Evaluating and Pricing Health Insurance in Lower-income Countries: A Field Experiment in India
Universal health coverage is a widely shared goal across lower-income countries. We conducted a large-scale, 4-year trial that randomized premiums and subsidies for India’s first national, public hospital insurance program, called RSBY. We find substantial demand (∼ 60% uptake) even when consumers were charged a price equal to the premium the government paid for insurance. We also find substantial adverse selection into insurance at positive prices. Insurance enrollment increases insurance utilization, partly due to spillovers from use of insurance by neighbors. However, healthcare utilization does not rise substantially, suggesting the primary benefit of insurance is financial. Many enrollees attempted to use insurance but failed, suggesting that learning is critical to the success of public insurance. We find very few statistically significant impacts of insurance access or enrollment on health. Because there is substantial willingness-to- pay for insurance, and given how distortionary it is to raise revenue in the Indian context, we calculate that our sample population should be charged a premium for RSBY between 67-95% of average costs (INR 528-1052, $30-60) rather than a zero premium to maximize the marginal value of public funds.
We thank Kate Baicker, Amitabh Chandra, Manasi Deshpande, Pascaline Dupas, Jacob Goldin, Joshua Gottlieb, Johannes Haushofer, Nathaniel Hendren, Rick Hornbeck, Radhika Jain, Neale Mahoney, Karthik Muralidharan, Joe Newhouse, Matt Notowodigdo, Julian Reif, and seminar participants at Brown University, Columbia University, University of Chicago, HBS, the Indian School of Public Policy, PUC-Rio, Stanford, Wharton, ASSA, Barcelona Summer School, BREAD, IFS-UCL-LSE-STICERD Development seminar, and LEAP for comments. For exceptional research assistance, we thank Tanay Balantrapu, Afia Khan, Sneha Stephen, Tianyu Zheng, and the JPAL-SA and Outline India field teams. This study was funded by the Department for International Development in the UK Government; the Tata Trusts through the Tata Centre for Development at the University of Chicago; the MacLean Center, the Becker-Friedman Institute, the Neubauer Collegium, and the Law School at the University of Chicago; the Sloan Foundation; SRM University; Northwestern University and the International Growth Centre. The study received IRB approval from U. of Chicago (IRB12-2085), Northwestern (STU00073184), the Public Health Foundation of India (TRCIEC- 182/13), and the Institute for Financial Management and Research. This study was registered with ClinicalTrials.gov (NCT03144076) and the American Economic Association Registry (AEARCTR-0001793). The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
- randomized controlled trials registry entry
- online appendix
- March 15, 2024

Working Groups
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .
Effect of Health Insurance in India: A Randomized Controlled Trial
University of Chicago, Becker Friedman Institute for Economics Working Paper No. 2021-146
52 Pages Posted: 27 Dec 2021
Anup Malani
University of Chicago - Law School; National Bureau of Economic Research (NBER); University of Chicago Pritzker School of Medicine; Resources for the Future
Phoebe Holtzman
Jones Lang LaSalle
Kosuke Imai
Harvard University
Cynthia Kinnan
Northwestern University - Department of Economics
Morgen Miller
University of Chicago
Shailender Swaminathan
University of Alabama at Birmingham - School of Public Health
Alessandra Voena
Stanford University
Bartosz Woda
University of Chicago - Law School
Gabriella Conti
University College London
Date Written: December 17, 2021
We report on a large randomized controlled trial of hospital insurance for above poverty-line Indian households. Households were assigned to free insurance, sale of insurance, sale plus cash transfer, or control. To estimate spillovers, the fraction of households offered insurance varied across villages. The opportunity to purchase insurance led to 59.91% uptake and access to free insurance to 78.71% uptake. Access increased insurance utilization. Positive spillover effects on utilization suggest learning from peers. Many beneficiaries were unable to use insurance, demonstrating hurdles to expanding access via insurance. Across a range of health measures, we estimate no significant impacts on health.
Suggested Citation: Suggested Citation
Anup Malani (Contact Author)
University of chicago - law school ( email ).
1111 E. 60th St. Chicago, IL 60637 United States 773-702-9602 (Phone) 773-702-0730 (Fax)
HOME PAGE: http://www.law.uchicago.edu/faculty/malani/
National Bureau of Economic Research (NBER)
1050 Massachusetts Avenue Cambridge, MA 02138 United States
University of Chicago Pritzker School of Medicine
Chicago, IL 60637 United States
Resources for the Future
1616 P Street, NW Washington, DC 20036 United States
Jones Lang LaSalle ( email )
330 Madison Ave 4th floor New York, NY 10017
Harvard University ( email )
1875 Cambridge Street Cambridge, MA 02138 United States
Northwestern University - Department of Economics ( email )
2003 Sheridan Road Evanston, IL 60208 United States
University of Chicago ( email )
1101 East 58th Street Chicago, IL 60637 United States
University of Alabama at Birmingham - School of Public Health ( email )
1665 University Blvd. Birmingham, AL 35294 United States
Stanford University ( email )
Stanford, CA 94305 United States
1111 E. 60th St. Chicago, IL 60637 United States
University College London ( email )
Gower Street London, WC1E 6BT United Kingdom
Do you have a job opening that you would like to promote on SSRN?
Paper statistics, related ejournals, becker friedman institute for economics working paper series.
Subscribe to this free journal for more curated articles on this topic
Randomized Social Experiments eJournal
Subscribe to this fee journal for more curated articles on this topic
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Impact of Publicly Financed Health Insurance Schemes on Healthcare Utilization and Financial Risk Protection in India: A Systematic Review
* E-mail: [email protected]
Affiliation School of Public Health, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Affiliation Indian Institute of Public Health, Delhi, Public Health Foundation of India, Delhi NCR, India
- Shankar Prinja,
- Akashdeep Singh Chauhan,
- Anup Karan,
- Gunjeet Kaur,
- Rajesh Kumar

- Published: February 2, 2017
- https://doi.org/10.1371/journal.pone.0170996
- Reader Comments
Several publicly financed health insurance schemes have been launched in India with the aim of providing universalizing health coverage (UHC). In this paper, we report the impact of publicly financed health insurance schemes on health service utilization, out-of-pocket (OOP) expenditure, financial risk protection and health status. Empirical research studies focussing on the impact or evaluation of publicly financed health insurance schemes in India were searched on PubMed, Google scholar, Ovid, Scopus, Embase and relevant websites. The studies were selected based on two stage screening PRISMA guidelines in which two researchers independently assessed the suitability and quality of the studies. The studies included in the review were divided into two groups i.e., with and without a comparison group. To assess the impact on utilization, OOP expenditure and health indicators, only the studies with a comparison group were reviewed. Out of 1265 articles screened after initial search, 43 studies were found eligible and reviewed in full text, finally yielding 14 studies which had a comparator group in their evaluation design. All the studies (n-7) focussing on utilization showed a positive effect in terms of increase in the consumption of health services with introduction of health insurance. About 70% studies (n-5) studies with a strong design and assessing financial risk protection showed no impact in reduction of OOP expenditures, while remaining 30% of evaluations (n-2), which particularly evaluated state sponsored health insurance schemes, reported a decline in OOP expenditure among the enrolled households. One study which evaluated impact on health outcome showed reduction in mortality among enrolled as compared to non-enrolled households, from conditions covered by the insurance scheme. While utilization of healthcare did improve among those enrolled in the scheme, there is no clear evidence yet to suggest that these have resulted in reduced OOP expenditures or higher financial risk protection.
Citation: Prinja S, Chauhan AS, Karan A, Kaur G, Kumar R (2017) Impact of Publicly Financed Health Insurance Schemes on Healthcare Utilization and Financial Risk Protection in India: A Systematic Review. PLoS ONE 12(2): e0170996. https://doi.org/10.1371/journal.pone.0170996
Editor: Cheng-Yi Xia, Tianjin University of Technology, CHINA
Received: June 30, 2016; Accepted: January 13, 2017; Published: February 2, 2017
Copyright: © 2017 Prinja et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper.
Funding: This research was supported by USAID India grant AID-386-A-14-00006. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors declared that no competing interests exist.
Introduction
Achieving Universal Health Coverage (UHC) is a major policy goal in health sector globally. [ 1 , 2 ] Despite the acceptance of UHC at policy level in India, around three-quarters of healthcare spending is borne by households. [ 3 ] The recent National Sample Survey (NSS) report reveals that only 12% of the urban and 13% of the rural population is under any kind of health protection coverage. [ 4 ] Not surprisingly, nearly 26% of the total health spending by rural households is sourced from either borrowings or selling of assets. [ 4 ] Further, OOP spending pushes approximately 3.5% to 6.2% of the India’s population below the poverty line every year. [ 5 – 7 ]
Traditionally, health care financing in India had been mostly restricted to the supply side, focussing on the strengthening of infrastructure and human resource. The advent of National Rural Health Mission (NRHM) in 2005 also served as an instrument of strengthening the supply-side infrastructure. [ 8 ] The Planning Commission’s High Level Expert Group (HLEG) proposed a model to achieve UHC under which citizens would have full access to free healthcare from a combination of public and private facilities. [ 9 ] This shifted government’s attention from its prior focus on supply side to demand side financing models in the form of publicly sponsored health insurance schemes.
Since 2007, several publicly financed health insurance schemes have been launched in India both at the state level such as Rajiv Aarogyasri Health Insurance Scheme (RAS) in Andhra Pradesh [ 10 ], Rajiv Gandhi Jeevandayee Arogya Yojana (RGJAY) in Maharashtra [ 11 ], Chief Minister’s Comprehensive Health Insurance scheme (CMCHIS) in Tamil Nadu [ 12 ], and Rashtriya Swasthya Bima Yojana (RSBY) at the Central level. [ 13 ] These demand-side financing mechanisms entitle poor and other vulnerable households to choose cashless healthcare from a pool of empanelled private or public providers. While the RSBY scheme was designed and implemented by the Ministry of Labour and Employment (MOLE), the implementation role for RSBY–now called Rashtriya Swasthya Suraksha Yojana (RSSY, however we refer to as RSBY in the entire paper), has been recently transferred to Ministry of Health and Family Welfare in 2015. [ 14 ]
In the last 7–8 years, a large amount of government’s money has been invested in the implementation of these health insurance schemes. A total of INR 370 billion (USD 587 million) tax money has been allocated for RSBY since its launch in 2008–09. [ 15 ] If the budgets of state sponsored schemes are also pooled, it amounts to a significant amount of public exchequer’s money, thereby justifying a need to determine whether these schemes are achieving their desired objectives.
In line with this policy need for an appraisal, the Government of India constituted a task force on costing of health services. One of the terms of reference for this Task Force included an assessment of RSBY. [ 16 ] Also, several State Governments have set up independent commissions to determine the best way forward to achieve universal health coverage. [ 17 , 18 ] As a result, there is a need to systematically review evidence in terms of whether these schemes have been able to achieve the objectives of universalizing health care for which they were launched. Two reviews have been published earlier, both of which measured the impact of health insurance in low and middle income countries as a whole without a specific focus on India. [ 19 , 20 ] Specific characteristics of the scheme implementation and contextual differences in various countries support a case for a systematic review with a national focus. Further, one of these review focussed on only social and community based health insurance schemes. [ 20 ] However, much of the current interest is on determining success or failure of tax-funded health insurance schemes which cover nearly 14% out of the total 15% population who have any form of health care insurance.
As a result, we conducted a systematic review to primarily assess the impact of publicly financed health insurance schemes on utilization of health care services, out of pocket expenditure, financial risk protection and on the health of population in India. Secondly, we also summarise the findings of various process evaluations, which have assessed the performance of these schemes in terms of extent of community awareness, determinants of enrolment and utilization, accessibility and utilization of different services across states in India.
Methodology
Search strategy.
A comprehensive computerised search was conducted to search for empirical studies focussing on the impact or evaluation of publicly sponsored health insurance schemes in India. PubMed, Google scholar, Ovid, Scopus and Embase databases were searched to identify eligible studies published till September 2015. Official websites of various health insurance schemes ( www.rsby.gov.in , www.aarogyasri.telangana.gov.in , www.sast.gov.in/home/VAS.html , http://www.cmchistn.com and / www.chiak.org ) were also searched. The review used the search strategy consisting of following key words:
(((((((((((Publicly sponsored health insurance) OR government sponsored health insurance) OR Rashtriya Swasthya Bima Yojana) OR RSBY) OR rajiv arogyasree health insurance scheme) OR rajiv aarogyasri community health insurance scheme) OR vajpayee arogyasri) OR vajpayee arogyasri yojana) OR chief minister kalaignar insurance scheme) OR rajiv gandhi jeevandayee arogya yojana) OR comprehensive health insurance scheme)”.
The search strategy was defined by reviewing the previously done systematic reviews and in consultation with the research staff from the Advanced Centre for Evidence-Based Child Health and the library staff of the Post-Graduate Institute of Medical Education and Research, Chandigarh. The key words were checked for controlled vocabulary under Medical Subject Headings (MeSH) of PubMed. Two investigators (ASC and GK) had access to abstract and full text of the paper to decide on its inclusion. Discrepancies between the two investigators were solved by discussion with the third investigator (SP). Two authors of this review are familiar with the methods of systematic review (SP and AK), two are experts in health economics with strong interest and familiarity with the health financing policies (SP and AK), while another author is a senior public health expert (RK).
Inclusion criteria and study selection
The review included peer-reviewed articles, government reports and working papers that were reported in the English language and excludes abstracts, expert opinions, narrative reviews, commentaries, case reports and conference papers.
The studies were selected based on a two stage screening process as per PRISMA guidelines [ 21 ] ( S1 Table ). The first step comprised of searching for studies based on the search strategy from the selected databases and websites. Following this, duplicates were removed and the remaining studies were then screened by applying inclusion criteria to the titles and abstracts. Based on the screening of titles and abstracts, potentially relevant articles were selected for further review, which involved examining the content of their full text. After reviewing full text, only empirical research studies were considered eligible while others were excluded. At this stage, a bibliographic search of the selected studies was also carried out to identify additional relevant articles. The search was continued until no new article was found ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0170996.g001
Data extraction and quality
A standardised data extraction form was developed to collect information from the selected studies on the relevant impact outcomes, besides the general and methodological aspects. The latter included information on year of publication, funding agency, study design or type of study (experimental and observational), description of intervention and control group, duration and location of the study, sample size, type of outcome assessed, etc. Two researchers (ASC and GK) independently extracted the data and assessed the quality of the studies.
The studies selected in the review were divided into two groups i.e., with a comparison or control group (against which the insured group was measured) and without a control group (descriptive in nature). To assess the impact on utilization, OOP expenditure and health indicators, studies with a comparison group alone were reviewed. Process level indicators were assessed based on the findings of studies from both the groups, i.e. with and without control group. Further, quality of these studies was assessed by Effective Public Health Practice Project (EPHPP) quality assessment tool for quantitative studies. [ 22 ] The components of quality assessment in the EPHPP tool include type of study, presence of any kind of selection bias, consideration to blinding and confounders, validity and reliability of the data collection tools and consideration to withdrawals and loss to follow ups, if any. We also categorised the studies (having a control group) based on their analytical approach–i.e. Intention to Treat (ITT) and Average Treatment effect on the Treated (ATT) analysis. [ 23 ] Basically, ITT measures impact on the eligible population irrespective of getting enrolled or utilising the services while ATT measures impact on those who are enrolled in the scheme.
A total of 1265 articles were identified from databases (n = 1244), websites (n = 18) and bibliographic search (n = 3) as shown in Fig 1 . After removing duplicates, the remaining 814 articles were screened by applying inclusion criteria to the titles and abstracts. A total of 671 articles were excluded in the 1 st stage screening and 143 studies were identified as eligible for 2 nd screening. Full text papers of these 143 studies were reviewed. Ultimately, 43 articles were found eligible for this systematic review. Out of this, 14 studies had a comparison group [ 24 – 37 ] and the remaining 29 were without a comparison group [ 38 – 66 ].
General characteristics of selected studies
Out of the 14 studies with a comparison group, 7 were cross-sectional studies with data collected from intervention and control group, while 6 studies were quasi experimental in nature adopting a pre and post design. Out of these 6 studies, 2 studies evaluated the impact based on difference in difference analysis and one study followed geographic discontinuity design ( Table 1 ). Most of these studies (n = 8) were published in peer reviewed journals while the remaining were reports (n = 3) and working papers (n = 3). Around half of the studies (n = 6) evaluated RSBY scheme, followed by studies on RAS (n = 3), Vajpayee Aarogyashri Scheme (VAS) (n = 1) and Comprehensive Health Insurance Scheme in Kerala (n = 1). Further, focus of the remaining 3 studies was on both RSBY and RAS. Twelve studies evaluated the health insurance scheme within 3 years of their implementation while the remaining 2 studies evaluated the scheme following 3 years of implementation.
https://doi.org/10.1371/journal.pone.0170996.t001
With regards to studies without a comparison group (n = 29), majority of them (59%, n = 17) were published in peer reviewed journals, 28% (n = 8) were working papers and the remaining were reports (13%) ( Table 1 ). All the studies had a cross sectional study design, out of which 8 studies were based on secondary data and 4 had a regression model based analysis. Nearly 83% (n = 24) of the studies evaluated RSBY, followed by 10% studies (n = 3) on RAS. More than half (56%, n = 16) of these studies were done within 3 years of the implementation of the scheme, followed by 31% (n = 9), assessing the scheme following 3 years of implementation. For the rest, 13% of the studies duration between implementation of the scheme and evaluation of the study was not clearly stated in the article.
Impact assessment
Table 2 summarises the impact of various publicly financed health insurance schemes reported in the selected 14 studies with a comparison group. Nine of these studies were based on ATT analysis approach [ 26 – 29 , 31 , 34 – 37 ], while remaining 5 studies were ITT in nature. [ 24 , 25 , 30 , 32 , 33 ]
https://doi.org/10.1371/journal.pone.0170996.t002
Among these, 7 studies (50%) assessed financial risk protection only, one study measured utilization alone, while remaining 5 studies (36%) evaluated both utilization and financial risk protection. Only one study included all the impact outcomes including the impact of insurance on the health of the population.
Financial risk protection.
Out of the 13 studies assessing financial risk protection [ 24 – 36 ], 9 (69%) reported no reduction in OOP expenditure among enrolled households after implementation of health insurance schemes. [ 24 – 27 , 30 – 32 , 34 , 35 ] In terms of quality, 7 studies had a strong methodological design [ 24 , 30 – 33 , 35 , 36 ], out of which 5 reported increase in the OOP expenses. [ 24 , 30 – 32 , 35 ] The remaining 2 studies, which evaluated state sponsored insurance schemes of Andhra Pradesh and Karnataka, showed a decline in OOP expenses. [ 33 , 36 ] Out of the five strong quality studies showing increase in OOP expenditure, 3 studies were based on the same data and methodology but had measured varied outcomes in terms of financial protection. [ 24 , 30 , 32 ] Specifically, among studies measuring catastrophic health expenditure as a measure of financial protection, 3/4 th showed increase in the incidence of catastrophic health count. [ 24 – 26 ] Only a single high quality study, which evaluated Andhra Pradesh’s RAS scheme showed a reduction in incidence catastrophic head count after implementation of the scheme. [ 33 ]
The studies (n = 5) which measured the impact of RSBY only, were either of a low or moderate quality and among these, 2 studies reported a reduction in OOP expenses [ 28 , 29 ], but none showed any decrease in incidence of catastrophic health expenditure. Among the 4 studies which evaluated state sponsored schemes [ 33 – 36 ], 2 reported reduction in OOP expenses [ 33 , 36 ], and one study showed decrease in number of catastrophic head count [ 33 ]. One study which considered all the publicly sponsored health insurance schemes together as one, reported that all these were associated with rise in OOP expenditure and catastrophic health expenditure. [ 25 ]
Three studies, which were based on similar data and methodology, compared the impact of RAS in Andhra Pradesh with that of RSBY in Maharashtra. [ 24 , 30 , 32 ] One of these studies showed that in both the states, schemes were associated with increase in OOP expenditure and catastrophic health expenditure, with higher increase in the state of Maharashtra. [ 24 ] Other study showed that this increase in expenditure was observed among both the household groups who accessed care in public or private health facilities. [ 32 ] The latter finding implied some protective effect of RAS in Andhra Pradesh, relative to RSBY in Maharashtra. However, independently, RAS did not result in a reduction in OOP expenses among insured. Another study inferred that this relative reduction in OOP expenditure and catastrophic health expenditure in Andhra Pradesh (compared to Maharashtra) was concentrated more among the richest 60%, implying an inequitable effect. [ 30 ]
Among 7 studies with a quasi-experimental design, 5 showed that the insurance schemes were associated with a rise in OOP expenditure. [ 24 , 30 – 32 , 35 ] Similarly, among the 3 studies based on DID analysis, 2 reported showed rise in OOP expenditure. [ 24 , 25 ] Among 6 cross sectional studies, a study reported similar [ 27 ] amount of OOP expenditures among enrolled and non-enrolled group and 2 studies reported reduction in incurring of OOP expenses. [ 28 , 29 ]
Out of the 7 studies with a strong methodological design, 4 were done within 3 years of the implementation of the schemes, of which 2 studies reported reduction in OOP expenditure [ 33 , 36 ] and a study showed reduction in catastrophic health expenditure. [ 33 ] Studies done at and after 3 year of implementation showed, that schemes were associated with increase in OOP expenses and number of catastrophic head count. [ 24 , 28 , 30 , 32 ]
Utilization.
Overall 7 articles assessed the impact of health insurance on utilization of health services and the findings of all these studies showed that these insurance schemes were associated with increase in consumption of health care services. In terms of quality, 5 studies were of strong methodological rigour [ 24 , 30 , 32 , 35 , 36 ] and the remaining 2 had a moderate or weak quality. [ 26 , 37 ] The increase in utilization among these studies varied from 12.3% to 244% among the insured as compared to non-insured households. The studies based on ATT analysis showed that this increase was in in the range of 12.3%-244%, [ 26 , 35 – 37 ] whereas studies based on ITT analysis showed the increase in the range of 22%-56% among the enrolled households. [ 24 ]
Among the studies which evaluated RSBY alone (n = 2), increase in utilization varied from 15.3% in Maharashtra [ 37 ] to 244% in Karnataka. [ 26 ] For the state-specific insurance schemes, increase in consumption of health care varied from 12.3% in Karnataka’s VAS [ 36 ] to 35.4% for Comprehensive Health Insurance Scheme of Kerala. [ 35 ]
One out of the 3 studies which were based on same data and methodology, comparing the impact of RAS in Andhra Pradesh with that of RSBY in Maharashtra, showed an increase in utilization in post insurance period in both states with higher increase in the state of Andhra Pradesh. [ 24 ] Another study showed that this significant positive growth in the utilization was more among both the poor and better-off households in Andhra Pradesh as compared to Maharashtra. Further, it also showed that the increase in utilization of simpler conditions such as fever was more among poor while the rich reported more consumption of services required for the management of chronic conditions such as kidney problems. [ 30 ] The third study showed that in the post insurance period utilization of services in private hospitals increased in Andhra Pradesh and decreased in Maharashtra. On the other hand, utilization in public facilities reduced in both the states with more decrease seen in the state of Andhra Pradesh. [ 32 ]
Increase in the utilization rate in early years of implementation was much higher (12.3% to 244%) [ 26 , 35 , 36 ], than the increase in utilization reported (15%) when the scheme was evaluated after 5 years of its implementation. [ 37 ]
Impact on health.
A single study assessed the impact of health insurance on the improvement of health among those enrolled in the scheme. It reported that the mortality rate from conditions covered by the scheme was less in eligible households as compared to ineligible households (0.32% vs 0.90%). [ 36 ] While about half (52%) of deaths among enrolled households were among people aged <60 years, this rose to more than three-fourths (76%) among those not enrolled. The study also showed that impact of the scheme in reducing mortality was more pronounced among poor in the treatment areas and not among population above poverty line.
Process evaluation
Out of the 29 studies without a control group, 77% of them (n = 24) were on RSBY only and the remaining studies either assessed state sponsored health insurance scheme only or compared it with RSBY. The process indicators included in these studies were level of awareness, determinants of enrolment and utilisation and accessibility to hospitals.
Eight studies done across states in India measured the awareness level of various attributes related to the health insurances schemes. [ 26 , 29 , 38 , 41 , 43 , 44 , 53 , 63 ] Further, 10 studies also assessed the source of awareness about these schemes across various states in India. [ 26 , 29 , 38 , 41 , 43 , 44 , 53 , 57 , 63 , 66 ] Furthermore, 6 studies evaluated the role of determinants for enrolment. [ 37 , 42 , 46 , 47 , 49 , 50 ] Similarly, 8 studies measured the association of factors influencing utilization of health services, among the enrolled households. [ 24 , 33 , 37 , 40 , 47 – 49 , 51 ]
Awareness levels of various attributes related the insurance schemes were reported to be in the range of 13.6% to 90% as shown in Table 3 . Awareness was highest for information on BPL status and 5 member per household as the eligibility criteria and relatively lowest for transport allowances and diseases/conditions covered under the insurance schemes. Specifically, information on eligibility condition of 5 members per household varied from 31% in Chhattisgarh to around 63% in Haryana. Further, awareness level ranged from 32% in Gujarat to 65% in Himachal Pradesh regarding information on free treatment being given under the scheme. Similarly regarding knowledge of transport allowance, information levels ranged from 13.6% in Haryana to 43% in Uttar Pradesh. Panchayats (median: 61%) and friends/ neighbours (median: 44.5%) were the most common source of awareness. In around 60% and 43% of the reported studies, panchayat and friends/neighbour respectively were stated as the source of awareness in more than 60% of the studied population. Less than 15% of the population stated the contribution of health care workers for awareness generation ( Table 4 ).
https://doi.org/10.1371/journal.pone.0170996.t003
https://doi.org/10.1371/journal.pone.0170996.t004
Determinants of enrolment.
The studies selected in the review showed that enrolment was inversely associated with administrative areas having a larger geographic size [ 42 , 49 ] and families belonging to socially disadvantaged communities [ 42 , 46 , 50 ] ( Table 5 ). Further, 2 studies also reported that low enrolment was related to the poverty status of the households. [ 46 , 47 ] On the contrary, higher enrolment was associated with households headed by a female. [ 37 , 46 ] Further, districts with good development indicators in terms of better business index [ 49 ], low corruption index [ 46 ], higher coverage of preventive health services such as DPT immunization [ 50 ] and better accessibility to commercial banks or nearby town [ 50 ] were also positively associated with high enrolment rates. None of the selected studies identified ‘self-selection’ while analysing the determinants of enrolment although one study mentioned that there is less likelihood of self-selection in RSBY as the scheme is open only for poor. [ 50 ]
https://doi.org/10.1371/journal.pone.0170996.t005
Determinants of utilization.
Higher the number of empanelled hospitals and proportion of private hospitals in a district, higher were the rates of hospitalization [ 47 – 49 , 51 ] ( Table 6 ). Less advantaged castes were associated with lowest utilization rates. [ 24 , 33 , 37 , 40 ] In contrast to trends in enrolment, districts with better indicators of economic development such as access to educational, commercial, hospitals and transportation institutions and better coverage of preventive or primary health services (such as DPT3 immunization rate) were linked with low utilization rates. [ 48 , 49 ] RSBY scheme was mostly utilized for gynaecological procedures (5–20%), urogenital (33.4%), gastrointestinal (11%) and ophthalmic (6%) conditions ( Fig 2 ). On the contrary, state sponsored health insurance schemes catered mainly to tertiary care needs for injuries (21–27%), oncology (6–17%) and cardiovascular/respiratory/nephrology conditions (9–10%). RSBY scheme was used predominantly for medical as compared to surgical procedures.
https://doi.org/10.1371/journal.pone.0170996.g002
https://doi.org/10.1371/journal.pone.0170996.t006
Private facilities were observed as the preferred ones by the beneficiaries of both RSBY and state level health insurance schemes. Findings from the states of Gujarat [ 40 ], Uttar Pradesh [ 29 ] and Haryana [ 66 ], showed private facilities to be most commonly utilized (73%, 87% and 67% respectively) under RSBY. Three-quarters of all claims under RSBY in India were reported to have utilized care in private facilities, with Bihar, Madhya Pradesh, and Rajasthan reporting 100% of claims from private facilities. [ 51 ] Over time, claims in Chattisgarh increased by 266% (INR 38436 to 140900) in private hospitals, as compared to 204% increase in public facilities (INR 30525 to 92905). [ 45 ] Considering, state sponsored scheme of Andhra Pradesh, number of surgeries performed in private hospitals were 2.85 times higher than in public facilities. [ 60 ]
It could be assumed that large percentage of empanelled private providers is the reason for high utilization of these facilities under RSBY. The states of Haryana, West Bengal and Bihar, where proportion of private empanelled hospitals was around 90%, the proportion of overall claims in these facilities was more than 95% in each of these states. ( Fig 3 ), [ 67 ] Similarly, in Tripura, Himachal Pradesh and Assam where proportion of private facilities was less than 20%, the proportion of claims in these facilities was less than 30%. Districts such as Kanpur Nagar from UP, Dangs from Gujarat and Karnal from Haryana, having more than 90% of total empanelled hospitals as private had highest hospitalisation rate across the state. [ 47 ]
https://doi.org/10.1371/journal.pone.0170996.g003
Even states with lower private sector empanelment, also continue to show higher share of private sector utilization. Private sector contributed 65% and 25% of the total empanelled facilities in the states of Madhya Pradesh and Rajasthan, while 100% of the claims were from private sector in these states ( Fig 3 ). Similarly, Uttar Pradesh and Jharkhand having 98% of claims from private facilities had 62% and 54% of the total empanelled facilities as private respectively. Kerala and Assam were the outliers, where the despite a proportion of private empanelled hospitals of around 50%, the utilization of these facilities was below 30%.
Uniformity and accessibility of hospitals.
Hospitalisation rates under RSBY scheme fell steadily with distance of home from health facility. [ 40 ] Those who lived more than 30 km had a lower inpatient rates as compared to those who lived within 30 km. Likewise, for Andhra Pradesh’s RAS scheme, as distance from the nearest treatment facility increased, the utilization rates declined. [ 58 ] Density of the empanelled hospitals was significantly and positively correlated with the utilization rate. [ 47 , 48 ]
Historically, the health system in India has had a maternal and child health (MCH) centric approach, both in financing and delivery of health services. [ 68 ] Low public spending on health care shifted the burden of seeking care on households by paying out of pocket expenditures. [ 9 ] This led to either a barrier in accessing health services, or catastrophic outcomes for those who sought care. [ 4 , 5 , 7 ] Further, low capacity of public health system has resulted in rapid development of private health care delivery system, as well as a push towards various demand-side financing mechanisms. [ 69 , 70 ] The recent policy thrust on UHC has shifted attention towards a broader focus on health system to meet all the needed preventive as well as curative health care needs of the population.
It is in this contextual framework that various publicly financed health insurance schemes evolved in India. At a time when the debate of ‘how’ to achieve universal health care is raging wide discussions, our paper attempts at summarizing the existing evidence. Our review is the first comprehensive systematic review which focuses on Indian publicly financed health insurance schemes. We find that there is positive evidence that the utilization of hospital services increased after introduction of these insurance schemes. Moreover, this increase in utilization has sustained over time and across regions. However, commensurate with an increase in utilization of services, so far we do not find substantial evidence on reduction of out-of-pocket expenditures or improvement of financial risk protection. In fact, 5 out of 8 studies actually reported either no impact or an increase in OOP expenditures. Finally, although one study does point to some beneficial effect on health of population, there is dearth of robust evidence on the impact of these schemes on the health of the population.
Although our review finds a general increase in utilization of hospitalization services, there are still several unanswered questions. This increase in utilization of hospitalizations could be attributed to 3 reasons: firstly, it could be a result of a pent-up demand on account of previously present barriers to access. However, this could explain the increase in hospitalization during early years of the implementation of health insurance schemes. Persistence of increased utilization over the last 7–8 years rules out this reason. Secondly, it could be attributed to either genuine reduction of financial barriers to access or a supplier induced demand. Given the available evidence, it is difficult to single out the reason from amongst the latter two. Examination of presence and extent of supplier-induced demand is certainly an important future area of research for health economists, although establishing a causal link is fraught with several methodological issues and problems with data availability. It can also be seen that the positive impact on utilization of services which we find in most existing studies could be an underestimate of the true effect considering low awareness level among the enrolled population. As time passes and awareness level improve, this could lead to further increase in utilization of health services [ 71 – 73 ]. Moreover, our review also shows that this increase in utilization is more concentrated in private sector hospitals. Together these two findings imply that it is not only likely to impose fiscal constraints on the government for sustainability of these schemes, but also expected to divert large amount of tax based public money towards private sector.
A second point of concern which points to inefficiency is the presence of conditions such as gynaecological problems, deliveries, cataract etc. among some of leading conditions for which hospitalizations are done. [ 40 , 49 ] This is a pointer to inefficient allocation of resources since while on one hand the Government is already allocating significant supply-side resources through flagship health programs on strengthening public sector facilities for providing universal access to these conditions [ 74 ]; on other hand these conditions continue to be major sources of utilization in the demand-side financing schemes. Considering that much of this utilization in these demand-side financing schemes happens in the private sector, it is inefficient as it leads to double allocation for meeting the same demand. Moreover, this also points to a possible gaming by providers [ 75 , 76 ], where dual practice could possibly result in siphoning off of public sector demand to private sector for provisioning under these schemes.
Contradicting findings in terms of increase in utilization and lack of significant improvement in financial risk protection needs careful examination. This could be explained based on several possible reasons, Firstly, the height of benefit package under existing schemes such as RSBY is inadequate. With a cover of INR 30,000 per year per household, several high cost illnesses leave the individuals at risk of impoverishment. Secondly, the depth of coverage could possibly be inadequate. RSBY and other state health insurance schemes primarily cover the services requiring hospitalization, while nearly 70% of overall health expenditure is on account of outpatient care which is not covered. [ 77 ] So, even enrolled households continue to pay for outpatient care. Thirdly, there is a possibility that even the private empanelled hospitals are charging the patients who pay the same out-of-pocket. [ 40 ] Finally, and importantly, it is possible that the bulk of private empanelled providers which exist in the urban areas remain elusive to the vast rural population which continues to face geographic barriers to accessing care. [ 78 ] This possibility is also substantiated by the finding that the benefits are mostly gained by the richer quintiles and urban population. In view of limitations of existing evidence, a conclusive statement will require further research which examines these possible explanations. Important policy inferences emerge from the latter point–firstly, that no such demand-side health financing scheme can succeed in providing financial risk protection in the absence of a strong primary health infrastructure. Secondly, this primary health infrastructure needs to be equitably distributed and utilized. Finally, since the rural and disadvantaged areas have not seen the growth of private sector, there is significant merit in the role of investing to strengthen public sector infrastructure.
An important finding from the process evaluation reports is the inequitable nature of the enrolment and utilization. This point towards inefficient targeting towards those who need the services most. Several reasons could be considered to explain this finding. Firstly, insurance companies have an incentive to enrol less than the maximum number of 5 household members, because the premium payment is linked to the number of households enrolled, rather than members. Moreover, villages with higher proportion of BPL population have poorer enrolment. This could be a result of systematic attempt to enrol the better-offs rather than worse offs. Average family size reported in India is 4.8. However studies from the review shows average family size of households under RSBY in the range of 1.46–3.77. [ 27 , 29 , 48 , 50 ]. This points to the need for comparing the characteristics of family member enrolled in RSBY against those who are left out. This would help ascertain whether there is any cream skimming by insurance companies. Secondly, it could be seen that in more backward villages, due to paucity of means, poorer households are not able to get a BPL card. And since the means test to identify a poor household is the BPL card, hence the very poor are unable to enrol in the scheme. [ 42 , 47 ] This in turn could lead to poor targeting under the scheme as most needy and poor are unable to obtain BPL card. Another reason which could contribute to poor enrolment among the poorest could be low level of awareness regarding the means to get an insurance card. This also correlates with the finding of low awareness about publicly sponsored health insurance schemes among the target population. [ 26 , 29 , 38 , 43 , 53 ]
We would like to acknowledge that impact evaluation was the primary objective of the present paper, and as a result we might have missed out on some studies which were purely describing the processes. Secondly, we are also likely to miss qualitative narrative of the implementation of these insurance programs, and which do provide important insights. This also explains our reporting of impact assessment results first, followed by process evaluation. However, it is also important to understand that the process evaluations in literature are not as standardized as the impact evaluations, which makes it difficult to systematically report. Not every process evaluation reported findings on the same set of indicators. This is an important gap in literature and needs to be bridged in future studies.
Given the current policy directions for universal health care, publicly financed health insurance schemes are likely to stay. Hence there is a need to design the schemes and implement safeguards so that the benefits of the risk pooling can be maximized. Firstly, benefits of these demand-side financing mechanisms will be not reaped unless the basic health care infrastructure for delivery of primary health services is strong. This primary health care infrastructure will be necessary to provide basic health services, besides serving as gatekeeping for specialist services. Examples from Thailand, United Kingdom and Mexico substantiate this claim. [ 79 ] Secondly, the public sector needs to be strengthened and incentivized to compete for provision of services. This will generate much needed extra revenue for the public health system, which can in turn be used to strengthen provision of health services. The public sector has demonstrated that it can provide universal access for health care services, which are delivered efficiently and utilized equitably, the only condition being that enough resources are spent. Various interventions for improving access to maternal health care services and institutional delivery in public sector illustrates this point. [ 80 – 82 ] Thirdly, there is a need to invest in systems to monitor and evaluate implementation of health insurance schemes. This is also essential in view of large private sector presence, which has perverse incentives to induce demand; and the intermediary purchaser/ insurer, who has perverse incentive to reduce utilization through cream-skimming. Overall, publicly financed health insurance schemes are not the panacea to achieve UHC in India. Instead, these schemes need to be aligned with proper strengthening of the public sector for provision of comprehensive primary health care. Secondly, presence of health insurance schemes could be used as an opportunity to reform the tenets of the health sector which are beyond the routine regulatory frameworks.
Supporting Information
S1 table. prisma checklist..
https://doi.org/10.1371/journal.pone.0170996.s001
Acknowledgments
We are grateful to the assistance provided by the Mrs Neelima Chadha from the library of Post Graduate Institute of Medical Education and Research (PGIMER) Chandigarh.
Author Contributions
- Conceptualization: SP RK AK.
- Data curation: ASC GK.
- Formal analysis: ASC SP.
- Funding acquisition: AK SP.
- Methodology: SP RK.
- Validation: RK AK.
- Writing – original draft: ASC SP.
- Writing – review & editing: SP ASC AK GK RK.
- 1. World Health Organization. The world health report: health systems financing: the path to universal coverage. 2010.
- 2. Norheim O, Ottersen T, Berhane F, Chitah B, Cookson R, Daniels N, et al. Making fair choices on the path to universal health coverage: Final report of the WHO consultative group on equity and universal health coverage: World Health Organization; 2014.
- 3. Government of India, Ministry of Health and Family Welfare. NCMH: Report of the National Commission on Macroeconomics and Health. 2005.
- 4. Government of India, Ministry of Statistics and Programme Implementation. NSSO 71st Round (January—June 2014): Key Indicators of Social Consumption in India Health. 2015.
- View Article
- Google Scholar
- PubMed/NCBI
- 8. Government of India, Ministry of Health and Family Welfare. National Rural Health Mission (2005–2012) Mission Document.
- 9. Bang A, Chatterjee M, Dasgupta J, Garg A, Jain Y, Shiv Kumar AK, et al. High level expert group report on universal health coverage for India. New Delhi, Planning Commission of India. 2011.
- 10. Rajiv Aarogyasri Health Insurance Scheme. [Internet]. [cited 2016 17 Feb]. Available from: http://www.aarogyasri.telangana.gov.in/ .
- 11. Rajiv Gandhi Jeevandayee Arogya Yojana [Internet]. [cited 2016 17 Feb]. Available from: https://www.jeevandayee.gov.in/ .
- 12. Chief Minister’s Comprehensive Health Insurance scheme [Internet]. [cited 2016 17 Feb]. Available from: http://www.cmchistn.com/ .
- 13. Rashtriya Swasthya Bima Yojana [cited 2015 20 November]. Available from: http://www.rsby.gov.in/ .
- 14. Press Information Bureau, Government of India, Ministry of Labour & Employment. Health and Family Welfare Ministry to Implement RSBY Scheme from Tomorrow. 2015.
- 15. Ministry of Health and Family Welfare, Directorate General of Health Services, Central Bureau of Health Intellegence. National Health Profile, 2015.
- 17. Universal Health Coverage Project to Revolutionize Health Care Delivery System in Punjab. Directorate of Information and Public Relations, Punjab; 2015.
- 18. Government of Himachal Pradesh, Department of Health and Family Welfare. Order No.: 13454-4676/2014. 2014.
- 19. Escobar ML, Griffin CC, Shaw RP. The impact of health insurance in low-and middle-income countries: Brookings Institution Press; 2011.
- 20. Acharya A, Vellakkal S, Taylor F, Masset E, Satija A, Burke M, et al. Impact of National Health Insurance for the Poor and Informal Sector in Low-and Middle-income Countries: EPPI-Centre; 2012.
- 22. National Collaborating Centre for Methods and Tools. Quality Assessment Tool forQuantitative Studies Method. Hamilton, ON: McMaster University. (Updated 13 April, 2010). [Internet]. 2008 [cited 2015 12 Nov]. Available from: http://www.nccmt.ca/registry/view/eng/15.html .
- 23. Asian Development Bank. A Review of Recent Developments in Impact Evaluation. 2011. [cited 2016 April 25]. Available from: http://www.adb.org/sites/default/files/publication/28622/developments-impact-evaluation.pdf .
- 26. Aiyar A, Sharma V, Narayanan K, Jain N, Bhat P, Mahendiran S, et al. Rashtriya Swasthya Bima Yojana (A study in Karnataka). 2013.
- 27. The Research Institute Rajagiri College of Social Sciences Kochi, Kerala. RSBY–CHIS Evaluation Survey (Facility Level Survey to Assess Quality of Hospitals in RSBY Network & Post Utilization Survey of RSBY Patient Experience at Empanelled Hospitals in Kerala).
- 28. GIZ. Evaluation of Implementation Process of Rashtriya Swasthya Bima Yojana in Select Districts of Bihar, Uttarakhand and Karnataka. 2012.
- 29. Amicus Advisory Private Limited. Rashtriya Swasthya Bima Yojana: Studying Jaunpur (Uttar Pradesh).
- 30. Bergkvist S, Wagstaff A, Katyal A, Singh P, Samarth A, Rao M. What a difference a state makes: health reform in Andhra Pradesh. World Bank Policy Research Working Paper. 2014(6883).
- 31. Dhanaraj S. Health shocks and coping strategies: State health insurance scheme of Andhra Pradesh, India. WIDER Working Paper, 2014.
- 35. Philip NE, Kannan S, Sarma SP. Utilization of comprehensive health insurance scheme, Kerala: a comparative study of insured and uninsured BPL households. BMC Proceedings; 2012: BioMed Central Ltd.
- 37. Ghosh S. Publicly-Financed Health Insurance for the Poor Understanding RSBY in Maharashtra. 2014.
- 38. Patel J, Shah J, Agarwal M, Kedia G. Post utilization survey of RSBY beneficiaries in civil hospital, Ahmedabad: A cross sectional study. 2013.
- 43. Amicus Advisory Pvt. Ltd. Evaluation Study of Rashtriya Swasthya Bima Yojana in Shimla & Kangra Districts in Himachal Pradesh.
- 44. Mott MacDonald. Ministry of Labour & Employment. Pilot Post-enrolment Survey of the RSBY Programme in Gujarat, March 2011.
- 48. Hou X, Palacios R. Hospitalization patterns in RSBY: preliminary evidence from the MIS. 2011.
- 49. Krishnaswamy K, Ruchismita R. Performance trends and policy recommendations: an evaluation of the mass health insurance scheme of Government of India. Chennai: Centre for Insurance and Risk Management. 2011.
- 50. Sun C. An analysis of RSBY enrolment patterns: Preliminary evidence and lessons from the early experience. RSBY Working Paper, 2010.
- 51. Shoree S, Ruchismita R, Desai KR. Evaluation of RSBY’s Key performance indicators: A biennial study. Geneva: International Labour Office.
- 53. Thakur H, Ghosh S. Social Exclusion and Rashtriya Swasthya Bima Yojana (RSBY) in Maharashtra. 2013.
- 56. Kilaru A, Saligram P, Giske A, Nagavarapu S. State insurance schemes in Karnataka and users’ experiences–Issues and concerns.
- 62. Arora D. Towards alternative health financing: the experience of RSBY in Kerala. 2010.
- 63. Council for Tribal and Rural Development (CTRD). Final report on evaluation of "Rashtriya Swasthiya Bima Yojana" in Chhattisgarh. 2012.
- 64. Chaupal Gramin Vikas Prashikshan Evum Shodh Sansthan (Chaupal). (2013b). Study on status of Public Health Services at various levels in Chhattisgarh. Unpublished.
- 65. Chaupal Gramin Vikas Prashikshan Evum Shodh Sansthan (Chaupal). (2013a). Study on patient experiences in availing RSBY in private hospitals in Chhattisgarh. Unpublished.
- 66. Mott MacDonald. Pilot Post-enrolment Survey of the RSBY Programme in Haryana, March 2011. Ministry of Labour & Employment
- 67. Rashtriya Swasthiya Bima Yojana. RSBY Connect Issue No. 20. 2013.
- 68. Mor N. The Best Way to Address Maternal and Child Health (MCH) Is Not to Build an MCH Focussed Health System. Available at SSRN 2648846. 2015.
- 70. Bajpai V. The challenges confronting public hospitals in india, their origins, and possible solutions. Advances in Public Health. 2014.
- 74. Government of India, Ministry of Health and Family Welfare. Framework for Implementation of National Health Mission, 2012–2017. [cited 2016 April 27]. Available from: http://nrhm.gov.in/images/pdf/NHM/NRH_Framework_for_Implementation__08-01-2014_.pdf .
- 76. Berman P, Cuizon D. Multiple public-private jobholding of health care providers in developing countries. An exploration of theory and evidence Issue paper-private sector London: Department for International Developmnent Health Systems Resource Centre Publication. 2004.
- 77. Government of India, Ministry of Health and Family Welfare. National Health Policy 2015 draft. [cited 2016 April 27]. Available from: http://www.mohfw.nic.in/showfile.php?lid=3014 .
- 82. Prinja S, Gupta R, Bahuguna P, Sharma A, Aggarwal AK, Phogat A, et al. A Composite Indicator to Measure Universal Health Care Coverage in India: Way Forward for Post-2015 Health System Performance Monitoring Framework. Health Policy Plannning. 2016: pii: czw097. [Epub ahead of print].
Health Insurance in India Opportunities, Challenges and Concerns
- January 2000
- In book: Indian Insurance Industry: Transition and Prospects
- Publisher: New Century Publications, New Delhi
- Editors: Srivastava D C and Srivastava S (eds

- Public Health Foundation of India

- Narsee Monjee Institute of Management Studies
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Saloni Devi

- Papai Barman
- Ranjan Karmakar

- Amrik Singh

- Harinder Singh
- Pavithra Rajan

- Harneet Kaur
- Saurabh Sharma
- Suruchi Sharma
- Yuti Rohit Chandan
- Dr Waghmare

- A. Sai Bhavana
- P. L. Srinivasa Murthy
- Econ Polit Wkly

- Michael Kent Ranson
- U E Reinhardt
- D C Srivastava
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Research article
- Open access
- Published: 07 September 2020
Effect of health insurance program for the poor on out-of-pocket inpatient care cost in India: evidence from a nationally representative cross-sectional survey
- Shyamkumar Sriram ORCID: orcid.org/0000-0003-4906-1405 1 &
- M. Mahmud Khan 1
BMC Health Services Research volume 20 , Article number: 839 ( 2020 ) Cite this article
19k Accesses
66 Citations
6 Altmetric
Metrics details
In India, Out-of-pocket expenses accounts for about 62.6% of total health expenditure - one of the highest in the world. Lack of health insurance coverage and inadequate coverage are important reasons for high out-of-pocket health expenditures. There are many Public Health Insurance Programs offered by the Government that cover the cost of hospitalization for the people below poverty line (BPL), but their coverage is still not complete. The objective of this research is to examine the effect of Public Health Insurance Programs for the Poor on hospitalizations and inpatient Out-of-Pocket costs.
Data from the recent national survey by the National Sample Survey Organization, Social Consumption in Health 2014 are used. Propensity score matching was used to identify comparable non-enrolled individuals for individuals enrolled in health insurance programs. Binary logistic regression model, Tobit model, and a Two-part model were used to study the effects of enrolment under Public Health Insurance Programs for the Poor on the incidence of hospitalizations, length of hospitalization, and Out-of- Pocket payments for inpatient care.
There were 64,270 BPL people in the sample. Individuals enrolled in health insurance for the poor have 1.21 higher odds of incidence of hospitalization compared to matched poor individuals without the health insurance coverage. Enrollment under the poor people health insurance program did not have any effect on length of hospitalization and inpatient Out-of-Pocket health expenditures. Logistic regression model showed that chronic illness, household size, and age of the individual had significant effects on hospitalization incidence. Tobit model results showed that individuals who had chronic illnesses and belonging to other backward social group had significant effects on hospital length of stay. Tobit model showed that days of hospital stay, education and age of patient, using a private hospital for treatment, admission in a paying ward, and having some specific comorbidities had significant positive effect on out-of-pocket costs.
Conclusions
Enrolment in the public health insurance programs for the poor increased the utilization of inpatient health care. Health insurance coverage should be expanded to cover outpatient services to discourage overutilization of inpatient services. To reduce out-of-pocket costs, insurance needs to cover all family members rather than restricting coverage to a specific maximum defined.
Peer Review reports
Achieving Universal Health Coverage (UHC) is an important goal for almost every nation in the world [ 1 ]. Financial risk protection is one aspect or dimension of UHC and providing financial risk protection is a specific target of the Sustainable Development Goals (SDGs) of the United Nations [ 2 ]. The level of financial protection realized by different population groups depends on the out-of-pocket expenditures (OOP) incurred by them for financing health care [ 3 , 4 ]. High OOP health expenditures, by definition, happens when households decide to access and utilize health care services but do not have protection against high expenditures due to high medical care costs and/or lack of access to insurance coverage and other safeguards against out of pocket costs [ 5 ]. Evidence from Indian National Health Account 2017 shows that OOP health expenditures for inpatient care constitutes around 32% of the total OOP health expenditures, despite the coverage offered by various health insurance programs [ 6 ]. The public healthcare system in India, with geographically distributed primary health centers and sub-centers, is very weak and lacks basic infrastructure. In addition, waiting times in the public sector primary health care facilities are very long, encouraging most of the patients to choose private providers for their health care needs [ 7 , 8 , 9 ]. Increasing propensity to use private sector health care providers increases the costs and lack of health insurance coverage and inadequate coverage make the OOP expenditure high with negative impacts on health care utilization [ 10 ]. Since cost of inpatient services is high, protecting households from hospital OOP expenses should significantly improve financial equity in health service delivery. Moreover, access to health care can be improved significantly if the system can protect the poor households from significant OOP expenses. In order to improve access to health care by the poor, India initiated a number of health insurance programs since 2008 [ 10 ]. This paper advances our knowledge about financial risk protection and effect of health insurance programs for the poor on access, utilization and out-of-pocket expenses in India.
The increase in health insurance coverage may lead to increase in health care utilization because of the change in behavior of the insured as well as the health care provider. A study by Anderson et al. (2012) in the USA found that there was a 61% reduction in inpatient hospital admissions and 40% reduction in emergency department visits among the uninsured population compared to insured population with similar sociodemographic characteristics [ 11 ]. Evidence from literature has shown that increased health insurance coverage leads to increase in utilization of health services, but the effect of health insurance coverage on financial risk protection is less clear, especially for poor beneficiaries [ 12 ]. This is because, there are two opposing forces in play due to increased coverage of insurance; one aspect is the increased access and utilization due to insurance coverage, which increases total health care cost and second, even with lower OOP rates per service, total OOP may actually become higher due to higher utilization. The health insurance for the poor in India covers only inpatient services. This creates an incentive for the patients to visit hospitals and get hospitalized, instead of using basic primary health care services. Studies on hospitalization trends in India showed that an annual hospitalization rate increased from 16.6 per 1000 population to 37.0 per 1000 from 1995 to 2014 [ 13 ]. Although, we expect to see an increase in hospital utilization rate with improving access and availability, a part of this increase may be due to hospital insurance offered to the poor by the Government of India.
There are many Public Health Insurance Programs for the Poor offered by the Government of India (GOI) and some states to cover the cost of hospitalization and inpatient care [ 14 ]. RSBY is a health insurance program started by the Ministry of Labor and Employment of the GOI in April 2008 and it provides a wide range of hospital-based healthcare services to Below Poverty Line (BPL) families [ 15 ]. There are a number of state-run public health insurance programs for the poor in three of the southern states in India which provide higher coverage than RSBY and are exempted from the national program. The programs are the Chief Minister’s Comprehensive Health Insurance Scheme in Tamil Nadu State, Rajiv Aarogyasri Community Health Insurance (RACHI) in Andhra Pradesh State, and Vajpayee Aarogyasri Scheme (VAS) in Karnataka State [ 14 ]. Table 1 summarizes the important features of the national RSBY program and the state health insurance programs for the poor in the states of Andhra Pradesh, Karnataka, and Tamil Nadu.
Around 41 million families are enrolled in RSBY, covering around 150 million poor people as of September 2016. The enrolment under the program has been increasing starting from only 55 districts in 2008–2009. Nationally, around 460 districts participate in the program, with 57% of the eligible households are currently enrolled [ 16 ]. There is significant inter-district and inter-state variation in the percentage of eligible households enrolled in RSBY. Across states, the degree of enrolment of households varies from a low of 24% in Arunachal Pradesh and 36% in Haryana to more than 75% in Kerala. The degree of enrollment of households by district varies significantly across the country, with a low rate of enrollment of 3% in Kannauj district and 6% in Kanpur district in the Uttar Pradesh state to a high enrollment rate of 90% of households in most of districts in the Chhattisgarh and Kerala states of India. Enrolment is not complete in many states, even a decade after the start of the program. Also, as of September 2016, the state of Rajasthan was still in its early stage for enrolling households in RSBY [ 16 ]. This shows that enrollment in the RSBY program has been slow in some parts of India. Not all states in India participate in RSBY. The state of Andhra Pradesh has not adopted RSBY as it already has a substantially more generous state level health insurance program than RSBY which pre-dates RSBY with relatively high population coverage, covering nearly 80% of its population [ 17 ]. Studies show that coverage rate of RSBY is low with half of the poor individuals not covered because of problems with targeting due to incomplete information on poor individuals and households, high migration rates among the poor [ 16 ] and possibly the rapid changes in social mobility.
Under the Public Health Insurance Programs for the poor only the hospitalization services and expenses associated with inpatient care are covered. It is expected that the health insurance for the poor will increase utilization of hospital services by the BPL households who would usually be forced to postpone their non-urgent procedures for a later time because of cost. Even with insurance, there may be OOP payments for drugs, tests and post-treatment care which are not covered by the health insurance. Therefore, hospital insurance may actually end-up increasing the OOP payments for inpatient and inpatient-related care for the poor. Hence the direction of effect of the Poor People Health Insurance Programs on total inpatient OOP health expenditure is unclear. Also, RSBY may lead to misuse of services, since both the physician and the patient have the incentive to convert an outpatient case into an inpatient admission, leading to unnecessary utilization [ 18 ]. The objective of this research is to examine the effect of Public Health Insurance Programs for the Poor on incidence of hospitalizations and inpatient OOP health expenditures.
Many studies show that people incur high OOP health expenditures despite being covered by the national health insurance program RSBY or other state health insurance programs [ 19 , 20 , 21 , 22 , 23 , 24 ]. However, studies on state health insurance programs in Karnataka and Andhra Pradesh showed that OOP health expenditures significantly declined with health insurance coverage [ 17 , 25 , 26 ]. Cross-sectional studies done in Tamil Nadu and Maharashtra show that the utilization of healthcare was significantly higher among the insured compared to the uninsured population [ 27 ].
Previous studies on Poor People’s Health Insurance Programs such as RSBY dealt with issues related to program enrolment [ 28 ], barriers in implementation of the program [ 22 ], effect of information campaign [ 29 ], hospitalization patterns [ 30 ], and determinants of participation in the program [ 31 ]. There are only two district level studies on RSBY, one done in Amaravati district in Maharashtra [ 32 ] and the other in Gujarat [ 19 ], that showed increased hospitalizations and higher OOP health expenditures among the RSBY insured individuals. The study in Gujarat found that RSBY enrollees experienced higher OOP health expenditures because they had to pay for medicines and diagnostics during the hospital admission [ 25 ]. In contrast, another state level study for the Aarogyasri program found that insurance significantly reduced the OOP health expenditures for hospitalizations [ 17 ]. Most of other studies that studied the effect of health insurance on hospitalizations and OOP health expenditures were community-based health insurance programs in different parts of the country [ 25 , 33 , 34 , 35 ] and thus limiting its usefulness for national decision-making.
This study is a considerable improvement over other studies on Public Health Insurance Programs for the Poor in India on two important counts: i) the study uses nationally representative dataset which helps in estimating pan-India effects of Public Health Insurance Programs for the Poor ii) the study evaluates the effect of Public Health Insurance Programs for the Poor by comparing outcomes between poor people enrolled and not-enrolled in the insurance program. Many studies are based on RSBY enrollees alone and do not have any controls making it difficult to identify the effects of the Public Health Insurance Programs for the Poor. This study identified comparable control population from among those who are poor but were not enrolled in the insurance program. The specific research questions that will be addressed in this research are: (i) How do hospitalizations differ between the enrolled and not-enrolled groups under Public Health Insurance Programs for the Poor? and (ii) How does OOP health expenditure for inpatient care differ among people enrolled and not-enrolled under Public Health Insurance Programs for the Poor?
Data source
The data from the National Sample Survey Organization (NSSO) of the GOI were used for the study [ 36 ]. The NSSO is a national organization under the Ministry of Statistics and Implementation which was established in 1950 to regularly conduct surveys and provide useful statistics in the field of socio-economic status of households, demography, health, industries, agriculture, consumer expenditure etc. The specific data set from NSSO that was used in this study is the Social Consumption (Health), NSS 71st Round for 2014, which is the latest nationwide data available for India. The survey covered whole of the Indian Union. The survey used the interview method of data collection from a sample of 65,932 randomly selected households (36,480 in rural India and 29,452 in urban India) and 335,499 individuals, covering the members of the household in all the 36 states (including union territories). The data for the survey were collected over a period of six months, from January to June 2014. The NSSO Social Consumption (Health) collected data on demographic characters, employment, health conditions, source of payments, health insurance coverage, type of coverage, costs of various inpatient services, level of care, type of care and a number of other variables. The survey also collected information on medical care received at inpatient and outpatient facilities of medical institutions including health expenditures for various episodes of illness. This is the first NSSO health survey that collected data on utilization of alternative medicines. The details of hospitalization for all current and former members of the household were collected for the last 365 days (hospitalization occurred from January 2013 to June 2014) and the details of outpatient services were collected for the last 15 days.
Estimation of OOP health expenditures
‘Total Out-of-Pocket health expenditures for inpatient care’ is defined as the total health expenditure for inpatient care net of reimbursement by health insurance. It is a continuous variable calculated in Indian Rupees (INR). In the data provided by the government of India, hospitalization expenses were included under two heads namely medical (direct) and direct non-medical (indirect) costs. Direct medical expenditure consists of package component and non-package component (doctor fee, medicines, diagnostic tests, bed charges, other medical expenses) and direct non-medical expenditure consists of transport for patient, transport for others, lodging charges of escort, food expenses, and other expenses. There is a separate variable in the data which provided the “amount reimbursed by the health insurance”. All these variables were used to derive the OOP health expenditure for inpatient care.
Total inpatient healthcare expenditure = (Medical expenditure, X) + (Direct Non-Medical.
Expenditure, Y).
Total out-of-pocket inpatient health expenditure = (Total inpatient healthcare expenditure) –.
(Amount reimbursed by the health insurance, Z)
Empirical methodology
The main objective of this study is to estimate the effect of Public Health Insurance Programs for the Poor on hospitalizations and OOP inpatient care costs. The effects of the program were estimated by comparing the probability of hospitalizations and OOP inpatient healthcare costs between the groups who are eligible (poor) and covered by the insurance programs and who are eligible (poor) but not covered. In theory, the best approach of estimating the impact of a program is to adopt a Difference-in-difference (DID) framework with randomized allocation of eligible individuals in the program group and the no-program group. The framework requires data on the two groups in the pre-intervention period and then in the post-intervention period [ 37 ]. DID estimators compare the change in mean outcomes before and after the intervention among individuals who acquire coverage (treated) and those remaining not exposed.
To estimate the causal effect using DID, the assumptions of DID must be satisfied. The main assumptions are that the treatment and control groups have parallel trends in outcome, the composition of the treatment and control groups are stable for repeated cross-sectional design, the allocation of treatment is unrelated to the outcome at baseline, and there are no spillover effects. The most important assumption for DID is the ‘parallel trend assumption’. This means that in the absence of the intervention/treatment, the average difference in the outcome between the treatment and control groups would have remained constant in post-intervention time period as in pre-intervention period. The violation of this assumption will imply that the DID approach will not be able to obtain unbiased estimates of program impacts. The DID model cannot be used if composition of the pre-intervention and post-intervention groups are not stable, if the comparison group has a different outcome trend, and if the allocation of the treatment/intervention is determined by the baseline outcome [ 37 ].
However, the treated and untreated may differ in the distribution of both observable and unobservable characteristics. Heckman and Vytlacil (2007) highlighted that unobservable variables may play a bigger (or smaller) role in influencing the with-treatment outcome than the without-treatment outcome [ 38 ]. Inability to control for them is likely to provide under (over) estimation of the effects of the programs. Since the main assumption of DID is parallel trend assumption and checking for the constant difference in outcome over time is necessary for deriving impact of a program or intervention using DID approach.
For the purpose of this study, a number of simplifying assumptions must be made as the data set is cross-sectional in nature and we only observe the outcomes in the year the data were collected. Therefore, the data set does not provide any information on the individuals who were enrolled in the insurance program in the previous period and those who were not enrolled. The insurance program is designed for the poor households and since belonging to the poverty group is a dynamic event, a household in poverty in pre-insurance period may not necessarily be in poverty in the post-intervention period. Moreover, household in poverty in the current year (the year of data collection) may not have been in poverty in the previous period. Almost all programs also show some degree of mistargeting implying that some poor people may not be offered the insurance while some non-poors are offered the insurance benefit. These potential deviations from expected enrollment may affect the estimate of outcomes when a post-intervention year’s data are used.
In the DID model, the intervention effect will be the difference between the observed outcome in intervention group and the unobserved counterfactual outcome for intervention group as shown in Fig. 1 . It is possible to model the unobserved counterfactual outcome for intervention group in the post-intervention period in absence of the intervention if data on pre-intervention period are available. In the cross-sectional data of the study, we do not have information on the intervention and control groups in pre-intervention period and if intervention and control groups differed in terms of outcomes of interests, we have no way of correcting for this. The only alternative approach we can adopt is to select the comparison groups from the cross-sectional data in such a way that the likelihood of pre-intervention variability would be minimized.

Intervention Effect using Difference-in-Difference Method
Rather than identifying the economic status of individuals who were actually covered by insurance in the previous period, the implicit assumption we are using is complete absence of mistargeting or simply not allowing the mistargeted individuals to be in the analysis. It is also assumed the social mobility of poor households in India is relatively low and so the households belonging to poverty category in the current year (the year of the survey) were also poor in the previous few years. If the enrolment in the program by the poor is completely random, the unobserved characteristics will become increasingly similar between program participants and non-participants with increasing sample size. In the data set, the sample size of BPL individuals is quite large but, clearly, enrolment in programs are almost never purely random. For the insurance program in India, it is not clear how exactly the households were selected for enrollment, especially because so many of the poor households were not in the program. It appears that administrative listing of poor households rather than self-selection guided the enrolment. This process, to some extent, can reduce the variability between enrolled and non-enrolled poors in terms of both observable and unobservable variables. Although the observable differences can be controlled for, it is not possible to ensure minimization of unobserved differences between the groups. In the analysis, it is assumed that the factors other than insurance coverage that may cause differences between the intervention group and control group in terms of utilization of hospital services or out-of-pocket costs would be relatively low. If the intervention and control groups are matched using a list of observable characteristics, it further reduces the possibility of biased estimate or unequal starting points in terms of outcome variables. Thus, using the cross-sectional post-intervention data, the intervention effect will be the difference between the observed outcome in the intervention group and the observed outcome in the control group as shown in Fig. 2 .
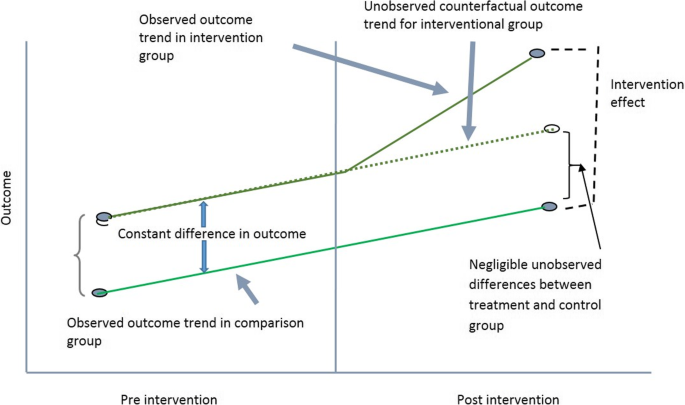
Intervention Effect using Cross-sectional data
Two important assumptions are made in the impact evaluation process when using this cross-sectional data. The assumptions are, at the starting point in the pre-intervention period, the unobservable differences between the intervention and control group are small, if any, and that both the intervention group and the matched control group would show similar trend in terms of outcomes in absence of the intervention.
Treatment group, control group and propensity score matching
The treatment group consist of all the poor people currently enrolled under the Public Health Insurance Programs for the Poor namely the RSBY and other state health insurance programs for the poor. The control group will consist of all people who are poor but not enrolled in the Public Health Insurance Programs for the Poor. In order to make both the groups comparable and to avoid selection bias, a propensity score matching was used to match the treatment and control groups. A propensity score is the conditional probability that a subject receives “treatment” given the subject’s observed covariates. A propensity score matched regression analysis incorporating survey weights can better account for selection bias based on observed variables than an unmatched regression [ 39 , 40 ]. The main goal of propensity score is to balance the observed covariates from the individuals in the treatment and control groups in order to imitate a randomized study [ 41 ]. The variables used to get the propensity scores were education, socioeconomic status, location of household (urban/rural), household size, and age of the individual, using a user-written command psmatch2 in STATA. After matching, a regression analysis was performed.
Data analysis
Incidence of hospitalization and length of hospital stay.
To study the effects of enrolment under Public Health Insurance Programs for the Poor on the incidence of hospitalizations after controlling for other factors, a binary logistic regression model was used. The logistic regression model is preferred since the dependent variable is dichotomous. “Whether the individual was hospitalized during the last 365 days?” was used as the dependent variable. A dichotomous variable for hospitalization was created with 0 for ‘not hospitalized during the last 365 days’ and 1 for ‘hospitalized during the last 365 days’. The independent variables include enrollment under the Poor People Health Insurance Program and other covariates. The model estimated the log odds of incidence of hospitalization adjusted for a set of explanatory variables. Individual is the unit of analysis. The results for the logistic regression are shown with the estimated regression coefficients, odds ratios and 95% confidence intervals. Tobit Regression Model was used to study the association between the Public Health Insurance Programs for the Poor and the length of stay in hospitals. The Tobit model is usually estimated when the dependent variable has a large number of observations clustered around a specific value, usually around zero. For the length of hospital stay, the dependent variable is either zero or higher than 0 [ 42 ]. Length of stay, by definition, is truncated below zero and thus the Tobit model is used.

OOP inpatient healthcare cost
Tobit Regression Model has also been used to study the association between Public Health Insurance Programs for the Poor and the OOP cost for inpatient care. Similar to length of stay, OOP cost is always positive or zero with a relatively high proportion showing zero OOP expenses.
The empirical equation for the Tobit model can be written as:
where \( {Y}_i^{\ast } \) is the latent dependent variable, and Y i is the observed values of the dependent variable.
Descriptive statistics
The total sample consisted of 336,470 individuals. In the total sample, 42,121 individuals were covered by the government sponsored health insurance programs such as Employee’s State Insurance Scheme (ESIS), Central Government Health Scheme (CGHS), and the poor people’s health insurance programs such as RSBY and other state health insurance programs. Poverty is a dynamic event where people move in and out of poverty. We used the poverty line for 2014 to identify individuals who were poor in 2014. Since the data had only one variable for the individuals covered by the government sponsored health insurance programs which included both the poor people health insurance programs and other government health insurance programs for the non-poor, we assumed that the people who were below the poverty line and enrolled in the government sponsored health insurance programs are enrolled in the public health insurance programs for the poor such as RSBY, RACHI etc. Since eligibility in the insurance programs like RSBY was defined by poverty status alone, the poor individuals not enrolled in the program were clearly eligible but not covered. Only the poor people below the poverty line as of 2014 has been used for defining eligibility for the public insurance in this study.
Descriptive statistics for categorical variables are presented in Table 2 for the poor individuals in the sample. The survey collected data from 64,270 poor individuals. Only 9.55% of the poor individuals in India were enrolled in any type of public health insurance programs for the poor. About 9.41% of the poor individuals were enrolled in RSBY in all states of India excepting Tamil Nadu, Andhra Pradesh, and Karnataka. In Andhra Pradesh, 40% of the poor people were enrolled in RACHI, 5.7% were enrolled in VAS in Karnataka, and only 4.5% were enrolled in CCHIS in Tamil Nadu. Around 41.3% of the poor in the sample were illiterate; 80.6% belonged to Hindu religion; 85.1% were from the disadvantaged classes; 64.2% belonged to medium sized households (5 to 8 members). About 2.5% of the poor individuals were suffering from chronic illnesses.
Table 3 reports the descriptive statistics for some continuous variables. The mean age of the poor population in the sample was 25.3 years. In terms of incidence of hospitalizations, only 3.3% of the weighted sample reported at least one hospitalization in the previous one year. The overall average days of hospital stay per poor person was only 0.17 days implying that average length of stay per admission as well as the proportion of poor individuals hospitalized in a year are quite small in general. The annual OOP health expenditure for inpatient health care for the whole poor population was 269.26 INR with average of annual consumption expenditure of 8505.62 INR. Therefore, on the average, poor households spent about 3% of their total annual consumption expenditure to inpatient care.
Table 4 shows the descriptive statistics for the poor individuals who were hospitalized during the recall period. Since the same person can be hospitalized more than once in a year, the length of hospital stay does not represent length of stay per admission. The mean duration of hospital stay was about five days for the poor individuals hospitalized in the year. The weighted average age of hospitalized individuals was 30.9 years in 2014. For this group, yearly consumption expenditure was 8449 INR and the yearly inpatient OOP health expenditure was 8149 INR. We mentioned earlier that the poor individuals, on the average, paid OOP about 3% of their annual consumption expenditure on inpatient care but if we focus on those who were actually hospitalized during the year, more than 95% of their annual consumption expenditure was due to OOP expenses related to inpatient care. Clearly, inpatient OOP expenditure has remained very high for the poor individuals in India.
One to One propensity score matching was done using a STATA user-written command ( psmatch2 ) by incorporating education, socioeconomic status, location of household (urban/rural), household size, and age of the individual as the matching variables. The results are reported in Table 5 . Number of individuals in the intervention group, 5917 in total, were matched with 5917 in the control group. Thus, the total matched sample consisted of 11,834 observations. After matching, various empirical modelling were carried out using the total matched sample. Using the matched sample ensures that we are comparing similar poor individuals in both enrolled and non-enrolled groups.
Multivariate analysis
The logistic regression model results for the effects of poor people health insurance program on incidence of hospitalization are shown in Table 6 . People enrolled in poor people health insurance program have 1.23 higher odds of incidence of hospitalization compared to poor people without health insurance. Chronic illness, household size, and age of the individual show significant effects on incidence of hospitalization. Individuals with chronic illnesses have higher probability of hospitalization compared to individuals without any chronic conditions. All the age groups show higher probability of hospitalization compared to the reference age group of less than 18 years. Interestingly, individuals belonging to the medium and large size households had lower probability of incidence of hospitalization compared to individuals from small households. Social group, religion, urban/rural location, household type, marital status, education, number of hospital beds in the state were not significant in explaining variability in the incidence of hospitalizations. Fixed effects for state of residence of the individual was included in the model but no significant effects of the state of residence were found in the empirical analysis.
Table 7 presents the Tobit model results on the effect of poor people health insurance program on the duration or length of hospitalization. Being enrolled in health insurance for the poor had no significant effect on the duration of hospitalization. People who did not have chronic illnesses had significantly lower duration of hospitalization compared to people with chronic illnesses. People belonging to “other backward classes” category had significantly higher duration of hospitalization compared to the reference group (scheduled tribes). Other covariates such as household type, religion, age, urban/rural location, household size, marital status, education, and number of hospital beds had no significant effect on the duration of hospitalization. Fixed effects for the state of residence of the individual was used in the model with Rajasthan, Uttar Pradesh, and Gujarat were the only three state showing significant results.
Results of the tobit regression model on the effects of poor people health insurance program on inpatient out-of-pocket health expenditures are shown in Table 8 . Enrollment under the poor people health insurance program did not have any effect on inpatient OOP health expenditures. Duration of stay in hospital, graduate level education, age groups of 19 to 60 years, using a private hospital for treatment, admission in paying ward (general and special), and having ailments such as cancers, blood, endocrine, metabolic, eye, ear diseases, cardiovascular, respiratory diseases, skin, musculoskeletal, psychiatric, neurological diseases, and injuries had significant positive effect on the OOP health expenditures experienced by the individual. Utilization of AYUSH type of treatment had significant negative effect on OOP health expenditures compared to individuals using allopathic treatment. Factors such as location, social group, household type, household size, and number of hospital beds in states had no statistically significant effect on OOP health expenditures. Gujarat and Kerala states show significantly lower OOP expenses, keeping all other factors contact, than other states of India in the state fixed effects model.
Discussions
Our study showed that poor people enrolled in the health insurance programs for the poor have higher incidence of hospitalization, but health insurance enrolment had no effect on the duration of hospitalizations. In general, health insurance coverage increases health care utilization because of higher access to care and changes in utilization behavior of both the insured and the health care provider. The results of our study are consistent with findings from other cross-sectional studies in Tamil Nadu and Maharashtra [ 27 ] which found significantly higher utilization of health care among the insured compared to the uninsured. Evidence from the US also indicates 61% reduction in inpatient hospital admissions and 40% reduction in emergency department visits among the uninsured compared to the insured population [ 11 ]. Lack of health insurance coverage usually forces people to delay or postpone medical care even when the medical care needed is of emergency type. With health insurance coverage, people can access health care with potentially lower financial risk. Currently, the health insurance for the poor people in India covers only inpatient services, which encourages patients to visit hospitals and get hospitalized instead of using basic primary health care services. Also, it creates a financial incentive for the provider to admit poor patients in the hospitals. Studies on hospitalization trends in India showed that annual hospitalization rate has increased from 16.6 to 37.0 per 1000 population from 1995 to 2014 [ 13 ]. Health insurance coverage affects total OOP expenses through two separate mechanisms – lower OOP expenses per unit of service and increased utilization of health services. Therefore, insurance coverage may or may not improve financial risk protection depending upon the degree of out-of-pocket price reduction of services and the change in the utilization levels [ 12 ].
Our study shows that incidence of chronic illnesses increases both the probability and the duration of hospitalizations. The findings are consistent with other results in the literature which show chronic diseases are important determinants of hospitalizations [ 43 ]. Since the health insurance programs for the poor do not cover outpatient services, people do not get preventive services or outpatient treatment for their illnesses during the initial stages of the diseases to better manage the disease progression and development of more severe chronic conditions. Although, public primary health care facilities provide free outpatient and preventive services, many poor individuals still face significant access barriers. In India, only 37% of the population in the rural areas have access to health care services within a 5-km radius and only 68% of the population have access to a basic outpatient health facility [ 44 ]. Further, India is facing demographic transition with increasing proportion of population in the higher age groups and epidemiological transition with increasing burden of non-communicable and chronic diseases [ 45 ]. In this study, we find that the incidence of hospitalization among poor people tends to increase with age. Elderly people over 80 years of age showed the highest incidence of hospitalization. These findings are consistent with another study in India that showed age of the individual as an important predictor of hospitalization [ 46 ]. Hospital readmissions [ 47 ] and increase in the number of comorbidities in an individual also increase with age [ 48 ]. Women in the age group of 19 to 40 years have higher incidence of hospitalization, which is an expected result for women in the reproductive age group [ 49 , 50 ].
Our results show that medium and larger households have lower probability of hospitalization compared to smaller households. The odds of hospitalization for medium households is 0.77 and for the large households is 0.48. One of the probable reasons may be that larger households can arrange someone within the family to act as a caregiver in the case of illness or disability. This family caregiving may prevent hospitalization for many common conditions. It is also possible that larger household sizes are more averse to the likelihood of incurring high OOP expenses associated with hospitalizations. Evidence from US have shown that home health provision has reduced both the number of visits and duration of stay in the hospital [ 51 ]. Another reason may be related to the design of the health insurance program itself. Poor people health insurance programs in India cover hospitalization costs only for a limited number of household members. For example, health insurance programs such as RSBY and VAS in Karnataka are limited to a maximum of five members in the household, but some of the state health insurance programs in Andhra Pradesh and Tamil Nadu cover the whole family [ 14 , 16 , 17 ]. The RSBY program has a benefit ceiling of INR 30,000 and some of the state health insurance programs have much higher coverage limits, e.g., up to INR 200,000 in Andhra Pradesh [ 14 ]. These enrolment restrictions and relatively low maximum threshold adversely affect the households with higher number of members reducing their healthcare utilization and hospitalization.
People belonging to the scheduled tribe social group category had significantly lower duration of hospitalization compared to the other backward classes (reference group). Scheduled tribes have poor access to healthcare facilities since they usually live in areas with limited access to health care facilities [ 52 ]. This may explain their lower duration of hospitalizations. People belonging to the other disadvantaged groups including the backward classes and scheduled classes live in the cities or villages that are not as inaccessible as the tribal areas where the scheduled tribal people live. Thus, the access to the healthcare facilities and coverage by health insurance programs were significantly better for the other disadvantaged groups than the tribal population.
Our study showed that coverage under the public health insurance programs for the poor had no significant effect on OOP health expenditures for inpatient care. This is contradictory to the studies done in Andhra Pradesh [ 17 , 20 ] and Karnataka [ 26 ] where significant reductions in OOP hospital expenditure were found with enrollment in the health insurance programs. However, other studies in Tamil Nadu and Andhra Pradesh [ 24 ] showed that households with health insurance coverage had higher OOP health expenditures. At the national level, another study by Karan et al. (2017) showed that the likelihood of incurring OOP health expenditures increased by 30% due to RSBY program and that RSBY has not been effective in reducing the burden of OOP health expenditures for poor households [ 16 ]. Despite the higher OOP expenses, the wellbeing of the poor improved due to the program. The evidence on OOP expenses is also mixed internationally with studies from Indonesia and Laos showing reductions in OOP health expenses for insurance coverage [ 53 ] but Vietnam study did not find any effect of health insurance program on OOP health expenditures [ 54 ]. We find that the OOP health expenditures increases with higher duration of hospital stay. A report from the World Bank in India [ 55 ] and a study based on low and middle income countries [ 56 ] showed that OOP expenses increases with increasing hospitalizations.
India has a pluralistic system of medical culture with a number of different types of alternative medical systems (apart from the allopathic systems of medicine) widely practiced and used [ 57 ]. The alternative systems of medicine (AYUSH) training programs are officially regulated by the government of India but there are many practicing healers in the country who have no formal training or qualifications. In our study, we found that the individuals who reported using AYUSH for their treatment incurred a lower OOP health expenditures compared to others who did not use AYUSH. This finding is not consistent with the results found for Tanzania [ 49 ] and Sri Lanka [ 58 ] where the utilization of traditional systems increased the OOP health expenditures. The reason may be that in India, the people who use AYUSH may be poorer and/or use it for medical conditions perceived to be not serious. In general, individuals with relatively complex medical conditions are more likely to use the modern or allopathic systems of medicine.
Our results showed that individuals who were admitted to private tertiary hospitals incurred higher OOP health expenditures compared to individuals admitted to public hospitals or primary health centers. A systematic review assessing OOP health expenditures across a number of countries found that the use of private healthcare facilities and inpatient admissions in private sector hospitals were associated with higher OOP health expenditures [ 59 ]. Evidence from Thailand also indicates higher OOP health expenditures for utilizing private hospitals [ 60 ]. The use of private sector hospitals for specific health services such as maternal health [ 61 , 62 ], chronic disease treatment [ 63 ] were also associated with higher OOP expenditures. The level of hospital care (i.e., primary, secondary, and tertiary care), as expected, also affect OOP costs with higher expenses at higher levels and the likelihood of expenditures being catastrophic becomes significantly higher for tertiary hospitals [ 63 ]. People who are getting admitted to a paying ward incur higher OOP expenses compared to those who are admitted to a free ward. Most of the public health facilities in India provide inpatient admission free or at a very subsidized cost. Poor patients who are admitted in the paying wards incur higher OOP costs because the health insurance coverage is quite limited and patients may associate free bed with poor quality. India has a wide network of unregulated private sector hospitals with around 49% of total available hospitals being in the private sector [ 64 ].
In India, compared to the OOP expenses associated with infectious diseases, all other conditions and diseases showed significantly higher OOP inpatient health expenditures. India is facing an epidemiological transition from infectious diseases to chronic and non-communicable diseases [ 65 ]. The higher incidence and duration of hospitalizations for chronic diseases appear to be associated with higher OOP costs. These results are consistent with studies from India and other countries that found positive association between OOP expenses and incidence of medical conditions like disabilities, injuries due to road traffic accidents, and chronic illnesses [ 60 , 66 , 67 , 68 , 69 , 70 , 71 ].
Poor people with a diploma/graduate/post graduate level of education showed higher OOP health expenditures compared to poor people who were illiterate. The results are consistent with the evidence from China which indicates that better educated individuals had higher OOP health expenditures [ 70 ]. Also, educational attainment had an effect on OOP costs for specific services. Studies in India [ 72 ] and Brazil [ 73 ] show that educated mothers reported higher OOP health expenditures. Our analysis shows that individuals in the age group 41 to 60 years had higher OOP health expenditures compared to those below 18 years. The odds of experiencing chronic diseases increase with age and chronic diseases are important determinants of hospitalizations and OOP costs. A number of studies showed that healthcare expenditures were significantly associated with age, and the effect of age on health expenditures was highest among the elderly [ 66 , 74 , 75 , 76 , 77 , 78 , 79 ]. In India, however, the highest age group (81 years or over) did not show the highest OOP expenses. It appears that society assigns more value to the health and wellbeing of individuals in the age groups 41 to 60 years and 19–40 years compared to other age groups. India does not have any specific health insurance or social security program for the elderly population and provision of such specialized programs will help improve the wellbeing of the elderly.
Limitations
The main limitations of this study arise from the use of secondary data. The contents and questions asked in the survey are not what an assessment of a program would have done to explore the specific research questions of this study. One of the most important concern is the lack of information on the coverage of public health insurance for the poor. The NSSO dataset includes a variable that indicates insurance coverage by all public health insurance schemes, i.e., all those covered by the government sponsored health insurance programs. Government sponsored health insurance schemes are many in India and includes Employee’s State Insurance Scheme (ESIS), Central Government Health Scheme (CGHS), and the poor people’s health insurance programs such as RSBY and other state health insurance programs. Clearly, government sponsored health insurance programs cover poor as well as non-poor households. Employees of the central and state governments are covered by government insurance and none of them are likely to be below the poverty line. It is also possible that many households covered by the insurance for the poor are not below the poverty line. Since the enrollment into the insurance for the poor happens infrequently, economic status of households may change from enrollment date to the date of the survey.
This research needed to identify the individuals and households who are covered by the government sponsored insurance for the poor. To identify the group covered by public insurance for the poor, a number of implicit assumptions were made: first, it is assumed that no insurance schemes of the government, other than the insurance program designed for the poor, covers the households or individuals below the poverty lines defined by the states. This conjecture is likely to be valid because governmental salary structure is such that almost no one covered by government employee health insurance program should be below the poverty line, irrespective of the size of the household. Second assumption is that all the poor individuals with insurance coverage must be enrolled in the public health insurance programs for the poor such as RSBY, RACHI etc.
These assumptions do not identify all the households and individuals covered under the government insurance schemes for the poor but identifies only those who are covered by the insurance scheme and are below the poverty line. The households that are below poverty line and not enrolled in the government sponsored health insurance programs are assumed to be the control group, i.e., the households that are eligible for participation in the health insurance program but were not enrolled. Poverty is a dynamic event where people move in and out of poverty and it is almost impossible for any program to be as dynamic as the underlying dynamics of social mobility. The households who were covered by the insurance for the poor at the time of the survey but were not below the poverty line can happen for two very different reasons. The first reason could be simple mis-targeting, i.e., the household should not be in the program based on the economic status of the household but were enrolled in the program. The second reason could be that the household belonged to the poverty category when the household got enrolled but the household graduated from poverty to above the poverty line during the intervening period. Since enrollment in the program and disenrollment from the program happens only infrequently, a certain percent of enrollees will be above the poverty line. Given the data we have, it is not possible to identify households who were covered by the insurance for the poor even though they were not poor.
In the empirical analysis, we have used the poverty line for 2014 to identify the individuals who were poor in 2014. Thus, our study focuses on the group who was below the poverty line and enrolled in any government health insurance program. Since the government health insurance scheme that covers individuals below the poverty line are the insurance schemes for the poor, it is likely that all those who are poor and covered by government health insurance are actually covered by the public health insurance for the poor. The implication of these implicit assumptions is that the study cannot conduct an assessment or evaluation of the insurance program for the poor. It is only assessing the differences in utilization and out-of-pocket expenses between the poor households and individuals covered by the public health insurance schemes for the poor and those not covered by the scheme. Therefore, it is not an assessment of the insurance program.
The cross-sectional nature of the data also creates another important limitation – the study can only observe the associations between health insurance coverage and other outcomes and no causal relationships can be determined. Thus, to understand the causal effect of the insurance programs on various outcomes, we need data over a number of years. Another limitation of the study is that the survey did not collect data from the floating population (people without any normal residence), but households residing in open spaces, roadside shelters and people who reside in the same place were listed. People residing in the protected residential areas of military, paramilitary, police areas and people in orphanages, rescue homes, etc., were not covered. The NSSO health survey data does not collect detailed consumption expenditure and the consumption expenditure in the NSSO survey does not differentiate between food and non-food expenditures. It should also be noted that all information is reported by the surveyed individuals in the households and some information required quite long recall time. Therefore, the data is prone to strategic, recall and other types of biases.
The first set of analysis of this study examined the hospital utilization pattern by health insurance status of poor individuals. There are two aspects of hospital utilization – incidence of hospitalization and duration of hospitalization. The incidence indicates the need and/or willingness to get admitted in a hospital. Decision to become hospitalized is often not made by the patients; in most cases, individuals follow the instructions of physicians and other health care providers. Some individuals, however, may decide not to seek care from hospitals due to other barriers faced even though the hospitalization may be considered medically necessary. Once the patients decide to get admitted in hospitals, the length of stay is most likely determined by the health care providers and hospital managers.
The empirical results imply that the poor individuals enrolled in health insurance program are more likely to get admitted in a hospital than those who are not covered by health insurance. Incidence of hospitalization is a reflection of access to inpatient hospital services and it is not surprising to find that having insurance increases the likelihood of hospitalization. Even though the regression models do not show causal relationship, in this case it probably indicates causal pathway. Enrollment in insurance happens before utilization of hospital services and there exists no mechanism of obtaining insurance coverage due to the need for hospitalization. Therefore, only reasonable implication of the result would be that having insurance for inpatient services increases the incidence of hospitalization among poor individuals in India.
The second aspect of hospital service use is the intensity of service utilization after the patients are admitted. The empirical model indicates that insurance status had no relationship on the level of utilization of hospital services, measured by the length of stay. Since the insurance status had no effect on duration of hospital stay, health care providers did not discriminate between insured and uninsured once they are admitted in the hospitals. Again, this is not surprising for a number of reasons. The coverage limits in the health insurance programs for the poor is low and the coverage limits did not create any incentive for increasing the duration of hospitalizations by the physician. The other reason may be that physicians are driven by the intrinsic motivation to provide better care for the patients, irrespective of their health insurance coverage or their capacity to pay. There is always the possibility that the clinicians are unaware of the insurance status of the patient, which are usually handled by the administrative divisions of the hospitals, and thus their clinical decisions are independent of any health insurance enrolment status.
Apart from the insurance status, a number of other factors affect hospitalization and hospital duration. Chronic illnesses increase both the incidence and duration of hospitalization. Early detection by preventive screenings and early treatment initiation will help in decreasing disease progression, and thus reduce preventable hospitalizations. This early detection and treatment initiation could be delivered through the PHC system. India has a wide network of PHCs and the PHCs should be upgraded adequately with diagnostic and treatment facilities to detect and treat chronic conditions to help reduce hospital rates, the duration of hospitalizations, and the associated higher OOP healthcare costs for inpatient care. Many chronic diseases can be treated effectively in the ambulatory setting. Thus, better approaches to manage the chronic diseases in the outpatient settings should be considered for improving effective utilization of scarce medical resources.
The study found lower incidence of hospitalization among the larger size households. The insurance for the poor may not cover all individuals in the household and in many states, enrollment is limited to only five members of the household and these five members must be selected at enrollment in the program. Therefore, for large households, a number of members may not be covered by the program even though the household is enrolled in the insurance plan. Lack of insurance coverage for some members may reduce access and service utilization. Since the non-covered members do not get reimbursed for hospital expenses, they may end up showing lower rates of hospitalizations. This barrier in hospital utilization may adversely affect the health status of patients and overall health status of members in larger households. Thus, removing these enrolment restrictions will be helpful in improving hospital utilization for members of the larger households.
Our study shows that the Scheduled tribes in India have lower duration of hospitalization. Scheduled tribes have been traditionally neglected in the country with lower capacity to pay because of their limited employment opportunities in the formal sector, lack of access to cash, and their area of residence which is mostly located in the hilly and remote tribal areas of India. They also have poor physical access to health care facilities [ 52 ]. In addition, the enrolment of tribal people in the health insurance programs for the poor is quite low because of the presence of access barriers as well as general mistrust of any governmental programs by the tribal groups. One important policy implication is that all efforts should be undertaken to reduce access barriers for the Scheduled tribes. Government should initiate outreach program to reach this hard-to-reach group so that their enrolment in the insurance program can be expanded.
Both men and women in the age group 40 years or more had higher incidence of hospitalizations than other groups. Women in the age groups of 19 to 40 years have higher incidence of hospitalizations but men in the age group do not show higher incidence. The main reason for this may be that women in the reproductive age group have higher hospital admissions related to childbirth in healthcare facilities. In order to encourage safe deliveries, the Government of India promotes institutional deliveries through the Janani Suraksha Yojana (JSY) program, a conditional cash transfer scheme, which may have further increased hospitalizations among women in the reproductive age group.
Utilization of private hospitals have higher OOP health expenditures. Utilization of private hospitals, by itself, is not a problem but when the poor households obtain care from private hospitals, out-of-pocket expenses become too high for the poor households to afford. The poor households need to be protected from the high OOP health expenditures when they have no option other than using private hospitals due to non-availability of public facilities in the locality.
The private healthcare system in India is highly unregulated and patients often have no idea about the health care charges of hospitals. Government can regulate the private sector by fixing prices for different diagnosis groups so that households would become fully aware of total hospital bill for their specific medical conditions. Making the charges of hospitals more transparent will help protect households from the uncertainty related to hospital expenses. Government hospitals are potentially an important source of healthcare in India, especially for the poor. Unfortunately, many poor people do not use the government healthcare facilities because of their perceived low quality, poor infrastructure, absences of health care providers and significant travel distances. Strengthening the government health facilities will reduce access barriers for the poor and will help lower the OOP expenditures.
This research finds that specific diseases such as cancers, cardiovascular, endocrine, respiratory, neurological, obstetric and childbirth, and injuries have higher OOP inpatient health expenditures. Specific national health programs can be established to improve access to outpatient and inpatient care for some of these medical conditions. India is currently establishing a national health program for non-communicable diseases which is being piloted in some districts. Faster nation-wide implementation of this program will help the poor individuals to get specific health service packages. Also, the health insurance maximum benefit limits may be increased for the poor individuals who are suffering from these diseases. Increasing coverage limits for specific medical conditions may encourage “up coding” without a rigorous monitoring system and health information system should be strengthened to identify potential mis-classification of cases to increase reimbursement received by hospitals.
This study has helped identify the groups most affected by OOP inpatient expenses and should be useful to help design national insurance programs to protect health and wellbeing of the poor households. This investigation will serve as a basis for assessing India’s policy options to reduce financial burden due to OOP inpatient expenditures by households below the poverty line.
Availability of data and materials
The datasets used for the current study is available from the corresponding author on reasonable request. The data can also be obtained from the Ministry of Statistics and Implementation of the Government of India with appropriate permission.
Abbreviations
Out-of-Pocket
Universal Health Coverage
Sustainable Development Goals
Government of India
Rashtriya Swasthiya Bima Yojana
Rajiv Aarogyasri; Community Health Insurance
Vajpayee Aarogyasri Scheme
Below-Poverty-Line
National Sample Survey Organization
Difference-in-Difference
Employee’s; State Insurance Scheme
Central Government Health Scheme
Ayurveda, Yoga, Unani, Siddha and Homeopathy
Indian Rupee
Primary Health Center
Janani Suraksha Yojana
The world health report. health systems financing: the path to universal coverage. Geneva: World Health Organization; 2010. https://apps.who.int/iris/bitstream/handle/10665/44371/9789241564021_eng.pdf;jsessionid=491323CCE04887DBCA9F9768D12E6597?sequence=1 .
Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014;11(9):e1001701.
PubMed PubMed Central Google Scholar
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet (London, England). 2003;362(9378):111–7.
Google Scholar
Sriram S. Critical evaluation of two approaches to achieve universal health coverage in India. Int J Community Med Public Health. 2018;5:3159–63.
Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health affairs (Project Hope). 2007;26(4):972–83.
National Health Accounts: Estimates for India 2014–15. Ministry of Health and Family Welfare. Government of India. http://nhsrcindia.org/sites/default/files/NHA%20Estimates%20Report%20-%20Final%20Web%20Optimized%20PDF%20Version%20-%2022.11.17_0.pdf .
Sriram S. Availability of infrastructure and manpower for primary health centers in a district in Andhra Pradesh, India. J Family Med Prim Care. 2018;7:1256–62.
Sriram S. Are the subcenters adequately equipped to deliver primary healthcare? A study of public health manpower and infrastructure in the health district in Andhra Pradesh, India. J Family Med Prim Care. 2019;8:102–8.
Sriram S, Noochpoung R. Determinants of hospital waiting time for outpatient care in India: how demographic characteristics, hospital ownership, and ambulance arrival affect waiting time. Int J Community Med Public Health. 2018;5:2692–8.
Shahrawat R, Rao KD. Insured yet vulnerable: out-of-pocket payments and India's poor. Health Policy Plan. 2012;27(3):213–21.
PubMed Google Scholar
Anderson M, Dobkin C, Gross T. The effect of health insurance coverage on the use of medical services. Am Econ J Econ Pol. 2012;4(1):1–27.
The Impact of Health Insurance in Low- and Middle-Income Countries. Escobar M-L, Griffin CC, Shaw RP, editors: Brookings Institution Press; 2010.
Pandey A, Ploubidis GB, Clarke L, Dandona L. Hospitalisation trends in India from serial cross-sectional nationwide surveys: 1995 to 2014. BMJ Open. 2017;7(12):e014188.
Hooda SK. Out-of-pocket payments for healthcare in India: who have affected the Most and why? J Health Manag. 2017;19(1):1–15.
Kumar AKS, Chen LC, Choudhury M, Ganju S, Mahajan V, Sinha A, et al. Financing health care for all: challenges and opportunities. Lancet. 2011;377(9766):668–79.
Karan A, Yip W, Mahal A. Extending health insurance to the poor in India: An impact evaluation of Rashtriya Swasthya Bima Yojana on out of pocket spending for healthcare. Soc Sci Med (1982). 2017;181:83–92.
Fan VY, Karan A, Mahal A. State health insurance and out-of-pocket health expenditures in Andhra Pradesh, India. Int J Health Care Finance Econ. 2012;12(3):189–215.
Taneja PK, Taneja S. Rashtriya Swasthya Bima Yojana (RSBY) for universal health coverage. Asian J Management Cases. 2016;13(2):108–24.
Devadasan N, Seshadri T, Trivedi M, Criel B. Promoting universal financial protection: evidence from the Rashtriya Swasthya Bima Yojana (RSBY) in Gujarat, India. Health Res Policy Syst. 2013;11:29.
Rao M, Katyal A, Singh PV, Samarth A, Bergkvist S, Kancharla M, et al. Changes in addressing inequalities in access to hospital care in Andhra Pradesh and Maharashtra states of India: a difference-in-differences study using repeated cross-sectional surveys. BMJ Open. 2014;4(6):e004471.
Selvaraj S, Karan AK. Why publicly-financed health insurance schemes are ineffective in providing financial risk protection. Econ Polit Wkly. 2012;47(11):60–8.
Rajasekhar D, Berg E, Ghatak M, Manjula R, Roy S. Implementing health insurance: the rollout of Rashtriya Swasthya Bima Yojana in Karnataka. Econ Polit Wkly. 2011;46(20):56–63.
Rent P, Ghosh S. Understanding the “cash-less” nature of government-sponsored health insurance schemes: evidence from Rajiv Gandhi Jeevandayee Aarogya Yojana in Mumbai. SAGE Open. 2015;5(4):2158244015614607.
Mitchell A, Mahal A, Bossert T. Healthcare utilisation in rural Andhra Pradesh. Econ Polit Wkly. 2011;46(5):15–9.
Aggarwal A. Impact evaluation of India's 'Yeshasvini' community-based health insurance programme. Health Econ. 2010;19(Suppl):5–35.
Sood N, Bendavid E, Mukherji A, Wagner Z, Nagpal S, Mullen P. Government health insurance for people below poverty line in India: quasi-experimental evaluation of insurance and health outcomes. BMJ. 2014;349:g5114.
Ghosh S. Publicly-financed health Insurance for the Poor Understanding RSBY in Maharashtra. Econ Polit Wkly. 2014;49(44):93–9.
Shahi AK, Singh H. Impact of Rashtriya Swasthya Bima Yojna on below poverty line population: an interstate analysis. J Health Manag. 2015;17(3):316–27.
Das J, Leino J. Evaluating the RSBY: lessons from an experimental information campaign. Econ Polit Wkly. 2011;46(32):85–93.
Thakur H. Study of Awareness, Enrollment, and Utilization of Rashtriya Swasthya Bima Yojana (National Health Insurance Scheme) in Maharashtra, India. Frontiers Public Health. 2016;3(282):1–13.
Nandi A, Ashok A, Laxminarayan R. The socioeconomic and institutional determinants of participation in India’s health insurance scheme for the poor. PLoS One. 2013;8(6):e66296.
CAS PubMed PubMed Central Google Scholar
Rathi P, Mukherji A, Sen G. Rashtriya Swasthya Bima Yojana Evaluating Utilisation, Roll-out and Perceptions in Amaravati District, Maharashtra. Econ Polit Wkly. 2012;XLVII:57–64.
Devadasan N, Criel B, Van Damme W, Manoharan S, Sarma PS, Van der Stuyft P. Community health insurance in Gudalur, India, increases access to hospital care. Health Policy Plan. 2010;25(2):145–54.
Devadasan N, Criel B, Van Damme W, Ranson K, Van der Stuyft P. Indian community health insurance schemes provide partial protection against catastrophic health expenditure. BMCHhealth Services Res. 2007;7:43.
Ranson MK. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. Bull World Health Organ. 2002;80(8):613–21.
Key Indicators of Social Consumption in India Health 2014. National Sample Survey Organization. Government of India. http://www.mospi.gov.in/sites/default/files/publication_reports/KI_Health_75th_Final.pdf .
Abadie A. Difference-in-Difference Estimators. The New Palgrave Dictionary of Economics. London: Palgrave Macmillan UK; 2016. p. 1–4.
Heckman J, Vytlacil J. Econometric evaluation of social programs, part II: Using the marginal treatment effect to organize alternative econometric estimators to evaluate social programs, and to forecast their effects in new environments. In: Heckman JJ, Leamer EE, editors. Handbook of econometrics; Vol. 6B.[u.a.]. Amsterdam: Elsevier; ISBN 978-0-444-53200-8. 2007. p. 4875–5143.
Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014;49(1):284–303.
Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference. 2015;3(2):237–49.
Faries D, Leon A, Haro J, Obenchain R. Analysis of observational health care data using SAS®. Cary: SAS Institute Inc.; 2010.
Wooldridge JM. Introductory econometrics. A modem approach. Second edition. Thomson South-Western USA: South-Western Cengage Learning products; 2003.
Dantas I, Santana R, Sarmento J, Aguiar P. The impact of multiple chronic diseases on hospitalizations for ambulatory care sensitive conditions. BMC Health Serv Res. 2016;16(1):348.
Kasthuri A. Challenges to healthcare in India - the five A's. Indian J Community Med. 2018;43(3):141–3.
Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers C, et al. Chronic diseases and injuries in India. Lancet. 2011;377(9763):413–28.
Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS One. 2018;13(5):e0196106.
Berry JG, Gay JC, Joynt Maddox K, Coleman EA, Bucholz EM, O’Neill MR, et al. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ (Clinical research ed). 2018;360:k497.
McPhail SM. Multimorbidity in chronic disease: impact on health care resources and costs. Risk Manag Healthc Policy. 2016;9:143–56.
Brinda EM, Andres AR, Enemark U. Correlates of out-of-pocket and catastrophic health expenditures in Tanzania: results from a national household survey. BMC Int Health Hum Rights. 2014;14:5.
Getachew B, Liabsuetrakul T. Health care expenditure for delivery care between maternity waiting home users and nonusers in Ethiopia. Int J Health Plann Manage. 2019;34(2):e1334–e1345.
O'Connor M, Hanlon A, Naylor MD, Bowles KH. The impact of home health length of stay and number of skilled nursing visits on hospitalization among Medicare-reimbursed skilled home health beneficiaries. Res Nurs Health. 2015;38(4):257–67.
Barik D, Thorat A. Issues of Unequal Access to Public Health in India. Front Public Health. 2015;3:245.
Aji B, De Allegri M, Souares A, Sauerborn R. The impact of health insurance programs on out-of-pocket expenditures in Indonesia: an increase or a decrease? Int J Environ Res Public Health. 2013;10(7):2995–3013.
Ekman B. Catastrophic health payments and health insurance: some counterintuitive evidence from one low-income country. Health Policy. 2007;83(2–3):304–13.
Forgia G, Nagpal S. Government-sponsored health Insurance in India: are You covered?. Directions in development. Washington DC: World Bank; 2012.
McIntyre D, Thiede M, Dahlgren G, Whitehead M. What are the economic consequences for households of illness and of paying for health care in low- and middle-income country contexts? Soc Sci Med. 2006;62(4):858–65.
Rudra S, Kalra A, Kumar A, Joe W. Utilization of alternative systems of medicine as health care services in India: Evidence on AYUSH care from NSS 2014. PLoS One. 2017;12(5):e0176916.
Weerasinghe M, Fernando DN. Access to Care in a Plural Health System: concerns for policy reforms. J Coll Commun Physicians Sri Lanka. 2011;14:39–45.
Alam K, Mahal A. Economic impacts of health shocks on households in low and middle income countries: a review of the literature. Glob Health. 2014;10:21.
Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage. Health affairs (Project Hope). 2009;28(3):w467–78.
Leone T, James KS, Padmadas SS. The burden of maternal health care expenditure in India: multilevel analysis of national data. Matern Child Health J. 2013;17(9):1622–30.
Bonu S, Bhushan I, Rani M, Anderson I. Incidence and correlates of 'catastrophic' maternal health care expenditure in India. Health Policy Plan. 2009;24(6):445–56.
Bhojani U, Thriveni BS, Devadasan R, Munegowda CM, Devadasan N, Kolsteren P, et al. Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore. India BMC Public Health. 2012;12(1):990.
Thadani K. Public private Partnership in the Health Sector: boon or bane. Procedia - Social and Behavioral Sciences. 2014;157:307–16.
Yadav S, Arokiasamy P. Understanding epidemiological transition in India. Global health action. 2014;7:23248.
Li Y, Wu Q, Xu L, Legge D, Hao Y, Gao L, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. Bull World Health Organ. 2012;90(9):664–71.
Kronenberg C, Barros PP. Catastrophic healthcare expenditure – drivers and protection: the Portuguese case. Health Policy. 2014;115(1):44–51.
K X, P S, Durairaj V, O'Donnell O. The Drivers of Catastrophic Expenditure: Outpatient Services, Hospitalization or Medicines? The World Health Report Background Paper No 21. 2010.
Molla AA, Chi C, Mondaca ALN. Predictors of high out-of-pocket healthcare expenditure: an analysis using Bangladesh household income and expenditure survey, 2010. BMC Health Serv Res. 2017;17(1):94.
You X, Kobayashi Y. Determinants of out-of-pocket health expenditure in China: analysis using China health and nutrition survey data. Appl Health Econ Health Policy. 2011;9(1):39–49.
Mondal S, Lucas H, Peters D, Kanjilal B. Catastrophic out-of-pocket payment for healthcare and implications for household coping strategies: evidence from West Bengal, India. Econ Bull. 2014;34:1303–16.
Mohanty SK, Srivastava A. Out-of-pocket expenditure on institutional delivery in India. Health Policy Plan. 2013;28(3):247–62.
da Silva MT, Barros AJD, Bertoldi AD, de Andrade JP, Matijasevich A, Santos IS, et al. Determinants of out-of-pocket health expenditure on children: an analysis of the 2004 Pelotas birth cohort. Int J Equity Health. 2015;14(1):53.
Sarker AR, Mahumud RA, Sultana M, Ahmed S, Ahmed W, Khan JA. The impact of age and sex on healthcare expenditure of households in Bangladesh. SpringerPlus. 2014;3:435.
Jiang C, Ma J, Zhang X, Luo W. Measuring financial protection for health in families with chronic conditions in rural China. BMC Public Health. 2012;12(1):988.
Shi W, Chongsuvivatwong V, Geater A, Zhang J, Zhang H, Brombal D. Effect of household and village characteristics on financial catastrophe and impoverishment due to health care spending in Western and Central Rural China: A multilevel analysis. Health Res Policy Syst. 2011;9:16.
Alemayehu B, Warner KE. The lifetime distribution of health care costs. Health Serv Res. 2004;39(3):627–42.
Fiestas NL. Impact of universal health coverage on catastrophic health expenditure: Evidence from Ghana. European J Public Health. 2018;28(suppl_4):349–50.
Fiestas Navarrete L, Ghislandi S, Stuckler D, Tediosi F. Inequalities in the benefits of national health insurance on financial protection from out-of-pocket payments and access to health services: cross-sectional evidence from Ghana. Health Policy Plan. 2019;34(9):694–705.
Sriram S. Health Insurance Programs for the Poor and Out-of-Pocket Healthcare Costs: Evidence using National Sample Survey Data. Value Health. 2020;23(Supplement 1):S95. https://doi.org/10.1016/j.jval.2020.04.1069 .
Article Google Scholar
Download references
Acknowledgements
The authors would like to give their sincere thanks to the Government of India for providing the data for the study. The abstract of this paper has been previously submitted to the International Society of Pharmacoeconomics and Outcomes Research (ISPOR) Conference 2020 and the abstract has been published in Value in Health [ 80 ].
Not Applicable.
Author information
Authors and affiliations.
Department of Health Services Policy and Management, University of South Carolina, Columbia, SC, USA
Shyamkumar Sriram & M. Mahmud Khan
You can also search for this author in PubMed Google Scholar
Contributions
SS was involved in the conception of the study, design, analysis and writing of the manuscript. MK helped in the analysis framework and writing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Shyamkumar Sriram .
Ethics declarations
Ethics approval and consent to participate.
The dataset is available in the public domain after removing all individual level identification variables. It is not possible to identify the residence of any of the households as well. Therefore, ethical approval is not needed for the study. Permission has been obtained from the Ministry of Statistics and Implementation of the Government of India for this research and potential future publications using the data set.
Consent for publication
Competing interests.
Dr. Mahmud Khan is an associate editor of BMC Health Services Research. The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sriram, S., Khan, M.M. Effect of health insurance program for the poor on out-of-pocket inpatient care cost in India: evidence from a nationally representative cross-sectional survey. BMC Health Serv Res 20 , 839 (2020). https://doi.org/10.1186/s12913-020-05692-7
Download citation
Received : 02 January 2020
Accepted : 31 August 2020
Published : 07 September 2020
DOI : https://doi.org/10.1186/s12913-020-05692-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health insurance
- Financial protection
- Out-of-pocket health expenditure
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Health insurance in India: what do we know and why is ethnographic research needed
Affiliations.
- 1 a University of Amsterdam, Amsterdam Institute of Social Science Research , Nieuwe Achtergracht 166 , 1018 WV Amsterdam , the Netherlands.
- 2 b School of Anthropology , University of Arizona , 1009 E. South Campus drive, Tucson , AZ 85721 , USA.
- 3 c University of Leiden, Leyden Academy on Vitality and Aging , Poortgebouw LUMC, Rijnburgerweg 10, 2333 AA, Leiden , the Netherlands.
- PMID: 26828125
- DOI: 10.1080/13648470.2015.1135787
The percentage of India's national budget allocated to the health sector remains one of the lowest in the world, and healthcare expenditures are largely out-of-pocket (OOP). Currently, efforts are being made to expand health insurance coverage as one means of addressing health disparity and reducing catastrophic health costs. In this review, we document reasons for rising interest in health insurance and summarize the country's history of insurance projects to date. We note that most of these projects focus on in-patient hospital costs, not the larger burden of out-patient costs. We briefly highlight some of the more popular forms that government, private, and community-based insurance schemes have taken and the results of quantitative research conducted to assess their reach and cost-effectiveness. We argue that ethnographic case studies could add much to existing health service and policy research, and provide a better understanding of the life cycle and impact of insurance programs on both insurance holders and healthcare providers. Drawing on preliminary fieldwork in South India and recognizing the need for a broad-based implementation science perspective (studying up, down and sideways), we identify six key topics demanding more in-depth research, among others: (1) public awareness and understanding of insurance; (2) misunderstanding of insurance and how this influences health care utilization; (3) differences in behavior patterns in cash and cashless insurance systems; (4) impact of insurance on quality of care and doctor-patient relations; (5) (mis)trust in health insurance schemes; and (6) health insurance coverage of chronic illnesses, rehabilitation and OOP expenses.
Keywords: Health Policy and Systems Research (HPSR); Health insurance; India; ethnography.
PubMed Disclaimer
Similar articles
- "Demand Side" Health Insurance in India: The Price of Obfuscation. Ecks S. Ecks S. Med Anthropol. 2021 Jul;40(5):404-416. doi: 10.1080/01459740.2021.1929208. Epub 2021 May 28. Med Anthropol. 2021. PMID: 34047660
- Insured yet vulnerable: out-of-pocket payments and India's poor. Shahrawat R, Rao KD. Shahrawat R, et al. Health Policy Plan. 2012 May;27(3):213-21. doi: 10.1093/heapol/czr029. Epub 2011 Apr 12. Health Policy Plan. 2012. PMID: 21486910
- Healthcare provision in rural India: does micro health insurance help or hinder? Forbes DJ. Forbes DJ. Int J Health Care Qual Assur. 2012;25(3):216-25. doi: 10.1108/09526861211210439. Int J Health Care Qual Assur. 2012. PMID: 22755476
- Pricing-out effect from possible user-fee policies under Taiwan's National Health Insurance. Chen WY, Liang YW, Lin YH. Chen WY, et al. Expert Rev Pharmacoecon Outcomes Res. 2010 Aug;10(4):453-64. doi: 10.1586/erp.10.43. Expert Rev Pharmacoecon Outcomes Res. 2010. PMID: 20715921 Review.
- Universal access to health care: a practical perspective. Battistella RM, Kuder JM. Battistella RM, et al. J Health Hum Resour Adm. 1993 Summer;16(1):6-34. J Health Hum Resour Adm. 1993. PMID: 10129845 Review.
- Social and demographic determinants of health insurance status in India: Evidence from a nationally representative cross-sectional survey. Vootukuri K, Kumar KSV, Naik VS. Vootukuri K, et al. J Educ Health Promot. 2024 Apr 29;13:150. doi: 10.4103/jehp.jehp_1006_23. eCollection 2024. J Educ Health Promot. 2024. PMID: 38784293 Free PMC article.
- Self-reported symptom burden among patients attending public health care facilities in India: Looking through ICPC-3 lens. Gupta P, Bharati B, Sundar Sahu K, Mahapatra P, Pati S. Gupta P, et al. PLOS Glob Public Health. 2024 May 6;4(5):e0001835. doi: 10.1371/journal.pgph.0001835. eCollection 2024. PLOS Glob Public Health. 2024. PMID: 38709793 Free PMC article.
- Public Health Insurance Status and Utilization of Healthcare Services Across India: A Narrative Review. Shende V, Wagh V. Shende V, et al. Cureus. 2024 Feb 16;16(2):e54308. doi: 10.7759/cureus.54308. eCollection 2024 Feb. Cureus. 2024. PMID: 38496075 Free PMC article. Review.
- Evaluation of short-acting Beta-2-agonist prescriptions and associated clinical outcomes: Findings from the SABA use IN Asthma (SABINA) study in Asia. Wang HC, Djajalaksana S, Sharma L, Theerakittikul T, Lim HF, Yoo KH, Yu-Lin AB, Diaz DV, Yang L, Beekman MJHI. Wang HC, et al. World Allergy Organ J. 2023 Oct 16;16(10):100823. doi: 10.1016/j.waojou.2023.100823. eCollection 2023 Oct. World Allergy Organ J. 2023. PMID: 37869560 Free PMC article.
- A Systematic Review of the World's Largest Government Sponsored Health Insurance Scheme for 500 Million Beneficiaries in India: Pradhan Mantri Jan Arogya Yojana. Aashima, Sharma R. Aashima, et al. Appl Health Econ Health Policy. 2024 Jan;22(1):17-32. doi: 10.1007/s40258-023-00838-0. Epub 2023 Oct 6. Appl Health Econ Health Policy. 2024. PMID: 37801262
- Search in MeSH
LinkOut - more resources
Full text sources.
- Taylor & Francis
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- My Shodhganga
- Receive email updates
- Edit Profile
Shodhganga : a reservoir of Indian theses @ INFLIBNET
- Shodhganga@INFLIBNET
- University of Mysore
- Department of Development Studies
| Title: | Health economics impact of health insurance on health care services in India : |
| Researcher: | Poursamad, Abdollah |
| Guide(s): | |
| Keywords: | Building Health Systems Health Health Care Services - India Health Economics Health Insurance Health Services System Health System - India Public Health |
| Upload Date: | 1-Oct-2015 |
| University: | University of Mysore |
| Completed Date: | 2014 |
| Abstract: | newline |
| Pagination: | |
| URI: | |
| Appears in Departments: | |
| File | Description | Size | Format | |
|---|---|---|---|---|
| Attached File | 141.76 kB | Adobe PDF | ||
| 154.46 kB | Adobe PDF | |||
| 185.26 kB | Adobe PDF | |||
| 120.39 kB | Adobe PDF | |||
| 206.05 kB | Adobe PDF | |||
| 239.15 kB | Adobe PDF | |||
| 121.02 kB | Adobe PDF | |||
| 476.76 kB | Adobe PDF | |||
| 910.75 kB | Adobe PDF | |||
| 2.6 MB | Adobe PDF | |||
| 210.24 kB | Adobe PDF | |||
| 102.46 kB | Adobe PDF | |||
| 107.85 kB | Adobe PDF | |||
| 107.03 kB | Adobe PDF | |||
| 109.72 kB | Adobe PDF | |||
| 116.31 kB | Adobe PDF |
Items in Shodhganga are licensed under Creative Commons Licence Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0).

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.11(4); 2021

Health insurance awareness and its uptake in India: a systematic review protocol
Bhageerathy reshmi.
1 Health Information Management, Manipal College of Health Professionals, Manipal Academy of Higher Education, Manipal, India
Bhaskaran Unnikrishnan
2 Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, India
Shradha S Parsekar
3 Public Health Evidence South Asia, Department of Health Information, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal Academy of Higher Education, Manipal, India
Ratheebhai Vijayamma
4 Manipal Institute of Communication, Manipal Academy of Higher Education, Manipal, India
Bhumika Tumkur Venkatesh
Associated data, introduction.
Health insurance is one of the important approaches that can help in boosting universal healthcare coverage through improved healthcare utilisation and financial protection. This objectives of this review are to identify various interventions implemented in India to promote awareness of health insurance, and to provide evidence for the effectiveness of such interventions on the awareness and uptake of health insurance by the resident Indian population.
Methods and analysis
A systematic review will be carried out based on the Cochrane handbook for systematic reviews of interventions. The review will include experimental and analytical observational studies that have included adult population (>18 years) in India. We will include any intervention, policy or programme that directly or indirectly affects awareness or uptake of health insurance. The following outcomes will be eligible to be included: awareness or health insurance literacy, attitude such as readiness to buy health insurance or decision making, uptake of health insurance, demand-side and supply-side factors for awareness of health insurance, and awareness as a factor for uptake and re-enrolment in health insurance. Databases such as MEDLINE (PubMed), Web of Science, Scopus, 3ie impact evaluation repository and Social Science Research Network will be searched from January 2010 to 15 July 2020. Additionally, important government websites and references of the included studies will be scanned to identify potential records. Three authors, independently, will carry out screening and data extraction. Studies will be categorised into quantitative and qualitative, and mixed-methods synthesis will be employed to analyse the findings.
Ethics and dissemination
This review will be based on published studies and will not recruit human participants directly, therefore, ethical clearance is not applicable. We will disseminate the final review findings in a national or international conference and publish in a peer-reviewed journal.
Strengths and limitations of this study
- This systematic review will use mixed-methods analysis involving findings from quantitative and qualitative studies conducted in India.
- We will comprehensively search the evidence in various databases, grey literature and reference and forward citations of included studies, however, the publications will be restricted to English.
- We anticipate heterogeneity owing to study designs of potentially included studies, however, to mitigate this challenge we have planned to conduct subgroup analysis based on PROGRESS-Plus framework.
Low-income and middle-income countries (LMICs) contribute to around 84% of the world population and 90% of the global burden of disease. 1 People living in the LMICs rely majorly on out-of-pocket payments as the prime source for managing healthcare expenses, that results in a massive demand for services and financial burden of households (usually catastrophic), which in turn leads to impoverishment. 1–5 It is projected that every year approximately 150 million people experience financial catastrophe, by spending more than 40% on health expenses other than food. 6 Families generally spend more than 10% of the household income on illness-related expenses, due to which other household expenses are affected. 2 5 To make it worse, evidence suggests that per capita spending on healthcare in many LMICs is expected to increase in coming years. 4 Additionally, the increased costs of seeking and receiving care can hinder the access to healthcare. 7
The Universal Health Coverage (UHC) is embedded within the Sustainable Development Goals (SDGs) and aims ‘to ensure healthy lives and promote well-being for all at all ages by 2030’. 8 It includes financial risk protection and equal access to quality essential healthcare services. 8 9 In other terms, UHC encourages equitable healthcare 2 and nations across the world are committed to achieving SDGs through UHC. 10
Health insurance is one of the important approaches that can help in boosting UHC through improved healthcare utilisation and financial protection. 7–9 11 There are multiple types of insurance in LMICs that differ with providers (government vs private sector), scales and types of beneficiaries. 8 However, in many LMICs, due lack of acceptability and unwillingness to pay (WTP) premiums, health insurance coverage is limited. 2 4 This increases the risk of excluding vulnerable and at-risk population, who cannot afford to pay health insurance premium. 8 Additionally, the older adults, and the individuals with disability and chronic diseases, have less probability of enrolling in health insurance schemes or their specific needs may not be covered under the scheme. 8
The coverage of health insurance policies or programmes in India is improving, however, the publicly funded health insurance schemes are mostly restricted to socioeconomically backward people or government employees. 12 India’s first health insurance programme, launched in the 1950s, was limited to central government employees and certain low-income population. 11 Over the years, the private healthcare providers’ dominance in quality healthcare service provision can be seen. 11 Nevertheless, many economically backward families are either deprived of healthcare or are pushed into poverty in the absence of financial protection. 11 In 2002, targeted health insurance programmes for low-income households were introduced by central and state governments in partnership with private sector and non-governmental organisations (NGO). Since 2002 (recommendations of National Health Policy 2002), more than 17 health insurance schemes have been launched by various governments in India. 11 The most recent one is ‘Ayushman Bharat’ or Pradhan Mantri Jan Arogya Yojana (PMJAY) (Prime minister’s health assurance scheme) launched in 2018 to achieve UHC. PMJAY is fully financed by the government and seeks to cover 500 million citizens with an annual cover of approximately US$7000 per household. The main aim of the PMJAY is to lessen the economic burden experienced by poor and vulnerable groups for access to healthcare facility. 13
Despite the availability of multiple health insurance schemes, evidence suggests that the uptake of health insurance in India is poor. As per the recently concluded National Sample Survey Office data, there were as low as 14% rural and 18% urban residents of India having some form of health insurance. 14 The low coverage of health insurance was evident in other literature, wherein it was reported to be less than 20%. 5 12 Similarly, other LMICs have reported poor registrations in the national health insurance schemes. 8 9 12 15
There are multiple factors that are responsible for awareness and enrolment in health insurance schemes. 2 4 These factors can be broadly divided into individual (age, gender, education, employment status, marital status), 2 9 16 and household characteristics (wealth, size of family). 1 9 17 Other factors are programme-related (premium amount, rules, regulation and procedures), social capital (trust, networks and group participation, social norms and solidarity and togetherness features of the social organisation of the community), institutional factors (regulatory mechanisms, complaint handling systems and insurance education) and supply-side factors (quality of care and distance of house from the nearest health facility). 2 The aforementioned factors may also determine the consumer preference in selecting the health insurance. 17 Inadequate claim returns, poor accountability and non-transparent operations hinders the uptake of health insurance. 18
In Indian studies, a scant that is, 34% of the participants who did not have health insurance were willing to pay for any health insuance. 5 Previous research in LMICs suggests that financial status of household is positively associated with WTP. 2 4 9 18 Whereas level of education received contradictory findings, that is, a study conducted in Nigeria reported that education was negatively associated with WTP 4 contrary to study conducted in Uganda, 1 Ghana 16 and India. 5 Family who had good perceived health had less probability of getting insurance as compared with those individuals who perceived their health as poor. Similarly, those individuals who had chronic diseases were more inclined to have health insurance than those who did not have chronic diseases. 2 Corruption and mistrust in the health insurance scheme 1 5 18 and expensive plans 5 18 were some of the reasons for non-WTP. Lack of information or health insurance illiteracy is another important reason for non-WTP. 1 5 18
Health insurance literacy is defined as ‘the degree to which individuals have the knowledge, ability and confidence to find and evaluate information about health plans, select the best plan for their own (or their families) financial and health circumstances, and use the plan once enrolled.’ 1 Lack of health insurance literacy or education hinders the uptake of health insurance and in many LMICs health insurance literacy is poor. A study conducted in Uganda reported that about 34% of the studied population were not aware of health insurance. 1 Whereas, proportion of people having inadequate knowledge about health insurance was found to be high in countries such as India (46%), 5 Myanmar (66%) 3 and Hispanic American in the USA (70%). 19
Familiarity or awareness of the insurance schemes increases the utilisation of health insurance and subsequently help in healthcare uptake. 1 2 19 Individuals usually enrol into health insurance because of their personal experiences, awareness or word-of-mouth advertisements. 17 Mass media such as newspaper, radio and television play an important role in making people aware of health insurance schemes. 1 Friends, community meetings, school gatherings and health workers have an influence on increasing the health insurance awareness of the people. 1 Although, aforesaid factors help in increasing the awareness and enrolment in health insurance scheme, some enrollees may not pay premium on regular basis and might not get to know even after health insurance is lapsed. 9 Women farmers, as compared with other occupations, had more odds of unawareness that their insurance was lapsed. 9
It is evident from the above description that there is inadequate awareness of health insurance among general population in LMICs. Knowledge about health insurance can boost individuals’ confidence and self-efficacy; thus, it is an important a priori factor that is required to get enrolled in health insurance scheme. 19 Outreach programmes to increase general knowledge of health insurance and integrating health insurance education within health delivery systems may help to improve the uptake of health insurance. 19 Globally, there are different methods available to promote and raise awareness about different health insurance schemes. However, India is a diverse country with a complex health system and numerous contextual factors. A ‘one size fits all’ approach for any policy or intervention is not suitable for the country. Therefore, it is imperative to understand the different approaches implemented to raise awareness about health insurance in the country. Additionally, due to increased population and a meagre public health spending on healthcare, it is important to understand if the resources are being used appropriately. To ensure this, understanding the effectiveness of such policies is essential, so that focus is directed towards the suitable interventions. ‘Ayushman Bharat Scheme-PMJAY’ is implemented to ensure increased utilisation of the healthcare facilities with financial protection of the beneficiaries. The evidence available on the effectiveness of the PMJAY scheme states no effect of the scheme on utilisation of healthcare and financial protection of enrolled beneficiaries, 13 however, this evidence is limited. Therefore, in the Indian context, it is important to understand if awareness is a factor that has led to decreased utilisation of PMJAY or failure of the other schemes (viz. Rashtriya Swasthya Bima Yojana-RSBY) in securing financial protection of the beneficiaries. 20 Also, it is vital to understand the importance of awareness programmes for success of the health insurance schemes, which will be the focus of this review.
A systematic review will help in synthesising high-quality evidence in a systematic manner, for this important topic of interest. The proposed systematic review will, therefore, identify the different approaches and interventions for increasing health insurance awareness in India and will give information about the impact of these interventions. This review is planned to address the following research questions:
- What are the various interventions implemented in India to promote awareness of health insurance?
- What is the effectiveness of the above interventions on the awareness and uptake of health insurance by people of India?
Methodology for this systematic review will be based on the Cochrane handbook for systematic reviews of interventions 21 and we have adhered to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-Protocols guidelines for reporting this protocol. 22
Criteria for including studies in the review
Population: The review will include studies conducted in India that involve adult population (>18 years). We will consider the studies having household as a unit of analysis, if the head of the family (or the family member who was interviewed) is an adult.
Intervention/exposure: We will include any intervention, policy or programme that directly or indirectly affects awareness of health insurance. The health insurance scheme could be of any type, including but not limited to, public, private, for profit and not-for-profit. Contribution for premiums could be made by individual, NGO, employer or government. There is no restriction on focus of health insurance for example, hospital stay, surgery or critical illness.
Intervention/exposure could be educational, informative, training, technology and m-health or e-health related. The interventions could be focused on raising income threshold to be eligible for health insurance, such as, conditional or unconditional cash transfers that indirectly influences awareness of health insurance. Similarly, training and performance-based financing for healthcare staff or other groups will be eligible for inclusion. The intervention could be a modification of the enrolment procedure, changes in the premium or organisational changes in handling health insurance. Intervention could be directed on general population or targeted groups such as vulnerable population, indigenous groups, community leaders, employees, formal or informal groups and healthcare staff.
Comparison: This review will not restrict the studies based on comparison, as having a comparison group may not always be feasible.
- Awareness/health insurance literacy (refers to knowledge of the household head or household member on the presence of insurance schemes, its principles and significance. The outcome measure can be objective or subjective).
- Attitude: Readiness to buy health insurance, decision making.
- Uptake of health insurance.
- Demand-side and supply-side factors for awareness of health insurance.
- Awareness of health insurance as a factor for uptake or re-enrolment of health insurance.
Types of study designs: This review will include experimental studies that assessed the effect of intervention to promote awareness and uptake of health insurance. It is sometimes not practical to conduct randomised controlled trials (RCTs) to measure the effect of public health interventions, therefore, the review will also include other study designs. Studies with following designs will be included: RCTs, interrupted time-series studies, difference-in-difference, regression discontinuity designs, statistical matching, quasi-randomised and non-randomised trials. Additionally, this review will include prospective, retrospective, analytical cross-sectional and studies related to process evaluation and policy analysis, if the studies have provided description of intervention or exposure of our interest. Qualitative studies are important source of information about barriers and enabling factors that can complement the findings, therefore, we will also include these types of studies. This review will exclude descriptive cross-sectional (prevalence) studies, commentaries, perspectives, editorials, reviews and conference abstracts. Policy papers that do not provide details of implementation of intervention will not be considered.
Searching and locating the studies
The electronic databases such as MEDLINE (PubMed), Web of Science and Scopus will be searched to identify potential records. Additionally, 3ie impact evaluation repository and Social Science Research Network will be searched. Databases will be searched from January 2010 to 15 July 2020 and publications will be restricted to English language. Ministry of Health and Family Welfare, RSBY, Ayushman Bharat and other state health insurance websites will be searched for reports on the health insurance schemes. We will also scan through references of the included studies for any additional eligible records. After identifying the keywords, initial search will be carried out in PubMed, which will then be replicated in other databases. A designated information scientist will be responsible for conducting search. The preliminary search concepts and key terms are given in table 1 .
Search concepts and key words
| Concept | Key terms |
| Intervention or exposure | ‘Information Education Communication’, ‘Mass Media’, ‘Television’, ‘Leaflet’, ‘Brochure’, ‘Flyer’, ‘Radio’, ‘Television’, ‘Advertisement’, ‘Behavioural change communication’, Awareness programme/ programme/ campaign/ initiatives/policy’, ‘Promotion’, ‘Marketing’, ‘Social media’, ‘E-health’, ‘M-health’. |
| Insurance names | ‘Community insurance’, ‘Health insurance’, ‘Health insurance programmes/programmes/schemes’, ‘Health finance /financing’, ‘Healthcare reform’, ‘Insurance coverage’, ‘National health insurance’, ‘National health insurance scheme’, ‘Medical insurance’, ‘Micro health insurance’, ‘Public health insurance’, ‘Social insurance’, ‘Social protection’, ‘Universal healthcare’, ‘Universal healthcare’, ‘Ayushman Bharat’, ‘Pradhan Mantri Jan Arogya Yojana’, ‘Mukhyamantri Swasthya Bima Yojana’, ‘Rashtriya Swastya Bima Yojana’, ‘Aarogysri’, ‘Rajiv Arogyabhagya’, ‘Rajiv Arogyashree health insurance’, ‘Rajiv Gandhi Jeevandayee Arogya Yojana’, ‘Yesasvini health insurance’, ‘Yashshvini Community based health insurance programme’, ‘Vajpayee Arogyashree’, ‘Biju Krushak Kalyan’, ‘Kalainagar', ‘CHIS’, ‘Employee State Insurance Scheme’, ‘Central Government Health Scheme’, ‘Mediclaim’, ‘Deen Dayal Swasthya Seva Yojana’. |
| Outcome | ‘Awareness of health insurance’, ‘Health insurance literacy’, ‘Uptake of health insurance’, ‘Utilisation of healthcare services’, ‘Enrolment under health insurance’, ‘Health insurance enrolment’, ‘Health insurance retention’, ‘Healthcare utilisation’, ‘Medical service utilisation’, ‘Readiness to buy health insurance’, ‘Decision making’, ‘Perceptions’, ‘Knowledge’, ‘Demand-side and supply-side factors’, ‘factors’, ‘barriers’, ‘enablers’. |
| Region | India |
Applying eligibility and screening the studies
The results of search will be imported to Endnote X7 reference manager software and duplicates will be removed. MS Excel spreadsheet will be used to screen the records. Based on inclusion and exclusion criteria, all the records will be subjected to two stage—title/abstracand full text (FT)—screening process, independently by three (SSP, ER and BTV) reviewers (in pairs). Any disagreements between the reviewers will be resolved by discussion, and senior reviewer will be involved in decision making in case of disagreements between the reviewers. The reasons for excluding FTs will be documented and the PRISMA flow diagram will be provided. A detailed screening protocol will be used as a back-up document to aid the screening process. Table 2 gives detailed screening protocol.
Screening protocol
| 1 | Title and abstract screening | ||
| A | Is the study published in English? AND Is it published in the year 2000 or later? | If answer to both the components are ‘yes’, Go to B | If it is non-English or published before 2000 then exclude the study |
| B | Is it a study conducted in India? | If it is clearly stated that it is conducted elsewhere, but India, then exclude the study | |
| C | Does study involve one of the following design or analysis: RCTs, interrupted time series studies, difference-in-difference, regression discontinuity designs, statistical matching, quasi-randomised and non-randomised trials, prospective, retrospective and analytical cross-sectional studies and studies related to process evaluation and policy analysis. | If answer is ‘yes’ OR it is not clearly stated in abstract, Go to D | If the study is descriptive cross-sectional (or prevalence study) having single group OR if the publication is a commentary, perspective, editorial, reviews, conference abstracts OR policy paper that does not provide details of implementation of intervention: exclude the study |
| D | Does the study describe the intervention for increasing awareness of and uptake of health insurance? (The intervention could be any intervention, policy or programme (eg, behavioural change communication or educational) that directly or indirectly affects awareness of health insurance. There is no restriction on mode of intervention, for example, mass media or group discussions. There is no restriction on who provides the intervention, for example, researcher, community-based workers or insurance agent. There is no restriction on duration and frequency of providing intervention. The health insurance scheme could be of any type, including but not limited to, public, private, for profit and not-for-profit. Contribution for premiums could be made by individual, non-governmental organisations, employer or government. There is no restriction on focus of health insurance, for example, hospital stay or surgery.)OR Does the study describe about the factors associated with awareness of health insurance? OR Does the study describe awareness as a factor for uptake or re-enrolment of health insurance? | If answer to one of the components is ‘yes’ OR if it is not clearly stated and you are in doubt, then Include the study for full-text screening If you are in doubt: flag for discussion | If no, exclude the study |
| 2 | |||
| E | Is it a study conducted in India? | If it is ‘yes’, Go to F | If no exclude the study |
| F | Did the study involve adult population? | If it is ‘yes’, Go to G | If no exclude the study |
| G | Does the study involve one of the following design or analysis: RCTs, interrupted time series studies, difference-in-difference, regression discontinuity designs, statistical matching, quasi-randomised and non-randomised trials, prospective, retrospective and analytical cross-sectional studies and studies related to process evaluation and policy analysis. | If answer is ‘yes’ Go to H OR If you are doubtful, then flag for discussion | If the study is descriptive cross-sectional (or prevalence study) having single group OR If the publication is a commentary, perspective, editorial, reviews, conference abstracts or policy paper that does not provide details of implementation of intervention: exclude the study |
| H | Does the study describe the intervention for increasing awareness of and uptake of health insurance? (The intervention could be any intervention, policy or programme (eg, behavioural change communication or educational) that directly or indirectly affects awareness of health insurance. There is no restriction on mode of intervention, for example, mass media or group discussions. There is no restriction on who provides the intervention, for example, researcher, community-based workers or insurance agent. There is no restriction on duration and frequency of providing intervention. The health insurance scheme could be of any type, including but not limited to, public, private, for profit and not-for-profit. Contribution for premiums could be made by individual, non-governmental organisations, employer or government. There is no restriction on focus of health insurance, for example, hospital stay or surgery.) OR Does the study describe about the factors associated with awareness of health insurance? OR Does the study describe awareness as a factor for uptake or re-enrolment of health insurance? | If answer to one of the components is ‘yes’ Go to I OR If you are in doubt, then flag for discussion | If no exclude the study |
| I | Did the study measure the outcomes of our interest? | If answer is ‘yes’ then include for data analysis | If no, exclude the study |
RCT, randomised controlled trial.
Data extraction
Data will be extracted independently by three reviewers (SSP, ER and BTV). A predesigned data extraction form will be used for extraction of the data. The data extraction form will be subjected to pilot testing and will be revised as per the suggestions by the reviewers and the experts at this stage. Any disagreements during data extraction will be resolved by consensus supported by the senior reviewer. Data will be extracted based on the characteristics mentioned in the table 3 .
Data extraction format
| Publication details | First author’s last name |
| Year of publication | |
| Publication type: report/ journal publication | |
| Population characteristics | Age |
| Gender | |
| Religion/race/ethnicity | |
| No of participants included | |
| Location/setting | State/district or other details of place where study was conducted |
| Setting: hospital/community based Rural/urban | |
| Study methodology/ design | Study design: RCT, quasi-randomised trial, case–control study. Type of analysis |
| Intervention details | Type of intervention, mode of delivery, other details such as content/ frequency, who provided it. Start time and duration of intervention Details of comparison |
| Insurance details | Public/private/community-based insurance Start or launch date (month and year) of insurance Type of plan, for example, individual, family, senior citizen, critical illness. Benefits of health insurance, for example, cashless facility, hospitalisation, prehospitalisation and posthospitalisation, medical check-up, maternity benefits, childcare, critical illness. |
| Exposure details | List different factors or themes |
| Outcome details | List down outcome, variable type: continuous or categorical, type of analysis Effect measures with 95% CI (such as OR, risk ratio, HR) No of participants analysed, number lost to follow-up Details of subgroup analysis, if any. |
| Themes and subthemes | |
| Other details |
Critical appraisal of included studies
Effective Public Health Practice Project (EPHPP) tool 23 will be used to assess the methodological quality of quantitative studies (except observational studies) and Newcastle-Ottawa scale (NOS) 24 will be used for the observational studies. The EPHPP rates the study as ‘strong’, ‘moderate’ or ‘weak’ based on eight domains. These domains are selection bias, study design, confounders, blinding, data collection methods, withdrawals and drop-outs, intervention integrity and analysis. 23 NOS rates the study based on three domains viz. selection, comparability and outcome, and the final score ranges between 0 and 10. 24 Reviewers (BTV, ER and SSP), independently in pairs, will appraise the included studies. Any discrepancies between the decisions of reviewers will be resolved by discussion until consensus is achieved. If required, a senior reviewer will be involved as arbitrator and final decision maker to rate the study quality.
Data analysis
Study characteristics consisting of population, intervention/exposure, comparator, outcome, study design components across studies will be tabulated, which will help us to compare and analyse. Subsequently, studies will be categorised into quantitative and qualitative and will be analysed separately. This step will be followed by mixed methods synthesis as suggested by Panda et al . 25
Quantitative studies
Studies will be grouped based on study design, and type of data available (continuous or categorical). If possible, similar studies will be pooled to perform meta-analysis using random effect model. If data are continuous, standardised mean difference will be calculated with 95% CI. For categorical data, OR or risk ratio will be calculated and reported with 95% CI. Meta-analysis will be visually represented with a forest plot. We assume possibility of heterogeneity owing to differences in study design or analysis, intervention, type of insurance and other contextual factors. If heterogeneity exists due to aforementioned components, we will not perform meta-analysis. After ruling out clinical or methodological heterogeneity, we will statistically measure heterogeneity by using I 2 test. If significant heterogeneity (>50%) persists for a particular outcome, meta-analysis will not be conducted. In this case, our focus would be on conducting narrative synthesis and undertaking a subgroup analysis. Key findings of the studies will be summarised in tables/figures or vote counting will be considered. Subgroups could be based on study design, intervention type, insurance type (such as private and public), region and other contextual factors (eg, urban/rural).
Qualitative synthesis
We will carry out thematic analysis as suggested by Thomas and Harden. 26 An iterative process of line-by-line coding will be undertaken as a first step, which will be followed by categorising the codes into code families. Subsequently, a code tree will be created, and themes and subthemes will be generated. Three reviewers (SSP, ER and BTV) will code the data independently and resolve the discrepancies by discussion until consensus is achieved.
Mixed-methods synthesis
The result from both, qualitative and quantitative synthesis will be merged for each outcome. Parallel synthesis will be carried out, and the findings will be summarised narratively. 25 To understand the influence of inequality in uptake of health insurance based on type of insurance, we will explore the possibility of conducting subgroup analysis based on some of the components of PROGRESS ( P lace of residence, R ace/ethnicty/culture/language, O ccupation, G ender, R eligion, E ducation, S ocio-economic status, S ocial capital)-Plus framework. 27
Grading the evidence
We will use the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach to evaluate the certainty of evidence for each outcome. 21 Using GRADE profiler software, we will present the main findings of the systematic review in a summary of findings table.
Patient and public involvement
We did not involve patients or public while designing and writing this protocol.
This review will be based on published studies, therefore, an ethical clearance is not applicable. We have planned following activities to communicate and disseminate the findings of this review. We plan to make at least one national or international conference presentation. We will prepare policy brief to be shared with funder and to get a wider reader, we plan to submit the manuscript to a peer-reviewed journal. On journal publication, we intend to circulate the findings through our social media platform and website.
Supplementary Material
Acknowledgments.
We are grateful to Dr Prachi Pundir, Research Officer, public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, for proof reading the final document.
Twitter: @ParsekarShrads
Contributors: RB is the guarantor of the review. RB, SSP, ER and BTV conceptualised the manuscript. SSP drafted the first manuscript, which was further edited by ER. RV developed the search strategy. All the authors (RB, BU, SSP, ER, RV and BTV) read, edited, provided feedback and approved the final manuscript.
Funding: This work was supported by PHRI-RESEARCH grants awarded by PHFI with the financial support of Department of Science and Technology (DST). We appreciate the technical support provided by public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal.
Disclaimer: Funder did not have any role in writing this protocol and decision to submit it for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
We use cookies to ensure best experience for you
We use cookies and other tracking technologies to improve your browsing experience on our site, show personalize content and targeted ads, analyze site traffic, and understand where our audience is coming from. You can also read our privacy policy , We use cookies to ensure the best experience for you on our website.
- Leaders Speak
- Brand Solutions
- Research & Development
- Eli Lilly's weight-loss drug cuts diabetes risk by 94% in three-year trial
- Updated On Aug 20, 2024 at 06:40 PM IST

- Published On Aug 20, 2024 at 06:36 PM IST
All Comments
By commenting, you agree to the Prohibited Content Policy
Find this Comment Offensive?
- Foul Language
- Inciting hatred against a certain community
- Out of Context / Spam
Join the community of 2M+ industry professionals
Subscribe to our newsletter to get latest insights & analysis., download ethealthworld app.
- Get Realtime updates
- Save your favourite articles
- weight-loss drug
- diabetes risk
- type 2 diabetes
- tirzepatide
- obesity drugs
- Novo Nordisk
- insurance coverage
- metabolic space
- BMO Capital Markets
- Health news
- Pharma Home

IMAGES
COMMENTS
The present paper is an attempt to outline the current picture of health insurance sector in India which is a part and parcel of general insurance. Health insurance sector in India has gained huge ...
The growth of health insurance in India has been from Rs.1909 crores for the financial year 2006-2007 to Rs. 33011crores for the financial year 2018-2019. The growth percentage is 1629% i.e. growing at an average rate of 135% per annum. Compounded Annual Growth Rate (CAGR) is working out to be 27%.
Introduction. India has a complex and mixed healthcare framework with presence of parallel public and private healthcare systems. 1 2 There is a stark difference in government spending on both public and private healthcare. 3 Health policies in India have been guided by the principle of equity with prioritising the needs of the poor and underprivileged. 4 Out-of-pocket expenditure (OOPE) for ...
India has run multiple Government-Funded Health Insurance schemes (GFHIS) over the past decades to ensure affordable healthcare. We assessed GFHIS evolution with a special focus on two national schemes - Rashtriya Swasthya Bima Yojana (RSBY) and Pradhan Mantri Jan Arogya Yojana (PMJAY). RSBY suffered from a static financial coverage cap, low enrollment, inequitable service supply, utilization ...
The public-sector non-life insurance, standalone health insurance, and private non-life insurance companies had shares of 52%, 24%, and 24%, respectively, in health insurance premium collected. Out of the three broad lines of business, that is, group, individual, and government, from 2014-2015 to 2018-2019, there was a decrease in the share ...
Introduction Health insurance is one of the important approaches that can help in boosting universal healthcare coverage through improved healthcare utilisation and financial protection. This objectives of this review are to identify various interventions implemented in India to promote awareness of health insurance, and to provide evidence for the effectiveness of such interventions on the ...
This type of health insurance plan is for older people in the family. It provides covers and protection from health issues during old age. 1.5.5 Maternity Health insurance. Maternity health insurance ensures coverage for maternity and other additional expenses. 1.5.6 Hospital daily cash bene t plans.
In India, Ayushman Bharat Pradhan Mantri Jan Aarogya Yojana (PMJAY), a cashless publicly financed health insurance scheme, was launched in 2018, to provide secondary and tertiary hospitalisation care for surgical and medical care to 40% of India's population. Under the PMJAY, the empanelled public and private hospitals are reimbursed, who are paid a uniform case-based bundled payment.
Effect of Health Insurance in India: A Randomized Controlled Trial. Anup Malani, Phoebe Holtzman, Kosuke Imai, Cynthia Kinnan, Morgen Miller, Shailender Swaminathan, Alessandra Voena, Bartosz Woda & Gabriella Conti. Working Paper 29576. DOI 10.3386/w29576. Issue Date December 2021.
Despite the availability of multiple health insurance schemes, evidence suggests that the uptake of health insurance in India is poor. As per the recently concluded National Sample Survey Office data, there were as low as 14% rural and 18% urban residents of India having some form of health insurance.14 The low coverage of health
In this paper we explore how India's growing commercial health insurance (CHI) segment can be reformed to deliver adequate financial protection and good health outcomes. ... 1 Dvara Research, Chennai, Tamil Nadu, India. PMID: 36504961 PMCID: PMC9727186 DOI: 10.3389/fpubh.2022.1006483 Abstract In this paper we explore how India's growing ...
Introduction: Health insurance is one of the important approaches that can help in boosting universal healthcare coverage through improved healthcare utilisation and financial protection. This objectives of this review are to identify various interventions implemented in India to promote awareness of health insurance, and to provide evidence for the effectiveness of such interventions on the ...
The present study explores the health insurance penetration in India using the latest two rounds of nationally representative datasets of the National Family Health Survey (2005-06 and 2015-16). This study identifies the covariates of households' participation and their choice for different health insurance schemes, using the average marginal ...
Research; Working Papers; ... A Field Experiment in India. Anup Malani, Cynthia Kinnan, Gabriella Conti, ... We find very few statistically significant impacts of insurance access or enrollment on health. Because there is substantial willingness-to- pay for insurance, and given how distortionary it is to raise revenue in the Indian context, we ...
This paper examines challenges to implementing health insurance in India and makes a case for anthropological studies of the social life of insurance schemes (Dao and Nichter Citation 2015) as a means of providing fresh insights to the emerging interdisciplinary field of health policy and service research (Gilson et al. Citation 2011; Mills ...
Households were assigned to free insurance, sale of insurance, sale plus cash transfer, or control. To estimate spillovers, the fraction of households offered insurance varied across villages. The opportunity to purchase insurance led to 59.91% uptake and access to free insurance to 78.71% uptake. Access increased insurance utilization.
Binny, Dr. Meenu Gupta (2017), Health insurance in India- Oppor tunities and challenges. The. paper is about present trends of health insurance sector in India. Growth oppo rtunities and ...
Several publicly financed health insurance schemes have been launched in India with the aim of providing universalizing health coverage (UHC). In this paper, we report the impact of publicly financed health insurance schemes on health service utilization, out-of-pocket (OOP) expenditure, financial risk protection and health status. Empirical research studies focussing on the impact or ...
The paper attempts to review a variety of health insurance systems in India (defined here as any mechanism which covers the risks of payment for health care at the time of its requirement), their ...
In India, Out-of-pocket expenses accounts for about 62.6% of total health expenditure - one of the highest in the world. Lack of health insurance coverage and inadequate coverage are important reasons for high out-of-pocket health expenditures. There are many Public Health Insurance Programs offered by the Government that cover the cost of hospitalization for the people below poverty line (BPL ...
We argue that ethnographic case studies could add much to existing health service and policy research, and provide a better understanding of the life cycle and impact of insurance programs on both insurance holders and healthcare providers. Drawing on preliminary fieldwork in South India and recognizing the need for a broad-based implementation ...
The Shodhganga@INFLIBNET Centre provides a platform for research students to deposit their Ph.D. theses and make it available to the entire scholarly community in open access. ... India Health Economics Health Insurance Health Services System Health System - India Public Health: Upload Date: 1-Oct-2015: University: University of Mysore ...
While, on paper, mainland China has had a 75-year commitment to universal health coverage from 1949 to 2024, in practice, access to health insurance and care has been a privilege closely related to...
A study conducted in Uganda reported that about 34% of the studied population were not aware of health insurance. 1 Whereas, proportion of people having inadequate knowledge about health insurance was found to be high in countries such as India (46%), 5 Myanmar (66%) 3 and Hispanic American in the USA (70%). 19.
London: Eli Lilly's weight-loss drug cut the risk of developing type 2 diabetes by 94 per cent in pre-diabetic adults who were overweight or obese after three years of weekly injections, the ...