental health service providers. Furthermore, seeking ethical approval from the relevant committee, meeting with consumers of services before data collection, arranging a mutually acceptable venue for the groups, and providing transport services, are all further important considerations. The review findings establish that researchers conducting mental health research should consider several quality assurance issues. Issues such as adequate training prior to data collection, seeking informed consent from consumers of mental health services, pre-testing of tools, minimising non-response rates and monitoring of the data collection process. More specifically, quality assurance for qualitative data can be achieved by applying the principles of credibility, dependability, transferability, reflexivity, confirmability.
Based on the findings from this review, it is recommended that mental health research should adequately consider the methodological issues regarding study design, sampling, data collection procedures and quality assurance issues to effectively conduct meaningful research.
Availability of data and materials
Not applicable
Abbreviations
focus group discussions
Joanna Briggs Institute
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
National Ethics Advisory Committee. Ethical guidelines for intervention studies: revised edition. Wellington (New Zealand): Ministry of Health. 2012.
Mann C. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J. 2003;20(1):54–60.
Article CAS Google Scholar
DiPietro NA. Methods in epidemiology: observational study designs. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2010;30(10):973–84.
Article Google Scholar
Hong NQ, Pluyr P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT). Canada.: Intellectual Property Office, Canada; 2018.
Creswell JW, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches: sage publications; 2017.
Google Scholar
Wisdom J, Creswell JW. Mixed methods: integrating quantitative and qualitative data collection and analysis while studying patient-centered medical home models. Rockville: Agency for Healthcare Research and Quality; 2013.
Bonita R, Beaglehole R, Kjellström T. Basic epidemiology: World Health Organization; 2006.
Centers for Disease Control Prevention [CDC]. Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics. Atlanta, GA: US Dept. of Health and Human Services, Centers for Disease Control and Prevention (CDC), Office of Workforce and Career Development; 2012.
Parab S, Bhalerao S. Study designs. International journal of Ayurveda research. 2010;1(2):128.
Yang W, Zilov A, Soewondo P, Bech OM, Sekkal F, Home PD. Observational studies: going beyond the boundaries of randomized controlled trials. Diabetes Res Clin Pract. 2010;88:S3–9.
Department of Family Medicine (McGill University). Mixed Methods Appraisal Tool (MMAT) – Version 2011 Canada: McGill University; 2011 [Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/84371689/MMAT%202011%20criteria%20and%20tutorial%202011-06-29updated2014.08.21.pdf .
Besen J, Gan DS. A critical evaluation of clinical research study designs. J Investig Dermatol. 2014;134.
Axelrod DA, Hayward R. Nonrandomized interventional study designs (quasi-experimental designs). Clinical research methods for surgeons: Springer; 2006. p. 63–76.
Thiese MS. Observational and interventional study design types; an overview. Biochemia medica: Biochemia medica. 2014;24(2):199–210.
Velengtas P, Mohr P, Messner DA. Making informed decisions: assessing the strengths and weaknesses of study designs and analytic methods for comparative effectiveness research. National Pharmaceutical Council 2012.
Guerrera F, Renaud S, Tabbò F, Filosso PL. How to design a randomized clinical trial: tips and tricks for conduct a successful study in thoracic disease domain. Journal of thoracic disease. 2017;9(8):2692.
Bhide A, Shah PS, Acharya G. A simplified guide to randomized controlled trials. Acta Obstet Gynecol Scand. 2018;97(4):380–7.
Palinkas L, Horwitz SM, Chamberlain P, Hurlburt MS, Landsverk J. Mixed-methods designs in mental health services research: a review. Psychiatr Serv. 2011;62(3):255–63.
Palinkas L. Qualitative and mixed methods in mental health services and implementation research. J Clin Child Adolesc Psychol. 2014;43(6):851–61.
World Health Organization [WHO]. Mental health: a state of well-being 2014 [Available from: http://www.who.int/features/factfiles/mental_health/en/ .
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. 2016;30(4):662–9.
Pearson A, White H, Bath-Hextall F, Apostolo J, Salmond S, Kirkpatrick P. Methodology for JBI mixed methods systematic reviews. The Joanna Briggs Institute Reviewers Manual. 2014;1:5–34.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Sampling and methods of the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;109(420):8–20.
Baarnhielm S, Ekblad S. Qualitative research, culture and ethics: a case discussion. Transcultural Psychiatry. 2002;39(4):469–83.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Brown C, Lloyd K. Qualitative methods in psychiatric research. Adv Psychiatr Treat. 2001;7(5):350–6.
Davidsen AS. Phenomenological approaches in psychology and health sciences. Qual Res Psychol. 2013;10(3):318–39.
de Jong JT, Van Ommeren M. Toward a culture-informed epidemiology: combining qualitative and quantitative research in transcultural contexts. Transcultural Psychiatry. 2002;39(4):422–33.
Ekblad S, Baarnhielm S. Focus group interview research in transcultural psychiatry: reflections on research experiences. Transcultural Psychiatry. 2002;39(4):484–500.
Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36(6):717–32.
Jacobi F, Wittchen H-U, Holting C, Sommer S, Lieb R, Hofler M, et al. Estimating the prevalence of mental and somatic disorders in the community: aims and methods of the German National Health Interview and examination survey. Int J Methods Psychiatr Res 2002;11(1):1–18.
Koch A, Vogel A, Holzmann M, Pfennig A, Salize HJ, Puschner B, et al. MEMENTA-‘Mental healthcare provision for adults with intellectual disability and a mental disorder’. A cross-sectional epidemiological multisite study assessing prevalence of psychiatric symptomatology, needs for care and quality of healthcare provision for adults with intellectual disability in Germany: a study protocol. BMJ Open. 2014;4(5):e004878.
Korver N, Quee PJ, Boos HB, Simons CJ, de Haan L, Investigators G. Genetic risk and outcome of psychosis (GROUP), a multi site longitudinal cohort study focused on gene–environment interaction: objectives, sample characteristics, recruitment and assessment methods. Int J Methods Psychiatr Res. 2012;21(3):205–21.
Larkin M, Watts S, Clifton E. Giving voice and making sense in interpretative phenomenological analysis. Qual Res Psychol. 2006;3(2):102–20.
Latvala E, Vuokila-Oikkonen P, Janhonen S. Videotaped recording as a method of participant observation in psychiatric nursing research. J Adv Nurs. 2000;31(5):1252–7.
Leese MN, White IR, Schene AH, Koeter MW, Ruggeri M, Gaite L. Reliability in multi-site psychiatric studies. Int J Methods Psychiatr Res. 2001;10(1):29–42.
Liu Z, Huang Y, Lv P, Zhang T, Wang H, Li Q, et al. The China mental health survey: II. Design and field procedures. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1547–57.
Montgomery P, Bailey PH. Field notes and theoretical memos in grounded theory. West J Nurs Res. 2007;29(1):65–79.
Owen S. The practical, methodological and ethical dilemmas of conducting focus groups with vulnerable clients. J Adv Nurs. 2001;36(5):652–8.
Palinkas L, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health Ment Health Serv Res. 2015;42(5):533–44.
Palinkas L, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Adm Policy Ment Health Ment Health Serv Res. 2011;38(1):44–53.
Razafsha M, Behforuzi H, Azari H, Zhang Z, Wang KK, Kobeissy FH, et al. Qualitative versus quantitative methods in psychiatric research. Methods Mol Biol. 2012;829:49–62.
Robins CS, Ware NC, Dosreis S, Willging CE, Chung JY, Lewis-Fernández R. Dialogues on mixed-methods and mental health services research: anticipating challenges, building solutions. Psychiatr Serv. 2008;59(7):727–31.
Robinson OC. Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25–41.
Schilder K, Tomov T, Mladenova M, Mayeya J, Jenkins R, Gulbinat W, et al. The appropriateness and use of focus group methodology across international mental health communities. International Review of Psychiatry. 2004;16(1–2):24–30.
Schoonenboom J, Johnson RB. How to construct a mixed methods research DesignWie man ein mixed methods-Forschungs-design konstruiert. KZfSS Kölner Zeitschrift für Soziologie und Sozialpsychologie. 2017;69(2):107–31.
Yin H, Phillips MR, Wardenaar KJ, Xu G, Ormel J, Tian H, et al. The Tianjin mental health survey (TJMHS): study rationale, design and methods. Int J Methods Psychiatr Res. 2017;26(3):09.
Download references
Acknowledgements
The authors wish to thank the University of Newcastle Graduate Research and the School of Nursing and Midwifery, for the Doctoral Scholarship offered to the lead author. The authors are also grateful for the support received from Ms. Debbie Booth, the Librarian for supporting the literature search.
Author information
Authors and affiliations.
School of Nursing and Midwifery, The University of Newcastle, Callaghan, Australia
Faculty of Health and Medicine, School Nursing and Midwifery, University of Newcastle, Callaghan, Australia
Anthony Paul O’Brien
Faculty of Business and Economics, Macquarie University, North Ryde, Australia
Rebecca Mitchell
You can also search for this author in PubMed Google Scholar
Contributions
EB, APO’B, and RM conceptualized the study. EB conducted the data extraction, APO’B, and RM, conducted the second review of the extracted data. EB, working closely with APO’B and RM performed the content analysis and drafted the manuscript. EB, APO’B, and RM, reviewed and made inputs into the intellectual content and agreed on its submission for publication. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Eric Badu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Data extraction form. (DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Badu, E., O’Brien, A.P. & Mitchell, R. An integrative review on methodological considerations in mental health research – design, sampling, data collection procedure and quality assurance. Arch Public Health 77 , 37 (2019). https://doi.org/10.1186/s13690-019-0363-z
Download citation
Received : 13 November 2018
Accepted : 22 July 2019
Published : 10 October 2019
DOI : https://doi.org/10.1186/s13690-019-0363-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Methodological approach
- Mixed methods
- Data collection
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Acquisition
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Religion
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Science
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Legal System - Costs and Funding
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Restitution
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business Strategy
- Business History
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Systems
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Pollution and Threats to the Environment (Social Science)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Theory
- Politics and Law
- Politics of Development
- Public Policy
- Public Administration
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Disability Studies
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >
35 Qualitative research methods in mental health
- Published: July 2011
- Cite Icon Cite
- Permissions Icon Permissions
In this chapter I set out to introduce the reader to qualitative research in mental health. I describe its main methods of inquiry, and its underpinning foundational and philosophical principles. I give numerous examples of where qualitative research has been fruitfully employed in community psychiatry. I then describe criteria of rigour which can be used to assess the strength and contribution of any qualitative study in mental health. I believe qualitative research continues to offer interesting insights into the prevention, diagnosis, phenomenology, treatment, management, and understanding of psychiatric disorder. It may also assist resolution of current policy imperatives, such as calls for person-centred care, and more thorough evaluations of service effectiveness.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| October 2022 | 11 |
| December 2022 | 3 |
| January 2023 | 7 |
| February 2023 | 6 |
| March 2023 | 6 |
| April 2023 | 1 |
| May 2023 | 5 |
| June 2023 | 5 |
| July 2023 | 2 |
| August 2023 | 2 |
| September 2023 | 4 |
| October 2023 | 4 |
| November 2023 | 4 |
| December 2023 | 8 |
| January 2024 | 4 |
| February 2024 | 5 |
| March 2024 | 9 |
| April 2024 | 5 |
| May 2024 | 5 |
| June 2024 | 4 |
| July 2024 | 7 |
| August 2024 | 5 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
10 September 2024: Due to technical disruption, we are experiencing some delays to publication. We are working to restore services and apologise for the inconvenience. For further updates please visit our website: https://www.cambridge.org/universitypress/about-us/news-and-blogs/cambridge-university-press-publishing-update-following-technical-disruption
We use cookies to distinguish you from other users and to provide you with a better experience on our websites. Close this message to accept cookies or find out how to manage your cookie settings .
Login Alert

- > Journals
- > The British Journal of Psychiatry
- > Volume 200 Issue 5
- > Qualitative Research Methods in Mental Health and Psychotherapy:...

Article contents
Qualitative research methods in mental health and psychotherapy: a guide for students and practitioners edited by david harper & andrew r. thompson. wiley-blackwell. 2011. £29.99 (pb). 272 pp. isbn: 978-0470663707.
Published online by Cambridge University Press: 02 January 2018
This is a very useful book that introduces qualitative research in mental health contexts for those wishing to better understand the approaches behind papers they read. It is also a source of specific guidance for those considering doing their own research.
The structure of the book, across and within chapters, is cleverly designed to promote effective use of appropriate methods. There are three sections. The first introduces the basic tenets; the second includes chapters on each of a range of approaches, and the third addresses research quality and future directions. This works well. In particular, it sets the various qualitative approaches in the wider mental health context. This will help students and trainees to gain an appreciation of the underpinning and implications of the different traditions and so make an informed choice of method to address their particular research question.
The editors have drawn together contributions from many experienced researchers with genuine expertise, leading to generally high-quality contributions covering many of the main approaches. Within the chapters on approaches, the consistency of a uniform set of straightforward, practical headings makes each easy to follow, and allows quick comparison between methods. In addition to the more obvious ‘how to’ content, particular sections that are valuable include those on the type of questions each method best suits and on service user involvement. My only disappointment was the lack of coverage of some of the less verbally focused qualitative methods such as ethnography and participant observation. The integrative chapters contain some of the major highlights of the book, including the thoughtful set of recommendations for ethical practice in chapter 3, the material on asking the right questions in chapter 5, and the considered and balanced overview on judging quality in chapter 16.
In a field that at times feels dominated by obfuscating jargon and a cult-like zeal, the editors have produced an accessible, illuminating text that will be of great value to those wishing to gain an introduction to this essential and developing area of mental health research.

This article has been cited by the following publications. This list is generated based on data provided by Crossref .
- Google Scholar
View all Google Scholar citations for this article.
Save article to Kindle
To save this article to your Kindle, first ensure [email protected] is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about saving to your Kindle .
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
- Volume 200, Issue 5
- Jan Oyebode (a1)
- DOI: https://doi.org/10.1192/bjp.bp.112.108746
Save article to Dropbox
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox .
Save article to Google Drive
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive .
Reply to: Submit a response
- No HTML tags allowed - Web page URLs will display as text only - Lines and paragraphs break automatically - Attachments, images or tables are not permitted
Your details
Your email address will be used in order to notify you when your comment has been reviewed by the moderator and in case the author(s) of the article or the moderator need to contact you directly.
You have entered the maximum number of contributors
Conflicting interests.
Please list any fees and grants from, employment by, consultancy for, shared ownership in or any close relationship with, at any time over the preceding 36 months, any organisation whose interests may be affected by the publication of the response. Please also list any non-financial associations or interests (personal, professional, political, institutional, religious or other) that a reasonable reader would want to know about in relation to the submitted work. This pertains to all the authors of the piece, their spouses or partners.
Mixed-Methods Designs in Mental Health Services Research: A Review
Information & authors, metrics & citations, view options, conclusions:, mixed-methods rationale, mixed-methods structure, mixed-methods functions, process of mixing methods, conclusions, acknowledgments and disclosures, figures and tables.
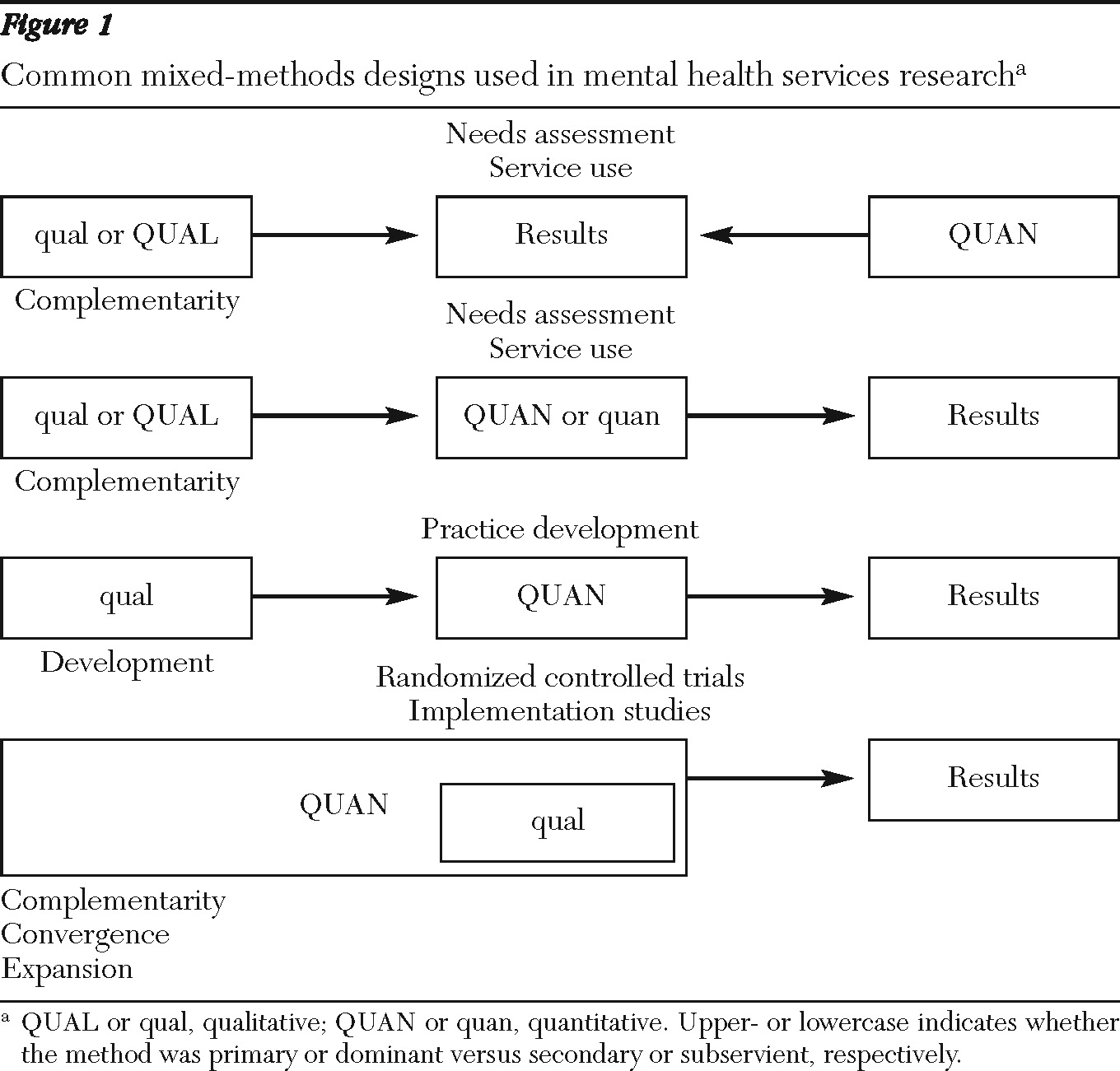
Information
Published in.

Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
To download the citation to this article, select your reference manager software.
There are no citations for this item
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Purchase Options
Purchase this article to access the full text.
PPV Articles - Psychiatric Services
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
PREVIOUS ARTICLE
Next article, request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
- Health, Fitness & Dieting
- Mental Health
Sorry, there was a problem.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Qualitative Research Methods in Mental Health: Innovative and Collaborative Approaches 1st ed. 2021 Edition
This book examines innovative approaches to the use of qualitative methods in mental health research. It describes the development and use of methods of data collection and analysis designed. These methods address contemporary and interdisciplinary research questions, such as how to access the voices of vulnerable populations, understand the relationship between experience and discourse, and identify processes and patterns that characterize institutional practices. The book offers insight into projects that reflect various cultural contexts and geographical locations as well as involve diverse research teams, ranging in their methodology from individual case studies to community-based interventions.
Key areas of coverage include projects that describe research with: • Individuals confronted with critical life events. • Former psychiatric patients. • Individual and couple psychotherapy clients. • Clients in a forensic setting. • Persons affected by psychosis. • Dementia patients. • People living with cancer. • Health care professionals.
- ISBN-10 3030653307
- ISBN-13 978-3030653309
- Edition 1st ed. 2021
- Publisher Springer
- Publication date July 1, 2021
- Language English
- Dimensions 6.25 x 0.75 x 9.25 inches
- Print length 285 pages
- See all details
Editorial Reviews
From the back cover.
Qualitative Research Methods in Mental Health is a valuable resource for researchers, professors, and graduate students as well as therapists and other professionals in clinical and counseling psychology, psychotherapy, social work, and family therapy as well as all interrelated psychology and medical disciplines.
Chapter 10, “Engraved in the Body: Ways of Reading Finnish People’s Memories of Mental Hospitals” is available open access under a Creative Commons Attribution 4.0 International License via link.springer.com.
About the Author
Product details.
- Publisher : Springer; 1st ed. 2021 edition (July 1, 2021)
- Language : English
- Hardcover : 285 pages
- ISBN-10 : 3030653307
- ISBN-13 : 978-3030653309
- Item Weight : 1.32 pounds
- Dimensions : 6.25 x 0.75 x 9.25 inches
- #1,580 in Schizophrenia (Books)
- #3,340 in Public Health (Books)
- #3,714 in Clinical Psychology (Books)
Customer reviews
- 5 star 4 star 3 star 2 star 1 star 5 star 0% 0% 0% 0% 0% 0%
- 5 star 4 star 3 star 2 star 1 star 4 star 0% 0% 0% 0% 0% 0%
- 5 star 4 star 3 star 2 star 1 star 3 star 0% 0% 0% 0% 0% 0%
- 5 star 4 star 3 star 2 star 1 star 2 star 0% 0% 0% 0% 0% 0%
- 5 star 4 star 3 star 2 star 1 star 1 star 0% 0% 0% 0% 0% 0%
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
No customer reviews
- About Amazon
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell products on Amazon
- Sell on Amazon Business
- Sell apps on Amazon
- Become an Affiliate
- Advertise Your Products
- Self-Publish with Us
- Host an Amazon Hub
- › See More Make Money with Us
- Amazon Business Card
- Shop with Points
- Reload Your Balance
- Amazon Currency Converter
- Amazon and COVID-19
- Your Account
- Your Orders
- Shipping Rates & Policies
- Returns & Replacements
- Manage Your Content and Devices
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Open access
- Published: 11 September 2024
Implementing peer support into practice in mental health services: a qualitative comparative case study
- Steve Gillard 1 ,
- Rhiannon Foster 1 ,
- Sarah White 2 ,
- Rahul Bhattacharya 3 ,
- Paul Binfield 3 ,
- Rachel Eborall 4 ,
- Sarah L Gibson 5 ,
- Daniella Harnett 3 ,
- Alan Simpson 6 ,
- Mike Lucock 7 ,
- Jacqueline Marks 8 ,
- Julie Repper 9 ,
- Miles Rinaldi 10 , 11 ,
- Anthony Salla 1 &
- Jessica Worner 12
BMC Health Services Research volume 24 , Article number: 1050 ( 2024 ) Cite this article
Metrics details
Peer workers are people with personal experience of mental distress, employed within mental health services to support others with similar experiences. Research has identified a range of factors that might facilitate or hinder the introduction of new peer worker roles into mental health services. While there is mixed evidence for the effectiveness of peer worker delivered interventions, there are no studies exploring how implementation might be associated with effect.
This was a qualitative comparative case study using data from interviews with 20 peer workers and their five supervisors. Peer workers delivered peer support for discharge from inpatient to community mental health care as part of a randomised controlled trial. In the trial, level of participant engagement with peer support was associated with better outcome (hospital readmission). Study sites with higher levels of engagement also had higher scores on a measure of fidelity to peer support principles. We compared data from sites with contrasting levels of engagement and fidelity using an analytical framework derived from implementation theory.
In high engagement-high fidelity sites, there was regular work with clinical teams preparing for working alongside peer workers, and a positive relationship between staff on inpatient wards and peer workers. The supervisor role was well resourced, and delivery of peer support was highly consistent with the intervention manual. In low engagement-low fidelity sites peer workers were employed in not-for-profit organisations to support people using public mental health services and in rural areas. Supervisors faced constrained resources and experienced barriers to joint working between organisations. In these sites, peer workers could experience challenging relationships with ward staff. Issues of geography and capacity limited opportunities for supervision and team-building, impacting consistency of delivery.
Conclusions
This study provides clear indication that implementation can impact delivery of peer support, with implications for engagement and, potentially, outcomes of peer worker interventions. Resourcing issues can have knock-on effects on consistency of delivery, alongside challenges of access, authority and relationship with clinical teams, especially where peer workers were employed in not-for-profit organisations. Attention needs to be paid to the impact of geography on implementation.
Trial registration
ISRCTN registry number ISRCTN10043328, registered 28 November 2016.
Peer Review reports
Peer support in mental health services
People with personal experience of mental distress, often referred to as peer workers, are increasingly employed within mental health services internationally to support others with similar experiences. An extensive literature explores a range of implementation issues that might dilute the distinctive qualities of peer support when introduced into public mental health services [ 1 , 2 ]. These include adequate provision of role specific training for PWs, [ 3 , 4 ] support and supervision for PWs, [ 5 ] clarity of expectation around the way in which PWs bring experience-based knowledge to mental healthcare, [ 2 . 6 ] and preparation of clinical teams to work alongside PWs [ 7 ]. It has been argued that ‘over-professionalisation’ or ‘institutionalisation’ of the PW role constrains the distinctive contribution of peer support [ 8 , 9 , 10 , 11 ].
Trials of peer support in mental health services continue to demonstrate inconsistent results, with some studies indicating that peer support might be superior to care-as-usual or a comparator intervention, [ 12 , 13 ] while others indicate no difference in effect [ 14 , 15 ]. Some of this variation might be explained by heterogeneity of interventions, population or outcome, but it is also possible that the quality of implementation of peer support into mental healthcare settings is associated with the effect of peer support interventions [ 16 , 17 ].
It has been noted that peer support is often poorly described in the trial literature, [ 17 , 18 ] with a lack of research assessing association between implementation and outcome. A recent review of one-to-one peer support in mental health services categorised peer support as being well implemented where at least two of the following criteria were reported: dedicated peer support training; clear description of the underlying processes of peer support; well-defined support structures for PWs (e.g. supervision) [ 19 ]. However, only a small number of studies reported sufficient data to conduct an analysis and results were unclear. There is a need for research that explicitly considers the possible relationship between quality of implementation and the outcomes of peer support.
Implementation theory
Implementation science offers a range of frameworks for understanding the facilitators and barriers to successful implementation of healthcare innovation into practice [ 20 ]. There is a clear recognition that the effects of any intervention will always depend on successful implementation [ 21 ]. The well-established Promoting Action on Research Implementation in Health Services (PARIHS) framework conceptualises successful implementation of research-based innovation into healthcare in terms of the nature of the evidence on which the innovation is based, the context or environment into which the innovation is placed, and the method by which implementation is facilitated [ 22 ]. In recent years, the co-design [ 23 ] or coproduction [ 24 ] of new interventions in mental health has gained prominence, with people who use mental health services bringing experience-based knowledge to the process, alongside the professional and practice-based knowledge brought by healthcare professionals. Given that this experiential knowledge is core to peer support, and that a number of members of the research term brought their own experiences of mental distress and/ or of using mental health services to the design and conduct of the research, we adapted the PARIHS framework for the purposes of this study. An earlier scoping review of implementation literature and an empirical case study, [ 25 ] undertaken by members of the team (SG and RF), identified five domains where experiential knowledge might impact research implementation, and we mapped these domains directly onto the framework (Table 1 ).
The ENRICH trial
A trial of peer support for discharge from inpatient to community mental health care indicated that peer support was not superior to care-as-usual (follow up by community mental health services within seven days of discharge) in terms of either the primary outcome – readmission within 12 months of discharge – or a range of secondary outcomes [ 26 ]. PWs received eight days of training focused on individual strengths and connecting to community, met the people they were supporting at least once while still inpatients and then weekly for up to four months post-discharge. Peer support was flexible and collaborative, informed by a peer support principles framework [ 27 ]. PWs received group and individual supervision from an experienced peer worker coordinator (PWC) who had access to an action learning set with other PWCs across study sites. The trial and intervention are described in detail in a protocol paper [ 28 ].
Findings from the trial indicated that 62.5% of participants offered peer support had at least two contacts with their PW, at least one of which was post-discharge, and that those participants were significantly less likely to be readmitted than a similar group of PWs in the care-as-usual group [ 26 ]. There might be many reasons why people chose not to, or were unable to engage with their PW, including the possibility that peer support was not always well implemented into practice in the trial.
This paper aims to explore if and how levels of engagement in a new peer support intervention were associated with implementation of the intervention, and therefore how implementation of peer support in mental health services might be optimised in the future.
Study design
We take a comparative case study approach, informed by case-orientated Qualitative Comparative Analysis [ 29 ] and pattern-matching [ 30 ] techniques, considering the seven sites where the study took place as cases. Sites were National Health Services (NHS) mental health trusts (public healthcare provider organisations) in England, where the new peer support intervention was delivered as part of the ENRICH trial. Sites were selected to provide contrast in urban, town and rural localities, geographical spread across England, and where mental health trusts were committed to introducing new PW roles into mental health services. In most sites PWs were directly employed by the mental health trust, while in others a much smaller, voluntary (not-for-profit) sector organisation was sub-contracted by the trust to employ PWs to provide support to people using mental health trust services. Information about each site is given in Table 2 below.
To inform case selection for the comparative analysis we charted level of engagement at each site – percentage of trial participants offered peer support who had at least two contacts with their PW, at least one of which was post-discharge – against site fidelity score, measured using an index designed to assess fidelity of delivery of peer support at site level against a set of principles articulating what is distinctive about peer support compared to other forms of mental health support [ 31 ] (Fig. 1 ). Fidelity was assessed through a semi-structured interview with PWs, the people they supported and their supervisor, rated by researchers against criteria based on the principles framework. A high fidelity score indicates that peer support had been implemented according to those principles. Fidelity was assessed after peer support had been delivered for at least six months at each site.

Relationship between engagement with peer support and fidelity
Figure 1 is indicative of a direct relationship between engagement with peer support and fidelity, offering rationale for selecting sites with higher or lower levels of both engagement and fidelity as cases for comparative analysis. There was one outlier, site 2, where fidelity was high (11) but engagement was mid-range (51%). We included this site in the comparative analysis as engagement might be explained by implementation issues not related to fidelity of delivery.
We report on the Evidence domain of the framework in a paper describing how experiential knowledge was central to developing the ENRICH peer support intervention [ 32 ]. Our research questions here are based on the Context and Facilitation domains of the framework, with context referring largely to the NHS Trust in which implementation took place (question 1), and facilitators being the PWs and PWCs who delivered the peer support (questions 2–4):
How did the culture of organisations, leadership (including issues of access and authority ) and monitoring and feedback impact implementation of peer support?
How did PWs and PWCs feel that their roles were characterised?
How did PWs and PWCs feel they were able to exercise flexibility while remaining consistent in their approach to delivering peer support?
How did experiential knowledge underpin peer support as it was delivered at each site?
Data sources
Peer worker interviews. Thirty-two PWs delivered peer support in the ENRICH trial and were invited to give written informed consent to participate in the research. All 32 consented and were interviewed after 12 months of delivering peer support. Interviews explored how well training prepared them for the role, their experiences of working as a PW, the support they received in the role and their relationship with clinical teams they worked alongside.
Peer worker coordinator interviews. Eight PWCs supervised PWs in the trial. Seven PWCs were themselves experienced PWs and one was a mental health nurse who shared the role with an experienced PW. All 8 PWCs gave informed consent to participate in the research and were interviewed at the same timepoint as PWs. Interviews explored PWCs’ experiences of supporting PWs, how well they thought the role was supported and organisational issues impacting delivery of peer support.
Interviews were conducted by researchers working from a perspective of having experienced mental distress and/ or having used mental health services, and played a key role in schedule development. Interview schedules can be found in the Supplementary Material file.
Data analysis
Interviews were audio-recorded, pseudonymised at the point of collection and transcribed verbatim.
Interview data were analysed using a framework approach [ 33 ] based on the Context and Facilitation domains of the modified PARIHS framework (see Table 1 ). Data were first coded to the constructs within those domains, with inductive space retained to code factors not related to the framework that participants described as impacting delivery of peer support. Second, a comparative, cross-case analysis was used to look for patterns of implementation that were: A, shared across cases; B, characterised high fidelity-high engagement cases; C, characterised low fidelity-low engagement cases; D, described implementation in the outlier case [ 30 ]. Preliminary analyses were undertaken by the first author and refined through iterative rounds of discussion with the whole team.
Characteristics of included cases
The two high engagement-high fidelity cases (sites 3,5), and the outlier high fidelity-low engagement case (site 2), were in urban areas with PWs directly employed in mental health NHS Trusts (see Table 2 ). The two low engagement-low fidelity cases (sites 4,6) were in areas that were a mix of rural localities with small towns or urban localities respectively. In both the latter sites PWs were employed by voluntary sector organisations outside of the NHS.
Characteristics of participants
A total of 20 PWs were included in the analysis, five each from sites 3 and 4, three each from sites 2 and 5, and two from site 6. Twelve PWs were female, seven were male and one preferred not to say. Three PWs were aged under 35 years of age, 12 aged from 35 to 55 years, one over 55 and four preferred not to say. Eleven PWs were White British, two were White Irish, one White other, one Black/ Black British, one Asian/ Asian British, one Arab, one Mixed White Asian with two preferring not to say.
There were five PWCs, one from each site. Four PWCs were female and one was male; two were aged from 35 to 55 and three over 55; all were White British.
Participant quotes presented below are identified with a site code (e.g. S1 = site 1) and role identifier (PW = Peer Worker; PWC = Peer Worker Coordinator) plus an additional number to distinguish between PWs at each site.
Implementation across cases
A number of implementation features were evident across all five cases, including characterisation of the PW role as largely consistent with the principles that were used to inform development of the intervention; [ 27 , 32 ] taking a non-judgemental approach and sharing experiences to create a safe space, make connections and build relationships:
‘We’re not going to be judgemental so to speak. It’s a safe place really for people to be themselves regardless of what their mental health issues are or mental health diagnoses are.’ (S5PW2). ‘I’m always sharing lived experience, whether that’s just generally or whether that’s personally with mental health … obviously you share when appropriate but you try to match that experience together so you have something in common, and then there is that mutuality and reciprocity and creating that trusting relationship.’ (S3PW3).
On the whole, training – as specified in the ENRICH manual – was consistently delivered and worked well to provide PWs with the range of skills they felt they needed for the role:
‘We did a lot about strengths-based approaches and I think that’s really informed the way that I interact with people, so I think I’m always trying to bring it back to what can you do, what is strong for you … we did a lot about active listening and also about discussing difficult issues … I think it’s been very helpful the stuff we did in training … definitely the boundaries and relationships sessions that we did …’ (S3PW1).
The importance of group supervision facilitated by the PWC, as well as individual supervision where required (both specified in the handbook), was indicated across sites, providing the opportunity for PWs to share experiences and receive feedback from one another as well as from the PWC:
‘I will hold these feelings until supervision and that’s when I let it out, offload it to my colleagues. And it’s been great because we’ve been bouncing it off each other and I’ve noticed that it’s not just me that was going through it, so it’s such a relief …’ (S2PW2). ‘… [PWC] will always ask how I am, if anything has triggered me or anything like that and she’s quite easy to talk to and it’s OK to be open with her.’ (S6PW3).
Participants in all sites described differences between the culture of clinical services in the host trust and the ethos underpinning peer support:
‘…it’s about the values because what I find with the other types of support, it all tends to be clinical and deficits based … very directive and judgemental … some of the clinical teams are stuck in that way of seeing things, that deficit-based thing and they don’t really know too much about peer support.’ (S5PW1).
At all sites, there was a perceived lack of contact with, and feedback from, community mental health teams, sometimes accompanied by a lack of understanding of the PW role:
‘Whenever I got a new service user, I’d email their [Community Psychiatric Nurse] or care coordinator … to give them more information about it and nobody, apart from I think one person, got back to me. So that’s been quite challenging, not really having any communication or contact really with the mental health teams that are working with the service users …’ (S5PW3).
Interviewees in all sites remarked that the timing of the offer of peer support - prior to discharge from hospital - was particularly challenging for some, especially in relation to maintaining contact with the PW following discharge. This represented a barrier to engagement that was related to the clinical context, rather than implementation:
‘… they are being introduced to it as soon as they come out … they are going through a tough period of fear, of not knowing what’s next for them. The last thing they want is to commit to 16 weeks of meeting someone that they don’t even know.’ (S2PW2). ‘I suspect that the post-discharge needs more targeting, that would be my sense. There are people who really get so much out of it, but then there are an awful lot who just disengage. It’s another stress for them I think.’ (S4PWC).
Implementation in high fidelity-high engagement cases
There was evidence of features supporting implementation in the high fidelity-engagement cases which contrasted with low fidelity-lowengagement cases (see below). In high fidelity cases, cultural differences between clinical services and peer support were generally seen as an asset and were valued, rather than as a source of tension:
‘… you need a values-based practice and how important it is, as opposed to the clinical based practice and how helpful that is … I’m not saying the clinical approach is wrong or anything like that, what I’m saying is we need to complement each other, we need to take a holistic approach.’ (S5PW1).
Some aspects of organisational culture were seen as supportive of peer support, including the role of recovery colleges in preparing PWs for the role or providing additional training once in post (recovery colleges employ an adult education model to supporting people with their mental health, often co-delivered by people using mental health services [ 34 ]):
‘… we were in a really fortunate position being linked with a Recovery College, that, where later in their work they then wanted to do specific recovery focused training around diagnosis we were able to provide that for people.’ (S3PWC).
In these cases, staff on the wards (inpatient units) were reported as largely familiar with and valuing the role of peer support:
‘… when I’d go on the ward … they seemed to see great value in the transparency of people being there because they’ve got lived experience. That aspect of it was really nice … good for the culture of the organisation in many ways.’ (S5PWC). ‘… the clinical teams are aware … they’re very excited that we’ve got peer workers on the ward. They’re very positive about it.’ (S3PW3).
PWCs described PW recruitment as having followed the process specified in the intervention handbook, and as such the PWs who were appointed were well equipped to deliver the role:
‘… we had the right people to execute these roles effectively really … we had quite a diverse selection panel … we had the right people that expressed the interest I think …’ (S5PWC).
There was evidence that PWs and PWCs – as intervention facilitators - had worked hard in delivering clinical team preparation sessions, as specified in the handbook, offering repeat sessions where necessary, and that this had supported a good relationship with ward teams:
‘… [in] the early days we went in to talk about ENRICH and then if they’d had significant staff turnover, which is really happening a lot … we’d then go back to the teams just so that they were aware of what ENRICH was about, what their role was … it certainly meant that staff were much more welcoming of the ENRICH peer workers when they came onto the wards.’ (S3PWC).
PWCs reported being well resourced in their leadership role, both in terms of having sufficient time to do the work and having sufficient supervision themselves around any difficult issues that might arise:
‘… [my role] was two days a week and that was plenty of time…’ (S3PWC). ‘I have had unconditional support from my manager … it’s been part of my regular monthly supervision … any kind of difficulties I’ve had or frustrations or whatever that has come up, that has been an ideal time to go through it. But I’ve also been supported to discuss things as and when they come up …’ (S5PWC).
In these sites, there was evidence that delivery of peer support was highly consistent with the manual. There was notable emphasis on flexible application of peer support, especially around pacing support in response to the individual’s needs, spending as much time as necessary alongside the participant to build a trusting relationship:
‘… it doesn’t necessarily follow a linear path a lot of the time. Sometimes, somebody might be having a really bad week and they actually want you to listen to what’s been going on for them … at the beginning, because you are getting to know the person as well, I think the kind of conversation you’d have is a bit more general … and then it might actually take a completely different path however many meetings down the line and they’ll actually go … “I haven’t told anyone about a particular issue, but I want to talk it through with you and see what you think”.’ (S3PW1).
PWs at these sites demonstrated confidence in taking a lead from the person they were supporting, consistent with the principles of choice and control that underpinned the intervention:
‘… I’m kind of getting to know things that they’re interested in and this is influencing where I signpost them to … it’s just about giving them the option and then they can make their own decision then whether they want to go, and again that’s putting them back in control, which is all about helping people to recover really and take control back of their lives.’ (S5PW2).
PWs also described learning from the people they were supporting, and the importance of validating their experiences, consistent with the principle of reciprocity in the underpinning framework:
‘There are people who I’m supporting who … realise that the medication is very important to them and that they will probably always be on it. So, I gain insight from that, just because maybe I found that medication in my own lived experience wasn’t particularly fantastic but for others it’s very important. So, you learn from other things … you’ve got to validate their experience because … they know what works for them and you can’t tell somebody else what will work for them …’ (S5PW1).
Implementation in low fidelity-low engagement cases
There was evidence of barriers to implementation in low fidelity-lowengagement cases. In both, PWs were employed in not-for-profit organisations, resulting in organisational context-related barriers to implementation. Resource issues impacted leadership of the intervention with, in one site, the organisation not having capacity to provide cover or suitable supervision for the PWC:
‘… we’ve had different staff line managing me over the past year because of maternity. But to be fair none of them really knew about ENRICH … there was nobody who could have covered my role here … it’s felt like a bit of pressure to continue doing it because I took a bit of time off … I couldn’t physically go out and do anything when I wasn’t well …’ (S6PWC).
Support for PWCs at these sites, including an Action Learning Set with other PWCs, was difficult to access because of lack of sufficient funding to travel to meetings:
‘I think the action learning sets worked really well … maybe they should have been planned for a bit more financially … because ultimately we had to go back to our Trust and say we need to find more money or I’m not going.’ (S4PWC).
Being outside of the NHS also created issues of access and authority for PWCs:
‘I would have thought there should be regular team meetings, but we never seemed to be able to get in on them … an additional disadvantage from being an organisation outside of the Trust …’ (S4PWC). ‘… it’s been difficult with the [NHS Trust], some of the staff there … I don’t want to say too much, but that’s been difficult.’ (S6PWC).
This extended to PWs being able to communicate with clinical teams about the people using:
‘A few times they didn’t want to talk to me because I didn’t have enough information for them … to establish who I was … I just wanted to know whether they were seeing [participant] or whether they’d stopped seeing him, and they wouldn’t tell me.’ (S4PW3).
At these sites there was, generally, a challenging relationship with ward-based clinical staff, potentially impacting on the initial relationship building phase of the peer support:
‘There were certainly, on that site, a lot of suspicious looks and “what on earth is this all about” type conversations. However much we tried to prepare the staff team, and we’d gone in and visited and talked to them all, but there was still that “what’s this all about”? People didn’t get it straight off.’ (S4PWC).
Cultural differences with the host NHS Trust were keenly felt by PWs employed in not-for-profit organisations:
‘… the ward environment is, well obviously it’s clinical. It sometimes feels some staff, but not all staff, who work on the wards are not really sure what my role is or have a vague understanding. There’s perhaps a little bit of a difference in terms of pecking order and me in the pecking order.’ (S6PW2). ‘… they will be looking at the patient’s files … they can build up a judgement before seeing you … when the patient sees the peer support worker they might talk to us because we’re non-judgemental, we don’t feedback unless there is a safeguarding issue or danger to themselves or others … I don’t think peers should be seeing files …’ (S4PW44).
Both sites also combined rural localities with urban areas, with issues of geography hindering timely delivery of peer support at remote hospital sites:
‘… the geography issue was a great challenge in itself in our area because I was one bit of the triangle and the [hospitals] were in two different places … I’d have had an hour or so travelling and then get there and “oh, they’re on leave until 10pm tonight”.’ (S4PWC).
Geography could also impact on building a strong sense of PW team:
‘I did lots of talking to [the PWC] but not so much my fellow peers. There was one fellow peer that I talk quite a lot to … the other two were very close to each other and so they were almost functioning as one … I got on OK with the people at [the other town] … it’s just that we had differences of opinion.’ (S4PW3).
There was some inconsistent delivery of training, with one PW reporting having received a truncated version of the training programme as a result of capacity issues:
‘I didn’t actually do [the full training] … because I was covering a maternity leave it was the girl did all the training. So, I basically had a morning with the coordinator where we went through the whole bumph together … ’ (S6PW3).
While the importance of group supervision was acknowledged in these sites, there was disruption leading to inconsistency with the pattern of weekly group supervision as a result geography in one site, and capacity in the other:
‘We don’t generally do weekly anymore … generally we do monthly although I check in by phone with them.’ (S4PWC). ‘… a lot of the supervision has ended up being one-to-one just because it’s a small team here … sometimes I would be able to meet with them together but often because my day, I’ve only got one a day week, I’d have to fit them in if one of them couldn’t do it that day …’ (S6PWC).
Possibly as a result of disruption to supervision or opportunities to support each other as a team, PWs at these sites at times appeared to lack confidence in delivering peer support:
‘… it made me feel that I was getting it all wrong … she didn’t really talk at all about, and I felt that I couldn’t, I just felt that I had to wait for her to give information to me … because that’s what I understood you are supposed to do, is wait for them to give you information to talk about their problems …’ (S4PW3). ‘… I’m imagining it’s going to be quite hard for a long time because the expression that I’ve used that comes to mind is pulling teeth. It’s going to be probably like that every time we meet … it is frustrating because you want to help them.’ (S6PW2).
Implementation in the outlier high fidelity-low engagement case
The outlier case shared contrasting sets of features with the other cases. Like high fidelity and engagement sites, the outlier case reported feedback from management describing a positive impact of peer support on culture in the NHS trust:
‘… within senior management they’ve seen the power of peer working and they really like it … we’re in discussions on when ENRICH finishes, that we’re going to have a number of peer workers within teams, exactly to try and change the nature and change the culture …’ (S2PWC).
PWs in this site also demonstrated a more confident, patient approach to relationship building:
‘… trying to build that friendly rapport, getting them to trust you, showing them that you understand them in a way … creating that safe space environment for them to be able to talk about how they are feeling or what’s going on for them … just finding out what they want to do for themselves not someone else telling them what to do … ’ (S2PW0).
However, as in the two low fidelity-low engagement cases, in the outlier site barriers to implementation included a challenging relationship with ward staff:
‘… [I feel] looked down upon sometimes, “oh, you’re just a peer support worker” … it’s the environment. The days that I do go for ward meetings are usually the days I need a long break, I’ll be honest with you …’ (S2PW2).
In this site there was also disruption to group supervision, with some PWs needing considerable additional support from the PWC and a challenging team dynamic emerging:
‘I was definitely doing weekly one-to-one supervisions with the peer workers when they first started … it kind of came apparent that it was what people needed … for me it didn’t work very well, I was exhausted … people want one-to-one sessions to talk about colleagues and issues they are having with their colleagues … I think there are two other peer workers who are less, they don’t see themselves as much as part of the team.’ (S2PWC).
The PWC indicated that they would have benefitted from additional support for their role:
‘I feel like we could have done more support around, more training kind of stuff on managing people with lived experience … … maybe one thing would have been more meetings with other peer worker coordinators and just see how other people are doing it … more guidance on what group supervision actually was … ’ (S2PWC).
This study used a qualitative, comparative case study design to explore how implementation of a peer support intervention might be associated with engagement with peer support and, as indicated in results elsewhere, [ 26 ] with outcomes. We noted clear differences related to organisational context between high fidelity-high engagement cases and low fidelity-low engagement cases. Lack of a positive working relationship between PW and ward (inpatient) clinical teams, exacerbated by lack of awareness of the potential role of peer support, is likely to be crucial to engagement where people begin peer support in hospital. Levels of engagement were highest in cases where those relationships were reported as largely positive and where differences in approach (between clinical practice and peer support) were highly valued [ 6 , 35 ].
We note that the two low fidelity-low engagement sites employed PWs in the not-for-profit sector rather than within the NHS. Elsewhere, research has indicated that the principles underpinning peer support might be better maintained within peer-led or not-for-profit organisations, [ 7 ] and that doing so might provide an opportunity to bring a change of culture into statutory services [ 35 ]. However, we observed constraints on resourcing for leadership roles, and lack of access and authority for managers in the not-for-profit sector, compounded, perhaps coincidentally, by the additional challenges of geography. Neither did we observe, in those sites, evidence of leadership for peer support from within the host NHS organisation that might have facilitated better implementation [ 36 ]. In our outlier high fidelity-low engagement case, resourcing for leadership also impacted support for PWs. Proper resourcing for PWCs has been identified elsewhere as crucial to providing good peer support [ 5 , 37 ]. PWCs at sites that struggled with levels of engagement identified the need for a wider network of mutual support beyond their immediate organisation, with work elsewhere highlighting the need to develop communities of practice around lived experience leadership roles in mental health services [ 38 , 39 ]. As such, our findings reinforce the link that has been observed elsewhere between leadership in implementation, and the outcomes of a newly implemented intervention [ 40 ].
At the two high engagement-high fidelity sites, PWCs noted that robust recruitment processes resulted in a PW team that were well equipped to deliver what was a challenging role. An experience of the PW team as mutually supportive, complemented with group supervision led by a PWC bringing experiential knowledge to their role, was identified as important at all five sites included in our analysis, as it is in the wider literature [ 2 , 5 ]. The PW training programme was equally valued across all sites with PWs indicating that it prepared them well for their roles. Again, the importance of training that is specifically tailored to peer support having been widely noted [ 3 , 4 ]. In sites where there were inconsistencies in delivery of supervision and training, this appeared to impact confidence among PWs in offering peer support that reflected the underpinning principles framework. Sites with high fidelity scores were indicative of a clear focus on relationship and trust building, characterised by spending time alongside the individual offered peer support, learning from them, before taking their lead in exploring new possibilities. These values have been identified as fundamental to peer support, [ 41 ] and our own analysis of data from the trial indicated that relationship building at the beginning of the peer support was predictive of ongoing engagement [ 42 ].
It is worth noting here that not all challenges to engaging people with the peer support were attributable to implementation issues. Across sites, interviewees felt that discharge from hospital was a challenging time for some people to consider taking up peer support. Other trials of peer support for discharge have also struggled in this respect, [ 43 ] especially where participants were those with a higher level of need (people with multiple admissions) as they were in our study [ 15 ].
Strengths and limitations
We employed a robust, theoretically informed comparative case study design, with case selection determined by a priori measures of fidelity [ 31 ] and engagement [ 26 ] made independently of this analysis. We analysed a complete data set – interviews of PWs and PWCs – in all sites included in the analysis, although we might usefully have also interviewed NHS clinicians and managers as they also played a role in implementation. Analysis of in-depth interviews exploring the experiences of people offered peer support will be reported elsewhere. Our original interview schedules were not directly informed by the PAHRIS framework [ 22 ] and so may not have elicited a full range of data relating to implementation variables. Other frameworks might have been indicative of different barriers and facilitators of successful implementation. Nevertheless, we note the work adapting the PAHRIS framework to elucidate the role of experiential knowledge in implementation was particularly suited to a study of peer support and informed by lived experience on the research team [ 25 ].

Implications for policy, practice and research
Mental health workforce policy in England, as elsewhere, is encouraging employment of large numbers of PWs into mental health services.[ 44 ]. A range of training programmes have emerged [ 45 ] that, to some degree, share a set of principles similar to those that informed ENRICH. This study suggests that specific supports for PWs need to be properly resourced as integral to the offer of peer support in mental health services. These include supervision from an experienced PW, opportunities for group supervision, and an emphasis on relationship building in PW training that is consistent with a principles-based peer support framework. While it has been suggested that peer support can drive cultural change in mental health provider organisations, [ 46 ] our research suggests that lack of supportive culture can constrain delivery. Peer leadership, provided with sufficient support and authority, is needed to support change work with clinical teams, in hospital and in the community, so that peer support and clinical care are part of a complementary offer.
This study identifies policy and practice implications when peers are employed through not-for-profit organisations to work in partnership with public mental health providers. Research elsewhere highlights the potential challenges and opportunities of this ‘hybrid’ approach, [ 35 , 47 ] indicating a need for strategies that effectively align implementation expectations between the not-for-profit organisation and the mental health provider.
Further research to develop and evaluate the introduction of peer support in mental health might usefully be informed by a change model that incorporates this range of implementation variables to optimise delivery of peer support. We also note that in our study, PWs were employed to, and supervised within a dedicated PW team that provided peer support across several clinical teams, while in many mental health services internationally PWs are employed as embedded members of multi-disciplinary clinical teams. There is a need for research that considers the implications for implementation and outcome of these contrasting organisational configurations.
This study provides clear indication that implementation issues can impact delivery of peer support, with implications for engagement and, potentially, outcomes. Resourcing can impact consistency of delivery, alongside challenges of access, authority and relationship with clinical teams, especially where PWs are employed outside of the mental health service. Attention needs to be paid to the impact of geography on implementation.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Mirbahaeddin E, Chreim S. A narrative review of factors influencing peer support role implementation in mental health systems: implications for research, policy and practice. Adm Policy Ment Health Ment Health Serv Res. 2022;11:1–7.
Google Scholar
Gillard S, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. 2013;13(1):1–3.
Article Google Scholar
Simpson A, Quigley J, Henry SJ, Hall C. Evaluating the selection, training, and support of peer support workers in the United Kingdom. J Psychosoc Nurs Ment Health Serv. 2014;52(1):31–40.
Article PubMed Google Scholar
Tse S, Tsoi EW, Wong S, Kan A, Kwok CF. Training of mental health peer support workers in a non-western high-income city: preliminary evaluation and experience. Int J Soc Psychiatry. 2014;60(3):211–8.
Forbes J, Pratt C, Cronise R. Experiences of peer support specialists supervised by nonpeer supervisors. Psychiatr Rehabil J. 2022;45(1):54.
Oborn E, Barrett M, Gibson S, Gillard S. Knowledge and expertise in care practices: the role of the peer worker in mental health teams. Sociol Health Illn. 2019;41(7):1305–22.
Stewart S, Watson S, Montague R, Stevenson C. Set up to fail? Consumer participation in the mental health service system. Australasian Psychiatry. 2008;16(5):348–53.
Otte I, Werning A, Nossek A, Vollmann J, Juckel G, Gather J. Challenges faced by peer support workers during the integration into hospital-based mental health-care teams: results from a qualitative interview study. Int J Soc Psychiatry. 2020;66(3):263–9.
Voronka J. The mental health peer worker as informant: performing authenticity and the paradoxes of passing. Disabil Soc. 2019;34(4):564–82.
Simpson A, Oster C, Muir-Cochrane E. Liminality in the occupational identity of mental health peer support workers: a qualitative study. Int J Ment Health Nurs. 2018;27(2):662–71.
Adams WE. Unintended consequences of institutionalizing peer support work in mental healthcare. Soc Sci Med. 2020;262:113249.
Mahlke CI, Priebe S, Heumann K, Daubmann A, Wegscheider K, Bock T. Effectiveness of one-to-one peer support for patients with severe mental illness - a randomised controlled trial. Eur Psychiatry. 2016;42:103–10.
Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet. 2018;392(10145):409–18.
Article PubMed PubMed Central Google Scholar
Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the veterans health administration. J Behav Health Serv Res. 2013;42(1):109–21.
Rogers ES, Maru M, Johnson G, Cohee J, Hinkel J, Hashemi L. A randomized trial of individual peer support for adults with psychiatric disabilities undergoing civil commitment. Psychiatr Rehabil J. 2016;39(3):248–55.
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;3:CD004807.
King AJ, Simmons MB. A systematic review of the attributes and outcomes of peer work and guidelines for reporting studies of peer interventions. Psychiatr Serv. 2018;69(9):961–77.
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14:39.
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, Sin J, Gillard S. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):1–20.
Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, Benrimoj SI. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Syst. 2015;13(1):1–1.
Bertram RM, Blase KA, Fixsen DL. Improving programs and outcomes: implementation frameworks and organization change. Res Social Work Pract. 2015;25(4):477–87.
Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. BMJ Qual Saf. 1998;7(3):149–58.
Article CAS Google Scholar
Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ. 2015;350.
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sector Manag. 2016;29(1):72–90.
Gillard S, Foster R, Papoulias C. Patient and public involvement and the implementation of research into practice. J Mental Health Train Educ Pract. 2016;11(4):256–67.
Gillard S, Bremner S, Patel A, Goldsmith L, Marks J, Foster R, Morshead R, White S, Gibson SL, Healey A, Lucock M. Peer support for discharge from inpatient mental health care versus care as usual in England (ENRICH): a parallel, two-group, individually randomised controlled trial. Lancet Psychiatry. 2022;9(2):125–36.
Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Mental Health Social Inclusion. 2017;21(3):133–43.
Gillard S, Bremner S, Foster R, Gibson SL, Goldsmith L, Healey A, Lucock M, Marks J, Morshead R, Patel A, Priebe S. Peer support for discharge from inpatient to community mental health services: study protocol clinical trial (SPIRIT compliant). Medicine. 2020;99(10).
Berg-Schlosser D, De Meur G, Ragin C, Rihoux B. (2008). Qualitative comparative analysis (QCA) as an approach. Pp 1–18 in Rihoux, B., & Ragin, C. Configurational comparative methods: Qualitative comparative analysis (QCA) and related techniques. Thousand Oaks, CA; Sage.
Yin RK. Case study research: design and methods. Thousand Oaks, CA: Sage; 2009.
Gillard S, Banach N, Barlow E, Byrne J, Foster R, Goldsmith L, Marks J, McWilliam C, Morshead R, Stepanian K, Turner R. Developing and testing a principle-based fidelity index for peer support in mental health services. Soc Psychiatry Psychiatr Epidemiol. 2021 Oct;1:1–9.
Marks J, Foster R, Gibson SL, Simpson A, Rinaldi M, Repper J, Worner J, Patel S, Lucock M, Ussher M, White S. Development of a peer support intervention to improve the experience and outcomes of discharge from inpatient mental health care: the role of experiential knowledge in a coproduced approach. BMC Res Notes. 2021;14(1):1–0.
Ritchie J, Spencer L. Qualitative data analysis for applied policy research. Analyzing qualitative data. Routledge; 2002. pp. 173–94.
Whitley R, Shepherd G, Slade M. Recovery colleges as a mental health innovation. World Psychiatry. 2019;18(2):141.
Gillard S, Holley J, Gibson S, Larsen J, Lucock M, Oborn E, Rinaldi M, Stamou E. Introducing new peer worker roles into mental health services in England: comparative case study research across a range of organisational contexts. Adm Policy Mental Health Mental Health Serv Res. 2015;42:682–94.
World Health Organisation. World Mental Health Report: transforming Mental Health for all. Geneva: World Health Organisation; 2022.
Grim K, Bergmark M, Argentzell E, Rosenberg D. Managing peer support workers in Swedish mental health services—A leadership perspective on implementation and sustainability. J Psychosocial Rehabilitation Mental Health. 2023;10(3):313–29.
Byrne L, Stratford A, Davidson L. The global need for lived experience leadership. Psychiatr Rehabil J. 2018;41(1):76.
Loughhead M, Hodges E, McIntyre H, Procter NG, Barbara A, Bickley B, Harris G, Huber L, Martinez L. A model of lived experience leadership for transformative systems change: activating lived Experience Leadership (ALEL) project. Leadersh Health Serv. 2023;36(1):9–23.
Egeland KM, Borge RH, Peters N, Bækkelund H, Braathu N, Sklar M, Aarons GA, Skar AM. Individual-level associations between implementation leadership, climate, and anticipated outcomes: a time-lagged mediation analysis. Implement Sci Commun. 2023;4(1):75.
Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. 2001;25(2):134.
Article CAS PubMed Google Scholar
White S, Bhattacharya R, Bremner S, Faulkner A, Foster R, Gibson S, Goldsmith L, Harnett D, Lucock M, Patel A, Priebe S. Predictors of engagement with peer support: analysis of data from a randomised controlled trial of one-to-one peer support for discharge from inpatient psychiatric care. Int J Soc Psychiatry. 2023;69(4):994–1003.
Simpson A, Flood C, Rowe J, Quigley J, Henry S, Hall C, Evans R, Sherman P, Bowers L. Results of a pilot randomised controlled trial to measure the clinical and cost effectiveness of peer support in increasing hope and quality of life in mental health patients discharged from hospital in the UK. BMC Psychiatry. 2014;14(1):1–4.
Health Education England. NHS Mental Health Implementation Plan 2019/20–2023/24. July 2019.
Bradstreet S, Buelo A. lmROC peer support theory and practice training: an independent evaluation. Matter of Focus: Edinburgh; 2023.
Berry C, Hayward MI, Chandler R. Another rather than other: experiences of peer support specialist workers and their managers working in mental health services. J Public Mental Health. 2011;10(4):238–49.
Jones N, Teague GB, Wolf J, Rosen C. Organizational climate and support among peer specialists working in peer-run, hybrid and conventional mental health settings. Adm Policy Mental Health Mental Health Serv Res. 2020;47:150–67.
Download references
This study was funded by the UK National Institute for Health Research (NIHR), Programme Grants for Applied Research funding programme (grant number RP-PG-1212-20019). This paper presents independent research funded by NIHR. The views expressed are those of the authors and not necessarily those of the UK National Health Service (NHS), the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
City, University of London, London, UK
Steve Gillard, Rhiannon Foster & Anthony Salla
St George’s, University of London, London, UK
Sarah White
East London NHS Foundation Trust, London, UK
Rahul Bhattacharya, Paul Binfield & Daniella Harnett
South London & Maudsley NHS Foundation Trust, London, UK
Rachel Eborall
Kingston University, Kingston, UK
Sarah L Gibson
King’s College London, London, UK
Alan Simpson
University of Huddersfield, Huddersfield, UK
Mike Lucock
Kingston Hospital, Kingston, UK
Jacqueline Marks
Implementing Recovery through Organisational Change, Nottingham, UK
Julie Repper
South West London & St George’s Mental Health NHS Trust, London, UK
Miles Rinaldi
Nordland Hospital Trust, Bodø, Norway
Independent Researcher, London, UK
Jessica Worner
You can also search for this author in PubMed Google Scholar
Contributions
SG, SW, SLG, AlS, ML, JR, MR and JW contributed to the conception of the original study. SG, RF, SW, RB, PB, RE, DH, AlS and AnS contributed to the design of the work reported here. SG, RF, SW, RB, RE, AlS, ML, JR, MR and JW contributed to interpretation of the data. SG, RF, SW and JM contributed to the acquisition and analysis of data. SG, RF and SW drafted and substantively revised the work. All authors approved the submitted version of the study.
Corresponding author
Correspondence to Steve Gillard .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was granted by the UK National Research Ethics Service, Research Ethics Committee London - London Bridge on 10 May 2016, reference number 16/LO/0470. Written, informed consent was given by all research participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gillard, S., Foster, R., White, S. et al. Implementing peer support into practice in mental health services: a qualitative comparative case study. BMC Health Serv Res 24 , 1050 (2024). https://doi.org/10.1186/s12913-024-11447-5
Download citation
Received : 24 May 2024
Accepted : 16 August 2024
Published : 11 September 2024
DOI : https://doi.org/10.1186/s12913-024-11447-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Mental health services
- Lived experience
- Role adoption
- Implementation
- Comparative case study methods.
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Impact of work and coping factors on mental health: Australian truck drivers' perspective
Affiliations.
- 1 School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia. [email protected].
- 2 School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia.
- 3 Monash University Accident Research Centre, Melbourne, VIC, Australia.
- 4 Turning Point, Eastern Health and Monash Addiction Research Centre, Eastern Health Clinical School, Monash University, Victoria, Australia.
- 5 Centre for Work Health and Safety, New South Wales Government, Australia.
- PMID: 37280567
- PMCID: PMC10242603
- DOI: 10.1186/s12889-023-15877-4
Introduction: Truck driving is one of the most common male occupations worldwide. Drivers endure long working hours, isolation, separation from family, compromised sleep, and face rigid regulatory requirements. Studies have documented the work factors contributing to poor health outcomes, however these have not been explored in the Australian context. The aim of this grounded theory study was to explore the impact of work and coping factors on mental health of Australian truck drivers from their perspective.
Methods: Recruitment used a purposive snowball sampling, through social media campaigns and direct email invites. Interview data were collected via phone/teleconference, audio recorded and typed verbatim. Inductive coding and thematic analysis were completed with triangulation of themes.
Results: Seventeen interviews were completed (94% male). Six themes arose, two supporting (Connections; Coping methods), and four disrupting mental health (Compromised supports; Unrealistic demands; Financial pressures; Lack of respect). Drivers had concerns regarding the many things beyond their control and the interactions of themes impacting their health even further.
Conclusion: This study explored the impact of work and coping factors affecting truck driver mental health in Australia. Themes described the importance of connections and coping methods drivers had to support their health. Many factors that compromised their health were often outside their control. These results highlight the need for a multi-faceted collaboration between stakeholders; the driver, employing companies, policy makers/regulators and the public to address the negative impact of truck driving on mental health.
Keywords: Australia; Mental health; Qualitative research; Risk and supportive factors; Truck Drivers.
© 2023. Crown.
PubMed Disclaimer
Conflict of interest statement
The authors declare no competing interests.
Truck driver work and coping…
Truck driver work and coping factors impacting mental health
Similar articles
- Factors Associated with Fatigued Driving among Australian Truck Drivers: A Cross-Sectional Study. Ren X, Pritchard E, van Vreden C, Newnam S, Iles R, Xia T. Ren X, et al. Int J Environ Res Public Health. 2023 Feb 3;20(3):2732. doi: 10.3390/ijerph20032732. Int J Environ Res Public Health. 2023. PMID: 36768095 Free PMC article.
- Lone workers attitudes towards their health: views of Ontario truck drivers and their managers. McDonough B, Howard M, Angeles R, Dolovich L, Marzanek-Lefebvre F, Riva JJ, Laryea S. McDonough B, et al. BMC Res Notes. 2014 May 14;7:297. doi: 10.1186/1756-0500-7-297. BMC Res Notes. 2014. PMID: 24886231 Free PMC article.
- The physical and mental health of Australian truck drivers: a national cross-sectional study. van Vreden C, Xia T, Collie A, Pritchard E, Newnam S, Lubman DI, de Almeida Neto A, Iles R. van Vreden C, et al. BMC Public Health. 2022 Mar 8;22(1):464. doi: 10.1186/s12889-022-12850-5. BMC Public Health. 2022. PMID: 35260120 Free PMC article.
- Challenges in Conducting Empirical Epidemiological Research with Truck and Bus Drivers in Diverse Settings in North America. Soccolich S, Ridgeway C, Mabry JE, Camden MC, Miller A, Iridiastadi H, Hanowski RJ. Soccolich S, et al. Int J Environ Res Public Health. 2022 Sep 30;19(19):12494. doi: 10.3390/ijerph191912494. Int J Environ Res Public Health. 2022. PMID: 36231791 Free PMC article. Review.
- Fatigue in Long-Haul Truck Drivers: A Concept Analysis. Wise JM, Heaton K, Patrician P. Wise JM, et al. Workplace Health Saf. 2019 Feb;67(2):68-77. doi: 10.1177/2165079918800509. Epub 2018 Oct 29. Workplace Health Saf. 2019. PMID: 30370839 Review.
- Exploring the challenges faced by Dutch truck drivers in the era of technological advancement. de Winter J, Driessen T, Dodou D, Cannoo A. de Winter J, et al. Front Public Health. 2024 Apr 24;12:1352979. doi: 10.3389/fpubh.2024.1352979. eCollection 2024. Front Public Health. 2024. PMID: 38726231 Free PMC article.
- International Road Transport Union. Tackling driver shortage in Europe 2019 [Available from: https://www.ecta.com/resources/Documents/Other%20publications/Tackling%2... .
- U.S. Bureau of Labor Statistics. Injuries, Illnesses, and Fatalities: Truck Drivers 2018. In: Statistics USBoL, editor. Washington, DC2020.
- Australian Bureau of Statistics. Labour Force, Australia. In: Australian Bureau of Statistics, editor. Canberra, Australia2020.
- Crizzle AM, Bigelow P, Adams D, Gooderham S, Myers AM, Thiffault P. Health and wellness of long-haul truck and bus drivers: a systematic literature review and directions for future research. Journal of Transport & Health; 2017.
- Xia T, Iles R, Newnam S, Lubman D, Collie A. National Transport and Logistics Industry Health and Wellbeing Study Report No 1: Work-related injury and disease in Australian transport sector workers. Healthy Working Lives Group, Faculty of Medicine Nursing and Health Sciences: Monash University; 2018 a.
Publication types
- Search in MeSH
Supplementary concepts
Related information, linkout - more resources, full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 07 September 2024
Using online methods to recruit participants into mental health clinical trials: considerations and recommendations from the RE-MIND study
- Mais Iflaifel 1 ,
- Charlotte L. Hall 2 , 3 ,
- Heidi R. Green 4 , 5 ,
- Andrew Willis 6 ,
- Stefan Rennick-Egglestone 3 , 7 ,
- Edmund Juszczak 1 ,
- Mark Townsend 8 ,
- Jennifer Martin 2 , 3 &
- Kirsty Sprange ORCID: orcid.org/0000-0001-6443-7242 1
Trials volume 25 , Article number: 596 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Ensuring diversity in clinical trials can be a challenge, which may be exacerbated when recruiting vulnerable populations, such as participants with mental health illness. As recruitment continues to be the major cause of trial delays, researchers are turning to online recruitment strategies, e.g. social media, to reach a wider population and reduce recruitment time and costs. There is mixed evidence for the use of online recruitment strategies; therefore, the REcruitment in Mental health trials: broadening the ‘net’, opportunities for INclusivity through online methoDs (RE-MIND) study aimed to identify evidence and provide guidance for use of online strategies in recruitment to mental health trials, with a focus on whether online strategies can enhance inclusivity. This commentary, as part of the RE-MIND study, focusses on providing recommendations for recruitment strategy selection in future research with the aim to improve trial efficiency.
A mixed-methods approach was employed involving three work packages: (I) an evidence review of a cohort of 97 recently published randomised controlled trials/feasibility or pilot studies in mental health to assess the impact of online versus offline recruitment; (II) a qualitative study investigating the experiences of n = 23 key stakeholders on use of an online recruitment approach in mental health clinical trials; (III) combining the results of WP1 and WP2 to produce recommendations on the use of an online recruitment strategy in mental health clinical trials. The findings from WP1 and 2 have been published elsewhere; this commentary represents the results of the third work package.
For external validity, clinical trial participants should reflect the populations that will ultimately receive the interventions being tested, if proven effective. To guide researchers on their options for inclusive recruitment strategies, we have developed a list of considerations and practical recommendations on how to maximise the use of online recruitment methods.
Peer Review reports
Introduction
Recruitment to clinical trials is challenging, and those in mental health research are no exception and people with mental health illness have been identified as an under-served group in health research [ 1 ]. The importance of broader representation of under-served populations in clinical trials is already well established to ensure they reflect the populations that stand to benefit from the intervention being tested [ 2 ]. The question is how do we improve recruitment when we already know that mental health service use is proportionately lower for the socioeconomically disadvantaged [ 3 ], males [ 4 ], people from ethnic minority backgrounds [ 5 ], and older participants or those living in more rural areas [ 6 ]. Traditionally, recruitment into mental health trials has been dependent upon face-to-face referrals and therefore limited to those individuals actively seeking service intervention, thus perpetuating the problem [ 7 ]. Furthermore, increasing pressures on mental health services has become an obstacle to the delivery of trials using this approach; however, technological advances are allowing researchers to be more creative and dynamic in their choice of recruitment strategies to target potential participants typically outside of services and reach wider groups of people [ 8 ]. Despite this potential, deciding upon what might be the best recruitment strategy for those living with mental health illness needs further careful consideration.
To help address, this we conducted a study, “REcruitment in Mental health trials: broadening the ‘net’, opportunities for Inclusivity through online methoDs’ (RE-MIND)” https://www.nctu.ac.uk/our-research/methodology.aspx . The objective was to explore the use of offline and online recruitment strategies with the aim of helping researchers improve recruitment reach and increase the efficiency of clinical trials of mental health interventions.
This project focussed on the recruitment strategy used to make the initial approach to potential participants, informing them about an active clinical trial. As our focus was on the initial stage in recruitment, we did not cover issues surrounding the consent process itself. Despite this, we acknowledge the importance of the methods of taking informed consent, and this should be considered when deciding on a recruitment strategy.
The RE-MIND study consisted of two work packages which have been published separately [ 9 , 10 ]. First is an evidence review of 97 recently published randomised controlled trials (RCTs) and randomised feasibility/pilot studies in mental health to assess the impact of online recruitment versus offline recruitment in clinical trials [ 9 ]. Second is a qualitative study investigating the experiences, opinions, and ideas of n = 23 key stakeholders (research staff and patients and public involvement members with experience working in mental health research) on the use of online recruitment as an approach in mental health clinical trials [ 10 ]. The findings were then triangulated [ 11 ] by researchers MI, KS, and CLH to develop draft considerations and practical recommendations which then underwent a review process by the study Advisory Group (HRG, AW, SRE, EJ, MT, and JM) who have experience in digital research, design, and delivery of online and offline RCTs and equality, diversity, and inclusion resulting in the final recommendations.
Throughout the RE-MIND study, we used the following definitions to broadly categorise offline or online recruitment. These definitions describe an overarching strategy to recruitment:
Online recruitment strategies —the use of Internet technologies such as social media advertisements, Google search engine advertisements, and other website campaigns [ 12 ].
Offline recruitment strategies —in-clinic recruitment, approaching potential participants through mail and telephone using health records and registers, media campaigns, newspaper advertisements, and input during radio and television interviews [ 12 ].
In this commentary, we present a list of considerations and practical recommendations for research teams on the use of online recruitment of participants into mental health clinical trials with the aim to improve recruitment efficiency in clinical trials of mental health interventions. It is worth noting that although the RE-MIND study focussed on mental health interventions the findings may also be beneficial in wider clinical research.
- Recommendations
Complexity of mental illness
Severity of mental health illness has previously been identified as a barrier to participation in mental health research [ 13 , 14 ]. RE-MIND reported that the type of mental health illness, its stage, participants’ feelings about their illness, and carers’ responsibilities were key factors when selecting a recruitment strategy [ 10 ]. Alongside meaningful and authentic patient and public involvement (PPI) to guide and inform the recruitment strategy, using a multi-method approach to recruitment could improve accessibility and inclusivity, by supporting the diverse and changing needs of those living with mental health illness.
Considerations
Consider any relationships between recruitment strategy and mental health symptomatology:
For example, individuals with learning disabilities, autism, anxiety, or obsessive compulsive disorder may have difficulty interfacing in public and therefore may benefit from online recruitment.
Online recruitment may, however, be a barrier for other mental health illnesses such as low mood disorders, depression, personality disorders, and psychosis where an in-person approach offers more security, contact, and support to the individual.
Consider using the stage or severity of illness to inform recruitment method:
Will the person’s diagnostic and treatment experience impact on selection of recruitment method, for example, both patients and carers may be reluctant to talk about or need more time to process a diagnosis in the early stages?
Are personal cues, such as body language, important for communicating with your participants and supporting greater engagement in a trial, for example, recognising changes in mental health state, physical discomfort, increasing tics, loss of concentration, fatigue, etc.?
Is personal contact preferable or more encouraging, for example, for building rapport and trust with the individual?
Consider whether the recruitment method selected may impact on any experience of stigma around mental health:
Providing a virtual safe space (online) may be beneficial, but the safety of this space relies on participants having secure and private access to a safe space and a device that can access the Internet.
Consider the impact of the relationship between participants living with mental illness and the research team:
Trusting relationships are deemed important for both recruitment and retention of participants living with mental ill health. Knowing that a health care provider understands an illness and can offer personalised support can be reassuring.
Will your recruitment strategy choices contribute to maintaining or building trust with this group? Online recruitment, such as social media, can be seen as distant and disengaging compared to in-person recruitment. Regular trial updates and information sharing through short videos or live ‘chats’ may help ‘humanise’ the trial on digital platforms.
Develop your recruitment approach (offline/online/mixed) by working in partnership with potential participants and members of the public that share characteristics with your target population group. You can identify PPI contributors through your local employing organisation or through professional or existing research or public contributor groups such as Sprouting Minds https://digitalyouth.ac.uk/the-digital-youth-programme/about-sprouting-minds/ . Please note that most UK National Health Service (NHS) Trusts have established PPI Groups.
Build in flexibility where possible at the protocol development stage, to ensure that participants with fluctuating symptoms can remain engaged in a safe and supported way. This may be achieved in several ways, for example, by offering a mixed recruitment strategy to allow individuals to choose how they want to participate. Alternatively, you may select an online recruitment strategy via Facebook for the initial approach to participate but then build in telephone or in-person opportunities for eligibility checks or follow-ups. It is important to ensure participants know that these options exist at the earliest opportunity.
- Inclusivity
RE-MIND identified a number of specific challenges to inclusive recruitment into mental health clinical trials. Continuing stigma surrounding mental health was a significant factor on a political, cultural, community, and individual level, underpinned by lack of education and mistrust of services and research [ 10 ]. In addition, lack of researcher skills and experience in inclusive recruitment strategies has also been found to contribute to underrepresentation in clinical research [ 15 , 16 ]. This highlights the critical role of PPI in understanding a trial population’s needs. It is also vital to educate researchers on equality and diversity, to enable co-design and selection of suitable recruitment methods to improve representation in mental health clinical trials, for example, through better implementation of the UK’s National Institute for Health Research (NIHR) INCLUDE ethnicity framework [ 1 ].
Consider the impact of the relationship between participants from marginalised groups and the research team:
Will your recruitment strategy choices contribute to maintaining or building trust with this group, for example, those living with mental health illness in rural or under-served communities may benefit from an online recruitment strategy?
Can you develop relationships with local and/or national community groups to build trust in your research? Identify community group leaders who will advocate for your research.
Do you have connections with trusted members of the community to support the building and development of relationships to facilitate inclusive recruitment? This can be in-person or online for example. through administrators of Facebook groups, libraries, or leaders of interest groups.
Do you have a PPI member with lived experience on your research team who can advocate for your research with community groups? Establishing connections through shared experience can help break down barriers of mistrust and misunderstanding.
Consider which recruitment methods your target participant populations may prefer. Living with a mental health illness can be complex due to fluctuating health status or exacerbation of symptoms:
Think about what factors may be most important to them, e.g. if they are working, parents, carers, and/or attending school, then convenience may be the main factor to target.
Consider the range of media platforms available to target people who are educationally or socioeconomically diverse.
If local IT access, e.g. poor Internet access is known in a geographical area, consider using mixed methods for recruitment to improve inclusivity.
Consider information provision and accessibility when selecting your recruitment methods:
Consider whether the methods you are using to recruit and retain participants allow for language (written and/or spoken) needs to be met, e.g., using a translation service.
Consider whether the recruitment method selected allows you to adequately communicate what you need to your participants for example:
Social media platforms such as X (previously Twitter) or use of SMS text-based services have character limitations. Could any language or phrasing lead to misinterpretation or misunderstanding
Use of clinical or diagnostic terms, phrases and labels when considering issues of stigma.
If you are using offline methods, are they accessible for people in a physical sense? E.g., people with motor/mobility needs, or visual or auditory difficulties.
If you are using online methods, are the colours, font, and imagery that you are using inclusive? E.g., alt text for images, colour blindness, colour contrast and font readability.
Work in partnership with people with lived experience and members of the public that share characteristics with your target population group. Explore the needs of both the trial team and the target population group and select methods that are effective for both parties.
Greater sensitivities and confidentiality in mental health care mean that relationships and trust are critical, which may be easier to facilitate face-to-face. However, online recruitment may offer greater flexibility and convenience for participants, for example, by supporting those who may find in-person contact challenging due to their illness. When selecting a recruitment strategy , be mindful of both advantages and drawbacks of the strategy used.
Avoid stereotypes, particularly related to age, when thinking about online methods. For example, technology as a barrier is likely reduced with each generation as well as recent necessity to engage with digital communications (e.g. smartphones, WhatsApp, Facebook, videoconferencing platforms) due to the COVID pandemic.
Identify the main demographic characteristic(s) that is important to engage with your trial, and then consider how other characteristics may impact how they react to the recruitment strategy you have in mind. For example, if you know you want to include young people, consider using TikTok, whereas Facebook may be preferable for older participants. It is important to think about other characteristics that may impact if/how social media is used, e.g. mental health status, socioeconomic status, health status, gender.
There are a growing number of community-led mental illness specific support groups on social media. Can you access and/or engage these groups to help with recruitment? Care should be taken not to harm the safe spaces afforded by these groups, for example for a researcher joining a group purely for the purpose of trial promotion.
Data management
RE-MIND found that for people living with mental health illness, there remained a significant element of fear and mistrust in using online methods underpinned by the stigma and vulnerability of mental health illness with the potential for confidentiality to be broken [ 10 ]. Understanding safeguards for the range of digital platforms was particularly complex and in line with other research suggests better regulation is needed of digital platforms [ 17 ], which at times were not deemed as stringent as clinical trial requirements.
Consider putting appropriate safeguards in place for the recruitment methods selected, e.g. firewalls, General data Protection Regulation (GDPR), secure server.
Can you use a quick response (QR) code to improve security and safety. A QR code is an image scannable by a digital device that can impart information.
Does your organisation have data management policies for use of digital platforms such as social media that must be adhered to? Consider local policies required for multi-site trials.
Is your recruitment method a credible source, e.g. not mistaken for spam, phishing?
Allocate a moderator for engagement with online public groups to ensure safeguarding and wellbeing of people engaging with the content.
How will you inform potential participants about how their data will be shared and/or managed online?
Consider the resources required to adequately manage large numbers of enquiries generated by online strategies:
Do you have the resources to support the additional work associated with screening and monitoring of data quality?
Ensure that eligibility criteria are clearly communicated to potential participants.
Invest adequate time and resources in ensuring your data management systems are secure and safe for participants. You may want to make use restrictive software features for online methods.
Invest time to ensure security and safety methods are communicated clearly. You should work in partnership with potential participants and members of the public that share characteristics with your potential participant group to do this.
Staff training and support
The process of targeting recruitment using an online strategy has been considered as more time-efficient and cost-effective than traditional offline (in-person) recruitment [ 12 ]. However, knowledge of digital platforms and access to organisational and technical support and funding were the most common challenges researchers cited when selecting a recruitment strategy in the RE-MIND study [ 10 ]. It appears that despite advances in technology offering greater opportunity to reach wider audiences, many of these advances remain underutilised without adequate support and resources.
Consider identifying trials involving similar participant populations to learn from their experience of recruitment:
For example, information on trials can be accessed from ClinicalTrials.Gov, PubMed, etc.
Remember that this relies on adequate reporting of recruitment strategy.
Think about how previous trials could have been improved.
Consider the impact of researchers/recruiters being in/adequately trained and knowledgeable on how to use the online recruitment methods you have chosen:
If you are using social media, does your organisation have policies and/or expertise that can be used to support engagement on specific platforms
Does your organisation have procedures for payment for social media promotion?
Do you have local services available to support at an organisational level when things go wrong, e.g. IT, marketing, or communications teams?
Ensure your recruitment methods are appropriately funded, for example, advertising costs per click; do you need a professional designer to produce visual summaries of the research, such as infographics?
Do you have lived experience patient and public input on the selection of recruitment strategy, including content and presentation?
Make a conscious effort to learn from previous trials aimed at the populations you are intending to recruit. Reflect upon how these trials may differ from yours and how that may impact your selection of recruitment process (e.g., severity or stage of mental health illness, intervention type, locality, country, setting, healthcare system, culture).
Ensure research teams are adequately trained on systems and software, and that they know where to go when systems fail, or if they have unanswered questions.
Conclusions
This list of considerations and recommendations is based on the experiences of key partners and the findings from the RE-MIND project, outlining factors to consider when planning recruitment strategies in mental health research/clinical trials. It should be used as a starting point for discussions among the trial team. We acknowledge the potential limitations of each consideration in context of individual and/or organisational capacity, funding and resources available.
The process of selecting a suitable recruitment method should give due consideration to the study population as well as the resources (including staff time and training) needed to implement that method. The ideal juncture to do this is when writing a trial grant funding proposal to ensure adequate resourcing. However, we encourage trial teams that are struggling to recruit to use our considerations and recommendations to re-evaluate their approach to recruitment.
The considerations are designed to be used flexibly based on the target population to be recruited. Greater consideration should be given to using online or mixed methods recruitment strategies that adopt a tailored approach, offering flexibility and choice, to enable wider participation. For future work, we recommend revisiting and re-evaluating these considerations after they have been implemented in practical settings. This process of reassessment will allow us to gain valuable insights into the real-world impact and effectiveness of our proposed strategies. It will also enable us to make necessary adjustments, fine-tune our recommendations, and ensure their continued relevance and success in evolving contexts.
Availability of data and materials
The data collected, used, and/or analysed during the current study are available from the Nottingham Clinical Trials Unit (NCTU) via the corresponding author on reasonable request.
Abbreviations
General Data Protection Regulation
Patient and public involvement
Nottingham Clinical Trials Unit
National health Service
National Institute for Health and Care Research
Quick response
Randomised controlled trial
Short message service
REcruitment in Mental health trials: broadening the ‘net’, opportunities for INclusivity through online methoDs
United Kingdom
National Institute for Health Research. Improving inclusion of under-served groups in clinical research: Guidance from the NIHR INCLUDE project 2020 [09August2023]. Available from: https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 .
Clark LT, Watkins L, Piña IL, Elmer M, Akinboboye O, Gorham M, et al. Increasing diversity in clinical trials: overcoming critical barriers. Curr Probl Cardiol. 2019;44(5):148–72.
Article PubMed Google Scholar
Robards F, Kang M, Usherwood T, Sanci L. How marginalized young people access, engage with, and navigate health-care systems in the digital age: systematic review. J Adolesc Health. 2018;62(4):365–81.
Pattyn E, Verhaeghe M, Bracke P. The gender gap in mental health service use. Soc Psychiatry Psychiatr Epidemiol. 2015;50(7):1089–95.
Tiwari SK, Wang J. Ethnic differences in mental health service use among White, Chinese, South Asian and South East Asian populations living in Canada. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):866–71.
Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Barriers to mental health treatment in rural older adults. Am J Geriatr Psychiatry. 2015;23(11):1172–8.
Article PubMed PubMed Central Google Scholar
Barak A. Psychological applications on the Internet: a discipline on the threshold of a new millennium. Appl Prev Psychol. 1999;8(4):231–45.
Article Google Scholar
Akers L, Gordon JS. Using Facebook for large-scale online randomized clinical trial recruitment: effective advertising strategies. J Med Internet Res. 2018;20(11): e290.
Iflaifel M, Hall CL, Green HR, Willis A, Rennick-Egglestone S, Juszczak E, et al. Recruitment strategies in mental health clinical trials: a scoping review (RE-MIND Study). Trials [In Peer Review]. June 2024.
Iflaifel M, Hall CL, Green HR, Willis A, Rennick-Egglestone S, Juszczak E, et al. Widening participation – recruitment methods in mental health randomised controlled trials: a qualitative study. BMC Med Res Methodol. 2023;23(1):211.
Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and Implementing a Triangulation Protocol for Qualitative Health Research. Qual Health Res. 2006;16(3):377–94.
Brøgger-Mikkelsen M, Ali Z, Zibert JR, Andersen AD, Thomsen SF. Online patient recruitment in clinical trials: systematic review and meta-analysis. J Med Internet Res. 2020;22(11): e22179.
Kaminsky A, Roberts LW, Brody JL. Influences upon willingness to participate in schizophrenia research: an analysis of narrative data from 63 people with schizophrenia. Ethics Behav. 2003;13(3):279–302.
Woodall A, Morgan C, Sloan C, Howard L. Barriers to participation in mental health research: are there specific gender, ethnicity and age related barriers? BMC Psychiatry. 2010;10:103.
Kusnoor SV, Villalta-Gil V, Michaels M, Joosten Y, Israel TL, Epelbaum MI, et al. Design and implementation of a massive open online course on enhancing the recruitment of minorities in clinical trials - Faster Together. BMC Med Res Methodol. 2021;21(1):44.
Niranjan SJ, Durant RW, Wenzel JA, Cook ED, Fouad MN, Vickers SM, et al. Training needs of clinical and research professionals to optimize minority recruitment and retention in cancer clinical trials. J Cancer Educ. 2019;34(1):26–34.
Mühlhoff R, Willem T. Social media advertising for clinical studies: ethical and data protection implications of online targeting. Big Data Soc. 2023;10(1):20539517231156130.
Download references
Acknowledgements
The study authors would like to thank all our focus group and interview participants and the UK Clinical Research Collaboration for their support of the project culminating in these recommendations for future practice.
This project is funded by the National Institute for Health and Care Research (NIHR) CTU Support Funding scheme. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Open Access funding provided by The University of Nottingham. Stefan Rennick-Egglestone and Charlotte L Hall were supported by the NIHR Nottingham Biomedical Research Centre (NIHR203310).
Author information
Authors and affiliations.
Nottingham Clinical Trials Unit, University of Nottingham, Nottingham, UK
Mais Iflaifel, Edmund Juszczak & Kirsty Sprange
Institute of Mental Health, School of Medicine, NIHR MindTech MedTech HRC, Mental Health and Clinical Neurosciences, University of Nottingham, Innovation Park, Triumph Road, Nottingham, UK
Charlotte L. Hall & Jennifer Martin
Institute of Mental Health, NIHR Nottingham Biomedical Research Centre, University of Nottingham, Innovation Park, Triumph Road, Nottingham, UK
Charlotte L. Hall, Stefan Rennick-Egglestone & Jennifer Martin
Health Services Research Unit, University of Aberdeen, Aberdeen, UK
Heidi R. Green
COUCH Health, Manchester, UK
Leicester/Diabetes Research Centre, Centre for Ethnic Health Research, University of Leicester, Leicester, UK
Andrew Willis
School of Health Sciences, Institute of Mental Health, University of Nottingham, Nottingham, UK
Stefan Rennick-Egglestone
NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC), Southampton, UK
Mark Townsend
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to designing the RE-MIND study. All authors contributed to the selection and refinement of the recommendations. MI and KS drafted the initial manuscript. All authors reviewed and edited drafts of the manuscript. All authors accepted the final version of the manuscript.
Corresponding author
Correspondence to Kirsty Sprange .
Ethics declarations
Ethics approval and consent to participate.
The RE-MIND study received approval from the University of Nottingham Research Ethics Committee (FMHS 13–0422) on 13 June 2022.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Iflaifel, M., Hall, C.L., Green, H.R. et al. Using online methods to recruit participants into mental health clinical trials: considerations and recommendations from the RE-MIND study. Trials 25 , 596 (2024). https://doi.org/10.1186/s13063-024-08435-9
Download citation
Received : 12 January 2024
Accepted : 23 August 2024
Published : 07 September 2024
DOI : https://doi.org/10.1186/s13063-024-08435-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Clinical trial
- Recruitment
ISSN: 1745-6215
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 06 September 2024
Breastfeeding experiences of women with perinatal mental health problems: a systematic review and thematic synthesis
- Hayley Billings 1 ,
- Janet Horsman 1 ,
- Hora Soltani 1 &
- Rachael Louise Spencer 2
BMC Pregnancy and Childbirth volume 24 , Article number: 582 ( 2024 ) Cite this article
Metrics details
Despite its known benefits, breastfeeding rates among mothers with perinatal mental health conditions are staggeringly low. Systematic evidence on experiences of breastfeeding among women with perinatal mental health conditions is limited. This systematic review was designed to synthesise existing literature on breastfeeding experiences of women with a wide range of perinatal mental health conditions.
A systematic search of five databases was carried out considering published qualitative research between 2003 and November 2021. Two reviewers conducted study selection, data extraction and critical appraisal of included studies independently and data were synthesised thematically.
Seventeen articles were included in this review. These included a variety of perinatal mental health conditions (e.g., postnatal depression, post-traumatic stress disorders, previous severe mental illnesses, eating disorders and obsessive-compulsive disorders). The emerging themes and subthemes included: (1) Vulnerabilities: Expectations versus reality; Self-perception as a mother; Isolation. (2) Positive outcomes: Bonding and closeness; Sense of achievement. (3) Challenges: Striving for control; Inconsistent advice and lack of support; Concerns over medication safety; and Perceived impact on milk quality and supply.
Conclusions
Positive breastfeeding experiences of mothers with perinatal mental health conditions can mediate positive outcomes such as enhanced mother/infant bonding, increased self-esteem, and a perceived potential for healing. Alternatively, a lack of consistent support and advice from healthcare professionals, particularly around health concerns and medication safety, can lead to feelings of confusion, negatively impact breastfeeding choices, and potentially aggravate perinatal mental health symptoms. Appropriate support, adequate breastfeeding education, and clear advice, particularly around medication safety, are required to improve breastfeeding experiences for women with varied perinatal mental health conditions.
Peer Review reports
Breastfeeding is a key public health measure, conferring short- and long-term health and socio-economic benefits for women and their offspring [ 1 , 2 , 3 , 4 ]. Breastfeeding has been identified as crucial in meeting the United Nations Sustainable Development Goals for 2030 [ 5 ] with the World Health Organisation aiming for global rates of 50% exclusive breastfeeding until 6 months of age by 2025 [ 6 ]. Despite an increasing research base about what helps or hinders breastfeeding, there is a dramatic drop in breastfeeding prevalence within the first six weeks of birth, especially in high income countries [ 1 , 7 , 8 , 9 ]. The reasons given for cessation of breastfeeding suggest that few mothers gave up because they planned to, citing challenges such as physical pain [ 10 ], perceived insufficient milk supply [ 11 ], and breastfeeding not fitting in with family and/ or work life [ 12 ], and although complex physiological and psychosocial factors influence breastfeeding practices, evidence also suggests that mothers who experience postnatal depression may be at a greater risk of early breastfeeding cessation [ 13 , 14 ].
Perinatal mental health (PMH) conditions are mental illnesses which occur during pregnancy and up to a year following birth [ 15 , 16 ] and include a range of conditions such as: depression, anxiety, obsessive compulsive disorder, post-traumatic stress disorder (PTSD), tokophobia, bipolar disorder, postpartum psychosis, eating disorders and personality disorders [ 17 ]. These conditions are associated with increased morbidity and are a leading cause of maternal death in high-income countries [ 17 ]. Globally it is estimated that between 15 and 25% of women experience mental illness during the perinatal period, either as a new condition or as a reoccurrence of a pre-existing condition [ 17 ].
Breastfeeding is known to have psychological benefits, such as improving mood and protecting against postnatal depression in mothers, enhancing socio-emotional development in the child and strengthening mother-child bonding [ 13 , 14 , 18 , 19 ]. However, previous reviews of women’s experiences of breastfeeding whilst experiencing mental health conditions have focused primarily on postnatal depression (PND) [ 19 ]. No previous reviews have been identified which investigate the experiences and perspectives of women with a variety of perinatal mental illnesses with a view to improving breastfeeding health intervention strategies for women with such conditions.
This systematic review was reported in accordance with the PRISMA 2020 statement [ 20 ]. The review protocol was registered with PROSPERO in 2021 (registration number CRD42021297076 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021297076 ). There was no requirement to deviate from this protocol during the study.
Search strategy
A literature search was undertaken for studies published from 2003 to Nov 2021. The selection of 2003 was to identify research undertaken following publication of the World Health Organisation Global Strategy for Infant and Young Child Feeding [ 21 ]. This advised that women exclusively breastfeed for six months and continue breastfeeding for two years and beyond for optimal health benefits to mother and infant.
The search was conducted using five electronic databases: Medline and CINAHL Complete (EBSCOhost), Maternity & Infant Care (Ovid), APA PsycInfo ® (ProQuest) and Web of Science Core Collection (Clarivate).
Search terms were devised according to the SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) framework [ 22 ] (Table 1 ). Reference lists of included articles were scrutinised for possible additional studies.
Eligibility criteria
Eligible studies included:
published from 2003.
peer-reviewed articles.
published in English.
any setting.
qualitative primary research data.
participants were women experiencing mental health issues.
described experiences, perceptions, views, and opinions in relation to breastfeeding.
Study selection
Titles, abstracts, and potentially relevant full texts were screened independently by two authors against the eligibility criteria. Disagreement was resolved through discussion and consultation with a third author.
Data extraction
Data extracted included study authors, title, year of publication, country of origin, source of funding, study aims, study design, recruitment strategies, participant ethnicity, PMH condition, and study results. Two authors independently extracted data.
Quality appraisal of included studies was carried out to demonstrate rigour, using a Critical Appraisal Skills Programme (CASP) appraisal tool [ 23 ], however this was not used as an indicator for inclusion in the analysis.
Data synthesis
Thematic synthesis, a method of analysis widely used for qualitative systematic reviews, was undertaken [ 24 ]. This involved line by line coding of extracted quotations followed by development of descriptive and analytical themes. NVivo software was used to systematically code extracted data. Verbatim quotations, along with information on themes and sub-themes they were assigned to in the original study, were imported into the software. Codes and their supporting data were reviewed to identify related categories which could be grouped into broader descriptive themes. From this, overarching analytic themes were identified.
Author reflexivity was considered and addressed throughout the review with regular discussions between authors to debate and establish aspects such as definitions of mental health, use of terminology, themes, subthemes and the interplay between them.
Patient and public involvement
Once key findings were established, the project team organised two patient and public involvement events, which included ethnic minority perinatal peer supporters and a pre/postnatal peer support group with PMH experiences. Feedback from these groups showed that the themes identified by the review captured the main priorities of the groups.
The study selection process is outlined on the PRISMA [ 20 ] flow diagram (Fig. 1 ). A total of 5510 studies were retrieved. After removing duplicates ( n = 2604) and excluding articles which were not relevant following screening of title and abstract ( n = 2878), full text of the remaining 28 studies were screened. Of these, 11 studies were excluded, resulting in 17 studies being included in this review.
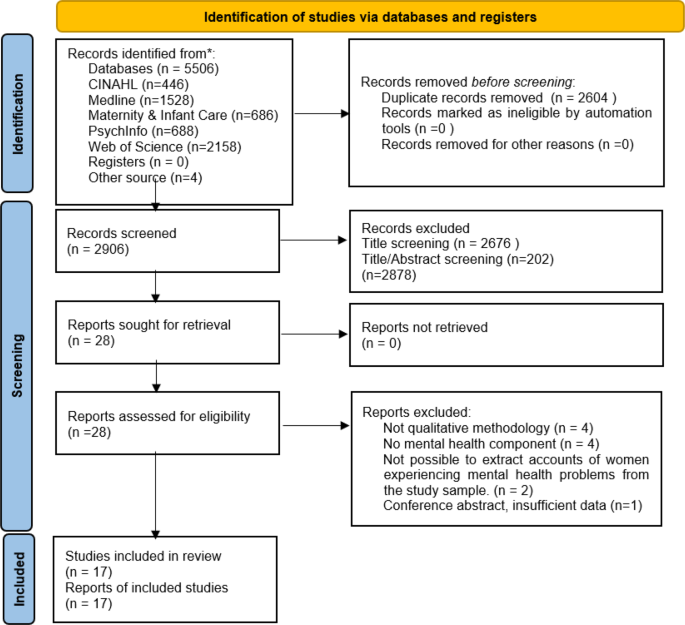
PRISMA flow diagram detailing study selection [ 20 ]. CINAHL – Cumulative Index to Nursing and Allied Health Literature. PRISMA flow diagram- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ . 2021;372(71). DOI: https://doi.org/10.1136/bmj.n71
Characteristics of the studies
From the 17 included studies, four used thematic analysis, two in a qualitative study [ 25 , 26 ] and two within a mixed methods secondary analysis of existing data [ 27 , 28 ]. Six studies used phenomenological methods [ 29 , 30 , 31 , 32 , 33 , 34 ], two used an ethnographic approach [ 35 , 36 ] and three undertook a Grounded Theory approach [ 37 , 38 , 39 ]. One study used a psychoanalytically informed analysis [ 40 ] and one used comparative analysis [ 41 ].
Following CASP quality appraisal, the methodological quality of included papers was ranked as either low ( n = 3), moderate ( n = 2) or high ( n = 12), (Table 2 ).
Of the included studies, seven focused on PND, four included patients with PND and/or emotional difficulties, postnatal blues or mental distress, two focused on mood disorders, four included women previously diagnosed with severe mental illnesses, eating disorders, obsessive compulsive disorder, and/or traumatic childbirth/PTSD.
There were a total of 551 participants across the studies. Of these, 456 were married/cohabiting, 18 were single/separated, and 77 did not specify. For educational attainment, 321 participants identified as either ‘well educated’ or having studied beyond high school level. A total of 86 participants received a school education (high school or below), 14 participants had no schooling and 130 did not specify. Of the 17 studies, 15 were carried out in high-income countries and two in low-income countries (Table 3 ).
Through in-depth analysis of the data, three overarching themes: Vulnerabilities, Positive outcomes, and Challenges, emerged. These themes and associated sub themes are shown in Table 4 . The interplay among these major domains within the context of themes and subthemes are summarised in Fig. 2 .
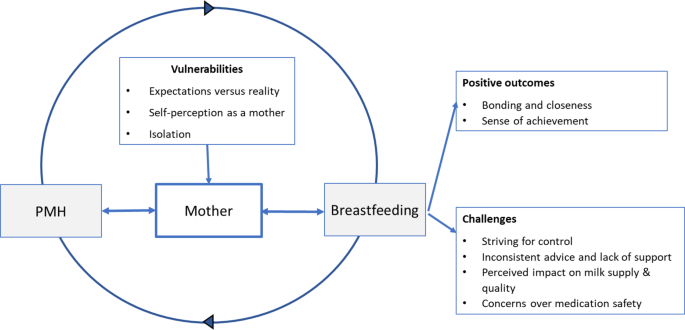
Illustration of the interplay of themes and subthemes of the breastfeeding experiences of women with perinatal mental health problems PMH – Perinatal mental health
Theme: vulnerabilities
Expectations versus reality.
For some new mothers the reality of breastfeeding did not meet their expectations of being easy and ‘natural’, leaving them feeling unprepared and disillusioned when they experienced difficulties.
“You think you’re a completely useless mother and, you know, you should be able to know how to do this instinctively [breastfeeding] and in fact it’s probably the hardest thing I’ve ever done.” (25, p255).
Limited availability of antenatal breastfeeding advice led to mothers being unaware of the potential complexities of breastfeeding during the early days and weeks.
“Everyone make it seem like it’s natural because your body produces [milk]. It’s just something that should frequently come to you as soon as you have the baby., but it’s not like that. You had to hold the baby a certain way, you got to adjust your thing a certain way, you got to put the nipple in far enough for the baby to get it. There’s a lot to it. It’s really complicated.” (26, p5).
Self-perception as a mother
To be perceived as a ‘good mother’, by themselves and others, some women felt they must breastfeed at all costs. This perceived association of breastfeeding as the representation of ‘good mothering’, appeared to result in self-imposed pressure.
“I was so desperate to breastfeed him and I felt as if it was my, I felt as if I had some moral obligation as a mother and if I didn’t breast feed him I was badly letting him down.” (25, p255).
If these women were then unable to breastfeed, or if they faced significant breastfeeding difficulties, this sometimes led to feelings of guilt or inadequacy.
“There’s so much pressure on you to breastfeed. so you’re told that breast is best and you should do it and so when you don’t you think you are a failure and it’s what you should be doing.” (39, p322).
The opinions of family, friends and health professionals also played a significant part in the woman’s perception of her status as a ‘good mother’.
“The approval thing was a big factor. Everyone was telling me how well I’d done to keep breastfeeding. All that approval made me feel really good about myself, and that I was being a good mother to (baby). I wasn’t thinking negative thoughts about myself, I was feeling very positive really.” (35, p114).
However, for some mothers, this resulted in added pressure, causing them to hide their feelings and maintain an outward display of happiness.
“I didn’t want to talk with anybody about it, I always had to pretend that I was doing just great … I thought that wasn’t normal, that I was a bad mom who felt that way.” (37, p264).
Finding the right support could be very beneficial but some women had negative experiences of clinics or groups, undermining their self-belief.
“Daggers are drawn and everybody’s acting as if they can rule the world and the trouble is, when you’re depressed you just see that image and you think, I’m never going to be as good as this.” (39, p323).
Feelings of isolation felt by breastfeeding women were exacerbated by mental health issues, with Homewood et al. (39, p325) suggesting that breastfeeding could contribute to depression by increasing the sense of being trapped by the infant’s dependency.
“abandoned and alone … .scared all the time that something would happen to the baby…” (37, p264).
The sense of isolation was increased by the fact that seeking help could be difficult for women who were distressed because they were reluctant to reveal their negative feelings.
“I was feeling like really sad and just really isolated and really stuck!. . I just thought. . “How am I going to take care of this baby? And I am feeling so crappy!” I found it to be really hard just to reach out and admit that I was feeling the way that I was. I don’t know why I was so worried about being stigmatized, but I was. I just didn’t want that label of being a person with postpartum depression.” (32, p12) “.
Theme: positive outcomes
Bonding and closeness.
Whilst struggling with mental health issues, the experience of breastfeeding successfully could increase mothers’ positive feelings toward the baby, allowing them to enjoy time spent together and enhance their confidence.
“I used to feed her and it was the time I got a little lump in my throat and thought, oh, perhaps she’s not that bad, and I thought, this is perhaps how people feel a bit more of the time than I feel it.” (39, p323).
Some women reported that the physical aspect of breastfeeding allowed a connection that could compensate, to a degree, for the mental withdrawal caused by the depressive symptoms.
“I think [breastfeeding] helps because even if I feel like some days I’m not very connected emotionally, I know that at least I’m providing the baby with physical touch and bonding and all that. Even if I’m not mentally 100% there. So, I think it makes me feel better about myself as a mom.” (33, p641).
One mother noted that breastfeeding could reduce feelings of stress.
‘‘When I’m nursing her, I’m able to just hold her. And that just alleviates any worries, any stress that I’ve had through the day, just knowing that she needs me, that she’s finding comfort in me, that I’m able to comfort her. She’s comforting me at the same time.” (26, p5).
Sense of achievement
Achieving success with breastfeeding was a factor in mitigating some of the guilt that women with eating disorders might feel about the possible effects of their eating disorder on the baby, positively affecting their self-esteem.
“It wasn’t my instinct to want to breastfeed him but in the end I did. In some ways it made up for all the damage I thought I’d done to him because of my eating disorder.” (35, p113).
Some women who had experienced a traumatic birth perceived breastfeeding as having the potential to heal and reinforced their self-perception as a good mother.
“I would cover her up to feed her and hide her little head in the clothing. Not because of dignity, but because I did not want anyone else to see the magic and healing that was happening between us. Being able to breastfeed my daughter, despite all the odds, is my proudest achievement in life. I wear it in my soul as a badge of honor.” (29, p233).
Women described how breastfeeding was within their sphere of control whereas other aspects of motherhood were not.
“[Breastfeeding] was the one thing that I could control. . I think that it made me feel better because it was the one thing that I was successful at, as a mom, because my birth went so shitty, and everything just kind of spiraled down and my mood and everything. . .I lean on [breastfeeding] a lot. It is my thing with her that no one can take away. . .I don’t like other people doing it. I don’t even like the suggestion of other people doing it.” (32, p12).
Theme: challenges
Striving for control.
Some women with eating disorders perceived stopping breastfeeding as the only way to allow them to resume control over their body and their eating.
“I wanted my body back and I knew I wouldn’t get it back until I’d stopped breastfeeding. I knew the minute that stopped feeding him I could control my food again and that’s what I wanted. When I was feeding I needed to eat properly because he needs the nutrients.” (35, p114).
For women with obsessive compulsive disorder [ 30 ], some responded to contamination fears by breastfeeding, sometimes for much longer than planned.
“I forced myself to breastfeed for the whole of the first year because I was convinced that formula would be contaminating his body.” (30, p317).
Other women with eating disorders chose not to breastfeed in order to allow themselves to return to purging and undertaking strenuous exercise in order to lose their pregnancy weight rapidly [ 35 ].
Some still struggled between eating a ‘good’ diet to produce ‘healthy’ milk and the desire to return to their usual strategies such as restricted eating or purging.
“I didn’t need to make myself sick so often [when breastfeeding] but that wasn’t because I didn’t want to! [Laughs] I had to fight with myself all the time to control the urge. I thought breastfeeding would take that urge away but it didn’t. It eased a bit but I was still vomiting all the time I was breastfeeding.” (35, p112).
Inconsistent advice and lack of support
Women’s difficulties and lack of confidence with breastfeeding were increased by inconsistent advice from both professionals and family [ 25 ]. Mothers frequently made reference to seeking advice from healthcare professionals during the early weeks of breastfeeding but felt they were often left unsupported.
“I was alone and . the nurse often didn’t answer the buzzer, my buzzer when I was trying to breast feed and things. Again I felt so kind of, incredibly sensitive about everything, and anxious about everything, and they just weren’t there, were never there for me.” (25, p256).
Mothers described feeling pressurised by healthcare professionals to continue breastfeeding [ 35 ] and, without adequate support, women would often turn to friends or relatives for infant feeding advice [ 25 ].
Concerns over medication safety
Concerns regarding medication safety and breastfeeding [ 26 , 27 , 34 ] led some women to discount breastfeeding as an option for them.
“….I could try and breastfeed, but yeah, I decided that wasn’t—a good idea. Because it’s too hard and I wouldn’t be able to go back on my medication—right away after the baby was born. You have to wait two months, or something like that. So I thought that was dangerous— for both of us.” (34, p383).
Whilst others discontinued breastfeeding due to health concerns for the baby.
“And I had to get my wisdom teeth pulled out, so I decided to stop because they put you on antibiotics and stuff like that. So I just stopped.”(26, p5).
Some women with severe mental illness felt that due to the complexities of their mental health, breastfeeding was not considered relevant and was “de-prioritized” for other aspects of acute care [ 27 ]. Despite many mothers expressing strong preferences to continue breastfeeding, the mothers often felt that their preferences were ignored.
“Medication was an issue as I was initially given medication that specified it should not be taken while breastfeeding, when I had made my wish to breastfeed very clear.” (27, p7).
Some women felt that they needed to prompt staff to consider whether the medication they were prescribed would allow breastfeeding, or, alternatively, be given the choice to cease breastfeeding to allow them to have the most suitable medication to treat their mental health condition.
“I wish they had told me to stop breastfeeding rather than give me diluted medication.” (27, p6).
Others described being given contradictory information from health professionals about breastfeeding whilst taking psychotropic medication:
“Early in pregnancy, the mental health midwife said not to take fluoxetine if breastfeeding and to change to sertraline or citalopram. Next time I saw her later on and she said I could stay on fluoxetine if I was happy on it.” (27, p6).
Such conflicting advice made mothers confused and distressed. A resultant lack of confidence in healthcare professionals “ prompted some women to conduct their own research or to disregard medical advice ” (27, p6).
Perceived impact on milk quality and supply
There was a perception that women with PMH conditions would be unable to produce a sufficient quality and/or volume of breastmilk to sustain their baby nutritionally. This concern could potentially generate feelings of depression for women [ 26 ].
Some mothers perceived that their own poor nutrition could potentially cause problems with breastfeeding. This concern was often associated with eating disorders [ 26 ], food unavailability or lack of appetite due to mental ill health [ 38 , 41 ]. For women with eating disorders there was a belief that frequent cycles of binging and purging were not compatible with producing sufficient good quality breast milk. This caused some women to discount breastfeeding, and some received pressure from partners to bottle feed in the belief that the child would not receive the necessary nutrition.
“He (husband) didn’t want me to breastfeed because he thought I wasn’t eating enough to feed her (baby) properly. [.] He was on and on about me giving her the bottle. He even dragged my sister in to try and get her to talk me round.” (35, p111).
Some women with eating disorders did wish to breastfeed and commented on needing to change their eating patterns to achieve this.
“I had to eat properly when I was breastfeeding because I had a baby to think about. The baby needs nutrition. I thought whatever I eat the baby is going to get it. So I had to eat properly. Like when I was pregnant I made myself eat properly.” (35, p112).
Depression and anxiety are a common problem in the perinatal period, and pregnancy and childbirth can put women at risk of relapse or exacerbation of pre-existing mental illness [ 17 ]. Although postpartum anxiety is more prevalent than postpartum depression [ 42 ] we did not find any studies of women’s experiences of anxiety and breastfeeding. In this review there were examples of specific mental illnesses being associated with specific issues in relation to breastfeeding along with the difficulties faced by many women. Data from the included studies replicated what is already known regarding the relationship between perinatal depression and breastfeeding, that this relationship is bidirectional, with evidence of depressive symptoms contributing to worse breastfeeding outcomes and breastfeeding challenges sometimes serving as a trigger for postnatal depressive symptoms [ 43 ].
In this study it was found that, for mothers who were struggling with their mental health, the sense of achievement obtained by successful breastfeeding could boost their self-esteem and bolster the perception of themselves as a good mother [ 29 , 32 , 40 ]. These mothers found that breastfeeding could increase their mother/child bond and reinforce their confidence as a mother and felt that the closeness experienced during breastfeeding could reduce feelings of stress and compensate their baby for times when they were feeling withdrawn [ 26 , 33 , 35 , 39 ].
However, the perception that ‘good mothering’ is defined by successful breastfeeding can also result in overwhelming pressure for mothers, who may feel obliged to breastfeed despite experiencing challenges [ 44 , 45 , 46 ]. This pressure can then be further compounded by the attitudes and behaviours of healthcare professionals, family members and society in general [ 46 ]. A large proportion of the women in the included studies had a strong intention to breastfeed [ 25 , 28 , 31 , 33 , 37 ] and were often motivated to continue, despite difficulties, because of the pressure they placed on themselves to fulfil the role of the ‘good mother’. If they then had difficulties or ceased breastfeeding they often experienced feelings of guilt, inadequacy, and failure [ 25 , 27 , 40 ].
There is a wealth of literature describing the guilt and despair experienced when women’s expectations for breastfeeding to occur naturally, the desire to be a good mother, and ‘breast is best’, clash with the demands and labour-intensive workload that breastfeeding often entails [ 43 , 44 , 47 , 48 ]. A lack of antenatal education regarding potential breastfeeding challenges appears to be evident, with much of this being dedicated to the benefits of breastfeeding to both mother and baby, and although this information is important, it can provide a skewed ideal of the breastfeeding process [ 47 ]. Findings from studies by Hoddinott et al. [ 47 ] and Redshaw and Henderson [ 48 ] suggested realistic antenatal education is key to preparing women for common difficulties and suggest providing a realistic view rather than rosy pictures or patronising breastfeeding workshops with knitted breasts and dolls [ 47 ]. This lack of preparation for the challenges that frequently arise during the early days of breastfeeding can result in mothers feeling inadequate and unable to cope [ 45 , 46 ], potentially resulting in early discontinuation of breastfeeding and/or a decline in mental wellbeing.
The perception that mental health conditions can lead to insufficient or poor-quality breast milk is a common perception amongst breastfeeding women. A systematic review of breastfeeding problems by Karaçam and Sağlık, [ 49 ], found that 12 out of 34 studies referred problems such as “inadequate breastmilk/lack of breastmilk/ concern for inadequate breastmilk/thought that the baby was not satiated adequately/inadequate weight gain.” The theme was again identified by this study, particularly amongst those with eating disorders [ 29 , 35 ] and women from the two African based studies [ 38 , 41 ]. Women’s perceptions were primarily that poor mental health leads to inadequate nutritional intake (due to lack of appetite/disordered eating) and therefore impacts breastmilk volume and quality. This added burden of believing that their breastmilk may not adequately sustain their child could potentially further impact their mental health as a perceived failure [ 29 ].
For some women a sense of isolation in their role as carer, and specifically regarding breastfeeding was expressed in the included studies [ 25 , 32 , 34 ]. The sense of isolation can be magnified both by the symptoms of mental health issues and the reluctance of the mothers to reveal their condition, either pre-existing or newly emerging, to their loved ones and health professionals, worrying about what they may think [ 30 , 32 , 37 ]. This is reflected in previous research, which found stigma associated with mental ill health, compounded by a pervasive social stigma attached to being seen to ‘fail’ as a mother, leads to under-reporting of perinatal mental health issues [ 50 ]. A study of Australian women undergoing routine psychosocial assessment also found that 11.1% reported they were not always honest in the assessment and lack of trust in the midwife was the most frequent reason for non-disclosure [ 51 ]. Failure to reveal previous mental health issues may lead to inappropriate or sub-optimal advice [ 35 ].
The findings also identified that a lack of trust in the support and advice given by health professionals was also a contributing factor when considering medication safety and was stated as a reason to cease or not commence breastfeeding [ 27 , 34 ]. These inconsistencies sometimes prompted women to undertake their own research to gain answers [ 27 ], which could potentially lead to serious health consequences. The concerns held by women regarding medication safety and breastfeeding were highlighted in a Swedish study [ 52 ] which found that 57.7% of pregnant participants classed medication use during breastfeeding as harmful/probably harmful.
This lack of consistent advice regarding medication safety is largely due to a lack of high-quality evidence [ 53 ]. However, for those requiring medication during the postnatal period, clearer guidance is needed from healthcare professionals on the suitability of each type of medication when breastfeeding, and whether alternative medications can be considered so that breastfeeding can be undertaken safely without additional worry. Some women in the study felt they did not have the opportunity to make an informed choice regarding their medication and that desire to breastfeed was deprioritised over their mental health [ 27 ]. However, findings from this and previous studies have shown that when breastfeeding is successful it can improve mood and help protect against postnatal depression [ 32 , 33 , 54 , 55 ], as well as strengthen mother-child bonding [ 26 , 33 ]. It may therefore be the case that, in conjunction with suitable medication, breastfeeding may further help to boost mood and improve the overall wellbeing of the mother by providing a sense of achievement and control.
Negative attitudes towards diagnosis and treatment of perinatal mental health conditions result in women avoiding help seeking and reinforces feelings of stigma and guilt. Organisational-level factors such as inadequate resources, fragmentation of services and poor interdisciplinary communication compound these individual-level issues [ 50 , 56 ]. Structural factors (especially poor policy implementation) and sociocultural factors (for example language barriers) also cause significant barriers to accessing services for this group of women [ 50 , 56 ].
A strength of this review is the inclusion of literature regarding various mental health conditions (not purely depression) which had not been previously synthesised. This review highlights that each mental health condition may impact differently on breastfeeding experiences and merits separate investigation to inform policy and practice. The findings from this synthesis were based on a systematic literature search of five electronic databases. Inductive and in-depth analysis, using an iterative approach, allowed for immersion in the data, which strengthened the review findings.
Limitations were similar to those identified by previous studies relating to maternal mental health needs [ 57 ]. Participants were predominantly white and well educated, and studies were primarily undertaken in high income countries. This means that the findings may not be applicable to all women particularly those from low-income countries who may have different experiences and needs. None of the included studies incorporated the views and experiences of women from low socioeconomic status specifically, who are more likely to experience PMH conditions [ 47 ]. A comparison of the breastfeeding experiences of women with PMH conditions between different countries was beyond the scope of this review, however it must be acknowledged that differences are expected due to variations in culture, health systems, resource, and infant feeding attitudes.
The methods of diagnosing mental health conditions differed between studies. Some participants had a clinical diagnosis, whilst some were included based upon tools such as the Edinburgh Postnatal Depression Scale, or a self-diagnosis of distress/depression. This allowed us to increase the scope of studies included but may mean that some studies included women who may have not met the criteria for a clinal diagnosis of depression.
To ensure completeness prior to publication, the original search was again undertaken to capture any studies published between November 2021 and February 2024. The search identified two further papers which met the inclusion/exclusion criteria. Both papers supported the original themes found in the study and therefore further validated the findings. Scarborough et al. [ 58 ] reported a perceived pressure to breastfeed, mixed impact on the mental health of the mother and the mother infant bond, and challenges receiving adequate information and support. Frayne et al. [ 59 ] highlighted the importance of good communication, consistency of advice, and shared decision making for women taking psychotropic medication, and the challenges faced if these aspects were not achieved.
There is a complex dynamic relationship amongst breastfeeding intention, practice, and experiences for mothers with PMH conditions. The intensity and magnitude of positive outcomes that women describe, and the challenges experienced, are exacerbated in mothers with PMH conditions. The challenging experiences are particularly influenced by a lack of support, shame, fear of stigmatisation and additional health concerns, such as worries over medication safety.
The synthesis identified inconsistent advice from healthcare professionals, particularly in relation to medication. Further training and improved communication pathways between specialities may help enhance perinatal maternity care provision. An in depth understanding of the women’s views/needs in relation to their specific PMH condition could help enhance their experiences of infant feeding. This will help women to make informed choices about feeding, increasing their sense of control and improving self-efficacy, which could have a positive impact on their emotional and physical wellbeing, their ability to bond with their baby and their transition to motherhood.
Gaps identified through this systematic review include the need for further investigation on breastfeeding and PMH in women from minority groups, as well as a need for robust evidence and advice on medication use during breastfeeding for women experiencing perinatal mental ill health.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Victora CG, Bahl R, Barros AJ, Franca GV, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Lancet Breastfeeding Series Group. Breastfeeding in the 21st century: Epidemiology, mechanisms and lifelong effect. Lancet. 2016;387(10017):475–90. https://doi.org/10.1016/S0140-6736(15)01024-7 .
Article PubMed Google Scholar
Horta BL, Loret de Mola C, Victora CG. Breastfeeding and intelligence: a systematic review and meta-analysis. Acta Paediatr. 2015a;104:14–9. https://doi.org/10.1111/apa.13139 .
Horta BL, Loret de Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta analysis. Acta Paediatr. 2015b;104:30–7. https://doi.org/10.1111/apa.13133 .
Article CAS PubMed Google Scholar
Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, Piwoz EG, Richter LM, Victora CG. Lancet Breastfeeding Series. Why invest, and what will it take to improve breastfeeding practices? Lancet. 2016;387(10017):491–504. https://doi.org/10.1016/S0140-6736(15)01044-2 .
United Nations. Transforming our world: the 2030 agenda for sustainable development https://sdgs.un.org/2030agenda [Accessed 12th May 2021].
World Health Organisation. Breastfeeding . https://www.who.int/health-topics/breastfeeding#tab=tab_3 [Accessed 12 May 2021].
McFadden A, Gavine A, Renfrew MJ, Wade A, Buchanan P, Taylor JL, Veitch E, Rennie AM, Crowther SA, Neiman S, MacGillivray S. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Reviews. 2017;2017(2):CD001141–001141. https://doi.org/10.1002/14651858.CD001141.pub5 .
Article Google Scholar
Skouteris H, Bailey C, Nagle C, Hauck Y, Bruce L, Morris H. Interventions designed to promote exclusive breastfeeding in high-income countries: a systematic review update. Breastfeed Med. 2017;12(10):604–14. https://doi.org/10.1089/bfm.2017.0065 .
Public Health England. Breastfeeding prevalence at 6 to 8 weeks after birth (experimental statistics). London: TSO; 2021.
Google Scholar
Brown CR, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Health. 2014;105(3):179–85.
Galipeau R, Baillot A, Trottier A, Lemire L. ‘Effectiveness of interventions on breastfeeding self-efficacy and perceived insufficient milk supply: a systematic review and meta-analysis’. Matern Child Nutr 2018;14 (3).
Dagher RK, McGovern PM, Schold JD, Randall XJ. ‘Determinants of breastfeeding initiation and cessation among employed mothers: a prospective cohort study’. BMC Pregnancy Childbirth. 2016;16 (194).
Dennis C, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes. Acta Paediatr. 2007;96(4):590–4. https://doi.org/10.1111/j.1651-2227.2007.00184.x .
Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt. Gesundheitsforschung Gesundheitsschutz. 2018;61(8):977–85. https://doi.org/10.1007/s00103-018-2769-0 .
Daehn D, Rudolf., Pawils S, Renneberg B. Perinatal mental health literacy: knowledge, attitudes, and help-seeking among perinatal women and the public – a systematic review. BMC Pregnancy Childbirth. 2022;22(1):1–574. https://doi.org/10.1186/s12884-022-04865-y .
O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Practice & Research. Clin Obstet Gynecol. 2014;28(1):3–12. https://doi.org/10.1016/j.bpobgyn.2013.09.002 .
Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19(3):313–27. https://doi.org/10.1002/wps.20769 .
Article PubMed PubMed Central Google Scholar
Tucker Z, O’Malley C. Mental Health benefits of Breastfeeding: A literature review. Curēus. 2022;14(9):e29199–29199. https://doi.org/10.7759/cureus.29199 .
Tanganhito DDS, Bick D, Chang Y. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–9. https://doi.org/10.1016/j.wombi.2019.05.012 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71). https://doi.org/10.1136/bmj.n71 .
World Health Organisation. Global strategy for infant and young child feeding .https://www.apps.who.int/iris/bitstream/handle/10665/42590/9241562218.pdf [Accessed 10th May 2021].
Cooke A, Smith D, Booth A, Beyond PICO. The SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43. https://doi.org/10.1177/1049732312452938 .
Critical Appraisal Skills Programme. CASP Qualitative Studies Checklist . https://casp-uk.net/casp-tools-checklists/ . [Accessed 4th June 2021].
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. https://doi.org/10.1186/1471-2288-8-45 .
Shakespeare J, Blake F, Garcia J. Breast-feeding difficulties experienced by women taking part in a qualitative interview study of postnatal depression. Midwifery. 2004;20(3):251–60. https://doi.org/10.1016/j.midw.2003.12.011 .
Stelson EA, Kulkacek L, Frasso R, Hall M, Guevara JP. Perspectives on breastfeeding from mothers with Postpartum Depression symptoms: a qualitative Assessment of antecedents, barriers, facilitators, and intervention suggestions. Breastfeed Med. 2021;16(10):790–8. https://doi.org/10.1089/bfm.2020.0251 .
Baker N, Potts L, Jennings S, Trevillion K, Howard LM. Factors affecting infant feeding practices among women with severe Mental illness. Front Global Women’s Health. 2021;2:624485. https://doi.org/10.3389/fgwh.2021.624485 .
Gordon LK, Mason KA, Mepham E, Sharkey EM. A mixed methods study of perinatal sleep and breastfeeding outcomes in women at risk for postpartum depression. Sleep Health. 2021;7(3):353–61. https://doi.org/10.1016/j.sleh.2021.01.004 .
Beck CT, Watson S. Impact of birth trauma on Breast-feeding: a tale of two pathways. Nurs Res. 2008;57(4):228–36. https://doi.org/10.1097/01.NNR.0000313494.87282.90 .
Burton HAL. How women with established obsessive compulsive disorder experience pregnancy and postpartum: an interpretative phenomenological analysis. J Reproductive Infant Psychol. 2021;39(3):313–25. https://doi.org/10.1080/02646838.2020.1718628 .
Coates R, Ayers S, de Visser R. Women’s experiences of postnatal distress: a qualitative study. BMC Pregnancy Childbirth. 2014;14:359. https://doi.org/10.1186/1471-2393-14-359 .
Olson T, Holstlander L, Bowen A. Mother’s milk, mother’s tears breastfeeding with postpartum depression. Clin Lactation. 2014;5(1):9–15. https://doi.org/10.1891/2158-0782.5.1.9 .
Pratt BA, Longo J, Gordon SC, Jones NA. Perceptions of breastfeeding for women with Perinatal Depression: a descriptive phenomenological study. Issues Ment Health Nurs. 2020;41(7):637–44. https://doi.org/10.1080/01612840.2019.1691690 .
Humphries JM, McDonald C. Unveiling new dimensions: a hermeneutic exploration of perinatal mood disorder and infant feeding. Issues Ment Health Nurs. 2012;33(6):377–86. https://doi.org/10.3109/01612840.2012.656824 .
Stapleton H, Fielder A, Kirkham M. Breast or bottle? Eating disordered childbearing women and infant-feeding decisions. Maternal Child Nutr. 2008;4(2):106–20. https://doi.org/10.1111/j.1740-8709.2007.00121.x .
Fooladi MM. Therapeutic tears and postpartum blues. Holist Nurs Pract. 2006;20(4):204–11. https://doi.org/10.1097/00004650-200607000-00009 .
Edhborg M, Friberg M, Lundh W, Widström AM. Struggling with life: narratives from women with signs of postpartum depression. Scand J Public Health. 2005;33(4):261–7. https://doi.org/10.1080/14034940510005725 .
Emerson JA, Tol W, Caulfield LE, Doocy S. Maternal psychological distress and perceived impact on child feeding practices in South Kivu, DR Congo. FoodNutr Bull. 2017;38(3):319–37. https://doi.org/10.1177/0379572117714385 .
Homewood E, Tweed A, Cree M, Crossley J. Becoming occluded: the transition to motherhood of women with postnatal depression. Qualitative Res Psychol. 2009;6(4):313–29. https://doi.org/10.1080/14780880802473860 .
Hesse Tyson C, O’Connor J, Sheehan JD. No space for mother’s mind: a psychoanalytically oriented qualitative study of the experiences of women with a diagnosis of postnatal depression. Int J Appl Psychoanal Stud. 2020;18(4):393–407. https://doi.org/10.1002/aps.1687 .
Scorza P, Owusu-Agyei S, Asampong E, Wainberg ML. The expression of perinatal depression in rural Ghana. Int J Cult Mental Health. 2015;8(4):370–81. https://doi.org/10.1080/17542863.2015.1037849 .
Zappas M, Becker K, Walton-Moss B. Postpartum anxiety. J Nurse Practitioners. 2021;17(1):60–4. https://doi.org/10.1016/j.nurpra.2020.08.017 .
Fox R, McMullen S, Newburn M. UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of Baby Café services. BMC Pregnancy Childbirth. 2015;15(1). https://doi.org/10.1186/s12884-015-0581-5 .
Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Maternal Child Nutr. 2010;6(3):201–19. https://doi.org/10.1111/j.1740-8709.2009.00209.x .
Jackson L, De Pascalis L, Harrold J, Fallon V. Guilt, shame, and postpartum infant feeding outcomes: a systematic review. Maternal Child Nutr. 2021;17(3):e13141–n/a. https://doi.org/10.1111/mcn.13141
Beggs B, Koshy L, Neiterman E. Women’s perceptions and experiences of Breastfeeding: a scoping review of the literature. BMC Public Health. 2021;21(1):1–2169. https://doi.org/10.1186/s12889-021-12216-3 .
Hoddinott P, Craig LCA, Britten J, McInnes RM. A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open. 2012;2(2):000504–000504. https://doi.org/10.1136/bmjopen-2011-000504 .
Redshaw M, Henderson J. Safely delivered: a national survey of women’s experience of maternity care 2014. University of Oxford: National Perinatal Epidemiology Unit; 2015. https://www.npeu.ox.ac.uk/research/projects/119-national-maternity-survey-2014 . [Accessed 10th June 2021].
Karacam Z, Saglik M. Breastfeeding problems and interventions performed on problems: systematic review based on studies made in Turkey. Turk Pediatri Arsivi. 2018;53(3):134–48. https://doi.org/10.5152/TurkPediatriArs.2018.6350 .
Sambrook Smith M, Lawrence V, Sadler E, Easter A. Barriers to accessing mental health services for women with perinatal mental illness: systematic review and meta-synthesis of qualitative studies in the UK. BMJ Open. 2019;9:e024803. https://doi.org/10.1136/bmjopen-2018-024803 .
Mule V, Reilly NM, Schmied V, Kingston D, Austin MV. Why do some pregnant women not fully disclose at comprehensive psychosocial assessment with their midwife? Women Birth: J Australian Coll Midwives. 2022;35(1):80–6. https://doi.org/10.1016/j.wombi.2021.03.001 .
Wolgast E, Lindh-Åstrand L, Lilliecreutz C. Women’s perceptions of medication use during pregnancy and breastfeeding—A Swedish cross‐sectional questionnaire study. Acta Obstet Gynecol Scand. 2019;98(7):856–64. https://doi.org/10.1111/aogs.13570 .
University of Birmingham. Healthy Mum, Healthy Baby, Healthy Future The Case for UK Leadership in the Development of Safe, Effective and Accessible Medicines for Use in Pregnancy. University of Birmingham. 2022 https://www.birminghamhealthpartners.co.uk/wp-content/uploads/2022/05/Final-Healthy-Mum-Healthy-Baby-Healthy-Future-Report-AW_Accessible-PDF-REDUCED-FILE-SIZE.pdf [Accessed 11 June 2022].
Borra C, Iacovou M, Sevilla A. New evidence on breastfeeding and postpartum depression: the importance of understanding women’s intentions. Matern Child Health J. 2015;19(4):897–907. https://doi.org/10.1007/s10995-014-1591-z .
Kendall-Tackett K, Cong Z, Hale TW. The Effect of Feeding Method on Sleep Duration, maternal Well-being, and Postpartum Depression. Clin Lactation. 2011;2(2):22–6. https://doi.org/10.1891/215805311807011593 .
Manolova G, Waqas A, Chowdhary N, Salisbury TT, Dua T. Integrating perinatal mental healthcare into maternal and perinatal services in low and middle income countries. BMJ (Online). 2023;381, e073343–073343. https://doi.org/10.1136/bmj-2022-073343
Sacks E, Finlayson K, Brizuela V, Crossland N, Ziegler D, Sauvé C, Langlois ÉV, Javadi D, Downe S, Bonet M. Factors that influence uptake of routine postnatal care: findings on women’s perspectives from a qualitative evidence synthesis. PLoS ONE. 2022;17(8):e0270264–0270264. https://doi.org/10.1371/journal.pone.0270264 .
Article CAS PubMed PubMed Central Google Scholar
Scarborough J, Norman A, Cooper L. The bidirectional relationship between breastfeeding and mental health. Br J Midwifery. 2022;30(10):554–62. https://doi.org/10.12968/bjom.2022.30.10.554 .
Frayne J, Ellies R, Nguyen T. Experiences of decision making about psychotropic medication during pregnancy and breastfeeding in women living with severe mental illness: a qualitative study. Arch Womens Ment Health. 2023;26:379–87. https://doi.org/10.1007/s00737-023-01325-0 . https://www.doi-org.hallam.idm.oclc .
Download references
Acknowledgements
For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
This research was sponsored by British Academy with the partnership of the Leverhulme Trust. The sponsors had no involvement in the study design; in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Author information
Authors and affiliations.
College of Health, Wellbeing and Life Sciences, Sheffield Hallam University, Collegiate Campus, Sheffield, S10 2DN, UK
Hayley Billings, Janet Horsman & Hora Soltani
Nursing and Midwifery College of Health, Wellbeing and Life Sciences, Sheffield Hallam University, Collegiate Campus, Sheffield, S10 2DN, UK
Rachael Louise Spencer
You can also search for this author in PubMed Google Scholar
Contributions
Conception - R.S, H.S; Design - H.B, J.H, R.S, H.S; Funding acquisition - R.S; Acquisition of data - H.B, J.H; Analysis and interpretation of data - H.B, J.H; Validation - H.B, J.H, R.S, H.S; Writing - Original Draft - H.B, J.H, Writing - Review & Editing - H.B, R.S, H.S; Supervision - R.S, H.S;
Corresponding author
Correspondence to Hayley Billings .
Ethics declarations
Ethical approval.
Ethical approval was not required for this systematic review as all material was available in the public domain.
Consent for publication
Not applicable.
Competing interests
Hora Soltani is on the editorial board for BMC Pregnancy and Childbirth.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Billings, H., Horsman, J., Soltani, H. et al. Breastfeeding experiences of women with perinatal mental health problems: a systematic review and thematic synthesis. BMC Pregnancy Childbirth 24 , 582 (2024). https://doi.org/10.1186/s12884-024-06735-1
Download citation
Received : 09 August 2023
Accepted : 02 August 2024
Published : 06 September 2024
DOI : https://doi.org/10.1186/s12884-024-06735-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Mental health
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 10.9.2024 in Vol 8 (2024)
Assessment of a Pilot Program for Remote Support on Mental Health for Young Physicians in Rural Settings in Peru: Mixed Methods Study
Authors of this article:

Original Paper
- Kelly De la Cruz-Torralva 1 , BSc ;
- Stefan Escobar-Agreda 1 , MD ;
- Pedro Riega López 1 , MD ;
- James Amaro 1 , MD ;
- C Mahony Reategui-Rivera 1, 2 , MD ;
- Leonardo Rojas-Mezarina 1 , MD
1 Unidad de Telesalud, Facultad de Medicina, Universidad Nacional Mayor de San Marcos, Cercado de Lima, Peru
2 Department of Biomedical Informatics, University of Utah, Salt Lake City, UT, United States
Corresponding Author:
Pedro Riega López, MD
Unidad de Telesalud
Facultad de Medicina
Universidad Nacional Mayor de San Marcos
Av Grau 755
Cercado de Lima, 15001
Phone: 51 619 7000 ext 4650
Email: [email protected]
Background: Telemedicine-based interventions show promise in addressing mental health issues among rural populations, yet evidence regarding their impact among the health care workforce in these contexts remains limited.
Objective: This study aimed to evaluate the characteristics and the responses and perceptions of recently graduated physicians who work in rural areas of Peru as part of the Servicio Rural Urbano Marginal en Salud (Rural-Urban Marginal Health Service [SERUMS], in Spanish) toward a telehealth intervention to provide remote orientation and accompaniment in mental health.
Methods: A mixed methods study was carried out involving physicians who graduated from the Universidad Nacional Mayor de San Marcos and participated in the Mental Health Accompaniment Program (MHAP) from August 2022 to February 2023. This program included the assessment of mental health conditions via online forms, the dissemination of informational materials through a website, and, for those with moderate or high levels of mental health issues, the provision of personalized follow-up by trained personnel. Quantitative analysis explored the mental health issues identified among physicians, while qualitative analysis, using semistructured interviews, examined their perceptions of the services provided.
Results: Of 75 physicians initially enrolled to the MHAP, 30 (41.6%) opted to undergo assessment and use the services. The average age of the participants was 26.8 (SD 1.9) years, with 17 (56.7%) being female. About 11 (36.7%) reported have current or previous mental health issues, 17 (56.7%) indicating some level of depression, 14 (46.7%) indicated some level of anxiety, 5 (16.6%) presenting a suicidal risk, and 2 (6.7%) attempted suicide during the program. Physicians who did not use the program services reported a lack of advertising and related information, reliance on personal mental health resources, or neglect of symptoms. Those who used the program expressed a positive perception regarding the services, including evaluation and follow-up, although some faced challenges accessing the website.
Conclusions: The MHAP has been effective in identifying and managing mental health problems among SERUMS physicians in rural Peru, although it faced challenges related to access and participation. The importance of mental health interventions in this context is highlighted, with recommendations to improve accessibility and promote self-care among participants.
Introduction
In Peru, recently graduated physicians participate in the Servicio Rural Urbano Marginal en Salud (Rural-Urban Marginal Health Service [SERUMS], in Spanish), which involves working in rural areas of Peru for 1 year [ 1 ]. This kind of initiative undertaken in several countries in Latin America has been shown to be effective in attracting the participation of health professionals in these areas, enhancing the distribution of and access to health services in underserved populations [ 2 ]. Although SERUMS allows newly graduated physicians their first work experience in a primary care setting, participation in this service raises several challenges for these professionals, such as limited logistical and human resources in rural health facilities [ 3 ] and physicians’ lack of knowledge about the sociocultural factors [ 4 ] of the population they serve [ 5 , 6 ]. This situation, observed in various countries, has shown to affect doctors practicing in rural areas, reducing their job satisfaction and levels of well-being [ 7 ].
In line with this evidence, SERUMS physicians in Peru have been identified as a population with a remarkably high prevalence of mental health problems, even higher than that observed in the general population [ 5 , 6 ]. In addition, the COVID-19 pandemic is likely to have exacerbated this problem, as the prevalence of disorders, such as burnout, anxiety, depression, and alcohol use, among health care workers has increased [ 8 - 12 ]. In alignment with this, the Universidad Nacional Mayor de San Marcos (UNMSM) introduced a program to offer remote accompaniment and orientation to support mental health for physicians serving in rural areas during the SERUMS period.
In general, the use of telemedicine-based interventions has been shown to have positive effects on the well-being of physicians [ 13 ] and has proven to be effective in managing mental health problems among rural populations [ 14 ]. However, there is limited evidence regarding the effects of such interventions among SERUMS physicians in rural areas where the implementation of other remote interventions has proven to have a limited reach [ 15 ]. Therefore, our study aimed to describe the characteristics and perceptions of recently graduated physicians who work in rural areas of Peru toward a telehealth intervention to provide remote orientation and accompaniment in mental health.
Study Design and Context
We conducted a mixed methods study using a sequential explanatory design, which is a recommended approach that sequentially integrates quantitative cross-sectional and qualitative data for evaluating telehealth interventions [ 16 ].
Study Population
Participants were SERUMS physicians enrolled in the Mental Health Accompaniment Program (MHAP) of the UNMSM. We used a list of 2021 medical graduates from the university who were scheduled to join SERUMS in 2022. To recruit participants, we implemented a process that involved distributing invitations via WhatsApp messages and phone calls. Approximately 1 month after starting their SERUMS, stakeholders who accepted the invitation received a questionnaire of mental problems screened. This questionnaire included an informed consent form.
The Mental Health Accompaniment Program
The MHAP was designed and implemented by the Faculty of Medicine of the UNMSM from August 2022 to February 2023. Its main objective was to provide remote orientation and accompaniment on mental health for physicians graduating from this university who were going to participate in SERUMS. The program used a virtual platform and involved a team of trained personnel comprising psychiatrists, psychologists, and trained general physicians responsible for providing brief intervention and suicide prevention services. A designated coordinator team was responsible for supervising all program activities to ensure its smooth and effective implementation.
The MHAP included 4 services: evaluation and screening, self-help, brief intervention, and suicide prevention.
Evaluation and Screening Service
During the first months of SERUMS, all registered physicians at the MHAP were required to complete virtual questionnaires to assess the presence and severity of conditions such as depression, anxiety, alcohol consumption, and suicidal risk. Based on their results, participants were provided with appropriate care options tailored to their mental health status. In this process, specific criteria were established to determine the severity of cases and the history of mental health problems:
- Severe cases: These included problems showing high scores on different psychometric scales: the 9-item Patient Health Questionnaire (PHQ-9), score≥20; 7-item Generalized Anxiety Disorder (GAD-7), score≥15; the Alcohol Use Disorders Identification Test (AUDIT), score≥20; and Ask Suicide-Screening Questions (ASQ), a positive response to any of the 5 questions, including question 5, which was considered an emergency, or refusal to answer.
- History of mental health problems: This referred to any mental health problem that had required prior pharmacological treatment.
- Treatment received: This included any mental health problem that had already received the recommended treatment previously.
Self-Help Service
All physicians enrolled in the program had low severity of mental health problems and were offered access to the self-help service that includes the use of the Kusikuy website ( Multimedia Appendix 1 ), an exclusive platform designed for the program that offers psychoeducational material on mental health, including self-help tools that allowed SERUMS physicians to self-manage issues, such as depression, anxiety, stress, problematic alcohol consumption, and fear of COVID-19
Brief Intervention Service
The brief intervention [ 17 , 18 ] is a transdiagnostic strategy based on the focused acceptance and commitment therapy developed by Stroshal and Robinson [ 19 ] that has the characteristics of being time limited, has been shown to be effective, and is short term. In addition, it aims to promote psychological flexibility in people through dialogue focusing on 3 pillars (as the authors call it): openness, awareness, and commitment.
The intervention process involves (1) framing, where therapists presents themselves as having an attitude of validation; (2) an assessment, which consists of a contextual interview, identification of the level of functionality, and the 3 pillars (in the commitment pillar, personal values are identified); and (3) the intervention itself, which includes behavioral experiments through a commitment to change aligned with the identified personal values [ 19 ].
The brief intervention varies from 2 to 4 sessions of approximately 20-40 minutes per participant. The first session develops the entire process, and subsequent sessions are a reinforcement of the observation of the 3 pillars and analysis of the results of the behavioral experiments, with emphasis on behaviors that promote or limit behavioral change [ 20 ]. The therapists were mental health professionals who participated in training on contextual therapies training by a certified professional, including acceptance and commitment therapy.
Suicide Prevention Service
SERUMS physicians who exhibited any level of suicide risk were provided with the suicide prevention service. A specialized psychiatrist contacted the physicians through instant messaging or phone calls to provide immediate assistance and guidance for managing their condition and facilitate prompt attention.
The provision of the brief intervention Service and suicide prevention services included several appointments between mental health professionals and SERUMS physicians for ongoing support and guidance until the physicians’ condition improved or was effectively managed. Severe cases receive additional counseling to continue meeting a specialist in a health care facility.
Variables and Instruments
For the quantitative phase, we used data about the sociodemographic characteristics of physicians, such as gender and age, as well as the characteristics of the health care facilities where they worked, such as the region, level of complexity, and originating institution, collected during the program through virtual forms. This also included the evaluation of the mental health conditions of physicians through validated questionnaires, such as depression (PHQ-9), anxiety (GAD-7), alcohol use (AUDIT), and suicide screening (ASQ) [21–24]; the application of these instruments lasted for approximately 20-25 minutes. The presence of a history of mental health issues, including current or previous presence of mental health problems or the use of psychiatric medication, was also reported. Furthermore, the total number of participants and sessions conducted in the counseling and suicide prevention services was evaluated.
For the qualitative phase, the study had a qualitative inductive phenomenological design because of its usefulness in understanding and interpreting people’s experiences and meanings. This design is considered suitable for locating the meanings that people give to the events, processes, and structures of their lives and their perceptions, presuppositions, and assumptions. The use of this method allows us to know in depth their perceptions, appreciating their particularities, entering into the phenomenological explanations that quantitative research does not reach to analyze [ 21 ].
In-depth interviews were conducted using a semistructured interview guide. Physicians who initially agreed to participate in the MHAP were interviewed over the phone. All the interviewed physicians were asked about their perceptions of (1) the current mental health situation in SERUMS physicians and (2) the importance of developing a mental health intervention for this population. Specifically, those physicians who received some of the services of the MHAP were asked about their perceptions of and recommendations for these services, and those physicians who did not receive any service were asked about their reasons for not using the program. Interviews lasted approximately 15 minutes each and were audio-recorded and transcribed for subsequent analysis.
Data Analysis
For quantitative analysis, we conducted a descriptive analysis using RStudio version 4.2.3 (Posit). Numeric variables were summarized using means (SDs), while categorial variables were presented in tables showing frequencies and percentages. For qualitative analysis, we conducted a thematic analysis using ATLAS.ti 9.0 software (ATLAS.ti Scientific Software Development GmbH). This involved coding the content according to the objectives of the interviews and subsequently linking those codes to generate categories that reflected the interviewees’ perceptions. Finally, quantitative and qualitative results were evaluated and interpreted together in order to draw conclusions that addressed the stated objectives.
Ethical Considerations
The study was approved by the Research Ethics Committee of the Faculty of Medicine at the UNMSM (approval number 0172). Compliance with all relevant ethical approvals and established procedures for research involving human subjects was ensured. All participants in the study provided their informed consent to participate. No form of financial compensation was offered to participants for their involvement in this study. Furthermore, measures were implemented to analyze the data anonymously, ensuring the privacy and confidentiality of the collected information.
Quantitative Results
Of the 116 physicians who graduated from the UNMSM and participated in SERUMS, 79 (68.1%) were contactable and 75 (94.9%) agreed to participate in the MHAP (see Figure 1 ). By the end of this intervention, 30 (41.6%) of the enrolled physicians ended up using at least 1 of the services offered in the MHAP (see Table 1 ). The mean age of these 30 physicians was 26.8 (SD 1.9) years, and 17 (56.7%) were women. Concerning their health care facilities during SERUMS, 15 (50%) belonged to category I-2, and 28 (93.3%) belonged to the Peruvian Ministry of Health (MINSA). Most of these facilities were located in Huanuco (n=7, 23.3%) and Huancavelica (n=6, 20%).
All the 9 (30%) evaluated physicians who exhibited moderate (n=7, 77.8%) or high (n=2, 22.2%) severity in at least 1 of the evaluated conditions agreed to receiving the brief intervention service over the phone or via video calls from a member of the MHAP health staff. The 2 (22.2%) participants categorized as “high severity” expressed suicidal intent during the program. Their evaluations were conducted by a psychiatrist, who confirmed the presence of a clinical syndrome in these physicians. Upon concluding their follow-up in the program, both physicians expressed a preference to continue treatment with the program’s psychiatrist, opting not to seek care in other institutions, such as the social security system in Peru (EsSalud), through which they are insured via their employment. During the follow-up period, no incidents of relapse (high risk) or worsening (moderate risk) were detected in the intervened cases.

| Characteristics | Depression | Anxiety | Alcoholic risk | Suicide risk | Any mental disease | Total (N=30) | |||||||||||||
| Any (n=17) | None (n=13) | Any (n=14) | None (n=16) | Any (n=4) | None (n=26) | Any (n=5) | None (n=25) | Any (n=21) | None (n=9) | ||||||||||
| Female | 11 (64.7) | 6 (46.2) | 10 (71.4) | 7 (43.8) | 2 (50.0) | 15 (57.7) | 4 (80.0) | 13 (52.0) | 13 (61.9) | 4 (44.4) | 17 (56.7) | ||||||||
| Male | 6 (35.3) | 7 (53.8) | 4 (28.6) | 9 (56.2) | 2 (50.0) | 11 (42.3) | 1 (20.0) | 12 (48.0) | 8 (38.1) | 5 (55.6) | 13 (43.3) | ||||||||
| Age (years), mean (SD) | 26.9 (1.60) | 26.5 (2.30) | 27.1 (1.92) | 26.4 (1.90) | 25.5 (3.32) | 27.0 (1.61) | 27.2 (2.28) | 26.7 (1.86) | 26.5 (2.02) | 27.3 (1.58) | 26.8 (1.91) | ||||||||
| Anxiety and depression | 1 (5.9) | 0 | 1 (7.1) | 0 | 0 | 1 (3.8) | 0 | 1 (4.0) | 1 (4.8) | 0 | 1 (3.3) | ||||||||
| Anxiety | 4 (23.5) | 0 | 3 (21.4) | 1 (6.3) | 1 (25.0) | 3 (11.5) | 1 (20.0) | 3 (12.0) | 4 (19.0) | 0 | 4 (13.3) | ||||||||
| Depression | 5 (29.4) | 0 | 3 (21.4) | 2 (12.5) | 0 | 5 (19.2) | 1 (20.0) | 4 (16.0) | 5 (23.8) | 0 | 5 (16.7) | ||||||||
| Suicide attempt | 1 (5.9) | 0 | 1 (7.1) | 0 | 1 (25.0) | 0 | 1 (20.0) | 0 | 1 (4.8) | 0 | 1 (3.3) | ||||||||
| No history of mental disorder | 6 (35.3) | 13 (100.0) | 6 (42.9) | 13 (81.3) | 2 (50.0) | 17 (65.4) | 2 (40.0) | 17 (68.0) | 10 (47.6) | 9 (100.0) | 19 (63.3) | ||||||||
| No therapy | 4 (36.4) | 0 | 3 (37.5) | 1 (33.3) | 2 (100.0) | 2 (22.2) | 2 (66.7) | 2 (25.0) | 4 (36.4) | 0 | 4 (36.4) | ||||||||
| Pharmacological and psychological therapy | 3 (27.3) | 0 | 1 (12.5) | 2 (66.7) | 0 | 3 (33.3) | 0 | 3 (37.5) | 3 (27.3) | 0 | 3 (27.3) | ||||||||
| Psychological therapy | 4 (36.4) | 0 | 4 (50.0) | 0 | 0 | 4 (44.4) | 1 (33.3) | 3 (37.5) | 4 (36.4) | 0 | 4 (36.4) | ||||||||
a SERUMS: Servicio Rural Urbano Marginal en Salud (Rural-Urban Marginal Health Service).
b MHAP: Mental Health Accompaniment Program.
c The sum of percentages for some subheadings might be less than or more than 100 because of rounding.
d Only those who reported a history of mental disease.
Qualitative Results
For the qualitative phase, we interviewed 8 (26.7%) of the 30 participants, 4 (50%) who used the program and 4 (505) who did not. To estimate the number of selected physicians in this phase, we used the saturation technique, which incorporates participants until their responses no longer provide further information regarding the objectives of the interview.
Mental Health Situation in SERUMS Physicians
Participants reported experiencing behavioral and mood changes, increased anxiety, nervousness, sadness, difficulty sleeping, headaches, and adjustment disorders during the initial months of SERUMS. They also noted that several colleagues underwent similar experiences, including episodes of depression.
I believe that I experienced a mental health problem, perhaps it could be an adjustment disorder. I realized it because normally I am cheerful and always feel like doing things, or at least most of the time I feel like doing things, but the joy decreased, I felt less joyful and less motivated to do things. [Participant 3]
Several of my colleagues with whom I have a close relationship from university also had mental health problems...one of my colleagues was quite depressed, I don’t know to what extent, but he was definitely quite depressed, and another one of my colleagues also experienced depression, and that is what we see the most among SERUMS physicians. [Participant 1]
Importance of Mental Health Interventions
Participants emphasized the critical nature of mental health interventions for physicians in SERUMS. They highlighted the necessity of guidance for all SERUMS health care professionals who consistently face stressful situations. These stressors are motivated by challenges arising from adapting to new environments, distance from family and friends, internet connectivity issues limiting communication with loved ones, and difficulties in their work environment. Consequently, they require tools to cope with such events effectively.
Well, I believe it is fundamental, it is essential for a health care professional, regardless of whether they are going through a specific problem. I think we all should have mental health support because, in SERUMS, for example, we face different things. We are not in Lima, but in an environment that is not comfortable, so we face different adversities, and we need guidance that helps us stay calmer and cope with the situation. [Participant 4]
For example, I am from Piura. I finished high school and then came to Lima alone. I even went abroad for a month for an exchange program. And when my SERUMS came, I thought it wouldn't affect me, everything would be fine, but it is very different...perhaps because you have greater responsibility, and every action you take will weigh on and affect others. That is why you experience a lot of stress. So, I believe providing mental health support for us is very important, and I appreciate this initiative. [Participant 3]
Perception of the Mental Health Program
SERUMS physicians indicated that the resources provided in the MHAP were significantly beneficial, expressing satisfaction with the services received. From their perspective, interactions with the mental health team were highly professional, and they established a good relationship as they were provided with a trusting, listening, and guiding space, enabling them to cope with their challenges. Regarding the resources on the Kusikuy website, they mentioned having difficulties accessing the page due to an unstable internet connection. Nonetheless, they found the content they could access useful.
In my experience so far, everything has been good. I am quite satisfied with the service they have provided me, so everything is fine, and it has helped me a lot, to be honest. [Participant 4]
Very good, really. It supports you a lot, knows how to listen to you, knows how to guide you…excellent! [Participant 2]
Very good service with the doctor, it gave me confidence...I think it has been a good initiative on your part to provide this mental health service. [Participant 3]
I took a general look at it, but I didn’t use it much. From what I could see, it seemed like an interesting website with plenty of resources, but I couldn’t explore it further due to internet problems, and when I had a good internet connection, I forgot about it. [Participant 1]
Reasons for Not Using the Program
Some physicians did not engage with the program, even though they reported experiencing emotionally distressing situations and mental health issues. Among the reasons for not accessing the program, many physicians mentioned not having sufficient time to properly inform themselves about the program, or they received information during their working hours, which led to postponing reading those messages and eventually forgetting to respond. This resulted in them being uninformed about the program and, therefore, not using it.
Basically, it is because I didn’t have time. Being a head at my health center, I was busy almost all the time. At one point, I did consider seeking help from the service, but I didn’t have the time. [Participant 1]
I think the main reason is that, for example, when I wanted to enroll or get information about the program, they would call or send messages during working hours, which is actually an inconvenient time because you are attending to patients and can't respond at that moment. Then, I would forget to reply, and that is how it went...I would prefer them to call me outside of working hours, where I could attend to them better and get more information. [Participant 3]
Another reason mentioned by participants is that although they experienced feelings of discomfort, they chose to ignore those sensations and continue with their routine. Alternatively, they mentioned using their personal resources, such as maintaining stronger connections with their support network and engaging in distracting and entertaining activities, among others. Therefore, they did not feel the need to use the service, as they used their personal tools.
I wanted to use the mental health service; I was interested in the program since the SERUMS experience was quite challenging for me...it is just that I think I preferred to ignore my discomfort and continue with my routine. I buried all my distress and sadness to focus on my other tasks. [Participant 2]
While the first few months were difficult in SERUMS, I feel like I didn't require the service, because it was an adaptation process that was mine to handle. I chose to call my friends, be with my family, study for the residency exam, watch TV series, and that is how the days passed. I adapted with my own resources. [Participant 4]
Other reasons mentioned were related to the lack of publicity for the program. Not everyone was clear about the services provided in the program, and they were unaware of the existence of the Kusikuy website, which they believed could have been a great help. They also expressed the hope that the program would include other tools, such as workshops on communication and leadership, among other topics, as they are necessary and useful for SERUMS, and could also be attractive for encouraging participation in the program.
I think they need to improve the advertising because I was unaware of the website, which would have been very helpful due to all the materials they had, but I didn’t know about it. So, one of the reasons why we didn’t use their resources is because we didn’t know about them. [Participant 3]
In addition to the services I knew they would provide, it would also be useful if they organized workshops on communication tools, leadership models, improving the work environment, and even workshops on how to interact better with patients. I think it would also be appealing to the SERUMS participants to encourage us to use the program. [Participant 2]
Recommendations for Improving the Mental Health Program
Among the recommendations for the MHAP, SERUMS physicians suggested increasing the frequency of sessions with mental health professionals, as they are currently limited to once a month. They also deemed it necessary to reduce the time between completing the initial survey and the first session with the mental health professionals, as it took between 3 and 4 weeks before receiving communication. Additionally, they expressed a preference for having an application instead of the Kusikuy website, due to the difficulties they experienced in accessing it. They also wished to have the option to download resources and use them offline.
Beyond the services provided in the MHAP, participants expressed their desire to have support groups composed of other serum physicians and led by mental health professionals. They requested the inclusion of more resources related to stress management, anxiety, study techniques, personality tests, work environments, and conflict resolution among colleagues, and they wanted those resources to be provided through WhatsApp.
Perhaps the sessions with the doctor could be a little more frequent and not just once a month. I know it is due to the teachers’ time and that it is free, but I would like it to be more than once a month. Apart from that, I have no criticism of the program; I am satisfied with this initiative. [Participant 2]
Regarding the website you designed, I think it could be an application or through WhatsApp or whatever it may be, but it should have the ability to download videos or use videos offline...without relying so much on the internet. [Participant 3]
Principal Findings
The results of the study suggest that the implementation of the MHAP is effective in identifying and managing mental health conditions in newly graduated physicians working in rural areas of Peru in the context of SERUMS. Although we found no evidence of digital mental health interventions for these professionals, our findings are consistent with other studies highlighting the usefulness of digital tools in identifying and treating mental health problems [ 22 ]. In addition, it is suggested that interventions aimed at addressing COVID-19–related mental health issues among health care workers may improve coping skills and reduce symptoms, such as anxiety, depression, and posttraumatic stress disorder [ 23 ], as well as problematic alcohol use [ 24 ].
Despite the initial interest of SERUMS physicians in the MHAP, their real commitment diminished once they were assessed in the initial part of the program. This phenomenon could be due to the current tendency seen in people to ignore mental health concerns in their daily routine and the stigma associated with seeking help [ 25 - 27 ]. Among the factors that we found to limit their participation included a preference for using personal resources to address mental health issues and a lack of time or connectivity to participate in online activities that are in concordance with evidence reported elsewhere [ 28 - 32 ]. These findings highlight the complexity of addressing mental health difficulties and underscore the importance of considering various factors, from beliefs and stigma to resource availability and satisfaction with proposed interventions, to promote a more effective approach.
Another noteworthy finding of our study was the high proportion (around 50%) of SERUMS physicians who reported experiencing depression or anxiety, and 5 of them even expressed suicidal thoughts, indicating a significant problem in their mental health compared to previous studies [ 4 , 5 ]. Despite being noticeable, this result should be interpreted cautiously as it may overestimate the true prevalence, because it was based only on physicians who agreed to be evaluated in the program. Nevertheless, the fact that there is a significant frequency of SERUMS physicians with mental health problems highlights the need to address this problem. The inherent vulnerability to SERUMS conditions and concern about the increase in mental health problems among undergraduate medical students [ 33 ] leads to an increased risk of mental health problems among physicians. It is crucial to address this concern by deploying more health staff or teams to meet the growing demand for psychological support.
SERUMS physicians with moderate and severe levels of mental health issues demonstrated good engagement with the services of the program, participating in all sessions with specialists. Similar findings have been observed in other studies, where mental health status influenced the interest in and the use of digital mental health interventions [ 25 , 34 , 35 ]. It is important to note that this engagement was more common within the program than in the usual care channels provided to SERUMS physicians through social security hospitals. In addition, although SERUMS physicians had a mostly positive perception of MHAP services, some experienced difficulties with virtual tools, such as access to the Kusikuy website, which has been identified in other research as a barrier to participation in similar interventions [ 25 , 27 , 35 ]. Therefore, it is essential to ensure that broadcasting and distance education services are available on platforms with low connectivity requirements or are easily accessible through mobile devices, which are the most used by these professionals.
Limitations and Strengths
Although these results are significant, it is important to recognize certain limitations. The interviews were conducted at the end of the SERUMS year, which increased the possibility of recall bias and could have affected the accuracy of the information collected. In addition, it is important to consider the influence of social desirability bias on our results, given the stigma still associated with mental health problems, so participants may have tended to underestimate or minimize their experiences. This bias could have influenced the reported incidence rates of mental health problems among SERUMS physicians, which could have led to an underestimation of the true prevalence.
Despite these limitations, our study provides important insights into the high incidence of mental health problems among SERUMS physicians and the potential of digital mental health interventions to close the gap in access to mental health services. In addition, the MHAP demonstrated several strengths that have shown positive outcomes in the mental health of SERUMS physicians, such as timely identification, participation in services, and satisfaction with them.
The MHAP has proven to be a valuable intervention for addressing mental health issues among SERUMS physicians in rural areas of Peru, demonstrating its effectiveness in both identifying and managing mental health conditions in this population. Despite the good participation and reception of the services by the participants, challenges were faced in terms of access and participation. The identification of previous mental health problems among physicians and their willingness to participate in the program highlights the importance of mental health interventions in this context. However, barriers related to the lack of time, the stigma associated with seeking help, and a preference for personal resources underscore the need to improve program accessibility and promotion. Some recommendations that can be included are diversifying the resources offered, raising awareness about the importance of self-care, and promoting support spaces among participating physicians. This will maximize the impact and benefits of the program for SERUMS physicians in Peru.
Acknowledgments
We would like to thank the Servicio Rural Urbano Marginal en Salud (SERUMS) physicians who participated in this study and the mental health professional team (Patricia Bacigalupo and Daniela Málaga).
Data Availability
The data sets analyzed during the study are not publicly available as they are part of confidential information of Servicio Rural Urbano Marginal en Salud (SERUMS) physicians involved in the Mental Health Accompaniment Program of the Universidad Nacional Mayor de San Marcos. However, these could be anonymized and shared by the corresponding author upon reasonable request.
Conflicts of Interest
None declared.
Kusikuy website interface.
Scores of mental health outcomes in MHAP. AUDIT: Alcohol Use Disorders Identification Test; GAD-7: 7-item Generalized Anxiety Disorder; MHAP: Mental Health Accompaniment Program; PHQ-9: 9-item Patient Health Questionnaire.
- Ministerio de Salud. Ley del Servicio Rural y Urbano Marginal de Salud. Ley no 23330. Búsquedas El Peruano. 1981. URL: https://tinyurl.com/hyna52kp [accessed 2024-09-03]
- Carpio C, Bench N. The Health Workforce in Latin America and the Caribbean: An Analysis of Colombia, Costa Rica, Jamaica, Panama, Peru, and Uruguay. Washington, DC. World Bank; 2015.
- Anticona Huaynate CF, Pajuelo Travezaño MJ, Correa M, Mayta Malpartida H, Oberhelman R, Murphy LL, et al. Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. Oct 05, 2015;15(1):454. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Reyes Solari E. "Allá es clínicamente así: saber llegar". De la formación a la práctica profesional médica. El Servicio Rural Urbano Marginal en Salud (SERUMS). Apunt Rev Cienc Soc. 2011;38(69):55-80. [ CrossRef ]
- Mejia CR, Vega-Melgar V, Jiménez-Meza Y, Chacón JI, Inga-Berrospi F. Factores asociados a depresión en médicos que trabajarán en zonas rurales del Perú. Rev Chil Neuro-Psiquiatr. Dec 2019;57(4):320-328. [ CrossRef ]
- Galán-Rodas E, Gálvez-Buccollini JA, Vega-Galdós F, Osada J, Guerrero-Padilla D, Vega-Dienstmaier J, et al. [Mental health in physicians doing the rural and suburban health service in Peru: a baseline study]. Rev Peru Med Exp Salud Publica. Jun 2011;28(2):277-281. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Haggerty TS, Fields SA, Selby-Nelson EM, Foley KP, Shrader CD. Physician wellness in rural America: a review. Int J Psychiatry Med. Feb 10, 2014;46(3):303-313. [ CrossRef ]
- Villarreal-Zegarra D, Reátegui-Rivera CM, Otazú-Alfaro S, Yantas-Alcantara G, Soto-Becerra P, Melendez-Torres GJ. Estimated impact of the COVID-19 pandemic on the prevalence and treatment of depressive symptoms in Peru: an interrupted time series analysis in 2014-2021. Soc Psychiatry Psychiatr Epidemiol. Sep 08, 2023;58(9):1375-1385. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Glob Health. Sep 25, 2020;16(1):89. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yáñez JA, Afshar Jahanshahi A, Alvarez-Risco A, Li J, Zhang S. Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. Am J Trop Med Hyg. Oct 2020;103(4):1614-1620. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. Apr 9, 2020;89(4):242-250. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Halsall L, Irizar P, Burton S, Waring S, Giles S, Goodwin L, et al. Hazardous, harmful, and dependent alcohol use in healthcare professionals: a systematic review and meta-analysis. Front Public Health. Nov 28, 2023;11:1304468. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nakagawa K, Yellowlees PM. University of California Technology Wellness Index: a physician-centered framework to assess technologies’ impact on physician well-being. Psychiatr Clin North Am. Dec 2019;42(4):669-681. [ CrossRef ] [ Medline ]
- Hilty DM, Gentry MT, McKean AJ, Cowan KE, Lim RF, Lu FG. Telehealth for rural diverse populations: telebehavioral and cultural competencies, clinical outcomes and administrative approaches. mHealth. Apr 2020;6:20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rojas-Mezarina L, Escobar-Agreda S, Chahuara-Rojas M, Silva-Valencia J, Espinoza-Herrera DH, Reátegui-Rivera CM, et al. Usability and perceptions of a one-on-one telementoring program for young physicians in rural settings of Peru: a mixed method study. BMC Med Educ. Mar 22, 2023;23(1):175. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Caffery LJ, Martin-Khan M, Wade V. Mixed methods for telehealth research. J Telemed Telecare. Sep 03, 2016;23(9):764-769. [ CrossRef ]
- Ruiz FJ, Luciano C, Flórez CL, Suárez-Falcón JC, Cardona-Betancourt V. A multiple-baseline evaluation of acceptance and commitment therapy focused on repetitive negative thinking for comorbid generalized anxiety disorder and depression. Front Psychol. Mar 13, 2020;11:356. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Glasgow RE, Fisher L, Strycker LA, Hessler D, Toobert DJ, King DK, et al. Minimal intervention needed for change: definition, use, and value for improving health and health research. Transl Behav Med. Mar 10, 2014;4(1):26-33. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Strosahl K, Robinson P, Gustavsson T. Brief Interventions for Radical Change. Oakland, CA. New Harbinger Publications; 2012.
- Glover NG, Sylvers PD, Shearer EM, Kane M, Clasen PC, Epler AJ, et al. The efficacy of focused acceptance and commitment therapy in VA primary care. Psychol Serv. May 2016;13(2):156-161. [ CrossRef ] [ Medline ]
- Al-Busaidi ZQ. Qualitative research and its uses in health care. Sultan Qaboos Univ Med J. Mar 2008;8(1):11-19. [ FREE Full text ] [ Medline ]
- Frehywot S, Mullan F, Payne PW, Ross H. Compulsory service programmes for recruiting health workers in remote and rural areas: do they work? Bull World Health Org. May 01, 2010;88(5):364-370. [ CrossRef ]
- Robins-Browne K, Lewis M, Burchill LJ, Gilbert C, Johnson C, O'Donnell M, et al. Interventions to support the mental health and well-being of front-line healthcare workers in hospitals during pandemics: an evidence review and synthesis. BMJ Open. Nov 07, 2022;12(11):e061317. [ FREE Full text ] [ CrossRef ] [ Medline ]
- King SC, Richner KA, Tuliao AP, Kennedy JL, McChargue DE. A comparison between telehealth and face-to-face delivery of a brief alcohol intervention for college students. Subst Abus. Oct 01, 2020;41(4):501-509. [ CrossRef ] [ Medline ]
- Borghouts J, Eikey E, Mark G, De Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res. Mar 24, 2021;23(3):e24387. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Deen TL, Fortney JC, Schroeder G. Patient acceptance of and initiation and engagement in telepsychotherapy in primary care. Psychiatr Serv. Apr 01, 2013;64(4):380-384. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Simblett S, Matcham F, Siddi S, Bulgari V, Barattieri di San Pietro C, Hortas López J, et al. RADAR-CNS Consortium. Barriers to and facilitators of engagement with mHealth technology for remote measurement and management of depression: qualitative analysis. JMIR Mhealth Uhealth. Jan 30, 2019;7(1):e11325. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brooks HL, Bee P, Lovell K, Rogers A. Negotiating support from relationships and resources: a longitudinal study examining the role of personal support networks in the management of severe and enduring mental health problems. BMC Psychiatry. Feb 07, 2020;20(1):50. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harjumaa M, Halttu K, Koistinen K, Oinas-Kukkonen H. User experience of mobile coaching for stress-management to tackle prevalent health complaints. In: Oinas-Kukkonen H, Iivari N, Kuutti K, Öörni A, Rajanen M, editors. Nordic Contributions in IS Research. Cham. Springer International Publishing; 2015:152-164.
- Wilhelmsen M, Lillevoll K, Risør MB, Høifødt R, Johansen M, Waterloo K, et al. Motivation to persist with internet-based cognitive behavioural treatment using blended care: a qualitative study. BMC Psychiatry. Nov 7, 2013;13(1):296. [ CrossRef ]
- Sinha DK, Tuli A, Sood M, Chadda R, Verma R, Kumar S, et al. Is India ready for mental health apps (MHApps)? A quantitative-qualitative exploration of caregivers' perspective on smartphone-based solutions for managing severe mental illnesses in low resource settings. PLOS ONE. Sep 19, 2018;13(9):e0203353. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Perales A, Izaguirre M, Sánchez E, Barahona L, Martina M, Amemiya I, et al. Salud mental en estudiantes de pregrado de la Facultad de Medicina de la Universidad Nacional Mayor de San Marcos. An Fac Med. Dec 27, 2019;80(4):443-450. [ CrossRef ]
- Crisp D, Griffiths K. Participating in online mental health interventions: who is most likely to sign up and why? Depress Res Treat. 2014;2014:790457. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arjadi R, Nauta MH, Bockting CL. Acceptability of internet-based interventions for depression in Indonesia. Internet Interv. Sep 2018;13:8-15. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Berry N, Lobban F, Bucci S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry. Jan 21, 2019;19(1):35. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| Ask Suicide-Screening Questions |
| Alcohol Use Disorders Identification Test |
| 7-item Generalized Anxiety Disorder |
| Mental Health Accompaniment Program |
| Patient Health Questionnaire |
| Servicio Rural Urbano Marginal en Salud (Rural-Urban Marginal Health Service) |
| Universidad Nacional Mayor de San Marcos |
Edited by A Mavragani; submitted 04.11.23; peer-reviewed by P Kumwichar, D Hilty; comments to author 11.12.23; revised version received 27.03.24; accepted 18.04.24; published 10.09.24.
©Kelly De la Cruz-Torralva, Stefan Escobar-Agreda, Pedro Riega López, James Amaro, C Mahony Reategui-Rivera, Leonardo Rojas-Mezarina. Originally published in JMIR Formative Research (https://formative.jmir.org), 10.09.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in JMIR Formative Research, is properly cited. The complete bibliographic information, a link to the original publication on https://formative.jmir.org, as well as this copyright and license information must be included.
Implementing peer support into practice in mental health services: a qualitative comparative case study
- Open access
- Published: 11 September 2024
- Volume 24 , article number 1050 , ( 2024 )
Cite this article
You have full access to this open access article

- Steve Gillard 1 ,
- Rhiannon Foster 1 ,
- Sarah White 2 ,
- Rahul Bhattacharya 3 ,
- Paul Binfield 3 ,
- Rachel Eborall 4 ,
- Sarah L Gibson 5 ,
- Daniella Harnett 3 ,
- Alan Simpson 6 ,
- Mike Lucock 7 ,
- Jacqueline Marks 8 ,
- Julie Repper 9 ,
- Miles Rinaldi 10 , 11 ,
- Anthony Salla 1 &
- Jessica Worner 12
Peer workers are people with personal experience of mental distress, employed within mental health services to support others with similar experiences. Research has identified a range of factors that might facilitate or hinder the introduction of new peer worker roles into mental health services. While there is mixed evidence for the effectiveness of peer worker delivered interventions, there are no studies exploring how implementation might be associated with effect.
This was a qualitative comparative case study using data from interviews with 20 peer workers and their five supervisors. Peer workers delivered peer support for discharge from inpatient to community mental health care as part of a randomised controlled trial. In the trial, level of participant engagement with peer support was associated with better outcome (hospital readmission). Study sites with higher levels of engagement also had higher scores on a measure of fidelity to peer support principles. We compared data from sites with contrasting levels of engagement and fidelity using an analytical framework derived from implementation theory.
In high engagement-high fidelity sites, there was regular work with clinical teams preparing for working alongside peer workers, and a positive relationship between staff on inpatient wards and peer workers. The supervisor role was well resourced, and delivery of peer support was highly consistent with the intervention manual. In low engagement-low fidelity sites peer workers were employed in not-for-profit organisations to support people using public mental health services and in rural areas. Supervisors faced constrained resources and experienced barriers to joint working between organisations. In these sites, peer workers could experience challenging relationships with ward staff. Issues of geography and capacity limited opportunities for supervision and team-building, impacting consistency of delivery.
Conclusions
This study provides clear indication that implementation can impact delivery of peer support, with implications for engagement and, potentially, outcomes of peer worker interventions. Resourcing issues can have knock-on effects on consistency of delivery, alongside challenges of access, authority and relationship with clinical teams, especially where peer workers were employed in not-for-profit organisations. Attention needs to be paid to the impact of geography on implementation.
Trial registration
ISRCTN registry number ISRCTN10043328, registered 28 November 2016.
Explore related subjects
- Artificial Intelligence
Avoid common mistakes on your manuscript.
Peer support in mental health services
People with personal experience of mental distress, often referred to as peer workers, are increasingly employed within mental health services internationally to support others with similar experiences. An extensive literature explores a range of implementation issues that might dilute the distinctive qualities of peer support when introduced into public mental health services [ 1 , 2 ]. These include adequate provision of role specific training for PWs, [ 3 , 4 ] support and supervision for PWs, [ 5 ] clarity of expectation around the way in which PWs bring experience-based knowledge to mental healthcare, [ 2 . 6 ] and preparation of clinical teams to work alongside PWs [ 7 ]. It has been argued that ‘over-professionalisation’ or ‘institutionalisation’ of the PW role constrains the distinctive contribution of peer support [ 8 , 9 , 10 , 11 ].
Trials of peer support in mental health services continue to demonstrate inconsistent results, with some studies indicating that peer support might be superior to care-as-usual or a comparator intervention, [ 12 , 13 ] while others indicate no difference in effect [ 14 , 15 ]. Some of this variation might be explained by heterogeneity of interventions, population or outcome, but it is also possible that the quality of implementation of peer support into mental healthcare settings is associated with the effect of peer support interventions [ 16 , 17 ].
It has been noted that peer support is often poorly described in the trial literature, [ 17 , 18 ] with a lack of research assessing association between implementation and outcome. A recent review of one-to-one peer support in mental health services categorised peer support as being well implemented where at least two of the following criteria were reported: dedicated peer support training; clear description of the underlying processes of peer support; well-defined support structures for PWs (e.g. supervision) [ 19 ]. However, only a small number of studies reported sufficient data to conduct an analysis and results were unclear. There is a need for research that explicitly considers the possible relationship between quality of implementation and the outcomes of peer support.
Implementation theory
Implementation science offers a range of frameworks for understanding the facilitators and barriers to successful implementation of healthcare innovation into practice [ 20 ]. There is a clear recognition that the effects of any intervention will always depend on successful implementation [ 21 ]. The well-established Promoting Action on Research Implementation in Health Services (PARIHS) framework conceptualises successful implementation of research-based innovation into healthcare in terms of the nature of the evidence on which the innovation is based, the context or environment into which the innovation is placed, and the method by which implementation is facilitated [ 22 ]. In recent years, the co-design [ 23 ] or coproduction [ 24 ] of new interventions in mental health has gained prominence, with people who use mental health services bringing experience-based knowledge to the process, alongside the professional and practice-based knowledge brought by healthcare professionals. Given that this experiential knowledge is core to peer support, and that a number of members of the research term brought their own experiences of mental distress and/ or of using mental health services to the design and conduct of the research, we adapted the PARIHS framework for the purposes of this study. An earlier scoping review of implementation literature and an empirical case study, [ 25 ] undertaken by members of the team (SG and RF), identified five domains where experiential knowledge might impact research implementation, and we mapped these domains directly onto the framework (Table 1 ).
The ENRICH trial
A trial of peer support for discharge from inpatient to community mental health care indicated that peer support was not superior to care-as-usual (follow up by community mental health services within seven days of discharge) in terms of either the primary outcome – readmission within 12 months of discharge – or a range of secondary outcomes [ 26 ]. PWs received eight days of training focused on individual strengths and connecting to community, met the people they were supporting at least once while still inpatients and then weekly for up to four months post-discharge. Peer support was flexible and collaborative, informed by a peer support principles framework [ 27 ]. PWs received group and individual supervision from an experienced peer worker coordinator (PWC) who had access to an action learning set with other PWCs across study sites. The trial and intervention are described in detail in a protocol paper [ 28 ].
Findings from the trial indicated that 62.5% of participants offered peer support had at least two contacts with their PW, at least one of which was post-discharge, and that those participants were significantly less likely to be readmitted than a similar group of PWs in the care-as-usual group [ 26 ]. There might be many reasons why people chose not to, or were unable to engage with their PW, including the possibility that peer support was not always well implemented into practice in the trial.
This paper aims to explore if and how levels of engagement in a new peer support intervention were associated with implementation of the intervention, and therefore how implementation of peer support in mental health services might be optimised in the future.
Study design
We take a comparative case study approach, informed by case-orientated Qualitative Comparative Analysis [ 29 ] and pattern-matching [ 30 ] techniques, considering the seven sites where the study took place as cases. Sites were National Health Services (NHS) mental health trusts (public healthcare provider organisations) in England, where the new peer support intervention was delivered as part of the ENRICH trial. Sites were selected to provide contrast in urban, town and rural localities, geographical spread across England, and where mental health trusts were committed to introducing new PW roles into mental health services. In most sites PWs were directly employed by the mental health trust, while in others a much smaller, voluntary (not-for-profit) sector organisation was sub-contracted by the trust to employ PWs to provide support to people using mental health trust services. Information about each site is given in Table 2 below.
To inform case selection for the comparative analysis we charted level of engagement at each site – percentage of trial participants offered peer support who had at least two contacts with their PW, at least one of which was post-discharge – against site fidelity score, measured using an index designed to assess fidelity of delivery of peer support at site level against a set of principles articulating what is distinctive about peer support compared to other forms of mental health support [ 31 ] (Fig. 1 ). Fidelity was assessed through a semi-structured interview with PWs, the people they supported and their supervisor, rated by researchers against criteria based on the principles framework. A high fidelity score indicates that peer support had been implemented according to those principles. Fidelity was assessed after peer support had been delivered for at least six months at each site.

Relationship between engagement with peer support and fidelity
Figure 1 is indicative of a direct relationship between engagement with peer support and fidelity, offering rationale for selecting sites with higher or lower levels of both engagement and fidelity as cases for comparative analysis. There was one outlier, site 2, where fidelity was high (11) but engagement was mid-range (51%). We included this site in the comparative analysis as engagement might be explained by implementation issues not related to fidelity of delivery.
We report on the Evidence domain of the framework in a paper describing how experiential knowledge was central to developing the ENRICH peer support intervention [ 32 ]. Our research questions here are based on the Context and Facilitation domains of the framework, with context referring largely to the NHS Trust in which implementation took place (question 1), and facilitators being the PWs and PWCs who delivered the peer support (questions 2–4):
How did the culture of organisations, leadership (including issues of access and authority ) and monitoring and feedback impact implementation of peer support?
How did PWs and PWCs feel that their roles were characterised?
How did PWs and PWCs feel they were able to exercise flexibility while remaining consistent in their approach to delivering peer support?
How did experiential knowledge underpin peer support as it was delivered at each site?
Data sources
Peer worker interviews. Thirty-two PWs delivered peer support in the ENRICH trial and were invited to give written informed consent to participate in the research. All 32 consented and were interviewed after 12 months of delivering peer support. Interviews explored how well training prepared them for the role, their experiences of working as a PW, the support they received in the role and their relationship with clinical teams they worked alongside.
Peer worker coordinator interviews. Eight PWCs supervised PWs in the trial. Seven PWCs were themselves experienced PWs and one was a mental health nurse who shared the role with an experienced PW. All 8 PWCs gave informed consent to participate in the research and were interviewed at the same timepoint as PWs. Interviews explored PWCs’ experiences of supporting PWs, how well they thought the role was supported and organisational issues impacting delivery of peer support.
Interviews were conducted by researchers working from a perspective of having experienced mental distress and/ or having used mental health services, and played a key role in schedule development. Interview schedules can be found in the Supplementary Material file.
Data analysis
Interviews were audio-recorded, pseudonymised at the point of collection and transcribed verbatim.
Interview data were analysed using a framework approach [ 33 ] based on the Context and Facilitation domains of the modified PARIHS framework (see Table 1 ). Data were first coded to the constructs within those domains, with inductive space retained to code factors not related to the framework that participants described as impacting delivery of peer support. Second, a comparative, cross-case analysis was used to look for patterns of implementation that were: A, shared across cases; B, characterised high fidelity-high engagement cases; C, characterised low fidelity-low engagement cases; D, described implementation in the outlier case [ 30 ]. Preliminary analyses were undertaken by the first author and refined through iterative rounds of discussion with the whole team.
Characteristics of included cases
The two high engagement-high fidelity cases (sites 3,5), and the outlier high fidelity-low engagement case (site 2), were in urban areas with PWs directly employed in mental health NHS Trusts (see Table 2 ). The two low engagement-low fidelity cases (sites 4,6) were in areas that were a mix of rural localities with small towns or urban localities respectively. In both the latter sites PWs were employed by voluntary sector organisations outside of the NHS.
Characteristics of participants
A total of 20 PWs were included in the analysis, five each from sites 3 and 4, three each from sites 2 and 5, and two from site 6. Twelve PWs were female, seven were male and one preferred not to say. Three PWs were aged under 35 years of age, 12 aged from 35 to 55 years, one over 55 and four preferred not to say. Eleven PWs were White British, two were White Irish, one White other, one Black/ Black British, one Asian/ Asian British, one Arab, one Mixed White Asian with two preferring not to say.
There were five PWCs, one from each site. Four PWCs were female and one was male; two were aged from 35 to 55 and three over 55; all were White British.
Participant quotes presented below are identified with a site code (e.g. S1 = site 1) and role identifier (PW = Peer Worker; PWC = Peer Worker Coordinator) plus an additional number to distinguish between PWs at each site.
Implementation across cases
A number of implementation features were evident across all five cases, including characterisation of the PW role as largely consistent with the principles that were used to inform development of the intervention; [ 27 , 32 ] taking a non-judgemental approach and sharing experiences to create a safe space, make connections and build relationships:
‘We’re not going to be judgemental so to speak. It’s a safe place really for people to be themselves regardless of what their mental health issues are or mental health diagnoses are.’ (S5PW2). ‘I’m always sharing lived experience, whether that’s just generally or whether that’s personally with mental health … obviously you share when appropriate but you try to match that experience together so you have something in common, and then there is that mutuality and reciprocity and creating that trusting relationship.’ (S3PW3).
On the whole, training – as specified in the ENRICH manual – was consistently delivered and worked well to provide PWs with the range of skills they felt they needed for the role:
‘We did a lot about strengths-based approaches and I think that’s really informed the way that I interact with people, so I think I’m always trying to bring it back to what can you do, what is strong for you … we did a lot about active listening and also about discussing difficult issues … I think it’s been very helpful the stuff we did in training … definitely the boundaries and relationships sessions that we did …’ (S3PW1).
The importance of group supervision facilitated by the PWC, as well as individual supervision where required (both specified in the handbook), was indicated across sites, providing the opportunity for PWs to share experiences and receive feedback from one another as well as from the PWC:
‘I will hold these feelings until supervision and that’s when I let it out, offload it to my colleagues. And it’s been great because we’ve been bouncing it off each other and I’ve noticed that it’s not just me that was going through it, so it’s such a relief …’ (S2PW2). ‘… [PWC] will always ask how I am, if anything has triggered me or anything like that and she’s quite easy to talk to and it’s OK to be open with her.’ (S6PW3).
Participants in all sites described differences between the culture of clinical services in the host trust and the ethos underpinning peer support:
‘…it’s about the values because what I find with the other types of support, it all tends to be clinical and deficits based … very directive and judgemental … some of the clinical teams are stuck in that way of seeing things, that deficit-based thing and they don’t really know too much about peer support.’ (S5PW1).
At all sites, there was a perceived lack of contact with, and feedback from, community mental health teams, sometimes accompanied by a lack of understanding of the PW role:
‘Whenever I got a new service user, I’d email their [Community Psychiatric Nurse] or care coordinator … to give them more information about it and nobody, apart from I think one person, got back to me. So that’s been quite challenging, not really having any communication or contact really with the mental health teams that are working with the service users …’ (S5PW3).
Interviewees in all sites remarked that the timing of the offer of peer support - prior to discharge from hospital - was particularly challenging for some, especially in relation to maintaining contact with the PW following discharge. This represented a barrier to engagement that was related to the clinical context, rather than implementation:
‘… they are being introduced to it as soon as they come out … they are going through a tough period of fear, of not knowing what’s next for them. The last thing they want is to commit to 16 weeks of meeting someone that they don’t even know.’ (S2PW2). ‘I suspect that the post-discharge needs more targeting, that would be my sense. There are people who really get so much out of it, but then there are an awful lot who just disengage. It’s another stress for them I think.’ (S4PWC).
Implementation in high fidelity-high engagement cases
There was evidence of features supporting implementation in the high fidelity-engagement cases which contrasted with low fidelity-lowengagement cases (see below). In high fidelity cases, cultural differences between clinical services and peer support were generally seen as an asset and were valued, rather than as a source of tension:
‘… you need a values-based practice and how important it is, as opposed to the clinical based practice and how helpful that is … I’m not saying the clinical approach is wrong or anything like that, what I’m saying is we need to complement each other, we need to take a holistic approach.’ (S5PW1).
Some aspects of organisational culture were seen as supportive of peer support, including the role of recovery colleges in preparing PWs for the role or providing additional training once in post (recovery colleges employ an adult education model to supporting people with their mental health, often co-delivered by people using mental health services [ 34 ]):
‘… we were in a really fortunate position being linked with a Recovery College, that, where later in their work they then wanted to do specific recovery focused training around diagnosis we were able to provide that for people.’ (S3PWC).
In these cases, staff on the wards (inpatient units) were reported as largely familiar with and valuing the role of peer support:
‘… when I’d go on the ward … they seemed to see great value in the transparency of people being there because they’ve got lived experience. That aspect of it was really nice … good for the culture of the organisation in many ways.’ (S5PWC). ‘… the clinical teams are aware … they’re very excited that we’ve got peer workers on the ward. They’re very positive about it.’ (S3PW3).
PWCs described PW recruitment as having followed the process specified in the intervention handbook, and as such the PWs who were appointed were well equipped to deliver the role:
‘… we had the right people to execute these roles effectively really … we had quite a diverse selection panel … we had the right people that expressed the interest I think …’ (S5PWC).
There was evidence that PWs and PWCs – as intervention facilitators - had worked hard in delivering clinical team preparation sessions, as specified in the handbook, offering repeat sessions where necessary, and that this had supported a good relationship with ward teams:
‘… [in] the early days we went in to talk about ENRICH and then if they’d had significant staff turnover, which is really happening a lot … we’d then go back to the teams just so that they were aware of what ENRICH was about, what their role was … it certainly meant that staff were much more welcoming of the ENRICH peer workers when they came onto the wards.’ (S3PWC).
PWCs reported being well resourced in their leadership role, both in terms of having sufficient time to do the work and having sufficient supervision themselves around any difficult issues that might arise:
‘… [my role] was two days a week and that was plenty of time…’ (S3PWC). ‘I have had unconditional support from my manager … it’s been part of my regular monthly supervision … any kind of difficulties I’ve had or frustrations or whatever that has come up, that has been an ideal time to go through it. But I’ve also been supported to discuss things as and when they come up …’ (S5PWC).
In these sites, there was evidence that delivery of peer support was highly consistent with the manual. There was notable emphasis on flexible application of peer support, especially around pacing support in response to the individual’s needs, spending as much time as necessary alongside the participant to build a trusting relationship:
‘… it doesn’t necessarily follow a linear path a lot of the time. Sometimes, somebody might be having a really bad week and they actually want you to listen to what’s been going on for them … at the beginning, because you are getting to know the person as well, I think the kind of conversation you’d have is a bit more general … and then it might actually take a completely different path however many meetings down the line and they’ll actually go … “I haven’t told anyone about a particular issue, but I want to talk it through with you and see what you think”.’ (S3PW1).
PWs at these sites demonstrated confidence in taking a lead from the person they were supporting, consistent with the principles of choice and control that underpinned the intervention:
‘… I’m kind of getting to know things that they’re interested in and this is influencing where I signpost them to … it’s just about giving them the option and then they can make their own decision then whether they want to go, and again that’s putting them back in control, which is all about helping people to recover really and take control back of their lives.’ (S5PW2).
PWs also described learning from the people they were supporting, and the importance of validating their experiences, consistent with the principle of reciprocity in the underpinning framework:
‘There are people who I’m supporting who … realise that the medication is very important to them and that they will probably always be on it. So, I gain insight from that, just because maybe I found that medication in my own lived experience wasn’t particularly fantastic but for others it’s very important. So, you learn from other things … you’ve got to validate their experience because … they know what works for them and you can’t tell somebody else what will work for them …’ (S5PW1).
Implementation in low fidelity-low engagement cases
There was evidence of barriers to implementation in low fidelity-lowengagement cases. In both, PWs were employed in not-for-profit organisations, resulting in organisational context-related barriers to implementation. Resource issues impacted leadership of the intervention with, in one site, the organisation not having capacity to provide cover or suitable supervision for the PWC:
‘… we’ve had different staff line managing me over the past year because of maternity. But to be fair none of them really knew about ENRICH … there was nobody who could have covered my role here … it’s felt like a bit of pressure to continue doing it because I took a bit of time off … I couldn’t physically go out and do anything when I wasn’t well …’ (S6PWC).
Support for PWCs at these sites, including an Action Learning Set with other PWCs, was difficult to access because of lack of sufficient funding to travel to meetings:
‘I think the action learning sets worked really well … maybe they should have been planned for a bit more financially … because ultimately we had to go back to our Trust and say we need to find more money or I’m not going.’ (S4PWC).
Being outside of the NHS also created issues of access and authority for PWCs:
‘I would have thought there should be regular team meetings, but we never seemed to be able to get in on them … an additional disadvantage from being an organisation outside of the Trust …’ (S4PWC). ‘… it’s been difficult with the [NHS Trust], some of the staff there … I don’t want to say too much, but that’s been difficult.’ (S6PWC).
This extended to PWs being able to communicate with clinical teams about the people using:
‘A few times they didn’t want to talk to me because I didn’t have enough information for them … to establish who I was … I just wanted to know whether they were seeing [participant] or whether they’d stopped seeing him, and they wouldn’t tell me.’ (S4PW3).
At these sites there was, generally, a challenging relationship with ward-based clinical staff, potentially impacting on the initial relationship building phase of the peer support:
‘There were certainly, on that site, a lot of suspicious looks and “what on earth is this all about” type conversations. However much we tried to prepare the staff team, and we’d gone in and visited and talked to them all, but there was still that “what’s this all about”? People didn’t get it straight off.’ (S4PWC).
Cultural differences with the host NHS Trust were keenly felt by PWs employed in not-for-profit organisations:
‘… the ward environment is, well obviously it’s clinical. It sometimes feels some staff, but not all staff, who work on the wards are not really sure what my role is or have a vague understanding. There’s perhaps a little bit of a difference in terms of pecking order and me in the pecking order.’ (S6PW2). ‘… they will be looking at the patient’s files … they can build up a judgement before seeing you … when the patient sees the peer support worker they might talk to us because we’re non-judgemental, we don’t feedback unless there is a safeguarding issue or danger to themselves or others … I don’t think peers should be seeing files …’ (S4PW44).
Both sites also combined rural localities with urban areas, with issues of geography hindering timely delivery of peer support at remote hospital sites:
‘… the geography issue was a great challenge in itself in our area because I was one bit of the triangle and the [hospitals] were in two different places … I’d have had an hour or so travelling and then get there and “oh, they’re on leave until 10pm tonight”.’ (S4PWC).
Geography could also impact on building a strong sense of PW team:
‘I did lots of talking to [the PWC] but not so much my fellow peers. There was one fellow peer that I talk quite a lot to … the other two were very close to each other and so they were almost functioning as one … I got on OK with the people at [the other town] … it’s just that we had differences of opinion.’ (S4PW3).
There was some inconsistent delivery of training, with one PW reporting having received a truncated version of the training programme as a result of capacity issues:
‘I didn’t actually do [the full training] … because I was covering a maternity leave it was the girl did all the training. So, I basically had a morning with the coordinator where we went through the whole bumph together … ’ (S6PW3).
While the importance of group supervision was acknowledged in these sites, there was disruption leading to inconsistency with the pattern of weekly group supervision as a result geography in one site, and capacity in the other:
‘We don’t generally do weekly anymore … generally we do monthly although I check in by phone with them.’ (S4PWC). ‘… a lot of the supervision has ended up being one-to-one just because it’s a small team here … sometimes I would be able to meet with them together but often because my day, I’ve only got one a day week, I’d have to fit them in if one of them couldn’t do it that day …’ (S6PWC).
Possibly as a result of disruption to supervision or opportunities to support each other as a team, PWs at these sites at times appeared to lack confidence in delivering peer support:
‘… it made me feel that I was getting it all wrong … she didn’t really talk at all about, and I felt that I couldn’t, I just felt that I had to wait for her to give information to me … because that’s what I understood you are supposed to do, is wait for them to give you information to talk about their problems …’ (S4PW3). ‘… I’m imagining it’s going to be quite hard for a long time because the expression that I’ve used that comes to mind is pulling teeth. It’s going to be probably like that every time we meet … it is frustrating because you want to help them.’ (S6PW2).
Implementation in the outlier high fidelity-low engagement case
The outlier case shared contrasting sets of features with the other cases. Like high fidelity and engagement sites, the outlier case reported feedback from management describing a positive impact of peer support on culture in the NHS trust:
‘… within senior management they’ve seen the power of peer working and they really like it … we’re in discussions on when ENRICH finishes, that we’re going to have a number of peer workers within teams, exactly to try and change the nature and change the culture …’ (S2PWC).
PWs in this site also demonstrated a more confident, patient approach to relationship building:
‘… trying to build that friendly rapport, getting them to trust you, showing them that you understand them in a way … creating that safe space environment for them to be able to talk about how they are feeling or what’s going on for them … just finding out what they want to do for themselves not someone else telling them what to do … ’ (S2PW0).
However, as in the two low fidelity-low engagement cases, in the outlier site barriers to implementation included a challenging relationship with ward staff:
‘… [I feel] looked down upon sometimes, “oh, you’re just a peer support worker” … it’s the environment. The days that I do go for ward meetings are usually the days I need a long break, I’ll be honest with you …’ (S2PW2).
In this site there was also disruption to group supervision, with some PWs needing considerable additional support from the PWC and a challenging team dynamic emerging:
‘I was definitely doing weekly one-to-one supervisions with the peer workers when they first started … it kind of came apparent that it was what people needed … for me it didn’t work very well, I was exhausted … people want one-to-one sessions to talk about colleagues and issues they are having with their colleagues … I think there are two other peer workers who are less, they don’t see themselves as much as part of the team.’ (S2PWC).
The PWC indicated that they would have benefitted from additional support for their role:
‘I feel like we could have done more support around, more training kind of stuff on managing people with lived experience … … maybe one thing would have been more meetings with other peer worker coordinators and just see how other people are doing it … more guidance on what group supervision actually was … ’ (S2PWC).
This study used a qualitative, comparative case study design to explore how implementation of a peer support intervention might be associated with engagement with peer support and, as indicated in results elsewhere, [ 26 ] with outcomes. We noted clear differences related to organisational context between high fidelity-high engagement cases and low fidelity-low engagement cases. Lack of a positive working relationship between PW and ward (inpatient) clinical teams, exacerbated by lack of awareness of the potential role of peer support, is likely to be crucial to engagement where people begin peer support in hospital. Levels of engagement were highest in cases where those relationships were reported as largely positive and where differences in approach (between clinical practice and peer support) were highly valued [ 6 , 35 ].
We note that the two low fidelity-low engagement sites employed PWs in the not-for-profit sector rather than within the NHS. Elsewhere, research has indicated that the principles underpinning peer support might be better maintained within peer-led or not-for-profit organisations, [ 7 ] and that doing so might provide an opportunity to bring a change of culture into statutory services [ 35 ]. However, we observed constraints on resourcing for leadership roles, and lack of access and authority for managers in the not-for-profit sector, compounded, perhaps coincidentally, by the additional challenges of geography. Neither did we observe, in those sites, evidence of leadership for peer support from within the host NHS organisation that might have facilitated better implementation [ 36 ]. In our outlier high fidelity-low engagement case, resourcing for leadership also impacted support for PWs. Proper resourcing for PWCs has been identified elsewhere as crucial to providing good peer support [ 5 , 37 ]. PWCs at sites that struggled with levels of engagement identified the need for a wider network of mutual support beyond their immediate organisation, with work elsewhere highlighting the need to develop communities of practice around lived experience leadership roles in mental health services [ 38 , 39 ]. As such, our findings reinforce the link that has been observed elsewhere between leadership in implementation, and the outcomes of a newly implemented intervention [ 40 ].
At the two high engagement-high fidelity sites, PWCs noted that robust recruitment processes resulted in a PW team that were well equipped to deliver what was a challenging role. An experience of the PW team as mutually supportive, complemented with group supervision led by a PWC bringing experiential knowledge to their role, was identified as important at all five sites included in our analysis, as it is in the wider literature [ 2 , 5 ]. The PW training programme was equally valued across all sites with PWs indicating that it prepared them well for their roles. Again, the importance of training that is specifically tailored to peer support having been widely noted [ 3 , 4 ]. In sites where there were inconsistencies in delivery of supervision and training, this appeared to impact confidence among PWs in offering peer support that reflected the underpinning principles framework. Sites with high fidelity scores were indicative of a clear focus on relationship and trust building, characterised by spending time alongside the individual offered peer support, learning from them, before taking their lead in exploring new possibilities. These values have been identified as fundamental to peer support, [ 41 ] and our own analysis of data from the trial indicated that relationship building at the beginning of the peer support was predictive of ongoing engagement [ 42 ].
It is worth noting here that not all challenges to engaging people with the peer support were attributable to implementation issues. Across sites, interviewees felt that discharge from hospital was a challenging time for some people to consider taking up peer support. Other trials of peer support for discharge have also struggled in this respect, [ 43 ] especially where participants were those with a higher level of need (people with multiple admissions) as they were in our study [ 15 ].
Strengths and limitations
We employed a robust, theoretically informed comparative case study design, with case selection determined by a priori measures of fidelity [ 31 ] and engagement [ 26 ] made independently of this analysis. We analysed a complete data set – interviews of PWs and PWCs – in all sites included in the analysis, although we might usefully have also interviewed NHS clinicians and managers as they also played a role in implementation. Analysis of in-depth interviews exploring the experiences of people offered peer support will be reported elsewhere. Our original interview schedules were not directly informed by the PAHRIS framework [ 22 ] and so may not have elicited a full range of data relating to implementation variables. Other frameworks might have been indicative of different barriers and facilitators of successful implementation. Nevertheless, we note the work adapting the PAHRIS framework to elucidate the role of experiential knowledge in implementation was particularly suited to a study of peer support and informed by lived experience on the research team [ 25 ].
Implications for policy, practice and research
Mental health workforce policy in England, as elsewhere, is encouraging employment of large numbers of PWs into mental health services.[ 44 ]. A range of training programmes have emerged [ 45 ] that, to some degree, share a set of principles similar to those that informed ENRICH. This study suggests that specific supports for PWs need to be properly resourced as integral to the offer of peer support in mental health services. These include supervision from an experienced PW, opportunities for group supervision, and an emphasis on relationship building in PW training that is consistent with a principles-based peer support framework. While it has been suggested that peer support can drive cultural change in mental health provider organisations, [ 46 ] our research suggests that lack of supportive culture can constrain delivery. Peer leadership, provided with sufficient support and authority, is needed to support change work with clinical teams, in hospital and in the community, so that peer support and clinical care are part of a complementary offer.
This study identifies policy and practice implications when peers are employed through not-for-profit organisations to work in partnership with public mental health providers. Research elsewhere highlights the potential challenges and opportunities of this ‘hybrid’ approach, [ 35 , 47 ] indicating a need for strategies that effectively align implementation expectations between the not-for-profit organisation and the mental health provider.
Further research to develop and evaluate the introduction of peer support in mental health might usefully be informed by a change model that incorporates this range of implementation variables to optimise delivery of peer support. We also note that in our study, PWs were employed to, and supervised within a dedicated PW team that provided peer support across several clinical teams, while in many mental health services internationally PWs are employed as embedded members of multi-disciplinary clinical teams. There is a need for research that considers the implications for implementation and outcome of these contrasting organisational configurations.
This study provides clear indication that implementation issues can impact delivery of peer support, with implications for engagement and, potentially, outcomes. Resourcing can impact consistency of delivery, alongside challenges of access, authority and relationship with clinical teams, especially where PWs are employed outside of the mental health service. Attention needs to be paid to the impact of geography on implementation.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Mirbahaeddin E, Chreim S. A narrative review of factors influencing peer support role implementation in mental health systems: implications for research, policy and practice. Adm Policy Ment Health Ment Health Serv Res. 2022;11:1–7.
Google Scholar
Gillard S, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res. 2013;13(1):1–3.
Article Google Scholar
Simpson A, Quigley J, Henry SJ, Hall C. Evaluating the selection, training, and support of peer support workers in the United Kingdom. J Psychosoc Nurs Ment Health Serv. 2014;52(1):31–40.
Article PubMed Google Scholar
Tse S, Tsoi EW, Wong S, Kan A, Kwok CF. Training of mental health peer support workers in a non-western high-income city: preliminary evaluation and experience. Int J Soc Psychiatry. 2014;60(3):211–8.
Forbes J, Pratt C, Cronise R. Experiences of peer support specialists supervised by nonpeer supervisors. Psychiatr Rehabil J. 2022;45(1):54.
Oborn E, Barrett M, Gibson S, Gillard S. Knowledge and expertise in care practices: the role of the peer worker in mental health teams. Sociol Health Illn. 2019;41(7):1305–22.
Stewart S, Watson S, Montague R, Stevenson C. Set up to fail? Consumer participation in the mental health service system. Australasian Psychiatry. 2008;16(5):348–53.
Otte I, Werning A, Nossek A, Vollmann J, Juckel G, Gather J. Challenges faced by peer support workers during the integration into hospital-based mental health-care teams: results from a qualitative interview study. Int J Soc Psychiatry. 2020;66(3):263–9.
Voronka J. The mental health peer worker as informant: performing authenticity and the paradoxes of passing. Disabil Soc. 2019;34(4):564–82.
Simpson A, Oster C, Muir-Cochrane E. Liminality in the occupational identity of mental health peer support workers: a qualitative study. Int J Ment Health Nurs. 2018;27(2):662–71.
Adams WE. Unintended consequences of institutionalizing peer support work in mental healthcare. Soc Sci Med. 2020;262:113249.
Mahlke CI, Priebe S, Heumann K, Daubmann A, Wegscheider K, Bock T. Effectiveness of one-to-one peer support for patients with severe mental illness - a randomised controlled trial. Eur Psychiatry. 2016;42:103–10.
Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet. 2018;392(10145):409–18.
Article PubMed PubMed Central Google Scholar
Chinman M, Oberman RS, Hanusa BH, Cohen AN, Salyers MP, Twamley EW, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the veterans health administration. J Behav Health Serv Res. 2013;42(1):109–21.
Rogers ES, Maru M, Johnson G, Cohee J, Hinkel J, Hashemi L. A randomized trial of individual peer support for adults with psychiatric disabilities undergoing civil commitment. Psychiatr Rehabil J. 2016;39(3):248–55.
Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev. 2013;3:CD004807.
King AJ, Simmons MB. A systematic review of the attributes and outcomes of peer work and guidelines for reporting studies of peer interventions. Psychiatr Serv. 2018;69(9):961–77.
Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry. 2014;14:39.
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, Sin J, Gillard S. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):1–20.
Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, Benrimoj SI. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Syst. 2015;13(1):1–1.
Bertram RM, Blase KA, Fixsen DL. Improving programs and outcomes: implementation frameworks and organization change. Res Social Work Pract. 2015;25(4):477–87.
Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. BMJ Qual Saf. 1998;7(3):149–58.
Article CAS Google Scholar
Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ. 2015;350.
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sector Manag. 2016;29(1):72–90.
Gillard S, Foster R, Papoulias C. Patient and public involvement and the implementation of research into practice. J Mental Health Train Educ Pract. 2016;11(4):256–67.
Gillard S, Bremner S, Patel A, Goldsmith L, Marks J, Foster R, Morshead R, White S, Gibson SL, Healey A, Lucock M. Peer support for discharge from inpatient mental health care versus care as usual in England (ENRICH): a parallel, two-group, individually randomised controlled trial. Lancet Psychiatry. 2022;9(2):125–36.
Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Mental Health Social Inclusion. 2017;21(3):133–43.
Gillard S, Bremner S, Foster R, Gibson SL, Goldsmith L, Healey A, Lucock M, Marks J, Morshead R, Patel A, Priebe S. Peer support for discharge from inpatient to community mental health services: study protocol clinical trial (SPIRIT compliant). Medicine. 2020;99(10).
Berg-Schlosser D, De Meur G, Ragin C, Rihoux B. (2008). Qualitative comparative analysis (QCA) as an approach. Pp 1–18 in Rihoux, B., & Ragin, C. Configurational comparative methods: Qualitative comparative analysis (QCA) and related techniques. Thousand Oaks, CA; Sage.
Yin RK. Case study research: design and methods. Thousand Oaks, CA: Sage; 2009.
Gillard S, Banach N, Barlow E, Byrne J, Foster R, Goldsmith L, Marks J, McWilliam C, Morshead R, Stepanian K, Turner R. Developing and testing a principle-based fidelity index for peer support in mental health services. Soc Psychiatry Psychiatr Epidemiol. 2021 Oct;1:1–9.
Marks J, Foster R, Gibson SL, Simpson A, Rinaldi M, Repper J, Worner J, Patel S, Lucock M, Ussher M, White S. Development of a peer support intervention to improve the experience and outcomes of discharge from inpatient mental health care: the role of experiential knowledge in a coproduced approach. BMC Res Notes. 2021;14(1):1–0.
Ritchie J, Spencer L. Qualitative data analysis for applied policy research. Analyzing qualitative data. Routledge; 2002. pp. 173–94.
Whitley R, Shepherd G, Slade M. Recovery colleges as a mental health innovation. World Psychiatry. 2019;18(2):141.
Gillard S, Holley J, Gibson S, Larsen J, Lucock M, Oborn E, Rinaldi M, Stamou E. Introducing new peer worker roles into mental health services in England: comparative case study research across a range of organisational contexts. Adm Policy Mental Health Mental Health Serv Res. 2015;42:682–94.
World Health Organisation. World Mental Health Report: transforming Mental Health for all. Geneva: World Health Organisation; 2022.
Grim K, Bergmark M, Argentzell E, Rosenberg D. Managing peer support workers in Swedish mental health services—A leadership perspective on implementation and sustainability. J Psychosocial Rehabilitation Mental Health. 2023;10(3):313–29.
Byrne L, Stratford A, Davidson L. The global need for lived experience leadership. Psychiatr Rehabil J. 2018;41(1):76.
Loughhead M, Hodges E, McIntyre H, Procter NG, Barbara A, Bickley B, Harris G, Huber L, Martinez L. A model of lived experience leadership for transformative systems change: activating lived Experience Leadership (ALEL) project. Leadersh Health Serv. 2023;36(1):9–23.
Egeland KM, Borge RH, Peters N, Bækkelund H, Braathu N, Sklar M, Aarons GA, Skar AM. Individual-level associations between implementation leadership, climate, and anticipated outcomes: a time-lagged mediation analysis. Implement Sci Commun. 2023;4(1):75.
Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. 2001;25(2):134.
Article CAS PubMed Google Scholar
White S, Bhattacharya R, Bremner S, Faulkner A, Foster R, Gibson S, Goldsmith L, Harnett D, Lucock M, Patel A, Priebe S. Predictors of engagement with peer support: analysis of data from a randomised controlled trial of one-to-one peer support for discharge from inpatient psychiatric care. Int J Soc Psychiatry. 2023;69(4):994–1003.
Simpson A, Flood C, Rowe J, Quigley J, Henry S, Hall C, Evans R, Sherman P, Bowers L. Results of a pilot randomised controlled trial to measure the clinical and cost effectiveness of peer support in increasing hope and quality of life in mental health patients discharged from hospital in the UK. BMC Psychiatry. 2014;14(1):1–4.
Health Education England. NHS Mental Health Implementation Plan 2019/20–2023/24. July 2019.
Bradstreet S, Buelo A. lmROC peer support theory and practice training: an independent evaluation. Matter of Focus: Edinburgh; 2023.
Berry C, Hayward MI, Chandler R. Another rather than other: experiences of peer support specialist workers and their managers working in mental health services. J Public Mental Health. 2011;10(4):238–49.
Jones N, Teague GB, Wolf J, Rosen C. Organizational climate and support among peer specialists working in peer-run, hybrid and conventional mental health settings. Adm Policy Mental Health Mental Health Serv Res. 2020;47:150–67.
Download references
This study was funded by the UK National Institute for Health Research (NIHR), Programme Grants for Applied Research funding programme (grant number RP-PG-1212-20019). This paper presents independent research funded by NIHR. The views expressed are those of the authors and not necessarily those of the UK National Health Service (NHS), the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
City, University of London, London, UK
Steve Gillard, Rhiannon Foster & Anthony Salla
St George’s, University of London, London, UK
Sarah White
East London NHS Foundation Trust, London, UK
Rahul Bhattacharya, Paul Binfield & Daniella Harnett
South London & Maudsley NHS Foundation Trust, London, UK
Rachel Eborall
Kingston University, Kingston, UK
Sarah L Gibson
King’s College London, London, UK
Alan Simpson
University of Huddersfield, Huddersfield, UK
Mike Lucock
Kingston Hospital, Kingston, UK
Jacqueline Marks
Implementing Recovery through Organisational Change, Nottingham, UK
Julie Repper
South West London & St George’s Mental Health NHS Trust, London, UK
Miles Rinaldi
Nordland Hospital Trust, Bodø, Norway
Independent Researcher, London, UK
Jessica Worner
You can also search for this author in PubMed Google Scholar
Contributions
SG, SW, SLG, AlS, ML, JR, MR and JW contributed to the conception of the original study. SG, RF, SW, RB, PB, RE, DH, AlS and AnS contributed to the design of the work reported here. SG, RF, SW, RB, RE, AlS, ML, JR, MR and JW contributed to interpretation of the data. SG, RF, SW and JM contributed to the acquisition and analysis of data. SG, RF and SW drafted and substantively revised the work. All authors approved the submitted version of the study.
Corresponding author
Correspondence to Steve Gillard .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was granted by the UK National Research Ethics Service, Research Ethics Committee London - London Bridge on 10 May 2016, reference number 16/LO/0470. Written, informed consent was given by all research participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Gillard, S., Foster, R., White, S. et al. Implementing peer support into practice in mental health services: a qualitative comparative case study. BMC Health Serv Res 24 , 1050 (2024). https://doi.org/10.1186/s12913-024-11447-5
Download citation
Received : 24 May 2024
Accepted : 16 August 2024
Published : 11 September 2024
DOI : https://doi.org/10.1186/s12913-024-11447-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Mental health services
- Lived experience
- Role adoption
- Implementation
- Comparative case study methods.
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Qualitative methods offer an effective way of involving service-users in developing interventions for mental health problems 5 ensuring that the questions asked are meaningful to individuals. This may be particularly beneficial if participants are stakeholders, for example potential users of a new service.
Qualitative methods are also used in combination with quantitative methods in mixed method designs for convergence, complementarity, expansion, development, and sampling. Rigorously applied qualitative methods offer great potential in contributing to the scientific foundation of mental health services research.
Qualitative Research Methods in Mental Health is a valuable resource for researchers, professors, and graduate students as well as therapists and other professionals in clinical and counseling psychology, psychotherapy, social work, and family therapy as well as all interrelated psychology and medical disciplines.
1 Introduction. Qualitative research has played a vital role in the mental health field. From its roots in descriptive case studies to current contributions in program evaluation, policy development, and social action, qualitative research has helped shape our understanding of and responses to mental health and mental illness.
This book provides a user-friendly introduction to the qualitative methods most commonly used in the mental health and psychotherapy arena. Chapters are written by leading researchers and the editors are experienced qualitative researchers, clinical trainers, and mental health practitioners Provides chapter-by-chapter guidance on conducting a qualitative study from across a range of approaches ...
The greatest strength of the qualitative research approach lies in the richness and depth of the healthcare exploration and description it makes. In health research, these methods are considered as the most humanistic and person-centered way of discovering and uncovering thoughts and actions of human beings. Table 1.
The theme also addresses methodological considerations for using qualitative methods in mental health research. The key emerging issues are discussed below: Considering qualitative components in conducting mental health research. Six studies recommended the use of qualitative methods in mental health research [19, 26, 28, 32, 36, 44].
Generated through interviews, observation of naturally occurring phenomenon, focus groups, document analysis. Data are rich and involve few participants. Inductive, i.e. data driven. Findings are exploratory and form hypotheses and theory Findings supported by evidence of textual, pictorial or narrative data.
Qualitative Research*. As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions p ….
Qualitative Research Methods in Mental Health Innovative and Collaborative Approaches. Editors Maria Borcsa Institute of Social Medicine Rehabilitation Sciences and Healthcare Research University of Applied Sciences Nordhausen Nordhausen, Germany Carla Willig Department of Psychology
A Professor Emeritus of Psychology at the University of Toledo (Ohio), he is co-author of four books, including Learning Process-Experiential Psychotherapy (2004), and Research Methods in Clinical Psychology (2002), as well as more than 120 journal articles and book chapters.
What Approach is Taken to the Involvement of Research Participants, Including Mental Health Service Users? How to Use This Method. What Makes for a Better Quality Thematic Analysis? What are the Recent Developments and Innovations Concerning this Method? Conclusions. Acknowledgements. References
Qualitative research in mental health usually relies on either 1) a series of in-depth interviews with individuals from a group of interest, e.g. immigrants with a mental illness who have dropped out of psychiatric treatment (Whitley, et al., 2006a; 2006b; 2007); 2) a series of focus groups held with different stakeholders on a topic of ...
to invest more in the promotion of mental health of individuals and societies, and to develop effective ways of prevention, support, care and recovery in the field of mental health. There seems to be a broad consensus regarding this part of the new discourse about mental health as an emerging priority. This is, actually, an easier part of the ...
stood. This paper presents a scoping review of mental health research using QDMs. This review aims to find out how QDMs are used in mental health research, the key benefits and challenges, and to provide an overview of decisions involv. nning and conducting a qualitative diary study in mental health research.MethodsA scoping review was chosen ...
Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practitioners Edited by David Harper & Andrew R. Thompson. Wiley-Blackwell. 2011. £29.99 (pb). 272 pp. ISBN: 978-0470663707 - Volume 200 Issue 5
The objective of this paper is to describe two methods of qualitative analysis - thematic analysis and content analysis - and to examine their use in a mental health context. Method: A description of the processes of thematic analysis and content analysis is provided.
The number of published mental health services research studies with mixed-methods designs increased by 67% between 2005 and 2006, by 80% between 2006 and 2007, and by 155% between 2007 and 2008. Furthermore, 21 of the 50 published studies (42%) that we reviewed appeared in journals with 2008 IFs of 2.0 or higher, including ten articles ...
• Health care professionals. Qualitative Research Methods in Mental Health is a valuable resource for researchers, professors, and graduate students as well as therapists and other professionals in clinical and counseling psychology, psychotherapy, social work, and family therapy as well as all interrelated psychology and medical disciplines.
1 Qualitative Research Part 3: Publication. The first two papers in this series on qualitative research for mental health nursing explored the basics of qualitative research—methodologies and methods. This paper will explore how your research can be transformed into a publication. There is an art in reducing that work into a succinct research ...
Peer workers are people with personal experience of mental distress, employed within mental health services to support others with similar experiences. Research has identified a range of factors that might facilitate or hinder the introduction of new peer worker roles into mental health services. While there is mixed evidence for the effectiveness of peer worker delivered interventions, there ...
This study explored the impact of work and coping factors affecting truck driver mental health in Australia. Themes described the importance of connections and coping methods drivers had to support their health. Many factors that compromised their health were often outside their control. These resul …
A mixed-methods approach was employed involving three work packages: (I) an evidence review of a cohort of 97 recently published randomised controlled trials/feasibility or pilot studies in mental health to assess the impact of online versus offline recruitment; (II) a qualitative study investigating the experiences of n = 23 key stakeholders ...
In 2014, the National Mental Health Commission (NMHC) argued that increased focus and funding addressing mild to moderate mental ill-health could assist in early intervention and treatment to ensure individuals had earlier access to support, rather than having to wait for their mental health to worsen to receive adequate assistance (NMHC, Citation 2014).
Introduction: A lack of research investigating the specific role that various observational techniques may have in shaping the therapeutic relations in mental health care during seclusion warranted this study. Aim: The aim of the study was to explore patients' experience of different methods of observation used while the patient was in seclusion. Method: A retrospective phenomenological ...
Developing a Research Question. Qualitative Methods and Their Assumptions. What is Epistemology and Why Does it Matter? References. References & (). & ... Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practitioners. References; Related; Information; Close Figure Viewer.
Characteristics of the studies. From the 17 included studies, four used thematic analysis, two in a qualitative study [25, 26] and two within a mixed methods secondary analysis of existing data [27, 28].Six studies used phenomenological methods [29,30,31,32,33,34], two used an ethnographic approach [35, 36] and three undertook a Grounded Theory approach [37,38,39].
Background: Telemedicine-based interventions show promise in addressing mental health issues among rural populations, yet evidence regarding their impact among the health care workforce in these contexts remains limited. Objective: This study aimed to evaluate the characteristics and the responses and perceptions of recently graduated physicians who work in rural areas of Peru as part of the ...
Methods. This was a qualitative comparative case study using data from interviews with 20 peer workers and their five supervisors. Peer workers delivered peer support for discharge from inpatient to community mental health care as part of a randomised controlled trial. ... Implications for policy, practice and research. Mental health workforce ...