You are using an outdated browser. Please upgrade your browser to improve your experience and security.

Henning Tiemeier, MD, PhD
Professor of Social and Behavioral Science
Research Roles/Affiliations
Sumner and Esther Feldberg Chair in Maternal and Child Health at HSPH
Director of the Harvard Center of Excellence in Maternal and Child Health
Lead of the Population Neuroscience group at the Harvard Chan School
Adjunct Professor of Psychiatric Epidemiology, Erasmus Medical Center, Rotterdam, Netherlands
Contact Information
Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health
677 Huntington Ave., 6th floor, Room 619, Boston, MA 02115
E-mail: [email protected]
Relevant Links
Harvard School of Public Health profile
Google Scholar
Tiemeier has worked broadly in psychiatric epidemiology for more than 20 years with a focus on child developmental research. Currently, he leads the Maternal and Child Center of Excellence at the Harvard T.H. Chan School of Public Health. He successfully managed a large research group with more than 20 persons at the Erasmus Medical Center in Rotterdam for several years, before being appointed Professor of Social and Behavioral Science at Harvard.
His research line evolved around two large population-based cohorts, the Rotterdam Study, an adult cohort, and Generation R, a pre-birth cohort. He planned, and now still conducts and supervises research in the domains of cognitive, emotional and behavioral development in the Generation R cohort.
His research is mostly aimed at understanding the etiology of common psychiatric problems and characterized by an interest in detailed phenotype assessment, neuroimaging, and genetics combined with modern quantitative and epidemiological methods. His child studies typically take a neurodevelopmental approach and, in particular, his work on prenatal exposures is internationally well-known. The work on intrauterine exposure to maternal hypothyroxinemia and neurodevelopment has influenced research, clinical practice and guidelines. This work documented the importance of a carefully regulated thyroid function of women in early pregnancy.
Tiemeier obtained substantial competitive funding which allowed him to perform home visits, detailed observational developmental assessments, and brain imaging in large groups and combine a developmental approach with a biological approach in a unique way. Under his supervision and, in close collaboration with Tonya White (now NIMH), he largely co-funded and led the data collection of more than 8,000 brain MRIs in children and pre-adolescents. While most of his work was observational, he has conducted randomized trials and was involved in guideline development.
He mentored and supervised students, postgraduates, post docs and assistant professors in diverse stages of their careers. In the Generation R Study , and now at Harvard Chan again, he established a Population Neuroscience group of post doc and PhD student researchers. Most of his work is collaborative, he (co) led several national and international consortia, including CHARGE-depression, CORNET, EAGLE-behaviour group and participated in the PGC depression working group. He is an experienced teacher of social, psychiatric, and general epidemiology at Harvard and internationally. At Harvard Chan he teaches 4 full credit courses, although some bi-annually, per year.
Research Interests
Child development in the general population
Epidemiology
Brain development in longitudinal studies
Population Neuroscience
Family context
Training Grant in Maternal and Child Health Source: Maternal and Child Health Bureau
The Training Program in Reproductive, Perinatal, and Pediatric Life Course Epidemiology NICHD T32 1T32HD104612
How we shape our children’s brains: From early adversity to adolescent depression Netherlands Organization for Scientific Research
SEED: - Social Inequality and its effects on child development: A study of birth cohorts in the UK, Germany and the Netherlands EU-NORFACE EraNet: Dynamics of Inequality Across the Life-course
Running in the Family – Understanding and Predicting the Intergenerational Transmission of Mental Health Horizon 101057529 - GAP-101057529 European Union
Citations per year
Duplicate citations, merged citations, add co-authors co-authors, cited by view all.
| All | Since 2019 | |
|---|---|---|
| 89478 | 56884 | |
| 154 | 111 | |
| 782 | 712 |
| 2018 | ||
| 2009 | ||
| 2016 | ||
| 2018 | ||
| 2016 | ||
| 2016 | ||
| 2010 | ||
| 2019 | ||
| 2017 | ||
| 2013 | ||
| 2016 | ||
| – and affect smoking behavior | 2010 | |
| 2016 | ||
| 2019 | ||
| 2021 | ||
| 2019 | ||
| 2012 | ||
| 2018 | ||
| 2002 | ||
| 2010 |

- About the Journal
- Role of Associate & Senior Editors
- Board Disclosures
- Supplemental Issues
- Advertising
- Recommend JAD
- Related IOS Press Journals
- Upcoming Meetings
- For Authors
- Submission Letter and Manuscript Transmission
- Manuscript Preparation
- Submission Checklist
- Permissions
- Review Process
- Publication Fee / Open Access Option
- Proofs/Reprints
- Financial Disclosure
- Open Access Mandates
- Preprints/Preprint Servers
- Policy on Use of Human Subjects
- Policy on Animal Use
- Policy on Ethics
- Current Issue
- All Issues (including upcoming)
- Articles in Pre-Press
- Letters to the Editor
- Rankings/Awards
- Journal of Alzheimer's Disease Reports
User Top Menu
- Welcome, Guest
- Information For Reviewers
- Pre-Press/Proofs
- Blog Guidelines
- Alzheimer Award
- Top 100 Most Cited AD Investigators
- Top 100 Most Prolific AD Investigators
- The Article
- Top 50 Results
You are here
2023 alzheimer award goes to henning tiemeier, md, phd, and rosanne freak-poli, phd, 10 july 2023.
This annual award recognizes outstanding contributions to the advancement of AD research published in the Journal of Alzheimer’s Disease
Amsterdam, the Netherlands – The Journal of Alzheimer’s Disease (JAD) is pleased to announce the joint recipients of the 2023 Alzheimer Award are Henning Tiemeier, MD, PhD, Erasmus Medical Center, Rotterdam, and the Harvard TH Chan School of Public Health, and Rosanne Freak-Poli, PhD, Monash University.
The 2023 winning paper presents important insights into the impact of poor social health, specifically loneliness, on cognitive decline and risk of dementia in older adults. The article is Freak-Poli R, Wagemaker N, Wang R, Lysen TS, Ikram MA, Vernooij MW, Dintica CS, Vernooij-Dassen M, Melis RJF, Laukka EJ, Fratiglioni L, Xu W, Tiemeier H. Loneliness, Not Social Support, Is Associated with Cognitive Decline and Dementia Across Two Longitudinal Population-Based Cohorts . J Alzheimers Dis. 2022;85(1):295-308, https://doi.org/10.3233/JAD-210330 . It is openly available to everyone to read, download, and share.
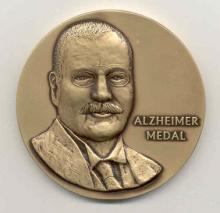
Each year, members of JAD’s extensive editorial board select the article published during the previous year that has had the most significant impact on Alzheimer’s disease (AD) research. The awardees receive the Alzheimer Medal, a bronze medal featuring the likeness of Alois Alzheimer, and a monetary award of $7,500. The award will be presented at the JAD Editorial Board meeting in Amsterdam on July 17, 2023, in conjunction with the Alzheimer's Association International Conference.
Dr. Tiemeier, Dr. Freak-Poli and their co-investigators explored whether loneliness and social support are independently associated with cognitive decline and risk of dementia, and further, whether depressive symptoms confound the association.
“While recent studies had suggested that loneliness or lack of social support may increase the risk of cognitive decline, studies that assess different social health factors, adjust for depression, and follow participants over many years to rule out reverse causality, were lacking,” explained lead investigator Dr. Tiemeier. “Our research was designed to address these knowledge gaps.”
To study behavioral and social determinants of dementia, researchers investigated loneliness, perceived social support, and structural social support (specifically marital status and number of children). They utilized a large ongoing population-based cohort, the Rotterdam Study, with 4,514 participants (mean age 70) who were followed up to 14 years for follow-up of dementia. Importantly, investigators replicated results in 2,112 participants (mean age 72) in the Swedish National Study on Aging and Care in Kungs (SNAC-K), who were followed up to 10 years. In both groups, dementia was diagnosed and cognitive function was repeatedly assessed with the Mini-Mental State Examination (MMSE) and a global cognitive factor (g-factor).
The results clearly showed that loneliness was prospectively associated with a decline in the MMSE in both groups studied. Consistently, people who were lonely had an increased risk of developing dementia independent of depressive symptoms. Neither perceived nor structural social support was associated with cognitive decline or dementia risk.
Lead author Dr. Freak-Poli, elaborated, “Loneliness is a serious societal problem across all ages. Our findings highlight the importance of developing successful preventive measures for loneliness. Importantly, loneliness may be modified and reductions in loneliness may be possible through interventions focused on social network enhancement or modifying maladaptive social cognition.”
About the 2023 Alzheimer Award Recipients

Dr. Tiemeier has received numerous prizes in recognition of this work including the VIDI (2009) and VICI (2017) awards from the Dutch Medical Research Council and the Leon Eisenberg Award in 2019. He has published over 750 peer-reviewed articles.

She is a Senior Research Fellow at the School of Clinical Sciences at Monash Health, Melbourne, Australia. She has been awarded an NHMRC Early Career Research Fellowship and a National Heart Foundation of Australia Postdoctoral Fellowship.
Dr. Freak-Poli has made an internationally significant and impactful contribution to understanding the population impact of social determinants as risk factors for chronic disease. Most recently, Dr. Freak-Poli has demonstrated that social health is associated with a greater severity of chronic disease risk-factors and lower quality of life; increased risk of cardiovascular disease and dementia; and worse mental health during cardiovascular disease recovery. Furthermore, she has progressed the field by examining the social health components of social isolation, social support, and loneliness separately to assess their independent contribution to health and wellbeing.
“On behalf of all our co-investigators and the study participants, we would like to sincerely thank the members of the JAD Editorial Board for their recognition of the significance of our work. We are extremely honored to receive this award from a group of our peers within the AD community,” commented Dr. Tiemeier and Dr. Freak-Poli.
“The editorial board and I are delighted to formally recognize the enormous contribution of Freak-Poli et al. to the AD research literature, selected from more than 800 excellent articles published by JAD in 2022. This research is particularly robust because it presents consistent results from two independent cohorts, simultaneously investigated two measures of cognitive decline and dementia risk over considerable follow-up periods, analyzed several social health factors, and carefully adjusted for potential important confounders including depressive symptoms. This study further supports the critical role of social determinents in AD,” noted George Perry, PhD, Editor-in-Chief, Journal of Alzheimer's Disease, and Semmes Foundation Distinguished University Chair in Neurobiology at The University of Texas at San Antonio.
Contacts: George Perry, PhD Editor-in-Chief, Journal of Alzheimer's Disease +1 210 458 4450 [email protected]
Pim van Holst IOS Press +31 20 688 3355 [email protected]
NOTES FOR EDITORS Winning paper (open access): Freak-Poli R, Wagemaker N, Wang R, Lysen TS, Ikram MA, Vernooij MW, Dintica CS, Vernooij-Dassen M, Melis RJF, Laukka EJ, Fratiglioni L, Xu W, Tiemeier H. Loneliness, Not Social Support, Is Associated with Cognitive Decline and Dementia Across Two Longitudinal Population-Based Cohorts . J Alzheimers Dis. 2022;85(1):295-308, https://doi.org/10.3233/JAD-210330 .
This research project is part of the CoSTREAM consortium ( www.costream.eu ) and received funding from the European Union’s Horizon 2020 research and innovation programme (grant no. 667375).
Click here to view information about previous Alzheimer Award winners.
ABOUT THE JOURNAL OF ALZHEIMER’S DISEASE (JAD) The Journal of Alzheimer's Disease (JAD) is an international multidisciplinary journal to facilitate progress in understanding the etiology, pathogenesis, epidemiology, genetics, behavior, treatment, and psychology of Alzheimer's disease. The journal publishes research reports, reviews, short communications, book reviews, and letters-to-the-editor. Groundbreaking research that has appeared in the journal includes novel therapeutic targets, mechanisms of disease, and clinical trial outcomes. JAD has a Journal Impact Factor of 4 according to Journal Citation Reports™ (Clarivate, 2023). www.j-alz.com
ABOUT IOS PRESS IOS Press is an independent international scientific, technical, medical (STM) publishing house established in 1987 in Amsterdam. We produce around 90 journals and 70 books annually in a broad range of subject categories, primarily specializing in health and life sciences (including neurosciences, medical informatics, cancer research, and rehabilitation) and computer sciences (including artificial intelligence, data science, and semantic web). In addition, we offer specialized services that support scientific advancement. www.iospress.com
- Utility Menu
Willows Impact Evaluation: Reproductive Health Study
in Ghana, Pakistan, Tanzania, and Turkey
WIE Speaker Series: Dr. Henning Tiemeier presents "Intrauterine exposures and child development: Findings from a population-based birth cohort"
Date: , location: .
Henning Tiemeier, MA MD PhD, is Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair in Maternal and Child Health at HSPH. He is also Professor of Psychiatric Epidemiology at the Erasmus Medical Center in Rotterdam, Netherlands. Dr. Tiemeier received both his medical and his sociological degree from the University of Bonn, Germany, and his PhD from Erasmus University, Rotterdam.
Tiemeier has published extensively on the etiology of child developmental problems with a particular focus on prenatal exposures. Most of his research was performed in population-based cohort studies and his work often takes a neurodevelopmental approach. He is a principal investigator of the Generation R Study, a large pre-birth cohort in Rotterdam, that enrolled nearly 10,000 mothers and their children.
Dr. Tiemeier is a ISI Highly Cited Researcher (General Social Science).
Past Activities
Willows seminar series.

Dr. Sunder specializes in using microeconomics and econometrics to address questions in international development, with a focus on topics...

Dr. Larson is a post-doctoral research fellow in the...

Dr. Rokicki’s research focuses on reproductive, maternal, and child health both locally and globally. She applies experimental and quasi-...

Sarah Huber-Krum is a Research Associate for the Willows Reproductive Health Impact...

Nina is a Ph.D. Candidate in the Emmett Interdisciplinary Program in Environment and Resources at the School of Earth,...

Dr. Ana Langer joined the...
- Introduction
- Conclusions
- Article Information
Estimated mean trajectories are shown for global (A and B) and subcortical (C and D) brain volumes for each exposure group, including the reference (n = 2749; 4813 scans), prenatal selective serotonin reuptake inhibitor (SSRI) exposure (n = 41; 80 scans), SSRI use before pregnancy (n = 77; 126 scans), prenatal depression exposure (n = 257; 477 scans), and postnatal depression exposure (n = 74; 128 scans). Adjustment was made for child sex and age at the neuroimaging assessment; maternal age at intake, national origin, marital status, educational level, substance use (tobacco, cannabis, and alcohol), benzodiazepine use during pregnancy, and monthly household income; and child intracranial volume for subcortical volumes. Shaded areas indicate 95% CIs.
Color maps represent the directions and estimated volume differences. Red indicates increased volume, and blue indicates decreased volume compared with the reference group (white). Adjustment was made for child sex and age at the neuroimaging assessment; maternal age at intake, national origin, marital status, educational level, substance use (tobacco, cannabis, and alcohol), benzodiazepine use during pregnancy, and monthly household income; and child intracranial volume. Since the models were built using bilateral averages of each cortical region, lateral, medial, and inferior views of the right hemisphere are shown purely for visualization purposes. CCA indicates cingulate, caudal anterior; CRA, cingulate, rostral anterior; FG, fusiform gyrus; FM, frontal medial orbital; FS, frontal, superior; PC, postcentral gyrus; PCC, posterior cingulate; PHG, parahippocampal gyrus; SSRI, selective serotonin reuptake inhibitor.
eMethods. Neuroimaging, Maternal Depressive Symptoms, Psychopathology and SSRI Use, Pregnancy Complications, Covariates, Statistical Analyses
eResults. Nonresponse and Sensitivity Analyses
eFigure 1. Flow Diagram of Study Population
eFigure 2. Showing the Age of Each Participant at Each Study Time Point
eFigure 3. Direct Acyclic Graph Showing the Hypothesized Relationship Between Maternal SSRI Use During Pregnancy and Brain Outcomes
eFigure 4. Developmental Trajectories of Cortical Brain Structural Volumes
eFigure 5. Difference in Parameter Estimates (DFBETAS) for Each Data Point and All Exposure Groups in the Analyses of Primary Outcomes
eTable 1. Number of Images of the Participants in Each Group at the Three Assessments
eTable 2. Comparison of Linear and Nonlinear (Quadratic) Models Using the Likelihood Ratio Test
eTable 3. Nonresponse Analysis
eTable 4. Association of Prenatal SSRI Use and Maternal Depressive Symptoms With Cortical Brain Volumes
eTable 5. Comparison of Results From the Unweighted Model With Inverse Probability of Attrition Weighting (IPAW) Models for the Associations of Prenatal SSRI and Maternal Depressive Symptoms Exposure and Brain Morphology
eTable 6. Impact of Potentially Influential Observations on Primary Outcomes
eReferences
Data Sharing Statement
- Maternal Depression, SSRI Use, and Child Brain Trajectories JAMA Psychiatry Editorial December 1, 2023 Ardesheer Talati, PhD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Koc D , Tiemeier H , Stricker BH , Muetzel RL , Hillegers M , El Marroun H. Prenatal Antidepressant Exposure and Offspring Brain Morphologic Trajectory. JAMA Psychiatry. 2023;80(12):1208–1217. doi:10.1001/jamapsychiatry.2023.3161
Manage citations:
© 2024
- Permissions
Prenatal Antidepressant Exposure and Offspring Brain Morphologic Trajectory
- 1 Generation R Study Group, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands
- 2 Department of Child and Adolescent Psychiatry/Psychology, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands
- 3 Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, Massachusetts
- 4 Department of Epidemiology, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands
- 5 Department of Radiology and Nuclear Medicine, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands
- 6 Department of Psychology, Education and Child Studies, Erasmus School of Social and Behavioural Sciences, Erasmus University Rotterdam, Rotterdam, the Netherlands
- Editorial Maternal Depression, SSRI Use, and Child Brain Trajectories Ardesheer Talati, PhD JAMA Psychiatry
Question Is intrauterine exposure to selective serotonin reuptake inhibitors (SSRIs) and prenatal or postnatal depressive symptoms associated with brain morphologic trajectory in offspring?
Findings In this cohort study of 3198 mother-infant dyads, compared with no maternal SSRI exposure or depressive symptoms, prenatal SSRI use was associated with less cerebral gray matter in children that persisted from 7 to 15 years of age and greater increases in volumes of the amygdala and fusiform gyrus in children that did not persist until early adolescence.
Meaning Maternal SSRI use during pregnancy may be associated with altered brain development in offspring.
Importance Clinical decision-making on antidepressant treatment during pregnancy, particularly selective serotonin reuptake inhibitors (SSRIs), is challenging, as both prenatal SSRI exposure and maternal depressive symptoms may be associated with negative outcomes in offspring.
Objective To investigate the association between intrauterine SSRI exposure and maternal depressive symptoms and structural brain development in offspring from mid-childhood to early puberty.
Design, Setting, and Participants This prospective, population-based cohort study was embedded in the Generation R Study in Rotterdam, the Netherlands. All pregnant individuals with an expected delivery date between April 1, 2002, and January 31, 2006, were invited to participate. Data were analyzed from February 1 to September 30, 2022.
Exposure Maternal-reported SSRI use verified by pharmacy records. In mid-pregnancy and 2 and 6 months after delivery, participants reported depressive symptoms using the Brief Symptom Inventory and were divided into 5 groups: SSRI use during pregnancy (n = 41; 80 scans), SSRI use only before pregnancy (n = 77; 126 scans), prenatal depressive symptoms without prenatal SSRI use (n = 257; 477 scans), postnatal depressive symptoms only (n = 74; 128 scans), and nonexposed control individuals (n = 2749; 4813 scans).
Main Outcomes and Measures The main outcome was brain morphometry in offspring, including global and cortical brain volumes, measured at 3 magnetic resonance imaging assessments from 7 to 15 years of age.
Results The study included 3198 mother-child dyads. A total of 3198 mothers (100%) identified as women; mean (SD) age at intake was 31.1 (4.7) years. Children (1670 [52.2%] female) underwent brain imaging assessment from 7 to 15 years of age with 5624 total scans. Most brain gray matter volumes showed an inverted U–shaped trajectory. Compared with nonexposed controls, children prenatally exposed to SSRIs had less cerebral gray matter (β [SE], −20 212.2 [7285.6] mm 3 ; P = .006), particularly within the corticolimbic circuit, which persisted up to 15 years of age. Children exposed to SSRIs prenatally showed a steeper increase in volumes of the amygdala (age interaction: β [SE], 43.3 [13.4] mm 3 ; P = .006) and fusiform gyrus (age interaction: β [SE], 168.3 [51.4] mm 3 ; P = .003) from 7 to 15 years of age. These volumetric differences in the amygdala and fusiform observed in childhood did not persist until early adolescence. Prenatal depression was associated with a smaller volume in the rostral anterior cingulate gyrus (β [SE], −166.3 [65.1] mm 3 ; P = .006), and postnatal depression was associated with a reduced fusiform gyrus (β [SE], −480.5 [189.2] mm 3 ; P = .002). No association of SSRI use before pregnancy with brain outcomes was observed.
Conclusions and Relevance The results of this cohort study suggest that prenatal SSRI exposure may be associated with altered developmental trajectories of brain regions involved in emotional regulation in offspring. Further research on the functional implications of these findings is needed.
During pregnancy, approximately 7% to 20% of women experience depressive symptoms and anxiety. 1 In the US, about 10% of pregnant individuals receive antidepressant treatment, mostly selective serotonin reuptake inhibitors (SSRIs). 1 In northern Europe, the prevalence of prenatal SSRI use is lower and approximately 1% to 2%. 2 SSRIs are often used throughout pregnancy as maintenance treatment to prevent relapse of psychiatric symptoms. 3 Maternal depression and prenatal exposure to SSRIs have been associated with negative outcomes in offspring, including adverse neurodevelopment. 4 - 8 Currently, prescribing SSRIs to pregnant individuals is generally considered safe. However, methodologic limitations complicate understanding of potential direct consequences of prenatal SSRI exposure for offspring. Confounding by indication is 1 such limitation, which arises from the possibility that pregnant individuals who use SSRIs may have characteristics or conditions, including more severe depressive symptoms, that may be independently associated with adverse outcomes in offspring. 8 , 9 Correspondingly, separating the potential negative consequences of prenatal SSRI exposure from maternal depressive symptoms and controlling for confounding are challenging. We used a hierarchical approach based on animal and human imaging studies. 5 - 10 In the primary analyses, we examined the associations between prenatal exposure to SSRIs or maternal depressive symptoms and global volumes, including total gray and white matter, and volumes of the hippocampus and amygdala. In secondary analyses, we examined frontolimbic structures and somatosensory and higher-order visual areas.
SSRIs inhibit the reuptake of serotonin, a crucial neurotransmitter broadly distributed across brain areas that influences cognition, attention, and emotional regulation. 5 , 10 Animal studies have shown that serotonin regulates neuronal proliferation, differentiation, migration, and synaptogenesis. 10 , 11 Furthermore, a prenatal SSRI exposure model using serotonin transporter knockout mice demonstrated somatosensory cortex and corticolimbic circuits alterations. 12 In humans, prenatal SSRI exposure has been associated with an increased risk of neurodevelopmental, affective, and anxiety disorders emerging from early childhood to puberty. 8 , 13 - 16 Knowledge on prenatal SSRI treatment and brain morphometry in humans is growing. Previously, our research group showed that prenatal SSRI exposure was associated with reduced fetal head growth assessed by ultrasonography. 17 To our knowledge, only 3 structural magnetic resonance imaging (MRI) studies have examined prenatal SSRI exposure and brain volume in humans, of which 2 were retrospective studies in neonates. 18 - 20 SSRI-exposed newborns had larger amygdala and superior frontal cortices. 19 Also, prenatal SSRI exposure was associated with lower white matter diffusivity in infants. 18 However, these 2 studies had small samples (14-16 infants). 18 , 19 The third study showed that prenatal SSRI exposure (n = 235) was associated with a larger surface area in the left superior parietal cortex and a thicker left lateral occipital cortex in children aged 9 to 10 years. 20 However, the study was based on retrospective maternal reports of SSRI use and depressive symptoms during pregnancy, which could be prone to recall bias. Importantly, exposure to maternal depressive symptoms (without SSRI use) during pregnancy was also associated with differences in cortical thickness and volumes in the limbic, frontal, and temporal lobes in neonates and young children. A systematic review of neuroimaging studies also indicated changes in white matter microstructure and functional connectivity in limbic and mesocortical networks. 21
The prospective association of prenatal SSRI exposure with structural brain developmental trajectories is still largely unknown. 22 This prospective, population-based cohort study investigated the association of prenatal SSRI exposure and prenatal and postnatal maternal depressive symptoms with offspring brain morphometry in children aged 7 to 15 years. In an effort to address confounding by indication, we triangulated results from different contrasting groups: SSRI use only before pregnancy, prenatal depressive symptoms, and postnatal depressive symptoms only.
We hypothesized that children prenatally exposed to SSRIs would have altered trajectories of brain morphologic growth, particularly in the corticolimbic and somatosensory circuits, compared with nonexposed control individuals. We also expected volumetric differences, albeit to a lesser extent, in children exposed to prenatal and postnatal maternal depressive symptoms.
The current study was embedded within the Generation R Study, a large, population-based cohort in Rotterdam, the Netherlands, that spans from fetal life until adolescence. 23 , 24 Recruitment details have been described elsewhere. 23 , 24 Briefly, pregnant individuals with a delivery date between April 1, 2002, and January 31, 2006, who were living in Rotterdam were invited to participate. Mothers who participated during pregnancy were eligible (eFigure 1 in the Supplement ). We excluded mothers without data on SSRI use or information on prenatal depressive symptoms. Children of participating mothers underwent at least 1 neuroimaging assessment. Children with unusable MRI data (mostly poor image quality, but also incidental findings) were excluded. The medical ethics committee of the Erasmus Medical Centre, Rotterdam, approved the study. Participants provided written informed consent for each phase of the study (fetal, preschool, childhood, and adolescence). This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
To optimize ascertainment of maternal SSRI use in pregnancy, information was collected using maternal-reported questionnaires and prescription records from pharmacies. During the first trimester, pregnant individuals were asked whether they had used medications in the previous 6 months (during pregnancy, only before pregnancy, or stopped when they knew they were pregnant). In the second and third trimester, we asked which medication was used in the preceding 3 months. From these questionnaires, we assessed SSRI exposure and timing (before or during pregnancy). To validate filled SSRI prescriptions, we used pharmacy data to verify SSRI use. The agreement between self-reports and prescription records was high: Yule Y was 0.94. 17 , 25
Information on maternal psychopathology was obtained during pregnancy (20 weeks’ gestation) and postnatally (2 and 6 months) with the Brief Symptom Inventory, a validated self-report questionnaire containing 53 items. The 6-item depression scale of the Brief Symptom Inventory was used (Cronbach α at 3 assessments ranged from 0.82 to 0.88). According to Dutch normative data, mothers with a score higher than 0.75 had clinically relevant depressive symptoms 25 (eMethods in Supplement 1 ).
Based on the aforementioned information, pregnant individuals were classified into 5 groups. First, the reference (control) group included individuals not using SSRIs who had low scores for depressive symptoms during pregnancy. Second, the prenatal SSRI exposure group included individuals with and without depressive symptoms who used SSRIs during pregnancy. Third, the group with SSRI use before pregnancy included individuals with and without depressive symptoms who used SSRIs before pregnancy. Fourth, the group with prenatal depression included individuals not using SSRIs before and during pregnancy who had clinically relevant depressive symptoms during pregnancy. Fifth, the group with postnatal depression only included individuals not using an SSRI before or during pregnancy who had clinically relevant depressive symptoms postnatally only.
Children underwent 3 neuroimaging waves: T1, T2, and T3. Age at each time point is shown in eFigure 2 in Supplement 1 . Magnetic resonance imaging scans were obtained at T1 using a Discovery MR750 3.0T MRI system (GE HealthCare) and at T2 and T3 using a dedicated Discovery MR750w 3.0T MRI system (GE HealthCare). Technical details are provided in the eMethods in Supplement 1 .
Cortical reconstruction and volumetric segmentation were performed with FreeSurfer, version 6.0 (Athinoula A. Martinos Center for Biomedical Imaging). 26 FreeSurfer morphometry has shown good test-retest reliability across scanners and field strengths. 27 Briefly, nonbrain tissue was removed, voxel intensities were adjusted for B 1 inhomogeneity, whole-brain tissue segmentation was done, and a surface-based model of the cortex was reconstructed. Cortical labeling was performed using the Desikan-Killiany Atlas (eMethods in Supplement 1 ).
Based on the literature, 18 - 20 , 22 the following potential covariates were selected: maternal age at intake, national origin (Dutch, non-Dutch [including European, Western American, and Western Asian], and non-Dutch, non-Western [including African, Cape Verdean, Dutch Antillean, Indonesian, Moroccan, non-Western American, non-Western Asian, Oceanian, Surinamese, and Turkish]), educational level, marital status, substance use (tobacco, cannabis, and alcohol), benzodiazepine use during pregnancy, and household income and child sex and age at the assessment. National origin was determined based on the country of birth of the mother and her parents using a questionnaire with categories corresponding to those used by the Dutch Central Bureau of Statistics. Because many of the national origins have a small number of participants in the Generation R Study, we operationalized these data following prior work in the Generation R Study as a 3-category variable. Details are provided in the eMethods in Supplement 1 .
Data were analyzed from February 1 to September 30, 2022. The association of prenatal SSRI exposure and depressive symptoms with brain morphometry from ages 7 to 15 years was examined with linear mixed-effects models. We used a hierarchical approach. To minimize multiple testing, we conducted follow-up analyses only if associations with the primary outcomes (total gray and white matter and hippocampus and amygdala) were observed. Cortical regions of interest, including cortical volumes of frontal, cingulate, somatosensory (postcentral gyrus), and higher-order visual areas (fusiform gyrus, parahippocampal gyrus), were included in the second tier to investigate how frontolimbic systems could contribute to the observed global associations. 10 , 19 , 22 , 28 , 29 Exposure and confounder variables were included as fixed effects with a random intercept to allow for the repeated observations of participants. Main associations and interaction terms of the exposure and child age with the brain outcomes were included.
The fully adjusted model was corrected for child sex and age at neuroimaging assessment and maternal age at intake, national origin, marital status, educational level, substance use (tobacco, cannabis, and alcohol), benzodiazepine use during pregnancy, and household income. Models with subcortical and cortical volumes included intracranial volume to account for head size. To account for scanner differences, a random-effect term was added in the model. We additionally explored interaction by child sex. Directed acyclic graphs and model equations are shown in the eMethods and eFigure 3 in Supplement 1 .
Post hoc group comparisons were performed in cortical regions associated with both prenatal SSRI and depressive symptoms exposure. For nonresponse analyses, we performed a t test or Wilcoxon rank sum test for continuous variables and χ 2 tests for categorical variables. Since participants included in the study population and those lost to follow-up differed in multiple characteristics (eTable 3 in Supplement 1 ), we used inverse probability of attrition weighting to account for potential selection bias (eMethods and eTable 5 in Supplement 1 ). To assess potential influential observations, we performed an additional analysis to detect influential data in mixed-effects models 30 (eMethods, eResults, eFigure 5, and eTable 6 in Supplement 1 ).
Multiple comparison correction was applied using a false discovery rate (Benjamini-Hochberg procedure). 31 Statistical significance was considered at 2-sided P < .05. Missing covariate data were imputed using multivariate imputation by chained equations with 25 imputations; variables and outcomes were not imputed. All analyses were conducted using R, version 4.1.2 (R Project for Statistical Computing).
Among 8756 eligible mothers, we excluded 756 without data on SSRI use, 1783 without information on prenatal depressive symptoms, and 2572 because children did not have MRI scans at T1, T2, or T3, leaving 3645 mother-child pairs (eFigure 1 in Supplement 1 ). After excluding 447 children with unusable MRI data, the final sample included 3198 mother-child pairs with 5624 scans. eTable 1 in Supplement 1 outlines the number of images in each neuroimaging wave.
The mean (SD) age of mothers at intake was 31.1 (4.7) years, and 3198 (100%) identified as women. Of the children, 1670 were female (52.2%) and 1528 were male (47.8%) and underwent brain imaging assessment from 7 to 15 years of age with 5624 total scans. A total of 41 participants were in the group with SSRI use during pregnancy (80 scans), 77 in the group with SSRI use only before pregnancy (126 scans), 257 in the group with prenatal depressive symptoms without prenatal SSRI use (477 scans), 74 in the group with postnatal depressive symptoms only (128 scans), and 2749 in the group of nonexposed control individuals (4813 scans). Compared with nonexposed controls, participants who used SSRIs during pregnancy had lower household income, consumed less alcohol, and were more likely to smoke tobacco and use benzodiazepines ( Table 1 ). Participants who reported clinically relevant prenatal depressive symptoms were younger, had fewer years of education, and were more likely to be non-Dutch. Women with postnatal depression only were younger, had fewer years of education, and had lower income.
Overall, the development of global and cortical brain structures from midchildhood to early puberty was nonlinear and best modeled by adding a quadratic age term (eTable 2 in Supplement 1 ). Only the hippocampal and postcentral gyrus volume trajectories were best modeled linearly.
Table 2 shows the associations of prenatal SSRI use with the repeated measures of global and subcortical brain volume. Figure 1 depicts the estimated trajectories of different brain volumes for each exposure group separately. The development of the cerebral gray matter volume followed an inverted U shape, while white matter increased from ages 7 to 15 years. As shown in Figure 1 A, compared with the nonexposed condition, prenatal SSRI exposure was associated with lower cerebral gray matter volume (β [SE], −20 212.2 [7285.6] mm 3 ; P = .006), particularly within the corticolimbic circuit, that persisted up to 15 years of age. Likewise, exposure to SSRIs during pregnancy was associated with lower cerebral white matter (β [SE], −16 336.7 [4167.2] mm 3 ; P < .001) and amygdala (β [SE], −159.1 [31.3] mm 3 ; P < .001) volume from 9 to 12 years of age ( Table 2 ), but these volume differences attenuated with age. The age interaction (β [SE]) for cerebral white matter was 1548.8 [432.2] mm 3 ( P = .004) and for amygdala was 43.3 (13.4) mm 3 ( P = .006) ( Figure 1 B and C and Table 2 ). Exposure to an SSRI was not associated with volume and growth trajectory of the hippocampus ( Figure 1 D and Table 2 ).
No associations of postnatal exposure to depressive symptoms or SSRI use before pregnancy with primary brain outcomes were observed. Prenatal exposure to depressive symptoms was associated with a steeper increase in cerebral white matter volume (age interaction: β [SE], 1495.2 [357.1] mm 3 ; P < .001) ( Figure 1 B and Table 2 ). No interaction by child sex in any of the models was observed.
In follow-up analyses, we further explored the developmental trajectories of specific cortical brain regions as defined by the Desikan-Killiany parcellation. Cortical maps from ages 7 to 15 years were plotted and represent estimated volume differences in each exposure group compared with the reference ( Figure 2 ). Prenatal SSRI exposure was consistently associated with lower volume, ranging from 5% to 10% in the frontal, cingulate, and temporal cortex across ages.
eFigure 4 and eTable 4 in Supplement 1 show the persistent association between prenatal SSRI exposure and less cortical volumes across the 10-year follow-up period, including in the superior frontal cortex, medial orbitofrontal cortex, parahippocampal gyrus, rostral anterior cingulate cortex, and posterior cingulate. In the fusiform gyrus, the estimated difference was age dependent: the difference between the prenatal SSRI exposure group and the reference group decreased from 7.4% at age 7 years to 1.2% at age 15 years ( Figure 2 and eFigure 4 in Supplement 1 ). The catch-up growth in the fusiform gyrus was explained by the steeper volume increase in prenatally exposed children (age interaction: β [SE], 168.3 [51.4] mm 3 ; P = .003) (eFigure 4 and eTable 4 in Supplement 1 ). Catch-up growth of the fusiform gyrus was also observed in children postnatally exposed to maternal depressive symptoms (age interaction: β [SE], 140.3 [51.6] mm 3 ; P = .003) (eFigure 4 and eTable 4 in Supplement 1 ). However, prenatal SSRI exposure was associated with lower volume in the fusiform gyrus than was exposure to postnatal depressive symptoms (β [SE], −621.4 [164.2] mm 3 ; P = .007).
No associations of SSRI use before pregnancy with cortical volumes were observed. Exposure to prenatal depressive symptoms was only associated with less volume reduction in the rostral anterior cingulate cortex. Prenatal depression was associated with smaller volume in the rostral anterior cingulate gyrus (β [SE], −166.3 [65.1] mm 3 ; P = .006), and postnatal depression was associated with reduced volume in the fusiform gyrus (β [SE], −480.5 [189.2] mm 3 ; P = .002) (eTable 4 in Supplement 1 ). No interaction by child sex was identified in any of the models.
In this prospective, population-based cohort study of mother-child pairs, we observed that prenatal SSRI exposure was associated with reduced global gray and white matter volume in children from 7 to 15 years of age. However, children exposed to SSRIs during gestation showed catch-up growth of the white matter, the amygdala, and the fusiform gyrus during early adolescence. Comparing these findings with those from the contrasting exposure groups suggests a specific association of prenatal SSRI exposure with brain morphometry. Children exposed to prenatal depressive symptoms had smaller rostral anterior cingulate gyri, and those exposed to postnatal depressive symptoms had smaller fusiform gyrus only. SSRI use before conception was not associated with any brain differences.
Several potential mechanisms may underly the association of exposure to prenatal SSRIs and depressive symptoms with brain development. Previous animal studies have demonstrated that high levels of serotonin during the perinatal period may impact the somatosensory and corticolimbic network. 4 , 10 , 32 Perinatal SSRI exposure could contribute to altered serotonin receptor distribution, 10 transcription factors expression, 33 or neurotrophic factor level fluctuations. 34 In humans, biomarker studies have shown reduced levels of cord trophic factor, such as S100 calcium-binding protein B, in SSRI-exposed neonates. 35 Maternal SSRI use may also be associated with epigenetic dysregulation of genes crucial in embryonic brain development (insulinlike growth factor 2, glial cell–derived neurotrophic factor). 36 Alterations of corticolimbic structures in the offspring in the present study were in line with these studies. 4 , 10 , 32 - 36
While maternal depressive symptoms have been associated with a larger amygdala volume, 37 , 38 we did not find this in the present study; we found a specific association of prenatal SSRI exposure with amygdala and fusiform gyrus maturation. Taken together, our longitudinal results suggest an increased volume growth of the amygdala and fusiform gyrus, a neural circuitry that has been associated with affective disorders in individuals prenatally exposed to SSRIs.
A recent systematic review by Rommel et al 8 reported that prenatal exposure to antidepressants was associated with multiple physical, neurodevelopmental, and psychiatric outcomes in offspring. However, the authors suggested that these associations were mostly related to underlying maternal psychopathology rather than a direct association with the medication. The same research team reported similar associations in children whose fathers used antidepressants during pregnancy, indicating another association with parental psychopathology rather than with direct in utero antidepressant exposure. 16 To address potential confounding, we included several comparison groups. Despite our efforts to control for confounding, there were still disparities in group characteristics. Notably, women using SSRIs prenatally had higher depression scores and benzodiazepine use compared with the reference group, suggesting a more severe or comorbid depressive phenotype.
Strengths of the study were the use of a population-based sample, a longitudinal design with the combined use of self-reports and pharmacy records, repeated assessments of pediatric neuroimaging, and multiple sociodemographic confounders. However, several limitations must be discussed. First, we were unable to investigate trimester-specific outcomes of SSRI use and assess associations with specific SSRI types due to the low prevalence of SSRI use. While we used a validated 6-item, self-reported depressive symptom scale, more detailed psychiatric evaluations might further increase the validity of assessments. Our main results were based on a small subsample (n = 41; 80 scans) with prenatal SSRI exposure; thus, findings should be interpreted cautiously. Second, while child brain structure has been associated with a variety of cognitive and sensorimotor functions in the general population, 39 the functional implications of the reported morphologic variations have yet to be explored. Future research on the long-term behavioral and psychological outcomes associated with these brain trajectories is needed. Third, even though we adjusted for multiple factors, residual confounding cannot be ruled out (eg, genetic factors, nutrition, stress, and other medical problems during and before pregnancy). Fourth, while sex differences in prenatal programming are commonly observed, 40 our study did not find any sex differences. This may be attributed to the limited sample size of SSRI-exposed offspring. Fifth, confounding by indication is difficult to rule out in an observational study even when triangulating different contrasting groups and adjusting for multiple confounders. Thus, these results should be cautiously interpreted.
This cohort study found that exposure to maternal SSRI use during pregnancy was associated with offspring brain morphometry development from ages 7 to 15 years. We reported smaller volumes of the corticolimbic circuit and catch-up growth of the white matter, amygdala, and fusiform gyrus. This study may increase understanding of the association between in utero SSRI exposure and brain growth. Well-designed replication studies in diverse settings are needed before evidence-based recommendations can be derived, as the prevalence of SSRI use during pregnancy varies across populations.
Accepted for Publication: June 13, 2023.
Published Online: August 30, 2023. doi:10.1001/jamapsychiatry.2023.3161
Corresponding Author: Henning Tiemeier, MD, PhD, Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, 677 Huntington Ave, Kresge Building, Room 619, Boston, MA 02115 ( [email protected] ).
Author Contributions: Prof Tiemeier had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Koc, Tiemeier, El Marroun.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Koc, El Marroun.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Koc.
Obtained funding: Tiemeier, El Marroun.
Administrative, technical, or material support: Koc, Stricker, Muetzel, Hillegers.
Supervision: Tiemeier, Stricker, El Marroun.
Conflict of Interest Disclosures: None reported.
Funding/Support: Dr Koc was supported by grant 953327 from the Marie Skłodowska-Curie Actions Innovative Training Networks program (Serotonin and Beyond; Profs Tiemeier and El Marroun). This study was supported by Stichting Volksbond Rotterdam, grant 015.016.056 from the Netherlands Organisation for Scientific Research (NWO) Aspasia (Prof El Marroun), grant 101057390 from the European Union’s Horizon Research and Innovation Program (HappyMums; Prof El Marroun), grant 016.VICI.170.200 from the Netherlands Organisation for Health Research and Development (ZonMw; Prof Tiemeier), grant S18-20 from the Sophia Foundation for neuroimaging, image analysis, and informatics (Dr Muetzel), and grant 101057529 from the European Union’s Horizon Research and Innovation 5 Program (FAMILY; Prof Tiemeier and Dr Muetzel).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: We acknowledge the contributions of the participating children, parents, general practitioners, hospitals, midwives, and pharmacies in Rotterdam, the Netherlands.
Additional Information: Supercomputing resources were supported by the NWO (Exacte Wetenschappen) and SURFsara (Snellius). The general design of the Generation R Study was supported by Erasmus University Medical Centre, Erasmus University Rotterdam; ZonMw; the NWO; the Ministry of Health, Welfare and Sport; and the Ministry of Youth and Families.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Prenatal Antidepressant Exposure and Offspring Brain Morphologic Trajectory
Affiliations.
- 1 Generation R Study Group, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands.
- 2 Department of Child and Adolescent Psychiatry/Psychology, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands.
- 3 Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, Massachusetts.
- 4 Department of Epidemiology, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands.
- 5 Department of Radiology and Nuclear Medicine, Erasmus University Medical Centre, Erasmus University Rotterdam, Rotterdam, the Netherlands.
- 6 Department of Psychology, Education and Child Studies, Erasmus School of Social and Behavioural Sciences, Erasmus University Rotterdam, Rotterdam, the Netherlands.
- PMID: 37647036
- PMCID: PMC10469300
- DOI: 10.1001/jamapsychiatry.2023.3161
Importance: Clinical decision-making on antidepressant treatment during pregnancy, particularly selective serotonin reuptake inhibitors (SSRIs), is challenging, as both prenatal SSRI exposure and maternal depressive symptoms may be associated with negative outcomes in offspring.
Objective: To investigate the association between intrauterine SSRI exposure and maternal depressive symptoms and structural brain development in offspring from mid-childhood to early puberty.
Design, setting, and participants: This prospective, population-based cohort study was embedded in the Generation R Study in Rotterdam, the Netherlands. All pregnant individuals with an expected delivery date between April 1, 2002, and January 31, 2006, were invited to participate. Data were analyzed from February 1 to September 30, 2022.
Exposure: Maternal-reported SSRI use verified by pharmacy records. In mid-pregnancy and 2 and 6 months after delivery, participants reported depressive symptoms using the Brief Symptom Inventory and were divided into 5 groups: SSRI use during pregnancy (n = 41; 80 scans), SSRI use only before pregnancy (n = 77; 126 scans), prenatal depressive symptoms without prenatal SSRI use (n = 257; 477 scans), postnatal depressive symptoms only (n = 74; 128 scans), and nonexposed control individuals (n = 2749; 4813 scans).
Main outcomes and measures: The main outcome was brain morphometry in offspring, including global and cortical brain volumes, measured at 3 magnetic resonance imaging assessments from 7 to 15 years of age.
Results: The study included 3198 mother-child dyads. A total of 3198 mothers (100%) identified as women; mean (SD) age at intake was 31.1 (4.7) years. Children (1670 [52.2%] female) underwent brain imaging assessment from 7 to 15 years of age with 5624 total scans. Most brain gray matter volumes showed an inverted U-shaped trajectory. Compared with nonexposed controls, children prenatally exposed to SSRIs had less cerebral gray matter (β [SE], -20 212.2 [7285.6] mm3; P = .006), particularly within the corticolimbic circuit, which persisted up to 15 years of age. Children exposed to SSRIs prenatally showed a steeper increase in volumes of the amygdala (age interaction: β [SE], 43.3 [13.4] mm3; P = .006) and fusiform gyrus (age interaction: β [SE], 168.3 [51.4] mm3; P = .003) from 7 to 15 years of age. These volumetric differences in the amygdala and fusiform observed in childhood did not persist until early adolescence. Prenatal depression was associated with a smaller volume in the rostral anterior cingulate gyrus (β [SE], -166.3 [65.1] mm3; P = .006), and postnatal depression was associated with a reduced fusiform gyrus (β [SE], -480.5 [189.2] mm3; P = .002). No association of SSRI use before pregnancy with brain outcomes was observed.
Conclusions and relevance: The results of this cohort study suggest that prenatal SSRI exposure may be associated with altered developmental trajectories of brain regions involved in emotional regulation in offspring. Further research on the functional implications of these findings is needed.
PubMed Disclaimer
Conflict of interest statement
Conflict of Interest Disclosures: None reported.
Figure 1.. Developmental Trajectories of Global and…
Figure 1.. Developmental Trajectories of Global and Subcortical Structural Brain Volumes Across the Follow-Up Period
Figure 2.. Cortical Maps Showing Estimated Volume…
Figure 2.. Cortical Maps Showing Estimated Volume Differences in Cortical Regions Between Each Exposure Group…
- Maternal Depression, Prenatal SSRI Exposure, and Brain Trajectories in Childhood. Talati A. Talati A. JAMA Psychiatry. 2023 Dec 1;80(12):1191-1192. doi: 10.1001/jamapsychiatry.2023.2664. JAMA Psychiatry. 2023. PMID: 37647051 No abstract available.
Similar articles
- Intrauterine Exposure to Antidepressants or Maternal Depressive Symptoms and Offspring Brain White Matter Trajectories From Late Childhood to Adolescence. Koc D, El Marroun H, Stricker BH, Muetzel RL, Tiemeier H. Koc D, et al. Biol Psychiatry Cogn Neurosci Neuroimaging. 2024 Feb;9(2):217-226. doi: 10.1016/j.bpsc.2023.10.009. Epub 2023 Nov 4. Biol Psychiatry Cogn Neurosci Neuroimaging. 2024. PMID: 37926188
- Associations Between Brain Structure and Connectivity in Infants and Exposure to Selective Serotonin Reuptake Inhibitors During Pregnancy. Lugo-Candelas C, Cha J, Hong S, Bastidas V, Weissman M, Fifer WP, Myers M, Talati A, Bansal R, Peterson BS, Monk C, Gingrich JA, Posner J. Lugo-Candelas C, et al. JAMA Pediatr. 2018 Jun 1;172(6):525-533. doi: 10.1001/jamapediatrics.2017.5227. JAMA Pediatr. 2018. PMID: 29630692 Free PMC article.
- Association of Selective Serotonin Reuptake Inhibitor Exposure During Pregnancy With Speech, Scholastic, and Motor Disorders in Offspring. Brown AS, Gyllenberg D, Malm H, McKeague IW, Hinkka-Yli-Salomäki S, Artama M, Gissler M, Cheslack-Postava K, Weissman MM, Gingrich JA, Sourander A. Brown AS, et al. JAMA Psychiatry. 2016 Nov 1;73(11):1163-1170. doi: 10.1001/jamapsychiatry.2016.2594. JAMA Psychiatry. 2016. PMID: 27732704
- Variations in Neurodevelopmental Outcomes in Children with Prenatal SSRI Antidepressant Exposure. Rotem-Kohavi N, Oberlander TF. Rotem-Kohavi N, et al. Birth Defects Res. 2017 Jul 17;109(12):909-923. doi: 10.1002/bdr2.1076. Birth Defects Res. 2017. PMID: 28714603 Review.
- [Treatment of depressed pregnant women by selective serotonin reuptake inhibitors: risk for the foetus and the newborn]. Favrelière S, Nourrisson A, Jaafari N, Pérault Pochat MC. Favrelière S, et al. Encephale. 2010 Jun;36 Suppl 2:D133-8. doi: 10.1016/j.encep.2009.06.005. Epub 2009 Sep 19. Encephale. 2010. PMID: 20513456 Review. French.
- Impact of prenatal maternal depression on gestational length: post hoc analysis of a randomized clinical trial. Davis EP, Demers CH, Deer L, Gallop RJ, Hoffman MC, Grote N, Hankin BL. Davis EP, et al. EClinicalMedicine. 2024 Apr 22;72:102601. doi: 10.1016/j.eclinm.2024.102601. eCollection 2024 Jun. EClinicalMedicine. 2024. PMID: 38680516 Free PMC article.
- Vigod SN, Wilson CA, Howard LM. Depression in pregnancy. BMJ. 2016;352:i1547. doi:10.1136/bmj.i1547 - DOI - PubMed
- Ververs T, Kaasenbrood H, Visser G, Schobben F, de Jong-van den Berg L, Egberts T. Prevalence and patterns of antidepressant drug use during pregnancy. Eur J Clin Pharmacol. 2006;62(10):863-870. doi:10.1007/s00228-006-0177-0 - DOI - PubMed
- Liu X, Molenaar N, Agerbo E, et al. . Antidepressant discontinuation before or during pregnancy and risk of psychiatric emergency in Denmark: a population-based propensity score-matched cohort study. PLoS Med. 2022;19(1):e1003895. doi:10.1371/journal.pmed.1003895 - DOI - PMC - PubMed
- Gemmel M, Bögi E, Ragan C, et al. . Perinatal selective serotonin reuptake inhibitor medication (SSRI) effects on social behaviors, neurodevelopment and the epigenome. Neurosci Biobehav Rev. 2018;85:102-116. doi:10.1016/j.neubiorev.2017.04.023 - DOI - PubMed
- Hutchison SM, Mâsse LC, Pawluski JL, Oberlander TF. Perinatal selective serotonin reuptake inhibitor (SSRI) and other antidepressant exposure effects on anxiety and depressive behaviors in offspring: a review of findings in humans and rodent models. Reprod Toxicol. 2021;99:80-95. doi:10.1016/j.reprotox.2020.11.013 - DOI - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- PubMed Central
- Silverchair Information Systems
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Terms, Privacy & Notices
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Faculty Facing Caregiving Need
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Faculty & Staff
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Yale Child Study Center Grand Rounds speakers: winter/spring 2023 update
With just over four months remaining in the spring semester, the YCSC Grand Rounds Committee shared an updated list of distinguished speakers for the department’s Grand Rounds series, as confirmed to date. This weekly seminar-style series is typically presented live from the YCSC Cohen Auditorium on Tuesdays at 1:00 p.m, while also live streamed via zoom. Community members can request a meeting with a speaker in advance of each session. For updated details as sessions approach, please visit the web calendar .
February 21, 2023 Identifying Adolescents at Risk for Substance Misuse Using Digital Tools: Why, Where, When and How Kammarauche Asuzu Aneni, MBBS, MHS Assistant Professor of Child Psychiatry, Yale Child Study Center
February 28, 2023 The Struggle is (Still) Real: Reflections on Modern Day Black Resistance Tara Davila and Belinda Oliver Yale Child Study Center
March 7, 2023 “My World,” and the Musical, Medical, and Social Narratives of Autism Jacob Gluckman, Premedical student at Bryn Mawr College’s Premedical Post-baccalaureate program
March 14, 2023 Clinical Care for LGBTQ Youth: Ethical Case Studies Lisa Campo-Engelstein, PhD Chair, Department of Bioethics & Health Humanities, University of Texas Medical Branch View session poster for meet and greet opportunities with this speaker
March 21, 2023 M aking it Real: from telling to showing , sharing , and doing in psychiatric education Andrés Martin, MD, PhD Riva Ariella Ritvo Professor, Yale Child Study Center; Director, Simulated Participant Program, Teaching and Learning Center, Yale School of Medicine
March 28, 2023 Social Work Month Event Details TBA
April 4, 2023 Compassionate Care Rounds Details TBA
April 11, 2023 Best Minds: How Allen Ginsberg Made Revolutionary Poetry from Madness Stevan Weine MD Director, Global Medicine ; Director, Center for Global Health; Professor of Psychiatry, University of Illinois at Chicago
April 18, 2023 Population Neuroscience and Public Health Henning Tiemeier, MA, MD, PhD Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair of Maternal and Child Health , Harvard T.H. Chan School of Public Health
April 25, 2023 Viola Bernard Special Lecture Jessica Cerdena, PhD MD Candidate and Medical Anthropologist at Yale
May 2, 2023 Max Ritvo ‘13 and Alan B. Slifka ‘51 Program for the Medical Humanities Special Lecture Transformation Through Art: A Personal and Professional Perspective Eva Ritvo, MD
May 9, 2023 (VIRTUAL) Christine Moutier, MD Chief Medical Officer, American Foundation for Suicide Prevention
May 16, 2023 Ami Klin, PhD Director, Marcus Autism Center
May 23, 2023 Child and adolescent mental health trainees portrayed: Narratives of heritage and legacy Ayotunde Ayobello, MD Clinical Instructor and Artist-in-Residence, Yale Child Study Center
May 30, 2023 (VIRTUAL) Thema Bryant-Davis PhD President, American Psychological Association
June 6, 2023 YCSC Postdoctoral Fellowship in Childhood Neuropsychiatric Disorders (T32) Trainee Talks Mike Crowley, PhD Associate Professor, Yale Child Study Center
June 13, 2023 TBD
June 20, 2023 Honoring Juneteenth Details TBA
June 27, 2023 TBD
A weekly forum for YCSC faculty, staff, and affiliates, these sessions offer multidisciplinary opportunities to come together and learn about a variety of topics relevant to the mental health of children, adolescents, families, and communities. YCSC Grand Rounds are the oldest series exclusively dedicated to topics in child psychiatry and allied disciplines.
To find upcoming Grand Rounds and other department events, visit the YCSC web calendar . Visit the YCSC website for recordings of past sessions . To receive information and updates about upcoming sessions, subscribe to the Center's monthly newsletter .
- Grand Rounds
- MyU : For Students, Faculty, and Staff
Center for Leadership Education in Maternal & Child Public Health
School of public health, we are jiwc.
The Cross-Center Collaboration on the Health of Justice-Involved Women and Children (JIWC) is a group of HRSA-funded faculty, staff and trainees working on research, policy, training issues and topics at the intersection of incarceration and MCH. We are affiliated with the Centers of Excellence in Maternal and Child Health (MCH) Education, Science and Practice located at the UMN, UIC, Harvard and Emory.


2023 Alzheimer Award Goes to Henning Tiemeier, MD, PhD, and Rosanne Freak-Poli, PhD
Amsterdam, the Netherlands – The Journal of Alzheimer’s Disease (JAD) is pleased to announce the joint recipients of the 2023 Alzheimer Award are Henning Tiemeier, MD, PhD, Erasmus Medical Center, Rotterdam, and the Harvard TH Chan School of Public Health, and Rosanne Freak-Poli, PhD, Monash University.
The 2023 winning paper presents important insights into the impact of poor social health, specifically loneliness, on cognitive decline and risk of dementia in older adults. The article is Freak-Poli R, Wagemaker N, Wang R, Lysen TS, Ikram MA, Vernooij MW, Dintica CS, Vernooij-Dassen M, Melis RJF, Laukka EJ, Fratiglioni L, Xu W, Tiemeier H. Loneliness, Not Social Support, Is Associated with Cognitive Decline and Dementia Across Two Longitudinal Population-Based Cohorts . J Alzheimers Dis. 2022;85(1):295-308, https://doi.org/10.3233/JAD-210330 . It is openly available to everyone to read, download, and share.
Each year, members of JAD’s extensive editorial board select the article published during the previous year that has had the most significant impact on Alzheimer’s disease (AD) research. The awardees receive the Alzheimer Medal, a bronze medal featuring the likeness of Alois Alzheimer, and a monetary award of $7,500. The award will be presented at the JAD Editorial Board meeting in Amsterdam on July 17, 2023, in conjunction with the Alzheimer's Association International Conference.
Dr. Tiemeier, Dr. Freak-Poli and their co-investigators explored whether loneliness and social support are independently associated with cognitive decline and risk of dementia, and further, whether depressive symptoms confound the association.
“While recent studies had suggested that loneliness or lack of social support may increase the risk of cognitive decline, studies that assess different social health factors, adjust for depression, and follow participants over many years to rule out reverse causality, were lacking,” explained lead investigator Dr. Tiemeier. “Our research was designed to address these knowledge gaps.”
To study behavioral and social determinants of dementia, researchers investigated loneliness, perceived social support, and structural social support (specifically marital status and number of children). They utilized a large ongoing population-based cohort, the Rotterdam Study, with 4,514 participants (mean age 70) who were followed up to 14 years for follow-up of dementia. Importantly, investigators replicated results in 2,112 participants (mean age 72) in the Swedish National Study on Aging and Care in Kungs (SNAC-K), who were followed up to 10 years. In both groups, dementia was diagnosed and cognitive function was repeatedly assessed with the Mini-Mental State Examination (MMSE) and a global cognitive factor (g-factor).
The results clearly showed that loneliness was prospectively associated with a decline in the MMSE in both groups studied. Consistently, people who were lonely had an increased risk of developing dementia independent of depressive symptoms. Neither perceived nor structural social support was associated with cognitive decline or dementia risk.
Lead author Dr. Freak-Poli, elaborated, “Loneliness is a serious societal problem across all ages. Our findings highlight the importance of developing successful preventive measures for loneliness. Importantly, loneliness may be modified and reductions in loneliness may be possible through interventions focused on social network enhancement or modifying maladaptive social cognition.”
About the 2023 Alzheimer Award Recipients

Henning Tiemeier, MD, PhD , received his Doctorate in Medicine and his sociology degree from the University of Bonn, Germany, and his PhD in Epidemiology from the Erasmus University in Rotterdam, the Netherlands. He is Professor of Psychiatric Epidemiology at the Erasmus University Medical Center Rotterdam and in 2018, was appointed Professor of Social and Behavioral Science and Sumner and Esther Feldberg Chair in Maternal and Child Health at the Harvard TH Chan School of Public Health. His research focuses primarily on understanding the etiology of common psychiatric problems such as depression in adults and elderly persons (neurodegeneration) and children (neurodevelopment). He has a great interest in detailed phenotype assessment, neuroimaging, and genetics combined with modern quantitative methods.
Dr. Tiemeier has received numerous prizes in recognition of this work including the VIDI (2009) and VICI (2017) awards from the Dutch Medical Research Council and the Leon Eisenberg Award in 2019. He has published over 750 peer-reviewed articles.

Rosanne Freak-Poli, PhD , is a life-course epidemiologist. Her work is strongly driven by social justice, being the distribution of wealth, opportunities, and privileges within a society.
She is a Senior Research Fellow at the School of Clinical Sciences at Monash Health, Melbourne, Australia. She has been awarded an NHMRC Early Career Research Fellowship and a National Heart Foundation of Australia Postdoctoral Fellowship.
Dr. Freak-Poli has made an internationally significant and impactful contribution to understanding the population impact of social determinants as risk factors for chronic disease. Most recently, Dr. Freak-Poli has demonstrated that social health is associated with a greater severity of chronic disease risk-factors and lower quality of life; increased risk of cardiovascular disease and dementia; and worse mental health during cardiovascular disease recovery. Furthermore, she has progressed the field by examining the social health components of social isolation, social support, and loneliness separately to assess their independent contribution to health and wellbeing.
“On behalf of all our co-investigators and the study participants, we would like to sincerely thank the members of the JAD Editorial Board for their recognition of the significance of our work. We are extremely honored to receive this award from a group of our peers within the AD community,” commented Dr. Tiemeier and Dr. Freak-Poli.
“The editorial board and I are delighted to formally recognize the enormous contribution of Freak-Poli et al. to the AD research literature, selected from more than 800 excellent articles published by JAD in 2022. This research is particularly robust because it presents consistent results from two independent cohorts, simultaneously investigated two measures of cognitive decline and dementia risk over considerable follow-up periods, analyzed several social health factors, and carefully adjusted for potential important confounders including depressive symptoms. This study further supports the critical role of social determinents in AD,” noted George Perry, PhD, Editor-in-Chief, Journal of Alzheimer's Disease, and Semmes Foundation Distinguished University Chair in Neurobiology at The University of Texas at San Antonio.
NOTES FOR EDITORS Winning paper (open access): Freak-Poli R, Wagemaker N, Wang R, Lysen TS, Ikram MA, Vernooij MW, Dintica CS, Vernooij-Dassen M, Melis RJF, Laukka EJ, Fratiglioni L, Xu W, Tiemeier H. Loneliness, Not Social Support, Is Associated with Cognitive Decline and Dementia Across Two Longitudinal Population-Based Cohorts . J Alzheimers Dis. 2022;85(1):295-308, https://doi.org/10.3233/JAD-210330 .
This research project is part of the CoSTREAM consortium ( www.costream.eu ) and received funding from the European Union’s Horizon 2020 research and innovation programme (grant no. 667375).
Click here to view information about previous Alzheimer Award winners.
ABOUT THE JOURNAL OF ALZHEIMER’S DISEASE (JAD) The Journal of Alzheimer's Disease (JAD) is an international multidisciplinary journal to facilitate progress in understanding the etiology, pathogenesis, epidemiology, genetics, behavior, treatment, and psychology of Alzheimer's disease. The journal publishes research reports, reviews, short communications, book reviews, and letters-to-the-editor. Groundbreaking research that has appeared in the journal includes novel therapeutic targets, mechanisms of disease, and clinical trial outcomes. JAD has a Journal Impact Factor of 4 according to Journal Citation Reports™ (Clarivate, 2023). www.j-alz.com
ABOUT IOS PRESS IOS Press is an independent international scientific, technical, medical (STM) publishing house established in 1987 in Amsterdam. We produce around 90 journals and 70 books annually in a broad range of subject categories, primarily specializing in health and life sciences (including neurosciences, medical informatics, cancer research, and rehabilitation) and computer sciences (including artificial intelligence, data science, and semantic web). In addition, we offer specialized services that support scientific advancement. www.iospress.com
Related news items

Journal of Alzheimer's Disease's Outreach Initiatives Aim to Amplify Underrepresented Voices from Africa and South America
As part of its commitment to represent researchers from all parts of the world, the Journal of Alzheimer's Disease (JAD) is pleased to announce active outreach...
Research Spotlight: Implementation of a Lifestyle Dementia Prevention Intervention
Ryan Andrew Mace, PhD, an investigator in the Center for Health Outcomes and Interdisciplinary Research (CHOIR) within the department of Psychiatry at ...

Promising New Screening Tool May Help Manage Neurobehavioral Difficulties in Children With Duchenne Muscular Dystrophy
Amsterdam, the Netherlands – A pilot study using a new screening tool shows promise for assessing neurobehavioral difficulties in children with Duchenne...
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts
- PMC11062447

Prenatal exposure to common plasticizers: A longitudinal study on phthalates, brain volumetric measures, and IQ in youth
Akhgar ghassabian.
1 Department of Pediatrics, New York University School of Medicine, New York, NY, USA
2 Department of Population Health, New York University School of Medicine, New York, NY, USA
Michiel van den Dries
3 Department of Child and Adolescent Psychiatry, Erasmus University Medical Center, Rotterdam, the Netherlands
4 The Generation R Study Group, Erasmus University Medical Center, Rotterdam, the Netherlands
5 ISGlobal, Barcelona, Spain
6 Pompeu Fabra University, Barcelona, Spain
7 Spanish Consortium for Research on Epidemiology and Public Health, Instituto de Salud Carlos III, 28029 Madrid, Spain
Leonardo Trasande
8 New York University College of Global Public Health, New York City, NY, USA
9 New York University Wagner School of Public Service, New York City, NY, USA
Sander Lamballais
10 Department of Clinical Genetics, Erasmus University Medical Center, Rotterdam, the Netherlands
Suzanne Spaan
11 Department of Risk Analysis for Products in Development, TNO, Utrecht, the Netherlands
Maria-Pilar Martinez-Moral
12 Oncology Area, Center for Biomedical Research of La Rioja, Logroño, Spain
Kurunthachalam Kannan
Vincent wv jaddoe.
13 Department of Pediatrics, Erasmus University Medical Center, Rotterdam, the Netherlands
Stephanie M Engel
14 Department of Epidemiology, Gilling School of Global Public Health, University of North Carolina Chapel Hill, Chapel Hill, NC, USA
Anjoeka Pronk
Tonya white.
15 Section on Social and Cognitive Developmental Neuroscience, National Institute of Mental Health Bethesda, MD, USA
Henning Tiemeier
16 Department of Social and Behavioral Sciences, Harvard TH Chan School of Public Health, Boston, MA, USA
Mònica Guxens
Author Contributions
Associated Data
Exposure to phthalates, used as plasticizers and solvents in consumer products, is ubiquitous. Despite growing concerns regarding their neurotoxicity, brain differences associated with gestational exposure to phthalates are understudied. We included 775 mother-child pairs from Generation R, a population-based pediatric neuroimaging study with prenatal recruitment, who had data on maternal gestational phthalate levels and T 1 -weighted magnetic resonance imaging in children at age 10 years. Maternal urinary concentrations of phthalate metabolites were measured at early, mid-, and late pregnancy. Child IQ was assessed at age 14 years. We investigated the extent to which prenatal exposure to phthalates is associated with brain volumetric measures and whether brain structural measures mediate the association of prenatal phthalate exposure with IQ. We found that higher maternal concentrations of monoethyl phthalate (mEP, averaged across pregnancy) were associated with smaller total gray matter volumes in offspring at age 10 years (β per log10 increase in creatinine adjusted mEP=−10.7, 95%CI: −18.12, −3.28). Total gray matter volumes partially mediated the association between higher maternal mEP and lower child IQ (β for mediated path =−0.31, 95%CI: −0.62, 0.01, p = 0.05, proportion mediated = 18%). An association of higher monoisobutyl phthalate (mIBP) and smaller cerebral white matter volumes was present only in girls, with cerebral white matter volumes mediating the association between higher maternal mIBP and lower IQ in girls. Our findings suggest the global impact of prenatal phthalate exposure on brain volumetric measures that extends into adolescence and underlies less optimal cognitive development.
Introduction
Mental health problems and intellectual disability are a leading cause of health loss among children and adolescents in high income countries. 1 A combination of genetic predisposition, social determinants, environmental factors, and stochastic processes affect the developing brain and contribute to cognitive impairments and mental health problems in children. Given the rapid developmental changes in the brain and immaturity of metabolic pathways, the fetal period is a critical window of susceptibility for environmental insults. 2 Toxic environmental chemicals receive particular attention because their contribution is potentially preventable. 3 One group of such chemicals that presents a concern are phthalates, which are ubiquitously used as plasticizers and solvents in a wide range of commercial products, such as personal care products, food packaging, and vinyl flooring. In recent years the use of certain phthalates (e.g., di-2-ethylhexyl phthalate [DEHP]) in consumer products have been regulated under European Union Regulations 4 and their use are restricted in toys and childcare products in the United States. 5 Nonetheless, pregnant women are still ubiquitously exposed to phthalates, such as DEHP 6 – 8 and its replacements such as di-iso-nonyl phthalate, 9 , 10 even though proportion of women exposed to legacy phthalates and newer replacement phthalates varies by the compound, location, and year of assessment. For this reason, the American Academy of Pediatrics and several other scientific organizations urged a call for action on this emerging child health concern, with recommendations to expand translational research on emerging neurotoxicants. 3 , 11 , 12
Epidemiological studies have shown that prenatal exposures to DEHP, butyl-benzyl phthalate (BBzP), di-ethyl phthalate (DEP), and di-n-butyl phthalate (DBP) are associated with less optimal cognitive function, social development, and motor skills as well as behavioral problems in children. 13 , 14 In the Generation R Study, we reported that maternal prenatal urinary concentrations of phthalates, i.e., monoethyl phthalate (mEP) and a metabolite of di-n-octyl phthalate (DnOP), i.e., mono(3-carboxypropyl) phthalate (mCPP), were associated with lower IQ in school-age children. 15 , 16 There is some evidence that prenatal exposure to mono-n-butyl phthalate (mnBP, a metabolite of DBP) is related to brain development using ultrasound measurements. 17 Most of our knowledge on specific brain regions and developmental processes influenced by phthalate exposure comes from animal models. For example, developmental DEHP exposure inhibits the cerebellar granule cell proliferation in male rat/mouse offspring. 18 In animal models, prenatal phthalate exposure to a mixture of phthalates (DEHP, DEP, and others) results in a reduction in neuron number, synapse number, and size of the medial prefrontal cortex. 19 Developmental exposure to DEHP also reduces proliferation and neurogenesis and leads to an abnormal neuronal distribution in the neocortex. 20
Several studies have examined the neural basis of cognitive development and brain structure and function. 21 The relationship between brain development as identified by structural magnetic resonance imaging (MRI) and children’s and adolescents’ cognitive abilities is not limited to global development. Relations of subcortical structural and regional development in prefrontal cortex with cognitive abilities have also been demonstrated. 22 – 25 Neuroimaging studies have also been used to identify brain influences of environmental toxicants, such as lead, air pollution or neurotoxicants, such as organophosphate pesticides. 26 – 29 Yet, brain MRI has rarely been used to study whether specific neurobiological influences of phthalate exposure is present in humans. 30 One study examined the association between prenatal phthalate exposure and white matter microstructure in 76 preschool age children and found that higher maternal urinary concentrations of high molecular weight phthalates (metabolites of DEHP and BBzP) during the second trimester were associated with a higher mean diffusivity in diffusional tensor imaging, an indicator of impairments in white matter microstructure. 30 However, other structural brain differences, including global and regional volumetric measures, and child IQ were not examined in that study.
We used data from Generation R, a population-based pediatric neuroimaging study with prenatal recruitment, to examine the extent to which repeatedly measured in utero exposure to phthalates is associated with brain volumetric measures at age 10 years and whether brain structural differences mediate the association of prenatal phthalate exposure and child IQ assessed at age 14 years. We hypothesized that prenatal exposure to phthalates would be associated with global alterations in the brain, and brain alterations would be mediators in the association of prenatal phthalates and child IQ. This hypothesis is grounded on observations from epidemiological studies that showed a wide range of behavioral and cognitive outcomes affected by prenatal phthalate exposure. 12 – 14 These studies reported sex differences in neurodevelopmental outcomes associated with prenatal phthalate exposure. Therefore, we examined sex differences in the association between prenatal phthalate exposure and brain volumetric measures and further tested sex differences in brain alterations that explained the association between prenatal phthalate exposure and child cognition. Since a recent meta-analysis reported associations of moderate effect size between prenatal phthalate exposure and neurodevelopment in girls, 14 we hypothesize that sex-specific associations will be present in girls.
Materials and Methods
Study participants.
Participants were mother-child pairs from the Generation R Study, a population-based birth cohort in Rotterdam, the Netherlands. Briefly, Generation R recruited pregnant women with a delivery date between April 2002 and January 2006 in the city of Rotterdam. 31 – 33 A sample of women provided spot urine samples three times in pregnancy, which was used for measurement of phthalates and creatinine. Children and their families have been followed across various life stages using questionnaires and in-person visits, including brain MRI scans and other objective measurement of neuropsychological functioning. In total, 2083 pregnant women provided three spot urine samples during gestation [early (<18 weeks), mid- (18-25 weeks), and late pregnancy (>25 weeks of gestational age)]. In this group, phthalate metabolites were repeatedly measured in urine sample of 1431 women with singleton pregnancy who provided postnatal consent. 34 At age 10 years, participating children underwent brain MRI scans [mean age=9.8 years, standard deviation (SD) = 0.3] and at age 14 years children’s IQ was evaluated (mean age=13.48, SD=0.26). We included 775 mother-child pairs in the analysis with maternal urinary phthalate levels and good quality brain MRI. For a subgroup including 671 mother-child pairs, data on IQ at age 14 was also available. Additional mediation analyses including IQ were performed on these 671 mother-child pairs.
The Medical Ethics Committee of the Erasmus Medical Centre approved the study. Parents provided written informed consent, and confidentiality was guaranteed. We obtained assent from children older than age 12 years.
Phthalate Exposure
Urine samples of pregnant women were collected between 8 am and 8 pm in 100 mL polypropylene urine collection containers that were kept for a maximum of 20 h at 4°C before being frozen at −20°C in 20 mL portions in 25 mL polypropylene vials. Specimens were shipped on dry ice in 4 ml polypropylene vials to the Wadsworth Center, New York State Department of Health, Albany, New York for analysis of phthalate metabolites. Phthalate metabolite concentrations were determined using high performance liquid chromatography-electrospray ionization-tandem mass spectrometry (HPLC-ESI-MS/MS), with details of measurements reported elsewhere. 34 Briefly, urine samples were processed using enzymatic deconjugation of the glucuronidated phthalate monoesters followed by on-line solid phase extraction (SPE) coupled with reversed phase HPLC-ESI-MS/MS. This selective method allows for rapid detection of phthalate metabolites with limits of detection in the range of 0.1-0.5 ng/mL. We quantified concentrations of phthalic acid (PA), a proxy for total phthalate exposure, and 17 metabolites, included mnBP, monobenzyl phthalate (mBzP), monocyclohexyl phthalate, mono(7-carboxy-n-heptyl) phthalate, mono(2-carboxymethyl)hexyl phthalate (mCMHP), mCPP, mono(2-ethyl-5-carboxypentyl) phthalate (mECPP), mono(2-ethyl-5-hydroxyhexyl) phthalate (mEHHP), mono(2-ethyl-5oxohexyl) phthalate (mEOHP), mEP, mono(2-heptyl) phthalate, monohexyl phthalate, monoisobutyl phthalate (mIBP), mono(8-methyl-1-nonyl) phthalate, monoisononyl phthalate, monomethyl phthalate (mMP), and monooctyl phthalate. For phthalate metabolites with detection rate higher than 80%, concentrations below the limit of detection (LOD) were imputed by LOD/√2. We calculated ∑DEHP concentration as the molar sum of mECPP, mEHHP, mEOHP, and mCMHP concentrations, after imputing the levels below LOD by LOD/√2. 34 All metabolite concentrations were divided by creatinine level and effect sizes were expressed per increase in ng/g of creatinine for individual phthalates and μmol/g creatinine for ∑DEHP.
In Generation R, 3992 visited the center for brain MRI at age 10 years for whom brain images were acquired on a 3T General Electric scanner (MR750w, Milwaukee, WI). A high-resolution T 1 -weighted sequence was obtained using a 3D coronal inversion recovery fast spoiled gradient recalled sequence (T R =8.77 ms, T E =3.4 ms, T I =600 ms, flip angle=10°, field of view=220×220 mm, number of slices=230, voxel size=1.0 mm 3 , ARC acceleration factor=2). 31 Prior to the actual MRI scanning session, the children participated in a mock scanning session. Following the mock scanner session, the child was shown two pictures of an MRI scan of the brain, one with little movement and one with considerable movement. This was done to help the child visualize that the ‘pictures of the brain become blurred with movement’. In addition, if excessive movement was seen on the MRI console following image reconstruction, the scan was repeated.
Structural MRI data were processed through the FreeSurfer analysis suite, version 6.0 recon-all tool . 35 A number of automated steps were involved to segment the brain into multiple regions. These steps include the removal of nonbrain tissue, normalizing the image intensity to account for B1 inhomogeneities, whole-brain tissue segmentation, and creatubg a surface-based model of the cortex. Measures of global brain regions (e.g., total brain volume and subcortical volume), and a number of subcortical and cortical structures (amygdala, orbitofrontal cortex, etc.) were automatically labeled according to the Desikan-Killiany atlas. 36 For quality assessment, T 1 images underwent both visual inspection and an automated quality assessment measure for motion-related artifacts. 31 Images were once rated at the time of MRI acquisitions using a six-point Likert scale and scans were repeated for images with unusable or poor rating. After FreeSurfer reconstruction, 2-D segmentations and 3-D morphometry were visually inspected using a 3-point Likert scale with the following levels: “Excellent to Very Good,” “Good to Fair,” and “Poor to Unusable”. Eventually, scans were also systematically rated using an algorithm developed in house and tested in two external neuroimaging datasets. 37 To improve precision, the MRI quality score was added as a covariates to all association models (See below).
From 3992 children who visited the center for brain MRI, 806 scans were excluded, mainly due to poor/insufficient data quality after image processing (80%) as well as missing complete T 1 scan (14%), a different T 1 acquisition (3%), or incidental finding (3%). 38 Characteristics of children who were excluded because of poor quality scans (n=806) were comparable to 3186 children with brain scans (e.g., 49% boys in both groups, mean age = 10.1 at the time of scan or sociodemographic characteristics). See full characteristics in Table S1 ( Supplemental Information ). From 3186 with good quality images, data on prenatal phthalates were available in included 775 mother-child pairs who were included in this analysis (See above, Study Participants ).
To address our hypothesis regarding the global effect of prenatal phthalate exposure on brain development, we examined total brain, total gray matter, subcortical gray matter, cerebral white matter, and total cerebellum volumes. See Table S2 ( Supplemental Information ) for the list of labels included in the analysis.
During visits to the study’s research center at age 14 years, children’s IQ was assessed using the Wechsler Intelligence Scale for Children ® Fifth Edition (WISC ® -V, Pearson Clinical Assessment, San Antonio, Texas). 39 In collaboration with Pearson, four core subtests from the WISC-V were selected to assess specific cognitive domains and to derive an estimated full scale IQ. 40 All four subtest were administered by research assistants trained by a clinical neuropsychologist. The subtests included (1) Matrix reasoning , which measures fluid reasoning; (2) Coding , measuring processing speed; (3) Vocabulary , which measures verbal comprehension; and (4) Digit Span , to assess working memory.
The Matrix Reasoning and Coding subtests were administered to the child via the Q-Interactive system of Pearson 41 on an iPad Air 2 and while the examiner remained in the room. In a small subset (less than 5%), the tablet was not functioning at the time of the assessment and thus a paper/pencil version of the Matrix Reasoning and the Coding subtest was used.
In the Matrix Reasoning subtest, children were provided with an incomplete matrix and asked to select the completing response option. In the Coding subtest, children were introduced to a key with numbers and corresponding symbols and were asked to match as many numbers with the corresponding symbols within 2 min. For the Vocabulary subtest, children had to provide definitions for words read out loud by the examiner. Responses by children were recorded with an audio recorder, which were then used for scoring of the subtest, additional to the responses written down by the examiner. The Digit Span subtest consisted of three separate tasks. First, children were asked to repeat a sequence of numbers in the same order that the numbers were presented. Then they were asked to repeat a sequence of numbers in reverse order. Last they were asked to repeat a sequence ordered from low to high.
Matrix Reasoning and Coding were scored automatically, whereas the Digit Span subtest was scored by trained research assistants. The three subtasks were equally weighted to compute a Digit Span summary score. The Vocabulary subtest was also scored by trained the research assistants. All examiners first scored the same subset of tests, and if scoring was adequate (reliability higher than the predefined threshold of 0.9), they could continue scoring. If examiners were in doubt about what was written down on the forms, they were instructed to listen to the recording of the task and then decide on the score. Other issues about scoring were discussed in monthly meetings with other examiners
Raw subtest scores of the Vocabulary , Matrix Reasoning , Digit Span , and Coding subtests were summed and converted to a four-subtest estimated full scale IQ (See Table S3 in Supplementary Materials for Sum of Scaled Score Range). Age-standardized T-scores were calculated using Dutch norm-scores (data from Table A1 in the Dutch Manual of the WISC V). The reliability across 6 – 16 years was tested by Pearson, which shows high reliability of the custom index and similarity with a full-scale IQ (See Supplementary Table S4 for the intraclass correlation between custom index and a Pearson full-scale IQ for different age groups).
Other Measures
Information on maternal age (year), highest educational levels achieved, maternal national origin, and marital status was obtained with questionnaires at enrollment during pregnancy. We categorized educational levels as ‘low’ (no primary school/primary school), ‘intermediate’ (secondary school or lower vocational training), and ‘high’ (higher vocational training, university). National origin was grouped as ‘the Netherlands’ and ‘other than the Netherlands’. We combined categories of married and living with partners and compared to those with no partner. Pregnant women also reported their smoking habits at enrollment, in mid-pregnancy, and in late pregnancy. We defined any smoking during pregnancy (yes/no) using this information. Pre-pregnancy body mass index (BMI) (kg/m 2 ) was calculated using self-reported pre-pregnancy weight and height. Maternal non-verbal IQ was assessed using a computerized version of the Ravens Advanced Progressive Matrices Test, set I during age six visits of children. 42 Information on parity (nulliparous, yes/no) and a child’s sex and date of birth were obtained from hospitals and midwives records.
Statistical Analysis
Because phthalates have short half-life, the average urinary concentrations of metabolites are likely a better estimate of the exposure across gestation. Therefore, we calculated an average of creatinine-adjusted concentrations throughout pregnancy. Phthalate concentration were expressed on a creatinine basis and log10 transformed.
The primary research question was the association between phthalate metabolites and brain volumetric measures. We performed linear regression models to examine the associations of phthalate metabolite concentrations with brain volumes, adjusted for confounders (see below). To correct for multiple hypothesis testing accounting for the correlation between concentrations of eight phthalate metabolites, we used False Discovery Rate (FDR). 43 In a sensitivity analysis, we also examined a more conservative approach of using FDR-corrected p values for 40 tests (eight phthalate metabolites and five brain measures). We explored the non-linearity of associations between exposures and outcomes using a smoothing curve spline. To further explore if the associations between prenatal phthalate exposure and brain volumetric measures differed by sex, we added interaction terms between phthalate measures and sex to the models and also stratified the analyses of phthalates/brain measures by sex.
We used linear regression models to examine the associations of phthalate metabolite concentrations with child IQ (full scale IQ score and the four domains), adjusted for confounders. The total effect of a specific exposure on an outcome might be very small or close to null, while in fact mediation effects exist. 44 Therefore, we pursued mediation analyses if associations were observed with a specific phthalate metabolite and brain volumetric measures, even when the associations between specific phthalates and child IQ were not significant in our sample. We used causal mediation analysis providing estimation of the natural direct effect, the natural indirect effect, and the total effect 45 and calculated proportion mediated (ratio of natural indirect effect and total effect). Indirect effects represent the effect of phthalate exposure on IQ that is mediated via brain volumes, while the direct effect denotes the remaining part of the total effect and represents the effect of phthalate exposure on IQ not mediated through brain volumes. The natural effect models were adjusted for potential exposure-outcomes, exposure-mediator, and mediator-outcome confounders (as listed below). Standard errors were calculated using bootstrapping. If interaction terms (phthalates X sex) were significant, we further tested if the association between prenatal phthalates and child IQ mediated by brain volumetric measures was moderated by sex (moderation of the mediated effect).
We selected potential confounders based on the directed acyclic graphs and factors shown to be associated with exposure or outcomes. 13 , 14 , 16 , 34 Models were adjusted for maternal age, national origin, marital status, IQ score, BMI, parity, smoking during pregnancy, and child sex and age at the neuroimaging assessment. Models with neuroimaging outcomes were also adjusted for MRI quality score and models with cerebellar volume for intracranial volume (ICV) to ascertain relativity to head size. There were high correlations between measures of total gray matter, subcortical gray matter, and cerebral white matter volumes and ICV (r=0.81-0.90), so models with these measured were adjusted for ICV in an additional step.
Missing data for covariates were: maternal body mass index in 93 (12%), parity in 2 (0.3%), national origin in 4 (0.5%), education in 23 (3%), marital status in 33 (4%), smoking in 67 (9%), and IQ in 11 individuals (1 %); child IQ in 104 (13%) individuals. We used the Multivariate Imputation by Chained Equations (MICE) method in R to impute the missing values for covariates, creating 20 imputed datasets using 25 iterations. 46 – 49 Mediation analysis were performed within all 20 imputed datasets, and since the results were similar across sets, we present findings from the 10 th and 20 th sets, randomly. For all other analyses, we present the results of combined effect estimates across imputation sets.
Within Generation R, factors predicted inclusion in this study were maternal age, education, national origin, and IQ, parity, household income, and child gestational age at birth. We used information on these factors to estimate the probability of participation in the study and applied the inverse of those probabilities as weights in all analyses to examine if the selective nonresponse influenced our findings.
Code availability
Analyses were performed in R Package version 3.4.1. Codes will be available upon request and communication with the corresponding author.
Table 1 presents participants’ characteristics. Pregnant women were on average 31.0 years (SD=4.6) at enrollment and mostly had Dutch national origin (n=439, 56.9%). More than half of women had high education levels (n=420, 55.9%), and 168 women (23.7%) smoked at any point during pregnancy. The mean (SD) full scale IQ score of children at age 14 years was 103.0 (SD=13.2). Median and interquartile range of phthalate metabolites detected in at least 80% of the samples are presented in Table S5 ( Supplemental Information ). These included mMP, mEP, mIBP, mnBP, mBzP), mCPP, metabolites of DEHP, as well as PA (See Table S6 for the correlation between phthalates). Intraclass correlation coefficients (ICC, estimated by using a 2-way mixed-effects model with absolute agreement) for phthalate measures varied between 0.37 (∑DEHP) and 0.68 (mEP) for the average of the three measurements across pregnancy. Concentrations of mEP was the highest among all metabolites measured.
Participants’ characteristics (n=775). The Generation R Study.
| Maternal characteristics | |
|---|---|
| Age at enrollment, years; mean (SD) | 31.0 (4.6) |
| Pre-pregnancy BMI; mean (SD) | 23.5 (4.1) |
| Parity; n (%) | |
| 0 | 487 (63.0) |
| ≥ 1 | 286 (37.0) |
| National origin; n (%) | |
| the Netherlands | 439 (56.9) |
| Others | 332 (43.1) |
| Education; n (%) | |
| Low | 97 (12.9) |
| Intermediate | 235 (31.2) |
| High | 420 (55.9) |
| Marital status; n (%) | |
| Married/living with partner | 663 (89.4) |
| No partner | 79 (10.6) |
| IQ score; mean (SD) | 98.6 (14.4) |
| Any smoking during pregnancy; n (%) | 168 (23.7) |
| Child characteristics | |
| Child sex, boys; n (%) | 390 (50.3) |
| Full scale IQ score at age 14 years; mean (SD) | 103.0 (13.2) |
| Total brain volume at age 10 years, cm ; mean (SD) | 1211.3 (106.1) |
| Total gray matter volume at age 10 years, cm , means (SD) | 761.4 (63.1) |
| Cerebral white matter volume at age 10 years, cm , means (SD) | 422.9 (46.2) |
| Subcortical gray matter volume at age 10 years, cm , means (SD) | 60.3 (4.5) |
| Total cerebellum volume at age 10 years, cm , means (SD) | 144.1 (13.1) |
Body mass index: BMI; Magnetic resonance imaging: MRI; Standard deviation: SD
Associations of prenatal phthalate exposure with brain volumetric measures
Table 2 summarizes the associations of maternal urinary concentration of phthalate metabolites (averaged across pregnancy) with brain global and regional volumetric measures in children aged 10 years. After correction for multiple comparisons using FDR, higher gestational concentrations of maternal mEP were associated with smaller total gray matter volumes (β per log10 increase in creatinine adjusted mEP=−10.70, 95%CI: −18.12, −3.28), but not with other brain volumetric measure. When we adjusted the models with total gray matter, cerebral white matter, and subcortical gray matter for ICV, we found a significant association between prenatal mIBP exposure and total gray matter volume (β=−8.11, 95%CI: −13.56, −2.66) that remained significant with FDR correction ( Table S7 in the Supplemental Information ). The associations between other phthalate metabolites and brain measures did not remain significant after correction for multiple comparisons using FDR. When we used P FDR for 40 tests, none of the associations remained significant. We found no indication of non-linearity in the association between phthalate metabolite concentrations and brain measures (data not shown).
Associations of prenatal exposure to phthalate metabolites (averaged across pregnancy) with brain structure at age 10 years. The Generation R Study.
| Brain volumes, cm (n=775) | |||||
|---|---|---|---|---|---|
| Global measures | Regional measures | ||||
| Total brain | Total gray matter | Cerebral white matter | Subcortical gray matter | Total cerebellum | |
| β 95%CI | β 95%CI | β (95%CI) | β (95%CI) | β (95%CI) | |
| −3.19 (−21.67, 15.28) | −0.91 (−11.67, 9.85) | −2.22 (−10.66, 6.23) | 0.15 (−0.69, 0.99) | −1.34 (−3.37, 0.70) | |
| −5.22 (−11.06, 0.62) | −0.55 (−1.13, 0.03) | −0.65 (−2.06, 0.77) | |||
| 2.01 (−21.51, 25.53) | 1.28 (−12.43, 14.99) | 1.10 (−9.63, 11.83) | 0.59 (−0.49, 1.66) | −2.38 (−4.95, 0.20) | |
| −16.14 (−35.41, 3.13) | −10.87 (−22.10, 0.36) | −4.78 (−13.58, 4.01) | −0.2 (−1.08, 0.67) | ||
| −6.81 (−28.15, 14.52) | −3.53 (−15.97, 8.90) | −2.94 (−12.68, 6.8) | 0.43 (−0.54, 1.41) | −1.49 (−3.83, 0.85) | |
| −10.38 (−26.56, 5.79) | −6.18 (−15.60, 3.23) | −4.00 (−11.39, 3.39) | −0.27 (−1.01, 0.47) | −0.96 (−2.73, 0.81) | |
| 7.47 (−17.07, 32.01) | 3.06 (−11.24, 17.36) | 4.65 (−6.55, 15.86) | 0.53 (−0.59, 1.65) | −2.50 (−5.20, 0.19) | |
| −18.47 (−41.43, 4.49) | −14.30 (−27.66, −0.94) | −3.61 (−14.11, 6.90) | −0.41 (−1.45, 0.64) | ||
CI: confidence interval; DEHP: di-2-ethylhexyl phthalate; mnBP: mono-n-butyl phthalate; mBzP: monobenzyl phthalate; mCPP: mono(3-carboxypropyl) phthalate; mEP: monoethyl phthalate; mIBP: monoisobutyl phthalate; mMP: monomethyl phthalate.
Models were adjusted for maternal age, national origin, education, marital status, IQ score, pre-pregnancy body mass index, parity, smoking during pregnancy, MRI quality score, and child sex and age at the neuroimaging assessment. Models with total cerebellar volume were additionally adjusted for intracranial volume.
Bold: association with p-value <0.05.
Estimates are reported per log10 increase in creatinine adjusted maternal urinary phthalate concentrations (ng/g of creatinine of individual phthalates and μmol/g creatinine for ∑DEHP).
We found sex interactions in associations of maternal mIBP concentrations with cerebral white matter volumes (significant after correction for multiple comparison, P FDR = 0.04). We examined the associations across strata of sex and found that girls with higher phthalate exposure, including mIBP and mEP, had smaller volumes in several brain features ( Table S8 ). The associations of prenatal phthalate exposure with brain volumetric measures were not present in boys ( Table S9 ).
Associations of prenatal phthalate exposure with child cognition and mediation by brain morphology
Table 3 shows the associations between maternal phthalate metabolite concentrations and child cognition (total IQ scores and subtests) at age 14 years. Children exposed to higher maternal mEP and mnBP concentrations had lower IQ: β for matrix reasoning per log10 increase in creatinine adjusted mEP = −0.45, 95%CI: −0.84, −0.07; and β for verbal vocabulary per log10 increase in creatinine adjusted mnBP −0.97, 95%CI: −1.65, −0.29.
Associations of prenatal exposure to phthalate metabolites (averaged across pregnancy) with and child IQ at age 14 years (n=671). The Generation R Study.
| Full scale IQ score | Vocabulary | Matrix Reasoning | Digit Span | Coding | |
|---|---|---|---|---|---|
| β (95%CI) | β (95%CI) | β (95%CI) | β (95%CI) | β (95%CI) | |
| 0.91 (−1.91, 3.73) | 0.15 (−0.45, 0.75) | 0.02 (−0.54, 0.58) | 0.24 (−0.36, 0.84) | 0.14 (−0.58, 0.86) | |
| −1.68 (−3.61, 0.25) | −0.13 (−0.54, 0.28) | −0.32 (−0.73, 0.09) | −0.08 (−0.57, 0.41) | ||
| −1.42 (−5.07, 2.24) | −0.58 (−1.36, 0.19) | 0.41 (−0.32, 1.14) | 0.11 (−0.66, 0.89) | −0.76 (−1.69, 0.16) | |
| −0.53 (−3.42, 2.36) | −0.52 (−1.13, 0.09) | −0.37 (−0.94, 0.21) | 0.56 (−0.06, 1.17) | 0.01 (−0.72, 0.74) | |
| −3.15 (−6.39, 0.09) | (−1.65, −0.29) | −0.23 (−0.88, 0.41) | −0.20 (−0.89, 0.49) | −0.49 (−1.31, 0.34) | |
| 1.08 (−1.437, 3.59) | −0.09 (−0.62, 0.44) | 0.39 (−0.11, 0.89) | 0.42 (−0.12, 0.95) | −0.06 (−0.70, 0.58) | |
| −1.83 (−5.59, 1.93) | −0.44 (−1.23, 0.36) | −0.10 (−0.85, 0.65) | −0.21 (−1.01, 0.58) | −0.34 (−1.29, 0.62) | |
| −1.82 (−5.35, 1.72) | −0.44 (−1.19, 0.31) | −0.23 (−0.93, 0.48) | −0.42 (−1.17, 0.33) | 0.03 (−0.87, 0.92) | |
Models were adjusted for maternal age, national origin, education, marital status, IQ score, pre-pregnancy body mass index, parity, smoking during pregnancy, and child sex and age at the IQ assessment.
Estimates are reported per log10 increase in creatinine adjusted maternal urinary phthalate concentrations (ng/g of creatinine of individual phthalates and μmol/g creatinine for ∑DEHP)
We next examined the extent to which brain volumetric measures that were associated with mEP and mIBP exposures, i.e., total gray and white matter volumes, mediated the association of prenatal phthalates and child general IQ. We observed that smaller total gray volumes partially mediated the association between prenatal mEP exposure and lower full scale IQ scores (natural indirect effect which shows the mediated path: β per log10 increase in creatinine adjusted mEP = −0.31, 95%CI: −0.62, 0.01; proportion mediated = 18%) ( Figure 1 and Figure S1 ). We did not pursue mediation analysis with subcortical measure residualized for intracranial volumes because we found no associations between residualized measures and child IQ. We found that the mediated path by white matter volume in the association of mIBP exposure and child IQ was present in girls (natural indirect effect: β per log10 increase in creatinine adjusted mIBP = −1.08, 95%CI: −1.95, −0.16), but not in boys ( Figure 2 and Figure S2 ).

Associations between prenatal monoethyl phthalate (mEP) exposure (averaged across pregnancy) and child full scale IQ score at age 14 years, mediated by total gray matter volume at age 10 years.
Models were adjusted for maternal age, national origin, education, marital status, IQ score, pre-pregnancy body mass index, parity, smoking during pregnancy, MRI quality score, and child sex and age at the neuroimaging assessment and/or age at assessment child IQ. Data shown from the 20 th imputation set.

Associations between prenatal monoisobutyl phthalate (mIBP) exposure and child full scale IQ score at age 14, mediated by cerebral white matter volume at age 10 years in girls (A) and boys (B).
Models were adjusted for maternal age, national origin, education, marital status, IQ score, pre-pregnancy body mass index, parity, smoking during pregnancy, MRI quality score, and child age at the neuroimaging assessment and/or age at assessment child IQ. P value for sex interaction: 0.01. Data shown from the 20 th imputation set.
We found that higher maternal prenatal concentrations of mEP were associated with smaller total gray matter volumes in offspring at age 10 years. Smaller gray matter volumes partially mediated the association between higher maternal mEP and lower child full score IQ at age 14 years. In the association between prenatal mEP exposure and child full scale IQ scores, the proportion mediated by total gray matter volumes was 18%. The inverse association of higher mIBP and lower child IQ was mediated by smaller cerebral white matter volumes only in girls, with a proportion mediated of 76%. While effect sizes were overall small, for example, one-sixth of SD deviation decrease total gray matter volumes per 10 times increase in mEP exposure, these findings have high public health impact because of the high and widespread exposure to phthalates and poor regulations in pregnant populations. Moreover, we observed a pattern in the data that suggested an inverse relationship between phthalates with low molecular weights associated with smaller volumetric measures, even though the estimates were imprecise.
This study is the first to investigate the brain volumetric measure associated with prenatal phthalate exposure using brain MRI. Strengths include the large sample size and the availability of data on important confounders, such as maternal IQ. We used biomonitoring, with multiple urine samples during pregnancy, which is the method of choice for measuring rapidly metabolized organic compounds. 50 Findings of this study should be interpreted considering the following limitations. First, phthalates are non-persistent chemicals with a short half-life and urine spot samples during pregnancy might not be the accurate reflection of the whole pregnancy exposure and long-terms effects of early life exposure should be interpreted considering this limitation. In this sample, we observed moderate ICCs between the three measures of phthalates in pregnant women and subsequently used concentrations of metabolites from three spot urine samples in the main analyses; yet, measurement error remains an issue in studies of non-persistent chemicals. 51 Particularly, the short half-lives of these chemicals should be considered when interpreting trimester-specific analyses. Second, we did not examine exposure to plasticizers that are used as replacement of DEHP, while their potential neurotoxicity is a growing concern and relevant to more recent cohorts. 12 Third, although we adjusted the models for several confounders, residual confounding by unmeasured factors cannot be ruled out. This is particularly important for the mediation analysis, which was performed under the assumption that no unmeasured confounding existed on any of the paths. Fourth, to minimize the participant burden, we used four subtests of WISC ® -V. These subtests were selected from the 10 core subtests that are usually used to measure the four index scores to measure full IQ score, but lack information on other important constructs such as visual spatial scale. Last, Generation R sample represents the diversity of Rotterdam and its surrounding area, and as such participants reported a wide spectrum of backgrounds. Because many of these groups have a small number of participants in the Generation R Study, we operationalized this data as a two-category variable.
Developmental neurotoxicity of certain phthalates, e.g., DEHP and DBP, is widely studied in experimental studies, with possible mechanisms suggested to be thyroid disruption, 52 epigenetic modifications, 53 or sex hormone disruption. 54 Influences of phthalates on sex hormones are particularly important during the organizational effects of gonadal steroids on fetal brain development. 55 Experimental data also suggest that the effect of phthalate exposure on brain development can be both global and early (e.g., interference in the cytoarchitecture of neocortex 20 ) and region-specific (e.g., morphology of specific structures such as the cerebellum 18 , 53 ). Epidemiological data in humans applying neuroimaging to investigate the impact of prenatal phthalate exposure on the brain are limited. One report from the Alberta Pregnancy Outcomes and Nutrition (APrON) study showed associations between high molecular weight phthalates (metabolites of DEHP and BBzP), measured once in mid-pregnancy, and impairments in structural connectivity (white matter microstructure) in preschool age children. 30 But the APrON study did not examine global or regional volumetric measures of the brain, while brain structural measures are shown to be implicated in children’s behavioral and cognitive functioning, e.g., the established relationship of cortical and subcortical gray matter volumes with IQ. 22 , 23 The present study is the first to examine the associations of prenatal phthalate exposure with offspring brain volumetric measure and potential implications for general cognition. We found that higher prenatal exposure to mEP, a metabolite of DEP, was associated with a global effect on the brain, as seen with smaller gray matter volume. Higher exposure to mEP was associated with lower scores in Matrix Reasoning. Fluid reasoning, important for later achievement and academic performance, 56 is highly heritable but the role of environmental factors are also proposed, particularly in earlier stages of development. 57 Our current analysis extends our earlier report of an association between prenatal mEP and child non-verbal IQ at age six years 15 , 16 by showing that the impact of prenatal phthalate exposure on the brain and child cognition continues into adolescence. DEP is less often examined in experimental studies (as opposed to DEHP and DBP); with few studies confirming that DEP exposure can interfere with brain processes, 58 , 59 and others report no effect. 60 It is important to note that DEP is the phthalate to which individuals are most highly exposed, 14 which was also found in this sample (see Table 2 for concentrations of urinary mEP concentrations, a metabolite of DEP). Thus, it is critical to identify exposure reduction strategies for DEP, possibly similar to current regulations that exist for DEHP, for example.
Our findings on sex differences in the associations of prenatal phthalates with brain measures was expected based on earlier studies of child cognition and behavior. 13 , 14 A recent meta-analysis of epidemiological studies on prenatal phthalate exposure and several neurodevelopmental outcomes concluded that despite some inconsistencies, girls are often more susceptible to exposure to diisobutyl phthalate (DIBP, the parent compound of mIBP) for lower motor and cognitive abilities. 14 For example, two studies reported associations between higher DIBP exposure (measured by urinary mIBP) and lower child cognition only in girls. 61 , 62 Our study, with a large sample size that allowed examination of sex interaction and mediation analysis, provides the first evidence on the neural substrate for sex differences in cognitive outcomes associated with mIBP exposure. Phthalates interfere with sex hormone production and are associated with estrogenic and anti-androgenic reproductive effects in males and females. 54 Fetal exposure to both androgens and estrogens are associated with differential growth in sexually dimorphic brain areas. 55 Anti-androgenic effects of phthalates in girls, in particular mid-gestation through the end of gestation, might interfere with brain organizational development.
Findings from models adjusted for the ICV showed also associations with smaller total gray matter volumes, but in with mIBP exposure (compared to associations with mEP in models not adjusted for ICV). We speculate that these differences might be due to the mechanism of action of phthalate compounds (specific vs global effect) that should be investigated further in mechanistic studies.
In conclusion, despite increased regulations for certain phthalates, such as DEHP in the US and EU for childhood exposure, our findings suggest the global impact of prenatal exposure to phthalates, such as mEP and mIBP that are less regulated, through adolescence. Further investigations are warranted, which replicate our findings on brain global measures in larger and more diverse samples and further examine associated regional differences. Sex differences in some associations indicate potential involvement of sex steroid signaling pathways, which should be investigated in future mechanistic studies.
Supplementary Material
Supplementary materials, acknowledgments.
The Generation R Study is conducted by the Erasmus Medical Center in close collaborations with the School of Law and Faculty of Social Sciences of the Erasmus University Rotterdam, the Municipal Health Service Rotterdam area, Rotterdam, the Rotterdam Homecare Foundation, Rotterdam and the Stichting Trombosedienst and Artsenlaboratorium Rijnmond (STAR-MDC), Rotterdam. We gratefully acknowledge the contribution of children and parents, general practitioners, hospitals, midwives and pharmacies in Rotterdam.
The general design of the Generation R Study is made possible by financial support from the Erasmus Medical Center, Rotterdam, the Netherlands, the Organization for Health Research and Development (ZonMw) and the Ministry of Health, Welfare and Sport. This study was supported by grant R01ES022972 and R01ES029779 from the National Institutes of Health (NIH) to LT. Neuroimaging and infrastructure was supported by the Netherlands Organization for Health Research and Development (ZonMw) TOP project number 9121102. The work of AG is supported by grant R01ES032826 from NIH. The work of MD is supported by grant 824989 from the Horizon2020 programme of the European Union. HT is supported by the ZonMW grant 016.VICI.170.200. MG is funded by a Miguel Servet fellowship (CPII18/00018) awarded by the Spanish Institute of Health Carlos III. We acknowledge support from the Spanish Ministry of Science and Innovation through the “Centro de Excelencia Severo Ochoa 2019-2023” Program (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program. SME was supported by P30ES010126 and R01ES021777. VWVJ and MG received funding from the European Union’s Horizon 2020 research and innovation programme (Grant Agreement No. 733206 LifeCycle and Grant Agreement No. 874583 ATHLETE). The research was supported in part by the Intramural Research Program of the NIMH.
Conflict of Interest
The spouse of H.T. is an employee of Eastman Chemical, a company that manufactures substitutes for ortho-phthalate plasticizers. Other authors have no conflict of interest.

IMAGES
VIDEO
COMMENTS
Dr. Tiemeier received both his medical and sociological degree from the University of Bonn, Germany, and his PhD from the Erasmus University in Rotterdam, Netherlands. Since 2018, he leads the Maternal and Child Center of Excellence at Harvard Chan. As one of just 13 HRSA-funded Centers of Excellence in Maternal and Child Health in the United ...
Harvard TH Chan School of Public Health. Henning Tiemeier is a psychiatric epidemiologist who studies child development in population-based cohort studies. His work has a particular focus on prenatal exposures such as maternal depression, cannabis, or low thyroid function. Much of his work takes a neurodevelopmental approach and his group ...
Henning Tiemeier, MD, PhD, was recently appointed as the Esther Feldberg Professor of Maternal and Child Health in the Department of Social & Behavioral Sciences. Dr. Tiemeier will also serve as the Director of the Maternal and Child Health Training Grant.
Henning Tiemeier, MA, MD, PhD, is Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair of Maternal and Child Health at the Harvard T.H. Chan School of Public Health. Dr. Tiemeier received both his medical and sociological degree from the University of Bonn, Germany, and his PhD from the Erasmus University in Rotterdam, Netherlands.
Faculty Spotlight: Henning Tiemeier Can you tell us about your research background and what drew you to the SBS Department and more specifically to Maternal and Child Health? About 15 years ago, I began studying child development and in particular child psychiatric problems.
677 Huntington Ave., 6th floor, Room 619, Boston, MA 02115. E-mail: [email protected] . Relevant Links. Harvard School of Public Health profile. Google Scholar. Research. Tiemeier has worked broadly in psychiatric epidemiology for more than 20 years with a focus on child developmental research.
Associate Editor Allie Oh interviewed Henning Tiemeier, MA, MD, PhD, a Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair of Maternal and Child Health at the Harvard T.H. Chan School of Public Health. Dr. Tiemeier received both his medical and sociological degree from the University of Bonn, Germany, and his PhD ...
Henning Tiemeier, MD, PhD, and Rosanne Freak-Poli, PhD, are the recipients of the 2023 Alzheimer Award J Alzheimers Dis. 2023 Jul 20. doi: 10.3233/JAD-239005. Online ahead of print. PMID: 37483009 DOI: 10.3233/JAD-239005 No abstract available ...
Henning Tiemeier. Social and Behavioral Science, Harvard T.H. Chan School of Public Health, Erasmus University ... MG Nivard, MA Fontana, ... Nature genetics 48 (6), 624-633, 2016. 1109: 2016: Genome-wide meta-analyses identify multiple loci associated with smoking behavior. Nature genetics 42 (5), 441-447, 2010. 1109: ... H Tiemeier, HR Van ...
This annual award recognizes outstanding contributions to the advancement of AD research published in the Journal of Alzheimer's Disease. Amsterdam, the Netherlands - The Journal of Alzheimer's Disease (JAD) is pleased to announce the joint recipients of the 2023 Alzheimer Award are Henning Tiemeier, MD, PhD, Erasmus Medical Center, Rotterdam, and the Harvard TH Chan School of Public ...
Henning Tiemeier, MA MD PhD, is Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair in Maternal and Child Health at HSPH. He is also Professor of Psychiatric Epidemiology at the Erasmus Medical Center in Rotterdam, Netherlands. ... Dr. Henning Tiemeier presents "Intrauterine exposures and child development ...
Zou R, Tiemeier H, van der Ende J, et al. Exposure to maternal depressive symptoms in fetal life or childhood and offspring brain development: a population-based imaging study. Am J Psychiatry . 2019;176(9):702-710. doi: 10.1176/appi.ajp.2019.18080970 PubMed Google Scholar Crossref
Objective: To investigate the association between intrauterine SSRI exposure and maternal depressive symptoms and structural brain development in offspring from mid-childhood to early puberty. Design, setting, and participants: This prospective, population-based cohort study was embedded in the Generation R Study in Rotterdam, the Netherlands.
Jill S. Roncarati, ScD, MPH, PA-C, National Cancer Institute Postdoctoral Fellow, Henning Tiemeier, MA, MD, PhD, Professor of Social and Behavioral Science, Rebecca Tachick, BHCHP Street Team Manager, Tyler J. VanderWeele, PhD, John L. Loeb and Frances Lehman Loeb Professor of Epidemiology, and James J. O'Connell, MD, Assistant Professor, Harvard Medical School,President Boston Health Care ...
Harvard T.H. Chan School researchers are involved in projects promoting global health on nearly every continent. From advancing scientific discovery to training international health leaders, Harvard Chan School is at the forefront of efforts to benefit the health of populations worldwide.
Henning Tiemeier, MA, MD, PhD, is Professor of Social and Behavioral . Science and the Sumner and Esther Feldberg Chair of Maternal and Child : Health at the Harvard T.H. Chan School of Public Health. Dr. Tiemeier received both his medical and sociological degree from the . University of Bonn, Germany, and his PhD from the Erasmus University in
Henning Tiemeier, MA, MD, PhD Professor of Social and Behavioral Science and the Sumner and Esther Feldberg Chair of Maternal and Child Health, Harvard T.H. Chan School of Public Health. April 25, 2023 Viola Bernard Special Lecture Jessica Cerdena, PhD MD Candidate and Medical Anthropologist at Yale. May 2, 2023
Background: Evidence suggests a link between depressive symptoms and risk of subsequent stroke. However, most studies assess depressive symptoms at only one timepoint, with few examining this relationship using repeatedly measured depressive symptoms. This study aimed to examine the relationship between depressive symptom trajectories and risk of incident stroke. Methods: This prospective ...
PhD Candidate, Harvard T.H. Chan School of Public Health Associate Director, Maternal Health Task Force. Crystal M. Hayes. PhD, MSW, Birth Doula at the University of North Carolina at Chapel Hill Gillings School of Global Public Health ... Henning Tiemeier, MA, MD, PhD. Professor of Social and Behavioral Science, Sumner and Esther Feldberg ...
Amsterdam, the Netherlands - The Journal of Alzheimer's Disease (JAD) is pleased to announce the joint recipients of the 2023 Alzheimer Award are Henning Tiemeier, MD, PhD, Erasmus Medical Center, Rotterdam, and the Harvard TH Chan School of Public Health, and Rosanne Freak-Poli, PhD, Monash University.
This cohort study analyzed data obtained between 2016 and 2019 from the Adolescent Brain Cognitive Development Study at 21 sites in the US. The sample included children aged 9 to 11 years of genetically assigned European ancestry with self-reported screen time. Data were analyzed between November 2021 and September 2023.
Boston, MA 02115 Open to the Public Refreshments will be provided Brain Imaging in Child Psychiatric Research: Novel Toy or Cool Tool? Henning Tiemeier, MD, PhD Sumner and Esther Feldberg Professor of Maternal and Child Health, Department of Social and Behavioral Sciences Harvard T.H. Chan School of Public Health
The work of MD is supported by grant 824989 from the Horizon2020 programme of the European Union. HT is supported by the ZonMW grant 016.VICI.170.200. MG is funded by a Miguel Servet fellowship (CPII18/00018) awarded by the Spanish Institute of Health Carlos III.