- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplement Archive
- Editorial Commentaries
- Perspectives
- Cover Archive
- IDSA Journals
- Clinical Infectious Diseases
- Open Forum Infectious Diseases
- Author Guidelines
- Open Access
- Why Publish
- IDSA Journals Calls for Papers
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About The Journal of Infectious Diseases
- About the Infectious Diseases Society of America
- About the HIV Medicine Association
- IDSA COI Policy
- Editorial Board
- Self-Archiving Policy
- For Reviewers
- For Press Offices
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Unconscious bias—the role it plays and how to measure it, impact of bias on healthcare delivery, measuring bias—the implicit association test (iat), mitigating unconscious bias, call to action.
- < Previous
The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It
- Article contents
- Figures & tables
- Supplementary Data
Jasmine R Marcelin, Dawd S Siraj, Robert Victor, Shaila Kotadia, Yvonne A Maldonado, The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It, The Journal of Infectious Diseases , Volume 220, Issue Supplement_2, 15 September 2019, Pages S62–S73, https://doi.org/10.1093/infdis/jiz214
- Permissions Icon Permissions
The increasing diversity in the US population is reflected in the patients who healthcare professionals treat. Unfortunately, this diversity is not always represented by the demographic characteristics of healthcare professionals themselves. Patients from underrepresented groups in the United States can experience the effects of unintentional cognitive (unconscious) biases that derive from cultural stereotypes in ways that perpetuate health inequities. Unconscious bias can also affect healthcare professionals in many ways, including patient-clinician interactions, hiring and promotion, and their own interprofessional interactions. The strategies described in this article can help us recognize and mitigate unconscious bias and can help create an equitable environment in healthcare, including the field of infectious diseases.
There is compelling evidence that increasing diversity in the healthcare workforce improves healthcare delivery, especially to underrepresented segments of the population [ 1 , 2 ]. Although we are familiar with the term “underrepresented minority” (URM), the Association of American Medical Colleges, has coined a similar term, which can be interchangeable: “Underrepresented in medicine means those racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population” [ 3 ]. However, this definition does not include other nonracial or ethnic groups that may be underrepresented in medicine, such as lesbian, gay, bisexual, transgender, or questioning/queer (LGBTQ) individuals or persons with disabilities. US census data estimate that the prevalence of African American and Hispanic individuals in the US population is 13% and 18%, respectively [ 4 ], while the prevalence of Americans identifying as LGBT was estimated by Gallup in 2017 to be about 4.5% [ 5 ]. Yet African American and Hispanic physicians account for a mere 6% and 5%, respectively, of medical school graduates, and account for 3% and 4%, respectively, of full-time medical school faculty [ 6 ]. As for LGBTQ medical graduates, the Association of American Medical Colleges does not report their prevalence [ 6 ]. Persons with disabilities are estimated to be 8.7% of the general population [ 4 ], while the prevalence of physicians with disabilities has been estimated to be a mere 2.7% [ 7 ]. Furthermore, although women currently outnumber men in first-year medical school classes [ 8 ], gender disparities still exist at higher ranks in women’s medical careers [ 9–11 ].
Unconscious or implicit bias describes associations or attitudes that reflexively alter our perceptions, thereby affecting behavior, interactions, and decision-making [ 12–14 ]. The Institute of Medicine (now the National Academy of Medicine) notes that bias, stereotyping, and prejudice may play an important role in persisting healthcare disparities and that addressing these issues should include recruiting more medical professionals from underrepresented communities [ 1 ]. Bias may unconsciously influence the way information about an individual is processed, leading to unintended disparities that have real consequences in medical school admissions, patient care, faculty hiring, promotion, and opportunities for growth ( Figure 1 ). Compared with heterosexual peers, LGBT populations experience disparities in physical and mental health outcomes [ 15 , 16 ]. Stigma and bias (both conscious and unconscious) projected by medical professionals toward the LGBTQ population play a major role in perpetuating these disparities [ 17 ]. Interventions on how to mitigate this bias that draw roots from race/ethnicity or gender bias literature can also be applied to bias toward gender/sexual minorities and other underrepresented groups in medicine.

Glossary of key terms.
The specialty of infectious diseases is not free from disparities. Of >11 000 members of the Infectious Diseases Society of America (IDSA), 41% identify as women, 4% identify as African American, 8% identify as Hispanic, and <1% identify as Native American or Pacific Islander (personal communication, Chris Busky, IDSA chief executive officer, 2019). However, IDSA data on members who identify as LGBTQ and members with disabilities are not available.
The 2017 IDSA annual compensation survey reports that women earn a lower income than men [ 18 ], and a review of the full report demonstrates similar disparities among URM physicians, compared with their white peers [ 19 ]. While it may not be feasible to assign a direct causal relationship between unconscious bias and disparities within the infectious diseases specialty, it is reasonable and ethical to attempt to address any potential relationship between the two. In this article, we define unconscious bias and describe its effect on healthcare professionals. We also provide strategies to identify and mitigate unconscious bias at an organizational and individual level, which can be applied in both academic and nonacademic settings.
Even in 2019, overt racism, misogyny, and transphobia/homophobia continue to influence current events. However, in the decades since the healthcare community has moved toward becoming more egalitarian, overt discrimination in medicine based on gender, race, ethnicity, or other factors have become less conspicuous. Nevertheless, unconscious bias still influences all human interactions [ 13 ]. The ability to rapidly categorize every person or thing we encounter is thought to be an evolutionary development to ensure survival; early ancestors needed to decide quickly whether a person, animal, or situation they encountered was likely to be friendly or dangerous [ 20 ]. Centuries later, these innate tendencies to categorize everything we encounter is a shortcut that our brains still use.
Stereotypes also inadvertently play a significant role in medical education ( Figure 1 ). Presentation of patients and clinical vignettes often begin with a patient’s age, presumed gender, and presumed racial identity. Automatic associations and mnemonics help medical students remember that, on examination, a black child with bone pain may have sickle-cell disease or a white child with recurrent respiratory infections may have cystic fibrosis. These learning associations may be based on true prevalence rates but may not apply to individual patients. Using stereotypes in this fashion may lead to premature closure and missed diagnoses, when clinicians fail to see their patients as more than their perceived demographic characteristics. In the beginning of the human immunodeficiency virus (HIV) epidemic, the high prevalence of HIV among gay men led to initial beliefs that the disease could not be transmitted beyond the gay community. This association hampered the recognition of the disease in women, children, heterosexual men, and blood donor recipients. Furthermore, the fact that white gay men were overrepresented in early reported prevalence data likely led to lack of recognition of the epidemic in communities of color, a fact that is crucial to the demographic characteristics of today’s epidemic. Today, there is still no clear solution to learning about the epidemiology of diseases without these imprecise associations, which can impact the rapidity of accurate diagnosis and therapy.
Unconscious bias describes associations or attitudes that unknowingly alter one’s perceptions and therefore often go unrecognized by the individual, whereas conscious bias is an explicit form of bias that is based on one’s discriminatory beliefs and values and can be targeted in nature [ 14 ]. While neither form of bias belongs in the healthcare profession, conscious bias actively goes against the very ethos of medical professionals to serve all human beings regardless of identity. Conscious bias has manifested itself in severe forms of abuse within the medical profession. One notable historical example being the Tuskegee syphilis study, in which black men were targeted to determine the effects of untreated, latent syphilis. The Tuskegee study demonstrated how conscious bias, in this case manifested in the form of racism, led to the unethical treatment of black men that continues to have long-lasting effects on health equity and justice in today’s society [ 21 ]. Given the intentional nature of conscious bias, a different set of tools and a greater length of time are likely required to change one’s attitudes and actions. Tackling unconscious bias involves willingness to alter one’s behaviors regardless of intent, when the impact of one’s biases are uncovered and addressed [ 22 ]
There is still debate, however, about the degree to which unconscious bias affects clinician decision-making. In one systematic review on the impact of unconscious bias on healthcare delivery, there was strong evidence demonstrating the prevalence of unconscious bias (encompassing race/ethnicity, gender, socioeconomic status, age, weight, persons living with HIV, disability, and persons who inject drugs) affecting clinical judgment and the behavior of physicians and nurses toward patients [ 12 ]. However, another systematic review found only moderate-quality evidence that unconscious racial bias affects clinical decision-making [ 23 ]. A detailed discussion of the impact of unconscious bias on healthcare delivery is out of the scope of this article, which is focused on the impact of unconscious bias as it relates to healthcare professionals themselves. Nevertheless, strategies to mitigate the effects of unconscious bias (discussed later) can be applied to healthcare delivery and patient interactions.
While we know that unconscious bias is ubiquitous, it can be difficult to know how much it affects a person’s daily interactions. In many cases, an individual’s unconscious beliefs may differ from their explicit actions. For example, healthcare professionals, if asked, might say they try to treat all patients equally and may not believe they hold negative attitudes about patients. However, by definition, they may lack awareness of their own potential unconscious biases, and their actions may unknowingly suggest that these biases are active.
To measure unconscious bias, Drs Mahzarin Banaji and Anthony Greenwald developed the IAT in 1998 [ 24 ]. Many versions of the IAT are accessible online (available at: https://implicit.harvard.edu/implicit/ ), but one of the most studied is the Race IAT. The IAT has been extensively studied as an inexpensive tool that provides feedback on an individual biases for self-reflection. The IAT calculates how quickly people associate different terms with each other. To determine unconscious race bias, the race IAT asks the subject to sort pictures (of white and black people) and words (good or bad) into pairs. For example, in one part of the Race IAT, participants must associate good words with white people and bad words with black people. In another part of the Race IAT, they must associate good words with black people and bad words with white people. Based on the reaction times needed to perform these tasks, the software calculates a bias score [ 20 , 24 ]. Category pairs that are unconsciously preferred are easier to sort (and therefore take less time) than those that are not [ 24 ]. These unconscious associations can be identified even in individuals who outwardly express egalitarian beliefs [ 20 , 24 ]. According to Project Implicit, the Race IAT has been taken >4 million times between 2002 and 2017, and 75% of test takers demonstrate an automatic white preference, meaning that most people (including a small group of black people) automatically associate white people with goodness and black people with badness [ 20 ]. Proponents of the IAT state that automatic preference for one group over another can signal potential discriminatory behavior even when the individuals with the automatic preference outwardly express egalitarian beliefs [ 20 ]. These preferences do not necessarily mean that an individual is prejudiced, which is associated with outward expressions of negative attitudes toward different social groups [ 20 ].
Many of the studies of unconscious bias described in this article use the IAT as the primary tool for measuring the phenomenon. Nevertheless, the degree to which the IAT predicts behavior is as of yet unclear, and it is important to recognize the limitations and criticisms of the IAT, as this is pertinent to its potential application in mitigating unconscious bias. Blanton et al reanalyzed data from 2 studies supporting the validity of the IAT, claiming that there is no evidence predicting individual behavior, with concerns for interjudge reliability and inclusion of outliers affecting results [ 25 ]. Response to this criticism by McConnell et al describes extensive training of test judges and evidence that the reanalysis was not a perfect replication of methods [ 26 ]. Blanton et al argue further in a different article that attempting to explain behavior on the basis of results of the IAT is problematic because the test relies on an arbitrary metric, leading to identified preferences when individuals are “behaviorally neutral” [ 27 ]. Notwithstanding the limitations of the IAT, none of its critics refute the existence of unconscious bias and that it can influence life experiences. The following sections review how unconscious bias affects different groups in the healthcare workforce.
Racial Bias
Medical school admissions committees serve as an important gatekeeper to address the significant disparities between racial and ethnic minorities in healthcare as compared to the general population. Yet one study demonstrated that members of a medical school admissions committee displayed significant unconscious white preference (especially among men and faculty members) despite acknowledging almost zero explicit white preference [ 28 ]. An earlier study of unconscious racial and social bias in medical students found unconscious white and upper-class preference on the IAT but no obvious unconscious preferences in students’ response to vignette-based patient assessments [ 29 ]. Unconscious bias affects the lived experiences of trainees, can potentially influence decisions to pursue certain specialties, and may lead to isolation. A recent study by Osseo-Asare et al described African American residents’ experiences of being only “one of a few” minority physicians; some major themes included discrimination, the presence of daily microaggressions, and the burden of being tasked as race/ethnic “ambassadors,” expected to speak on behalf of their demographic group [ 30 ].
Gender Bias
Gender bias in medical education and leadership development has been well documented [ 11 , 31 ]. Medical student evaluations vary depending on the gender of the student and even the evaluator [ 31 ]. Similar studies have demonstrated gender bias in qualitative evaluations of residents and letters of recommendations, with a more positive tone and use of agentic descriptors in evaluations of male residents as compared to female residents [ 11 ]. Studies evaluating inclusion of women as speakers have also demonstrated gender bias, with fewer women invited to speak at grand rounds [ 9 ] and differences in the formal introductions of female speakers as compared to male speakers [ 32 , 33 ], with men more likely referred to by their official titles than women.
Sexual and Gender Minority Bias
Sexual and gender minority groups are underrepresented in medicine and experience bias and microaggressions similar to those experience by racial and ethnic minorities. Experiences with or perceptions of bias lead to junior physicians not disclosing their sexual identity on the personal statement part of their residency applications for fear of application rejection or not disclosing that they are gay to colleagues and supervisors for fear of rejection or poor evaluations [ 34 ]. In one study, some physician survey respondents indicated some level of discomfort about people who are gay, transgender, or living with HIV being admitted to medical school. These respondents were less likely to refer patients to physician colleagues who were gay, transgender, or living with HIV [ 35 ]. These explicit biases were significantly reduced, compared with those revealed in prior surveys done in 1982 and 1999; opposition to gay medical school applicants went from 30% in 1982 to 0.4% in 2017, and discomfort with referring patients to gay physicians went from 46% in 1982 to 2% in 2017 [ 35 ]. The 2017 survey did not measure levels of unconscious bias, which is likely to still be pervasive despite decreased explicit bias. As with other types of bias, these data reveal that explicit bias against gay physicians has decreased over time; the degree of unconscious bias, however, likely persists. While this is encouraging to some degree, unconscious bias may be much more challenging to confront than explicit bias. Thus, members of underrepresented groups may be left wondering about the intentions of others and being labeled as “too sensitive.”
Studies including the perspectives of LGBTQ healthcare professionals demonstrate that major challenges to their academic careers persist to this day. These include lack of LGBTQ mentorship, poor recognition of scholarship opportunities, and noninclusive or even hostile institutional climates [ 36 ]. Phelan et al studied changes in biased attitudes toward sexual and gender minorities during medical school and found that reduced unconscious and explicit bias was associated with more-frequent and favorable interactions with LGBTQ students, faculty, residents, and patients [ 37 ].
Disability Bias
Physicians with disabilities constitute another minority group that may experience bias in medicine, and the degree to which they experience this may vary, depending on whether disabilities may be visible or invisible. One study estimated the prevalence of self-disclosed disability in US medical students to be 2.7% [ 7 ]. Medical schools are charged with complying with the Americans With Disabilities Act, but only a minority of schools support the full spectrum of accommodations for students with disabilities [ 38 ]. Many schools do not include a specific curriculum for disability awareness [ 39 ]. Physicians with disabilities have felt compelled to work twice as hard as their able-bodied peers for acceptance, struggled with stigma and microaggressions, and encountered institutional climates where they generally felt like they did not belong [ 40 ]. These are themes that are shared by individuals from racial and ethnic minorities.
A strategy to counter unconscious bias requires an intentional multidimensional approach and usually operates in tandem with strategies to increase diversity, inclusion, and equity [ 41 , 42 ]. This is becoming increasingly important in training programs in the various specialties, including infectious diseases. The Accreditation Council for Graduate Medical Education recently updated their common program requirements for fellowship programs and has stipulated that, effective July 2019, “[t]he program’s annual evaluation must include an assessment of the program’s efforts to recruit and retain a diverse workforce” [ 43 ]. The implication of this requirement is that recognition and mitigation of potential biases that may influence retention of a diverse workforce will ultimately be evaluated (directly or indirectly).
Mitigating unconscious bias and improving inclusivity is a long-term goal requiring constant attention and repetition and a combination of general strategies that can have a positive influence across all groups of people affected by bias [ 44 ]. These strategies can be implemented at organizational and individual levels and, in some cases, can overlap between the 2 domains ( Figure 2 ). In this section, we review how infectious diseases clinicians and organizations like IDSA and hospitals can use some of these strategies to address and mitigate implicit bias in our specialty.

Organization-level and personal-level strategies to mitigate unconscious bias. Orange circles indicate organization-specific strategies, green circles indicate individual-level strategies, and blue circles represent strategies that can be emphasized on both organizational and individual levels to mitigate implicit bias.
Organizational Strategies
Commitment to a culture of inclusion: more than just diversity training or cultural competency.
Creating change requires more than just a climate survey, a vision statement, or creation of a diversity committee [ 45 ]. Organizations must commit to a culture shift by building institutional capacity for change [ 41 , 46 ]. This involves reaffirming the need not only for the recruitment of a critical mass of underrepresented individuals, but equally importantly, the recruitment of critical actor leaders who take the role of change agents and have the power to create equitable environments [ 41 , 47–49 ]. These change agents need not themselves be underrepresented; indeed, the success of culture change requires the involvement of allies within the majority group (eg, men, white people, and cis-gender heterosexual individuals). IDSA has demonstrated a commitment to this type of culture change with recent changes in leadership structure and with intentional recruitment of individuals invested in diversity and inclusion; however, there is always room for reevaluation of other areas where diversity is desired.
Committing to a culture of inclusion at the academic-institution level involves creating a deliberate strategy for medical trainee admission and evaluation and faculty hiring, promotion, and retention. Capers et al describe strategies for achieving diversity through medical school admissions, many of which can also be applied to faculty hiring and promotion [ 49 ]. Notable strategies they suggest include having admissions (or hiring) committee members take the IAT and reflect on their own potential biases before they review applications or interview candidates [ 49 ]. They also recommend appointing women, minorities, and junior medical professionals (students or junior faculty) to admissions committees, emphasizing the importance of different perspectives and backgrounds [ 49 ]. Organizations can also survey employee perception of inclusivity. These assessments include questions on the degree to which an individual feels a sense of belonging within an institution, alongside questions pertaining to experiences of bias on the grounds of cultural or demographic factors [ 50 ]. Conducting regular assessments and analysis of survey results, particularly on how individuals of diverse backgrounds feel they can exist within the organization and their culture simultaneously, allows organizations to ensure that their trainings on unconscious bias and promotion of cultural humility lead to long-term positive change. Furthermore, realizing that different demographic groups may feel less respected than others provides information on areas of focus for consequent refresher seminars on combating unconscious bias in conjunction with cultural humility.
Meaningful Diversity Training and the Usefulness of the IAT
Notwithstanding potential criticisms of the IAT with respect to prediction of discriminatory behavior, this can be a useful tool within a comprehensive organizational training seminar directed toward understanding and addressing individual unconscious bias. In the study by Capers et al, over two thirds of admissions committee members who took the IAT and responded to the post-IAT survey felt positive about the potential value of this tool in reducing their unconscious bias [ 28 ]. Additionally, almost half were cognizant of their IAT results when interviewing for the next admissions cycle, and 21% maintained that knowledge of this bias affected their decisions in the next admissions cycle [ 28 ]. Perhaps this knowledge led to conscious changes in committee member behavior because, in the following year, the matriculating class was the most diverse in that institution’s history [ 28 , 49 ]. A similar bias education intervention coupled with the IAT led to a decreased unconscious gender leadership bias in one academic center [ 48 ]. IDSA and infectious diseases practices (or academic divisions) could consider ways to incorporate this into already established training for those in leadership roles or on leadership search committees.
Of course, the potential applicability of the IAT can be overstated—at best, several meta-analyses have demonstrated that there may only be a weak correlation between IAT scores and individual behavior [ 51–53 ], and several criticisms of the IAT have already been discussed here. Additionally, while important to acknowledge that bias is pervasive, care must be taken to avoid normalizing bias and stereotypes because this may have the unintended consequence of reinforcing them [ 54 ]. Important points that should be emphasized when using the IAT as part of diversity training include that (1) people should be aware of their own biases and reflect on their behaviors individually; (2) the IAT can suggest generally how groups of people with certain results may behave, rather than how each individual will behave; and (3) on its own, the IAT is not a sufficient tool to mitigate the effects of bias, because if there is to be any chance of success, an active cultural/behavioral change must be engaged in tandem with bias awareness and diversity training [ 55 ].
Individual Strategies
Deliberative reflection.
Before encounters that are likely to be affected by bias (such as trainee evaluations, letters of recommendation, feedback, interviews, committee decisions, and patient encounters), deliberative reflection can help an individual recognize their own potential for bias and correct for this [ 56 ]. It is also a good time to consider the perspective of the individual whom they will be evaluating or interacting with and the potential impact of their biases on that individual. Participants can be encouraged to evaluate how their own experiences and identities influence their interactions. Including data on lapses in proper care due to provider bias also proves helpful in giving workers real-life examples of the consequences of not being vigilant for bias [ 51 , 57 ]. This motivated self-regulation based on reflections of individual biases has been shown to reduce stereotype activation and application [ 44 , 58 ]. If one unintentionally behaves in a discriminatory manner, self-reflection and open discussion can help to repair relationships ( Figure 3 ).

Strategies to address personal bias before and after it occurs.
Question and Actively Counter Stereotypes
Individuals may question how they can actively counter stereotypes and bias in observed interactions. The active-bystander approach adapted from the Kirwan Institute [ 59 ] can provide insight into appropriate responses in these situations ( Figure 4 ).

Kirwan Institute approach to countering unconscious bias as an active bystander.
Strategies That Apply to Both Organizations and Individuals
Cultural competency and beyond: cultural humility.
Healthcare organizations seeking to develop providers who can work seamlessly with colleagues and more effectively treat patients from all cultural backgrounds have been conducting trainings in cultural competency [ 60 ]. The term “cultural competency” implies that one has achieved a static goal of championing inclusivity. This approach imparts a false sense of confidence in leaders and healthcare professionals and fails to recognize that our understanding of cultural barriers is continually growing and evolving [ 61 ]. Cultural humility has been proposed as an alternate approach, subsuming the teachings of cultural competency while steering participants toward a continuous path of discovery and respect during interactions with colleagues and patients of different cultural backgrounds [ 62 ]. Other synonymous terms include “cultural sensitivity” and “cultural curiosity.” Rather than checking a box for training, cultural humility focuses on the individual and teaches that developing one’s self-awareness is a critical step in achieving mindfulness for others [ 63 ]. Cultural humility emphasizes that individuals must acknowledge the experiential lens through which they view the world and that their view is not nearly as extensive, open, or dynamic as they might perceive [ 61 ]. By training leaders and healthcare professionals that they do not need to be and ultimately cannot be experts in all the intersecting cultures that they encounter, healthcare professionals can focus on a readiness to learn that can translate to greater confidence and willingness in caring for patients of varying backgrounds [ 61 ].
As cultural humility is important to recognizing and mitigating conscious and unconscious biases, patient simulations and diversity-related trainings should be augmented with discussions about cultural humility. By integrating cultural humility into healthcare training procedures, organizations can strive to eliminate the perceived unease healthcare professionals might experience when interacting with individuals from backgrounds or cultures unfamiliar to them. Cultural humility starts from a condition of empathy and proceeds through the asking of open questions in each interaction ( Figure 1 ). Instilling elements of cultural humility training within simulation-based learning provides participants with experience in treating a wide array of patients while providing low-risk, feedback-based learning opportunities [ 22 , 64 ].
Diversify Experiences to Provide Counterstereotypical Interactions
Exposing individuals to counterstereotypical experiences can have a positive impact on unconscious bias [ 10 , 44 , 55 ]. Therefore, intentional efforts to include faculty from underrepresented groups as preceptors, educators, and invited speakers can help reduce the unconscious associations of these responsibilities as unattainable. Capers et al suggest that including students, women, and African Americans and other racial and ethnic minorities on admissions committees may be part of a strategy to reduce unconscious bias in medical school admissions [ 49 ]. If institutions, organizations, and conference program committees are aware of their own metrics in this respect, following this information with deliberate choices to remedy inequities can have a profound impact on increasing diversity [ 65 ]. Furthermore, in medical training, while deliberate curricula involving disparities and care of underrepresented individuals are beneficial, educators must be aware of the impact of the hidden curriculum on their trainees. The term “hidden curriculum” refers to the aspects of medicine that are learned by trainees outside the traditional classroom/didactic instruction environment. It encompasses observed interactions, behaviors, and experiences often driven by unconscious and explicit bias and institutional climate [ 66–68 ]. Students can be taught to actively seek out the hidden curriculum in their training environment, reflect on the lessons, and use this reflection to inform their own behaviors [ 67 ]. Individuals can intentionally diversify their own circles, connecting with people from different backgrounds and experiences. This can include the occasionally awkward and uncomfortable introductions at professional meetings or at community events, making an effort to read books by diverse authors, or trying new foods with a colleague. These are small behavioral changes that, with time, can help to retrain our brain to classify people as “same” instead of “other.”
Mentorship and Sponsorship
Mentors can, at any stage in one’s career, provide advice and career assistance with collaborations, but sponsors are typically more senior individuals who can curate high-profile opportunities to support a junior person, often with potential personal or professional risk if that person does not meet expectations. URMs and women physicians tend not to have as much support with mentoring and sponsorship as the majority group, white men. Qualitative studies of URM physician perspectives typically reveal themes of isolation and lack of mentorship, regardless of the URM group being studied [ 30 , 36 , 69 ]. Possible reasons include lack of mentors from similar backgrounds or ineffective mentoring in discordant mentor-mentee relationships. Mentor-training workshops that intentionally include unconscious bias training can enhance the effectiveness of mentors working with diverse trainees and junior faculty and address this potential barrier to URM success [ 70 ]. Providing mentorship within an individual department, as well as support for participating in external mentorship and career development programs, can help create sponsorship opportunities that eventually influence career advancement [ 41 ]. Many professional societies such as IDSA provide mentorship opportunities, and these can be enhanced by encouraging more sponsorship of junior clinicians for opportunities such as podium lectures, moderating at conferences, writing editorials, or committee positions.
In the years since the IAT was first described, researchers have published countless data on the impact of unconscious bias. Fortunately, explicit and implicit attitudes toward many disenfranchised groups of people have regressed to a more neutral position over time [ 71 ], but this does not mean that unconscious bias has disappeared. Just as healthcare providers are required to stay up to date on medical techniques and procedures to best serve their patients, we propose that trainings involving the social aspects of medicine be treated similarly. Cultural humility is characterized by lifelong learning and is a key aspect of a successful provider-patient relationship. Thus, it is imperative that healthcare organizations and professional medical societies such as IDSA continually provide healthcare professionals with learning opportunities to enhance their interactions with individuals different from themselves. Effectively addressing unconscious bias and subsequent disparities in IDSA will need comprehensive, multifaceted, and evidence-based interventions ( Figure 5 ).

Unconscious bias highlights.
IDSA has demonstrated a commitment to diversifying its society leadership by commissioning the Gender Disparities Task Force and the Inclusion, Diversity, Access & Equity Task Force, reconfiguring existing committees, developing new committees (eg, the Leadership Development Committee), and creating new opportunities, such as the IDSA Leadership Institute. While these are important and impactful actions, we propose the following additional steps to address the role of unconscious bias in various settings. First, develop an IDSA-sponsored climate survey to assess perceptions of inclusion and belonging within the Society, and repeat this climate assessment after implementing bias reduction strategies. Second, provide IDSA-sponsored education/training on unconscious bias reduction strategies and cultural humility to academic infectious disease divisions and fellowship programs to support the recruitment and retention of a diverse infectious diseases physician workforce. Third, develop benchmarks for excellence in infectious diseases divisions and fellowship training programs to evaluate these bias reduction strategies. Fourth, provide education/training on unconscious bias–reduction strategies and cultural humility to leadership and membership within IDSA. Specifically, the board of directors, the Leadership Development Committee, the Awards Committee, and others involved in electing, nominating, or honoring members should consider including incorporating the IAT and bias-reduction education for their committee members. After implementing such strategies, IDSA should reevaluate metrics of awardees, committee chairs, and leadership to determine whether these strategies made an impact. Fifth, cultivate existing mentorship programs within IDSA, with the added focus of intentional mentoring and sponsorship of groups traditionally underrepresented in leadership. Sixth, commit to consistent review and revision of infectious diseases recruitment messaging, ensuring that materials and media counter harmful stereotypes and represent true diversity. Seventh, collect, review, and publish metrics of diversity in all facets of the membership, including IDWeek speaker demographic characteristics, IDSA journal editor/reviewers, guideline authorship, and committee membership, with intentional response strategies to change these demographic characteristics to a more diverse distribution. Eighth, be transparent about reporting of metrics, with clear accountability and flexibility to adjust initiatives based on results.
Although there are numerous data describing the impact of unconscious bias on healthcare delivery, clinician-patient interactions, and patient outcomes, discussion of these aspects is out of the scope of this article, which focuses on the impact of unconscious bias on healthcare professionals. Additionally, the majority of data on unconscious bias presented in this article relates to general academic training and career development, as data in the infectious diseases practice community is limited. This represents an area of need for evaluation within the specialty of infectious diseases, since a vast majority of members are in clinical practice and may experience bias in varying degrees. While it is important to support trainees who may experience unconscious bias, it is also critical to provide support for infectious diseases clinicians further along in their careers, as a means to maintain retention in the specialty. Finally, some individuals may prefer person-first language, while others may prefer identity-first language when referring to disabilities. We consistently used person-first language throughout this manuscript based on the recommendation by the Centers for Disease Control & Prevention ( https://www.cdc.gov/ncbddd/disabilityandhealth/pdf/disabilityposter_photos.pdf ).
Supplement sponsorship . This supplement is sponsored by the Infectious Diseases Society of America.
Acknowledgments . We thank Drs Molly Carnes, Ranna Parekh, and Arghavan Salles, as well as Lena Tenney, for critical review of this manuscript before publication; Mr Chris Busky, for providing written communications about the demographic characteristics of IDSA membership and leadership; and Catherine Hiller, for her assistance with manuscript preparation.
J. R. M. wrote first draft and subsequent revisions; D. S. and R. V. contributed to the first draft and subsequent revisions; S. K. contributed to the first draft and subsequent revisions; Y. A. M. contributed to subsequent revisions; and all authors reviewed a final version of the work before submission.
Potential conflicts of interest . J. R. M. and D. S. are members of the IDSA Inclusion, Diversity, Access & Equity Task Force. All other authors report no potential conflicts.
All authors have submitted the ICMJE form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Institute of Medicine (US) Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Healthcare Workforce . In the nation’s compelling interest: ensuring diversity in the health-care workforce . Smedley BD , Stith Butler A , Bristow LR , eds. Washington, DC : National Academies Press (US) , 2004 .
Google Scholar
Google Preview
American College of Physicians . Racial and ethnic disparities in health care, updated 2010 . https://www.acponline.org/system/files/documents/advocacy/current_policy_papers/assets/racial_disparities.pdf . Accessed 25 January 2019 .
Association of American Medical Colleges . Underrepresented in medicine definition . https://www.aamc.org/initiatives/urm/ . Accessed 19 January 2019 .
United States Census Bureau . US Census Bureau QuickFacts . https://www.census.gov/quickfacts/fact/table/US# . Accessed 2 January 2019 .
Newport F. In U.S., estimate of LGBT population rises to 4.5% . https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx . Accessed 25 January 2019 .
Association of American Medical Colleges (AAMC) . AAMC facts & figures 2016; diversity in medical education . http://www.aamcdiversityfactsandfigures2016.org/index.html . Accessed 25 January 2019 .
Meeks LM , Herzer KR . Prevalence of self-disclosed disability among medical students in US allopathic medical schools . JAMA 2016 ; 316 : 2271 – 2 .
Association of American Medical Colleges . U.S. medical school applications and matriculants by school, state of legal residence, and sex, 2018–2019 . https://www.aamc.org/download/321442/data/factstablea1.pdf . Accessed 4 January 2019 .
Boiko JR , Anderson AJM , Gordon RA . Representation of women among academic grand rounds speakers . JAMA Intern Med 2017 ; 177 : 722 – 4 .
Carnes M , Bartels CM , Kaatz A , Kolehmainen C . Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc 2015 ; 126 : 197 – 214 .
Gerull KM , Loe M , Seiler K , McAllister J , Salles A . Assessing gender bias in qualitative evaluations of surgical residents . Am J Surg 2019 ; 217 : 306 – 13 .
FitzGerald C , Hurst S . Implicit bias in healthcare professionals: a systematic review . BMC Med Ethics 2017 ; 18 .
Staats C , Dandar V , St Cloud T , Wright R . How the prejudices we don’t know we have affect medical education, medical careers, and patient health . In: Darcy Lewis and Emily Paulsen, eds. Proceedings of the 2014 diversity and inclusion innovation forum: unconscious bias in academic medicine . Association of American Medical Colleges . Association of American Medical Colleges and the Kirwan Institute for the Study of Race and Ethnicity at The Ohio State University, USA 2017;1–93.
Staats C , Patton C. State of the science: implicit bias review: the Ohio State University Kirwan Instiute for the study of race and ethnicity . OH : The Kirwan Institute for the Study of Race and Ethnicity at The Ohio State University , 2013 ; 1 – 102 .
Institute of Medicine . The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding . Washington, DC : The National Academies Press , 2011 .
Gonzales G , Przedworski J , Henning-Smith C . Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the united states: results from the national health interview survey . JAMA Intern Med 2016 ; 176 : 1344 – 51 .
Valdiserri RO , Holtgrave DR , Poteat TC , Beyrer C . Unraveling health disparities among sexual and gender minorities: a commentary on the persistent impact of stigma . J Homosex 2019 ; 66 : 571 – 89 .
Trotman R , Kim AI , MacIntyre AT , Ritter JT , Malani AN . 2017 infectious diseases society of america physician compensation survey: results and analysis . Open Forum Infect Dis 2018 ; 5 : ofy309 .
Marcelin JR , Bares SH , Fadul N . Improved infectious diseases physician compensation but continued disparities for women and underrepresented minorities . Open Forum Infect Dis 2019 ; 6 : ofz042 .
Banaji MR , Greenwald AG. Blindspot: hidden biases of good people . 1st ed. USA : Delacorte Press , 2013 .
Francis CK . Medical ethos and social responsibility in clinical medicine . J Urban Health 2001 ; 78 : 29 – 45 .
Teal CR , Gill AC , Green AR , Crandall S . Helping medical learners recognise and manage unconscious bias toward certain patient groups . Med Educ 2012 ; 46 : 80 – 8 .
Dehon E , Weiss N , Jones J , Faulconer W , Hinton E , Sterling S . A systematic review of the impact of physician implicit racial bias on clinical decision making . Acad Emerg Med 2017 ; 24 : 895 – 904 .
Greenwald AG , McGhee DE , Schwartz JL . Measuring individual differences in implicit cognition: the implicit association test . J Pers Soc Psychol 1998 ; 74 : 1464 – 80 .
Blanton H , Jaccard J , Klick J , Mellers B , Mitchell G , Tetlock PE . Strong claims and weak evidence: reassessing the predictive validity of the IAT . J Appl Psychol 2009 ; 94 : 567 – 82 ; discussion 583–603.
McConnell AR , Leibold JM. Weak criticisms and selective evidence: Reply to Blanton et al . (2009) . J Appl Psychol , 2009;94, 583-9. doi:10.1037/a0014649
Blanton H , Jaccard J , Strauts E , Mitchell G , Tetlock PE . Toward a meaningful metric of implicit prejudice . J Appl Psychol 2015 ; 100 : 1468 – 81 .
Capers Q 4th , Clinchot D , McDougle L , Greenwald AG . Implicit racial bias in medical school admissions . Acad Med 2017 ; 92 : 365 – 9 .
Haider AH , Sexton J , Sriram N , et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students . JAMA 2011 ; 306 : 942 – 51 .
Osseo-Asare A , Balasuriya L , Huot SJ , et al. Minority resident physicians’ views on the role of race/ethnicity in their training experiences in the workplace . JAMA Netw Open 2018 ; 1 : e182723 .
Riese A , Rappaport L , Alverson B , Park S , Rockney RM . Clinical performance evaluations of third-year medical students and association with student and evaluator gender . Acad Med 2017 ; 92 : 835 – 40 .
Files JA , Mayer AP , Ko MG , et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias . J Womens Health (Larchmt) 2017 ; 26 : 413 – 9 .
Mehta S , Rose L , Cook D , Herridge M , Owais S , Metaxa V . The speaker gender gap at critical care conferences . Crit Care Med 2018 ; 46 : 991 – 996 .
Lee KP , Kelz RR , Dubé B , Morris JB . Attitude and perceptions of the other underrepresented minority in surgery . J Surg Educ 2014 ; 71 : e47 – 52 .
Marlin R , Kadakia A , Ethridge B , Mathews WC . Physician attitudes toward homosexuality and HIV: the PATHH-III survey . LGBT Health 2018 ; 5 : 431 – 42 .
Sánchez NF , Rankin S , Callahan E , et al. LGBT trainee and health professional perspectives on academic careers–facilitators and challenges . LGBT Health 2015 ; 2 : 346 – 56 .
Phelan SM , Burke SE , Hardeman RR , et al. Medical school factors associated with changes in implicit and explicit bias against gay and lesbian people among 3492 graduating medical students . J Gen Intern Med 2017 ; 32 : 1193 – 201 .
Zazove P , Case B , Moreland C , et al. U.S. medical schools’ compliance with the americans with disabilities act: findings from a national study . Acad Med 2016 ; 91 : 979 – 86 .
Seidel E , Crowe S . The state of disability awareness in american medical schools . Am J Phys Med Rehabil 2017 ; 96 : 673 – 6 .
Meeks LM , Herzer K , Jain NR . Removing barriers and facilitating access: increasing the number of physicians with disabilities . Acad Med 2018 ; 93 : 540 – 3 .
DiBrito SR , Lopez CM , Jones C , Mathur A . Reducing implicit bias: association of women surgeons #HeForShe task force best practice recommendations . J Am Coll Surg 2019 ; 228 : 303 – 9 .
South-Paul JE , Roth L , Davis PK , et al. Building diversity in a complex academic health center . Acad Med 2013 ; 88 : 1259 – 64 .
Accreditation Council for Graduate Medical Education . Common program requirements (fellowship) . https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRFellowship2019.pdf . Accessed 19 January 2019 .
Devine PG , Forscher PS , Austin AJ , Cox WT . Long-term reduction in implicit race bias: a prejudice habit-breaking intervention . J Exp Soc Psychol 2012 ; 48 : 1267 – 78 .
Carnes M , Fine E , Sheridan J . Promises and pitfalls of diversity statements: proceed with caution . Acad Med 2019 ; 94 : 20 – 4 .
Smith DG . Building institutional capacity for diversity and inclusion in academic medicine . Acad Med 2012 ; 87 : 1511 – 5 .
Helitzer DL , Newbill SL , Cardinali G , Morahan PS , Chang S , Magrane D . Changing the culture of academic medicine: critical mass or critical actors? J Womens Health (Larchmt) 2017 ; 26 : 540 – 8 .
Girod S , Fassiotto M , Grewal D , et al. Reducing implicit gender leadership bias in academic medicine with an educational intervention . Acad Med 2016 ; 91 : 1143 – 50 .
Capers Q , McDougle L , Clinchot DM . Strategies for achieving diversity through medical school admissions . J Health Care Poor Underserved 2018 ; 29 : 9 – 18 .
Person SD , Jordan CG , Allison JJ , et al. Measuring diversity and inclusion in academic medicine: the diversity engagement survey . Acad Med 2015 ; 90 : 1675 – 83 .
Greenwald AG , Banaji MR , Nosek BA . Statistically small effects of the implicit association test can have societally large effects . J Pers Soc Psychol 2015 ; 108 : 553 – 61 .
Oswald FL , Mitchell G , Blanton H , Jaccard J , Tetlock PE . Predicting ethnic and racial discrimination: a meta-analysis of IAT criterion studies . J Pers Soc Psychol 2013 ; 105 : 171 – 92 .
Oswald FL , Mitchell G , Blanton H , Jaccard J , Tetlock PE . Using the IAT to predict ethnic and racial discrimination: small effect sizes of unknown societal significance . J Pers Soc Psychol 2015 ; 108 : 562 – 71 .
Duguid MM , Thomas-Hunt MC . Condoning stereotyping? How awareness of stereotyping prevalence impacts expression of stereotypes . J Appl Psychol 2015 ; 100 : 343 – 59 .
Dasgupta N . Chapter five—implicit attitudes and beliefs adapt to situations: a decade of research on the malleability of implicit prejudice, stereotypes, and the self-concept . In: Devine P , Plant A , eds. Advances in experimental social psychology . Vol. 47 . USA: Academic Press, 2013 : 233 – 79 .
Phillips NA , Tannan SC , Kalliainen LK . Understanding and overcoming implicit gender bias in plastic surgery . Plast Reconstr Surg 2016 ; 138 : 1111 – 6 .
Nelson SC , Prasad S , Hackman HW . Training providers on issues of race and racism improve health care equity . Pediatr Blood Cancer 2015 ; 62 : 915 – 7 .
Burns MD , Monteith MJ , Parker LR . Training away bias: the differential effects of counterstereotype training and self-regulation on stereotype activation and application . J Exp Soc Psychol 2017 ; 73 : 97 – 110 .
Tenney L. Being an active bystander: strategies for challenging the emergence of bias. Columbus, OH: Ohio State University Kirwan Institute for the Study of Race and Ethnicity , 2017 .
Harrison G , Turner R . Being a ‘culturally competent’ social worker: making sense of a murky concept in practice . Br J Soc Work 2010 ; 41 : 333 – 350 .
Juarez JA , Marvel K , Brezinski KL , Glazner C , Towbin MM , Lawton S . Bridging the gap: a curriculum to teach residents cultural humility . Fam Med 2006 ; 38 : 97 – 102 .
Chang ES , Simon M , Dong X . Integrating cultural humility into health care professional education and training . Adv Health Sci Educ Theory Pract 2012 ; 17 : 269 – 78 .
Kumagai AK , Lypson ML . Beyond cultural competence: critical consciousness, social justice, and multicultural education . Acad Med 2009 ; 84 : 782 – 7 .
Beauchamp GA , McGregor AJ , Choo EK , Safdar B , Rayl Greenberg M . Incorporating sex and gender into culturally competent simulation in medical education . J Womens Health (Larchmt) 2019 . doi:10.1089/jwh.2018.7271
van Ryn M , Hardeman R , Phelan SM , et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student CHANGES study report . J Gen Intern Med 2015 ; 30 : 1748 – 56 .
Hafferty FW . Beyond curriculum reform: confronting medicine’s hidden curriculum . Acad Med 1998 ; 73 : 403 – 7 .
Neve H , Collett T . Empowering students with the hidden curriculum . Clin Teach 2018 ; 15 : 494 – 9 .
Fallin-Bennett K . Implicit bias against sexual minorities in medicine: cycles of professional influence and the role of the hidden curriculum . Acad Med 2015 ; 90 : 549 – 52 .
Liebschutz JM , Darko GO , Finley EP , Cawse JM , Bharel M , Orlander JD . In the minority: black physicians in residency and their experiences . J Natl Med Assoc 2006 ; 98 : 1441 – 8 .
Gandhi M , Fernandez A , Stoff DM , et al. Development and implementation of a workshop to enhance the effectiveness of mentors working with diverse mentees in HIV research . AIDS Res Hum Retroviruses 2014 ; 30 : 730 – 7 .
Charlesworth TES , Banaji MR . Patterns of implicit and explicit attitudes: I. Long-Term change and stability from 2007 to 2016 . Psychol Sci 2019 ; 30 : 174 – 92 .
Yeager KA , Bauer-Wu S . Cultural humility: essential foundation for clinical researchers . Appl Nurs Res 2013 ; 26 : 251 – 6 .
Sue DW , Capodilupo CM , Torino GC , et al. Racial microaggressions in everyday life: implications for clinical practice . Am Psychol 2007 ; 62 : 271 – 86 .
- bias (epidemiology)
- communicable diseases
- delivery of health care
- personnel selection
- cultural competence
- infectious diseases society of america
- mentorships
| Month: | Total Views: |
|---|---|
| August 2019 | 509 |
| September 2019 | 589 |
| October 2019 | 1,410 |
| November 2019 | 2,042 |
| December 2019 | 1,411 |
| January 2020 | 2,310 |
| February 2020 | 2,600 |
| March 2020 | 2,346 |
| April 2020 | 3,582 |
| May 2020 | 1,716 |
| June 2020 | 4,194 |
| July 2020 | 3,754 |
| August 2020 | 4,157 |
| September 2020 | 5,002 |
| October 2020 | 5,731 |
| November 2020 | 5,337 |
| December 2020 | 4,038 |
| January 2021 | 4,439 |
| February 2021 | 5,264 |
| March 2021 | 7,110 |
| April 2021 | 6,594 |
| May 2021 | 5,651 |
| June 2021 | 4,077 |
| July 2021 | 3,769 |
| August 2021 | 4,415 |
| September 2021 | 6,403 |
| October 2021 | 6,028 |
| November 2021 | 5,996 |
| December 2021 | 3,551 |
| January 2022 | 4,581 |
| February 2022 | 5,716 |
| March 2022 | 7,015 |
| April 2022 | 6,583 |
| May 2022 | 5,686 |
| June 2022 | 3,767 |
| July 2022 | 4,020 |
| August 2022 | 3,778 |
| September 2022 | 4,958 |
| October 2022 | 6,260 |
| November 2022 | 6,488 |
| December 2022 | 3,963 |
| January 2023 | 4,203 |
| February 2023 | 5,460 |
| March 2023 | 6,441 |
| April 2023 | 6,362 |
| May 2023 | 5,624 |
| June 2023 | 3,688 |
| July 2023 | 4,267 |
| August 2023 | 4,484 |
| September 2023 | 5,618 |
| October 2023 | 5,793 |
| November 2023 | 5,414 |
| December 2023 | 3,800 |
| January 2024 | 4,855 |
| February 2024 | 4,375 |
| March 2024 | 5,673 |
| April 2024 | 5,649 |
| May 2024 | 5,069 |
| June 2024 | 2,952 |
| July 2024 | 2,798 |
| August 2024 | 2,871 |
Email alerts
More on this topic, related articles in pubmed, citing articles via, looking for your next opportunity.
- Recommend to your Library
Affiliations
- Online ISSN 1537-6613
- Print ISSN 0022-1899
- Copyright © 2024 Infectious Diseases Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Patient satisfaction and experience

Getty Images
What is implicit bias, how does it affect healthcare?
Healthcare leaders working toward health equity will need to recognize their own implicit biases to truly enhance patient care..

- Sara Heath, Executive Editor
Medicine's focus on racial health disparities and health equity has brought to the forefront another key concept in healthcare delivery and patient care: implicit bias.
Implicit bias, a phrase that is not unique to healthcare, refers to the unconscious prejudice individuals might feel about another thing, group, or person.
According to the Kirwan Institute for the Study of Race and Ethnicity at the Ohio State University, implicit bias is involuntary, can refer to positive or negative attitudes and stereotypes, and can affect actions without an individual knowing it:
Also known as implicit social cognition, implicit bias refers to the attitudes or stereotypes that affect our understanding, actions, and decisions in an unconscious manner. These biases, which encompass both favorable and unfavorable assessments, are activated involuntarily and without an individual’s awareness or intentional control. Residing deep in the subconscious, these biases are different from known biases that individuals may choose to conceal for the purposes of social and/or political correctness. Rather, implicit biases are not accessible through introspection.
Implicit bias can be a factor in any aspect of our everyday lives: when we interact with colleagues, make new friends, or meet parents at our children’s schools. That means the interactions providers and medical workers have with patients are likewise not immune to implicit bias.
In 2015, a group of researchers conducted a literature review to understand the pervasiveness of and impacts of implicit bias. Through the review, the team was able to conclude at least moderate implicit bias in most medical providers. The Implicit Association Test, which measures implicit bias, detected about equal bias across Black, Latinx, and dark-skinned patients.
To be clear, implicit bias is unconscious, and most researchers investigating the subject assert that very few medical professionals maliciously seek to do harm to some of their patients.
But that 2015 review showed that implicit bias does have some consequences, not least of which are strained patient-provider relationships and clinical outcomes. This, like other clinical quality challenges, warrants a closer look from the medical community.
Below, PatientEngagementHIT will outline what implicit bias looks like in healthcare, how it can affect patient-provider communication and outcomes, and how the healthcare industry is beginning to recognize its own implicit biases.
What is implicit bias in healthcare?
In healthcare, implicit bias can shape the way medical providers interact with patients. Because everyone is susceptible to implicit bias, even clinicians, these unconscious preconceptions will naturally seep into patient-provider communication.
There is already some evidence indicating such. In September 2020, the Regenstrief Institute published data from the Department of Veterans Affairs (VA) suggesting that veterans accessing mental health treatment could sense some non-verbal cues that signaled implicit bias.
The survey of 85 Black veterans showed that most had good patient-provider relationships, but many expressed some issues that indicated race could play a role in their healthcare.
"They explained that structural characteristics such as the physical space of an institution project how welcoming an institution might be to minority patients, and that staff diversity, especially in position of power, reflects the facility's values and culture related to racial equity," the researchers reported.
The study went on to describe various subtle behaviors and microaggressions that indicated to patients that implicit biases could be tainting their healthcare experiences.
Since 2020, more studies have explored patient perceptions of implicit bias, with four in 10 patients telling a 2022 MITRE-Harris Poll Survey on Patient Experience that the perceive their providers as biased against them. Hispanic and Black patients were more likely to report this than any other demographic group.
But implicit bias is at play not just when it comes to race and ethnicity. A September 2022 Urban Institute/Robert Wood Johnson Foundation report showed that 17 percent of publicly insured people and 13 percent of uninsured people perceived implicit bias from their providers.
And nearly a third of people with disabilities said in a different Urban Institute/RWJF poll that they perceived unfair treatment in healthcare settings.
Meanwhile, a separate third of LGBT patients said they've had disrespectful healthcare experiences, indicating some bias on the part of their providers.
Again, most experts agree that most clinicians are committed to providing excellent medical care to all of their patients, regardless of race, gender, sexual orientation, or ability to pay. But again, since nobody is immune to implicit bias, it is at play in many medical encounters.
What are the consequences of implicit bias in healthcare?
As with any interaction, implicit bias can have adverse effects on the patient experience. By damaging patient-provider interactions, implicit bias can adversely impact health outcomes.
In many situations, patients are able to pick up on a provider’s implicit bias, and patients often report a poor experience for that. A patient who picks up on a provider’s implicit bias naturally may feel less inclined to engage deeply with care.
Patients with similar experiences as the veteran from the Regenstrief study, for example, could be dissuaded from visiting a provider if they feel the provider treated them like an "angry, big Black man."
This kind of implicit discrimination has born itself out in many Black and Brown patients lacking trust in the medical institution and being reticent to engage with it.
Additionally, implicit bias could put a cap on how well a patient understands her own health or is invited to engage in her care. For example, some providers may limit the depth of shared decision-making or explanations of medical concepts because their implicit bias tells them a patient does not have the health literacy to fully engage with her care.
This, coupled with some implicit biases that tell providers a patient may not be able to afford specialty care, can decrease the odds a patient gets the depth of medical care she might need.
In December 2022, researchers from the University of Minnesota Medical School showed racial health disparities in treatment recommendation . Specifically, the team found that Black patients and other patients of color were less likely to be advised on primary brain tumor removal, which they said was likely a byproduct of implicit bias.
Another study from November 2023 showed that Black patients were modestly more likely to receive low-value care , or "services that provide little to no benefit in specific clinical scenarios yet have potential for harm," the researchers wrote in BMJ. That disparity is likewise potentially driven by implicit bias.
For example, limited patient trust among Black populations could be behind the slightly greater risk for low-value acute diagnostic tests, the researchers said. Because this population tends to report lower trust in medical providers, they may be more likely to agree to diagnostic testing because it is more reassuring than a provider’s assessment.
On the provider side, implicit or explicit biases could also impact communication, which in turn could result in misunderstandings of patient care needs and preferences.
Implicit bias is still a sneaky specter infecting healthcare interactions and contributing to the racial health disparities being seen today. Organizations working to close health disparities must incorporate implicit bias and cultural competency training into their practice.
Addressing implicit bias
Eliminating implicit bias is a challenging task because, as the experts at OSU's Kirwan Institute said, one's own implicit bias is not something most people are aware of. Implicit bias is not purposeful -- purposeful discrimination is referred to as explicit.
But a strong education campaign can be a good first step to helping clinicians pick up on their own biases.
Currently, there's no standardized course for implicit bias training in hospitals and health systems. But as more governing bodies begin to require implicit bias training for things like licensure, organizations are working to build out their own curricula. Implicit bias training courses need to incorporate the existing evidence base, center key stakeholders, and hold space for participants' humanity .
In short, implicit bias training needs to be informative and actionable and avoid judgment. Organizations can potentially increase participation numbers by making it easy to attend implicit bias training, so it may be helpful to consider holding training sessions over Zoom and at various times and days to accommodate staff schedules.
Notably, implicit bias training is not just for clinicians, experts agree. Training that includes administrative, front office, and other staff like environmental services helps fortify and organizational culture of inclusion and equity.
Implicit bias training is essential, but looking into the distant future, many experts have said increasing the diversity of the medical workforce will be a key step in mitigating implicit bias. Although anyone of any demographic has implicit biases, having a workforce reflective of the community it serves may lessen the damage those biases have.
Indeed, data has shown that a diverse medical workforce can improve outcomes because it increases the odds of racial concordance, something that’s been proven to enrich the patient-provider relationship and some outcomes.
Right now, a diverse medical workforce is out of reach. Part of the issue is lack of diversity in medical education; hospitals and health systems can only hire as diverse a staff as they have applicants. Some higher education institutions are cultivating a more diverse medical school applicant pool by hosting elementary, middle, and high school STEM exposure course. Some medical schools are also beginning to offer tuition-free education.
But healthcare can only maintain a diverse medical workforce if its institutions remain inviting to all. Building out a peer-to-peer culture of belonging will be critical in this area.
The process of identifying and acknowledging implicit bias in healthcare is only in its infancy. But as more organizations commit to ending racial health disparities and working toward health equity, this will be an important step toward that end.
Sara Heath has been covering news related to patient engagement and health equity since 2015.
- What is the Difference Between Health Disparities, Equity?
Dig Deeper on Patient satisfaction and experience

How Do Income & SDOH Affect Cardiovascular Healthcare?

Discrimination in Pediatrics Raises Questions About Weathering

Low Trust, Bias Taint Shared Decision-Making for Black Patients

How U-M Health Got 27K Staff Members in Implicit Bias Training
A 'JAMA Internal Medicine' study found that team-based documentation increased visit volume and reduced physician EHR ...
Ambient AI technology is helping Ochsner Health improve patient-provider relationships by allowing clinicians to spend ...
Epic's goal to bring customers live on TEFCA by the end of 2025 complements Carequality's plan to align with TEFCA as the ...

Taking steps to recognize and correct unconscious assumptions toward groups can promote health equity.
JENNIFER EDGOOSE, MD, MPH, MICHELLE QUIOGUE, MD, FAAFP, AND KARTIK SIDHAR, MD
Fam Pract Manag. 2019;26(4):29-33
Author disclosures: no relevant financial affiliations disclosed.

Jamie is a 38-year-old woman and the attending physician on a busy inpatient teaching service. On rounds, she notices several patients tending to look at the male medical student when asking a question and seeming to disregard her. Alex is a 55-year-old black man who has a history of diabetic polyneuropathy with significant neuropathic pain. His last A1C was 7.8. He reports worsening lower extremity pain and is frustrated that, despite his bringing this up repeatedly to different clinicians, no one has addressed it. Alex has been on gabapentin 100 mg before bed for 18 months without change, and his physicians haven't increased or changed his medication to help with pain relief.
Alisha is a 27-year-old Asian family medicine resident who overhears labor and delivery nurses and the attending complain that Indian women are resistant to cervical exams.
These scenarios reflect the unconscious assumptions that pervade our everyday lives, not only as practicing clinicians but also as private citizens. Some of Jamie's patients assume the male member of the team is the attending physician. Alex's physicians perceive him to be a “drug-seeking” patient and miss opportunities to improve his care. Alisha is exposed to stereotypes about a particular ethnic group.
Although assumptions like these may not be directly ill-intentioned, they can have serious consequences. In medical practice, these unconscious beliefs and stereotypes influence medical decision-making. In the classic Institute of Medicine report “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care,” the authors concluded that “bias, stereotyping, and clinical uncertainty on the part of health care providers may contribute to racial and ethnic disparities in health care” often despite providers' best intentions. 1 For example, studies show that discrimination and bias at both the individual and institutional levels contribute to shocking disparities for African-American patients in terms of receiving certain procedures less often or experiencing much higher infant mortality rates when compared with non-Hispanic whites. 2 , 3 As racial and ethnic diversity increases across our nation, it is imperative that we as physicians intentionally confront and find ways to mitigate our biases.
Implicit bias is the unconscious collection of stereotypes and attitudes that we develop toward certain groups of people, which can affect our patient relationships and care decisions.
You can overcome implicit bias by first discovering your blind spots and then actively working to dismiss stereotypes and attitudes that affect your interactions.
While individual action is helpful, organizations and institutions must also work to eliminate systemic problems.
DEFINING AND REDUCING IMPLICIT BIAS
For the last 30 years, science has demonstrated that automatic cognitive processes shape human behavior, beliefs, and attitudes. Implicit or unconscious bias derives from our ability to rapidly find patterns in small bits of information. Some of these patterns emerge from positive or negative attitudes and stereotypes that we develop about certain groups of people and form outside our own consciousness from a very young age. Although such cognitive processes help us efficiently sort and filter our perceptions, these reflexive biases also promote inconsistent decision making and, at worst, systematic errors in judgment.
Cognitive processes lead us to associate unconscious attributes with social identities. The literature explores how this influences our views on race, ethnicity, age, gender, sexual orientation, and weight, and studies show many people are biased in favor of people who are white, young, male, heterosexual, and thin. 4 Unconsciously, we not only learn to associate certain attributes with certain social groupings (e.g., men with strength, women with nurturing) but also develop preferential ranking of such groups (e.g., preference for whites over blacks). This unconscious grouping and ranking takes root early in development and is shaped by many outside factors such as media messages, institutional policies, and family beliefs. Studies show that health care professionals have the same level of implicit bias as the general population and that higher levels are associated with lower quality care. 5 Providers with higher levels of bias are more likely to demonstrate unequal treatment recommendations, disparities in pain management, and even lack of empathy toward minority patients. 6 In addition, stressful, time-pressured, and overloaded clinical practices can actually exacerbate unconscious negative attitudes. Although the potential impact of our biases can feel overwhelming, research demonstrates that these biases are malleable and can be overcome by conscious mitigation strategies. 7
We recommend three overarching strategies to mitigate implicit bias – educate, expose, and approach – which we will discuss in greater detail. We have further broken down these strategies into eight evidence-based tactics you can incorporate into any quality improvement project, diagnostic dilemma, or new patient encounter. Together, these eight tactics spell out the mnemonic IMPLICIT. (See “ Strategies to combat our implicit biases .”)
| Explore and identify your own implicit biases by taking implicit association tests or through other means. | ||
| Practice ways to reduce stress and increase mindfulness, such as meditation, yoga, or focused breathing. | “ ” | |
| Consider experiences from the point of view of the person being stereotyped. This can involve consuming media about those experiences, such as books or videos, and directly interacting with people from that group. | “ ” | |
| Pause and reflect on your potential biases before interacting with people of certain groups to reduce reflexive reactions. This could include thinking about positive examples of that stereotyped group, such as celebrities or personal friends. | “ ” | |
| Evaluate people based on their personal characteristics rather than those affiliated with their group. This could include connecting over shared interests or backgrounds. | “ ” | |
| Embrace evidence-based statements that reduce implicit bias, such as welcoming and embracing multiculturalism. | “ ” | |
| Promote procedural change at the organizational level that moves toward a socially accountable health care system with the goal of health equity. | ||
| Practice cultural humility, a lifelong process of critical self-reflection to readdress the power imbalances of the clinician-patient relationship. | “ ” |
When we fail to learn about our blind spots, we miss opportunities to avoid harm. Educating ourselves about the reflexive cognitive processes that unconsciously affect our clinical decisions is the first step. The following tactics can help:
Introspection . It is not enough to just acknowledge that implicit bias exists. As clinicians, we must directly confront and explore our own personal implicit biases. As the writer Anais Nin is often credited with saying, “We don't see things as they are, we see them as we are.” To shed light on your potential blind spots and unconscious “sorting protocols,” we encourage you to take one or more implicit association tests . Discovering a moderate to strong bias in favor of or against certain social identities can help you begin this critical step in self exploration and understanding. 8 You can also complete this activity with your clinic staff and fellow physicians to uncover implicit biases as a group and set the stage for addressing them. For instance, many of us may be surprised to learn after taking an implicit association test that we follow the typical bias of associating males with science — an awareness that may explain why the patient in our first case example addressed questions to the male medical student instead of the female attending.
Mindfulness .It should come as no surprise that we are more likely to use cognitive shortcuts inappropriately when we are under pressure. Evidence suggests that increasing mindfulness improves our coping ability and modifies biological reactions that influence attention, emotional regulation, and habit formation. 9 There are many ways to increase mindfulness, including meditation, yoga, or listening to inspirational texts. In one study, individuals who listened to a 10-minute meditative audiotape that focused them and made them more aware of their sensations and thoughts in a nonjudgmental way caused them to rely less on instinct and show less implicit bias against black people and the aged. 10
It is also helpful to expose ourselves to counter-stereotypes and to focus on the unique individuals we interact with. Similarity bias is the tendency to favor ourselves and those like us. When our brains label someone as being within our same group, we empathize better and use our actions, words, and body language to signal this relatedness. Experience bias can lead us to overestimate how much others see things the same way we do, to believe that we are less vulnerable to bias than others, and to assume that our intentions are clear and obvious to others. Gaining exposure to other groups and ways of thinking can mitigate both of these types of bias. The following tactics can help:
Perspective-taking . This tactic involves taking the first-person perspective of a member of a stereotyped group, which can increase psychological closeness to that group. 8 Reading novels, watching documentaries, and listening to podcasts are accessible ways to reach beyond our comfort zone. To authentically perceive another person's perspective, however, you should engage in positive interactions with stereotyped group members in real life. Increased face-to-face contact with people who seem different from you on the surface undermines implicit bias.
Learn to slow down . To recognize our reflexive biases, we must pause and think. For example, the next time you interact with someone in a stereotyped group or observe societal stereotyping, such as through the media, recognize what responses are based on stereotypes, label those responses as stereotypical, and reflect on why the responses occurred. You might then consider how the biased response could be avoided in the future and replace it with an unbiased response. The physician treating Alex in the introduction could use this technique by slowing down and reassessing his medical care. By acknowledging the potential for bias, the physician may recognize that safe options remain for managing Alex's neuropathic pain.
Additionally, research strongly supports the use of counter-stereotypic imaging to replace automatic responses. 11 For example, when seeking to contradict a prevailing stereotype, substitute highly defined images, which can be abstract (e.g., modern Native Americans), famous (e.g., minority celebrities like Oprah Winfrey or Lin-Manuel Miranda), or personal (e.g., your child's teacher). As positive exemplars become more salient in your mind, they become cognitively accessible and challenge your stereotypic biases.
Individuation . This tactic relies on gathering specific information about the person interacting with you to prevent group-based stereotypic inferences. Family physicians are trained to build and maintain relationships with each individual patient under their care. Our own social identities intersect with multiple social groupings, for example, related to sexual orientation, ethnicity, and gender. Within these multiplicities, we can find shared identities that bring us closer to people, including shared experiences (e.g., parenting), common interests (e.g., sports teams), or mutual purpose (e.g., surviving cancer). Individuation could have helped the health care workers in Alisha's labor and delivery unit to avoid making judgments based on stereotypes. We can use this tactic to help inform clinical decisions by using what we know about a person's specific, individual, and unique attributes. 11
Like any habit, it is difficult to change biased behaviors with a “one shot” educational approach or awareness campaign. Taking a systematic approach at both the individual and institutional levels, and incorporating a continuous process of improvement, practice, and reflection, is critical to improving health equity.
Check your messaging . Using very specific messages designed to create a more inclusive environment and mitigate implicit bias can make a real difference. As opposed to claiming “we don't see color” or using other colorblind messaging, statements that welcome and embrace multiculturalism can have more success at decreasing racial bias.
Institutionalize fairness . Organizations have a responsibility to support a culture of diversity and inclusion because individual action is not enough to deconstruct systemic inequities. To overcome implicit bias throughout an organization, consider implementing an equity lens – a checklist that helps you consider your blind spots and biases and assures that great ideas and interventions are not only effective but also equitable (an example is included in the table above ). Another example would be to find opportunities to display images in your clinic's waiting room that counter stereotypes. You could also survey your institution to make sure it is embracing multicultural (and not colorblind) messaging.
Take two . Resisting implicit bias is lifelong work. The strategies introduced here require constant revision and reflection as you work toward cultural humility. Examining your own assumptions is just a starting point. Talking about implicit bias can trigger conflict, doubt, fear, and defensiveness. It can feel threatening to acknowledge that you participate in and benefit from systems that work better for some than others. This kind of work can mean taking a close look at the relationships you have and the institutions of which you are a part.
MOVING FORWARD
Education, exposure, and a systematic approach to understanding implicit bias may bring us closer to our aspirational goal to care for all our patients in the best possible way and move us toward a path of achieving health equity throughout the communities we serve. The mnemonic IMPLICIT can help us to remember the eight tactics we all need to practice. While disparities in social determinants of health are often beyond the control of an individual physician, we can still lead the fight for health equity for our own patients, both from within and outside the walls of health care. With our specialty-defining goal of getting to know each patient as a unique individual in the context of his or her community, family physicians are well suited to lead inclusively by being humble, respecting the dignity of each person, and expressing appreciation for how hard everyone works to overcome bias.
Smedley BD, Stith AY, Nelson AR, eds Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care . Washington, DC: Institute of Medicine, National Academy Press; 2003.
Hannan EL, van Ryn M, Burke J, et al.; Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Med Care . 1999;37(1):68-77.
Infant mortality and African Americans. U.S Department of Health and Human Services Office of Minority Health website. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23 . Updated Nov. 9, 2017. Accessed June 10, 2019.
Nosek BA, Smyth FL, Hansen JJ, et al.; Pervasiveness and correlates of implicit attitudes and stereotypes. Eur Rev Soc Psychol . 2007;18(1):36-88.
FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics . 2017;18(1):19.
Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med . 2018;199:219-229.
Charlesworth TES, Banaji MR. Patterns of implicit and explicit attitudes: I. long-term change and stability from 2007 to 2016. Psychol Sci . 2019;30(2):174-192.
Sukhera J, Wodzinski M, Teunissen PW, Lingard L, Watling C. Striving while accepting: exploring the relationship between identity and implicit bias recognition and management. Acad Med . 2018;93(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 57th Annual Research in Medical Education Sessions):S82-S88.
Burgess DJ, Beach MC, Saha S. Mindfulness practice: A promising approach to reducing the effects of clinician implicit bias on patients. Patient Educ Couns . 2017;100(2):372-376.
Lueke A, Gibson B. Mindfulness meditation reduces implicit age and race bias: the role of reduced automaticity of responding. Soc Psychol Personal Sci . 2015;6(3):284-291.
Devine PG, Forscher PS, Austin AJ, Cox WTL. Long-term reduction in implicit race bias: a prejudice habit-breaking intervention. J Exp Soc Psychol . 2012;48(6):1267-1278.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Research article
- Open access
- Published: 01 March 2017
Implicit bias in healthcare professionals: a systematic review
- Chloë FitzGerald 1 &
- Samia Hurst 1
BMC Medical Ethics volume 18 , Article number: 19 ( 2017 ) Cite this article
247k Accesses
1346 Citations
621 Altmetric
Metrics details
Implicit biases involve associations outside conscious awareness that lead to a negative evaluation of a person on the basis of irrelevant characteristics such as race or gender. This review examines the evidence that healthcare professionals display implicit biases towards patients.
PubMed, PsychINFO, PsychARTICLE and CINAHL were searched for peer-reviewed articles published between 1st March 2003 and 31st March 2013. Two reviewers assessed the eligibility of the identified papers based on precise content and quality criteria. The references of eligible papers were examined to identify further eligible studies.
Forty two articles were identified as eligible. Seventeen used an implicit measure (Implicit Association Test in fifteen and subliminal priming in two), to test the biases of healthcare professionals. Twenty five articles employed a between-subjects design, using vignettes to examine the influence of patient characteristics on healthcare professionals’ attitudes, diagnoses, and treatment decisions. The second method was included although it does not isolate implicit attitudes because it is recognised by psychologists who specialise in implicit cognition as a way of detecting the possible presence of implicit bias. Twenty seven studies examined racial/ethnic biases; ten other biases were investigated, including gender, age and weight. Thirty five articles found evidence of implicit bias in healthcare professionals; all the studies that investigated correlations found a significant positive relationship between level of implicit bias and lower quality of care.
The evidence indicates that healthcare professionals exhibit the same levels of implicit bias as the wider population. The interactions between multiple patient characteristics and between healthcare professional and patient characteristics reveal the complexity of the phenomenon of implicit bias and its influence on clinician-patient interaction. The most convincing studies from our review are those that combine the IAT and a method measuring the quality of treatment in the actual world. Correlational evidence indicates that biases are likely to influence diagnosis and treatment decisions and levels of care in some circumstances and need to be further investigated. Our review also indicates that there may sometimes be a gap between the norm of impartiality and the extent to which it is embraced by healthcare professionals for some of the tested characteristics.
Conclusions
Our findings highlight the need for the healthcare profession to address the role of implicit biases in disparities in healthcare. More research in actual care settings and a greater homogeneity in methods employed to test implicit biases in healthcare is needed.
Peer Review reports
A patient should not expect to receive a lower standard of care because of her race, age or any other irrelevant characteristic. However, implicit associations (unconscious, uncontrollable, or arational processes) may influence our judgements resulting in bias. Implicit biases occur between a group or category attribute, such as being black, and a negative evaluation (implicit prejudice) or another category attribute, such as being violent (implicit stereotype) [ 1 ]. Footnote 1 In addition to affecting judgements, implicit biases manifest in our non-verbal behaviour towards others, such as frequency of eye contact and physical proximity. Implicit biases explain a potential dissociation between what a person explicitly believes and wants to do (e.g. treat everyone equally) and the hidden influence of negative implicit associations on her thoughts and action (e.g. perceiving a black patient as less competent and thus deciding not to prescribe the patient a medication).
The term ‘bias’ is typically used to refer to both implicit stereotypes and prejudices and raises serious concerns in healthcare. Psychologists often define bias broadly; such as ‘the negative evaluation of one group and its members relative to another’ [ 2 ]. Another way to define bias is to stipulate that an implicit association represents a bias only when likely to have a negative impact on an already disadvantaged group; e.g. if someone associates young girls with dolls, this would count as a bias. It is not itself a negative evaluation, but it supports an image of femininity that may prevent girls from excelling in areas traditionally considered ‘masculine’ such as mathematics [ 3 ]. Another option is to stipulate that biases are not inherently bad, but only to be avoided when they incline us away from the truth [ 4 ].
In healthcare, we need to think carefully about exactly what is meant by bias. To fulfil the goal of delivering impartial care, healthcare professionals should be wary of any kind of negative evaluation they make that is linked to membership of a group or to a particular characteristic. The psychologists’ definition of bias thus may be adequate for the case of implicit prejudice; there are unlikely, in the context of healthcare, to be any justified reasons for negative evaluations related to group membership. The case of implicit stereotypes differs slightly because stereotypes can be damaging even when they are not negative per se. At least at a theoretical level, there is a difference between an implicit stereotype that leads to a distorted judgement and a legitimate association that correctly tracks real world statistical information. Here, the other definitions of bias presented above may prove more useful.
The majority of people tested from all over the world and within a wide range of demographics show responses to the most widely used test of implicit attitudes, the Implicit Association Test (IAT), that indicate a level of implicit anti-black bias [ 5 ]. Other biases tested include gender, ethnicity, nationality and sexual orientation; there is evidence that these implicit attitudes are widespread among the population worldwide and influence behaviour outside the laboratory [ 6 , 7 ]. For instance, one widely cited study found that simply changing names from white-sounding ones to black-sounding ones on CVs in the US had a negative effect on callbacks [ 8 ]. Implicit bias was suspected to be the culprit, and a replication of the study in Sweden, using Arab-sounding names instead of Swedish-sounding names, did in fact find a correlation between the HR professionals who preferred the CVs with Swedish-sounding names and a higher level of implicit bias towards Arabs [ 9 ].
We may consciously reject negative images and ideas associated with disadvantaged groups (and may belong to these groups ourselves), but we have all been immersed in cultures where these groups are constantly depicted in stereotyped and pejorative ways. Hence the description of ‘aversive racists’: those who explicitly reject racist ideas, but who are found to have implicit race bias when they take a race IAT [ 10 ]. Although there is currently a lack of understanding of the exact mechanism by which cultural immersion translates into implicit stereotypes and prejudices, the widespread presence of these biases in egalitarian-minded individuals suggests that culture has more influence than many previously thought.
The implicit biases of concern to health care professionals are those that operate to the disadvantage of those who are already vulnerable. Examples include minority ethnic populations, immigrants, the poor, low health-literacy individuals, sexual minorities, children, women, the elderly, the mentally ill, the overweight and the disabled, but anyone may be rendered vulnerable given a certain context [ 11 ]. The vulnerable in health-care are typically members of groups who are already disadvantaged on many levels. Work in political philosophy, such as the De-Shalit and Wolff concept of ‘corrosive disadvantage’, a disadvantage that is likely to lead to further disadvantages, is relevant here [ 12 ]. For instance, if a person is poor and constantly worried about making ends meet, this is a disadvantage in itself, but can be corrosive when it leads to further disadvantages. In a country such as Switzerland, where private health insurance is mandatory and yearly premiums can be lowered by increasing the deductible, a high deductible may lead such a person to refrain from visiting a physician because of the potential cost incurred. This, in turn, could mean that the diagnosis of a serious illness is delayed leading to poorer health. In this case, being poor is a corrosive disadvantage because it leads to a further disadvantage of poor health.
The presence of implicit biases among healthcare professionals and the effect on quality of clinical care is a cause for concern [ 13 , 14 , 15 ]. In the US, racial healthcare disparities are widely documented and implicit race bias is one possible cause. Two excellent literature reviews on the issue of implicit bias in healthcare have recently been published [ 16 , 17 ]. One is a narrative review that selects the most significant recent studies to provide a helpful overall picture of the current state of the research in healthcare on implicit bias [ 16 ]. The other is a systematic review that focusses solely on racial bias and thus captures only studies conducted in the US, where race is the most prominent issue [ 17 ]. Our review differs from the first because it poses a specific question, is systematic in its collection of studies, and includes an examination of studies solely employing the vignette method. Its systematic method lends weight to the evidence it provides and its inclusion of the vignette method enables it to compare two different literatures on bias in healthcare. It differs from the second because it includes all types of bias, not only racial; partly as a consequence, it captures many studies conducted outside the US. It is important to include studies conducted in non-US countries because race understood as white/black is not the source of the most potentially harmful stereotypes and disparities in all cultural contexts. For example, a recent vignette study in Switzerland found that in the German-speaking part of the country, physicians displayed negative bias in treatment decisions towards fictional Serbian patients (skin colour was unspecified, but it would typically be assumed to be white), but no significant negative bias towards fictional patients from Ghana (skin colour would be assumed to be black) [ 18 ]. In the Swiss German context, the issue of skin colour may thus be less significant for potential bias than that of country of origin. Footnote 2
Data sources and search strategy
Our research question was: do trained healthcare professionals display implicit biases towards certain types of patient? PubMed (Medline), PsychINFO, PsychARTICLE and CINAHL were searched for peer-reviewed articles published between 1st March 2003 and 31st March 2013. When we performed exploratory searches on PubMed before conducting the final search, we noticed that in 2003 there was a sharp increase in the number of articles on implicit bias and so we decided to begin from this year. The final searches were conducted on the 31st March 2013. We used a combination of subject headings and free text terms that related to the attitudes of healthcare professionals (e.g. “physician-patient relations”, “attitude of health personnel”), implicit biases (e.g. “prejudice”, “stereotyping”, “unconscious bias”), particular kinds of discrimination (e.g. “aversive racism”, anti-fat bias”, “women’s health”), and healthcare disparities (e.g. “health status disparities”, “delivery of health care”) which were combined with the Boolean operators “AND” and “OR”.
Study selection
3767 titles were retrieved and independently screened by the two reviewers (SH and CF). The titles that were agreed by both after discussion to be ineligible according to our inclusion criteria were discarded (3498) and the abstracts of the remaining articles (269) were independently screened by both reviewers. Abstracts that were agreed by both reviewers to be ineligible according to our inclusion criteria were discarded (241). When the ineligible abstracts were discarded, the remaining 28 articles were read and independently rated by us both. Out of these, 27 articles were agreed after discussion to merit inclusion in the final selection. One article was excluded at this stage because it did not fit our inclusion criteria (it did not employ the assumption method or an implicit measure). Additionally, the reference lists of these 27 articles were manually scanned by CF, and the full text articles resulting from this were independently read by both reviewers, resulting in the inclusion of a further 11 articles that both reviewers agreed fitted the inclusion criteria. After a repeat process of scanning the reference lists of the 11 articles from the second round, the final number of eligible articles was 42. All disagreements were resolved through discussion.
The inclusion criteria were:
Empirical study.
A method identifying implicit rather than explicit biases.
Participants were physicians or nurses who had completed their studies.
Written in English or another language spoken by CF or SH (CF: French, Italian, Spanish, Catalan; SH: French, Italian, German).
There is no clear consensus on the meaning of the term ‘implicit’. The term is used in psychology to refer to a feature or features of a mental process. We chose a wide negative definition of implicit processes, assuming that implicit social cognition is involved in the absence of any of the four features that characterise explicit cognition: intention, conscious availability, controllability, and the need for mental resources. This absence does not rule out the involvement of explicit processes, but indicates the presence of implicit processes. While most institutional policies against bias focus on explicit cognition, research on implicit bias shows that this is mistaken [ 6 ].
There is broad agreement in psychology that methods known as ‘implicit measures’, including the affective priming task, the IAT and the affective Simon task, reveal implicit attitudes [ 19 ]. We included articles using these measures. We also included studies that employed a method popular in bioethics literature that we label ‘the assumption method’. It involves measuring differences across participants in response to clinical vignettes, identical except for one feature, such as the race, of the character in the vignette. There is no direct measure of the implicitness or non-explicitness of the processes at work in participants; instead, there is an assumption that the majority are explicitly motivated to disregard factors such as race. If there is a statistically significant difference in the diagnosis or treatment prescribed correlated with –for example- the race of the patient, the researchers infer that it is partly a result of implicit processes in the physicians’ decision-making. The assumption method of measuring implicit bias has been used in a variety of naturalistic contexts where it is harder to bring subjects into the laboratory. It is recognised by psychologists who specialise in implicit cognition as a way of detecting the possible presence of implicit bias, if not as an implicit measure in itself [ 6 ].
Studies that used self-report questionnaires were not included because, although they can use subtle methods to estimate a subject’s attitudes, they are typically used in psychology as a measure of explicit mental processes. There are potential problems with the implicit/explicit distinction as applied to psychological measures and it may be preferable in future research to speak of ‘direct’ and ‘indirect’ measures, but for the purposes of the review we followed this convention in psychology. The original idea behind implicit measures was that they attempted to measure something other than explicit mental processes, whereas self-report questionnaires ask a subject direct questions and thus prompt a chain of explicit conscious reasoning in the subject.
Data extraction
Data were extracted by CF and reviewed by SH for accuracy and completeness. All disagreements with the information extracted were resolved through discussion. We contacted the corresponding author of an article to obtain information that was not available in the published manuscript that related to the nature of the presentation given to recruit participants, but received no response.
Identified studies
The eligible studies are described in Table 1 and their main characteristics are outlined in Table 2 . The most frequently examined biases were racial/ethnic and gender, but ten other biases were investigated (Table 2 ). Four of the assumption studies compared results from two or more countries to explore effects of differences in healthcare systems.
The 14 assumption method studies examining multiple biases investigated interactions between biases. They recorded the socio-demographic characteristics of the participants to reveal complex interactions between physician characteristics and the characteristics of the imaginary ‘patient’ in the vignette.
All IAT studies measured implicit prejudice; five also measured implicit stereotypes. When implicit prejudice is measured, words or images from one category are matched with positive or negative words (e.g., black faces with ‘pleasant’). When implicit stereotypes are measured, words or images from one category are matched with words from a conceptual category (e.g. female faces and ‘home’).
Nine IAT studies combined the IAT with a measure of physician behaviour or treatment decision to see if there were correlations between these and levels of implicit bias.
The subliminal priming studies were dissimilar: one was an exploratory study to see if certain diseases were stereotypically associated with African Americans, using faces as primes and reaction times to the names of diseases as the measure of implicit association; the other study used race words as primes and tested the effect of time pressure on responses to a clinical vignette.
A variety of media were used for the clinical vignette and the method of questioning participants within the assumption method. One unusual study used simulations of actual encounters with patients, hiring actors and using a set for the physicians to role-play. Physicians’ treatment decisions were recorded by observers, and the physician recorded his own diagnosis, prognosis and perceptions after the encounter.
Limitations
Of specific studies.
Limitations are detailed in Table 3 . Some studies failed to report response rates, or to provide full information on statistical methods or participant characteristics. Some had very small sample sizes and the majority did not mention calculating the power of their sample. Some authors explicitly informed participants of the purpose of the study, or gave participants questionnaires or other tests that indicated the subject of the study before presenting them with the vignette. For optimal results, participants should not be alerted to the particular patient characteristic(s) under study, particularly in an assumption study where knowing the characteristic(s) may influence the interpretation of the vignette. In IAT studies, this is less worrying because IAT effects are to some extent uncontrollable.
Of the field
Implicit bias in healthcare is an emerging field of research with no established methodology. This is to be expected and is not a problem in itself, but it does present an obstacle when conducting a review of this kind. The range of methods used and the variety of journals with differing standards and protocols for describing experiments made it difficult to compare the results. In addition, authors focusing on a particular bias (e.g. gender), often in combination with a particular health issue (e.g. heart disease), frequently did not appear to be familiar with one another’s research. This lack of familiarity meant that often used different terms to describe the same phenomenon, which also made conducting the review more difficult.
Few of the existing results can be described as ‘real world’ treatment outcomes. The two priming studies involved very small samples and were more exploratory than result-seeking [ 20 , 21 ]. The IAT and assumption studies were conducted under laboratory conditions. The only three studies conducted in naturalistic settings combined the IAT with measures of physician-patient interaction [ 22 , 23 , 24 ]. However, many of the assumption studies attempted to make their vignettes as realistic as possible by having them validated by clinicians [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 ] and also by having participants view/read the vignettes as part of a normal day at work [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 39 , 41 ].
Because the studies of interest used psychological techniques, but were mainly to be found in a medical database (PubMed), the classification of the studies was not always optimal. There is no heading in Medline for ‘implicit bias’ and studies using similar methods were sometimes categorized under different subject headings, some of which were introduced during the last ten years, which increased the risk of missing eligible studies.
Existence of implicit biases/stereotypes in healthcare professionals and influence on quality of care
Healthcare professionals have implicit biases.
Almost all studies found evidence for implicit biases among physicians and nurses. Based on the available evidence, physicians and nurses manifest implicit biases to a similar degree as the general population. The following characteristics are at issue: race/ethnicity, gender, socio-economic status (SES), age, mental illness, weight, having AIDS, brain injured patients perceived to have contributed to their injury, Footnote 3 intravenous drug users, disability, and social circumstances.
Of the seven studies that did not find evidence of bias, one compared the mentally ill with another potentially unfavourable category, welfare recipients; this study did find a positive correlation between levels of implicit bias and over-diagnosis of the mentally ill patient in the vignette [ 42 ]. Another used simulated interactions with actors, which may result in participants being on ‘best behaviour’ in the role-play [ 41 ]. The two studies that reported no evidence of bias in diagnosis of depression found that physicians’ estimates of SES were influenced by race (lower SES estimated for black patients); [ 37 , 38 ] one reported that estimates of SES in turn were significantly related to estimates of patient demeanour (lower SES associated with hostile patient demeanour) [ 37 ]. A further study failed to find differences due to patient race in the prescription of opioids, but found an interaction whereby black patients who exhibited ‘challenging’ behaviour (such as belligerence and asking for a specific opioid) were more likely to be prescribed opioids than those who did not, an effect possibly due to a racial stereotype [ 43 ]. Another study that failed to find implicit race bias suggested that this was due to the setting of the study in an inner-city clinic with high levels of black patients and the fact that many physicians were born outside the US [ 24 ]. Finally, one study that found no evidence of racial bias in prescription of opioid analgesics presented each participant with three vignettes depicting patients of three different ethnicities, thus probably alerting them to the objective of the study [ 40 ].
The interaction effects between different patient characteristics in assumption studies are varied and a few are surprising. The authors of one study expected that physicians would be less likely to prescribe a higher dose of opioids to black patients who exhibited challenging behaviours; in fact, physicians were more likely to prescribe higher doses of opioids to challenging black patients, yet slightly less likely to do so to white patients exhibiting the same behaviour. Sometimes significant effects on the responses to the vignette of a patient characteristic, e.g. race, are only found when the interaction between gender and race or SES and race is examined. For example, physicians in one study were less certain of the diagnosis of coronary heart disease for middle-aged women, who were thus twice as likely to receive a mental health diagnosis than their male counterparts [ 34 ]. In another, low SES Latinas and blacks were more likely to have intrauterine contraception recommended than low SES whites, but there was no effect of race for high SES patients [ 39 ].
Implicit bias affects clinical judgement and behaviour
Three studies found a significant correlation between high levels of physicians’ implicit bias against blacks on IAT scores and interaction that was negatively rated by black patients [ 23 , 24 , 44 ] and, in one study, also negatively rated by external observers [ 23 ]. Four studies examining the correlation between IAT scores and responses to clinical vignettes found a significant correlation between high levels of pro-white implicit bias and treatment responses that favoured patients specified as white [ 42 , 45 , 46 , 47 ]. In one study, implicit prejudice of nurses towards injecting drug users significantly mediated the relationship between job stress and their intention to change jobs [ 48 ].
Twenty out of 25 assumption studies found that some kind of bias was evident either in the diagnosis, the treatment recommendations, the number of questions asked of the patient, the number of tests ordered, or other responses indicating bias against the characteristic of the patient under examination.
Determinants of bias
Socio-demographic characteristics of physicians and nurses (e.g. gender, race, type of healthcare setting, years of experience, country where medical training received) are correlated with level of bias. In one study, male staff were significantly less sympathetic and more frustrated than female staff with self-harming patients presenting in A&E [ 26 ]. Black patients in the US –but not the UK- were significantly more likely to be questioned about smoking than white [ 28 ]. In another study, international medical graduates rated the African-American male patient in the vignette as being of significantly lower SES than did US graduates [ 38 ]. One study found that paediatricians held less implicit race bias compared with other MDs [ 47 ].
Correlations between explicit and implicit attitudes varied depending on the type of bias and on the kind of explicit questions asked. For instance, implicit anti-fat bias tends to correlate more with an explicit anti-fat bias than racial bias, where explicit and implicit attitudes often diverge significantly. Because physicians’ and nurses’ implicit attitudes diverged frequently from their explicit attitudes, explicit measures cannot be used alone to measure the presence of bias among healthcare professionals.
A variety of studies, conducted in various countries, using different methods, and testing different patient characteristics, found evidence of implicit biases among healthcare professionals and a negative correlation exists between level of implicit bias and indicators of quality of care. The two most common methods employed were the assumption method and the IAT, the latter sometimes combined with another measure to test for correlations with the behaviour of healthcare professionals.
Our study has several limitations. Four studies included participants who were not trained physicians or nurses and failed to report separate results for these categories of participants [ 42 , 44 , 49 , 50 ]. Since either the majority of participants were qualified physicians and nurses, or were other health care professionals involved in patient care, we included these studies despite this limitation. Excluding them would not have changed the conclusions of this paper. In addition, we initially centred our research on studies employing implicit measures recognised in psychology, but the majority of the included studies in the final review used the assumption method. However, the limitations imposed by the lack of consistency in keywords and categorization of articles actually worked in our favour here, enabling us to capture a variety of methods and thus to consider including the assumption method. Scanning the references of the articles that were initially retained and repeating this process until there were no new articles helped us to capture further pertinent articles. From the degree of cross-referencing we are confident that we succeeded in identifying most of the relevant articles using the assumption method.
Publication bias could limit the availability of results that reveal little or no implicit bias among healthcare professionals. Moreover, eight articles appeared to refer to the same data collected in a single cross-country comparison study [ 27 , 28 , 29 , 30 , 31 , 32 , 34 , 35 ] and a further two articles analysed the same data [ 45 , 47 ]. The sum of 42 articles thus can give the impression that more research has been carried out on more participants than is the case. The solidity of data revealing high levels of implicit bias among the general population suggest that this is unlikely to have invalidated the conclusion that implicit bias is present in healthcare professionals [ 6 , 7 ].
However, our decision to exclude studies that involved students rather than fully-trained healthcare professionals meant that we did not include a study conducted on medical students that showed no significant association between implicit bias and clinical assessments [ 51 ]. Several studies post 2013 (thus after our cut-off date) have also indicated a null relationship between levels of implicit bias and clinical decision-making [ 52 , 53 , 54 ]. The scientific community working in this area agrees that the relationship between levels of implicit bias in healthcare professionals and clinical decision-making is complex and that there is currently a lack of good evidence for a direct negative influence of biases [ 16 , 17 ]. As our review shows, there is clearer evidence for a relationship between implicit bias and negative effects on clinical interaction [ 23 , 24 , 44 ]. While this may not always translate into negative treatment outcomes, the relationship between a healthcare professional and her patient is essential to providing good treatment, thus it seems likely that the more negative the clinical interaction, the worse the eventual treatment outcome (not to mention the likelihood that the patient will consult healthcare services for future worries or problems). This is where the bulk of future research should be concentrated.
The interactions between multiple patient characteristics and between healthcare professional and patient characteristics reveal the complexity of the phenomenon of implicit bias and its influence on clinician-patient interaction. They also highlight the pertinence of work in feminist theory on ‘intersectionality’, a term for the distinctive issues that arise when a person belongs to multiple identity categories that bring disadvantage, such as being both black and female [ 55 ]. For instance, one study only found evidence of bias against low SES Latina patients, not against high SES Latinas, illustrating how belonging to more than one category (here, both low SES and Latina) can have negative effects that are not present if membership of one category is eliminated (here, low SES) [ 39 ]. Class may trump race in some circumstances so that being high SES is more salient than being non-white. One criticism of mainstream feminism by theorists who work on intersectionality is that pertinent issues are unexplored because of the dominance of high SES white women in feminist theory. Using our example from the review, high SES Latina women may not experience the same prejudice as low SES Latina women and thus may falsely assume that there is no prejudice against Latina women tout court in this context. This could be frustrating for low SES Latina women who have unrecognized lived experiences of prejudice in a clinical setting.
In some studies, the attitudes of patients towards healthcare professionals were recorded and used to evaluate clinical interaction [ 23 , 24 , 44 ]. It is important to remember that patients also may come to a clinical interaction with biases. In these cases, the biases of one participant may trigger the biases of the other, magnifying the first participant’s biased responses and leading to a snowball effects [ 56 ]. Past experience of discrimination may mean that a patient may come to an interaction with negative expectations [ 57 ].
Our findings in the review suggest that the relationship between training and experience and levels of implicit bias is mixed. In one study, increased contact with patients with Hepatitis C virus was associated with more favourable explicit attitudes, yet more negative implicit attitudes towards intravenous drug users [ 49 ]. Another study demonstrated that nursing students were less prejudiced, more willing to help and desired more social interaction with patients with brain injury, when compared with qualified nurses [ 58 ]. Exposure to communication skills training was not associated with lower race-IAT scores for physicians [ 23 ]. However, individuals with mental health training demonstrated more positive implicit and explicit evaluations of people with mental illness than those without training [ 42 ]. Yet in the same study, graduate students had more positive implicit attitudes towards the mentally ill than mental health professionals.
We included all types of implicit bias in our review, not only race bias, partly in an effort to capture non-US studies, hypothesising that the focus on race in the US leaves fewer resources for investigation into other biases. It is possibly the case that a wider range of biases were investigated in non-US countries, but there is not enough evidence to deduce this from our review alone. For instance, two British studies examine bias against brain-injured patients who are perceived as having contributed to their injury [ 58 , 59 ], and two Australian studies looked at bias against intravenous drug users [ 48 , 49 ], but the sample size of studies is too small to warrant drawing any conclusions from this.
Is it possible that there are implicit associations that are justified because they are based on prevalence data for diseases? One study in our review aimed to test the statistical discrimination hypothesis by asking physicians to estimate the prevalence data among males and females for coronary heart disease in addition to presenting them with vignettes of a female or male coronary heart disease patient. It found that 48% of physicians were inconsistent in their population-level and individual level assessments and that the physicians’ gender-based population prevalence assessments were not associated with the certainty of their diagnosis of coronary heart disease. There was no evidence to support the theory of statistical discrimination as an explanation for why physicians were less certain of their diagnoses of CHD in women [ 36 ]. Another exploratory study looked at the diseases that were stereotypically associated with African-Americans and found that many diseases were associated with African-Americans that did not match prevalence data, such as drug abuse [ 20 ]. The danger in these cases is that a physician may apply a group-level stereotype to an individual and fail to follow-up with a search for individuating information.
Impartial treatment of patients by healthcare professionals is an uncontroversial norm of healthcare. Implicit biases have been identified as one possible factor in healthcare disparities and our review reveals that they are likely to have a negative impact on patients from stigmatized groups. Our review also indicates that there may sometimes be a gap between the norm of impartiality and the extent to which it is embraced by healthcare professionals for some of the tested characteristics. For instance, explicit anti-fat bias was found to be prevalent among healthcare professionals [ 60 ]. Since weight can be relevant to diagnosis and treatment, it is understandable that it is salient. It is nonetheless disturbing that healthcare professionals exhibit the same explicit anti-fat attitudes prevalent in the general population.
The most convincing studies from our review are those that combine the IAT and a method measuring the quality of treatment in the actual world. These studies provide some evidence for a relationship between bias as measured by the IAT and behaviour by clinicians that may contribute to healthcare disparities. More studies using real-world interaction measures would be helpful because studies using vignettes remain open to the criticism that they do not reveal the true behaviour of healthcare professionals. In this respect, the three studies using measures of physician-patient interaction are exemplary [ 22 , 23 , 24 ], in particular when using independent evaluators of the interactions [ 23 ]. Overall, our review reveals the need for discussion of methodology and for more interaction between different literatures that focus on different biases.
Our findings highlight the need for the healthcare profession to address the role of implicit biases in disparities in healthcare. In addition to addressing implicit biases, measures need to be taken to raise awareness of the potential conflict between holding negative explicit attitudes towards some patient characteristics, such as obesity, and committing to a norm to treat all patients equally.
Our review reveals that this is an area in need of more uniform methods of research to enable better comparison and communication between researchers interested in different forms of bias. Important avenues for further research include examination of the interactions between patient characteristics, and between healthcare professional and patient characteristics, and of possible ways in which to tackle the presence of implicit biases in healthcare.
There are conceptual problems with this distinction as used in psychology that have been pointed out by philosophers, but we will ignore these for the purposes of this review.
Interestingly, physicians were also asked for how they expected their colleagues to rate the vignette, and in these ratings there was a negative bias towards both patients from Ghana and from Serbia.
Bias against patients who are seen as contributing to their injury initially seems to be an odd category compared to the more familiar ones of race and gender. Clinicians may treat brain injured patients differently if they are somehow seen as ‘responsible’ for their injury, for instance, if they were engaging in risk-taking behaviour such as drug taking. Our review was intended to capture studies such as these that identify biases that are specific to clinical contexts and thus of particular interest to clinicians.
Holroyd J, Sweetman J. The Heterogeneity of Implicit Bias. In Brownstein, Michael, Saul, Jennifer, editors. Implicit Bias and Philosophy, Volume 1: Metaphysics and Epistemology 1. Oxford: Oxford University Press; 2016. p. 80–103.
Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: where do we go from here? Perm J. 2011;15:71.
Google Scholar
Ambady N, Shih M, Kim A, Pittinsky TL. Stereotype susceptibility in children: effects of identity activation on quantitative performance. Psychol Sci. 2001;12:385–90.
Article Google Scholar
Louise A. Bias: Friend or Foe? Reflections on Saulish Skepticism. In Brownstein, Michael, Saul, Jennifer, editors. Implicit Bias and Philosophy, Volume 1: Metaphysics and Epistemology 1. Oxford: Oxford University Press; 2016. p. 157–190.
Nosek BA, et al. Pervasiveness and correlates of implicit attitudes and stereotypes. Eur Rev Soc Psychol. 2007;18:36–88.
Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issues Policy Rev. 2012;6:113–47.
Jost JT, et al. The existence of implicit bias is beyond reasonable doubt: a refutation of ideological and methodological objections and executive summary of ten studies that no manager should ignore. Res Organ Behav. 2009;29:39–69.
Bertrand M, Mullainathan S. Are Emily and Greg more employable than lakisha and Jamal? a field experiment on labor market discrimination. Am Econ Rev. 2004;94:991–1013.
Rooth D-O. Automatic associations and discrimination in hiring: real world evidence. Labour Econ. 2010;17:523–34.
Dovidio JF, Gaertner SL. Aversive racism. Adv Exp Soc Psychol. 2004;36:1–52.
Martin AK, Tavaglione N, Hurst S. Resolving the conflict: Clarifying’ Vulnerability’ in health care ethics. Kennedy Inst Ethics J. 2014;24:51–72.
De-Shalit A, Wolff J. Disadvantage. Oxford: Oxford University Press; 2007.
Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22:882–7.
Stone J, Moskowitz GB. Non-conscious bias in medical decision making: what can be done to reduce it? Med Educ. 2011;45:768–76.
Shavers VL, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102:953–66.
Zestcott, C. A., Blair, I. V. & Stone, J. Examining the presence, consequences, and reduction of implicit bias in health care: A narrative review. Group Process Intergroup Relat. 2016. doi: 10.1177/1368430216642029 .
Hall WJ, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–76.
Drewniak D, Krones T, Sauer C, Wild V. The influence of patients’ immigration background and residence permit status on treatment decisions in health care. Results of a factorial survey among general practitioners in Switzerland. Soc Sci Med. 2016;161:64–73.
De Houwer J, Moors A. How to define and examine the implicitness of implicit measures. In Wittenbrink B, Schwartz N. (eds.). Implicit measures of attitudes: Procedures and controversies. New York: Guilford Press; 2007. pp. 179–194.
Moskowitz GB, Stone J, Childs A. Implicit stereotyping and medical decisions: unconscious stereotype activation in practitioners’ thoughts about African americans. Am J Public Health. 2012;102:996–1001.
Stepanikova I. Racial-ethnic biases, time pressure, and medical decisions. J Health Soc Behav. 2012;53:329–43.
Blair IV, et al. Assessment of biases against Latinos and African americans among primary care providers and community members. Am J Public Health. 2013;103:92–8.
Cooper LA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102:979–87.
Penner LA, et al. Aversive racism and medical interactions with black patients: a field study. J Exp Soc Psychol. 2010;46:436–40.
Protière C, Viens P, Rousseau F, Moatti JP. Prescribers’ attitudes toward elderly breast cancer patients. Discrimination or empathy? Crit Rev Oncol Hematol. 2010;75:138–50.
Mackay N, Barrowclough C. Accident and emergency staff’s perceptions of deliberate self-harm: attributions, emotions and willingness to help. Br J Clin Psychol. 2005;44:255–67.
Arber S, et al. Influence of patient characteristics on doctors’ questioning and lifestyle advice for coronary heart disease: a UK/US video experiment. Br J Gen Pract. 2004;54:673–8.
McKinlay J, et al. How do doctors in different countries manage the same patient? results of a factorial experiment. Health Serv Res. 2006;41:2182–200.
Lutfey KE, et al. Diagnostic certainty as a source of medical practice variation in coronary heart disease: results from a cross-national experiment of clinical decision making. Med Decis Making. 2009;29(5):606–18.
McKinlay JB, et al. Sources of variation in physician adherence with clinical guidelines: results from a factorial experiment. J Gen Intern Med. 2007;22:289–96.
Bönte M, et al. Women and men with coronary heart disease in three countries: are they treated differently? Womens Health Issues. 2008;18:191–8.
Arber S, et al. Patient characteristics and inequalities in doctors’ diagnostic and management strategies relating to CHD: a video-simulation experiment. Soc Sci Med. 2006;62:103–15.
Lutfey KE, Eva KW, Gerstenberger E, Link CL, McKinlay JB. Physician cognitive processing as a source of diagnostic and treatment disparities in coronary heart disease results of a factorial priming experiment. J Health Soc Behav. 2010;51:16–29.
Maserejian NN, Link CL, Lutfey KL, Marceau LD, McKinlay JB. Disparities in physicians’ interpretations of heart disease symptoms by patient gender: results of a video vignette factorial experiment. J Womens Health. 2009;18:1661–7.
Lutfey KE, Link CL, Grant RW, Marceau LD, McKinlay JB. Is certainty more important than diagnosis for understanding race and gender disparities?: An experiment using coronary heart disease and depression case vignettes. Health Policy. 2009;89:279–87.
Maserejian NN, Lutfey KE, McKinlay JB. Do physicians attend to base rates? prevalence data and statistical discrimination in the diagnosis of coronary heart disease. Health Serv Res. 2009;44:1933–49.
Kales HC, et al. Race, gender, and psychiatrists’ diagnosis and treatment of major depression among elderly patients. Psychiatr Serv. 2005;56:721–8.
Kales HC, et al. Effect of race and Sex on primary care Physicians’ diagnosis and treatment of late-life depression. J Am Geriatr Soc. 2005;53:777–84.
Dehlendorf C, et al. Recommendations for intrauterine contraception: a randomized trial of the effects of patients’ race/ethnicity and socioeconomic status. Am J Obstet Gynecol. 2010;203:319–e1.
Tamayo-Sarver JH, et al. The effect of race/ethnicity and desirable social characteristics on physicians’ decisions to prescribe opioid analgesics. Acad Emerg Med. 2003;10:1239–48.
Barnato AE, et al. A randomized trial of the effect of patient race on physician ICU and life-sustaining treatment decisions for an acutely unstable elder with end-stage cancer. Crit Care Med. 2011;39:1663.
Peris TS, Teachman BA, Nosek BA. Implicit and explicit stigma of mental illness: Links to clinical care. J Nerv Ment Dis. 2008;196:752–60.
Burgess DJ, et al. Patient race and physicians’ decisions to prescribe opioids for chronic low back pain. Soc Sci Med. 2008;67:1852–60.
Blair IV, et al. Clinicians’ implicit ethnic/racial bias and perceptions of care among black and Latino patients. Ann Fam Med. 2013;11:43–52.
Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for four common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102:988–95.
Green AR, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–8.
Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46:678–85.
von Hippel W, Brener L, von Hippel C. Implicit prejudice toward injecting drug users predicts intentions to change jobs among drug and alcohol nurses. Psychol Sci. 2008;19:7–11.
Brener L, von Hippel W, Kippax S. Prejudice among health care workers toward injecting drug users with hepatitis C: does greater contact lead to less prejudice? Int J Drug Policy. 2007;18:381–7.
Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–9.
Haider AH, et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. JAMA. 2011;306:942–51.
Oliver MN, Wells KM, Joy-Gaba JA, Hawkins CB, Nosek BA. Do physicians’ implicit views of African americans affect clinical decision making? J Am Board Fam Med. 2014;27:177–88.
Blair IV, et al. An investigation of associations between clinicians’ ethnic or racial bias and hypertension treatment, medication adherence and blood pressure control. J Gen Intern Med. 2014;29:987–95.
Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16:558–68.
Cole ER. Intersectionality and research in psychology. Am Psychol. 2009;64:170.
Burgess DJ, Fu SS, Van Ryn M. Why do providers contribute to disparities and what can be done about it? J Gen Intern Med. 2004;19:1154–9.
Dominicé Dao M. Vulnerability in the clinic: case study of a transcultural consultation. J Med Ethics. 2016. doi: 10.1136/medethics-2015-103337 .
Linden MA, Redpath SJ. A comparative study of nursing attitudes towards young male survivors of brain injury: a questionnaire survey. Int J Nurs Stud. 2011;48:62–9.
Redpath SJ, et al. Healthcare professionals’ attitudes towards traumatic brain injury (TBI): the influence of profession, experience, aetiology and blame on prejudice towards survivors of brain injury. Brain Inj. 2010;24:802–11.
Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One. 2012;7:e48448.
Li L, et al. Using case vignettes to measure HIV-related stigma among health professionals in China. Int J Epidemiol. 2007;36:178–84.
Aaberg VA. A path to greater inclusivity through understanding implicit attitudes toward disability. J Nurs Educ. 2012;51:505–10.
Abuful A, Gidron Y, Henkin Y. Physicians’ attitudes toward preventive therapy for coronary artery disease: is there a gender bias? Clin Cardiol. 2005;28:389–93.
Chow LY, Kam WK, Leung CM. Attitudes of healthcare professionals towards psychiatric patients in a general hospital in Hong Kong. J Psychiatry. 2007;17(1):3–9.
Neauport A, et al. Effects of a psychiatric label on medical residents’ attitudes. Int J Soc Psychiatry. 2012;58:485–7.
Barnhart JM, Wassertheil-Smoller S. The effect of race/ethnicity, sex, and social circumstances on coronary revascularization preferences: a vignette comparison. Cardiol Rev. 2006;14:215–22.
Sabin DJA, Nosek DBA, Greenwald DAG, Rivara DFP. Physicians’ implicit and explicit attitudes about race by MD race, ethnicity, and gender. J Health Care Poor Underserved. 2009;20:896.
Michael Vallis T, Currie B, Lawlor D, Ransom T. Healthcare professional bias against the obese: how do we know if we have a problem? Can J Diabetes. 2007;31:365–70.
Download references
Acknowledgements
Not applicable. Only the two authors were implicated in the review.
This work was carried out with the support of grants from the Swiss National Science Foundation under grants numbers: PP00P3_123340 and 32003B_149407.
Availability of data and materials
The search strategy is available in the Appendix to the paper.
Authors’ contributions
Both authors discussed to select the databases and decide on the research question, based on CF’s knowledge of the field of implicit bias and SH’s knowledge of systematic reviews and bioethics literature. CF compiled the key words for the search strategy with constant advice and input from SH. CF drafted the inclusion criteria and received constant input on this from SH: CF carried out the search and downloaded the relevant articles to be scrutinised. CF and SH both independently read all the initial titles to select which were relevant, then the abstracts, and then the final included articles and discussed at each stage to resolve any disagreements. CF drafted the initial tables including the information from the studies and this was revised by SH. SH particularly revised the statistical methods used by the studies and both reviewed their methodology. CF drafted the manuscript and it was revised with comments by SH a number of times until both authors were satisfied with the manuscript. Both authors read and approved the final manuscript.
Competing interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and affiliations.
Institute for Ethics, History, and the Humanities, Faculty of Medicine University of Geneva, Genève, Switzerland
Chloë FitzGerald & Samia Hurst
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chloë FitzGerald .
Search Strategy
The following combination of subject headings and free text terms was used:
(“Prejudice” [MAJR] AND “Attitude of health personnel” [MAJR]) OR (“Attitude of health personnel/ethnology” [MH] AND “Prejudice”[MH]) OR (“Stereotyping”[MH] AND “Attitude of health personnel”) OR (“Prejudice”[MH] AND “Healthcare disparities” [MH]) OR (“Prejudice”[MH] AND “Cultural Competency” [MH]) OR (“Social Class” [MH] AND “Attitude of health personnel” [MH]) OR (“Prejudice”[MH] AND “Physicians” [MH]) OR (“Prejudice”[MAJR] AND “Delivery of Health Care”[MAJR] AND “stereotyping”[MAJR]) OR (“Physician-Patient Relations” [MH] AND “health status disparities”[MH]) OR (“Prejudice”[MH] AND “Obesity”[MH]) OR (“African Americans/psychology” [MH] AND “Healthcare disparities” [MH]) OR (“Prejudice”[MH] AND “Mentally Ill Persons”[MH]) OR (“Prejudice”[MH] AND “Women’s Health”[MH]) OR “aversive racism” OR “anti-fat bias” OR “racial-ethnic bias” OR “racial-ethnic biases” OR “ethnic/racial bias” OR “ethnic/racial biases” OR (“disabled persons”[MAJR] AND “prejudice”[MAJR])
Dates: 1st March 2003 to 31st March 2013
Final number of retrieved articles: 2510
PsychINFO and PsychARTICLE
The following combination of subject headings and free text terms was used was used:
Health personnel AND (prejudice OR bias)
Other filters: Scholarly journals
Final number of retrieved articles: 377
Final result when duplicates removed: 360.
Prejudice [MM Exact Major Subject Heading] OR stereotyping [MM Exact Major Subject Heading] OR Discrimination [MM Exact Major Subject Heading] OR implicit bias OR unconscious bias
Other filters:
Exclude Medline records
Peer reviewed
Final number of retrieved articles: 897
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
FitzGerald, C., Hurst, S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics 18 , 19 (2017). https://doi.org/10.1186/s12910-017-0179-8
Download citation
Received : 19 October 2016
Accepted : 14 February 2017
Published : 01 March 2017
DOI : https://doi.org/10.1186/s12910-017-0179-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implicit bias
- Stereotyping
- Attitudes of health personnel
- Healthcare disparities
BMC Medical Ethics
ISSN: 1472-6939
- General enquiries: [email protected]

How does implicit bias by physicians affect patients' health care?
Research is exploring how specific factors affect patients’ perception of treatment
By Tori DeAngelis
March 2019, Vol 50, No. 3
Print version: page 22
13 min read

- Health and Behavior
- Implicit Bias
CE credits: 1
Learning objectives: After reading this article, CE candidates will be able to:
- Discuss research that suggests some health-care providers have implicit bias toward various patient groups.
- Discuss how certain combinations of physicians and patients lead to poorer interactions.
- Describe possible interventions to improve patient-physician interactions.
For more information on earning CE credit for this article, go to www.apa.org/ed/ce/resources/ce-corner.aspx .
The theory of aversive racism, first posed in the 1970s, encompasses some of the most widely studied ideas in social psychology. According to theory developers Samuel L. Gaertner, PhD, of the University of Delaware, and John F. Dovidio, PhD, of Yale University, people may hold negative nonconscious or automatic feelings and beliefs about others that can differ from their conscious attitudes, a phenomenon known as implicit bias. When there’s a conflict between a person’s explicit and implicit attitudes—when people say they’re not prejudiced but give subtle signals that they are, for example—those on the receiving end may be left anxious and confused.
Lab studies have long tested these ideas in relation to employment decisions, legal decisions and more.
In 2003, the concepts received an empirical boost from “Unequal Treatment,” a report from an Institute of Medicine (IoM) panel made up of behavioral scientists, physicians, public health experts and other health professionals. The report concluded that even when access-to-care barriers such as insurance and family income were controlled for, racial and ethnic minorities received worse health care than nonminorities, and that both explicit and implicit bias played potential roles.
“The report really opened a lot of doors to further research on bias in care,” says Dovidio, who served on the IoM panel.
Psychologists and others are now building on the IoM findings by exploring how specific factors, including physicians’ use of patronizing language and patients’ past experiences with discrimination, affect patients’ perception of providers and care. Research is also starting to look at how implicit bias affects the dynamics of physician-patient relationships and subsequent care for patients with particular diseases, such as cancer and diabetes.
Tackling this topic can be difficult because of the real-world challenges of getting medical professionals to engage in these studies, researchers say. Another problem is that the main measure used to assess implicit bias, the Implicit Association Test (IAT), has come under fire in recent years for reasons including poor test-retest reliability and the argument that higher IAT scores do not necessarily predict biased behavior.
While this disagreement remains to be resolved, researchers are starting to use other measures and techniques to assess implicit bias, as well as new methodologies to track patient attitudes and outcomes. And while the predictive power of the IAT may be relatively small, in the aggregate, even small effects can have large consequences for minority patients (see Journal of Personality and Social Psychology , Vol. 108, No. 4, 2015).
Implicit bias is called implicit for a reason—it’s not easy to capture or to fix, says Michelle van Ryn, PhD, an endowed professor at Oregon Health & Science University (OHSU). But it is worth a deeper dive because of its implications for patient treatment on both a personal and a health-care level, she says.
“Implicit bias creates inequalities through many difficult-to-measure pathways, and as a consequence,people tend to underestimate its impact,” says van Ryn. “This kind of research is essential in making real progress toward health-care equality.”
How bias plays out
One of the first psychologists to apply theories of aversive racism and implicit bias in a real-world medical setting is social psychologist Louis A. Penner, PhD, senior scientist at Wayne State University’s Karmanos Cancer Institute. Along with Dovidio, Gaertner and others, he asked patients and physicians before a medical appointment about their race-related attitudes, and measured physicians’ implicit bias. The researchers also video-recorded patients and physicians during the appointment and asked them to complete questionnaires afterward.
The team found that black patients felt most negatively toward physicians who were low in explicit bias but high in implicit bias, demonstrating the validity of the implicit-bias theory in real-world medical interactions, says Penner ( Journal of Experimental Social Psychology , Vol. 46, No. 2, 2010).
Researchers are also examining ways that providers may inadvertently demonstrate such bias, including through language. In a study in Social Science & Medicine (Vol. 87, 2013), Nao Hagiwara, PhD, at Virginia Commonwealth University, and colleagues found that physicians with higher implicit-bias scores commandeered a greater portion of the patient-physician talk time during appointments than did physicians with lower scores. Those findings are consistent with research by Lisa A. Cooper, MD, of Johns Hopkins University School of Medicine and colleagues, who found that physicians high in implicit bias were more likely to dominate conversations with black patients than were those lower in implicit bias, and that black patients trusted them less, had less confidence in them, and rated their quality of care as poorer ( American Journal of Public Health , Vol. 102, No. 5, 2012).
The individual words that physicians use can also signal implicit bias, Hagiwara has found. She looked at physicians’ tendency to use first-person plural pronouns such as “we,” “ours” or “us” when interacting with black patients. According to social psychology theories related to power dynamics and social dominance, people in power use such verbiage to maintain control over others of lesser power. In line with those theories, she found that physicians who scored higher in implicit bias spoke more of these words than colleagues lower in implicit bias, using language such as, “We’re going to take our medicine, right?” ( Health Communication , Vol. 32, No. 4, 2017).
Specific diseases and populations
Another line of research is investigating physician and patient attitudes among patients with specific diseases. This work is shedding more light on the role that patients may play in poor communication and relationship outcomes, and eventually aims to show whether poor communication affects health outcomes.

In another study, Penner and colleagues looked more specifically at how past discrimination may influence black cancer patients’ perception of care and their reactions to it. Patients who reported high rates of past discrimination and general suspicion of their health care talked more during sessions, showed fewer positive emotions and rated their physicians more negatively than those who reported less past discrimination and lower suspicion ( Social Science & Medicine , Vol. 191, 2017).
“Individually and jointly, the race-related attitudes of both nonblack physicians and their black patients negatively affect what transpires during their medical interactions and the outcomes that follow them,” Penner says.
Meanwhile, Hagiwara is focusing on black patients with Type 2 diabetes as part of a four-year study funded by the National Institute of Diabetes and Digestive and Kidney Diseases ( BMJ Open , Vol. 8, e022623, 2018). She and colleagues will assess the role of physician communication behaviors as they relate to patients’ trust in and satisfaction with their providers, and then see how those interactions relate to health outcomes.
In addition to using surveys and video recordings of patient-physician interactions, the team will attempt to gain a deeper understanding of patient reactions than previous studies. They’ll do this first by having patients view the videos without interruption as the team gathers their physiological responses, including heart rate, skin conductance and eye gaze. Then, patients will watch the video a second time, stop the videos whenever they have a positive or negative reaction to them, and explain why. The team will also stop the videos in places where they recorded patients’ physiological responses and ask patients additional questions to ascertain possible nonconscious responses. Six months later, the team will examine how those findings influence health behaviors and outcomes by examining patients’ lab values, diabetes complications, and self-reported treatment adherence—the first study to directly assess such health outcomes.
Focusing intensively on one disease “will help our understanding of the role of implicit bias in clinical outcomes,” Hagiwara says.
Medical students and more
While most implicit-bias studies in health-care treatment have been conducted with black patients and nonblack providers, other researchers are investigating implicit bias in relation to other ethnic groups, people with obesity, sexual and gender minorities, people with mental health and substance use disorders, older adults and people with various health conditions.
Medical school is one arena where this work is taking place. OHSU’s van Ryn, who is founder and head of a translational research company called Diversity Science in Portland, Oregon, is principal investigator in a long-term study of medical students and residents examining whether and how the medical school and residency training environments might influence future doctors’ racial and other biases. For the past eight years, she, Dovidio and colleagues have been surveying a cadre of 4,732 medical students attending 49 of the nation’s 128 allopathic medical schools, who first entered medical school in 2010.
The study , funded by a number of sources, including the National Institutes of Health, asks students on a regular basis about their implicit and explicit attitudes toward racial and other minorities, and how these views might change over time.
In several studies using this data set, the team has found that student reports of organizational climate, contact with minority faculty and patients, and faculty role-modeling were more strongly related to changes in implicit and explicit bias than their experiences with formal curricula or formal training ( Journal of General Internal Medicine , Vol. 30, No. 12, 2015). These include studies headed by health services researcher Sean Phelan, PhD, of the Mayo Clinic, that examine medical student reactions to patients who are obese and who identify as LGBT. In prospective studies of the initial medical student cohort, he found results similar to those involving race: for example, that students with lower implicit-bias scores were more likely to have had frequent contact with LGBT faculty, residents, students and patients, and that those with higher scores were more likely to have been exposed to faculty who exhibited discriminatory behavior ( Journal of General Internal Medicine , Vol. 32, No. 11, 2017).
In terms of race, van Ryn’s team also found that students who entered medical school with lower implicit-bias scores and many positive experiences with people of different races were likely to build on those experiences during medical school, says Dovidio.
“It’s like a ripple effect,” he says. “They come into medical school with more positive racial attitudes, so during medical school they feel less interracial anxiety and interact in more positive ways with patients. And those experiences of contact in medical school have an additive effect that goes over and above their earlier contact experiences.”
How to intervene

Such findings suggest the importance of using psychological methods to address psychological problems, Penner adds. “The goal of interventions shouldn’t be to confront physicians with their implicit bias and get them to change it,” he says, “but rather to make it less important in their interactions.”
Promising strategies include those aimed at getting physicians to see a patient as an individual rather than as a stereotyped member of a group, helping patients become more engaged with their treatment and fostering patients’ sense of being “on the same team” as their doctor ( Journal of General Internal Medicine , Vol. 28, No. 9, 2013).
Researcher Jeff Stone, PhD, a professor of psychology at the University of Arizona, is using some of these ideas in workshops he’s developed for medical students. “For them, this is about how to improve their skills as a doctor or nurse,” he says. “We don’t just expose them to these ideas and leave it at that—we have them practice them.”
For example, the workshop uses the strategy of individualizing patients to encourage medical students to question stereotypes about a patient’s ethnic group, such as the notion that Hispanics don’t adhere to medical advice. Instead, a medical student may be told to ask all patients specific questions about adherence, like whether they have finished all of their medications or have made an appointment for a referral. Stone has just completed a study related to this work and is now examining whether changes in implicit bias correspond with better treatment of patients in the clinic.
Another promising intervention, the prejudice habit-breaking intervention, is based on a theory developed by Patricia G. Devine, PhD, and William T.L. Cox, PhD, of the University of Wisconsin—Madison. The intervention, which adopts the premise that bias, whether implicit or explicit, is a habit that can be overcome with motivation, awareness and effort, includes experiential, educational and training components. A study by Patrick S. Forscher, PhD, of the University of Arkansas, and colleagues found that compared with controls, people who received the intervention were more likely after 14 days to feel concern about the targets of prejudice and to label biases as wrong, though that awareness later declined. However, in a subsample of original participants two years later, those who received the intervention were more likely than controls to object to an online essay endorsing racial stereotyping, the team found ( Journal of Experimental Social Psychology , Vol. 72, 2017).
What's next?
Psychologists who study implicit bias in health care acknowledge there is much more to learn. That includes discovering ways that patient-physician interactions might lead to poorer health outcomes down the road, and conducting research on other populations besides black patients and nonblack physicians. On a more discrete level, it includes achieving a better understanding of how situational factors like stress and time constraints could activate bias and influence treatment decisions.
Researchers also acknowledge that individual interventions are just one way to reduce providers’ implicit bias. Equally important are systemic interventions, the mission of van Ryn’s company, Diversity Science. The company helps organizations apply the best findings and interventions on implicit bias to create inclusive cultures. Ways they do this include conducting climate assessments using evidence-based tools and questionnaires, giving leaders feedback on that data, and providing ongoing training for all employees, including case demonstrations and refreshers.
Also important is conducting this work with other disciplines and recognizing that environmental factors such as access to transportation and proximity to toxic environments can play significant roles in health disparities, says Dovidio.
“When you put together physicians’ implicit bias, geography, patient attitudes, the patient-doctor interaction and organizational, historical and structural factors,” he says, “you get a holistic picture of what can cause health disparities and specific avenues to remedy them. Understanding how these processes contribute jointly to health-care disparities,” he adds, “is necessary for addressing such a persistent and complex problem—one with life-or-death consequences.”
Further reading
Racial Biases in Medicine and Healthcare Disparities Dovidio, J., et al., TPM , 2016
Examining the Presence, Consequences, and Reduction of Implicit Bias in Health Care: A Narrative Review Zestcott, C.A., et al., Group Processes & Intergroup Relations , 2016
Implicit Bias in U.S. Medicine: Complex Findings and Incomplete Conclusions Chisolm-Straker, M., & Straker, H.O., International Journal of Human Rights in Healthcare , 2017
Doing Harm to Some: Patient and Provider Attitudes and Healthcare Disparities Penner, L.A., et al. In D. Albarracin & B.T. Johnson (Eds.), The Handbook of Attitudes , 2nd ed., Vol. 2—Applications, 2019
- Research shows that many providers hold some level of implicit bias toward various patient groups, with most studies examining interactions between black patients and nonblack providers.
- Certain combinations of physicians and patients lead to poorer interactions, specifically those in which physicians are high in implicit bias and patients are high in mistrust of the medical system and reported past discrimination.
- Research on interventions is still developing, but one promising strategy includes helping patients feel that they are on the same team as the provider.
"CE Corner" is a continuing education article offered by APA's Office of CE in Psychology. To earn CE credit, after you read this article, complete an online learning exercise and take a CE test. Upon successful completion of the test—a score of 75 percent or higher—you can immediately print your certificate.
To purchase the online program visit www.apa.org/ed/ce/resources/ce-corner.aspx . The test fee is $25 for members and $35 for nonmembers. For more information, call (800) 374-2721.
As an APA member, take advantage of your five free CE credits per year. Select the free online programs through your MyAPA account.
Letters to the Editor
- Send us a letter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Implicit bias in healthcare professionals: a systematic review
Affiliations.
- 1 Institute for Ethics, History, and the Humanities, Faculty of Medicine University of Geneva, Genève, Switzerland. [email protected].
- 2 Institute for Ethics, History, and the Humanities, Faculty of Medicine University of Geneva, Genève, Switzerland.
- PMID: 28249596
- PMCID: PMC5333436
- DOI: 10.1186/s12910-017-0179-8
Background: Implicit biases involve associations outside conscious awareness that lead to a negative evaluation of a person on the basis of irrelevant characteristics such as race or gender. This review examines the evidence that healthcare professionals display implicit biases towards patients.
Methods: PubMed, PsychINFO, PsychARTICLE and CINAHL were searched for peer-reviewed articles published between 1st March 2003 and 31st March 2013. Two reviewers assessed the eligibility of the identified papers based on precise content and quality criteria. The references of eligible papers were examined to identify further eligible studies.
Results: Forty two articles were identified as eligible. Seventeen used an implicit measure (Implicit Association Test in fifteen and subliminal priming in two), to test the biases of healthcare professionals. Twenty five articles employed a between-subjects design, using vignettes to examine the influence of patient characteristics on healthcare professionals' attitudes, diagnoses, and treatment decisions. The second method was included although it does not isolate implicit attitudes because it is recognised by psychologists who specialise in implicit cognition as a way of detecting the possible presence of implicit bias. Twenty seven studies examined racial/ethnic biases; ten other biases were investigated, including gender, age and weight. Thirty five articles found evidence of implicit bias in healthcare professionals; all the studies that investigated correlations found a significant positive relationship between level of implicit bias and lower quality of care.
Discussion: The evidence indicates that healthcare professionals exhibit the same levels of implicit bias as the wider population. The interactions between multiple patient characteristics and between healthcare professional and patient characteristics reveal the complexity of the phenomenon of implicit bias and its influence on clinician-patient interaction. The most convincing studies from our review are those that combine the IAT and a method measuring the quality of treatment in the actual world. Correlational evidence indicates that biases are likely to influence diagnosis and treatment decisions and levels of care in some circumstances and need to be further investigated. Our review also indicates that there may sometimes be a gap between the norm of impartiality and the extent to which it is embraced by healthcare professionals for some of the tested characteristics.
Conclusions: Our findings highlight the need for the healthcare profession to address the role of implicit biases in disparities in healthcare. More research in actual care settings and a greater homogeneity in methods employed to test implicit biases in healthcare is needed.
Keywords: Attitudes of health personnel; Healthcare disparities; Implicit bias; Prejudice; Stereotyping.
PubMed Disclaimer
Similar articles
- Implicit Bias. Shah HS, Bohlen J. Shah HS, et al. 2023 Mar 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. 2023 Mar 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 36944001 Free Books & Documents.
- Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review. Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, Coyne-Beasley T. Hall WJ, et al. Am J Public Health. 2015 Dec;105(12):e60-76. doi: 10.2105/AJPH.2015.302903. Epub 2015 Oct 15. Am J Public Health. 2015. PMID: 26469668 Free PMC article. Review.
- A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. Maina IW, et al. Soc Sci Med. 2018 Feb;199:219-229. doi: 10.1016/j.socscimed.2017.05.009. Epub 2017 May 4. Soc Sci Med. 2018. PMID: 28532892 Review.
- Estimating Implicit and Explicit Gender Bias Among Health Care Professionals and Surgeons. Salles A, Awad M, Goldin L, Krus K, Lee JV, Schwabe MT, Lai CK. Salles A, et al. JAMA Netw Open. 2019 Jul 3;2(7):e196545. doi: 10.1001/jamanetworkopen.2019.6545. JAMA Netw Open. 2019. PMID: 31276177
- Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. Haider AH, Schneider EB, Sriram N, Dossick DS, Scott VK, Swoboda SM, Losonczy L, Haut ER, Efron DT, Pronovost PJ, Lipsett PA, Cornwell EE 3rd, MacKenzie EJ, Cooper LA, Freischlag JA. Haider AH, et al. JAMA Surg. 2015 May;150(5):457-64. doi: 10.1001/jamasurg.2014.4038. JAMA Surg. 2015. PMID: 25786199
- Parent and healthcare professional experiences of critical congenital heart disease in New Zealand to advance health equity. Watkins S, Ward K, Brown R, Crengle S, Wm de Laat M, Percival T, Sadler L, Cloete E, Gorinski R, Gentles T, Bloomfield FH. Watkins S, et al. BMC Health Serv Res. 2024 Aug 26;24(1):991. doi: 10.1186/s12913-024-11410-4. BMC Health Serv Res. 2024. PMID: 39187808 Free PMC article.
- The prevalence of Black/African American individuals in concussion literature: a systematic review and meta-analysis. MacEachern T, John-Baptiste A, Christie A. MacEachern T, et al. Front Public Health. 2024 Aug 8;12:1430428. doi: 10.3389/fpubh.2024.1430428. eCollection 2024. Front Public Health. 2024. PMID: 39185117 Free PMC article.
- Skin Type Diversity in Skin Lesion Datasets: A Review. Alipour N, Burke T, Courtney J. Alipour N, et al. Curr Dermatol Rep. 2024;13(3):198-210. doi: 10.1007/s13671-024-00440-0. Epub 2024 Aug 14. Curr Dermatol Rep. 2024. PMID: 39184010 Free PMC article. Review.
- Alignment of contraception use with the ACR reproductive health guidelines in women with systemic lupus erythematosus within the RISE registry. Clowse MEB, Li J, Snyderman A, Schmajuk G. Clowse MEB, et al. Lupus Sci Med. 2024 Aug 24;11(2):e001192. doi: 10.1136/lupus-2024-001192. Lupus Sci Med. 2024. PMID: 39181689 Free PMC article.
- The nature and validity of implicit bias training for health care providers and trainees: A systematic review. Hagiwara N, Duffy C, Cyrus J, Harika N, Watson GS, Green TL. Hagiwara N, et al. Sci Adv. 2024 Aug 16;10(33):eado5957. doi: 10.1126/sciadv.ado5957. Epub 2024 Aug 14. Sci Adv. 2024. PMID: 39141723 Free PMC article. Review.
- Holroyd J, Sweetman J. The Heterogeneity of Implicit Bias. In Brownstein, Michael, Saul, Jennifer, editors. Implicit Bias and Philosophy, Volume 1: Metaphysics and Epistemology 1. Oxford: Oxford University Press; 2016. p. 80–103.
- Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: where do we go from here? Perm J. 2011;15:71. - PMC - PubMed
- Ambady N, Shih M, Kim A, Pittinsky TL. Stereotype susceptibility in children: effects of identity activation on quantitative performance. Psychol Sci. 2001;12:385–390. doi: 10.1111/1467-9280.00371. - DOI - PubMed
- Louise A. Bias: Friend or Foe? Reflections on Saulish Skepticism. In Brownstein, Michael, Saul, Jennifer, editors. Implicit Bias and Philosophy, Volume 1: Metaphysics and Epistemology 1. Oxford: Oxford University Press; 2016. p. 157–190.
- Nosek BA, et al. Pervasiveness and correlates of implicit attitudes and stereotypes. Eur Rev Soc Psychol. 2007;18:36–88. doi: 10.1080/10463280701489053. - DOI
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
How Does Implicit Bias Influence Behavior?
Strategies to Reduce the Impact of Implicit Bias
Getty Images
- Measurement
- Discrimination
An implicit bias is an unconscious association, belief, or attitude toward any social group. Implicit biases are one reason why people often attribute certain qualities or characteristics to all members of a particular group, a phenomenon known as stereotyping .
It is important to remember that implicit biases operate almost entirely on an unconscious level . While explicit biases and prejudices are intentional and controllable, implicit biases are less so.
A person may even express explicit disapproval of a certain attitude or belief while still harboring similar biases on a more unconscious level. Such biases do not necessarily align with our own sense of self and personal identity. People can also hold positive or negative associations about their own race, gender, religion, sexuality, or other personal characteristics.
Causes of Implicit Bias
While people might like to believe that they are not susceptible to these implicit biases and stereotypes, the reality is that everyone engages in them whether they like it or not. This reality, however, does not mean that you are necessarily prejudiced or inclined to discriminate against other people. It simply means that your brain is working in a way that makes associations and generalizations.
In addition to the fact that we are influenced by our environment and stereotypes that already exist in the society into which we were born, it is generally impossible to separate ourselves from the influence of society.
You can, however, become more aware of your unconscious thinking and the ways in which society influences you.
It is the natural tendency of the brain to sift, sort, and categorize information about the world that leads to the formation of these implicit biases. We're susceptible to bias because of these tendencies:
- We tend to seek out patterns . Implicit bias occurs because of the brain's natural tendency to look for patterns and associations in the world. Social cognition , or our ability to store, process, and apply information about people in social situations, is dependent on this ability to form associations about the world.
- We like to take shortcuts . Like other cognitive biases , implicit bias is a result of the brain's tendency to try to simplify the world. Because the brain is constantly inundated with more information than it could conceivably process, mental shortcuts make it faster and easier for the brain to sort through all of this data.
- Our experiences and social conditioning play a role . Implicit biases are influenced by experiences, although these attitudes may not be the result of direct personal experience. Cultural conditioning, media portrayals, and upbringing can all contribute to the implicit associations that people form about the members of other social groups.
How Implicit Bias Is Measured
The term implicit bias was first coined by social psychologists Mahzarin Banaji and Tony Greenwald in 1995. In an influential paper introducing their theory of implicit social cognition, they proposed that social behavior was largely influenced by unconscious associations and judgments.
In 1998, Banaji and Greenwald published their now-famous Implicit Association Test (IAT) to support their hypothesis . The test utilizes a computer program to show respondents a series of images and words to determine how long it takes someone to choose between two things.
Subjects might be shown images of faces of different racial backgrounds, for example, in conjunction with either a positive word or a negative word. Subjects would then be asked to click on a positive word when they saw an image of someone from one race and to click on a negative word when they saw someone of another race.

Interpreting the Results
The researchers suggest that when someone clicks quickly, it means that they possess a stronger unconscious association. If a person quickly clicks on a negative word every time they see a person of a particular race, the researchers suggest that this would indicate that they hold an implicit negative bias toward individuals of that race.
In addition to a test of implicit racial attitudes, the IAT has also been utilized to measure unconscious biases related to gender, weight, sexuality, disability, and other areas. The IAT has grown in popularity and use over the last decade, yet has recently come under fire.
Among the main criticisms are findings that the test results may lack reliability . Respondents may score high on racial bias on one test, and low the next time they are tested.
Also of concern is that scores on the test may not necessarily correlate with individual behavior. People may score high for a type of bias on the IAT, but those results may not accurately predict how they would relate to members of a specific social group.
Link Between Implicit Bias and Discrimination
It is important to understand that implicit bias is not the same thing as racism, although the two concepts are related. Overt racism involves conscious prejudice against members of a particular racial group and can be influenced by both explicit and implicit biases.
Other forms of discrimination that can be influenced by unconscious biases include ageism , sexism, homophobia, and ableism.
One of the benefits of being aware of the potential impact of implicit social biases is that you can take a more active role in overcoming social stereotypes, discrimination, and prejudice.
Effects of Implicit Bias
Implicit biases can influence how people behave toward the members of different social groups. Researchers have found that such bias can have effects in a number of settings, including in school, work, and legal proceedings.
Implicit Bias in School
Implicit bias can lead to a phenomenon known as stereotype threat in which people internalize negative stereotypes about themselves based upon group associations. Research has shown, for example, that young girls often internalize implicit attitudes related to gender and math performance.
By the age of 9, girls have been shown to exhibit the unconscious beliefs that females have a preference for language over math. The stronger these implicit beliefs are, the less likely girls and women are to pursue math performance in school. Such unconscious beliefs are also believed to play a role in inhibiting women from pursuing careers in science, technology, engineering, and mathematics (STEM) fields.
Studies have also demonstrated that implicit attitudes can also influence how teachers respond to student behavior, suggesting that implicit bias can have a powerful impact on educational access and academic achievement.
One study, for example, found that Black children—and Black boys in particular—were more likely to be expelled from school for behavioral issues. When teachers were told to watch for challenging behaviors, they were more likely to focus on Black children than on White children.
Implicit Bias In the Workplace
While the Implicit Attitude Test itself may have pitfalls, these problems do not negate the existence of implicit bias. Or the existence and effects of bias, prejudice, and discrimination in the real world. Such prejudices can have very real and potentially devastating consequences.
One study, for example, found that when Black and White job seekers sent out similar resumes to employers, Black applicants were half as likely to be called in for interviews as White job seekers with equal qualifications.
Such discrimination is likely the result of both explicit and implicit biases toward racial groups.
Even when employers strive to eliminate potential bias in hiring, subtle implicit biases may still have an impact on how people are selected for jobs or promoted to advanced positions. Avoiding such biases entirely can be difficult, but being aware of their existence and striving to minimize them can help.
Implicit Bias in Healthcare Settings
Certainly, age, race, or health condition should not play a role in how patients get treated, however, implicit bias can influence quality healthcare and have long-term impacts including suboptimal care, adverse outcomes, and even death.
For example, one study published in the American Journal of Public Health found that physicians with high scores in implicit bias tended to dominate conversations with Black patients and, as a result, the Black patients had less confidence and trust in the provider and rated the quality of their care lower.
Researchers continue to investigate implicit bias in relation to other ethnic groups as well as specific health conditions, including type 2 diabetes, obesity, mental health, and substance use disorders.
Implicit Bias in Legal Settings
Implicit biases can also have troubling implications in legal proceedings, influencing everything from initial police contact all the way through sentencing. Research has found that there is an overwhelming racial disparity in how Black defendants are treated in criminal sentencing.
Not only are Black defendants less likely to be offered plea bargains than White defendants charged with similar crimes, but they are also more likely to receive longer and harsher sentences than White defendants.
Strategies to Reduce the Impact of Implict Bias
Implicit biases impact behavior, but there are things that you can do to reduce your own bias. Some ways that you can reduce the influence of implicit bias:
- Focus on seeing people as individuals . Rather than focusing on stereotypes to define people, spend time considering them on a more personal, individual level.
- Work on consciously changing your stereotypes . If you do recognize that your response to a person might be rooted in biases or stereotypes, make an effort to consciously adjust your response.
- Take time to pause and reflect . In order to reduce reflexive reactions, take time to reflect on potential biases and replace them with positive examples of the stereotyped group.
- Adjust your perspective . Try seeing things from another person's point of view. How would you respond if you were in the same position? What factors might contribute to how a person acts in a particular setting or situation?
- Increase your exposure . Spend more time with people of different racial backgrounds. Learn about their culture by attending community events or exhibits.
- Practice mindfulness . Try meditation, yoga, or focused breathing to increase mindfulness and become more aware of your thoughts and actions.
While implicit bias is difficult to eliminate altogether, there are strategies that you can utilize to reduce its impact. Taking steps such as actively working to overcome your biases , taking other people's perspectives, seeking greater diversity in your life, and building your awareness about your own thoughts are a few ways to reduce the impact of implicit bias.
A Word From Verywell
Implicit biases can be troubling, but they are also a pervasive part of life. Perhaps more troubling, your unconscious attitudes may not necessarily align with your declared beliefs. While people are more likely to hold implicit biases that favor their own in-group, it is not uncommon for people to hold biases against their own social group as well.
The good news is that these implicit biases are not set in stone. Even if you do hold unconscious biases against other groups of people, it is possible to adopt new attitudes, even on the unconscious level. This process is not necessarily quick or easy, but being aware of the existence of these biases is a good place to start making a change.
Jost JT. The existence of implicit bias is beyond reasonable doubt: A refutation of ideological and methodological objections and executive summary of ten studies that no manager should ignore . Research in Organizational Behavior . 2009;29:39-69. doi:10.1016/j.riob.2009.10.001
Greenwald AG, Mcghee DE, Schwartz JL. Measuring individual differences in implicit cognition: The implicit association test . J Pers Soc Psychol. 1998;74(6):1464-1480. doi:10.1037/0022-3514.74.6.1464
Sabin J, Nosek BA, Greenwald A, Rivara FP. Physicians' implicit and explicit attitudes about race by MD race, ethnicity, and gender . J Health Care Poor Underserved. 2009;20(3):896-913. doi:10.1353/hpu.0.0185
Capers Q, Clinchot D, McDougle L, Greenwald AG. Implicit racial bias in medical school admissions . Acad Med . 2017;92(3):365-369. doi:10.1097/ACM.0000000000001388
Kiefer AK, Sekaquaptewa D. Implicit stereotypes and women's math performance: How implicit gender-math stereotypes influence women's susceptibility to stereotype threat . Journal of Experimental Social Psychology. 2007;43(5):825-832. doi:10.1016/j.jesp.2006.08.004
Steffens MC, Jelenec P, Noack P. On the leaky math pipeline: Comparing implicit math-gender stereotypes and math withdrawal in female and male children and adolescents . Journal of Educational Psychology. 2010;102(4):947-963. doi:10.1037/a0019920
Edward Zigler Center in Child Development & Social Policy, Yale School of Medicine. Implicit Bias in Preschool: A Research Study Brief .
Pager D, Western B, Bonikowski B. Discrimination in a low-wage labor market: A field experiment . Am Sociol Rev. 2009;74(5):777-799. doi:10.1177/000312240907400505
Malinen S, Johnston L. Workplace ageism: Discovering hidden bias . Exp Aging Res. 2013;39(4):445-465. doi:10.1080/0361073X.2013.808111
Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care . Am J Public Health . 2012;102(5):979-87. doi:10.2105/AJPH.2011.300558
Leiber MJ, Fox KC. Race and the impact of detention on juvenile justice decision making . Crime & Delinquency. 2005;51(4):470-497. doi:10.1177/0011128705275976
Van Ryn M, Hardeman R, Phelan SM, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: A medical student CHANGES study report . J Gen Intern Med. 2015;30(12):1748-1756. doi:10.1007/s11606-015-3447-7
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- How unconscious bias...
How unconscious bias can discriminate against patients and affect their care
- Related content
- Peer review
This article has a correction. Please see:
- How unconscious bias can discriminate against patients and affect their care - November 13, 2020
- Kathy Oxtoby , journalist
- kathyoxtoby1{at}gmail.com
Our assumptions, which we may not even be aware of, can lead to erroneous clinical decisions. More research, awareness, training, and diverse teams are needed to tackle this, Kathy Oxtoby finds
Older patients are typically sedentary, you assume—without realising it. A patient you relate to well receives that bit more time and attention, although you’re not aware of giving preferential treatment. Or maybe you speak to some patients in a certain way because of your beliefs about their social class. If not these exactly, you’re likely to have made assumptions like them, and all are examples of unconscious bias.
Sarah Mumford, programmes director at IVE, a company that delivers workshops on unconscious bias, describes this type of bias as “what happens when our brains make snap judgments about people, places, and things based upon past experiences.”
Like the wider population, healthcare professionals exhibit unconscious bias, a 2017 systematic review found. 1 Scarlett A McNally, vascular surgeon and a council member of the Royal College of Surgeons of England, says that doctors are “only human” and are therefore not exempt from making assumptions about someone “because of their age, race, sexual orientation, or religion.”
This unconscious bias, also known as implicit bias, is important in a medical setting “because it may affect decision making about how care proceeds,” she says.
Discrimination against patients
Many types of implicit bias discriminate against patients (box 1). Pete Jones, a chartered psychologist at Shire Professional Chartered Psychologists, which provides unconscious bias training, says that it “leads us to value some groups more than others, based on such factors as ethnicity, gender, and disability, which all play a critical role in patient care.”
Patients’ implicit biases
It’s not only healthcare professionals who will have unconscious bias—their patients will too. “Unconscious bias can cut both ways in the patient-doctor relationship,” says Scarlett A …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
- Find Accredited Organizations

Quick Safety 23: Implicit bias in health care
“Of all forms of inequity, injustice in health care is the most shocking and inhuman.”
— Martin Luther King, Jr., National Convention of the Medical Committee for Human Rights, Chicago, 1966
Issue:
On the eve of the 15th anniversary of two seminal reports from the Institute of Medicine (IOM) – Crossing the Quality Chasm 1 and Unequal Treatment 2 – we find that racial and socioeconomic inequity persists in health care. In Crossing the Quality Chasm, the IOM stressed the importance of equity in care as one of the six pillars of quality health care, along with efficiency, effectiveness, safety, timeliness and patient-centeredness. Indeed, Unequal Treatment found that even with the same insurance and socioeconomic status, and when comorbidities, stage of presentation and other confounders are controlled for, minorities often receive a lower quality of health care than do their white counterparts.
Professor Margaret Whitehead, head of the World Health Organization (WHO) Collaborating Centre for Policy Research on Social Determinants of Health, perhaps provides the most intuitive and clear definition of health inequalities (the term used in most countries, where it is generally assumed to refer to socioeconomic differences in health). She defines health inequalities as health differences that “are not only unnecessary and avoidable but, in addition, are considered unfair and unjust.” She also states that “equity in health implies that, ideally, everyone should have a fair opportunity to attain their full health potential and, more pragmatically, that no one should be disadvantaged from achieving this potential, if it can be avoided.” 3,4
There is extensive evidence and research that finds unconscious biases can lead to differential treatment of patients by race, gender, weight, age, language, income and insurance status. The purpose of this issue of Quick Safety is to discuss the impact of implicit bias on patient safety. Bias in clinical decision-making does result in overuse or underuse problems that can directly lead to patient harm.
What is “implicit bias?”
Implicit (subconscious) bias refers to the attitudes or stereotypes that affect our understanding, actions and decisions in an unconscious manner. 13 These biases, which encompass both favorable and unfavorable assessments, are activated involuntarily and without an individual’s awareness or intentional control. 14
In 1995, Anthony Greenwald and M.R. Benaji hypothesized that our social behavior was not entirely under our conscious control. According to their study, the concept of unconscious bias (hidden bias or implicit bias ) suggests that “much of our social behavior is driven by learned stereotypes that operate automatically – and therefore unconsciously – when we interact with other people.” 15
Hidden bias tests measure unconscious, or automatic, biases. An individual’s willingness to examine their own possible biases is an important step in understanding the roots of stereotypes and prejudice in our society. The ability to distinguish friend from foe helped early humans survive, and the ability to quickly and automatically categorize people is a fundamental quality of the human mind. Categories give order to life, and every day, we group other people into categories based on social and other characteristics. This is the foundation of stereotypes, prejudice and, ultimately, discrimination.
Once learned, stereotypes and prejudices resist change, even when evidence fails to support them or points to the contrary. People will embrace anecdotes that reinforce their biases, but disregard experience that contradicts them. The statement "Some of my best friends are _____," captures this tendency to allow some exceptions without changing our bias. Research has demonstrated that biases thought to be absent or extinguished remain as "mental residue." Studies show people can be consciously committed to egalitarianism, and deliberately work to behave without prejudice, yet still possess hidden negative prejudices or stereotypes. Studies have found that school teachers clearly telegraph prejudices, so much so that some researchers believe children of color and white children in the same classroom effectively receive different educations. Jerry Kang, vice chancellor for equity, diversity and inclusion, and professor of law at UCLA Law, states: “Automatically, we categorize individuals by age, gender, race and role. Once an individual is mapped into that category, specific meanings associated with that category are immediately activated and influence our interaction with that individual.”
Implicit bias develops early in life from repeated reinforcement of social stereotypes. Implicit pro-white bias occurs among children as young as 3-5 years old. 5 The Implicit Association Test (IAT) is a computerized, timed dual-categorization task that measures implicit preferences by bypassing conscious processing. 6 The IAT is part of Project Implicit, a collaborative investigation effort between researchers at Harvard University, University of Virginia, and University of Washington. The studies examine thoughts and feelings that exist either outside of conscious awareness or conscious control. The goal of the project is to make this technique available for education (including self-education) and awareness.
Between October 1998 and October 2006, more than 4.5 million IAT tests were completed on the IAT website. The project found that:
- Implicit bias is pervasive
- People are often unaware of their implicit biases
- Implicit biases predict behavior
- People differ in levels of implicit bias
Many health care organizations have begun administering the IAT, and when it is applied to physicians, significant pro-white bias has been found. 7 However, implicit bias is not limited to race. When the IAT was administered at an obesity conference, participants implicitly associated obese people with negative cultural stereotypes, such as “bad, stupid, lazy and worthless.” 8,9 Implicit gender bias among physicians also may unknowingly sway treatment decisions. Women are three times less likely than men to receive knee arthroplasty when clinically appropriate. 10,11,12 One of the stereotypical reasons for this inequity and underuse problem is that men are viewed as being more stoic and more inclined to participate in strenuous or rigorous activity.
This difference in treatment and clinical decision-making, though unintentional, could lead to failures in patient-centered care, interpersonal treatment (e.g., does the doctor care for you), communication (e.g., did the doctor answer my questions), trust (e.g., the clinicians’ integrity), and contextual knowledge (e.g., your doctor’s knowledge of your values and beliefs). How a physician communicates, his or her body language and verbal cues can be an expression of subconscious bias.
Implicit bias and its effect on health care
Research supports a relationship between patient care and physician bias in ways that could perpetuate health care disparities. 9 What makes implicit bias “frightening” in health and health care is that the result is “unthinking discrimination” of which caregivers are not aware.
Academic researchers, in efforts to explain differences in health outcomes, posit that the reasons include lack of trust, communications problems, or simply “unknown and complex” reasons. 16 A 2011 study conducted by van Ryn et al. concludes that racism can interact with cognitive biases to affect clinicians’ behavior and decisions and in turn, patient behavior and decisions (e.g., higher treatment dropout, lower participation in screening, avoidance of health care, delays in seeking help and filling prescriptions, and lower ratings of health care quality). 17 This unconscious or implicit bias indicates many white health care providers harbor a broad racial framing of Americans of color, one that can be causative in their not providing equitable health care.
Some examples of how implicit bias plays out in health care include:
- Non-white patients receive fewer cardiovascular interventions and fewer renal transplants
- Black women are more likely to die after being diagnosed with breast cancer
- Non-white patients are less likely to be prescribed pain medications (non-narcotic and narcotic)
- Black men are less likely to receive chemotherapy and radiation therapy for prostate cancer and more likely to have testicle(s) removed
- Patients of color are more likely to be blamed for being too passive about their health care
Implicit bias is not isolated to adult care. At a well-known academic medical center, a child presented with difficulty breathing that baffled the care team. The team of physicians were agonizing over a light box, reviewing the patient’s X-rays, puzzled because they couldn’t determine a diagnosis. Another physician just passing through looked at the X-rays and immediately said, “cystic fibrosis.” The team was tripped up by the patient’s race, which was black, and that the patient had a “white disease.”
Can we overcome implicit bias in health care?
The good news is that with organizational support, skills training, and cognitive resources, clinicians who are highly motivated to control prejudice and bias awareness can successfully prevent racism from affecting the quality of care they provide. 17 Some of the skills (from van Ryn et al.) 17 that help lower racial bias include:
- Perspective-taking: The cognitive component of empathy, 17 perspective-taking can reduce bias and inhibit unconscious stereotypes and prejudices. Physician empathy positively affects patient satisfaction, self-efficacy perceptions of control, emotional distress, adherence, and health outcomes.
- Emotional regulation skills: Clinicians who have good emotional regulation skills and who experience positive emotion during clinical encounters may be less likely to view patients in terms of their individual attributes, and to use more inclusive social categories. It’s easier to empathize with others when people view themselves as being part of a larger group.
- Partnership-building skills: Clinicians who create partnerships with patients are more likely to develop a sense that their partner is on the same “team,” working toward a common goal.
Safety Actions to Consider:
In order to ensure best outcomes and zero harm for all patients, implicit bias and racial discrimination in health and health care should be better understood, assessed and corrected. The following recommendations (from van Ryn et al.) 17 should be understood by hospital administrators and clinicians, as well as medical educators and policymakers. In order to begin to address the impact of implicit bias on clinical care decisions, health care organizations should:
- Evaluate the racial climate by evaluating employees’ shared perceptions of the policies and practices that communicate the extent to which fostering diversity and eliminating discrimination are priorities in the organization.
- Investigate reports of subtle or overt discrimination and unfair treatment.
- Identify and work to transform formal and informal norms that ignore and/or support racism.
- Establish monitoring systems in which processes and outcomes of care can be compared by patient race. Collecting data on race and other indicators of social position can be used to self-assess, monitor and evaluate the effectiveness of the organization’s strategies for eradicating inequities in care.
- Give care units and, where appropriate, individual clinicians, equity-specific targeted feedback. When inequities are found, support creative solutions for remediation and create accountability for improvement.
- Implement work policies and clinical procedures that protect clinicians from high cognitive load and promote positive emotions. When clinicians’ cognitive capacity is low or overtaxed, memory is biased toward information that is consistent with stereotypes. High cognitive load can be created by: productivity pressures, time pressure, high noise levels, inadequate staffing, poor feedback, inadequate supervision, inadequate training, high communication load, and overcrowding.
- Promote racial diversity at all levels of the organizational hierarchy and support positive intergroup contact. Intergroup contact can reduce intergroup prejudice and help reduce feelings of interracial anxiety. Additionally, institutional support for interaction can increase the benefits of intergroup contact.
- Implement and evaluate training that ensures that clinicians have the knowledge and skills needed to prevent racial biases from affecting the quality of care they provide. The training should cover self-awareness regarding implicit biases, and skills related to perspective-taking, emotional regulation, and partnership-building. 17
Actions that health care providers can take to combat implicit bias, include:
- Having a basic understanding of the cultures from which your patients come.
- Avoiding stereotyping your patients; individuate them.
- Understanding and respecting the magnitude of unconscious bias.
- Recognizing situations that magnify stereotyping and bias.
- Knowing the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care (the National CLAS Standards ).
- Performing “teach back (e.g., the National Patient Safety Foundation’s “Ask Me 3 ® ” educational program). 18
- Assiduously practicing “evidenced-based medicine.”
- Using techniques to de-bias patient care, which include training, intergroup contact, perspective-taking, emotional expression, and counter-stereotypical exemplars.
1. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press. 2001.
2. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine, Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors. 2002.
3. Whitehead M, Dahlgren M. Concepts and principles for tackling social inequities in health: Levelling up Part 1. Studies on social and economic determinants of population health, No. 2. World Health Organization Collaborating Centre for Policy Research on Social Determinants of Health, University of Liverpool. 2006.
4. Braverman P. Public Health Reports, 2014 Supplement 2, Volume 129.
5. Baron AS, Banaji MR. The development of implicit attitudes. Evidence of race evaluations from ages 6 and 10 and adulthood. Psychological Science. 2006;17(1):53-8.
6. Greenwald AG, et al. Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology. 1998;74(6):1464-80.
7. Green AR, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. Journal of General Internal Medicine. 2007;22(9):1231-8.
8. Schwartz MB, et al. Weight bias among health professionals specializing in obesity. Obesity Research. 2003;11(9):1033-9.
9. Chapman E, et al. Journal of General Internal Medicine. 28(11):1504-10.
10. Hawker GA, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. New England Journal of Medicine. 2000;343(14):1016-22.
11. Coyte PC, et al. Variation in rheumatologists’ and family physicians’ perceptions of the indications for and outcomes of knee replacement surgery. The Journal of Rheumatology. 1996;23(4):730-8.
12. Wright JG, et al. Variation in orthopedic surgeons’ perceptions of the indications for and outcomes of knee replacement. Canadian Medical Association Journal. 1995;152(5):687-97.
13. Staats C. State of the science: Implicit bias review 2014. Kirwan Institute for the Study of Race and Ethnicity.
14. Rudman LA. Social justice in our minds, homes, and society: The nature, causes and consequences of implicit bias. Social Justice Research, 17(2):129-142.
15. Implicit Social Cognition: Attitudes, Self-Esteem and Stereotypes (1995)
16. Feagin J, Benenefield Z. Systemic racism in U.S. health care. Social Science & Medicine. 103(2014):7-14.
17. van Ryn M, et al. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review. 8:1(2011):199-218.
18. National Patient Safety Foundation. Ask Me 3 ® : Good questions for your good health Web page. 2016.
Dovidio JF, et al. Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology, 2002;82(1):62-8. Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;185(4157):1124-31. Blair IV. The malleability of automatic stereotypes and prejudice. Personality and Social Psychology Review, 6(3):242-261. Wilkerson I. No, you’re not imaging it. September 2013. Essence, 44:132-137.
Note: This is not an all-inclusive list.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical and Population Health Research, University of Massachusetts Medical School, Worcester, MA, United States of America
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources
Affiliation Division of Nephrology, Duke University, Durham, NC, United States of America
Affiliation Department of Family Medicine, University of Washington Medical School, Seattle, WA, United States of America
Roles Conceptualization, Project administration, Supervision, Writing – review & editing
Affiliation Office of Student Affairs, University of Massachusetts Medical School, Worcester, MA, United States of America
Roles Conceptualization, Methodology, Writing – review & editing
Affiliation Department of Psychiatry, University of Massachusetts Medical School, Worcester, MA, United States of America
Roles Supervision, Visualization, Writing – review & editing
Affiliation Department of Biomedical Informatics and Medical Education, University of Washington, School of Medicine, Seattle, WA, United States of America
Roles Conceptualization, Methodology, Supervision, Visualization, Writing – original draft
Affiliation Department of Population and Quantitative Health Sciences University of Massachusetts Medical School, Worcester, MA, United States of America
Roles Conceptualization, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Family Medicine and Community Health, University of Massachusetts Medical School, Worcester, MA, United States of America
- Christine Motzkus,
- Racquel J. Wells,
- Xingyue Wang,
- Sonia Chimienti,
- Deborah Plummer,
- Janice Sabin,
- Jeroan Allison,
- Suzanne Cashman

- Published: November 15, 2019
- https://doi.org/10.1371/journal.pone.0225058
- Reader Comments
Implicit bias affects health professionals’ clinical decision-making; nevertheless, published reports of medical education curricula exploring this concept have been limited. This research documents a recent approach to teaching implicit bias.
Medical students matriculating during 2014 and 2015 participated in a determinants of health course including instruction about implicit bias. Each submitted a reflective essay discussing implicit bias, the experience of taking the Implicit Association Test (IAT), and other course content. Using grounded theory methodology, student essays that discussed reactions to the IAT were analyzed for content themes based on specific statements mapping to each theme. Twenty-five percent of essays underwent a second review to calculate agreement between raters regarding identification of statements mapping to themes.
Of 250 essays, three-quarters discussed students’ results on the IAT. Theme comments related to: a) experience taking the IAT, b) bias in medicine, and c) prescriptive comments. Most of the comments (84%) related to students’ acknowledging the importance of recognizing implicit bias. More than one-half (60%) noted that bias affects clinical decision-making, and one-fifth (19%) stated that they believe it is the physician’s responsibility to advocate for dismantling bias.
Conclusions
Through taking the IAT and developing an understanding of implicit bias, medical students can gain insight into the effect it may have on clinical decision-making. Having pre-clinical medical students explore implicit bias through the IAT can lay a foundation for discussing this very human tendency.
Citation: Motzkus C, Wells RJ, Wang X, Chimienti S, Plummer D, Sabin J, et al. (2019) Pre-clinical medical student reflections on implicit bias: Implications for learning and teaching. PLoS ONE 14(11): e0225058. https://doi.org/10.1371/journal.pone.0225058
Editor: Andrew Carl Miller, East Carolina University Brody School of Medicine, UNITED STATES
Received: July 31, 2019; Accepted: October 28, 2019; Published: November 15, 2019
Copyright: © 2019 Motzkus et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Implicit bias, also known as hidden or unconscious bias, refers to the attitudes or stereotypes that affect our understanding, actions, and decisions in a non-conscious manner of which we are typically unaware [ 1 – 4 ]. Implicit biases are automatic, lower level beliefs that can be difficult to recognize, acknowledge and manage [ 1 , 5 ]. Implicit bias is distinct from explicit biases which are our attitudes and beliefs which we consciously endorse and can report as our beliefs. In the health professions, implicit bias has been documented among medical students [ 6 ] as well as among resident and attending physicians, who routinely assume the role of medical education instructors and who serve as role models to students [ 7 , 8 ]. Recognition of implicit bias has been shown to produce dissonance for health professionals as they consider their conscious beliefs versus their non-conscious selves [ 9 ]. Becoming aware of one’s own implicit bias results may result in a disconnect between the clinician’s idealized desire to treat all patients equitably and actual clinical decisions that are influenced by unconscious attitudes towards a patient based on his/her subgroup identity. It has been well documented that in clinical settings, negative implicit bias leads to poorer quality of care, poor or inadequate clinician-patient communication, and ultimately to healthcare disparities and inequities [ 8 , 10 – 14 ].
For more than a decade, medical education leaders have urged medical education to embrace cultural competence instruction [ 4 ], including training about how to manage unconscious bias, thus introducing learners to this foundational issue that affects quality of care. This instruction sets an expectation that students consider their biases when caring for patients [ 13 ]. For students to learn how to address implicit bias, however, they must first be open to confronting the fact that they likely have biases functioning at an unconscious level and to recognizing the potential effect these biases may have [ 4 ]. This can be particularly challenging when evidence suggests one’s own implicit bias conflicts with one’s personal or professional identity [ 9 , 14 ].
One approach used to self-identify unconscious biases is the Implicit Association Test (IAT) [ 15 ]. Increasingly, health professions schools are using the IAT to introduce the issue of bias and stereotype [ 16 ]. Results from a recent study using the IAT with a small group of physicians and nurses emphasized the necessity of understanding how individuals process and integrate their IAT results [ 17 ]. Studies have suggested that improving our understanding about how individuals react to their IAT results should increase our ability to use the IAT to manage bias by promoting self-awareness as well as contribute to personal and professional development [ 17 – 19 ].
While the IAT is being used more frequently in health professions education, the additional step of asking medical students to reflect in writing on the outcome of their self-assessment is less common, and reports on these reflections in the literature are rarer still. Given the power of reflective practice [ 20 ] and its use in medical education to raise awareness of bias [ 7 , 17 , 20 – 22 ], we hypothesized that we could gain insight into understanding students’ readiness to accept their implicit biases and to address unconscious bias from their written responses reflecting on their assessment results. Using grounded theory methodology, we examined the content of two cohorts of one school’s first year medical students’ required written reflections on their IAT results. We explored whether three-hours of focused content and discussion regarding bias and stereotypes could produce student reflections demonstrating insight into these issues. We were particularly curious about whether students would include comments indicating that 1) they believe bias has the potential to influence decisions within their newly chosen profession and 2) where responsibility lay for reducing bias’s effects.
Determinants of health course
All first and second year medical students at University of Massachusetts Medical School (UMMS) are enrolled in the course: Determinants of Health (DOH). This required course provides students with a systematic framework for understanding the disparities and inequities found in humans’ health status as well as the impact of context/environment on health. For first-year students, DOH consists of five hours of lecture/discussion in the fall semester and three in the spring, with an Epidemiology/Biostatistics module taking place in the winter.
Bias/stereotyping is a determinant of health that is featured as part of DOH’s three-hour spring session. Complementing their learning regarding how our brains receive and catalogue information that results in stereotyping, students are asked to complete the Implicit Association Test (IAT) [ 15 ] on any topic of their choosing (e.g. race, religion, weight). We used the IAT with feedback as a tool for self-reflection. Research in healthcare shows that the IAT may engender critique of its validity and defensiveness, yet it is considered to be either a positive or neutral experience and provokes test takers to acknowledge the need to address their biases [ 23 ]. The IAT is a computerized test that measures the strength of association between target concepts such as race (Black versus White), ethnicity (Hispanic/Latino versus White), or body type (X versus Y) with either pleasant or unpleasant words. Test takers are asked to rapidly sort and pair images and words as they appear on a computer screen using a right and left key. While the main idea of the IAT is that response time is faster when items are closely associated and slower when they are not, it should not be used as a diagnostic of prejudicial or discriminatory behavior.
Reflective essays
One requirement for completing the DOH course’s spring segment is that each student compose and submit a two-page reflective essay in response to the prompt “ Please select a particular reading assigned for this class , your experience taking the Implicit Association Test , or a specific discussion that occurred in class and comment on how this material leads to new insight about the potential effect of your personal biases or stereotyping on future clinical decisions .” To meet this study’s objectives, we de-identified each essay that students in the 2014–2015 and 2015–2016 academic years submitted, selected those commenting on the IAT (n = 188; 74%), and used qualitative analytic techniques for analysis.
Qualitative analysis
Grounded theory methodology was used to anchor the qualitative analysis of students’ essays. With its inductive approach, grounded theory is a systematic research methodology that uses the analysis of data to construct theory. Studies using grounded theory begin with the collection of qualitative data. In reading and re-reading the data, analysts identify ideas or concepts that appear repeatedly. Text is tagged with codes which are noted in a code book and then grouped into emerging themes [ 24 ].
One author (RW) developed the codebook for the first cohort of essays through an iterative process of essay review until saturation of content was reached. The codebook was organized such that specific statements (typically sentences or clauses) were mapped to one of 25 themes identified. A student could make multiple statements in an essay that mapped to the same theme; however, themes were not double counted for this repetition. Themes were loosely grouped under three broader “thematic categories” including: Experience with the Implicit, Bias in Medicine, and Prescriptive Comments. The codebook was reviewed by a second author (CM) with discussion to ensure the scope of the codebook was adequate. The second cohort’s essays were reviewed using the initial codebook by one author (XW) undergoing the same process of mapping statements to themes.
Inter-rater reliability
Twenty-five percent from each of the two years of essays reflecting on the IAT experience were randomly selected using a random number generator to undergo coding by a second rater (CM). These essays were specifically reviewed to identify statements that mapped to a theme that may have been missed by initial review or statements that the second rater felt had been misidentified as corresponding to a theme. Using Cohen’s Kappa statistic in SAS 9.3 (Cary,NC), inter-rater reliability was calculated for rater agreement.
Ethics statement
As the University of Massachusetts Institutional Review Board deemed this research not human subjects research, the informed consent requirement was waived.
A total of 250 student essays were de-identified by DOH faculty leaders. Slightly more than one-half (135) of these two medical student cohorts were women; their average age was 24, and 35 were first generation to attend college. Twenty-six were from groups underrepresented in medicine. With the exception of 12 of the 18 MD/PhD students in this cohort, all were residents of Massachusetts.
Approximately three-quarters (74%) of the essays mapped directly to discussion of the IAT and the student’s IAT results. For the final code book, 25 themes were identified. (See Table 1 ) Themes related to the experience of taking the IAT included recognition of bias’s inevitability, as bias is a product of society, cultural backgrounds, and media. Themes related to the potential influence of implicit bias in medicine included comments on the existence of racial bias in medicine and the harm that can be caused by the inability to acknowledge bias. Finally, several themes supported the prescriptive ideas that in order to provide high quality patient care, bias must be recognized and that it is a physician’s responsibility to dismantle the bias found in the healthcare system through avenues such as advocacy and legislation. Inter-rater reliability was high (kappa = 0.87, p<0.0001).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0225058.t001
We identified 10 specific themes that reflected broadly on the general concept of students’ experience with the IAT . Promisingly, slightly more than one-half of students (56%) felt that the IAT promoted self-reflection. More than one-quarter (28%) wrote that their IAT results surprised them. The students who professed surprise generally noted one of two sentiments. Either surprise was the reaction to discovering biases that seemed to run counter to their own self-identification, or it was surprising that they harbored any form of prejudice.
“The most shocking part of taking the test, however, was how official it made my prejudices.”
More than one-half of students (55%) acknowledged the inevitability of personal biases and that these biases—whether acknowledged or unacknowledged—affect behavior. Most (56%) also acknowledged that bias is a product of society/cultural background/media/upbringing; these students discussed the importance of recognizing the impact of their own background and experiences.
“It's OK to admit that we are not perfect. It's OK to recognize the fear and vulnerability that comes with realizing our personal prejudices. Because we're all raised differently under different circumstances, and because biases are natural and undeniable.”
Overall, comments regarding bias and the IAT generally reflected acceptance of biases and the importance of self-awareness.
“Every person has certain impressions and biases that they are not proud of, but the lesson to take away from tests like the Implicit Association Test is to acknowledge these associations and separate them from their actions.”
Students frequently commented on areas of bias in clinical medicine and medical education that mapped to themes that related to the influence of bias on health care . While slightly more than one-half (52%) acknowledged that racial bias/racism exists in medicine, three-fifths (60%) stated that they felt bias affected patient care decision-making.
“We all have some degree of inherent bias whether we are aware of it or not and those subtle subconscious decisions we make on a daily basis can have a large impact on others.”
Almost one-fifth (18%) identified historic events as having affected the medical field’s overall climate related to bias and stereotype. A common thread throughout the essays was surprise at the pervasiveness of racial bias within systems students had previously believed to be objective. Some expressed dismay that historical events they considered quite distant are still frequently recalled by patients and that as a result, likely perpetuate inequities.
“Historical events institutionalized racism into American society, and remnants of prejudiced attitudes and differential treatment translate into gaps in health care outcomes across racial groups.” “Prior to this class, I had never thought about how racial biases could be manifested within such a seemingly objective and technical system such as the organ procurement organization.”
A small proportion (8%) of students also highlighted the difficulty of balancing clinical judgement and a patient’s potential risk factors while not stereotyping a patient based on those same risk factors.
“[It] made me realize that there needs to be a balance between not letting race and ethnicity bias your opinions and also taking race and ethnicity into account to provide the best care for your patients.”
A few students (6%) noted feeling that passive reinforcement of implicit bias in medical education was commonplace. The common example given was that race was mentioned only when the patient was not White, implying that unless otherwise stated that the default and thus the norm was White.
Themes related to how the medical profession might address the issue of implicit bias began with more than four-fifths (84%) of the students who reflected on the IAT expressing the feeling that bias needs to be acknowledged and three-quarters (75%) of them noted that this can be done through making conscious efforts to recognize it. Nearly one-fifth (19%) proceeded to write that they believe it is the physician’s responsibility to advocate for dismantling institutional bias.
“I believe that as physicians we have a responsibility towards the public good and the health of the population and I think that part of this purview is working to undo the injustices that have become established in our society.”
Almost one-quarter (22%) wrote that they felt a call to act on the problems causing disparities and noted the importance of contributing to the work needed both in healthcare and society at large to combat institutional bias.
“The question evolves from how can I be less racist, to how can I help our institutions be less racist?”
A very small proportion (4%) commented that while they thought discussion of implicit and institutional bias was valuable, there needed to be more concrete evidence and quantitative research to truly move forward with combating racism in medicine. One student concluded that more work remains to be done to engage students and clinicians.
“I think that education and discussion around issues like this is an incredibly important thing in our training, but it can also be a difficult thing to get earnest participation in.”
As another student, apparently frustrated by his/her own powerlessness to engage some of his/her reluctant colleagues in this topic put it:
“We dutifully learn about rare cancers which we will likely never see and genetic disorders only described in a handful of patients, which we will certainly never see and yet race, which we will see every day for the rest of our careers is a topic that only manages to draw a small group of students. I can't help but feel that the apathy towards the subject of race … is a part of what has wrought the shocking disparities we are faced with today in healthcare.”
This study achieved its objective of having students include reflections on 1) implicit bias having the potential to influence decisions within their newly chosen profession and 2) where they thought responsibility lay for reducing implicit bias’s effects. This objective was achieved through analyzing the content of two cohorts of students’ required reflective essays resulting from three hours of bias and stereotyping instruction and discussion.
The majority (74%) chose to reflect on the IAT and bias. In addition, they seem to have reflected frankly on their perceptions of implicit biases and the role they can play in clinical decision-making. The students may have been open to this as, in accordance with at least one study’s recommendation, this reflective essay was a personal exercise and did not include a foundational anchor related to normative expectations of physicians [ 19 ]. The fact that the exercise was part of a required course and not an elective may have contributed to students approaching this work as normative in medical education. As a required exercise with several options for focusing one’s reflection, this work demonstrates that early in their education, medical students are open to accepting and considering the implications of bias in medicine and within themselves.
Overall, students discussed their experience with the IAT and how that experience created an opportunity for self-reflection and newfound appreciation of their own internalized biases. They also expressed a desire for further training on this subject as well as a need for action and advocacy from themselves as clinicians but also from their colleagues to achieve changes to institutionalized biases and improve future care for patients. There is no empirical evidence in any sector that shows use of the IAT reduces personal bias long term; self-reflection, however, may help individuals become aware of their own biases and take steps to reduce the impact of bias on behavior. Steps to mitigate the impact of bias on behavior may include reducing discretion in decision-making, collecting data to identify inequities, and using checklists. [ 25 ]
Physicians have always served as advocates for their patients; indeed, this advocacy role has been institutionalized as a competency to achieve at the University of Massachusetts Medical School [ 26 ] and has been mandated by the Royal College of Physicians and Surgeons of Canada [ 27 ]. The role of the physician in advocating for broader institutional and cultural change, however, has been the subject of heated debate [ 28 , 29 ]. Students in this study cohort were motivated to comment on the role of physician advocacy related to countering institutional and personal bias, which creates a sense that momentum towards physicians playing a key role in institutional change exists and could be building. Whether and how students may assume this type of advocacy role is an empirical question that should be studied. Given society’s heightened awareness of the role negative implicit bias plays in a wide range of settings, there is an urgency to determining answers to these questions.
Some students identified the pre-clinical years as an ideal time for addressing issues of implicit bias; nevertheless, few explicitly outlined how they would like to see medical education address implicit and institutionalized bias. While identifying additional curricular time is often seen as an insurmountable barrier, the issue of implicit bias could be threaded throughout existing curricula. One method to integrate implicit bias into existing curricula would be through modifying elements of the patient vignettes frequently used for educational purposes in order to remedy what may be passive reinforcement of implicit biases, particularly to introduce counter-stereotypical information that does not reinforce racial/ethnic stereotypes and inclusion of non-White patient race and ethnicity when it does not affect the patient’s diagnosis or treatment plan [ 30 , 31 ]. An additional approach could be to review all curricula for bias and stereotyping in materials and assessment of what had been left omitted [ 32 ]. This could be accomplished through faculty self-reviewing materials or through a school’s curriculum committee, inclusive of student representatives, conducting the review.
Our brief curriculum and assignment stimulated reflection. Preclinical medical students, have not yet been fully exposed to the institutional culture of stereotyping of patients on the wards and in the outpatient clinics that may reinforce bias and, therefore, may lack experiential insight into the practice of medicine and the reality of a typical clinical day’s pressures [ 33 ]. Other studies of student perceptions and attitudes have identified preclinical years as an ideal time to intervene, with the acknowledgement that there is a widely documented loss of empathy as students enter their clinical experiences and become assimilated into hospital culture.[ 34 – 36 ] Results from a recent comprehensive study [ 37 ] of 3547 medical students at 49 medical schools affirms the importance of early, varied, and continued educational interventions regarding implicit bias. In this study, researchers concluded that medical student experiences within any of the three domains they termed formal curricula, informal curricula, and interracial contact had small but statistically significant associations with changes in reducing implicit racial bias among non- African American students between first and fourth years of medical school. The research found that for students who witnessed attending and resident physicians make negative comments about African American patients, implicit race bias actually increased.
In the past decade, the social determinants of health (SDOH)—the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life [ 38 ] have moved from holding a position on the sidelines of health to one closer to center stage. Health care systems and medical educators have accepted the need to address and to influence elements of the SDOH. But as social determinants of health such as housing, education, transportation, and employment are often predicated on the more distal determinant of bias, discrimination, stereotyping, and marginalization, this move upstream must include examining the potential influence of implicit/unconscious bias. Thus, cultural competency curricula have begun to include examining societal and personal bias. Our results indicate that assigning students the IAT with reflection on their experience is a worthwhile curricular element.
This study provides important insight into the attitudes and self-reflections of students’ implicit biases; nevertheless, considerations and limitations are present. The University of Massachusetts Medical School’s Institutional Review Board deemed this body of work “not research.” In educational institutions, it is generally accepted that using either students themselves or their work from a required course to conduct research could be viewed as coercive, therefore sensitivity to potential ethical issues is heightened. Notable issues in the case of the work presented in this article are that 1) the students’ assignment did not require them to write about the IAT (it gave them the option of reflecting on any of the materials that had been part of the class; nevertheless, 74% elected to focus on the IAT in their essays) and 2) the instructors intended the assignment to guide them as they strove to improve one element of the course. Nevertheless, if standards of practice surrounding using either students or their work for research change, it will be critical to ensure ethical standards guide this type of work.
The IAT is a validated tool, yet still faces criticism for its approach to identifying and measuring associations related to bias [ 39 , 40 ]. Authors of the IAT are careful to note that the tool indicates relative association strengths between two concepts but does not reflect actual biases or acts of discrimination related to identified preferences [ 4 ]. Moreover, while theme coding accuracy and interrater reliability were high, it remains possible that coders interpreted student responses differently. Students were not explicitly required to reflect on their experience with the IAT or implicit bias; some may have withheld true feelings about the role of implicit bias in medical education due to fear of repercussion to their grades. Additionally, given that these are preclinical students, we cannot measure how these reflections may or may not change future clinical outcomes. Finally, active participation in the curriculum and with the IAT may reflect self-selection bias of students who already exhibit interest in the subject. Despite these limitations, our study found that pre-clinical medical students chose to explore implicit bias through self-reflection. In addition, students expressed motivation to engage in advocacy around bias in medicine.
Our study demonstrates that medical education curricula can introduce the issue of bias to preclinical medical students who are then able to grapple with and reflect upon issues of implicit bias. Given the extent to which implicit bias permeates our psyches, having medical students early in their education take and reflect on implicit bias through the IAT offers opportunity to confront and address bias. This is likely one necessary—though not sufficient—step among many towards striving for equity in health care. Additional studies of medical students’ perceptions of implicit bias and determinations of how these reflections impact patient l outcomes as students’ progress on their journey to becoming physicians are needed.
Acknowledgments
A sincere appreciation to the medical students of the entering classes of 2014 and 2015 for their honest and open opinions surrounding these critical components of the medical student professional identity development. The authors would also like to acknowledge Dr. Jen Tjia for sharing her wealth of knowledge on implicit bias and medical education.
- 1. Banaji MR, Greenwald AG. 2016. Blindspot : Hidden biases of good people . New York (NY): Bantam.
- View Article
- Google Scholar
- PubMed/NCBI
- 26. University of Massachusetts Medical School. UMMS competencies for medical education. [cited 2018 Nov 20]. Available from: www.umassmed.edu/oume/oume/umms-competencies-for-medical-education1 .
- 38. Social determinants of health. [cited 2018 Oct 15]. Available from: https://www.who.int/social_determinants/en/ .
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Research bias
- What Is Implicit Bias? | Definition & Examples
What Is Implicit Bias? | Definition & Examples
Published on January 27, 2023 by Kassiani Nikolopoulou . Revised on December 18, 2023.
Implicit bias is a collection of associations and reactions that emerge automatically upon encountering an individual or group. We associate negative or positive stereotypes with certain groups and let these influence how we treat them rather than remaining neutral.
This can lead to discriminatory behaviour in a wide range of contexts such as healthcare, the workplace, and education.
Table of contents
What is implicit bias, what causes implicit bias, implicit vs. explicit bias, implicit bias examples, what is the harvard implicit bias association test (iat), how to reduce implicit bias, other types of research bias, frequently asked questions about implicit bias.
Implicit bias is an unconscious preference for (or aversion to) a particular person or group. Although these feelings can be either positive or negative, they cause us to be unfair towards others. Affinity bias or the tendency to favor people who are similar to us, is an example of this unfair behaviour. However, any aspect of an individual’s identity, such as age, gender, or socioeconomic background, can be the target of implicit bias.
Under implicit bias, we are unaware that our biases (rather than objective facts) affect our decisions and judgments. For example, when most people hear the word “kindergarten teacher,” they are more likely to picture a female. This can happen without intention or awareness and may even contradict openly held beliefs. Because implicit bias is unconscious, it is difficult to acknowledge and control.
Implicit bias occurs due to unconscious mental processes. There are several factors at play in the development of implicit biases:
- Our brains create categories . We have the natural tendency to assign everything we see into a category. Even though this happens unconsciously, after categorising things or people, we also assign a positive or negative association to them. Categories allow our brains to know what to do or how to behave. The downside of this is that classifications often cause us to overgeneralise.
- We rely on mental shortcuts. Most of the time, we rely on “automatic” information processing that involves little conscious thought. This allows us to exert little mental effort in our everyday lives and make swift judgments.
- Social and cultural influences. Our upbringing, social environment, and direct and indirect experiences with members of various social groups imprint on us. These shape our perception at a deeper level, even if we are not conscious of it.
Both implicit and explicit bias involve judging others based on our assumptions rather than the situation or the facts at hand. However, they are actually quite different.
- Implicit bias occurs when we have an inclination for or against a person or group that emerges automatically. In other words, our evaluation, positive or negative, is unintentional and beyond our conscious awareness.
- Conversely, explicit bias refers to positive or negative attitudes that we are fully aware of. We openly express them and share them with others, because these attitudes are part of our worldview.
Despite their differences, implicit bias can be just as problematic as explicit bias because both may lead to discriminatory behaviour.
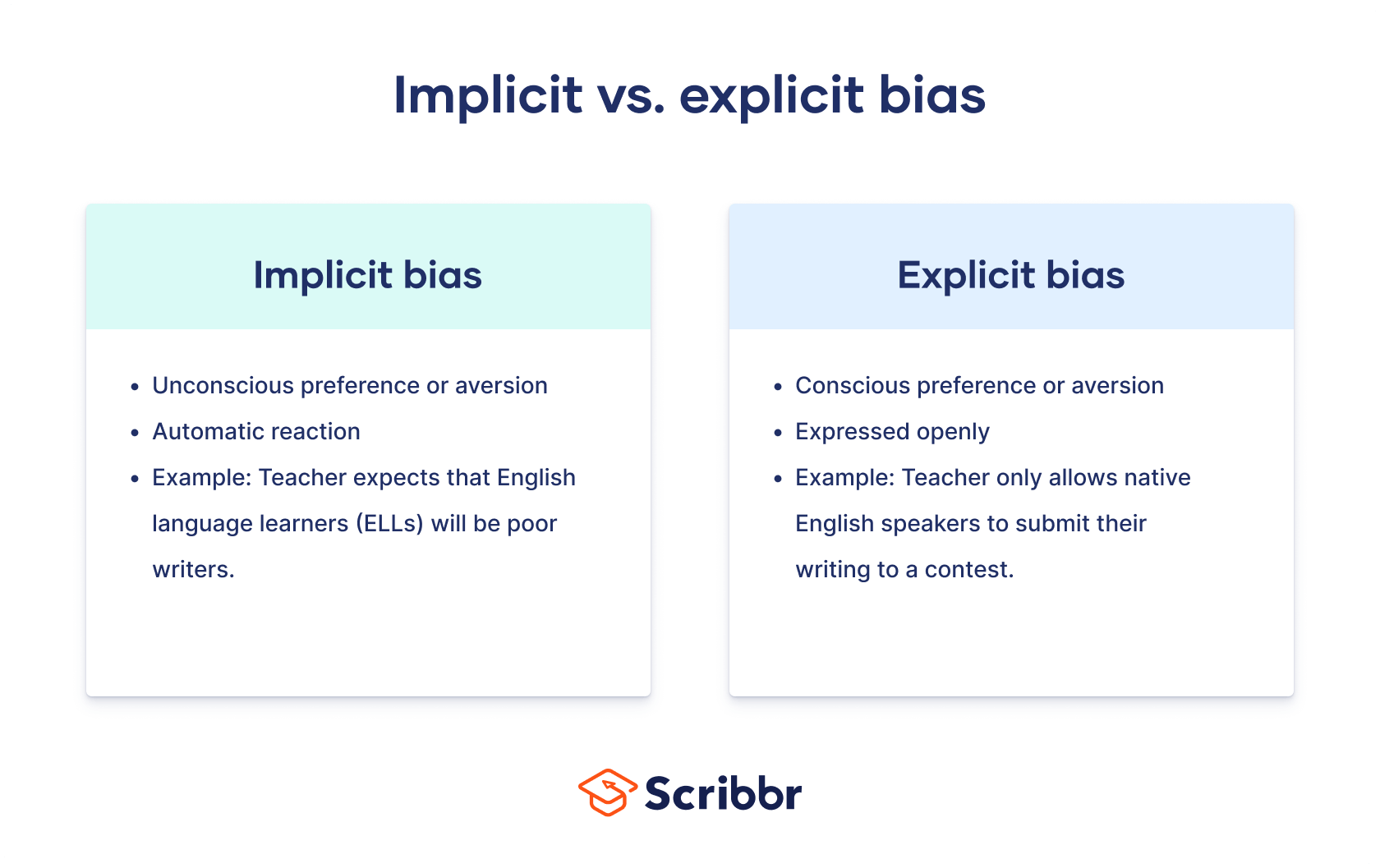
Implicit bias can lead to discriminatory behaviour when it comes to hiring a diverse workforce.
In a field experiment measuring racial discrimination in the labor market, researchers responded to job ads in Boston and Chicago using fictitious resumes. To manipulate perception of race, each resume was assigned either an African-American-sounding name or a white-sounding name. The results showed significant discrimination against African-American names: applicants with white-sounding names received 50 percent more callbacks for interviews.
The amount of discrimination was uniform across occupations and industries. Additionally, federal contractors and employers who mentioned “Equal Opportunity Employer” in their ad discriminated as much as other employers.
The researchers concluded that there was little evidence that employers were trying to infer something other than race, such as social class, from the name.
The Harvard Implicit Bias Association Test (IAT) is a computer-based assessment measuring the strength of associations between concepts or stereotypes to reveal an individual’s implicit or subconscious biases.
The idea behind IAT is that, while we can measure explicit bias by asking respondents directly about their views regarding something like gender roles, the same does not apply for implicit biases. When we want to measure hidden or implicit attitudes, we need to do so indirectly. Otherwise, respondents will not answer truthfully due to social desirability or a lack of awareness of their own biases.
There are different versions of the IAT, but it typically consists of five rounds. In each round, respondents need to quickly sort words (e.g., “parents”) into categories that are on the left- and right-hand side of the screen (e.g., “career” and “family”). The key assumption underlying any IAT is that the stronger the association a respondent has between two concepts, the faster they are to make these associations.
Understanding implicit bias is critical because both positive and negative unconscious beliefs can lead to structural and systemic inequalities. However, because it operates outside our awareness, if we want to reduce it, we first need to become conscious of it. The following strategies can be helpful:
- Taking the IAT can help you realise that everyone, including you, has implicit biases. Recognising them for what they are increases the likelihood that next time you won’t let these hidden biases affect your behaviour.
- Positive intergroup contact. Unconscious bias towards a particular group can be reduced through interaction with members of that group. For example, you can make it a point to engage in activities that include individuals from diverse backgrounds.
- Counter-stereotyping. Exposure to information that defies stereotypes that persist about groups or individuals, such as images of female scientists, can counter gender stereotypes.
- Implicit bias training. Although raising awareness is important, it’s not enough. The most successful training programs are ones that allow individuals to discover their biases in a non-confrontational manner and also give them the tools to reduce and manage their biases.
Cognitive bias
- Confirmation bias
- Baader–Meinhof phenomenon
- Availability heuristic
- Halo effect
- Framing effect
- Optimism bias
- Negativity bias
- Affect heuristic
- Representativeness heuristic
- Anchoring heuristic
- Primacy bias
Selection bias
- Sampling bias
- Ascertainment bias
- Attrition bias
- Self-selection bias
- Survivorship bias
- Nonresponse bias
- Undercoverage bias
- Hawthorne effect
- Observer bias
- Omitted variable bias
- Publication bias
- Pygmalion effect
- Recall bias
- Social desirability bias
- Placebo effect
- Actor-observer bias
- Ceiling effect
- Ecological fallacy
- Affinity bias
Bias can be either positive or negative. However, all forms of bias (whether favorable or unfavorable) prevent us from judging others fairly.
For example, because of explicit bias , a teacher might openly claim that students from a certain ethnic background are exceptionally good in math. Even though this sounds positive, it means that other students are automatically treated as second-rate. For this reason, bias is linked to unfairness and thus has a negative connotation.
There are two main types of bias:
Implicit bias is the positive or negative attitudes, feelings, and stereotypes we maintain about members of a certain group without us being consciously aware of them.
Explicit bias is the positive or negative attitudes, feelings, and stereotypes we maintain about others while being consciously aware of them.
Bias is a systematic error in the design, administration, or analysis of a study. Because of bias, study results deviate from their true value and researchers draw erroneous conclusions.
There are several types of bias and different research designs or fields are susceptible to different types of research bias. For example, in health research, bias arises from two main sources:
- The approach adopted for selecting study participants
- The approach adopted for collecting or measuring data
These are, respectively, selection bias and information bias .
The opposite of implicit bias is explicit bias , or conscious bias. This refers to preferences, opinions, and attitudes of which people are generally consciously aware. In other words, explicit bias is expressed openly and deliberately.
Sources in this article
We strongly encourage students to use sources in their work. You can cite our article (APA Style) or take a deep dive into the articles below.
Nikolopoulou, K. (2023, December 18). What Is Implicit Bias? | Definition & Examples. Scribbr. Retrieved September 3, 2024, from https://www.scribbr.com/research-bias/implicit-bias/
Bertrand, M., & Mullainathan, S. (2004). Are Emily and Greg More Employable Than Lakisha and Jamal? A Field Experiment on Labor Market Discrimination. American Economic Review , 94 (4), 991–1013. https://doi.org/10.1257/0002828042002561
Daumeyer, N. M., Onyeador, I. N., Brown, X., & Richeson, J. A. (2019). Consequences of attributing discrimination to implicit vs. explicit bias. Journal of Experimental Social Psychology , 84 , 103812. https://doi.org/10.1016/j.jesp.2019.04.010
Is this article helpful?

Kassiani Nikolopoulou
Other students also liked, what is affinity bias | definition & examples, what is explicit bias | definition & examples, what is the halo effect | definition & examples.
Academic Support for Nursing Students
No notifications.
Disclaimer: This essay has been written by a student and not our expert nursing writers. View professional sample essays here.
View full disclaimer
Any opinions, findings, conclusions, or recommendations expressed in this essay are those of the author and do not necessarily reflect the views of NursingAnswers.net. This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
Implicit Bias in Women’s Healthcare
Info: 1773 words (7 pages) Nursing Essay Published: 11th Feb 2020
Reference this
If you need assistance with writing your nursing essay, our professional nursing essay writing service is here to help!
Our nursing and healthcare experts are ready and waiting to assist with any writing project you may have, from simple essay plans, through to full nursing dissertations.
- TodayShow. “Do Doctors Treat Women Differently?” TODAY.com , TODAY, www.today.com/health/gender-bias-health-care-may-be-harming-women-s-health-t133583 .
- Bedford, Megan. “Conversations in Cultural Competency.” Unconscious Bias in Healthcare , www.qualityinteractions.com/blog/unconscious-bias-in-healthcare .
- Schopen, Fay. “The Healthcare Gender Bias: Do Men Get Better Medical Treatment?” The Guardian , Guardian News and Media, 20 Nov. 2017, www.theguardian.com/lifeandstyle/2017/nov/20/healthcare-gender-bias-women-pain .
- Alspach, JoAnn Grif. “Is There Gender Bias in Critical Care?” Critical Care Nurse , 1 Dec. 2012, ccn.aacnjournals.org/content/32/6/8.full.
- Cedars-Sinai , www.cedars-sinai.org/newsroom/today-show-gender-bias-in-healthcare/ .
- “Understanding Implicit Bias in Health Care.” NATA , 26 Mar. 2018, www.nata.org/blog/jordan-grantham/understanding-implicit-bias-health-care .
- Mahone, Regina. “New Paper Examines How Gender Bias in Health Care Can Be Deadly.” Rewire.News , Rewire.News, 4 Oct. 2018, rewire.news/article/2018/10/04/new-paper-examines-how-gender-bias-in-health-care-can-be-deadly/.
- “Implicit Bias Explained.” Perception Institute , perception.org/research/implicit-bias/.
- “The Healthcare Gender Bias – Do Men Get Better Medical Treatment than Women?” Talented Ladies Club , 26 Sept. 2018, www.talentedladiesclub.com/articles/the-healthcare-gender-bias-do-men-get-better-medical-treatment-than-women/ .
- “Gender Bias in Medicine.” Journal of Research in Crime and Delinquency , journals.sagepub.com/doi/full/10.2217/17455057.4.3.237.
- “Understanding Implicit Bias.” Kirwan Institute for the Study of Race and Ethnicity , kirwaninstitute.osu.edu/research/understanding-implicit-bias/.
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services

- Nursing Essay Writing Service

- Nursing Dissertation Service

- Reflective Writing Service
DMCA / Removal Request
If you are the original writer of this essay and no longer wish to have your work published on the NursingAnswers.net website then please:
Our academic writing and marking services can help you!
- Marking Service
- Samples of our Work
- Full Service Portfolio
Related Lectures
Study for free with our range of nursing lectures!
- Drug Classification
- Emergency Care
- Health Observation
- Palliative Care
- Professional Values

Write for Us
Do you have a 2:1 degree or higher in nursing or healthcare?
Study Resources
Free resources to assist you with your nursing studies!
- APA Citation Tool
- Example Nursing Essays
- Example Nursing Assignments
- Example Nursing Case Studies
- Reflective Nursing Essays
- Nursing Literature Reviews
- Free Resources
- Reflective Model Guides
- Nursing and Healthcare Pay 2021
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- All Summits
- STATUS List
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry

How race became ubiquitous in medical decision-making tools
By Usha Lee McFarling and Katie Palmer
Sept. 4, 2024
It was created with the best intentions: a government policy asking researchers to collect racial data to help address health disparities. But it may have had an unintended opposite effect, paving the way for the problematic use of race in an array of medical decision-making tools.
Starting in the 1990s, the National Institutes of Health began requiring the collection and reporting of racial data in its funded research. It was a major pivot point, revealing in stark, undeniable numbers racial divides in health outcomes. But to a new generation of researchers, that quantification enabled the development of algorithms that misused race as a health risk factor.
advertisement
Poorly understood correlations between race and outcomes were embraced as a way to make disease-risk calculations more precise, though the race data were actually quite imprecise.
It was a time when many in medicine, new to handling race data, used it in a sloppier way than they would today. Many categorized research subjects as simply being Black, Hispanic, or Asian without thinking about the complex ancestry within those groups.
Related: Doctors use problematic race-based algorithms to guide care every day. Why are they so hard to change?
Many also still considered race a biological explanation for differences, and not, as scientists agree today, a socially created category — with a weak relationship to genetic differences — that may be more connected to characteristics like income or neighborhood. In some instances, researchers devising new algorithms uncritically accepted faulty ideas about racial differences that date back to America’s slavery era.
“All we have is old research that was accepted under a lower standard of rigor,” said Lou Hart, medical director of health equity at Yale New Haven Health System. The federal government said, “‘You have to diversify your clinical trials. You have to report out this type of information and publish literature.’ And so people did.”
Eliseo Pérez-Stable, director of the National Institute on Minority Health and Health Disparities, said the collection of racial data “categorically” did not lead to the creation of race-based algorithms. “The reason we collect race and ethnicity, and we should collect other things like socioeconomic status that we don’t, is because they influence health outcomes in ways that we don’t fully understand,” he said.
Along the path to better understanding, racial data were collected inconsistently: Sometimes participants were asked, sometimes study leaders just guessed. And researchers often divided the world simply into Black and white, ignoring those who were other races or mixed race.
“The suggestion that Black people and only Black people are different than every other human on the planet is just ludicrous,” said Vanessa Grubbs, a nephrologist in Oakland, Calif. and a leading voice calling for the removal of race from algorithms used to assess kidney function.
Kidney function is estimated using a blood test that measures levels of creatinine, a waste product created when muscle breaks down that is filtered out by healthy kidneys. Studies found that, on average, Black people have higher levels of creatinine, leading researchers to introduce a race adjustment for Black people into the kidney algorithm.
In their original paper published in 1999, creators of the algorithm attributed high creatinine levels to Black people being more muscular — an assertion that was not widely questioned at the time but has more recently come under scrutiny for overgeneralization and racial stereotyping. The algorithm was updated with a more diverse subject pool, but the concept that Black muscle mass was a reason for difference persisted.
The idea that Black patients would have greater muscle mass was easy to believe, perhaps, because of the United States’ history of slavery. As recently as 2011, one urologist hypothesized that enslaved Africans who survived the passage to the Americas would have had greater lean muscle mass; others pointed out that those who were enslaved were “bred” for greater strength.
“When you ask where did these algorithms come from, not all roads, but many roads lead back to slavery-era race science,” said David Shumway Jones, a historian of science, physician, and professor at Harvard Medical School. “The notion that Black people have different skin, different bones, different bone density, it all goes back to these pre-Civil war claims.”
Until recently, even some high-profile scientific papers used race in ways that would not pass muster today. The studies cited in the kidney algorithm paper to suggest that higher creatinine levels in Black people were due to muscle mass were extremely thin; some were decades old.
None of the three cited studies — all small and using subjects from a single town, hospital, or in one case, staff at a single lab and their friends — directly measured muscle mass . One looked at body fat in children, another at potassium levels.
Health equity advocates don’t believe the equation creators were out to harm Black people. “No one was meeting in back rooms or alleys saying, ‘How can I hurt Black patients?’’’ said La’Tonzia Adams, a pathologist in Portland, Ore., working with the College of American Pathologists to ensure new race-free algorithms are being implemented. “This started with good intent.”
Instead, they say the mostly white people leading the field of nephrology and at its journals never questioned the careless thinking because notions that races differ biologically were so accepted. “These ubiquitous and pervasive race claims have been in medicine forever,” said Jones, who has examined how the New England Journal of Medicine has historically handled issues of race . “It’s very easy for editors not to notice them.”
Oversimplistic thinking about race has been repeated across medical specialties. For decades, hypertension in Black Americans was explained away because of the “salt-slavery hypothesis,” which posited that high blood pressure could be due to salt deficiencies in regions of Africa where enslaved people were stolen from, the trauma of the slave trade, or conditions of slavery. That idea was easily debunked by historians who showed that there wasn’t a salt deficiency at the time and that hypertension rates are not high among present-day West Africans.
There’s a similar issue with the race-adjusted STONE score algorithm developed to diagnose kidney stones. The presence of flank pain is considered as important as finding blood in urine — unless you’re Black . This algorithm stems from a single study conducted in 2014 at two hospitals in Connecticut finding that Black people were less likely to have kidney stones — data points now deeply questioned by those in the field, and being reevaluated by Hart and his colleagues .
Related: Why is eugenics still alive and well in scientific publishing?
In obstetrics, the unfounded slavery-era notion that the pelvises of Black women were narrow, “ degraded and animalized ,” remained a “ concerning echo ” in a birth risk calculator — causing some U.S. doctors to discourage vaginal deliveries after a C-section for Black women. In Canada, the mother’s race isn’t a factor. “Are pelvises different in Canada?” Jones asked.
In pulmonology, a sweeping generalization that Black people have lower normal lung function led physicians to long overlook chronic lung disease in Black patients. The idea, as chronicled by the late Lundy Braun, who was a professor of Africana Studies and pathology at Brown University in her history of the spirometer, traces to 1851.
Physician Samuel Cartwright built his own spirometer to measure lung function, which he quantified at 20% lower in Black people he enslaved. Cartwright argued that Black people needed to be forced to work or their weak lungs would suffer. “You can imagine what a powerful justification this is for enslaving human beings,” said Dorothy Roberts, a professor of law and sociology at the University of Pennsylvania.
For centuries, this racist concept echoed in clinicians’ estimates of lung function and adjustments of up to 15% to spirometer readings, which indicated the lung disease of Black people was less severe than the devices indicated. In March 2023, the American Thoracic Society urged that race and ethnicity should no longer be used to interpret spirometry results.
“Essentially structural racism is baked into the numbers because of what we set the norm at,” said Lauren Kearney, a pulmonology fellow who helped usher in race-free spirometry assessments at Boston Medical Center. “In the past, we were told in medical school that race does define biology.”
A number of new studies estimate the lung test adjustment has taken a toll. It has prevented or delayed disability and workers’ compensation payments for Black workers, and has led to missed cases of respiratory disease and severe lung impairment , more uncontrolled asthma , and the underestimation of COPD severity in Black patients.
Not all racial misconceptions have manifested in algorithms; some simply bled into medical practices that put Black patients at higher risk. For decades, radiologists, dentists, and manufacturers of X-ray equipment internalized the idea that Black people have thicker skin and denser bones, and therefore irradiated them with higher doses, until the practice was stopped in the 1970s.
There’s no direct evidence the practice increased cancer risk. But it highlights the easy adoption of racial categories in medicine, said Itai Bavli, a postdoctoral fellow in applied ethics at the University of British Columbia and lead author of a paper about the topic published in NEJM in 2022. The paper chronicled numerous characterizations in medical literature of Black skin as “perfectly opaque;” Black flesh as “harder;” and Black bones and skulls as “thicker and denser” or “almost impregnable.”
“The belief that Black people are different was so widespread,” said Bavli. “One might have expected X-ray technologies, which see through the skin to deeper structures beneath, to be spared racialization. They were not.”
STAT’s coverage of health inequities is supported by a grant from the Commonwealth Fund . Our financial supporters are not involved in any decisions about our journalism.
About the Authors
Usha lee mcfarling.
National Science Correspondent
Usha Lee McFarling, a veteran science reporter based in Los Angeles, has written for STAT since 2015 and covers health disparities.
Katie Palmer
Health Tech Correspondent
Katie Palmer covers telehealth, clinical artificial intelligence, and the health data economy — with an emphasis on the impacts of digital health care for patients, providers, and businesses.
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .
Recommended Stories

STAT Plus: Drug aimed at strengthening neurons to treat Alzheimer’s fails in trial

STAT Plus: Greece’s antitrust regulator probes Novartis over practices tied to a pricey eye drug

STAT Plus: UnitedHealth pledged a hands-off approach after buying a Connecticut medical group. Then it upended how doctors practice

STAT Plus: The weight loss drug shortage is driving patients to Hims. What happens when the shortage ends?

STAT Plus: 4 questions for neurology startups as venture investors pour millions into the field
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Public Health
- v.105(12); Dec 2015
Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review
W. J. Hall, M. V. Chapman, K. M. Lee, Y. M. Merino, T. W. Thomas, and S. H. Day participated in data extraction. W. J. Hall, M. V. Chapman, K. M. Lee, and B. K. Payne assisted with analysis and interpretation. All authors were involved in the conception or design of the review and assisted with writing, editing, or revising the content of the article.
Background. In the United States, people of color face disparities in access to health care, the quality of care received, and health outcomes. The attitudes and behaviors of health care providers have been identified as one of many factors that contribute to health disparities. Implicit attitudes are thoughts and feelings that often exist outside of conscious awareness, and thus are difficult to consciously acknowledge and control. These attitudes are often automatically activated and can influence human behavior without conscious volition.
Objectives. We investigated the extent to which implicit racial/ethnic bias exists among health care professionals and examined the relationships between health care professionals’ implicit attitudes about racial/ethnic groups and health care outcomes.
Search Methods. To identify relevant studies, we searched 10 computerized bibliographic databases and used a reference harvesting technique.
Selection Criteria. We assessed eligibility using double independent screening based on a priori inclusion criteria. We included studies if they sampled existing health care providers or those in training to become health care providers, measured and reported results on implicit racial/ethnic bias, and were written in English.
Data Collection and Analysis. We included a total of 15 studies for review and then subjected them to double independent data extraction. Information extracted included the citation, purpose of the study, use of theory, study design, study site and location, sampling strategy, response rate, sample size and characteristics, measurement of relevant variables, analyses performed, and results and findings. We summarized study design characteristics, and categorized and then synthesized substantive findings.
Main Results. Almost all studies used cross-sectional designs, convenience sampling, US participants, and the Implicit Association Test to assess implicit bias. Low to moderate levels of implicit racial/ethnic bias were found among health care professionals in all but 1 study. These implicit bias scores are similar to those in the general population. Levels of implicit bias against Black, Hispanic/Latino/Latina, and dark-skinned people were relatively similar across these groups. Although some associations between implicit bias and health care outcomes were nonsignificant, results also showed that implicit bias was significantly related to patient–provider interactions, treatment decisions, treatment adherence, and patient health outcomes. Implicit attitudes were more often significantly related to patient–provider interactions and health outcomes than treatment processes.
Conclusions. Most health care providers appear to have implicit bias in terms of positive attitudes toward Whites and negative attitudes toward people of color. Future studies need to employ more rigorous methods to examine the relationships between implicit bias and health care outcomes. Interventions targeting implicit attitudes among health care professionals are needed because implicit bias may contribute to health disparities for people of color.
PLAIN-LANGUAGE SUMMARY: Implicit attitudes are thoughts and feelings that often exist outside of conscious awareness, and thus are difficult to consciously acknowledge and control. Negative implicit attitudes about people of color may contribute to racial/ethnic disparities in health and health care. We systematically reviewed evidence on implicit racial/ethnic bias among health care professionals and on the relationships between health care professionals’ implicit attitudes about racial/ethnic groups and health care outcomes. Fifteen relevant studies were identified through searches of bibliographic databases and reference lists of studies that met inclusion criteria. Low to moderate levels of implicit racial/ethnic bias were found among health care professionals in all but 1 study. These implicit bias scores are similar to those in the general population. Levels of implicit bias against Black, Hispanic/Latino/Latina, and dark-skinned people were relatively similar across these groups. Although some associations between implicit bias and health care outcomes were nonsignificant, results also showed that implicit bias was significantly related to patient–provider interactions, treatment decisions, treatment adherence, and patient health outcomes.
In the United States, people of color face disparities in access to health care, the quality of care received, and health outcomes. 1–3 Compared with Whites, people of color face more barriers to accessing care, which includes preventive services, acute treatment, and chronic disease management. 4 People of color are also generally less satisfied with their interactions with health care providers. The National Healthcare Disparities Report showed that White patients received better quality of care than Black American, Hispanic, American Indian, and Asian patients. 4 Dominant communication styles, fewer demonstrated positive emotions, infrequent requests for input about treatment decisions, and less patient-centered care seem to characterize patient–provider interactions involving people of color. 4–6
People of color also face disparities in terms of morbidity, mortality, and health status. Black Americans, Hispanic Americans, and American Indians have higher infant mortality rates than White and Asian Americans. 1 The premature death rate from heart disease and stroke is highest among Black Americans. In addition, numerous disparities in health conditions and risk behaviors exist among people of color, including asthma, cigarette smoking, diabetes, early childbearing, HIV/AIDS, hypertension, low birth weight, obesity, periodontitis, preterm births, and tuberculosis. 1,4 Black Americans, Hispanic Americans, and American Indians were more likely to rate their health as fair or poor, and reported more days of feeling unwell in the past month, compared with White and Asian Americans. 1 Despite all of the advancements in health care in the past century, disparities based on race and ethnicity persist in access to health care, quality of care received, disease incidence and prevalence, life expectancy, and mortality.
HEALTH DISPARITIES AND PROVIDER ATTITUDES
Provider attitudes and behavior are a target area for researchers and practitioners attempting to understand and eradicate inequitable health care. 7 Although overt discriminatory behavior in the United States may have declined in recent decades, covert discrimination and institutional bias are sustained by subtle, implicit attitudes that may influence provider behavior and treatment choices. As a result, patients of color may be kept waiting longer for assessment or treatment than their White counterparts, or providers may spend more time with White patients than with patients of color. In addition, providers may vary in the extent to which they collaborate with patients in systematic though nondeliberate ways, in considering treatment options based on patients’ characteristics. Subtle biases may be expressed in several ways: approaching patients with a dominant and condescending tone that decreases the likelihood that patients will feel heard and valued by their providers, failing to provide interpreters when needed, doing more or less thorough diagnostic work, recommending different treatment options for patients based on assumptions about their treatment adherence capabilities, and granting special privileges, such as allowing some families to visit patients after hours while limiting visitation for other families. Variation in provider behaviors may be driven in part or in full by positive and negative attitudes that providers hold toward various racial and ethnic groups.
Negative attitudes toward certain social groups or personal characteristics often exist at the margins of awareness and are not easily accessible to individuals. Social psychology scholars have conceptualized prejudicial attitudes or bias as implicit and explicit. 8 Explicit attitudes are thoughts and feelings that people deliberately think about and can make conscious reports about. On the other hand, implicit attitudes often exist outside of conscious awareness, and thus are difficult to consciously acknowledge and control. These attitudes are often automatically activated and can influence human behavior without conscious volition. Racial/ethnic bias in attitudes, such as feeling that White people are nicer than Black people, whether conscious or not, can lead to prejudicial behavior, such as providers taking more time with White patients than Black patients and therefore learning more about the White patients’ needs and concerns.
Within the general population, significant research exists about implicit racial/ethnic bias. For example, White Americans have tended to associate negative valence in general, and certain feelings such as fear and distrust, with Black Americans. 9–15 Such group notions are automatically activated and applied most often when people are busy, distracted, tired, and under pressure. 16 The cognitive effort to assess and process a person’s individual characteristics appears to be greater than that required to quickly categorize a person into a particular group with particular characteristics. 9 Such short cuts in thinking may be useful in certain situations, but when providers are seeking to establish genuine working relationships with their patients and deliver equitable health care, fast thinking or quick categorization may get in the way. For example, during a diagnostic examination with a Black American adolescent, a provider may automatically presume that they are sexually active rather than asking open-ended questions about sexual activity and listening carefully to the responses.
Some White health care providers maintain problematic explicit ideas about their Black American patients, viewing them as less intelligent, less able to adhere to treatment regimens, and more likely to engage in risky health behaviors than their White counterparts. 17 Hispanic/Latino/Latina patients too were viewed as unlikely to accept responsibility for their own care and more likely to be noncompliant with treatment recommendations. 18 Yet, even if explicit attitudes are modified, implicit bias among providers toward people of color is likely to remain and influence care in ways that perpetuate disparity and inequity. Thus, even if explicit attitudes demonstrate a desire to provide equitable care, health care providers may unintentionally interact with patients of color less effectively than with White patients, which may contribute to health disparities. 19,20
PURPOSE OF THE SYSTEMATIC REVIEW
To reduce racial and ethnic disparities in health care, we must ascertain the prevalence of biased attitudes among health care providers and whether bias contributes to problems in patient–provider interactions and relationships, quality of care, continuity of care, treatment adherence, and patient health status. Although significant research has been conducted on racial/ethnic bias in the general population, relatively few studies have examined implicit racial/ethnic bias among health care professionals, despite its potentially significant impact on service delivery and health. This is therefore an important and emerging area of research. Systematic literature reviews are particularly useful in emerging areas because they synthesize what is known about a topic area, summarize the methods used to study a particular topic, and provide directions for future research. This systematic review seeks to answer 2 research questions: (1) Is there evidence of implicit racial/ethnic bias among health care professionals toward people of color? (2) Are there relationships between implicit racial/ethnic bias among health care professionals and health care outcomes (e.g., patient–provider interactions, clinical decision-making, standards of care, treatment adherence, symptomatology, health status, and patient satisfaction with care)?
We prepared this review using methods outlined in Cooper 21 and Littell et al. 22 and adhering to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria. 23 We developed protocols for bibliographic searches, study inclusion and exclusion, and data extraction before beginning the systematic search for relevant studies. In addition, we registered this review with PROSPERO, an international database of systematic reviews on health and social well-being.
Inclusion and Exclusion Criteria
We included studies in the review if they met the following criteria: (1) collected data from participants who were health care providers or were in training to become health care providers, (2) measured and reported results on implicit attitudes toward racial/ethnic groups, and (3) were written in English. We defined health care professionals as individuals who provided or were in training to provide preventive, curative, therapeutic, or rehabilitative health services to patients. Examples include physicians, dentists, pharmacists, physician assistants, nurses, midwives, dieticians, chiropractors, podiatrists, clinical psychologists, clinical social workers, phlebotomists, physical therapists, respiratory therapists, occupational therapists, audiologists, speech pathologists, optometrists, emergency medical technicians, and paramedics.
We excluded studies that only examined explicit bias, as well as studies that examined implicit bias that was not related to race or ethnicity. We also excluded articles or reports that were strictly theoretical or conceptual. Because of our limited proficiency in other languages, and because implicit racial/ethnic bias may be a different phenomenon in non-Western or non–English-speaking countries, we included only studies written in English. Finally, we did not use time frame restrictions because implicit bias is a relatively recent construct and we wanted to perform an exhaustive review of the literature.
Search Strategy
We consulted a behavioral and social sciences librarian to assist with identifying relevant computerized bibliographic databases in which to search. We used the following search string to search all databases for studies completed prior to June 5, 2014: (“implicit bias” OR “implicit attitude” OR “implicit prejudice” OR “conscious bias” OR “conscious attitude” OR “conscious prejudice”) AND (race OR racial OR ethnic OR ethnicity OR Hispanic OR Black OR African OR Asian OR Latin*) AND (health OR health care OR “health care”). The term “conscious” was used because implicit bias is sometimes referred to as unconscious or nonconscious bias.
Searching multiple databases increases the likelihood of identifying all possible studies falling within the scope of the review; we therefore searched 10 databases, some of which included gray literature sources. We performed searches in the following databases via EBSCO, with terms searched within the titles, abstracts, subject headings, and keywords: Academic Search Complete, CINAHL, Health Source: Nursing/Academic, PsycInfo, and Social Work Abstracts. We searched the following databases via ProQuest with terms searched within the titles, abstracts, and subject headings: ASSIA, Dissertations & Theses Full Text, and Social Services Abstracts. In addition, we searched the Conference Proceedings Citations Index with terms searched within titles, abstracts, and keywords. Finally, we searched PubMed with terms searched within titles, abstracts, and subject headings. When available, we used the English language filter. In addition to database searches, we used a reference-harvesting technique to locate relevant studies whereby we examined the reference lists of included studies to identify studies that might have not been incorporated into computerized bibliographic databases, such as papers in press or unpublished studies.
Study Selection Methods
We created a checklist of the inclusion and exclusion criteria prior to the search and used it for eligibility assessment. We piloted the checklist using 4 articles, and then 2 members of the research team who were responsible for screening were trained on the checklist and screening procedures. After performing the bibliographic searches, we imported 105 results into the RefWorks software program to assist with organization and duplicate removal. Following duplicate removal, 84 studies remained. Two trained members of the research team independently screened each of the 84 studies to determine eligibility. We included or excluded most studies after reading the title and abstract; however, it was also necessary to examine the full text document of some studies to determine eligibility. To examine interrater agreement, we compared the screening decisions of the 2 screeners and calculated Cohen κ with SPSS version 21 (IBM, Somers, NY), which showed excellent agreement (κ = 0.82; P < .05). 24 There were only 6 disagreements between the screeners, which the first author resolved by examining the source documents. We excluded 69 studies because they did not meet all of the inclusion criteria. Many of these studies did not address implicit bias, some did not address racial/ethnic bias, and others were nonempirical.
Data Extraction Methods
After completing the inclusion and exclusion process, we included 15 studies and then subjected them to data extraction. Figure 1 shows the process of identifying and including studies. We developed a data extraction spreadsheet to assist with identifying and collecting relevant information from the included studies. Information extracted included the citation, purpose of the study, use of theory, study design, study site and location, sampling strategy, response rate, sample size and characteristics, measurement of relevant variables, analyses performed, and results and findings. Four members of the research team participated in the extraction process. Each study was independently extracted 2 times by 2 different researchers. Another researcher then compared the 2 extraction results for each study to examine agreement and Cohen κ statistics were calculated, which showed excellent agreement (κ = 0.83; P < .05). There were 21 disagreements between the extractors, which 2 researchers resolved by examining the full text source document.

Flowchart depicting the identification, screening, and inclusion of studies of implicit racial/ethnic bias among health care professionals.
We included 15 studies in this review: 14 peer-reviewed journal articles and 1 doctoral dissertation. We present a summary of the methodological characteristics of these studies followed by a synthesis of the substantive findings regarding the presence of implicit racial/ethnic bias among professionals and the relationships between implicit bias and health care outcomes. Table 1 shows a summary of information extracted from each study.
TABLE 1—
Summary of Studies Included in the Systematic Review of Implicit Racial/Ethnic Bias Among Health Care Professionals
| Citation | Purpose of the Study | Study Design, Location, and Sampling Strategy | Sample Description for Health Care Professionals | Sample Description for Patients | Assessment of Implicit Bias Among Professionals | Analysis and Results on Associations Between Implicit Bias and Health Care Outcomes |
| Bean et al. | To examine implicit stereotyping of Hispanic American patients among nursing and medical students | Cross-sectional study Tucson, AZ Convenience sampling | 36 students (53% nursing students, 47% medical students) 81% White, 19% non-White 78% female, 22% male Response rate not reported | NA | Sequential priming examined Hispanic/Latino/Latina vs White faces associated with words related to good and bad patients. Participants were faster in recognizing noncompliance ( = 0.68*), risk ( = 1.53*), and general stereotype words ( = 0.88*) after exposure to Hispanic/Latino/Latina faces vs White faces. | NA |
| Blair et al. | To assess implicit and explicit bias against Hispanics/Latinos and Black Americans among primary care providers and community members | Cross-sectional study Denver, CO Convenience sampling | 210 primary care physicians 84% White, 6% Hispanic/Latino/Latina, and 1% Black 53% female, 47% male 4% aged 18–35 y, 73% 36–55 y, 11% ≥ 56 y 47% 1–10 y of clinical experience, 30% 11–20 y of clinical experience, 21% ≥ 20 y of clinical experience Response rate = 60% | NA | Race IAT examined Black vs White faces and associated them with positive and negative words. Physicians showed moderate pro-White, anti-Black bias (Mean IAT D = 0.27; SD = 0.34). Race IAT examined Hispanic/Latino/Latina vs White faces associated with positive and negative words. Physicians showed moderate pro-White, anti- Hispanic/Latino/Latina bias (Mean IAT D = 0.33; SD = 0.38) | NA |
| Fitzsimmons | To examine the extent to which implicit racial bias against students of color exists in nursing faculty teaching in baccalaureate programs in nursing | Cross-sectional study United States Convenience sampling and snowball sampling | 107 nursing faculty members 92% White, 2% Black, 1% Hispanic/Latino/Latina, and 2% other 98% female, 2% male Mean years in nursing education = 14 Response rate = 30% | NA | Skin tone IAT examined associations between dark- vs light-skinned faces and positive and negative words. Nurses showed moderate bias against dark-skinned faces (mean IAT D = 0.35; SD = 0.42). | NA |
| Sabin et al. | To measure implicit and explicit attitudes about race among medical doctors | Cross-sectional study United States and abroad Convenience sampling | 2535 medical doctors 66% White, 11% Asian, 8% Black, and 5% Hispanic/Latino/Latina 62% male and 38% female Mean age = 37 y 79% reside in United States Response rate not reported | NA | Race IAT examined Black vs White faces associated with positive and negative words. Physicians showed moderate pro-White, anti-Black bias (Mean IAT D = 0.39; SD = 0.47). | NA |
| White-Means et al. | To examine race and skin tone preferences among preprofessional health care providers | Cross-sectional study Memphis, TN Convenience sampling | 333 students (57% pharmacy students, 34% medical students, and 9% nursing students) 74% White, 18% Black, 7% Asian, and 1% Hispanic/Latino/Latina Response rate = 38% | NA | Race IAT examined Black vs White faces associated with positive and negative words. 100% of Hispanics/Latinos/Latinas, 94% of Whites, 76% of Asians, and 62% of Blacks showed a preference for White over Black people. Overall, students showed moderate pro-White, anti-Black bias (Mean IAT D = 0.40; SD not reported). Skin tone IAT examined associations between dark- vs light-skinned faces and positive and negative words. 100% of Hispanics/Latinos/Latinas, 85% of Asians, 83% of Whites, 41% of Blacks, and 51% of mixed race (Black and White) were more likely to prefer light skin to dark skin. Overall, students showed a moderate bias against dark-skinned people (mean IAT D = 0.31; SD not reported). | NA |
| Blair et al. | To examine if clinicians’ explicit and implicit racial/ethnic bias is related to Black and Hispanic/Latino/Latina patients’ perceptions of their care in established clinical relationships | Cross-sectional study Denver, CO Convenience sampling | 134 primary care physicians 75% White, 25% non-White 54% female, 46% male 50% with ≥ 10 y of clinical experience Response rate = 60% | 2908 patients 49% White, 30% Hispanic/Latino/Latina, 21% Black 58% female, 42% male 2% aged 18–35 y, 33% 36–55 y, 64% ≥ 56 y Education: 18% < high school diploma, 27% high school diploma or GED, 30% 1–3 y of college, 24% ≥ 4 y of college Household income: 35% < $15 000; 19% $16 000–$35 000; 14% $36 000–$55 000; 25% ≥ $56 000 Response rate = 47% | Race IAT examined Black vs White and Hispanic/Latino/Latina vs White faces associated with positive and negative words. 66% of physicians showed some level of bias. 51% of physicians had moderate-to-strong levels of bias against Hispanics/Latinos/Latinas. 43% of physicians had moderate-to-strong levels of bias against Black people. IAT D score not reported. | Hierarchical linear modeling results: For Black patients: Provider’s interpersonal treatment (B = −5.81*; SE = 2.52) Patient–provider communication (B = −4.31c; SE = 2.47) Trust in provider (B = −2.65; SE = 2.09) Contextual knowledge of patient (B = −5.58*; SE = 2.73) Composite score of patient-centeredness (B = −4.61*; SE = 2.25) For Hispanic/Latino/Latina patients: Provider’s interpersonal treatment (B = −0.58; SE = 1.71) Patient–provider communication (B = −0.13; SE = 1.68) Trust in provider (B = 0.85; SE = 1.42) Contextual knowledge of patient (B = −0.19; SE = 1.86) Composite score of patient-centeredness (B = −0.04; SE = 1.53) |
| Blair et al. | To determine the relationship between implicit racial/ethnic bias among primary care providers and treatment processes and outcomes related to hypertension among Black and Hispanic/Latino/Latina patients compared with White patients | Cross-sectional survey of primary care providers merged with multiyear patient record data following initial visit with the provider Denver, CO Convenience sampling | 138 primary care physicians 83% White, 17% non-White 54% female, 46% male 49% with ≥ 10 y of clinical experience Response rate = 52% | 4794 patients 49% White, 31% Hispanic/Latino/Latina, 20% Black 58% female and 42% male Mean age = 60 y Response rate not reported | Race IAT examined Black vs White and Hispanic/Latino/Latina vs White faces associated with positive and negative words. 70% of physicians showed some level of implicit bias against Black people and Hispanics/Latinos. 51% of physicians had moderate-to-strong levels of bias against Hispanics/Latinos/Latinas. 42% of physicians had moderate-to-strong levels of bias against Black people. IAT D score not reported. | Multilevel random coefficient modeling results: For Black patients: Treatment intensification (B = 0.007; SE = 0.030) Medication adherence (B = −3.8*; SE = 1.7) Hypertension control (B = −1.9; SE = 2.2) Time out of stage 2 hypertension (B = −1.2; SE = 1.4) For Hispanic/Latino/Latina patients: Treatment intensification (B = 0.014; SE = 0.024) Medication adherence (B = 1.3; SE = 1.4) Hypertension control (B = 2.3; SE = 1.8) Time out of stage 2 hypertension (B = −1.0; SE = 1.1) |
| Cooper et al. | To examine associations of clinician’s implicit attitudes about race with visit communication and patient ratings of care | Cross-sectional study Baltimore, MD Convenience sampling | 40 clinicians (90% physicians, 10% nurse practitioners) 48% White, 30% Asian, 22% Black 62% female, 38% male 38% aged 27–39 y, 35% 40–49 y, 25% 50–62 y Mean experience since residency = 13 y Response rate = 63% | 269 patients 79% Black and 21% White 71% female and 29% male Mean age = 56 y 81% high school graduates 59% annual income > $35 000 Response rate = 67% | Race IAT examined Black vs White faces associated with positive and negative words. Physicians showed slightly moderate pro-White, anti-Black bias (Mean IAT D = 0.26; SD = 0.49). Medical Compliance IAT examined Black vs White faces associated with compliant and reluctant patients. Physicians showed moderate association of White race with compliance (Mean IAT D = 0.29; SD = 0.41). | Linear and logistic regression with generalized estimating equations results: For White patients: Clinician verbal dominance (B = 11.0*) Visit length (B = 8.0) Clinician speech speed (B = 0.25) Patient centeredness (B = −0.05) Clinician positive affect (B = −0.01) Patient positive affect (B = 0.01) Clinician asked for patient input (OR = 16.6*; 95% CI = 7.3, 33.5) Clinician respected patient (OR = 26.5*; 95% CI = 18.7, 36.0) Clinician liked patient (OR = 8.0*; 95% CI = 3.0, 19.5) Patient liked clinician (OR = 31.4; 95% CI = 20.8, 44.5) Patient trust in clinician (OR = 76.9; 95% CI = 68.9, 83.4) Patient confidence in clinician (OR = 79.0; 95% CI = 70.7, 85.4) Patient would recommend clinician (OR = 29.1; 95% CI = 19.4, 41.2) Clinician verbal dominance (B = −25.0*) Visit length (B = −21.0*) Clinician speech speed (B = 3.9*) Patient centeredness (B = 0.15*) Clinician positive affect (B = 0.12*) Patient positive affect (B = 0.11†) Clinician asked for patient input (OR = 19.4*; 95% CI = 6.8, 44.1) Clinician respected patient (OR = 21.6; 95% CI = 8.3, 45.5) Clinician liked patient (OR = 6.6; 95% CI = 1.8, 21.4) Patient liked clinician (OR = 31.6; 95% CI = 22.5, 42.5) Patient trust in clinician (OR = 73.9; 95% CI = 64.2, 81.7) Patient confidence in clinician (OR = 74.9; 95% CI = 66.0, 82.0) Patient would recommend clinician (OR = 23.7*; 95% CI = 15.5, 34.5) For Black patients: Clinician verbal dominance (B = 9.0†) Visit length (B = 7.0) Clinician speech speed (B = −0.76) Patient centeredness (B = −0.10) Clinician positive affect (B = −0.10) Patient positive affect (B = −0.10*) Clinician asked for patient input (OR = 28.3; 95% CI = 22.3, 35.1) Clinician respected patient (OR = 34.9*; 95% CI = 27.2, 43.5) Clinician liked patient (OR = 23.8; 95% CI = 17.9, 31.0) Patient liked clinician (OR = 32.7*; 95% CI = 26.2, 39.9) Patient trust in clinician (OR = 67.6; 95% CI = 60.6, 73.8) Patient confidence in clinician (OR = 71.4*; 95% CI = 64.1, 77.7) Patient would recommend clinician (OR = 34.4*; 95% CI = 27.1, 42.5) Clinician verbal dominance (B = 10.0) Visit length (B = 20.0*) Clinician speech speed (B = −1.75*) Patient centeredness (B = −0.93†) Clinician positive affect (B = −0.06) Patient positive affect (B = −0.04) Clinician asked for patient input (OR = 23.0*; 95% CI = 16.8, 30.7) Clinician respected patient (OR = 37.0; 95% CI = 28.7, 46.2) Clinician liked patient (OR = 23.2; 95% CI = 16.7, 31.3) Patient liked clinician (OR = 38.4; 95% CI = 31.7, 45.5) Patient trust in clinician (OR = 64.0*; 95% CI = 6.5, 70.9) Patient confidence in clinician (OR = 71.2†; 95% CI = 63.8, 77.7) Patient would recommend clinician (OR = 36.3; 95% CI = 29.4, 43.8) |
| Green et al. | To test the presence of implicit race bias among physicians and assess its prediction of thrombolysis recommendations for Black and White patients with acute coronary syndromes | Cross-sectional study Boston, MA, and Atlanta, GA Convenience sample | 220 resident physicians (83% internal medicine residents, 17% emergency medicine residents) 63% White, 24% Asian/Pacific Islander, 6% Other, 5% Black, 2% Hispanic/Latino/Latina 60% male, 40% female Response rate = 28% | NA | Race Preference IAT examined Black vs White faces associated with positive and negative words. Residents showed moderate pro-White, anti-Black bias (Mean IAT D = 0.36; SD = 0.40). Race Cooperative IAT examined Black vs White faces associated with general cooperativeness. Residents showed moderate association of White race with cooperativeness (mean IAT D = 0.30; SD = 0.39). Race Medical Cooperative/Compliance examined Black vs White faces associated with medical cooperativeness. Residents showed moderate association of White race with cooperativeness (mean IAT D = 0.22; SD = 0.40). | Multiple linear regression results: For White patients: Recommend thrombolysis for treatment of coronary artery disease (B = 0.17*) Recommend thrombolysis for treatment of coronary artery disease (B = 0.08) Recommend thrombolysis for treatment of coronary artery disease (B = 0.10) Recommend thrombolysis for treatment of coronary artery disease (B = 0.16*) For Black patients: Recommend thrombolysis for treatment of coronary artery disease (B = −0.19*) Recommend thrombolysis for treatment of coronary artery disease (B = −0.09) Recommend thrombolysis for treatment of coronary artery disease (B = 0.02) Recommend thrombolysis for treatment of coronary artery disease (B = −0.11*) |
| Hagiwara et al. | To examine how non-Black primary care physician’s explicit and implicit racial bias and Black patients’ perceived past discrimination affected physician–patient talk time ratio during medical interactions and the relationship between this ratio and patients’ subsequent adherence | Cross-sectional survey of physicians and longitudinal data collection with patients Detroit, MI Convenience sampling | 14 primary care physicians 86% Asian, 14% White 50% female, 50% male Mean age = 30 y Response rate = 83% | 112 patients 100% Black 77% female, 23% male Mean age = 43 y 100% low income Response rate = 75% | Race IAT examined Black vs White faces associated with positive and negative words. Physicians showed a very slight pro-Black, anti-White (Mean IAT D = −0.10; SD = 0.36). | Correlation and OLS regression results: For Black patients: Physician verbal dominance during patient encounter ( = 0.32*) Patient treatment adherence at baseline ( = 0.03) Patient treatment adherence at 4-wk follow-up ( = 0.11) Patient treatment adherence at 16-wk follow-up ( = 0.12) Patient trust in physician ( = 0.03) Physician verbal dominance during patient encounter (b = 0.33†; SE = 0.19) |
| Haider et al. | To estimate unconscious race and social class bias among 1st-year medical students and examine the association of these biases with clinical assessments | Cross-sectional study Baltimore, MD Convenience sampling | 202 medical students 54% White, 31% Asian, 6% Black, 6% Hispanic/Latino/Latina, 3% other 52% female, 48% male 16% aged ≤ 21 y, 76% 22–25 y, 8% ≥ 26 y Response rate = 84% | NA | Race IAT examined Black vs White faces associated with positive and negative words. No implicit bias among 17% of medical students. 69% of students demonstrated preference for White over Black. 14% of students demonstrated preference for Black over White. Students showed moderate pro-White, anti-Black bias (Mean IAT D = 0.32; SD = 0.33). | OLS regression and logistic regression results: For Black patient vignettes: Assessment of pain level (b = −0.35) Appropriate informed consent (OR = 0.60; 95% CI = 0.22, 6.2) Reliability of patient (OR = 2.45; 95% CI = 0.82, 5.36) Trust in patient (OR = 1.22; 95% CI = 0.35, 4.30) For White patient vignettes: Assessment of pain level (b = −0.69) Appropriate informed consent (OR = 0.93; 95% CI = 0.20, 4.20) Reliability of patient (OR = 1.50; 95% CI = 0.38, 5.80) Trust in patient (OR = 1.34; 95% CI = 0.43, 4.21) |
| Hausmann et al. | To examine implicit racial bias of SCI physicians and its association with functioning and well-being for individuals with SCI | Cross-sectional study United States Convenience sampling | 14 SCI physicians 57% White, 29% Asian, 7% Black, 7% Pacific Islander 93% male, 7% female Mean age = 48 y 57% had at least 15 y experience in SCI medicine Response rate = 49% | 162 patients with neurologic impairments from SCI 60% White, 40% Black 77% male, 33% female Mean age = 40 y Response rate not reported | Race IAT examined Black vs White faces associated with positive and negative words. 100% of SCI physicians show some level of implicit bias toward Black people. Physicians showed strong pro-White, anti-Black bias (Mean IAT D = 0.62; SD = 0.35). | Multilevel logistic and linear regression results for White and Black patients: Patients’ social integration (OR = 4.80*; 95% CI = 1.44, 16.04) Depression (B = 3.24*) Satisfaction with life (B = −4.54*) Patient mobility (OR = 0.38; 95% CI = 0.11. 1.35) Occupational engagement (OR = 0.61; 95% CI = 0.20, 1.89) Physical independence (OR = 2.91; 95% CI = 0.57, 14.80) General health status (OR = 1.40; 95% CI = 0.38, 5.16) |
| Penner et al. | To examine the relationship of non-Black physicians’ implicit and explicit racial bias to their perceived behavior and their perceptions of their interactions with Black patients | Cross-sectional study Detroit, MI Convenience sampling | 15 primary care physicians 80% Asian, 20% White 53% male, 47% female Mean age = 31 y Response rate = 83% | 150 patients 100% Black 75% female and 25% male Mean age = 44 y Response rate = 73% | Race IAT examined Black vs White faces associated with positive and negative words. Physicians showed slight pro-White, anti-Black bias (Mean IAT D = 0.10; SD not reported). | Multilevel modeling with general estimating equation results: Among physicians: Feeling on the same team (b = −0.28†) Consultation with patient on treatment decisions (β = 0.22) Among Black patients: Physician warmth and friendliness (b = −0.29*) Feeling on the same team (b = −0.18) Consultation with patient on treatment decisions (b = −0.08) Satisfaction with interaction (b = −0.31) Composite score of patients’ team feelings, physician warmth and friendliness, and satisfaction with interaction (b = −0.26†) |
| Sabin et al. | To assess implicit racial bias among pediatricians | Cross-sectional study Seattle, WA Convenience sample | 95 pediatricians (59% resident physicians, 41% attending physicians) 82% White, 18% non-White 65% female, 35% male 42% aged 20–30 y, 33% 31–40 y, 25% > 40 y Response rate = 58% | NA | Race Attitude IAT examined Black vs White faces associated with positive and negative words. Physicians showed slight pro-White, anti-Black bias (Mean IAT D = 0.18; SD = 0.44). Race and Compliant Patient IAT examined Black vs White faces associated with compliant and reluctant patients. Physicians showed a moderate implicit association between compliancy and White faces (Mean IAT D = 0.25; SD = 0.42). Race and Quality of Medicine IAT examined Black vs White faces associated with preferred and acceptable medical care. Physicians showed a moderate association between preferred care and Black faces (Mean IAT D = −0.21; SD = 0.33). | Correlation results regarding racial differences in ideal treatment recommendations for pain control, UTI management, ADHD, and asthma control: ( = 0.00, = −0.04) ( = 0.16, = −0.05) ( = −0.27, = 0.09) |
| Sabin and Greenwald | To examine the association between attitudes and beliefs about race among pediatricians and treatment recommendations for asthma, ADHD, UTI, and pain | Cross-sectional study Seattle, WA Convenience sampling | 86 pediatricians (59% resident physicians, 41% attending physicians) 82% White, 18% non-White 35% male, 65% female Response rate = 53% | NA | Race IAT examined Black vs White faces associated with positive and negative words. Physicians showed slight pro-White, anti-Black bias (Mean IAT D = 0.18; SD = 0.44). Medical Compliance IAT examined Black vs White faces associated with compliant and reluctant patients. Physicians showed a moderate pro-White implicit race and compliance bias (mean IAT D = 0.25; SD = 0.42). Race-Quality of Care IAT examined Black vs White faces associated with preferred and acceptable medical care. Physicians showed a moderate implicit association of Black patients with preferred medical care (Mean IAT D = −0.21; SD = 0.33). | Correlation results: For White patient vignettes: Recommended ideal treatment of pain ( = 0.47) Recommended ideal treatment of UTI ( = −0.12) Recommended ideal treatment of ADHD ( = −0.38) Recommended ideal treatment of asthma ( = −0.04) Recommended ideal treatment of pain ( = 0.37*) Recommended ideal treatment of UTI ( = −0.14) Recommended ideal treatment of ADHD ( = 0.11) Recommended ideal treatment of asthma ( = −0.09) Recommended ideal treatment of pain ( = 0.67*) Recommended ideal treatment of UTI ( = −0.06) Recommended ideal treatment of ADHD ( = −0.14) Recommended ideal treatment of asthma ( = −0.09) For Black patient vignettes: Recommended ideal treatment of pain ( = −0.38*) Recommended ideal treatment of UTI ( = −0.15) Recommended ideal treatment of ADHD ( = 0.49) Recommended ideal treatment of asthma ( = −0.10) Recommended ideal treatment of pain ( = −0.11) Recommended ideal treatment of UTI ( = 0.04) Recommended ideal treatment of ADHD ( = 0.04) Recommended ideal treatment of asthma ( = 0.16) Recommended ideal treatment of pain ( = 0.04) Recommended ideal treatment of UTI ( = −0.07) Recommended ideal treatment of ADHD ( = −0.21) Recommended ideal treatment of asthma ( = 0.43) |
Note . ADHD = attention deficit hyperactivity disorder; CI = confidence interval; IAT = Implicit Association Test; NA = not applicable; OLS = ordinary least squares; OR = odds ratio; SCI = spinal cord injury; UTI = urinary tract infection. IAT D score is an effect size: 0 indicates no bias, positive scores indicate preference for White people over people of color, and negative scores indicate preference for people of color over White people.
† P < .1; * P < .05.
Study Design Characteristics
Of the 15 included studies, 13 (87%) were cross-sectional and 2 studies used cross-sectional survey data from health care providers merged with longitudinal data from patients. All of the studies sampled participants from the United States, and only 1 study included a small portion of participants from outside the United States. All of the studies used convenience sampling. Eleven studies (73%) sampled participants from a single city; the cities were all large urban areas (e.g., Atlanta, GA; Baltimore, MD; and Denver, CO). Only 4 studies sampled participants from multiple locations across the United States. Among health care professional participants, the response rates ranged from 28% to 84% (mean = 57%; SD = 18.6%), and 2 studies did not report response rates. Among the 6 studies that used patient participants, 2 did not report response rates; among the studies that did report them, they ranged from 47% to 75% (mean = 66%; SD = 12.8%).
Study Samples
All 15 studies were conducted in the United States, although country in which the research was published was not an exclusion criteria. Twelve studies sampled practicing health care professionals, which included physicians, nurses, and nurse practitioners in the areas of primary care, pediatrics, internal medicine, emergency medicine, and spinal cord injury. Three studies included medical, nursing, and pharmacy students as participants. The sample sizes for health professionals varied drastically, from 14 to 2535 participants. Five studies had fewer than 50 participants, and 9 studies had between 50 and 350 professional participants. In most studies, about 75% to 80% of professionals were White, followed by small but substantial proportions of Asian professionals (10%–30%) and small proportions of Black and Hispanic/Latino/Latina professionals (0%–10%). In most studies, the proportions of males and females were about equal; however, samples tended to have more female than male participants. Six of the 12 studies that sampled practicing professionals measured their professional experience, which showed that about half had less than 10 years of experience. National estimates of physician demographics have shown that 72% of physicians are male, 74% are White, 17% are Asian, 5% are Hispanic, 4% are Black, 29% have less than 10 years of experience, 32% have between 10 and 20 years of experience, and 39% have more than 20 years of experience. 40 However, the 15 studies in this review included physicians and other health care professionals from a variety of disciplines, which may account for the demographic differences.
Six of the 15 studies (40%) collected data from patients. Patient sample sizes ranged from 112 to 4794 (mean = 1399; SD = 1991), with 2 studies having about 3000 or more participants and 4 studies having between 100 and 300 participants. All 6 studies included Black patients, 4 included White patients, and only 2 included Hispanic/Latino/Latina patients. Most studies had larger proportions of female (about 60%–70%) than male patients. Patient samples consisted primarily of middle-age and older adults. Only 3 of the 6 studies reported information about patients’ socioeconomic status, which showed that most patients’ highest level of education was a high school degree and most had low to moderate incomes (i.e., < $35 000 per year).
Measurement of Implicit Racial/Ethnic Bias
Of the 15 studies reviewed, 9 examined bias against Black people compared with White people; 3 examined bias against both Black and Hispanic/Latino/Latina people compared with White people; 1 examined bias against Hispanic/Latino/Latina compared with White people; 1 examined bias against individuals with darker versus lighter skin tones; and 1 examined bias against Black, Hispanic, and dark-skinned individuals versus White or light-skinned individuals. Fourteen of the 15 studies used the Implicit Association Test (IAT) 41 to measure implicit bias. The IAT is a computerized categorization task in which participants sort stimuli (e.g., pictures, names, and words) into opposing categories as quickly and as accurately as possible. For example, a participant might demonstrate faster reaction times between negative words (e.g., nasty) and pictures of Black faces than White faces, which would reflect an association between negativity and Black Americans. To score responses on the IAT, a D score is calculated, which is an effect size. 42 When interpreting IAT D scores, 0 indicates no bias, positive scores indicate preference for White people over people of color, and negative scores indicate preference for people of color over White people. All 14 studies examined associations along the dimension of positive versus negative using words such as wonderful and peace versus words like horrible and evil. Of these studies, 4 also examined associations related to the medical context, such as patient compliance and cooperativeness. Only 1 study 25 did not use the IAT, but instead used sequential priming. In this method, faces were presented very briefly, at a subliminal level, followed by positive and negative words to be evaluated. Meta-analytic data suggest that sequential priming measures show evidence of validity similar to that of the IAT. 43
Implicit Racial/Ethnic Bias Among Professionals
Of the 15 reviewed studies, 14 found evidence of low to moderate levels of implicit bias against people of color among health care professionals. Only 1 study reported no evidence of implicit bias against people of color. 34 Thirteen studies reported that health care professionals were more likely to associate Black Americans with negative words compared with White Americans. The D scores reported in these studies ranged from −0.10 to 0.62 (mean = 0.28; SD = 0.18). Two studies did not provide D scores, but found evidence of low to moderate bias against Black Americans in 42% and 43% of their samples of professionals. Four studies reported prevalence rates of anti-Black bias in their overall sample, which ranged from 42% to 100% (mean = 63.5; SD = 23.7). In sum, 13 of 14 studies examining implicit anti-Black bias found that health care professionals tended to possess low to moderate levels of negative associations with Black Americans.
Further, 4 studies found evidence of moderate anti-Black bias in health care professionals’ evaluations of Black Americans as patients, with D scores ranging from 0.22 to 0.30 (mean = 0.26; SD = 0.03). However, 2 studies also reported that their samples of professionals associated high-quality medical care, as opposed to low-quality care, more with Black Americans than with White Americans. 38,39 Thus, these 4 studies revealed that, overall, health care professionals associated Black Americans with being less cooperative, less compliant, and less responsible in a medical context.
Four studies reported evidence of moderate levels of implicit bias against Hispanic/Latino/Latina individuals compared with White individuals. Two studies did not report their D scores, but reported that about half of their participants demonstrated moderate to strong implicit bias against Hispanic/Latino/Latina individuals. 30,31 One study reported an overall moderate bias against Hispanic/Latino/Latina individuals relative to Whites on the IAT (D = 0.33). 26 Further, Bean et al. 25 reported that professionals tended to associate Hispanic/Latino/Latina people with noncompliance and risky behavior, and had general stereotypes of them (e.g., that they were unimaginative). These studies suggested that health care professionals possess implicit bias against Hispanic/Latino/Latina individuals at a level comparable to levels of implicit bias against Black Americans.
Finally, 2 studies reported moderate amounts of implicit bias among health care professionals against darker-skinned individuals compared with lighter-skinned individuals. 29,32 IAT D scores in these studies were 0.33 and 0.31, which are comparable to the D scores reported in other studies of implicit biases against Black Americans and Hispanic/Latino/Latina individuals.
To characterize the effect size in these studies, we performed a meta-analysis on the 13 studies that reported an effect size or sufficient information to compute one. The weighted mean effect size was d = 0.34, which is significantly different from zero ( z = 7.17; P < .001). Tests for heterogeneity of effects were not significant ( Q [12] = 3.94; P = .98) indicating a lack of heterogeneity across samples. Implicit bias scores were robust and showed little variability across studies, suggesting that this moderate effect size may provide a good estimate of the effect in the population of health care professionals.
Implicit Racial/Ethnic Bias and Health care Outcomes
Ten of the 15 studies examined the relationships between implicit racial/ethnic bias scores and particular types of health care outcomes. We chose to divide these outcomes into 4 general categories to succinctly summarize the literature: patient–provider interactions, treatment decisions, patient treatment adherence, and patient health outcomes. Within these categories the outcome data source (e.g., patient self-report, provider self-report, and medical records) varied. Five studies focused on patient–provider interactions. Four studies considered treatment decision-making and recommendations. Two examined treatment adherence, and 2 looked at health or mental health outcomes. Among the 80 associations between implicit bias and variables related to patient–provider interactions, 33 were significant or marginally significant. Among the 40 associations between implicit bias and variables related to treatment decisions, 7 were significant or marginally significant. Among the 5 associations between implicit bias and variables related to treatment adherence, 1 was significant. Finally, among the 11 associations between implicit bias and patient health outcomes, 3 were significant. We did not perform a meta-analysis on these associations because the 136 reported associations came from only 10 samples, which poses problems for the assumption that observed effects reflect independent estimates.
There were also differences in the ways implicit bias was measured and the presence of significant associations with health care outcomes. General good versus bad bias was the most common method used to assess bias; however, some studies attempted to tap more nuanced forms of bias in terms of compliant versus noncompliant, cooperative versus uncooperative, and high versus low quality of care. Among the 84 associations between general bias and health care outcomes, 26 were significant or marginally significant. Among the 102 associations between more nuanced forms of bias and outcomes, 18 were significant or marginally significant. Thus, the more general and perhaps visceral comparison, good versus bad, seemed more often to have an impact on health care outcomes.
Patient–provider interactions.
Black patients perceived poorer treatment in domains such as patient centeredness, contextual knowledge of the patient, and patient–provider communication from providers who demonstrated implicit bias against Blacks on the IAT; Latino patients in the same study did not perceive poorer treatment in these domains, although higher percentages of physicians showed bias against them than against Black patients. 30 In another study, White and Black patients found physicians with anti-Black bias to be more dominant in their communication styles. Pro-White, anti-Black physician bias was associated with White patients feeling more respected by the physician. However, among Black patients, provider bias was associated with less respect from providers, lower levels of liking the providers, and less willingness to recommend their provider to someone else. They also reported longer visits and experienced their visits with the provider as being less collaborative. 32 Another study also found an association between implicit racial bias and verbal dominance by physicians during encounters with Black patients. 34 Pro-White attitudes among primary care physicians were associated with lower scores by Black patients on physician warmth and friendliness, as well as lower scores by physicians regarding their feelings of “being on the same team” with their Black patients. 37 Conversely, no significant associations were noted when vignettes were used to assess the impact of bias on medical student responses in terms of assessment of pain delivery or proper informed consent. 35
Treatment decisions.
When treatment recommendation was used as an outcome, Green et al. 33 found that physicians demonstrating pro-White bias were less likely to recommend thrombolysis to Black patients and more likely to recommend this treatment of White patients. Among pediatricians, Sabin et al. 38 found no significant associations between implicit bias and treatment recommendations for pain control, urinary tract infection, attention deficit hyperactivity disorder, and asthma control. Yet in a similar study, Sabin and Greenwald 39 found pediatricians recommending the ideal management of pain at lower rates when responding to vignettes of Black patients as opposed to White patients.
Patient treatment adherence.
Pro-White bias was associated with Black patients being less likely to fill prescriptions; however, this relationship was not found for Hispanic/Latino/Latina patients. 31 Another study did not find significant relationships between implicit bias assessed at baseline and Black patient treatment adherence at 4 and 16 weeks follow-up. 34
Patient health outcomes.
Two studies examined health and mental health outcomes: one with spinal cord injury patients and another with hypertensive patients. The study of physicians specializing in spinal cord injury found significant relations between implicit bias scores and patient health outcomes. 36 Psychosocial health outcomes (i.e., social integration, depression, and life satisfaction) for Black and White patients appeared to be negatively affected by the presence of physician bias in this sample. However, physical health outcomes (i.e., mobility, physical independence, and general health status) appeared uninfluenced by the presence of bias. Another study found no significant associations between implicit bias and hypertension outcomes among Black and Hispanic/Latino/Latina patients. 31
Results of this review suggest that implicit bias against Black, Hispanic/Latino/Latina, and dark-skinned individuals is present among many health care providers of different specialties, levels of training, and levels of experience. Mean IAT scores and prevalence rates of implicit racial/ethnic bias among the reviewed studies are similar to those documented using the general population. 44 In addition, the levels of implicit bias among health care professionals against Black, Hispanic/Latino/Latina, and dark-skinned people appear to be relatively similar across these groups. Virtually absent in the literature, however, is evidence-based information on how to reduce an individual health care provider’s bias.
The extant literature is also unclear on how implicit bias affects health care outcomes both through direct and indirect pathways. Results were mixed, as some studies reported significant relationships between implicit racial/ethnic bias scores and health care outcomes and other studies found no significant relations. Nonetheless, implicit bias appears to be more frequently associated with patient–provider interactions and relationships than other outcomes. These findings may imply a pathway by which patient–provider interactions mediate the relationship between provider implicit bias and patient outcomes in terms of treatment adherence and health status. Other factors not considered in this review, such as health care system characteristics, provider background characteristics, and patients with multiple minority identities, may mediate or moderate the ways in which provider attitudes influence patient–provider relationships and health outcomes.
This review also raises questions of how biases may interact in terms of intersecting identities. The patient and professional samples used were predominantly female. Because women in the general population have been shown to have lower levels of implicit racial/ethnic bias, 45 it is possible that the estimates of bias, both in attitudes and in outcomes, in the samples represented in this review are lower than if the samples of both patient and providers were more gender balanced. Likewise, women, regardless of ethnicity, are more likely than men to experience biased interactions and treatment in care. 46,47
Implicit bias toward people of color may indeed interact with other characteristics such as gender, age, sexual orientation, national origin, and disability status to produce differential treatment outcomes. There is evidence of implicit bias based on gender, age, sexual orientation, ethnicity, religion, and disability in the general population. 44 However, research on implicit bias in health care has tended to focus on race, and few studies have investigated bias related to other identity characteristics.
Findings from this review suggest that implicit bias may be activated under stressful working conditions. Health profession students demonstrated levels of implicit racial/ethnic bias similar to those of practicing providers; however, students’ bias may have been less likely to affect decision-making and outcomes than practitioners’ bias. Only 1 study examined the relationship between implicit bias among students and health care outcomes, but it found no significant relationships. 35 However, 8 of the 9 studies of practicing providers found significant relationships between implicit bias scores and health care outcomes. Perhaps the impact of bias becomes more pronounced as professionals progress through their health care training and career. Repeated instances of certain patient situations may become engrained as “truths” about an entire population group. For example, Hispanic/Latino/Latina patients often coming to appointments late may lead to a provider’s belief that this group does not take responsibility for their health care, and consequently the provider is generally less respectful and pleasant with future Hispanic/Latino/Latina patients. In addition, exposure to bias among providers’ peers may reinforce their bias, making them more likely to make treatment decisions that are based on racial/ethnic stereotypes rather than an individual patient’s medical status. There is evidence of cultural and institutional bias in health care settings. 48–50 Researchers seeking to develop and test interventions to decrease bias should consider multiple targets, including primary prevention for health profession students, interventions for practitioners actively working with patients, and systemic interventions that neutralize biases that have been institutionalized in health care settings.
Finally, the reviewed studies focused on relatively few health care specialties, making comparisons of implicit bias between areas of health care difficult. Nonetheless, 2 studies 38,39 of pediatricians in this review found that they had lower levels of implicit bias than other types of health care providers. Certain health care disciplines may be more prone to implicit bias. It is possible that certain types of training address problematic attitudes throughout the education period so that practicing professionals demonstrate lower levels of bias. Within medicine, examinations of the curriculum and comparisons by specialty may prove useful. Interventions for bias may look different according to the needs and realities of particular specialties. For instance, because of time pressure, critical care professionals may need more systemic interventions, whereas specialties such as internal medicine, pediatrics, or family medicine may benefit from a combination of both individual and systemic intervention strategies.
In sum, the current literature suggests that implicit racial/ethnic bias is present in health care and bias can affect health care outcomes. However, the current literature is not strong enough to make definitive statements about the impact of implicit bias because of the methodological limitations of studies in the literature.
Methodological Limitations of Studies
We identified 5 prominent limitations among the studies reviewed. First, all but 2 of the studies used cross-sectional designs. Although cross-sectional designs are useful in determining the prevalence of a condition within a given population, they have limited ability to determine predictive relationships between variables. Because cross-sectional studies are conducted at 1 point in time, it is difficult to infer causality between a risk factor (e.g., exposure to a biased health care provider) and an outcome (e.g., a patient’s psychological distress).
A second limitation was the use of convenience sampling. Although convenience sampling may be highly feasible and efficient, it can lead to the underrepresentation or overrepresentation of particular groups within a sample. It is therefore unlikely that a convenience sample is representative of the population of interest, which raises questions about the generalizations that can be made from the findings.
Small sample size was a third limitation because the studies were estimating the prevalence of implicit bias and quantitatively examining the strength and direction of relationships between bias and health care outcomes. Eight studies had sample sizes of approximately 100 professional participants or less, and 3 of these studies had 15 participants or less. These small sample sizes raise the concern of whether these studies possessed enough statistical power to detect the prevalence of implicit bias in their sample and the effect of implicit bias on health care outcomes. In addition, certain statistical analyses in some studies relied on much smaller samples than the initially reported total sample size (e.g., Sabin and Greenwald 39 ), which reduces the chance of detecting a true effect.
A fourth limitation related to the measurement of implicit bias. Fourteen studies used the IAT to measure implicit bias. Although the IAT has demonstrated good internal consistency, with Cronbach alphas ranging from 0.70 to 0.90, 51 the instruments’ test–retest reliability has been criticized. 52 The relatively low test–retest reliability of the IAT, ranging from 0.25 to 0.60, 53 raises concerns about whether the IAT measures stable implicit attitudes or if other, nonattitudinal factors influence performance on the IAT. For example, contextual information such as whether a Black individual is presented in a positive or negative context influences the degree to which participants make negative associations with Black individuals. 54 Some researchers have also argued that performance on the IAT might be influenced by individuals’ knowledge or awareness about group stereotypes in a society rather than their personal attitudes. 55–58 Other researchers have argued that some effects of the IAT may be influenced by whether paired categories are similar in salience. 59,60 For example, images of people of color may be more salient to the average White participant because of unfamiliarity, whereas negative words may be more salient in general because of their affective nature. Thus, when 2 highly salient categories are paired (e.g., people of color and negative words), participants are quicker to respond than if categories different in salience are paired (e.g., White individuals and negative words). The IAT is the most widely known implicit measure but also the most controversial. 52,61
A final limitation was the narrowness in measurement of implicit bias. Most studies focused on bias against Black Americans. Few studies examined implicit bias against Hispanic/Latino/Latina Americans, and no studies examined bias toward other racial/ethnic minority groups, such as American Indians, Asian Americans, and Arab Americans. These groups also face health disparities, 1,4 and there is evidence of stereotypical and negative implicit attitudes toward these groups among the general population in the United States. 44 In addition, no study investigated implicit bias toward immigrants. Many people of color are also immigrants and may face a unique form of prejudice related to their race/ethnicity as well as their immigrant status. Finally, although Black versus White inequalities have tended to dominate the focus of race relations in the United States, Asian, Hispanic/Latino/Latina, and multiracial Americans are the fastest-growing racial/ethnic groups, 62 and examining bias toward these groups should not be neglected.
Recommendations for Future Research
Implicit attitudes appear to be an important target for further research in health care; however, methodological limitations need to be addressed in future studies to more fully and accurately understand how implicit bias affects care and health. In addition, researchers will need to ask more nuanced questions and use more rigorous designs and analytic methods to fully understand the role, impact, and appropriate intervention strategies for implicit bias within health care.
In the future, cross-sectional studies should primarily be used to ascertain national estimates of implicit bias among health care providers, to examine correlational research questions, or to test exploratory hypotheses. Longitudinal studies are needed to examine causal relations between implicit bias and health care outcomes. Longitudinal studies could also provide information on changes in implicit bias over time throughout providers’ careers and could help identify appropriate intervention points and factors that affect the acquisition of implicit bias. Interventions to address implicit bias are emerging; to date, they are not well tested, although some intervention studies are in process. 63–65 To evaluate the efficacy and effectiveness of such interventions, researchers should use pretest–posttest cohort designs, well-matched intervention–comparison group pretest–posttest designs, and randomized control trials, which are the gold standard design for measuring intervention impact. Finally, multilevel study designs may be needed to address clustering concerns, such as providers being nested within medical specialties and care delivery sites. Likewise, if the unit of analysis is patients and their experience, patients can be nested within families, providers, and health care settings. Not accounting for clustering during analyses can lead to biased estimated standard errors and spurious results. 66 Multilevel studies also allow researchers to examine the influence of both provider and institutional bias on health care outcomes.
In terms of sampling, futures studies should strive for samples that are more representative. Research on implicit bias would be strengthened by more geographically representative samples of providers and patients. At this point, we know little about whether providers in particular regions are more likely to be influenced by implicit bias than those in other geographic regions. Sampling of providers could be stratified by geographic location or specialty. Although this review focused on bias among various health care professionals from different specialties and levels of training and experience, future researchers may want to focus on specific groups of providers, such as those from a particular discipline, to investigate training and professional socialization related to implicit bias. In terms of sampling patients, researchers may stratify on the basis of geographic location or patient type. The influence of implicit bias may differ between patients experiencing only acute health problems and those struggling with chronic diseases, or between pediatric and adult patients. When patients are sampled, every effort must be made to extend beyond convenience sampling. Sampling practices should attempt to include all patients, not just those who are easy to reach or those who are nonintermittent patients—patients may stop or avoid care because of discriminatory experiences. In addition, although costly and perhaps difficult to obtain, large national samples would allow for more accurate prevalence estimates of implicit bias among US providers. Large sample sizes also provide more statistical power, which is needed for multilevel modeling, multivariate analyses, and the detection of small or moderate effects in terms of associations between variables and group differences.
A comprehensive understanding of the role of implicit bias in health care will require converging evidence using a wider variety of well-validated implicit measures. Although the research reviewed here relied almost exclusively on the IAT to assess implicit bias, this test is only one of several well-studied implicit assessments. Sequential priming tasks are another well-validated class of implicit measures, and meta-analytic comparisons show that the average association between priming tasks and behavior ( r = 0.28) 43 is similar to the meta-analytic association between the IAT and behavior ( r = 0.27). 67 Sequential priming tasks include evaluative priming, 12 lexical decision tasks, and the Affect Misattribution Procedure. 68 Of these, the Affect Misattribution Procedure displays the highest reliability (meta-analytic average Cronbach α = 0.81) 69 and associations with behavior (meta-analytic r = 0.35). 43 Because each type of measure has unique strengths and weaknesses, future research should employ a broader array of measures to avoid systematic biases in results.
Future studies should also expand the assessment of implicit bias. Although health disparities are particularly prominent among Black Americans, inequities also exist for other people of color, including American Indians, Asian Americans, and Hispanic/Latino/Latina Americans. Thus, future studies should examine levels of implicit bias among providers regarding these groups and whether bias contributes to health disparities. Researchers should also measure bias based on social identity characteristics in addition to race/ethnicity, such as age, gender, socioeconomic status, national origin, sexual orientation, gender identity, religious orientation, and disability status. Bias can exist on multiple social dimensions, and patients with multiple minority identities may be particularly affected. In addition, measuring various demographic characteristics among patients and providers would allow more advanced hypothesis testing. For example, a patient’s gender may moderate the relationship between a provider’s implicit racial/ethnic bias and quality of care, and providers in some specialties may have significantly higher levels of implicit bias than those in other areas (e.g., emergency medicine physicians vs pediatricians).
Finally, findings from this review indicate that we are at the fetal stage of understanding what represents the construct of implicit racial/ethnic bias, how it functions in health care, and what it influences. Theory can be useful as we move forward in this area. However, of the 15 studies reviewed, only 3 were informed explicitly by theory (e.g., aversive racism theory). 27,31,37 The predictive utility of a theory depends on whether it can be applied to distinguish underlying processes and their respective effects on outcomes. Although implicit attitudes may influence a range of outcomes in health care, very few studies examined the relationship between implicit bias and the end result of care—patient health. Our findings suggest that greater conceptual clarity is needed for interpreting existing differential effects of implicit bias on behavior and patient health outcomes, developing new theories, and designing future studies. New intervention research questions for future studies to consider are on the malleability of implicit bias and the mechanisms for regulating the effects on behavior that contribute to racial/ethnic inequities in health.
Acknowledgments
We were supported by a grant from the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health (grant no. 1R23EB018620-01 ). In addition, the first author was supported by the National Research Service Award Postdoctoral Traineeship from the National Institute of Mental Health sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, and the Department of Psychiatry and Behavioral Sciences, Duke University School of Medicine (grant no. T32 MH019117).
We also appreciate the support of the entire Envisioning Health research team: Mimi Chapman, Robert Colby, Tamera Coyne-Beasley, Steven Day, Geni Eng, William Hall, Janet Jarman, Kent Lee, Alexandra Lightfoot, John McGowan, Yesenia Merino, Xan McKnight, Rachele McFarland, Keith Payne, Florence Simán, Kari Thatcher, and Tainayah Thomas.
Human Participant Protection
No human participant protection was required because no human participants were involved in this study.

IMAGES
VIDEO
COMMENTS
DOI: 10.1056/NEJMp2201180. Implicit and explicit biases are among many factors that contribute to disparities in health and health care. 1 Explicit biases, the attitudes and assumptions that we ...
1. INTRODUCTION. Although expressions of explicit bias have declined in the United States over time, implicit bias has remained unrelenting. Health care providers hold negative explicit and implicit biases against many marginalized groups of people, including racial and ethnic minoritized populations, disabled populations, and gender and sexual minorities, among others (29, 63).
Introduction. Bias is the evaluation of something or someone that can be positive or negative, and implicit or unconscious bias is when the person is unaware of their evaluation. 1,2 It is negative implicit bias that is of particular concern within healthcare. Explicit bias, on the other hand, implies that there is awareness that an evaluation is taking place.
Discussion. The evidence indicates that healthcare professionals exhibit the same levels of implicit bias as the wider population. The interactions between multiple patient characteristics and between healthcare professional and patient characteristics reveal the complexity of the phenomenon of implicit bias and its influence on clinician-patient interaction.
Patients from underrepresented groups in the United States can experience the effects of unintentional cognitive (unconscious) biases that derive from cultural stereotypes in ways that perpetuate health inequities. Unconscious bias can also affect healthcare professionals in many ways, including patient-clinician interactions, hiring and ...
Implicit bias, a phrase that is not unique to healthcare, refers to the unconscious prejudice individuals might feel about another thing, group, or person. According to the Kirwan Institute for the Study of Race and Ethnicity at the Ohio State University, implicit bias is involuntary, can refer to positive or negative attitudes and stereotypes ...
Studies show that health care professionals have the same level of implicit bias as the general population and that higher levels are associated with lower quality care. 5 Providers with higher ...
Implicit biases involve associations outside conscious awareness that lead to a negative evaluation of a person on the basis of irrelevant characteristics such as race or gender. This review examines the evidence that healthcare professionals display implicit biases towards patients. PubMed, PsychINFO, PsychARTICLE and CINAHL were searched for peer-reviewed articles published between 1st March ...
Psychologists and others are now building on the IoM findings by exploring how specific factors, including physicians' use of patronizing language and patients' past experiences with discrimination, affect patients' perception of providers and care. Research is also starting to look at how implicit bias affects the dynamics of physician ...
This review examines the evidence that healthcare professionals display implicit biases towards patients. Methods: PubMed, PsychINFO, PsychARTICLE and CINAHL were searched for peer-reviewed articles published between 1st March 2003 and 31st March 2013. Two reviewers assessed the eligibility of the identified papers based on precise content and ...
An implicit bias is an unconscious association, belief, or attitude toward any social group. Implicit biases are one reason why people often attribute certain qualities or characteristics to all members of a particular group, a phenomenon known as stereotyping. It is important to remember that implicit biases operate almost entirely on an ...
The concept of implicit bias, also termed unconscious bias, and the related Implicit Association Test (IAT) rests on the belief that people act on the basis of internalised schemas of which they are unaware and thus can, and often do, engage in discriminatory behaviours without conscious intent.1 This idea increasingly features in public discourse and scholarly inquiry with regard to ...
In addition to structural racism, implicit bias—defined as unconscious attitudes, positive or negative, toward a person, group, or idea—often leads to differential treatment based on perceived race. 2, 3 Implicit bias further restricts quality healthcare as a separate factor above and beyond inequities of structural racism.
A 2015 systematic review showed that low to moderate levels of implicit racial or ethnic bias were found among healthcare professionals in all but one of 15 studies.3 The results also showed that implicit bias was "significantly related to patient-provider interactions, treatment decisions, treatment adherence, and patient health outcomes."
Quick Safety 23: Implicit bias in health care. "Of all forms of inequity, injustice in health care is the most shocking and inhuman.". — Martin Luther King, Jr., National Convention of the Medical Committee for Human Rights, Chicago, 1966. On the eve of the 15th anniversary of two seminal reports from the Institute of Medicine (IOM ...
The Health Care Institution, Population Health and Black Lives. Journal of the National Medical Association, May 2016. Sreshta, Nina, et al. The Social Justice Coalition of the Cambridge Health Alliance: An open letter to our patients in the Trump era. Saadi, Altaf: A Muslim-American doctor on the racism in our hospitals. Gupta, Renuka. Slaves.
Racial bias happens when attitudes and judgments toward people because of their race affect personal thoughts, decisions, and behaviors. Whether implicit or otherwise, racial bias is evident in ...
Context Implicit bias affects health professionals' clinical decision-making; nevertheless, published reports of medical education curricula exploring this concept have been limited. This research documents a recent approach to teaching implicit bias. Methods Medical students matriculating during 2014 and 2015 participated in a determinants of health course including instruction about ...
On-line training (reading essay, survey, open- ended questions) Qualitative descriptive analysis/none: New insights (attitudes and behaviors that sustain racism) ... Integration of implicit bias training into health professional education: Training guide/none: Self awareness, understand how bias affects healthcare: FitzGerald et al. (2019)
Implicit bias is an unconscious preference for (or aversion to) a particular person or group. Although these feelings can be either positive or negative, they cause us to be unfair towards others. Affinity bias or the tendency to favor people who are similar to us, is an example of this unfair behaviour. However, any aspect of an individual's ...
An Implicit Healthcare Bias A lifetime of communication and experiences shapes our society's views and judgements of others throughout so many aspects of our lives. Women have h ... This essay should not be treated as an authoritative source of information when forming medical opinions as information may be inaccurate or out-of-date.
The goal was to collect racial data to help address health disparities. The unintended effect was the introduction of race in medical decision-making tools. ... This is Part 2 of Embedded Bias ...
HEALTH DISPARITIES AND PROVIDER ATTITUDES. Provider attitudes and behavior are a target area for researchers and practitioners attempting to understand and eradicate inequitable health care. 7 Although overt discriminatory behavior in the United States may have declined in recent decades, covert discrimination and institutional bias are sustained by subtle, implicit attitudes that may ...
The Future of AI in Healthcare: Striving for Equity. As AI continues to integrate into healthcare systems, addressing and mitigating bias becomes increasingly important to ensure equitable care for all individuals. Achieving this requires a concerted effort from developers, healthcare providers, policymakers, and communities.