

Chapter 11. Interviewing
Introduction.
Interviewing people is at the heart of qualitative research. It is not merely a way to collect data but an intrinsically rewarding activity—an interaction between two people that holds the potential for greater understanding and interpersonal development. Unlike many of our daily interactions with others that are fairly shallow and mundane, sitting down with a person for an hour or two and really listening to what they have to say is a profound and deep enterprise, one that can provide not only “data” for you, the interviewer, but also self-understanding and a feeling of being heard for the interviewee. I always approach interviewing with a deep appreciation for the opportunity it gives me to understand how other people experience the world. That said, there is not one kind of interview but many, and some of these are shallower than others. This chapter will provide you with an overview of interview techniques but with a special focus on the in-depth semistructured interview guide approach, which is the approach most widely used in social science research.
An interview can be variously defined as “a conversation with a purpose” ( Lune and Berg 2018 ) and an attempt to understand the world from the point of view of the person being interviewed: “to unfold the meaning of peoples’ experiences, to uncover their lived world prior to scientific explanations” ( Kvale 2007 ). It is a form of active listening in which the interviewer steers the conversation to subjects and topics of interest to their research but also manages to leave enough space for those interviewed to say surprising things. Achieving that balance is a tricky thing, which is why most practitioners believe interviewing is both an art and a science. In my experience as a teacher, there are some students who are “natural” interviewers (often they are introverts), but anyone can learn to conduct interviews, and everyone, even those of us who have been doing this for years, can improve their interviewing skills. This might be a good time to highlight the fact that the interview is a product between interviewer and interviewee and that this product is only as good as the rapport established between the two participants. Active listening is the key to establishing this necessary rapport.
Patton ( 2002 ) makes the argument that we use interviews because there are certain things that are not observable. In particular, “we cannot observe feelings, thoughts, and intentions. We cannot observe behaviors that took place at some previous point in time. We cannot observe situations that preclude the presence of an observer. We cannot observe how people have organized the world and the meanings they attach to what goes on in the world. We have to ask people questions about those things” ( 341 ).
Types of Interviews
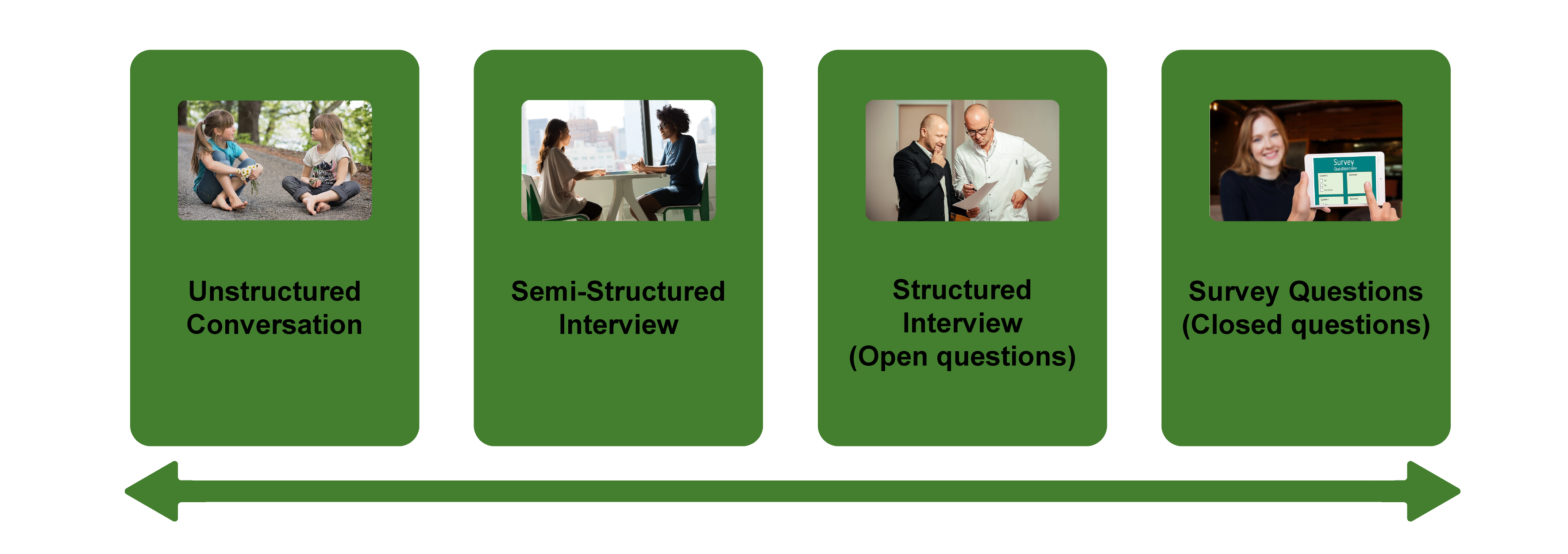
There are several distinct types of interviews. Imagine a continuum (figure 11.1). On one side are unstructured conversations—the kind you have with your friends. No one is in control of those conversations, and what you talk about is often random—whatever pops into your head. There is no secret, underlying purpose to your talking—if anything, the purpose is to talk to and engage with each other, and the words you use and the things you talk about are a little beside the point. An unstructured interview is a little like this informal conversation, except that one of the parties to the conversation (you, the researcher) does have an underlying purpose, and that is to understand the other person. You are not friends speaking for no purpose, but it might feel just as unstructured to the “interviewee” in this scenario. That is one side of the continuum. On the other side are fully structured and standardized survey-type questions asked face-to-face. Here it is very clear who is asking the questions and who is answering them. This doesn’t feel like a conversation at all! A lot of people new to interviewing have this ( erroneously !) in mind when they think about interviews as data collection. Somewhere in the middle of these two extreme cases is the “ semistructured” interview , in which the researcher uses an “interview guide” to gently move the conversation to certain topics and issues. This is the primary form of interviewing for qualitative social scientists and will be what I refer to as interviewing for the rest of this chapter, unless otherwise specified.
Informal (unstructured conversations). This is the most “open-ended” approach to interviewing. It is particularly useful in conjunction with observational methods (see chapters 13 and 14). There are no predetermined questions. Each interview will be different. Imagine you are researching the Oregon Country Fair, an annual event in Veneta, Oregon, that includes live music, artisan craft booths, face painting, and a lot of people walking through forest paths. It’s unlikely that you will be able to get a person to sit down with you and talk intensely about a set of questions for an hour and a half. But you might be able to sidle up to several people and engage with them about their experiences at the fair. You might have a general interest in what attracts people to these events, so you could start a conversation by asking strangers why they are here or why they come back every year. That’s it. Then you have a conversation that may lead you anywhere. Maybe one person tells a long story about how their parents brought them here when they were a kid. A second person talks about how this is better than Burning Man. A third person shares their favorite traveling band. And yet another enthuses about the public library in the woods. During your conversations, you also talk about a lot of other things—the weather, the utilikilts for sale, the fact that a favorite food booth has disappeared. It’s all good. You may not be able to record these conversations. Instead, you might jot down notes on the spot and then, when you have the time, write down as much as you can remember about the conversations in long fieldnotes. Later, you will have to sit down with these fieldnotes and try to make sense of all the information (see chapters 18 and 19).
Interview guide ( semistructured interview ). This is the primary type employed by social science qualitative researchers. The researcher creates an “interview guide” in advance, which she uses in every interview. In theory, every person interviewed is asked the same questions. In practice, every person interviewed is asked mostly the same topics but not always the same questions, as the whole point of a “guide” is that it guides the direction of the conversation but does not command it. The guide is typically between five and ten questions or question areas, sometimes with suggested follow-ups or prompts . For example, one question might be “What was it like growing up in Eastern Oregon?” with prompts such as “Did you live in a rural area? What kind of high school did you attend?” to help the conversation develop. These interviews generally take place in a quiet place (not a busy walkway during a festival) and are recorded. The recordings are transcribed, and those transcriptions then become the “data” that is analyzed (see chapters 18 and 19). The conventional length of one of these types of interviews is between one hour and two hours, optimally ninety minutes. Less than one hour doesn’t allow for much development of questions and thoughts, and two hours (or more) is a lot of time to ask someone to sit still and answer questions. If you have a lot of ground to cover, and the person is willing, I highly recommend two separate interview sessions, with the second session being slightly shorter than the first (e.g., ninety minutes the first day, sixty minutes the second). There are lots of good reasons for this, but the most compelling one is that this allows you to listen to the first day’s recording and catch anything interesting you might have missed in the moment and so develop follow-up questions that can probe further. This also allows the person being interviewed to have some time to think about the issues raised in the interview and go a little deeper with their answers.
Standardized questionnaire with open responses ( structured interview ). This is the type of interview a lot of people have in mind when they hear “interview”: a researcher comes to your door with a clipboard and proceeds to ask you a series of questions. These questions are all the same whoever answers the door; they are “standardized.” Both the wording and the exact order are important, as people’s responses may vary depending on how and when a question is asked. These are qualitative only in that the questions allow for “open-ended responses”: people can say whatever they want rather than select from a predetermined menu of responses. For example, a survey I collaborated on included this open-ended response question: “How does class affect one’s career success in sociology?” Some of the answers were simply one word long (e.g., “debt”), and others were long statements with stories and personal anecdotes. It is possible to be surprised by the responses. Although it’s a stretch to call this kind of questioning a conversation, it does allow the person answering the question some degree of freedom in how they answer.
Survey questionnaire with closed responses (not an interview!). Standardized survey questions with specific answer options (e.g., closed responses) are not really interviews at all, and they do not generate qualitative data. For example, if we included five options for the question “How does class affect one’s career success in sociology?”—(1) debt, (2) social networks, (3) alienation, (4) family doesn’t understand, (5) type of grad program—we leave no room for surprises at all. Instead, we would most likely look at patterns around these responses, thinking quantitatively rather than qualitatively (e.g., using regression analysis techniques, we might find that working-class sociologists were twice as likely to bring up alienation). It can sometimes be confusing for new students because the very same survey can include both closed-ended and open-ended questions. The key is to think about how these will be analyzed and to what level surprises are possible. If your plan is to turn all responses into a number and make predictions about correlations and relationships, you are no longer conducting qualitative research. This is true even if you are conducting this survey face-to-face with a real live human. Closed-response questions are not conversations of any kind, purposeful or not.
In summary, the semistructured interview guide approach is the predominant form of interviewing for social science qualitative researchers because it allows a high degree of freedom of responses from those interviewed (thus allowing for novel discoveries) while still maintaining some connection to a research question area or topic of interest. The rest of the chapter assumes the employment of this form.
Creating an Interview Guide
Your interview guide is the instrument used to bridge your research question(s) and what the people you are interviewing want to tell you. Unlike a standardized questionnaire, the questions actually asked do not need to be exactly what you have written down in your guide. The guide is meant to create space for those you are interviewing to talk about the phenomenon of interest, but sometimes you are not even sure what that phenomenon is until you start asking questions. A priority in creating an interview guide is to ensure it offers space. One of the worst mistakes is to create questions that are so specific that the person answering them will not stray. Relatedly, questions that sound “academic” will shut down a lot of respondents. A good interview guide invites respondents to talk about what is important to them, not feel like they are performing or being evaluated by you.
Good interview questions should not sound like your “research question” at all. For example, let’s say your research question is “How do patriarchal assumptions influence men’s understanding of climate change and responses to climate change?” It would be worse than unhelpful to ask a respondent, “How do your assumptions about the role of men affect your understanding of climate change?” You need to unpack this into manageable nuggets that pull your respondent into the area of interest without leading him anywhere. You could start by asking him what he thinks about climate change in general. Or, even better, whether he has any concerns about heatwaves or increased tornadoes or polar icecaps melting. Once he starts talking about that, you can ask follow-up questions that bring in issues around gendered roles, perhaps asking if he is married (to a woman) and whether his wife shares his thoughts and, if not, how they negotiate that difference. The fact is, you won’t really know the right questions to ask until he starts talking.
There are several distinct types of questions that can be used in your interview guide, either as main questions or as follow-up probes. If you remember that the point is to leave space for the respondent, you will craft a much more effective interview guide! You will also want to think about the place of time in both the questions themselves (past, present, future orientations) and the sequencing of the questions.
Researcher Note
Suggestion : As you read the next three sections (types of questions, temporality, question sequence), have in mind a particular research question, and try to draft questions and sequence them in a way that opens space for a discussion that helps you answer your research question.
Type of Questions
Experience and behavior questions ask about what a respondent does regularly (their behavior) or has done (their experience). These are relatively easy questions for people to answer because they appear more “factual” and less subjective. This makes them good opening questions. For the study on climate change above, you might ask, “Have you ever experienced an unusual weather event? What happened?” Or “You said you work outside? What is a typical summer workday like for you? How do you protect yourself from the heat?”
Opinion and values questions , in contrast, ask questions that get inside the minds of those you are interviewing. “Do you think climate change is real? Who or what is responsible for it?” are two such questions. Note that you don’t have to literally ask, “What is your opinion of X?” but you can find a way to ask the specific question relevant to the conversation you are having. These questions are a bit trickier to ask because the answers you get may depend in part on how your respondent perceives you and whether they want to please you or not. We’ve talked a fair amount about being reflective. Here is another place where this comes into play. You need to be aware of the effect your presence might have on the answers you are receiving and adjust accordingly. If you are a woman who is perceived as liberal asking a man who identifies as conservative about climate change, there is a lot of subtext that can be going on in the interview. There is no one right way to resolve this, but you must at least be aware of it.
Feeling questions are questions that ask respondents to draw on their emotional responses. It’s pretty common for academic researchers to forget that we have bodies and emotions, but people’s understandings of the world often operate at this affective level, sometimes unconsciously or barely consciously. It is a good idea to include questions that leave space for respondents to remember, imagine, or relive emotional responses to particular phenomena. “What was it like when you heard your cousin’s house burned down in that wildfire?” doesn’t explicitly use any emotion words, but it allows your respondent to remember what was probably a pretty emotional day. And if they respond emotionally neutral, that is pretty interesting data too. Note that asking someone “How do you feel about X” is not always going to evoke an emotional response, as they might simply turn around and respond with “I think that…” It is better to craft a question that actually pushes the respondent into the affective category. This might be a specific follow-up to an experience and behavior question —for example, “You just told me about your daily routine during the summer heat. Do you worry it is going to get worse?” or “Have you ever been afraid it will be too hot to get your work accomplished?”
Knowledge questions ask respondents what they actually know about something factual. We have to be careful when we ask these types of questions so that respondents do not feel like we are evaluating them (which would shut them down), but, for example, it is helpful to know when you are having a conversation about climate change that your respondent does in fact know that unusual weather events have increased and that these have been attributed to climate change! Asking these questions can set the stage for deeper questions and can ensure that the conversation makes the same kind of sense to both participants. For example, a conversation about political polarization can be put back on track once you realize that the respondent doesn’t really have a clear understanding that there are two parties in the US. Instead of asking a series of questions about Republicans and Democrats, you might shift your questions to talk more generally about political disagreements (e.g., “people against abortion”). And sometimes what you do want to know is the level of knowledge about a particular program or event (e.g., “Are you aware you can discharge your student loans through the Public Service Loan Forgiveness program?”).
Sensory questions call on all senses of the respondent to capture deeper responses. These are particularly helpful in sparking memory. “Think back to your childhood in Eastern Oregon. Describe the smells, the sounds…” Or you could use these questions to help a person access the full experience of a setting they customarily inhabit: “When you walk through the doors to your office building, what do you see? Hear? Smell?” As with feeling questions , these questions often supplement experience and behavior questions . They are another way of allowing your respondent to report fully and deeply rather than remain on the surface.
Creative questions employ illustrative examples, suggested scenarios, or simulations to get respondents to think more deeply about an issue, topic, or experience. There are many options here. In The Trouble with Passion , Erin Cech ( 2021 ) provides a scenario in which “Joe” is trying to decide whether to stay at his decent but boring computer job or follow his passion by opening a restaurant. She asks respondents, “What should Joe do?” Their answers illuminate the attraction of “passion” in job selection. In my own work, I have used a news story about an upwardly mobile young man who no longer has time to see his mother and sisters to probe respondents’ feelings about the costs of social mobility. Jessi Streib and Betsy Leondar-Wright have used single-page cartoon “scenes” to elicit evaluations of potential racial discrimination, sexual harassment, and classism. Barbara Sutton ( 2010 ) has employed lists of words (“strong,” “mother,” “victim”) on notecards she fans out and asks her female respondents to select and discuss.
Background/Demographic Questions
You most definitely will want to know more about the person you are interviewing in terms of conventional demographic information, such as age, race, gender identity, occupation, and educational attainment. These are not questions that normally open up inquiry. [1] For this reason, my practice has been to include a separate “demographic questionnaire” sheet that I ask each respondent to fill out at the conclusion of the interview. Only include those aspects that are relevant to your study. For example, if you are not exploring religion or religious affiliation, do not include questions about a person’s religion on the demographic sheet. See the example provided at the end of this chapter.
Temporality
Any type of question can have a past, present, or future orientation. For example, if you are asking a behavior question about workplace routine, you might ask the respondent to talk about past work, present work, and ideal (future) work. Similarly, if you want to understand how people cope with natural disasters, you might ask your respondent how they felt then during the wildfire and now in retrospect and whether and to what extent they have concerns for future wildfire disasters. It’s a relatively simple suggestion—don’t forget to ask about past, present, and future—but it can have a big impact on the quality of the responses you receive.
Question Sequence
Having a list of good questions or good question areas is not enough to make a good interview guide. You will want to pay attention to the order in which you ask your questions. Even though any one respondent can derail this order (perhaps by jumping to answer a question you haven’t yet asked), a good advance plan is always helpful. When thinking about sequence, remember that your goal is to get your respondent to open up to you and to say things that might surprise you. To establish rapport, it is best to start with nonthreatening questions. Asking about the present is often the safest place to begin, followed by the past (they have to know you a little bit to get there), and lastly, the future (talking about hopes and fears requires the most rapport). To allow for surprises, it is best to move from very general questions to more particular questions only later in the interview. This ensures that respondents have the freedom to bring up the topics that are relevant to them rather than feel like they are constrained to answer you narrowly. For example, refrain from asking about particular emotions until these have come up previously—don’t lead with them. Often, your more particular questions will emerge only during the course of the interview, tailored to what is emerging in conversation.
Once you have a set of questions, read through them aloud and imagine you are being asked the same questions. Does the set of questions have a natural flow? Would you be willing to answer the very first question to a total stranger? Does your sequence establish facts and experiences before moving on to opinions and values? Did you include prefatory statements, where necessary; transitions; and other announcements? These can be as simple as “Hey, we talked a lot about your experiences as a barista while in college.… Now I am turning to something completely different: how you managed friendships in college.” That is an abrupt transition, but it has been softened by your acknowledgment of that.
Probes and Flexibility
Once you have the interview guide, you will also want to leave room for probes and follow-up questions. As in the sample probe included here, you can write out the obvious probes and follow-up questions in advance. You might not need them, as your respondent might anticipate them and include full responses to the original question. Or you might need to tailor them to how your respondent answered the question. Some common probes and follow-up questions include asking for more details (When did that happen? Who else was there?), asking for elaboration (Could you say more about that?), asking for clarification (Does that mean what I think it means or something else? I understand what you mean, but someone else reading the transcript might not), and asking for contrast or comparison (How did this experience compare with last year’s event?). “Probing is a skill that comes from knowing what to look for in the interview, listening carefully to what is being said and what is not said, and being sensitive to the feedback needs of the person being interviewed” ( Patton 2002:374 ). It takes work! And energy. I and many other interviewers I know report feeling emotionally and even physically drained after conducting an interview. You are tasked with active listening and rearranging your interview guide as needed on the fly. If you only ask the questions written down in your interview guide with no deviations, you are doing it wrong. [2]
The Final Question
Every interview guide should include a very open-ended final question that allows for the respondent to say whatever it is they have been dying to tell you but you’ve forgotten to ask. About half the time they are tired too and will tell you they have nothing else to say. But incredibly, some of the most honest and complete responses take place here, at the end of a long interview. You have to realize that the person being interviewed is often discovering things about themselves as they talk to you and that this process of discovery can lead to new insights for them. Making space at the end is therefore crucial. Be sure you convey that you actually do want them to tell you more, that the offer of “anything else?” is not read as an empty convention where the polite response is no. Here is where you can pull from that active listening and tailor the final question to the particular person. For example, “I’ve asked you a lot of questions about what it was like to live through that wildfire. I’m wondering if there is anything I’ve forgotten to ask, especially because I haven’t had that experience myself” is a much more inviting final question than “Great. Anything you want to add?” It’s also helpful to convey to the person that you have the time to listen to their full answer, even if the allotted time is at the end. After all, there are no more questions to ask, so the respondent knows exactly how much time is left. Do them the courtesy of listening to them!
Conducting the Interview
Once you have your interview guide, you are on your way to conducting your first interview. I always practice my interview guide with a friend or family member. I do this even when the questions don’t make perfect sense for them, as it still helps me realize which questions make no sense, are poorly worded (too academic), or don’t follow sequentially. I also practice the routine I will use for interviewing, which goes something like this:
- Introduce myself and reintroduce the study
- Provide consent form and ask them to sign and retain/return copy
- Ask if they have any questions about the study before we begin
- Ask if I can begin recording
- Ask questions (from interview guide)
- Turn off the recording device
- Ask if they are willing to fill out my demographic questionnaire
- Collect questionnaire and, without looking at the answers, place in same folder as signed consent form
- Thank them and depart
A note on remote interviewing: Interviews have traditionally been conducted face-to-face in a private or quiet public setting. You don’t want a lot of background noise, as this will make transcriptions difficult. During the recent global pandemic, many interviewers, myself included, learned the benefits of interviewing remotely. Although face-to-face is still preferable for many reasons, Zoom interviewing is not a bad alternative, and it does allow more interviews across great distances. Zoom also includes automatic transcription, which significantly cuts down on the time it normally takes to convert our conversations into “data” to be analyzed. These automatic transcriptions are not perfect, however, and you will still need to listen to the recording and clarify and clean up the transcription. Nor do automatic transcriptions include notations of body language or change of tone, which you may want to include. When interviewing remotely, you will want to collect the consent form before you meet: ask them to read, sign, and return it as an email attachment. I think it is better to ask for the demographic questionnaire after the interview, but because some respondents may never return it then, it is probably best to ask for this at the same time as the consent form, in advance of the interview.
What should you bring to the interview? I would recommend bringing two copies of the consent form (one for you and one for the respondent), a demographic questionnaire, a manila folder in which to place the signed consent form and filled-out demographic questionnaire, a printed copy of your interview guide (I print with three-inch right margins so I can jot down notes on the page next to relevant questions), a pen, a recording device, and water.
After the interview, you will want to secure the signed consent form in a locked filing cabinet (if in print) or a password-protected folder on your computer. Using Excel or a similar program that allows tables/spreadsheets, create an identifying number for your interview that links to the consent form without using the name of your respondent. For example, let’s say that I conduct interviews with US politicians, and the first person I meet with is George W. Bush. I will assign the transcription the number “INT#001” and add it to the signed consent form. [3] The signed consent form goes into a locked filing cabinet, and I never use the name “George W. Bush” again. I take the information from the demographic sheet, open my Excel spreadsheet, and add the relevant information in separate columns for the row INT#001: White, male, Republican. When I interview Bill Clinton as my second interview, I include a second row: INT#002: White, male, Democrat. And so on. The only link to the actual name of the respondent and this information is the fact that the consent form (unavailable to anyone but me) has stamped on it the interview number.
Many students get very nervous before their first interview. Actually, many of us are always nervous before the interview! But do not worry—this is normal, and it does pass. Chances are, you will be pleasantly surprised at how comfortable it begins to feel. These “purposeful conversations” are often a delight for both participants. This is not to say that sometimes things go wrong. I often have my students practice several “bad scenarios” (e.g., a respondent that you cannot get to open up; a respondent who is too talkative and dominates the conversation, steering it away from the topics you are interested in; emotions that completely take over; or shocking disclosures you are ill-prepared to handle), but most of the time, things go quite well. Be prepared for the unexpected, but know that the reason interviews are so popular as a technique of data collection is that they are usually richly rewarding for both participants.
One thing that I stress to my methods students and remind myself about is that interviews are still conversations between people. If there’s something you might feel uncomfortable asking someone about in a “normal” conversation, you will likely also feel a bit of discomfort asking it in an interview. Maybe more importantly, your respondent may feel uncomfortable. Social research—especially about inequality—can be uncomfortable. And it’s easy to slip into an abstract, intellectualized, or removed perspective as an interviewer. This is one reason trying out interview questions is important. Another is that sometimes the question sounds good in your head but doesn’t work as well out loud in practice. I learned this the hard way when a respondent asked me how I would answer the question I had just posed, and I realized that not only did I not really know how I would answer it, but I also wasn’t quite as sure I knew what I was asking as I had thought.
—Elizabeth M. Lee, Associate Professor of Sociology at Saint Joseph’s University, author of Class and Campus Life , and co-author of Geographies of Campus Inequality
How Many Interviews?
Your research design has included a targeted number of interviews and a recruitment plan (see chapter 5). Follow your plan, but remember that “ saturation ” is your goal. You interview as many people as you can until you reach a point at which you are no longer surprised by what they tell you. This means not that no one after your first twenty interviews will have surprising, interesting stories to tell you but rather that the picture you are forming about the phenomenon of interest to you from a research perspective has come into focus, and none of the interviews are substantially refocusing that picture. That is when you should stop collecting interviews. Note that to know when you have reached this, you will need to read your transcripts as you go. More about this in chapters 18 and 19.
Your Final Product: The Ideal Interview Transcript
A good interview transcript will demonstrate a subtly controlled conversation by the skillful interviewer. In general, you want to see replies that are about one paragraph long, not short sentences and not running on for several pages. Although it is sometimes necessary to follow respondents down tangents, it is also often necessary to pull them back to the questions that form the basis of your research study. This is not really a free conversation, although it may feel like that to the person you are interviewing.
Final Tips from an Interview Master
Annette Lareau is arguably one of the masters of the trade. In Listening to People , she provides several guidelines for good interviews and then offers a detailed example of an interview gone wrong and how it could be addressed (please see the “Further Readings” at the end of this chapter). Here is an abbreviated version of her set of guidelines: (1) interview respondents who are experts on the subjects of most interest to you (as a corollary, don’t ask people about things they don’t know); (2) listen carefully and talk as little as possible; (3) keep in mind what you want to know and why you want to know it; (4) be a proactive interviewer (subtly guide the conversation); (5) assure respondents that there aren’t any right or wrong answers; (6) use the respondent’s own words to probe further (this both allows you to accurately identify what you heard and pushes the respondent to explain further); (7) reuse effective probes (don’t reinvent the wheel as you go—if repeating the words back works, do it again and again); (8) focus on learning the subjective meanings that events or experiences have for a respondent; (9) don’t be afraid to ask a question that draws on your own knowledge (unlike trial lawyers who are trained never to ask a question for which they don’t already know the answer, sometimes it’s worth it to ask risky questions based on your hypotheses or just plain hunches); (10) keep thinking while you are listening (so difficult…and important); (11) return to a theme raised by a respondent if you want further information; (12) be mindful of power inequalities (and never ever coerce a respondent to continue the interview if they want out); (13) take control with overly talkative respondents; (14) expect overly succinct responses, and develop strategies for probing further; (15) balance digging deep and moving on; (16) develop a plan to deflect questions (e.g., let them know you are happy to answer any questions at the end of the interview, but you don’t want to take time away from them now); and at the end, (17) check to see whether you have asked all your questions. You don’t always have to ask everyone the same set of questions, but if there is a big area you have forgotten to cover, now is the time to recover ( Lareau 2021:93–103 ).
Sample: Demographic Questionnaire
ASA Taskforce on First-Generation and Working-Class Persons in Sociology – Class Effects on Career Success
Supplementary Demographic Questionnaire
Thank you for your participation in this interview project. We would like to collect a few pieces of key demographic information from you to supplement our analyses. Your answers to these questions will be kept confidential and stored by ID number. All of your responses here are entirely voluntary!
What best captures your race/ethnicity? (please check any/all that apply)
- White (Non Hispanic/Latina/o/x)
- Black or African American
- Hispanic, Latino/a/x of Spanish
- Asian or Asian American
- American Indian or Alaska Native
- Middle Eastern or North African
- Native Hawaiian or Pacific Islander
- Other : (Please write in: ________________)
What is your current position?
- Grad Student
- Full Professor
Please check any and all of the following that apply to you:
- I identify as a working-class academic
- I was the first in my family to graduate from college
- I grew up poor
What best reflects your gender?
- Transgender female/Transgender woman
- Transgender male/Transgender man
- Gender queer/ Gender nonconforming
Anything else you would like us to know about you?
Example: Interview Guide
In this example, follow-up prompts are italicized. Note the sequence of questions. That second question often elicits an entire life history , answering several later questions in advance.
Introduction Script/Question
Thank you for participating in our survey of ASA members who identify as first-generation or working-class. As you may have heard, ASA has sponsored a taskforce on first-generation and working-class persons in sociology and we are interested in hearing from those who so identify. Your participation in this interview will help advance our knowledge in this area.
- The first thing we would like to as you is why you have volunteered to be part of this study? What does it mean to you be first-gen or working class? Why were you willing to be interviewed?
- How did you decide to become a sociologist?
- Can you tell me a little bit about where you grew up? ( prompts: what did your parent(s) do for a living? What kind of high school did you attend?)
- Has this identity been salient to your experience? (how? How much?)
- How welcoming was your grad program? Your first academic employer?
- Why did you decide to pursue sociology at the graduate level?
- Did you experience culture shock in college? In graduate school?
- Has your FGWC status shaped how you’ve thought about where you went to school? debt? etc?
- Were you mentored? How did this work (not work)? How might it?
- What did you consider when deciding where to go to grad school? Where to apply for your first position?
- What, to you, is a mark of career success? Have you achieved that success? What has helped or hindered your pursuit of success?
- Do you think sociology, as a field, cares about prestige?
- Let’s talk a little bit about intersectionality. How does being first-gen/working class work alongside other identities that are important to you?
- What do your friends and family think about your career? Have you had any difficulty relating to family members or past friends since becoming highly educated?
- Do you have any debt from college/grad school? Are you concerned about this? Could you explain more about how you paid for college/grad school? (here, include assistance from family, fellowships, scholarships, etc.)
- (You’ve mentioned issues or obstacles you had because of your background.) What could have helped? Or, who or what did? Can you think of fortuitous moments in your career?
- Do you have any regrets about the path you took?
- Is there anything else you would like to add? Anything that the Taskforce should take note of, that we did not ask you about here?
Further Readings
Britten, Nicky. 1995. “Qualitative Interviews in Medical Research.” BMJ: British Medical Journal 31(6999):251–253. A good basic overview of interviewing particularly useful for students of public health and medical research generally.
Corbin, Juliet, and Janice M. Morse. 2003. “The Unstructured Interactive Interview: Issues of Reciprocity and Risks When Dealing with Sensitive Topics.” Qualitative Inquiry 9(3):335–354. Weighs the potential benefits and harms of conducting interviews on topics that may cause emotional distress. Argues that the researcher’s skills and code of ethics should ensure that the interviewing process provides more of a benefit to both participant and researcher than a harm to the former.
Gerson, Kathleen, and Sarah Damaske. 2020. The Science and Art of Interviewing . New York: Oxford University Press. A useful guidebook/textbook for both undergraduates and graduate students, written by sociologists.
Kvale, Steiner. 2007. Doing Interviews . London: SAGE. An easy-to-follow guide to conducting and analyzing interviews by psychologists.
Lamont, Michèle, and Ann Swidler. 2014. “Methodological Pluralism and the Possibilities and Limits of Interviewing.” Qualitative Sociology 37(2):153–171. Written as a response to various debates surrounding the relative value of interview-based studies and ethnographic studies defending the particular strengths of interviewing. This is a must-read article for anyone seriously engaging in qualitative research!
Pugh, Allison J. 2013. “What Good Are Interviews for Thinking about Culture? Demystifying Interpretive Analysis.” American Journal of Cultural Sociology 1(1):42–68. Another defense of interviewing written against those who champion ethnographic methods as superior, particularly in the area of studying culture. A classic.
Rapley, Timothy John. 2001. “The ‘Artfulness’ of Open-Ended Interviewing: Some considerations in analyzing interviews.” Qualitative Research 1(3):303–323. Argues for the importance of “local context” of data production (the relationship built between interviewer and interviewee, for example) in properly analyzing interview data.
Weiss, Robert S. 1995. Learning from Strangers: The Art and Method of Qualitative Interview Studies . New York: Simon and Schuster. A classic and well-regarded textbook on interviewing. Because Weiss has extensive experience conducting surveys, he contrasts the qualitative interview with the survey questionnaire well; particularly useful for those trained in the latter.
- I say “normally” because how people understand their various identities can itself be an expansive topic of inquiry. Here, I am merely talking about collecting otherwise unexamined demographic data, similar to how we ask people to check boxes on surveys. ↵
- Again, this applies to “semistructured in-depth interviewing.” When conducting standardized questionnaires, you will want to ask each question exactly as written, without deviations! ↵
- I always include “INT” in the number because I sometimes have other kinds of data with their own numbering: FG#001 would mean the first focus group, for example. I also always include three-digit spaces, as this allows for up to 999 interviews (or, more realistically, allows for me to interview up to one hundred persons without having to reset my numbering system). ↵
A method of data collection in which the researcher asks the participant questions; the answers to these questions are often recorded and transcribed verbatim. There are many different kinds of interviews - see also semistructured interview , structured interview , and unstructured interview .
A document listing key questions and question areas for use during an interview. It is used most often for semi-structured interviews. A good interview guide may have no more than ten primary questions for two hours of interviewing, but these ten questions will be supplemented by probes and relevant follow-ups throughout the interview. Most IRBs require the inclusion of the interview guide in applications for review. See also interview and semi-structured interview .
A data-collection method that relies on casual, conversational, and informal interviewing. Despite its apparent conversational nature, the researcher usually has a set of particular questions or question areas in mind but allows the interview to unfold spontaneously. This is a common data-collection technique among ethnographers. Compare to the semi-structured or in-depth interview .
A form of interview that follows a standard guide of questions asked, although the order of the questions may change to match the particular needs of each individual interview subject, and probing “follow-up” questions are often added during the course of the interview. The semi-structured interview is the primary form of interviewing used by qualitative researchers in the social sciences. It is sometimes referred to as an “in-depth” interview. See also interview and interview guide .
The cluster of data-collection tools and techniques that involve observing interactions between people, the behaviors, and practices of individuals (sometimes in contrast to what they say about how they act and behave), and cultures in context. Observational methods are the key tools employed by ethnographers and Grounded Theory .
Follow-up questions used in a semi-structured interview to elicit further elaboration. Suggested prompts can be included in the interview guide to be used/deployed depending on how the initial question was answered or if the topic of the prompt does not emerge spontaneously.
A form of interview that follows a strict set of questions, asked in a particular order, for all interview subjects. The questions are also the kind that elicits short answers, and the data is more “informative” than probing. This is often used in mixed-methods studies, accompanying a survey instrument. Because there is no room for nuance or the exploration of meaning in structured interviews, qualitative researchers tend to employ semi-structured interviews instead. See also interview.
The point at which you can conclude data collection because every person you are interviewing, the interaction you are observing, or content you are analyzing merely confirms what you have already noted. Achieving saturation is often used as the justification for the final sample size.
An interview variant in which a person’s life story is elicited in a narrative form. Turning points and key themes are established by the researcher and used as data points for further analysis.
Introduction to Qualitative Research Methods Copyright © 2023 by Allison Hurst is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
How to conduct qualitative interviews (tips and best practices)
Last updated
18 May 2023
Reviewed by
Miroslav Damyanov
However, conducting qualitative interviews can be challenging, even for seasoned researchers. Poorly conducted interviews can lead to inaccurate or incomplete data, significantly compromising the validity and reliability of your research findings.
When planning to conduct qualitative interviews, you must adequately prepare yourself to get the most out of your data. Fortunately, there are specific tips and best practices that can help you conduct qualitative interviews effectively.
- What is a qualitative interview?
A qualitative interview is a research technique used to gather in-depth information about people's experiences, attitudes, beliefs, and perceptions. Unlike a structured questionnaire or survey, a qualitative interview is a flexible, conversational approach that allows the interviewer to delve into the interviewee's responses and explore their insights and experiences.
In a qualitative interview, the researcher typically develops a set of open-ended questions that provide a framework for the conversation. However, the interviewer can also adapt to the interviewee's responses and ask follow-up questions to understand their experiences and views better.
- How to conduct interviews in qualitative research
Conducting interviews involves a well-planned and deliberate process to collect accurate and valid data.
Here’s a step-by-step guide on how to conduct interviews in qualitative research, broken down into three stages:
1. Before the interview
The first step in conducting a qualitative interview is determining your research question . This will help you identify the type of participants you need to recruit . Once you have your research question, you can start recruiting participants by identifying potential candidates and contacting them to gauge their interest in participating in the study.
After that, it's time to develop your interview questions. These should be open-ended questions that will elicit detailed responses from participants. You'll also need to get consent from the participants, ideally in writing, to ensure that they understand the purpose of the study and their rights as participants. Finally, choose a comfortable and private location to conduct the interview and prepare the interview guide.
2. During the interview
Start by introducing yourself and explaining the purpose of the study. Establish a rapport by putting the participants at ease and making them feel comfortable. Use the interview guide to ask the questions, but be flexible and ask follow-up questions to gain more insight into the participants' responses.
Take notes during the interview, and ask permission to record the interview for transcription purposes. Be mindful of the time, and cover all the questions in the interview guide.
3. After the interview
Once the interview is over, transcribe the interview if you recorded it. If you took notes, review and organize them to make sure you capture all the important information. Then, analyze the data you collected by identifying common themes and patterns. Use the findings to answer your research question.
Finally, debrief with the participants to thank them for their time, provide feedback on the study, and answer any questions they may have.
Free AI content analysis generator
Make sense of your research by automatically summarizing key takeaways through our free content analysis tool.
- What kinds of questions should you ask in a qualitative interview?
Qualitative interviews involve asking questions that encourage participants to share their experiences, opinions, and perspectives on a particular topic. These questions are designed to elicit detailed and nuanced responses rather than simple yes or no answers.
Effective questions in a qualitative interview are generally open-ended and non-leading. They avoid presuppositions or assumptions about the participant's experience and allow them to share their views in their own words.
In customer research , you might ask questions such as:
What motivated you to choose our product/service over our competitors?
How did you first learn about our product/service?
Can you walk me through your experience with our product/service?
What improvements or changes would you suggest for our product/service?
Have you recommended our product/service to others, and if so, why?
The key is to ask questions relevant to the research topic and allow participants to share their experiences meaningfully and informally.
- How to determine the right qualitative interview participants
Choosing the right participants for a qualitative interview is a crucial step in ensuring the success and validity of the research . You need to consider several factors to determine the right participants for a qualitative interview. These may include:
Relevant experiences : Participants should have experiences related to the research topic that can provide valuable insights.
Diversity : Aim to include diverse participants to ensure the study's findings are representative and inclusive.
Access : Identify participants who are accessible and willing to participate in the study.
Informed consent : Participants should be fully informed about the study's purpose, methods, and potential risks and benefits and be allowed to provide informed consent.
You can use various recruitment methods, such as posting ads in relevant forums, contacting community organizations or social media groups, or using purposive sampling to identify participants who meet specific criteria.
- How to make qualitative interview subjects comfortable
Making participants comfortable during a qualitative interview is essential to obtain rich, detailed data. Participants are more likely to share their experiences openly when they feel at ease and not judged.
Here are some ways to make interview subjects comfortable:
Explain the purpose of the study
Start the interview by explaining the research topic and its importance. The goal is to give participants a sense of what to expect.
Create a comfortable environment
Conduct the interview in a quiet, private space where the participant feels comfortable. Turn off any unnecessary electronics that can create distractions. Ensure your equipment works well ahead of time. Arrive at the interview on time. If you conduct a remote interview, turn on your camera and mute all notetakers and observers.
Build rapport
Greet the participant warmly and introduce yourself. Show interest in their responses and thank them for their time.
Use open-ended questions
Ask questions that encourage participants to elaborate on their thoughts and experiences.
Listen attentively
Resist the urge to multitask . Pay attention to the participant's responses, nod your head, or make supportive comments to show you’re interested in their answers. Avoid interrupting them.
Avoid judgment
Show respect and don't judge the participant's views or experiences. Allow the participant to speak freely without feeling judged or ridiculed.
Offer breaks
If needed, offer breaks during the interview, especially if the topic is sensitive or emotional.
Creating a comfortable environment and establishing rapport with the participant fosters an atmosphere of trust and encourages open communication. This helps participants feel at ease and willing to share their experiences.
- How to analyze a qualitative interview
Analyzing a qualitative interview involves a systematic process of examining the data collected to identify patterns, themes, and meanings that emerge from the responses.
Here are some steps on how to analyze a qualitative interview:
1. Transcription
The first step is transcribing the interview into text format to have a written record of the conversation. This step is essential to ensure that you can refer back to the interview data and identify the important aspects of the interview.
2. Data reduction
Once you’ve transcribed the interview, read through it to identify key themes, patterns, and phrases emerging from the data. This process involves reducing the data into more manageable pieces you can easily analyze.
The next step is to code the data by labeling sections of the text with descriptive words or phrases that reflect the data's content. Coding helps identify key themes and patterns from the interview data.
4. Categorization
After coding, you should group the codes into categories based on their similarities. This process helps to identify overarching themes or sub-themes that emerge from the data.
5. Interpretation
You should then interpret the themes and sub-themes by identifying relationships, contradictions, and meanings that emerge from the data. Interpretation involves analyzing the themes in the context of the research question .
6. Comparison
The next step is comparing the data across participants or groups to identify similarities and differences. This step helps to ensure that the findings aren’t just specific to one participant but can be generalized to the wider population.
7. Triangulation
To ensure the findings are valid and reliable, you should use triangulation by comparing the findings with other sources, such as observations or interview data.
8. Synthesis
The final step is synthesizing the findings by summarizing the key themes and presenting them clearly and concisely. This step involves writing a report that presents the findings in a way that is easy to understand, using quotes and examples from the interview data to illustrate the themes.
- Tips for transcribing a qualitative interview
Transcribing a qualitative interview is a crucial step in the research process. It involves converting the audio or video recording of the interview into written text.
Here are some tips for transcribing a qualitative interview:
Use transcription software
Transcription software can save time and increase accuracy by automatically transcribing audio or video recordings.
Listen carefully
When manually transcribing, listen carefully to the recording to ensure clarity. Pause and rewind the recording as necessary.
Use appropriate formatting
Use a consistent format for transcribing, such as marking pauses, overlaps, and interruptions. Indicate non-verbal cues such as laughter, sighs, or changes in tone.
Edit for clarity
Edit the transcription to ensure clarity and readability. Use standard grammar and punctuation, correct misspellings, and remove filler words like "um" and "ah."
Proofread and edit
Verify the accuracy of the transcription by listening to the recording again and reviewing the notes taken during the interview.
Use timestamps
Add timestamps to the transcription to reference specific interview sections.
Transcribing a qualitative interview can be time-consuming, but it’s essential to ensure the accuracy of the data collected. Following these tips can produce high-quality transcriptions useful for analysis and reporting.
- Why are interview techniques in qualitative research effective?
Unlike quantitative research methods, which rely on numerical data, qualitative research seeks to understand the richness and complexity of human experiences and perspectives.
Interview techniques involve asking open-ended questions that allow participants to express their views and share their stories in their own words. This approach can help researchers to uncover unexpected or surprising insights that may not have been discovered through other research methods.
Interview techniques also allow researchers to establish rapport with participants, creating a comfortable and safe space for them to share their experiences. This can lead to a deeper level of trust and candor, leading to more honest and authentic responses.
- What are the weaknesses of qualitative interviews?
Qualitative interviews are an excellent research approach when used properly, but they have their drawbacks.
The weaknesses of qualitative interviews include the following:
Subjectivity and personal biases
Qualitative interviews rely on the researcher's interpretation of the interviewee's responses. The researcher's biases or preconceptions can affect how the questions are framed and how the responses are interpreted, which can influence results.
Small sample size
The sample size in qualitative interviews is often small, which can limit the generalizability of the results to the larger population.
Data quality
The quality of data collected during interviews can be affected by various factors, such as the interviewee's mood, the setting of the interview, and the interviewer's skills and experience.
Socially desirable responses
Interviewees may provide responses that they believe are socially acceptable rather than truthful or genuine.
Conducting qualitative interviews can be expensive, especially if the researcher must travel to different locations to conduct the interviews.
Time-consuming
The data analysis process can be time-consuming and labor-intensive, as researchers need to transcribe and analyze the data manually.
Despite these weaknesses, qualitative interviews remain a valuable research tool . You can take steps to mitigate the impact of these weaknesses by incorporating the perspectives of other researchers or participants in the analysis process, using multiple data sources , and critically analyzing your biases and assumptions.
Mastering the art of qualitative interviews is an essential skill for businesses looking to gain deep insights into their customers' needs , preferences, and behaviors. By following the tips and best practices outlined in this article, you can conduct interviews that provide you with rich data that you can use to make informed decisions about your products, services, and marketing strategies.
Remember that effective communication, active listening, and proper analysis are critical components of successful qualitative interviews. By incorporating these practices into your customer research, you can gain a competitive edge and build stronger customer relationships.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 18 April 2023
Last updated: 27 February 2023
Last updated: 22 August 2024
Last updated: 5 February 2023
Last updated: 16 August 2024
Last updated: 9 March 2023
Last updated: 30 April 2024
Last updated: 12 December 2023
Last updated: 11 March 2024
Last updated: 4 July 2024
Last updated: 6 March 2024
Last updated: 5 March 2024
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next, log in or sign up.
Get started for free
Qualitative Interviewing
- Reference work entry
- First Online: 13 January 2019
- Cite this reference work entry

- Sally Nathan 2 ,
- Christy Newman 3 &
- Kari Lancaster 3
4687 Accesses
26 Citations
8 Altmetric
Qualitative interviewing is a foundational method in qualitative research and is widely used in health research and the social sciences. Both qualitative semi-structured and in-depth unstructured interviews use verbal communication, mostly in face-to-face interactions, to collect data about the attitudes, beliefs, and experiences of participants. Interviews are an accessible, often affordable, and effective method to understand the socially situated world of research participants. The approach is typically informed by an interpretive framework where the data collected is not viewed as evidence of the truth or reality of a situation or experience but rather a context-bound subjective insight from the participants. The researcher needs to be open to new insights and to privilege the participant’s experience in data collection. The data from qualitative interviews is not generalizable, but its exploratory nature permits the collection of rich data which can answer questions about which little is already known. This chapter introduces the reader to qualitative interviewing, the range of traditions within which interviewing is utilized as a method, and highlights the advantages and some of the challenges and misconceptions in its application. The chapter also provides practical guidance on planning and conducting interview studies. Three case examples are presented to highlight the benefits and risks in the use of interviewing with different participants, providing situated insights as well as advice about how to go about learning to interview if you are a novice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Interviews in the social sciences

Interviewing in Qualitative Research
Baez B. Confidentiality in qualitative research: reflections on secrets, power and agency. Qual Res. 2002;2(1):35–58. https://doi.org/10.1177/1468794102002001638 .
Article Google Scholar
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: Sage Publications; 2013.
Google Scholar
Braun V, Clarke V, Gray D. Collecting qualitative data: a practical guide to textual, media and virtual techniques. Cambridge: Cambridge University Press; 2017.
Book Google Scholar
Bryman A. Social research methods. 5th ed. Oxford: Oxford University Press; 2016.
Crotty M. The foundations of social research: meaning and perspective in the research process. Australia: Allen & Unwin; 1998.
Davies MB. Doing a successful research project: using qualitative or quantitative methods. New York: Palgrave MacMillan; 2007.
Dickson-Swift V, James EL, Liamputtong P. Undertaking sensitive research in the health and social sciences. Cambridge: Cambridge University Press; 2008.
Foster M, Nathan S, Ferry M. The experience of drug-dependent adolescents in a therapeutic community. Drug Alcohol Rev. 2010;29(5):531–9.
Gillham B. The research interview. London: Continuum; 2000.
Glaser B, Strauss A. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine Publishing Company; 1967.
Hesse-Biber SN, Leavy P. In-depth interview. In: The practice of qualitative research. 2nd ed. Thousand Oaks: Sage Publications; 2011. p. 119–47
Irvine A. Duration, dominance and depth in telephone and face-to-face interviews: a comparative exploration. Int J Qual Methods. 2011;10(3):202–20.
Johnson JM. In-depth interviewing. In: Gubrium JF, Holstein JA, editors. Handbook of interview research: context and method. Thousand Oaks: Sage Publications; 2001.
Kvale S. Interviews: an introduction to qualitative research interviewing. Thousand Oaks: Sage; 1996.
Kvale S. Doing interviews. London: Sage Publications; 2007.
Lancaster K. Confidentiality, anonymity and power relations in elite interviewing: conducting qualitative policy research in a politicised domain. Int J Soc Res Methodol. 2017;20(1):93–103. https://doi.org/10.1080/13645579.2015.1123555 .
Leavy P. Method meets art: arts-based research practice. New York: Guilford Publications; 2015.
Liamputtong P. Researching the vulnerable: a guide to sensitive research methods. Thousand Oaks: Sage Publications; 2007.
Liamputtong P. Qualitative research methods. 4th ed. South Melbourne: Oxford University Press; 2013.
Mays N, Pope C. Quality in qualitative health research. In: Pope C, Mays N, editors. Qualitative research in health care. London: BMJ Books; 2000. p. 89–102.
McLellan E, MacQueen KM, Neidig JL. Beyond the qualitative interview: data preparation and transcription. Field Methods. 2003;15(1):63–84. https://doi.org/10.1177/1525822x02239573 .
Minichiello V, Aroni R, Hays T. In-depth interviewing: principles, techniques, analysis. 3rd ed. Sydney: Pearson Education Australia; 2008.
Morris ZS. The truth about interviewing elites. Politics. 2009;29(3):209–17. https://doi.org/10.1111/j.1467-9256.2009.01357.x .
Nathan S, Foster M, Ferry M. Peer and sexual relationships in the experience of drug-dependent adolescents in a therapeutic community. Drug Alcohol Rev. 2011;30(4):419–27.
National Health and Medical Research Council. National statement on ethical conduct in human research. Canberra: Australian Government; 2007.
Neal S, McLaughlin E. Researching up? Interviews, emotionality and policy-making elites. J Soc Policy. 2009;38(04):689–707. https://doi.org/10.1017/S0047279409990018 .
O’Reilly M, Parker N. ‘Unsatisfactory saturation’: a critical exploration of the notion of saturated sample sizes in qualitative research. Qual Res. 2013;13(2):190–7. https://doi.org/10.1177/1468794112446106 .
Ostrander S. “Surely you're not in this just to be helpful”: access, rapport and interviews in three studies of elites. In: Hertz R, Imber J, editors. Studying elites using qualitative methods. Thousand Oaks: Sage Publications; 1995. p. 133–50.
Chapter Google Scholar
Patton M. Qualitative research & evaluation methods: integrating theory and practice. Thousand Oaks: Sage Publications; 2015.
Punch KF. Introduction to social research: quantitative and qualitative approaches. London: Sage; 2005.
Rhodes T, Bernays S, Houmoller K. Parents who use drugs: accounting for damage and its limitation. Soc Sci Med. 2010;71(8):1489–97. https://doi.org/10.1016/j.socscimed.2010.07.028 .
Riessman CK. Narrative analysis. London: Sage; 1993.
Ritchie J. Not everything can be reduced to numbers. In: Berglund C, editor. Health research. Melbourne: Oxford University Press; 2001. p. 149–73.
Rubin H, Rubin I. Qualitative interviewing: the art of hearing data. 2nd ed. Thousand Oaks: Sage Publications; 2012.
Serry T, Liamputtong P. The in-depth interviewing method in health. In: Liamputtong P, editor. Research methods in health: foundations for evidence-based practice. 3rd ed. South Melbourne: Oxford University Press; 2017. p. 67–83.
Silverman D. Doing qualitative research. 5th ed. London: Sage; 2017.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (coreq): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Download references
Author information
Authors and affiliations.
School of Public Health and Community Medicine, Faculty of Medicine, UNSW, Sydney, NSW, Australia
Sally Nathan
Centre for Social Research in Health, Faculty of Arts and Social Sciences, UNSW, Sydney, NSW, Australia
Christy Newman & Kari Lancaster
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sally Nathan .
Editor information
Editors and affiliations.
School of Science and Health, Western Sydney University, Penrith, NSW, Australia
Pranee Liamputtong
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry.
Nathan, S., Newman, C., Lancaster, K. (2019). Qualitative Interviewing. In: Liamputtong, P. (eds) Handbook of Research Methods in Health Social Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-10-5251-4_77
Download citation
DOI : https://doi.org/10.1007/978-981-10-5251-4_77
Published : 13 January 2019
Publisher Name : Springer, Singapore
Print ISBN : 978-981-10-5250-7
Online ISBN : 978-981-10-5251-4
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Harvard Library
- Research Guides
- Faculty of Arts & Sciences Libraries
Library Support for Qualitative Research
- Interview Research
General Handbooks and Overviews
Qualitative research communities.
- Types of Interviews
- Recruiting & Engaging Participants
- Interview Questions
- Conducting Interviews
- Recording & Transcription
- Data Analysis
- Managing Interview Data
- Finding Extant Interviews
- Past Workshops on Interview Research
- Methodological Resources
- Remote & Virtual Fieldwork
- Data Management & Repositories
- Campus Access
- Interviews as a Method for Qualitative Research (video) This short video summarizes why interviews can serve as useful data in qualitative research.
- InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating to interviewing: the interview as conversation, hermeneutics, phenomenology, concerns about ethics as well as validity, and postmodernism. Having established this framework, the author then analyzes the seven stages of the interview process - from designing a study to writing it up.
- Practical Evaluation by Michael Quinn Patton Surveys different interviewing strategies, from, a) informal/conversational, to b) interview guide approach, to c) standardized and open-ended, to d) closed/quantitative. Also discusses strategies for wording questions that are open-ended, clear, sensitive, and neutral, while supporting the speaker. Provides suggestions for probing and maintaining control of the interview process, as well as suggestions for recording and transcription.
- The SAGE Handbook of Interview Research by Amir B. Marvasti (Editor); James A. Holstein (Editor); Jaber F. Gubrium (Editor); Karyn D. McKinney (Editor) The new edition of this landmark volume emphasizes the dynamic, interactional, and reflexive dimensions of the research interview. Contributors highlight the myriad dimensions of complexity that are emerging as researchers increasingly frame the interview as a communicative opportunity as much as a data-gathering format. The book begins with the history and conceptual transformations of the interview, which is followed by chapters that discuss the main components of interview practice. Taken together, the contributions to The SAGE Handbook of Interview Research: The Complexity of the Craft encourage readers simultaneously to learn the frameworks and technologies of interviewing and to reflect on the epistemological foundations of the interview craft.
- International Congress of Qualitative Inquiry They host an annual confrerence at the University of Illinois at Urbana-Champaign, which aims to facilitate the development of qualitative research methods across a wide variety of academic disciplines, among other initiatives.
- METHODSPACE An online home of the research methods community, where practicing researchers share how to make research easier.
- Social Research Association, UK The SRA is the membership organisation for social researchers in the UK and beyond. It supports researchers via training, guidance, publications, research ethics, events, branches, and careers.
- Social Science Research Council The SSRC administers fellowships and research grants that support the innovation and evaluation of new policy solutions. They convene researchers and stakeholders to share evidence-based policy solutions and incubate new research agendas, produce online knowledge platforms and technical reports that catalog research-based policy solutions, and support mentoring programs that broaden problem-solving research opportunities.
- << Previous: Taguette
- Next: Types of Interviews >>
Except where otherwise noted, this work is subject to a Creative Commons Attribution 4.0 International License , which allows anyone to share and adapt our material as long as proper attribution is given. For details and exceptions, see the Harvard Library Copyright Policy ©2021 Presidents and Fellows of Harvard College.
Root out friction in every digital experience, super-charge conversion rates, and optimise digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered straight to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Meet the operating system for experience management
- Free Account
- Product Demos
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Ultimate Guide to Market Research
- Qualitative Research Interviews
Try Qualtrics for free
How to carry out great interviews in qualitative research.
11 min read An interview is one of the most versatile methods used in qualitative research. Here’s what you need to know about conducting great qualitative interviews.
What is a qualitative research interview?
Qualitative research interviews are a mainstay among q ualitative research techniques, and have been in use for decades either as a primary data collection method or as an adjunct to a wider research process. A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom.
There are three main types of qualitative research interview – structured, unstructured or semi-structured.
- Structured interviews Structured interviews are based around a schedule of predetermined questions and talking points that the researcher has developed. At their most rigid, structured interviews may have a precise wording and question order, meaning that they can be replicated across many different interviewers and participants with relatively consistent results.
- Unstructured interviews Unstructured interviews have no predetermined format, although that doesn’t mean they’re ad hoc or unplanned. An unstructured interview may outwardly resemble a normal conversation, but the interviewer will in fact be working carefully to make sure the right topics are addressed during the interaction while putting the participant at ease with a natural manner.
- Semi-structured interviews Semi-structured interviews are the most common type of qualitative research interview, combining the informality and rapport of an unstructured interview with the consistency and replicability of a structured interview. The researcher will come prepared with questions and topics, but will not need to stick to precise wording. This blended approach can work well for in-depth interviews.
Free eBook: The qualitative research design handbook
What are the pros and cons of interviews in qualitative research?
As a qualitative research method interviewing is hard to beat, with applications in social research, market research, and even basic and clinical pharmacy. But like any aspect of the research process, it’s not without its limitations. Before choosing qualitative interviewing as your research method, it’s worth weighing up the pros and cons.
Pros of qualitative interviews:
- provide in-depth information and context
- can be used effectively when their are low numbers of participants
- provide an opportunity to discuss and explain questions
- useful for complex topics
- rich in data – in the case of in-person or video interviews , the researcher can observe body language and facial expression as well as the answers to questions
Cons of qualitative interviews:
- can be time-consuming to carry out
- costly when compared to some other research methods
- because of time and cost constraints, they often limit you to a small number of participants
- difficult to standardise your data across different researchers and participants unless the interviews are very tightly structured
- As the Open University of Hong Kong notes, qualitative interviews may take an emotional toll on interviewers
Qualitative interview guides
Semi-structured interviews are based on a qualitative interview guide, which acts as a road map for the researcher. While conducting interviews, the researcher can use the interview guide to help them stay focused on their research questions and make sure they cover all the topics they intend to.
An interview guide may include a list of questions written out in full, or it may be a set of bullet points grouped around particular topics. It can prompt the interviewer to dig deeper and ask probing questions during the interview if appropriate.
Consider writing out the project’s research question at the top of your interview guide, ahead of the interview questions. This may help you steer the interview in the right direction if it threatens to head off on a tangent.
Avoid bias in qualitative research interviews
According to Duke University , bias can create significant problems in your qualitative interview.
- Acquiescence bias is common to many qualitative methods, including focus groups. It occurs when the participant feels obliged to say what they think the researcher wants to hear. This can be especially problematic when there is a perceived power imbalance between participant and interviewer. To counteract this, Duke University’s experts recommend emphasising the participant’s expertise in the subject being discussed, and the value of their contributions.
- Interviewer bias is when the interviewer’s own feelings about the topic come to light through hand gestures, facial expressions or turns of phrase. Duke’s recommendation is to stick to scripted phrases where this is an issue, and to make sure researchers become very familiar with the interview guide or script before conducting interviews, so that they can hone their delivery.
What kinds of questions should you ask in a qualitative interview?
The interview questions you ask need to be carefully considered both before and during the data collection process. As well as considering the topics you’ll cover, you will need to think carefully about the way you ask questions.
Open-ended interview questions – which cannot be answered with a ‘yes’ ‘no’ or ‘maybe’ – are recommended by many researchers as a way to pursue in depth information.
An example of an open-ended question is “What made you want to move to the East Coast?” This will prompt the participant to consider different factors and select at least one. Having thought about it carefully, they may give you more detailed information about their reasoning.
A closed-ended question , such as “Would you recommend your neighbourhood to a friend?” can be answered without too much deliberation, and without giving much information about personal thoughts, opinions and feelings.
Follow-up questions can be used to delve deeper into the research topic and to get more detail from open-ended questions. Examples of follow-up questions include:
- What makes you say that?
- What do you mean by that?
- Can you tell me more about X?
- What did/does that mean to you?
As well as avoiding closed-ended questions, be wary of leading questions. As with other qualitative research techniques such as surveys or focus groups, these can introduce bias in your data. Leading questions presume a certain point of view shared by the interviewer and participant, and may even suggest a foregone conclusion.
An example of a leading question might be: “You moved to New York in 1990, didn’t you?” In answering the question, the participant is much more likely to agree than disagree. This may be down to acquiescence bias or a belief that the interviewer has checked the information and already knows the correct answer.
Other leading questions involve adjectival phrases or other wording that introduces negative or positive connotations about a particular topic. An example of this kind of leading question is: “Many employees dislike wearing masks to work. How do you feel about this?” It presumes a positive opinion and the participant may be swayed by it, or not want to contradict the interviewer.
Harvard University’s guidelines for qualitative interview research add that you shouldn’t be afraid to ask embarrassing questions – “if you don’t ask, they won’t tell.” Bear in mind though that too much probing around sensitive topics may cause the interview participant to withdraw. The Harvard guidelines recommend leaving sensitive questions til the later stages of the interview when a rapport has been established.
More tips for conducting qualitative interviews
Observing a participant’s body language can give you important data about their thoughts and feelings. It can also help you decide when to broach a topic, and whether to use a follow-up question or return to the subject later in the interview.
Be conscious that the participant may regard you as the expert, not themselves. In order to make sure they express their opinions openly, use active listening skills like verbal encouragement and paraphrasing and clarifying their meaning to show how much you value what they are saying.
Remember that part of the goal is to leave the interview participant feeling good about volunteering their time and their thought process to your research. Aim to make them feel empowered , respected and heard.
Unstructured interviews can demand a lot of a researcher, both cognitively and emotionally. Be sure to leave time in between in-depth interviews when scheduling your data collection to make sure you maintain the quality of your data, as well as your own well-being .
Recording and transcribing interviews
Historically, recording qualitative research interviews and then transcribing the conversation manually would have represented a significant part of the cost and time involved in research projects that collect qualitative data.
Fortunately, researchers now have access to digital recording tools, and even speech-to-text technology that can automatically transcribe interview data using AI and machine learning. This type of tool can also be used to capture qualitative data from qualitative research (focus groups,ect.) making this kind of social research or market research much less time consuming.
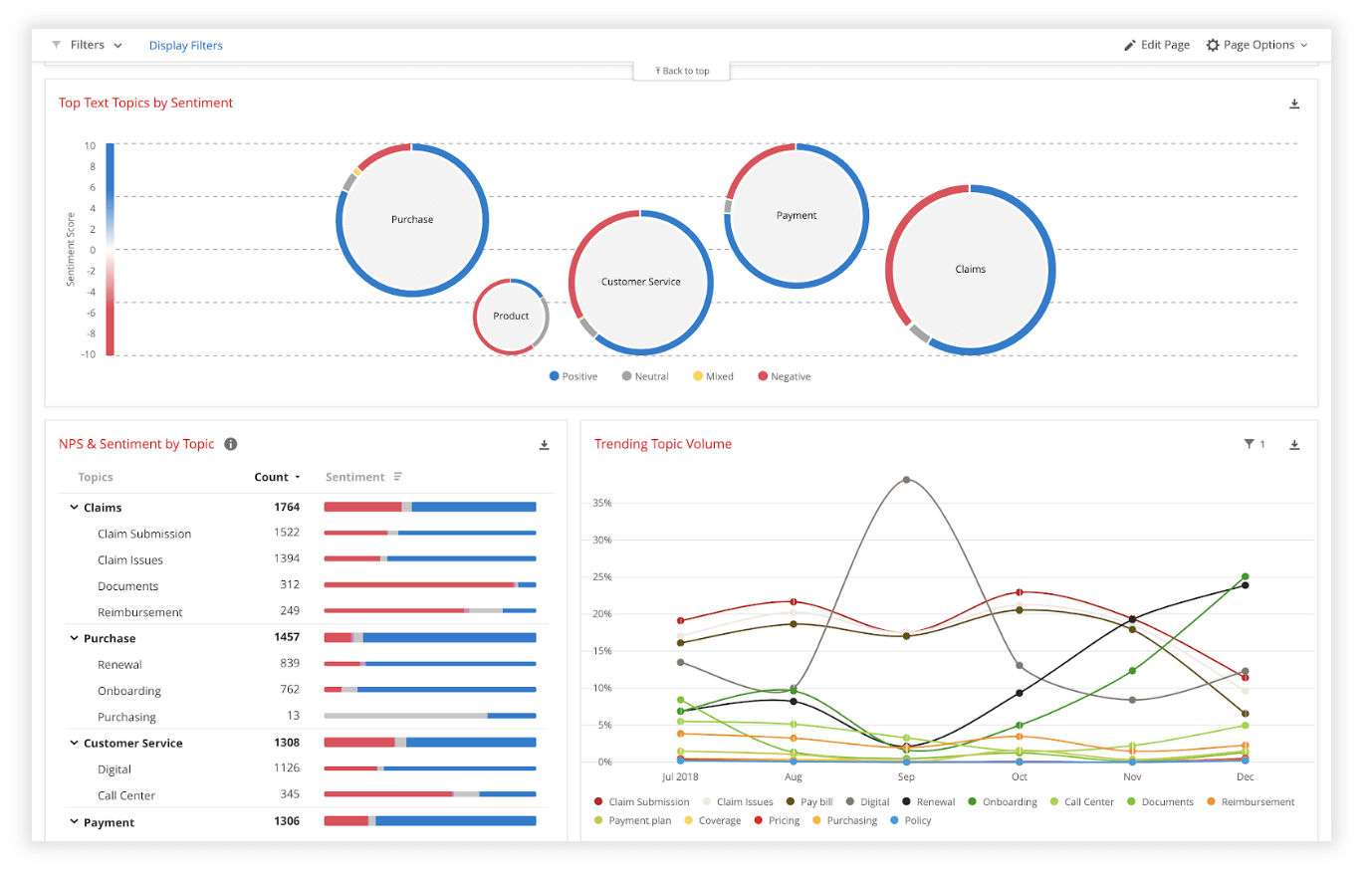
Data analysis
Qualitative interview data is unstructured, rich in content and difficult to analyse without the appropriate tools. Fortunately, machine learning and AI can once again make things faster and easier when you use qualitative methods like the research interview.
Text analysis tools and natural language processing software can ‘read’ your transcripts and voice data and identify patterns and trends across large volumes of text or speech. They can also perform khttps://www.qualtrics.com/experience-management/research/sentiment-analysis/
which assesses overall trends in opinion and provides an unbiased overall summary of how participants are feeling.
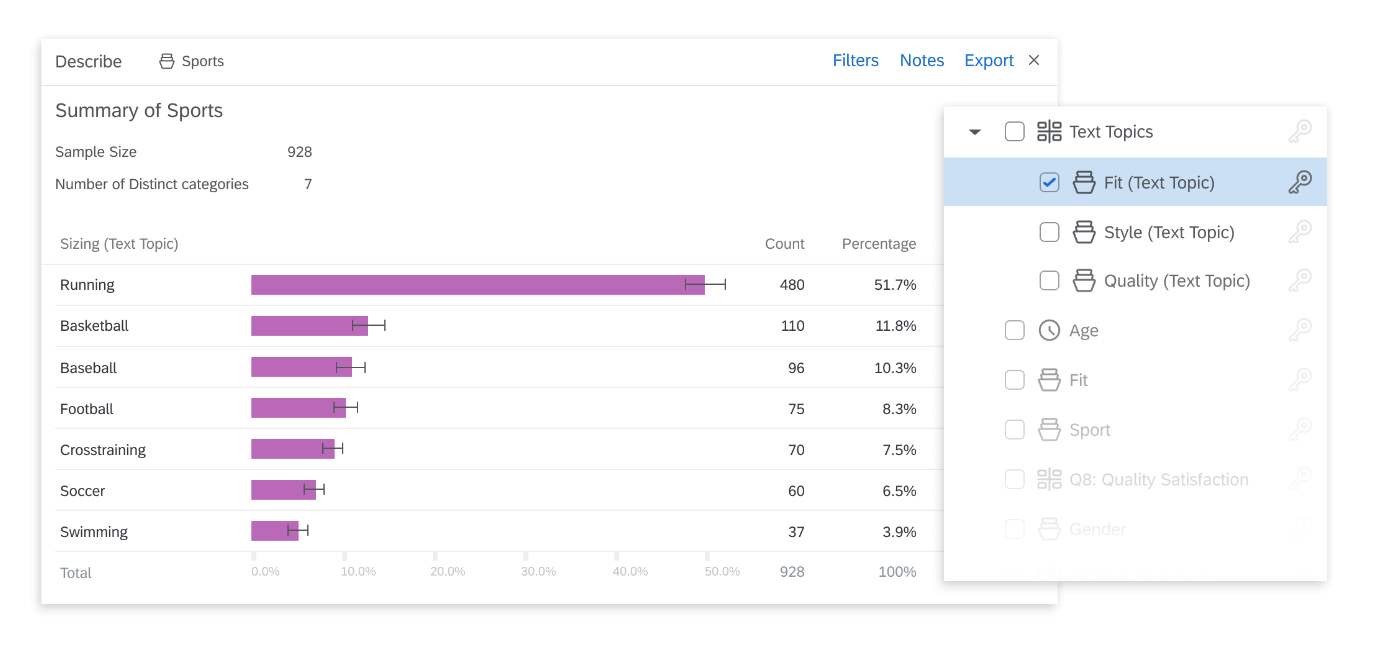
Another feature of text analysis tools is their ability to categorise information by topic, sorting it into groupings that help you organise your data according to the topic discussed.
All in all, interviews are a valuable technique for qualitative research in business, yielding rich and detailed unstructured data. Historically, they have only been limited by the human capacity to interpret and communicate results and conclusions, which demands considerable time and skill.
When you combine this data with AI tools that can interpret it quickly and automatically, it becomes easy to analyse and structure, dovetailing perfectly with your other business data. An additional benefit of natural language analysis tools is that they are free of subjective biases, and can replicate the same approach across as much data as you choose. By combining human research skills with machine analysis, qualitative research methods such as interviews are more valuable than ever to your business.
Related resources
Video in qualitative research 10 min read, descriptive research 8 min read, market intelligence 9 min read, qualitative research questions 11 min read, ethnographic research 11 min read, business research methods 12 min read, qualitative research design 12 min read, request demo.
Ready to learn more about Qualtrics?

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Chapter 13: Interviews
Danielle Berkovic
Learning outcomes
Upon completion of this chapter, you should be able to:
- Understand when to use interviews in qualitative research.
- Develop interview questions for an interview guide.
- Understand how to conduct an interview.
What are interviews?
An interviewing method is the most commonly used data collection technique in qualitative research. 1 The purpose of an interview is to explore the experiences, understandings, opinions and motivations of research participants. 2 Interviews are conducted one-on-one with the researcher and the participant. Interviews are most appropriate when seeking to understand a participant’s subjective view of an experience and are also considered suitable for the exploration of sensitive topics.
What are the different types of interviews?
There are four main types of interviews:
- Key stakeholder: A key stakeholder interview aims to explore one issue in detail with a person of interest or importance concerning the research topic. 3 Key stakeholder interviews seek the views of experts on some cultural, political or health aspects of the community, beyond their personal beliefs or actions. An example of a key stakeholder is the Chief Health Officer of Victoria (Australia’s second-most populous state) who oversaw the world’s longest lockdowns in response to the COVID-19 pandemic.
- Dyad: A dyad interview aims to explore one issue in a level of detail with a dyad (two people). This form of interviewing is used when one participant of the dyad may need some support or is not wholly able to articulate themselves (e.g. people with cognitive impairment, or children). Independence is acknowledged and the interview is analysed as a unit. 4
- Narrative: A narrative interview helps individuals tell their stories, and prioritises their own perspectives and experiences using the language that they prefer. 5 This type of interview has been widely used in social research but is gaining prominence in health research to better understand person-centred care, for example, negotiating exercise and food abstinence whilst living with Type 2 diabetes. 6,7
- Life history: A life history interview allows the researcher to explore a person’s individual and subjective experiences within a history of the time framework. 8 Life history interviews challenge the researcher to understand how people’s current attitudes, behaviours and choices are influenced by previous experiences or trauma. Life history interviews have been conducted with Holocaust survivors 9 and youth who have been forcibly recruited to war. 10
Table 13.4 provides a summary of four studies, each adopting one of these types of interviews.
Interviewing techniques
There are two main interview techniques:
- Semi-structured: Semi-structured interviewing aims to explore a few issues in moderate detail, to expand the researcher’s knowledge at some level. 11 Semi-structured interviews give the researcher the advantage of remaining reasonably objective while enabling participants to share their perspectives and opinions. The researcher should create an interview guide with targeted open questions to direct the interview. As examples, semi-structured interviews have been used to extend knowledge of why women might gain excess weight during pregnancy, 12 and to update guidelines for statin uptake. 13
- In-depth: In-depth interviewing aims to explore a person’s subjective experiences and feelings about a particular topic. 14 In-depth interviews are often used to explore emotive (e.g. end-of-life care) 15 and complex (e.g. adolescent pregnancy) topics. 16 The researcher should create an interview guide with selected open questions to ask of the participant, but the participant should guide the direction of the interview more than in a semi-structured setting. In-depth interviews value participants’ lived experiences and are frequently used in phenomenology studies (as described in Chapter 6) .
When to use the different types of interview s
The type of interview a researcher uses should be determined by the study design, the research aims and objectives, and participant demographics. For example, if conducting a descriptive study, semi-structured interviews may be the best method of data collection. As explained in Chapter 5 , descriptive studies seek to describe phenomena, rather than to explain or interpret the data. A semi-structured interview, which seeks to expand upon some level of existing knowledge, will likely best facilitate this.
Similarly, if conducting a phenomenological study, in-depth interviews may be the best method of data collection. As described in Chapter 6 , the key concept of phenomenology is the individual. The emphasis is on the lived experience of that individual and the person’s sense-making of those experiences. Therefore, an in-depth interview is likely best placed to elicit that rich data.
While some interview types are better suited to certain study designs, there are no restrictions on the type of interview that may be used. For example, semi-structured interviews provide an excellent accompaniment to trial participation (see Chapter 11 about mixed methods), and key stakeholder interviews, as part of an action research study, can be used to define priorities, barriers and enablers to implementation.
How do I write my interview questions?
An interview aims to explore the experiences, understandings, opinions and motivations of research participants. The general rule is that the interviewee should speak for 80 per cent of the interview, and the interviewer should only be asking questions and clarifying responses, for about 20 per cent of the interview. This percentage may differ depending on the interview type; for example, a semi-structured interview involves the researcher asking more questions than in an in-depth interview. Still, to facilitate free-flowing responses, it is important to use open-ended language to encourage participants to be expansive in their responses. Examples of open-ended terms include questions that start with ‘who’, ‘how’ and ‘where’.
The researcher should avoid closed-ended questions that can be answered with yes or no, and limit conversation. For example, asking a participant ‘Did you have this experience?’ can elicit a simple ‘yes’, whereas asking them to ‘Describe your experience’, will likely encourage a narrative response. Table 13.1 provides examples of terminology to include and avoid in developing interview questions.
Table 13.1. Interview question formats to use and avoid
| Use | Avoid |
|---|---|
| Tell me about… | Do you think that… |
| What happened when… | Will you do this… |
| Why is this important? | Did you believe that… |
| How did you feel when…How do you… | Were there issues from your perspective… |
| What are the…What does... |
How long should my interview be?
There is no rule about how long an interview should take. Different types of interviews will likely run for different periods of time, but this also depends on the research question/s and the type of participant. For example, given that a semi-structured interview is seeking to expand on some previous knowledge, the interview may need no longer than 30 minutes, or up to one hour. An in-depth interview seeks to explore a topic in a greater level of detail and therefore, at a minimum, would be expected to last an hour. A dyad interview may be as short as 15 minutes (e.g. if the dyad is a person with dementia and a family member or caregiver) or longer, depending on the pairing.
Designing your interview guide
To figure out what questions to ask in an interview guide, the researcher may consult the literature, speak to experts (including people with lived experience) about the research and draw on their current knowledge. The topics and questions should be mapped to the research question/s, and the interview guide should be developed well in advance of commencing data collection. This enables time and opportunity to pilot-test the interview guide. The pilot interview provides an opportunity to explore the language and clarity of questions, the order and flow of the guide and to determine whether the instructions are clear to participants both before and after the interview. It can be beneficial to pilot-test the interview guide with someone who is not familiar with the research topic, to make sure that the language used is easily understood (and will be by participants, too). The study design should be used to determine the number of questions asked and the duration of the interview should guide the extent of the interview guide. The participant type may also determine the extent of the interview guide; for example, clinicians tend to be time-poor and therefore shorter, focused interviews are optimal. An interview guide is also likely to be shorter for a descriptive study than a phenomenological or ethnographic study, given the level of detail required. Chapter 5 outlined a descriptive study in which participants who had undergone percutaneous coronary intervention were interviewed. The interview guide consisted of four main questions and subsequent probing questions, linked to the research questions (see Table 13.2). 17
Table 13.2. Interview guide for a descriptive study
| Research question | Open questions | Probing questions and topics |
|---|---|---|
| How does the patient feel, physically and psychologically, after their procedure? | From your perspective, what would be considered a successful outcome of the procedure? | Did the procedure meet your expectations? How do you define whether the procedure was successful? |
| How did you feel after the procedure?
| How did you feel one week after the procedure and how does that compare with how you feel now? | |
| How does the patient function after their procedure? | After your procedure, tell me about your ability to do your daily activities? | Prompt for activities including gardening, housework, personal care, work-related and family-related tasks.Did you attend cardiac rehabilitation? Can you tell us about your experience of cardiac rehabilitation? What effect has medication had on your recovery?
|
| What are the long-term effects of the procedure? | What, if any, lifestyle changes have you made since your procedure? |
Table 13.3 is an example of a larger and more detailed interview guide, designed for the qualitative component of a mixed-methods study aiming to examine the work and financial effects of living with arthritis as a younger person. The questions are mapped to the World Health Organization’s International Classification of Functioning, Disability, and Health, which measures health and disability at individual and population levels. 18
Table 13.3. Detailed interview guide
| Research questions | Open questions | Probing questions |
|---|---|---|
| How do young people experience their arthritis diagnosis? | Tell me about your experience of being diagnosed with arthritis.How did being diagnosed with arthritis make you feel?Tell me about your experience of arthritis flare ups what do they feel like?What impacts arthritis flare ups or feeling like your arthritis is worse?What circumstances lead to these feelings?Based on your experience, what do you think causes symptoms of arthritis to become worse? | When were you diagnosed with arthritis?What type of arthritis were you diagnosed with?Does anyone else in your family have arthritis? What relation are they to you? |
| What are the work impacts of arthritis on younger people? | What is your field of work, and how long have you been in this role?How frequently do you work (full-time/part-time/casual)? | How has arthritis affected your work-related demands or career? How so?Has arthritis led you to reconsider your career? How so?Has arthritis affected your usual working hours each week? How so?How have changes to work or career because of your arthritis impacted other areas of life, i.e. mental health or family role? |
| What are the financial impacts of living with arthritis as a younger person? | Has your arthritis led to any financial concerns? | Financial concerns pertaining to:• Direct costs: rheumatologist, prescribed and non-prescribed medications (as well as supplements), allied health costs (rheumatology, physiotherapy, chiropractic, osteopathy, myotherapy), Pilates, and gym/personal trainer fees, complementary therapies.• Indirect costs: workplace absenteeism, productivity, loss of wages, informal care, cost of different types of insurance: health insurance (joint replacements) |
It is important to create an interview guide, for the following reasons:
- The researcher should be familiar with their research questions.
- Using an interview guide will enable the incorporation of feedback from the piloting process.
- It is difficult to predict how participants will respond to interview questions. They may answer in a way that is anticipated or they may provide unanticipated insights that warrant follow-up. An interview guide (a physical or digital copy) enables the researcher to note these answers and follow-up with appropriate inquiry.
- Participants will likely have provided heterogeneous answers to certain questions. The interview guide enables the researcher to note similarities and differences across various interviews, which may be important in data analysis.
- Even experienced qualitative researchers get nervous before an interview! The interview guide provides a safety net if the researcher forgets their questions or needs to anticipate the next question.
Setting up the interview
In the past, most interviews were conducted in person or by telephone. Emerging technologies promote easier access to research participation (e.g. by people living in rural or remote communities, or for people with mobility limitations). Even in metropolitan settings, many interviews are now conducted electronically (e.g. using videoconferencing platforms). Regardless of your interview setting, it is essential that the interview environment is comfortable for the participant. This process can begin as soon as potential participants express interest in your research. Following are some tips from the literature and our own experiences of leading interviews:
- Answer questions and set clear expectations . Participating in research is not an everyday task. People do not necessarily know what to expect during a research interview, and this can be daunting. Give people as much information as possible, answer their questions about the research and set clear expectations about what the interview will entail and how long it is expected to last. Let them know that the interview will be recorded for transcription and analysis purposes. Consider sending the interview questions a few days before the interview. This gives people time and space to reflect on their experiences, consider their responses to questions and to provide informed consent for their participation.
- Consider your setting . If conducting the interview in person, consider the location and room in which the interview will be held. For example, if in a participant’s home, be mindful of their private space. Ask if you should remove your shoes before entering their home. If they offer refreshments (which in our experience many participants do), accept it with gratitude if possible. These considerations apply beyond the participant’s home; if using a room in an office setting, consider privacy and confidentiality, accessibility and potential for disruption. Consider the temperature as well as the furniture in the room, who may be able to overhear conversations and who may walk past. Similarly, if interviewing by phone or online, take time to assess the space, and if in a house or office that is not quiet or private, use headphones as needed.
- Build rapport. The research topic may be important to participants from a professional perspective, or they may have deep emotional connections to the topic of interest. Regardless of the nature of the interview, it is important to remember that participants are being asked to open up to an interviewer who is likely to be a stranger. Spend some time with participants before the interview, to make sure that they are comfortable. Engage in some general conversation, and ask if they have any questions before you start. Remember that it is not a normal part of someone’s day to participate in research. Make it an enjoyable and/or meaningful experience for them, and it will enhance the data that you collect.
- Let participants guide you. Oftentimes, the ways in which researchers and participants describe the same phenomena are different. In the interview, reflect the participant’s language. Make sure they feel heard and that they are willing and comfortable to speak openly about their experiences. For example, our research involves talking to older adults about their experience of falls. We noticed early in this research that participants did not use the word ‘fall’ but would rather use terms such as ‘trip’, ‘went over’ and ‘stumbled’. As interviewers we adopted the participant’s language into our questions.
- Listen consistently and express interest. An interview is more complex than a simple question-and-answer format. The best interview data comes from participants feeling comfortable and confident to share their stories. By the time you are completing the 20th interview, it can be difficult to maintain the same level of concentration as with the first interview. Try to stay engaged: nod along with your participants, maintain eye contact, murmur in agreement and sympathise where warranted.
- The interviewer is both the data collector and the data collection instrument. The data received is only as good as the questions asked. In qualitative research, the researcher influences how participants answer questions. It is important to remain reflexive and aware of how your language, body language and attitude might influence the interview. Being rested and prepared will enhance the quality of the questions asked and hence the data collected.
- Avoid excessive use of ‘why’. It can be challenging for participants to recall why they felt a certain way or acted in a particular manner. Try to avoid asking ‘why’ questions too often, and instead adopt some of the open language described earlier in the chapter.
After your interview
When you have completed your interview, thank the participant and let them know they can contact you if they have any questions or follow-up information they would like to provide. If the interview has covered sensitive topics or the participant has become distressed throughout the interview, make sure that appropriate referrals and follow-up are provided (see section 6).
Download the recording from your device and make sure it is saved in a secure location that can only be accessed by people on the approved research team (see Chapters 35 and 36).
It is important to know what to do immediately after each interview is completed. Interviews should be transcribed – that is, reproduced verbatim for data analysis. Transcribing data is an important step in the process of analysis, but it is very time-consuming; transcribing a 60-minute interview can take up to 8 hours. Data analysis is discussed in Section 4.
Table 13.4. Examples of the four types of interviews
| Title | ||||
|---|---|---|---|---|
| CC Licence | ||||
| First author and year | Cuthbertson, 2019 | Bannon, 2021 | McGranahan, 2020 | Gutierrez-Garcia, 2021 |
| Interview type | Key stakeholder | Dyad | Narrative | Life history |
| Interview guide | Appendix A | eAppendix Supplement | Not provided, but the text states that ‘qualitative semi-structured narrative interviews’ were conducted.’ [methods] | Not provided, but the text states that ‘an open and semi-structured question guide was designed for use.' [methods] |
| Study design | Convergent mixed-methods study | Qualitative dyadic study | Narrative interview study | Life history and lifeline techniques |
| Number of participants | 30Key stakeholders were emergency management or disaster healthcare practitioners, academics specialising in disaster management in the Oceania region, and policy managers. | 23 dyads | 28 | 7 |
| Aim | ‘To investigate threats to the health and well-being of societies associated with disaster impact in Oceania.’ [abstract] | ‘To explore the lived experiences of couples managing young-onset dementia using an integrated dyadic coping model.’[abstract] | ‘To explore the experiences and views of people with psychotic experiences who have not received any treatment or other support from mental health services for the past 5 years.’ [abstract] | ‘To analyse the use of life histories and lifelines in the study of female genital mutilation in the context of cross-cultural research in participants with different languages.’ [abstract] |
| Country | Australia, Fiji, Indonesia, Aotearoa New Zealand, Timor Leste and Tonga | United States | England | Spain |
| Length of interview | 45–60 minutes | 60 minutes | 40-120 minutes | 3 sessionsSession 1: life history interviewSession 2: Lifeline activity where participants used drawings to complement or enhance their interviewSession 3: The researchers and participants worked together to finalise the lifeline. The life history interviews ran for 40 – 60 minutes. The timing for sessions 2 and 3 is not provided. |
| Sample of interview questions from interview guide | 1. What do you believe are the top five disaster risks or threats in the Oceania region today?2. What disaster risks do you believe are emerging in the Oceania region over the next decade?3. Why do you think these are risks?4. What are the drivers of these risks?5. Do you have any suggestions on how we can improve disaster risk assessment?6. Are the current disaster risk plans and practices suited to the future disaster risks? If not, why? If not, what do you think needs to be done to improve them?7. What are the key areas of disaster practice that can enhance future community resilience to disaster risk?8. What are the barriers or inhibitors to facilitating this practice?9. What are the solutions or facilitators to enhancing community resilience?[Appendix A]
| 1. We like to start by learning more about what you each first noticed that prompted the evaluations you went through to get to the diagnosis.• Can you each tell me about the earliest symptoms you noticed?2. What are the most noticeable or troubling symptoms that you have experienced since the time of diagnosis?• How have your changes in functioning impacted you?• Emotionally, how do you feel about your symptoms and the changes in functioning you are experiencing?3. Are you open with your friends and family about the diagnosis?• Have you experienced any stigma related to your diagnosis?4. What is your understanding of the diagnosis?• What is your understanding about the how this condition will affect you both in the future? How are you getting information about this diagnosis?[eAppendix Supplement]
| Not provided. | Not provided. |
| Analysis | Thematic analysis guided by The Hazard and Peril Glossary for describing and categorising disasters applied by the Centre for Research on the Epidemiology of Disasters Emergency Events Database | Thematic analysis guided by the Dyadic Coping Theoretical Framework | Inductive thematic analysis outlined by Braun and Clarke. | Phenomenological method proposed by Giorgi (sense of the whole):1. Reading the entire description to obtain a general sense of the discourse2. The researcher goes back to the beginning and reads the text again, with the aim of distinguishing the meaning units by separating the perspective of the phenomenon of interest3. The researcher expresses the contents of the units of meaning more clearly by creating categories4. The researcher synthesises the units and categories of meaning into a consistent statement that takes into account the participant’s experience and language. |
| Main themes | 1. Climate change is observed as a contemporary and emerging disaster risk2. Risk is contextual to the different countries, communities and individuals in Oceania.3. Human development trajectories and their impact, along with perceptions of a changing world, are viewed as drivers of current and emerging risks.4. Current disaster risk plans and practices are not suited to future disaster risks.5. Increased education and education of risk and risk assessment at a local level to empower community risk ownership.[Results, Box 1] | 1. Stress communication2. Positive individual dyadic coping3. Positive conjoint dyadic coping4. Negative individual dyadic coping5. Negative conjoint dyadic coping[Abstract] | 1. Perceiving psychosis as positive2. Making sense of psychotic experiences3. Finding sources of strength4. Negative past experiences of mental health services5. Positive past experiences with individual clinicians[Abstract] | 1. Important moments and their relationship with female genital mutilation2. The ritual knife: how sharp or blunt it is at different stages, where and how women are subsequently held as a result3. Changing relationships with family: how being subject to female genital mutilation changed relationships with mothers4. Female genital mutilation increases the risk of future childbirth complications which change relationships with family and healthcare systems5. Managing experiences with early exposure to physical and sexual violence across the lifespan. |
Interviews are the most common data collection technique in qualitative research. There are four main types of interviews; the one you choose will depend on your research question, aims and objectives. It is important to formulate open-ended interview questions that are understandable and easy for participants to answer. Key considerations in setting up the interview will enhance the quality of the data obtained and the experience of the interview for the participant and the researcher.
- Gill P, Stewart K, Treasure E, Chadwick B. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J . 2008;204(6):291-295. doi:10.1038/bdj.2008.192
- DeJonckheere M, Vaughn LM. Semistructured interviewing in primary care research: a balance of relationship and rigour. Fam Med Community Health . 2019;7(2):e000057. doi:10.1136/fmch-2018-000057
- Nyanchoka L, Tudur-Smith C, Porcher R, Hren D. Key stakeholders’ perspectives and experiences with defining, identifying and displaying gaps in health research: a qualitative study. BMJ Open . 2020;10(11):e039932. doi:10.1136/bmjopen-2020-039932
- Morgan DL, Ataie J, Carder P, Hoffman K. Introducing dyadic interviews as a method for collecting qualitative data. Qual Health Res . 2013;23(9):1276-84. doi:10.1177/1049732313501889
- Picchi S, Bonapitacola C, Borghi E, et al. The narrative interview in therapeutic education. The diabetic patients’ point of view. Acta Biomed . Jul 18 2018;89(6-S):43-50. doi:10.23750/abm.v89i6-S.7488
- Stuij M, Elling A, Abma T. Negotiating exercise as medicine: Narratives from people with type 2 diabetes. Health (London) . 2021;25(1):86-102. doi:10.1177/1363459319851545
- Buchmann M, Wermeling M, Lucius-Hoene G, Himmel W. Experiences of food abstinence in patients with type 2 diabetes: a qualitative study. BMJ Open . 2016;6(1):e008907. doi:10.1136/bmjopen-2015-008907
- Jessee E. The Life History Interview. Handbook of Research Methods in Health Social Sciences . 2018:1-17:Chapter 80-1.
- Sheftel A, Zembrzycki S. Only Human: A Reflection on the Ethical and Methodological Challenges of Working with “Difficult” Stories. The Oral History Review . 2019;37(2):191-214. doi:10.1093/ohr/ohq050
- Harnisch H, Montgomery E. “What kept me going”: A qualitative study of avoidant responses to war-related adversity and perpetration of violence by former forcibly recruited children and youth in the Acholi region of northern Uganda. Soc Sci Med . 2017;188:100-108. doi:10.1016/j.socscimed.2017.07.007
- Ruslin., Mashuri S, Rasak MSA, Alhabsyi M, Alhabsyi F, Syam H. Semi-structured Interview: A Methodological Reflection on the Development of a Qualitative Research Instrument in Educational Studies. IOSR-JRME . 2022;12(1):22-29. doi:10.9790/7388-1201052229
- Chang T, Llanes M, Gold KJ, Fetters MD. Perspectives about and approaches to weight gain in pregnancy: a qualitative study of physicians and nurse midwives. BMC Pregnancy & Childbirth . 2013;13(47)doi:10.1186/1471-2393-13-47
- DeJonckheere M, Robinson CH, Evans L, et al. Designing for Clinical Change: Creating an Intervention to Implement New Statin Guidelines in a Primary Care Clinic. JMIR Hum Factors . 2018;5(2):e19. doi:10.2196/humanfactors.9030
- Knott E, Rao AH, Summers K, Teeger C. Interviews in the social sciences. Nature Reviews Methods Primers . 2022;2(1)doi:10.1038/s43586-022-00150-6
- Bergenholtz H, Missel M, Timm H. Talking about death and dying in a hospital setting – a qualitative study of the wishes for end-of-life conversations from the perspective of patients and spouses. BMC Palliat Care . 2020;19(1):168. doi:10.1186/s12904-020-00675-1
- Olorunsaiye CZ, Degge HM, Ubanyi TO, Achema TA, Yaya S. “It’s like being involved in a car crash”: teen pregnancy narratives of adolescents and young adults in Jos, Nigeria. Int Health . 2022;14(6):562-571. doi:10.1093/inthealth/ihab069
- Ayton DR, Barker AL, Peeters G, et al. Exploring patient-reported outcomes following percutaneous coronary intervention: A qualitative study. Health Expect . 2018;21(2):457-465. doi:10.1111/hex.12636
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). WHO. https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health#:~:text=ICF%20is%20the%20WHO%20framework,and%20measure%20health%20and%20disability.
- Cuthbertson J, Rodriguez-Llanes JM, Robertson A, Archer F. Current and Emerging Disaster Risks Perceptions in Oceania: Key Stakeholders Recommendations for Disaster Management and Resilience Building. Int J Environ Res Public Health . 2019;16(3)doi:10.3390/ijerph16030460
- Bannon SM, Grunberg VA, Reichman M, et al. Thematic Analysis of Dyadic Coping in Couples With Young-Onset Dementia. JAMA Netw Open . 2021;4(4):e216111. doi:10.1001/jamanetworkopen.2021.6111
- McGranahan R, Jakaite Z, Edwards A, Rennick-Egglestone S, Slade M, Priebe S. Living with Psychosis without Mental Health Services: A Narrative Interview Study. BMJ Open . 2021;11(7):e045661. doi:10.1136/bmjopen-2020-045661
- Gutiérrez-García AI, Solano-Ruíz C, Siles-González J, Perpiñá-Galvañ J. Life Histories and Lifelines: A Methodological Symbiosis for the Study of Female Genital Mutilation. Int J Qual Methods . 2021;20doi:10.1177/16094069211040969
Qualitative Research – a practical guide for health and social care researchers and practitioners Copyright © 2023 by Danielle Berkovic is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Types of Interviews in Research | Guide & Examples
Types of Interviews in Research | Guide & Examples
Published on March 10, 2022 by Tegan George . Revised on June 22, 2023.
An interview is a qualitative research method that relies on asking questions in order to collect data . Interviews involve two or more people, one of whom is the interviewer asking the questions.
There are several types of interviews, often differentiated by their level of structure.
- Structured interviews have predetermined questions asked in a predetermined order.
- Unstructured interviews are more free-flowing.
- Semi-structured interviews fall in between.
Interviews are commonly used in market research, social science, and ethnographic research .
Table of contents
What is a structured interview, what is a semi-structured interview, what is an unstructured interview, what is a focus group, examples of interview questions, advantages and disadvantages of interviews, other interesting articles, frequently asked questions about types of interviews.
Structured interviews have predetermined questions in a set order. They are often closed-ended, featuring dichotomous (yes/no) or multiple-choice questions. While open-ended structured interviews exist, they are much less common. The types of questions asked make structured interviews a predominantly quantitative tool.
Asking set questions in a set order can help you see patterns among responses, and it allows you to easily compare responses between participants while keeping other factors constant. This can mitigate research biases and lead to higher reliability and validity. However, structured interviews can be overly formal, as well as limited in scope and flexibility.
- You feel very comfortable with your topic. This will help you formulate your questions most effectively.
- You have limited time or resources. Structured interviews are a bit more straightforward to analyze because of their closed-ended nature, and can be a doable undertaking for an individual.
- Your research question depends on holding environmental conditions between participants constant.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Semi-structured interviews are a blend of structured and unstructured interviews. While the interviewer has a general plan for what they want to ask, the questions do not have to follow a particular phrasing or order.
Semi-structured interviews are often open-ended, allowing for flexibility, but follow a predetermined thematic framework, giving a sense of order. For this reason, they are often considered “the best of both worlds.”
However, if the questions differ substantially between participants, it can be challenging to look for patterns, lessening the generalizability and validity of your results.
- You have prior interview experience. It’s easier than you think to accidentally ask a leading question when coming up with questions on the fly. Overall, spontaneous questions are much more difficult than they may seem.
- Your research question is exploratory in nature. The answers you receive can help guide your future research.
An unstructured interview is the most flexible type of interview. The questions and the order in which they are asked are not set. Instead, the interview can proceed more spontaneously, based on the participant’s previous answers.
Unstructured interviews are by definition open-ended. This flexibility can help you gather detailed information on your topic, while still allowing you to observe patterns between participants.
However, so much flexibility means that they can be very challenging to conduct properly. You must be very careful not to ask leading questions, as biased responses can lead to lower reliability or even invalidate your research.
- You have a solid background in your research topic and have conducted interviews before.
- Your research question is exploratory in nature, and you are seeking descriptive data that will deepen and contextualize your initial hypotheses.
- Your research necessitates forming a deeper connection with your participants, encouraging them to feel comfortable revealing their true opinions and emotions.
A focus group brings together a group of participants to answer questions on a topic of interest in a moderated setting. Focus groups are qualitative in nature and often study the group’s dynamic and body language in addition to their answers. Responses can guide future research on consumer products and services, human behavior, or controversial topics.
Focus groups can provide more nuanced and unfiltered feedback than individual interviews and are easier to organize than experiments or large surveys . However, their small size leads to low external validity and the temptation as a researcher to “cherry-pick” responses that fit your hypotheses.
- Your research focuses on the dynamics of group discussion or real-time responses to your topic.
- Your questions are complex and rooted in feelings, opinions, and perceptions that cannot be answered with a “yes” or “no.”
- Your topic is exploratory in nature, and you are seeking information that will help you uncover new questions or future research ideas.
Prevent plagiarism. Run a free check.
Depending on the type of interview you are conducting, your questions will differ in style, phrasing, and intention. Structured interview questions are set and precise, while the other types of interviews allow for more open-endedness and flexibility.
Here are some examples.
- Semi-structured
- Unstructured
- Focus group
- Do you like dogs? Yes/No
- Do you associate dogs with feeling: happy; somewhat happy; neutral; somewhat unhappy; unhappy
- If yes, name one attribute of dogs that you like.
- If no, name one attribute of dogs that you don’t like.
- What feelings do dogs bring out in you?
- When you think more deeply about this, what experiences would you say your feelings are rooted in?
Interviews are a great research tool. They allow you to gather rich information and draw more detailed conclusions than other research methods, taking into consideration nonverbal cues, off-the-cuff reactions, and emotional responses.
However, they can also be time-consuming and deceptively challenging to conduct properly. Smaller sample sizes can cause their validity and reliability to suffer, and there is an inherent risk of interviewer effect arising from accidentally leading questions.
Here are some advantages and disadvantages of each type of interview that can help you decide if you’d like to utilize this research method.
| Type of interview | Advantages | Disadvantages |
|---|---|---|
| Structured interview | ||
| Semi-structured interview | , , , and | |
| Unstructured interview | , , , and | |
| Focus group | , , and , since there are multiple people present |
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Student’s t -distribution
- Normal distribution
- Null and Alternative Hypotheses
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Data cleansing
- Reproducibility vs Replicability
- Peer review
- Prospective cohort study
Research bias
- Implicit bias
- Cognitive bias
- Placebo effect
- Hawthorne effect
- Hindsight bias
- Affect heuristic
- Social desirability bias
The four most common types of interviews are:
- Structured interviews : The questions are predetermined in both topic and order.
- Semi-structured interviews : A few questions are predetermined, but other questions aren’t planned.
- Unstructured interviews : None of the questions are predetermined.
- Focus group interviews : The questions are presented to a group instead of one individual.
The interviewer effect is a type of bias that emerges when a characteristic of an interviewer (race, age, gender identity, etc.) influences the responses given by the interviewee.
There is a risk of an interviewer effect in all types of interviews , but it can be mitigated by writing really high-quality interview questions.
Social desirability bias is the tendency for interview participants to give responses that will be viewed favorably by the interviewer or other participants. It occurs in all types of interviews and surveys , but is most common in semi-structured interviews , unstructured interviews , and focus groups .
Social desirability bias can be mitigated by ensuring participants feel at ease and comfortable sharing their views. Make sure to pay attention to your own body language and any physical or verbal cues, such as nodding or widening your eyes.
This type of bias can also occur in observations if the participants know they’re being observed. They might alter their behavior accordingly.
A focus group is a research method that brings together a small group of people to answer questions in a moderated setting. The group is chosen due to predefined demographic traits, and the questions are designed to shed light on a topic of interest. It is one of 4 types of interviews .
Quantitative research deals with numbers and statistics, while qualitative research deals with words and meanings.
Quantitative methods allow you to systematically measure variables and test hypotheses . Qualitative methods allow you to explore concepts and experiences in more detail.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
George, T. (2023, June 22). Types of Interviews in Research | Guide & Examples. Scribbr. Retrieved September 2, 2024, from https://www.scribbr.com/methodology/interviews-research/
Is this article helpful?
Tegan George
Other students also liked, unstructured interview | definition, guide & examples, structured interview | definition, guide & examples, semi-structured interview | definition, guide & examples, get unlimited documents corrected.
✔ Free APA citation check included ✔ Unlimited document corrections ✔ Specialized in correcting academic texts

Qualitative Research 101: Interviewing
5 Common Mistakes To Avoid When Undertaking Interviews
By: David Phair (PhD) and Kerryn Warren (PhD) | March 2022
Undertaking interviews is potentially the most important step in the qualitative research process. If you don’t collect useful, useable data in your interviews, you’ll struggle through the rest of your dissertation or thesis. Having helped numerous students with their research over the years, we’ve noticed some common interviewing mistakes that first-time researchers make. In this post, we’ll discuss five costly interview-related mistakes and outline useful strategies to avoid making these.
Overview: 5 Interviewing Mistakes
- Not having a clear interview strategy /plan
- Not having good interview techniques /skills
- Not securing a suitable location and equipment
- Not having a basic risk management plan
- Not keeping your “ golden thread ” front of mind
1. Not having a clear interview strategy
The first common mistake that we’ll look at is that of starting the interviewing process without having first come up with a clear interview strategy or plan of action. While it’s natural to be keen to get started engaging with your interviewees, a lack of planning can result in a mess of data and inconsistency between interviews.
There are several design choices to decide on and plan for before you start interviewing anyone. Some of the most important questions you need to ask yourself before conducting interviews include:
- What are the guiding research aims and research questions of my study?
- Will I use a structured, semi-structured or unstructured interview approach?
- How will I record the interviews (audio or video)?
- Who will be interviewed and by whom ?
- What ethics and data law considerations do I need to adhere to?
- How will I analyze my data?
Let’s take a quick look at some of these.
The core objective of the interviewing process is to generate useful data that will help you address your overall research aims. Therefore, your interviews need to be conducted in a way that directly links to your research aims, objectives and research questions (i.e. your “golden thread”). This means that you need to carefully consider the questions you’ll ask to ensure that they align with and feed into your golden thread. If any question doesn’t align with this, you may want to consider scrapping it.
Another important design choice is whether you’ll use an unstructured, semi-structured or structured interview approach . For semi-structured interviews, you will have a list of questions that you plan to ask and these questions will be open-ended in nature. You’ll also allow the discussion to digress from the core question set if something interesting comes up. This means that the type of information generated might differ a fair amount between interviews.
Contrasted to this, a structured approach to interviews is more rigid, where a specific set of closed questions is developed and asked for each interviewee in exactly the same order. Closed questions have a limited set of answers, that are often single-word answers. Therefore, you need to think about what you’re trying to achieve with your research project (i.e. your research aims) and decided on which approach would be best suited in your case.
It is also important to plan ahead with regards to who will be interviewed and how. You need to think about how you will approach the possible interviewees to get their cooperation, who will conduct the interviews, when to conduct the interviews and how to record the interviews. For each of these decisions, it’s also essential to make sure that all ethical considerations and data protection laws are taken into account.
Finally, you should think through how you plan to analyze the data (i.e., your qualitative analysis method) generated by the interviews. Different types of analysis rely on different types of data, so you need to ensure you’re asking the right types of questions and correctly guiding your respondents.
Simply put, you need to have a plan of action regarding the specifics of your interview approach before you start collecting data. If not, you’ll end up drifting in your approach from interview to interview, which will result in inconsistent, unusable data.

2. Not having good interview technique
While you’re generally not expected to become you to be an expert interviewer for a dissertation or thesis, it is important to practice good interview technique and develop basic interviewing skills .
Let’s go through some basics that will help the process along.
Firstly, before the interview , make sure you know your interview questions well and have a clear idea of what you want from the interview. Naturally, the specificity of your questions will depend on whether you’re taking a structured, semi-structured or unstructured approach, but you still need a consistent starting point . Ideally, you should develop an interview guide beforehand (more on this later) that details your core question and links these to the research aims, objectives and research questions.
Before you undertake any interviews, it’s a good idea to do a few mock interviews with friends or family members. This will help you get comfortable with the interviewer role, prepare for potentially unexpected answers and give you a good idea of how long the interview will take to conduct. In the interviewing process, you’re likely to encounter two kinds of challenging interviewees ; the two-word respondent and the respondent who meanders and babbles. Therefore, you should prepare yourself for both and come up with a plan to respond to each in a way that will allow the interview to continue productively.
To begin the formal interview , provide the person you are interviewing with an overview of your research. This will help to calm their nerves (and yours) and contextualize the interaction. Ultimately, you want the interviewee to feel comfortable and be willing to be open and honest with you, so it’s useful to start in a more casual, relaxed fashion and allow them to ask any questions they may have. From there, you can ease them into the rest of the questions.
As the interview progresses , avoid asking leading questions (i.e., questions that assume something about the interviewee or their response). Make sure that you speak clearly and slowly , using plain language and being ready to paraphrase questions if the person you are interviewing misunderstands. Be particularly careful with interviewing English second language speakers to ensure that you’re both on the same page.
Engage with the interviewee by listening to them carefully and acknowledging that you are listening to them by smiling or nodding. Show them that you’re interested in what they’re saying and thank them for their openness as appropriate. This will also encourage your interviewee to respond openly.
Need a helping hand?
3. Not securing a suitable location and quality equipment
Where you conduct your interviews and the equipment you use to record them both play an important role in how the process unfolds. Therefore, you need to think carefully about each of these variables before you start interviewing.
Poor location: A bad location can result in the quality of your interviews being compromised, interrupted, or cancelled. If you are conducting physical interviews, you’ll need a location that is quiet, safe, and welcoming . It’s very important that your location of choice is not prone to interruptions (the workplace office is generally problematic, for example) and has suitable facilities (such as water, a bathroom, and snacks).
If you are conducting online interviews , you need to consider a few other factors. Importantly, you need to make sure that both you and your respondent have access to a good, stable internet connection and electricity. Always check before the time that both of you know how to use the relevant software and it’s accessible (sometimes meeting platforms are blocked by workplace policies or firewalls). It’s also good to have alternatives in place (such as WhatsApp, Zoom, or Teams) to cater for these types of issues.
Poor equipment: Using poor-quality recording equipment or using equipment incorrectly means that you will have trouble transcribing, coding, and analyzing your interviews. This can be a major issue , as some of your interview data may go completely to waste if not recorded well. So, make sure that you use good-quality recording equipment and that you know how to use it correctly.
To avoid issues, you should always conduct test recordings before every interview to ensure that you can use the relevant equipment properly. It’s also a good idea to spot check each recording afterwards, just to make sure it was recorded as planned. If your equipment uses batteries, be sure to always carry a spare set.

4. Not having a basic risk management plan
Many possible issues can arise during the interview process. Not planning for these issues can mean that you are left with compromised data that might not be useful to you. Therefore, it’s important to map out some sort of risk management plan ahead of time, considering the potential risks, how you’ll minimize their probability and how you’ll manage them if they materialize.
Common potential issues related to the actual interview include cancellations (people pulling out), delays (such as getting stuck in traffic), language and accent differences (especially in the case of poor internet connections), issues with internet connections and power supply. Other issues can also occur in the interview itself. For example, the interviewee could drift off-topic, or you might encounter an interviewee who does not say much at all.
You can prepare for these potential issues by considering possible worst-case scenarios and preparing a response for each scenario. For instance, it is important to plan a backup date just in case your interviewee cannot make it to the first meeting you scheduled with them. It’s also a good idea to factor in a 30-minute gap between your interviews for the instances where someone might be late, or an interview runs overtime for other reasons. Make sure that you also plan backup questions that could be used to bring a respondent back on topic if they start rambling, or questions to encourage those who are saying too little.
In general, it’s best practice to plan to conduct more interviews than you think you need (this is called oversampling ). Doing so will allow you some room for error if there are interviews that don’t go as planned, or if some interviewees withdraw. If you need 10 interviews, it is a good idea to plan for 15. Likely, a few will cancel , delay, or not produce useful data.

5. Not keeping your golden thread front of mind
We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don’t want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims . Your research aims, objectives and research questions – i.e., your golden thread – should influence every design decision and should guide the interview process at all times.
A useful way to avoid this mistake is by developing an interview guide before you begin interviewing your respondents. An interview guide is a document that contains all of your questions with notes on how each of the interview questions is linked to the research question(s) of your study. You can also include your research aims and objectives here for a more comprehensive linkage.
You can easily create an interview guide by drawing up a table with one column containing your core interview questions . Then add another column with your research questions , another with expectations that you may have in light of the relevant literature and another with backup or follow-up questions . As mentioned, you can also bring in your research aims and objectives to help you connect them all together. If you’d like, you can download a copy of our free interview guide here .
Recap: Qualitative Interview Mistakes
In this post, we’ve discussed 5 common costly mistakes that are easy to make in the process of planning and conducting qualitative interviews.
To recap, these include:
If you have any questions about these interviewing mistakes, drop a comment below. Alternatively, if you’re interested in getting 1-on-1 help with your thesis or dissertation , check out our dissertation coaching service or book a free initial consultation with one of our friendly Grad Coaches.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

The Qualitative Interview in Psychology and the Study of Social Change: Sexual Identity Development, Minority Stress, and Health in the Generations Study
David m. frost.
University College London
Phillip L. Hammack
University of California, Santa Cruz
Bianca D. M. Wilson
University of California, Los Angeles
Stephen T. Russell
University of Texas at Austin
Marguerita Lightfoot
University of California, San Francisco
Ilan H. Meyer
Associated data.
Interviewing is considered a key form of qualitative inquiry in psychology that yields rich data on lived experience and meaning making of life events. Interviews that contain multiple components informed by specific epistemologies have the potential to provide particularly nuanced perspectives on psychological experience. We offer a methodological model for a multi-component interview that draws upon both pragmatic and constructivist epistemologies to examine generational differences in the experience of identity development, stress, and health among contemporary sexual minorities in the United States. Grounded in theories of life course, narrative, and intersectionality, we designed and implemented a multi-component protocol that was administered among a diverse sample of three generations of sexual minority individuals. For each component, we describe the purpose and utility, underlying epistemology, foundational psychological approach, and procedure, and we provide illustrative data from interviewees. We discuss procedures undertaken to ensure methodological integrity in process of data collection, illustrating the implementation of recent guidelines for qualitative inquiry in psychology. We highlight the utility of this qualitative multi-component interview to examine the way in which sexual minorities of distinct generations have made meaning of significant social change over the past half-century.
The interview method has a long and distinguished history in qualitative inquiry across the social sciences ( Platt, 2012 ). Interviewing has become increasingly widespread in psychology ( Brinkmann, 2016 ), as qualitative methods have gained prominence in the discipline ( Gergen, Josselson, & Freeman, 2015 ). More than simply providing an account of attitudes or experience, the interview represents a site of social practice in which meaning is made in the interaction ( Mishler, 1986 ; Potter & Hepburn, 2005 ). An approach that integrates multiple epistemologies acknowledges the co-constructed nature of the interview and capitalizes on the potential of this interaction to produce knowledge grounded in lived experience ( Tappan, 1997 ).
Because of its ability to provide access to meaning making about lived experience in context, the qualitative interview affords the potential to study social change. That is, because the method calls upon individuals to make meaning of life events and experiences, it produces discourse content that can be analysed for its relation to larger cultural discourses and narratives (e.g., Hammack & Toolis, 2014 , 2016 ). The personal narratives produced through qualitative interviewing thus reveal the way in which individuals are in active states of navigating social and cultural change ( Hammack & Toolis, 2014 ).
One area of considerable social change has been the meaning of sexual diversity and the rights accorded individuals who identify as sexual minorities (i.e., lesbian, gay, bisexual, queer, and other individuals who do not identify as heterosexual) in the United States, Western Europe, and some Central and South American countries. These developments (for example, marriage equality for same-sex couples) highlight how social and policy changes create different environments for sexual minorities of different generations. It is clear that the coming of age of a sexual minority person in the US in the 2010s is vastly different from, for example, that of a sexual minority person in the 1960s, when homosexuality was still criminalized and considered a mental disorder (e.g., Hammack, Frost, Meyer, & Pletta, 2018 ; Russell & Fish, 2016 ).
Despite the overall improvements in the social and political climate, inequalities in health based on sexual orientation persist, and sexual minority youth continue to experience high levels of bullying and evidence high rates of suicidality relative to the general population ( Meyer, 2016 ; Russell & Fish, 2016 ). Thus, important questions about the impact of social change on the lived experience of sexual minorities remain unanswered in the research literature. Are recent social changes translating to more positive lived experiences for today’s sexual minority youth relative to older cohorts of sexual minority individuals? Does sexual identity matter less for young people who have more open-minded peers than it did for sexual minorities who came of age in less accepting times? To what extent do sexual minority youth experience prejudice and discrimination in a more progressive climate? Do contemporary sexual minority youth differ from older sexual minorities in the centrality they ascribe to a sexual minority identity (McCormack, 2012; Savin-Williams, 2005 )? How should investigators aiming to study the lived experience of sexual minorities assess and adequately account for these shifting social environments?
This paper presents a qualitative approach to answering questions surrounding the lived experience of sexual minority individuals in the context of rapid social change. We use the term “lived experience” to generally refer to people’s personal and subjective descriptions, perceptions, understandings, and interpretations of their own psychological and social experiences (e.g., Tappan, 1997 ). Specifically, the purpose of this article is to describe a methodological approach for understanding sexual identity development and minority stress in the context of social change as developed for and used within the Generations Study: a multi-site, mixed methods study of sexual identity, minority stress, and health across three generations of sexual minorities in the US. The methodological approach consists mainly of an interview protocol informed by multiple epistemologies and innovative it its integration of component methods typically used in isolation (i.e., lifeline methods, identity mapping methods, life story methods, and comparative temporal reflection). Through this integration, this new methodological approach is able to investigate generational differences in the experience of minority stress processes in tandem with identity development processes for the first time in a single study.
The minority stress framework ( Meyer, 2003 ) describes prejudice and stigma as stressors to which sexual minorities are exposed, which, in turn, have an adverse effect on their health and well-being. The minority stress framework outlines how prejudice and stigma lead to specific stress processes, including expectations of rejection, concealment of a stigmatized identity, internalization of negative beliefs about one’s social identities, and experiences of discrimination (both acute events and chronic everyday mistreatment). Like all stress, minority stress processes create strain on individuals’ ability to adapt to their environment and are therefore associated with decreases in mental health and well-being. Sexual minority individuals utilize a variety of resources located both in the individual (e.g., coping, mastery, meaning-making) and the LGBT community (e.g., connectedness, positive identity development, support from other sexual minority people), which build resilience that can reduce or eliminate the negative impact of minority stress on health (e.g., Bruce, Harper, & Bauermeister, 2015 ; Frost & Meyer, 2012; Meyer, 2015 ).
Because minority stress is a theory about socially embedded stress, historical shifts in the social environment should correspond with significant shifts in the experience of minority stress. Thus, if prejudice and stigma related to sexual minorities were reduced, we would expect a corresponding reduction in the experience of minority stressors. Not only could the level of stress exposure be changed, but also the types and quality of stressors could change with shifting norms and values. For example, internalized homophobia—a minority stressor—is related to the socialization of a sexual minority person in an environment that teaches prejudice and stigma about homosexuality and bisexuality (e.g., Herek, Gillis, & Cogan, 2009 ; Herek & McLemore, 2013 ). Both heterosexual and sexual minority people learn this as they are socialized. People who identify as sexual minorities are at risk of applying negative notions about being a sexual minority to their own sense of self, thus being exposed to internalized homophobia (e.g., Newcomb & Mustanski, 2010 ; Puckett & Levitt, 2015 ). To the extent that socialization in a more positive social environment would reduce homophobic and biphobic prejudice and stigma, then there would be no, or reduced, internalization of such negative attitudes. In this example, because the underlying social environment has changed, internalized homophobia could be eliminated as a stressor.
The Shifting Social Environment of Sexual Minorities
Despite understandable concerns about possible setbacks in LGBT-inclusive public policy in the current presidential administration, the last two decades have nonetheless witnessed significant increases in positive attitudes toward and social inclusion of sexual minorities in the US. For example, sexual minorities can now serve openly in the military and same-sex couples can now get married in all US states. Also, attitudes toward sexual minority individuals and same-sex couples have drastically improved, with most of the US population supporting same-sex marriage for the first time as of 2014 (Pew, 2016). Acceptance of and positive attitudes toward sexual minorities is very strongly related to age, with younger people having more favorable attitudes than older people (cf. Frost, Meyer, & Hammack, 2015 ).
Improving attitudes toward same-sex sexuality and relationships among younger generations have led some researchers to contend that youth and emerging adult sexual minorities come of age in a “post-gay” era (e.g., McCormack, 2012; Savin-Williams, 2005 ). This research suggests that adolescents and emerging adults with same-sex attractions, desires, and behaviors are not as marginalized and stigmatized as older cohorts have been, and thus their sexual minority identity may be a less central component of their overall self, compared with the experience of sexual identity among older cohorts of sexual minorities. This research stands in contrast to other studies, which show that sexual orientation continues to be an important aspect of youth identity and overall sense of self (e.g., Cohler & Hammack, 2007 ; Russell, Clarke, & Clary, 2009 ). Further, in spite of a more positive climate for sexual identity diversity, young sexual minorities continue to experience minority stress (e.g., Baams, Grossman, & Russell, 2015 ) and to engage with cultural discourses of stigma (e.g., Hammack & Cohler, 2011 ; Hatzenbuehler, 2017 ). There is little doubt that today many sexual minority adolescents and emerging adults are socialized in a radically different social environment than any previous generation ( Russell & Fish, 2016 ). Consistently, studies have shown that the current cohort of sexual minority youth are coming out (i.e., disclosing their sexual orientation to important others) at increasingly younger ages ( Floyd & Bakeman, 2006 ; Grov et al., 2006 ; for review, see Russell & Fish, 2016 ).
Despite the overall improvements in attitudes toward same-sex sexuality and relationships, inequalities persist ( Meyer, 2016 ). For example, federal law does not protect sexual minorities against employment discrimination. Also, sexual minorities continue to be victims of very high rates of antigay violence and bullying ( Kahn, 2016 ). Researchers continue to speculate that prejudice and related victimization underlie findings that sexual minority youth (regardless of gender) report higher rates of mental health problems, substance use, sexual risk, and suicidality than their heterosexual peers (e.g., Fish & Pasley, 2015 ; Marshal et al., 2011 ; Mohr & Husain, 2012 ; Russell & Fish, 2016 ). Thus, it is likely that sexual minority youth and emerging adults continue to experience stigma and victimization, navigating both a new, liberating narrative of “normality” regarding same-sex desire and an older narrative of stigma and subordinate status in the course of their development (e.g., Cohler & Hammack, 2007 ; Hammack, Thompson, & Pilecki, 2009 ; White, Moeller, Ivcevic, & Brackett, 2018 ). Further, sexual minority youth of color and gender non-conforming youth may experience changes in the social climate (or lack thereof) in importantly unique ways that are not accurately represented in the existing body of research evidence ( Fine, Torre, Frost, Cabana, & Avory, 2018 ). Research on sexual identity and minority stress and resilience has not adequately assessed the role of the shifting sociohistorical context in the lives and health of sexual minorities and important variability within such experiences. As a result, many claims have been made about the importance of a sexual minority identity and the extent to which the current social climate for sexual minorities has indeed “gotten better” (e.g., Savin-Williams, 2016 ), which warrant further rigorous research to fully investigate ( Frost et al., 2014 ; Hammack, 2018 ).
In addition to historical consideration of the social environment, research on sexual minorities has yet to fully integrate intersectional and life course perspectives. Specifically, a life course perspective ( Elder, 1998 ) allows for an understanding of how differences in the social and policy context, along with cohort-defining events (e.g., the Stonewall riots, the onset of AIDS, the repeal of “Don’t Ask, Don’t Tell”) shape the identities and lived experience of each generation differently. From a developmental perspective, a life course paradigm further concerns the complex interplay between social and historical context and individual development ( Cohler & Galatzer-Levy, 2000 ; Hammack, 2005 ). Thus, specific generations of sexual minorities can be considered distinct based on differential exposure to cohort-defining events and other aspects of the social and political context that shaped the historical periods in which they “came of age” ( Hammack et al., 2018 ). Thus, a life course perspective is essential to any attempt to directly investigate the degree to which the kinds of social and policy changes described above translate to differences in the lived experiences of the current cohort of sexual minority youth relative to previous generations.
Sexual minorities are diverse with regard to many characteristics including race/ethnicity, geographic region or residence, socio-economic status, immigration status, etc., all of which shape their lived experiences. Intersectionality frameworks implore researchers pay attention to unique intersectional circumstances, especially related to sexual orientation, race/ethnicity, and gender ( Cole, 2009 ; Crenshaw, 1996; McCall, 2005 ; Rosenthal, 2016 ; Stirratt et al., 2008 ; Warner, 2008 ; Wilson et al., 2010 ). For example, lesbian and bisexual Black women have unique experiences of identity, stress, and health associated with their sexual orientation, race/ethnicity, and gender that cannot be fully captured by considering race and gender categories separately ( Bowleg, 2008 ). Researchers need to explore how multiple social statuses shape the relationship among cohort, identity, minority stress, and health.
Although our focus was primarily on the development of sexual identity, we operate from a position that recognizes that sexual identity development and the experience of minority stress does not occur in isolation and is theoretically and analytically inseparable from other identities, including but not limited to gender and race/ethnicity. Further, as Bowleg (2008) argues, “…questions about intersectionality should focus on meaningful constructs such as stress, prejudice, discrimination rather than relying on demographic questions alone” (p. 316). Thus, there is a need for qualitative research to develop experience-oriented tools to examine intersectional experiences of what it is like to live minority stress as a person who is, for example, a young queer Latina woman, rather than simply striving to identify differences in the types and frequencies of minority stress across groups defined by age cohort, sexual orientation, race/ethnicity, and gender.
Examination of intersectionality has been previously achieved through the use of tools such as identity mapping, developed by Narvaéz and colleagues (2009) and Sirin and Fine (2007) , which was designed to study the experience of minority stress at the intersection of various forms of oppression and stigmatized identities. Such tools for assessing these elements of intersectional experiences of oppression and minority stress have thus far been anchored in studies of specific temporal and geographic contexts and have yet to incorporate understandings of intersectionality with understandings of where such intersectional experiences occur within the life course. Conversely, qualitative approaches to understanding the development of identity across the life course, such as narrative life story methods (e.g., McAdams, 1995 ) and lifeline drawing techniques (e.g., Grambling & Carr, 2004 ), do not explicitly include the kind of intersectionality focus advocated for by Bowleg and other methodologists operating from critical race, feminist, and queer theoretical and methodological perspectives (e.g., Bowleg, 2008 ; Cho et al., 2013 ; Crenshaw, 1991 ). Thus, in order to understand the complex diversity of lived experiences in sexual identity development and minority stress in the context of social change, a qualitative approach is needed which combines component methods which have thus far been largely isolated in their use in psychological research.
Following a life course approach to sexual identity development, individuals are understood to make meaning of their same-sex desire in the context of specific historical, cultural, and political contexts ( Cohler & Galatzer-Levy, 2000 ; Hammack & Cohler, 2009 ). The words and narratives individuals have to understand and describe their desire are historically contingent ( Hammack, 2005 ). Thus, a qualitative approach to access this meaning making directly is essential to document how sexual minorities engage with cultural narratives that shape their sexual identity development and experiences of minority stressors in the context of rapid social change and at the intersection of multiple social identities and statuses. The field still lacks an understanding of generational differences in the experience of minority stress processes in tandem with identity development processes. Research is needed to address these questions about the role of social change across the lifespan in sexual identity development and experience of minority stress, while taking into consideration intersecting identities and social statuses. Addressing these important but unanswered questions therefore requires an integrative methodological approach that is able to examine the complex interrelations of minority stress, social change, and sexual identity development.
We present one such approach developed by the authors who are co-investigators in a national multi-phase mixed methods research project called the Generations Study, funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD Grant#: 1R01HD078526). All aspects of the research involving human subjects were approved by the Institutional Review Board (IRB) at [University of California, Los Angeles], with which all other universities’ IRBs involved in the study established a relying agreement. The Generations Study explored generation-cohort similarities and differences in sexual identity, minority stress and resilience, access to health care, and health outcomes. The study focused on three cohorts of sexual minorities in the USA.
The three cohorts were defined by the distinct nature of their social environments during two critical periods of development: adolescence and emerging adulthood. The youngest generation was 18–25 at the beginning of our study in 2015. We refer to them as the cultural inclusion generation, as they experienced an improved social context for sexual diversity in which sodomy laws had been ruled unconstitutional and the cultural discourse had shifted to that of equality, leading to inclusion of sexual minorities in the military and equal access to legal marriage. Members of the institutional advancement generation were 34–41 years old at the time of our study and had experienced childhood and adolescence at the height of the AIDS epidemic, which disproportionately impacted sexual and gender minorities and led to the development of health organizations around the country that went on to aim to serve the broader LGBT communities. This generation was also the first to have greater access to resources through the Internet. LGBT people in general, not just the gay men and transgender women who were disproportionately impacted by the epidemic, gained heightened public scrutiny and increased stigma and prejudice due to fear of HIV/AIDS but also greater political awareness and consolidation of LGBT community institutions (like health centers). Members of the identity formation generation were 52–59 years old at the time of our study and experienced the post-Stonewall environment, when homosexuality was considered a mental disorder and sodomy was illegal in many states but when the first Gay Pride event took place (in 1970) and a larger discourse of pride in sexual minority identity took hold in the LGBT community.
The qualitative approach of the Generations Study sought to address the following specific aims: (a) To describe similarities and differences among sexual minority cohorts in trajectories of the formation, expression, and experience of sexual identity; (b) To describe similarities and differences among sexual minority cohorts in trajectories of exposure to minority stress and resilience (availability of coping and social support resources); and (c) To describe similarities and differences among sexual minority cohorts in trajectories of utilization of health and social services and public health information. Reflected in the combination of these aims, the Generations Study was guided by both scholarly and practical goals. These goals include the advancement of social scientific knowledge about how social changes have shaped the experience of sexual identity development and minority stress, as well as goals to inform interventions and policy change directed at improving the health and well-being of sexual minority individuals, who continued to experience health inequalities relative to their heterosexual peers ( Meyer, 2016 ).
The Qualitative Interview: A Multi-Component Approach
Links between paradigm, epistemology, and method.
The scholarly and pragmatic aims of the Generations Study required an approach to qualitative inquiry which can best be categorized as operating within a paradigm of methodological pluralism and emphasizing paradigmatic complementarity (see Madill & Gough, 2008 , for a discussion of qualitative paradigms within psychology). Specifically, our aim was to examine participants’ accounts of their lived experiences through the combination of multiple methodological components and the accumulation of multiple researchers’ perspectives in the design of the study collection of data aimed toward achieving scholarly and practical purposes ( Madill, Jordan, & Shirley, 2000 ). The epistemological positions underpinning the design of the qualitative approach can be best described as straddling elements of constructivism and pragmatism Namely, the approach stems from constructivism in its emphasis on narrative and lived experience and that it did not assume a knowable truth or an “objective” reality of lived experience to exist, but rather that idiographic and subjective meaning of participants’ experiences could be examined through one-on-one engagement in research interviews (e.g., Ponterotto, 2005). Elements of pragmatism shaping our approach are evident in our implementation of a diversity of methods and the accumulation of multiple researchers’ perspectives for both scholarly and practical purposes ( Madill et al., 2000 ), such as informing social and health policy. As noted in recent guidelines for designing qualitative research, these epistemological positions need not be considered mutually exclusive ( Levitt, Motulsky, Wertz, Morrow, & Ponterotto, 2017 ).
This paradigmatic and epistemological position required a semi-structured interview protocol that was open enough to provide storied accounts of lived experience reflective of narrative meaning making processes, as well as specific content-oriented questions about phenomena central to the aims and research questions of the study (e.g., sex and sexual cultures, community, stress and coping, access to healthcare). Thus, the instrument included general questions about key events and trajectories in participants’ general life stories, as well as specific questions about same-sex desire awareness, sexual experiences and sexual identity development, and minority stress experiences, including stressful life events related to sexuality, experiences with stigma and expectations of discrimination based on sexuality, internalized homophobia, and perceptions of relationships between sexual minority stress and the structural and cultural dimensions of other social statuses (e.g., race/ethnicity, gender, rural residence). Given the focus of the study on identity development and individual-level meaning making of experiences of minority stress, the design of the study involved individual one-on-one interviews (rather than, for example, focus groups). Interviews were conducted by trained interviewers and lasted on average between two and a half to three hours.
Qualitative Interview Protocol
The interview protocol (provided in the online supplemental material ) was organized in eight sections. The course of the interview was designed to progressively narrow in scope from the opening section which was the broadest and most unstructured (i.e., the life story) to the most specific content-focused sections nearing the end of the interview (e.g., health care utilization). The narrowing scope of the interview allowed for the emergence of constructs relevant to the study (e.g., minority stress, coping) to emerge naturally within the participant’s discussion of his/her/their overall lived experience initially, with opportunity to obtain more specific accounts of such experiences later in the interview, as opposed to using the focal constructs of the study to guide the course of the interview from the start.
We present each section of the interview protocol below along with a discussion of the conceptual purpose, epistemological foundations, methodological intent, and exemplar data excerpts to illustrate the section’s utility. Table 1 provides an overview of the interview components and summarizes these linkages. It is important to note that the data exemplars are included for the purpose of illustrating the methodological utility of the approach and the richness of the types of data that emerged from the interview: The data presented are in no way intended to reflect the full range of study findings. The sections are presented in the order in which most interviews progressed. However, interviewers were given the freedom to change the order of the sections when warranted by the natural flow of conversation with participants.
Linkages between epistemology, method, and utility within an integrative qualitative approach.
| Interview Component | Purpose and Utility | Epistemology | Foundational Psychological Approach | Procedure |
|---|---|---|---|---|
| Lifeline | Obtain a broad sense of participants’ life stories and overall life trajectories; obtain visual depictions of events and transitions that constitute individuals’ understandings of their own life histories | Pragmatism | Life Course | Lifeline drawing activity |
| Life Story | Explore identity development through a constructed life story narrative; understand broader life history as context for discussion of specific lived experiences in subsequent sections | Constructivism | Life Course & Narrative | Adapted Life Story Interview |
| Identity Mapping | Provide participants with a space to describe their identities in their preferred terms and as they relate to one another; elicit detailed discussions of identities and how they relate to one another in the context of a focal lived experience | Pragmatism | Intersectionality | Identity map of social identities and communities |
| Lived experiences of: Sex and sexual cultures Challenges, stress, and coping Social and historical change | Obtain understandings of focal aspects of lived experience in the context of different points in the life course (i.e., adolescence and puberty and at the present time); Understand experiences and meanings of continuity and change over time | Constructivism | Life Course & Narrative | Comparative Temporal Reflection |
| Healthcare utilization | Understand participants’ perceptions of, barriers to, and ways of engaging with health care; perspectives on LGBT specific healthcare providers | Pragmatism | Behavioral Model of Health Service Use | Descriptive Interview |
| Reflections and goals | Account for imagined futures within a life course framework; end the interview in a positive discussion | Constructivism | Life Course & Narrative | Comparative Temporal Reflection |
Note - This table describes the primary elements shaping each section of the interview. However, the entire interview protocol was informed by a blending of life course, narrative, and intersectionality approaches, and thus no section was exclusively informed by a singular approach.
1. Lifeline.
The first section of the interview was designed to obtain a broad sense of participants’ life stories and overall life trajectories. Specific experiences around the focal constructs of the study could be contextualized in later sections. To facilitate this, we used two established qualitative tools to elicit life story narratives: Lifeline drawings and the life story interview.
First, participants were asked to complete a lifeline drawing activity. Lifeline techniques have been used in life course and developmental research to obtain visual depictions of events and transitions that constitute individuals’ understandings of their own life histories (e.g., de Vries, LeBlanc, Frost, Alston-Stepnitz, Stephenson, & Woodyatt, 2016 ; Gramling & Carr, 2004 , Hammack, 2006 ). Informed by both life course and life events traditions (e.g., Elder, 1998 ), lifeline tools reveal important moments of continuity and change within the life course and provide the foundation for discussion of the social and historical circumstances that shape the life course trajectory ( de Vries et al., 2016 ). In the present use, participants were asked to “Please draw a line that represents your life. The line should begin when you were born, go to today and then continue into your future. The line should go up when it was a good time in your life and down when it was a bad time in your life. Take a few minutes to think about your life and draw the line, and when you are finished we can discuss it.” Participants were provided with the visual tool, included in Figure 1 , on which they could draw their lifeline. After participants completed their drawing, interviewers asked participants to briefly describe why they drew the line the way they did (e.g., “Why did you start off the line at a high point?”; “Why did the line change directions here?”).

Example Lifeline Drawing.
The example lifeline provided in Figure 1A comes from a 24-year-old Latino gay man. His line illustrates several ups and downs in life, including early childhood bullying and problems with family, financial trouble and dropping out of college, followed by turning points characterised by weight loss, confidence gain, and re-enrolling in school. His line also notes a generally high (positive) interpretation of the present but flat trajectory headed toward the future, which he characterizes as exciting but also anxiety provoking.
A contrasting example can be seen in Figure 1B , the lifeline of a 21-year-old Latina lesbian woman. Her lifeline also can be characterized by several ups and downs, starting with immigrating to the US from Mexico when she was 5, through parental divorce, depression, and declaring a major in college. In contrast to Figure 1A , this woman’s lifeline ends in a positive upward trajectory anticipating a better future compared to her past and present.
Grounded in epistemological concerns relating to pragmatism, this section of the interview served several purposes. It provided participants with a “settling in” activity that served to build rapport with the interviewer. It provided the interviewer with broad context for how the participants viewed their overall life trajectory and key events and transitions within that trajectory. It provided a visual sketch of participants’ life trajectories that could be referenced in subsequent discussions and used later for formal analysis using narrative analytic methods ( Lieblich, Tuval-Mashiach, & Zilber, 1998 ). Finally, both the lifeline and discussion of its construction provided key data used to frame the following life story segment of the interview.
2. Life story.
Following the creation of the lifeline, the interview employed central elements of the Life Story Interview (LSI), a flexible protocol commonly used in personality and social psychology to explore identity development through a constructed life story narrative (McAdams et al., 2008). Modified versions of the LSI have been used successfully with diverse populations, including sexual minorities ( Frost, 2011 ; Hammack & Cohler, 2011 ). The portion of the LSI employed here inquired about participants’ critical life events, social influences, and values. Specifically, interviewers framed the LSI by telling participants: “Now, I’d like us to focus on a few key events that happened to you in your life. For each event, please describe what was happening, where you were, who you were with, and what you were thinking and feeling at the moment.” Participants were asked to talk about their first memory, a high point in their life, a low point in their life, and a turning point. For example, the Latino male participant ( Figure 1A ) identified the death of his aunt and cousin while he was in university as a low point, and a recent moment when he became financially stable and able to emerge from debt as his high point. In contrast, the Latina female participant ( Figure 1B ) identified her graduating high school as the high point in the life story, while her low point was a moment a few weeks before the interview in which she felt like she was “going into a depression,” having experienced “a crash” of negative emotions after being questioned by members of her family regarding her sexual orientation.
At no point during this broadest section of the interview were participants asked specifically to talk about sexual identity or minority stress, unless they brought up the topics themselves. However, the lifeline and life story, and associated narratives, were used to anchor specific events and discussions of sexual identity and minority stress in participants’ broader life histories when brought up in the following content-specific sections of the interview.
With its roots in narrative and constructivist epistemologies, the LSI provided data that was useful in understanding the meaning of significant events in participants’ life histories via processes of narrative (re)telling. Specifically, this portion of the interview provided access to the spontaneously constructed personal narrative of the interviewee. Narrative psychologists view the personal narrative as a source of coherence, continuity, and meaning making (e.g., Cohler, 1982 ; Hammack & Toolis, 2014 ; McAdams, 1990 , 1997 ). The personal narrative is especially significant for those who experience adversity or discontinuity in the anticipated life course ( Cohler, 1991 ; Hammack & Toolis, 2014 ), which describes the likely experience of sexual minorities who are socialized in a context of heterosexism and presumed heterosexuality ( Herek & McLemore, 2013 ). This portion of the interview allowed us to apply an interpretive, hermeneutic approach grounded in constructivist epistemology to the way in which our participants made meaning of significant life events. We were especially interested in the way in which events related to sexual identity development or the experience of sexual minority status might appear in the personal narrative absent specific prompting for such events. This approach allowed us to examine generational similarities and differences in the centrality of a sexual minority identity to the general life story and thus to address one of our central research questions about social change and the meaning of a sexual minority identity.
3. Identity mapping of social identities and communities.
To shift the discussion from participants’ general life histories to specific aspects of their social identities and community memberships, the interviewer guided participants through an identity mapping activity and discussion. Identity mapping activities have been successfully employed in previous research designed to elicit detailed discussions of multiple personal and social identities and how they relate to one another in the context of a focal lived experience (e.g., Cruwys et al., 2016 ; Narvaéz et al., 2009; Sirin & Fine, 2007 ). Specifically, participants were presented with the visual tool included in Figure 2 . They were asked to use that tool “as a starting point for listing the identities and roles that describe who you are. You can write words or phrases that represent different aspects of yourself. These might include social identities or labels related to gender, race, sexuality, class, occupation, different roles in your life, or any words or phrases that describe you.” As visible in the identity map provided in Figure 2 , a 38-year-old Pakistani man includes several identities pertaining to his sexual orientation (queer), race/ethnicity (Pakistani, South Asian, POC), gender (cis-gender male), as well as identities related to immigration, socioeconomic status, and health. He also notes identities related to his political views (e.g., progressive, activist) and his being a survivor of past abuse.

Example Identity Map.
Given the present study’s interest in intersectionality as it relates to the experience of sexual identity development, gender, and race/ethnicity in particular, the following discussion of participants’ identity maps focused on these core identities and their intersections. If participants did not spontaneously list something for each of these core identities, the interviewer prompted them to consider whether they would like to include them on their maps (e.g., “I noticed you did not include anything about your gender on your map…”). Such prompting was more often needed among those with typically privileged or dominant social identities that are often taken for granted in everyday life (e.g., male gender, White race/ethnicity). To prompt participants to reflect on their experiences of their intersecting core identities, interviewers asked participants a series of questions repeating versions of the following adaptable prompt for the possible intersections: “Tell me about your experience of being [SEXUAL IDENTITY] in the [RACE/ETHNICITY/GENDER] community.” These prompts were designed according to Bowleg’s (2008) recommendation that, in order to best assess intersectionality experiences, researchers should ask about them directly.
This direct discussion of intersectional identity experiences is reflected in the following experience of a 54-year-old Chinese gay man:
I feel sometime a double discrimination in both community… I think I didn’t come out to my family for the longest time, just because I hear these horror story about, especially in the Chinese culture, and probably lot of different culture can relate to it, that family’s very important, and that you don’t wanna disgrace your family. I just felt like they would disown me, and they would be ashame of me…. Then, being a Chinese gay in the gay community, [...] I don’t feel really totally accepted in the [gay community]. … I don’t consider it as my community. I always felt angry at people that said oh, “I’m only attracted to White guys only, or I’m only attracted only Asians.” Then I don’t want that, either, because I want people to like me for how I look.
As this excerpt from one interview reveals, this section of the protocol elicited narratives of intersectionality to capture the diversity of lived experience among sexual minorities typically unrepresented in traditional quantitative research.
In line with constructivist epistemological foundations, additional questions in this section of the interview focused on how participants see themselves in terms of masculinity and femininity in their gender expression, as well as what communities they feel they belong to and what it is like to be a member of such communities. Just as the life story section provided a life course anchor for specific events and experiences discussed later in the interview, the identity map served as a general sketch of identity intersections that interviewers returned to in discussing specific experiences related to sexual identity, race, and gender later in the interview. Thus, this section was designed to fulfil pragmatic epistemological goals not only for giving the participant an opportunity to nominate and describe their identities in their own words, but also providing additional foundational data for orienting the subsequent temporal reflective discussions.
4. Sex and sexual cultures.
Next, the interviewer turned the discussion to more narrowly focus on specific types of lived experience within specific life domains. The first of these more specific discussions focused on participants’ “sex life and relationships.” In this section, participants were asked to discuss their experiences of sex and relationships, including how they felt about sex and relationships, how they went about findings partners, and the things that both excited and worried them about sexuality.
Interviewers guided participants through these discussions using a series of questions designed to elicit comparative temporal reflection. Stemming from constructivist perspectives, these discussions were designed to explore the meanings participants give to their lived experiences and how they viewed their own lived experiences staying the same or changing across various ages and developmental periods. The guided discussions involving comparative temporal reflection were designed to avoid imposing an expectation of change, further allowing participants the freedom to describe and interpret the meaning of their lived experiences as stable or changing throughout the life course.
To illustrate this process of comparative temporal reflection, participants were asked to describe their sex life and relationships during adolescence and puberty and at the present time. Participants were asked to reflect on how aspects of their sex life and relationships have changed or stayed the same between puberty and adolescence to the present. If they described changes over time, interviewers prompted them to discuss why they thought the changes had occurred, the ages the changes had occurred, and specific life events or social factors that may have precipitated changes. Participants were also asked to relate their discussions to the identity map and locate them in relation to other events on their lifelines and in their life stories.
For example, in the following exchange, a 36-year-old Black woman discussed how the ways she looks for sexual and relationship partners have changed as she has gotten older, especially now that she has a child from a previous relationship. She reflected on the role that the Internet now plays—both positive and negative—in her search for sexual and relationship partners, along with her changing needs/desires from a partner.
Interviewer: How about the ways with age, what’s changed in the ways you go looking for sex, in the kinds of things you’re looking for in a relationship?
Interviewee: The kind of things I’m looking for? Nobody wants stability…. Nobody wants somebody with kids. That’s number one. [chuckles] Or, they’re young and they want kids. I’m like, “My eggs are powdered.” [chuckles] …As far as sex, my sex drive has not changed since I was 15… The sex is not an issue…. Just relationship.
Interviewer: How about the way you go about finding it? Where did you find your relationships before? How did you find [previous partner]?
Interviewee: Online…. Internet makes it a lot easier, but also Internet makes it a lot harder, because… It’s all about looks…. Going out in person, looking for relationships … is hard, because I don’t look like a lesbian from what I’ve been told. I’ve had to kind of learn to step up and be the aggressor.
As this excerpt reveals, in this section of the interview we were able to elicit narratives of sex and sexual culture in both the remembered past and the experienced present. This excerpt reveals the ways that changing personal motives for sex and relationships can be both facilitated and frustrated by elements of one’s sexual culture (e.g., online dating, community standards of attraction, gender roles). Interviewees provided rich data on understandings of intimacy and sexual minority communities that revealed the ways in which radical social change—in this case, coupled with technological change—over the past half-century impacted their understandings of identity, community, and sexual practice.
5. Challenges, stress, and coping.
Again involving comparative temporal reflection, the fifth section of the interview contained questions about challenges and stressors in participants’ lives and how they coped with them. The opening questions focused on participants’ “single greatest challenge in life,” how they “handled” that challenge, and how this challenge impacted them “as a person.” Participants were asked to locate the challenge on their lifeline to contextualize it within the broader scope of their life course development. This discussion was not focused on sexual orientation or minority stress. Indeed, we asked about “challenges” to avoid guiding participants to narratives of stress and pathology, allowing the participants’ narratives to take a natural form. This approach allowed us to document the degree to which participants’ most challenging and stressful life experiences came about, were shaped by, or involved minority stress, without explicitly prompting about sexual minority status.
After the general discussion of challenges, questions focused on participants’ experiences of minority stress and coping directly. Participants were asked if they experienced any challenges in their life specifically related to being a sexual minority person (the interviewer used the sexual identity label from each participant’s identity map). For any event that participants recalled, they were asked to narrate what happened, who was involved, how they felt about the experience, and how they coped with the experience. These prompts were used to produce an account of the experience with a clear narrative trajectory and evaluative frame. Participants were also asked to reflect back across their lives and discuss any times they struggled to accept themselves as a sexual minority person and times when they had to negotiate being out and concealing their sexual identities. This section also included an opportunity for participants to reflect on the question, “in your day-to-day experiences, do you feel that society is accepting of you and other LGB people?” and whether or not their perspectives on societal acceptance have changed over time.
The following exchange between an interviewer and a 22-year-old Asian man illustrates the kinds of narratives elicited in this section. The participant described challenges in accepting himself as gay during adolescence and how it has remained a challenge throughout his life:
Interviewee: When I was a kid, I did—I was a Boy Scout. I was on the swim team. I also did martial arts. I had a lot of very stereotypically masculine things. It was sort of okay for a while. Then I began to see small tinges of homophobia from time to time. Every single time, when I would see it, I would make a mental note of, “Prob’ly should not tell you.” Because you’ll have some offensive—they’ll shout out a homophobic slur. …When in other cases, for instance—a few years ago, actually, I was working with a project with a friend. …He said that he would not be comfortable with changing in front of me. I’ve known this guy for about three years. When he said that I was taken aback, because I told myself—I said, “Why am I friends with a bigot? Why is he the—the implicit homophobia? Why am I getting this from him?”
Interviewer: He knew you were gay and made the comment?
Interviewee: He knew I was gay, and then he made the comment. Which is, I would say, is even worse. …It reminds me to be very careful with my identity. Because there have been certain times when I’ve felt that if I were to share that bit of my identity, I would be unsafe. There have been a few times here or there. There are very few straight men that are truly comfortable with me. …There are certain people that stick out to me where just—no, it is not safe. It’s just feeling—being excluded from that community. From the greater community.
In addition to illustrating his struggle to feel fully included in society, this participant’s narrative illustrates experiences of prejudice and the cognitive burden and stress associated with managing concealment, which can be both psychologically damaging and protective (e.g., a cognitive burden of secret keeping, which can sometimes help to avoid prejudice and discrimination) ( Meyer, 2003 ).
This section of the interview ended with a discussion of participants’ use of coping strategies and access to social support available to help them deal with general challenges and challenges related to minority stress. Specifically, they were asked “what types of things helped you deal with challenges and negative experiences you’ve had related to being (sexual identity label)?” As in previous sections, participants were asked to reflect on whether or not their coping strategies and access to support have remained the same or changed over the years. Given the role of community connectedness as a coping resource in the minority stress experience (Frost & Meyer, 2012; Meyer, 2003 ), participants were also asked to reflect on the extent to which they utilized sexual minority community resources (e.g., an LGBT center) or services targeted to sexual minority communities.
6. Interpretations of social and historical change.
Again utilizing comparative temporal reflection methods, the next section of the interview focused on participants’ memories of historical events, cultural moments, and social representations of sexual minority people and issues. Participants were asked: “Can you tell me about your memories during puberty and adolescence about what was happening in society with regard to LGBT issues?” They were then prompted to reflect on how LGBT issues were talked about in the wider society at this time in their lives, from whom and where they heard LGBT issues discussed, and what they felt and thought about such mentions when they occurred. They were then asked to reflect on how LGBT issues are discussed today, and what they feel and think about such discussions.
Illustrating both perceptions of a shift in cultural discussions of LGBT issues, as well as the persistence of stigma in the dominant narratives that are told about the LGBT community, the following younger Black genderqueer person’s narrative illustrates the value of directly interrogating participants’ perceptions of social and historical moments and how they shape lived experiences of sexual identity and minority stress:
Interviewee: I don’t remember—yeah, my hometown wasn’t—so I didn’t have—I didn’t have super great Internet access all the time, as a kid. Or growing up, I didn’t— our computer was really shitty and wasn’t super great. Yeah, local media didn’t report on it. People didn’t talk about it.
Interviewer: How about now? What do you see as major issues today, with regard to LGBT people?
Interviewee: The murder of trans people I guess I’d include in that group, but also just homeless youth that are lesbian, gay, bi, queer youth that are homeless because they couldn’t stay where they lived, out of either because they weren’t accepted or violence happened or assault happened, I think is really intense and a lot more prevalent than a lot of people would realize. Yeah, and it’s not always super safe out there.
As this excerpt reveals, this section of the interview provided the opportunity for participants to offer their own interpretations of the social context of sexual identity development and minority stress at two points in their development—during adolescence (a critical period for identity development; Hammack & Toolis, 2015 ) and today. Notably, this participant reported not hearing much in the news about sexual minority people when growing up, but they remembered having access to a “space” that was accepting. They further noted a recognition of violence against trans people as characterizing the social and historical events shaping the present climate surrounding sexual minority lives. These narrative accounts allow us to examine diversity in how members of different generations have interpreted the massive social and historical changes for sexual minorities over the past half-century. They also allow us to examine generational differences in interpretations of the present social and political context for sexual and gender identity diversity.
7. Healthcare utilization.
Given the focus of the broader study on health and healthcare utilization, the last major section of the interview contained very specific questions about experiences of seeking and receiving care related to mental and physical health. Participants were asked to discuss where they go when they need care, including whether they go to or would prefer to use LGBT-specific healthcare providers. They were asked about their last experience seeking healthcare and specific aspects of that experience. Interviewers also prompted participants to discuss deterrents to seeking healthcare, how open they are about their sexual identities in healthcare contexts, and whether they have ever sought care for reasons related to sexual identity or gender expression.
To illustrate the types of narratives elicited by this section of the interview, the following example from a 39-year-old White woman exemplifies the complexities of navigating minority stress in healthcare contexts:
Healthcare’s harder to navigate in many ways. I feel like I end up making choices around what’s good for my lymphedema. Then secondary is, “Are they queer-friendly?” My GP, not particularly queer-friendly. In fact, on my—I can tell that she’s a little horrified that I’m poly on my diagnosis form for my last annual. One of the things she put was “high-risk bisexual activity” as one of my diagnoses. I don’t know how you get treated for that, [ laughs ] but I was pretty horrified, because I’d been with one man my whole life, right?
Noting how her identification as polyamorous on her medical records resulted in her provider’s assumption that she was engaging in high-risk sexual behaviour, this participant’s narrative provided a critical experiential window into the healthcare experiences of sexual minorities. Given she has a serious health problem, she noted she must privilege her seeking care for this over seeking care that is LGBT-affirming.
This portion of the interview was primarily rooted in pragmatist aims. Following from the behavioral model of health services use ( Martos, Wilson, Gordon, Lightfoot, & Meyer, 2018 ), it was designed to understand and document participants’ preferences for certain types of health care provision and allowed us to obtain data on the healthcare decisions and challenges associated with potential minority stressors in healthcare settings.
8. Reflections and goals.
In order to (a) account for imagined futures within a life course framework and (b) end the interview in a positive discussion (given that the last few sections of the interview were primarily focused on negative experiences), the last section prompted participants to discuss their goals for the future. They were asked to look back at their lifeline and tell the interviewer about their goals for the future regarding work, relationships, and family life. Finally, they were asked to consider their entire lifeline, and reflect on what they thought has been the most positive aspect of being a sexual minority (interviewers used participants’ preferred sexual identity labels).
The following excerpt from a 25-year-old Black woman provides an illustrative response to these final questions of the interview.
Interviewer: Finally, looking back over your life, what would you say has been the most positive aspect of being bisexual?
Interviewee: The struggles. It forces you to be accepting, I think, because I don’t feel like anyone who has this type of sexual orientation is any different from anyone else who is heterosexual. I think that other people would want to treat you like you’re different. I feel like it forces you to be able to express yourself and be able to be open-minded enough to accept that everybody’s not gonna accept your sexuality. You can still help them to understand you as a person, as much as they will allow. If you can be patient enough to help other people see that you’re just another person, and you just want to be respected as just that, then it makes you pretty strong.
As this excerpt reveals, this final section of the interview provided the valuable opportunity for participants to narrate their future life goals and to consider the positive value of a sexual minority identity. It also illustrates the concepts of resilience and stress-related growth, noting struggles associated with being a sexual minority person, but also the strength derived from such experiences.
Methodological Integrity
The Generations Study’s methodological approach strived to achieve methodological integrity throughout the process of data collection. In doing so, we follow the recommendations for promoting methodological integrity offered by Levitt and colleagues (2017 ). Specifically, we highlight how aspects of sampling, interviewing training, and quality assurance were implemented to enhance fidelity to the substantive focus of the study and utility of the methodological approach to achieve the study’s aims and purpose.
Sampling was central to achieving the aims of the study and allowing sufficient representation and diversity of lived experience to reflect the study’s conceptual foundations in minority stress, life course, intersectionality, and social change. For example, many qualitative studies focus on one geographic area and lack the ability to compare across locations, potentially missing important diversity in lived experiences. To address this issue, we recruited participants from culturally distinct geographic regions of the country. Each site had a catchment area of 80 miles, which included urban and non-urban areas. Based on the study’s foundations in intersectionality and life course perspectives, we used quota sampling to ensure roughly equal representation of participants across age cohort, gender, and racial/ethnic groups. Obtaining a diverse sample also contributes to the study’s potential to achieve a high degree of one form of generalizability in qualitative research— transferability ( Polit & Beck, 2010 ). Combined with thick descriptions of the data and study design, ensuring recruitment of participants from several core social status groups relevant to the phenomenon under study increases readers’ understandings of whether and under what conditions various findings may reflect the experiences of people not included in the study directly.
Several procedures were established to achieve consistency in the interviews across the four study sites and to ensure the data collected were sufficiently rich in detail pertaining to content and narrative reflection. First, interviewers from each study site met in person, were trained on the interview protocol, and conducted mock interviews. All investigators in the study listened to the mock interviews for each interviewer and provided feedback until interviewers were deemed ready to begin interviewing. Interview quality and consistency were assured through weekly in-site meetings between interviewers and the lead investigator at each site. In addition, online meetings among all interviewers across the sites took place bi-weekly using video conferencing software. Different reflexive and engagement exercises were conducted. The purpose of this engagement in reflexivity and positionality was to recognize and manage the role of researchers’ perspectives in the data collection process, to maintain consistency in the implementation of the interview protocol, and to continue to hone the skills of the interviewers ( Barry, Britten, Barber, Bradley, & Stevenson, 1999 ).
Discussion and Conclusions
Interview methods are increasingly common in qualitative psychology ( Brinkmann, 2016 ), but few interview studies specify the purpose, epistemological grounding, theoretical foundation, or procedure associated with their protocol. With greater attention to methodological standards in qualitative psychology, there is a need for greater specificity of protocols and practices to ensure integrity and fidelity in the data collection process. Our aim was to provide a model for qualitative inquiry that can address this need.
In presenting the methodological approach utilized in the Generations Study, our goal was to highlight the unique potential for a qualitative approach—employing life course, narrative, and intersectionality perspectives through a combination of component methods previously used in isolation from one another—to provide a rich and nuanced understanding of the complex lived experiences of diverse sexual minority individuals in the context of social change. At the center of this methodological approach is a novel multi-component interview protocol, the first to integrate lifeline methods, life story methods, identity mapping methods, and comparative temporal reflection about personal identity, social change, minority stress, and health. Through this integration, this new methodological approach was able to investigate generational similarities and differences in the experience of minority stress processes in tandem with identity development processes for the first time in a single study. This approach also achieves an understanding of the experience of sexual identity and minority stress at the intersection of multiple social identities and forms of oppression related to sexual orientation, gender, and race/ethnicity, rather than falling into the methodological “trap” of using simplistic additive combinations of demographic characteristics as a proxy for an intersectionality approach ( Bowleg, 2008 ).
To understand how social change has shaped the lives of sexual minority individuals, research needs to directly investigate generational differences in lived experience of sexual identity development and minority stress. The life course (e.g., Elder, 1998 ; Hammack et al., 2018 ) and intersectionality perspectives (e.g., Bowleg, 2008 ; Cole, 2009 ; Crenshaw, 1996) highlight the importance of understanding sexual identity development in relation to sociohistorical context and focus on how variability in lived experience exists within unique intersections of age cohort, gender, race/ethnicity, and geographic location ( McCall, 2005 ; Stirratt et al., 2008 ; Warner, 2008 ; Wilson et al., 2010 ). The qualitative approach we presented reflects these theoretical and methodological foundations, and as a result is positioned to address gaps in existing knowledge about how social change has shaped the lives of sexual minority individuals (e.g., Frost et al, 2015 ; Hammack, 2018 ; Meyer, 2016 ).
The general approach utilized in the content-specific sections of the interview protocol prompted participants to reflect on specific events or experiences in adolescence relative to their present experiences and the changes they see over their lives. This methodological strategy was designed to directly interrogate developmental trajectories and changes throughout the life course, along with the meanings and explanations of such trajectories. Furthermore, because each participant was asked to provide such reflection, regardless of their present age cohort, the resulting dataset as a whole allowed for generational comparisons in experiences (during the same historical period, but different ages), as well as for all individuals when they were in adolescence (same age, different historical period).
The novel structure of the interview protocol, along with the purposive sampling strategy, allows for between-cohort analyses in the study’s aims to answer nomothetic research questions focused on group differences. Additionally, the intra-individual developmental reflections discussed previously allow for change analyses oriented toward answering idiographic questions focusing on individual persons and the nuances of their lived experience. Thus, the qualitative data obtained within the present approach allows for an examination of the broader aims relating to the role of social change in the experience of sexual identity development and minority stress with a direct analytic window into the role that social change plays in these experiences. The data exemplars included in this methodological paper were intended to illustrate the utility of this approach and analytic potentials emerging from its use. However, it is important to reiterate that the data presented in the paper are for illustrative purposes only and do not reflect the breadth of findings of the Generations Study.
In addition to understanding the role that social change has played in the lives and well-being of sexual minority individuals, data produced from the present qualitative approach is intended to be useful within policy making and social change efforts ( Gergen et al., 2015 ). Specifically, the qualitative data in the Generations Study has the potential to illustrate how social policies have potentially both restricted and facilitated development of positive sexual identities and shaped the experiences of minority stress throughout the target generations’ lived experiences. Qualitative data, particularly in the form of narratives, has the potential to illuminate the intersection of lived experience and the social influence of structural factors such as cultural attitudes and social policies (e.g., Frost, 2018 ). Given sexual minorities continue to experience social and health inequalities due to their stigmatized social status ( Meyer, 2016 ), there remains a need for data on how the shifting social climate shapes their identities and lived experiences, in both negative and positive ways.
We recognise that this study is potentially unique in terms of its scope and scale, and not all qualitative researchers interested in similar questions will have access to the same amount of resources for staffing and sampling that Generations had as a result of its federal funding. However, the possibilities produced by the integration of the various component methods (i.e., lifeline drawing, life story interview, identity mapping, narrative reflection) will likely prove useful to researchers who desire the ability to simultaneously understand intersectional identity development and social change by using a single interview protocol. Thus, we intend this integrative aspect of the present methodological approach to be adaptable for future research. Similarly, the processes undertaken to promote methodological integrity in the form of fidelity and utility can serve as useful illustrations of such processes ( Levitt et al., 2017 ) and hopefully prove useful in other team-based qualitative research projects.
The qualitative approach utilized in the Generations Study is not without its limitations. As a result of the scale and collaborative nature of the research, a significant amount of effort was needed to train interviewers and engage a team of researchers across the country in simultaneous data collection efforts, thus posing a challenge to consistency in data collection. As described above, several procedures were implemented to address these concerns and promote methodological integrity, but these may not be possible in smaller scale projects. Further, the scope of the work required a significant amount of burden on the participants and researchers, both in terms of time investment and willingness to engage with emotionally difficult topics in a high degree of depth in the interviews. For these reasons, the degree to which the current approach can be useful in achieving similar aims with a smaller sample remains a question.
Despite these limitations, the success of Generations Study in achieving its aims hinges on its nuanced and multifaceted qualitative approach. Namely, the insights produced from this approach will allow for an understanding of the ways in which social change has shaped the lived experience of three diverse cohorts of sexual minority individuals through the application of life course, narrative, and intersectionality perspectives. This article outlined the qualitative approach utilized to examine the impact of social change with the hope that it can be usefully adapted for other researchers in need of tools to assess the impact of social change on the lived experience of sexual minorities or other populations of people who face the challenge of identity development within rapidly shifting social environments. By combining life course and intersectionality frameworks, along with multiple qualitative methods that allow for a variety of analytical potentials, we hope this integrative qualitative approach will prove valuable in such socially engaged qualitative research efforts.
Supplementary Material
Supplemental materials, contributor information.
David M. Frost, University College London.
Phillip L. Hammack, University of California, Santa Cruz.
Bianca D. M. Wilson, University of California, Los Angeles.
Stephen T. Russell, University of Texas at Austin.
Marguerita Lightfoot, University of California, San Francisco.
Ilan H. Meyer, University of California, Los Angeles.
- Baams L, Grossman AH, & Russell ST (2015). Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth . Developmental Psychology , 51 ( 5 ), 688–696. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barry CA, Britten N, Barber N, Bradley C, & Stevenson F (1999). Using reflexivity to optimize teamwork in qualitative research . Qualitative Health Research , 9 ( 1 ), 26–44. [ PubMed ] [ Google Scholar ]
- Brinkmann S (2016). Methodological breaching experiments: Steps toward theorizing the qualitative interview . Culture & Psychology , 22 ( 4 ), 520–533. [ Google Scholar ]
- Bruce D, Harper GW, & Bauermeister JA (2015). Minority stress, positive identity development, and depressive symptoms: Implications for resilience among sexual minority male youth . Psychology of Sexual Orientation and Gender Diversity , 2 ( 3 ), 287–296. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bowleg L (2008). When Black+ lesbian+ woman≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research . Sex Roles , 59 ( 5–6 ), 312–325. [ Google Scholar ]
- Cho S, Crenshaw KW, & McCall L (2013). Toward a field of intersectionality studies: Theory, applications, and praxis . Signs : Journal of Women in Culture and Society , 38 ( 4 ), 785–810. [ Google Scholar ]
- Clarke V, & Peel E (2005). LGBT psychology and feminist psychology: Bridging the divide . Psychology of Women Section Review , 7 ( 2 ), 4–10. [ Google Scholar ]
- Cohler BJ (1982). Personal narrative and life course. In Baltes P & Brim OG (Eds.), Life span development and behavior (Vol. 4 , pp. 205–241). New York: Academic Press. [ Google Scholar ]
- Cohler BJ (1991). The life story and the study of resilience and response to adversity . Journal of Narrative and Life History , 1 , 169–200. [ Google Scholar ]
- Cohler BJ, & Galatzer-Levy RM (2000). The course of gay and lesbian lives: Social and psychoanalytic perspectives . Chicago, IL: University of Chicago Press. [ Google Scholar ]
- Cohler BJ, & Hammack PL (2007). The psychological world of the gay teenager: Social change, narrative, and “normality .” Journal of Youth and Adolescence , 36 , 47–59. [ Google Scholar ]
- Cole ER (2009). Intersectionality and research in psychology . American Psychologist , 64 ( 3 ), 170–180. [ PubMed ] [ Google Scholar ]
- Crenshaw K (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color . Stanford Law Review , 43 ( 6 ), 1241–1299. [ Google Scholar ]
- Cruwys T, Steffens NK, Haslam SA, Haslam C, Jetten J, et al. (2016). Social Identity Mapping: A procedure for visual representation and assessment of subjective multiple group memberships . British Journal of Social Psychology , 55 , 613–642. [ PubMed ] [ Google Scholar ]
- Dedoose Version 7.0.23, web application for managing, analyzing, and presenting qualitative and mixed method research data (2016). Los Angeles, CA: SocioCultural Research Consultants, LLC; ( www.dedoose.com ). [ Google Scholar ]
- de Vries B, LeBlanc AJ, Frost DM, Alston-Stepnitz E, Stephenson R, & Woodyatt CR (in press). The relationship timeline: A method for the study of shared lived experiences in relational contexts . Advances in Life Course Research . DOI: 10.1016/j.alcr.2016.07.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elder GH (1998). The life course as developmental theory . Child Development , 69 , 1–12. [ PubMed ] [ Google Scholar ]
- Fine M, Torre ME, Frost D, Cabana A, & Avory S (2018). Refusing to check the box. In Gallagher K (Ed.), The methodological dilemma revisited: Creative, critical and collaborative approaches to qualitative research for a new era (p. 11–31). New York, NY: Routledge. [ Google Scholar ]
- Fish JN, & Pasley K (2015). Sexual (minority) trajectories, mental health, and alcohol use: A longitudinal study of youth as they transition to adulthood . Journal of Youth and Adolescence , 44 ( 8 ), 1508–1527. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Floyd FJ, & Bakeman R (2006). Coming-out across the life course: Implications of age and historical context . Archives of Sexual Behavior , 35 ( 3 ), 287–296. [ PubMed ] [ Google Scholar ]
- Frost DM (2011). Stigma and intimacy in same-sex relationships: A narrative approach . Journal of Family Psychology , 25 ( 1 ), 1–10. [ PubMed ] [ Google Scholar ]
- Frost DM (2018). Narrative approaches within a social psychology of social justice: The potential utility of narrative evidence. In Hammack PL (Ed.) The Oxford handbook of social psychology and social justice (pp. 83–93). New York, NY: Oxford University Press. [ Google Scholar ]
- Frost DM, McClelland SI, Clark JB, & Boylan EA (2014). Phenomenological research methods in the psychological study of sexuality. In Tolman D & Diamond L (Eds.), APA handbook of sexuality and psychology (pp. 121–141). Washington D.C.: American Psychological Association Press. [ Google Scholar ]
- Frost DM, Meyer IH, & Hammack PL (2015). Health and well-being in emerging adults’ same-sex relationships: Critical questions and directions for research in developmental science . Emerging Adulthood , 3 ( 1 ), 3–13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Frost DM, & Ouellette SC (2004). Meaningful voices: How psychologists, speaking as psychologists, can inform social policy . Analyses of Social Issues and Public Policy , 4 , 219–226. [ Google Scholar ]
- Frost DM, & Ouellette SC (2011). A search for meaning: Recognizing the potential of narrative research in social policy-making efforts . Sexuality Research & Social Policy , 8 ( 3 ), 151–161. [ Google Scholar ]
- Gergen KJ, Josselson R, & Freeman M (2015). The promises of qualitative inquiry . American Psychologist , 70 ( 1 ), 1–9. [ PubMed ] [ Google Scholar ]
- Gramling LF, & Carr RL (2004). Lifelines: A life history methodology . Nursing Research , 53 ( 3 ), 207–210. [ PubMed ] [ Google Scholar ]
- Grov C, Bimbi DS, Nanín JE, & Parsons JT (2006). Race, ethnicity, gender, and generational factors associated with the coming‐out process among gay, lesbian, and bisexual individuals . Journal of Sex Research , 43 ( 2 ), 115–121. [ PubMed ] [ Google Scholar ]
- Hammack PL (2005). The life course development of human sexual orientation: An integrative paradigm . Human Development , 48 , 267–290. [ Google Scholar ]
- Hammack PL (2006). Identity, conflict, and coexistence: Life stories of Israeli and Palestinian adolescents . Journal of Adolescent Research , 21 ( 4 ), 323–369. [ Google Scholar ]
- Hammack PL (2018). Gay men’s identity development in the twenty-first century: Continuity and change, normalization and resistance . Human Development , 61 , 101–125. doi: 10.1159/000486469 [ CrossRef ] [ Google Scholar ]
- Hammack PL, & Cohler BJ (2009). Narrative engagement and sexual identity: An interdisciplinary approach to the study of sexual lives. In Hammack PL & Cohler BJ (Eds.), The story of sexual identity: Narrative perspectives on the gay and lesbian life course (pp. 3–22). New York, NY: Oxford University Press. [ Google Scholar ]
- Hammack PL, & Cohler BJ (2011). Narrative, identity, and the politics of exclusion: Social change and the gay and lesbian life course . Sexuality Research and Social Policy , 8 , 162–182. [ Google Scholar ]
- Hammack PL, Frost DM, Meyer IH, & Pletta D (2018). Gay men’s health and identity: Social change and the life course . Archives of Sexual Behavior , 47 , 59–74. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hammack PL, Thompson EM, & Pilecki A (2009). Configurations of identity among sexual minority youth: Context, desire, and narrative . Journal of Youth and Adolescence , 38 ( 7 ), 867–883. [ PubMed ] [ Google Scholar ]
- Hammack PL, & Toolis E (2014). Narrative and the social construction of adulthood . New Directions in Child and Adolescent Development , 145 , 43–56. [ PubMed ] [ Google Scholar ]
- Hammack PL, & Toolis E (2015). Identity, politics, and the cultural psychology of adolescence. In Jensen L (Ed.), The Oxford handbook of human development and culture (pp. 396–409). New York, NY: Oxford University Press. [ Google Scholar ]
- Hammack PL, & Toolis EE (2016). Putting the social into personal identity: The master narrative as root metaphor for psychological and developmental science . Human Development , 58 , 350–364. [ Google Scholar ]
- Hatzenbuehler ML (2017). Advancing research on structural stigma and sexual orientation disparities in mental health among youth . Journal of Clinical Child and Adolescent Psychology , 46 ( 3 ), 463–475. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hendricks ML, & Testa RJ (2012). A conceptual framework for clinical work with transgender and gender nonconforming clients . Professional Psychology: Research and Practice , 43 ( 5 ), 460–467. [ Google Scholar ]
- Herek GM, Gillis JR, & Cogan JC (2009). Internalized stigma among sexual minority adults: Insights from a social psychological perspective . Journal of Counseling Psychology , 56 ( 1 ), 32–43. [ Google Scholar ]
- Herek GM, & McLemore KA (2013). Sexual prejudice . Annual Review of Psychology , 64 , 309–333. [ PubMed ] [ Google Scholar ]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis . Qualitative Health Research , 15 ( 9 ), 1277–1288. [ PubMed ] [ Google Scholar ]
- Kahn L (2016). Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12 — United States and selected sites, 2015 . Morbidity and Mortality Weekly Report , 65 ( 9 ), 2–202. [ PubMed ] [ Google Scholar ]
- Levitt HM, Motulsky SL, Wertz FJ, Morrow SL, & Ponterotto JG (2017). Recommendations for designing and reviewing qualitative research in psychology: Promoting methodological integrity . Qualitative Psychology , 4 ( 1 ), 2–22. [ Google Scholar ]
- Lieblich A, Tuval-Mashiach R, & Zilber T (1998). Narrative research: Reading, analysis, and interpretation . Thousand Oaks, CA: Sage. [ Google Scholar ]
- Madill A, & Gough B (2008). Qualitative research and its place in psychological science . Psychological Methods , 13 ( 3 ), 254–271. [ PubMed ] [ Google Scholar ]
- Madill A, Jordan A, & Shirley C (2000). Objectivity and reliability in qualitative analysis: Realist, contextualist and radical constructionist epistemologies . British Journal of Psychology , 91 ( 1 ), 1–20. [ PubMed ] [ Google Scholar ]
- Marshal MP, Dietz LJ, Friedman MS, Stall R, Smith HA, McGinley J, … & Brent DA (2011). Suicidality and depression disparities between sexual minority and heterosexual youth: A meta-analytic review . Journal of Adolescent Health , 49 ( 2 ), 115–123. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martos AJ, Wilson PA, Gordon AR, Lightfoot M, & Meyer IH (2018). “ Like finding a unicorn”: Healthcare preferences among lesbian, gay, and bisexual people in the United States . Social Science & Medicine , 208 , 126–133. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McAdams DP (1990). Unity and purpose in human lives: The emergence of identity as a life story. In Rabin AI, Zucker RA, Emmons RA, & Frank S (Eds.), Studying persons and lives (pp. 148–200). New York, NY: Springer. [ Google Scholar ]
- McAdams DP (1995). The life story interview . Evanston, IL: Northwestern University. [ Google Scholar ]
- McAdams DP (1997). The case for unity in the (post)modern self: A modest proposal. In Ashmore RD & Jussim L (Eds.), Self and identity: Fundamental issues (pp. 46–80). New York, NY: Oxford University Press. [ Google Scholar ]
- McAdams DP, & Bowman PJ (2001). Narrating life’s turning points: Redemption and contamination. In McAdams DP, Josselson R, & Lieblich A (Eds.), Turns in the road: Narrative studies of lives in transition (pp. 3–34). Washington, D.C.: American Psychological Association Press. [ Google Scholar ]
- McAdams DP, Reynolds J, Lewis M, Patten A, & Bowman PJ (2001). When bad things turn good and good things turn bad: Sequences of redemption and contamination in life narrative, and their relation to psychosocial adaptation in midlife adults and in students . Personality and Social Psychology Bulletin , 27 , 472–483. [ Google Scholar ]
- McCall L (2005). The complexity of intersectionality . Signs , 30 ( 3 ), 1771–1800. [ Google Scholar ]
- McCormack M (2013). The declining significance of homophobia . Oxford, UK: Oxford University Press. [ Google Scholar ]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence . Psychological Bulletin , 129 ( 5 ), 674–697. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meyer IH (2015). Resilience in the study of minority stress and health of sexual and gender minorities . Psychology of Sexual Orientation and Gender Diversity , 2 ( 3 ), 209–213. [ Google Scholar ]
- Meyer IH (2016). The elusive promise of LGBT equality . American Journal of Public Health , 106 ( 8 ), 1356–1358. doi: 10.2105/AJPH.2016.303221 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meyer IH, & Frost DM (2013). Minority stress and the health of sexual minorities. In Patterson CJ & D’Augelli AR (Eds.) Handbook of psychology and sexual orientation (pp. 252–266). New York, NY: Oxford University Press. [ Google Scholar ]
- Meyer IH, Schwartz S, & Frost DM (2008). Social patterning of stress and coping: Does disadvantaged social status confer excess exposure and fewer coping resources? Social Science & Medicine , 67 , 368–379. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mishler EG (1986). The analysis of interview-narratives. In Sarbin TR (Ed.), Narrative psychology: The storied nature of human conduct (pp. 233–255). New York: Praeger. [ Google Scholar ]
- Mohr A, & Husain A (2012). The Youth Risk Behavior Survey and sexual minority youth in Wisconsin, 2007–2011 . Madison, WI: Wisconsin Dept. of Health Services. Accessed June 20, 2016. https://www.dhs.wisconsin.gov/publications/p0/p00827.pdf . [ Google Scholar ]
- Narváez RF, Meyer IH, Kertzner RM, Ouellette SC, & Gordon AR (2009). A qualitative approach to the intersection of sexual, ethnic, and gender identities . Identity , 9 ( 1 ), 63–86. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: A meta-analytic review . Clinical Psychology Review , 30 ( 8 ), 1019–1029. [ PubMed ] [ Google Scholar ]
- Peel E (2001). Mundane heterosexism: Understanding incidents of the everyday . Women’s Studies International Forum , 24 , 541–554. [ Google Scholar ]
- Platt J (2012). The history of the interview. In Gubrium JF, Holstein JA, Marvasti AB, & McKinney KD (Eds.), The SAGE handbook of interview research: The complexity of the craft (2nd ed., pp. 9–26). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Polit DF, & Beck CT (2010). Generalization in quantitative and qualitative research: Myths and strategies . International Journal of Nursing Studies , 47 ( 11 ), 1451–1458. 10.1016/J.IJNURSTU.2010.06.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Potter J, & Hepburn A (2005). Qualitative interviews in psychology: Problems and possibilities . Qualitative Research in Psychology , 2 ( 4 ), 281–307. [ Google Scholar ]
- Puckett JA, & Levitt HM (2015). Internalized stigma within sexual and gender minorities: Change strategies and clinical implications . Journal of LGBT Issues in Counseling , 9 ( 4 ), 329–349. [ Google Scholar ]
- Rosenthal L (2016). Incorporating intersectionality into psychology: An opportunity to promote social justice and equity . American Psychologist , 71 ( 6 ), 474–485. [ PubMed ] [ Google Scholar ]
- Russell ST, Clarke TJ, & Clary J (2009). Are teens “post-gay”? Contemporary adolescents’ sexual identity labels . Journal of Youth and Adolescence , 38 ( 7 ), 884–890. [ PubMed ] [ Google Scholar ]
- Russell ST, & Fish JN (2016). Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth . Annual Review of Clinical Psychology , 12 , 465–487. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Savin-Williams RC (2005) The new gay teenager . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Savin-Williams RC (2016). Becoming who I am: Young men on being gay . Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Sirin SR, & Fine M (2007). Hyphenated selves: Muslim American youth negotiating identities on the fault lines of global conflict . Applied Development Science , 11 ( 3 ), 151–163. [ Google Scholar ]
- Stirratt MJ, Meyer IH, Ouellette SC, & Gara MA (2008). Measuring identity multiplicity and intersectionality: Hierarchical classes analysis (HICLAS) of sexual, racial, and gender identities . Self and Identity , 7 ( 1 ), 89–111. [ Google Scholar ]
- Tappan MB (1997). Interpretive psychology: Stories, circles, and understanding lived experience . Journal of Social Issues , 53 ( 4 ), 645–656. [ Google Scholar ]
- Warner LR (2008). A best practices guide to intersectional approaches in psychological research . Sex Roles , 59 ( 5–6 ), 454–463. [ Google Scholar ]
- Watters JK, & Biernacki P (1989). Targeted sampling: options for the study of hidden populations . Social Problems , 36 ( 4 ), 416–430. [ Google Scholar ]
- White AE, Moeller J, Ivcevic Z, & Brackett MA (2018). Gender identity and sexual identity labels used by U.S. high school students: A co-occurrence network analysis . Psychology of Sexual Orientation and Gender Diversity , 5 ( 2 ), 243–252. [ Google Scholar ]
- Wilson BD, Harper GW, Hidalgo MA, Jamil OB, Torres RS, & Isabel Fernandez M (2010). Negotiating dominant masculinity ideology: Strategies used by gay, bisexual and questioning male adolescents. American Journal of Community Psychology , 45 ( 1–2 ), 169–185. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westrate NM, & McLean KC (2010). The rise and fall of gay: A cultural-historical approach to gay identity development . Memory , 18 ( 2 ), 225–240. [ PubMed ] [ Google Scholar ]
How to Conduct Interviews in Qualitative Research: Interview Guidelines for Qualitative Research
Rev › Blog › Market Research › How to Conduct Interviews in Qualitative Research: Interview Guidelines for Qualitative Research
Qualitative research interviews are depth interviews. They elicit detailed feedback from your leads and customers. Unstructured interviews reveal why people react in a certain way or make certain decisions. According to The Hartford , qualitative research provides an anecdotal look into your business. That provides an important form of data.
Why Your Business Should Use a Qualitative Interview Process
Qualitative research helps business owners:
- Identify customer needs
- Clarify marketing messages
- Generate ideas for improvements of a product
- Decide to extend a line or brand
- Gain perspective on how a product fits into a customer’s lifestyle
How Is Conducting Qualitative Research & Quantitative Research Different?
Quantitative research concerns measurable quantities and numbers. It involves close-ended questions. Answer possibilities include yes or no, true or false, or various set choices. Qualitative research is descriptive and concerned with understanding behavior. It invites people to tell their stories in their own words.
Examples of Qualitative Research
Qualitative research helps researchers understand the social reality of individuals, groups and cultures. Qualitative research for businesses involves understanding consumer behavior. It can involve ethnographic techniques, including participant observation and field research. It also includes phenomenology, understanding life experiences using written or recorded narratives. Qualitative research also includes in-depth interviews.
What Is a Qualitative Interview?
A qualitative interview is a more personal form of research compared to questionnaires. The interviewer can probe or ask follow-up research questions of the interview participant. In some cases, subjects may start to interview the interviewer. This fosters deep discussion of the interview topic.
Why Are Interview Techniques in Qualitative Research Effective?
Qualitative research interviews help you explain, understand and explore opinions, behavior and experiences. Qualitative research can provide insights into a phenomenon. Qualitative research discoveries can be further researched and analyzed to influence business decisions.
How Are Interviews in Qualitative Research Formatted?
Qualitative research interviews may take place one-on-one or in focus groups. Learn how to run a successful focus group . Interviews span around 30 to 90 minutes. The interview can take place in person, over the phone or through video chat. The interviewer collects information about opinions, behavior, attitudes, feelings, preferences and knowledge.
How to Conduct Interviews in Qualitative Research
1. determine your goal., 2. target people to interview., 3. design interview questions., 4. prep the interview., 5. conduct the interview., 6. transcribe and analyze the interview., 7. optimize and evolve your interview guide., the first step in qualitative research: determine your goal.
Determine what you want to study:
- A current or potential product, service or brand positioning
- Strengths and weaknesses in products
- Purchasing decisions
- Reactions to advertising or marketing campaigns
- Usability of a website or other interactive services
- Perceptions about the company, brand or product
- Reactions to packaging and design
How Can You Decide a Goal for a Qualitative Interview?
Have your business team ask the following questions:
- What information do you want to get?
- Why do you want to pursue in-depth information about this research topic?
- Why is a qualitative interview process the best solution for this research?
- How will you use qualitative data to improve your business?
How to Determine the Right Interview Participants
When looking for people to talk to for a qualitative interview, consider your goal. If you want to expand a product line, interview existing customers about their needs. If you’re researching marketing, ask new customers how they found your business. Match interview subjects with the goal of the interview.
How to Design Interview Questions for Qualitative Research
When you’re creating an interview guide, it’s a good idea to:
- Plan structured interviews with open ended questions.
- Avoid leading questions.
- Create interview questions that are clear and easy to understand.
- Make research questions focused but flexible.
- Design questions that align with data collection and data analysis goals.
Tips for Preparing a Qualitative Research Interview
Preparation improves interview effectiveness. Tips to prepare include:
- Create an interview guide. The guide should include questions, question intent and answer-based paths to take.
- Choose a setting where the subject feels comfortable.
- Build rapport with interview participants.
- Have a reliable way to record the interview.
- Rehearse the interview first.
Environmental Concerns for Qualitative Interviews
The setting of a qualitative interview also affects the quality of the interview. Consider the needs of the subject. For example, if you’re interviewing a teenager, a formal boardroom may not be the best setting. Some cultures may not value direct eye contact. An interview that’s non-face-to-face may be better.
How to Make Qualitative Interview Subjects Comfortable
For long interviews, offer water and breaks to participants. Be polite and respectful when interacting with interview subjects. Let interview participants know the purpose of the research. Explain exactly how you’ll use their answers. Address terms of confidentiality if necessary. Thank participants after the interview and let them know what to expect next.
What Are Interview Techniques in Qualitative Research?
Qualitative research techniques include:
- Start interviews with “get-to-know-you” questions to put the interview participant at ease.
- Pay attention.
- Use active listening techniques.
- Watch for body language cues.
- Pivot questions as needed.
- Acknowledge emotions.
- Avoid interrogation.
- Ending interviews, ask subjects if they have anything to add.
What Is Active Listening in Interviews in Qualitative Research?
Active listening techniques include:
- Make eye contact.
- Lean in and use body language to show you’re listening.
- Don’t get distracted by devices.
- Use verbal affirmation.
- Paraphrase answers for reflection.
- Reference earlier answers.
- Avoid interrupting.
- Embrace pauses.
- Ask for clarification.
- Pay attention in the moment.
Tips for Transcribing a Qualitative Interview
It’s best to transcribe and analyze a qualitative research interview right away. This helps you optimize future interviews. Transcribe the interview word for word. Note non-verbal interactions in your transcription. Interactions like pauses and laughter can provide deeper insights into responses.
How to Analyze a Qualitative Interview
Analyze your qualitative research data early. That way, you can identify emerging themes to shape future interviews. Consider adding these to each interview report:
- The goal of the interview
- Details about the interview participant
- Questions asked, summarized responses and key findings
- Recommendations
Relate the analysis to the goal of the qualitative research interview.
Optimize the Interview Guide for Qualitative Research
Each interview can help you improve the efficiency and effectiveness of future ones. Adjust your interview guide based on insights from each previous interview. Keep all versions of your transcriptions and interview guides with notes on them. You can reference these for future qualitative research.
Get Reliable Transcription Services for Qualitative Research Interviews
As mentioned, you should transcribe qualitative research interviews as soon as possible. There are several reasons for this.
- You can gain insights that help you shape your interview guide. You might identify questions to add or questions to clarify.
- Your interview participants may not be appropriate for this type of qualitative research. Finding more targeted interview subjects may be better.
- Answers may evolve the qualitative research goal and/or data analysis.
At Rev, we understand the need for fast transcription for accurate market research. We provide a turnaround time of as few as 12 hours, no matter how big your project is. We guarantee 99%+ accuracy. Learn about Rev’s market research transcription . We can help make your qualitative research project a success.
Download our FREE Qualitative Research Interview Checklist
Everybody’s favorite speech-to-text blog.
We combine AI and a huge community of freelancers to make speech-to-text greatness every day. Wanna hear more about it?
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 22 March 2008
Methods of data collection in qualitative research: interviews and focus groups
- P. Gill 1 ,
- K. Stewart 2 ,
- E. Treasure 3 &
- B. Chadwick 4
British Dental Journal volume 204 , pages 291–295 ( 2008 ) Cite this article
1.70m Accesses
1066 Citations
46 Altmetric
Metrics details
Interviews and focus groups are the most common methods of data collection used in qualitative healthcare research
Interviews can be used to explore the views, experiences, beliefs and motivations of individual participants
Focus group use group dynamics to generate qualitative data
Qualitative research in dentistry
Conducting qualitative interviews with school children in dental research
Analysing and presenting qualitative data
This paper explores the most common methods of data collection used in qualitative research: interviews and focus groups. The paper examines each method in detail, focusing on how they work in practice, when their use is appropriate and what they can offer dentistry. Examples of empirical studies that have used interviews or focus groups are also provided.
You have full access to this article via your institution.
Similar content being viewed by others

Interviews in the social sciences

A review of technical and quality assessment considerations of audio-visual and web-conferencing focus groups in qualitative health research
Professionalism in dentistry: deconstructing common terminology, introduction.
Having explored the nature and purpose of qualitative research in the previous paper, this paper explores methods of data collection used in qualitative research. There are a variety of methods of data collection in qualitative research, including observations, textual or visual analysis (eg from books or videos) and interviews (individual or group). 1 However, the most common methods used, particularly in healthcare research, are interviews and focus groups. 2 , 3
The purpose of this paper is to explore these two methods in more detail, in particular how they work in practice, the purpose of each, when their use is appropriate and what they can offer dental research.
Qualitative research interviews
There are three fundamental types of research interviews: structured, semi-structured and unstructured. Structured interviews are, essentially, verbally administered questionnaires, in which a list of predetermined questions are asked, with little or no variation and with no scope for follow-up questions to responses that warrant further elaboration. Consequently, they are relatively quick and easy to administer and may be of particular use if clarification of certain questions are required or if there are likely to be literacy or numeracy problems with the respondents. However, by their very nature, they only allow for limited participant responses and are, therefore, of little use if 'depth' is required.
Conversely, unstructured interviews do not reflect any preconceived theories or ideas and are performed with little or no organisation. 4 Such an interview may simply start with an opening question such as 'Can you tell me about your experience of visiting the dentist?' and will then progress based, primarily, upon the initial response. Unstructured interviews are usually very time-consuming (often lasting several hours) and can be difficult to manage, and to participate in, as the lack of predetermined interview questions provides little guidance on what to talk about (which many participants find confusing and unhelpful). Their use is, therefore, generally only considered where significant 'depth' is required, or where virtually nothing is known about the subject area (or a different perspective of a known subject area is required).
Semi-structured interviews consist of several key questions that help to define the areas to be explored, but also allows the interviewer or interviewee to diverge in order to pursue an idea or response in more detail. 2 This interview format is used most frequently in healthcare, as it provides participants with some guidance on what to talk about, which many find helpful. The flexibility of this approach, particularly compared to structured interviews, also allows for the discovery or elaboration of information that is important to participants but may not have previously been thought of as pertinent by the research team.
For example, in a recent dental public heath study, 5 school children in Cardiff, UK were interviewed about their food choices and preferences. A key finding that emerged from semi-structured interviews, which was not previously thought to be as highly influential as the data subsequently confirmed, was the significance of peer-pressure in influencing children's food choices and preferences. This finding was also established primarily through follow-up questioning (eg probing interesting responses with follow-up questions, such as 'Can you tell me a bit more about that?') and, therefore, may not have emerged in the same way, if at all, if asked as a predetermined question.
The purpose of research interviews
The purpose of the research interview is to explore the views, experiences, beliefs and/or motivations of individuals on specific matters (eg factors that influence their attendance at the dentist). Qualitative methods, such as interviews, are believed to provide a 'deeper' understanding of social phenomena than would be obtained from purely quantitative methods, such as questionnaires. 1 Interviews are, therefore, most appropriate where little is already known about the study phenomenon or where detailed insights are required from individual participants. They are also particularly appropriate for exploring sensitive topics, where participants may not want to talk about such issues in a group environment.
Examples of dental studies that have collected data using interviews are 'Examining the psychosocial process involved in regular dental attendance' 6 and 'Exploring factors governing dentists' treatment philosophies'. 7 Gibson et al . 6 provided an improved understanding of factors that influenced people's regular attendance with their dentist. The study by Kay and Blinkhorn 7 provided a detailed insight into factors that influenced GDPs' decision making in relation to treatment choices. The study found that dentists' clinical decisions about treatments were not necessarily related to pathology or treatment options, as was perhaps initially thought, but also involved discussions with patients, patients' values and dentists' feelings of self esteem and conscience.
There are many similarities between clinical encounters and research interviews, in that both employ similar interpersonal skills, such as questioning, conversing and listening. However, there are also some fundamental differences between the two, such as the purpose of the encounter, reasons for participating, roles of the people involved and how the interview is conducted and recorded. 8
The primary purpose of clinical encounters is for the dentist to ask the patient questions in order to acquire sufficient information to inform decision making and treatment options. However, the constraints of most consultations are such that any open-ended questioning needs to be brought to a conclusion within a fairly short time. 2 In contrast, the fundamental purpose of the research interview is to listen attentively to what respondents have to say, in order to acquire more knowledge about the study topic. 9 Unlike the clinical encounter, it is not to intentionally offer any form of help or advice, which many researchers have neither the training nor the time for. Research interviewing therefore requires a different approach and a different range of skills.
The interview
When designing an interview schedule it is imperative to ask questions that are likely to yield as much information about the study phenomenon as possible and also be able to address the aims and objectives of the research. In a qualitative interview, good questions should be open-ended (ie, require more than a yes/no answer), neutral, sensitive and understandable. 2 It is usually best to start with questions that participants can answer easily and then proceed to more difficult or sensitive topics. 2 This can help put respondents at ease, build up confidence and rapport and often generates rich data that subsequently develops the interview further.
As in any research, it is often wise to first pilot the interview schedule on several respondents prior to data collection proper. 8 This allows the research team to establish if the schedule is clear, understandable and capable of answering the research questions, and if, therefore, any changes to the interview schedule are required.
The length of interviews varies depending on the topic, researcher and participant. However, on average, healthcare interviews last 20-60 minutes. Interviews can be performed on a one-off or, if change over time is of interest, repeated basis, 4 for example exploring the psychosocial impact of oral trauma on participants and their subsequent experiences of cosmetic dental surgery.
Developing the interview
Before an interview takes place, respondents should be informed about the study details and given assurance about ethical principles, such as anonymity and confidentiality. 2 This gives respondents some idea of what to expect from the interview, increases the likelihood of honesty and is also a fundamental aspect of the informed consent process.
Wherever possible, interviews should be conducted in areas free from distractions and at times and locations that are most suitable for participants. For many this may be at their own home in the evenings. Whilst researchers may have less control over the home environment, familiarity may help the respondent to relax and result in a more productive interview. 9 Establishing rapport with participants prior to the interview is also important as this can also have a positive effect on the subsequent development of the interview.
When conducting the actual interview it is prudent for the interviewer to familiarise themselves with the interview schedule, so that the process appears more natural and less rehearsed. However, to ensure that the interview is as productive as possible, researchers must possess a repertoire of skills and techniques to ensure that comprehensive and representative data are collected during the interview. 10 One of the most important skills is the ability to listen attentively to what is being said, so that participants are able to recount their experiences as fully as possible, without unnecessary interruptions.
Other important skills include adopting open and emotionally neutral body language, nodding, smiling, looking interested and making encouraging noises (eg, 'Mmmm') during the interview. 2 The strategic use of silence, if used appropriately, can also be highly effective at getting respondents to contemplate their responses, talk more, elaborate or clarify particular issues. Other techniques that can be used to develop the interview further include reflecting on remarks made by participants (eg, 'Pain?') and probing remarks ('When you said you were afraid of going to the dentist what did you mean?'). 9 Where appropriate, it is also wise to seek clarification from respondents if it is unclear what they mean. The use of 'leading' or 'loaded' questions that may unduly influence responses should always be avoided (eg, 'So you think dental surgery waiting rooms are frightening?' rather than 'How do you find the waiting room at the dentists?').
At the end of the interview it is important to thank participants for their time and ask them if there is anything they would like to add. This gives respondents an opportunity to deal with issues that they have thought about, or think are important but have not been dealt with by the interviewer. 9 This can often lead to the discovery of new, unanticipated information. Respondents should also be debriefed about the study after the interview has finished.
All interviews should be tape recorded and transcribed verbatim afterwards, as this protects against bias and provides a permanent record of what was and was not said. 8 It is often also helpful to make 'field notes' during and immediately after each interview about observations, thoughts and ideas about the interview, as this can help in data analysis process. 4 , 8
Focus groups
Focus groups share many common features with less structured interviews, but there is more to them than merely collecting similar data from many participants at once. A focus group is a group discussion on a particular topic organised for research purposes. This discussion is guided, monitored and recorded by a researcher (sometimes called a moderator or facilitator). 11 , 12
Focus groups were first used as a research method in market research, originating in the 1940s in the work of the Bureau of Applied Social Research at Columbia University. Eventually the success of focus groups as a marketing tool in the private sector resulted in its use in public sector marketing, such as the assessment of the impact of health education campaigns. 13 However, focus group techniques, as used in public and private sectors, have diverged over time. Therefore, in this paper, we seek to describe focus groups as they are used in academic research.
When focus groups are used
Focus groups are used for generating information on collective views, and the meanings that lie behind those views. They are also useful in generating a rich understanding of participants' experiences and beliefs. 12 Suggested criteria for using focus groups include: 13
As a standalone method, for research relating to group norms, meanings and processes
In a multi-method design, to explore a topic or collect group language or narratives to be used in later stages
To clarify, extend, qualify or challenge data collected through other methods
To feedback results to research participants.
Morgan 12 suggests that focus groups should be avoided according to the following criteria:
If listening to participants' views generates expectations for the outcome of the research that can not be fulfilled
If participants are uneasy with each other, and will therefore not discuss their feelings and opinions openly
If the topic of interest to the researcher is not a topic the participants can or wish to discuss
If statistical data is required. Focus groups give depth and insight, but cannot produce useful numerical results.
Conducting focus groups: group composition and size
The composition of a focus group needs great care to get the best quality of discussion. There is no 'best' solution to group composition, and group mix will always impact on the data, according to things such as the mix of ages, sexes and social professional statuses of the participants. What is important is that the researcher gives due consideration to the impact of group mix (eg, how the group may interact with each other) before the focus group proceeds. 14
Interaction is key to a successful focus group. Sometimes this means a pre-existing group interacts best for research purposes, and sometimes stranger groups. Pre-existing groups may be easier to recruit, have shared experiences and enjoy a comfort and familiarity which facilitates discussion or the ability to challenge each other comfortably. In health settings, pre-existing groups can overcome issues relating to disclosure of potentially stigmatising status which people may find uncomfortable in stranger groups (conversely there may be situations where disclosure is more comfortable in stranger groups). In other research projects it may be decided that stranger groups will be able to speak more freely without fear of repercussion, and challenges to other participants may be more challenging and probing, leading to richer data. 13
Group size is an important consideration in focus group research. Stewart and Shamdasani 14 suggest that it is better to slightly over-recruit for a focus group and potentially manage a slightly larger group, than under-recruit and risk having to cancel the session or having an unsatisfactory discussion. They advise that each group will probably have two non-attenders. The optimum size for a focus group is six to eight participants (excluding researchers), but focus groups can work successfully with as few as three and as many as 14 participants. Small groups risk limited discussion occurring, while large groups can be chaotic, hard to manage for the moderator and frustrating for participants who feel they get insufficient opportunities to speak. 13
Preparing an interview schedule
Like research interviews, the interview schedule for focus groups is often no more structured than a loose schedule of topics to be discussed. However, in preparing an interview schedule for focus groups, Stewart and Shamdasani 14 suggest two general principles:
Questions should move from general to more specific questions
Question order should be relative to importance of issues in the research agenda.
There can, however, be some conflict between these two principles, and trade offs are often needed, although often discussions will take on a life of their own, which will influence or determine the order in which issues are covered. Usually, less than a dozen predetermined questions are needed and, as with research interviews, the researcher will also probe and expand on issues according to the discussion.
Moderating a focus group looks easy when done well, but requires a complex set of skills, which are related to the following principles: 15
Participants have valuable views and the ability to respond actively, positively and respectfully. Such an approach is not simply a courtesy, but will encourage fruitful discussions
Moderating without participating: a moderator must guide a discussion rather than join in with it. Expressing one's own views tends to give participants cues as to what to say (introducing bias), rather than the confidence to be open and honest about their own views
Be prepared for views that may be unpalatably critical of a topic which may be important to you
It is important to recognise that researchers' individual characteristics mean that no one person will always be suitable to moderate any kind of group. Sometimes the characteristics that suit a moderator for one group will inhibit discussion in another
Be yourself. If the moderator is comfortable and natural, participants will feel relaxed.
The moderator should facilitate group discussion, keeping it focussed without leading it. They should also be able to prevent the discussion being dominated by one member (for example, by emphasising at the outset the importance of hearing a range of views), ensure that all participants have ample opportunity to contribute, allow differences of opinions to be discussed fairly and, if required, encourage reticent participants. 13
Other relevant factors
The venue for a focus group is important and should, ideally, be accessible, comfortable, private, quiet and free from distractions. 13 However, while a central location, such as the participants' workplace or school, may encourage attendance, the venue may affect participants' behaviour. For example, in a school setting, pupils may behave like pupils, and in clinical settings, participants may be affected by any anxieties that affect them when they attend in a patient role.
Focus groups are usually recorded, often observed (by a researcher other than the moderator, whose role is to observe the interaction of the group to enhance analysis) and sometimes videotaped. At the start of a focus group, a moderator should acknowledge the presence of the audio recording equipment, assure participants of confidentiality and give people the opportunity to withdraw if they are uncomfortable with being taped. 14
A good quality multi-directional external microphone is recommended for the recording of focus groups, as internal microphones are rarely good enough to cope with the variation in volume of different speakers. 13 If observers are present, they should be introduced to participants as someone who is just there to observe, and sit away from the discussion. 14 Videotaping will require more than one camera to capture the whole group, as well as additional operational personnel in the room. This is, therefore, very obtrusive, which can affect the spontaneity of the group and in a focus group does not usually yield enough additional information that could not be captured by an observer to make videotaping worthwhile. 15
The systematic analysis of focus group transcripts is crucial. However, the transcription of focus groups is more complex and time consuming than in one-to-one interviews, and each hour of audio can take up to eight hours to transcribe and generate approximately 100 pages of text. Recordings should be transcribed verbatim and also speakers should be identified in a way that makes it possible to follow the contributions of each individual. Sometimes observational notes also need to be described in the transcripts in order for them to make sense.
The analysis of qualitative data is explored in the final paper of this series. However, it is important to note that the analysis of focus group data is different from other qualitative data because of their interactive nature, and this needs to be taken into consideration during analysis. The importance of the context of other speakers is essential to the understanding of individual contributions. 13 For example, in a group situation, participants will often challenge each other and justify their remarks because of the group setting, in a way that perhaps they would not in a one-to-one interview. The analysis of focus group data must therefore take account of the group dynamics that have generated remarks.
Focus groups in dental research
Focus groups are used increasingly in dental research, on a diverse range of topics, 16 illuminating a number of areas relating to patients, dental services and the dental profession. Addressing a special needs population difficult to access and sample through quantitative measures, Robinson et al . 17 used focus groups to investigate the oral health-related attitudes of drug users, exploring the priorities, understandings and barriers to care they encounter. Newton et al . 18 used focus groups to explore barriers to services among minority ethnic groups, highlighting for the first time differences between minority ethnic groups. Demonstrating the use of the method with professional groups as subjects in dental research, Gussy et al . 19 explored the barriers to and possible strategies for developing a shared approach in prevention of caries among pre-schoolers. This mixed method study was very important as the qualitative element was able to explain why the clinical trial failed, and this understanding may help researchers improve on the quantitative aspect of future studies, as well as making a valuable academic contribution in its own right.
Interviews and focus groups remain the most common methods of data collection in qualitative research, and are now being used with increasing frequency in dental research, particularly to access areas not amendable to quantitative methods and/or where depth, insight and understanding of particular phenomena are required. The examples of dental studies that have employed these methods also help to demonstrate the range of research contexts to which interview and focus group research can make a useful contribution. The continued employment of these methods can further strengthen many areas of dentally related work.
Silverman D . Doing qualitative research . London: Sage Publications, 2000.
Google Scholar
Britten N . Qualitative interviews in healthcare. In Pope C, Mays N (eds) Qualitative research in health care . 2nd ed. pp 11–19. London: BMJ Books, 1999.
Legard R, Keegan J, Ward K . In-depth interviews. In Ritchie J, Lewis J (eds) Qualitative research practice: a guide for social science students and researchers . pp 139–169. London: Sage Publications, 2003.
May K M . Interview techniques in qualitative research: concerns and challenges. In Morse J M (ed) Qualitative nursing research . pp 187–201. Newbury Park: Sage Publications, 1991.
Stewart K, Gill P, Treasure E, Chadwick B . Understanding about food among 6-11 year olds in South Wales. Food Culture Society 2006; 9 : 317–333.
Article Google Scholar
Gibson B, Drenna J, Hanna S, Freeman R . An exploratory qualitative study examining the social and psychological processes involved in regular dental attendance. J Public Health Dent 2000; 60 : 5–11.
Kay E J, Blinkhorn A S . A qualitative investigation of factors governing dentists' treatment philosophies. Br Dent J 1996; 180 : 171–176.
Pontin D . Interviews. In Cormack D F S (ed) The research process in nursing . 4th ed. pp 289–298. Oxford: Blackwell Science, 2000.
Kvale S . Interviews . Thousand Oaks: Sage Publications, 1996.
Hammersley M, Atkinson P . Ethnography: principles in practice . 2nd ed. London: Routledge, 1995.
Kitzinger J . The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illn 1994; 16 : 103–121.
Morgan D L . The focus group guide book . London: Sage Publications, 1998.
Book Google Scholar
Bloor M, Frankland J, Thomas M, Robson K . Focus groups in social research . London: Sage Publications, 2001.
Stewart D W, Shamdasani P M . Focus groups. Theory and practice . London: Sage Publications, 1990.
Krueger R A . Moderating focus groups . London: Sage Publications, 1998.
Chestnutt I G, Robson K F. Focus groups – what are they? Dent Update 2002; 28 : 189–192.
Robinson P G, Acquah S, Gibson B . Drug users: oral health related attitudes and behaviours. Br Dent J 2005; 198 : 219–224.
Newton J T, Thorogood N, Bhavnani V, Pitt J, Gibbons D E, Gelbier S . Barriers to the use of dental services by individuals from minority ethnic communities living in the United Kingdom: findings from focus groups. Primary Dent Care 2001; 8 : 157–161.
Gussy M G, Waters E, Kilpatrick M . A qualitative study exploring barriers to a model of shared care for pre-school children's oral health. Br Dent J 2006; 201 : 165–170.
Download references
Author information
Authors and affiliations.
Senior Research Fellow, Faculty of Health, Sport and Science, University of Glamorgan, Pontypridd, CF37 1DL,
Research Fellow, Academic Unit of Primary Care, University of Bristol, Bristol, BS8 2AA,
Dean and Professor of Dental Public Health, School of Dentistry, Dental Health and Biological Sciences, School of Dentistry, Cardiff University, Heath Park, Cardiff, CF14 4XY,
E. Treasure
Professor of Paediatric Dentistry, School of Dentistry, Dental Health and Biological Sciences, School of Dentistry, Cardiff University, Heath Park, Cardiff, CF14 4XY,
B. Chadwick
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to P. Gill .
Additional information
Refereed paper
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gill, P., Stewart, K., Treasure, E. et al. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 204 , 291–295 (2008). https://doi.org/10.1038/bdj.2008.192
Download citation
Published : 22 March 2008
Issue Date : 22 March 2008
DOI : https://doi.org/10.1038/bdj.2008.192
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Imprisonment for south ethiopian people living with hiv presents a double health burden: lived experiences of prisoners.
- Terefe Gone Fuge
- George Tsourtos
- Emma R Miller
BMC Health Services Research (2024)
Employees’ experiences of a large-scale implementation in a public care setting: a novel mixed-method approach to content analysis
- My Säfström
- Ulrika Löfkvist
Translating brand reputation into equity from the stakeholder’s theory: an approach to value creation based on consumer’s perception & interactions
- Olukorede Adewole
International Journal of Corporate Social Responsibility (2024)

Nurses’ and patients’ perceptions of physical health screening for patients with schizophrenia spectrum disorders: a qualitative study
- Camilla Långstedt
- Daniel Bressington
- Maritta Välimäki
BMC Nursing (2024)
Heteronormative biases and distinctive experiences with prostate cancer among men who have sex with men: a qualitative focus group study
- Evan Panken
- Noah Frydenlund
- Channa Amarasekera
BMC Urology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A qualitative exploration of barriers to efficient and effective structured medication reviews in primary care: Findings from the DynAIRx study
Roles Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing
Affiliations Academic Unit for Ageing & Stroke Research, Bradford Teaching Hospitals NHS Foundation Trust, University of Leeds, Bradford, United Kingdom, Faculty of Medicine and Health, School of Medicine, University of Leeds, Leeds, United Kingdom
Roles Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing
Affiliation Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliations Institute of Population Health, University of Liverpool, Liverpool, United Kingdom, Directorate of Mental Health and Learning Disabilities, Powys Teaching Health Board, Bronllys, United Kingdom
Roles Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing
Affiliation General Practice and Primary Care, School of Health and Wellbeing, University of Glasgow, Glasgow, United Kingdom
Roles Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing
Roles Conceptualization, Supervision, Writing – review & editing
Roles Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing
Roles Writing – review & editing
Affiliations Faculty of Medicine and Health, School of Medicine, University of Leeds, Leeds, United Kingdom, Leeds Institute for Data Analytics, University of Leeds, Leeds, United Kingdom
Roles Conceptualization, Writing – review & editing
Affiliation Department of Computer Science, University of Liverpool, Liverpool, United Kingdom
Affiliation Division of Informatics, Imaging & Data Science, University of Manchester, Manchester, United Kingdom
Affiliation NIHR Applied Research Collaboration North West Coast, United Kingdom
Affiliations Leeds Institute for Data Analytics, University of Leeds, Leeds, United Kingdom, School of Computing, University of Leeds, Leeds, United Kingdom
Roles Project administration, Resources
Affiliation Department of Electrical Engineering and Electronics, University of Liverpool, Liverpool, United Kingdom
Affiliation Merseycare NHS Foundation Trust, Liverpool, United Kingdom
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Writing – review & editing
- [ ... ],
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Centre for Experimental Therapeutics, University of Liverpool, Liverpool, United Kingdom, Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom
- [ view all ]
- [ view less ]
- Aseel S. Abuzour,
- Samantha A. Wilson,
- Alan A. Woodall,
- Frances S. Mair,
- Andrew Clegg,
- Eduard Shantsila,
- Mark Gabbay,
- Michael Abaho,
- Asra Aslam,

- Published: August 30, 2024
- https://doi.org/10.1371/journal.pone.0299770
- Reader Comments
Introduction
Structured medication reviews (SMRs), introduced in the United Kingdom (UK) in 2020, aim to enhance shared decision-making in medication optimisation, particularly for patients with multimorbidity and polypharmacy. Despite its potential, there is limited empirical evidence on the implementation of SMRs, and the challenges faced in the process. This study is part of a larger DynAIRx (Artificial Intelligence for dynamic prescribing optimisation and care integration in multimorbidity) project which aims to introduce Artificial Intelligence (AI) to SMRs and develop machine learning models and visualisation tools for patients with multimorbidity. Here, we explore how SMRs are currently undertaken and what barriers are experienced by those involved in them.
Qualitative focus groups and semi-structured interviews took place between 2022–2023. Six focus groups were conducted with doctors, pharmacists and clinical pharmacologists (n = 21), and three patient focus groups with patients with multimorbidity (n = 13). Five semi-structured interviews were held with 2 pharmacists, 1 trainee doctor, 1 policy-maker and 1 psychiatrist. Transcripts were analysed using thematic analysis.
Two key themes limiting the effectiveness of SMRs in clinical practice were identified: ‘Medication Reviews in Practice’ and ‘Medication-related Challenges’. Participants noted limitations to the efficient and effectiveness of SMRs in practice including the scarcity of digital tools for identifying and prioritising patients for SMRs; organisational and patient-related challenges in inviting patients for SMRs and ensuring they attend; the time-intensive nature of SMRs, the need for multiple appointments and shared decision-making; the impact of the healthcare context on SMR delivery; poor communication and data sharing issues between primary and secondary care; difficulties in managing mental health medications and specific challenges associated with anticholinergic medication.
SMRs are complex, time consuming and medication optimisation may require multiple follow-up appointments to enable a comprehensive review. There is a need for a prescribing support system to identify, prioritise and reduce the time needed to understand the patient journey when dealing with large volumes of disparate clinical information in electronic health records. However, monitoring the effects of medication optimisation changes with a feedback loop can be challenging to establish and maintain using current electronic health record systems.
Citation: Abuzour AS, Wilson SA, Woodall AA, Mair FS, Clegg A, Shantsila E, et al. (2024) A qualitative exploration of barriers to efficient and effective structured medication reviews in primary care: Findings from the DynAIRx study. PLoS ONE 19(8): e0299770. https://doi.org/10.1371/journal.pone.0299770
Editor: Kathleen Bennett, Royal College of Surgeons in Ireland, IRELAND
Received: February 16, 2024; Accepted: June 24, 2024; Published: August 30, 2024
Copyright: © 2024 Abuzour et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: DynAIRx has been funded by the National Institute for Health and Care Research (NIHR) Artificial Intelligence for Multiple Long-Term Conditions (AIM) call (NIHR 203986). MG is partly funded by the NIHR Applied Research Collaboration North West Coast (ARC NWC). AW is partly funded by a Health and Care Research Wales Research Time Award (NHS-RTA-21-02). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. This research is supported by the NIHR ARC NWC. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Competing interests: No competing interests
Structured medication reviews (SMRs) were introduced in the United Kingdom (UK) in October 2020 and incorporated into the NHS England Directed Enhanced Service (DES) contract for 2021 [ 1 ]. SMRs represent a National Institute for Health and Care Excellence (NICE)-approved clinical intervention facilitating shared-decision making between clinicians and patients, to inform treatment decisions. The objective is to reduce medication-related harm in patients with complex or problematic polypharmacy [ 1 , 2 ]. While General Practitioners (GPs), pharmacists and advanced nurse practitioners (ANPs) who meet training criteria can conduct SMRs, the prevailing expectation is for clinical pharmacists within Primary Care Networks (PCNs) to assume primary responsibility as a commissioned service [ 3 ]. The varied methods employed by PCNs to proactively identify patients suitable for SMRs, and conduct these reviews, is contingent on available resources and capacity. Anecdotal evidence suggests that PCNs currently use limited digital tools, such as searching electronic health records (EHR) based on the total number of drugs prescribed or disease codes, to identify patients at risk of medication-related harm.
There is sparse empirical evidence reporting on the implementation of SMRs, their impact on patient outcomes, and the challenges faced by healthcare professionals (HCPs) and patients during SMRs [ 4 , 5 ]. This scarcity of evidence is unsurprising given that SMRs were introduced in 2020 amidst the COVID-19 pandemic [ 1 ]. Nonetheless, estimates suggest a percentage reduction in per-patient medicines following an SMR ranging from 2.7% to 9.9%, with up to 19.5% reduction in use for the highest-risk group in care homes [ 6 ].
Patients with complex multimorbidity and polypharmacy, whose medicines have not been optimised are at risk of adverse outcomes and medication-related harm [ 7 ]. The definition of complex multimorbidity is contentious [ 8 ] but here we are referring to patients living with four or more conditions, which is strongly associated with polypharmacy [ 8 , 9 ]. The use of data from EHRs to develop evidence-based digital health tools can be a promising resource to assist HCPs in conducting targeted, efficient and effective SMRs.
The NIHR-funded DynAIRx study (Artificial Intelligence for dynamic prescribing optimisation and care integration in multimorbidity) aims to develop AI-driven tools that integrate information from electronic health and social care records, clinical guidelines and risk-prediction models in order to support the delivery of SMRs [ 10 ]. The DynAIRx project will produce machine learning models, dashboards, and different tools including Causal Inferencing to provide clinicians and patients with evidence-based information to prioritise patients at most risk of harm and/or patients most likely to benefit from SMRs. Aligned with the NICE multimorbidity guidelines, [ 7 , 11 ] DynAIRx will focus on three patient groups at high-risk of rapidly worsening health from multimorbidity: (a) individuals with mental and physical health co-morbidity, [ 12 – 14 ] in whom the prescribing for mental health improvement can lead to adverse physical health consequences; (b) those with complex multimorbidity (four or more long-term health conditions taking ten or more drugs); [ 9 , 15 ] and (c) older people with frailty who are at high risk of adverse outcomes [ 16 ].
The initial step towards introducing AI-driven prescribing support tools into clinical practice involves understanding the current scope of work, how SMRs are presently undertaken and by whom, the time required in real-world clinical practice to undertake them, and crucially, investigate what determinants act as potential barriers to efficient and effective SMR implementation. The aim of this study was to explore how SMRs are undertaken and what barriers those undertaking them (and receiving them) experience.
Participants and recruitment
This study sought to recruit health care or management professionals working in health care settings (primary care in the community or secondary care in hospital services) across the UK where review of prescription medications is a regular part of the clinical workload. This included those working in General Practice, secondary care hospital services (geriatric medicine, clinical pharmacology, falls clinics, mental health practitioners), clinical commissioning of services or management of clinical services (practice managers), and pharmacists, including PCN pharmacists (those involved in conducting SMRs across several neighbouring GP practices). Patient participants included those with (a) multiple and physical co-morbidities; (b) complex multimorbidity; (c) older people with frailty. Patient and carer representatives of the three key multimorbidity groups outlined above were also invited. This included recruiting adult individuals (over the age of 18) with/or caring for someone with multiple (4 or more) long-term health conditions, co-existing mental and physical health problems, prescribed ≥10 regular medications, frailty.
Purposive sampling identified potential HCP participants that were known to be involved in medicines optimisation services through the researchers own clinical and professional networks. Snowballing (wherein research participants were asked to assist the recruitment by attempting to identify other potential participants) was employed to identify contacts through existing service providers along with advertisement in GP forums and at national events for individuals participating in clinical polypharmacy research [ 17 ]. Purposive sampling of potential patient representatives were identified through advertisement across the NIHR Applied Research Collaboration public advisor networks and through research databases at the researchers host institutions. Potential participants were provided with study information and an invitation to participate. Participants received comprehensive briefings from researchers about the study, and written consent was obtained prior to the focus group or interview participation. Withdrawal of consent was permitted at any stage, even after the focus group or interview.
Ethical approval
The Newcastle North Tyneside Research Ethics Committee (REC reference:22/NE/0088) granted ethical approval for the DynAIRx study.
Data collection
Data collection occurred from November 2022 to November 2023. Focus groups and semi-structured interviews were conducted to gather participant views. Focus groups were utilised for patient participants in order to stimulate discussion of common and shared experiences. Individual interviews supplemented the HCP focus groups in order to ensure as many HCPs could be involved as possible owing to time constraints for some HCPs. Focus group topic guides and interview schedules were developed and refined by the clinical members of the research team (LW, AA, AW, FM, AG) and tailored to HCP and patient groups. The topic guides (see S1 Appendix ) included questions exploring the experience of conducting or receiving SMRs, barriers to undertaking them and opinions on key medication challenges in multimorbidity groups from both the clinician and patient perspective. Sessions occurred in person and online (via Microsoft Teams), lasting from 49 to 109 minutes. Audio recordings underwent verbatim transcription and anonymisation to remove any potentially identifiable information. Each participant was assigned a code, and recordings were subsequently deleted. Data collection and analysis occurred concurrently. The Consolidated Criteria for Reporting Qualitative Research checklist was used to ensure comprehensive reporting of our qualitative study (see S1 Appendix ). No participant withdrew consent for their data to be used in the study.
Data analysis
Transcripts were imported into QSR NVivo 12® and analysed using thematic analysis [ 18 ]. Transcripts were read to familiarise researchers with the data. Inductive reasoning guided the initial coding by AA and SW, who collated and examined codes to identify themes. The multidisciplinary coding team (AA, SW, LW, AW, FM) consisted of clinicians and researchers, and engaged in regular reflexive practices to ensure a rigorous and transparent qualitative study. Recognising the diverse expertise and perspectives within the team, we held regular coding clinics where codes and initial themes were reviewed and discussed. By openly sharing our perspectives and challenging each other’s viewpoints, we aimed to balance our interpretations and avoid overemphasis on any single disciplinary lens. This allowed us to critically examine how our professional backgrounds and assumptions might shape the interpretation of findings. These reflexive sessions were instrumental in identifying and mitigating biases, ensuring that our analysis remained grounded in the participants’ narratives rather than our preconceptions. Themes were defined and supported by quotes. Detailed notes of discussions and developments were kept to ensure analytical rigour and plausibility [ 19 ]. The remaining dataset underwent hybrid inductive and deductive thematic analysis using the inductively defined themes, with codes and themes iteratively revised. Once all team members agreed no new codes or meaning to influence thematic analysis were emerging, we assumed saturation was achieved [ 20 ]. At this point, further recruitment was stopped.
Six focus groups with HCPs (n = 21) and 3 patient focus groups (n = 13) were conducted. A further five semi-structured interviews with HCPs took place (see Table 1 for details).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0299770.t001
Two overarching themes developed from analysis of the HCP and patient interviews and focus groups, within which a number of sub-themes emerged:
- Limited availability of digital tools to assist in identifying and prioritising patients for a SMR
- Organisational challenges and patient factors affecting patient engagement for a SMR
- Time consuming “detective work”
- SMRs require multiple appointments
- Influence of healthcare context on delivering SMR
- Factors influencing deprescribing discussions
- Poor communication and data sharing between primary and secondary care
- Difficulties managing mental health medication for prescriber and patient
- Challenges around anticholinergic medication optimisation for prescriber
Fig 1 displays each key theme from this study and a detailed list of the barriers to each stage of the SMR process. Supplementary quotes for each theme can be found in S2 Appendix .
https://doi.org/10.1371/journal.pone.0299770.g001
- a. Limited availability of digital tools to assist in identifying and prioritising patients for a SMR
PCN pharmacists reported proactively identifying and prioritising patients to conduct SMRs. Patient identification was based on the criteria outlined by the DESGP contract, which includes patients in care homes (both nursing and residential facilities), individuals with complex multimorbidity and polypharmacy, urgently referred patients, older individuals encountering medication-related harms, and patients recently discharged from hospital. HCPs also referenced using available healthcare management automated search tools within the EHR, including ‘Ardens search’ [ 21 ] and ‘ProActive Register Management (PARM) diabetes’ [ 22 ], to identify pre-determined conditions, prescribing alerts and other variables that form part of the practice workload. They also used targets from the Investment and Impact Fund (IIF) for patient identification (IIF is an incentive scheme where PCNs can improve health and the quality of care for patients with multimorbidity), which participants described as beneficial but a waste of resources in the context of SMRs which should focus on patients with complex multimorbidity and polypharmacy [ 23 ]. Despite this, HCPs noted a limited number of digital tools to assist in identifying and prioritising patients for a SMR.
“I’ll be honest that we’ve not really had any tools that have been developed specific for supporting SMR.” (Pharmacist 2, Interview)
Since the introduction of EHRs in the NHS, HCPs are expected to assign ‘SNOMED codes’ to document patients with specific diagnostic, symptom or treatment codes in a logical hierarchical manner to specify clinical information [ 24 ]. These codes facilitate searches for specific medical conditions, symptoms and treatments within the GP EHR, facilitating the identification of individuals requiring an SMR. Pharmacists noted that EHR searches do not adequately consider the complexity of patients, making it challenging to stratify those that would benefit most from an SMR. Additionally, participants highlighted a lack of sensitivity and specificity in the current search mechanisms (meaning the searches either do not identify all the intended patients or identify too many).
“ The actual indicator that my team has been focusing on is supposed to be the ones where patients are prone to medication errors … but when I actually look at the patients, I haven’t got a clue why the actual computer system has decided that most of the time.” (Participant 1, Pharmacist FG1)
HCPs were concerned that the identification of patients who would benefit from an SMR could exceed the clinical capacity of the staff available to meet the need. They felt that any digital tool used to prioritise patients’ needs should match the clinical capacity of the practice.
“ The tools have to be a bit cleverer … We can generate a list of patients today … PCNs at the moment essentially do that, but what you have to do is almost the list that’s generated to the capacity … People would not switch it on if they felt that it could generate lots of patients you would not then see.” (Policy-maker, Interview)
- b. Organisational challenges and patient factors affecting patient engagement for a SMR
GPs or secondary care clinicians (excluding clinical pharmacologists) often conducted opportunistic medication reviews, compared to the proactive SMRs conducted by PCN pharmacists. In alignment with the DES requirements, HCPs described how the task of conducting an SMR was contingent upon organisational contracts, practice size, and staff availability. The presence of a PCN pharmacist for SMRs facilitated streamlined tasks, enabling GPs to focus on patients with more complex medical profiles. GPs voiced concerns about burnout in areas where demand for SMR exceeded the clinical capacity to undertake them. This challenge was particularly pronounced in regions of lower socioeconomic status where patients often presented with complex multimorbidity and polypharmacy at a younger age, especially those with co-morbid mental and physical health problems. Moreover, respondents felt that patients residing in deprived areas were less likely to attend scheduled SMRs, compelling GPs to resort to opportunistic reviews. This highlights potential inequity in access to SMRs and overall health surveillance.
“In the poorer area of the practice there’s no clinical pharmacist, that’s all done opportunistically, if done at all, by the GP partners there. I think that there’s a couple that are approaching burn out, if not complete burn out and the practice is almost run by locums. So, when I’m going in there, it’s quite tough and I will often see medications that are inappropriately prescribed, polypharmacy, several of the same drugs, and I will opportunistically undertake a structured medical review.” (Participant 3, GP FG1)
- c. Time consuming “detective work”
Whether HCPs identified patients proactively or opportunistically, the preparation time for a medication review ranged from 10 minutes to 1 hour. Several factors influenced this preparation time, including the availability of information, case complexity, barriers to accessing information, information density, and time constraints. The challenge in finding and collating information within the patient’s clinical records constituted a significant portion of the preparation time. For instance, discharge letters from hospitals are often located as attachments within the patient record, requiring HCPs to locate and read the letter. These necessary preparatory activities take away from the face-to-face time available with the patient.
“ Probably double the amount of prep time than it was actually with the patient. I mean, granted we did spend a while with the patient because we both like to talk, and the patient certainly did, but I think, and that’s the problem, isn’t it? You get the best information out of your patient when you let them talk and you let them tell you lots of things that you wouldn’t normally ask, but you haven’t got the time to do that so it’s tricky isn’t it to find the balance. But the biggest thing with the prep time was getting the information.” (Participant 3, Pharmacist FG1)
HCPs also conveyed frustration regarding the substantial time required to determine the original indication for a particular prescription and the ongoing necessity for it, even during major transition periods such as a patient’s admission to a care home.
“ We don’t get enough actual structured reviews, so they’ll be getting put on medication, people in care homes, and then left on those medicines. There’s no recognition of the changes. As you move in a care home, you’re generally more frailer, your renal function, haematic function might not be as great and, you know, you’re not moving as much, so your need for some medicines might not be as great as it was when the medicine was first started. ” (Policy-maker, Interview) “So along with what you said about deprescribing Selective Serotonin Reuptake Inhibitors (SSRIs) , especially , you know they’ve been on them for 4–5 years and they are adamant they don’t want to reduce them or stop them or have any sort of conversation about it , yeah , they’re quite challenging I think . Also , I think sometimes you can’t quite work out what medications people have been on . I mean if we talk about SSRIs they may have tried multiple different ones in the past and sometimes it’s difficult to work out what they’ve been on without having to go through the long , long list searching all the different medications that are SSRIs that they’ve tried . It would be so helpful if you know it could just bring up yeah been used before , and then know which one you could try…knowing that you want to try a different one . ” (Participant 6, GP FG1)
Although it is possible within the EHR system to link the prescription of an individual drug to its clinical indication, anecdotal evidence suggests this is time consuming and therefore may not be done in clinical practice.. As such, indications for prescribed medicines are recorded in the free text for the consultation which can easily become obscured over time within the extensive information contained in the clinical record. Examining the clinical free text for this information was emphasised as a challenge in efficiently conducting SMRs.
“ Although in my letters I would clearly state to the GP why I am prescribing the second line antipsychotic just so that people know, but over time that tends to get lost, the rationale for that prescribing tends to get lost and before you know you leave post, somebody else comes and begins to increase that second antipsychotic you know, so that becomes a problem. ” (Participant 1, Psychiatrist FG)
Moreover, existing EHRs are not adept at presenting patient histories in a manner conducive to HCPs pinpointing areas for potential deprescribing. This deficiency in the system leads to a cumulative high pill burden for patients, as illustrated in the quote below.
“ At the age of [ 18 – 20 ], I was diagnosed with bipolar. I am now [71–74] and I have lived for that period of time on medication, a lot of medication actually … I counted the number of tablets and my boxes on my bedside the other day and there was 13 different tablets, so that is what I am being prescribed by my GP. ” (Patient 1, Mental and physical co-morbidities FG)
Patients also expressed uncertainty about the initial reasons for starting medications. Patients reported receiving medications for many years and being unsure whether the medication was still necessary.
“ She is also on a daily injection of adult growth hormone which another consultant put her on at the time and she has been having them for probably 10 to 15 years, and no-one seems to know now who initially prescribed it and who is in charge of that. I am concerned, does she really need them? She is having them every day … Initially it was an asset to go with the immunodeficiency but now I don’t really know. ” (Patient 5, Mental and physical co-morbidities FG)
- d. SMRs require multiple appointments
SMRs typically lasted a minimum of 30 minutes, often extending beyond this duration. The variability in duration was contingent upon the patient’s complexity and the focused nature of the review. Allowing adequate time to address broader health concerns was deemed crucial, enabling the identification of potential issues requiring deeper exploration by the clinician.
HCPs acknowledged that SMRs were not a singular event, and patients might necessitate multiple appointments for a comprehensive review. Consequently, EHR systems were recognised as needing functionality to alert HCPs to schedule additional appointments after the initial SMR, emphasising the iterative and ongoing nature of medication reviews.
“ The first time I see patients, you want almost a bit of a holistic conversation, but actually when you start making interventions you go with what matters most to the patient or where the biggest risk is and you then table the others … You can imagine that being 2 or 3 hours in 4 different appointments before you get to the bottom of where you want to be … I think we had to contact on average about 2 to 3 times per patient, but there were more complex patients as well … I don’t think you can stop medicines or optimise medicines without seeing that patient again as least once. ” (Policy-maker interview)
Patients expressed a desire to be involved in the decision-making during reviews and valued the opportunity to discuss issues such as how medications fit into their routines and other resources that may be available to them.
"I’ve got a series of chronic things, take a load of pills and they’re each for separate things, and I have been concerned for years whether there’s any interaction with them, between them. And also they make me feel tired all the time and perhaps there are some of them where I could actually get rid of them." (Patient 1, Older people with frailty FG)
- e. Influence of healthcare context on delivering SMR
The duration of conducting a SMR was also contingent on the specific healthcare setting in which it took place. One pharmacist highlighted that SMRs conducted in care homes lacked a strict time limit and were oriented towards achieving specific outcomes, such as the number of medicines deprescribed in particular patient groups. This reflected the contextual variability in the conduct and objectives of SMRs, emphasising the need for flexibility in the approach based on the healthcare environment and patient population.
“ We were just told take whatever time you need but because we were not measured on the quantity, we were measured on the quality, and we were recorded the number of medicines basically stopped and in particular groups actually so, and then that would have gone on the report because that was the way of showing what we were doing and the basic value for money I guess .” (Participant 1, Pharmacist FG1)
The emphasis placed on a medication list varied depending on the reviewer and the healthcare setting. A pharmacist working in secondary care articulated a tendency to allocate less attention to certain medicines in a hospital setting, prioritising focus on medications more likely to cause harm. This perspective highlights the nuanced approach that different HCPs may adopt based on their expertise and the specific context in which they operate.
“ At the moment, the bisphosphonate would be something that I’m less concerned about it a very high acuity environment, that’s the thing that I’m probably going to, maybe if I get a chance, write in the discharge summary for the GP to check up on whether or not that’s still appropriate. Whereas I’m chasing those big harms .” (Participant 2, Pharmacist FG1)
- f. Factors influencing deprescribing discussions
Discussions around deprescribing between HCPs and patients were reported to be influenced by several factors. These included the specific type of medicine to be deprescribed, the patient’s willingness to discontinue the medication, sociodemographic location, availability of additional health services in the area, whether the medication was initially prescribed in primary or secondary care and the existence of pre-established stopping criteria for certain medications (e.g., bisphosphonates for more than 5 years). Additionally, HCPs and patients acknowledged a degree of reluctance to engage in deprescribing due to perceived potential risks associated with the cessation of certain medications. These multifaceted factors contribute to the complexity and individualised nature of deprescribing discussions within the healthcare context.
“I find it really, really difficult because all of the guidelines will say, oh, you should have this patient on statins, etc., and you think I really probably shouldn’t they’re 95, but having stopped them in the past then a patient unfortunately ends up with a stroke, they go to hospital, the hospital tells them it’s because their GP stopped their statin and puts them back on .” (Participant 2, GP FG2) “ The antidepressant one is interesting . So , I did work for 9 years in a really deprived area . . . SSRIs for a long time and they were pretty reluctant to come off it but usually willing to accept if it didn’t work out just put them back on it . It just meant in a much more middle-class area there’s the opposite where they’re all desperate to come off it and probably coming off it far too soon . So , I don’t think it needs to be doctor-led , it seems to be more about their external pressures and there’s been a lot of areas done in deprived communities with link workers and social prescribers and I think if you’re going to look at polypharmacy in these sort of groups then that’s probably the way to do it stopping all their meds .” (Participant 4, GP FG1)
In one case, a pharmacist highlighted the challenges associated with decision-making when optimising medicines for complex, younger patients, emphasising the impact of side-effects on their quality of life. Equally, the importance of considering quality of life in frail older adults with polypharmacy was acknowledged, although perceived as less complicated than in younger adults.
"I know well that’s it isn’t it, it’s not necessarily that they’re a complex medicine it’s that there is evidence to say that this can prolong your life but it’s causing them that much upset, so it’s, for me it’s not necessarily the, I can’t think of any particular group of drug its more the younger you get, you know 50 is very young and that you have got a lot of life left to live so that’s when it becomes more of a clinical decision for me that as a pharmacist I don’t feel like I would be able to make" (Participant 1, Pharmacist FG1)
- 2. Medication-related Challenges
Potential for medication-related harm identified by our key stakeholder groups included issues with specific medicines, conditions, and risky medication combinations; mental health medications; prescriptions from specialists; anticholinergic medicines; difficulties in determining prescription timelines to assist in decision-making; challenges with younger complex patients; and siloed care.
- a. Poor communication & data sharing between primary and secondary care
HCPs identified the challenge of extracting information from hospital discharge letters as a key source of frustration. Patients, in particular, assumed that EHRs seamlessly connected primary and secondary care, and in some cases, their community pharmacy. This assumption left patients bewildered and, in certain cases, reliant on the HCPs knowing the complete narrative behind their health records. The disjointed communication and misconceptions surrounding record integration emphasised the need for improved interoperability to enhance the continuum of care.
“ We will be waiting a week for an outpatient letter to come through and it’s really confusing, stop this, change that, increase the dose here, and you’re kind of stuck in the middle. So sometimes the patient will have left that meeting there and it will be ‘like go and see your GP and they will do this bit’, well [that’s] not happening until I’ve got that letter. There is that real mismatch of communication. ” (Participant 1, GP FG2) “ When the repeat prescription came through , despite the fact that the surgery had received the discharge letter , everything was all wrong , and this is just one of those things that happens . So , you get a review and it is whether that data from that review and the story behind it and who it goes back to and whether it is acted on , I think that is important .” (Patient 3, Complex multimorbidity FG)
Communication gaps between GPs, specialist clinicians, and patients were evident due to varying expectations. GPs expressed challenges in managing specialist medications with patients, including concerns about patients’ ability to self-manage their medicines. These challenges highlighted aspects of fragmented care between primary care and specialist clinicians. HCPs also cited difficulties and reluctance in communicating and potentially engaging in conflict with specialist doctors. Participants described specialist doctors as lacking a holistic view when prescribing for patients, favouring certain medicines, and having limited knowledge in drug interactions.
“I think multidisciplinary is key, however when I notice that I liaise with specialists, depending on who I speak to, their drug is the most important and trying to get a consensus about what is best for the patient is obviously one of the challenges like that’s how we got in this situation to begin with you know, so I do find that’s one of the challenges. so, I think you need someone who is you know, who is a specialist but has also got a sort of holistic view of patient care as well which doesn’t always happen in secondary care, but sometimes does.” (Participant 3, Polypharmacy FG)
Participants noted that central nervous system medicines had complicated medication regimens and hence required more coordinated care and responsibility between the specialist prescriber and GP. Addressing these challenges calls for enhanced collaboration, knowledge exchange, and a holistic approach to patient care between primary care and specialist clinicians.
“ I find it, with the pain management clinic, they stop medication, give you a list of all these other tablets you need to start to see how things go and then sort of leave you to it, discharge the patient in your hands and expect you to sort of manage it all. And the same thing is with migraine and headaches from neurology. That’s just a minefield … I think when you’re in specialty, you feel that you can give any sort of long protracted complicated regime and the patient is just going to manage it because that’s the only medication that you think that they’re on. So yeah, they can be quite difficult .” (Participant 5, GP FG1) “ He [GP] says that we can’t actually change any medication to do with your bipolar , that has got to be done by your psychiatrists … I don’t think they would change anything to do with psychiatry .” (Patient 1, Mental and physical co-morbidities FG)
- b. Difficulties managing mental health medication
Mental health medication and management emerged as a consistent sub-theme across key HCP stakeholder groups, irrespective of their professional background. Both doctors and pharmacists described difficulties in monitoring and adjusting psychiatric medicines, including uncertainties about how to address specific issues related to psychiatric medicines. Participants expressed a sense of being ‘out of their depth’, particularly concerning antipsychotic medicines. They conveyed a lack of confidence in assessing the risks and benefits of antipsychotic prescribing, feeling deskilled in this specific area of medication management, and finding it challenging to safely challenge prescribers. This sense of unease prompted participants to seek ways of contacting the mental health team, only to encounter additional hurdles, such as difficulties in locating relevant information within patient records to facilitate multidisciplinary coordinated patient care.
“ But the other one is someone with very complex psychiatric problems, still maybe under the mental health team, and I haven’t got really access to the details apart from maybe I’ve got, you know, some of the other diagnoses. But if I think maybe one of those drugs is potentially causing more harm than could then I’m not clear how then to action that and who to speak to and who were they actually seeing ” (Participant 1, Polypharmacy FG)
For example, a clinical pharmacologist explained that evaluating the success of managing antipsychotics is not as straightforward as assessing physical health conditions. This complexity may contribute to the observed lack of confidence among HCPs when it comes to deprescribing psychiatric medicines. The nuanced nature of mental health outcomes, compared to more tangible markers of success in physical health, adds an additional layer of intricacy to the decision-making process in psychiatry. This includes the complexity of managing mental health medication.
“ The biggest challenge group that I think we face in a deprived area is the patients who are on long term opioid medication, long term neuropathic meds, they’ve probably got a diagnosis of fibromyalgia, they’ve probably got personality disorder plus / minus mental health problems. And the issues that we have is that they’ve almost been sequentially added medication on because GPs don’t really often know what to do with them unless you have a special interest in that field like I do. And when they go and see pharmacists, they are very challenging to pharmacists and pharmacists don’t have the clinical knowledge to be able to sift through what can often be quite dramatic presentations. ” (Participant 1, GP FG1)
- c. Challenges around anticholinergic medicines
Anticholinergic medicines, which inhibit the neurotransmitter acetylcholine involved in numerous physiological functions, has been associated with adverse outcomes such as cognitive decline and falls, particularly when multiple anticholinergic medicines are used concurrently (termed anticholinergic burden) [ 25 , 26 ]. GPs, clinical pharmacologists, and pharmacists described the importance of reviewing and deprescribing anticholinergic medicines where possible. However, the process of calculating anticholinergic burden (ACB) in frail, older adults is time consuming, primarily due to the absence of automated calculators embedded within the EHR system.
Doctors and pharmacists expressed frustrations around the re-prescribing of anticholinergics after deprescribing them. They attributed the persistence of high ACB to limitations in prescribing guidelines and a scarcity of alternative options to replace anticholinergic drugs. These challenges highlighted the need for tools within EHR systems to facilitate efficient assessment of ACB, alongside a broader exploration of prescribing guidelines and alternatives to enhance deprescribing practices.
“ One of the things that I often see in general practice is that there’s lots of anticholinergics, usually amitriptyline because it’s kind of given out for other reasons for what it’s licensed for. So, sleep is probably the most common thing that I see it used for, or avoiding long term opioids in chronic arthritic pain, and often that’s because we have other options for them but we’re not allowed to prescribe them. So, melatonin is probably the most common thing that we could put them on which has a lot better safety profile, but we are just completely discouraged from prescribing it. And likewise access to other interventions that would help arthritic pain rather than putting them on NSAIDS which obviously carry risk or opioids which aren’t overly effective outside the acute pain window. It’s often the lack of other stuff that raises all of the anticholinergic burden. ” (Participant 1, GP FG1)
Participants welcomed any digital tool that could streamline routine work processes, including information retrieval, automated dose calculations, and assessing the risk of developing diseases to optimise medicines during a SMR in a patient-centred manner, with the goal of enhancing efficiency in the medication optimisation process.
Medication reviews by HCPs can take significant preparation, and are time consuming, primarily due to the need to gather and understand patient information and to develop an understanding of a patient’s medical history and social circumstances. In addition, currently, there is no easy way to identify from the EHR which patients are at greatest risk of medication-related harm and those most likely to benefit from an SMR. The EHR systems used in primary care contain enormous volumes of information which becomes particularly challenging and time-consuming to navigate for complex individuals living with multiple long-term conditions and taking many medications. The way that information is organised in the system leads to a large proportion of time spent linking medications to their original indication and examining the patient journey. This time could be better spent discussing shared decisions with the patient. The EHR has not evolved in line with increasing patient complexity. The findings of this report emphasise the need for enhanced functionalities in EHRs to support effective medication management in the context of deprescribing discussions where a nuanced understanding of a patient’s medication history is crucial.
Our study has highlighted the challenges facing those undertaking SMRs in more socioeconomically disadvantaged areas, where people experience multimorbidity (and co-existent polypharmacy) 10–15 years earlier than their affluent peers [ 27 , 28 ]. These populations have complex healthcare needs at a younger age, the care of which falls to the already over-stretched GPs. Areas with greater socioeconomic disadvantage often have lower health literacy, resulting from a combination of lower educational attainment, economic barriers like the need to prioritise food and heating over health seeking, and psychosocial stressors affecting decision-making relating to health [ 29 , 30 ]. Health literacy applies not only to the patient but to the clinician who may also be unaware of the psychosocioeconomic situation of the patient, leading to a communication gap when discussing the risk and benefit of medicines to reach a shared-decision [ 31 – 33 ]. Accordingly, complex conversations involving numeracy calculations of risk may take longer and require repetition, but may also be of less priority for the patient and/or carer than other more immediate life concerns.
As preparation time is repeatedly cited as a barrier to effective SMR, a potential solution that would support SMRs in those with lower health literacy should include any digital intervention that saves on preparation time. This would enable more time for the clinician to engage with the patient and discuss complexities around risk and benefit, which would go some way to addressing the existing health disparity that affects those experiencing socioeconomic disadvantage. For HCPs working in areas of socioeconomic deprivation, lack of HCP capacity alongside patients declining SMR invitations were cited as barriers to undertaking SMRs. Moreover, HCPs described the usefulness of a system to identify availability of different health services in surrounding areas (e.g. weight management service) [ 27 , 28 ]. A recent study co-produced SMR resources to empower patients in their healthcare and support them in making the most out of their SMR. This included producing resources in a number of different languages including audio recorded resources for patients with visual impairment [ 34 , 35 ]. Embedded links to resources for HCPs to provide to patients before and/or after an SMR can be one potential way to utilise digital health and empower patients to reduce inequity in access to healthcare.
Our study also highlighted medication-related challenges such as difficulties managing mental health, specialist and anticholinergic medications. HCPs reported that a lack of alternatives to medication for symptom management hampered their ability to optimise some of the more potentially harmful medication classes such as opioids, anti-depressants, anticholinergics and gabapentinoids. Non-pharmacological alternatives, where appropriate, such as counselling need to be readily and equitably accessible for this approach to be considered a reliable option [ 36 ]. Mental health medication management stood out as a consistent challenge. HCPs in our study, regardless of their professional background, expressed difficulty in monitoring and adjusting psychiatric drugs. There was also a general lack of confidence and skill when it came to monitoring and adjusting antipsychotic medications, with the measurement of success in managing these medications being ambiguous. This is consistent with previous studies that note GPs lack of confidence in managing patients with serious mental health illness [ 12 , 37 ]. One recent study reported that less than half of GP trainees in England and Wales have trained in a mental health setting between 2013 and 2015 [ 38 ]. In addition to the need for HCPs in primary care to become trained to address issues related to psychiatric medicines, EHRs must include basic information about the indication for the prescribed psychiatric medicine and the appropriate mental health team contact details for GPs to be able to address these issues. This would have the potential to enable multidisciplinary coordination of care with mental health patients.
Another challenging group of medicines was those with anticholinergic effects. This drug class was also a recurring issue among GPs, clinical pharmacologists, and pharmacists. HCPs found it time consuming to calculate the ACB in frail, older adults. Although there are several ACB scales available that have been developed and validated, participants stated that automated calculators to calculate ACB are not easily accessible or embedded into EHRs. In addition, there is considerable variability between anticholinergic scales making it difficult to ascertain which scale to use to calculate ACB [ 39 ]. As such, taking the time out to include every medicine a patient is taking to calculate their ACB is time consuming, reducing opportunities for potential deprescribing discussions with patients.
Limitations
This study was conducted in the UK, which provides universal access to healthcare. However, findings from our study may also be applicable internationally to other health systems which operate a universal social insurance model where there is a primary care and secondary care gatekeeping model, including the need for HCP coordination [ 40 , 41 ] or deprescribing challenges [ 42 , 43 ]. This study is part of a larger qualitative study examining both barriers to SMRs and potential digital solutions, including AI-assisted approaches. As such, the HCP participants likely included a number of clinicians with a particular interest in digital-driven solutions in healthcare. We sought to include a wide variety of HCPs from different practice backgrounds in order to mitigate this. In addition, some of the focus groups contained unexpected small numbers of clinicians at one time, owing to the competing demands on clinician time. However, the data collected were rich and contributed significantly to achieving thematic saturation. The insights gained from these discussions were consistent with those from larger groups, reinforcing the validity of our findings.
Conclusions
There are few useful digital tools that can identify patients that would benefit most from an SMR or monitor the effects of medication optimisation when medicines are altered. Our findings showed that significant time is needed to prepare and conduct a SMR, with complex patients sometimes needing multiple appointments to enable a comprehensive review. The DynAIRx project will use findings from this study to address the barriers of conducting an SMR by producing dashboards and visualisations to summarise the patient’s medical journey; develop digital tools to prioritise patients that would benefit most from an SMR; and identify optimal interventions for specific multimorbidity and polypharmacy patient groups.
Supporting information
S1 appendix. topic guides for interviews and focus groups and coreq checklist..
https://doi.org/10.1371/journal.pone.0299770.s001
S2 Appendix. Table containing additional explanatory quotes relating to subthemes.
https://doi.org/10.1371/journal.pone.0299770.s002
- 1. NHS. Network Contract Directed Enhanced Service. Structured medication reviews and medicines optimisation: guidance. In: NHS, editor. 2020.
- 2. NHS England. Network contract DES guidance for 2024/25: Part A ‐ Clinical and support services (Section 8). In: NHS England, editor. 2024.
- 3. NHS. Network Contract Directed Enhanced Service. Contract specification 2021/22 ‐ PCN Requirements and Entitlements. 2021.
- View Article
- PubMed/NCBI
- Google Scholar
- 7. NICE. Multimorbidity and polypharmacy 2017 [Available from: https://www.nice.org.uk/advice/ktt18 ].
- 11. NICE. Multimorbidity: clinical assessment and management: NICE,; 2016 [Available from: https://www.nice.org.uk/guidance/ng56 ].
- 20. Pope C, Mays N. Qualitative research in health care. Fourth edition ed. Hoboken: Wiley-Blackwell; 2020.
- 21. Ardens Healthcare Informatics. The leaders in providing EMIS Web & SystmOne templates & resources [Available from: https://www.ardens.org.uk/ ].
- 22. PARM Diabetes. A health management tool for people with diabetes co-created by Lilly and NHS Devon CCG [Available from: https://parmdiabetes.co.uk/ ].
- 23. NHS. Network Contract Directed Enhanced Service. Investment and Impact Fund 2020/21: guidance. 2020.
- 24. NHS Digital. SNOMED CT 2023 [Available from: https://digital.nhs.uk/services/terminology-and-classifications/snomed-ct ].
- 32. Citizens Advice. A very general practice. How much time do GPs spend on issues other than health?: Citizens Advice,; 2015 [Available from: https://www.citizensadvice.org.uk/Global/CitizensAdvice/Public%20services%20publications/CitizensAdvice_AVeryGeneralPractice_May2015.pdf ].
- 35. Health Innovation Network. Resources to support patients having a Structured Medication Review [Available from: https://thehealthinnovationnetwork.co.uk/programmes/medicines/polypharmacy/patient-information/ ].
- 38. MIND. Better equipped, better care. Improving mental health training for GPs and practice nurses 2016 [cited 2023 December 11]. Available from: https://www.mind.org.uk/media-a/4501/find-the-words-report-better-equipped-better-care.pdf .
- Open access
- Published: 02 September 2024
Understanding how and why travel mode changes: analysis of longitudinal qualitative interviews
- Kate Garrott ORCID: orcid.org/0009-0009-8714-5408 1 , 2 ,
- Louise Foley 1 ,
- David Ogilvie 1 &
- Jenna Panter 1
International Journal of Behavioral Nutrition and Physical Activity volume 21 , Article number: 96 ( 2024 ) Cite this article
Metrics details
Encouraging alternatives to the car such as walking, cycling or public transport is a key cross-sector policy priority to promote population and planetary health. Individual travel choices are shaped by individual and environmental contexts, and changes in these contexts – triggered by key events – can translate to changes in travel mode. Understanding how and why these changes happen can help uncover more generalisable findings to inform future intervention research. This study aimed to identify the mechanisms and contexts facilitating changes in travel mode.
Prospective longitudinal qualitative cohort study utilising semi-structured interviews at baseline (in 2021), three- and six-month follow up. Participants were residents in a new town in Cambridgeshire, UK, where design principles to promote walking, cycling and public transport were used at the planning stage. At each interview, we followed a topic guide asking participants about previous and current travel patterns and future intentions. All interviews were audio recorded and transcribed. Data analysis used the framework approach based on realist evaluation principles identifying the context and mechanisms described by participants as leading to travel behaviour change.
We conducted 42 interviews with 16 participants and identified six mechanisms for changes in travel mode. These entailed increasing or reducing access, reliability and financial cost, improving convenience, increasing confidence and raising awareness. Participants described that these led to changes in travel mode in contexts where their existing travel mode had been disrupted, particularly in terms of reducing access or reliability or increasing cost, and where there were suitable alternative travel modes for their journey. Experiences of the new travel mode played a role in future travel intentions.
Implications
Applying realist evaluation principles to identify common mechanisms for changes in travel mode has the potential to inform future intervention strategies. Future interventions using mechanisms that reduce access to, reduce reliability of, or increase the financial cost of car use may facilitate modal shift to walking, cycling and public transport when implemented in contexts where alternative travel modes are available and acceptable.
Introduction
Replacing car use with active travel and public transport could facilitate multiple favourable outcomes for public and planetary health [ 1 , 2 ] including increasing physical activity [ 3 ], reducing sedentary behaviour [ 4 ] and improving air quality [ 5 ]. Despite these benefits, the private car remains the dominant transport mode in many countries [ 6 , 7 ], and reducing car use is a shared cross-sectoral policy priority [ 5 ].
Individual travel choices are shaped by both individual and environmental context, and changes to these contexts can explain periods of stability or change in individual mobility [ 8 ]. Key events may change the context within which people make their travel choices, and may therefore lead to changes in the travel mode selected. Within the literature on mobility geographies, the term ‘key events’ embraces both life events (e.g. having a child, moving house or acquiring a driving licence) and exogenous interventions (e.g. the introduction of a new bus timetable) that change contexts and may consequently influence travel patterns [ 9 ].
Exogenous interventions may be introduced that change travel patterns, either as their deliberate intention or as an unintended consequence. Deliberate interventions are typically implemented by actors such as national or local governments or transport service providers, and may target individual behaviour or wider economic, physical and social conditions. These interventions take place within a dynamic wider social context in which life events [ 8 , 10 ] or other changes in the environment may also affect travel choices. Some research has focused on estimating the effect of specific types of key events on travel behaviour, such as residential relocation or the introduction of cycle lanes. While this has provided insights useful for policy and practice, findings have been mixed across travel modes [ 8 ], population subgroups [ 11 ] and locations, and estimating the effects of these changes without also considering the mechanisms involved may limit our understanding of how change occurs and therefore of the transferability of the findings [ 12 ].
Understanding the mechanisms by which key events bring about changes in travel mode is central to the approach of realist evaluation, which aims to understand what works, in what circumstances and for whom and is often used to evaluate or synthesise evidence about complex interventions [ 13 ]. Within realist evaluation, the term mechanisms denotes explanatory accounts that include the resources provided by an intervention and the reasoning and responses of participants to the intervention [ 14 ]. Furthermore, this approach explicitly considers that differences in contexts (the conditions of the setting in which an event occurs) or in the characteristics of individuals exposed to events may lead to different outcomes [ 12 ]. Identifying the contexts, mechanisms and outcomes can help build an explanation of how interventions work to bring about their effects that is both more detailed and more generalisable [ 15 ]. Applying this approach beyond intervention evaluation to understand mechanisms of changes in travel behaviour arising from key events has potential to uncover useful insights that can be applied within interventions.
There is limited research explicitly using realist approaches to explore the underlying processes of how a broader range of key events (i.e. not limited to ‘interventions’) may change the context for travel behaviour and thereby bring about changes in travel mode. One longitudinal qualitative study explored changes in cycling over three years in Cycling Demonstration Towns (CDT) in England, where there were major investments in cycling infrastructure, training and marketing [ 16 ]. This study identified triggers arising from key events that led to changes in cycling behaviour, while personal history, intrinsic motivations and the existing environment were contextual aspects that influenced behaviour. The authors provide illustrative examples to explain the reasoning for cycling behaviour change [ 17 ]. A young cyclist getting their first job, cites financial (cycling is cheaper than the bus), safety (there is somewhere safe to keep the bike) and availability (no car available) reasoning as forming the mechanism for a change in travel patterns.
We hypothesise that elaborating this type of analysis to describe and synthesise mechanisms across participants exposed to a variety of key events may be helpful in understanding the potential of a broader range of policy strategies to promote alternatives to the car. In this exploratory study, we tested a novel approach using longitudinal qualitative interviews to explore changes in travel mode arising from a variety of key events. We applied principles of realist evaluation to understanding the mechanisms and contexts that facilitate these changes, with a view to informing more generalisable principles for intervention design. Our specific objectives were to identify common mechanisms arising from key events that lead to changes in context, and to understand the contextual conditions that facilitate changes in travel mode.
Study design
This was a prospective longitudinal qualitative cohort study nested within a randomised controlled trial (RCT) to assess the feasibility of financial incentives for promoting alternatives to the car, implemented in Northstowe, a new town in Cambridgeshire, United Kingdom [ 18 ]. Eligible individuals for the RCT were those aged over 16 years and living in a household in Northstowe that had not claimed financial incentives, meaning they were either unaware of the incentives or had previously chosen not to claim them. The RCT was conducted while covid-19 was circulating (October 2021- July 2022), which may have influenced participants’ travel patterns and their attitudes towards different travel modes. A subset of participants from the RCT was invited to complete remote semi-structured interviews at baseline and at three and six months post-baseline. Participants who completed at least one follow-up interview were eligible for this analysis. No additional incentives were provided to participate in the semi-structured interviews.
All participants gave written informed consent at the beginning of each interview. The School of Humanities and Social Sciences Research Ethics Committee, University of Cambridge provided ethical approval (HVS/2019/2778).
Northstowe is a new town currently under construction eight miles north of Cambridge, United Kingdom. At the time of the study, 908 of the projected 10,000 new homes were occupied. The town received Healthy New Town funding [ 19 ] and is intended to provide a sustainable environment promoting health and wellbeing. During the study, all residents lived within one mile of a bus stop, providing a service to Cambridge City Centre within 20 min. At the time of the study, available public facilities were two schools, open spaces, children’s play parks and outdoor leisure facilities but no shops or other amenities.
Sample recruitment and representativeness
From RCT participants, we purposively selected a sample of participants for invitation to interview based on treatment group allocation, age, car ownership and baseline travel patterns in order to understand a broad range of perspectives and experiences. There were no additional eligibility criteria to participate in the interviews. Interested participants responded and completed an online consent form before arranging an appropriate time for the interview. For those who completed baseline interviews, we repeated this process at three and six months post baseline.
Data collection
We conducted semi-structured interviews following a flexibly applied topic guide (Supplementary material A ). The topic guide covered impressions of living in Northstowe, experiences of the environment, current travel patterns and intentions to change. Open-ended questions were used to minimise the risk of social desirability bias. Three and six month interviews also discussed changes in travel since the previous interview. The interviews also explored the use of financial incentives, which were the subject of the RCT. KG conducted all interviews between November 2021 and July 2022 via video call or telephone due to the continued circulation of covid-19 and wrote detailed field notes. Each interview lasted between 18 and 70 min, and was audio recorded and transcribed verbatim by a third party.
Data analysis
All transcripts were imported to NVivo software to facilitate and manage the coding process. We analysed the transcripts using a framework approach [ 20 ] based on pre-defined realist evaluation principles [ 21 ]. We coded key events, contexts, mechanisms and outcomes as defined in Table 1 . We linked these codes to maintain individual configurations and wrote contextual descriptions for each participant. We did not code any data related to the use of financial incentives (the intervention being tested in the parent RCT). While only one participant reported a direct effect of incentives on travel mode, we cannot rule out that the intervention worked in more implicit ways, for example by signalling approval of alternative travel modes. We compared the emerging codes and developed an analytical framework which was refined throughout the coding process, until a final analytical framework was applied to all transcripts.
We charted the data, maintaining the linked individual configurations. Each row in our data table represented a unique configuration and each column represented a participant, with its heading containing the individual’s contextual description. Where a configuration was reported by a participant, we summarised the verbatim quotes within the applicable cell, retaining the original feel of the transcript. We analysed the matrix to identify mechanisms for changes in travel and to describe the contexts that facilitated or inhibited these changes.
Participants
Figure 1 displays participant recruitment in the context of the RCT. Of the 99 participants in the RCT, 20 of the invited subset completed baseline interviews. 16 participants completed at least one follow-up and were eligible for this analysis. Ten participants completed three interviews and six participants completed two interviews, making a total of 42 interviews included in this analysis (Baseline, n = 16; 3-month, n = 15; 6-month, n = 11). Table 2 presents demographic details of interview participants collected at baseline.
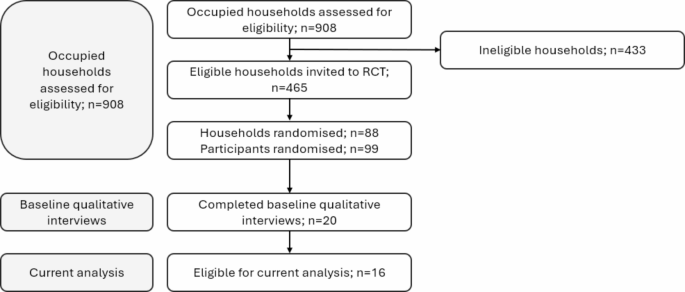
Participant flow diagram
Summary of common mechanisms identified
We identified six common mechanisms that facilitated modal shift in response to a diverse range of key events. We take each of these mechanisms in turn and describe the key events that led to a change in contexts and the individual and environmental contexts that influenced whether a change in travel mode change occurred. Table 3 describes the generalisable configurations identified. Using an illustrative example, when a bus cancellation (key event) occurs in a context where (i) an individual had planned to use the bus to commute, (ii) they are not able to work from home and are required to be at work on time (for example, a teacher) and (iii) they have access to a car, this leads to a modal shift from bus to car (outcome). The reasoning (mechanism) is that access to the planned transport mode has been removed and the individual is unable to reach the destination on time, leading to a deliberation process and the selection of an alternative mode.
Changing access
Reduced access.
When access to a transport mode was reduced or removed and the planned mode was unable to transport participants to their destination, modal shift was dependent on available alternative modes and characteristics of the planned journey. The key event that reduced access to the existing travel mode triggered modal shift in contexts where the journey was necessary and there was an acceptable alternative mode available. For example, ‘ Yesterday I was not allowed on the bus going into work in the morning and I wasn’t the only one , there were about 15 or 20 other people who couldn’t get on the bus because it was full , and where they’ve changed the timetable , the next bus isn’t for another half an hour after that , so I wouldn’t have got to work on time , so I had to drive (P0811)’. We observed examples of events that reduced access to the bus through acute cancellations, occurring due to timetable changes, driver strikes and adverse weather; and that reduced access to the car when ‘ my car was having its service done (P0371)’ , participants had been drinking alcohol, or car parking was unavailable at the destination.
In contexts where travel was required but there was no acceptable alternative mode available, participants implemented alternative strategies which included staying overnight at the destination, changing travel route or time, or taking annual leave because it was not possible to get to the workplace: ‘ I used to be a 9 to 5.30 person. Since using the [local bus service] I’ve changed to being an 8 to 4.30 person just to avoid the rush hour traffic (P3291)’. This was evident among people without access to a car who used the bus. Where there was no alternative mode available and the journey was not necessary, participants simply did not travel or, where flexibility allowed, worked from home.
Increasing access
Some key events led to increased access to alternative travel modes. These included new jobs or colleagues moving to Northstowe. Modal shift occurred among participants who had new jobs when the new workplace was accessible by an alternative travel mode, generating a new stable context with potential to facilitate longer-term modal shift. In some cases, however, the alternative travel modes described would not have been feasible for everyone (for example, not everyone can realistically run to work). For others, meanwhile, both the original and new work locations were accessible only by car, and despite exploring alternative options no modal shift happened for those participants.
Changing reliability
Reducing reliability.
The ongoing reduced access led participants to reason that they were unable to rely on those transport modes for consistent journey times that enabled them to arrive at the destination on time. Within this study, the ongoing bus cancellations and overcrowding was sparked from wider contextual changes influencing the transport infrastructure. Participants reported that Britain’s exit from the European Union, led to HGV driver shortages, resulting in a shift of bus drivers to HGV driving leading to an acute shortage of bus drivers and a reduced bus timetable. Once again, modal shift occurred in contexts where reduced reliability affected the existing travel mode and within the context of journeys that were time dependent, for example, travelling to an airport or repeated journeys such as the commute: ‘ On a number of occasions either the bus hasn’t turned up because it’s been cancelled , or I’ve not been allowed on because it’s been too full … I think the last interview was close to the point at which I just stopped using the bus altogether because I couldn’t rely on it (P0811)’. The repeating nature of journeys exposed individuals to the ongoing unreliability which they viewed as disruptive. It was notable that tolerance towards reduced reliability was variable and affected by weather and sustainability values. For those making journeys infrequently or leisure time journeys that were not time dependent, unreliability did not seem appear to trigger modal shift.
Faced with deterioration of the reliability of the bus service, participants who had no alternative travel mode were unable to immediately switch mode. However, the consequences of unreliable bus travel affected their ability to arrive at work on time: ‘ I usually reach five to ten minutes late … despite all the running I do (P1291)’. This triggered participants to seek alternative travel modes, such as purchasing bikes and learning to drive for those who were physically and financially capable: ‘ My experience for the past two months have kind of like proven that the busway’s not very reliable with regards to time. So I would still gear towards having at least a car for the household , just for the situations when I have to get somewhere on time (P1281).’ One participant’s coping mechanism was to change to a job not in line with their career goals in order to cope with the unreliability of the bus service.
Improving reliability
Restoration of the bus timetable resulted in a more reliable bus service which reversed the reasoning described above: ‘ it is now my intention to try and use the bus again going forwards and from that one experience I had it does seem to have made things a little better (P0811)’. In the case of the bus, improving reliability triggered a modal shift among participants whose travel preference was the bus and who were aware of the improvements. We noted a difference in timing returning to bus travel dependent on sustainability motivations, whereby participants with stronger motivations were more eager to restore bus travel.
Changing financial cost
Increasing financial cost.
We found that modal shift occurred when participants were faced with rising travel costs, resulting in this study from rising petrol costs linked to global fuel prices, coupled with increased frequency of office working following lifting of covid-19 restrictions. Participants who changed travel mode reasoned that the cost of their current travel mode was becoming intolerable and sought cheaper alternatives. Modal shift occurred in the context of commuting journeys which were required and where cheaper and acceptable alternatives were available. For example, one participant initiated a car share with a colleague who lived nearby, sacrificing the convenience of being a sole car user to reduce journey costs.
In a context in which individuals believed they were already travelling in the cheapest way, no modal shift occurred, but as one participant noted ‘ I’m so glad I’m car sharing because it’s like £10 more expensive to fill up my car (P1191)’. Furthermore discretionary journeys, for example to eat out at restaurants, did not appear to be subject to modal shift. Instead, participants chose not to make these journeys.
Reducing financial cost
We identified one event that reduced the financial cost of travel: ‘ They’ve [bus company] introduced some flexible fares that mean it’s very economical , it works out at £2.94 a day for bus travel , which is definitely cheaper than petrol (P0811)’. When this occurred simultaneously with increased commuting frequency described above, the cost difference was amplified and the participant reasoned that bus travel was the cheapest mode and modal shift occurred from the car to the bus. In this context, the participant was actively seeking alternative travel modes due to the cost of using the car. We saw no instances of modal shift due to the reduced bus fares among participants who were unable to use the bus for commuting. Among participants already using the bus, the reduced cost was welcome and while no modal shift occurred, the reduced cost may have contributed to maintaining that travel mode.
Changing convenience
Convenience to meet changing demands of dependents.
We noted instances where the key event led to changes in the convenience required of travel due to the demands of dependents. Where this required greater convenience (e.g. the acquisition of a new pet) and an alternative mode provided greater convenience, modal shift occurred. For example, shifting from car-sharing to sole car use enhanced the flexibility to leave work early, or switching from walking to car use decreased the journey time. In contrast, when the key event reduced the need for convenient travel – because a participant’s child was starting school near home, and no longer travelled to with her to the workplace nursery – intentions were formed to travel by bus.
Increasing confidence
We found that prompts to encourage individuals to try alternative travel modes, including suggestions from friends – ‘ She [friend] said , do you want to walk or shall we cycle? So I said , no , let’s cycle (P2591)’ – or workplace initiatives, resulted in a modal shift towards the bicycle. This shift happened among nervous cyclists when there was social support in place and cycling equipment was available in the wider environment, via spare bicycles or local cycle hire schemes. The social support increased participant confidence that they were capable of cycling. When similar prompts were experienced by nervous cyclists without social support, modal shift did not occur and the participant did not trial cycling, despite the availability of cycling equipment in the local environment.
Raising awareness
Raising awareness of pro-environmental behaviour.
Finally, we observed modal shift from the car to walking or cycling for journeys to complete short errands (e.g. posting letters, visiting doctors) due to an enhanced awareness of the environmental impacts of car use and the health benefits of active travel. ‘ I don’t use the car quite so much. I’m either not going anywhere or I’m walking … so I do try and not use it . .because it’s better for me to just to walk everywhere (P2691)’. These participants reasoned that their current car use did not align with their view on environmental impact, and therefore changed mode. Both participants had sufficient time to complete these journeys, and the proximity of the errands to their homes enabled these journeys to be completed via walking or cycling.
Common principles
Across the six mechanisms, we identified three notable commonalities. Firstly, when key events disrupted existing travel modes, they often led to changes in travel modes because participants were required to consider alternative travel modes. For example, two participants reported changing their travel mode when their car was in the garage, reflecting a disruption in their current patterns of car use for commuting or errands. In contrast, when events acted on travel modes not currently used by participants they had little influence on their travel choices. For example, deterioration of the bus service was not reported to influence car users’ choice of travel mode. Secondly, we identified the availability of alternative modes and the journey characteristics as important contextual influences. Changes in travel mode were only observed where there was a suitable alternative mode available. In the absence of a suitable alternative participants continued their current travel patterns, although we did observe them forming intentions to increase the availability of alternative modes, by obtaining a driving license or purchasing a bike. We identified the characteristics of the journey as an important context and participants’ travel choice was different dependent on whether a journey was discretionary, necessary or time-dependent. Thirdly, we observed that the experience of the new travel mode played an important role and positive or negative experiences of the alternative mode informed future travel intentions. For example, one participant described a pleasant experience of cycling after commuting as part of a workplace sustainability day, citing the sunset and social aspect as enjoyable aspects that prompted intentions to continue with this mode.
Summary of findings
We identified six mechanisms, potentially generalisable as intervention strategies, that explained the process of how changes in travel mode occurred: changing access, reliability, financial cost, convenience, confidence and awareness. For some mechanisms we found evidence that they could operate in either a positive or a negative direction, for example increasing and reducing access. We found that these mechanisms were triggered by a diverse set of key events, and we identified the features that may be generalisable to apply as intervention strategies. Firstly, key events acting on existing travel modes appeared to have a greater influence than those acting on potential alternative modes. Secondly, modal shift was only observed among participants who had a suitable and acceptable alternative for the journey, and for whom the journey was not discretionary. Individuals without alternative travel modes available may have to implement coping strategies, for example starting work at a different time or taking annual leave if their existing transport mode is disrupted. Thirdly, the experience of the alternative travel mode appeared to influence future intentions.
Comparison to previous literature
Similar to the findings from this study, previous reviews of interventions have identified that financial mechanisms appear to be effective for reducing driving behaviour [ 22 ], and mechanisms involving accessibility, awareness and experience appear to be effective for increasing active travel [ 22 , 23 ]. The fact that we identified these mechanisms suggests commonalities in the mechanisms of travel behaviour change, regardless of whether the event originates from deliberate interventions or from other sources. Previous research has identified additional mechanisms relating to aesthetics, safety, skills and space [ 22 ]. These may be more likely to originate from interventions or environmental changes with a deliberate intention to change travel behaviour, and are unlikely to have occurred in Northstowe during the six months of our study. We have previously identified that the same event might have different mechanisms depending on its context, and that within some contexts these mechanisms may not be triggered at all [ 23 ]. Those principles are reinforced by the current study, in which we identified that individuals responded differently to the same events depending on characteristics of the journey and the availability of alternative travel modes. This analysis therefore contributes to an emerging field of research focusing on understanding the process of how travel behaviour change occurs.
Many of the concepts identified in this analysis are consistent with other conceptualisations or framings. We identified mechanisms operating in both positive (reducing cost or increasing confidence) and negative directions (reducing access, increasing cost or reducing reliability), described elsewhere as ‘carrots’ or ‘sticks’ respectively [ 24 ]. We found no evidence of a negative direction for the mechanisms of experience, awareness and convenience in this study, but it is plausible, for example, a change in bus route may reduce the convenience of the bus. A previous review found that interventions using carrot and stick strategies in combination, or sticks alone, were more effective than interventions using only carrot strategies [ 22 ]. For example, workplace travel plans including parking restrictions and charging (sticks) plus off-site parking provision and improved bus services (carrots) were more effective than strategies to encourage alternatives to driving (carrot) alone [ 25 ]. Our study gleans additional insight, suggesting that ‘sticks’ often disrupted existing travel modes. We found that key events that operate as ‘carrots’ often act on travel modes not currently used, and may therefore be more influential among those predisposed to walking and cycling but insufficient to spur broader modal shift among those without such dispositions [ 24 ]. The habit discontinuity hypothesis supports these insights, whereby disruptions to a stable context lead to active deliberation about travel mode [ 26 ]. Research in this domain suggests that strong habitual tendencies attenuate information acquisition whereby those with strong travel habits are less likely to notice and acquire information about alternative travel modes [ 26 ], potentially explaining why few participants noted key events that affected alternative travel modes. Furthermore, interventions that require individuals to use a high levels of personal resources (or agency) in order to benefit from the intervention are hypothesised to be less effective and equitable, compared to those with low demands [ 27 ]. Exposure to key events that impact on existing travel modes require individuals to use few or no personal resources compared to those operating on alternative travel modes [ 28 ], suggesting that they are more likely to trigger deliberation. Taken together, this suggests that an event disrupting existing travel behaviour, and acceptable alternatives may be required to ensure such policies are equitable.
Implementing more disruptive ‘stick’ approaches poses challenges for public and political acceptability [ 29 ], due to the perceived political risk that has potential to instigate policy conflict or public backlash against future policies [ 24 ]. However, implementing these alongside positive and supportive ‘carrot’ approaches that provide acceptable alternatives to facilitate travel behaviour change has the potential to enhance their acceptability. The different disciplinary theories described above describes commonalities and synergies, and bringing them together contributes to ‘ holistic sense-making’ and strengthens the generalisability of these findings across behaviours, contexts and populations which can inform future interventions [ 15 ].
Implications for intervention research
Understanding how changes in travel mode occur in response to a variety of events can help to inform intervention strategies. Key events that act on existing travel modes, particularly those that operate to deter their use, appear to influence modal shift. Applying this principle to interventions suggests strategies to reduce access, reduce reliability and increase financial cost of car use to facilitate modal shift towards active travel and public transport. These mechanisms could be triggered by interventions such as road user charging, pedestrian zones or speed restrictions. However, a cautious approach is required because interventions of this kind are often less publicly and politically acceptable [ 29 ], and ensuring that walking, cycling and public transport infrastructure provides and accessible, convenient and pleasant alternative is likely to be a pre-requisite to enhance their effectiveness, equity and acceptability [ 30 ]. Without this, we found that individuals are likely to continue using their existing transport mode with barriers in place by implementing coping strategies, such as changing jobs, taking annual leave, changing working hours or being late to work. This may have important implications for some population groups and these should be identified to assess the equity impacts of interventions and to explore potential unintended consequences, for example on wellbeing or employment.
We also found that key events acting on transport modes not currently used by participants were described as leading to travel behaviour change among participants already considering those travel modes, suggesting that this approach may have limited success for attracting new walkers, cyclists and public transport users. Furthermore, we observed several instances of one-off travel behaviour change and found that these presented opportunities to form opinions on alternative travel modes. In order to capitalise on such chance opportunities, efforts should be made to ensure that experiences are pleasant, reliable and accessible to increase the likelihood of future modal shift [ 31 ].
Strengths and limitations
A strength of the study is its longitudinal design to assess temporal travel behaviour trends. The follow-up period was sufficient to report on intentions for travel behaviour change and allowed sufficient time for changes to occur, while being short enough to be unlikely to impact recall. We purposively sampled participants according to their car ownership and travel patterns to understand experiences from a range of participants with differing initial travel patterns. This analysis is based on interviews collected as part of an RCT exploring financial incentives to reduce car use, and therefore participants may have self-selected to participate in a travel related study. Further selection bias is possible whereby participants in the semi-structured interviews may have been more interested in environmental and health issues. Despite little evidence that these incentives affected travel behaviour [ 15 ], participation in the study may have subliminally primed individuals to consider or change their travel behaviour. Furthermore, our reliance on information provided by participants may have not have identified additional mechanisms that operate via less deliberative process of reasoning. Participants in this study reflect a relatively affluent population [ 18 ], and it is unclear whether key events would trigger the same functions in different population groups, or whether the availability of alternative travel modes differs by population group.
In this study we applied realist evaluation principles to understanding travel behaviour change. We identified six common mechanisms that facilitate travel behaviour change: increasing or reducing access, reliability and financial cost, improving convenience and confidence, and raising awareness. We observed changes in travel behaviour when these mechanisms disrupted an existing travel mode and when an alternative travel mode was available. This study contributes to understanding how key events change travel behaviour and provides evidence about what contexts appear supportive of change. The mechanisms identified here could form targets for intervention strategies and could be generalisable to a range of other settings.
Data availability
The datasets analysed during the current study are not publicly available as it is not possible to fully anonymise the interview transcripts.
Lee I-M, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29.
Article PubMed PubMed Central Google Scholar
Haines A. Health co-benefits of climate action. Lancet Planet Health. 2017;1(1):e4–5.
Article PubMed Google Scholar
Sahlqvist S, Song Y, Ogilvie D. Is active travel associated with greater physical activity? The contribution of commuting and non-commuting active travel to total physical activity in adults. Prev Med. 2012;55(3):206–11.
Foley L, et al. Patterns of health behaviour associated with active travel: a compositional data analysis. Int J Behav Nutr Phys Activity. 2018;15:1–12.
Article Google Scholar
Woodcock J, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: urban land transport. Lancet. 2009;374(9705):1930–43.
D.f.T., Transport Statistics Great Britain . 2021.
Saeidizand P, Fransen K, Boussauw K. Revisiting car dependency: a worldwide analysis of car travel in global metropolitan areas. Cities. 2022;120:103467.
Whittle C, et al. Life events and their association with changes in the frequency of transport use in a large UK sample. Travel Behav Soc. 2022;28:273–87.
Müggenburg H, et al. A review of achievements and challenges of the mobility biographies approach and a framework for further research. J Transp Geogr. 2015;46:151–63.
Li W, Kamargianni M. Investigating the mode switching behavior from different non-car modes to car: the role of life course events and policy opportunities. Transp Res Rec. 2019;2673(3):676–85.
Jin L, et al. Clustering life course to understand the heterogeneous effects of life events, gender, and generation on habitual travel modes. IEEE Access. 2020;8:190964–80.
Scheiner J. Why is there change in travel behaviour? In search of a theoretical framework for mobility biographies. Erdkunde. 2018;72(1):41–62.
Pawson R, Tilley N. An introduction to scientific realist evaluation. Evaluation 21st Century: Handb. 1997;1997:405–18.
Lemire S, et al. What is this thing called a mechanism? Findings from a review of realist evaluations. New Dir Evaluation. 2020;167:73–86.
Ogilvie D, et al. Making sense of the evidence in population health intervention research: building a dry stone wall. BMJ Global Health. 2020;5(12):e004017.
Chatterjee K, et al. Conceptual model to explain turning points in travel behavior: application to bicycle use. Transp Res Rec. 2012;2322(1):82–90.
Chatterjee K, et al. Triggers for changes in cycling: the role of life events and modifications to the external environment. J Transp Geogr. 2013;30:183–93.
Garrott K, et al. Feasibility of a randomised controlled trial of financial incentives to promote alternative travel modes to the car. J Transp Health. 2023;32:101673.
NHS England. Healthy New Towns. [cited 2023 03 October]; https://www.england.nhs.uk/ourwork/innovation/healthy-new-towns/
Gale NK, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):1–8.
Ritchie J, et al. Qualitative research practice: a guide for social science students and researchers. sage; 2013.
Xiao C, et al. Shifting towards healthier transport: carrots or sticks? Systematic review and meta-analysis of population-level interventions. Lancet Planet Health. 2022;6(11):e858–69.
Panter J, et al. Can changing the physical environment promote walking and cycling? A systematic review of what works and how. Volume 58. Health & place; 2019. p. 102161.
Piatkowski DP, Marshall WE, Krizek KJ. Carrots versus sticks: assessing intervention effectiveness and implementation challenges for active transport. J Plann Educ Res. 2019;39(1):50–64.
Petrunoff N, et al. Carrots and sticks vs carrots: comparing approaches to workplace travel plans using disincentives for driving and incentives for active travel. J Transp Health. 2015;2(4):563–7.
Verplanken B, et al. Context change and travel mode choice: combining the habit discontinuity and self-activation hypotheses. J Environ Psychol. 2008;28(2):121–7.
Adams J, et al. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 2016;13(4):e1001990.
Garrott K et al. Development and application of the DePtH framework for categorising the agentic demands of population health interventions. BMC Global Public Health, 2024. 2(13).
Karreman N, et al. Understanding the role of the state in dietary public health policymaking: a critical scoping review. Health Promot Int. 2023;38(5):daad100.
Heath GW, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet. 2012;380(9838):272–81.
Buck M. Disruption, an opportunity to facilitate long-term modal shift to cycling? Stories, lessons and reflections from the COVID-19 pandemic. Act Travel Stud, 2023. 3(2).
Download references
Acknowledgements
The authors would like to thank local authority partners for facilitating the research. Specifically, we would like to than Clare Gibbons, Jon London and Mihaela Stan (South Cambridgeshire District Council), Prajina Baisyet (Smart Journeys) and Christine Sprowell (Living Sport). We would also like to thank the Data Management Team at the MRC Epidemiology Unit, University of Cambridge, particularly Susie Boatman and Anna Melachrou. For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising.
This work was supported by the National Institute for Health and Care Research (NIHR) School for Public Health Research is a partnership between the Universities of Sheffield; Bristol; Cambridge; Imperial; and University College London; the London School for Hygiene and Tropical Medicine(LSHTM); LiLaC–a collaboration between the Universities of Liverpool and Lancaster; and Fuse–The Centre for Translational Research in Public Health, a collaboration between Newcastle, Durham, Northumbria, Sunderland and Teesside Universities. This study is funded by the National Institute for Health Research (NIHR) School for Public Health Research (Grant Reference Number: SPHR-PROG-WSBT-CS2). JP and DO are supported by the Medical Research Council (MRC; Unit Programme number MC_UU_12015/6 & MC_UU_00006/7). LF was funded by the National Institute for Health Research (NIHR) (NIHR 133205) using UK aid from the UK Government to support global health research. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
MRC Epidemiology Unit, University of Cambridge, Cambridge, UK
Kate Garrott, Louise Foley, David Ogilvie & Jenna Panter
Institute of Applied Health Research, University of Birmingham, Birmingham, UK
Kate Garrott
You can also search for this author in PubMed Google Scholar
Contributions
KG, LF and JP were involved in the conception and design of the study. KG collected the data. All authors were involved in analysing and interpreting the data. KG wrote the manuscript. All authors were involved in reviewing and editing the final manuscript.
Corresponding author
Correspondence to Kate Garrott .
Ethics declarations
Ethics approval and consent to participate.
The School of Humanities and Social Sciences Research Ethics Committee, University of Cambridge provided ethical approval (HVS/2019/2778). All participants gave informed consent to participate at the beginning of each interview.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Garrott, K., Foley, L., Ogilvie, D. et al. Understanding how and why travel mode changes: analysis of longitudinal qualitative interviews. Int J Behav Nutr Phys Act 21 , 96 (2024). https://doi.org/10.1186/s12966-024-01647-x
Download citation
Received : 21 February 2024
Accepted : 20 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12966-024-01647-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Active travel
- Modal shift
- Qualitative
International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Extract insights from Customer & Employee Interviews. At Scale.
8 best qualitative research tools.
Home » 8 Best Qualitative Research Tools
Qualitative research plays a vital role in understanding human experiences, motivations, and behaviors. Researchers often face the challenge of analyzing complex data gathered through interviews and focus groups. To navigate this intricacy, selecting the right qualitative tools is essential. This section explores the top qualitative tools available, designed to simplify the analysis process and enhance research quality.
With an array of options, these tools cater to varying expertise levels, ensuring accessibility for both seasoned researchers and newcomers. By harnessing these top qualitative tools, you can effectively convert rich qualitative data into meaningful insights, guiding critical decisions in your projects. As we delve into our top picks, you will discover how they can transform your research experience.
Why Qualitative Research Matters
Qualitative research plays a crucial role in understanding users' experiences, motivations, and behaviors. It sheds light on the nuances that quantitative data might overlook, providing rich insights that can drive meaningful change. When organizations aim to improve products, services, or customer interactions, qualitative research tools become invaluable. They enable researchers to unearth deep sentiments and perspectives that help in crafting solutions tailored to real needs.
These tools can reveal patterns and shared themes that inform strategic decisions. For instance, by analyzing verbatim responses, researchers can identify key insights that resonate across different participants. This understanding goes beyond surface-level statistics, facilitating a more profound comprehension of user needs. Embracing qualitative research empowers teams to ask the right questions and engage with customers on a deeper level, ultimately enhancing the effectiveness of their strategies. Understanding these aspects is essential for anyone looking to utilize top qualitative tools effectively.
Key Features of Top Qualitative Tools
Top Qualitative Tools share several key features that enhance their effectiveness for researchers. Ease of use is crucial; tools should simplify complex processes, making them accessible to users without extensive research experience. User-friendly interfaces enable quick learning and seamless integration into various projects. Furthermore, robust data analysis capabilities allow researchers to extract meaningful insights effortlessly, breaking down intricate interview transcripts and qualitative data effectively.
Another vital feature is customization. The best tools can adapt to unique research needs, allowing users to tailor their analysis workflows. Added functionalities such as tagging, sorting, and interactive visualizations enhance understanding of collected data. Collaborative features also stand out, enabling teams to work together efficiently and share valuable insights. In sum, Top Qualitative Tools provide comprehensive solutions that transform raw data into actionable insights, empowering researchers to make informed decisions based on nuanced interpretations.
Top Qualitative Tools for Effective Research
Understanding the top qualitative tools for effective research can significantly enhance your insights and findings. These tools allow researchers to collect, analyze, and interpret qualitative data, making the process more structured and insightful. From interview analysis to survey response evaluation, these tools cater to various research needs.
Key tools in this domain include transcription software, qualitative data analysis platforms, and user feedback systems. For instance, transcription software simplifies converting spoken words into written text, enabling more focused analysis. Qualitative data analysis tools provide robust frameworks for identifying patterns, themes, and insights from collected information. Additionally, user feedback systems facilitate direct engagement with participants, ensuring that the insights gained are relevant and actionable. Together, these top qualitative tools empower researchers to derive meaningful conclusions, ultimately driving informed decision-making.
Software Solutions for Qualitative Data Analysis
Qualitative data analysis is essential for understanding complex human behaviors and emotions. Utilizing software solutions can significantly enhance this process, making it efficient and systematic. The top qualitative tools are designed to simplify the transcription, analysis, and reporting of qualitative data, which often involves text, audio, and video formats. These tools help researchers focus on deriving meaningful insights instead of spending excessive time on tedious manual tasks.
When selecting software solutions for qualitative data analysis, consider key features such as automation, ease of use, and collaboration capabilities. Here are some crucial aspects to evaluate:
Automation : Look for tools that offer automated transcription and analysis to save time and reduce errors.
Collaboration : Opt for software that facilitates teamwork, allowing multiple researchers to work on the same project seamlessly.
Data Visualization : Choose tools that provide visualization options to make insights more digestible.
Integration : Ensure that the software can integrate with other research tools or databases.
Support and Training : Good software comes with responsive customer support and educational resources.
Choosing the right software can lead to more accurate insights and a streamlined research process, ultimately enhancing the quality of qualitative analysis.
NVivo: An In-Depth Look
NVivo stands out among the top qualitative tools by providing researchers with a user-friendly and efficient platform for data analysis. Its innovative features allow users to quickly organize, manage, and analyze qualitative data, transforming complex datasets into actionable insights. One notable aspect is its ability to adapt to various project needs. Researchers can utilize ready-made templates tailored for market research, employee engagement, or product development.
Additionally, NVivo enhances the analysis process through AI integrations. This capability enables users to pose intricate questions and receive clear, data-driven responses in moments. With its visual dashboards, researchers can easily track their findings, facilitating a deeper understanding of the data at hand. Overall, NVivo is not only a powerful tool for qualitative research but also an essential asset for those seeking to derive meaningful insights from their data efficiently.
Atlas.ti: Simplifying Complex Data
The tool excels in simplifying complex data, making it easier for researchers to analyze. By integrating various features, it allows users to create robust datasets while highlighting relevant insights. Researchers can delve into multi-project queries to extract information across numerous datasets. This capability is especially beneficial in qualitative research, as it provides a holistic view of varied data sources.
Moreover, visual experiences like journey maps enhance data interpretation by transforming abstract concepts into tangible representations. Users can draft recommendations based on concrete data, guiding decision-making processes in fields such as banking and customer experience. With its user-friendly approach, the tool stands out as one of the top qualitative tools for researchers aiming to uncover meaningful insights efficiently. Streamlining the analysis process ultimately empowers researchers to focus on their core objectives while navigating the complexities of qualitative data.
Online Tools for Qualitative Surveys
Online tools for qualitative surveys have revolutionized the research process, enabling researchers to gather insights efficiently. These tools facilitate the collection and analysis of qualitative data, allowing for a deeper understanding of participants' perspectives. Throughout this journey, the challenge lies in selecting the right technology that meets the needs of your study while ensuring ease of use for all participants.
Several key online tools can enhance your qualitative research efforts. Firstly, engaging survey platforms offer intuitive designs that make it simple for respondents to share their thoughts. Secondly, transcription services convert verbal interviews into text quickly, saving valuable time. Additionally, visualization tools help researchers to interpret and present their findings in a compelling manner. Each of these solutions aims to streamline the process and improve data quality, making your research more effective. Remember, selecting the right tool can significantly impact the quality of insights you gain.
SurveyMonkey: Powering Research with Ease
When it comes to qualitative research, efficient data collection and analysis are crucial. This platform excels in powering research with ease, allowing users to create insightful surveys quickly. With user-friendly features, researchers can effortlessly design tailored surveys to capture rich qualitative data. Through engaging formats, such as open-ended questions, the platform encourages participants to share their thoughts and experiences in greater detail.
Additionally, the platform offers a powerful AI-driven analysis tool that transforms raw data into valuable insights. By using customizable templates, researchers can streamline their projects for various purposes like market analysis or employee engagement. This capability ensures that researchers can extract actionable insights faster, aiding in decision-making processes. With these robust features, the platform stands out among the top qualitative tools, enabling better understanding and more informed strategies.
Google Forms: A Free and Flexible Tool
Google Forms is a robust option among the top qualitative tools available today. Its user-friendly interface is designed to cater to researchers of all experience levels. With this tool, you can easily create surveys, collect data, and analyze responses without needing advanced technical skills. This flexibility makes it an ideal platform for various research needs, from academic studies to user feedback initiatives.
Here are some key features that enhance Google Forms' appeal:
Customization : Users can incorporate various question types, including multiple choice, text responses, and checkboxes to tailor surveys to specific research goals.
Real-Time Collaboration : Teams can collaborate on forms simultaneously, allowing seamless communication and faster data collection.
Accessibility : Since it is cloud-based, researchers can access their forms and data from any device, enhancing workflow efficiency.
Automatic Data Collection : Responses are automatically gathered and can be visualized in charts for easy analysis, facilitating quick insights.
These features underscore why Google Forms remains a go-to tool for qualitative research efforts.
Tools for Ethnographic Research
Ethnographic research often requires specific tools that facilitate in-depth understanding of cultural and social dynamics. These tools gather qualitative data through direct observation, interviews, and participatory methods. Among the top qualitative tools available, researchers can utilize field notes, audio recordings, and video documentation. Each of these tools plays a significant role in capturing the nuances of human experience.
Field notes allow researchers to document their observations in real-time, offering insights that might not be captured through formal interviews. Audio recordings of conversations can provide deeper context, enabling researchers to analyze tone and emotional cues. Video documentation captures visual interactions and settings, further enriching the understanding of a subject's environment. Employing these tools in ethnographic research ensures a comprehensive approach to data collection, ultimately leading to richer insights and more reliable conclusions.
Dedoose: Multi-Method Research Simplified
Dedoose simplifies multi-method research by seamlessly integrating qualitative and quantitative data analysis tools. Researchers can explore and synthesize complex information without the hassle of traditional methods. This tool is particularly useful for projects that involve multiple interviews, allowing users to manage and analyze data effectively. By offering features like the research matrix, it facilitates the comparison of themes across various transcripts, leading to richer insights.
Developers designed this software to enhance collaboration and streamline workflows. Users can easily mix standard spreadsheet tasks with advanced AI functions, making it a standout choice among top qualitative tools. As a result, researchers can extract specific insights and identify trends efficiently. This capabilities ultimately empower teams to make data-driven decisions that are informed by clear, actionable findings, ensuring a more structured approach to qualitative research.
MAXQDA: Bridging Quantitative and Qualitative Data
MAXQDA plays a vital role in bridging the gap between qualitative and quantitative data, acting as a robust research tool. In the realm of qualitative research, it supports users by analyzing text, audio, and video data, thus enriching the understanding of complex insights. This dual approach allows researchers to complement numerical data with rich narratives, providing a more holistic view of their studies.
One of the standout features of MAXQDA is its ability to automate insights and streamline reporting workflows. By minimizing the need for manual data transcriptions and analyses, it significantly enhances efficiency while maintaining high-quality outcomes. The integration of AI technologies ensures a reduction in bias, prompting better decision-making based on reliable data. Ultimately, tools like this exemplify the future of qualitative research, allowing for deeper insights that greatly inform strategies and outcomes.
Real-Time Collaboration Tools
In today’s rapidly evolving work environment, real-time collaboration tools have become essential for qualitative research teams. These tools allow multiple team members to contribute ideas and insights simultaneously, fostering creativity and enhancing productivity. Tools like shared digital whiteboards and brainstorming platforms enable researchers to organize thoughts visually, ensuring that no critical perspective is overlooked.
Moreover, real-time collaboration enhances communication among team members, providing instant feedback and support. Using chat features or video conferencing, teams can discuss findings and refine strategies immediately. This synergy is crucial when adapting to emerging trends or shifts in data. Ultimately, incorporating real-time collaboration into qualitative research processes streamlines workflows and produces richer, more nuanced insights. By utilizing the best qualitative tools available, research teams can transform their approach to gathering and analyzing information effectively.
Microsoft OneNote: Collaborative Note-Taking
Microsoft OneNote is a powerful tool for collaborative note-taking, making it a top contender among qualitative research tools. It enables users to gather and organize ideas from various discussions in a structured manner. By storing conversations, summaries, and highlights, users can easily revisit key insights that emerge during collaborative sessions. This capability encourages seamless communication among team members while allowing everyone to contribute their thoughts and perspectives.
Moreover, OneNote supports various media formats, allowing users to incorporate images, links, and documents. This versatility enhances the richness of data collected, encouraging dynamic interactions. The tool also enables project integration, simplifying the process of linking notes to specific tasks or objectives. Its user-friendly interface streamlines collaboration, ensuring that teams can work together efficiently, making it an invaluable asset in qualitative research.
Trello: Organizing Research Processes
Trello excels at organizing research processes by providing a dynamic platform for project management. It allows teams to create boards that can categorize various qualitative research tasks, making collaboration straightforward and effective. For researchers, maintaining clarity amidst complex data collection and analysis is essential, and this tool facilitates that by enabling users to establish individual cards for each aspect of their research.
Each card can include descriptions, checklists, and attachments, ensuring that every detail is covered. Additionally, Trello’s commenting feature allows team members to communicate directly on respective tasks, thus reducing miscommunication. By visually representing tasks and their progress, Trello enhances the overall workflow. This level of organization is vital for researchers striving to achieve quality insights while managing time efficiently. Ultimately, utilizing such a tool is crucial for anyone looking to streamline their qualitative research efforts.
Conclusion: Choosing the Right Top Qualitative Tools
In conclusion, selecting the right top qualitative tools can significantly enhance your research efforts. The ideal tools should be user-friendly while offering powerful analytics capabilities. This balance allows researchers, regardless of their experience level, to draw valuable insights from their qualitative data.
Consider your specific needs when evaluating these tools. Features such as ease of use, scalability, and integration with existing systems can impact your choice. Ultimately, the right tool will empower you to gather rich, meaningful data, enabling informed decision-making and deeper understanding of your target audience.
Turn interviews into actionable insights
On this Page
5 Effective Market Research Strategies for Product Development
You may also like, 8 alternatives to saturate for research analysis.
8 Alternatives to Getwhy for Qualitative Research
8 alternatives to qualtrics for customer & employee insights.
Unlock Insights from Interviews 10x faster
- Request demo
- Get started for free
- Open access
- Published: 30 August 2024
Experiences and impacts of psychological support following adverse neonatal experiences or perinatal loss: a qualitative analysis
- Gill Thomson 1 ,
- Lara McNally 1 &
- Rebecca Nowland 1
BMC Pregnancy and Childbirth volume 24 , Article number: 569 ( 2024 ) Cite this article
2 Altmetric
Metrics details
Poor parental mental health in the perinatal period has detrimental impacts on the lives and relationships of parents and their babies. Parents whose babies are born premature and/or sick and require neonatal care or those who experience perinatal loss are at increased risk of adverse mental health outcomes. In 2021 a North-West charity received funding to offer psychological support to service users of infants admitted to neonatal care or those who had experienced perinatal loss, named the Family Well-being Service (FWS). The FWS offered three different types of support – ad hoc support at the neonatal units or specialist clinics; one-to-one person-centred therapy; or group counselling. Here we report the qualitative findings from an independent evaluation of the FWS.
Thirty-seven interviews took place online or over the phone with 16 service users (of whom two took part in a follow-up interview), eight FWS providers and 11 healthcare professionals. Interviews were coded and analysed using thematic analysis.
The analysis revealed two themes. ‘Creating time and space for support’ detailed the informational, contextual, and relational basis of the service. This theme describes the importance of tailoring communications and having a flexible and proactive approach to service user engagement. Service users valued being listened to without judgement and having the space to discuss their own needs with a therapist who was independent of healthcare. Communication, access, and service delivery barriers are also highlighted. The second theme - ‘making a difference’ - describes the cognitive, emotional, and interpersonal benefits for service users. These included service users being provided with tools for positive coping, and how the support had led to enhanced well-being, improved relationships, and confidence in returning to work.
The findings complement and extend the existing literature by offering new insights into therapeutic support for service users experiencing adverse neonatal experiences or perinatal loss. Key mechanisms of effective support, irrespective of whether it is provided on a one-to-one or group basis were identified. These mechanisms include clear information, flexibility (in access or delivery), being independent of statutory provision, focused on individual needs, active listening, the use of therapeutic tools, and positive relationships with the therapist. Further opportunities to engage with those less willing to take up mental health support should be developed.
Peer Review reports
Introduction
Perinatal mental health refers to mental health during pregnancy or within the first year after having a baby [ 1 ]. It is estimated that up to 20% of women experience poor mental health such as antenatal or postnatal depression, anxiety, post-traumatic stress, or other complications such as postpartum psychosis [ 1 ]. Two key areas that can impact perinatal mental health relate to having a baby admitted to neonatal care, or experiencing a perinatal loss (such as miscarriage, stillbirth, or early neonatal death). Both situations induce similar responses but for different reasons. The need to promote positive parental health is well-reported due to the links between poor mental health and parent relationships [ 2 ] and poorer infant and child social, emotional, behavioural, and cognitive developmental outcomes [ 3 , 4 , 5 ].
Having a baby admitted to neonatal care can be a devastating experience for parents [ 6 ] due to experiencing a traumatic birth, concerns over infant viability and the unfamiliar and technological nature of the neonatal environment [ 7 ]. A recent systematic review and meta-analysis to explore prevalence rates of depression and anxiety for mothers and fathers of preterm infants reported depression rates of 29.2% for mothers and 17.4% for fathers, and anxiety rates of 37.7% and 18.3% for mothers and fathers respectively [ 8 ]. Mothers of premature infants have also been found to experience higher rates of post-traumatic stress when compared to fathers [ 9 ]. Perinatal loss is also reported to have profound and lasting effects on the mental health of parents due to feelings of intense grief manifested through feelings of sadness, anger, guilt, and emptiness [ 10 , 11 , 12 ]. Individuals who have experienced perinatal loss are also at increased risk of trauma symptoms, such as flashbacks and nightmares [ 13 ] and developing, or exacerbating depression and anxiety [ 10 ]. Both having a premature and/or sick infant or a perinatal loss can induce guilt due to parents blaming themselves for their baby’s prematurity or untimely death [ 10 , 11 , 14 , 15 ]. These parents can also experience social isolation through feeling disconnected from friends and family due to a lack of understanding [ 10 , 16 ].
Interventions for perinatal mental health are crucial to ensure the well-being of the parents and infants. Within neonatal care, interventions can include family-centred care [ 17 , 18 ], skin-to-skin [ 19 ] and education programmes [ 20 ]. An integrative review focused on interventions designed to improve the psychosocial needs of parents of premature and/or sick infants identified 36 different studies/interventions including creative activities, peer support, relaxation/mindfulness, spiritual/religious and psychotherapeutic support [ 7 ]. This review found varying results with a general lack of effectiveness trials and wide heterogeneity within similar interventions; mechanisms of self-care, relaxation and social opportunities were highlighted as important [ 7 ]. A further systematic review and meta-analysis of 17 psychosocial interventions for individuals experiencing perinatal loss found significant impacts on reducing depression, anxiety, and grief; with most interventions offering either counselling or structured debriefing sessions [ 21 ].
In 2021 a North-West charity received government funding to develop and evaluate a two-year (April 2021-March 2023) Family Well-being Service (FWS). This service involved three types of support. (A) Ad hoc emotion-based support provided to service users while their babies were admitted to neonatal care or attending specialist clinics following perinatal loss. (B) Person-centred one-to-one therapy (~ 10–12 weeks) delivered over the telephone or face-to-face to service users whose infants were admitted to neonatal care, had experienced perinatal loss and those attending foetal medicine clinics due to their infants experiencing complex health conditions. (C) Group support, via a 6-week face-to-face guided bereavement course designed by two of the FWS therapists for service users who had experienced perinatal loss. Group support was initially introduced as an interim measure to enable service users to receive support while they waited for one-to-one therapy. The FWS was provided to service users who received care from any of four maternity Trusts in one North-West region. Here we report some of the qualitative findings from the evaluation to highlight the experiences and impacts of the FWS on service users. This work complements existing research by offering qualitative findings of a therapeutic-based intervention for those experiencing perinatal mental health difficulties following adverse neonatal outcomes [ 22 ]. It also extends the current literature by providing insights into an ad hoc form of therapeutic support delivered during a sensitive period of infant admission.
Methodology
An exploratory descriptive approach was undertaken due to this study focusing on a new area of service delivery [ 23 ].
During the evaluation, we planned to collect demographic and outcome data from all those who received one-to-one therapy from the FWS (with this information not routinely recorded for those who received ad hoc or group-based support). The service users were asked by the FWS therapists to provide consent for data-sharing purposes. Overall, less than a third of service users who received one-to-one therapy over the evaluation period provided consent. As this meant that only a partial, and potentially unrepresentative data set was available, this information has not been reported (a full copy of the evaluation report that includes all data and outcome analyses is available from the lead author). The reason for non-consent was not recorded in case this had a negative impact on the FWS therapist-service user relationship.
As part of the evaluation, we undertook interviews with the FWS therapists who provided the therapeutic support; wider healthcare care, e.g., neonatal nurses/staff who work on the neonatal units - to capture their perceptions about the FWS being delivered at the units; and service users who had received support (ad hoc, one-to-one therapy, group-based counselling) from the FWS. In this paper, we report on insights from the qualitative data that describe the experiences and impacts of the FWS on service users.
Data collection
Data collection involved interviews with the FWS therapists, wider healthcare professionals and service users. Service users were also invited to participate in a follow-up interview ~ 6 months later to assess for longer-term impacts of the FWS and whether any additional support had been accessed. While different semi-structured interview schedules were created for the different population groups (see overview of topics for each participant group in Table 1 ), all involved exploring experiences of the FWS and recommendations for service development.
All interviews were undertaken remotely via telephone or Microsoft Teams and were video and/or audio recorded. At the start of the interview, consent statements were read out by the researcher, with participants asked to verbalise their agreement to each. The consent recording was then stored separately from the interview recording. Service users were offered a £10.00 voucher for each interview completed. All interviews were between 20 and 60 min (average of 50 min) in length and were transcribed in full for analysis purposes.
Recruitment
Recruitment of FWS therapists involved the FWS project lead sending an invitation to all appropriate staff. To recruit wider healthcare professionals, FWS therapists were asked to provide contact details of relevant healthcare professionals (those who were aware of the FWS) for the evaluation team to invite. Any service user aged 16 + years who had received support from the FWS was eligible to take part. Service users were invited (via FWS therapists) by being asked to complete an Agreement to Contact form to receive further information about the evaluation. Posters about the evaluation were also displayed in key locations (e.g., neonatal unit, location where therapy or group support was provided) for service users to contact the evaluation team directly.
On all occasions, participants received an invitation email, an information sheet, and a consent form, and asked to respond to the evaluation team within two weeks if they wished to participate (with reminders issued ~ 3/4 weeks later).
Qualitative data were analysed using a reflexive thematic approach [ 24 ]. This involved the first and second authors creating an initial coding framework using MaxQDA qualitative software. The second author then continued to use this framework to code the remaining documents with codes added, re-named, or merged as appropriate. All the authors reviewed and agreed on final analytic decisions.
Reflexivity
All authors have a psychology-related background. The lead author has over 20 years of undertaking research with perinatal populations, and the other two have been undertaking research in this area for ~ 5 years. All the authors are parents. All authors consider that emotion-based support for parents who have faced these adverse situations is crucial due to the potential for negative impacts on parents, infants, and families. The second author who was responsible for data collection and analysis had experienced neonatal care with her first child and had previously worked as a volunteer with the charity. Care was taken to ensure that this prior relationship did not overtly bias data collection, or the interpretations generated – this was achieved through working closely with the project lead (first author) to review the transcripts and when analysing the data set. As listening to others’ experiences of neonatal care could trigger personal memories, regular check-ins were provided by the project lead for reflection and sign-posting purposes.
Ethics approval for this study was received from the Health ethics committee at the University of Central Lancashire (project no: 0262). All participants received a detailed information sheet and provided informed consent. As it was recognised that the interviews could elicit upset, a distress protocol was developed. This involved advising participants (in the information sheet and verbally) that the interview would be paused should they become upset, and a decision made together about how to proceed. All service users were provided with contact details of organisations where they could seek further support as needed. All information sheets noted that confidentiality would be broken should experiences of harm (to self and others) be disclosed.
A total of 37 interviews with 35 participants were undertaken, 35 interviews were completed via Microsoft Teams and two interviews were audio-recorded telephone calls. Participants included eight FWS staff, 11 healthcare professionals and 16 service users (of whom two were interviewed twice). The demographics and characteristics of service users are displayed in Table 2 .
All service users identified as female and were aged between 25 and 40 years, with a mean age of 33. Most service users were White British or White British American ( n = 14, 87.5%), over half were married or in a civil partnership ( n = 11, 62.5%) and the rest were single ( n = 6, 37.5%). The age of the service users’ youngest child ranged from 10 weeks to 4 years (with the average child age being 15 months). Reasons for referral varied and were due to several different types of adverse neonatal experiences or perinatal loss (see Table 2 ). The types of support that the service users received are detailed in Table 3 . These data highlight that one service user had only received ad hoc support on the neonatal unit; the remainder had all received more prolonged support via one-to-one or group-based therapeutic support (four of whom also had received ad hoc support at the neonatal unit or specialist clinic).
The FWS staff interviewed included seven psychological therapists ( n = 7) and the project lead. Healthcare professionals who participated in an interview held different roles including neonatal nurses, ward managers and sisters, education leads and mental health neonatal nurses. The healthcare professionals’ length of service ranged from 9 months to 14 years.
In the following sections, we present two themes and associated sub-themes. The first theme - ‘creating time and space for support’ - details the informational, contextual, and relational basis of the FWS service, as well as barriers to service delivery. The second theme - ‘making a difference’ - describes the cognitive, emotional, and interpersonal benefits of the FWS for service users. Illustrative quotes are included with identifiers that use the abbreviations SU – service user, FWSS – Family Well-being service staff, or HCP – healthcare professional. Additional identifiers that signify the type of support the service user received are also included using the codes A (ad hoc support), G (group counselling) and O (one-to-one therapy).
Creating time and space for support
In this section, we describe how the FWS therapists worked to facilitate time and space for therapeutic support across six sub-themes - ‘ tailoring the communications’ , ‘a flexible and proactive approach’ , ‘being listened to without judgement’ , ‘independent from others’ , ‘not just about the baby’ and ‘ shared experiences’. A final sub-theme reports on the ‘barriers to service delivery’.
Tailoring the communications
FWS staff used various communication modes - verbal, leaflets, email, telephone, or text – to inform and communicate with service users. Some service users spoke positively about the incremental information received and how valuable it had been to tell them ‘everything I could expect’ (SU4:O&G): this, together with the perceived ‘ non-pushy’ approach of the FWS staff enabled them to make their own decisions and to access the support on their terms, ‘I just read through it [ leaflet] because it wasn’t kind of like it straight away , we’re gonna refer you. They said have a think’ (SU16:O). Another service user reported:
It was a lot of like, what’s gonna fit for me really. Like I wasn’t just kind of told, this is what you’re going to do and that kind of thing. Like, every step of the way I was asked, like, do you want to do this? Do you want to try this? You know, do you think that would work for you? And it felt really personal. (SU4:O&G)
Service users also appreciated the immediacy of contact from the therapists, ‘found it really good , they contacted me really quick’ (SU9:O), once a decision to receive support had been made.
A further means by which FWS staff helped to tailor communications and support service user engagement was via data sharing. Several service users highlighted the benefits of the FWS staff sharing their information with others in the service, thereby mitigating the need for repeating painful accounts:
She [FWP therapist] was aware that I was gonna be contacting. I think it is helpful that they already knew my background because it can avoid questions that you don’t particularly want to answer, or things that you don’t want to have to repeatedly go over. (SU3:G)
Those receiving ad hoc support were all encouraged to take up formal therapy following infant discharge. However, the therapists also offered a text message contact for service users who were not receptive to receiving more prolonged therapeutic support during their infant’s neonatal stay, e.g., ‘six weeks after you’ve been discharged just to check in’ (FWSS1). For some, this delay in service offer was considered ‘perfect’ as it meant that they accessed support that they ‘would not have accessed’ but has ‘ helped me no end’ (SU7:A&O). Although one of the FWS staff reflected that whilst this follow-up approach was not always successful, it provided ‘peace of mind’ (FWSS5) to know that it had been offered.
A flexible and proactive approach
Participants who accessed different forms of therapeutic support from the FWS spoke very positively about the flexible and proactive nature of the service. Proactive ad hoc support on the neonatal unit enabled service users to receive support while being with their babies. Healthcare staff felt parents were unlikely to prioritise their own mental health needs when ‘all they are concerned about is the baby’ – proactively approaching them ‘ where they are’ was therefore perceived to be the ‘best way of doing it by far’ (HCP8). Ad hoc support was also considered important in preventing service users from ‘slipping through the net’ (HCP5) by expecting them to join a waiting list for an appointment that they then decide not to access.
Flexibility in how the one-to-one therapy was provided (i.e., by telephone or face-to-face) was highly appreciated. Telephone appointments were valued for practical reasons such as childcare - ‘I can’t attend in person with two children ’ and wider work commitments. Accessing support from home also allowed service users to feel comfortable in their own space, which in turn enabled them to be more open with their therapist:
You’re in your space. I was comfy, I had my coffee and then I just felt like, I don’t know if I’d have opened up so much if I was in a room and it felt like counselling, like therapy (SU6:O).
Flexibility in service users being able to change appointments, ‘they changed every appointment that I needed changing […]it was brilliant’ (SU1:O) or delaying appointments ‘she didn’t mind me texting and saying I’m running 5–10 minutes late ’ (SU6:O) was highly valued. Service users also appreciated the freedom to go at their own pace: ‘if you wanted to contribute [during the group counselling], you could do , if you didn’t , you didn’t have to ’ (SU10:O&G). One service user reflected on how this personalised approach stimulated reciprocity in terms of individuals being able to ‘get out’ what they ‘put in’ (SU15:G). This flexibility was also echoed in the bereavement groups, with the discussion topics being based on the needs of the group rather than a prescribed plan:
[Group therapists] had something as sort of an idea for each session but they would always ask if there was anything that we as a group or individually wanted to focus on or cover. (SU3:G)
Being listened to without judgement
Service users repeatedly spoke of how much they valued feeling ‘heard and listened to and valued’ (SU5) by the FWS therapists; with these accounts provided by service users who had received ad hoc, one-to-one, or group-based support. One service user also felt that while the therapist was ‘paid to listen’ it was the fact that she seemed to ‘want to listen’ that made a difference (SU1:O). Several service users reflected on how the therapists’ active listening and person-centred non-judgmental approach meant they ‘ found her really easy to talk to , it’s a really good relationship’ (SU12:A&G), and was someone who they ‘could be completely open with’ (SU6:O):
The most helpful thing is having someone to listen to me and that has no judgment whatsoever, I have to say when I went on, she was calm, she was soothing and never felt one bit of like, oh my God, I can’t believe that’s happened […] There’s no judgment, […] she was there for me and only for me. (SU14:O)
Feeling listened to and having a good relationship with their therapist gave service users a sense of being ‘wholly seen’ and a safe space to be ‘able to feel safe and valued and respected’ (SU5:A&O). Some service users described how it was like they were talking to a friend who was ‘there for me ’:
It was just like talking with an old friend, if you know what I mean. And even though I’ve never met the lady before, she was very friendly […]. So it was nice. (SU13:O)
Independent from others
Whilst service users appreciated the friendliness and authenticity of their therapist, they also talked about how helpful it was to receive regular support from the same therapist who was independent of friends, family, and healthcare professionals. Several participants who received one-to-one or group-based support considered this to be helpful as it meant they could openly share how they felt without feeling like a burden:
I was really worried that when I was talking to like my husband or my mum and my sister or anything that that I was saying was just going to end up upsetting them and having someone to talk to or just felt like I can say whatever I want, […] Like it’s not gonna ruin their day, I can just say what I want, it was just so helpful really (SU4:O&G).
The positives of the therapists being separate from clinicians were related to challenges in the relationships between healthcare providers and parents due, e.g., to life-saving care being administered to their babies which was uncomfortable to watch:
So, it’s quite nice that they have that extra person to talk to who isn’t the person that just stuck a gastric tube down your baby and made him cry or, you know, or that just cannulated your baby (HCP1).
Healthcare professionals also spoke of how parents could attempt to ‘hold it together’ during interactions with healthcare staff, due to not wanting to give the ‘impression that they’re struggling’ (HCP6). Support from an ‘outsider’ perspective was therefore perceived to be crucial in breaking down these barriers and offering dedicated needs-led support.
Not just about the baby
Another reason service users felt they could talk openly about their feelings and experiences was due to the support being focused on their needs as individuals, rather than being about the baby, or being a parent:
It helped me in a lot more ways as sometimes it was nothing to do with being a mum or [baby] and yeah, it just worked really well’ (SU6:O).
Service users acknowledged the need to process their negative experiences but also the necessity of talking about other things that were affecting their mental health and their ability to cope:
I had to grieve with what had happened in the past. Cause normally I just push everything down and deal with it, I just get on with the next day. So, we [therapist and service user] went backwards for me to be able to move forward. (SU14:O)
‘My helping hour’ (SU6:O) as one service user who had received therapy described, and mirrored in others’ narratives, related to how much they appreciated and looked forward to taking time out each week to think about their needs:
When you’ve got a newborn and you’re wrapped up with, especially with someone with a condition and wrapped up with a feeding schedule, medicines, nappies, sleepless nights, blah blah, blah blah blah. I would never have then thought, you know what? Let’s take care of you. Let’s have an hour that’s just for me. (SU7:A&O)
Shared experience
Some service users who received support on an ad hoc, one-to-one or group basis spoke of how receiving support from a therapist who had faced a similar experience had ‘definitely helped’ . One pregnant service user who had had a previous miscarriage reported the benefits of receiving one-to-one support from a therapist who had faced their own experiences of infertility and subsequent in vitro fertilisation:
She’d gone through pretty much a very similar experience to me. She’d had very similar infertility issues, and she’s also gone through losses herself. So, it was easy to bond with her very quickly because you do when someone’s gone through that same experience (SU11:O).
Others referred to how receiving support from therapists who had ‘been through it all the same’ (SU1:O) helped them to feel ‘normal’ and ‘I wasn’t being dramatic or crazy’ (SU8:A). Whereas for others, it was receiving support from a therapist who understood the realities of parenthood that mattered:
Motherhood is hard, you know, like and my counsellor was a parent as well, so really helped to, like, justify those feelings are rational and just rationalise. (SU5:A&O)
Opportunities for group support also enabled service users to normalise and validate their experiences ‘with other people who have all gone through the same thing and have the same feelings ’ (SU4:O&G).
Barriers to service delivery
Overall, there were some challenges and barriers reported in relation to communication, access, and service delivery. First, in relation to communication, some service users referred for one-to-one or group support complained about a lack of information about when it would be received:
So, it was a bit frustrating waiting and not knowing whether it was then gonna be like weeks and weeks, or months, or whether it was gonna be like a few days. (SU4:O&G)
Several service users also described communication difficulties about the delay in follow-up after the initial assessment (when referred for formal therapy). This delay meant they had to ‘unravel’ the ‘worst parts you are struggling with’ and then ’putting the phone down’ with ‘no follow-up plan or coping mechanisms’ in place (SU10:O&G). The gaps in support provision were also expressed from within the service: ’it’s not great , because those mums and dads are waiting , and they’ve reached out , and that’s when they need the help ’ (FWSS7).
Despite the benefits of ad hoc support, access-related issues were raised about therapists being unable to provide support for practical as well as emotional-based reasons. From a practical perspective, the therapists only had limited time on the units which meant ‘some people may not see her’ (HCP1), and if parents did not live in the catchment area, then support could not be offered. Healthcare staff were not always notified about the FWS therapists’ availability at the unit. This information was considered important to ensure effective signposting to, ‘just to say to a parent , well if you want to speak to anybody , we’ve got our counsellor in on such-a-day’ (HCP6). From an emotional perspective, it was recognised that therapeutic support was not suitable for all, such as those ‘who are very closed down’ (FWSS1) or ‘scared’ of disclosing negative emotions particularly ‘the ones where there are social issues’ (HCP6).
Regarding service delivery, while several service users made positive comments about the flexible nature of support, in terms of access, delivery and amount received, some wished the sessions had been longer. One also spoke of an ‘awkward finish’ when the one-to-one sessions were ending:
[So, it can be like] ohh sorry, I think I’ve lost track of time a little bit, I think we’re gonna have to pull it up there and we’re gonna have to end. So, I’ll be like, alright, OK, right, yeah fine. And it can be a bit clunky in the way that it finishes rather than it drawing naturally to a conclusion. (SU10:O&G)
Making a difference
In this section, we describe service users’ reflections on the psychological, cognitive, behavioural, and social benefits of FWS support. Four sub-themes are detailed - ‘tools for positive coping’ , ‘enhanced well-being’ , ‘improved relationships with others’ and ‘confidence in returning to work’ .
Tools for positive coping
Several service users described how the therapeutic tools they were taught as part of their therapy sessions either on the ward, one-to-one, or in the group provided positive coping mechanisms to help with ongoing adversities: with one describing them as a ‘ toolbox’ to draw on when needed (SU4:O&G). The techniques were reported to have helped them understand and articulate how they were feeling, ‘to unpick , how it was that I was feeling what I was struggling with (SU10:O&G) and the breathing and distraction techniques enabled them to ‘stop blaming myself and start breathing’ and to ‘do something else to try take my mind off it’ (SU2:O). Other service users referred to how the support had helped them to know ‘more about their triggers’ which helped them to feel strong and to retain a sense of control during uncontrollable and uncertain situations:
The tools just to step back and be like right, […] write down everything I can’t control and everything I can control of what my memories are and then cross everything I can’t change. Like I can’t control how sick she is. I can’t control her temperature, but what I can control is her feeds and being her mum and stuff like that […] They made me feel the strength that I’ve not felt in about 5 years. (SU5:A&O)
The therapeutic techniques provided by the therapists were an ongoing source of support to help service users in the extreme circumstances of the neonatal unit as well as in day-to-day life:
I relied on one of the meditations she sent me, and it just really, really centred me at night, even as I was feeling overwhelmed, just like putting my headphones in and just saying to my husband, if he wakes up and you just see to him, and that just helped me so much. (SU6:O)
Enhanced well-being
Many service users described how the FWS support had improved their psychological well-being, using terms such as feeling ‘lighter’ , more ‘optimistic’ and a ‘stronger person’ . Some service users referred to how the therapist had provided important crisis management. For one participant who received one-to-one therapy, this related to how the support helped to ‘pull her back’ from an emotional crisis each week, associated with the threats of a further potential pregnancy loss:
If I didn’t have [therapist] once a week, I dread to think where I would have been. It was kind of like, yeah, like each week she’d pull me back in, and then I’d probably go a bit crazy again, and then she’d pull me back in. (SU11:O)
Others described fundamental changes such as moving from a state of being unable to ‘ function properly’ to being back at work and ‘happy and getting on’ and feeling ‘like a different person ’ (SU4:O&G). Another service user also described how the one-to-one therapy had improved her well-being after a traumatic birth and neonatal stay to such an extent that she had become ‘ a better version’ of herself:
I just literally feel like me again, I suppose I think you just get so wrapped up with being mum and just being on all the time and as a mum you do normally lose your confidence and you do lose yourself so it’s more like feeling like me but even a better version that I liked of me. (SU6:O)
Improved relationships with others
Service users who received one-to-one or group-based support talked openly about how their relationships with their partners and family had been enhanced due to the support the FWS had provided. One reported how the support had helped her and her husband to ‘communicate with each other’ and ‘discuss how we were both feeling ’ (SU15:G). Another service user shared how the one-to-one telephone therapy had restored her relationship with her mother:
I don’t know what magic she’s done but my mum and my relationship it’s been really good to a point where before I couldn’t wait to get my mum out of my house, but now, it’s kind of like mum I need you and I appreciate you (SU16:O).
A further way the FWS support influenced relationships with others was regarding a future conception. While following a traumatic birth, neonatal stay or loss of a baby, individuals can be hesitant to have more children [ 25 ], the FWS was reported to have helped service users’ address these concerns. Bereavement group participants also reported finding hope for future family planning together, thereby enabling a futural peer support element to the therapeutic intervention:
Hopefully, we’ll be able to support each other, hopefully in the future through future pregnancies. Like it’d just be amazing if we all managed to get pregnant together and had our babies together that’d just be unbelievable. (SU15:G)
Confidence in returning to work
Service users who had received one-to-one support reflected on how the support had helped them to address their anxieties in returning to paid employment:
[Baby] is going to nursery that was quite triggering […] And I think if I had to deal with that a long time ago, like a few months ago, I’d have just blow my head there, I just couldn’t have done that. But now, I’ve just been, like, really calm and just quite open to it and just, sort of kept my cool really. (SU6:O)
Another service user who had experienced a neonatal loss reported: ‘ If I hadn’t had had the support I wouldn’t have gone back to work and I’d probably be in a much darker place’ (SU13:O). This woman reflected that working was positive for her emotional well-being, and how this would not have been possible without the support from the FWS.
In this paper, we present findings from an evaluation of a charity that provided ad hoc support, formal therapy and group support to service users who had a premature and/or sick infant or who had suffered a perinatal loss. We highlight the informational, contextual, and relational basis of how the support was experienced, and the cognitive, emotional, and interpersonal impacts of the FWS for service users. The findings of this paper contribute to the evidence supporting the need for emotional and psychological support for those who experience adverse maternity and neonatal outcomes in the perinatal period [ 3 ]. Overall, there appear to be key mechanisms - defined as the entities or activities responsible for the phenomenon (i.e., positive experiences and impact of FWS support) [ 26 ] – that underpinned effective support, irrespective of whether it was delivered on a one-to-one or group basis. These mechanisms include clear information, flexibility (in access and/or delivery), being independent of statutory provision, focused on individual needs, active listening, the use of therapeutic tools, and positive relationships with the therapist. Furthermore, while ‘ shared experiences’ are a key mechanism of group-based support, this was also evident in one-to-one therapy when service users received support from a therapist with a shared history.
A number of our findings echo those reported in a recent qualitative systematic review of women’s experiences of specialist perinatal mental health services [ 22 ]. Similar findings concern the importance of the therapist-service user relationship, with the therapist’s open, non-judgemental, and person-centred approach found to be essential to meaningful service experiences [ 22 ]. As reported in the review, and in our study, continuity was a key feature of relationship building that engendered safety and dependability [ 22 ] and for meaningful change. While some of the included papers in the review reported how women felt clinicians had real insight and understanding of perinatal mental health conditions [ 27 , 28 , 29 ], in our work, this also related to the therapists sharing their personal experience of perinatal mental health and/or loss. These findings resonate with those by Cleary and Armour who explored the dual identity of counsellors and therapists with experiential experiences of mental health issues [ 30 ] whereby self-disclosure enhanced the therapeutic relationship. They also concur with a qualitative study by Parker et al. who found counsellors having a working knowledge of neonates and the neonatal environment was crucial [ 31 ].
Similar to the wider literature, we found that service users benefitted from receiving support independent of health care and focused on their needs as individuals [ 32 , 33 ]. This finding further supports the need for independent specialist support such as provided within the UK-based specialist perinatal mental health and maternal mental health services [ 3 ]. While specialist mental health support has been found to help service users understand their infant’s needs and develop parent-infant relationships [ 22 , 27 , 34 ], in our study, the benefits were more individualised and included enhanced personal and social well-being. Our findings of the positive impacts of group-based support also align with the wider literature regarding the value of receiving validation and reassurance from peers with shared experiences [ 29 , 35 , 36 ], as well as opportunities for ongoing social support after the groups had ended [ 35 ]. The benefits gained via support from the therapists and within the groups signal post-traumatic growth described as “positive psychological change experienced as the result of the struggle with highly challenging life circumstances” [ 37 ]. This was evidenced through women feeling stronger, developing new relationships, more able to cope with future adversities and with a new and improved outlook on themselves and their situation [ 37 ].
Flexibility in rearranging appointments and the location of support being organised to suit individual service users encouraged access and an openness to share personal issues [ 22 ]. While complaints have been reported in the previous literature about service users being unaware of wider support provision and a lack of follow-up support [ 22 , 36 ], in our study, we found that tailored information and communications provided at multiple points helped facilitate engagement. Although resource-related challenges concerning the availability of the therapists on the unit and a lack of communication as to when this support was available were noted. A further difficulty related to the reported time lag following an initial assessment: this signifies a need for ongoing contact to ensure service users gain access to the right support at the right time [ 38 ]. Proactive support is a central tenet of emotional-based care [ 39 ]. This was clear in our study as the proactive nature of the support was essential to provide parents with care at a harrowing time and to facilitate access to more structured support post-infant discharge. However, as some service users can be reluctant to disclose perinatal mental health problems, due to feeling overwhelmed or potential fears of stigma and negative reprisals [ 40 ], alternative methods to ensure that all parents receive timely support is needed. Furthermore, despite service users from minoritised ethnic communities being at increased risk of poor perinatal mental health [ 41 , 42 , 43 ], they are less likely to access support [ 40 , 43 ]. A recent systematic review to explore the reasons why minoritised ethnic women do not access mental health services identified barriers at the individual (stigma, lack of awareness), organisational (inadequate resources), sociocultural (language, cultural barriers) and structural (lack of clear policies) levels [ 44 ]. Therefore, while approaching parents in the neonatal unit may help to overcome some of these barriers, further work to elicit if and how this can influence access to specialist support amongst ethnically minoritised service users is needed.
The limitations of this study are that overall, only ~ 30% of service users who accessed one-to-one therapy consented to share their demographic and outcome data for the evaluation. However, typically studies involving mental health intervention have difficulties with recruitment and retention of participants and often achieve very low response rates [ 45 ]. It also suggests that further work on how to encourage consent and provide reassurance about how their data will be used may be needed. The intention was to interview ~ 20 service users, with only 16 recruited, despite numerous recruitment efforts. This may be due to asking service users to participate while still receiving support, and indicates that other potentially more sensitive methods, such as writing to participants after they have ended support with the FWS may have been more successful. Also, while all service users had the opportunity to be re-interviewed ~ 6 months later, only two took up this offer – both of whom had received one-to-one therapy. This low take-up may be due to symptom resolution or symptom continuation, both of which could be associated with concerns for re-triggering or magnifying negative emotions. More flexible ways, such as using a journal, may encourage long-term qualitative insights to be captured. A further limitation is that over 30% of the participants had received more than one type of support and any nuances in the experiences of the different support options were not fully explored in the interviews. Most of the participants were from a White demographic background, which may reflect wider barriers to access to mental health support in ethnic minority populations [ 40 ]. We also intended to interview more healthcare professionals, and the small number recruited is likely indicative of busy, time-poor professionals. Future research could include focus groups incorporated as part of existing professional-based meetings to maximise participation. However, despite the recruitment challenges, a total of 35 participants is a large sample for qualitative research, and generated rich, in-depth insights into the views, experiences, impacts, facilitators, and challenges associated with the FWS.
This study describes how psychological support was provided for service users experiencing adverse maternity and neonatal outcomes and the impact of this support on individual and familial well-being. This work complements existing research into perinatal counselling-based interventions and highlights the value of providing therapeutic support during a sensitive time. Despite study limitations, the findings signify the need for independent, timely, flexible, needs-based, proactive, well-resourced psychological-based support. They also emphasise how the therapists’ open and non-judgmental approach and experiential knowledge are essential mechanisms of meaningful service provision. Implications for practice concern better communication regarding support availability, and timely follow-ups. Further means to engage those less willing to take up mental health support and who may have greater needs should be developed.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B, Hogg S. The costs of perinatal mental health problems. London: Centre for Mental Health and London School of Economics. 2014. Costs of perinatal mental health problems - Centre for Mental Health.
Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49(6):608–15.
Article PubMed Google Scholar
National Health Service, Long-Term NHS. Plan. 2019. NHS Long Term Plan » The NHS Long Term Plan.
Goodman A, Goodman R. Population mean scores predict child mental disorder rates: validating SDQ prevalence estimators in Britain. J Child Psychol Psychiatry. 2011;52(1):100–8.
Fitzsimons E, Goodman A, Kelly E, Smith JP. Poverty dynamics and parental mental health: determinants of childhood mental health in the UK. Soc Sci Med. 2017;175:43–51.
Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH, et al. Closeness and separation in neonatal intensive care. Acta Paediatr. 2012;101(10):1032–7.
Article PubMed PubMed Central Google Scholar
Thomson G, Feeley C, Types. Evidence, and resources of interventions focused on improving the Psychosocial Well-being of parents of Premature/Sick infants: a scoping review. Advances in neonatal care. official journal of the National Association of Neonatal Nurses; 2021.
Nguyen CTT, Sandhi A, Lee GT, Nguyen LTK, Kuo S-Y. Prevalence of and factors associated with postnatal depression and anxiety among parents of preterm infants: a systematic review and meta-analysis. J Affect Disord. 2022.
Malouf R, Harrison S, Burton HA, Gale C, Stein A, Franck LS, Alderdice F. Prevalence of anxiety and post-traumatic stress (PTS) among the parents of babies admitted to neonatal units: a systematic review and meta-analysis. EClinicalMedicine. 2022;43.
Kersting A, Wagner B. Complicated grief after perinatal loss. Dialog Clin Neurosci. 2022;14(2):187–94.
Article Google Scholar
Kishimoto M, Yamaguchi A, Niimura M, Mizumoto M, Hikitsuchi T, Ogawa K, et al. Factors affecting the grieving process after perinatal loss. BMC Womens Health. 2021;21:1–6.
Shear MK, Simon N, Wall M, Zisook S, Neimeyer R, Duan N, et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28(2):103–17.
Andersen LB, Melvaer LB, Videbech P, Lamont RF, Joergensen JS. Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. 2012;91(11):1261–72.
Sutan R, Miskam HM. Psychosocial impact of perinatal loss among muslim women. BMC Womens Health. 2012;12(1):1–9.
Support Like a Walking Stick. Parent-Buddy matching for Language and Culture in the NICU. Neonatal Netw. 2011;30(2):89–98.
Flacking R, Ewald U, Nyqvist KH, Starrin B. Trustful bonds: a key to becoming a mother and to reciprocal breastfeeding. Stories of mothers of very preterm infants at a neonatal unit. Soc Sci Med. 2006;62(1):70–80.
George K, Axelin A, Feeley N, Cambell-Yeo M, Tandberg BS, Szczapa T. Symptoms of depression in parents after discharge from NICU associated with family-centred care. Women Birth. 2022;35:23–4.
Franck LS, Gay CL, Hoffmann TJ, Kriz RM, Bisgaard R, Cormier DM, et al. Maternal mental health after infant discharge: a quasi-experimental clinical trial of family integrated care versus family-centered care for preterm infants in US NICUs. BMC Pediatr. 2023;23(1):1–10.
Charpak N, Gabriel Ruiz J, Zupan J, Cattaneo A, Figueroa Z, Tessier R, et al. Kangaroo mother care: 25 years after. Acta Paediatr. 2005;94(5):514–22.
Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the creating opportunities for parent empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118(5):e1414–27.
Shaohua L, Shorey S. Psychosocial interventions on psychological outcomes of parents with perinatal loss: a systematic review and meta-analysis. Int J Nurs Stud. 2021;117:103871.
Moran E, Noonan M, Mohamad MM, O’Reilly P. Women’s experiences of specialist perinatal mental health services: a qualitative evidence synthesis. Arch Women Ment Health. 2023:1–19.
Hunter D, McCallum J, Howes D. Defining exploratory-descriptive qualitative (EDQ) research and considering its application to healthcare. J Nurs Health Care. 2019;4(1).
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qualitative Res Sport Exerc Health. 2019;11(4):589–97.
Fenech G, Thomson G. Tormented by ghosts from their past’: a meta-synthesis to explore the psychosocial implications of a traumatic birth on maternal well-being. Midwifery. 2014;30(2):185–93.
Illari PM, Williamson J. What is a mechanism? Thinking about mechanisms across the sciences. Eur J Philos Sci. 2012;2:119–35.
Coates D, Davis E, Campbell L. The experiences of women who have accessed a perinatal and infant mental health service: a qualitative investigation. Adv Mental Health. 2017;15(1):88–100.
Lever Taylor B, Cavanagh K, Strauss C. The effectiveness of mindfulness-based interventions in the perinatal period: a systematic review and meta-analysis. PLoS ONE. 2016;11(5):e0155720.
Powell C, Bedi S, Nath S, Potts L, Trevillion K, Howard L. Mothers’ experiences of acute perinatal mental health services in England and Wales: a qualitative analysis. J Reproductive Infant Psychol. 2022;40(2):155–67.
Cleary R, Armour C. Exploring the role of practitioner lived experience of mental health issues in counselling and psychotherapy. Counselling Psychother Res. 2022;22(4):1100–11.
Parker L. Mothers’ experience of receiving counselling/psychotherapy on a neonatal intensive care unit (NICU). J Neonatal Nurs. 2011;17(5):182–9.
Thomson G, Mortimer R, Baybutt M, Whittaker K. Evaluation of birth companions perinatal and peer support provision in two prison settings in England: a mixed-methods study. Int J Prison Health. 2022.
Balaam M-C, Kingdon C, Thomson G, Finlayson K, Downe S. We make them feel special’: the experiences of voluntary sector workers supporting asylum seeking and refugee women during pregnancy and early motherhood. Midwifery. 2016;34:133–40.
Wright T, Jowsey T, Stanton J, Elder H, Stevens S, Wouldes TA. Patient experience of a psychiatric Mother Baby Unit. PLoS ONE. 2018;13(5):e0198241.
Griffiths J, Lever Taylor B, Morant N, Bick D, Howard LM, Seneviratne G, Johnson S. A qualitative comparison of experiences of specialist mother and baby units versus general psychiatric wards. BMC Psychiatry. 2019;19:1–15.
Article CAS Google Scholar
Viveiros CJ, Darling EK. Barriers and facilitators of accessing perinatal mental health services: the perspectives of women receiving continuity of care midwifery. Midwifery. 2018;65:8–15.
Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq. 2004;15(1):1–18.
Royal College of Midwives. Strengthening perinatal mental health: A roadmap to the right support at the right time. 2023. rcm-perinatal-mental-health-report-2023.pdf .
Gray M, Monti K, Katz C, Klipstein K, Lim S. A Mental Health PPE model of proactive mental health support for frontline health care workers during the COVID-19 pandemic. Psychiatry Res. 2021;299:113878.
Article CAS PubMed PubMed Central Google Scholar
Webb R, Uddin N, Constantinou G, Ford E, Easter A, Shakespeare J, et al. Meta-review of the barriers and facilitators to women accessing perinatal mental healthcare. BMJ Open. 2023;13(7):e066703.
Womersley K, Ripullone K, Hirst JE. Tackling inequality in maternal health: beyond the postpartum. Future Healthc J. 2021;8(1):31.
Prady SL, Endacott C, Dickerson J, Bywater TJ, Blower SL. Inequalities in the identification and management of common mental disorders in the perinatal period: an equity focused re-analysis of a systematic review. PLoS ONE. 2021;16(3):e0248631.
Watson H, Harrop D, Walton E, Young A, Soltani H. A systematic review of ethnic minority women’s experiences of perinatal mental health conditions and services in Europe. PLoS ONE. 2019;14(1):e0210587.
Webb R, Ford E, Shakespeare J, Easter A, Alderdice F, Holly J, et al. Conceptual framework on barriers and facilitators to implementing perinatal mental health care and treatment for women: the MATRIx evidence synthesis. Health Social Care Delivery Res. 2024;12(2):1–187.
Brown JS, Murphy C, Kelly J, Goldsmith K. How can we successfully recruit depressed people? Lessons learned in recruiting depressed participants to a multi-site trial of a brief depression intervention (the ‘CLASSIC’ trial). Trials. 2019;20:1–12.
Download references
Acknowledgements
Thanks to all the participants for their time and invaluable contributions.
The research was commissioned and funded by Lancashire Women.
Author information
Authors and affiliations.
School of Nursing and Midwifery, University of Central Lancashire, Preston, UK
Gill Thomson, Lara McNally & Rebecca Nowland
You can also search for this author in PubMed Google Scholar
Contributions
GT was project lead who designed the original study, with support from RN. LN conducted interviews. LN and GT developed a coding framework which was applied to the transcripts by LN. All authors reviewed analyses and agreed final analytical decisions. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Gill Thomson .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was received from the Health ethics committee at the University of Central Lancashire (project no: 0262). All participants provided verbal consent to participate in the study, which was audio-recorded.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Thomson, G., McNally, L. & Nowland, R. Experiences and impacts of psychological support following adverse neonatal experiences or perinatal loss: a qualitative analysis. BMC Pregnancy Childbirth 24 , 569 (2024). https://doi.org/10.1186/s12884-024-06713-7
Download citation
Received : 21 March 2024
Accepted : 22 July 2024
Published : 30 August 2024
DOI : https://doi.org/10.1186/s12884-024-06713-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Perinatal loss
- Mental health
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 02 September 2024
Clinical supervisor’s experiences of peer group clinical supervision during COVID-19: a mixed methods study
- Owen Doody ORCID: orcid.org/0000-0002-3708-1647 1 ,
- Kathleen Markey ORCID: orcid.org/0000-0002-3024-0828 1 ,
- James Turner ORCID: orcid.org/0000-0002-8360-1420 2 ,
- Claire O. Donnell ORCID: orcid.org/0000-0003-2386-7048 1 &
- Louise Murphy ORCID: orcid.org/0000-0003-2381-3963 1
BMC Nursing volume 23 , Article number: 612 ( 2024 ) Cite this article
Metrics details
Providing positive and supportive environments for nurses and midwives working in ever-changing and complex healthcare services is paramount. Clinical supervision is one approach that nurtures and supports professional guidance, ethical practice, and personal development, which impacts positively on staff morale and standards of care delivery. In the context of this study, peer group clinical supervision provides allocated time to reflect and discuss care provided and facilitated by clinical supervisors who are at the same grade/level as the supervisees.
To explore the clinical supervisor’s experiences of peer group clinical supervision a mixed methods study design was utilised within Irish health services (midwifery, intellectual disability, general, mental health). The Manchester Clinical Supervision Scale was used to survey clinical supervisors ( n = 36) and semi-structured interviews ( n = 10) with clinical supervisors were conducted. Survey data were analysed through SPSS and interview data were analysed utilising content analysis. The qualitative and quantitative data’s reporting rigour was guided by the CROSS and SRQR guidelines.
Participants generally had a positive encounter when providing clinical supervision. They highly appreciated the value of clinical supervision and expressed a considerable degree of contentment with the supervision they provided to supervisees. The advantages of peer group clinical supervision encompass aspects related to self (such as confidence, leadership, personal development, and resilience), service and organisation (including a positive working environment, employee retention, and safety), and patient care (involving critical thinking and evaluation, patient safety, adherence to quality standards, and elevated levels of care).
There are many benefits of peer group clinical supervision at an individual, service, organisation, and patient level. Nevertheless, there is a need to address a lack of awareness and misconceptions surrounding clinical supervision to create an environment and culture conducive to realising its full potential. It is crucial that clinical supervision be accessible to nurses and midwives of all grades across all healthcare services, with national planning to address capacity and sustainability.
Peer Review reports
Within a dynamic healthcare system, nurses and midwives face growing demands, underscoring the necessity for ongoing personal and professional development. This is essential to improve the effectiveness and efficiency of care delivery for patients, families, and societies. Despite the increased emphasis on increasing the quality and safety of healthcare services and delivery, there is evidence highlighting declining standards of nursing and midwifery care [ 1 ]. The recent focus on re-affirming and re-committing to core values guiding nursing and midwifery practice is encouraging such as compassion, care and commitment [ 2 ], competence, communication, and courage [ 3 ]. However, imposing value statements in isolation is unlikely to change behaviours and greater consideration needs to be given to ways in which compassion, care, and commitment are nurtured and ultimately applied in daily practice. Furthermore, concerns have been raised about global staff shortages [ 4 ], the evidence suggesting several contributing factors such as poor workforce planning [ 5 ], job dissatisfaction [ 6 ], and healthcare migration [ 7 ]. Without adequate resources and staffing, compromising standards of care and threats to patient safety will be imminent therefore the importance of developing effective strategies for retaining competent registered nurses and midwives is paramount in today’s climate of increased staff shortages [ 4 ]. Clinical supervision serves as a means to facilitate these advancements and has been linked to heightened job satisfaction, enhanced staff retention, improved staff effectiveness, and effective clinical governance, by aiding in quality improvements, risk management, and heightened accountability [ 8 ].
Clinical supervision is a key component of professional practice and while the aim is largely known, there is no universally accepted definition of clinical supervision [ 8 ]. Clinical supervision is a structured process where clinicians are allowed protected time to reflect on their practice within a supportive environment and with the purpose of developing high-quality clinical care [ 9 ]. Recent literature published on clinical supervision [ 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 ] highlights the advantages and merits of clinical supervision. However, there are challenges also identified such as a lack of consensus regarding the meaning and goal, implementation issues, variations in approaches in its operationalisation, and an absence of research evidence on its effectiveness. Duration and experience in clinical supervision link to positive benefits [ 8 ], but there is little evidence of how clinical supervision altered individual behaviours and practices. This is reinforced by Kuhne et al., [ 15 ] who emphasise that satisfaction rather than effectiveness is more commonly examined. It is crucial to emphasise that reviews have pinpointed that clinical supervision lowers the risks of adverse patient outcomes [ 9 ] and demonstrates enhancements in the execution of certain care processes. Peer group clinical supervision is a form of clinical supervision whereby two or more practitioners engage in a supervision or consultation process to improve their professional practice [ 17 ]. There is limited evidence regarding peer group clinical supervision and research on the experiences of peer clinical supervision and stakeholders is needed [ 13 ]. In Ireland, peer group clinical supervision has been recommended and guidelines have been developed [ 18 ]. In the Irish context, peer clinical supervision is where both clinical supervisees and clinical supervisors are peers at the same level/grade. However, greater evidence is required to inform future decisions on the implementation of peer group clinical supervision and the purpose of this study is to explore clinical supervisors’ experiences of peer group clinical supervision. As the focus is on peer group supervisors and utilising mixed methods the experiences of the other stakeholders were investigated and reported separately.
A mixed methods approach was used (survey and semi-structured interviews) to capture clinical supervisor’s experiences of clinical supervision. The study adhered to the Consensus-Based Checklist for Reporting of Survey Studies guidelines [ 19 ] (Supplementary File S1 ) and Standards for Reporting Qualitative Research guidelines [ 20 ] (Supplementary File S2 ).
Participants
This study was conducted with participants who successfully completed a professionally credited award: clinical supervision module run by a university in Ireland (74 clinical supervisors across 5 programmes over 3 years). The specific selection criteria for participants were that they were registered nurses/midwives delivering peer group clinical supervision within the West region of Ireland. The specific exclusion criteria were as follows: (1) nurses and midwives who haven’t finished the clinical supervision module at the University, (2) newly appointed peer group clinical supervisors who have yet to establish their groups and initiate the delivery of peer group clinical supervision.
Measures and procedures
The Manchester Clinical Supervision Scale-26 was used to survey participants in February/March 2022 and measure the peer group clinical supervisors’ overall experiences of facilitating peer group clinical supervision. The Manchester Clinical Supervision Scale-26 is a validated 26-item self-report questionnaire with a Likert-type (1–5) scale ranging from strongly disagree (1) to strongly agree (5) [ 21 ]. The Manchester Clinical Supervision Scale-26 measures the efficiency of and satisfaction with supervision, to investigate the skills acquisition aspect of clinical supervision and its effect on the quality of clinical care [ 21 ]. The instrument consists of two main sections to measure three (normative, restorative, and formative) dimensions of clinical supervision utilising six sub-scales: (1) trust and rapport, (2) supervisor advice/support, (3) improved care/skills, (4) importance/value of clinical supervision, (5) finding time, (6) personal issues/reflections and a total score for the Manchester Clinical Supervision Scale-26 is also calculated. Section two consisted of the demographic section of the questionnaire and was tailored to include eight demographic questions concerning the supervisor’s demographics, supervisee characteristics, and characteristics of clinical supervision sessions. There were also two open field questions on the Manchester Clinical Supervision Scale-26 (model of clinical supervision used and any other comments about experience of peer group clinical supervision). The main question about participants’ experiences with peer clinical supervision was “What was your experience of peer clinical supervision?” This was gathered through individual semi-structured interviews lasting between 20 and 45 min, in March/April 2022 (Supplementary file 3 ).
Ethical considerations
Health service institutional review boards of two University hospitals approved this study (Ref: 091/19 and Ref: C.A. 2199). Participants were recruited after receiving a full explanation of the study’s purpose and procedure and all relevant information. Participants were aware of potential risks and benefits and could withdraw from the study, or the survey could be stopped at any time. Informed consent was recorded, and participant identities were protected by using a pseudonym to protect anonymity.
Data analysis method
Survey data was analysed using the data analysis software package Statistical Package for the Social Sciences, version 26 (SPSS Inc., Chicago, Il, USA). Descriptive analysis was undertaken to summarise responses to all items and categorical variables (nominal and ordinal) were analysed using frequencies to detail the number and percentage of responses to each question. Scores on the Manchester Clinical Supervision Scale-26 were reverse scored for 9 items (Q1-Q6, Q8, Q20,21) and total scores for each of the six sub-scales were calculated by adding the scores for each item. Raw scores for the individual sub-scales varied in range from 0 to 20 and these raw scores were then converted to percentages which were used in addition to the raw scores for each sub-scale to describe and summarise the results of the Manchester Clinical Supervision Scale-26. Cronbach’s alpha coefficient was undertaken with the 26 questions included within the Manchester Clinical Supervision Scale-26 and more importantly with each of the dimensions in the Manchester Clinical Supervision Scale-26. The open-ended questions on the Manchester Clinical Supervision Scale-26 and interviews were analysed using content analysis guided by Colorafi and Evans [ 22 ] and categories were generated using their eight steps, (1) creating a coding framework, (2) adding codes and memos, (3) applying the first level of coding, (4) categorising codes and applying the second level of coding, (5) revising and redefining the codes, (6) adding memos, (7) visualising data and (8) representing the data.
Research rigour
To ensure the validity and rigour of this study the researchers utilised the Manchester Clinical Supervision Scale-26 a recognised clinical supervision tool with good reliability and wide usage. Interviews were recorded, transcribed, and verified by four participants, data were collected until no new components appeared, data collection methods and analysis procedures were described, and the authors’ biases were minimised throughout the research process. The Manchester Clinical Supervision Scale-26 instrument internal consistency reliability was assessed which was overall good (α = 0.878) with individual subscale also good e.g., normative domain 0.765, restorative domain 0.864, and formative domain 0.900. Reporting rigour was demonstrated using the Consensus-Based Checklist for Reporting of Survey Studies guidelines [ 19 ] and Standards for Reporting Qualitative Research guidelines [ 20 ].
Quantitative data
Participant and clinical supervision characteristics.
Thirty-six of the fifty-two (69.2%) peer group clinical supervisors working across a particular region of Ireland responded to the Manchester Clinical Supervision Scale-26 survey online via Qualtrics. Table 1 identifies the demographics of the sample who were predominantly female (94.4%) with a mean age of 44.7 years (SD. 7.63).
Peer group clinical supervision session characteristics (Table 2 ) highlight over half of peer group clinical supervisors ( n = 20, 55.6%) had been delivering peer group clinical supervision for less than one year and were mainly delivered to female supervisees ( n = 28, 77.8%). Most peer group clinical supervision sessions took place monthly ( n = 32, 88.9%) for 31–60 min ( n = 27, 75%).
Manchester Clinical Supervision Scale-26 results
Participants generally viewed peer group clinical supervision as effective (Table 3 ), the total mean Manchester Clinical Supervision Scale-26 score among all peer group clinical supervisors was 76.47 (SD. 12.801) out of 104, Surpassing the clinical supervision threshold score of 73, which was established by the developers of the Manchester Clinical Supervision Scale-26 as the benchmark indicating proficient clinical supervision provision [ 21 ]. Of the three domains; normative, formative, and restorative, the restorative domain scored the highest (mean 28.56, SD. 6.67). The mean scores compare favourably to that of the Manchester Clinical Supervision Scale-26 benchmark data and suggest that the peer group clinical supervisors were satisfied with both the level of support, encouragement, and guidance they provided and the level of trust/rapport they had developed during the peer group clinical supervision sessions. 83.3% ( n = 30) of peer group clinical supervisors reported being either very satisfied ( n = 12, 33.3%) or moderately satisfied ( n = 18, 50%) with the peer group clinical supervision they currently delivered. Within the peer group clinical supervisor’s supervisee related issues ( n = 17, 47.2%), work environment-related issues ( n = 16, 44.4%), staff-related issues ( n = 15, 41.7%) were reported as the most frequent issues, with patient/client related issues being less frequent ( n = 8, 22.2%). The most identified model used to facilitate peer group clinical supervision was the Proctors model ( n = 8, 22.22%), which was followed by group ( n = 2, 5.55%), peer ( n = 2, 5.55%), and a combination of the seven-eyed model of clinical supervision and Proctors model ( n = 1, 2.77%) with some not sure what model they used ( n = 2, 5.553%) and 58.33% ( n = 21) did not report what model they used.
Survey open-ended question
‘Please enter any additional comments , which are related to your current experience of delivering Peer Group Clinical Supervision.’ There were 22 response comments to this question, which represented 61.1% of the 36 survey respondents, which were analysed using content analysis guided by Colorafi & Evans [ 22 ]. Three categories were generated. These included: personal value/benefit of peer group clinical supervision, challenges with facilitating peer group clinical supervision, and new to peer group clinical supervision.
The first category ‘personal value/benefit of peer group clinical supervision’ highlighted positive experiences of both receiving and providing peer group clinical supervision. Peer group clinical supervisors reported that they enjoyed the sessions and found them both worthwhile and beneficial for both the group and them as peer group clinical supervisors in terms of creating a trusted supportive group environment and motivation to develop. Peer group clinical supervision was highlighted as very important for the peer group clinical supervisors working lives and they hoped that there would be more uptake from all staff. One peer group clinical supervisor expressed that external clinical supervision was a ‘lifeline’ to shaping their supervisory journey to date.
The second category ‘challenges with facilitating peer group clinical supervision’, identified time constraints, lack of buy-in/support from management, staff shortages, lack of commitment by supervisees, and COVID-19 pandemic restrictions and related sick leave, as potential barriers to facilitating peer group clinical supervision. COVID-19 was perceived to have a negative impact on peer group clinical supervision sessions due to staff shortages, which resulted in difficulties for supervisees attending the sessions during work time. Peer group clinical supervisors felt that peer group clinical supervision was not supported by management and there was limited ‘buy-in’ at times. There was also a feeling expressed that peer group clinical supervision was in its infancy, as COVID-19 and its related restrictions impacted on this by either slowing down the process of commencing peer group clinical supervision in certain areas or having to move online. However, more recently improvements in managerial support and supervisee engagement with the peer group clinical supervision process are noted.
The final category ‘new to peer group clinical supervision’ highlighted that some peer group clinical supervisors were new to the process of providing peer group clinical supervision and some felt that this survey was not a true reflection of their experience of delivering peer group clinical supervision, as they were not fully established yet as clinical supervisors due to the impact of COVID-19. Peer group clinical supervisors identified that while they were new to providing peer group clinical supervision, they were enjoying it and that it was a learning curve for them.
Qualitative data
The qualitative phase explored peer group clinical supervisors’ ( n = 10) own experiences of preparation received and experiences of being a peer group clinical supervisor. Three themes were identified through data analysis, building the foundations, enacting engagement and actions, and realities (Table 4 ).
Building the foundations
This theme highlights the importance of prior knowledge, awareness, and training but also the recruitment process and education in preparing peer group clinical supervisors.
Knowledge and awareness
Participant’s prior knowledge and awareness of peer group clinical supervision was mixed with some reporting having little or no knowledge of clinical supervision.
I’m 20 years plus trained as a nurse , and I had no awareness of clinical supervision beforehand , I really hadn’t got a clue what all of this was about , so it was a very new concept to me (Bernie) .
Others were excited about peer group clinical supervision and while they could see the need they were aware that there may be limited awareness of the value and process of clinical supervision among peers.
I find that there’s great enthusiasm and passion for clinical supervision as it’s a great support mechanism for staff in practice , however , there’s a lack of awareness of clinical supervision (Jane) .
Recruitment
Some participants highlighted that the recruitment process to become a peer group clinical supervisor was vague in some organisations with an unclear and non-transparent process evident where people were chosen by the organisation’s management rather than self-selecting interested parties.
It was just the way the training was put to the people , they were kind of nominated and told they were going and there was a lot of upset over that , so they ended up in some not going at all (Ailbhe) .
In addition, the recruitment process was seen as top loaded where senior grades of staff were chosen, and this limited staff nurse grade opportunities where there was a clear need for peer group clinical supervisors and support.
We haven’t got down to the ground level like you know we’ve done the directors , we’ve done the CNM3s the CNM2s we are at the CNM1s , so we need to get down to the staff nurse level so the nurses at the direct frontline are left out and aren’t receiving supervision because we don’t have them trained (Bernie) .
Training and education
Participants valued the training and education provided but there was a clear sense of ‘imposter syndrome’ for some peer group clinical supervisors starting out. Participants questioned their qualifications, training duration, and confidence to undertake the role of peer group clinical supervisor.
Because it is group supervision and I know that you know they say that we are qualified to do supervision and you know we’re now qualified clinical supervisors but I’m not sure that a three-month module qualifies you to be at the top of your game (Maria) .
Participants when engaged in the peer group clinical supervisor educational programme did find it beneficial and the true benefit was the actual re-engagement in education and published evidence along with the mix of nursing and midwifery practice areas.
I found it very beneficial , I mean I hadn’t been engaged in education here in a while , so it was great to be back in that field and you know with the literature that’s big (Claire) .
Enacting engagement and actions
This theme highlights the importance of forming the groups, getting a clear message out, setting the scene, and grounding the group.
Forming the groups
Recruitment for the group was of key importance to the peer group clinical supervisor and they all sent out a general invitation to form their group. Some supervisors used invitation letters or posters in addition to a general email and this was effective in recruiting supervisees.
You’re reaching out to people , I linked in with the ADoN and I put together a poster and circulated that I wasn’t ‘cherry picking , and I set up a meeting through Webex so people could get a sense of what it was if they were on the fence about it or unsure if it was for them (Karen) .
In forming the peer clinical supervision groups consideration needs to be given to the actual number of supervisees and participants reported four to six supervisees as ideal but that number can alter due to attendance.
The ideal is having five or six consistent people and that they all come on board and that you get the dynamics of the group and everything working (Claire) .
Getting a clear message out
Within the recruitment process, it was evident that there was a limited and often misguided understanding or perception of peer group clinical supervision.
Greater awareness of what actually clinical supervision is , people misjudge it as a supervision where someone is appraising you , when in fact it is more of a support mechanism , I think peer support is the key element that needs to be brought out (Jane) .
Given the lack of clarity and understanding regarding peer group clinical supervision, the participants felt strongly that further clarity is needed and that the focus needs to be on the support it offers to self, practice, and the profession.
Clinical supervision to me is clinical leadership (Jane) .
Setting the scene and grounding the group
In the initial phase of the group coming together the aspect of setting the scene and grounding the group was seen as important. A key aspect of this process was establishing the ground rules which not only set the boundaries and gave structure but also ensured the adoption of principles of trust, confidentiality, and safety.
We start with the ground rules , they give us structure it’s our contract setting out the commitment the expectation for us all , and the confidentiality as that’s so important to the trust and safety and building the relationships (Brid) .
Awareness of group dynamics is important in this process along with awareness of the group members (supervisees) as to their role and expectations.
I reiterate the role of each person in relation to confidentiality and the relationship that they would have with each other within the group and the group is very much aware that it is based on respect for each person’s point of view people may have a fear of contributing to the group and setting the ground rules is important (Jane) .
To ground the group, peer group clinical supervisors saw the importance of being present and allowing oneself to be in the room. This was evident in the time allocated at the start of each session to allow ‘grounding’ to occur in the form of techniques such as a short meditation, relaxation, or deep breathing.
At the start , I do a bit of relaxation and deep breathing , and I saw that with our own external supervisor how she settled us into place so very much about connecting with your body and you’ve arrived , then always come in with the contract in my first sentence , remember today you know we’re in a confidential space , of course , you can take away information , but the only information you will take from today is your own information and then the respect aspect (Mary Rose) .
This settling in and grounding was seen as necessary for people to feel comfortable and engage in the peer group clinical supervision process where they could focus, be open, converse, and be aware of their role and the role of peer group clinical supervision.
People have to be open, open about their practice and be willing to learn and this can only occur by sharing, clinical supervision gives us the space to do it in a space where we know we will be respected, and we can trust (Claire) .
This theme highlights the importance of the peer group clinical supervisors’ past experiences, delivering peer group clinical supervision sessions, responding to COVID-19, personal and professional development, and future opportunities.
Past experiences
Past experiences of peer group clinical supervisors were not always positive and for one participant this related to the lack of ground rules or focus of the sessions and the fact it was facilitated by a non-nurse.
In the past , I suppose I would have found it very frustrating as a participant because I just found that it was going round in circles , people moaning and you know it wasn’t very solution focused so I came from my situation where I was very frustrated with clinical supervision , it was facilitated by somebody that was non-nursing then it wasn’t very , there wasn’t the ground rules , it was very loose (Caroline) .
However, many did not have prior experience of peer group clinical supervision. Nonetheless, through the education and preparation received, there was a sense of commitment to embrace the concept, practice, and philosophy.
I did not really have any exposure or really much information on clinical supervision , but it has opened my eyes , and as one might say I am now a believer (Brid) .
Delivering peer group clinical supervision
In delivering peer group clinical supervision, participants felt supervisees were wary, as they did not know what peer group clinical supervision was, and they had focused more on the word supervision which was misleading to them. Nonetheless, the process was challenging, and buy-in was questioned at an individual and managerial level.
Buy-in wasn’t great I think now of course people will blame the pandemic , but this all happened before the pandemic , there didn’t seem to be you know , the same support from management that I would have expected so I kind of understood it in a way because then there wasn’t the same real respect from the practitioners either (Mary Rose) .
From the peer group clinical supervisor’s perspective, they were all novices in delivering/facilitating peer group clinical supervision sessions, and the support of the external clinical supervisors, and their own peer group clinical supervision sessions were invaluable along with a clinical supervision model.
Having supervision myself was key and something that is vital and needed , we all need to look at our practice and how we work it’s no good just facilitating others without being part of the process yourself but for me I would say the three principles of clinical supervision , you know the normative , formative and restorative , I keep hammering that home and bring that in regularly and revisit the contract and I have to do that often you know (Claire) .
All peer group clinical supervisors commented on the preparation for their peer group clinical supervision sessions and the importance of them having the right frame of mind and that often they needed to read over their course work and published evidence.
I want everybody to have a shared voice and you know that if one person , there is something that somebody feels very strongly and wants to talk about it that they e-mail in advance like we don’t have a set agenda but that’s agreed from the participant at the start (Caroline) .
To assist this, the peer group clinical supervisors noted the importance of their own peer group clinical supervision, the support of their peers, and external clinical supervisors. This preparation in an unpredictable situation can be difficult but drawing on one’s experience and the experience within the group can assist in navigating beyond unexpected situations.
I utilise the models of clinical supervision and this helps guide me , I am more of a facilitator of the group we are experts in our own area and our own role but you can only be an expert if you take the time to examine your practice and how you operate in your role (Brid) .
All clinical supervisors noted that the early sessions can be superficial, and the focus can be on other practice or management issues, but as time moves on and people become more engaged and involved it becomes easier as their understanding of supervision becomes clearer. In addition, there may be hesitancy and people may have difficulty opening up with certain people in the group and this is a reality that can put people off.
Initially there was so much managerial bashing and I think through supervision , I began to kind of think , I need the pillars of supervision , the governance , bringing more knowledge and it shifted everything in the room , trying to marry it with all the tensions that people have (Mary Rose) .
For some clinical supervisors, there were expected and unexpected challenges for them as clinical supervisors in terms of the discussions veering off course and expectations of their own ability.
The other big challenge is when they go off , how do you bring him back , you know when they veer off and you’re expected to be a peer , but you have to try and recoil that you have to get the balance with that right (Mary Rose) .
While peer group clinical supervision is accepted and seen as a valuable process by the peer group clinical supervisors, facilitating peer group supervision with people known to you can be difficult and may affect the process.
I’d love to supervise a group where I actually don’t know the people , I don’t know the dynamics within the group , and I’d love to see what it would be like in a group (Bernie) .
Of concern to clinical supervisors was the aspect of non-attendance and while there may be valid reasons such as COVID-19 the absence of a supervisee for several sessions can affect the group dynamics, especially if the supervisee has only engaged with early group sessions.
One of the ones that couldn’t attend because of COVID and whatever , but she’s coming to the next one and I just feel there’s a lot of issues in her area and I suppose I’m mindful that I don’t want that sort of thing to seep in , so I suppose it’s just for me just to keep reiterating the ground rules and the boundaries , that’s something I just have to manage as a facilitator , but what if they don’t attend how far will the group have progressed before she attends (Caroline) .
Responding to COVID-19
The advent of COVID-19 forced peer group clinical supervisors to find alternative means of providing peer group clinical supervision sessions which saw the move from face-to-face to online sessions. The online transition was seen as seamless for many established groups while others struggled to deliver sessions.
With COVID we did online for us it was fine because we were already formed (Corina) .
While the transition may have been positive many clinical supervisors came across issues because they were using an online format that would not be present in the face-to-face session.
We did have a session where somebody was in the main office and they have a really loud booming voice and they were saying stuff that was not appropriate to say outside of clinical supervision and I was like are you in the office can you lower it down a bit can you put your headphones on (Maria) .
However, two peer group clinical supervisors ceased or hasted the progress of rolling out peer group clinical supervision sessions mainly due to redeployment and staff availability.
With COVID it just had to be canceled here , it’s just the whole thing was canceled so it was very , very difficult for people (Mary Rose) .
It was clear from clinical supervisors that online sessions were appropriate but that they felt they were only appropriate for existing established groups that have had the opportunity to build relationships, develop trust, embed the ground rules, and create the space for open communication and once established a combined approach would be appropriate.
Since we weren’t as established as a group , not everybody knew each other it would be difficult to establish that so we would hold off/reschedule , obviously COVID is a major one but also I suppose if you have an established group now , and again , you could go to a remote one , but I felt like since we weren’t established as a group it would be difficult to develop it in that way (Karen) .
Within practice COVID-19 took priority and other aspects such as peer group clinical supervision moved lower down on the priority list for managers but not for the clinical supervisors even where redeployment occurred.
With COVID all the practical side , if one of the managers is dealing with an outbreak , they won’t be attending clinical supervision , because that has to be prioritised , whereas we’ve prioritised clinical supervision (Maria) .
The valuing of peer group clinical supervision was seen as important by clinical supervisors, and they saw it as particularly needed during COVID-19 as staff were dealing with many personal and professional issues.
During the height of COVID , we had to take a bit of a break for four months as things were so demanding at work for people but then I realised that clinical supervision was needed and started back up and they all wanted to come back (Brid) .
Having peer group clinical supervision during COVID-19 supported staff and enabled the group to form supportive relationships.
COVID has impacted over the last two years in every shape and they needed the supervision and the opportunity to have a safe supportive space and it gelled the group I think as we all were there for each other (Claire) .
While COVID-19 posed many challenges it also afforded clinical supervisors and supervisees the opportunity for change and to consider alternative means of running peer group clinical supervision sessions. This change resulted in online delivery and in reflecting on both forms of delivery (face-to-face and online) clinical supervisors saw the benefit in both. Face-to-face was seen as being needed to form the group and then the group could move online once the group was established with an occasional periodic face-to-face session to maintain motivation commitment and reinforce relationships and support.
Online formats can be effective if the group is already established or the group has gone through the storming and forming phase and the ground rules have been set and trust built , then I don’t see any problem with a blended online version of clinical supervision , and I think it will be effective (Jane) .
Personal and professional development
Growth and development were evident from peer group clinical supervisors’ experiences and this growth and development occurred at a personal, professional, and patient/client level. This development also produced an awakening and valuing of one’s passion for self and their profession.
I suppose clinical supervision is about development I can see a lot of development for me and my supervisees , you know personally and professionally , it’s the support really , clinical supervision can reinvigorate it’s very exciting and a great opportunity for nursing to support each other and in care provision (Claire) .
A key to the peer group clinical supervisor’s development was the aspect of transferable skills and the confidence they gained in fulfilling their role.
All of these skills that you learn are transferable and I am a better manager because of clinical supervision (Maria) .
The confidence and skills gained translated into the clinical supervisor’s own practice as a clinical practitioner and clinical supervisor but they were also realistic in predicting the impact on others.
I have empowered my staff , I empower them to use their voice and I give my supervisees a voice and hope they take that with them (Corina) .
Fundamental to the development process was the impact on care itself and while this cannot always be measured or identified, the clinical supervisors could see that care and support of the individual practitioner (supervisee) translated into better care for the patient/client.
Care is only as good as the person delivering it and what they know , how they function and what energy and passion they have , and clinical supervision gives the person support to begin to understand their practice and how and why they do things in a certain way and when they do that they can begin to question and even change their way of doing something (Brid) .
Future opportunities
Based on the clinical supervisor’s experiences there was a clear need identified regarding valuing and embedded peer group clinical supervision within nursing/midwifery practice.
There has to be an emphasis placed on supervision it needs to be part of the fabric of a service and valued by all in that service , we should be asking why is it not available if it’s not there but there is some work first on promoting it and people knowing what it actually is and address the misconceptions (Claire) .
While such valuing and buy-in are important, it is not to say that all staff need to have peer group clinical supervision so as to allow for personal choice. In addition, to value peer group clinical supervision it needs to be evident across all staffing grades and one could question where the best starting point is.
While we should not mandate that all staff do clinical supervision it should become embedded within practice more and I suppose really to become part of our custom and practice and be across all levels of staff (Brid) .
When peer group clinical supervision is embedded within practice then it should be custom and practice, where it is included in all staff orientations and is nationally driven.
I suppose we need to be driving it forward at the coal face at induction , at orientation and any development for the future will have to be driven by the NMPDUs or nationally (Ailbhe) .
A formalised process needs to address the release of peer group clinical supervisors but also the necessity to consider the number of peer group clinical supervisors at a particular grade.
The issue is release and the timeframe as they have a group but they also have their external supervision so you have to really work out how much time you’re talking about (Maria) .
Vital within the process of peer group clinical supervision is receiving peer group clinical supervision and peer support and this needs to underpin good peer group clinical supervision practice.
Receiving peer group supervision helps me , there are times where I would doubt myself , it’s good to have the other group that I can go to and put it out there to my own group and say , look at this , this is what we did , or this is what came up and this is how (Bernie) .
For future roll out to staff nurse/midwife grade resourcing needs to be considered as peer group clinical supervisors who were managers could see the impact of having several peer group clinical supervisors in their practice area may have on care delivery.
Facilitating groups is an issue and needs to be looked at in terms of the bigger picture because while I might be able to do a second group the question is how I would be supported and released to do so (Maria) .
While there was ambiguity regarding peer group clinical supervision there was an awareness of other disciplines availing of peer group clinical supervision, raising questions about the equality of supports available for all disciplines.
I always heard other disciplines like social workers would always have been very good saying I can’t meet you I have supervision that day and I used to think my God what’s this fabulous hour that these disciplines are getting and as a nursing staff it just wasn’t there and available (Bernie) .
To address this equity issue and the aspect of low numbers of certain grades an interdisciplinary approach within nursing and midwifery could be used or a broader interdisciplinary approach across all healthcare professionals. An interdisciplinary or across-services approach was seen as potentially fruitful.
I think the value of interprofessional or interdisciplinary learning is key it addresses problem-solving from different perspectives that mix within the group is important for cross-fertilisation and embedding the learning and developing the experience for each participant within the group (Jane) .
As we move beyond COVID-19 and into the future there is a need to actively promote peer group clinical supervision and this would clarify what peer group clinical supervision actually is, its uptake and stimulate interest.
I’d say it’s like promoting vaccinations if you could do a roadshow with people , I think that would be very beneficial , and to launch it , like you have a launch an official launch behind it (Mary Rose) .
The advantages of peer group clinical supervision highlighted in this study pertain to self-enhancement (confidence, leadership, personal development, resilience), organisational and service-related aspects (positive work environment, staff retention, safety), and professional patient care (critical thinking and evaluation, patient safety, adherence to quality standards, elevated care standards). These findings align with broader literature that acknowledges various areas, including self-confidence and facilitation [ 23 ], leadership [ 24 ], personal development [ 25 ], resilience [ 26 ], positive/supportive working environment [ 27 ], staff retention [ 28 ], sense of safety [ 29 ], critical thinking and evaluation [ 30 ], patient safety [ 31 ], quality standards [ 32 ] and increased standards of care [ 33 ].
In this study, peer group clinical supervision appeared to contribute to the alleviation of stress and anxiety. Participants recognised the significance of these sessions, where they could openly discuss and reflect on professional situations both emotionally and rationally. Central to these discussions was the creation of a safe, trustworthy, and collegial environment, aligning with evidence in the literature [ 34 ]. Clinical supervision provided a platform to share resources (information, knowledge, and skills) and address issues while offering mutual support [ 35 ]. The emergence of COVID-19 has stressed the significance of peer group clinical supervision and support for the nursing/midwifery workforce [ 36 ], highlighting the need to help nurses/midwifes preserve their well-being and participate in collaborative problem-solving. COVID-19 impacted and disrupted clinical supervision frequency, duration and access [ 37 ]. What was evident during COVID-19 was the stress and need for support for staff and given the restorative or supportive functions of clinical supervision it is a mechanism of support. However, clinical supervisors need support themselves to be able to better meet the supervisee’s needs [ 38 ].
The value of peer group clinical supervision in nurturing a conducive working environment cannot be overstated, as it indorses the understanding and adherence to workplace policies by empowering supervisees to understand the importance and rationale behind these policies [ 39 ]. This becomes vital in a continuously changing healthcare landscape, where guidelines and policies may be subject to change, especially in response to situations such as COVID-19. In an era characterised by international workforce mobility and a shortage of healthcare professionals, a supportive and positive working environment through the provision of peer group clinical supervision can positively influence staff retention [ 40 ], enhance job satisfaction [ 41 ], and mitigate burnout [ 42 ]. A critical aspect of the peer group clinical supervision process concerns providing staff the opportunity to reflect, step back, problem-solve and generate solutions. This, in turn, ensures critical thinking and evaluation within clinical supervision, focusing on understanding the issues and context, and problem-solving to draw constructive lessons for the future [ 30 ]. Research has determined a link between clinical supervision and improvements in the quality and standards of care [ 31 ]. Therefore, peer group clinical supervision plays a critical role in enhancing patient safety by nurturing improved communication among staff, facilitating reflection, promoting greater self-awareness, promoting the exchange of ideas, problem-solving, and facilitating collective learning from shared experiences.
Starting a group arose as a foundational aspect emphasised in this study. The creation of the environment through establishing ground rules, building relationships, fostering trust, displaying respect, and upholding confidentiality was evident. Vital to this process is the recruitment of clinical supervisees and deciding the suitable group size, with a specific emphasis on addressing individuals’ inclination to engage, their knowledge and understanding of peer group clinical supervision, and dissipating any lack of awareness or misconceptions regarding peer group supervision. Furthermore, the educational training of peer group clinical supervisors and the support from external clinical supervisors played a vital role in the rollout and formation of peer group clinical supervision. The evidence stresses the significance of an open and safe environment, wherein supervisees feel secure and trust their supervisor. In such an environment, they can effectively reflect on practice and related issues [ 41 ]. This study emphasises that the effectiveness of peer group supervision is more influenced by the process than the content. Clinical supervisors utilised the process to structure their sessions, fostering energy and interest to support their peers and cultivate new insights. For peer group clinical supervision to be effective, regularity is essential. Meetings should be scheduled in advance, allocate protected time, and take place in a private space [ 35 ]. While it is widely acknowledged that clinical supervisors need to be experts in their professional field to be credible, this study highlights that the crucial aspects of supervision lie in the quality of the relationship with the supervisor. The clinical supervisor should be supportive, caring, open, collaborative, sensitive, flexible, helpful, non-judgmental, and focused on tacit knowledge, experiential learning, and providing real-time feedback.
Critical to the success of peer group clinical supervision is the endorsement and support from management, considering the organisational culture and attitudes towards the practice of clinical supervision as an essential factor [ 43 ]. This support and buy-in are necessary at both the management and individual levels [ 28 ]. The primary obstacles to effective supervision often revolve around a lack of time and heavy workloads [ 44 ]. Clinical supervisors frequently struggle to find time amidst busy environments, impacting the flexibility and quality of the sessions [ 45 ]. Time constraints also limit the opportunity for reflection within clinical supervision sessions, leaving supervisees feeling compelled to resolve issues on their own without adequate support [ 45 ]. Nevertheless, time-related challenges are not unexpected, prompting a crucial question about the value placed on clinical supervision and its integration into the culture and fabric of the organisation or profession to make it a customary practice. Learning from experiences like those during the COVID-19 pandemic has introduced alternative ways of working, and the use of technology (such as Zoom, Microsoft Teams, Skype) may serve as a means to address time, resource, and travel issues associated with clinical supervision.
Despite clinical supervision having a long international history, persistent misconceptions require attention. Some of these include not considering clinical supervision a priority [ 46 ], perceiving it as a luxury [ 41 ], deeming it self-indulgent [ 47 ], or viewing it as mere casual conversation during work hours [ 48 ]. A significant challenge lies in the lack of a shared understanding regarding the role and purpose of clinical supervision, with past perceptions associating it with surveillance and being monitored [ 48 ]. These negative connotations often result in a lack of engagement [ 41 ]. Without encouragement and recognition of the importance of clinical supervision from management or the organisation, it is unlikely to become embedded in the organisational culture, impeding its normalisation [ 39 ].
In this study, some peer group clinical supervisors expressed feelings of being impostors and believed they lacked the knowledge, skills, and training to effectively fulfil their roles. While a deficiency in skills and competence are possible obstacles to providing effective clinical supervision [ 49 ], the peer group clinical supervisors in this study did not report such issues. Instead, their concerns were more about questioning their ability to function in the role of a peer group clinical supervisor, especially after a brief training program. The literature acknowledges a lack of training where clinical supervisors may feel unprepared and ill-equipped for their role [ 41 ]. To address these challenges, clinical supervisors need to be well-versed in professional guidelines and ethical standards, have clear roles, and understand the scope of practice and responsibilities associated with being a clinical supervisor [ 41 ].
The support provided by external clinical supervisors and the peer group clinical supervision sessions played a pivotal role in helping peer group clinical supervisors ease into their roles, gain experiential learning, and enhance their facilitation skills within a supportive structure. Educating clinical supervisors is an investment, but it should not be a one-time occurrence. Ongoing external clinical supervision for clinical supervisors [ 50 ] and continuous professional development [ 51 ] are crucial, as they contribute to the likelihood of clinical supervisors remaining in their roles. However, it is important to interpret the results of this study with caution due to the small sample size in the survey. Generalising the study results should be approached with care, particularly as the study was limited to two regions in Ireland. However, the addition of qualitative data in this mixed-methods study may have helped offset this limitation.
This study highlights the numerous advantages of peer group clinical supervision at individual, service, organisational, and patient/client levels. Success hinges on addressing the initial lack of awareness and misconceptions about peer group clinical supervision by creating the right environment and establishing ground rules. To unlock the full potential of peer group clinical supervision, it is imperative to secure management and organisational support for staff release. More crucially, there is a need for valuing and integrating peer group clinical supervision into nursing and midwifery education and practice. Making peer group clinical supervision accessible to all grades of nurses and midwives across various healthcare services is essential, necessitating strategic planning to tackle capacity and sustainability challenges.
Data availability
Data are available from the corresponding author upon request owing to privacy or ethical restrictions.
Zelenikova R, Gurkova E, Friganovic A, Uchmanowicz I, Jarosova D, Ziakova K, Plevova I, Papastavrou E. Unfinished nursing care in four central European countries. J Nurs Manage. 2020;28(8):1888–900. https://doi.org/10.1111/jonm.12896 .
Article Google Scholar
Department of Health, Office of the Chief Nursing Officer. Position paper 1: values for nurses and midwives in Ireland. Dublin: The Stationery Office; 2016.
Google Scholar
Cummings J, Bennett V. Developing the culture of compassionate care: creating a new vision for nurses, midwives and care-givers. London: Department of Health; 2012.
Both-Nwabuwe JM, Dijkstra MT, Klink A, Beersma B. Maldistribution or scarcity of nurses: the devil is in the detail. J Nurs Manage. 2018;26(2):86–93. https://doi.org/10.1111/jonm.12531 .
Squires A, Jylha V, Jun J, Ensio A, Kinnunen J. A scoping review of nursing workforce planning and forecasting research. J Nurs Manage. 2017;25:587–96. https://doi.org/10.1111/jonm.12510 .
Sasso L, Bagnasco A, Catania G, Zanini M, Aleo G, Watson R. Push and pull factors of nurses’ intention to leave. J Nurs Manage. 2019;27:946–54. https://doi.org/10.1111/jonm.12745 .
Gea-Caballero V, Castro-Sánchez E, Díaz‐Herrera MA, Sarabia‐Cobo C, Juárez‐Vela R, Zabaleta‐Del Olmo E. Motivations, beliefs, and expectations of Spanish nurses planning migration for economic reasons: a cross‐sectional, web‐based survey. J Nurs Scholarsh. 2019;51(2):178–86. https://doi.org/10.1111/jnu.12455 .
Article PubMed Google Scholar
Cutcliffe J, Sloan G, Bashaw M. A systematic review of clinical supervision evaluation studies in nursing. Int J Ment Health Nurs. 2018;27:1344–63. https://doi.org/10.1111/inm.12443 .
Snowdon DA, Hau R, Leggat SG, Taylor NF. Does clinical supervision of health professionals improve patient safety? A systematic review and meta-analysis. Int J Qual Health C. 2016;28(4):447–55. https://doi.org/10.1093/intqhc/mzw059 .
Turner J, Hill A. Implementing clinical supervision (part 1): a review of the literature. Ment Health Nurs. 2011;31(3):8–12.
Dilworth S, Higgins I, Parker V, Kelly B, Turner J. Finding a way forward: a literature review on the current debates around clinical supervision. Contemp Nurse. 2013;45(1):22–32. https://doi.org/10.5172/conu.2013.45.1.22 .
Buss N, Gonge H. Empirical studies of clinical supervision in psychiatric nursing: a systematic literature review and methodological critique. Int J Ment Health Nurs. 2009;18(4):250–64. https://doi.org/10.1111/j.1447-0349.2009.00612.x .
Pollock A, Campbell P, Deery R, Fleming M, Rankin J, Sloan G, Cheyne H. A systematic review of evidence relating to clinical supervision for nurses, midwives and allied health professionals. J Adv Nurs. 2017;73(8):1825–37. https://doi.org/10.1111/jan.13253 .
Snowdon DA, Leggat SG, Taylor NF. Does clinical supervision of healthcare professionals improve effectiveness of care and patient experience: a systematic review. BMC Health Serv Res. 2017;17(1):1–11. https://doi.org/10.1186/s12913-017-2739-5 .
Kühne F, Maas J, Wiesenthal S, Weck F. Empirical research in clinical supervision: a systematic review and suggestions for future studies. BMC Psychol. 2019;7(1):1–11. https://doi.org/10.1186/s40359-019-0327-7 .
Snowdon DA, Sargent M, Williams CM, Maloney S, Caspers K, Taylor NF. Effective clinical supervision of allied health professionals: a mixed methods study. BMC Health Serv Res. 2020;20(1):1–11. https://doi.org/10.1186/s12913-019-4873-8 .
Borders LD. Dyadic, triadic, and group models of peer supervision/consultation: what are their components, and is there evidence of their effectiveness? Clin Psychol. 2012;16(2):59–71.
Health Service Executive. Guidance document on peer group clinical supervision. Mayo: Nursing and Midwifery Planning and Development Unit Health Service Executive West Mid West; 2023.
Sharma A, Minh Duc NT, Lam Thang L, Nam T, Ng NH, Abbas SJ, Huy KS, Marušić NT, Paul A, Kwok CL. Karamouzian, M. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med. 2021;36(10):3179–87. https://doi.org/10.1007/s11606-021-06737-1 .
Article PubMed PubMed Central Google Scholar
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;899:1245–51. https://doi.org/10.1097/ACM.0000000000000388 .
Winstanley J, White E. The MCSS-26©: revision of the Manchester Clinical Supervision Scale© using the Rasch Measurement Model. J Nurs Meas. 2011;193(2011):160–78. https://doi.org/10.1891/1061-3749.19.3.160 .
Colorafi KJ, Evans B. Qualitative descriptive methods in health science research. HERD-Health Env Res. 2016;9:16–25. https://doi.org/10.1177/1937586715614171 .
Agnew T, Vaught CC, Getz HG, Fortune J. Peer group clinical supervision program fosters confidence and professionalism. Prof Sch Couns. 2000;4(1):6–12.
Mc Carthy V, Goodwin J, Saab MM, Kilty C, Meehan E, Connaire S, O’Donovan A. Nurses and midwives’ experiences with peer-group clinical supervision intervention: a pilot study. J Nurs Manage. 2021;29:2523–33. https://doi.org/10.1111/jonm.13404 .
Rothwell C, Kehoe A, Farook SF, Illing J. Enablers and barriers to effective clinical supervision in the workplace: a rapid evidence review. BMJ Open. 2021;119:e052929. https://doi.org/10.1136/bmjopen-2021-052929 .
Francis A, Bulman C. In what ways might group clinical supervision affect the development of resilience in hospice nurses. Int J Palliat Nurs. 2019;25:387–96. https://doi.org/10.12968/ijpn.2019.25.8.387 .
Chircop Coleiro A, Creaner M, Timulak L. The good, the bad, and the less than ideal in clinical supervision: a qualitative meta-analysis of supervisee experiences. Couns Psychol Quart. 2023;36(2):189–210. https://doi.org/10.1080/09515070.2021.2023098 .
Stacey G, Cook G, Aubeeluck A, Stranks B, Long L, Krepa M, Lucre K. The implementation of resilience based clinical supervision to support transition to practice in newly qualified healthcare professionals. Nurs Educ Today. 2020;94:104564. https://doi.org/10.1016/j.nedt.2020.104564 .
Feerick A, Doyle L, Keogh B. Forensic mental health nurses’ perceptions of clinical supervision: a qualitative descriptive study. Issues Ment Health Nurs. 2021;42:682–9. https://doi.org/10.1080/01612840.2020.1843095 .
Corey G, Haynes RH, Moulton P, Muratori M. Clinical supervision in the helping professions: a practical guide. Alexandria, VA: American Counseling Association; 2021.
Sturman N, Parker M, Jorm C. Clinical supervision in general practice training: the interweaving of supervisor, trainee and patient entrustment with clinical oversight, patient safety and trainee learning. Adv Health Sci Educ. 2021;26:297–311. https://doi.org/10.1007/s10459-020-09986-7 .
Alfonsson S, Parling T, Spännargård Å, Andersson G, Lundgren T. The effects of clinical supervision on supervisees and patients in cognitive behavioral therapy: a systematic review. Cogn Behav Therapy. 2018;47(3):206–28. https://doi.org/10.1080/16506073.2017.1369559 .
Coelho M, Esteves I, Mota M, Pestana-Santos M, Santos MR, Pires R. Clinical supervision of the nurse in the community to promote quality of care provided by the caregiver: scoping review protocol. Millenium J Educ Technol Health. 2022;2:83–9. https://doi.org/10.29352/mill0218.26656 .
Toros K, Falch-Eriksen A. Structured peer group supervision: systematic case reflection for constructing new perspectives and solutions. Int Soc Work. 2022;65:1160–5. https://doi.org/10.1177/0020872820969774 .
Bifarin O, Stonehouse D. Clinical supervision: an important part of every nurse’s practice. Brit J Nurs. 2017;26(6):331–5. https://doi.org/10.12968/bjon.2017.26.6.331 .
Turner J, Simbani N, Doody O, Wagstaff C, McCarthy-Grunwald S. Clinical supervision in difficult times and at all times. Ment Health Nurs. 2022;42(1):10–3.
Martin P, Tian E, Kumar S, Lizarondo L. A rapid review of the impact of COVID-19 on clinical supervision practices of healthcare workers and students in healthcare settings. J Adv Nurs. 2022;78:3531–9. https://doi.org/10.1111/jan.15360 .
van Dam M, van Hamersvelt H, Schoonhoven L, Hoff RG, Cate OT, Marije P. Hennus. Clinical supervision under pressure: a qualitative study amongst health care professionals working on the ICU during COVID-19. Med Edu Online. 2023;28:1. https://doi.org/10.1080/10872981.2023.2231614 .
Martin P, Lizarondo L, Kumar S, Snowdon D. Impact of clinical supervision on healthcare organisational outcomes: a mixed methods systematic review. PLoS ONE. 2021;1611:e0260156. https://doi.org/10.1371/journal.pone.0260156 .
Article CAS Google Scholar
Hussein R, Salamonson Y, Hu W, Everett B. Clinical supervision and ward orientation predict new graduate nurses’ intention to work in critical care: findings from a prospective observational study. Aust Crit Care. 2019;325:397–402. https://doi.org/10.1016/j.aucc.2018.09.003 .
Love B, Sidebotham M, Fenwick J, Harvey S, Fairbrother G. Unscrambling what’s in your head: a mixed method evaluation of clinical supervision for midwives. Women Birth. 2017;30:271–81. https://doi.org/10.1016/j.wombi.2016.11.002 .
Berry S, Robertson N. Burnout within forensic psychiatric nursing: its relationship with ward environment and effective clinical supervision? J Psychiatr Ment Health Nurs. 2019;26:7–8. https://doi.org/10.1111/jpm.12538 .
Markey K, Murphy L, O’Donnell C, Turner J, Doody O. Clinical supervision: a panacea for missed care. J Nurs Manage. 2020;28:2113–7. https://doi.org/10.1111/jonm.13001 .
Brody AA, Edelman L, Siegel EO, Foster V, Bailey DE Jr., Bryant AL, Bond SM. Evaluation of a peer mentoring program for early career gerontological nursing faculty and its potential for application to other fields in nursing and health sciences. Nurs Outlook. 2016;64(4):332–8. https://doi.org/10.1016/j.outlook.2016.03.004 .
Bulman C, Forde-Johnson C, Griffiths A, Hallworth S, Kerry A, Khan S, Mills K, Sharp P. The development of peer reflective supervision amongst nurse educator colleagues: an action research project. Nurs Educ Today. 2016;45:148–55. https://doi.org/10.1016/j.nedt.2016.07.010 .
Pack M. Unsticking the stuckness’: a qualitative study of the clinical supervisory needs of early-career health social workers. Brit J Soc Work. 2015;45:1821–36. https://doi.org/10.1093/bjsw/bcu069 .
Bayliss J. Clinical supervision for palliative care. London: Quay Books; 2006.
Kenny A, Allenby A. Implementing clinical supervision for Australian rural nurses. Nurs Educ Pract. 2013;13(3):165–9. https://doi.org/10.1016/j.nepr.2012.08.009 .
MacLaren J, Stenhouse R, Ritchie D. Mental health nurses’ experiences of managing work-related emotions through supervision. J Adv Nurs. 2016;72:2423–34. https://doi.org/10.1111/jan.12995 .
Wilson HM, Davies JS, Weatherhead S. Trainee therapists’ experiences of supervision during training: a meta-synthesis. Clinl Psychol Psychother. 2016;23:340–51. https://doi.org/10.1002/cpp.1957 .
Noelker LS, Ejaz FK, Menne HL, Bagaka’s JG. Factors affecting frontline workers’ satisfaction with supervision. J Aging Health. 2009;21(1):85–101. https://doi.org/10.1177/0898264308328641 .
Download references
Acknowledgements
The research team would like to thank all participants for their collaboration, the HSE steering group members and Carmel Hoey, NMPDU Director, HSE West Mid West, Dr Patrick Glackin, NMPD Area Director, HSE West, Annette Cuddy, Director, Centre of Nurse and Midwifery Education Mayo/Roscommon; Ms Ruth Hoban, Assistant Director of Nursing and Midwifery (Prescribing), HSE West; Ms Annette Connolly, NMPD Officer, NMPDU HSE West Mid West.
The authors declare that there are no sources of funding associated with this paper.
Author information
Authors and affiliations.
Department of Nursing and Midwifery, Health Research Institute, University of Limerick, Limerick, Ireland
Owen Doody, Kathleen Markey, Claire O. Donnell & Louise Murphy
Department of Nursing and Midwifery, Sheffield Hallam University, Sheffield, UK
James Turner
You can also search for this author in PubMed Google Scholar
Contributions
OD: Conceptualization, Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Project administration, Funding acquisition. COD: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition. KM: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition. JT: Methodology, Formal analysis, Writing - Original Draft, Writing - Review & Editing. LM: Methodology, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing, Funding acquisition.
Corresponding author
Correspondence to Owen Doody .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by two health service institutional review boards University Hospital Limerick (Ref: 091/19) and Galway University Hospitals (Ref: C.A. 2199). The study was conducted in accordance with the principles of the Declaration of Helsinki and all study details were fully disclosed to participants, who were assured of the voluntary nature of participation and withdrawal. The study questionnaires were coded, and identities were not disclosed to guarantee participants’ anonymity and all participants provided written informed consent before interviews.
Consent for publication
No identifying images or other personal or clinical details of participants are presented in this paper that would compromise anonymity and all participants were aware and informed through the Participant Information Leaflet that the data collected may be reported through article and/or conference publications and this was reiterated during the qualitative data collection stage.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Doody, O., Markey, K., Turner, J. et al. Clinical supervisor’s experiences of peer group clinical supervision during COVID-19: a mixed methods study. BMC Nurs 23 , 612 (2024). https://doi.org/10.1186/s12912-024-02283-3
Download citation
Received : 04 January 2024
Accepted : 22 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12912-024-02283-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical supervision
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 02 September 2024
Implementation of health-promoting retail initiatives in the Healthier Choices in Supermarkets Study—qualitative perspectives from a feasibility study
- Katrine Sidenius Duus ORCID: orcid.org/0000-0002-1630-3132 1 ,
- Tine Tjørnhøj-Thomsen ORCID: orcid.org/0000-0003-3621-6682 1 &
- Rikke Fredenslund Krølner ORCID: orcid.org/0000-0002-4928-4310 1
BMC Medicine volume 22 , Article number: 349 ( 2024 ) Cite this article
Metrics details
Improving food environments like supermarkets has the potential to affect customers’ health positively. Scholars suggest researchers and retailers collaborate closely on implementing and testing such health-promoting interventions, but knowledge of the implementation of such interventions is limited. We explore the implementation of four health-promoting food retail initiatives selected and developed by a partnership between a research institution, a large retail group, and a non-governmental organisation.
The four initiatives included downsizing of bags for pick’n’ mix sweets and soda bottles at the check-out registers, shelf tags promoting healthier breakfast cereal options, and replacing a complimentary bun with a banana offered to children. The initiatives were implemented for 6 weeks (or longer if the store manager allowed it) in one store in Copenhagen, Denmark. Data were collected through observations, informal interviews with customers, and semi-structured interviews with retailers. We conducted a thematic analysis of transcripts and field notes inspired by process evaluation concepts and included quantitative summaries of selected data.
Two out of four initiatives were not implemented as intended. The implementation was delayed due to delivery issues, which also resulted in soda bottles not being downsized as intended. The maintenance of the shelf tags decreased over time. Retailers expressed different levels of acceptability towards the initiatives, with a preference for the complimentary banana for children. This was also the only initiative noticed by customers with both positive and negative responses. Barriers and facilitators of implementation fell into three themes: Health is not the number one priority, general capacity of retailers, and influence of customers and other stakeholders on store operation.
Conclusions
The retailers’ interests, priorities, and general capacity influenced the initiative implementation. Retailers’ acceptability of the initiatives was mixed despite their involvement in the pre-intervention phase. Our study also suggests that customer responses towards health-promoting initiatives, as well as cooperation with suppliers and manufacturers in the development phase, may be determining to successful implementation. Future studies should explore strategies to facilitate implementation, which can be applied prior to and during the intervention.
Peer Review reports
What we eat affects our health and well-being [ 1 ]. Diet is associated with obesity, cancers [ 2 ], and mental well-being [ 3 ], and a healthy diet has been associated with lower all-cause mortality [ 4 ]. One important factor in improving diet is to create a food environment that supports a healthy diet [ 5 , 6 ]. In modern societies, such as Denmark, supermarkets are the main source of food [ 7 ]. Supermarkets therefore hold a significant influence on what food we buy and potentially also eat [ 7 , 8 , 9 ]. Studies report associations between the concentration of supermarkets and overweight and obesity in the neighbourhood [ 10 ] and between the healthfulness of supermarkets and people’s diets [ 11 , 12 ]. Moreover, unhealthy food and beverage products are promoted more often than healthy products and beverages in, for example, supermarkets [ 9 , 13 , 14 ]. This indicates a need to explore how and if it is possible to implement health promotion initiatives in supermarkets and whether customers respond to such initiatives as intended.
Studies show that health-promoting interventions in supermarkets can affect customers to purchase more healthy products [ 7 , 9 , 15 , 16 , 17 ]. Reviews and a meta-analysis have concluded that the most effective initiative in supermarket settings is price changes—the evidence points to the positive effects of reduced prices to increase the purchase of healthier products, especially fruit and vegetables [ 7 , 17 ]. Even though price reductions seem to be effective, they seem more challenging to implement due to retailers’ drive for profit and low preference for financing such price cuts [ 7 , 18 ]. There is some evidence that nudges in terms of product information and positioning, as well as altering the number of available products, can impact what products are being purchased [ 15 , 16 ]. However, the quality of this evidence is low. Overall, most of the studies that have explored the effect of interventions in supermarkets have been conducted in the USA and other high-income countries [ 15 , 16 ], in controlled settings, or applied a weak study design, such as non-randomised studies [ 16 , 17 ]. To our knowledge, only a few studies have been conducted in Denmark [ 19 , 20 , 21 , 22 , 23 , 24 , 25 ]. These studies represent different designs and types of interventions: reformulation of private-label products to reduce calorie content [ 24 ], informational claims to promote low-salt foods [ 23 ], nudges via signs to promote sales of fruit and vegetables [ 22 ], positioning (shelf-space management) of dairy products [ 20 ], replacement of sugar confectionery with fruit and healthy snacks at the checkout [ 19 ], discount on fruit and vegetables combined with space management [ 25 ] and structural changes in supermarkets and education of supermarket employees as part of a multicomponent intervention [ 21 ] (the three latter studies are reporting from the same project). All but one study [ 23 ] found an effect of the applied intervention strategies, although mostly small or modest. This calls for more studies in real-life settings and investigations of why some interventions have the desired effect while others do not. Lack of effect may be explained by 1) customers not noticing or finding the initiatives relevant [ 19 , 23 ], 2) customers buying other products instead of or additionally to promoted intervention products [ 20 , 24 ], 3) the shelf organising effect [ 20 ], or 4) theory fail in regards to customer behaviour [ 22 ].
Several studies have explored facilitators and barriers to the implementation of health-promoting interventions in supermarkets. Reviews show that implementation is supported if the retailer is receptive to innovation, feels responsible for community health, and receives financial support or subsidies [ 26 ]. Furthermore, implementation is supported if the intervention provides the retailers with knowledge of health promotion and business skills [ 26 , 27 ]. Other facilitators include compatibility with context and customers’ needs, positive customer responses to the initiative, the prospect of improved public image, establishment of partnerships, low retailer effort requirements, and increased profit or sales [ 26 , 27 ]. Health-promoting interventions in supermarkets are hindered by high customer demand for unhealthy products and lower demand for healthy products, constraints of store infrastructure, challenges in product supply, high staff turnover, and lack of time [ 26 , 27 ]. Other barriers are doubt regarding changing customers’ behaviour, poor communication between collaborators [ 26 ], high running costs, and risk of spoilage [ 26 , 27 ].
Middle et al. [ 26 ] conclude that the underlying mechanism of barriers and facilitators of implementation is the (mis)alignment of retailers’ and intervention researchers’ interests. The authors, therefore, suggest a close collaboration between intervention researchers and retailers to work towards an alignment of interests and resolving or avoiding misalignment, which is supported by Gupta et al. [ 27 ]. However, knowledge of how such collaborative efforts affect the implementation of healthy food retail interventions is warranted.
The aim of this study is to explore the implementation, acceptability, and feasibility of four different health-promoting food retail initiatives to increase customers’ purchase of healthy food and beverages, which were selected and developed together with food retailers: 1) Promotion of healthier breakfast cereals and products using shelf tags, 2) downsizing of sodas sold at the checkout desks, 3) downsizing of bags for the pick’n’ mix sweets, 4) replacement of a complimentary bun for children with a banana. The study has three research objectives:
To document the implementation and sustainment of the initiatives over time
To explore the retailers’ and customers’ responses to and acceptability of the initiatives
To investigate barriers and facilitators of implementation and sustainment of the initiatives.
Setting and the initiatives
This study was conducted in Denmark during 2020 and 2021, 2 years that involved two major societal events, first the coronavirus disease pandemic and later the start of the Russia-Ukraine war. Both events heavily influenced the circumstances of everyday life including opportunities for conducting research and running businesses. The specific influences on this study will be unfolded later in the findings and discussion sections.
In this study, we collaborated with the retailer Salling Group, which holds 34.2% of the market share of grocery retailers in Denmark [ 28 ]. Salling Group is owned by the Salling Foundations and has no shareholders—all profits go to reinvestment in the business and donations to sports (amateur and professional), charity, education, and research. Salling Group owns three national supermarket chains: føtex, Netto and Bilka, alongside other businesses. For the feasibility test, we collaborated with føtex, which owns over 100 stores all over Denmark, including 23 stores called føtex food. føtex (except føtex food) offers both groceries and many different non-food products (e.g. textiles, cosmetics, toys, electronics, and home accessories).
The initiatives were selected and developed by a partnership, including a group of researchers at the National Institute of Public Health, University of Southern Denmark, consultants from the Danish Cancer Society, and employees at the Corporate Social Responsibility (CSR) department in Salling Group, the marketing department at føtex, and two store managers (hereafter referred collectively to as ‘the retailers’) over approximately 2 years. The process involved in-person meetings, desk research (the use of existing material [ 29 ]), visits to the test store, and a prototype test of three suggested initiatives. The researchers initiated the collaboration and were responsible for designing the research study and data collection and analyses. The retailers hosted the site of the feasibility test, contributed to the selection and development of initiatives and co-managed the practical part of the study. The Danish Cancer Society was recruited by the research project to develop the initiatives. A detailed description of the collaboration and development process is reported elsewhere (Duus et al. unpublished ).
The feasibility test ended up including four initiatives: 1) Promotion of healthier breakfast cereals and products using shelf tags, 2) downsizing of soda sold at the checkout desks, 3) downsizing of bags for the pick’n’ mix sweets, 4) replacement of a complimentary bun for children with a banana (suggested by the retailers). The initiatives were based on a compromise between the willingness of the retailers and the interest and ideas of the remaining partners rather than on what the literature suggests are the most effective strategies (Duus et al. unpublished ). Detailed descriptions of the initiatives and the rationale behind them are found in Table 1 .
The prototype test showed that 1) It was important to have a sign informing the customers about the initiative that offered a free banana to children instead of the usual free bun to create a better understanding of the changed offer; 2) Promotional shelf tags needed weekly maintenance as some would fall off; 3) It was difficult to sustain an initiative promoting ready-to-serve salads and ready-to-cook vegetables next to different fresh meats, as it met resistance among the staff due to being an additional task and led to more product waste (Customers did not expect to find these products next to the meat and therefore might not notice them). The learnings from the prototype test led to modifications of the implementation plan and the discard of the latter initiative. The prototype test also made us aware of how quickly the selection of food offered and the layout of the store changed over time, which the researcher, therefore, paid extra attention to during subsequent data collection. Moreover, the researcher made sure to update the list of products that should have a shelf tag a few weeks before the implementation to include new products offered.
The føtex marketing department developed a script to inform the staff at the test store about the feasibility test, explaining and showing each initiative and the aim of the study overall. This was sent to the store manager after being reviewed by the researchers. The store manager was responsible for informing all relevant staff about the implementation and maintenance of the initiatives. The føtex marketing department also made sure to inform the relevant suppliers. Employees at the test store and brand staff from a brewery (who stock the coolers at the check-out desks) implemented the initiatives in the store. The research group did not correct or maintain the initiatives in the store after they were launched; however, the researchers monitored it and reported back to the retailers, either at meetings or by email.
Overall study design
The four initiatives were implemented in the test store for 6 weeks (or longer if the store manager allowed it) starting in September 2021. A føtex store in central Copenhagen (the capital city of Denmark) was chosen as the test store. This decision was made for pragmatic reasons, as the research institute is based in Copenhagen, and based on Salling Group’s decision as it offered their new store layout, which all stores were in the process of being converted to (it was the same store as where the prototype test was conducted).
We designed a qualitative study involving participant observations and interviews to evaluate the feasibility of the initiatives. The methods were designed to explore the partnership and collaboration (the aim of another publication [Duus et al. Unpublished ]), as well as the implementation of the initiatives [ 30 ]. In the design of this study, we were inspired by McGill et al.'s (2020) two-phase framework of qualitative process evaluation from a complex systems perspective. This framework suggests an evaluation that looks at changes over time, starting with phase 1, the static system description and hypothesis generation about how the system might change when the intervention is introduced, followed by phase 2, an adaptive evaluation approach to the system undergoing change which follows emerging findings [ 31 ].
Data collection
In-store observations.
During October and November 2020, we mapped the store layout and customer flow in the test store as part of the static system description. Over 3 weeks, three research assistants performed 12 participant observations of 1005 min in total. The observations followed an observation guide which covered 1) the physical setting (e.g. the layout, placement of products, signs, and pictures); 2) the people (e.g. who are the customers? Are people shopping alone or together with others? How do they move around the store? What are the staff doing?) and 3) short interviews with customers (if possible) about their shopping at the particular store, and their thoughts about the layout of the store. The research teams’ access to the store was approved by the store manager, and research assistants wore a key chain with a sign showing their name and affiliation during the observations. During this data collection period, it was made mandatory to use face masks in supermarkets due to the coronavirus disease pandemic. As the implementation was delayed to approximately 1 year after this static description was completed, one participant observation in the test store was performed at the end of August 2021, just before initiative implementation, to document any major changes in the store layout and selection. Key lessons from these observations about the test supermarket and customers’ behaviour in the store included knowledge on 1) the route around the store, 2) the different times spent at the store, 3) interactions with objects (e.g. products and phones), 4) interactions with children, 5) behaviour of the staff, and 6) sensory impression (Additional file 1). These lessons informed our following data generation and assisted in contextualising our analysis.
The first author monitored the implementation process through participant observations of status meetings ( n = 2) and correspondence via email and phone with the store manager and the contact person at føtex. In-store participant observations were conducted during and after the feasibility test period, September 2021–May 2022 ( n = 25 ~ 1795 min in total; see Additional file 2). These observations focused on documenting the presence of the initiatives as well as customers’ and staff’s responses to the initiatives. Access to the store was once again approved by the store manager, and the researcher wore a key chain. During the participant observations in-store, we conducted informal interviews with customers (see Additional file 2 for examples of questions), which lasted a maximum of 5 min each. The first author would approach people and ask if they were interested in answering a brief question. She introduced herself by her first name, where she worked and explained she was doing a research project about shopping patterns. The participant observations were documented by taking notes and photos. Handwritten notes were digitalised and written down at the first chance after leaving the store.
Qualitative interviews
Between November 2021 and February 2023, the first author conducted four semi-structured interviews with retailers ( n = 3) who had been involved in the study (Table 2 ) to explore their views on the initiatives and the implementation process. Interview guides were used in all interviews alongside different prompts (e.g. timelines and documents). Interview guides were tailored to each participant’s specific role and involvement in the development and implementation of the initiatives. Besides questions related to the initiatives and the implementation effort, the guides included questions about the informants’ background and motivation for the project (personally and professionally), their view on their role and scope for action (individually and organisationally) and their perception of the collaboration with the other organisations. After the participants’ consent was given verbally right before the interview, the interviews were recorded and later transcribed verbatim.
To explore the level of implementation (research objective I), all field notes and photos taken during and after the feasibility test were reviewed to assess whether the initiatives were present and to what degree (e.g. x out of x possible tags).
To explore the perception of the initiatives among employees and customers (research objective II) and identify barriers and facilitators for implementing the initiatives (research objective III), we followed a thematic analysis inspired by Braun and Clarke [ 32 ]. Firstly, field notes and interview transcripts were read thoroughly and openly coded, by writing keywords in the margin of the material, with a focus on the two research objectives. After initial coding, the codes were summarised into broader themes, by writing them into a document with short descriptions and revised according to data excerpts and the full empirical material. The themes drew on the process evaluation concepts: acceptability, responsiveness [ 30 ], motivation, general capacity to implement [ 33 ] and commercial viability [ 34 ]. Lastly, the themes were named, and the final analysis was written up.
We have structured the presentation of study findings as follows: Firstly, we present the implementation of the initiatives overall. Secondly, we present the implementation of each initiative, customers’ responses to them, and the retailers’ perspectives. Lastly, we present the overall facilitators and barriers to the implementation of the initiatives.
Implementation of the initiatives
The implementation of the initiatives was challenged. Firstly, we found that not all the preparations for the implementation were finished in time for the scheduled day. On the scheduled day, the retailer decided to push back the implementation by 1 week. The main reasons were that there had been some misunderstandings around the ordering of the smaller sodas. It was informed that the smaller soda would be a 330 ml can instead of the 375 ml bottle at the price of DKK 10.00 (~ 1.3 euros). The 500 ml bottle usually sold at the coolers cost DKK 16.00 (~ 2.2 euros). The Danish Cancer Society and the research group had two concerns about this: 1) the use of a can instead of a bottle would make the interpretation of the results very difficult, as the bottle and the can have two different functions to the customer—with the can, the product would be consumed all at once, whereas the bottle with the screw lid could be saved for later after it had been open; 2) the price was too low—the price per litre would be lower on the smaller sodas than it had been on those replaced. No changes were made despite these concerns.
Secondly, just days before the implementation, the retailers informed the other partners that they would stick with cans for the test of smaller-sized sodas and that they would now be 250 ml. They acknowledged that both the size and the packing were not optimal but that the optimal 375 ml in a bottle was just not possible. Additionally, they informed the researchers that they could no longer find the new bags produced for the pick’n’mix sweet display.
These challenges led to a delay of the implementation of the initiatives by 1 week, but also a staggered implementation, where the initiatives were implemented when ready (the soda initiative 2 weeks later and the bags for pick’n’ mix sweets 8 weeks later). The retailers agreed to push back the end day correspondingly, upholding the 6 weeks of implementation. Table 3 shows an overview of the implementation of the four initiatives according to the day and week of the feasibility test period.
Smaller product sizes of sodas at the checkout desk
As seen from Table 3 , we did observe the implementation of a smaller product size of the targeted sodas in all coolers, besides the one at the bakery, in the week leading up to the agreed date. We hereafter observed a full implementation of 250 ml cans during the first 2 weeks of implementation. During the third week and the beginning of the fourth week, we observed a mix of 250 and 330 ml cans or only 330 ml cans. The store manager explained that this was probably due to non-delivering from the supplier. At the end of the fourth week and for the last 2 weeks, we observed a full implementation of 250 ml cans. As the targeted size of the initiative was a 375 ml bottle, the initiative was not implemented as intended. After the 6-week feasibility test period, we observed that the smaller 250 ml cans were available in all coolers for at least eight more weeks. As expected, the presentation of the coolers fluctuated over the period. On days of stocking (Monday, Wednesday, and Friday), the coolers would look neat and full, while they would appear more empty or messy on other days.
Customer responsiveness
We observed very few customers who bought any products from the coolers, and we did not get to talk to any customers about the initiative. However, the observations in the store showed no distinct change in customers’ behaviour around the coolers nor expressions of discontent or excitement with the initiative. In an interview with the store manager, he explained that he believed customers had not noticed the change.
Retailer perspectives
The store manager was positive about the initiative, but from his perspective, the decision to implement it should be made at the procurement level and by the suppliers. However, he did have an opinion on how to implement it. The price needed to be fair according to the product it replaced. Moreover, he drew attention to the fact that it was the supplier’s personnel who stocked the products rather than his own. The store manager was, therefore, not surprised that the employees at the store had little to say about the initiative. føtex’s representative (B) was also positive about the initiative and expressed in the interview that the chain would be willing to implement it—if they found it to be the ‘right thing’ to do. However, the representative also emphasised the importance of agreeing with the suppliers, which is a time-consuming process and ‘not done in just six months’.
Shelf tags for breakfast cereal products
From the first day of the implementation, some tags were missing, and one tag was consistently misplaced (Table 3 ). During the first 3 weeks, 10% ( n = 3) of the tags were missing. This portion progressively increased to 23% until the end of the fifth week. In the sixth week, the portion decreased at first to 16% but decreased again and ended at 26%. In the weeks after the implementation period, the tags stayed present but slowly came off. Approximately 6 months later, three (10%) of the tags were still present. We observed throughout the feasibility test that the presentation of the area varied, which is to be expected in a busy supermarket. At times, the area looked messy; boxes would block access to some products, products would be sold out, some would change packaging, and new products would be introduced to the selection.
When we asked customers about the tags, we learned that they had been unaware of them and that some believed that it was not something they would use—some did not know the meaning of the labels on the tags, while others did not find the labels relevant for them.
[The tags] don’t matter. My wife is pretty health conscious, so we don’t use those, let alone know with such a thing as breakfast cereal. (Male customer)
From our observations of the behaviour of the customers in the breakfast products and cereals department, we find two interesting groups: Those who shop alone and those who shop together with others (primarily children). These groups seem to practice different behaviours.
Among those who do their grocery shopping by themselves, we find two subgroups: 1) those who have planned or know exactly what they want to buy, and 2) those who decide at the store. For the first sub-group, we observed that some showed this by practising a behaviour where they would walk quickly and purposefully towards the shelves and quickly pick up a product. Others would look determined to find a specific product, as the fieldnote excerpt illustrates:
A woman stands looking at the muesli. She first grabs an orange bag on the bottom shelf, then a more yellow one next door and puts the first one back on the shelf. She inspects the bag she took. She starts to look around the shelves more and reaches for a bag that has a pinker look on the top shelf. She puts it back and reaches into the space next to it, where there are a few bags at the very back, but she has difficulty reaching them. A man comes by, notices the woman, and offers to help her. The woman indicates a yes, and the man reaches up and grabs a bag ‘that's the one!’ says the woman as the man hands her the bag.
Another example was a man who kept looking back and forth between some muesli and granola products and his phone before he eventually chose a product. It is unknown whether the man was looking at a specific note, a text request from his family, or a picture on his phone, yet what was on his phone seemed to determine the product he bought. Overall, this group seemed very unlikely to be influenced by the tags, as they had made their choice already before they entered the store.
For the second sub-group, those who seemed to make their decision in the store, we observed that some would just stop and glance at the products without choosing one before moving on with their shopping. Others would look more randomly at the selection than those described above, walk back and forth in the aisle, compare different products and read the info on the back of the products.
For those who shopped together with others (most often children), we observed that when adults shopped with children, the choices of the child and the choices of the adult often conflicted. In one example of a child and a woman who looked at breakfast cereal products, the child was initially allowed to pick a product and asked for different chocolate variants, which all featured cartoon figures; however, the woman rejected all of the child’s choices. In the interaction, the child was met with demands from the woman regarding the attributes of the products: they could not contain chocolate or sugar. In the end, it was the woman who chose a product based on her experience of the child’s preferences and her criteria. In similar situations, we did observe an attempt at compromising between the adult’s and the child’s criteria, which was explained by this woman:
I ask them [woman and boy aged about 10] what they look for when choosing breakfast cereals. The woman looks at the boy and says, ‘Well, what are we looking for?’. The boy does not answer but looks at her and me and smiles. The woman herself replies, ‘Something we can agree on. Something he likes but is not too unhealthy, either’. I ask her what she considers unhealthy. She waffles for a bit and then replies, ‘Yes, but he wants that Lions cereal, for example, and I don’t want him to have that. So something that’s not de facto sweets’. She takes the box of granola that they have chosen [Paulún's blueberry/lemon granola] out of the basket, looks at it and says, ‘So we chose this one. There's probably also a lot of fructose and caramelised stuff in it, but yeah.’
This illustrates the high impact children had on the choices of breakfast products, but also how the parents tried to control and negotiate the final choice.
Retailer perspective
The store manager had little faith in the effectiveness of the shelf tags:
The thing about tagging cereals, I don't think that makes the slightest difference. The reason why I’m sceptical in that regard is that it’s a mixture of what I do on a daily basis. It’s especially the behavioural patterns of our customers, but also how I act as a customer myself to a degree. I don't think shelf tags with the whole grain label or anything like that; in my experience it hasn’t changed things much. (Store manager)
His view on the effect of the initiative was in line with our observations of the customers in the store. Furthermore, the store manager explained that it was difficult to maintain the initiative, as it was not part of the employees’ daily routine. This was also the argument of why the tags lingered after the test period—it was just not part of the usual protocol either to hang them up or take them down. This perspective was shared by the føtex representative (B), who also highlighted the cost of this maintenance.
Contrary to the store managers’ sceptics, the føtex representative (B) was more positive about the initiative:
I think it’s a good initiative. We work a lot with tags and labels in general. [...] I think making it transparent to the consumer is really interesting because there’s nothing wrong with buying a box of Nesquick cereal every once in a while. At least we should not claim it’s the wrong thing to do. But you just have to be clear about what you’re buying, and I think those labels help with that. (føtex representative (B))
She explained that the initiative was highly compatible with their usual strategies. However, she also explained in the interview that a barrier to using shelf tags to promote the buying of certain products was that the chain was trying to reduce the printed material they used in their stores as part of their CSR strategy and to reduce costs.
Replacement of the complimentary bun for children with a banana
The complimentary banana was fully implemented in the feasibility test period except for 1 day of observation, where the signs were not visible (Table 3 ). The initiative also remained available and present by the sign for at least 10 weeks after the implementation period. Furthermore, the store manager informed the researcher that they would continue to provide bananas for customers requesting this as an act of customer service. From the observations, we do find that the presentation of the initiative changed throughout the period. At first, the bananas were placed in a cardboard box on the display counter, which was later replaced with a nicer-looking basket. The number of bananas and their colour also fluctuated during the different days, which would be expected due to the delivery of the bananas and how often they are restocked. However, compared to the buns, we never observed that the bananas were not available, making it a reliable offer no matter the time of the day.
We observed two ways (1 and 2) that the complimentary offer for children was brought up: 1) A customer would ask for the ‘bun for children’, or 2) the staff would offer the complimentary banana to buying customers. In the first way 1), we saw two responses from the staff (a and b) and the customers (i and ii): (a) The customer would be offered the bun with no mention of the banana, or (b) the staff would inform the customer that they no longer offered buns but that they offered a banana instead. The customers had two primary responses to this message: (i) The customer rejected the offer and decided to buy a bun or another item instead. The child was often included in this decision. (ii) The customer accepted the offer and received the banana. In some cases, the child did not accept the offer and the customer compensated for this response by buying a bun or another product for the child. In the second way 2), in which the staff offered the banana spontaneously, the customers almost always reacted positively and accepted the offer.
The following excerpt illustrates why some customers rejected the offer:
A woman with a child of about 1-year-old in a stroller walks up to the bakery and asks for a children's bun. The child has already noticed the buns from the moment they arrive and sits, pointing at the buns through the glass window and babbling. The shop assistant says that there are no children's buns but bananas and points to the sign. The woman replies, ‘I’d like to buy a bun, then’. The assistant takes the bun and enters it into the till, while the woman says, ‘Bananas are so messy’. The assistant smiles and says, ‘Well yeah, I'll pass that on’. The woman replies, ‘It's just that the banana is rather a bother, and the assistant replies, ‘But I think we’ll be offering [the buns] again eventually’.
Thus, adults rejected the offer because eating a banana was a messier process than eating a bun. During meetings and interviews, the retailer also highlighted this as the main reason for rejections of the offer, especially among those with younger children. Another reason for rejection was that the parents did not appreciate the offer nor perceived a need to offer their children a banana instead of a bun.
This initiative was the most successful and interesting one in the eyes of the store manager.
I’d like to highlight the banana for kids, which is clearly the initiative I found most customers were pleased with. (Store manager)
Many customers responded positively to the new offer, which was emphasised as a marker of success. It was also the reason why the initiative continued after the 6-week period, and the store manager explained that they would continue to give bananas to those who asked for them.
The following excerpt illustrates what the bun meant to føtex and the chain’s relationship with its customers.
The children's bun has been around for donkey’s years, and it’s become ingrained in parents and kids alike that you can get them in føtex. So, we’re quite interested in learning how many people would actually, if presented with the alternative, choose something else, like, for example, the banana. I’m quite surprised by that – we can't track it, unfortunately – but off the top of my head, up to 40 to 50 percent actually choose the banana. I find that very interesting. (føtex representative (B))
Thus, it came as a surprise that the initiative was so well received. However, despite the positive experiences with the initiative, the retailers also commented on the cost. They highlighted that the banana was more expensive than the bun, and if it should be an option offered in all stores, then it would have to be prioritised at the executive level as an additional expenditure. In this case, the banana would only be an alternative to the bun and not a replacement. This was rationalised by the retailers’ attitude of not making choices on behalf of the customers.
Smaller bags for pick’n’ mix sweets
This initiative was not implemented until 8 weeks after the initial implementation date. It was fully implemented for five out of the six weeks; during the third week, we observed that the old, larger bags had been hung in front of the new smaller bags. At 2 weeks and four and a half months after the feasibility test, the smaller bags could still be found behind the larger bags—however, it is unlikely that these would have been used, as the obvious choice would have been the bag at the very front. As described for the other areas, this also fluctuated in its presentation and stocking.
We did not get any direct reactions from customers on the smaller bag. However, our observations showed that different strategies were used to decide the amount of candy among customers who bought pick’n’mix sweets. Some showed signs of visually assessing the amount of sweets in the bag, which were the customers we would expect to influence. We often observed this strategy among adults with children, where it was the adult who would visually assess the amount and communicate to the child when they had picked enough.
Those with very young children would walk alongside the child and select the sweets for them, and some adults would encourage the choice of the child by pointing out different variants and commenting on the appearance of the sweets.
Other strategies were to mix according to a pre-defined number of pieces or volume:
A boy of about 10 and a girl of about 8 come over and mix sweets. They repeatedly weigh the bag while doing so. A woman comes over, and the girl says, ‘Hello mummy!’ The woman says, ‘Don’t forget to weigh it’. She then grabs a bag herself and begins to mix sweets. The boy asks the girl, ‘Did you weigh it?’. The girl walks over to the scales and says, ‘I think I’ve got enough’. However, she does not close the bag, and she begins to walk around somewhat restlessly, then says, ‘I don’t know what to pick. I’m still [a few] grammes short’.
An interesting aspect of the situation above is that the girl expressed that she was satisfied with what she had chosen, but she felt that she had to meet the prespecified weight and, therefore, tried to find more sweets to put in her bag. Such strategies undermine the mechanism which the initiative was trying to influence.
Overall, the retailers were positive about this initiative. The føtex representative (B) highlighted that this initiative was interesting as it was a stealth initiative, compared to the initiatives with the sodas, and would change the behaviour of the customers without them noticing. In her opinion, this was not a problem, as people paid per gram.
The store manager had a clear demand for the implementation; it should be easy for both the staff and customers to use. This perspective was backed up by a føtex representative (B) who said:
If there’s something that doesn’t work for us, it’s... if it doesn’t work for our customers, that’s what we need to solve first. (føtex representative (B))
This shows how one success criterion of the retailers is customer satisfaction, which we elaborate on later (See: Influence of customers and other stakeholders on store operation).
The initiative was very delayed, and one reason was that it was challenging to create a new bag that would work in the store. This resulted in the order of many different bags in large quantities due to the agreements with the suppliers, which had been very costly for the retailer.
The føtex representative (B) also reflected on what the potential evidence of an effect would mean to the retailer:
Then we’ll have to wait and see if people buy fewer sweets. And of course, this is something that we must take into account because it’s no secret that part of being a responsible business is to make a profit. And if we sell fewer sweets, then we make less money. (føtex representative (B))
This shows how health and financial profit were seen as opposites and how the success of the initiative would not necessarily lead to it being viewed favourably, as it would negatively affect their profit. Any implementation in the chain would, therefore, have to be a strategic decision.
Facilitators and barriers
In the sections above, we have focused on the four specific initiatives. In the following, we will present analytical findings that go across the initiatives and elucidate what facilitated and hampered the implementation of the initiatives overall. We have organised our findings under three headings: Health is not the number one priority; General capacity of the retailer; and Influence of customers and other stakeholders on store operation.
Health is not the number one priority
In this section, we present the retailers’ motivation for and interest in engaging in the project and working with health and health promotion and what drives and/or curbs this motivation. In our understanding of motivation, we draw on Scaccia et al. [ 33 ] and view motivation as incentives and disincentives that contribute to the desirability of using an initiative focusing on health.
We find that the retailers expressed motivation for working with health and health promotion, which at first seemed to be based on interest. The retailer representatives explained how they personally were interested in health and wanted to learn more, but also that the organisation had an interest in health, especially among children and young people, and wanted to contribute to health-preventing activities, for example, by financially supporting local sports clubs. According to one retailer representative, this was because physical activity and healthy eating promote happier customers, as well as happy employees. The argument points to retailers’ focus on customer satisfaction (see: Influence of customers and other stakeholders on store operation). The focus on the customers relates to another factor of motivation: Working with health was also seen as a relative advantage in that customers increasingly demand healthier products and alternatives. Lastly, we found that the motivation for working with health was a feeling of obligation due to the view of having a social responsibility:
I would say, in purely business and commercial terms, we are, indeed, a commercial business that was created to make money. There’s no ignoring that (laughs). So, of course, this is our main KPI [key performance indicator]. But that being said, we also agree that we have a social responsibility because we are as big as we are. We make a lot of foodstuffs available to the Danes, as do many of our colleagues in our industry, so there is no doubt that we have a role to play in terms of what we make available. (føtex representative (A))
According to the excerpt, this obligation was rooted in the size of the organisation and, thereby, the major influence on people’s selection of food products. However, the excerpt also highlighted that health was not their first priority, which was profit. This point has been repeatedly mentioned among retailers, which reinforces its validity; they were a business and had to gain profit to keep running their operation, which presented limits for what could be implemented. The store manager even expressed how he perceived the running of a supermarket and promotion of public health as incompatible goals and something he had never seen an example of in a real-life supermarket.
However, from the interviews with the retailers and our fieldwork, it seemed that this was not completely black and white, as the retailers were willing to give up their profit in some cases. An example is the hiding of tobacco products in all Salling Groups’ supermarket chains, which they voluntarily implemented in 2018, which led to a significant decrease in profit from tobacco products.
After all, the Salling Group pioneered this with tobacco products. I'm proud of that, but I also think it’s the right thing to do. My personal opinion is that it was the absolutely correct move they chose to make, by making it harder to market a product that is obviously bad for my health. We’re not there with pick‘n’mix sweets just yet, in that we would claim they’re bad for your health, but the mindset in terms of; that is, upholding the mindset when it comes to cigarettes is something that we, as an industry, can easily support in close cooperation with, among others, yourselves [researchers] and the industry. (Store manager)
Risk seemed to be the driver. If the retailer was convinced that the risk was real or big enough, then they were willing to give up some of their profits because it was the ‘right thing to do’, and they would have the courage and power to do so. It was mentioned by all three informants that they did not believe in bans, limitations or hiding of products, as this interfered with the customer’s freedom of choice. This viewpoint was a barrier to the implementation of all initiatives that used strategies that would minimise or reduce the availability of a product. Yet, as with the tobacco products, we found other examples where this restriction of choice was justified by the retailer. One example was that the føtex chain only sold organic bananas. From a sign in the store, this was because:
‘we want to avoid the spray agent chlorpyrifos. Among other things, it is suspected of harming the development of children and foetuses. We can’t live with that suspicion and therefore you can only buy organic bananas in the future’
As with the cigarettes, the argument here was the health risks. In the interview with the store manager about restricting choices, animal welfare and political reasons (e.g. Russia’s warfare against Ukraine) were mentioned as other arguments for doing so.
So, despite an immediate motivation for working with health, the retailer also expressed how other interests and priorities may hinder and set aside the work with health.
General capacity of the retailer
This section presents our findings relating to the general capacity of the retailer in the form of resources, organisational size, and culture. General capacity is understood as the readiness or ability to implement any new initiative [ 33 ].
Through the interviews with the føtex representative (B) and working together with the retailer during the project, we have found that the retailer seemed to be used to and willing to implement new initiatives. In this current study, they accounted for all expenses related to the development of materials for the test and were also willing to risk some of their profit for a short period of time. The føtex representative (B) highlighted this high level of available resources several times in the interview:
I have some leverage, so when we do something, we don’t do it by halves. What I find most motivating, and I can say that with complete peace of mind, is that if the Salling Group says they’re going to do something, or if føtex says they’re going to do something or says they want to win this particular battle, then we win it, and then we do it to the full. [...] So when we say, for example, with this health project, that ‘we want to work with health,’ then we do want to work with health, and we’re going to make a difference in health, too. (føtex representative (B))
In this excerpt, she expressed that the mere size of the company allowed them to push any agenda if they wanted to. However, this also underlines that this capacity is dependent on the retailer’s willingness, a willingness that was not in favour of many of the initiatives that the researcher, based on the literature, thought would have the greatest effect.
Even though the size of the company came with many available resources, the retailer also explained how the size of the company had worked against the project in several ways:
What I think made it difficult for us to get through with some of these things let's just take the sodas, in that case, we have a private label collaborator who has production facilities, and when they press the ‘Salling sodas’ button, it doesn't just spew out a few thousand bottles, but millions. So saying ‘can't we just try to reduce the size and give it a try.’ It's a giant setup, so it’s not possible to do that at a whim. You’d need to get a whole or half chain on board that can help sell such volumes because otherwise, the costs would go through the roof. (føtex representative (A))
What this excerpt explains is that even changes that appeared small would take tremendous effort and be very costly, due to the size of the organisation.
Another challenge of the implementation was embedded in the retailers’ organisational culture. Føtex representative (B) explained in the interview that conflicting goals between employees made it difficult and time-consuming when implementing new initiatives. Another barrier to implementing the initiatives was high staff turnover at the retailer. In an interview with a føtex representative, she explained that people often shifted around different positions in the organisation, which ended in the project falling between two stools, leading to misunderstandings of agreements and changes in attitudes towards the initiatives.
In summary, we find that the retailers could, in some respects, have a strong general capacity to implement new initiatives by having available resources and being used to implement new initiatives. Regardless, this study shows that this was not utilised due to a lack of willingness. Moreover, we find that the size and organisational culture of the retailer hampered the implementation of the initiatives.
Influence of customers and other stakeholders on store operation
The last section reports on the influence of customers on the retailer’s willingness to implement the initiatives, and the influence of other stakeholders, especially producers, on what can be implemented.
We found that the customer’s reactions and attitudes were determining to the retailer when implementing any new initiative, as indicated in the sections above. According to the retailer, the customer was the focus when designing the layout of the store:
We are in very close dialogue with our clients, we do quantitative surveys and we do focus groups, we do in-depth interviews. And in that context, we're trying to understand, when you're shopping, how do you go about it. Is it easy for you to find the items you are looking for? And based on the responses, we try to adapt our stores to make things easy for our customers. (føtex representative (A))
The same representative also mentioned that she thought it would have been a strength of the project to have conducted interviews with the customers as a part of the development process, emphasising the weight they put on the customer’s attitudes. The retailers highlighted the importance of customer satisfaction and convenience in their shopping experience as a barrier to implementing certain initiatives, such as changing the placement of products. However, these same factors have also proven to be facilitators for other initiatives, such as the tags for breakfast products and the complimentary banana for children, as demonstrated above.
Another important stakeholder for the supermarkets was the suppliers of their products. Others were government actors (e.g. the Danish Veterinary and Food Administration). For both downsizing initiatives, the suppliers of the products (sodas and bags for sweets) were key to the success of their implementation. In an interview with the store manager, he explained the huge role some of these suppliers have in the daily operation of the store and the chain.
After all, we’ve got a chain agreement that our head office has made with the breweries. I don’t get to decide which items are in our refrigerators. [...] The tricky thing is that we’re not only dealing with føtex or the Salling Group. We also have to do with some other, equally large companies that are also just coming in. Plus, I have people here X times a week to service their particular area. [...] [Another thing] that proved tricky, as far as I recall, was that the alternatives offered, people felt strongly about those because the breweries made some strategic choices, and because of those, some of the items that we might be able to stock, they didn't want to sell those. (Store manager)
This excerpt illustrates how suppliers like the breweries, as shown earlier, influenced the implementation and affected the decisions made by the retailer.
This section indicates that even though the retailer is convinced that a given initiative would be interesting to implement in their supermarket, the suppliers often must agree as well, and finally, the customers must also welcome it.
In this study, we have explored the implementation, acceptability, and feasibility of four different health-promoting food retail initiatives aimed at customers in a real-life supermarket setting, using different qualitative methods. We found that (i) Two initiatives (downsizing of bags for the pick’n’ mix sweets and the complimentary banana for children) were implemented to a high degree, yet delivery issues caused delays according to the planned date, especially for the bags. The downsizing of soda bottles was not implemented as intended; the size and packaging deviated from the original plan due to delivery failure. Moreover, the implementation decreased over the feasibility test for the initiative with shelf tags, as it took more continuous maintenance. For all initiatives, we found that they lingered after the feasibility test; however, only the banana for children was somewhat sustained for a period to accommodate customer demand. (ii) The retailers expressed different levels of acceptability towards the initiatives, and different representatives sometimes also showed different levels of acceptability towards the same initiative, such as the tags on the breakfast products. The most well-received initiative was the banana for children, which is somewhat unsurprising, as it was the retailers themselves that suggested including this initiative. Additionally, the positive response from the customers that they got supported the retailers’ positive attitude towards the initiative. We also found that many customers responded well to this initiative; however, we also observed a group that did not accept the initiative and preferred the bun over the banana. For the remaining initiatives, customers did not seem to notice them. Yet, we did observe customer behaviours that would probably work against the suggested mechanisms of some of the initiatives. (iii) In general, we describe three themes of barriers and facilitators that influence the implementation and possible sustainment of the initiatives: Health is not the number one priority, General capacity of the retailer, and Influence of customers and other stakeholders on store operation. Firstly, we found the retailers were motivated to work with health, both from a personal and professional perspective. The motivation was rooted in a feeling of social responsibility as well as health initiatives being viewed as a relative advantage, due to demand and making customers happier. Still, other priorities, such as profit and maintaining customers’ ‘free choice’, challenged the motivation to implement such initiatives. Secondly, the retailer showed a high level of available resources, which supported their general capacity to implement the initiatives; however, the large size of the organisation and its culture proved to be barriers to the implementation. Lastly, the analysis showed that the influence of both customers and other stakeholders was crucial to the implementation, both in terms of what is possible and what the retailers would be interested in and prioritise.
Our findings are similar to those of others [ 26 , 35 ]. Winkler et al. [ 35 ] found that even though supermarket actors found health-promoting initiatives meaningful to engage in, their engagement was challenged by a business mindset, practical routines, and structural requirements. Thus, despite the involvement of retailers in the development, selection and implementation of the initiatives, studies suggest that healthy food retail initiatives still encounter some fundamental barriers towards the implementation, such as the economical aspect or the view on customers’ free choice. However, our results also indicate that it might be possible to persuade food retailers to remove products or restrict choices if the evidence or arguments of it being the right thing to do are sufficiently strong, as with organic bananas or tobacco products. This has also been the case of another retailer in Denmark, which has decided that all their stores should be tobacco and nicotine-free by the end of 2028 to reduce the number of smokers [ 36 ]. Another solution is to identify win–win initiatives, as the complimentary banana for children was somewhat an example of (if we consider the banana as a healthier alternative) and which other studies have found as well [ 35 , 37 ].
Even though the four initiatives were implemented (yet two not as intended) in this study, and we found them to be somewhat acceptable to the retailers, we must still highlight that these initiatives represent a very small portion of the initiatives first suggested and entail several compromises from what the researchers had initially planned (Duus et al. Unpublished ). Moreover, the customer’s responses to the initiatives were mixed, and in some cases, their behaviour indicated that the initiatives would have little effect. Compared with studies testing similar initiatives, we find that 1) Shelf tags alone were found unlikely to change food purchases [ 38 ] and are likely to contribute to disparities in food purchases as not all customers know nutrition labels or have the literacy to read and understand them [ 39 ]. 2) Smaller bags for pick’n’ mix sweets could be successfully implemented and, based on results from another study, might be able to decrease the volume of sweets sold [ 40 ]. Moreover, others have also shown that customers are willing to buy smaller product options [ 41 ]. Taken together, this suggests that voluntary engagement with researchers might not suffice to make changes that would improve the supermarket environment as opted for to support population health. This view has also been suggested by Winkler et al. [ 35 ], and in the Lancet series on commercial determinants of health, an even more critical perspective on engagements with commercial actors as food retailers is presented [ 42 , 43 ]. Here they warn against how commercial actors use partnerships with researchers, among others, as a tool to improve their reputation and credibility [ 42 ].
In our collaborative process with the retailer, we experienced many challenges. We did not accomplish aligning retailers’ and researchers’ interests as scholars have suggested being the prerequisite of implementing healthy food retail interventions in supermarkets [ 26 , 27 ]. This underlines the importance of the pre-intervention phase, as described by Hawe, Shiell, and Riley [ 44 ], which is fundamental to a successful implementation. During the pre-intervention phase, the establishment of relationships between different people or agencies often occurs, and these relationships may play a crucial role in the implementation and the explanation of why some work and others do not [ 44 ]. In line with this, another study has suggested exploring what implementation strategies might promote the uptake of evidence-based interventions among food retailers [ 45 ]. They found that contrary to many other studies, the intervention in their study was compatible with the interest of the store managers to which it was presented—these store managers had a strong feeling of social responsibility towards the communities they operated in [ 45 ].
Strength and limitations
The investigation of the feasibility test was strengthened by using different methods, process evaluation concepts, and a broad view including both the delivery and presentation of the initiatives as well as customer and retailer perspectives. We primarily got the retailer perspective from a strategic level, yet we had planned on conducting focus group interviews with staff at the test store to get perspectives from an operational level on the initiatives and the implementation process. However, no staff wanted to participate in an interview. The store manager explained that this probably was due to three things: 1) They had no interest in the study, or they were tired of the study, 2) the recruitment was done too late (approximately 2 months after the feasibility test period), and 3) the staff was overworked as a result of understaffing due to the coronavirus disease pandemic. Future studies aim also to analyse sales data in order to evaluate whether any changes in sales of the products we intervened on occurred. However, with the available data, we will not be able to analyse whether the initiatives change people’s eating patterns or whether they influence people differently in terms of their socioeconomic factors or other characteristics.
A thorough needs assessment [ 46 ] among supermarket customers to test the initiative’s assumptions and their food purchase patterns would have strengthened the study. However, this was not possible within the timeframe and funding scheme, so the development drew primarily on existing knowledge and the experience of the retailer and the Danish Cancer Society. Furthermore, the store visits conducted in the store during the development of the initiative also provided a few customer perspectives, which led to the exclusion of some ideas (Duus et al. unpublished ).
Furthermore, we learned two methodological lessons from the in-store observations: 1) All observers were met by the feeling of being ‘in the way’ and a need to be in almost constant movement to not interfere with the order in the store. The observers were met with a feeling of self-awareness and a need to legitimise their presence at the store by wearing a sticker on their shirts saying ‘visitor’ or their university identification card. These feelings were amplified by the governmental advice of social distancing and the requirement to wear face masks in grocery stores, introduced during the period of observations. 2) Concerning this, the observers also found it challenging to approach customers for the short interviews due to the feeling of invading people’s private space, hence only five were conducted. This was especially challenging when wearing face masks, as it was impossible to produce and read non-verbal signals (e.g. smiles), and difficult to hear what people were saying.
Implications for future studies and practice
This study presents an investigation of the implementation of healthy food retail initiatives for supermarkets that have been developed and selected together with retailers as suggested by the literature. It suggests that the implementation of such initiatives is possible and—to some degree—high. Yet, the quality of the initiatives was rather low, and some were not implemented as intended. Moreover, we still present some of the same barriers and limitations as former studies that have not implemented collaborative strategies in the pre-intervention phase. Some of this may be due to challenges such as a high staff turnover at the retailer and a lack of a shared understanding, as shown in another study (Duus et al. unpublished ). Future studies must explore this further.
Lessons for future studies are to identify initiatives that customers appreciate, as this is important to retailers. Underlining a needs assessment as an important first step in intervention development [ 30 , 46 ]. Furthermore, future studies should involve a broader range of stakeholders, including manufacturers and suppliers, in the development of the initiatives, as they have significant power over what can be implemented. Future studies would also benefit from identifying and testing implementation strategies that can facilitate the implementation of this type of intervention in this setting.
We performed a qualitative investigation of the implementation, acceptability, and feasibility of four different healthy food retail initiatives aimed at customers in a real-life supermarket setting, which had been developed and selected together with retailers. Only two of the four initiatives were implemented as intended, and the perspectives of retailers and customers were mixed or unclear. Altogether, the study highlights the challenges of implementing healthy retail food initiatives despite early involvement of retailers in the selection and design of those initiatives. Adding to the challenges of implementation, the initiatives also represent a compromise between the interests of the researcher and the retailers and do not represent what the literature suggests as the most effective strategies. A compromise made to uphold the partnership and complete the funded research project. Future studies should further examine the impact and pitfalls of including retailers (or other commercial actors) in the development and selection of healthy food retail initiatives and try to identify successful implementation strategies facilitating implementation.
Availability of data and materials
The data generated and analysed during the current study are not publicly available due to their sensitive and confidential nature but are available from the corresponding author upon reasonable request.
Abbreviations
Corporate Social Responsibility
Key Performance Indicator
Healthy diet. WHO. 2020. https://www.who.int/news-room/fact-sheets/detail/healthy-diet . Accessed 20 July 2023.
Greenwald P, Clifford CK, Milner JA. Diet and cancer prevention. Eur J Cancer. 2001May 1;37(8):948–65.
Article PubMed CAS Google Scholar
Firth J, Gangwisch JE, Borsini A, Wootton RE, Mayer EA. Food and mood: how do diet and nutrition affect mental wellbeing? BMJ. 2020Jun;29(369): m2382.
Article Google Scholar
English LK, Ard JD, Bailey RL, Bates M, Bazzano LA, Boushey CJ, et al. Evaluation of Dietary Patterns and All-Cause Mortality. JAMA Netw Open. 2021Aug 31;4(8): e2122277.
Article PubMed PubMed Central Google Scholar
Swinburn B, Caterson I, Seidell J, James W. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr. 2004Feb;7(1a):123–46.
Brug J. Determinants of healthy eating: motivation, abilities and environmental opportunities. Fam Pract. 2008 Dec 1;25(suppl_1):i50–5.
Adam A, Jensen JD. What is the effectiveness of obesity related interventions at retail grocery stores and supermarkets? —a systematic review. BMC Public Health. 2016Dec;16(1):1247.
Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: where should we look and what should we count? Int J Behav Nutr Phys Act. 2006Sep 26;3(1):33.
Sonntag D, Schneider S, Mdege N, Ali S, Schmidt B. Beyond Food Promotion: A Systematic Review on the Influence of the Food Industry on Obesity-Related Dietary Behaviour among Children. Nutrients. 2015;7(10):8565–76.
Viola D, Arno PS, Maroko AR, Schechter CB, Sohler N, Rundle A, et al. Overweight and obesity: Can we reconcile evidence about supermarkets and fast food retailers for public health policy? J Public Health Policy. 2013Aug;34(3):424–38.
Black C, Moon G, Baird J. Dietary inequalities: What is the evidence for the effect of the neighbourhood food environment? Health Place. 2014May;27:229–42.
Article PubMed Google Scholar
Vogel C, Ntani G, Inskip H, Barker M, Cummins S, Cooper C, et al. Education and the Relationship Between Supermarket Environment and Diet. Am J Prev Med. 2016Aug;51(2):e27-34.
Chandon P, Wansink B. Does food marketing need to make us fat? A review and solutions Nutr Rev. 2012;70(10):571–93.
PubMed Google Scholar
Bennett R, Zorbas C, Huse O, Peeters A, Cameron AJ, Sacks G, et al. Prevalence of healthy and unhealthy food and beverage price promotions and their potential influence on shopper purchasing behaviour: A systematic review of the literature. Obes Rev. 2020 Jan;21(1).
Harbers MC, Beulens JWJ, Rutters F, de Boer F, Gillebaart M, Sluijs I, et al. The effects of nudges on purchases, food choice, and energy intake or content of purchases in real-life food purchasing environments: a systematic review and evidence synthesis. Nutr J. 2020Dec;19(1):103.
Hollands GJ, Carter P, Anwer S, King SE, Jebb SA, Ogilvie D, et al. Altering the availability or proximity of food, alcohol, and tobacco products to change their selection and consumption. Cochrane Public Health Group, editor. Cochrane Database Syst Rev. 2019 Sep 4.
Slapø H, Schjøll A, Strømgren B, Sandaker I, Lekhal S. Efficiency of In-Store Interventions to Impact Customers to Purchase Healthier Food and Beverage Products in Real-Life Grocery Stores: A Systematic Review and Meta-Analysis. Foods. 2021May;10(5):922.
Gravlee CC, Boston PQ, Mitchell MM, Schultz AF, Betterley C. Food store owners’ and managers’ perspectives on the food environment: an exploratory mixed-methods study. BMC Public Health. 2014Dec;14(1):1031.
Winkler LL, Christensen U, Glümer C, Bloch P, Mikkelsen BE, Wansink B, et al. Substituting sugar confectionery with fruit and healthy snacks at checkout – a win-win strategy for consumers and food stores? a study on consumer attitudes and sales effects of a healthy supermarket intervention. BMC Public Health. 2016Nov 22;16(1):1184.
Adam A, Jensen JD, Sommer I, Hansen GL. Does shelf space management intervention have an effect on calorie turnover at supermarkets? J Retail Consum Serv. 2017Jan;1(34):311–8.
Toft U, Buch-Andersen T, Bloch P, Reinbach HC, Jensen BB, Mikkelsen BE, et al. A Community-Based, Participatory, Multi-Component Intervention Increased Sales of Healthy Foods in Local Supermarkets—The Health and Local Community Project (SoL). Int J Environ Res Public Health. 2023Jan;20(3):2478.
Bauer JM, Aarestrup SC, Hansen PG, Reisch LA. Nudging more sustainable grocery purchases: Behavioural innovations in a supermarket setting. Technol Forecast Soc Change. 2022Jun;1(179): 121605.
Denver S, Christensen T, Nordström J. Consumer preferences for low-salt foods: a Danish case study based on a comprehensive supermarket intervention. Public Health Nutr. 2021;24(12):3956–65.
Jensen JD, Sommer I. Reducing calorie sales from supermarkets – ‘silent’ reformulation of retailer-brand food products. Int J Behav Nutr Phys Act. 2017Aug 23;14(1):104.
Toft U, Winkler LL, Mikkelsen BE, Bloch P, Glümer C. Discounts on fruit and vegetables combined with a space management intervention increased sales in supermarkets. Eur J Clin Nutr. 2017Apr;71(4):476–80.
Middel CNH, Schuitmaker-Warnaar TJ, Mackenbach JD, Broerse JEW. Systematic review: a systems innovation perspective on barriers and facilitators for the implementation of healthy food-store interventions. Int J Behav Nutr Phys Act. 2019Dec;16(1):108.
Gupta A, Alston L, Needham C, Robinson E, Marshall J, Boelsen-Robinson T, et al. Factors Influencing Implementation, Sustainability and Scalability of Healthy Food Retail Interventions: A Systematic Review of Reviews. Nutrients. 2022Jan;14(2):294.
Denmark: market share of grocery retailers 2020. https://www.statista.com/statistics/565747/market-share-of-selected-grocery-retailers-in-denmark/ . Accessed 19 July 2023.
Moore N, editor. Desk research. In: How to Do Research: The Practical Guide to Designing and Managing Research Projects. Facet; 2006. p. 106–11.
Schultz Petersen K, Maindal HT, Ledderer L, Overgaard C. Komplekse interventioner: Udvikling, test, evaluering og implementering. Aalborg Universitetsforlag; 2022.
McGill E, Marks D, Er V, Penney T, Petticrew M, Egan M. Qualitative process evaluation from a complex systems perspective: A systematic review and framework for public health evaluators. PLoS Med. 2020Nov 2;17(11): e1003368.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006Jan;3(2):77–101.
Scaccia JP, Cook BS, Lamont A, Wandersman A, Castellow J, Katz J, et al. A practical implementation science heuristic for organizational readiness: R = MC2. J Community Psychol. 2015Apr;43(4):484–501.
Blake MR, Backholer K, Lancsar E, Boelsen-Robinson T, Mah C, Brimblecombe J, et al. Investigating business outcomes of healthy food retail strategies: A systematic scoping review. Obes Rev. 2019Oct;20(10):1384–99.
Winkler LL, Toft U, Glümer C, Bloch P, Buch-Andersen T, Christensen U. Involving supermarkets in health promotion interventions in the Danish Project SoL. A practice-oriented qualitative study on the engagement of supermarket staff and managers. BMC Public Health. 2023 Apr 18;23(1):706.
Lidl Danmark. https://om.lidl.dk/ansvarlighed/vi-fremmer-sundheden/udfasning-af-tobak . Accessed 7 March 2024.
Blake MR, Sacks G, Zorbas C, Marshall J, Orellana L, Brown AK, et al. The ‘Eat Well @ IGA’ healthy supermarket randomised controlled trial: process evaluation. Int J Behav Nutr Phys Act. 2021Dec;18(1):36.
Vandevijvere S, Berger N. The impact of shelf tags with Nutri-Score on consumer purchases: a difference-in-difference analysis of a natural experiment in supermarkets of a major retailer in Belgium. Int J Behav Nutr Phys Act. 2021Nov 18;18(1):150.
Robertson A, Lobstein T, Knai C. Obesity and socio-economic groups in Europe: Evidence review and implications for action. 2007.
Mørck CJ. Nyt forsøg afslører: Bland selv-posens størrelse gør en stor forskel. 2024. https://www.cancer.dk/nyheder-og-fortaellinger/2024/nyt-forsoeg-afsloerer-bland-selv-posens-stoerrelse-goer-en-stor-forskel/ . Accessed 4 July 2024.
Vandenbroele J, Slabbinck H, Van Kerckhove A, Vermeir I. Curbing portion size effects by adding smaller portions at the point of purchase. Food Qual Prefer. 2018Mar;1(64):82–7.
Gilmore AB, Fabbri A, Baum F, Bertscher A, Bondy K, Chang HJ, et al. Defining and conceptualising the commercial determinants of health. Lancet. 2023Apr;401(10383):1194–213.
Lacy-Nichols J, Nandi S, Mialon M, McCambridge J, Lee K, Jones A, et al. Conceptualising commercial entities in public health: beyond unhealthy commodities and transnational corporations. Lancet. 2023Apr;401(10383):1214–28.
Hawe P, Shiell A, Riley T. Theorising Interventions as Events in Systems. Am J Community Psychol. 2009;43(3–4):267–76.
Brimblecombe J, Miles B, Chappell E, De Silva K, Ferguson M, Mah C, et al. Implementation of a food retail intervention to reduce purchase of unhealthy food and beverages in remote Australia: mixed-method evaluation using the consolidated framework for implementation research. Int J Behav Nutr Phys Act. 2023Feb 17;20(1):20.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021Sep;30(374): n2061.
Download references
Acknowledgements
We want to thank all the participating retail group and supermarket staff members involved in this project and the implementation process. We appreciate the time and effort you have dedicated to this project and your openness. Furthermore, we want to acknowledge the customers who took the time to share their opinions with us during their daily grocery shopping.
We acknowledge Johanne Aviaja Rosing, Louise Ayoe Sparvath Brautsch, and Carl Johannes Middelboe for their assistance in conducting the pre- and post-intervention observations.
Open access funding provided by University of Southern Denmark This study is funded by the Danish Cancer Society, grant no.: R274-A16920. The first author (Katrine Sidenius Duus) has also received a Faculty Scholarship from the Faculty of Health Sciences at the University of Southern Denmark to support the completion of her PhD thesis, which this study is part of.
Author information
Authors and affiliations.
The National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark
Katrine Sidenius Duus, Tine Tjørnhøj-Thomsen & Rikke Fredenslund Krølner
You can also search for this author in PubMed Google Scholar
Contributions
KSD, RFK, and TTT contributed to the funding acquisition, study conception and design. Data generation and analyses were performed by KSD. The first draft of the manuscript was written by KSD. RFK and TTT commented on previous versions of the manuscript and contributed in writing the final manuscript. KSD wrote up the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Katrine Sidenius Duus .
Ethics declarations
Ethics approval and consent to participate.
This study has been approved by SDU Research & Innovation Organization (notification no. 11.136). All informants who participated in interviews received written and verbal information about the aim, that participation was voluntary and that their information would be used for research purposes only and treated with confidentiality. By participating, consent for their data to be used for research was given. Data from the observation and documents were handled confidentially and with caution to protect sensitive information that could identify individuals.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Duus, K.S., Tjørnhøj-Thomsen, T. & Krølner, R.F. Implementation of health-promoting retail initiatives in the Healthier Choices in Supermarkets Study—qualitative perspectives from a feasibility study. BMC Med 22 , 349 (2024). https://doi.org/10.1186/s12916-024-03561-2
Download citation
Received : 24 May 2024
Accepted : 14 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12916-024-03561-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation
- Qualitative research
- Health promotion
- Supermarkets
- Involvement
- Intervention
BMC Medicine
ISSN: 1741-7015
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Interviewing. This is the most common format of data collection in qualitative research. According to Oakley, qualitative interview is a type of framework in which the practices and standards be not only recorded, but also achieved, challenged and as well as reinforced.[] As no research interview lacks structure[] most of the qualitative research interviews are either semi-structured, lightly ...
Qualitative Sociology 37(2):153-171. Written as a response to various debates surrounding the relative value of interview-based studies and ethnographic studies defending the particular strengths of interviewing. This is a must-read article for anyone seriously engaging in qualitative research! Pugh, Allison J. 2013.
Here are some steps on how to analyze a qualitative interview: 1. Transcription. The first step is transcribing the interview into text format to have a written record of the conversation. This step is essential to ensure that you can refer back to the interview data and identify the important aspects of the interview.
Qualitative interviewing is a foundational method in qualitative research and is widely used in health research and the social sciences. Both qualitative semi-structured and in-depth unstructured interviews use verbal communication, mostly in face-to-face interactions, to collect data about the attitudes, beliefs, and experiences of participants.
In-depth interviews are a qualitative research method that follow a deceptively familiar logic of human interaction: ... whether comparisons are to be made and the duration of interviews. Studies ...
Introduction. In medical education research, the qualitative research interview is a viable and highly utilized data-collection tool (DiCicco-Bloom and Crabtree Citation 2006; Jamshed Citation 2014).There are a range of interview formats, conducted with both individuals and groups, where semi-structured interviews are becoming increasingly prevalent in medical education research.
Qualitative interview is a broad term uniting semi-structured and unstructured interviews. Quali-tative interviewing is less structured and more likely to evolve as a natural conversation; it is of-ten conducted in the form of respondents narrating their personal experiences or life histories. Qualitative interviews can be part of ethnography ...
InterViews by Steinar Kvale Interviewing is an essential tool in qualitative research and this introduction to interviewing outlines both the theoretical underpinnings and the practical aspects of the process. After examining the role of the interview in the research process, Steinar Kvale considers some of the key philosophical issues relating ...
Qualitative literacy a guide to evaluating ethnographic and interview research. University of California Press. University of California Press. ISBN: 0520390652
A qualitative research interview is a one-to-one data collection session between a researcher and a participant. Interviews may be carried out face-to-face, over the phone or via video call using a service like Skype or Zoom. There are three main types of qualitative research interview - structured, unstructured or semi-structured.
structured qualitative research interviews, some of which were conducted by telephone and some face-to-face. This paper focuses on selected parts of the analysis, including the overall duration of the interviews and the amount and balance of talk in each mode. Analysis of further interactional
Qualitative interviews are a widely used method in applied linguistics research, with researchers incorporating interviews in a variety of research designs, including case studies, mixed methods, oral and life history studies, and ethnographies. This entry discusses commonly used forms of interviews, such as phenomenological, ethnographic, and ...
What are interviews? An interviewing method is the most commonly used data collection technique in qualitative research. 1 The purpose of an interview is to explore the experiences, understandings, opinions and motivations of research participants. 2 Interviews are conducted one-on-one with the researcher and the participant. Interviews are most appropriate when seeking to understand a ...
Types of Interviews in Research | Guide & Examples. Published on March 10, 2022 by Tegan George. Revised on June 22, 2023. An interview is a qualitative research method that relies on asking questions in order to collect data. Interviews involve two or more people, one of whom is the interviewer asking the questions.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives ...
5. Not keeping your golden thread front of mind. We touched on this a little earlier, but it is a key point that should be central to your entire research process. You don't want to end up with pages and pages of data after conducting your interviews and realize that it is not useful to your research aims.
Leveraging the intensive-extensive temporal plane of time, we explore research approaches employing both shorter and longer timeframes, as well as intensive and extensive tempos. ... Conducting rapid qualitative interview research during the COVID-19 pandemic—reflections on methodological choices. Frontiers in Sociology, 7, Article 953872 ...
The interview method has a long and distinguished history in qualitative inquiry across the social sciences (Platt, 2012).Interviewing has become increasingly widespread in psychology (Brinkmann, 2016), as qualitative methods have gained prominence in the discipline (Gergen, Josselson, & Freeman, 2015).More than simply providing an account of attitudes or experience, the interview represents a ...
The semi-structured interview has become a pillar of contemporary qualitative research in the social sciences and beyond, yet the training provided in interviewing tends to be focused on question wording and rapport building rather than the dynamics of probing (e.g. Brinkmann and Kvale Citation 2018; Silverman Citation 2013). The potential ...
Qualitative research interviews are depth interviews. They elicit detailed feedback from your leads and customers. Unstructured interviews reveal why people react in a certain way or make certain decisions. According to The Hartford, qualitative research provides an anecdotal look into your business. That provides an important form of data.
There are a variety of methods of data collection in qualitative research, including observations, textual or visual analysis (eg from books or videos) and interviews (individual or group). 1 ...
Interviews in Qualitative Research. Ejem Agwu. - 26 Jun 2023. - The Encyclopedia of Applied Linguistics. - pp 1-9. TL;DR: The authors discusses commonly used forms of interviews and provides examples to show how researchers use interview accounts to generate knowledge about topics in applied linguistics, including case studies, ethnographies ...
Methods. Qualitative focus groups and semi-structured interviews took place between 2022-2023. Six focus groups were conducted with doctors, pharmacists and clinical pharmacologists (n = 21), and three patient focus groups with patients with multimorbidity (n = 13).
Interested participants responded and completed an online consent form before arranging an appropriate time for the interview. For those who completed baseline interviews, we repeated this process at three and six months post baseline. ... et al. Qualitative research practice: a guide for social science students and researchers. sage; 2013.
As early as the 1980s, qualitative researchers demonstrated sensitivity to the impact of research interviews on participants (Cowles, 1988; Munhall, 1988).Reacting to the hegemony of standardized measures that were thought to "squelch or deform the localized and personal knowledge of research participants" (Gergen, 2001, p. 21), researchers focused on learning about people's often deeply ...
Ultimately, tools like this exemplify the future of qualitative research, allowing for deeper insights that greatly inform strategies and outcomes. Real-Time Collaboration Tools. In today's rapidly evolving work environment, real-time collaboration tools have become essential for qualitative research teams.
The research process was overseen by a doctoral student in nursing with expertise in qualitative research. The interviews and initial coding were reviewed and approved by the participants, with any ambiguities promptly addressed. ... The participants were informed about the possible duration of the interviews, the freedom and authority to stop ...
Here we report the qualitative findings from an independent evaluation of the FWS. Thirty-seven interviews took place online or over the phone with 16 service users (of whom two took part in a follow-up interview), eight FWS providers and 11 healthcare professionals. Interviews were coded and analysed using thematic analysis.
Background Providing positive and supportive environments for nurses and midwives working in ever-changing and complex healthcare services is paramount. Clinical supervision is one approach that nurtures and supports professional guidance, ethical practice, and personal development, which impacts positively on staff morale and standards of care delivery. In the context of this study, peer ...
Qualitative interviews. Between November 2021 and February 2023, the first author conducted four semi-structured interviews with retailers (n = 3) who had been involved in the study (Table 2) to explore their views on the initiatives and the implementation process. Interview guides were used in all interviews alongside different prompts (e.g ...