Human Services Organizations: Partnering for Better Community Health
Healthy outcomes initiative report and resources.
Human services organizations play a vital role in health by addressing the "social determinants of health" – economic stability, education, social connection, housing, safe neighborhoods, and food access. Human Services Organizations: Partnering for Better Community Health explores how collaboration between human services organizations and health systems can help people experience better health outcomes.
The report and comprehensive resources below capture knowledge and insights from the Healthy Outcomes Initiative, a multi-year project supported by The Kresge Foundation , and are intended for those new to human services and health collaborations as well as pioneering practitioners. Click through to explore resources, actionable research, and recommendations for community-based human services organizations to work more effectively with health systems.
Want the whole story? Download and read our full report.
- About the Healthy Outcomes Initiative
- Why human services organizations are increasingly partnering with health systems
- Examples of collaborations
- What it takes to partner successfully
- How pioneers are institutionalizing collaborative models
- Challenges in making collaboration work
- NFF's recommendations for how to accelerate this movement
- Initiative partners and project descriptions for deep-dive consulting engagements with NFF
- Full list of resources
"Seamless coordination between human services and healthcare organizations greatly increases well-being and opportunity for people, especially those with low-incomes. This is why the work of the Healthy Outcomes Initiative is essential for helping the health and human services sectors move beyond collaboration to integration." David Fukuzawa, Managing Director of The Kresge Foundation’s Health and Human Services Programs

1. About the Healthy Outcomes Initiative
The Healthy Outcomes Initiative (HOI) explored how partnership and integration between community-based human services organizations and health systems can propel large-scale improvements in the health of America’s communities.
In the Initiative, NFF:
- Built capacity through cohort-based group trainings and intensive, person-to-person consulting with human services organizations embarking on health partnerships, particularly those centering on outcomes. Click here for a complete list of HOI participants, and here for more detail on this work.
- Developed the Nonprofit Readiness for Health Partnership tool to help human services organizations prepare to engage in partnerships with healthcare organizations
- Created and shared knowledge on this dynamic issue through briefings with cross-sector stakeholders, conference presentations, and blogs, articles, and case studies, many of which are linked on this page.
- Fostered cross-sector dialogue through a Learning Network that featured six free virtual panel discussions with leaders in the field.
Learning Network Convenings:
- Context and Partnership Landscape (December 2016), with Kristin Giantris of NFF, and Michael Shaw of The Kresge Foundation
- Choosing A Partner (March 2017), featuring Project Nightingale partners: Jen Lewis and Jenny Symons of Sonoma County Health Department, and Daniel Schurman of St. Joseph Hospital
- Infrastructure, Culture, and Mission Alignment (July 2017), with Paul Castro and Todd Sosna of Jewish Family Services of Los Angeles, and featuring the report Working Together Toward Better Health Outcomes
- Key Capacities for Partnership (October 2017), featuring Angela Bovill and Tim Johnstone of Ascentria, and Jeremy Moore of Spectrum Health; NFF also presented two free tools, the Nonprofit Readiness for Health Partnership , and the Partnership Assessment Tool for Health
- Partnership and a Pay for Success model (February 2018), with Stephanie Mercier of Corporation for Supportive Housing and Dave Sharar of Chestnut Health Systems on early stage efforts to employ Pay for Success models to improve the health outcomes among homeless populations in McLean County
- Addressing Social Determinants of Health (May 2018), featuring Lutheran Social Services of North Dakota and the California Food is Medicine Coalition, both of whom are negotiating contracts with state programs

(back to top)
2. Why human services organizations are increasingly partnering with health systems
Healthcare in the US is rife with patient dissatisfaction , soaring costs, and poor outcomes , all of which are particularly acute in low-income communities . Amid these challenges, a collective understanding has emerged that housing, employment, economic stability, education, neighborhood safety, nutrition/food security, and social connection shape a person’s well-being far more than medical care alone.
As the experts in addressing these “social determinants of health” and in providing social services in community settings, human services organizations play a critical role in achieving healthy outcomes . Unifying the formerly distinct sectors of human services and healthcare is key to transforming health outcomes in the US.
“A health system that can figure out how to work really collaboratively with community-based organizations will most definitely see improved health status of the people that they serve.” Jeremy Moore, Director of Community Health Innovations at Spectrum Health
3. Examples of collaborations
Pioneering human services organizations are working with hospitals, insurers, and government agencies to provide integrated whole-person care. While initially accelerated by the Affordable Care Act , the shift from “volume-based” to “value-based” care varies greatly according to state and local policies and leadership, waivers and pilot programs, and the unique needs of communities. Changing incentives, coupled with poor health outcomes and rising costs, have spurred a wave of partnerships between human services and healthcare organizations to address pressing issues, such as the opioid crisis , homelessness , chronic disease , infant mortality , “super-use” of emergency rooms , recidivism , and others .
A spectrum of integration exists among human services organizations/healthcare partnerships. Sometimes, partners are simply sharing information or making referrals. In deeper partnerships, providers are coordinating their services to serve people more holistically. Some go yet further and share staff, space, and/or resources. At the most integrated end of the continuum, multiple partners are forming new approaches with cohesive programs, planning, and funding.
These projects – like all efforts at greater integration of human services and healthcare – aim to harness data on both outcomes and cost to demonstrate the power of collaborative approaches.

4. What it takes to partner successfully
For human services organizations:
Investments in capacity and capital are often necessary to support effective partnership , such as:
- Financial management consulting to assist in mapping the growth and change implications of collaboration to equip leaders to negotiate fair and sustainable contracts.
- Increased reserves to help human services organizations mitigate risk and weather the ups and downs of exploring new approaches and partnerships in a changing funding environment.
- Data infrastructure and expertise to measure outcomes and the full cost associated with new approaches and provide the evidence to propel these models into the mainstream.
As part of HOI, NFF developed the Nonprofit Readiness for Health Partnership tool, a free downloadable resource for human services organizations to help identify investments they may need to be ready for partnership .
For healthcare organizations
Partnership also demands operational and cultural shifts on the healthcare side, to allow for joint decision-making and planning (with human services organizations), and to measure and bill for overall health outcomes as opposed to treatments and services. Like human services organizations, healthcare partners often need to bolster their capacity and infrastructure for collection, sharing, and analyzing data. The sharing of data can, in particular, be a new and sometimes uneasy prospect for traditional healthcare, as data has often been regarded as constrained by privacy regulations, proprietary, and a source of competitive advantage.
Developing a shared language . Human services organizations must articulate their value in dollars as well as mission; and healthcare must shift from seeing human services partners as “do-gooders” to recognizing them as strategic partners that drive improved health.
“To prepare for a partnership, organizations must self-assess to revamp their model. A focus on mission, the mechanics of contracting and billing, administrative and financial burdens, and program delivery models are crucial.” Alissa Wassung, Director of Policy and Planning (and trailblazing collaborator), God’s Love We Deliver

5. How pioneers are institutionalizing collaborative models
HOI identified a wave of efforts to institutionalize successful pilots within regular contracting practices and/or expand them into broader arenas to provide stable long-term funding for essential human services . Key to these efforts is in-depth financial modeling to ensure that full costs of growth, change due to new collaborative models of operating, data measurement, and ultimately, service delivery, are incorporated.

6. Challenges in making collaboration work
Vast differences between human services and health organizations.
- Cultural differences : There is a natural tension between the mission-driven role of human services organizations to address complex socioeconomic barriers and the traditional role of healthcare to address acute medical needs. These diverse orientations have led to differences in priorities, language, and decision-making processes that can inhibit effective partnership.
- Funding : Human services organizations and healthcare are traditionally funded through very different mechanisms. Healthcare is funded by Medicaid/Medicare and other private insurance, while human services are typically a mix of federal, state, and local government contracts. Braiding and blending funding and changing funding incentives/mechanisms is required.
- Data : Governments, hospitals, insurers, and managed care organizations hold critical data that is vital for tracking population health outcomes. But access to that data and aligning across sectors is challenging, for both client privacy and competitive reasons.
Given variability across jurisdictions, and uncertainty about future federal, state, and local healthcare policies, human services and healthcare organizations find themselves torn between investing in tomorrow’s promising innovations or continuing to maintain the essential safety net for today. Visionary leaders across the country understand they must somehow continue to do both.
The early activities of collaboration – such as agreeing on governance, navigating service integration, and aligning data systems – are laborious, and the short-term payoff can be hard to measure. Similarly, relationship-building – while vital to success – takes time, and contract reform at the payor level is complex and slow work. For these vital foundational elements of collaboration, funding has been limited.
Uncertain policy environment
Given variability across jurisdictions, and uncertainty about future federal, state, and local healthcare policies, human services, and healthcare organizations find themselves torn between investing in tomorrow’s promising innovations or continuing to maintain the essential safety net for today. Visionary leaders across the country understand they must somehow continue to do both.
Early work of integration is under-funded
“I don’t think we’ve ever been in a time of more uncertainty in terms of federal resources. We’re worried about the budget, Medicaid, and programs that affect vulnerable people, and we’ve never seen this level of proposed change. There is a real rollercoaster you’re riding as you look at programs and change. You have to be real flexible to see those curves in the road, because they are out there.” Shirley Dykshoorn, Vice President for Senior and Humanitarian Services, Lutheran Social Services of North Dakota
7. Recommendations for how to accelerate this movement
Build a pipeline of partnership-ready community-based human services organizations to increase the pace of integration..
Human services organizations are driving forces for improved social, economic, and health outcomes in the US. As the ultimate “doers,” they need to be strong voices in the development of integrative partnerships, and therefore must be equipped with knowledge of the true cost of social change through in-depth financial modeling (for more detail, see page 14 of the report Working Together Toward Better Health Outcomes ).
“We need to understand the full cost of meeting outcomes, including things like major investments in backbone support, data systems, and evaluations, all the things various players need to put into place to show outcomes that will reinforce the type of sustainable financing systems we want to put into place.” Jen Lewis, Special Projects Director at the Sonoma County Department of Health Services, and a leader in the Project Nightingale collaboration
Accelerate the momentum of integration efforts and policy reform through learning and knowledge sharing.
Working in new ways requires continual knowledge-sharing to provide potential partners information about funding arrangements, data and outcomes measures, timelines, cost approaches, contract terms, and service models. Cohorts, cross-sector learning networks, and geographically-focused consortia can amplify the lessons, challenges, and successes of partnership, and unify the many players into a stronger voice for policy reform.
“The challenges of bringing many players to a common table to agree on goals, share data, measure results, institute operating principles, and, ultimately, to fund only what works, are daunting. But continuing with the status quo is not an option. We are losing a generation. We need courageous leadership with new rules for engagement that emphasize true collaboration.” Melissa Skahan, Vice President of Mission Integration at Mercy Hospital, and Founder of the Greater Portland Addiction Collaborative
Fuel transformation with innovative, flexible capital.
In addition to addressing the persistent underinvestment in community-based human services, funders can invest in changing incentives to accelerate and motivate payors to shift toward collaboration. Finally, funding and financing for data infrastructure and overall improvements in interoperability across different sectors builds the evidence for the wisdom of integrated models.
People in the US have long strived for a society where every child can achieve his or her full potential. Yet in many communities, the obstacles to realizing this vision remain deep and complex, resulting in tragic inequities in opportunity, health, and life outcomes. Today, a deeper understanding of the role of social factors in health outcomes is spurring deeper integration across sectors. NFF believes we must invest in partnerships that address critical preventative social and economic factors like employment, housing, nutritious food, education, and safe neighborhoods . New models of collaboration between healthcare and human services can improve the quality of life for children and families across the country and advance us toward our shared ideals.
“It isn’t just about investors saving money, or hospitals making more, or governments having excess funds – it’s that people get better.” Mark Ryle, CEO of Project Open Hand
8. Initiative partners and project descriptions for deep-dive consulting with NFF
Hoi network organizations and members.

Project descriptions for deep-dive consulting engagements with NFF

9. Full list of resources
Nonprofit Readiness for Health Partnership for human services organizations considering partnership
Partnership Assessment Tool for Health for health and human services organizations in partnership
On the Broader Context of US Healthcare and Shift Toward Outcomes
- U.S. Health Care from a Global Perspective: Spending, Use of Services, Prices, and Health in 13 Countries
- Working Together Toward Better Outcomes
- ROI for Population Health: Evidencing a Double Standard
- Grant Makers, Put Results First in Deciding How to Give
- Using Short-term Data to Justify Spending Cuts is Dangerous
- Medically tailored food is the future of health care
- Using Nutrition to Improve Health and to Lower Costs
On Innovative Financing Models
- Using Pay for Success in Medicaid Managed Care and Value-Based Purchasing Initiatives
On Social Determinants of Health
- Aligning Health Systems with Community Development
- Doctors, Revolt!
- Conversations with Hospital and Health System Executives: How Hospitals and Health Systems Can Move Upstream to Improve Community Health
- Multi-Sector Partnerships in the US from 2012-Present
From HOI Clients and Partners
- Partnering in Health and Homelessness
- Oklahoma Pay for Success Supportive Housing Project
- Only Collaboration Can End America’s Opioid Crisis
- Innovative Partnerships in Medically Tailored Meals
Learning Network Convenings
Join over 24,000 social sector leaders who receive our latest insights and noteworthy stories throughout the year.
Other Reports
It takes a village. let’s make the village equitable., the promise, pitfalls, and potential of calaim, strengthening the los angeles food access ecosystem.
- Clear All Filters
- Arts and Culture
- Human Services
- Nonprofit Sector
- Financial Management
- Impact Investing

An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Office of the Assistant Secretary for Planning and Evaluation
Strengthening Human Services through Social Capital
ASPE has contracted with Research Triangle Institute and the University of North Carolina School of Government for this project, which seeks to understand how local, state, faith-based, and nonprofit human services programs and organizations can create and use social capital to increase employment, reduce poverty, and improve child and family well-being.
Project Overview – This project uses expert consultations, a program scan, and case studies to better understand how human services organizations help participants build and leverage social capital to improve economic opportunity.
The Value of Relationships: Improving Human Services Participant Outcomes through Social Capital - This handbook shares emerging practices that human services programs can implement to help participants build and leverage social capital, and it includes worksheets to help program managers and frontline staff apply these strategies to their own programmatic contexts. Findings are based on interviews and focus groups with national experts, a national program of organizations using social capital, and site visits and phone calls to human services programs using social capital strategies. A two page summary of common principles and emerging practices accompanies the handbook.
Networks that Work - This three-episode podcast features conversations with participants and practitioners from various human services programs. They discuss emerging practices for building social capital and participant perspectives. Episodes include:
- Close-Knit Communities for Better Outcomes: Using Peer Groups
- Friend Request Accepted: Using Technology to Build Social Capital
- Beyond Icebreakers: How to Help Participants Really Connect
Measuring How Social Relationships Contribute to the Outcomes of Program Participants - This webinar recording provides an overview of why human services programs should try to measure and evaluate their success in helping participants build social capital, offers concrete examples of ways to measure social capital, explores the role of logic models in the social capital context, and demonstrates how one program is doing this work.
Social Capital Considerations for the Incarcerated and Reentry Population – This issue brief summarizes six considerations for organizations working with currently incarcerated or recently released individuals who are interested in improving their participants' outcomes through strengthening their individual social capital. The brief provides specific examples of how these action-oriented considerations are being implemented by four different organizations currently doing this work.
Case Studies – Below are a series of case studies about human services programs that are helping participants build and use social capital in diverse ways. They cover a range of human services domains and have different emphases on bonding, bridging, and linking social capital. These case studies were selected for their focus on incorporating strategies to help participants build and use social capital, and not for other aspects of their programming.
- My Life My Choice (PDF) is a survivor-led organization fighting to end commercial sexual exploitation of children, which uses survivor mentorship and other services to help participants build social capital.
- Project CARE (PDF) provides services to individuals with disabilities who are affected by or at risk for domestic violence, sexual assault, dating violence, or stalking in the greater Cincinnati area, particularly through the use of peers who have shared experiences.
- Douglas County Community Mental Health Center (PDF) fosters relationships for incarcerated and reentering individuals recovering from substance use in Douglas County, Nebraska through coffee chats and connections with staff.
- Family Independence Initiative – Detroit (PDF) partners with families to form small cohorts that meet regularly to hold each other accountable toward achieving their goals by leveraging their existing social capital, tracking progress through technology, and using small grants from the program;
- CAP Tulsa (PDF) uses a two-generation approach that intentionally creates opportunities for families to build and use social capital by using a peer-to-peer cohort model that encourages families to connect with each other and develop a peer support network;
- Roca, Inc. (PDF) “relentlessly” engages high-risk young people in Maryland and Massachusetts to help them tap into new, positive social networks, including with employers in the community;
- Teen Challenge Arizona (PDF) offers faith-based residential drug and alcohol recovery centers that foster relationships with others going through similar experiences to build and leverage participants’ social capital; and
- Connections to Success (PDF) helps individuals in the St. Louis and Kansas City, MO regions build lasting social capital ties with their peers and others in the community through the use of one-on-one mentoring and professional development classes to support employment and other goals.
Visit the social capital landing page for more research on this topic.
Managing the Challenges in Human Service Organizations: A Casebook
- January 2009
- ISBN: 9781412941273
- This person is not on ResearchGate, or hasn't claimed this research yet.

- San Diego State University
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Daru Wahyuni

- Sri Umi Mintarti Widjaya
- Hari Wahyono

- William C Rezentes III
- George K Makini Jr
- Sung-Ju Kim

- Roseanne Mirabella
- Eur J Soc Work

- Max M. Schubert

- Richard H. Rothman
- Chui-man Pak
- Johnson Chun-Sing Cheung

- Michael J. Austin
- David Menefee
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Evidence-Based Policymaking: What Human Service Agencies Can Learn from Implementation Science and Integrated Data Systems
Sharon zanti.
1 Actionable Intelligence for Social Policy, University of Pennsylvania, School of Social Policy and Practice, 3701 Locust Walk, Philadelphia, PA 19104 USA
M. Lori Thomas
2 School of Social Work, UNC Charlotte Urban Institute/Institute for Social Capital, 9201 University City Boulevard, Charlotte, NC 28223 USA
The evidence-based policymaking movement compels government leaders and agencies to rely on the best available research evidence to inform policy and program decisions, yet how to do this effectively remains a challenge. This paper demonstrates how the core concepts from two emerging fields—Implementation Science (IS) and Integrated Data Systems (IDS)—can help human service agencies and their partners realize the aims of the evidence-based policymaking movement. An IS lens can help agencies address the role of context when implementing evidence-based practices, complement other quality and process improvement efforts, simultaneously study implementation and effectiveness outcomes, and guide de-implementation of ineffective policies. The IDS approach offers governance frameworks to support ethical and legal data use, provides high-quality administrative data for in-house analyses, and allows for more time-sensitive analyses of pressing agency needs. Ultimately, IS and IDS can support human service agencies in more efficiently using government resources to deliver the best available programs and policies to the communities they serve. Although this paper focuses on examples within the United States context, key concepts and guidance are intended to be broadly applicable across geographies, given that IS, IDS, and the evidence-based policymaking movement are globally relevant.
Introduction
Public administration of human service agencies aims to advance social welfare through efficient, effective delivery of policies, programs, and services. Yet, the complex array of modern-day human services issues—such as the Opioid Overdose Crisis (National Institute on Drug Abuse, 2020 ; World Health Organization, 2020 ), the lack of affordable housing and chronic homelessness crisis (Baptista et al., 2017 ; Culhane & Byrne, 2010 ; Marr, 2015 ; Rohe, 2017 ), the over-institutionalization of children and youth (Chege & Ucembe, 2020 ; Laklija et al., 2020 ; Wulczyn et al., 2015 )—have not been adequately addressed on a large scale in the United States (U.S.) (Fantuzzo et al., 2017 ; Kettl, 2002 , 2009 , 2012 ; Lindblom & Cohen, 1979 ). Out of this challenge, the movement toward evidence-based policymaking has emerged to encourage use of “the best available research and information on program results to guide decisions at all stages of the policy process and in each branch of government” (Pew-MacArthur Results First Initiative, 2014 , p. 2). In the U.S. context, both the Obama and Trump presidential administrations passed legislation that requires evidence-based policymaking across federal agencies (Foundations for Evidence-Based Policymaking Act, 2018 ; GPRA Modernization Act, 2010 ). State and local government organizations in the U.S. have similarly articulated that evidence-based policymaking is a priority (National Association of Counties, 2020 ; State Data Sharing Initiative, 2018 ). On an international scale, numerous countries are grappling with how to leverage evidence-based policymaking to tackle complex social problems (Kay, 2011 ; Nutley et al., 2007 ; Sanderson, 2002 ). The charge for government leaders and agencies at all levels is clear—rely on the best available data and evidence when making policy and practice decisions—but how to do this remains a challenge.
In this paper, we argue that in order to realize the aims of the evidence-based policymaking movement, human service agencies and their partners must bring together two emerging fields: Implementation Science (IS) and Integrated Data Systems (IDS). Together, the core concepts and practices from these fields can create the fertile ground from which to deliver the best available policies, programs, and services to human services clients. When rigorous research evidence goes unused by agencies, client populations are ultimately impacted by the inefficient use of government resources and lack of innovative, up-to-date services.
We begin this article with an overview of the IS and IDS fields and their applicability to public administration of human service agencies. We then describe how both IS and IDS can increase capacity for the uptake of evidence-based policies and practices (EBPs). We offer practical guidance for drawing upon IS and IDS in a human service setting. We use examples to highlight how IS and IDS can enhance evidence-based policymaking, including an extended example that applies these concepts to Housing First, an evidence-based practice and policy innovation that prioritizes housing to address homelessness, minimizes program eligibility criteria, and provides supportive services from a person-centered, harm reduction perspective. Housing First began in the U.S. in the late 1990s and has since been successfully implemented globally in several countries. We also include recommendations and resources for human service agencies looking to enhance their evidence-based policymaking. While we draw on examples and literature primarily from the U.S. context, key concepts and guidance aim to be broadly applicable across geographies in state and local agencies. We frequently and interchangeably use the terms policies, programs, services, and interventions throughout this article to broadly refer to practices that government agencies undertake in service of their client populations. The term EBPs is specifically used to refer to those policies, programs, services, and interventions that have been deemed “evidence-based.”
Background on Implementation Science
The field of IS began in the 1990s in response to the well-documented “evidence-to-practice gap” in health interventions (Dearing & Kee, 2012 ). The earliest documented example of this gap dates back to James Lind, who discovered through clinical trials in 1747 that citrus could treat scurvy; however, it was nearly a half-century later until the British Navy introduced this intervention on ships (Baron, 2009 ). Despite its roots in health care, the IS field has since expanded to psychology, public health, education, criminal justice, child welfare, and to most other human service domains, where a similar gap persists between development of EBPs and their use in practice (Dearing & Kee, 2012 ). Broadly, the goals of IS are to close this gap by studying the mechanisms through which front-line workers, administrators, institutions, and even governments are able to successfully implement EBPs that can improve outcomes (Eccles & Mittman, 2006 ).
IS starts with the assumption that there is an EBP to be implemented (Lane-Fall et al., 2019 ). The threshold for what constitutes “evidence-based” varies by field. For instance, the Canadian Best Practices Portal distinguishes public health interventions as either promising practices, best practices, or Aboriginal “Ways Tried and True” (Public Health Agency of Canada, n.d.). The European Monitoring Centre for Drugs and Drug Addiction (n.d.) provides clear standards for evidence ratings of drug-related interventions. In the U.S., the California Evidence-Based Clearinghouse for Child Welfare (n.d.) and the federal Title IV-E Prevention Services Clearinghouse (n.d.) catalog evidence for child welfare programs. The Results First Clearinghouse Database is another commonly used tool in the U.S. for locating EBPs applicable to social policymaking and human service agencies (The Pew Charitable Trusts, 2021 ). With an EBP to implement, IS then aims to study the strategies that promote successful uptake of the EBP, whether carried out at the individual, organizational, or jurisdictional level. Importantly, the context where the EBP is implemented is not viewed as a hindrance, but rather as a central component that informs strategies for minimizing the evidence-to-practice gap (Shea et al., 2018 ).
It is also important to note the difference between efficacy and effectiveness research and IS. Whereas efficacy and effectiveness examine whether policy and practice interventions achieve desired client and community outcomes (e.g., reduced homelessness, economic stability, successful family reunification, decreased opioid deaths), IS research examines outcomes like how acceptable a policy change is to agency staff, whether an employee training program or a policy mandate leads to more rapid adoption of a new program, or to what extent fidelity of an intervention model is achieved. Proctor et al. ( 2011 ) named eight types of implementation outcomes that can guide the development of IS studies—acceptability, adoption, appropriateness, feasibility, fidelity, cost, penetration, and sustainability. These implementation outcomes are critical to study given that they influence process or service outcomes (e.g., timeliness, efficiency, equity), and ultimately client outcomes (e.g., symptomology, satisfaction, function) (Proctor et al., 2011 ). Altogether, IS offers human service agencies a set of frameworks, theories, and models (hereafter referred to as frameworks) to guide the implementation of EBPs and further the study of how they are most effectively put into practice.
Background on Integrated Data Systems
Similar to IS, the newly emerging field of IDS aims to improve client outcomes and increase organizational efficiency but approaches these issues through the sharing and integration of cross-sector administrative data. Data integration is “a complex type of data sharing that involves record linkage, which refers to the joining or merging of data based on common data fields” (Hawn Nelson et al., 2020 , p. 1). An IDS is a formalized effort that enables the routine sharing and reuse of administrative data with strong governance and legal agreements in place; it is also sometimes referred to as a data hub, state longitudinal data system, data collaborative, or data trust (Hawn Nelson et al., 2020 ). This process of sharing and reusing administrative data enables government agencies and their partners, often siloed in daily operations, to observe their overlapping client populations and more accurately understand system-level complexities (Fantuzzo & Culhane, 2016 ). Thus, the IDS is more than a technology solution; it is a method that facilitates collaboration between government leaders, practitioners, researchers, and community stakeholders to better understand social problems and to develop and evaluate policy solutions (Fantuzzo & Culhane, 2016 ).
Dunn ( 1946 ) initially discussed linking records of vital statistics. However, in the U.S., state-level data integration for research and policymaking did not begin until the 1970s. At that time, South Carolina constructed an IDS to better understand disease prevalence, to define populations for needs assessments, and to measure service outcomes (Kitzmiller, 2014 ). Since then, the state has continued to expand their use of IDS data. Currently, over 90 state and local jurisdictions, non-profits, and universities in the U.S. have developed some form of IDS that seeks to leverage their vast stores of administrative data for social policymaking (Berkowitz et al., 2020 ). At the global level, the International Population Data Linkage Network (IPDLN) facilitates connections between administrative data linkage centers and those who use linked data for research and policymaking. There are over 1000 members in this global network (IPDLN, n.d.). The growth in IDS on a national and international scale means greater capacity for linked administrative data to support the policymaking process.
Building Agency Capacity for Evidence-Based Policymaking
Human service agencies have much to gain by incorporating IS and IDS principles and practices into regular operations. Doing so will increase organizational capacity for the uptake of EBPs in state and local agencies. The following sections highlight the core benefits of IS and IDS that human service agencies can draw upon to enhance their evidence-based policymaking.
Implementation Science and Evidence-Based Policymaking
Addressing the role of context in implementation.
Context refers to “the physical, organizational, institutional, and legislative structures that enable and constrain, and resource and realize, people and procedures” (May et al., 2007 , p. 3). The success of new policies and programs depends on more than just the available research evidence; it also matters how well the program or policy is adapted to fit the local setting. This is a delicate balance between preserving the integrity of the original policy or program intervention and fitting it to a real-world context. Consider the example of wearing masks during the COVID-19 pandemic, an EBP that U.S. public health agencies in particular have been grappling with how to implement given strong divisions of public opinion (Taylor, 2020 ). Public health studies provide clear evidence that wearing masks can prevent the spread of COVID-19 and other infectious diseases (Centers for Disease Control & Prevention, 2020 ). However, they do not delineate barriers and facilitators to mask wearing, the cost of providing masks to all patients who enter a public facility, or strategies to increase public acceptance of mask wearing in stores and restaurants compared to private social settings. IS can address these issues by studying how other important factors like the level of government (e.g., federal, state, local) where mask wearing policies are enacted, the surrounding sociopolitical context, and attitudes of public officials impact mask wearing behaviors.
The Consolidated Framework for Implementation Research (CFIR), one of the most cited IS frameworks, would be especially helpful for analyzing contextual issues that influence mask wearing in a jurisdiction (Kirk et al., 2015 ). The CFIR includes five constructs that influence implementation—the intervention (e.g., complexity and cost of mask wearing), outer setting (e.g., peer pressure from other jurisdictions), inner setting (e.g., culture of the jurisdiction and incentivizes for mask wearing), individuals (e.g., knowledge and beliefs of citizens in the jurisdiction), and process (e.g., influence of opinion leaders) (CFIR Research Team-Center for Clinical Management Research, 2021 ). This framework can facilitate the study of factors that influence uptake of mask wearing. Without such a framework, media and politicians may direct public attention toward a single factor that downplays the complexity of implementing mask wearing on a large scale. Policymakers can then develop strategies to increase mask wearing that draw upon the specific context.
Complementing Other Quality and Process Improvement Efforts
Quality and process improvement strategies help agencies improve their service delivery and efficiency by focusing on timely, incremental changes to process, workflow, and behavior (Koczwara et al., 2018 ). In contrast, IS emphasizes the use of theory, rigorous scientific methods, and the creation of generalizable knowledge that produces medium-to-long-term improvements (Koczwara et al., 2018 ). Ultimately, however, these fields converge in their action-oriented approaches to improving services and outcomes for clients and communities. Thus, IS can complement quality and process improvement efforts, which tend to emphasize short-term improvements, by adding conceptual frameworks and mixed methods approaches to the question of how to improve outcomes over the long term using the best available evidence.
Consider a child care licensing agency that seeks to increase the number of facilities that get licensed. These agencies issue licenses to child care facilities that meet certain quality standards, often based on evidence-based public health and early childhood guidelines (Childcare.gov, n.d.). A quality and process improvement approach might employ “Lean” and “Six Sigma” frameworks that streamline paperwork requirements for providers, allow initial application submission online instead of via mail, and reduce the number of licensing staff needed to conduct facility reviews (Antony, 2011 ). With the addition of IS frameworks, however, these strategies could be embedded in a larger effort to understand what works for increasing and sustaining child care licensure over the long term. The Exploration, Preparation, Implementation, Sustainment (EPIS) framework includes four phases that could guide an implementation study in this example—exploration (e.g., investigating needs and characteristics of facilities that influence their pursuit of licensure), preparation (e.g., identifying barriers and facilitators to certain types of facilities applying for licensure), implementation (e.g., enacting quality and process improvement and/or other strategies based on insights surfaced in exploration and preparation), and sustainment (e.g., adapting strategies from the implementation phase to be feasible and realistic for the licensing agency) (Aarons et al., 2011 ; Moullin et al., 2019 ).
Furthering Evidence on Policy Effectiveness and Implementation
There is rarely a saturation point at which policies and practices enacted by human service agencies no longer benefit from additional effectiveness studies. Whether improving the strength of evidence, testing interventions on new subpopulations, or satisfying stakeholder expectations to continue demonstrating outcomes, effectiveness research is often ongoing. However, at some point evidence generation can delay the delivery of better services above and beyond the best interest of the target population. The field of IS addresses this tension through effectiveness-implementation hybrid trials, which seek to narrow the evidence-to-practice gap by simultaneously studying effectiveness and implementation (Curran et al., 2012 ). There are three types of hybrid trials—Type 1 trials primarily test the effects of an intervention while also gathering data about implementation, Type 2 trials give equal weight to studying effectiveness and implementation, and Type 3 trials primarily test an implementation strategy while also studying effectiveness (Curran et al., 2012 ).
As an example, Kirchner et al. ( 2014 ) conducted a quasi-experimental Type 3 hybrid trial with the U.S. Department of Veterans Affairs (VA) that tested an implementation facilitation strategy for an integrated primary care and mental health intervention while also evaluating clinical outcomes of those who received the intervention. The strategy, developed in partnership with regional VA leaders, included a team of facilitators to support staff across seven intervention sites on implementation and tailoring of the intervention, provide ongoing performance monitoring and feedback, engage local change agents, and market the intervention. An evaluation based on the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework showed that this multifaceted strategy increased reach and adoption of the integrated primary care and mental health intervention, which ultimately led to improved patient access to mental health care (Glasgow et al., 1999 ). Specifically, patients at intervention sites (i.e., those with the implementation facilitation strategy) had nine times higher odds of accessing the integrated primary care and mental health intervention (reach) and providers at intervention sites were seven times more likely to refer patients to the integrated primary care and mental health intervention (adoption). There were no significant differences between patients at intervention sites and non-intervention sites in terms of their odds of getting referred to specialty mental health clinics (effectiveness). Hybrid trials like this allow agencies to continue to study policy effectiveness while also uncovering the mechanisms that facilitate uptake of EBPs so as to get clients effective programs faster and in ways that can be successfully implemented.
When discussing hybrid trials, it is important to note that the “gold standard” randomized controlled trial may not always be prudent or feasible to undertake in a human service setting (Fives et al. 2015 ). For example, ethical concerns may be raised around withholding interventions from those randomly assigned to a control group while experimental groups receive services. This is especially important to consider when client health and safety are at stake, such as in substance use, mental health, or child maltreatment interventions. In these instances, hybrid trials with quasi-experimental designs may be more appropriate, as demonstrated in the above example.
Guiding Systematic De-implementation of Policies and Programs
Sometimes evidence-based policymaking involves de-implementing practices that are ineffective, unproven, harmful, overused, inappropriate, and/or low-value (Norton et al. 2019 ). De-implementation is a unique subset within the IS field that studies how to systematically reduce or stop these types of practices. There are four key types of de-implementation: (1) removing a practice entirely, (2) replacing the practice with a more effective intervention, (3) reducing the frequency or intensity of use, and (4) restricting the setting or target population for the intervention (Norton et al. 2019 ).
De-implementation presents challenges, particularly for large agencies where practices are entrenched in the fabric of daily operations. Clients or service recipients may also be resistant to policies or interventions being removed or scaled back. Thus, Prusaczyk et al. ( 2020 ) articulate the importance of considering cultural and historical importance of the practice as part of the de-implementation process. The over-prescription of antibiotics provides a relevant example, where the risk to individuals of receiving unnecessary antibiotics are relatively low compared to the population-level risk of increasing development of antibiotic-resistant bacteria (Prusaczyk et al., 2020 ). Therefore, even when public health agencies recommend decreasing unnecessary antibiotic prescriptions, doctors may still encounter patients who expect to receive antibiotics and request them despite explanations of why they may be unnecessary and potentially harmful. Antibiotics were heralded as a panacea when their large-scale commercial production began around World War II and their discovery revolutionized the medical field (American Chemical Society International Historic Chemical Landmarks, n.d.). This history is important for understanding how widespread use of antibiotics has led to a culture where patients are accustomed to readily receiving antibiotics in primary care settings and may resist the idea that the drug could be damaging on a societal level.
De-implementation in human service settings has not been widely researched, though there are numerous practices ripe for de-implementation (McKay et al., 2018 ). Drug Abuse Resistance Education (D.A.R.E.) is frequently cited as an intervention known to be ineffective at its intended aims of reducing adolescent drug use, yet school districts in every state still use this program (D.A.R.E. America, 2021 ). McKay et al. ( 2018 ) suggest that D.A.R.E. and other interventions identified as ineffective, inefficient, or unnecessary could be successfully de-implemented using a four-step process—selecting an intervention for de-implementation, assessing the de-implementation context, carrying out strategies to de-implement, and evaluating de-implementation outcomes. Existing IS frameworks are available to support each of these steps. For example, when assessing context, the EPIS framework, CFIR, and De-Adoption framework could all support the study of contextual factors that influence de-implementation strategies (McKay et al., 2018 ). In the EPIS framework, historical and cultural considerations, like inter-organizational environment and networks and client characteristics, are seen as part of the outer context that influences implementation of an EBP (Moullin et al., 2019 ). The CFIR similarly encourages consideration of the outer setting—including external policies and incentives and peer pressure from competing organizations—when assessing the context surrounding de-implementation (CFIR Research Team-Center for Clinical Management Research, 2021 ).
Integrated Data Systems and Evidence-Based Policymaking
Facilitating governance processes for ethical, legal data access and use.
Administrative data are an enticing source for producing research evidence and insights, but it cannot be ethically and legally used without strong governance in place. The IDS approach encourages stakeholder engagement in the development of a governance process that meets the needs of the local context (Gibbs et al., 2017 ). For example, the Institute for Social Capital (ISC)—a community IDS housed at the University of North Carolina (UNC) Charlotte Urban Institute—was founded with a collaborative governance model, where government, non-profit, and university partners each have a role in data governance and oversight (Allison-Jacobs, 2018 ). However, over time ISC recognized the importance of moving beyond just organizational representation and the IDS is now building a process to include people represented within administrative data in the governance process, particularly those disproportionately represented. The board members and staff initiated an intentional planning process in order to prevent tokenized representation and develop, with community stakeholders, specific mechanisms that build representation into the organization. The non-profit organization that guides ISC is currently in the process of adding a Community Data Advisory Committee, which will be integrated into the board governance structure and include community stakeholders who are overrepresented within data held by ISC.
Governance is a crucial component for sharing and integrating cross-sector data as it establishes an ongoing process for secure data access, linkage, and analysis. An IDS can facilitate community engagement by building it into routine governance structures. Without governance, agencies rely on single-use data sharing agreements that are often inefficient, legally and administratively cumbersome, and not grounded in democratic, community-engaged processes (Gibbs et al., 2017 ). For instance, if a child welfare agency wants to understand housing instability among youth who “age out” of the foster care system, they might request access to Homeless Management Information System (HMIS) data, which could take months or even years to negotiate for a single project. When more data partners are involved or the complexity and sensitivity of the requested data increases, the timeline for legal data sharing negotiations only increases. The difficulty of recreating this process for each individual project can discourage cross-agency data sharing. However, establishing an IDS with a legally vetted data governance process can not only increase efficiency, but also foster collaboration across agencies and community partners to support evidence-based policymaking.
Compared to mere technology solutions for joining together administrative datasets, the IDS approach underscores the relational aspect of data sharing and integration. Though technical data integration challenges arise with any IDS effort (e.g., selecting an optimal database type and structure, marrying legacy databases with new software, implementing privacy preservation techniques), the definition of these challenges and their range of solutions tend to be more readily agreed upon by IDS stakeholders (National Implementation Research Network [NIRN], n.d.). However, more adaptive challenges abound—that is, complex challenges requiring adaptive leadership to engage stakeholders and build consensus on the nature of the challenge and how to address it—when bringing together diverse stakeholders to build data integration capacity (NIRN, n.d.). Through governance processes, an IDS can address adaptive challenges by facilitating a “community of people involved in the social problem-solving process engaging in bidirectional dialogue that converts data into actionable intelligence, uses actionable intelligence to propel decision making, analyzes and reflects on the success of their choices, and refines and revises operations accordingly” (Fantuzzo et al., 2017 , p. 10).
Providing Relevant, High-Quality Data for Efficient Analysis
Increasing evidence-based policymaking hinges on having access to the best available data and research evidence, which is often generated in unaffiliated academic settings rather than within agencies themselves. However, human service agencies are replete with potentially relevant administrative data that are collected throughout the course of regular operations. With the proper governance processes in place, these data can be ethically reused and linked at the individual level across multiple programs and/or agencies to provide a holistic, longitudinal view of clients, families, and communities served (Hawn Nelson et al., 2020 ). In this way, an IDS also becomes an essential Decision Support Data System for implementation projects (NIRN, 2021 ).
Furthermore, housing data within a government IDS or a non-profit or university IDS that closely collaborates with its government depositors builds capacity for human service agencies to conduct onsite or prioritized analyses that are directly applicable to their most pressing policy needs (Fantuzzo et al., 2017 ). For instance, a public benefits agency may need to understand how many clients will experience a “cliff effect” (i.e., a drop-off in benefits) in one program if a new policy increases food assistance benefits. An IDS can provide the most applicable data to facilitate this analysis in-house or as a part of an ongoing partnership rather than contracting with an unrelated third party to collect original data, which delays time-sensitive insights for the policymaking process and comes with privacy and security risks. It is important to note that data relevancy and quality vary across administrative datasets, but agency staff and regular data partners are often better equipped than unaffiliated outside researchers to uncover and address concerns around missing data, data entry consistency, data documentation, and other common issues when reusing administrative data (Hawn Nelson et al., 2020 ). Therefore, the IDS approach leverages agency and partner strengths to build internal capacity for analyzing their own data.
Efficiently Addressing Pressing Research, Evaluation, and Planning Needs
When relevant, high-quality datasets are made accessible within and between agencies, they can be linked across programs to reduce the time, funding, and energy that would typically be required for original data collection and linkage. Furthermore, the use of IDS can reconcile common issues in survey research, such as low response rates and inadequate sample sizes and comparison groups, as administrative data collection routinely captures population-level data (Hawn Nelson et al., 2020 ). For instance, an evaluation of a city’s youth employment program can leverage administrative data to compare outcomes of those who participated in the program to outcomes of the city’s broader youth population or to youth who participated in similar programs with different implementation strategies. Rapid evaluations that use embedded randomized controlled trial (RCT) or quasi-experimental designs also become more plausible with an existing IDS infrastructure, thus saving substantial time and cost—which can be repurposed for other important agency functions—compared to traditional causal research studies.
As another example, the State of South Carolina in the U.S. leveraged their IDS capacity to evaluate a pilot psychiatric telehealth initiative that aimed to address the shortage of rural mental health services. Findings showed improved patient outcomes compared to treatment as usual, which supported the state in scaling the telehealth program to additional rural hospitals to reach more individuals in need of psychiatric services (Cooner, 2018 ). The IDS creates capacity for agencies to conduct both small- and large- scale research, evaluation, and implementation studies, and to use these data to inform program planning.
Housing First Case Example
We will now look further into the example of how IS and IDS were applied to the broad scale implementation of Housing First in Charlotte, North Carolina. Housing First is an EBP that “addresses chronic homelessness by providing rapid access to permanent housing without pre-condition of treatment, along with ongoing support services such as crisis intervention, needs assessment, and case management” (The Pew Charitable Trusts, 2021 , database line 1244). Housing First permanent supportive housing began in New York, where it was first recognized as an evidence-based practice (Padgett et al., 2016 ). It has since been implemented throughout the United States and globally, including in Europe (Busch-Geertsema, 2013 ), Canada (Goering et al., 2014 ), and Australia (Whittaker et al., 2015 ).
Housing First Charlotte-Mecklenburg (HFCM)—a cross-sector collaborative effort to end chronic homeless—capitalized on the benefits of both IS and IDS to scale and evaluate Housing First at the local level in North Carolina. An earlier pilot study of one local Housing First permanent supportive housing effort demonstrated the initial effectiveness of the program as well as potential utility of multi-sector data to understand implementation and outcomes and convinced broader stakeholders of the promise of the Housing First approach. Between 2015 and 2019, HFCM applied eight implementation strategies, and a team of researchers at the University of North Carolina (UNC) Charlotte recently studied outcomes of this effort (Thomas et al., 2020b ).
The research team drew from the framework developed by the At Home/Chez Soi RCT of Housing First permanent supportive housing in Canada. The At Home/Chez Soi team relied on four different implementation frameworks and the broader implementation science literature to develop and test five constructs including Intervention Characteristics, Context of Implementation, Implementation Process, Organizational Characteristics, and Strategies of Implementation (Fleury et al., 2014 ). HFCM research utilized data and data integration capacity at the ISC (a community IDS housed at the UNC Charlotte Urban Institute discussed previously) to evaluate the implementation and outcomes. Below we further summarize the ways in which IS and IDS concepts were applied.
Implementation Science and Housing First
One of the key lessons highlighted by this study was the importance of situating chronic homelessness within a larger ecosystem. Socioeconomic forces, such as limited affordable housing and economic mobility in the Charlotte-Mecklenburg area, influenced the implementation strategies and ultimate outcomes of the effort to end chronic homelessness by scaling Housing First. An IS lens helped the HFCM research team identify the important contextual factors and suggest modifications to Housing First implementation in response.
While this study did not explicitly name other process and quality improvement frameworks, the eight implementation strategies included a focus on both incremental, short-term changes as well as theory-driven, long-term changes to homelessness services. For example, creating a registry of all individuals experiencing chronic homelessness (called the “By-Name-List”) allowed HFCM to continually monitor progress toward housing these individuals and to measure housing outcomes over five years. Additionally, IS helped the HFCM research team transform process improvement strategies into a robust, mixed methods study with a clear conceptual framework, which was necessary for such a complex policy implementation project.
Furthering the Evidence on Policy Effectiveness and Implementation
HFCM simultaneously studied implementation and effectiveness outcomes, as key leaders and stakeholders in this effort recognized the importance of understanding both sets of outcomes to inform future work. In terms of effectiveness, the study identified 1011 people on the By-Name-List who became housed in the course of the study and demonstrated high housing retention rates overall. The study also followed 330 people from the By-Name-List up to 24 months and gathered follow-up data on 294 of them—165 of whom were housed and 129 who were not and served as the comparison group on a range of standardized and service utilization measures (Thomas et al., 2020a ). On the implementation side, robust fidelity criteria established through research (Stefancic et al., 2013 ) were measured at multiple points in the study, a cost analysis was conducted, and the study looked at the impact of project structure and management on outcomes.
While this study did not directly address de-implementation, an IS lens allowed the HFCM research team to identify the importance of de-implementing old ways of thinking about chronic homelessness. Successful implementation of Housing First requires the broader homeless services system to adopt the philosophy that “housing is a foundation and not a reward…and services begin with the person instead of a threshold of eligibility criteria” (Thomas et al., 2020b , p. 3). The study findings identify the importance of paying attention to shifting philosophy alongside replacing program procedures in order to maintain fidelity to the EBP.
Integrated Data System and Housing First
Administrative data used in the study came from the Institute for Social Capital (ISC), an IDS housed at the UNC Charlotte Urban Institute. Due to ISC’s existing governance structure (i.e., an legally designated board of directors and its data oversight committee that thoroughly reviews and approves data requests and develops data privacy policies), this study was able to legally and ethically access administrative data from the Homeless Management Information System (HMIS) and integrate these data with 10 other health and human services sources (ISC, n.d.; Thomas et al., 2020a ). These data ultimately supported the study’s mixed methods analysis strategy.
Health and human services data were integrated with By-Name-List data and data collected through the research project in order to examine characteristics of those served by HFCM throughout the course of the initiative. Access to high-quality integrated data allowed HFCM to understand aggregate trends and outcomes that supplemented data from surveys, interviews, focus groups, observations, and artifacts. Without the IDS, HFCM would not have had robust decision support data. Importantly, ISC was not just a data provider for this study, but also an internal service and planning partner throughout the project. The ongoing, working relationship among IDS partners facilitated efficient analyses that without the services of an IDS, would not have been feasible.
Growing concerns of chronic homelessness galvanized HFCM partners to develop a cross-system strategy to implement Housing First. While IDS data integration and analysis was just one component of the overall implementation evaluation strategy, having access to readily available, high-quality data enabled more robust analyses of outcomes. Furthermore, the ability to interrogate multiple data sources allowed the HFCM team to pinpoint the need for a more hospitable intervention implementation environment (NIRN, 2021 ).
Recommendations for Human Service Agencies
For human service agencies looking to enhance their evidence-based policymaking, we offer two key recommendations to help navigate the use of IS and IDS in complex, real-world environments. First, we recommend drawing upon existing IS frameworks. There are over 100 frameworks to choose from, most of which fit into three overarching categories: process models (guide translation of research to practice), determinant frameworks (organize factors thought to influence implementation), or evaluation models (guide evaluation of the implementation itself) (Nilsen, 2015 ). Depending on where the agency is in the research process, frameworks can provide structure for thinking through existing knowledge of the social problem and potential EBP implementation strategies (e.g., Proctor et al., 2011 ), guidance for planning and outlining the IS research study flow (e.g., the EPIS Framework in Moullin et al., 2019 ), or mapping behavior change theory to implementation strategies (e.g., the COM-B Framework in Michie et al., 2011 ).
It is important to acknowledge that no framework is perfect and the best-fitting framework will largely depend on agency context. It may be helpful to choose a framework used in a similar IS study or one recommended by a colleague or key player in the implementation effort. Another option is combining applicable components of several frameworks. For additional guidance on choosing and using frameworks see Fixsen et al. ( 2021 ), Nilsen ( 2015 ), Tabak et al. ( 2012 ), the National Collaborating Centre for Methods and Tools ( 2016 ), the Implementation Science Resource Hub (n.d), and the Global Implementation Society ( 2021 ).
Second, we recommend that agencies looking to establish or strengthen their integrated data capacity start small, demonstrate impact early, and scale up over time. Most IDS efforts start with a single project or social problem that motivates a group of stakeholders to share and integrate their data. This creates an opportunity to align priorities for data sharing and gradually establish governance, legal, and technical procedures that meet the needs of all data contributors. Building IDS capacity is challenging and the best path forward largely depends on context—what works for one jurisdiction may not work as well in another. It can be helpful to think of IDS building in stages, where small steps to build trust, negotiate agreements, and conduct simple data sharing projects can create a strong foundation from which to gradually take on more complex projects and onboard new data partners.
We recommend looking for opportunities for quick, impactful wins that can demonstrate the value of IDS and build the necessary trust, buy-in, and resource commitment to improve data capacity and quality. For example, partners could create a cross-agency dashboard to track progress on an important goal or execute an ad hoc data sharing agreement to analyze data between agencies on a timely issue. See Hawn Nelson et al. ( 2020 ) for more guidance on how to begin an IDS effort and Zanti et al. ( 2021 ) for legislative and funding strategies to build and sustain an IDS. Both pieces are framed for a U.S. audience; however, the general principles shared may be applicable in global contexts.
Together, the fields of IS and IDS consist of principles and practices that are necessary to advance human service agency capacity for evidence-based policymaking. Specifically, IS can help agencies address the role of context when right-sizing EBPs to the populations they serve. It also complements existing quality and process improvement efforts, offers a hybrid trial method for continuing the study of effectiveness alongside implementation outcomes, and provides guidance for the systematic de-implementation of ineffective policies. On the other hand, the IDS approach offers a governance framework, which is necessary for the ethical and legal use of agency data to further effectiveness and implementation research. Additionally, an IDS can provide relevant, high-quality data that more efficiently address time-sensitive agency needs. The crux of this convergence between IS and IDS, however, is in helping human service agencies deliver the best possible services and outcomes for the communities they serve. As the Housing First Charlotte-Mecklenburg case suggests, IS and IDS can be leveraged in tandem to enhance evidence-based policymaking in human service agencies.
Acknowledgements
The authors would like to acknowledge Dr. Amy Hawn Nelson and Justin Lane for their reviews of this article; Mecklenburg County, North Carolina, Roof Above, and the UNC Charlotte Urban Institute and College of Health and Human Services for funding the Housing First Charlotte-Mecklenburg study; and, the Institute for Social Capital for providing integrated data for the study.
Author Contributions
SZ conceptualized the manuscript and prepared the initial draft. LT is the principal investigator of the Housing First Charlotte-Mecklenburg study, provided case content, and critically revised the manuscript. Both authors contributed to the reviewing and editing of the final manuscript.
The Housing First Charlotte-Mecklenburg study referenced in this manuscript was funded by Mecklenburg County, Roof Above, and UNC Charlotte.
Declarations
Author B has received research support from Mecklenburg County.
The Housing First Charlotte-Mecklenburg study referenced in this article was approved by the UNC Charlotte Institutional Review Board.
Contributor Information
Sharon Zanti, Email: ude.nnepu@itnazs .
M. Lori Thomas, Email: ude.ccnu@samohTirol .
- Aarons GA, Hurlburt M, Horwitz SM. Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011; 38 (1):4–23. doi: 10.1007/s10488-010-0327-7. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Allison-Jacobs, R. (2018). IDS case study: The Institute for Social Capital: Creating a hybrid IDS model for the greater Charlotte-Mecklenburg region . Actionable Intelligence for Social Policy. https://www.aisp.upenn.edu/wp-content/uploads/2018/11/ISC.pdf
- American Chemical Society International Historic Chemical Landmarks. (n.d.). Discovery and development of Penicillin . http://www.acs.org/content/acs/en/education/whatischemistry/landmarks/flemingpenicillin.html
- Antony J. Six Sigma vs Lean. International Journal of Productivity and Performance Management. 2011; 60 (2):185–190. doi: 10.1108/17410401111101494. [ CrossRef ] [ Google Scholar ]
- Baptista, I., Benjaminsen, L., Pleace, N., & Busch-Geertsema, V. (2017). Family homelessness in Europe: 7 EOH comparative studies in homeless. https://eprints.whiterose.ac.uk/125725/
- Baron JH. Sailors' scurvy before and after James Lind—A reassessment. Nutrition Reviews. 2009; 67 (6):315–332. doi: 10.1111/j.1753-4887.2009.00205.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Berkowitz, E., Jenkins, D., Culhane, D., Zanti, S., Hawn Nelson, A., & Burnett, T. (2020). IDS landscape analysis: Models, motivations, and capacity for cross-agency data sharing. University of Pennsylvania, Actionable Intelligence for Social Policy. Unpublished report.
- Busch-Geertsema, V. (2013). Housing First Europe: Final report. Bremen/Brussels: European Union Programme for Employment and Social Solidarity . https://www.habitat.hu/files/FinalReportHousingFirstEurope.pdf
- Centers for Disease Control and Prevention. (2020). Considerations for wearing masks . https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprevent-getting-sick%2Fcloth-face-cover.html
- CFIR Research Team-Center for Clinical Management Research. (2021). Constructs . Consolidated Framework for Implementation Research. https://cfirguide.org/constructs/
- Chege N, Ucembe S. Kenya’s Over-reliance on institutionalization as a child care and child protection model: A root-cause approach. Social Sciences. 2020; 9 (4):57. doi: 10.3390/socsci9040057. [ CrossRef ] [ Google Scholar ]
- Childcare.gov. (n.d.). Child care licensing and regulations . U.S. Department of Health and Human Services, Administration for Children and Families. https://www.childcare.gov/index.php/consumer-education/child-care-licensing-and-regulations
- Cooner, S. (2018). SCDMH Emergency Department Telepsychiatry Consultation Program . Rural Health Information Hub. https://www.ruralhealthinfo.org/project-examples/992
- Culhane, D. P., & Byrne, T. (2010). Ending chronic homelessness: Cost-effective opportunities for interagency collaboration. Penn School of Social Policy and Practice Working Paper . https://repository.upenn.edu/spp_papers/143/
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care. 2012; 50 (3):217. doi: 10.1097/MLR.0b013e3182408812. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- D.A.R.E. America (2021). D.A.R.E. Hometowns—U.S.A. & International . https://dare.org/where-is-d-a-r-e/
- Dearing, J. W., & Kee, K. F. (2012). Historical roots of dissemination and implementation science. In: Dissemination and implementation research in health: Translating science to practice (pp. 55–71). 10.1097/MLR.0b013e3182408812
- Dunn HL. Record linkage. American Journal of Public Health and the Nations Health. 1946; 36 (12):1412–1416. doi: 10.2105/AJPH.36.12.1412. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eccles MP, Mittman BS. Welcome to implementation science. Implementation Science. 2006 doi: 10.1186/1748-5908-1-1. [ CrossRef ] [ Google Scholar ]
- European Monitoring Centre for Drugs and Addiction. (n.d.). Best practice portal—Evidence database. https://www.emcdda.europa.eu/best-practice/evidence-summaries
- Fantuzzo J, Culhane DP. Actionable intelligence: Using integrated data systems to achieve a more effective, efficient, and ethical government. Palgrave Macmillan; 2016. [ Google Scholar ]
- Fantuzzo, J., Henderson, C., Coe, K., & Culhane, D. (2017). The integrated data system approach: A vehicle to more effective and efficient data-driven solutions in government . Actionable Intelligence for Social Policy, University of Pennsylvania. https://www.aisp.upenn.edu/resource-article/the-integrated-data-system-approach-a-vehicle-to-more-effective-and-efficient-data-driven-solutions-in-government/
- Fives A, Russell DW, Canavan J, Lyons R, Eaton P, Devaney C, Kearns N, O'Brien A. The ethics of randomized controlled trials in social settings: Can social trials be scientifically promising and must there be equipoise? International Journal of Research & Method in Education. 2015; 38 (1):56–71. doi: 10.1080/1743727X.2014.908338. [ CrossRef ] [ Google Scholar ]
- Fixsen, A., Aijaz, M., Fixsen, D.L., Burks, E., & Schultes, M. (2021). Implementation frameworks: An analysis. Active Implementation Research Network. https://www.activeimplementation.org/wp-content/uploads/2021/04/AIRN-AFixsen-FrameworksAnalysis-2021.pdf
- Fleury MJ, Grenier G, Vallée C. Evaluation of the implementation of the Montreal At Home/Chez Soi project. BMC Health Services Research. 2014; 14 :557. doi: 10.1186/s12913-014-0557-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foundations for Evidence-Based Policymaking Act of 2018, 5 U.S.C. §§ 101–311 (2018).
- Gibbs, L., Hawn Nelson, A., Dalton, E., Cantor, J., Shipp, S., & Jenkins, D. (2017). IDS governance: Setting up for ethical and effective use, expert panel report . Actionable Intelligence for Social Policy, University of Pennsylvania. https://www.aisp.upenn.edu/wp-content/uploads/2016/07/Governance.pdf
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. 1999; 89 (9):1322–1327. doi: 10.2105/AJPH.89.9.1322. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Global Implementation Society. (2021). Resource library. https://globalimplementation.org/resources/
- Goering, P., Veldhuizen, S., Watson, A., Adair, C., Kopp, B., Latimer, E., & Aubry, T. (2014). National at home/Chez Soi final report. Calgary, AB: Mental Health Commission of Canada, 48. https://www.mentalhealthcommission.ca
- GPRA Modernization Act of 2010, 31 U.S.C. §§ 1101–1115 (2010).
- Hawn Nelson, A., Jenkins, D., Zanti, S., Katz, M., Burnett, T., Culhane, D., & Barghaus, K. (2020). Introduction to data sharing and integration . Actionable Intelligence for Social Policy. University of Pennsylvania. https://www.aisp.upenn.edu/wp-content/uploads/2020/06/AISP-Intro-.pdf
- Implementation Science Resource Hub. (n.d.). Pick a theory, model, or framework . University of Washington. https://impsciuw.org/implementation-science/research/frameworks/
- Institute for Social Capital. (n.d.) ISC data and research oversight committee . UNC Charlotte Urban Institute. https://ui.uncc.edu/our-work/institute-social-capital/isc-data-and-research-oversight-committee
- International Population Data Linkage Network. (n.d.). About the international population data linkage network. https://www.ipdln.org
- Kay A. Evidence-based policy-making: The elusive search for rational public administration. Australian Journal of Public Administration. 2011; 70 (3):236–245. doi: 10.1111/j.1467-8500.2011.00728.x. [ CrossRef ] [ Google Scholar ]
- Kettl DF. The transformation of governance. Johns Hopkins University Press; 2002. [ Google Scholar ]
- Kettl DF. The next government of the United States: Why our institutions fail us and how to fix them. WW Norton & Company; 2009. [ Google Scholar ]
- Kettl DF. Politics of the administrative process. 5. CQ Press; 2012. [ Google Scholar ]
- Kirchner JE, Ritchie MJ, Pitcock JA, Parker LE, Curran GM, Fortney JC. Outcomes of a partnered facilitation strategy to implement primary care–mental health. Journal of General Internal Medicine. 2014; 29 (4):904–912. doi: 10.1007/s11606-014-3027-2. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the consolidated framework for implementation research. Implementation Science. 2015; 11 (1):1–13. doi: 10.1186/s13012-016-0437-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kitzmiller, E. (2014). The circle of love: South Carolina’s IDS case study. Actionable Intelligence for Social Policy, University of Pennsylvania. https://www.aisp.upenn.edu/wp-content/uploads/2015/08/SouthCarolina_CaseStudy.pdf
- Koczwara B, Stover AM, Davies L, Davis MM, Fleisher L, Ramanadhan S, Schroeck FR, Zullig LL, Chambers DA, Proctor E. Harnessing the synergy between improvement science and implementation science in cancer: A call to action. Journal of Oncology Practice. 2018; 14 (6):335. doi: 10.1200/JOP.17.00083. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Laklija M, Babić MM, Cheatham LP. Institutionalization of children with disabilities in Croatia: Social workers' perspectives. Child & Youth Services. 2020; 41 (2):184–203. doi: 10.1080/0145935X.2020.1752170. [ CrossRef ] [ Google Scholar ]
- Lane-Fall MB, Curran GM, Beidas RS. Scoping implementation science for the beginner: Locating yourself on the “subway line” of translational research. BMC Medical Research Methodology. 2019; 19 (1):133. doi: 10.1186/s12874-019-0783-z. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lindblom CE, Cohen DK. Usable knowledge: Social science and social problem solving. Yale University Press; 1979. [ Google Scholar ]
- Marr MD. Better must come. Cornell University Press; 2015. [ Google Scholar ]
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, Gask L, MacFarlane A, Murray E, Rapley T, Rogers A, Treweek S, Wallace P, Anderson G, Burns J, Heaven B. Understanding the implementation of complex interventions in health care: The normalization process model. BMC Health Services Research. 2007; 7 (1):1–7. doi: 10.1186/1472-6963-7-148. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McKay VR, Morshed AB, Brownson RC, Proctor EK, Prusaczyk B. Letting go: Conceptualizing intervention de-implementation in public health and social service settings. American Journal of Community Psychology. 2018; 62 (1–2):189–202. doi: 10.1002/ajcp.12258. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michie S, Van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Science. 2011; 6 (1):1–12. doi: 10.1186/1748-5908-6-42. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moullin JC, Dickson KS, Stadnick NA, Rabin B, Aarons GA. Systematic review of the exploration, preparation, implementation, sustainment (EPIS) framework. Implementation Science. 2019; 14 (1):1–16. doi: 10.1186/s13012-018-0842-6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Association of Counties. (2020). 2020 NACo policy priorities . https://www.naco.org/resources/featured/2020-naco-policy-priorities
- National Collaborating Centre for Methods and Tools. (2016). Implementation frameworks, theories and models: An interactive site for practitioners and researchers . McMaster University. http://www.nccmt.ca/resources/search/254
- National Implementation Research Network. (n.d.). Module 2: Implementation drivers. https://nirn.fpg.unc.edu/module-2/implementation-drivers
- National Institute on Drug Abuse. (2020). Opioid overdose crisis . https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis
- Nilsen P. Making sense of implementation theories, models and frameworks. Implementation Science. 2015; 10 (1):1–13. doi: 10.1186/s13012-015-0242-0. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Norton WE, Chambers DA, Kramer BS. Conceptualizing de-implementation in cancer care delivery. Journal of Clinical Oncology. 2019; 37 (2):93–96. doi: 10.1200/JCO.18.00589. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nutley SM, Walter I, Davies HT. Using evidence: How research can inform public services. Policy Press; 2007. [ Google Scholar ]
- Padgett D, Henwood BF, Tsemberis S, Tsemberis SJ. Housing first: Ending homelessness, transforming systems, and changing lives. Oxford University Press; 2016. [ PubMed ] [ Google Scholar ]
- The Pew Charitable Trusts. (2021). Results first clearinghouse database . https://www.pewtrusts.org/en/research-and-analysis/data-visualizations/2015/results-first-clearinghouse-database
- Pew-MacArthur Results First Initiative. (2014). Evidence-based policymaking: A guide for effective government . http://www.pewtrusts.org/~/media/assets/2014/11/evidencebasedpolicymakingaguideforeffectivegovernment.pdf
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research. 2011; 38 (2):65–76. doi: 10.1007/s10488-010-0319-7. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Prusaczyk B, Swindle T, Curran G. Defining and conceptualizing outcomes for de-implementation: Key distinctions from implementation outcomes. Implementation Science Communications. 2020; 1 :1–10. doi: 10.1186/s43058-020-00035-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Public Health Agency of Canada. (n.d.). Canadian best practices portal . https://cbpp-pcpe.phac-aspc.gc.ca/interventions/search-interventions/
- Rohe WM. Tackling the housing affordability crisis. Housing Policy Debate. 2017; 27 (3):490–494. doi: 10.1080/10511482.2017.1298214. [ CrossRef ] [ Google Scholar ]
- Sanderson I. Evaluation, policy learning and evidence-based policy making. Public Administration. 2002; 80 (1):1–22. doi: 10.1111/1467-9299.00292. [ CrossRef ] [ Google Scholar ]
- Shea CM, Turner K, Albritton J, Reiter KL. Contextual factors that influence quality improvement implementation in primary care: The role of organizations, teams, and individuals. Health Care Management Review. 2018; 43 (3):261. doi: 10.1097/HMR.0000000000000194. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- State Data Sharing Initiative. (2018). Data sharing toolkit. The Center for Regional Economic Competitiveness. http://www.statedatasharing.org/data-sharing/#toolkit
- Stefancic A, Tsemberis S, Messeri P, Drake R, Goering P. The Pathways Housing First fidelity scale for individuals with psychiatric disabilities. American Journal of Psychiatric Rehabilitation. 2013; 16 (4):240–261. doi: 10.1080/15487768.2013.847741. [ CrossRef ] [ Google Scholar ]
- Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: Models for dissemination and implementation research. American Journal of Preventive Medicine. 2012; 43 (3):337–350. doi: 10.1016/j.amepre.2012.05.024. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Taylor, A. (2020). How the split over masks sums up America’s chaotic coronavirus response. The Washington Post. https://www.washingtonpost.com/world/2020/06/25/face-masks-america-divided/
- The California Evidence-Based Clearinghouse for Child Welfare. (n.d.). CEBC overview . https://www.cebc4cw.org/
- Thomas, M.L., Hutchison, J., Lane, J., Carman, J., Schulkind, L., & Vercruysse, C. (2020a). Housing First Charlotte-Mecklenburg Research & Evaluation Project: Outcomes & service utilization final report. https://ui.uncc.edu/sites/ui.uncc.edu/files/media/HFCM%20Final%20Outcomes%20Report%202020-Final.pdf
- Thomas, M.L., Hutchison, J., Lane, J., Carman, J., Schulkind, L., & Vercruysse, C. (2020b). Housing First Charlotte-Mecklenburg Research & Evaluation Project: Process evaluation final report. University of North Carolina at Charlotte. https://ui.uncc.edu/sites/ui.uncc.edu/files/media/V3HFCM%20Final%20Process%20Evaluation%20Report%202020-Final%209-2-20v3.pdf
- Title IV-E Prevention Services Clearinghouse. (n.d.). Description . https://preventionservices.abtsites.com/
- Whittaker E, Swift W, Flatau P, Dobbins T, Schollar-Root O, Burns L. A place to call home: Study protocol for a longitudinal, mixed methods evaluation of two housing first adaptations in Sydney, Australia. BMC Public Health. 2015; 15 (1):1–9. doi: 10.1186/s12889-015-1700-y. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization. (2020). Opioid overdose . https://www.who.int/news-room/fact-sheets/detail/opioid-overdose
- Wulczyn, F., Alpert, L., Martinez, Z., & Weiss, A. (2015). Within and between state variation in the use of congregate care . The Center for State Child Welfare Data, Chapin Hall at theUniversity of Chicago. https://fcda.chapinhall.org/wp-content/uploads/2015/07/Congregate-Care_webcopy.pdf
- Zanti, S., Jenkins, D., Berkowitz, E., Hawn Nelson, A., Burnett, T., & Culhane, D. (2021). Building and sustaining state data integration efforts: Legislation, funding, and strategies . Actionable Intelligence for Social Policy. University of Pennsylvania. https://www.aisp.upenn.edu/resource-article/building-sustaining-state-data-integration-efforts-legislation-funding-and-strategies/

Enter the URL below into your favorite RSS reader.
“Teamwork Makes the Dream Work”: Infusing Interprofessional Education Into Human Services Curriculum and Training
- Citation (BibTeX)
View more stats
Given the provision of health and wellness services is shifting towards an interdisciplinary framework, human services professionals may be in a unique position to collaborate with various professionals in the pursuit of client welfare. To competently engage in interprofessional care, interprofessional education (IPE) in human services training programs is necessary. This paper points to the alignment between human services organizations, values, and practice with the Interprofessional Education Collaborative’s competencies and makes recommendations for the didactic infusion of IPE into human services programs, curricula, coursework, and experiences.
Within healthcare and human services, interprofessional collaboration (IPC) occurs when individuals from at least two distinct professional identities work together to achieve various client outcomes (Interprofessional Education Collaborative , 2016) . Interprofessional education (IPE) “occurs when two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes” (World Health Organization , 2010 , p. 13) and may serve as a key mediating factor in various professionals’ abilities to engage in effective IPC. This article provides a general overview into the competencies and effectiveness of IPC, leading to specific recommendations for didactic training and implications for IPE in human services educational programs.
Interprofessional Collaboration
Human services professionals (HSPs) have the capacity to be in collaboration with a variety of professionals to promote quality, comprehensive care for clients. The role of a HSP has been described as that of a generalist, in which they exhibit knowledge and skills that enable them to work collaboratively with interdisciplinary professionals (Johnson et al. , 2017; Neukrug , 2017) . This description highlights the importance of IPC for effective practice as an HSP. As they interact with clients and conceptualize their unique experiences, the opportunity to coordinate care with medical providers (i.e., physicians), specialty mental and behavioral health providers (i.e., counselors), and community welfare providers (i.e., social workers) becomes apparent and is documented in current research. Johnson (2016) has found HSPs to have a wide range of engagement in weekly IPC, varying between minimal to frequent collaboration with counselors and allied health professionals. Case managers specifically have been identified as inherently collaborative professionals (Fink-Samnick , 2019) . Within their roles, case managers are recognized as vital in facilitating IPC in medical settings and during mental health crises through care and referral coordination, the use of assessments, strong relationships with clients, and professional flexibility (Donovan et al. , 2018; Teper et al. , 2020; Winters et al. , 2015) .
HSPs also have the opportunity to influence the biological, psychosocial, and environmental conditions in which clients exist, known as social determinants of health (SDOH). As per the Health People 2030 initiative, SDOH encapsulates numerous factors towards health and wellness, including economic stability, education and healthcare quality and access, neighborhood environment, and the overarching social context (Office of Disease Prevention and Health Promotion , n.d.) Through IPC, HSPs have the opportunity to work on interdisciplinary teams to effectively address SDOH and increase overall health and wellness of clients (Robins et al. , 2021) . In this way, HSPs can serve to bridge the gap between various medical, psychological, community, and social services that can improve the quality of life of clients they serve.
IPC has been found to be vital for effective practice for a broad range of medical, mental health, and helping professions like human services. Further, it is related to improved patient outcomes when receiving health and wellness services, including enhanced quality of and access to services (Cox et al. , 2014; Donovan et al. , 2018) , positive client experience (Davidson et al. , 2022) , satisfaction (Will et al. , 2019) , and increased prevalence of holistic care related to case conceptualization and treatment planning (Winfield et al. , 2017) . Researchers emphasizing increased quality of care and improved client outcomes when IPC is practiced suggest that human services educational programs should incorporate IPC activities, assignments, and courses into their curricula. Because IPC smoothly aligns with the field of human services in values and practice, there can be a natural addition of IPC to already excellent human services education.
Interprofessional Competency Alignment with Human Services
With the goal of advancing team-based care amongst health and helping professionals for ameliorated client outcomes, the Interprofessional Education Collaborative (IPEC , 2016) has identified four core competencies for practical application of IPC: (1) Values and Ethics (work with individuals of other professions to maintain a climate of mutual respect and shared values), (2) Roles and Responsibilities (use the knowledge of one’s own role and those of other professions, (3) Interprofessional Communication (communicate in a manner that supports a team approach), and (4) Teams and Teamwork (apply relationship-building values and the principles of team dynamics to perform effectively in different team roles). The competencies were developed by purposefully building upon individual professions’ established competencies to both reaffirm them and broaden them to be applicable to integrated care. Englander et al. (2013) mapped 153 different competency lists from nine health professions and found IPC to be a generally applicable domain. While human services was not identified as a unique health profession in the research, the IPEC competencies directly align with the human services definition, practices, and values. The IPEC competencies are explicitly:
patient centered; community and population oriented; relationship focused; process oriented; linked to learning activities, educational strategies, and behavioral assessments that are developmentally appropriate for the learner; able to be integrated across the learning continuum; sensitive to the systems context and applicable across practice settings; applicable across professions; stated in language common and meaningful across the professions; and outcome driven. (IPEC , 2016 , p. 10)
This language mirrors language from several human services sources, including the National Organization for Human Services’ (NOHS) definition for itself, the Journal of Human Services , and the NOHS Ethical Code.
The definition of human services according to NOHS exemplifies its inherently interdisciplinary nature:
[Human services] uniquely approach[es] the objective of meeting human needs through an interdisciplinary knowledge base,… The Human Services profession is one which promotes improved service delivery systems by addressing not only the quality of direct services, but also by seeking to improve accessibility, accountability, and coordination among professionals and agencies in service delivery. (NOHS , 2022 , p. 1) .
Further, the Journal of Human Services produced a special interdisciplinary topics issue in 2021 that called for research and writing from “researchers, faculty, administrators, and practitioners in human services, psychology, social work, counseling, criminal justice, medicine and health, education, and associated fields… [such as] public safety, government and non-profit agencies, and faith-based programs” (NOHS , 2021 , pp. 1–2) . This issue of the journal recognized that the “perspectives of various disciplines and professions working together… [can] construct systematic, efficient, and effective approaches to care within the scope of human services’ mission to meet human needs through prevention, intervention, and advocacy to improve the overall quality of life” (NOHS , 2021 , p. 2) .
Finally, interdisciplinary language that mirrors the IPEC (2016) competencies is specifically demonstrated by the NOHS (2015) Code of Ethics. Here, we introduce the IPEC competencies and associated NOHS standards as they are written, followed by a brief discussion on the intersection of these two professional documents (see Table 1 ).
| : Work with individuals of other professions to maintain a climate of mutual respect and shared values. | : Human service professionals promote cooperation among related disciplines to foster professional growth and to optimize the impact of inter-professional collaboration on clients at all levels. |
| : Use the knowledge of one’s own role and those of other professions to appropriately assess and address the health care needs of patients and to promote and advance the health of populations. | : Human service professionals avoid duplicating another professional's helping relationship with a client. They consult with other professionals who are assisting the client in a different type of relationship when it is in the best interest of the client to do so. In addition, human services professionals seek ways to actively collaborate and coordinate with other professionals when appropriate. |
| : Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease | : Human service professionals avoid duplicating another professional's helping relationship with a client. They consult with other professionals who are assisting the client in a different type of relationship when it is in the best interest of the client to do so. In addition, human services professionals seek ways to actively collaborate and coordinate with other professionals when appropriate. |
| : Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable. | : Human service professionals know the limit and scope of their professional knowledge and offer services only within their knowledge, skill base, and scope of practice. : Human service professionals continually seek out new and effective approaches to enhance their professional abilities and use techniques that are conceptually or evidence based. When practicing techniques that are experimental or new, they inform clients of the status of such techniques as well as the possible risks. : Human service professionals hold a commitment to lifelong learning and continually advance their knowledge and skills to serve clients more effectively. |
First, IPEC competency 1: values and ethics for interdisciplinary practice is inherent in Standard 29, calling for cooperation among related disciplines to foster professional growth and to optimize the impact of inter-professional collaboration on clients at all levels. Next, IPEC competency 2: knowledge of one’s own role and those of other professions reflects Standard 19 stating that human service professionals avoid duplicating another professional’s helping relationship with a client. They consult with other professionals who are assisting the client in a different type of relationship. Third, for IPEC competency 3, they communicate in a responsive and responsible manner aligning with Standard 19 indicating that human services professionals seek ways to actively collaborate and coordinate with other professionals when appropriate. Fourth, for IPEC competency 4, they apply relationship-building values and team dynamics to perform effectively in different team roles as in Standard 27 through which human service professionals know the limit and scope of their professional knowledge; Standard 31 stating that human service professionals continually seek out new and effective approaches to enhance their professional abilities; and Standard 36 proclaiming that human service professionals hold a commitment to lifelong learning and continually advance their knowledge and skills. NOHS, its flagship journal, and its code of ethics indicate close alignment with the IPEC (2016) competencies. Thus, we can further promote the ethical standards and values of NOHS by integrating IPC into coursework, curricula, and programs, while also affirming a strong professional identity in HSPs and improving the quality of care they provide to clients.
IPE in Human Services Curriculum
The IPEC competencies were designed to guide curricula in myriad health fields including dentistry, medicine, public health, and any field devoted to improved health outcomes for populations it serves (IPEC , 2016) . IPE can be facilitated in human service programs through a variety of avenues. This may include embedded topics in core courses for human services students, independent coursework emphasizing IPC, and experiential learning activities alongside various healthcare and social service professionals within a campus community (Park et al. , 2019) . The crux of incorporating IPE into human services training is to promote a curriculum that fosters shared experiences, learning, and practice between various disciplines (Bridges et al. , 2011) .
Benefits of IPE
The importance of IPC has been recognized by a diverse range of health professions, leading towards research into the effects of IPE for effective practice. For allied health professionals who utilize IPC, IPE is related to improved confidence in discharge planning, shared decision making, and clinical thinking skills (Smith et al. , 2018) . Discharge planning has been identified as a critical role for health professionals, especially case managers, in which active collaboration with clients and interdisciplinary professionals is required to solve complex clinical concerns, such as hospital readmission (Hunter et al. , 2013) . Additionally, researchers have found IPE workshops and coursework is related to improved understanding of the roles of various disciplines, respect for interdisciplinary teams, communication for IPC, and self-assessment of IPEC competencies (Roberts et al. , 2019; Singh et al. , 2019) . This indicates the importance of IPE towards outcomes that may improve IPC and client care, such as meeting IPEC competencies, interdisciplinary communication, and collaborative problem solving between professionals. Further, IPE programs were found to be effective in increasing students’ skills and conceptualization of IPC, commitment to collaboration, and understanding of various professionals’ roles and responsibilities (Brandon & Knapp , 1999) .
While limited, available research on the impact of IPE specifically for human services students does indicate promising results regarding the effectiveness of IPE for HSPs-in-training. Researchers have found that an IPE course designed for human services, public health, and nursing students was related to improvements in all four IPC competency domains set forth by IPEC (Porter et al. , 2018 , 2020) . This highlights the relationship between IPE coursework and IPEC competencies for students studying to be HSPs. The importance of the IPEC competencies for effective IPC has been identified (Ansa et al., 2020; Chen et al. , 2018 ), and while research surrounding IPE for human services education is a recently emerging field, the available literature indicates the benefits of infusing IPE into educational programs for HSPs-in-training.
In addition to human services students, IPE has been related to benefits for other stakeholders, such as institutions and surrounding communities. These benefits include enhanced engagement and involvement with the local community, improved collaboration between departments within an academic setting, and the introduction of novel educational strategies faculty can implement to promote student learning (Brandon & Knapp , 1999) . Throughout undergraduate and graduate training experiences for human services professionals, there are opportunities to infuse IPE throughout didactic training and experiential learning.
Challenges of IPE
Despite the benefits of infusing IPE into human services education, it is important for educators to acknowledge the various professional, institutional, and interpersonal challenges associated with this adjustment to the curriculum (Lawlis et al. , 2014) so that human services faculty can effectively address them. Across professions that value IPC, lack of adequate funding is a common challenge in the implementation of IPE (Kruse , 2012; Lawlis et al. , 2014; Schapmire et al. , 2018; Ward et al. , 2018) . This lack of funding may contribute to difficulties compensating educators and allocating institutional funds towards facilitating interprofessional learning (Ward et al. , 2018) . For this reason, past literature exploring the challenges to implementing IPE across health and wellness professions have encouraged institutions to seek federal, state, and regional grants to better enable academic programs to provide IPE to students (Lawlis et al., 2018; Schapmire et al. , 2018 ). Federal organizations such as the Health Resources and Services Administration (HRSA) have historically provided grant funding for programs who seek to incorporate IPE, IPC, and integrated behavioral health into programs training the next generation of health and wellness professionals. For human services educators, grants from HRSA and similar organizations may be instrumental in developing and implementing IPE for future HSPs in academia.
Professional differences in values and vision surrounding IPE is another common challenge that educators must address (Kruse , 2012; Lash et al. , 2014; Lawlis et al. , 2014; Ward et al. , 2018) . Related to this issue, ensuring accurate representation of diverse professionals is a challenge (Schapmire et al. , 2018) , despite the importance of exposure to different professions in IPE experiences (Champagne-Langabeer et al. , 2019) . To address this concern, facilitators of IPE can model IPC by designing educational experiences that are informed by the values, ethics, and competencies of IPEC and the diverse organizations whose professionals engage in IPC, such as NOHS, American Counseling Association, American Psychological Association, National Association of Social Workers, American Nurses Association, American Medical Association, and other professional allied health organizations. Additional challenges related to educator training (Freeman et al. , 2010; Lawlis et al. , 2014; Schapmire et al. , 2018; Singh et al. , 2019) , logistical and administrative barriers such as campus location and scheduling (Kruse , 2012; Schapmire et al. , 2018; Ward et al. , 2018) , and institutional support for interdisciplinary education (Lash et al. , 2014) must be considered. These have the potential to be addressed with intentional collaboration and planning from interdisciplinary faculty of programs that would benefit from comprehensive IPE, including human services students.
Implications for Human Services Educators
In order to contribute and stay relevant to the health and helping professions, HSPs need the knowledge and skills to effectively participate in IPC. “Interprofessional,” “interdisciplinary,” and “integrative” are buzz words in the helping fields and in research on health and helping professions. So that HSPs stay current with the trends in health and helping practice, human services educators should further educate themselves and enhance their courses and curricula with IPC (Johnson et al. , 2017; Park et al. , 2019; Winfield et al. , 2017) . Human services is a unique and often misunderstood profession (Neukrug , 2017) ; thus, human services students need to learn how to identify their role in any interprofessional encounter. IPE may not only prepare students for IPC, but may increase their self-efficacy as professionals. The unique human services identity can be clarified by confident and knowledgeable HSPs who assert themselves as legitimate members of interprofessional teams. Human services educators already providing exceptional human services education can enact IPC activities, assignments, experiences, and curriculum to enhance the quality and relevancy of the education they provide to their students. Below we present examples of such activities, assignments, experiences, and curricula in the hope that they are a springboard for more research and practice of IPE in human services education.
Didactic Recommendations
Within human services educational programs, there are ample opportunities to incorporate IPE activities and experiences into existing coursework. Table 2 provides an exploration into potential IPE activities and associated human services courses in which integration of these activities may serve to enhance student learning and preparation for IPC.
| In class activity asking students to match a NOHS standard with each IPEC competency, followed by discourse about their alignment. Instructors may use Socratic questioning (thoughtful, curious questioning used to examine complex and challenging topics) to explore the implications for IPC. The above activity may be followed with an assignment asking students to critically examine how NOHS’ values and standards compare and contrast to the values and ethics of other professional organizations (i.e., American Counseling Association, American Medical Association). In the assignment students should a) compare and contrast human services values and practice to other related professions, b) identify new discoveries they find intriguing, and c) explore an area of growth for themselves as a future HSP engaging in IPC. | |
| Guest lectures from interdisciplinary professionals who work with HSPs in different settings (i.e., correctional facilities, hospitals, government agencies, educational settings, etc.) Instructors can prepare guest lectures to speak about a) their career journey, b) their conception of IPC and their role in it, c) how they view and have worked with HSPs in interprofessional settings, and d) what they predict continuing development of IPC will look like. | |
| Role-plays for basic IPC communication skills (i.e., active listening, sharing professional values) to provide foundational communication and collaborative skills necessary for interdisciplinary integration and competence. Instructors can ask students to take on assigned roles (HSP, medical doctor, nurse, counselor, social worker) and research the values of that profession. Students should engage in a group discussion sharing the values of each role. To conclude, they should write a reflection on the role-play to include a) a description of their profession’s values, b) an identification of the profession with which their profession most closely aligned and from which it most deviated, and c) a reflection on the challenges and benefits of sharing professional values they observed during the role play. | |
| Role-plays for advanced IPC communication skills (i.e., treatment planning, conflict resolution). Instructors can ask students to engage in a treatment planning process for a case scenario client by assigning students various interprofessional roles (i.e., HSP, medical doctor, nurse, counselor, social worker). Students prepare together to implement different treatments according to their roles. They should prepare a group presentation that a) describes each group member’s role in the IPC, b) explores how the interventions would support each other and potentially conflict, and c) explains why the integrative treatment they suggest is the best individualized treatment for the case scenario client by considering their medical, psychological, and social needs, as well as their backgrounds, cultures, and life experiences. | |
| Assignments emphasizing experiential and service learning in IPC (i.e., interprofessional communication plan, interprofessional advocacy plan, shadowing a practicing HSP). | |
| Following in-class role plays of sharing professional values and preparing an interdisciplinary treatment plan, they should engage in real life engagement with students from other departments (i.e., nursing, pre-medical/medical, psychology, physical therapy). Collaborating with multiple departments may be challenging, but the benefits to all students makes it worth considering. The goal of the interaction could be to a) create an IPC plan to comprehensively address the presenting concern(s) in a provided case scenario, b) reflect by writing on the barriers they encountered, c) reflect on the ways each profession enhanced the treatment plan in the scenario, and d) how they would work with other professionals in the future. | |
| Programs could explore the creation of a stand-alone IPE course. Topics and assignments could include reflections on HSPs’ roles in IPC, case conceptualization, treatment planning, using evidence-based practices, evaluation of practices in IPC setting. This could be supplemented by interdisciplinary seminars, lectures, and presentations led by faculty from various departments on campus. Additionally, assignments to address interdisciplinary conflict, ethical dilemmas, treatment planning, and discharge planning can serve to enhance preparation for IPC. |
Given the alignment between the IPEC (2016) competencies and NOHS (2015) ethical standards, human services faculty have the opportunity to integrate IPE into didactic coursework and curriculum that train future HSPs. IPE can be infused into introductory human services courses (i.e., Introduction to Human Services, Human Services Methods) that provide students with the foundational skills, knowledge, and professional dispositions for effective practice. This can be done by inviting guest lecturers from interdisciplinary professions to provide their perspectives on IPC, the roles of HSPs, and effective practices for IPC in their respective settings. Additionally, faculty can present students with opportunities to directly practice the broad range of skills for IPC, such as active listening, interdisciplinary communication, conflict resolution, treatment planning, navigating different professional values and ethics, and addressing systemic factors related to client outcomes. This can be done in both introductory and advanced (i.e., Crisis Intervention, Prevention, and Ethics, Substance Abuse Treatment and Research) human services courses, with faculty designing role plays and case studies that attend to the unique developmental levels of students at various stages of professional development. In this way, students in the beginning of their academic career can learn the basic skills for effective IPC based on IPEC competencies, while students who are preparing for the transition professional settings or graduate education can further hone their skills needed for competence in IPC.
Didactic training in IPE can also occur through the development of new elective courses. These courses can focus on IPEC competencies, best-practices for IPC, and consistent interaction with various professions. These learning experiences can be created collaboratively and offered between departments within a campus community, including human services, psychology, nursing, pre-medicine, and other allied health professions. Courses such as this may feature numerous co-instructors from these departments to promote regular engagement with interdisciplinary professionals who are called to collaborate for client health and wellness. Didactic activities in these electives may include group projects in which students from interdisciplinary departments are presented with case scenarios with client concerns that cannot be adequately addressed through the values, skills, and practices of a singular profession. These activities can be supplemented by lectures, presentations, and role-plays facilitated by interdisciplinary instructors, providing students with scaffolding through modeling effective IPC practices. In this format, students in human services education can experience stages of exposure, immersion, and mastery of IPC (Charles et al. , 2010) , improving preparation for collaboration.
Experiential Learning
Experiential learning is an important component of human services education (Patil et al. , 2020) and IPE (Curran et al. , 2010) , as it promotes application of basic and advanced concepts needed for competent practice. Students can engage in experiential learning by shadowing human services professionals who engage in IPC regularly, allowing for students to observe ways to engage in IPC as a human service professional and receive scaffolding for competent practice. Experiential learning could be integrated into observation and professional development courses such as Case Management & Crisis Techniques Through Field Observation. Additionally, human service internship opportunities within integrated institutions can be facilitated as a part of the Internship in Human Services course. Integrated settings for human services professionals in their internship may include correctional facilities, general hospitals, primary care clinics, inpatient and residential psychiatric facilities, specialty care medical and behavioral health settings, university health centers, regional and local government agencies, and community health centers, among others. In these experiences, students could directly practice IPC as a professional-in-training while under the supervision of a competent HSP supervisor. The experience of shadowing and internships may be significant in promoting skills and competencies of IPC while integrating IPE into human services educational programs.
Finally, IPE can be integrated into experiential learning by creating interprofessional learning activities enmeshed in various core and elective courses, where students from different departments are called to collaborate. These learning activities may include case studies, standardized role-plays, and advanced client simulations in which there is a problem to be solved from an interdisciplinary perspective. Emphasis can be placed on small groups of students from different professions working together to address interdisciplinary ethical dilemmas, collaborative treatment planning, and discharge planning. In these experiences, IPC may be taught and applied in a low-risk IPE environment, allowing students to make mistakes, attempt new skills, and learn more the professional identity of human services and other professionals.

Discussion and Future Research
There is limited research examining the benefits and outcomes of IPE in human services education, yet there is the promise to enhance the education of human services through these experiences and room to conduct studies. Currently, the bulk of research on IPE and IPC exists within the realms of medical (i.e., nursing, family medicine), social and behavioral health (i.e., social work, psychology), and allied health (i.e., occupational therapy) professions. Future research could explore the impact of IPE on human services student outcomes, such as HSPs’ self-efficacy as generalists within interdisciplinary settings, utilization and understanding of IPEC competencies, and ability to effectively engage in IPC with other professionals. This may serve to better inform human services educators on the unique benefits of infusing IPE into human services education. Additionally, human services educators can contribute to the growing empirical base for IPE in the profession by exploring the impact of experiential and service learning within educational settings for future HSPs. This can be done by exploratory research into the experiences of HSPs-in-training during IPE activities (i.e., case studies, role plays) and in supervised internship settings, such as hospitals, where students frequently engage in IPC.
To better understand the factors that facilitate effective IPE, research that explores the professional experiences, training, and challenges of IPE and IPC among human services faculty and professionals may yield information that can inform pedagogical, institutional, and interdepartmental practices that facilitate or hinder effective IPE. Additionally, an exploration of students’ perspectives on their experiences and understanding of IPE may yield important insights into the best practices for infusing IPE into human services curriculum.
HSPs seek to serve clients in a comprehensive manner, and they increasingly understand the importance of effective IPC for optimal client outcomes. As generalists, HSPs have the capacity to contribute to interdisciplinary teams in meaningful ways, ultimately improving the biopsychosocial conditions in which clients exist. In order to do so, an accurate understanding and effective practice of IPC is vital, yet human services programs may not be adequately preparing HSPs-in-training with the knowledge and skills to serve in this role. By incorporating IPE into coursework, human services faculty may provide students with experiences to better prepare them to work in an increasingly connected professional world.

Case Management for Human Services Before and After COVID-19
Human services organizations of all sizes rely heavily on case management to improve outcomes for their clients. As stated in the pre-pandemic Salesforce.org Nonprofit Trends Report , “demand for more nonprofit programs and services is rising, as the world is threatened by climate change, natural and human-made disasters, humanitarian crises, political chaos, food insecurity, and so much more.” Since COVID-19 has impacted communities globally, the need for case management to support increasing at-risk populations worldwide has only grown. Learn more about case management, the guiding principles of effective case management and how COVID-19 has impacted the practice on our new Exponent Case Management blog here.
Share this Content

Time is Ticking: A Roadmap for Replacing foundationConnect

Catholic Charities USA 2024 Annual Gathering
Case Study: Tipping Point Community

Ethical Standards
Ethical standards for human services professionals, national organization for human services adopted 2024.
| Preamble | Responsibility to the Public & Society |
| Responsibility to Clients | Responsibility to Employers |
| Responsibility to Colleagues | Responsibility to Students |
| Responsibility to the Profession | Responsibility to Self |
The field of human services is broadly defined, uniquely approaching the objective of meeting human needs through an interdisciplinary knowledge base, focusing on prevention as well as remediation of problems, and maintaining a commitment to improving the overall quality of life of service populations. The human services profession is one which promotes improved service delivery systems by addressing not only the quality of direct services, but also by seeking to improve accessibility, accountability, and coordination among professionals and agencies in service delivery.
Ethics Code Purpose :
The purpose of this ethics code is to establish a set of principles and standards to guide decision-making and conduct for all human services professionals. It serves to safeguard the well-being of clients, uphold the integrity of the profession, and foster trust and respect in all professional relationships. This code is designed to promote excellence in service delivery, ensure ethical practice in diverse social contexts, and address ethical dilemmas with professionalism and moral clarity. By adhering to this code, members commit to the highest standards of ethical behavior of their field which transcend legal requirements, foster enduring trust and respect, and advance the principles of human dignity, social justice, and responsible stewardship of the care placed in them by clients and society towards making profound contributions to their well-being.
Persons who use this code include members of the National Organization for Human Services, students in relevant academic degree programs, faculty in those same programs, researchers, administrators, practitioners, employers, supervisors, and others in community agencies who identify with the human services field (henceforth all are referred to throughout this code as human service professionals). The ethical standards are organized according to defined professional domains.
This ethics code emphasizes our unwavering commitment to ethical decision-making, a cornerstone of the human services profession. This commitment obliges all human service professionals to engage in continuous reflection, prioritize the welfare and rights of service recipients, and navigate complex ethical landscapes with diligence and moral clarity. It mandates the seeking of counsel and adherence to established ethical guidelines when confronting dilemmas, and ensures decisions are made with integrity and transparency.
Responsibility to Clients
STANDARD 1 Human service professionals recognize and build on client and community strengths.
STANDARD 2 At the beginning of the helping relationship, human service professionals obtain informed consent for services from clients. Clients should be informed that they may withdraw consent at any time and can ask questions before agreeing to the services. Clients who are unable to give consent should have those who are legally responsible for them review an informed consent statement document and provide appropriate consent. In the case of mandated services, human service professionals explain to clients their right to consent, including limitations to confidentiality and privacy, and possible consequences from service refusal.
STANDARD 3 Human service professionals protect the client's right to privacy and confidentiality except when such confidentiality would cause serious harm to the client or others, when agency guidelines state otherwise, or under other stated conditions (e.g., local, state, or federal laws). Human service professionals inform clients of the limits of confidentiality prior to the onset of the helping relationship.
STANDARD 4 When a human service professional suspects a client's behavior may endanger themselves or others, they must take appropriate and professional actions to ensure safety, which may include consulting, seeking supervision, or, in accordance with state and federal laws, breaching confidentiality.
STANDARD 5 Human service professionals recognize the potential harm and impaired judgment resulting from dual or multiple relationships with clients. If such relationships cannot be avoided, professionals must assess whether to limit or forego the professional relationship and make appropriate referrals as needed.
STANDARD 6 Human service professionals must not engage in sexual or romantic relationships with current clients. In the case of former clients, their friends, or family, professionals must thoroughly assess any potential harm or exploitative dynamics before considering such relationships.
STANDARD 7 Human service professionals ensure that their values or biases are not imposed upon their clients.
STANDARD 8 Human service professionals are responsible for safeguarding the integrity, safety, and security of client records. Client information, whether in written or electronic form, can only be shared with other professionals with the client's prior written consent, unless required or allowed by law or during professional supervision.
STANDARD 9 When providing services through the use of technology, human service professionals take precautions to ensure and maintain confidentiality and comply with all relevant laws and requirements regarding storing, transmitting, and retrieving data. In addition, human service professionals ensure that clients are aware of any issues and concerns related to confidentiality, service issues, and how technology might negatively or positively impact the helping relationship.
Responsibility to the Public and Society
STANDARD 10 Human service professionals are committed to delivering services equitably, ensuring inclusion and accessibility, and respective diversity by valuing and affirming differences in age, ethnicity, culture, race, ability, gender, gender identity, gender expression, language preference, religion, sexual orientation, socioeconomic status, nationality, and other identities associated with historically marginalized groups.
STANDARD 11 Human service professionals are knowledgeable about their cultures and communities within which they practice. They are aware of diversity in society and its impact on the community as well as individuals within the community. They respect the cultures and beliefs of individuals and groups.
STANDARD 12 Human service professionals have a duty to be informed about relevant local, state, and federal laws. They bear the responsibility to advocate for amendments or changes in regulations and statutes when they conflict with the ethical standards and/or the rights of clients.
STANDARD 13 Human service professionals stay informed about current social issues as they affect clients and communities. If appropriate to the helping relationship, they share this information with clients, groups, and communities as part of their work.
STANDARD 14 Human service professionals are aware of social and political issues, comprehend their effects on clients, and recognize how the impact of such issues vary among individuals from diverse backgrounds.
STANDARD 15 Human service professionals must establish processes to identify client needs and assets, actively draw attention to them, and facilitate planning and advocacy at individual, community, and societal levels to address them.
STANDARD 16 Human service professionals advocate for social justice and seek to eliminate oppression. They raise awareness about systems of discrimination and inequity that affect historically minoritized and marginalized groups and advocate for systemic change to address these inequalities within their workplace, communities, and legislative systems.
STANDARD 17 Human service professionals accurately represent the effectiveness of their treatment programs, interventions, and techniques, substantiating claims with empirical data and/or sound theoretical inferences whenever feasible.
Responsibility to Colleagues
STANDARD 18 Human service professionals avoid duplicating another professional's helping relationship with a client. With written permission from their client, human service professionals consult with other professionals who are assisting the client in a different type of relationship when it is in the best interest of the client to do so.
STANDARD 19 When human service professionals have a conflict with a colleague, they first seek out the colleague to manage the problem. If this effort fails, the professional then seeks the assistance of supervisors, consultants, or other professionals in efforts to address the conflict.
STANDARD 20 Human service professionals have a duty to respond appropriately to unethical behavior of colleagues. This generally means first discussing the issue directly with the colleague in question, unless there are extenuating circumstances, such as concerns about repercussions due to an existing power relationship. If a satisfactory resolution is not reached or extenuating circumstances exist, the professional should report the colleague's behavior to a supervisor. If the potential unethical behavior is seen as egregious, then the individual should report the behavior to the colleague’s professional association, credentialing board, police, and/or other administrators or boards, as appropriate.
STANDARD 21 Clients have a right to information discussed between their helper and other professionals, except when state or federal law notes otherwise. All information discussed among professionals should be kept confidential from all others, except when withholding information would lead to harm to clients, others, or communities.
Responsibility to Employers
STANDARD 22 Human service professionals honor their commitments to employers to the fullest extent possible.
STANDARD 23 Human service professionals participate in efforts to establish and maintain employment conditions which are conducive to high quality client services. Whenever possible, they assist in evaluating the effectiveness of the agency through reliable and valid assessment measures.
STANDARD 24 When a conflict arises between fulfilling the responsibility to the employer and the responsibility to the client, human service professionals work with all involved to manage the conflict.
Responsibility to the Profession
STANDARD 25 Human service professionals seek the training, experience, education, and supervision necessary to ensure their effectiveness in working with culturally diverse individuals, families, and communities.
STANDARD 26 Human service professionals provide services only within their expertise and scope of practice, recognizing the limits to their knowledge and skills.
STANDARD 27 Human service professionals must accurately represent their
qualifications, encompassing, but not limited to, their skills, education, credentials, training,
and areas of expertise, to the client, colleagues, and members of the public. When any intentional or accidental misrepresentation is discovered, they must take immediate action to rectify the situation.
STANDARD 28 Human service professionals must pursue relevant consultation and supervision to guide their decision-making in the face of legal, ethical, or other complex dilemmas.
STANDARD 29 Human service professionals promote cooperation across related disciplines, aiming to enhance professional development and maximize the benefits of inter-professional collaboration for clients at all levels.
STANDARD 30 Human service professionals are committed to the continued development of the field. They promote professional association memberships, support research initiatives, foster educational advancement, advocate for appropriate legislative actions, and engage in other professional development activities.
STANDARD 31 Human service professionals continually seek out new and effective approaches to enhance their professional abilities and use techniques that are evidence-based. When practicing techniques that are experimental or new, they inform clients of the status of such techniques as well as the possible risks and gain client consent for their usage.
STANDARD 32 Human service professionals engage in research that upholds ethical standards, meets institutional standards, and maintains scientific integrity. Such research accounts for cross-cultural and diversity bias and is reported with transparency regarding its limitations.
STANDARD 33 Human service professionals exercise discretion in sharing personal information on social media, knowing that they reflect the profession of human services. They also reflect on how their public behavior might impact their personal reputation and the perception of their professional community.
Responsibility to Self
STANDARD 34 Human service professionals maintain awareness of their own cultural and diverse backgrounds, beliefs, values, and biases. They recognize the potential impact of these factors on their relationships with others and commit to delivering culturally competent services to all clients.
STANDARD 35 Human service professionals are committed to their personal growth and well-being to ensure they provide the highest quality service to clients. Should they become aware of any physical, emotional, or psychological impediments to their ability to serve clients effectively, they direct clients to appropriate alternative services and seek measures for personal remediation of such impediments via consultation, treatment, or education.
STANDARD 36 Human service professionals are dedicated to lifelong learning, consistently seeking to enhance their knowledge and skills to better serve their clients.
Responsibility to Students
STANDARD 37 Human service educators develop and implement teaching methodologies that are culturally sensitive, using pedagogical approaches that recognize student’s diverse backgrounds and perspectives.
STANDARD 38 Human service educators commit to fostering equity and inclusion, actively employing measures to ensure educational accessibility for students of all abilities.
STANDARD 39 Human service educators uphold high standards of scholarship in their academic, pedagogical, and professional engagements. They remain abreast of developments in the field through active participation in professional associations, attendance at workshops and conferences, and engagement in both the review and conduct of research.
STANDARD 40 Human service educators recognize and acknowledge the contributions of students to their work including, but not limited to, case material, grants, workshops, research, publications, and other related activities.
STANDARD 41 Human service educators monitor students' field experiences to ensure the quality of the placement site, the supervisory experience, and that the educational outcomes align with the objectives of personal, professional, academic, career, and civic development of the student. When students experience potentially harmful situations during field placements, educators provide appropriate investigations and respond as necessary to safeguard the student.
STANDARD 42 Human service educators establish and uphold appropriate guidelines regarding student disclosure of sensitive or personal information. This involves providing students with advance notice of any activities requiring self-disclosure, offering students the option to opt-out of in-depth self-disclosure when reasonable, and ensuring that there are processes in place to discuss and debrief these activities.
STANDARD 43 Human service educators acknowledge the inherent power imbalance in their relationships with students and are committed to defining and upholding clear ethical and professional boundaries. This commitment includes avoiding any behavior that is demeaning, embarrassing, or exploitative. Human service educators are dedicated to treating all students with fairness and equity, actively working to eliminate discrimination in all forms, and ensuring a respectful and inclusive educational environment.
STANDARD 44 Human service educators ensure that students are familiar with, guided by, and held accountable to the ethical standards and policies established by their academic program or department, the specific guidelines outlined in the course syllabus by the instructor, the expectations of their advisors, and the Ethical Standards of Human Service Professionals.
Copyright © 2024 National Organization for Human Services. All rights reserved. Note: This document may be reproduced in its entirety without permission for non-commercial purposes only. Any reproduction, modification, distribution, transmission, or commercial use of this document, or any part thereof, without prior written permission is strictly prohibited.
For more information regarding Ethical Standard please email the NOHS Ethics Chair at [email protected] .
Printer-friendly version of Ethics Code 2024
Previous Code of Ethics
PDF verison of previously adopted Ethics Code 2015
PDF version of previously adopted Ethics Code 1996
- Open access
- Published: 06 September 2024
The state of decentralization of the healthcare system and nutrition programs in the Lao People’s Democratic Republic: an organizational study
- Phonevilay Viphonephom 1 ,
- Sengchanh Kounnavong 2 &
- Daniel Reinharz 1
BMC Health Services Research volume 24 , Article number: 1037 ( 2024 ) Cite this article
Metrics details
The Lao People’s Democratic Republic (Lao PDR), a lower-middle income country, has a higher malnutrition rate than other Southeast Asian countries. The decentralization of healthcare is a determinant of the effectiveness of programs to reduce malnutrition, but no study has focused on this factor in this country. This organizational study explores the state of decentralization of the healthcare system in Lao PDR that underlies the nutrition programs in the country.
A qualitative study, which is based on a neo-institutional theory conceptual framework, explored factors related to dominant structure (laws, regulations, resources) and interpretative schemes (dominant ideas and beliefs) that characterize the nutrition services provided in the Lao healthcare system. Twenty-four semistructured interviews were performed with representatives of healthcare institutions involved in nutrition programs at different government levels, external donors and civil society organizations. The interviews were completed with relevant documents. The analysis focused on the convergence of interpretative schemes of the organizations concerned and the coherence between the structure underpinning the nutrition programs and the interpretative schemes.
Services deployed to reduce malnutrition in the Lao PDR remain largely centralized, despite factors specific to the country that led it to promote decentralization of its services. The convergence of interpretive schemes and the coherence between the observed structure and the interpretative schemes of actors at all governance levels ensure the stability of this state of decentralization, which has persisted for almost 50 years.
Nutrition programs in the Laos PDR are largely under the responsibility of the central government. The transformations in the healthcare system, notably with the use of new information technologies and the fact that the provinces are populated by a growing number of professionals trained in nutrition in addition to factors that push the system to be decentralized, such as ethnic diversity, the increasing availability of human resources in provinces, and the use of communication technologies, are not strong enough to change the balance of power between governance levels. The deconcentration that characterizes decentralization is therefore likely to continue for the foreseeable future.
Peer Review reports
The World Health Organization (WHO) defines malnutrition as deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients, encompassing three broad groups of conditions: undernutrition (including wasting, stunting, and underweight); micronutrient-related malnutrition (including deficiencies or excesses of essential vitamins and minerals); and overweight, obesity, and diet-related noncommunicable diseases [ 1 ]. Undernutrition and micronutrient-related malnutrition are the main issues generally addressed by nutrition interventions aimed at five-year-old children in developing countries [ 2 , 3 ]. Children under 5 in lower-middle-income countries are particularly vulnerable to undernutrition and its lifelong effects [ 4 , 5 ], which manifest as wasting (acute undernutrition or severe weight loss due to insufficient food intake and/or infectious disease), stunting (chronic undernutrition leading to low height-for-age and irreversible long-term physical and cognitive damage), and underweight (low weight-for-age, potentially indicating stunting, wasting, or both) [ 5 ]. The WHO highlights that nearly half of deaths among children under 5 years of age are linked to undernutrition. These deaths predominantly occur in low-and middle-income countries [ 1 ].
Undernutrition among children under five years of age is a public health priority in the Lao PDR [ 6 ]. The prevalence of stunting, an indicator often used to estimate the prevalence of chronic malnutrition, is among the highest in East Asia [ 7 ], with a national rate estimated at 31.5% in 2022 [ 8 ]. This rate surpasses those in neighboring lower-middle-income countries, such as Vietnam (20%), Cambodia (22%), and Myanmar (27%) [ 9 ]. According to the WHO standards, stunting is considered critical if it exceeds the threshold of 30% [ 5 ]. Acute malnutrition, estimated by the prevalence of wasting, is still a public health problem among children under five years of age in Lao PDR. The prevalence of wasting is 10%, which is the same as that in Cambodia but higher than that in Myanmar (7%) and Vietnam (5%) [ 9 ]. Furthermore, the problem of malnutrition is unevenly distributed across the territory of Lao PDR. Rural and ethnic minority children are at greater risk of stunting than are urban and majority ethnic groups [ 10 ]. There was a 15% lower risk of stunting for urban children than for their rural counterparts (24% vs. 39%). In Phongsaly Province, the stunting prevalence is as high as 54%, in contrast to the 14% reported in the Vientiane Capital. Additionally, the prevalence of wasting was the lowest in the province of Luangnamtha (3%) and highest in the province of Xayabury (19%) [ 11 ].
The state of healthcare system decentralization has been shown to be a determinant of nutritional status in developing countries [ 12 , 13 ]. Decentralization involves transferring power and responsibility from the central government to lower levels of governance, impacting healthcare service accessibility, quality, and equity [ 14 , 15 , 16 , 17 ]. Decentralization is commonly categorized into three major forms: 1) Deconcentration involves the central government handing over some authority to local administrative offices within the health ministry, allowing local management to handle health-related activities with some discretion; 2) Delegation entails the central government transferring defined managerial and administrative functions to institutions outside the central government's hierarchical structure, which are indirectly controlled by the health ministry; and 3) Devolution refers to the central government legally transferring power to locally elected political organs that operate independently of the central government in specific functions [ 15 ].
Lao PDR has a deconcentration form of decentralization [ 18 , 19 ]. While local levels can provide input for program adaptation to local needs, ultimate control remains with the central government, which can veto decisions made by regional or local health offices [ 20 , 21 ]. In Lao PDR, the dynamics and forces influencing the current state of decentralization are shaped by the country's unique historical-political context and distinctive population characteristics. These factors contribute to the complex nature of power sharing across different government levels. The first factor is related to the historical concept of Lao PDR, which is rooted in the notion of " meuang "[ 22 ]. A meuang is a walled city led by a local ruler overseeing surrounding settlements and villages [ 22 , 23 ]. Each meuang maintained its governance, with oversight and protection from the kingdom but without interference in internal affairs. While the nineteenth century shift toward a centralized state model introduced Western administrative practices, the meuang concept remains deeply ingrained in Lao society, lending historical legitimacy to decentralization forces [ 22 , 24 ]. The second factor is the country's ethnic diversity. The country has 49 official minority groups constituting nearly half the population. Minorities often reside in remote areas [ 25 ]. Decentralizing power and assigning responsibilities to local levels is expected to empower authorities to more effectively customize health programs to meet the diverse needs of the population.
These decentralizing forces are counterbalanced by centralizing forces due in great part to the sociocultural context influenced by Confucianist ideology, which emphasizes social harmony and respect for authority and promotes political centralization in East Asia, including Lao PDR [ 26 , 27 , 28 ]. Moreover, the limited human and financial resources of the central government, which still rely heavily on donor funding, push toward the centralization of the healthcare system and program functioning [ 29 , 30 , 31 ]. From an organizational perspective, these factors create a complex balance between decentralization and centralization in the Lao healthcare system.
Little work has been done in Lao PDR on how the state of decentralization affects the functioning of public health programs, despite being an organizational determinant of health. This organizational study examines the status of decentralization of the healthcare system in Lao PDR and its influence on the National Nutrition Policy.
Conceptual framework
The conceptual framework used in this study was based on neo-institutional theory (NIT) [ 32 , 33 ]. NITs view organizations as social structures that must conform to the expectations and pressures of their institutional environment, which includes normative and regulatory forces [ 34 , 35 ]. This approach was considered relevant for this study because decentralization is an institutionalized concept. The form of decentralization that underlies the nutrition policy in the country arises from sociohistorical and legal factors that institutionalize the distribution of powers that govern the functioning of the policy.
Different NIT conceptual frameworks have been proposed. The one used in this study is the one that was proposed by Hinings and Greenwood in 1988 [ 36 ]. It considers the dialectic between the structure, i.e., the laws, rules, and resources that constrain the work performed in an organization, and the interpretive schemes and their meaning-making processes that shape individual and collective behavior that are dominant in a society, i.e., the dominant ideas and beliefs [ 36 , 37 ]. This dialectic approach has been widely used in studies on public policies concerning the nature of institutional structures [ 38 , 39 , 40 , 41 , 42 ]. From these two dimensions, the structural dimension emphasizes the importance of formalizing corporate values and standards in the organization’s standardized policies and procedures, formalizing decision-making processes, and creating hierarchical structures to ensure compliance with institutionalized environmental factors. On the other hand, the interpretive schemes dimension focuses on the importance of shared meanings and beliefs in shaping organizational behaviors [ 32 , 43 ]. This dimension emphasizes that organizations are influenced by both individual and shared beliefs, values, and norms within their institutional environment. These elements shape the organizational actors' understanding and interpretation of what constitutes legitimate and appropriate behaviors [ 35 , 44 , 45 ]. By doing so, organizations can gain legitimacy and ensure their survival in complex and dynamic institutional environments [ 34 , 35 , 45 , 46 ].
Study design
A case study based on an ethnographic design was conducted to examine patterns of social organization and ideational systems that underlie formal/informal structures, as well as the dominant values, behaviors and beliefs of the groups involved in nutrition interventions in Lao PDR [ 47 , 48 , 49 ]. The data were collected from documents and semistructured interviews with representatives of governmental organizations, nongovernmental organizations (NGOs), and civil society organizations (CSOs) involved in nutrition programs in four provinces of Lao PDR. The nutrition programs in this study are those that align with the Lao National Nutrition Plans and Strategies; they encompass interventions and programs from the health and other sectors that are expected to positively influence nutritional indicators. The data were collected between January and June 2022.
Data collection
Interview Guide
An interview guide (see Fig. 1 ) was developed for this study based on the dimensions of the conceptual framework. This interview guide included a pretest with three members of the Lao Tropical and Public Health Institute (Lao TPHI), who has experience in nutrition research in Lao PDR. These individuals were not part of the study's participants. The participants were asked about their current state of malnutrition in Lao PDR and changes over time, as well as insights into power sharing among government levels and external actors. The questions also covered the organization’s experiences and responsibilities in the field of nutrition. Discussions have further explored perspectives on structural elements (policies, regulations, rules) and common beliefs affecting the healthcare system's ability to address nutrition issues.
Study sites
To capture the diversity of the country, the latest available national-level data on nutritional status were presented for three provinces with contrasting nutrition situations: Luangnamtha, Xayabury, and Saravan (Table 1 ). Vientiane capital was chosen because of its status as the location of the Ministry of Health (MoH) and national child nutrition-focused institutions (Maternal and Child Health Center and Nutrition Center), as well as the headquarters of development donors and civil society organizations. Luangnamtha, a northern province and one of the most economically developed in the country, has seen remarkable improvements in nutrition indicators. Xayabury, which is also in the north and adjacent to the capital, has experienced little improvement in terms of stunting and underweight rates, with an increase in wasting in recent years. Saravan, in the southern region and one of the poorest provinces of the country, has among the highest prevalence rates of all types of malnutrition, with no significant changes in recent years [ 50 , 51 ].
Source of information
Two sources of information were used for the analysis in this study: interviews with representatives of key institutions and relevant documents [ 52 ].
Representatives of key institutions
The following criteria were used to recruit participants for individual interviews. The participants had to 1) occupy a formal position in relation to nutrition within their organization; 2) be in their current position for at least one year; 3) be authorized to speak on behalf of their organization regarding projects related to nutrition in children under five years of age; and 4) be able to speak one of the languages spoken by the interviewer: Lao (official language), English, or French.
A purposeful sampling approach was used to constitute the sample [ 53 , 54 ]. A preliminary list of participants was created by one of the researchers (SK). At the end of each interview, the participants were asked to suggest additional organizations or individuals who could offer different perspectives. This snowball sampling method aimed to diversify opinions until data saturation was achieved [ 47 , 55 ].
Following administrative protocols, a project summary and discussion topics were initially sent to organization directors for approval. The latter identified individuals within their organization who might have participated in the study. These persons were contacted and asked for their permission to receive project details via fax, WhatsApp, or email. Any queries were addressed through phone calls. If the solicited person agreed, they signed a consent form. The interviews were subsequently scheduled at a mutually convenient time. The participants could choose between face-to-face or online videoconference interviews (Zoom or Google Meet). The interviews, which lasted 45 to 90 min, were audio-recorded with consent, and handwritten notes were taken for documentation and impressions.
To supplement the information provided during the interviews, all documents written in English, Lao, or French on nutrition policies and power sharing between different government levels in Lao PDR were also analyzed. These documents included published academic papers, documents provided by individuals who were interviewed, and documents found on the website of their organization.
Data analysis
All interviews conducted in Lao or French were translated into English by the interviewer and sent to the coauthor who has the least mastery of the Lao language. The realism of the translation was verified by sending a first version of the analyses to three people interviewed, who had to confirm that they found their opinions there. The interviews and document content were analyzed using NVivo 11 software. The interviews and document contents were subsequently analyzed through four main steps: 1) data coding (where data were segmented into meaningful units such as phrases, sentences, or paragraphs); 2) categorization (coded data were then grouped into themes or concepts); 3) coding of themes in connection with the conceptual framework; and 4) comparison of emerging information with published studies on the topic [ 56 ].
The analysis was performed using an inductive-deductive approach [ 57 , 58 ]. The validity of the results was ensured by four elements: 1) credibility based on the triangulation of information provided by multiple sources; 2) transferability through a detailed description of the participants, research process and study context to help the reader judge the relevance of the results for another context [ 59 , 60 ]; 3) reliability based on analyses performed independently by the researcher and one of her supervisors and the search for a consensus between them in case of discrepancy; and 4) confirmability through a detailed and transparent record of the research process, including the data collection, analysis, interpretation and discussion notes from the meetings with coresearchers [ 61 ].
Twenty-four semistructured interviews were conducted with representatives of key organizations: government institutions, United Nations (UN) agencies, international nongovernmental organizations (NGOs), and civil society organizations (CSOs). The participants were primarily women (16 out of 24). The average age was 47 years, with a range from 32 to 61 years. Three participants worked in the healthcare system at the central level, five at the provincial level, five at the district level, and three in health centers (formally known as small hospitals). Three participants worked for UN agencies, and two worked for NGOs. One was a consultant, and two were active members of civil society associations. Twenty-two interviews were conducted in the Lao language (Table 2 ).
Eleven documents were analyzed: 1) Fiscal Decentralization in the People’s Democratic Republic of Lao; 2) Decentralization in Lao PDR: A case study of the Effectiveness of Three Build Directive Policy on Local Authority; 3) the role of Marxism in the Lao political system in the contemporary era; 4) the health system review of Lao PDR in 2014; 5) the Prime Minister’s Decree No. 570 on the organizations and operations of the Ministry of Health in 2021; 6) the National Plan of Action on Nutrition (NPAN) 2021–2025; 7) the National Immunization Programme. Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023; 8) Government spending on health in Lao PDR in 2012; 9) National Nutrition Policy in 2008; 10) National Nutrition strategies to 2025 and Plan of Action 2016–2020; and 11) Operational guideline for the implementation of the National Plan of Action on Nutrition (NPAN) 2021 to 2025 [ 6 , 18 , 19 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ].
State of decentralization of the Lao healthcare system
Formally, the decentralization of the Lao health system is of the deconcentration type (Fig. 2 ). The Ministry of Health (MoH) oversees the entire healthcare system, which operates across three levels of governance: central, provincial, and district. Provincial and district health authorities’ main responsibility is to ensure that health facilities comply with centrally defined rules [ 6 , 65 ]. Private providers must adhere to centrally defined regulations [ 6 ].
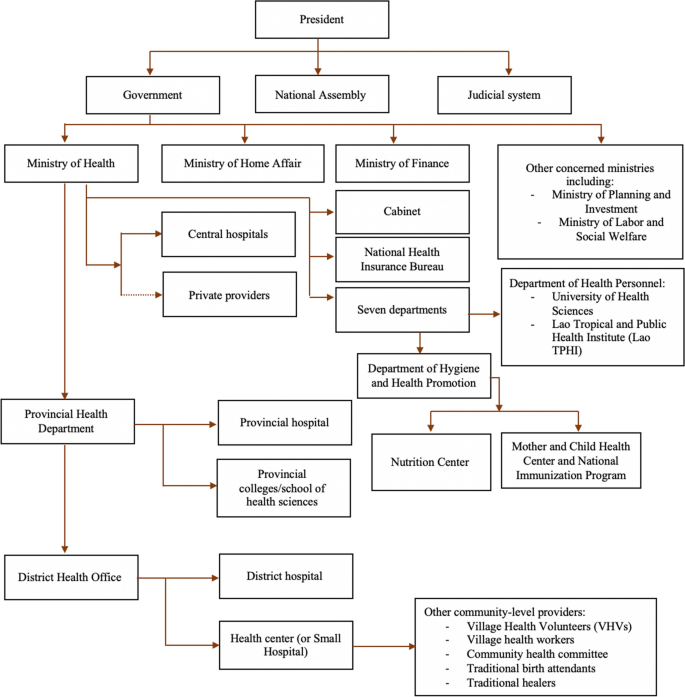
Government-level power sharing in Lao PDR. Sources: Health System Review in Lao 2014; National Plan of Action on Nutrition (NPAN) 2021–2025; National Immunization Programme: Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023; and the Prime Minister’s Decree No. 570 on the organizations and operations of the Ministry of Health in 2021 [ 6 , 63 , 64 , 68 ]
All decisions concerning human and financial resources in the health care sector must be routed through the central level, represented by the MoH and other ministries, notably the Ministry of Finance (MoF), which is responsible for overall fiscal policy and sectoral allocations of the annual recurrent budget. Other ministries are also involved. The Ministry of Planning and Investment (MPI) oversees capital budget allocation, whereas the Ministry of Home Affairs (MHA) manages the total number of civil servants and sectoral allocations of human resource quotas, including the annual recruitment of health personnel at all administrative levels [ 6 , 65 ].
Most respondents (19/24) highlighted the fact that in practice, the power dynamics between levels of governance are complex because constitutional power-sharing arrangements are also under political influence. Official documents support this assertion when they emphasize that in the Lao PDR, the Lao People's Revolutionary Party (LPRP) is the body that has the constitutional mandate to exercise leadership across all levels of government [ 18 , 62 ].
Power sharing between government levels and nutrition programs in Lao PDR
The Lao MoH has the ultimate responsibility for uni- and multisectoral nutrition programs. While the Provincial Health Department (PHD) and District Health Office (DHO) are responsible for implementing and ensuring the functionality of services, the central government retains control over which interventions to offer and over the allocation of human, financial, and material resources [ 66 , 69 ] (Table 3 ).
At the central level, operational leadership in the field of nutrition is formally led by the Multisectoral National Nutrition Committee (MSNNC), which comprises the Ministry of Health, Ministry of Planning and Investment, Ministry of Agriculture and Forestry, Ministry of Education and Sports, and other ministries and mass organizations. The MSNNC defines priorities, assesses local needs, and oversees the implementation of centrally sanctioned interventions at local levels (Table 3 ). Although the responsibility for the MSNNC falls under the MoH, the MSNNC is chaired by the Deputy Prime Minister and deputy chaired by the Deputy Minister of Health. Its members consist of deputy ministers of eight ministries and the vice-director or the secretary of the LPRP’s mass organizations. The MSNNC serves as the central committee overseeing the hierarchical structure of other nutrition committees at the provincial, district, and village levels. The MSNNC structure has been conceived with the idea of having leadership able to promote intersectionality of nutrition interventions [ 6 , 63 , 64 , 66 ].
Yet, under the authority of the Politburo of the LPRP, the Lao national government holds supreme authority, whereas provincial governments possess financial responsibilities and managerial duties. Provincial administration is directly supervised by the central government under the principle of democratic centralism [ 18 , 19 ].
Structure and interpretive schemes underlying the decentralization state of nutrition programs in the Lao PDR
Seven factors related to the structure and interpretative schemes that influence the effectiveness of nutrition programs emerged from the analysis of interviews and documents (Fig. 3 ).
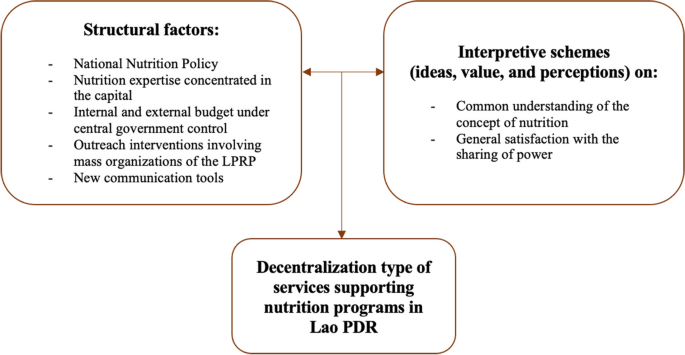
Factors associated with the decentralization type of nutrition programs in Lao PDR
Structural factors
Five main structural factors emerge from the data underlying the decentralization state of nutrition programs in Lao PDR: 1) the existence of a public policy; 2) the availability of human resources; 3) the source of funding; 4) the key role of mass organizations; and 5) communication tools.
A national nutrition public policy
Interventions on malnutrition in Lao PDR are primarily based on a public policy, the National Nutrition Policy (NNP), which was enacted in 2008. This policy provides the legal framework for mobilizing and coordinating actors that can contribute to improving nutrition indicators, regardless of their sector. The policy is operationalized through formal strategic plans developed by the MoH. These official documents define the responsibilities of agencies addressing malnutrition among the different levels of government in the country [ 63 , 66 , 69 ]. All participants agreed that a public policy on nutrition is essential for ensuring intersectoral collaboration at various levels of governance. The policy is seen as a structural foundation that, while centralizing, guarantees the ability of the concerned players to act.
Human resources
The second structuring element that emerges from the data is the fact emphasized by almost all respondents (21/24) and all documents dealing with nutrition [ 6 , 63 , 66 ] that the shortage of expertise outside the capital limits local governments from taking charge of nutrition programs more independently. The respondents also highlighted the fact that a shortage of human resources is compounded by a high turnover rate at all local levels. Turnover weakens the capacity to coordinate the numerous actors involved. Moreover, it drains a considerable part of the local budget, as it leads to continual staff training for nutrition interventions. In brief, all the participants recognized that the state of human resources made it difficult to imagine a program to combat malnutrition run by local authorities.
The health system, from the central to the village levels, is funded from three main sources: a budget allocated by the Ministry of Finance, direct payments at health facilities from users of health services, and funding from external donors, such as NGOs. Funds allocated by the central government are sent to provincial authorities, who then allocate these funds to districts according to planned budgets. These funds are designed for civil servants’ salaries as defined by the central government, as well as for the equipment needs of health establishments. Most of the money paid by service users can be kept by the hospital and used for recurrent costs, including staff wages, allowances, maintenance, utilities, and supplies. The rest (approximately 20%) should be handed over to the provincial or district finance department. Money provided by external donors for projects deployed in provinces and districts must be approved at the central level. One consequence of having multiple sources of financing nutrition activities is the variability in available funds for health services among districts and provinces [ 6 , 18 , 65 ].
The annual budget planning for nutrition interventions involves consultations and reports sent from the district to the provincial levels. The MoH then finalizes and submits it for approval by the National Assembly. In other words, nutrition programs are mainly under central government management. The majority of local-level participants (9/13) feel that this system is not optimal, the main reason being the uncertainty regarding the availability of financial resources over time. These respondents also deplore frequent delays in budget transfers, particularly transfers to remote areas. Above all, nearly all participants at the district and health center levels (6/8) mentioned that nutrition-targeted budgets are often merged with funds intended for non-nutrition public health interventions, as indicated in the following quotation.
“ There’s no other source of money. For the education or agriculture sector, the money would go to each sector separately. For these sectors, they have their own money for nutrition, but we don’t have. So, we need to depend on the integrated work. … Mainly, when we request to the central level, they said they don’t have money for our province anymore; there is only our provincial health office and their help that includes the budget, like they would include the nutrition on the integrated work, and then they manage the staff for it. The structure that divides clearly, it’s not always suitable in real situations ” said by the participant from the provincial level (P11)
The irregular flow of funds is partially offset by the availability of external funding, such as from NGOs [ 63 , 66 ]. However, activities funded by external entities require preapproval from the central government.
The fact that no respondent was able to propose solutions to the problem of funding uncertainty suggests that current funding mechanisms contribute significantly to the solidity of the structure underpinning the decentralization of nutrition programs and hence to the stability of the decentralization type that underlies nutrition programs.
LPRP’s mass organizations
In Lao PDR, the LPRP’s mass organizations, particularly Lao Women’s Union (LWU), are unavoidable collaborators in nearly all programs implemented at the population and community levels that aim to reduce the prevalence of malnutrition. Even if these organizations do not necessarily have expertise in health education which is one of their main contributions, there is a consensus among participants that they have proven to be a valuable substitute for the shortage of professionals in the field. This is expressed in the following quotation:
“…there are the LPRP grassroot members in the meeting (nutrition committee meeting at the district level), who we invited to join us, as well as the standing and district LPRP committee who divides the responsibility for guiding each population group, whoever is responsible for our target group, we would take them to the field, as well as the mass organization, especially the Lao Front for National Development as a main actor to discuss this, second is the Women Union that we can’t forget them, we would take them going to the field with us.” said by the participant from the district level (P17)
This general feeling is also recorded in several official documents [ 6 , 62 , 66 ].
In short, the constant presence of mass organizations whose primary function, in addition to contributing to health education programs, is to increase LPRP values in the population reinforces the power of the central level in nutrition programs deployed in communities.
Communication tools
All the participants underscore the pivotal role of social networks, such as Facebook and WhatsApp, in expediting decision-making processes that previously relied on formal communication channels and informal social gatherings. According to the participants, social media has increased the capacity of nutrition programs to reach their objectives by enabling professionals involved in nutrition programs everywhere to be easily reached and to ask questions without navigating through time consuming and poorly effective bureaucratic procedures. The participants also highlighted that these new technologies inject a sense of dynamism through the competition they foster among teams. This sentiment is captured in the following quotation:
“In the groups, there are staff (DHO staff) and department level (PHD staff) together... If the department (PHD staff) is not in the group, they will send the responsible staff to join the group. So, we always exchange (information) with each other. Whenever the central level (staff) sends messages in the group, everyone always responds. They couldn’t act like they haven’t seen it (messages) because we have the responsibilities for our work, and they also have their responsibilities. If they don’t answer, it means that they haven’t followed up (on the work)” said by the participant from the central level (P01)
There is a consensus that new communication tools have reshaped the power dynamics between central and local levels of governance in Lao PDR. They allow overpassing the traditional hierarchical structure of the healthcare system that is supported by communication channels such as those based on the exchange of information by paper (including faxes). This trend empowers lower levels to directly engage with higher-level actors at the central level, fostering a possible emerging capacity for a more decentralized dynamic inside the field of nutrition programs.
Interpretive schemes
Two main interpretive factors emerged from the data underlying the decentralization state of nutrition programs in Lao PDR: 1) the understanding of the causes and consequences of malnutrition; and 2) the perception of the roles of different levels of government in implementing malnutrition interventions.
Understanding the causes and consequences of malnutrition
The participants across different levels of governance in Lao PDR share a common understanding of the causes and challenges of malnutrition. All the participants recognized that malnutrition is a multifaceted issue requiring attention on both the demand and supply sides. They emphasized the fact that in a resource-limited country such as Lao PDR, factors such as a lack of human and financial resources, combined with contextual challenges in vulnerable communities such as poverty, cultural barriers, and food insecurity must all be considered. Additionally, there is a consensus among participants that addressing malnutrition necessitates multisectoral programs, as programs limited to calories and micronutrients may have a limited impact on improving the condition of malnourished children. Numerous other issues, such as water, sanitation, and hygiene (WASH), gender, and the educational levels of parents, have been found to be key determinants of nutrition. They require significant collaboration from different sectors and stakeholders. In short, there is a broad consensus among stakeholders on interpretive schemes.
Perception of the capacity of the different levels of governance to assume nutrition responsibilities
The majority of participants across various levels of government (10/16) spontaneously declared that interventions to address malnutrition should be led by the central government, citing the fact that the government has expertise and control over the human, financial and material resources necessary for the programs. It is also recognized that district-level health workers, particularly in remote regions, may lack sufficient training and resources. The remaining six participants did not express an opinion on this matter. Although half of the participants at the local level mentioned that regions are increasingly populated by well-trained healthcare professionals, they believe that this trend cannot have a significant impact on the power sharing arrangements for nutrition programs due to the shortage of human resources, especially in remote regions and because local health volunteers and mass organizations largely compensate for human resource needs.
Therefore, there is no question among participants regarding the state of decentralization of services that underpin nutrition programs in the country.
Dialectic between structure and interpretive schemes
In brief, there is coherence between the structure and interpretive schemes that underlie the sharing of responsibilities across governance levels in nutrition programs and interventions in Lao PDR. This coherence is reinforced by the respondents' belief that the desired effects of socioeconomic changes, such as an increase in the number of well-trained nutrition professionals and the use of communication tools empowering regional health workers, cannot sufficiently alleviate human resource needs in the provinces. The system of division of responsibilities between governance levels that has lasted for approximately fifty years is therefore likely to be stable. It is likely to remain so for the foreseeable future.
In Lao PDR, powerful forces are pushing the Lao healthcare system toward more centralization than decentralization, despite factors that support greater autonomy for local authorities.
Every organization concerned with nutrition programs seems to be satisfied with this situation and perceives it as a determinant of the effectiveness of nutrition programs. None of the respondents suggested an alternative approach, despite acknowledging that socioeconomic changes are endowing regions with the capacity to manage public health programs that were previously unimaginable. Therefore, there is convergence of interpretive schemes among concerned actors, as well as coherence between structure and interpretive schemes. This convergence signifies a shared vision of nutrition challenges in the country and the capacity to address them, regardless of organizational concerns or hierarchical levels of governance. The coherence between structure and interpretive schemes reveals a general feeling that the current distribution power among governance levels is the most appropriate way to meet the nutritional needs of the population.
From an organizational perspective seen through a neoinstitutional lens [ 70 ], the main consequence is that the distribution of responsibilities in nutrition services among different government levels has remained stable since the event of the Lao PDR in 1975.
The findings of this study highlight how a country's sociopolitical context influences the state of decentralization and the functioning of its public health programs. In the case of immunization programs in Lao PDR, three notable factors impact their implementation: the Lao sociopolitical background, the availability of resources, and the use of new technologies such as WhatsApp by health professionals. These elements have reshaped the dynamics of the deconcentrated healthcare system and its program operation [ 31 ].
Theoretically, a centralized healthcare system should lead to more standardized public health programs and health services across the country if it ensures consistent application, quality of care, and equitable distribution of resources [ 71 , 72 , 73 ]. However, given the diverse contexts among provinces, a one-size-fits-all approach may not be optimal, especially for complex and multisectoral interventions like nutrition programs. These programs often require adaptation to the specific needs and capacities of local contexts and populations in different communities to be truly effective [ 74 , 75 ].
In a diverse country like Lao PDR, public health interventions require adaptation and more flexible interventions and activities to meet the varied needs of different communities. Empowering local authorities, who are more familiar with local contexts and issues, could improve the management of activities and resources, leading to better interventions that address the specific needs of their populations. In other single-party countries, decentralization has been shown to effectively strengthen public health programs and enhance their effectiveness [ 76 , 77 ].
The documents and interview findings from this study indicate that the formal structure of the healthcare system in Lao PDR is well defined. The organizational structures of the NNP identify the roles and responsibilities of stakeholders from the central level of the MoH to the implementation level of the village. However, in practice, the implemented programs aimed at reducing the prevalence of malnutrition in children under age 5 in the country are far more challenging than the formal structure suggests [ 78 ]. Addressing nutrition outcomes requires a long-term and multifaceted approach, particularly when contributions among actors and power-sharing roles involve local governments working with multiple stakeholders at all levels.
Indeed, Lao PDR faces challenges in reversing the conditions that would allow local governments to put more of their own initiatives into nutrition programs. Unlike in neighboring countries like Vietnam or Thailand, in Lao PDR, the only training on nutrition is a course integrated into a public health master’s program. Additionally, Lao PDR, a country as large as the United Kingdom with a population of 7.7 million inhabitants, is a sparsely populated country. Fifteen of its eighteen provinces have fewer than 500,000 inhabitants. Only one has more than a million [ 79 ]. A small population reduces the likelihood of building a critical mass of people from a given province with expertise in nutrition. Although constraints on qualified human resources are common in many low-resource countries [ 80 , 81 ], these constraints, coupled with the population context in Lao PDR, obviously significantly contribute to the centralization of the Lao healthcare system. In fact, this need for expertise is not limited to nutrition. Optimizing interventions to reduce the prevalence of malnutrition in children under 5 years of age requires tailored approaches that consider the diverse cultural and regional contexts of the population and address multisectoral programs and interventions including food security, water, sanitation, hygiene, maternal education, and social protection. The complexity of these interventions requires multidisciplinary teams [ 63 , 67 , 82 ]. Poorly populated provinces might not be able to gather all this desired expertise. Finally, Lao PDR receives funding for its nutrition program from several external donors and NGOs. This necessitates central-level coordination that might be even more crucial once the country has left, supposedly in 2026, the group of the least developed countries [ 83 ]. Leaving this group will have consequences for the support provided by external actors. Expectations are that the central government will assume more responsibilities for its nutrition programs in the near future.
Finally, advancements in communication technologies and the arrival of better-trained human resources offer hope for addressing the shortage of quality human resources that hinder local authorities' leadership in nutrition programs. An increasing number of graduated individuals living in the provinces are proficient in the use of new technologies [ 84 ]. This increased utilization of technology is anticipated to further transform traditional barriers that govern interactions among stakeholders. Additionally, interpretive patterns are likely to evolve as professionals in provinces become better informed and more willing to customize nutrition programs to meet the specific needs of local populations. However, owing resource shortages and uneven population distribution in Lao PDR, there are unequal opportunities for local levels to assume more responsibility for nutrition interventions, with little to no chance for decision-making at the local level. This is expected to limit the capacity of sub-national levels from contributing more substantially to nutrition programs than they currently do.
None of the respondents evoked a future where nutrition programs would be more decentralized. Nevertheless, they acknowledged that the current state of decentralization is suboptimal. They recognized that one of the undesirable effects of centralization is the difficulty in adapting services to the specific needs of diverse populations.
Limitations
This study has several limitations. First, respondents were selected by their organization directors following administrative procedures mandated by research projects in Lao PDR. While this method has likely allowed to capture a diverse range of perspectives on malnutrition, it may have excluded individuals who disagreed with the official discourse. Although the two coders felt that additional interviews would not yield new information, it is possible that additional insights might have been generated by more interviews if soliciting directly potential participants directly could have been done.
Second, as is common in qualitative studies, unconscious subjectivity and bias among researchers may have influenced some interpretations. However, the risk is mitigated by ensuring the validity of four elements of the results, particularly through the triangulation of information from interviews and document reviews, as well as through independent analyses conducted by two researchers.
Finally, the generalizability of the results may be limited. The Lao context is unique, and nutrition programs have specificities that may differ from those of other national health programs functioning in the country. Consequently, the findings of this study may not be directly applicable to other programs or countries, including those with single-party governance structures.
Decentralization of the Lao healthcare system is of the deconcentrated type, i.e. a system largely under the responsibility of the central government. The transformations taking place in the healthcare system, notably with the use of new information technologies, are changing relationships between individuals across different levels of government and the fact that the provinces are populated by a growing number of professionals trained in nutrition. These factors could lead people to believe that the system would give more responsibility to provincial governments to improve their malnutrition status at local levels. However, the data show that these changes are probably not yet strong enough to change a structure that has endured for approximately fifty years. The deconcentration that characterizes decentralization is therefore likely to continue for the foreseeable future.
Availability of data and materials
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Civil society organizations
District health offices
Lao People’s Democratic Republic
Lao People's Revolutionary Party
Lao Women's Union
Ministry of Home Affairs
Multi-sectorial National Nutrition Committee
Ministry of finance
Ministry of health
Ministry of planning and investment
Nongovernmental organizations
National Nutrition Policy
National Nutrition Strategy and Plan of Action
National Plan of Action on Nutrition
- Neo-institutional Theory
Provincial health departments
United Nations
Village health volunteers
World Health Organization
World Health Organization. Malnutrition 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition .
Caulfield LE, Richard SA, Rivera JA, Musgrove P, Black RE. Stunting, wasting, and micronutrient deficiency disorders. In: Disease Control Priorities in Developing Countries 2nd edition. The International Bank for Reconstruction and Development / The World Bank. New York: Oxford University Press; 2006.
Google Scholar
Muller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005;173(3):279–86.
Article PubMed PubMed Central Google Scholar
UNICEF. Child Malnutrition 2023. Available from: https://data.unicef.org/topic/nutrition/malnutrition/ .
World Health Organization, United Nations Children's Fund (UNICEF) & World Bank. Levels and trends in child malnutrition: UNICEF / WHO / The World Bank Group joint child malnutrition estimates: key findings of the 2021 edition. World Health Organization. 2021. https://iris.who.int/handle/10665/341135 .
World Health Organization. The Lao People’s Democratic Republic: Health System Review. Asia Pacific Observatory on Health Systems and Policies; 2014. Contract No.: 1.
World Bank. Lao PDR: New Financing to Improve Access to Health and Nutrition Services. 2020.
Save the Children, CARE, EU, CCL, ChildFund. Partnership for Improved Nutrition in Lao PDR Pillar 3: Sustainable Change Achieved through Linking Improved Nutrition and Governance. Vientiane: Lao Social Research; 2022.
UNICEF/WHO/World Bank Joint Child Malnutrition Estimates Expanded Database. Malnutrition data 2023. Available from: https://data.unicef.org/resources/dataset/malnutrition-data/ .
Ministry of Health, World Health Organization. Overview of Lao health system development 2009–2017. Manila, Philippines: World Health Organization Regional Office for the Western Pacific; 2018. Report No.: Licence: CC BY-NC-SA 3.0 IGO.
UNICEF/WHO/World Bank Joint Child Malnutrition Estimates Expanded Database. Malnutrition data 2022. Available from: https://data.unicef.org/resources/dataset/malnutrition-data/ .
Constantinides SV. Determinants of Nutrition Agenda Setting in the Context of the Double Burden of Malnutrition in Tamil Nadu, India. South Carolina: University of South Carolina; 2020.
Acosta AM, Fanzo J. Sussex: Institute of Development Studies; 2012.
Boko SH. Decentralization_Definitions, theories and debates. Decentralization and Reform in Africa. Boston: Sringer; 2002. p. 1–10.
Book Google Scholar
Frumence G, Nyamhanga T, Mwangu M, Hurtig AK. Challenges to the implementation of health sector decentralization in Tanzania: experiences from Kongwa district council. Glob Health Action. 2013;6:20983.
Article PubMed Google Scholar
Mosca I. Decentralization as a determinant of health care expenditure: empirical analysis for OECD countries. Appl Econ Lett. 2007;14(7):511–5.
Article Google Scholar
Saltman RB, Bankauskaite V, Vrangbaek K. Decentralization in Health Care. Maidenhead: Mcgraw-Hill House; 2007.
Martinez-Vazquez J, Gomez JL, Yao G. Fiscal Decentralization in the People’s Democratic Republic of Lao. Georgia, United States: Georgia State University; 2006. Contract No.: Working Paper 06–22.
Luangrath S. Decentralization in Lao PDR: A Case Study of the Effectiveness of Three Build Directive Policy on Local Authority. Seoul, Korea: Seoul National University; 2019.
Litvack J, Seddon J. Decentralization briefly notes. Washington, DC: World Bank Institute; 1999.
Hutchinson PL, LaFond AK. Monitoring and Evaluation of Decentralization Reforms in Developing Country Health Sectors. Maryland, United States: Abt Associates Inc.; 2004.
Stuart-Fox M. Politics and Reform in the Lao People’s Democratic Republic. Working Paper No. 126, Asia Research Center, Murdoch, University. 2005.
Pholsena V, Banomyong R. Laos: From buffer state to crossroads? Chiang Mai, Thailand: Mekong Press; 2006.
Stuart-Fox M. Political Culture and Power in the Lao People’s Democratic Republic. J Asiatic Stud. 2009;138:222–54.
United Nations in Lao PDR. Country Analysis Report: Lao PDR: Analysis to inform the Lao People’s Democratic Republic-United Nations Partnership Framework (2017–2021). Vientiane: United Nations; 2015.
Nawrot KA. Does Confucianism promote cooperation and integration in East Asia? Int Commun Chin Culture. 2020;7(1):1–30.
Jiang Y-H. Confucian political theory in contemporary China. Annu Rev Polit Sci. 2018;21:155–73.
Kim Y, Lee H-K, Park S. The Confucian Tradition and Politics. Oxford Research Encyclopedia of Politics. 2019.
Dickovick JT. Foreign aid and decentralization: Policies for autonomy and programming for responsiveness. Helsinki: The United Nations University World Institute for Development Economics Research (UNU-WIDER); 2013.
Dickovick JT. Foreign aid and decentralization: limitations on impact in autonomy and responsiveness. Public Admin Dev. 2014;34(3):194–206.
Viphonephom P, Kounnavong S, Reinharz D. Decentralization and immunization program in a single-party state: the case of the Lao People’s Democratic Republic. Trop Med Health. 2024;52(1):35.
Meyer JW, Rowan B. Institutionalized organizations: formal structure as myth and ceremony. Am J Sociol. 1977;83(2):340–63.
DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev. 1983;48(2):147–60.
Marschlich S. Conceptual Framework: Sociological Neo-Institutionalism, Legitimacy, and Public Relations. Corporate Diplomacy: How Multinational Corporations Gain Organizational Legitimacy: A Neo-Institutional Public Relations Perspective. Amsterdam: University of Amsterdam; 2022.
Swaminathan A, Wade JB. Institutional Environment. The Palgrave Encyclopedia of Strategic Management. London: Palgrave Macmillan; 2016. p. 1–7.
Hinings CR, Royston G. The Dynamics of Strategic Change. Oxford: Basil Blackwell Ltd.; 1988.
Hinings CR, Greenwood R, Reay T, Suddaby R. Dynamics of change in Organizational field. Handbook of Organizational Change and Innovation: Oxford University Press; 2003.
Harimanana A, Barennes H, Reinharz D. Organizational analysis of maternal mortality reduction programs in Madagascar. Int J Health Plann Manage. 2011;26(3):e186–96.
Peyrot M. Institutional and organizational dynamics in community-based drug abuse treatment. Soc Probl. 1991;38(1):20–33.
Morrill C, Yalda C, Adelman M, Musheno M, Bejarano C. Telling tales in school- youth culture and conflict narratives. Law Soc Rev. 2000;34(3):521–65.
Addicott R, Furlie E. Sedimented archetype change in public sector organisations: the example of managed clinical networks for cancer. CQUniversity. Conference contribution. 2006. https://hdl.handle.net/10018/8418 .
Breunig KJ, Skjølsvik T. The virtual future of professional service firms: Identifying emerging interpretive schemes caused by technology enactment. Acad Manag Proc. 2016. https://hdl.handle.net/10642/4407 .
Greenwood R, Hinings CR. Understanding radical organizational change: Bringing together the old and the new institutionalism. Acad Manag Rev. 1996;21(4):1022–54.
Senge K. The ‘New Institutionalism’ in organization theory: Bringing society and culture back in. Am Sociol. 2013;44(1):76–95.
Scott WR. Institutions and organizations : ideas, interests and identities. 4th ed. Thousand Oaks: SAGE Publications, Inc.; 2013.
Rouleau L. Théories des organisations : Approches calssiques, contemporaines et de l’avant-garde. Quebec, Canada: Presse de Université du Québec; 2007.
Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. London, United Kingdom: SAGE Publications Inc; 2013.
Huby G, Hart E, McKevitt C, Sobo E. Addressing the complexity of health care: The practical potential of ethnography. J Health Serv Res Policy. 2007;12(4):193–4.
Kielmann K. The ethnographic lens. In: Gilson L, editor. Health policy and systems research: A methodology reader. Geneva, Switzerland: World Health Organization; 2012. p. 235–52.
Lao Statistic Bureau. Lao PDR: Lao Social Indicator Survey 2011–2012 (Multiple Indicator Cluster Survey/Demographic and Health Survey). Vientiane: Lao Statistic Bureau and UNICEF; 2012.
Lao Statistic Bureau. Lao Social Indicator Survey II 2017. Vientiane: Lao Statistic Bureau and UNICEF; 2018.
Pope C. Qualitative Research in Health Care. Hoboken: Wiley-Blackwell; 2020. p. 2020.
Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Los Angeles: Sage Publications; 2011.
Palinkas AP, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42(5):533–44.
Naderifar M, Goli H, Ghaljaie F. Snowball sampling: a purposeful method of sampling in qualitative research. Strides Dev Med Educ. 2017;14(3):1–4.
Fortin M-F, Gagnon J. Fondements et étapes du processus de recherche: Méthodes quantitatives et qualitatives. 3rd ed. Montreal: Chenelière éducation; 2016.
Park D, Bahrudin FI, Han J. Circular reasoning for the evolution of research through a strategic construction of research methodologies. Int J Quant Qual Res Methods. 2020;8(3):1–23.
CAS Google Scholar
Proudfoot K. Inductive/Deductive Hybrid Thematic Analysis in Mixed Methods Research. J Mixed Methods Res. 2022;0(0):1–19.
Ponterotto JG. Brief note on the origins, evolution, and meaning of the qualitative research concept “Thick Description.” Qual Rep. 2006;11(3):538–49.
Kharel D. VIsual enthnography, thick description and cultural representation. Dhaulagiri J Sociol Anthropol. 2015;9:147–60.
Korstjens I, Moser A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–4.
Dahuai Y, Phoutthaphone S, Jing W. The role of Marxism in the Lao political system in the contemporary era. Int J Soc Sci Human Invent. 2017;4(12):4216–26.
Ministry of Health. National Plan of Action on Nutrition (NPAN) 2021–2025. Vientiane: Ministry of Health; 2021.
Lao PDR National Immunization Programme. Updated Comprehensive Multi-Year Plan Lao PDR 2019–2023. Vientiane: Ministry of Health, GAVI, UNICEF/WHO; 2018.
World Bank. Government spending on health in Lao PDR: Evidence and issues. Vientiane: World Bank; 2012.
Ministry of Health. National Nutrition strategies to 2025 and Plan of Action 2016–2020. Vientiane: Ministry of Health; 2015.
Secretariat National Nutrition Committee. Operational guideline for the implementation of the National Plan of Action on Nutrition (NPAN) 2021 to 2025. Vientiane: National Nutrition Committee Secretariat; 2023.
Bureau PM. Prime Minister’s Decree No. 570 on the organization and activities of the Ministry of Health. Vientiane; 2021.
Ministry of Health. National Nutrition Policy. Vientiane: Ministry of Health; 2008.
Greenwood R, Hinings CRB. Radical organizational change. SAGE Publications Ltd. 2006.
Ostermann M, Vincent J-L. How much centralization of critical care services in the era of telemedicine? Crit Care. 2019;23(1):423.
Kobayashi D, Otsubo T, Imanaka Y. The effect of centralization of health care services on travel time and its equality. Health Policy. 2015;119(3):298–306.
Elson S. Regionalization of health care from a political and structural perspective. Healthc Manage Forum. 2009;22(1):6–11. https://doi.org/10.1016/S0840-4704(10)60279-7 .
Sanders D, Chopra M. Implementing comprehensive and decentralised health systems: the quest for integrated care in post-apartheid South Africa. Int J Integr Care. 2001;1:e33.
Kesale AM, Mahonge C, Muhanga M. Effects of decentralization on the functionality of health facility governing committees in lower and middle-income countries: a systematic literature review. Glob Health Action. 2022;15(1):2074662.
Zhu J, Ge Z, Xia J, Liu Q, Ran Q, Yang Y. Status quo and problem analysis of cervical cancer screening program in China: Based on RE-AIM framework. Front Public Health. 2022;10:987787. https://doi.org/10.3389/fpubh.2022.987787 .
Huang X, Yang B, Liu Q, Zhang R, Tang S, Story M. Improving maternal and child nutrition in China: an analysis of nutrition policies and programs initiated during the 2000–2015 Millennium Development Goals era and implications for achieving the Sustainable Development Goals. J Health Popul Nutr. 2020;39(1):12.
Sengchaleun V, Samri MA, Kounnavong S, Reinharz D. Advocacy Coalition by External Actors and Strategies Used to Influence the Emergence of the National Nutrition Policy in Lao PDR. Health. 2021;13(08):812–29.
World Health Organization. World Health Organization Data 2020. Available from: https://data.who.int/countries .
Delisle H, Shrimpton R, Blaney S, Du Plessis L, Atwood S, Sanders D, et al. Capacity-building for a strong public health nutrition workforce in low-resource countries. Bull World Health Organanization. 2017;95(5):385–8.
Diasso D, Doudou MH, Levrak MC, Sedutto HD, Savadogo A. Municipalities’ organisational capacity to support the implementation of the Multi-Sector Nutrition Plan in Burkina Faso. Glob Health Action. 2021;14(1):1979279.
European Union, UNICEF. Review of costing of the National Plan of Action for Nutrition 2016–2020. Vientiane: European Union and UNICEF; 2020.
Ministry of Foreign Affairs. Lao PDR is recommended to graduate in 2026 from the Least Developed Country Category with an extended preparatory period. Vientiane, Lao PDR: Ministry of Foreign Affairs 2021. Available from: http://www.mofa.gov.la/index.php/activities/state-leaders/3999-lao-pdr-is-recommended-to-graduate-in-2026-from-the-least-developed-country-category-with-an-extended-preparatory-period .
World Bank. Positioning The Lao PDR for a Digital Future. Vientiane: World Bank; 2021.
Download references
Acknowledgements
We would like to express our sincere thanks to all the participants who generously shared their valuable experiences with us. We would also like to express our thanks to the organizations that assisted us in participant recruitment. The first author P.V. extends her special thanks to the Canadian Francophonie Scholarship Program (CFSP) for their support during her doctoral studies.
This research was supported by the Canadian Francophonie Scholarship Program, under the Canadian Bureau for International Education, Government of Canada.
Author information
Authors and affiliations.
Department of Social and Preventive Medicine, Laval University, Quebec City, QC, Canada
Phonevilay Viphonephom & Daniel Reinharz
Lao Tropical and Public Health Institute (Lao TPHI, Ministry of Health, Vientiane, Lao PDR
Sengchanh Kounnavong
You can also search for this author in PubMed Google Scholar
Contributions
PV: conceptualization and design; acquisition of data; analysis and interpretation of data; writing original draft; and writing review and editing of the manuscript. SK: recruitment of participants; writing review and editing the manuscript; and supervision. DR: conceptualization and design; analysis and interpretation of data; writing review and editing of the manuscript and supervision. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Phonevilay Viphonephom .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. Written consent was obtained from all participants before data collection. Ethical approval for the study was obtained from the Research Ethics Board of Laval University, Quebec, Canada (number “2021–259/23–09-2021”) and the National Ethics Committee for Health Research, Ministry of Health, Vientiane, Lao PDR (number “08/NECHR”, 14/01/2022).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Viphonephom, P., Kounnavong, S. & Reinharz, D. The state of decentralization of the healthcare system and nutrition programs in the Lao People’s Democratic Republic: an organizational study. BMC Health Serv Res 24 , 1037 (2024). https://doi.org/10.1186/s12913-024-11513-y
Download citation
Received : 04 October 2023
Accepted : 29 August 2024
Published : 06 September 2024
DOI : https://doi.org/10.1186/s12913-024-11513-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decentralization
- Single-party state
- Lower-middle income country
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Margaret Janse van RensburgMaria PeddleKaren SewellClaire McMenemyHeather MacDonald. VAW services rely on workers who understand the dynamics of violence against women and have the capacity to witness/hold the emotional experiences of survivors. The Journal of Human Services (JHS) is the official journal of the National Organization for Human ...
In our view, outmoded human service organizations are in serious need of innovation to promote psychological and physical wellness, prevention of social problems, empowerment, and social justice. This project aims to develop and evaluate value-based organizational processes and outcomes designed to transform human services.
Pioneering human services organizations are working with hospitals, insurers, and government agencies to provide integrated whole-person care. While initially accelerated by the Affordable Care Act, the shift from "volume-based" to "value-based" care varies greatly according to state and local policies and leadership, waivers and pilot programs, and the unique needs of communities.
Introduction Case management is a service delivery approach in which staff meet with clients to provide direct, personalized one-on-one support to improve a comprehensive set of outcomes related to employment, education, housing, health, and public benefit receipt. This Evidence Snapshot summarizes what rigorous research tells us about 21 interventions that used case management as their ...
The brief provides specific examples of how these action-oriented considerations are being implemented by four different organizations currently doing this work. Case Studies - Below are a series of case studies about human services programs that are helping participants build and use social capital in diverse ways. They cover a range of ...
Human service organizations are reconfiguring to address diversifying populations and widening inequality. However, institutional change is challenging to implement and fund; resource scarcity and stakeholder buy-in are barriers. In this case study, we analyze a funding-driven, state-initiated program that supports mental health professionals who are people of color in order to decrease health ...
The final case study focuses on the Massachusetts Accountable Care Organization (ACO) and Community Partner model that requires all new Medicaid ACO's in the state to work with designated behavioral health and long-term services and supports providers for community-based care coordination.
This case study describes the development of an innovative case management team model consisting of functional specialists. Ten years of comparative data demonstrate client satisfaction, a significant reduction of health and safety concerns, and a transformation to a more effective and efficient model of case management.
Evaluated an organizational development initiative in the form of a competency-based supervisory training program evaluated in 2 group homes for individuals with mental retardation. Four supervisors (aged 23-43 yrs) received 5 hours of training to use selected performance antecedents (e.g., praise, feedback) and consequences (e.g. modeling) while they taught client-teaching skills to 4 ...
Request PDF | Blending ameliorative and transformative approaches in human service organizations: A case study | This paper describes the challenges and benefits of an action-research project with ...
The study identified the following challenges which charity organizations in Oman face in varying degrees: administrative planning, organization, staffing, supervision, records and reporting ...
Abstract. In response to a number of pressures, local human service organizations have been forced to develop greater capacity to evaluate their own programs. This case study reports the efforts of a state-funded evaluation support unit in Rhode Island to increase evaluation capacity in 13 community-based organizations by means of a needs ...
A Case Study in a Human Service Organization Richard K. Fleming Department of Psychology, Auburn University, Auburn, AL, 36849-5214, USA Julianne R. Oliver Department of Psychology, Auburn University, Auburn, AL, 36849-5214, USA
The crux of this convergence between IS and IDS, however, is in helping human service agencies deliver the best possible services and outcomes for the communities they serve. As the Housing First Charlotte-Mecklenburg case suggests, IS and IDS can be leveraged in tandem to enhance evidence-based policymaking in human service agencies.
Many human service organizations that had historically received public subsidies through long-term relationships with local government were suddenly in a much more precarious environment. ... A case study in canterbury, New Zealand. London, England: The King's Fund. ... International Studies of Management & Organization, 37(2), 11-31.
The mission of the US Department of Health and Human Services (HHS) is to enhance and protect the health and well-being of all Americans. 1 In my work as deputy assistant secretary for human services at HHS, I have noticed that people think that HHS focuses solely on fostering advances in medicine and public health and ensuring access to effective clinical services through Medicare and ...
IPEC (2016) Competencies: NOHS (2015) Standards: Values and Ethics: Work with individuals of other professions to maintain a climate of mutual respect and shared values.; Standard 29: Human service professionals promote cooperation among related disciplines to foster professional growth and to optimize the impact of inter-professional collaboration on clients at all levels.
presenting the findings of an extensive questionnaire survey, a specific case study is offered. The case study illustrates how a firm tailors its human resource practices to get very specific behaviors from employees in order to implement a customer-oriented strategy. Advances in Services Marketing and Management, Volume 1, pages 123-157.
Here, research is generating the crucial argument that partnerships can put enormous financial pressures on human service organizations. An important national study of human service organizations conducted by the Urban Institute and authored by Boris et al. (Citation 2010) reinforced this conclusion. They paint a bleak landscape of delayed ...
Human services organizations of all sizes rely heavily on case management to improve outcomes for their clients. As stated in the pre-pandemic Salesforce.org Nonprofit Trends Report, "demand for more nonprofit programs and services is rising, as the world is threatened by climate change, natural and human-made disasters, humanitarian crises, political chaos, food insecurity, and so much more."
STANDARD 1 Human service professionals recognize and build on client and community strengths. STANDARD 2 At the beginning of the helping relationship, human service professionals obtain informed consent for services from clients. Clients should be informed that they may withdraw consent at any time and can ask questions before agreeing to the ...
In the case of this current study, for instance, Dutch youth care workers generally experience a high level of unpredictability and non-linearity in keeping children safe, in a continuously evolving political, legal, financial, and social environment. ... Human Service Organizations: Management, ...
Conceptual framework. The conceptual framework used in this study was based on neo-institutional theory (NIT) [32, 33].NITs view organizations as social structures that must conform to the expectations and pressures of their institutional environment, which includes normative and regulatory forces [34, 35].This approach was considered relevant for this study because decentralization is an ...
ABSTRACT. Organizational resilience is an emerging and important concept that focuses on building the capacity of human service organizations. While numerous studies documented challenges arising from purchase of service contracting, few have investigated how social work agencies can foster organizational resilience while maintaining daily service contracting processes over longer periods of time.